- Page 1 and 2:
October 2006 EPA/600/R-05/144bF Air
- Page 3 and 4:
PREFACE National Ambient Air Qualit
- Page 5 and 6:
NCEA acknowledges the valuable cont
- Page 7 and 8:
Table of Contents Page PREFACE ....
- Page 9 and 10:
Authors, Contributors, and Reviewer
- Page 11 and 12:
Contributors and Reviewers (cont’
- Page 13 and 14:
Contributors and Reviewers (cont’
- Page 15 and 16:
Executive Direction U.S. Environmen
- Page 17 and 18:
Chair U.S. Environmental Protection
- Page 19 and 20:
Abbreviations and Acronyms αFGF α
- Page 21 and 22:
BLL blood lead level BLM biotic lig
- Page 23 and 24:
CRI chronic renal insufficiency CSF
- Page 25 and 26:
EPT macroinvertebrates from the Eph
- Page 27 and 28:
GRP78 glucose-regulated protein 78
- Page 29 and 30:
KABC Kaufman Assessment Battery for
- Page 31 and 32:
NADP nicotinamide adenine dinucleot
- Page 33 and 34:
Pb(Ac)2 lead acetate PbB blood lead
- Page 35 and 36:
RR RT RSEM RSUC RT ∑SEM SA7 SAB S
- Page 37 and 38:
TGF transforming growth factor TH t
- Page 39 and 40:
AX4. CHAPTER 4 ANNEX ANNEX TABLES A
- Page 41 and 42:
AX4-3 Table AX4-1 (cont’d). Analy
- Page 43 and 44:
AX4-5 Table AX4-2 (cont’d). Summa
- Page 45 and 46:
AX4-7 Table AX4-3. Bone Lead Measur
- Page 47 and 48:
AX4-9 Reference, Study Location, an
- Page 49 and 50:
AX4-11 Table AX4-4 (cont’d). Bone
- Page 51 and 52:
AX4-13 Table AX4-5 (cont’d). Bone
- Page 53 and 54:
AX4-15 Table AX4-5 (cont’d). Bone
- Page 55 and 56:
AX4-17 Table AX4-5 (cont’d). Bone
- Page 57 and 58:
AX4-19 Reference, Study Location, a
- Page 59 and 60:
AX4-21 Reference, Study Location, a
- Page 61 and 62:
AX4-23 Reference, Study Location, a
- Page 63 and 64:
AX4-25 Reference, Study Location, a
- Page 65 and 66:
AX4-27 Reference, Study Location, a
- Page 67 and 68:
AX4-29 Reference, Study Location, a
- Page 69 and 70:
AX4-31 Table AX4-8 (cont’d). Bone
- Page 71 and 72:
AX4-33 Table AX4-8 (cont’d). Bone
- Page 73 and 74:
AX4-35 Table AX4-8 (cont’d). Bone
- Page 75 and 76:
AX4-37 Table AX4-9 (cont’d). Lead
- Page 77 and 78:
AX4-39 Table AX4-11. Summary of Sel
- Page 79 and 80:
AX4-41 Table AX4-11 (cont’d). Sum
- Page 81 and 82:
AX-43 Table AX4-12 (cont’d). Summ
- Page 83 and 84:
Barltrop, D.; Meek, F. (1979) Effec
- Page 85 and 86:
Carroll, R. J.; Galindo, C. D. (199
- Page 87 and 88:
Flegal, A. R.; Smith, D. R. (1995)
- Page 89 and 90:
Gulson, B.; Mizon, K.; Smith, H.; E
- Page 91 and 92:
Khoury, G. A.; Diamond, G. L. (2003
- Page 93 and 94:
Morgan, W. D.; Ryde, S. J.; Jones,
- Page 95 and 96:
Pounds, J. G.; Leggett, R. W. (1998
- Page 97 and 98:
Skerfving, S. (1988) Biological mon
- Page 99 and 100:
U.S. Environmental Protection Agenc
- Page 101 and 102:
Air Quality Criteria for Lead Volum
- Page 103 and 104:
AQCD/Addendum and 1990 Supplement,
- Page 105 and 106:
Air Quality Criteria for Lead (Seco
- Page 107 and 108:
List of Tables AX4-1 Analytical Met
- Page 109 and 110:
List of Tables (cont’d) AX5-6.3 G
- Page 111 and 112:
List of Tables (cont’d) AX5-9.3 S
- Page 113 and 114:
Principal Authors (cont’d) Author
- Page 115 and 116:
Principal Authors Authors, Contribu
- Page 117 and 118:
Principle Authors (cont’d) Author
- Page 119 and 120:
Technical Support Staff U.S. Enviro
- Page 121 and 122:
Members (cont’d) U.S. Environment
- Page 123 and 124:
ANP atrial natriuretic peptide AP a
- Page 125 and 126:
CCE Coordination Center for Effects
- Page 127 and 128:
