insights - IMS Health
insights - IMS Health
insights - IMS Health
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
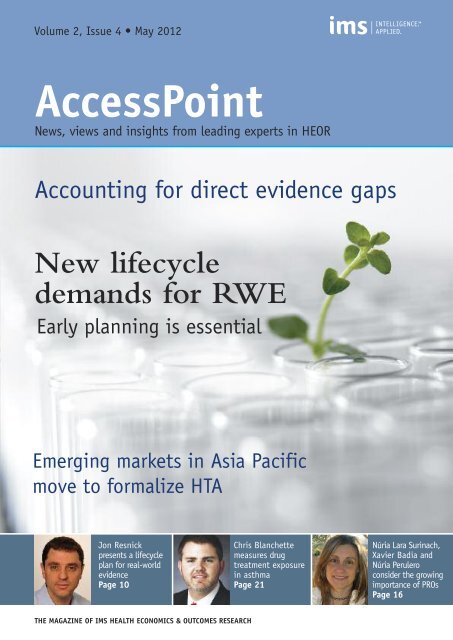
Volume 2, Issue 4 • May 2012<br />
AccessPoint<br />
News, views and <strong>insights</strong> from leading experts in HEOR<br />
Accounting for direct evidence gaps<br />
New lifecycle<br />
demands for RWE<br />
Early planning is essential<br />
Emerging markets in Asia Pacific<br />
move to formalize HTA<br />
Jon Resnick<br />
Chris Blanchette<br />
Núria Lara Surinach,<br />
presents a lifecycle<br />
measures drug<br />
Xavier Badia and<br />
plan for real-world<br />
Page OUTCOMES 1 - Issue 1<br />
evidence<br />
treatment exposure<br />
Núria Perulero<br />
<strong>IMS</strong> HEALTH ECONOMICS AND OUTCOMES RESEARCH Page 1<br />
in asthma<br />
consider the growing<br />
Page 10<br />
Page 21<br />
importance of PROs<br />
Page 16<br />
THE MAGAZINE OF <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
Volume 2, Issue 4 • May 2012<br />
AccessPoint<br />
News, views and <strong>insights</strong> from leading experts in HEOR<br />
providers<br />
Preparing for a lifecycle of real-world evidence<br />
Increasing demand brings a need for new capabilities, data<br />
considerations, and effective planning for RWE across the<br />
entire product lifecycle.<br />
page 10<br />
Accounting for direct evidence gaps<br />
with indirect treatment comparisons<br />
Network meta-analysis offers growing potential.<br />
page 26<br />
Who drives the lion’s share of costs?<br />
Understanding healthcare spending in the<br />
commercially-insured US population under age 65.<br />
page 32<br />
Pharmacogenomics comes of age<br />
Continued evolution of pharmacogenomics brings<br />
new considerations for RWE.<br />
page 44<br />
<strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
“2012 is shaping a future that will be<br />
transformed by real-world evidence”<br />
WELCOME<br />
Welcome to the fourth issue of AccessPoint, a twice-yearly<br />
highlight of news, views and <strong>insights</strong> from the international<br />
HEOR team at <strong>IMS</strong> <strong>Health</strong> – casting an expert eye on the<br />
evolving dynamics that are changing the basis for healthcare<br />
decision making with potential for improved efficiency through<br />
real-world evidence (RWE) generation.<br />
RWE is not a new concept - HEOR researchers have been<br />
generating evidence for years - but growing demand is driving<br />
new opportunities to expand, enhance and do more. As we move<br />
through 2012, we see a year that is shaping a future where<br />
healthcare is transformed by RWE: the emerging markets of Asia<br />
Pacific (page 40) have joined a growing body of countries<br />
globally that depend on RWE to inform HTA; significant, too, is<br />
an important shift in the timeframe over which value is<br />
determined, extending the use of RWE far into the product<br />
lifecycle (page 10); at the same time, the science of personalized<br />
medicine (page 44) brings further potential for the expanded<br />
application of RWE; and underpinning these trends, the bar is<br />
being raised for real-world studies, setting new standards for their<br />
design and validation (page 16).<br />
Today, regulators, HTA bodies, payers, practitioners, patients and<br />
manufacturers are united in the goal of improving treatment<br />
based on the best available evidence. <strong>IMS</strong> is committed to<br />
advancing the use of RWE to enable improved efficiency in<br />
healthcare and enrich the dialog across the healthcare setting. Our<br />
recent lead in a national debate on RWE studies in France (page<br />
6) has already paved the way for a smoother process based on a<br />
new collaborative spirit, and in our joint initiative with<br />
AstraZeneca in Europe (Page 7) we look forward to leveraging a<br />
shared perspective on the transformative power of RWE in<br />
informing the delivery of effective and cost-efficient healthcare.<br />
Fulfilling the potential of RWE requires new capabilities in<br />
managing, analyzing and leveraging real-world information. In<br />
responding to the demand for more compelling, credible evidence,<br />
companies will need to reconsider the way they collect and interact<br />
with real-world data.<br />
<strong>IMS</strong> has a global team of more than 200 experts in outcomes<br />
research, economic modeling, RWE and market access. Our<br />
research calls for creative thinking to connect and integrate<br />
fragmented information and build the tools, interfaces and technical<br />
platforms that will enable faster, more robust RWE generation.<br />
We continue to invest in research programs to ensure the strongest<br />
foundation for identifying, interpreting and communicating realworld<br />
outcomes. Our recent validations of the <strong>IMS</strong> CORE<br />
Diabetes Model (page 8) and integration of our global patient-level<br />
assets, including <strong>IMS</strong> LifeLink PharMetrics PLUS (page 2), confirm our<br />
ongoing efforts in this area.<br />
I hope you find this issue of AccessPoint timely, informative and<br />
stimulating in a year that is defining a clearer path to stronger,<br />
evidence-based decision making.<br />
Jon Resnick<br />
VICE PRESIDENT, REAL-WORLD EVIDENCE SOLUTIONS, <strong>IMS</strong> HEALTH<br />
Jresnick@uk.imshealth.com<br />
CONTENTS<br />
NEWS SECTION<br />
2 <strong>IMS</strong> announces LifeLink PharMetricsPLUS 4 Oncology leads <strong>IMS</strong> research agenda<br />
6 <strong>IMS</strong> drives French debate on RWE<br />
7 Landmark RWE partnership with AstraZeneca<br />
8 <strong>IMS</strong> CORE Diabetes Model maintains<br />
leadership position<br />
INSIGHTS<br />
10 REAL-WORLD EVIDENCE<br />
Developing a lifecycle plan<br />
16 PATIENT-REPORTED OUTCOMES<br />
Increasing relevance adds to expectations<br />
21 DRUG EXPOSURE MEASUREMENT<br />
Standardization key to meaningful results<br />
26 INDIRECT TREATMENT COMPARISONS<br />
Accounting for direct evidence gaps<br />
32 US PRIVATE HEALTHCARE SPENDING<br />
Who drives the lion’s share of costs?<br />
40 IMPLEMENTING HTA IN ASIA PACIFIC<br />
Critical success factors in emerging markets<br />
44 PHARMACOGENOMICS<br />
New imperatives for RWE strategy<br />
PROJECT FOCUS<br />
50 <strong>IMS</strong> CORE BUDGET IMPACT MODEL<br />
Payer-relevant pharmacy analyses<br />
52 DATA LINKAGE IN ONCOLOGY<br />
EMR oncology data platform<br />
54 METASTATIC COLORECTAL CANCER<br />
Informing optimal treatment strategies<br />
<strong>IMS</strong> HEOR OVERVIEW<br />
56 ENABLING YOUR REAL-WORLD SUCCESS<br />
Locations, expertise, <strong>IMS</strong> LifeLink AccessPoint is published twice yearly by the <strong>Health</strong><br />
Economics & Outcomes Research team of <strong>IMS</strong> <strong>Health</strong>.<br />
VOLUME 2 ISSUE 4. PUBLISHED MAY 2012.<br />
<strong>IMS</strong> HEALTH 210 Pentonville Road, London N1 9JY, UK<br />
Tel: +44 (0) 20 3075 4800 • HEORinfo@uk.imshealth.com<br />
www.imshealth.com/heor<br />
© 2012 <strong>IMS</strong> <strong>Health</strong> Incorporated and its affiliates. All rights reserved.<br />
Trademarks are registered in the United States and in various<br />
other countries.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 1
NEWS | <strong>IMS</strong> LIFELINK PHARMETRICS PLUS<br />
Major investment extends the leverage of <strong>IMS</strong> linked patient-level data bringing new<br />
possibilities for health economics and outcomes research.<br />
<strong>IMS</strong> announces LifeLink PharMetrics PLUS<br />
- the most comprehensive integrated<br />
database available in the US market<br />
Marking a strong commitment to advance the use<br />
of real-world evidence (RWE) for assessing the way<br />
in which a drug or medical device performs in<br />
actual clinical practice, <strong>IMS</strong> continues to make<br />
significant investments to enhance and better<br />
leverage its existing patient-level datasets.<br />
<strong>IMS</strong> is already widely recognized as a leading provider of the<br />
<strong>IMS</strong> LifeLink <strong>Health</strong> Plan Claims database. Formerly known as<br />
PharMetrics, this is the largest independent claims data source<br />
in the US, covering more than 73 million unique patients. With<br />
the acquisition of SDI in Q4 2011 came a range of<br />
complementary LifeLink Information Assets, providing <strong>insights</strong><br />
into the total patient experience in the US - as patients receive<br />
care from providers, pharmacies, hospitals, labs and other<br />
facilities – and the way in which this care is influenced by other<br />
factors, such as patient characteristics and behaviors, past<br />
treatments, managed care coverage, and further key attributes.<br />
<strong>IMS</strong> LIFELINK PHARMETRICSPLUS The SDI legacy further included established and published<br />
expertise in data linkage and integration which has now been<br />
leveraged to develop a new, integrated dataset, known as<br />
<strong>IMS</strong> LifeLink PharMetricsPLUS .<br />
LifeLink PharMetricsPLUS brings <strong>IMS</strong> <strong>Health</strong> Plan Claims data<br />
integrated with:<br />
• Hospital Charge Data Master: Collected from general<br />
medical-surgical and specialty hospital's in-patient and<br />
out-patient records. Includes detailed diagnoses, procedures,<br />
drugs, devices, applied charges, sites of service, as well as<br />
patient demographics and admission/discharge characteristics.<br />
• Oncology EMR data: Collected in the out-patient office<br />
setting from medium and large community-based oncology<br />
urology, dialysis, radiation, cancer registry, hospital, and<br />
general/ambulatory practices. Provides detailed clinical<br />
data, including diagnoses, treatments, oral and injectable<br />
medications, in-office procedures, lab results, vitals,<br />
patient demographics, cancer staging, tumor morphology,<br />
and metastatic identifier.<br />
• Ambulatory EMR: Collected from GP/IM practices and<br />
clinics. Out-patient, clinical, patient-level charts in an<br />
electronic format with representative coverage of most<br />
regions. Provides detailed clinical and patient attributes,<br />
including diagnoses, written prescriptions, procedures,<br />
test results, and clinical variables (eg, BMI, BP).<br />
• Lab data: Collected from a leading national lab provider,<br />
laboratory data including demographics, diagnosis, test<br />
date, test description, result, reference results ranges, and<br />
ordering provider's geographic location.<br />
• Consumer attributes: Collected from a respected global<br />
leader in compiling unique consumer data including<br />
financial, demographic, race/ethnicity, mortality, and<br />
psychographic profiles.<br />
• Retail purchasing OTC/CPG: Collected from a respected<br />
source of loyalty card purchasing data. Contains retail<br />
purchasing information which allows classification of<br />
consumers based on buying behavior.<br />
<strong>IMS</strong> LIFELINK PHARMETRICS PLUS INTEGRATED DATASETS<br />
Pharmacy<br />
prescription<br />
Hospital<br />
Retail<br />
purchasing<br />
OTC/CPG<br />
Ambulatory<br />
EMR<br />
<strong>Health</strong> Plan<br />
Claims<br />
Consumer<br />
attributes<br />
Oncology<br />
EMR<br />
PAGE 2 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH<br />
Medical<br />
claims
<strong>IMS</strong> DE-IDENTIFICATION ENGINE<br />
<strong>IMS</strong> LIFELINK PHARMETRICS PLUS | NEWS<br />
Retail & LTC Rx Customer data<br />
Medical claims<br />
Hospital charge<br />
detail master<br />
<strong>Health</strong>care provider<br />
attributes<br />
Labs<br />
Electronic medical<br />
Records<br />
Consumer<br />
demographics<br />
& psychographics<br />
• Medical claims: Pre-adjudicated claims (switch source)<br />
collected from office-based physicians and specialists.<br />
Expands the demographics of the database to include<br />
populations and claims that might be under-represented<br />
in health plan claims data, including Medicare and<br />
Medicaid. The data include patient demographics,<br />
physician demographics, diagnoses, procedures, and<br />
in-office administered drugs.<br />
• Pharmacy prescription data: Collected from retail, mailorder,<br />
long-term care and specialty pharmacy records.<br />
Includes claims submitted for payment and other<br />
prescriptions directly from key pharmacy locations.<br />
In addition to commercial and government payers, cash<br />
transactions are recorded.<br />
NEW ANALYTICAL POTENTIAL<br />
Directly linked via unique patient identifiers, using a unique<br />
and proprietary algorithm for de-identification of patients,<br />
ensuring HIPAA compliance, these data open up new<br />
analytical possibilities, overcoming the limitations in<br />
scope or clinical detail of current databases. Analyses types<br />
enabled include:<br />
• Monitoring post-discharge outcomes of detailed in-patient<br />
clinical pathways<br />
• Adding health status variables (eg, biomarkers and vitals)<br />
to comparative effectiveness and cost-of-care analyses<br />
Source<br />
<strong>IMS</strong><br />
de-identi�cation<br />
engine<br />
De-identi�ed data<br />
<strong>IMS</strong> uses a unique<br />
and proprietary<br />
algorithm for<br />
de-identi�cation of<br />
patients, ensuring<br />
compliance with<br />
HIPAA regulations<br />
Data<br />
warehouse<br />
• Enhancing drug exposure measures impacted by<br />
administrative data loss<br />
• Expanding the availability of clinical endpoints such as<br />
mortality and progression in database analyses<br />
EARLY ACCESS<br />
As this exciting development progresses, work on establishing<br />
linkage for the various datasets continues, reflecting the<br />
significant level of investment involved in incorporating<br />
information provided by multiple health plans and other<br />
data sources. In advance of full commercialization, <strong>IMS</strong> is<br />
