world cancer report - iarc
world cancer report - iarc
world cancer report - iarc
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
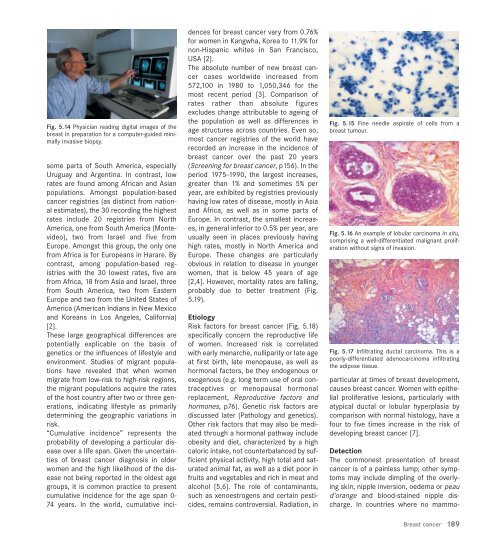
Fig. 5.14 Physician reading digital images of the<br />
breast in preparation for a computer-guided minimally<br />
invasive biopsy.<br />
some parts of South America, especially<br />
Uruguay and Argentina. In contrast, low<br />
rates are found among African and Asian<br />
populations. Amongst population-based<br />
<strong>cancer</strong> registries (as distinct from national<br />
estimates), the 30 recording the highest<br />
rates include 20 registries from North<br />
America, one from South America (Montevideo),<br />
two from Israel and five from<br />
Europe. Amongst this group, the only one<br />
from Africa is for Europeans in Harare. By<br />
contrast, among population-based registries<br />
with the 30 lowest rates, five are<br />
from Africa, 18 from Asia and Israel, three<br />
from South America, two from Eastern<br />
Europe and two from the United States of<br />
America (American Indians in New Mexico<br />
and Koreans in Los Angeles, California)<br />
[2].<br />
These large geographical differences are<br />
potentially explicable on the basis of<br />
genetics or the influences of lifestyle and<br />
environment. Studies of migrant populations<br />
have revealed that when women<br />
migrate from low-risk to high-risk regions,<br />
the migrant populations acquire the rates<br />
of the host country after two or three generations,<br />
indicating lifestyle as primarily<br />
determining the geographic variations in<br />
risk.<br />
“Cumulative incidence” represents the<br />
probability of developing a particular disease<br />
over a life span. Given the uncertainties<br />
of breast <strong>cancer</strong> diagnosis in older<br />
women and the high likelihood of the disease<br />
not being <strong>report</strong>ed in the oldest age<br />
groups, it is common practice to present<br />
cumulative incidence for the age span 0-<br />
74 years. In the <strong>world</strong>, cumulative inci-<br />
dences for breast <strong>cancer</strong> vary from 0.76%<br />
for women in Kangwha, Korea to 11.9% for<br />
non-Hispanic whites in San Francisco,<br />
USA [2].<br />
The absolute number of new breast <strong>cancer</strong><br />
cases <strong>world</strong>wide increased from<br />
572,100 in 1980 to 1,050,346 for the<br />
most recent period [3]. Comparison of<br />
rates rather than absolute figures<br />
excludes change attributable to ageing of<br />
the population as well as differences in<br />
age structures across countries. Even so,<br />
most <strong>cancer</strong> registries of the <strong>world</strong> have<br />
recorded an increase in the incidence of<br />
breast <strong>cancer</strong> over the past 20 years<br />
(Screening for breast <strong>cancer</strong>, p156). In the<br />
period 1975-1990, the largest increases,<br />
greater than 1% and sometimes 5% per<br />
year, are exhibited by registries previously<br />
having low rates of disease, mostly in Asia<br />
and Africa, as well as in some parts of<br />
Europe. In contrast, the smallest increases,<br />
in general inferior to 0.5% per year, are<br />
usually seen in places previously having<br />
high rates, mostly in North America and<br />
Europe. These changes are particularly<br />
obvious in relation to disease in younger<br />
women, that is below 45 years of age<br />
[2,4]. However, mortality rates are falling,<br />
probably due to better treatment (Fig.<br />
5.19).<br />
Etiology<br />
Risk factors for breast <strong>cancer</strong> (Fig. 5.18)<br />
specifically concern the reproductive life<br />
of women. Increased risk is correlated<br />
with early menarche, nulliparity or late age<br />
at first birth, late menopause, as well as<br />
hormonal factors, be they endogenous or<br />
exogenous (e.g. long term use of oral contraceptives<br />
or menopausal hormonal<br />
replacement, Reproductive factors and<br />
hormones, p76). Genetic risk factors are<br />
discussed later (Pathology and genetics).<br />
Other risk factors that may also be mediated<br />
through a hormonal pathway include<br />
obesity and diet, characterized by a high<br />
caloric intake, not counterbalanced by sufficient<br />
physical activity, high total and saturated<br />
animal fat, as well as a diet poor in<br />
fruits and vegetables and rich in meat and<br />
alcohol [5,6]. The role of contaminants,<br />
such as xenoestrogens and certain pesticides,<br />
remains controversial. Radiation, in<br />
Fig. 5.15 Fine needle aspirate of cells from a<br />
breast tumour.<br />
Fig. 5.16 An example of lobular carcinoma in situ,<br />
comprising a well-differentiated malignant proliferation<br />
without signs of invasion.<br />
Fig. 5.17 Infiltrating ductal carcinoma. This is a<br />
poorly-differentiated adenocarcinoma infiltrating<br />
the adipose tissue.<br />
particular at times of breast development,<br />
causes breast <strong>cancer</strong>. Women with epithelial<br />
proliferative lesions, particularly with<br />
atypical ductal or lobular hyperplasia by<br />
comparison with normal histology, have a<br />
four to five times increase in the risk of<br />
developing breast <strong>cancer</strong> [7].<br />
Detection<br />
The commonest presentation of breast<br />
<strong>cancer</strong> is of a painless lump; other symptoms<br />
may include dimpling of the overlying<br />
skin, nipple inversion, oedema or peau<br />
d’orange and blood-stained nipple discharge.<br />
In countries where no mammo-<br />
Breast <strong>cancer</strong><br />
189