DR drinking water DSA delayed spati
- Page 129 and 130:
FTII Fagan Test of Infant Intellige
- Page 131 and 132:
H3PO4 phosphoric acid HPRT hypoxant
- Page 133 and 134:
MATC maximum acceptable threshold c
- Page 135 and 136:
NOS nitric oxide synthase; not othe
- Page 137 and 138:
PPVT-R Peabody Picture Vocabulary T
- Page 139 and 140:
SOPR sperm-oocyte penetration rate
- Page 141 and 142:
vit C vitamin C vit E vitamin E VMA
- Page 143 and 144:
AX5-2 Table AX5-2.1. Effect of Lead
- Page 145 and 146:
AX5-4 Table AX5-2.1 (cont’d). Eff
- Page 147 and 148:
AX5-6 Table AX5-2.2. Lead, Erythroc
- Page 149 and 150:
AX5-8 Table AX5-2.2 (cont’d). Lea
- Page 151 and 152:
AX5-10 Table AX5-2.4. Lead Effects
- Page 153 and 154:
AX5-12 Table AX5-2.5. Lead Interact
- Page 155 and 156:
AX5-14 Table AX5-2.7. Lead, Erythro
- Page 157 and 158:
AX5-16 Subject Exposure Protocol Ra
- Page 159 and 160:
AX5-18 Subject Exposure Protocol Ra
- Page 161 and 162:
AX5-20 Subject Exposure Protocol Ra
- Page 163 and 164:
AX5-22 Subject Rat, female, 22 wks
- Page 165 and 166:
AX5-24 Subject Rat, F344, male Expo
- Page 167 and 168:
AX5-26 Subject Monkey, cynomolgus,
- Page 169 and 170:
AX5-28 Subject Rat, SD, male, PND 6
- Page 171 and 172:
AX5-30 Subject Monkey, cynomolgus,
- Page 173 and 174:
AX5-32 Subject Exposure Protocol Ta
- Page 175 and 176:
AX5-34 Table AX5-3.6 (cont’d). Ke
- Page 177 and 178:
AX5-36 Table AX5-3.6 (cont’d). Ke
- Page 179 and 180:
AX5-38 Citation Al-Hakkak et al. (1
- Page 181 and 182:
AX5-40 Citation Fox et al. (1997)
- Page 183 and 184:
AX5-42 Citation Pinon- Lataillade e
- Page 185 and 186:
AX5-44 Citation Wiebe et al. (1998)
- Page 187 and 188:
AX5-46 Citation Chowdhuri et al. (2
- Page 189 and 190:
AX5-48 Citation Graca et al. (2004)
- Page 191 and 192:
AX5-50 Citation Marchlewicz et al.
- Page 193 and 194:
AX5-52 Table AX5-4.2 (cont’d). Ef
- Page 195 and 196:
AX5-54 Citation Sokol et al. (1985)
- Page 197 and 198:
AX5-56 Citation Table AX5-4.3 (cont
- Page 199 and 200:
AX5-58 Citation Priya et al. (2004)
- Page 201 and 202:
ANNEX TABLES AX5-5 AX5-60
- Page 203 and 204:
AX5-62 Table AX5-5.1 (cont’d). In
- Page 205 and 206:
AX5-64 Table AX5-5.1 (cont’d). In
- Page 207 and 208:
AX5-66 Reference Watts et al. (1995
- Page 209 and 210:
AX5-68 Reference Lai et al. (2002)
- Page 211 and 212:
AX5-70 Reference Shelkovnikov and G
- Page 213 and 214:
AX5-72 Reference Fujiwara and Kaji
- Page 215 and 216:
AX5-74 Reference Fugiwara et al. (1
- Page 217 and 218:
AX5-76 Table AX5-6.1. Genotoxic/Car
- Page 219 and 220:
AX5-78 Table AX5-6.2. Genotoxic/Car
- Page 221 and 222:
AX5-80 Table AX5-6.3 (cont’d). Ge
- Page 223 and 224:
AX5-82 Table AX5-6.4 (cont’d). Ge
- Page 225 and 226:
AX5-84 Table AX5-6.4 (cont’d). Ge
- Page 227 and 228:
AX5-86 Compound Table AX5-6.6. Geno
- Page 229 and 230:
AX5-88 Compound Table AX5-6.7. Geno
- Page 231 and 232:
AX5-90 Table AX5-6.8. Genotoxic/Car
- Page 233 and 234:
AX5-92 Compound Table AX5-6.9. Geno
- Page 235 and 236:
AX5-94 Table AX5-6.9 (cont’d). Ge
- Page 237 and 238:
AX5-96 Table AX5-6.10 (cont’d). G
- Page 239 and 240:
AX5-98 Table AX5-6.12. Genotoxic/Ca
- Page 241 and 242:
AX5-100 Table AX5-6.14. Genotoxic/C
- Page 243 and 244:
AX5-102 Compound Table AX5-6.16. Ge
- Page 245 and 246:
AX5-104 Table AX5-6.18. Genotoxic/C
- Page 247 and 248:
AX5-106 Table AX5-6.18 (cont’d).
- Page 249 and 250:
AX5-108 Table AX5-6.19 (cont’d).