providing clients with early access to the new integrated<br />
dataset, LifeLink PharMetrics PLUS which is now ready for<br />
research. As from June 2012, the information available in the<br />
database can be used for client projects leveraging the<br />
analytical expertise and data knowledge of the <strong>IMS</strong> HEOR<br />
team. While the initial linked dataset is based on selected<br />
health plans, <strong>IMS</strong> anticipates significant growth in the size<br />
of the database over the course of the coming months,<br />
allowing even more research questions to be answered •<br />
If you would like to learn more about <strong>IMS</strong> LifeLink<br />
PharMetrics PLUS , the most comprehensive integrated database<br />
available in the US market, please email Michael Nelson at<br />
Mnelson@us.imshealth.com<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 3
NEWS | <strong>IMS</strong> ONCOLOGY EXPERTISE<br />
The <strong>IMS</strong> HEOR Bibliography captures more than 2200 research publications with a history<br />
of 25 years across all key therapy areas. Oncology is one of our leading fields of research.<br />
Oncology is a key research area for <strong>IMS</strong> HEOR<br />
The oncology market is experiencing spectacular<br />
growth and unprecedented innovation.<br />
It is predicted to become the largest single therapy<br />
sector in value terms by 2015 – worth US$75 billion.<br />
New molecular targeted therapies, diagnostics,<br />
genomics and proteomics are changing the face of<br />
cancer treatment, spurring exciting opportunities<br />
- and also new challenges - for this healthcare<br />
sector worldwide.<br />
The <strong>IMS</strong> HEOR global team has completed projects<br />
on 20 different tumor types, spanning all aspects<br />
of health economics and outcomes research, with<br />
particular emphasis on health economic modeling<br />
and retrospective outcomes research.<br />
The top ten cancers we have covered are:<br />
1. Breast<br />
2. Lung [NSCLC/SCLC]<br />
3. Colorectal<br />
4. Lymphoma<br />
5. Melanoma/BCC<br />
6. Prostate<br />
7. Multiple myeloma<br />
8. Leukemias [CLL/CML]<br />
9. Mesothelioma<br />
10. Cervical<br />
<strong>IMS</strong> HEOR ONCOLOGY PROJECTS SPAN ALL ASPECTS OF HEOR<br />
43%<br />
ONCOLOGY IS A LEADING AREA OF <strong>IMS</strong> HEOR EXPERTISE<br />
116 107<br />
PAGE 4 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH<br />
150<br />
233<br />
259<br />
330<br />
Diabetes Oncology Cardiovascular<br />
Mental health<br />
HE modeling<br />
Prospective<br />
outcomes research<br />
Neurological<br />
disorders<br />
14%<br />
30%<br />
13%<br />
Retrospective<br />
outcomes research<br />
Value<br />
communications<br />
Respiratory<br />
diseases
<strong>IMS</strong> HEOR Bibliography<br />
<strong>Health</strong> economics review of<br />
bowel cancer in Australia<br />
NSW Cancer Institute, 2008,<br />
Sydney, Australia (Review)<br />
Bishop J, Glass P, Tracey E,<br />
Hardy M, Warner K, Makino K,<br />
Gordois A, Wilson J,<br />
Guarnieri C, Feng J,<br />
Sartori L<br />
Economic model of granulocyte<br />
-colony stimulating factor (G-CSF)<br />
in primary (PP) and secondary<br />
prophylaxis (SP) of febrile<br />
neutropenia (FN) in Non-Hodgkin's<br />
Lymphoma (NHL) patients<br />
undergoing chemotherapy in France<br />
ISPOR 14th Annual European<br />
Congress, Madrid, Spain,<br />
5-8 November, 2011<br />
Perrier L, Sebban C,<br />
Leon N, Maurel F,<br />
Cohen-Nizard S,<br />
De Liège F<br />
<strong>IMS</strong> ONCOLOGY EXPERTISE | NEWS<br />
Our research expertise and therapy area knowledge are captured in more than<br />
200 publications each year, spanning virtually all therapy areas and 50+<br />
countries worldwide. Contact <strong>IMS</strong> (details on back cover) for a copy of the<br />
latest <strong>IMS</strong> HEOR Bibliography of published papers (2008-2012) or visit<br />
www.imsheorbibliography.com to explore our database online.<br />
The <strong>IMS</strong> HEOR bibliography in oncology spans all key areas of health economics and outcomes<br />
research, including retrospective and observational analyses, budget impact, cost-effectiveness and<br />
cost utility modeling, model adaptations, epidemiology and burden of disease studies, indirect<br />
comparisons, and meta-analyses, bringing important new findings across all key tumor types and<br />
countries around the world.<br />
Breast cancer diagnostic<br />
process: Management and cost<br />
evaluation in Italy<br />
ISPOR 12th Annual European<br />
Congress, Paris, France, 24-27<br />
October, 2009<br />
Pantaleoni M,<br />
Marchese E<br />
Second-line therapy for<br />
non-small cell lung cancer<br />
(NSCLC): A retrospective cost<br />
analysis<br />
Tumordiagn u Ther, 2008;<br />
29:211-217<br />
Gatzemeier U, Pirk O,<br />
Gabriel A,<br />
Kotowa W,<br />
Heigener D<br />
Development of a<br />
co-morbidity scale in patients<br />
with chronic lymphocytic<br />
leukemia<br />
ISPOR 13th Annual European<br />
Congress, Prague, Czech<br />
Republic, 6-9 November, 2010<br />
Carbonell F, De La Serna J,<br />
Giraldo P, Lopez A, Rios E,<br />
Perulero N,<br />
Castro-Gomez AJ<br />
Cost-effectiveness of cetuximab,<br />
bevacizumab, and panitumumab<br />
in first-line treatment of<br />
metastatic colorectal cancer<br />
(mCRC) for patients with KRAS<br />
wild-type (wt) tumors in the UK<br />
Journal of Clinical Oncology,<br />
2011;29(Suppl):A16571<br />
Samyshkin Y, Hertel N,<br />
Griebsch I<br />
Five-year routine cervical<br />
cancer screening rates and<br />
intervals in a United States<br />
health plan<br />
Current Medical Research and<br />
Opinion, 2008; 24(9):2429-<br />
2435<br />
Schabert VF, Ye X, Insinga RP,<br />
Singhal PK, Riedel AA<br />
Cost-utility analysis of dasatinib<br />
as a second-line treatment in<br />
the chronic phase of chronic<br />
myeloid leukaemia in Russia<br />
ISPOR 13th Annual European<br />
Congress, Prague, Czech<br />
Republic, 6-9 November, 2010<br />
Kuznetzov SV, Mungapen L,<br />
Samyshkin Y, Jakouloff D,<br />
Sbarigia U,<br />
van Baardewijk M<br />
Economic evaluation in the<br />
treatment of advanced and/or<br />
metastatic gastric cancer from<br />
the perspective of the public<br />
health system in Mexico<br />
ISPOR 17th Annual<br />
International Meeting,<br />
Washington, DC, USA,<br />
2-6 June, 2012<br />
Lechuga D, Alva M,<br />
Salinas GE, Leyva V<br />
Epidemiologic study to assess<br />
patient involvement in choice<br />
of adjuvant chemotherapy in<br />
breast cancer (PROSA study)<br />
Clinical and Translational<br />
Oncology, 2009; 11(4):221-7<br />
Tusquets I, Espinosa Arranz E,<br />
Méndez M, Gil JM,<br />
Guallar JL,<br />
Perulero N<br />
A retrospective analysis<br />
illustrating the substantial<br />
clinical and economic burden<br />
of prostate cancer<br />
Prostate Cancer and Prostatic<br />
Diseases, 2010; 13(2):162-167<br />
Crawford ED, Black L,<br />
Eaddy M, Kruep EJ<br />
Risk of treatment failure after<br />
first-line sunitinib therapy in<br />
patients with metastatic renal<br />
cell carcinoma<br />
Journal of Clinical Oncology,<br />
2012; 30 (Suppl 5): Abstract<br />
438<br />
Chen CC, Hess GP, Liu Z,<br />
Gesme DH, Agarwala SS,<br />
Hill JW, Guo MA<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 5
NEWS | REAL-WORLD EVIDENCE IN FRANCE<br />
Senior French healthcare stakeholders respond to <strong>IMS</strong> lead for tackling process<br />
bottlenecks hindering real-world evidence development.<br />
<strong>IMS</strong> HEOR drives national debate on<br />
RWE studies in France<br />
<strong>IMS</strong> HEOR has taken a leadership role in France to<br />
address problems that are hindering the<br />
development of real-world evidence (RWE) studies<br />
required for market access regulation. By creating<br />
a platform for stakeholder discussion at the highest<br />
level, the <strong>IMS</strong> HEOR team in France, led by<br />
Principal, Dana Morlet-Vigier, has paved the way<br />
for alignment and solutions.<br />
In France, every drug must pass through a value assessment<br />
by the High Authority for <strong>Health</strong> (HAS) and negotiation with<br />
the pricing committee (CEPS) to achieve reimbursement. Both<br />
government agencies are placing greater emphasis on RWE to<br />
determine how a new technology performs in actual clinical<br />
practice. Manufacturers can face significant financial sanctions<br />
if studies are not provided in a reasonable timeframe. However,<br />
the process for initiating RWE studies in France is currently<br />
slow and complex, involving multiple stakeholders. CEPS<br />
president, Gilles Johanet, has himself acknowledged the<br />
imperative for a more dynamic evaluative approach.<br />
PROPOSAL FOR ACTION<br />
With the entire economic life of a drug dependent on<br />
compulsory post-listing, post-reimbursement studies, <strong>IMS</strong><br />
recognized the need to kick-start change and approached<br />
CEPS direct with a proposal: as a “neutral” expert in RWE<br />
studies, the <strong>IMS</strong> HEOR team would organize and facilitate a<br />
workshop with all relevant stakeholders, as well as a<br />
specialist in process industrialization, to identify and analyze<br />
critical bottlenecks in the system.<br />
DRIVING ALIGNMENT<br />
The offer was accepted and in late 2011, 75 top decision<br />
makers in France came together at the invitation of <strong>IMS</strong> for<br />
a day of structured presentations and debate. Participants<br />
included pharma Directors/VPs of market access and HEOR,<br />
doctors/clinical investigators, and senior representatives<br />
from HAS, CEPS and other public policy stakeholders. The<br />
discussions, framed by <strong>IMS</strong>, focused on the need for RWE, its<br />
impact on the pharmaceutical industry, the process and subprocesses<br />
of RWE studies in France, database studies and<br />
ad-hoc observational trials.<br />
The workshop proved transformational, achieving consensus<br />
on issues compromising the timeliness and quality of RWE<br />
studies. It was so successful in reaching this point that <strong>IMS</strong><br />
was invited to set up and moderate a second, follow-on<br />
session early in 2012, where specific recommendations for<br />
the scope and management of RWE studies were identified.<br />
SMOOTHER PROCESS<br />
By coordinating brainstorming and communication between<br />
major public decision makers and pharma, this initiative has<br />
paved the way for a smoother process and helped to shape<br />
the future development of RWE in France. It also reaffirms<br />
the potential of alignment and collaboration in fostering<br />
positive change and advancing efforts to improve healthcare<br />
efficiency, ensure safety and demonstrate value for money. •<br />
75 top decision makers in France came together at the invitation<br />
of <strong>IMS</strong> for a day of structured presentations and debate on RWE.<br />
Above: Gilles Johanet (left) and Dana Morlet-Vigier<br />
Below: Workshop sessions during the event<br />
PAGE 6 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
REAL-WORLD EVIDENCE COLLABORATION | NEWS<br />
Groundbreaking partnership heralds potential for improving healthcare efficiency by<br />
advancing the use of real-world evidence (RWE) in Europe<br />
<strong>IMS</strong> enters collaboration with AstraZeneca<br />
to expand real-world evidence<br />
Early in 2012, AstraZeneca announced a three-year agreement with <strong>IMS</strong> to advance the use of<br />
real-world evidence (RWE) - and establish standards for RWE generation - based on observational and<br />
retrospective studies throughout Europe, to inform the delivery of effective and cost-efficient healthcare.<br />
The partnership with <strong>IMS</strong> <strong>Health</strong> will give AstraZeneca access<br />
to pre-existing anonymized electronic health records, which<br />
include clinical outcome, economic and treatment pattern<br />
data. In addition, the companies will jointly develop a<br />
customized research and data analysis platform. The<br />
information will provide a deeper insight into how medicines<br />
that are already on the market are working in real-world<br />
settings across Europe, painting a picture of unmet needs in<br />
the current standard of care and treatment patterns across a<br />
number of therapeutic areas, with an emphasis on chronic<br />
illnesses. The data will also be used to inform AstraZeneca’s<br />
discovery and clinical development programs.<br />
The collaboration reflects the interest among healthcare<br />
decision makers in examining the cost and effectiveness of<br />
new and existing medicines and health technologies to help<br />
allocate their increasingly limited resources more efficiently.<br />
Unlike controlled clinical trials, RWE studies use observational<br />
data such as electronic medical records, claims information,<br />
patient registries and patient surveys. By evaluating the data<br />
associated with the delivery of care, ‘real-world’ analyses can<br />
demonstrate treatment impact on measurable outcomes such<br />
as hospital length of stay, readmissions, overall health status<br />
and total cost of care.<br />
This is how senior leaders from AstraZenca and <strong>IMS</strong> see the<br />
partnership:<br />
“Our collaboration with <strong>IMS</strong> is a key milestone in our<br />
commitment to understand the impact of our medicines in the<br />
real world, beyond what we see in controlled clinical trials.<br />
This insight will help us and healthcare decision makers to<br />
improve the treatment of disease and ensure effective use of<br />
medicines to minimize the burden on individuals and<br />
healthcare budgets.”<br />
Martin Mackay, President of Research and Development,<br />
AstraZeneca<br />
“This joint initiative reflects a shared perspective on the<br />
transformative power of real-world evidence on global health<br />
systems. Our unique information assets, coupled with our<br />
services and technology capabilities, make <strong>IMS</strong> a leading<br />
partner for healthcare organizations in the identification,<br />
integration and interpretation of real-world outcomes.<br />
We are extremely pleased to be working with AstraZeneca on<br />
this collaboration.”<br />
Jon Resnick, Vice President of Real-World Evidence Solutions,<br />
<strong>IMS</strong> <strong>Health</strong><br />
The press release has since received wide media coverage and<br />
has featured in more than 30 articles, including reports in the<br />
Wall Street Journal, The Pink Sheet and Pharma Times online.<br />
In an interview on February 22 with PharmaExec, Jon Resnick,<br />
when asked how others could benefit from this partnership,<br />
confirmed that there will be active efforts to involve payers<br />
and other providers in “an honest set of conversations" about<br />
how to work with the information, both during and beyond<br />
the collaboration.<br />
“For this to work, you need the buy-in,” says Jon. “You can’t<br />
create real information in a vacuum; you can’t work with a set<br />
of databases that are closed to the universe and then hand<br />
the information to a payer and say you want to charge 20<br />
percent more.” Whichever data will eventually be made publicly<br />
available depends on the type of study it relates to, but Jon<br />
emphasizes that the <strong>IMS</strong>/AZ research is not just between the<br />
two companies. “Opening it up to academics and broader<br />
audiences is healthy if we want to maintain credibility. A<br />
broader set of participants will be needed to ratify<br />
the information.” •<br />
The full text of the press release can be found here:<br />
www.astrazeneca.com/Media/Pressreleases/Article/<br />
20120111--astrazeneca-and-ims-health<br />
For further information about <strong>IMS</strong> capabilities,<br />
please email Jon Resnick at Jresnick@imshealth.com<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 7
NEWS | <strong>IMS</strong> CORE DIABETES MODEL<br />
Strong research-focused investment maintains <strong>IMS</strong> CORE Diabetes Model at the<br />
forefront of decision support for diabetes.<br />
New validations enhance credibility of<br />
<strong>IMS</strong> CORE Diabetes Model<br />
Since 2011, <strong>IMS</strong> HEOR has undertaken extensive<br />
work on the validation and practical applications<br />
of its market leading <strong>IMS</strong> CORE Diabetes Model<br />
(CDM). Marking a continued commitment to<br />
ensuring robust, contemporary decision support in<br />
diabetes, the work has focused on enhancing the<br />
model's credibility and providing users with insight<br />
into the range of potential applications for the<br />
CDM. The results will ensure that evaluations of<br />
new technologies in diabetes are supported by a<br />
model that is at the forefront of health economic<br />
research in this area.<br />
Research abstracts have been submitted to several<br />
prestigious international conferences, including the ADA<br />
Scientific Sessions in Philadelphia and 1st Middle East<br />
Congress in Dubai; the EASD Meeting in Berlin; ISPOR in<br />
Washington, Berlin and Taipei; and the 2012 Mount Hood<br />
challenge in Baltimore – a particularly relevant platform for<br />
demonstrating the robustness of the CDM across a range of<br />
challenging validation exercises versus diabetes models from<br />
other research groups.<br />
Fully exploiting important new features of the CDM, such as<br />
modeling patient-level data, this latest <strong>IMS</strong> research also<br />
develops diabetes modeling methodology. Some of the key<br />
studies covering validation, applications, methodologies and<br />
cost are summarized below:<br />
MODEL VALIDATION<br />
• Type 1 and Type 2 long-term diabetes outcomes trials:<br />
Driven by extensive use of the CDM to estimate long-term<br />
clinical outcomes in diabetes, the goal of this study was<br />
to validate the model to trial data over a 20-30 year<br />
horizon against long-term observations of the DCCT (EDIC)<br />
and UKPDS, and to compare those to short- or<br />
intermediate time validations over 5 (Type 1) and 10 (Type<br />
2) years. In Type 1 diabetes, simulations produced R 2<br />
values of 0.9 and 0.67 against 5-year and 30-year followup<br />
studies respectively. In Type 2 diabetes, R2 values of<br />
0.89 and 0.86 were produced for intensive and<br />
conventional treatment in both short- and long-term<br />
observations. The study supports the CDM as a credible<br />
policy support tool for extrapolating health outcomes in<br />
DCCT and UKPDS like populations. 1<br />
• Risk-to-benefit ratio of glucose-lowering therapies in<br />
high cardiovascular risk Type 2 diabetes: In this study,<br />
the CDM was populated with characteristics consistent<br />
with the ACCORD trial to compare predicted 5-year relative<br />
risks of cardiovascular morbidity and all cause mortality<br />
to random effects meta-analysis of ACCORD, ADVANCE and<br />
VADT. Results were extrapolated over a lifetime to derive<br />
overall expected benefit. The CDM 5-year relative risk<br />
reductions associated with intensive glucose control in<br />
high-risk Type 2 diabetes patients were consistent with<br />
meta-analysis results and fell within the 95% confidence<br />
intervals. Long-term projections suggest intensive therapy<br />
contributes to both increased life and quality adjusted life<br />
expectancy. 2<br />
PRACTICAL APPLICATIONS OF<br />
CONTEMPORARY ISSUES<br />
• Relationship between effect of glycemic control and<br />
avoided symptomatic hypoglycemia on QoL in Type 2<br />
diabetes: Achieving optimal glycemic control (GC) while<br />
avoiding hypoglycemia is the basis of diabetes<br />
management. Tight GC, while reducing macro and<br />
microvascular complications also promotes hypoglycemia<br />
thus representing a barrier to low HbA1c values and<br />
directly impacting costs and health utility. Using the CDM,<br />
this equilibrium analysis showed that an HbA1c reduction<br />
of 0.54% is needed to achieve the same QoL benefit as<br />
achieved by avoiding one event of non-severe<br />
symptomatic hypoglycemia (NSHE) per year. The analysis<br />
is noteworthy in demonstrating the significant<br />
contribution to QALE by avoiding NSHE; particularly in<br />
comparison with levels of HbA1c change typically<br />
associated with current anti-hyperglycemic agents. The<br />
avoidance of NSHE is at least as powerful a driver of QALE<br />
as lowering HbA1c.<br />
continued opposite<br />
PAGE 8 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
• Significance of HbA1c durability in costeffectiveness<br />
analysis of second-line oral therapies<br />
in Type 2 diabetes: Patients with Type 2 diabetes<br />
generally require dose escalation and/or combination<br />
therapies to maintain acceptable glycemic control (GC).<br />
Time to escalation is a function of initial treatment<br />
effect and durability of GC. Durability can be assumed<br />
to be a key driver of cost-effectiveness especially when<br />
rescue therapies are expensive. The influence of<br />
different durability assumptions was explored in the<br />
CDM which evaluated scenarios to compare<br />
sulphonylurea vs DPP-4s as second-line therapies added<br />
to metformin, followed by insulin rescue therapy. CDM<br />
projections demonstrated that the annual rate of<br />
increase in HbA1c exerts considerable influence over<br />
predicted cost-effectiveness and is therefore an<br />
important variable in assessing value for money of new<br />
interventions for Type 2 diabetes.<br />
METHODOLOGICAL ASPECTS OF<br />
DIABETES MODELING<br />
• Correlating cost-effectiveness output with patientlevel<br />
data input: The CDM was used to ascertain if<br />
particular patient-level data (PLD) input profiles were<br />
predictive of cost-effectiveness sub-groups in Type 2<br />
diabetes subjects treated with second-line oral<br />
therapies. A series of patient characteristics were<br />
identified as being associated with greater potential for<br />
health gain. The study showed that the analysis of PLD,<br />
alongside simulation model output, provides an<br />
additional mechanism for informing healthcare<br />
decision making. 3<br />
• Reducing Monte Carlo error in stochastic<br />
simulations: This study sought to quantify the<br />
minimum run-time requirements for reducing Monte<br />
Carlo error to acceptable levels in probabilistic<br />
sensitivity analysis (PSA). Conducted with the CDM, it<br />
showed how Monte Carlo error can be quantified and<br />
put into context versus expected parameter uncertainty<br />
and further demonstrated that the degree of input<br />
parameter variability has an influence on the run-time<br />
requirements to reduce Monte Carlo error. 4<br />
<strong>IMS</strong> CORE DIABETES MODEL | NEWS<br />
COST QUANTIFICATION<br />
• Direct medical costs of diabetes mellitus in China:<br />
This research used the CDM to estimate annual cost of<br />
illness for all patients and lifetime diabetes costs for<br />
diagnosed patients in China. The 2011 cost of diabetes<br />
was estimated as CNY 13,326 per diagnosed patient and<br />
CNY 4,727 per undiagnosed patient, with the difference<br />
attributable to diabetes treatment and management costs.<br />
Based on a total population approaching 1.4 billion and<br />
previously reported disease prevalence rates, the national<br />
cost of diabetes in 2011 was estimated as CNY 1,214<br />
billion. In diagnosed patients the lifetime cost of diabetes<br />
was estimated as CNY 301,716 per patient (or CNY 18,253<br />
billion nationally); diabetes complications comprised 53%<br />
of the lifetime cost burden. 5 •<br />
For further information on recent research with the <strong>IMS</strong><br />
CORE Diabetes Model, please email David Grant, Senior<br />
Principal HEOR, <strong>IMS</strong> <strong>Health</strong> at Dgrant@uk.imshealth.com<br />
The <strong>IMS</strong> CDM allows comparison and correlation of input profile<br />
vs. output from patient-level data for each included patient –<br />
thereby offering the possibility of sub-group analysis. The graph<br />
below shows, for example, that patients with higher A1c level at<br />
baseline had a higher chance of being cost-effective vs. patients<br />
with lower levels.<br />
1 Validation of the CORE Diabetes Model to type 1 and type 2 long-term diabetes outcomes trials. Accepted as poster presentation at ADA, Philadelphia, June 2012<br />
2 Validation and evaluation of the risk-to-benefit ratio of glucose lowering therapies in high cardiovascular risk type 2 diabetes patients; Modeled projections<br />
using the CORE diabetes model. Accepted as oral presentation at ADA, Philadelphia, June 2012<br />
3 Correlating cost effectiveness output with patient level data input via the <strong>IMS</strong> Core Diabetes Model (CDM). Accepted at Mount Hood 2012 Challenge, Baltimore.<br />
4 Minimum run-time requirements to reduce Monte Carlo error in stochastic simulations. Accepted at Mount Hood 2012 Challenge, Baltimore<br />
5 Direct medical costs of diabetes mellitus in China: Annual cost of illness and long-term projections using a validated diabetes model. Accepted at ISPOR<br />
5th Asia Pacific Conference, Taipei, Sept 2012<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 9
INSIGHTS | REAL-WORLD EVIDENCE<br />
The increasing demand for real-world evidence by a<br />
growing body of decision makers is creating a need for<br />
new capabilities, data considerations, and<br />
effective planning for RWE generation across the entire<br />
product lifecycle.<br />
The authors<br />
Jon Resnick, MBA<br />
is Vice President Real-World Evidence Solutions, <strong>IMS</strong> <strong>Health</strong><br />
Jresnick@uk.imshealth.com<br />
Jacco Keja, PHD<br />
is Regional Principal HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Jkeja@nl.imshealth.com<br />
PAGE 10 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
A global plan for success<br />
REAL-WORLD EVIDENCE | INSIGHTS<br />
Preparing for a lifecycle of<br />
real-world evidence<br />
The concept of real-world evidence (RWE) is not a new one: researchers have been<br />
generating RWE to support product use among physicians and payers for nearly 20 years.<br />
However, recent growth in the demand for RWE to inform market access decisions has<br />
shifted the timeframe over which value is determined far into the post-launch lifecycle<br />
with significant implications for manufacturers.<br />
Traditionally, much of the work already completed for market access at the time of launch was<br />
based on evidence from randomized clinical trials (RCTs). While these remain the gold<br />
standard for demonstrating product safety and efficacy, the inherent limitations of their data –<br />
small sample size, controlled environment and focus on short-term outcomes – meant<br />
negotiations were primarily focused on qualitative documentation of value. Quantification was<br />
mainly extrapolated using health economic modeling.<br />
Increased payer interest in RWE reflects a shift toward more quantitative measurements of<br />
value and acceptance of data sources and endpoints that are not explicitly derived from RCTs.<br />
This comes with growing acknowledgment that while RWE may have limitations in data<br />
quality relative to RCTs, its findings are more relevant to the payer perspective. Regulators,<br />
too, recognize the value of RWE on safety, relative to that offered by RCTs.<br />
Other trends are also broadening the use of RWE. In recent years, payers have been<br />
experimenting with approaches that shift the risk to manufacturers, such as value-based<br />
contracting and conditional reimbursement or access, as well as to other stakeholders through<br />
pay-for-performance and consumer-directed plans. Disease management pilots with riskshifting<br />
consequences are also underway in several European countries. These developments<br />