- Page 251 and 252:
AX5-110 Compound Assay (Concentrati
- Page 253 and 254:
AX5-112 Table AX5-7.1. Light Micros
- Page 255 and 256:
AX5-114 Table AX5-7.2. Lead and Fre
- Page 257 and 258:
AX5-116 Table AX5-7.2 (cont’d). L
- Page 259 and 260:
AX5-118 Table AX5-7.4. Effect of Ch
- Page 261 and 262:
AX5-120 Table AX5-7.5 (cont’d). E
- Page 263 and 264:
AX5-122 Table AX5-8.1. Bone Growth
- Page 265 and 266:
AX5-124 Table AX5-8.1 (cont’d). B
- Page 267 and 268:
AX5-126 Table AX5-8.2. Regulation o
- Page 269 and 270:
AX5-128 Table AX5-8.2 (cont’d). R
- Page 271 and 272:
AX5-130 Table AX5-8.3 (cont’d). B
- Page 273 and 274:
AX5-132 Table AX5-8.3 (cont’d). B
- Page 275 and 276:
AX5-134 Table AX5-8.3 (cont’d). B
- Page 277 and 278:
AX5-136 Table AX5-8.4. Bone Lead as
- Page 279 and 280:
AX5-138 Table AX5-8.4 (cont’d). B
- Page 281 and 282:
AX5-140 Table AX5-8.4 (cont’d). B
- Page 283 and 284:
AX5-142 Table AX5-8.5. Uptake of Le
- Page 285 and 286:
AX5-144 Table AX5-8.7. Effects of L
- Page 287 and 288:
ANNEX TABLES AX5-9 AX5-146
- Page 289 and 290:
AX5-148 Nature of Exposure Table AX
- Page 291 and 292:
AX5-150 Table AX5-9.2. Effect of Le
- Page 293 and 294:
AX5-152 Species Strain/Gender Age M
- Page 295 and 296:
AX5-154 Table AX5-9.5 (cont’d). E
- Page 297 and 298:
ANNEX TABLES AX5-10 AX5-156
- Page 299 and 300:
AX5-158 Table AX5-10.1 (cont’d).
- Page 301 and 302:
AX5-160 Table AX5-10.1 (cont’d).
- Page 303 and 304:
AX5-162 Table AX5-10.2. Biochemical
- Page 305 and 306:
AX5-164 Table AX5-10.2 (cont’d).
- Page 307 and 308:
AX5-166 Table AX5-10.4. Lead, Oxida
- Page 309 and 310:
AX5-168 Table AX5-10.4 (cont’d).
- Page 311 and 312:
AX5-170 Table AX5-10.4 (cont’d).
- Page 313 and 314:
AX5-172 Table AX5-10.5 (cont’d).
- Page 315 and 316:
AX5-174 Table AX5-10.5 (cont’d).
- Page 317 and 318:
AX5-176 Table AX5-10.5 (cont’d).
- Page 319 and 320:
AX5-178 Table AX5-10.6 (cont’d).
- Page 321 and 322:
AX5-180 Table AX5-10.7. Lead and In
- Page 323 and 324:
AX5-182 Table AX5-10.8 (cont’d).
- Page 325 and 326:
AX5-184 Table AX5-10.9. Lead, Calci
- Page 327 and 328:
ANNEX TABLES AX5-11 AX5-186
- Page 329 and 330:
AX5-188 Source Organ Species Table
- Page 331 and 332:
REFERENCES Abdollahi, M.; Dehpour,
- Page 333 and 334:
Bataineh, H.; Al-Hamood, M. H.; Elb
- Page 335 and 336:
Buchet, J.-P.; Roels, H. E.; Huberm
- Page 337 and 338:
Cline, H. T.; Witte, S.; Jones, K.