converge with another important trend - the deferral of risk to healthcare practitioners, who<br />
need to understand in detail the right patient for a product and the way in which treatment<br />
algorithms can be optimized in the real world. If these models form the basis of future practice<br />
in healthcare delivery, RWE perspectives and endpoints will need to start resonating with the<br />
broader range of stakeholders, including providers and patients, who have been delegated more<br />
decision-making power.<br />
The future for RWE is one of certain challenge for all key stakeholders as scientific advancements<br />
and external dynamics place increasing demands on decision making. However, it is also one of<br />
tremendous potential for the expanded role of RWE.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 11
INSIGHTS | REAL-WORLD EVIDENCE<br />
EVOLVING PATTERNS OF USE<br />
Currently, there is no global or regional model for the practical application of RWE: requests<br />
vary in the intended use of findings, the timing during the product lifecycle when<br />
manufacturers are expected to product RWE, and the endpoints or analyses that are prioritized<br />
when making RWE-supported decisions. In key markets, these mainly concern the permitted<br />
use of a product, although in some cases, market access or pricing is becoming conditional on<br />
the results of RWE studies (Figure 1). There is also localized interest in using RWE for labeling<br />
modifications, further entrenching product positioning based on post-launch evaluations. Over<br />
time, both the number of countries requiring RWE and the scope of its application will<br />
continue to expand, further increasing the heterogeneity of the market access landscape.<br />
FIGURE 1: EXAMPLES OF NATIONAL VARIATION IN THE APPLICATION OF RWE<br />
Application<br />
Country Context Label Price Market<br />
access<br />
Use<br />
Germany AMNOG ruling specifies that prices are to be<br />
re-asssessed post-launch<br />
France Drug utilization studies specified as a condition<br />
of market access, pharmacovigilance<br />
Sweden Observational data used in post-launch<br />
decision making<br />
Spain Phase IV studies potentially influencing regional<br />
payer decisions<br />
UK Value-based pricing will potentially re-assess<br />
price post-launch<br />
US Private payer attention to Patient-Centered<br />
Outcomes Research Institute, private comparative<br />
effectiveness research, Food and Drug<br />
Administration Modernization Act Section 114<br />
DEVELOPING A LIFECYCLE RWE PLAN<br />
No application Limited application Application<br />
The complexity of logistics involved in fulfilling each country's RWE requirements calls for a<br />
heterogeneous approach, and fundamentally, early planning, to ensure the quality of responses,<br />
rational RWE spend throughout the lifecycle, and pro-activity to differentiation and<br />
positioning. This will be dependent on:<br />
1. Careful and routinely updated analysis of current and future comparators, drilling down to<br />
actual/perceived differentiation on specific claims, to enable tactical planning of individual<br />
studies to address those differentiation claims.<br />
2. A long-term view of supporting a product's claims with analyses of specific data sources,<br />
based on early inventory/vetting of databases that could support RWE studies of individual<br />
claims, and specific plans to address gaps by creating data sources where they are unavailable.<br />
PAGE 12 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
REAL-WORLD EVIDENCE | INSIGHTS<br />
3. A tactical evidence-generation plan enabling prioritization of data acquisition and<br />
analyses, both to anticipate external demands and to maximize the execution of a<br />
differentiation strategy.<br />
Ideally, the lifecycle plan should be initiated no later than Phase II; some subsequent data<br />
development activities may require a head start several years before launch. It may be<br />
appropriate to start these plans at therapy area or indication level when pipelines include<br />
multiple similar candidates, to mitigate the risks of early investment in RWE planning.<br />
1. Comparators<br />
• Pre-launch: RWE should focus here on documenting the real-world performance of<br />
existing comparators and the standard of care, particularly relative to the claims/endpoints<br />
that are central to the Target Product Profile (TPP). Patient segmentation and market sizing<br />
should also be completed pre-launch.<br />
• Post-launch: RWE emphasis after launch should shift towards not only replicating RCT<br />
efficacy and safety findings in real-world settings, but also seeking explicit head-to-head<br />
differentiation from comparators in the real world. In addition to safety and efficacy claims,<br />
this should consider product usage characteristics, such as dose adjustments, adherence,<br />
appropriate use, and cost-consequences of treatment, which can influence its costeffectiveness<br />
or value equation.<br />
• Established products: A range of RWE studies can be valuable for established products<br />
facing new market entrants or the generic conversion of comparators. By this stage in its<br />
lifecycle, the large body of RWE evidence supporting a product’s safety, effectiveness and<br />
use can be viewed as a competitive advantage – while competitive intelligence on the<br />
expected profile of new entrants can inspire RWE studies that cement differentiation claims<br />
before they can launch. RWE can also enhance generic defense strategies, highlighting the<br />
magnitude of a product's differentiation to prevent discussions coming down to price<br />
reductions alone.<br />
2. Supporting claims<br />
Manufacturers are familiar with developing new evidence during R&D to secure approval of<br />
particular endpoints, such as patient-reported outcomes (PROs), as part of their<br />
labeling/promotional claims. However, this investment rarely extends to planning for these<br />
endpoints in RWE and manufacturers may be caught out by the fact that they are not easily<br />
accessible in commercialized datasets.<br />
A good example is patient adherence to medication which continues to present a major<br />
problem for treatment effectiveness. In the US, poor medication adherence is reported to be<br />
responsible for between 33 and 69 percent of all medication-related hospital admissions,<br />
resulting in a cost of approximately $100 billion a year. 1 The difficulty in understanding poor<br />
adherence is that many of its predictors are patient-related factors, such as cognition,<br />
motivation, and relationships with doctors – all issues which claims data cannot enlighten.<br />
Classic retrospective approaches also have many confounders and sources of bias to overcome,<br />
including frequent under-reporting of diagnoses as well errors in diagnosis. The rate of<br />
inconsistencies is particularly high in pain, psychiatric and behavioral disorders. Primary care<br />
providers have been found to detect major depressive disorder in only one-third to half of<br />
patients with this condition. 2<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 13
INSIGHTS | REAL-WORLD EVIDENCE<br />
Additionally, the scope of the data is often very limited. With the primary focus on health<br />
insurance claims, pharmacy records, hospital discharge data, GP electronic patient records, etc,<br />
many aspects are simply not documented. Consequently, while prescription data, hospital data,<br />
diagnostic codes, tests and procedures are often captured, the elements that provide deep<br />
insight into patient status and motivation, such as quality of life, severity of symptoms, and<br />
treatment satisfaction, are not.<br />
Given the increasing evaluation of these endpoints by payers for post-launch price and market<br />
access reviews, it is critical to plan for data development to maximize timely access to RWE<br />
for TTP claims.<br />
Broader perspectives<br />
By giving consideration to the stakeholders who may use RWE, manufacturers can expand<br />
their thinking about data sources and endpoints that will be available and relevant for RWEsupported<br />
claims.<br />
• Payers: As payers have embraced RWE, their mindset has been shaped by the availability of<br />
their own billing and reimbursement claims data. This has allowed them to consider effects<br />
over longer time horizons, and costs from more sites of care and more diverse populations,<br />
than have typically been available in RCTs. Today, a growing number of patient-level health<br />
data initiatives, particularly in the US, are being built around claims data assets for outcomes<br />
research. However, payer data sources typically exclude key information on patient health<br />
status that drives medical decision making meaning that an even broader range of<br />
perspectives is required.<br />
• Providers and patients: As the importance of providers and patients grows in considering<br />
RWE, value determinations will be based more on the perspectives of disease management<br />
than market access. The alternatives considered by physicians will be driven by the types of<br />
health status information they typically record in their charts, practice management systems,<br />
and electronic records. RWE findings must be responsive to this and stratify patient<br />
populations appropriately. Patient choice is dominated by very practical considerations of<br />
ease of use and perceptions of anticipated benefits: RWE will be more likely to persuade<br />
them if it clarifies the behavioral costs and consequences of particular treatments.<br />
Approaches that go beyond claims data are thus important to consider. Potential ways forward<br />
include patient charts, dedicated registries and observational methodologies. A high degree of<br />
sophistication will be essential to ensure the right level of granularity, as will the ability to<br />
couple different data sources to accommodate the sheer size of data assets required to reach a<br />
better understanding of patients and patient segmentation. This is a skill set that requires<br />
significant development, implying investment in enabling technologies and in turn,<br />
partnerships, transparency and trust.<br />
PAGE 14 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
3.Tactical planning<br />
VALUE OF COLLABORATION<br />
BENEFITS OF RWE PLANNING<br />
REAL-WORLD EVIDENCE | INSIGHTS<br />
The final step in the planning process is to outline the specific tactical studies and activities<br />
required to execute an effective RWE strategy. This involves integrating the list of internal<br />
desires and external demands for RWE <strong>insights</strong>, mapping out the geographies where requests<br />
are relevant, and sequencing them for efficient budget and staffing allocation.<br />
Companies may judge that certain claims do not require support in specific countries, based<br />
on an assessment of the RWE environment. It is better to actively decide against RWE tactics<br />
in certain regions based on the perceived gains than be forced into inaction because it is too<br />
late to identify appropriate data sources or execute quality analyses.<br />
Developing an inventory of RWE activities further enables companies to optimize spending<br />
when new data sources are required to support specific RWE claims, as well as facilitate<br />
communication between global headquarters and affiliates. It can further become a platform<br />
for headquarters to communicate product strategy early to affiliates, who can in turn validate<br />
assumptions regarding the fulfillment of local demands for RWE to the satisfaction of local<br />
HTA bodies.<br />
To effectively execute an RWE plan, companies will need to consider and collaborate with<br />
internal and external stakeholders who are not always part of the standard operating model for<br />
market access teams, including R&D. Much of the investment in R&D goes beyond just<br />
demonstrating an outcome; they are also required to understand the drivers of outcomes and<br />
the mechanisms that make treatments work. These perspectives will be invaluable as lifecycle<br />
plans incorporate endpoints on product use factors such as dosing and adherence. R&D<br />
perspectives are also more closely aligned with those of the providers who may ultimately<br />
consider RWE findings as they take on added risk for patient care.<br />
The future for RWE is one of certain challenge for all key stakeholders as scientific<br />
advancements and external dynamics place increasing demands on decision making. However,<br />
it is also one of tremendous potential for the expanded role of RWE. For manufacturers, the<br />
adoption of a global, coordinated, lifecycle plan for RWE needs will bring four key benefits:<br />
1. Enable efficiency gains to be realized by anticipating environmental and competitive<br />
developments and investing in timely analyses with minimal duplication of effort<br />
2. Ensure that the existing patchwork of data sources is effectively utilized to provide<br />
information for addressing internal and external needs<br />
3. Increase the chance that staff and budgets will be available to produce high quality responses<br />
4. Allow companies to effectively transition from passive or reactive players in evidence-based<br />
access to successful competitors and industry leaders<br />
Overall, these gains will translate into greater returns in markets with RWE opportunities and<br />
more rational investment to achieve those gains. RWE will be useful for all parties: for physicians<br />
to optimize care by finding exactly the right patient; for regulators to continuously monitor<br />
benefit/risk; for decision makers to devise policy on usage (including HTA agencies that assess<br />
cost-effectiveness); and for business-to-business negotiations between industry and payers. •<br />
1 Osterberg, L, Blaschke, T N. Adherence to medication. N Engl J Med, 2005; 353:487–497<br />
2 Institute for Clinical Systems Improvement. Major Depression in Adults in Primary Care, May 2011. http://www.icsi.org<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 15
INSIGHTS | PATIENT-REPORTED OUTCOMES<br />
Patient-reported outcomes (PROs) are an increasingly<br />
relevant decision-making tool for a growing audience of<br />
stakeholders, capturing first-hand the disease and<br />
treatment experience from a real-world, patient perspective.<br />
But alongside their growing significance are increasing<br />
expectations of their design and validity – meriting careful<br />
review of the attributes that must be considered.<br />
The authors<br />
Núria Lara Surinach, MD, MSC<br />
is Principal HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Nlara@es.imshealth.com<br />
Xavier Badia, MD, PHD, MPH<br />
is Senior Principal HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Xbadia@es.imshealth.com<br />
Núria Perulero, BSC<br />
is Director HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Nperulero@es.imshealth.com<br />
PAGE 16 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
PATIENT-REPORTED OUTCOMES | INSIGHTS<br />
Getting the measure of PROs<br />
A review of key considerations<br />
The importance of understanding a patient’s perception of their disease and the impact<br />
of treatment has become increasingly recognized in recent years. Today, a patient<br />
perspective, captured in patient-reported outcomes (PROs), is a key consideration in<br />
everyday practice as well as in clinical development (Figure 1).<br />
FIGURE 1: PROs ARE A MAJOR FOCUS FOR ALL KEY HEALTHCARE STAKEHOLDERS<br />
PRO GUIDELINES<br />
Sponsor<br />
• Ensure product provides<br />
benefits from a patient<br />
as well as clinical<br />
perspective<br />
Decision makers<br />
• Provide important<br />
information for product<br />
approval, pricing and<br />
reimbursement<br />
PROs<br />
Prescribers<br />
• Support optimal<br />
treatment decisions<br />
based on patient<br />
perception<br />
Patients<br />
• Enable greater patient<br />
involvement in clinical<br />
and therapeutic<br />
management<br />
The increasing use of PROs to support manufacturer claims for medical products has given rise<br />
to the publication of specific guidance by the US Food and Drug Administration (FDA) and<br />
the European Medicines Agency (EMA) on the development and application of these measures.<br />
The FDA, in guidelines on the use of PROs in labeling claims issued in 2009, defines a PRO<br />
as “any report of the status of a patient’s health condition that comes directly from the patient, without<br />
interpretation of the patient’s response by a clinician or anyone else. (…) In clinical trials, a PRO<br />
instrument can be used to measure the effect of a medical intervention on one or more concepts (…)”. 1<br />
According to the EMA, in a reflection paper on regulatory guidance for the use of healthrelated<br />
quality of life (HRQoL) measures in evaluating medicinal products, “any outcome<br />
evaluated directly by the patient himself and based on patient’s perception of a disease and its treatment(s)<br />
is called patient-reported outcome (PRO)”. 2<br />
The overarching term of “PROs” embraces all elements of patient-reported data, including<br />
treatment preference, satisfaction, and adherence as well as burden of symptoms and HRQoL<br />
(Figure 2 overleaf).<br />
Although recommendations for PRO development are not mandatory, the bar is now set very<br />
high, particularly for outcomes that are complex and multi-domain, such as HRQoL. Broad<br />
claims invariably give rise to concern at the FDA. Simple, single items and single-domain<br />
instruments require less documentation, assuming adequate validation. Careful examination and<br />
analysis of PRO instruments can provide useful <strong>insights</strong> for improving the chances of success.<br />
continued on next page<br />
ACCESSPOINT - ISSUE 4 PAGE 17
INSIGHTS | PATIENT-REPORTED OUTCOMES<br />
FIGURE 2: PROs COVER ALL PATIENT-REPORTED HEALTH DATA<br />
Preference<br />
to treatment<br />
Treatment or<br />
health service<br />
satisfaction<br />
KEY CONSIDERATIONS<br />
According to the FDA guidance, the use of a PRO instrument to support claims in medical<br />
product labeling includes consideration of:<br />
• Population enrolled in the clinical trial<br />
• Clinical trial objectives and design<br />
The attributes of PRO instruments reviewed by the FDA include:<br />
• Concepts being measured<br />
• Number of items<br />
• Conceptual framework of the instrument<br />
• Medical condition for intended use<br />
• Population for intended use<br />
• Data collection method of administration<br />
• Response options<br />
Adherence<br />
to treatment<br />
Burden of<br />
symptoms<br />
HRQoL<br />
• PRO instrument’s conceptual framework<br />
• PRO instrument’s measurement properties<br />
• Recall period<br />
• Scoring<br />
• Weighting of items or domains<br />
• Format<br />
• Respondent burden<br />
• Translation or cultural adaptation availability<br />
PSYCHOMETRIC PROPERTIES<br />
The principal measurement properties for PROs are validity, reliability and ability to<br />
detect change.<br />
1. Validity: The relevance of a PRO is evaluated in terms of both its content and<br />
construct validity.<br />
• Content validity: Requires evidence that the instrument in question measures the<br />
concept of interest. This includes evidence from qualitative studies that the items and<br />
domains of an instrument are appropriate and comprehensive relative to its intended<br />
measurement concept, population and use. Testing other measurement properties will not<br />
replace or rectify problems with content validity.<br />
• Construct validity: Requires evidence that relationships among items, domains and<br />
concepts conform to an a priori hypothesis concerning logical relationships that should<br />
exist with measures of related concepts or scores produced in similar or diverse patient<br />
groups.<br />
PAGE 18 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
PATIENT-REPORTED OUTCOMES | INSIGHTS<br />
2. Reliability: The reliability of a PRO is assessed on several levels.<br />
• Test/re-test or intra-interviewer reliability: Stability of scores over time when no<br />
change is expected in the concept of interest<br />
• Internal consistency as determined by:<br />
• Extent to which items comprising a scale measure the same concept<br />
• Inter-correlation of items that contribute to a score<br />
• Internal consistency<br />
• Inter-interviewer reliability (for interviewer-administered PROs only): Agreement<br />
among responses when the PRO is administered by two or more different interviewers<br />
3. Ability to detect change: This requires evidence that a PRO instrument can identify<br />
differences in scores over time in individuals or groups (similar to those in the clinical trials)<br />
who have changed with respect to the measurement concept.<br />
VALIDATION PROCESS<br />
The validation process follows the structure shown in Figure 3. This involves evaluating the<br />
ability of the PRO to detect change (Group A), ensuring sufficient time between visits to<br />
allow for a treatment effect; assessing test/re-test reliability (Group B), with time between visits<br />
appropriate to ensure patient stability; and thirdly, determining construct validity in the general<br />
population as a control (Group C).<br />
FIGURE 3: PRO VALIDATION PROCESS<br />
Group A: To evaluate ability<br />
to detect change<br />
Patients diagnosed who need clinical<br />
and/or therapeutic intervention<br />
Visit 1 Visit 1 Visit 1<br />
Visit 2<br />
Time between visits must be<br />
sufficient to allow for treatment<br />
effect<br />
Group B: To evaluate<br />
test/re-test reliability<br />
Patients diagnosed who are stable<br />
according to clinical criteria<br />
Visit 2<br />
Time between visits must be<br />
sufficient to ensure patient<br />
stability<br />
Group C (control): To evaluate<br />
construct validity<br />
General population<br />
Once the appropriate questionnaire has been chosen, the frequency of assessments needs to be<br />
defined. This should correspond with the length of recall asked by the instrument’s response<br />
options, the natural history of the disease condition, the nature of treatment, the measurement<br />
properties and the specific research questions being addressed. Some diseases, conditions, or<br />
clinical trial designs may necessitate more than one baseline assessment and several PRO<br />
assessments during treatment.<br />
DEMONSTRATING QoL BENEFITS WITH A PRO QUESTIONNAIRE<br />
<strong>IMS</strong> HEOR has many years experience in developing and validating disease-specific<br />
questionnaires incorporating relevant patient-reported outcomes - an example<br />
is presented overleaf...<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 19
INSIGHTS | PATIENT-REPORTED OUTCOMES<br />
Case in practice: Demonstrating QoL benefits with a PRO questionnaire<br />
One recent case study involved a large international pharmaceutical company that wished to explore<br />
the impact of a particular disease on quality of life (QoL) and show that as well as being more<br />
effective, their new product also significantly improved QoL relative to its competitors. The<br />
involvement of key opinion leaders and a high number of physicians would be key to providing new<br />
arguments for increasing market access and demonstrating superior outcomes. These would be supported<br />
by a strong value communication plan to disseminate the results in national and international<br />
journals and congress communications and to underscore the company’s core scientific orientation.<br />
PRO questionnaire: <strong>IMS</strong> proposed the development and validation of a specific QoL questionnaire<br />
for patients with the disease in question. The two-stage process involved first the design of the<br />
questionnaire, leveraging input from an expert focus group, in-depth patient interviews, a consensus<br />
group of experts and a patient pilot to assess the questionnaire’s measurement properties; and<br />
secondly, comprehensive validation using an observational, naturalistic and prospective study with a<br />
sample of more than 200 patients (Figure 4).<br />
FIGURE 4: TWO-STAGE PROCESS TO STUDY DESIGN<br />
Phase 1: Questionnaire development<br />
Phase 2: Questionnaire validation<br />
(observational, naturalistic and prospective<br />
study with sample of more than 200 patients)<br />
Baseline visit<br />
Visit 1: certain period of time after baseline visit<br />
Visit 2: certain period of time after baseline visit<br />
Focus group with experts<br />
Interviews with patients<br />
Consensus group of experts<br />
Pilot study with patients<br />
Objective: to assess QoL before and after<br />
therapeutic intervention<br />
Relevant, reliable tool: The resulting questionnaire was short and its scoring system easy to<br />
administer in routine clinical practice. The questionnaire was shown to be a relevant tool under realworld<br />
conditions in terms of reliability, validity and sensitivity to change. In addition to QoL, other<br />
patient-based variables, such as treatment satisfaction and therapeutic compliance, were assessed<br />
with very positive results for the company’s product.<br />
Robust scientific validation of benefits: With patient-reported evidence demonstrating the disease<br />
impact on QoL, the company was able to position the product accordingly and communicate its benefits on<br />
the basis of proven clinical effectiveness and improved QoL. The involvement of multiple disease specialists<br />
significantly strengthened messaging to the scientific community. •<br />
1 Guidance for industry. Patient-reported outcome measures: Use in medical product development to support labeling claims. Accessed May 11, 2012 at:<br />
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM193282<br />
2 Reflection paper on the regulatory guidance for the use of health-related quality of life (HRQL) measures in the evaluation of medicinal products.<br />
Accessed May 11, 2012 at: http://www.emea.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003637.pdf<br />
PAGE 20 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
DRUG EXPOSURE MEASUREMENT | INSIGHTS<br />
Standardizing the measurement<br />
of drug exposure<br />
The ability to determine drug exposure in real-world clinical<br />
practice enables important <strong>insights</strong> for the optimal use of<br />
medicines and healthcare resources. With significant<br />
potential for treatment complexities to confound the<br />
measurement process, finding valid approaches to<br />
standardization can be key to meaningful results.<br />
Here we consider a recent case study in asthma.<br />
The author<br />
Christopher Blanchette, PHD, MS, MA<br />
is Principal HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Cblanchette@us.imshealth.com<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 21
INSIGHTS | DRUG EXPOSURE MEASUREMENT<br />
Standardizing the measurement<br />
of drug exposure<br />
A case study in asthma<br />
The measurement of drug treatment exposure can be complex, based on the underlying<br />
assumptions that drive the product’s use. These are most easily encountered with the<br />
classic 30-day prescription fills of oral medications. However, in cases where medications<br />
are prescribed as needed, where various routes of administration apply, or where dosing<br />
is inconsistent across diverse generics manufacturers, the accurate measurement of drug<br />
exposure becomes significantly more involved.<br />
STUDY DESIGN<br />
CAPTURING DATA<br />
All three of these issues were encountered in a series of studies assessing short-acting beta<br />
agonists (SABA) exposure as a predictor of subsequent asthma-related exacerbations, most<br />
notably dealing with as-needed prescribing of SABA in either a metered dose inhaler (MDI)<br />