- Page 339 and 340:
Cory-Slechta, D. A.; McCoy, L.; Ric
- Page 341 and 342:
children's health: immune and respi
- Page 343 and 344:
Ferguson, C.; Kern, M.; Audesirk, G
- Page 345 and 346:
Fullmer, C. S. (1991) Intestinal ca
- Page 347 and 348:
Goyer, R. A.; Leonard, D. L.; Moore
- Page 349 and 350:
Hengstler, J. G.; Bolm-Audorff, U.;
- Page 351 and 352:
Jacquet, P.; Leonard, A.; Gerber, G
- Page 353 and 354:
Kim, K. A.; Chakraborti, T.; Goldst
- Page 355 and 356:
Laughlin, N. K.; Bowman, R. E.; Fra
- Page 357 and 358:
Maldonado-Vega, M.; Cerbón-Solórz
- Page 359 and 360:
Moorman, W. J.; Skaggs, S. R.; Clar
- Page 361 and 362:
O'Flaherty, E. J.; Inskip, M. J.; F
- Page 363 and 364:
Price, R. G.; Taylor, S. A.; Chiver
- Page 365 and 366:
Rodamilans, M.; Mtz.-Osaba, M. J.;
- Page 367 and 368:
Schlipkoter, H.-W.; Frieler, L. (19
- Page 369 and 370:
Skoczyńska, A.; Smolik, R.; Jeleń
- Page 371 and 372:
Tavakoli-Nezhad, M.; Pitts, D. K. (
- Page 373 and 374:
Valentino, M.; Governa, M.; Marchis
- Page 375 and 376:
Wetmur, J. G.; Lehnert, G.; Desnick
- Page 377 and 378:
Zhou, J.; Xu, Y.-H.; Chang, H.-F. (
- Page 379 and 380:
Air Quality Criteria for Lead Volum
- Page 381 and 382:
The purpose of this revised Lead AQ
- Page 383 and 384:
Air Quality Criteria for Lead (Seco
- Page 385 and 386:
List of Tables Number Page AX6-2.1
- Page 387 and 388:
List of Tables (cont’d) Number Pa
- Page 389 and 390:
Principal Authors Authors, Contribu
- Page 391 and 392:
Principal Authors Authors, Contribu
- Page 393 and 394:
Principle Authors (cont’d) Author
- Page 395 and 396:
Technical Support Staff U.S. Enviro
- Page 397 and 398:
Members (cont’d) U.S. Environment
- Page 399 and 400:
ANOVA analysis of variance ANP atri
- Page 401 and 402:
CCD charge-coupled device CCE Coord
- Page 403 and 404:
DPPD N-N-diphenyl-p-phynylene-diami
- Page 405 and 406:
FTES free testosterone FTII Fagan T
- Page 407 and 408:
HPLC high-pressure liquid chromatog
- Page 409 and 410:
MAO monoamine oxidase MATC maximum
- Page 411 and 412:
NORs nucleolar organizing regions N
- Page 413 and 414:
ppm parts per million PPVT-R Peabod
- Page 415 and 416:
SOPR sperm-oocyte penetration rate
- Page 417 and 418:
vit C vitamin C vit E vitamin E VMA
- Page 419 and 420:
ANNEX TABLES AX6-2 AX6-2
- Page 421 and 422:
AX6-4 Table AX6-2.1 (cont’d). Pro
- Page 423 and 424:
AX6-6 Table AX6-2.1 (cont’d). Pro
- Page 425 and 426:
AX6-8 Table AX6-2.1 (cont’d). Pro
- Page 427 and 428:
AX6-10 Table AX6-2.2 (cont’d). Me
- Page 429 and 430:
AX6-12 Table AX6-2.3 (cont’d). Cr
- Page 431 and 432:
AX6-14 Table AX6-2.4. Effects of Le
- Page 433 and 434:
AX6-16 Table AX6-2.4 (cont’d). Ef
- Page 435 and 436:
AX6-18 Table AX6-2.5 (cont’d). Ef
- Page 437 and 438:
AX6-20 Table AX6-2.6 (cont’d). Ef
- Page 439 and 440:
AX6-22 Table AX6-2.6 (cont’d). Ef
- Page 441 and 442:
AX6-24 Table AX6-2.8. Effects of Le
- Page 443 and 444:
AX6-26 Table AX6-2.9 (cont’d). Ef
- Page 445 and 446:
AX6-28 Table AX6-2.10 (cont’d). R
- Page 447 and 448:
AX6-30 Table AX6-3.1. Neurobehavior
- Page 449 and 450:
AX6-32 Table AX6-3.1 (cont’d). Ne
- Page 451 and 452:
AX6-34 Table AX6-3.2 (cont’d). Sy
- Page 453 and 454:
AX6-36 Table AX6-3.3. Neurobehavior
- Page 455 and 456:
AX6-38 Table AX6-3.3 (cont’d). Ne
- Page 457 and 458:
AX6-40 Table AX6-3.3 (cont’d). Ne
- Page 459 and 460:
AX6-42 Table AX6-3.3 (cont’d). Ne
- Page 461 and 462:
AX6-44 Table AX6-3.3 (cont’d). Ne
- Page 463 and 464:
AX6-46 Table AX6-3.3 (cont’d). Ne
- Page 465 and 466:
AX6-48 Table AX6-3.3 (cont’d). Ne
- Page 467 and 468:
AX6-50 Table AX6-3.4 (cont’d). Me
- Page 469 and 470:
AX6-52 Table AX6-3.5 (cont’d). Ne
- Page 471 and 472:
AX6-54 Table AX6-3.5 (cont’d). Ne
- Page 473 and 474:
AX6-56 Table AX6-3.6. Evoked Potent
- Page 475 and 476:
AX6-58 Table AX6-3.6 (cont’d). Ev
- Page 477 and 478:
AX6-60 Table AX6-3.7 (cont’d). Po
- Page 479 and 480:
AX6-62 Table AX6-3.7 (cont’d). Po
- Page 481 and 482:
AX6-64 Table AX6-3.8 (cont’d). Oc
- Page 483 and 484:
AX6-66 Table AX6-3.9. Other Neurolo
- Page 485 and 486:
AX6-68 Table AX6-3.9 (cont’d). Ot
- Page 487 and 488:
AX6-70 Table AX6-4.1. Renal Effects
- Page 489 and 490:
AX6-72 Table AX6-4.1 (cont’d). Re
- Page 491 and 492:
AX6-74 Table AX6-4.1 (cont’d). Re
- Page 493 and 494:
AX6-76 Table AX6-4.1 (cont’d). Re
- Page 495 and 496:
AX6-78 Table AX6-4.1 (cont’d). Re
- Page 497 and 498:
AX6-80 Table AX6-4.1 (cont’d). Re
- Page 499 and 500:
AX6-82 Table AX6-4.2 (cont’d). Re
- Page 501 and 502:
AX6-84 Table AX6-4.2 (cont’d). Re
- Page 503 and 504:
AX6-86 Table AX6-4.2 (cont’d). Re
- Page 505 and 506: AX6-88 Table AX6-4.2 (cont’d). Re
- Page 507 and 508: AX6-90 Table AX6-4.2 (cont’d). Re
- Page 509 and 510: AX6-92 Table AX6-4.2 (cont’d). Re
- Page 511 and 512: AX6-94 Table AX6-4.2 (cont’d). Re
- Page 513 and 514: AX6-96 Table AX6-4.2 (cont’d). Re
- Page 515 and 516: AX6-98 Table AX6-4.2 (cont’d). Re
- Page 517 and 518: AX6-100 Table AX6-4.2 (cont’d). R
- Page 519 and 520: AX6-102 Table AX6-4.2 (cont’d). R
- Page 521 and 522: AX6-104 Table AX6-4.3. Renal Effect
- Page 523 and 524: AX6-106 Table AX6-4.3 (cont’d). R
- Page 525 and 526: AX6-108 Table AX6-4.3 (cont’d). R
- Page 527 and 528: AX6-110 Table AX6-4.3 (cont’d). R
- Page 529 and 530: AX6-112 Table AX6-4.3 (cont’d). R
- Page 531 and 532: AX6-114 Table AX6-4.3 (cont’d). R
- Page 533 and 534: AX6-116 Table AX6-4.3 (cont’d). R
- Page 535 and 536: AX6-118 Table AX6-4.3 (cont’d). R
- Page 537 and 538: AX6-120 Table AX6-4.4. Renal Effect
- Page 539 and 540: AX6-122 Table AX6-4.5. Renal Effect
- Page 541 and 542: AX6-124 Table AX6-4.5 (cont’d). R
- Page 543 and 544: AX6-126 Table AX6-4.5 (cont’d). R
- Page 545 and 546: AX6-128 Table AX6-4.5 (cont’d). R
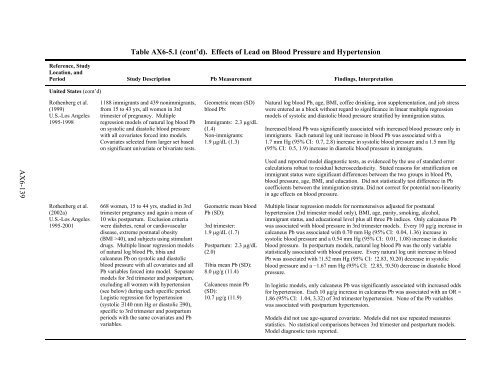
- Page 547 and 548: AX6-130 Table AX6-5.1. Effects of L
- Page 549 and 550: AX6-132 Table AX6-5.1 (cont’d). E
- Page 551 and 552: AX6-134 Table AX6-5.1 (cont’d). E
- Page 553 and 554: AX6-136 Table AX6-5.1 (cont’d). E
- Page 555: AX6-138 Table AX6-5.1 (cont’d). E
- Page 559 and 560: AX6-142 Table AX6-5.1 (cont’d). E
- Page 561 and 562: AX6-144 Table AX6-5.1 (cont’d). E
- Page 563 and 564: AX6-146 Table AX6-5.1 (cont’d). E
- Page 565 and 566: AX6-148 Table AX6-5.1 (cont’d). E
- Page 567 and 568: AX6-150 Table AX6-5.1 (cont’d). E
- Page 569 and 570: AX6-152 Table AX6-5.1 (cont’d). E
- Page 571 and 572: AX6-154 Table AX6-5.1 (cont’d). E
- Page 573 and 574: AX6-156 Table AX6-5.1 (cont’d). E
- Page 575 and 576: AX6-158 Table AX6-5.1 (cont’d). E
- Page 577 and 578: AX6-160 Table AX6-5.2 (cont’d). E
- Page 579 and 580: AX6-162 Table AX6-5.3. Effects of L
- Page 581 and 582: AX6-164 Table AX6-5.3 (cont’d). E
- Page 583 and 584: AX6-166 Table AX6-5.4. Cardiovascul