or in a nebulized inhalant form. 1,2,3,4,5<br />
This retrospective analysis included both prevalent and incident asthmatics, to assess patients<br />
with various levels of severity during the available observation period (Figure 1). For all<br />
analyses, evaluations were performed for three groups: all subjects (ages 6-56 years), pediatrics<br />
(ages 6-17 years) and adults (ages 18-56 years).<br />
Data were obtained on subjects enrolled in a health plan that participated in the PharMetrics<br />
Patient-Centric Database between July 1, 2003 and June 30, 2007. The database comprises<br />
information from enrollment files as well as facility, professional service and out-patient<br />
pharmacy claims, from a variety of private healthcare benefit plans. Its coverage extends to<br />
more than 40 million patients enrolled in over 70 health plans across the US, with health plans<br />
providing data on a continuous basis. The number of plans contributing to the PharMetrics<br />
FIGURE 1: RETROSPECTIVE STUDY DESIGN<br />
Baseline and medical<br />
characteristics assessed<br />
Q1 SABA use<br />
Q2<br />
exacerbation<br />
risk<br />
Q2 SABA use<br />
1 year pre-index period Index<br />
date<br />
1 year post-index period<br />
Q3<br />
exacerbation<br />
risk Q4<br />
Q3 SABA use exacerbation<br />
risk<br />
Q1 Q2 Q3 Q4<br />
PAGE 22 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
DRUG EXPOSURE MEASUREMENT | INSIGHTS<br />
dataset has increased over time. Demographic information (excluding race and ethnicity) is<br />
available for all patients. Most plans also provide information on dates of eligibility for medical<br />
and out-patient pharmacy benefits.<br />
Data available for each out-patient pharmacy claim (“prescription”) included the drug<br />
dispensed (in National Drug Code [NDC] format) and the dispensing date. Most plans also<br />
provided information on the quantity and number of therapy days dispensed. Data available for<br />
each facility or professional service claim (“medical claim”) include dates of service and<br />
International Classification of Diseases 9th Edition, Clinical Modification (ICD-9-CM)<br />
diagnosis codes and ICD-9-CM procedure codes (facility claims) or Current Procedural<br />
Terminology, Version 4 (CPT-4) procedure codes (professional service claims). All plans<br />
provided information on payments. Most plans also provided information on billed charges.<br />
Payments were imputed for claims with missing payment information (due to capitation<br />
arrangements). All claims for any given person could be linked using a unique encrypted identifier.<br />
The dataset is fully de-identified and HIPAA compliant.<br />
The criteria applied for the study population were as follows:<br />
Inclusion<br />
• Patients aged 6–56 years on the index date<br />
• Continuous enrollment in a health plan in the database for 2 years<br />
• Claim with asthma diagnosis (ICD-9 code 493.XX)<br />
• Claim for either a SABA or any asthma controller medication in each of the pre-index and<br />
post-index periods<br />
Exclusion<br />
• Any diagnosis of COPD, emphysema, chronic bronchitis, or bronchiectasis<br />
• Subjects with diagnoses requiring frequent oral corticosteroid (OCS) use<br />
• Subjects with a diagnosis of respiratory tract cancer<br />
DRUG EXPOSURE EVALUATION APPROACH<br />
Since pharmacy use can only be identified in the PharMetrics dataset using National Drug<br />
Codes (NDC), the first step was to compile an exhaustive list of NDCs for each drug of<br />
interest. The starting point for this was to link the list of identified brand and proprietary drug<br />
names to the in-house, composite drug dictionary.<br />
SABA dosing exposure standardization was determined through prior studies. These included<br />
the 2002 evaluation by Glauber and Fuhlbrigge which provided a compelling argument for<br />
using a canister-equivalent measure, comprised by inhaled and nebulized SABA, instead of just<br />
simple counts of medication. 6<br />
They introduced a scheme for standardizing doses of inhaled and nebulized SABA equivalent<br />
to two inhalations of albuterol, dispensed from a metered dose inhaler (MDI) as the standard<br />
for comparison.<br />
Using a high threshold level of >8 SABA canisters (counts method) or >8 canister-equivalents,<br />
the canister-equivalent method increased the population identified as having high SABA use<br />
by 39% (16.6% vs. 11.9%) relative to the simple-count method.<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 23
INSIGHTS | DRUG EXPOSURE MEASUREMENT<br />
Hospitalization<br />
ED/UC Visit<br />
OCS claim<br />
Any of the above<br />
Thus, in studies that do not recognize the use of nebulized SABA there is likely to be<br />
substantial misclassification of patient risk based on high SABA utilization.<br />
The present study utilized the method described by Chan, et al, 7 being inclusive of almost all<br />
MDI and nebulized SABA types identified in the dataset. Canister equivalents were<br />
determined for each claim represented. A standard SABA canister size was defined to be one<br />
containing 200 metered actuations, which encompassed more than 97% of MDI SABA claims.<br />
More than 96% of total SABA MDI claims were for albuterol; 2.2% were for pirbuterol; and<br />
1.6% were for levalbuterol. In the case of pirbuterol, whose standard dispensing contains 400<br />
actuations, claims were set to two canisters. Levalbuterol was considered to be equivalent in<br />
potency to albuterol. In cases where insufficient information was available to make the<br />
determination, canister size was imputed using days supply of medication. Thirty days supply or<br />
less was determined to be equivalent to one canister, 31 to 60 days supply as two canisters, etc.<br />
FIGURE 2: SABA CANISTER FILLS 2ND QUARTER (POST-INDEX YEAR)<br />
N=93,444<br />
0 Canisters<br />
1 ⁄2-3 Canisters<br />
> 3 Canisters<br />
0 5 10 15 20<br />
0 Canisters (n=59,653) Percentage of Patients<br />
1 ⁄2-3 Canisters (n= 26,525)<br />
> 3 Canisters (n= 4,266)<br />
32%<br />
5%<br />
64%<br />
FIGURE 3: Q3 EXACERBATION INCIDENCE BY Q2 SABA USE STRATA<br />
ED = Emergency department<br />
UC = Urgent care<br />
OCS = Oral corticosteroid<br />
Nebulized SABA canister claims comprised<br />
12% of all SABA claims. Based on the Chan<br />
study method, canister-equivalents were<br />
derived for each nebulized SABA claim.<br />
The vast majority of these claims were for<br />
albuterol or levalbuterol (considered<br />
equivalent in potency to albuterol), in which<br />
case one 3ml ampule was equivalent to 0.02<br />
canister-equivalents, making fifty ampules of<br />
3ml of medication equivalent to one canister.<br />
The quantity of medicine is typically given in<br />
ml in the dataset. Each ampule typically<br />
contains 3ml of medicine and is most often<br />
dispensed in boxes of 24, 25 or 30, each of<br />
which was equated to a half canister of SABA.<br />
It was determined that the most accurate<br />
method to represent these medication<br />
quantities was to round to the nearest halfcanister<br />
because most boxes contained 24, 25<br />
or 30 ampules and most claims were in<br />
multiples of these. Less than 1% of claims<br />
observed were clear outliers (eg, >180<br />
ampules). For these, the maximum dose was<br />
capped at three canister equivalents per claim.<br />
Due to the heterogeneity of asthma<br />
controller medications, it was elected to use<br />
annual days supply during the pre-index and<br />
post-index years, and days supply per quarter<br />
for the quarterly analysis regardless of the<br />
medication being inhaled (eg, ICS) or oral<br />
(eg, leukotriene modifiers). Controller<br />
medications prescribed concomitantly and<br />
measured as covariates were assessed as the<br />
sum of days supply provided on the claims,<br />
a proxy for days of exposure. A similar<br />
method was used to describe use of nasal<br />
steroid sprays and antibiotics.<br />
PAGE 24 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
CONCLUSIONS<br />
DRUG EXPOSURE MEASUREMENT | INSIGHTS<br />
FIGURE 4: RISK OF EXACERBATIONS BY Q2 SABA STRATA (REFERENCE=0 CANISTERS)<br />
Hospitalization<br />
1/2 -3<br />
>3<br />
ED/UC Visit<br />
1/2 -3<br />
>3<br />
OCS claim<br />
1/2 -3<br />
>3<br />
Any of the above<br />
1/2 -3<br />
>3<br />
1 2 3<br />
ED = Emergency department<br />
UC = Urgent care<br />
OCS = Oral corticosteroid<br />
4<br />
Odds Ratio (95% CI)<br />
5 6<br />
All oral corticosteroid (OCS) claims, regardless of days supplied, were counted as one claim.<br />
Ninety percent of prescription dispensing for OCS was found to be for 21 days or less. In the<br />
analysis, OCS were evaluated as a binary variable for the presence of one or more claims, and<br />
as a count of claims during the specified time period. Injectable corticosteroids were not<br />
captured, since these are typically administered in a physician’s office and are rarely registered<br />
as NDC-based claims.<br />
The study found that a quarterly assessment of SABA utilization can be used to identify<br />
patients at risk for asthma-related exacerbations. The incidence of an asthma exacerbation was<br />
associated with greater SABA use in the previous quarter (Figures 2,3,4).Variability in SABA<br />
exposure measurement and standardization between nebulized and MDI routes may have<br />
provided biased estimates on associated cost and asthma-related exacerbations.<br />
Notwithstanding this caveat, however, these findings provided critical <strong>insights</strong> for optimizing<br />
the treatment and management of asthma patients. •<br />
1 Blanchette CM, Silver H, Petersen H, Kamble S, Meddis D, Gutierrez B. Quarterly assessment of short-acting ß-agonist use as a predictor of subsequent<br />
healthcare services use for asthmatics in the US. ISPOR 14th Annual International Meeting, Orlando, FL; May 16-20, 2009.<br />
2 Blanchette CM, Silver H, Petersen H, Kamble S, Meddis D, Gutierrez B. Identification of a threshold for high utilization of short-acting ß2-agonists in a<br />
commercially insured adult asthmatic population in the United States. American Academy for Asthma, Allergy, and Immunology 2009 Annual Meeting,<br />
Washington, DC; March 13-17, 2009.<br />
3 Silver H, Blanchette CM, Petersen H, Kamble S, Meddis D, Gutierrez B. Short-acting beta agonist utilization and risk of asthma exacerbation among a<br />
commercially insured pediatric population in the United States. American Academy for Asthma, Allergy, and Immunology 2009 Annual Meeting;<br />
Washington, DC; March 13-17, 2009.<br />
4 Silver HS, Blanchette CM, Kamble S, Petersen H, Letter M, Meddis D, Gutierrez B. Relationship between short-acting ß2-adrenergic agonist use and<br />
healthcare costs. American Journal of Managed Care. 2011 Jan; 17(1):19-27.<br />
5 Silver HS, Blanchette CM, Kamble S, Petersen H, Letter M, Meddis D, Gutierrez B. Quarterly assessment of short-acting ß2-adrenergic agonist use as a<br />
predictor of subsequent health care use for asthmatic patients in the United States. Journal of Asthma. 2010 Aug; 47(6):660-6.<br />
6 Glauber JH, Fuhlbrigge AL. Stratifying asthma populations by medication use: How you count counts. Ann Allergy Asthma Immunol. 2002; 88:451-456.<br />
7 Chan J, Hui RL, Spence MM. Effects on resource utilization of adding salmeterol in combination or separately to inhaled corticosteroids. J Manag Care<br />
Pharm. Jan-Feb 2007; 13(1):21-27.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 25
INSIGHTS | INDIRECT TREATMENT COMPARISONS<br />
Direct evidence from randomized trials remains the ultimate<br />
gauge of relative value when comparing competing technologies.<br />
In its absence, the need for indirect methods is becoming<br />
increasingly accepted. Here, we consider the growing role of<br />
network meta-analysis and its evolving capabilities as a key<br />
enabler of indirect treatment comparisons.<br />
The authors<br />
Mark Lamotte, MD<br />
is Principal HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Mlamotte@be.imshealth.com<br />
Karen Moeremans, MD<br />
is Director HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Kmoeremans@be.imshealth.com<br />
Tiago Fonseca, MSC<br />
is Consultant HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Tfonseca@uk.imshealth.com<br />
Stijn Vandekerckhove, MSC<br />
is Analyst HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Svandekerckhove@be.imshealth.com<br />
PAGE 26 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
INDIRECT TREATMENT COMPARISONS | INSIGHTS<br />
Accounting for direct evidence gaps<br />
with indirect treatment comparisons<br />
Growing potential of network meta-analysis<br />
Direct, head-to-head comparisons via robustly designed randomized controlled clinical<br />
trials (RCTs) are still considered the gold standard for assessing the relative efficacy and<br />
safety of competing treatments. Where there are multiple trials of two interventions,<br />
pair-wise meta-analyses may be performed to obtain a pooled estimate and respective<br />
confidence interval for the relative efficacy of the target treatments, taking account of<br />
all available direct evidence. However, direct evidence is often lacking.<br />
Several factors can contribute to critical gaps in the necessary head-to-head RCT evidence base:<br />
• RCTs supporting drug licensing approval only, often compare the new intervention with<br />
placebo; industry perceptions of excessive risk negate the commercial incentive to compare<br />
with an active control.<br />
• Even if an active comparator is included in the RCT, it may not be relevant in all settings<br />
• As new evidence continues to be generated, available treatments change/increase over time.<br />
This is particularly true for hematologic diseases and oncology. A recent <strong>IMS</strong> research<br />
project identified 115 Phase III trials, including more than 80 alternative therapy regimens,<br />