- Page 585 and 586: ANNEX TABLES AX6-6 AX6-168
- Page 587 and 588: AX6-170 Table AX6-6.1 (cont’d). P
- Page 589 and 590: AX172 Table AX6-6.1 (cont’d). Pla
- Page 591 and 592: AX6-174 Table AX6-6.2. Lead Exposur
- Page 593 and 594: AX6-176 Table AX6-6.2 (cont’d). L
- Page 595 and 596: AX6-178 Table AX6-6.3. Lead Exposur
- Page 597 and 598: AX6-180 Table AX6-6.4. Lead Exposur
- Page 599 and 600: ANNEX TABLES AX6-7 AX6-182
- Page 601 and 602: AX6-184 Table AX6-7.1 (cont’d). R
- Page 603 and 604: AX6-186 Table AX6-7.2. Key Occupati
- Page 605 and 606: AX6-188 Table AX6-7.2 (cont’d). K
- Page 607 and 608:
AX6-190 Table AX6-7.2 (cont’d). K
- Page 609 and 610:
AX6-192 Table AX6-7.3. Key Studies
- Page 611 and 612:
AX6-194 Table AX6-7.4. Other Studie
- Page 613 and 614:
AX6-196 Table AX6-7.4 (cont’d). O
- Page 615 and 616:
AX6-198 Table AX6-7.4 (cont’d). O
- Page 617 and 618:
AX6-200 Table AX6-7.4 (cont’d). O
- Page 619 and 620:
AX6-202 Table AX6-7.4 (cont’d). O
- Page 621 and 622:
AX6-204 Table AX6-7.4 (cont’d). O
- Page 623 and 624:
ANNEX TABLES AX6-8 AX6-206
- Page 625 and 626:
AX6-208 Table AX6-8.1 (cont’d). E
- Page 627 and 628:
AX6-210 Table AX6-8.1 (cont’d). E
- Page 629 and 630:
AX6-212 Table AX6-8.2 (cont’d). E
- Page 631 and 632:
AX6-214 Table AX6-8.2 (cont’d). E
- Page 633 and 634:
AX6-216 Table AX6-8.2 (cont’d). E
- Page 635 and 636:
AX6-218 Table AX6-8.2 (cont’d). E
- Page 637 and 638:
ANNEX TABLES AX6-9 AX6-220
- Page 639 and 640:
AX6-222 Table AX6-9.1 (cont’d). E
- Page 641 and 642:
AX6-224 Table 6-9.2 (cont’d). Eff
- Page 643 and 644:
AX6-226 Table 6-9.2 (cont’d). Eff
- Page 645 and 646:
AX6-228 Table 6-9.2 (cont’d). Eff
- Page 647 and 648:
AX6-230 Table 6-9.2 (cont’d). Eff
- Page 649 and 650:
AX6-232 Table AX6-9.3 (cont’d.).
- Page 651 and 652:
AX6-234 Table AX6-9.4. Effects of L
- Page 653 and 654:
AX6-236 Table AX6-9.4 (cont’d). E
- Page 655 and 656:
AX6-238 Table AX6-9.4 (cont’d). E
- Page 657 and 658:
AX6-240 Table AX6-9.4 (cont’d). E
- Page 659 and 660:
AX6-242 Table AX6-9.5 (cont’d). E
- Page 661 and 662:
AX6-244 Table AX6-9.6 (cont’d). E
- Page 663 and 664:
AX6-246 Table AX6-9.6 (cont’d). E
- Page 665 and 666:
AX6-248 Table AX6-9.6 (cont’d). E
- Page 667 and 668:
AX6-250 Table AX6-9.6 (cont’d). E
- Page 669 and 670:
AX6-252 Table AX6-9.7 (cont’d). E
- Page 671 and 672:
AX6-254 Table AX6-9.8 (cont’d). E
- Page 673 and 674:
AX6-256 Table AX6-9.9 (cont’d). E
- Page 675 and 676:
AX6-258 Table AX6-9.10. Effects of
- Page 677 and 678:
REFERENCES Abbate, C.; Buceti, R.;
- Page 679 and 680:
Baghurst, P. A.; McMichael, A. J.;
- Page 681 and 682:
Bolla, K. I.; Schwartz, B. S.; Stew
- Page 683 and 684:
Chia, K. S.; Jeyaratnam, J.; Tan, C
- Page 685 and 686:
David, O. J.; Clark, J.; Hoffman, S
- Page 687 and 688:
Englyst, V.; Lundstrom, N. G.; Gerh
- Page 689 and 690:
Gennart, J. P.; Bernard, A.; Lauwer
- Page 691 and 692:
Haraguchi, T.; Ishizu, H.; Takehisa
- Page 693 and 694:
Jemal, A.; Graubard, B. I.; Devesa,
- Page 695 and 696:
Lanphear, B. P.; Howard, C.; Eberly
- Page 697 and 698:
Lundström, N.-G.; Nordberg, G.; En
- Page 699 and 700:
Muntner, P.; He, J.; Vupputuri, S.;
- Page 701 and 702:
Paksy, K.; Gáti, I.; Náray, M.; R
- Page 703 and 704:
Rhainds, M.; Levallois, P.; Dewaill
- Page 705 and 706:
Sargent, J. D.; Dalton, M. A.; O'Co
- Page 707 and 708:
Sheffet, A.; Thind, I.; Miller, A.
- Page 709 and 710:
Stevens, L. A.; Levey, A. S. (2005b
- Page 711 and 712:
Van Larebeke, N.; Koppen, G.; Nelen
- Page 713 and 714:
Winker, R.; Ponocny-Seliger, E.; R
- Page 715 and 716:
October 2006 EPA/600/R-05/144bF Air
- Page 717 and 718:
PREFACE National Ambient Air Qualit
- Page 719 and 720:
drafts of document materials were r
- Page 721 and 722:
Table of Contents PREFACE..........
- Page 723 and 724:
Table of Contents (cont’d) II-ix
- Page 725 and 726:
List of Tables (cont’d) AX7-2.3.1
- Page 727 and 728:
List of Figures (cont’d) Number P
- Page 729 and 730:
Principal Authors Authors, Contribu
- Page 731 and 732:
Principal Authors Authors, Contribu
- Page 733 and 734:
Principle Authors (cont’d) Author
- Page 735 and 736:
Technical Support Staff U.S. Enviro
- Page 737 and 738:
Members (cont’d) U.S. Environment
- Page 739 and 740:
ANOVA analysis of variance ANP atri
- Page 741 and 742:
CCD charge-coupled device CCE Coord
- Page 743 and 744:
DPPD N-N-diphenyl-p-phynylene-diami
- Page 745 and 746:
FTES free testosterone FTII Fagan T
- Page 747 and 748:
HPLC high-pressure liquid chromatog
- Page 749 and 750:
MAO monoamine oxidase MATC maximum
- Page 751 and 752:
NORs nucleolar organizing regions N
- Page 753 and 754:
ppm parts per million PPVT-R Peabod
- Page 755 and 756:
SOPR sperm-oocyte penetration rate
- Page 757 and 758:
vit C vitamin C vit E vitamin E VMA
- Page 759 and 760:
Pb is ideally suited for this task.
- Page 761 and 762:
Concept For a given metal or metall
- Page 763 and 764:
(1979) observed that “the smaller
- Page 765 and 766:
Figure AX7-1.1.3. Illustration of p
- Page 767 and 768:
• Colorimetric • Electrochemica
- Page 769 and 770:
Figure AX7-1.1.5. Bulk lead versus
- Page 771 and 772:
diffraction lines and comparing the
- Page 773 and 774:
The major disadvantage of SIMS to s
- Page 775 and 776:
techniques can be useful in a study
- Page 777 and 778:
have included phosphoric acid (H3PO
- Page 779 and 780:
to 15 years after biosolid applicat
- Page 781 and 782:
thin films (DGT), and ICP technique
- Page 783 and 784:
completely extract targeted phases.
- Page 785 and 786:
epresents Eb. The precise energy re
- Page 787 and 788:
1974; Ruby et al., 1994). However,
- Page 789 and 790:
T1/2 = 14 × 10 9 year). The result
- Page 791 and 792:
floor) time-series data to evaluate
- Page 793 and 794:
contributions of dry deposition may
- Page 795 and 796:
Compared to their estimated 20th-ce
- Page 797 and 798:
thought to enter the plant via the
- Page 799 and 800:
soil was not allowed to equilibrate
- Page 801 and 802:
Lead concentrations in various tiss
- Page 803 and 804:
that the nematode may detoxify Pb v
- Page 805 and 806:
plasma levels of uric acid and crea
- Page 807 and 808:
effective use of glutathione metabo
- Page 809 and 810:
and oats (Avena sativa) had signifi
- Page 811 and 812:
other metals is inconsistent (Påhl
- Page 813 and 814:
Speciation and Form of Lead Recent
- Page 815 and 816:
organism responses to Pb. Section A
- Page 817 and 818:
Primary Producers Commonly reported
- Page 819 and 820:
solution and minimal translocation
- Page 821 and 822:
AX7.1.3.3 Recent Studies on the Eff
- Page 823 and 824:
AX7-66 Avian Species Reproduction J
- Page 825 and 826:
AX7-68 Avian Species American kestr
- Page 827 and 828:
Very little research has been done
- Page 829 and 830:
AX7-72 Mammalian Species Reproducti
- Page 831 and 832:
AX7-74 Mammalian Species No. of Dos
- Page 833 and 834:
AX7-76 Mammalian Species No. of Dos
- Page 835 and 836:
AX7-78 Mammalian Species No. of Dos
- Page 837 and 838:
AX7-80 Mammalia n Species No. of Do
- Page 839 and 840:
A literature search and review was
- Page 841 and 842:
Table AX7-1.3.6. Invertebrate Toxic
- Page 843 and 844:
The effects of Pb-chloride on the p
- Page 845 and 846:
Ecological Soil Screening Levels (E
- Page 847 and 848:
Since the movement and fate of Pb i
- Page 849 and 850:
Land Use and Industry Changes in la
- Page 851 and 852:
lakes in the United Kingdom the dis