for the management of advanced non-small cell lung cancer over the last decade alone.<br />
Thus, for some indications, it is unfeasible to incorporate all the competing interventions in<br />
a single clinical trial. Furthermore, the most relevant comparator at the time of assessment<br />
may well differ from the standard at the time of trial design.<br />
These shortfalls in direct evidence impose challenges for the assessment of treatment pathways,<br />
leaving clinicians, patients, and health policy makers with an incomplete picture in<br />
determining which treatments are the most effective (and cost-effective).<br />
TAKING THE INDIRECT ROUTE<br />
In cases where direct evidence is insufficient or non-existent, indirect comparisons and mixed<br />
treatment comparisons, also known as network meta-analyses (NMAs), can provide the<br />
opportunity to compare what may not otherwise have been compared. NMAs represent<br />
extensions of the pair-wise meta-analysis1 : rather than pooling information on trials<br />
comparing treatments A and B, as in pair-wise meta-analysis, NMA combines data from<br />
different randomized comparisons: A vs B; A vs C; A vs D; and so on (Figure 1 overleaf).<br />
Additional advantages of NMAs include the increase in sample size derived from the<br />
combination of studies, and the systematic and quantitative nature of the synthesis, enabling a<br />
full assessment of uncertainty about the relative results. Furthermore, NMAs allow<br />
quantification of relative treatment effects (eg, odds ratio, relative risk, or difference in change<br />
from baseline) of different therapeutic classes (eg, Glucagon-like peptide-1 (GLP-1) receptor<br />
agonists and insulins), different drugs within the same class (eg, exenatide and liraglutide), and<br />
different doses of the same drug (eg, exenatide BID or QW vs liraglutide 1.2mg or 1.8mg).<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 27
INSIGHTS | INDIRECT TREATMENT COMPARISONS<br />
FIGURE 1: META-ANALYSIS AND NETWORK META-ANALYSIS<br />
A B A A<br />
Direct comparison<br />
Direct evidence<br />
TRIAL SELECTION KEY TO QUALITY<br />
To ensure that all relevant trials are considered for inclusion, ideally the potentially eligible<br />
studies should be identified via a systematic review.<br />
In order to obtain an internally consistent set of estimates, while respecting the randomization<br />
in the evidence, the underlying assumption is that the trials included are sufficiently<br />
homogeneous to be quantitatively combined, via a common comparator. This assumption<br />
requires not only similarity of trial populations (in- and exclusion criteria, patient<br />
characteristics, etc) but also methodological similarity (eg, trial quality, definition of outcomes,<br />
randomization method, etc). An example of consistency is that the treatment effect estimated<br />
by the BC trials would be the same as the treatment effect estimated by the AC and AB trials if<br />
they had included B and C arms.<br />
Trial quality should be sufficient for consideration. It is important to bear in mind that a set of<br />
badly conducted studies does not lead to a good analysis; hence, the importance of defining a<br />
coherent set of inclusion and exclusion criteria at an initial stage – usually when systematically<br />
reviewing the literature.<br />
PAGE 28 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH<br />
B<br />
C C<br />
Indirect comparison Mixed treatment comparison<br />
Meta-analysis Network meta-analysis<br />
D<br />
Indirect evidence<br />
NMAs enable the evaluation of competing treatment options that may not otherwise have been<br />
directly compared. Although the level of evidence they generate may be perceived to be inferior to<br />
that of gold standard RCTs, they nevertheless have important strengths.<br />
B
INDIRECT TREATMENT COMPARISONS | INSIGHTS<br />
FIGURE 2: EMBASE SEARCH RESULTS REVEAL MARKED RISE IN NMA, INDIRECT OR MIXED TREATMENT COMPARISONS<br />
Number<br />
of hits<br />
700<br />
600<br />
500<br />
400<br />
300<br />
200<br />
100<br />
Hits<br />
INCREASINGLY ACCEPTED ALTERNATIVE<br />
0 1992-1997 1997-2002<br />
2002-2007 2007-2012<br />
(week 15)<br />
Today, the use of NMA methods is becoming more widespread and, possibly as a consequence,<br />
more widely accepted in informing healthcare stakeholders. An ad hoc search in EMBASE,<br />
using "network meta-analysis”, “indirect comparison” and “mixed treatment comparison” as<br />
search terms, identified more than 640 publications between 2007 and 2012 with any of these<br />
words in the title, abstract or as key word fields. Between 1992 and 1997 this number was only<br />
12 (Figure 2). Experience at <strong>IMS</strong> confirms this trend, with an increase in client requests for<br />
these types of studies, primarily in support of market access submissions as well as to<br />
demonstrate (and communicate) product value.<br />
ACKNOWLEDGED NEED<br />
Globally, more payers and HTA bodies are acknowledging the need for and acceptability of<br />
indirect comparisons to accommodate the lack of direct comparative evidence from RCTs.<br />
Some have published statements relating to the admissibility of methodologies within the<br />
indirect and mixed treatment comparisons area (Table 1).<br />
The European Medicines Agency (EMA) notes that comparisons to active control will usually<br />
need to be ‘direct’ (ie, within the same trial) in order to estimate relative efficacy and safety,<br />
but acknowledges that there are some circumstances where an indirect comparison might be<br />
considered sufficiently reliable. 8 In the US, the FDA has not as yet published guidelines on<br />
indirect comparisons (based on keyword searches April, 2012).<br />
An Australian Indirect Comparison Working Group (IWCG) has written an extensive report<br />
on this topic for the Australian Pharmaceutical Benefits Advisory Committee (PBAC). This<br />
illustrates that the value of indirect comparisons largely depends on the underlying<br />
assumptions of the individual RCTs being compared.<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 29
INSIGHTS | INDIRECT TREATMENT COMPARISONS<br />
TABLE 1: PAYER/HTA PERSPECTIVE ON INDIRECT COMPARISONS IN KEY MARKETS<br />
COUNTRY PAYER/HTA PERSPECTIVE ON INDIRECT COMPARISONS<br />
Belgium KCE<br />
Canada CADTH<br />
France HAS<br />
Germany IQWiG<br />
Netherlands CVZ<br />
Scotland SMC<br />
Sweden TLV<br />
UK NICE<br />
KEY<br />
CADTH: Canadian Agency for Drugs and Technologies in <strong>Health</strong><br />
CVZ: College Voor Zorgverzekeringen<br />
HAS: Haute Autorité de Santé<br />
IQWiG: Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen<br />
Indirect comparisons are only allowed under specific conditions: the<br />
choice of an indirect instead of direct head-to-head comparison<br />
between study treatment and comparator should be explained, and<br />
limitations of the indirect comparison described. 2<br />
No formal guidance but best practices outlined by ISPOR and NICE<br />
should be considered for submissions.<br />
Methodological guide, Oct 2011, states:”If direct comparative data<br />
are not available or are insufficient, it may be necessary to perform<br />
indirect comparisons according to validated methodologies”. Offers<br />
two techniques: simple adjusted indirect comparison (straightforward<br />
and transparent); and network Bayesian methodology (provides best<br />
solution to determine hierarchy of treatment pathways). 3<br />
Recognizes methods supported by NICE. Stares that indirect<br />
comparisons can be considered useful, necessary and inevitable in<br />
some cases. However, also claims that results based on indirect<br />
comparisons are associated with more uncertainty than<br />
direct comparisons. 4<br />
Allows use of indirect comparisons while recognizing that this type<br />
of evidence is less valuable than direct comparisons. 5<br />
Guidance notes (2012) stipulate requirement for indirect comparisons<br />
if head-to-head evidence is not available. 6<br />
No published statement on indirect comparisons but in evaluations of<br />
reimbursement dossiers, TLV has been pragmatic, evaluating on a<br />
case-by-case basis. The use of MTC and indirect comparisons has been<br />
accepted when well supported and scientifically robust.<br />
NICE guidance states:<br />
“Data from head-to-head RCTs should be presented in the referencecase<br />
analysis, if available. When head-to-head RCTs exist, evidence<br />
from mixed treatment comparison analyses may be presented if it is<br />
considered to add information that is not available from the head-tohead<br />
comparison.” “If data from head-to-head RCTs are not available,<br />
indirect treatment comparison methods should be used.” “There may<br />
be circumstances in which data from head-to-head RCTs are less than<br />
ideal (for example, the sample size may be small or there may be<br />
concerns about the external validity). In such cases additional<br />
evidence from mixed treatment comparisons can be considered.” 7<br />
KCE: Federaal Kenniscentrum voor de Gezondheidszorg<br />
NICE: National Institute for <strong>Health</strong> and Clinical Excellence<br />
TLV: Tand-och Lakemedelsformansverket<br />
PAGE 30 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
INDIRECT TREATMENT COMPARISONS | INSIGHTS<br />
The authors conclude that indirect comparisons are not randomized and so the associated<br />
uncertainty should be recognized in the submission. Nevertheless, suggestions are provided on<br />
producing a more convincing indirect comparison. 9<br />
An ISPOR task force published two reports in 2011 to help guide decision bodies on<br />
generating and interpreting evidence that involves indirect comparisons. 10<br />
METHODOLOGICAL POSSIBILITIES<br />
When the indirect results are inconsistent with the direct evidence, it is important to<br />
investigate possible causes of discrepancy such as chance or heterogeneity across trials. For<br />
example, the synthesized evidence may be influenced by differences in the baseline<br />
characteristics of the patients across the included trials. In this case, statistical methods exist to<br />
produce a valid and coherent analysis.<br />
The recent development of computational power allows the use of the Bayesian framework in<br />
NMAs. The results produced within this framework can be interpreted in terms of<br />
probabilities – an advantage over the classical approach in allowing treatments to be rank<br />
ordered and the best ones to be determined. Furthermore, with RCTs still considered the<br />
gold standard for assessing relative efficacy and safety, the inclusion of other types of studies<br />
(eg, observational) would be seen as a weakness of the analysis. However, RCTs are<br />
experiments conducted in extremely controlled environments which may limit the<br />
applicability of their findings to the real world. The Bayesian approach allows the combination<br />
of real-world evidence with that observed in the controlled environments of RCTs, thus<br />
increasing the external validity of the analysis, ie, the extent to which the results can provide a<br />
correct basis for generalization to other circumstances.<br />
EVOLVING POTENTIAL<br />
NMAs enable the evaluation of competing treatment options that may not otherwise have<br />
been directly compared. Although the level of evidence they generate may be perceived to be<br />
inferior to that of gold standard RCTs, they nevertheless have important strengths. This topic<br />
continues to evolve; Bayesian methods are a good example of this evolution, allowing the<br />
expression of relative hierarchy of treatment efficacy and potentially increasing the<br />
generalizability of results to broader settings by combining RCT data with other sources, such<br />
as observational data. These methods are increasingly being used and accepted by authorities as<br />
solutions to address the absence of randomized direct comparative data. •<br />
1 Pair-wise meta analytic methods are typically restricted to comparisons of two interventions, using direct, head-to-head evidence alone.<br />
2 Cleemput I, Van Wilder P, Vrijens F, Huybrechts M, Ramaekers D. Richtlijnen voor farmacoeconomische evaluaties in België. <strong>Health</strong> Technology<br />
Assessment (HTA). Brussel: Federaal Kenniscentrum voor de Gezondheidszorg (KCE); 2008. KCE Reports 78A (D/2008/10.273/23).<br />
3 Guide méthodologique, choix méthodologiques pour l’évaluation économique à la HAS,Haute Autorité de santé, Octobre 2011.<br />
Available from www.has-sante.fr<br />
4 Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG). Stellenwert von Ergebnissen aus indirekten Vergleichen. Köln: IQWiG 2012.<br />
5 College voor zorgverzekeringen (CVZ). CFH-criteria voor beoordeling therapeutische waarde. Diemen: CVZ 2010. Available from www.cvz.nl<br />
6 Scottish Medicines Consortium. Guidance to Manufacturers for Completion of New Product Assessment Form (NPAF). November, 2011.<br />
7 National Institute for <strong>Health</strong> and Clinical Excellence (NICE). Guide to the Methods of Technology Appraisal. London: NICE, 2008.<br />
8 Reflection paper on the need for active control in therapeutic areas where use of placebo is deemed ethical and one or more established medicines are<br />
available. EMA/759784/2010. EMA, November 2010. Available from www.ema.europa.eu. Accessed 12/05/2012.<br />
9 Indirect Comparisons Working Group (ICWG) (30/01/2012). Report of the Indirect Comparisons Working Group to the Pharmaceutical Benefits<br />
Advisory Committee: Assessing indirect comparisons. Available from www.health.gov.au Accessed 10/04/2012.<br />
10 Jansen JP, Fleurence R, Devine B, Itzler R, Barrett A, Hawkins N, Lee K, Boersma C, Annemans L, Cappelleri JC. Interpreting indirect treatment<br />
comparisons and network meta-analysis for health-care decision making: report of the ISPOR Task Force on Indirect Treatment Comparisons Good<br />