- Page 853 and 854:
zinc; had very low pH; and were det
- Page 855 and 856:
Sites Affected by Long-Range Lead T
- Page 857 and 858:
iomass carbon. Because of this link
- Page 859 and 860:
in an oak woodland site 3 km from a
- Page 861 and 862:
the forested Lehstenbach catchment
- Page 863 and 864:
there is little evidence that Pb ac
- Page 865 and 866:
ecosystems. Just as in the terrestr
- Page 867 and 868:
To develop chronic AWQC, acceptable
- Page 869 and 870:
for the binding of free-metal ion a
- Page 871 and 872:
partition in sediment between acid-
- Page 873 and 874:
AX7.2.1.5 Metal Mixtures As discuss
- Page 875 and 876:
varies from 4:1 in rural streams to
- Page 877 and 878:
Organic compounds in surface waters
- Page 879 and 880:
solution phase, complexation with c
- Page 881 and 882:
The NAWQA dataset was chosen over o
- Page 883 and 884:
Lead Distributions Generated from t
- Page 885 and 886:
AX7-128 Figure AX7-2.2.3. Spatial d
- Page 887 and 888:
AX7-130 Figure AX7-2.2.5. Spatial d
- Page 889 and 890:
AX7-132 ` Figure AX7-2.2.7. Spatial
- Page 891 and 892:
Figure AX7-2.2.8. Frequency distrib
- Page 893 and 894:
Table AX7-2.2.4. Summary Statistics
- Page 895 and 896:
Table AX7-2.2.5. Comparison of NCBP
- Page 897 and 898:
AX7-140 Figure AX7-2.2.13. Spatial
- Page 899 and 900:
calculations indicate that only a s
- Page 901 and 902:
from municipal sewage, storm runoff
- Page 903 and 904:
AX7.2.3 Aquatic Species Response/Mo
- Page 905 and 906:
aquatic plants and insects and on t
- Page 907 and 908:
designed to model uptake, MINTEQ pr
- Page 909 and 910:
sequestering to organ tissues). The
- Page 911 and 912:
AbdAllah and Moustafa (2002) studie
- Page 913 and 914:
Summary of Detoxifiction Processes
- Page 915 and 916:
1.1 µg/L Cd, 12 µg/L Cu, 55 µg/L
- Page 917 and 918:
Studies have identified ALAD in fis
- Page 919 and 920:
metals over nonessential metals. Th
- Page 921 and 922:
In summary, relationships between a
- Page 923 and 924:
potential toxic effects in other or
- Page 925 and 926:
esulted in 91.7% survival (Horne an
- Page 927 and 928:
carbon sources (including glucose),
- Page 929 and 930:
separate concentration-effects mode
- Page 931 and 932:
1994. mSQGQs are useful to risk ass
- Page 933 and 934:
Algae The 1986 Lead AQCD (U.S. Envi
- Page 935 and 936:
observed in Selenastrum capricornut
- Page 937 and 938:
Nitrate uptake reported after 48, 7
- Page 939 and 940:
1997). The most sensitive primary p
- Page 941 and 942:
Freshwater Invertebrates Acute and
- Page 943 and 944:
AX7-186 Amphipod (Hyalella azteca)
- Page 945 and 946:
concentrations of
- Page 947 and 948:
AX7-190 Freshwater Species Chemical
- Page 949 and 950:
AX7-192 Species Chemical Frogs (Ran
- Page 951 and 952:
studied using Spirodela polyrhiza,
- Page 953 and 954:
However, in other cases multivariat
- Page 955 and 956:
species was observed. Similar, sign
- Page 957 and 958:
AX7-200 Table AX7-2.5.2. Essential
- Page 959 and 960:
AX7-202 Table AX7-2.5.2 (cont’d).
- Page 961 and 962:
variables, it does not imply causat
- Page 963 and 964:
Poulton et al. (1995), the effects
- Page 965 and 966:
metal levels. Furthermore, although
- Page 967 and 968:
environment through bioaccumulation
- Page 969 and 970:
Angle, C. R.; McIntire, M. S.; Colu
- Page 971 and 972:
Black, M. C.; Ferrell, J. R.; Horni
- Page 973 and 974:
Clements, W. H. (1994) Benthic inve
- Page 975 and 976:
Ekenler, M.; Tabatabai, M. (2002) E
- Page 977 and 978:
Getz, L. L.; Haney, A. W.; Larimore
- Page 979 and 980:
Houlton, B. Z.; Driscoll, C. T.; Fa
- Page 981 and 982:
Krüger, F.; Gröngröft, A. (2003)
- Page 983 and 984:
Manceau, A.; Lanson, B.; Schlegel,
- Page 985 and 986:
Niyogi, S.; Wood, C. M. (2003) Effe
- Page 987 and 988:
Rand, G. M.; Wells, P. G.; McCarty,
- Page 989 and 990:
Scherer, E.; McNicol, R. E. (1998)
- Page 991 and 992:
Sturges, W. T.; Barrie, L. A. (1987
- Page 993 and 994:
U.S. Environmental Protection Agenc
- Page 995 and 996:
Zenk, M. H. (1996) Heavy metal deto