Research Practices: Part 1. Value <strong>Health</strong>. 2011 Jun;14(4):417-28.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 31
INSIGHTS | US PRIVATE HEALTHCARE SPENDING<br />
The US Affordable Care Act is expected to extend health<br />
insurance coverage to an additional 44 million Americans<br />
through 2020. New research from the <strong>IMS</strong> Institute<br />
suggests that a deeper understanding of spending patterns<br />
among private plan enrollees – especially for the smaller<br />
number who significantly impact overall costs – will be<br />
essential to ensuring effective strategies for the future.<br />
The author<br />
Murray Aitken, MBA<br />
is Executive Director, <strong>IMS</strong> Institute for <strong>Health</strong>care Informatics<br />
Maitken@theimsinstitute.org<br />
This article is summarized from “<strong>Health</strong>care Spending Among<br />
Privately Insured Individuals Under Age 65” published by the<br />
<strong>IMS</strong> Institute for <strong>Health</strong>care Informatics in February, 2012.<br />
PAGE 32 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
US PRIVATE HEALTHCARE SPENDING | INSIGHTS<br />
Who drives the lion’s share of costs?<br />
Understanding healthcare spending in the commercially-insured<br />
US population under age 65<br />
<strong>Health</strong>care spending and utilization patterns among the privately insured population in<br />
the US are not widely understood – or widely available – yet are critical to addressing<br />
trends in cost growth and ensuring appropriate planning for this evolving population.<br />
THE SCOPE OF THE STUDY<br />
With limited access to information on the private sector, health services researchers have<br />
traditionally relied on analyses of publicly available data (principally Medicare) to advance<br />
policy recommendations. This analysis uses comprehensive, proprietary data for more than<br />
10 million privately insured members under age 65 to examine their patterns of outpatient,<br />
inpatient and pharmacy healthcare spending and consider the potential implications. The<br />
analysis also highlights distinctions between <strong>IMS</strong> aggregated healthcare use and spending<br />
patterns and those commonly cited among health services researchers, including the Agency<br />
for <strong>Health</strong>care Research and Quality (AHRQ) and Centers for Medicare and Medicaid<br />
Services (CMS).<br />
The findings are derived from an analytic subset of the LifeLink <strong>Health</strong> Plan Claims<br />
Database, which comprises 6.7 billion medical and pharmacy claims, 79 health plans, and 79.4<br />
million members from 2001 to the present. The time period covered was from January 1, 2009<br />
through December 31, 2010. Only privately insured health plan members under age 65 with<br />
continuous enrollment and medical and pharmacy benefit coverage were included.<br />
Cost and usage patterns across 17 chronic conditions, 12 cancers, and 10 auto-immune and<br />
other specialty conditions were evaluated in the study population. Costs reported reflect the<br />
plan-allowed amount (ie, plan paid amount plus member contribution) for a given service.<br />
Members were identified by condition based on Year 1 experience, and their cost and<br />
utilization is reported based on Year 2.<br />
More than 50% of the total cost was accounted for by just 5% of all health plan members.<br />
More than 25% of total spending was for just 1% of all members. Conversely, only 3% of total<br />
cost was incurred by the 50% of members with the least annual spending.<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 33
INSIGHTS | US PRIVATE HEALTHCARE SPENDING<br />
TOTAL HEALTHCARE SPENDING<br />
All payers<br />
In 2010, 184 million Americans, representing 63% of the insured population, were enrolled in<br />
a private health insurance plan (Figure 1). Collectively, they were responsible for $822 billion<br />
in healthcare expenditures. Medicare and Medicaid expenditures were $525 billion and<br />
$400.7 billion respectively.<br />
By 2020, enrollment in private health insurance is expected to be 198 million with<br />
expenditures reaching $1.4 trillion. Private health insurance enrollees are projected to remain<br />
the largest segment (57%) of the overall covered population and their expenditures the largest<br />
share of insurance spending (41%), even as the impact of implementing the Affordable Care<br />
Act transforms the healthcare landscape. Medicare and Medicaid will represent 27.7% and<br />
26.7% of total healthcare spending on insurance respectively.<br />
FIGURE 1: US ENROLLMENT IN PRIVATE HEALTH INSURANCE REACHES 197.8 MN BY 2020<br />
48.5<br />
21.1<br />
162.8<br />
5.9<br />
53.7<br />
183.9Mn<br />
individuals,<br />
63% of<br />
insured<br />
population<br />
46.8 55.4 62.3<br />
PAGE 34 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH<br />
25.8<br />
18.8<br />
7.3<br />
168.9<br />
5.2<br />
80.6<br />
195Mn<br />
individuals,<br />
58% of<br />
insured<br />
population<br />
25.9<br />
24.8<br />
5.2<br />
167.8<br />
1.4<br />
83.5<br />
2010 2016 2020<br />
Uninsured Exchanges Other Private Employer<br />
CHIP Medicaid Medicare<br />
Source: Centers for Medicare & Medicaid Services, Office of the Actuary,<br />
National <strong>Health</strong> Statistics Group 1 , Dec 2010<br />
197.8Mn<br />
individuals,<br />
57% of<br />
insured<br />
population<br />
Understanding at a more granular level the profile, behavior and usage patterns of the privately<br />
insured under age 65 health plan members who will have the greatest overall impact on<br />
healthcare costs, is key to the design and implementation of more effective, efficient care<br />
management programs.
US PRIVATE HEALTHCARE SPENDING | INSIGHTS<br />
PRIVATELY INSURED<br />
Highly concentrated<br />
For the total sample of more than 10.6 million privately insured health plan members, average<br />
healthcare spending in 2010 was $3,840, or $320 per member per month. However, more than<br />
50% of the total cost was accounted for by just 5% of all health plan members. More than 25%<br />
of total spending was for just 1% of all members. Conversely, only 3% of total cost was<br />
incurred by the 50% of members with the least annual spending (Figure 2). Understanding the<br />
profile, behavior and interventions that can be optimally applied to the relatively small number<br />
of members who have a substantial impact on overall healthcare costs is thus critical.<br />
Age-related increase<br />
<strong>Health</strong> plan members between the ages of 45 and 64 expended, on average, nearly twice the<br />
amount on health services annually as their counterparts between the ages of 20 and 44, and<br />
four times that of members in the youngest group of 0 to 9 years of age. Analysis of Medicare<br />
enrollees also shows increased spending with age, with average annual spending per enrollee<br />
higher than for the <strong>IMS</strong> privately-insured study population.<br />
FIGURE 2: DISTRIBUTION OF SPENDING IN THE US PRIVATELY INSURED<br />
25.6%<br />
50.6%<br />
Top 1% Top 5%<br />
65.2%<br />
Outpatient driven<br />
The largest share of all spending of the privately insured under age 65 population was for<br />
outpatient services, which represented 59% of total spending. Expenditures for retail pharmacy<br />
and inpatient services accounted for the remaining 21% and 20% of spending respectively.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 35<br />
74.3%<br />
80.7%<br />
85.4%<br />
96.9%<br />
3.1%<br />
Top 10% Top 15% Top 20% Top 25% Top 50% Bottom<br />
50%<br />
(>=$44,957) (>=$14,947) (>=$8,582) (>=$5,773) (>=$4,169) (>=$3,130) (>=$874) (
INSIGHTS | US PRIVATE HEALTHCARE SPENDING<br />
This distribution of costs differs significantly from that reported by the Medical Expenditure<br />
Panel Survey (MEPS) for all payers and for the Medicare 65 and over population2 .<br />
In particular, Medicare 65 and over population spending on inpatient services represented 43%<br />
of total spending, while outpatient and pharmacy services were 39% and 18%, respectively<br />
(Figure 3).<br />
The differences in spending distribution between the privately insured under age 65<br />
population and the Medicare 65 and over population are substantial and highlight the need for<br />
correspondingly differentiated analysis, understanding, and actions aimed at bending the overall<br />
US healthcare cost curve.<br />
FIGURE 3: SIGNIFICANT DIFFERENCES IN DISTRIBUTION OF SPENDING BY PAYER TYPE<br />
21% 22%<br />
59%<br />
20%<br />
<strong>IMS</strong> Privately Insured<br />
Under Age 65<br />
Inpatient<br />
Disproportionate for certain conditions<br />
Among health plan members, there were noteworthy differences in treatment patterns across<br />
diseases, which were outpatient driven among those with chronic or oncology conditions, and<br />
pharmacy driven for members with auto-immune or other specialty conditions.<br />
Members with chronic conditions like diabetes, congestive heart failure, chronic renal failure<br />
or back pain, were responsible for a disproportionate share of spending. When the prevalence<br />
of the 17 chronic conditions evaluated was compared to total spending for members affected<br />
by these conditions, their impact was immediately evident and dramatic: more than one third<br />
of members had at least one chronic condition and accounted for more than two-thirds of<br />
total spending for all members.<br />
Members with cancers, auto-immune or other conditions treated with specialty medications<br />
also accounted for larger shares of spending. Those with cancers accounted for only 1.5% of all<br />
health plan members and almost 8% of total spending, while members with auto-immune or<br />
other specialty conditions represented 1.7% of all members, and were responsible for 7% of<br />
total spending.<br />
PAGE 36 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH<br />
47%<br />
31%<br />
18%<br />
39%<br />
43%<br />
MEPS All Payers MEPS Medicare<br />
65 and Over<br />
Outpatient<br />
Source: <strong>IMS</strong> LifeLink <strong>Health</strong> Plan Claims Database, Dec 2010;<br />
Medical Expenditure Panel Survey 2 , 2009<br />
Pharmacy
US PRIVATE HEALTHCARE SPENDING | INSIGHTS<br />
OUTPATIENT SPENDING<br />
INPATIENT SPENDING<br />
PHARMACY SPENDING<br />
TOP 1% SPENDING COHORT<br />
Outpatient services represented the largest share of total spending, averaging $2,251 per<br />
member per year, or $188 per member per month. Professional and facility visits accounted for<br />
74% of overall outpatient spending, with emergency room visits a further 10%.<br />
Outpatient medical drug therapy, including office, facility and home-based injections and<br />
infusions, represented 5% of all outpatient spending, or $9 per member per month on average.<br />
However, outpatient drug therapy for oncology, auto-immune and other specialty condition<br />
populations studied were significantly higher, amounting to 19% and 18%, respectively.<br />
Facility-based costs represented 84% of the total inpatient spending, with the balance being<br />
professional service costs. Spending per inpatient admission was $14,248 on average, and<br />
represented 20% of overall spending per member.<br />
Members with chronic conditions accounted for the largest share of all hospital admissions at<br />
63%, equating to 29 admissions per 1,000 members. They also had the largest share of<br />
professional visits, at 219 per 1,000 members. Average spending per admit was $15,566, with<br />
an average 4.5 days of stay.<br />
Members with oncology conditions had the highest average cost per admission at $20,074 but<br />
admissions only totaled 2.8 per 1,000 members. Oncology patients also had a longer average<br />
length of stay compared to the overall member population and members with chronic<br />
conditions, making cancer admissions the most expensive.<br />
Inpatient services were only 16% of all spending among members with auto-immune or other<br />
specialty conditions.<br />
Average pharmacy spending – including outpatient drug claims for both specialty and nonspecialty<br />
medicines – amounted to 21% of total healthcare spending for the privately insured<br />
under age 65 population. For every 1,000 members, 11,950 prescriptions were filled in 2010,<br />
of which 78% were for members with chronic illnesses. Those with oncology and those with<br />
auto-immune or other specialty conditions filled only 4% and 5% of the total number of<br />
prescriptions, respectively.<br />
Specialty drugs represented about 1% of total pharmacy prescriptions but 17% of total<br />
pharmacy spending. Relative to total healthcare spending – including inpatient costs,<br />
outpatient medical costs and non-specialty pharmacy costs – specialty drug therapy and<br />
outpatient medical drug therapy were particularly high for members with auto-immune or<br />
other specialty conditions, representing 33% of their total healthcare spending. This reflects the<br />
growing availability of treatment options for members with auto-immune or other specialty<br />
conditions, where medications can be administered outside of the hospital setting.<br />
By comparison, these drugs accounted for 17% of spending for oncology patients, and just 6%<br />
for those members with chronic conditions.<br />
Consistent with patterns across the healthcare system, privately insured under age 65 health<br />
plan members who are among the top 1% in annual spending were found to be vastly<br />
disproportionate users of healthcare resources, averaging almost $100,000 in annual spending<br />
per member.<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 37
INSIGHTS | US PRIVATE HEALTHCARE SPENDING<br />
POTENTIAL IMPLICATIONS<br />
Within the top 1% cohort, our analysis shows that 77% of the members had at least one<br />
chronic condition, 16% had one or more cancers, and 13% suffered from auto-immune or<br />
other specialty conditions (some members had conditions in more than one of these<br />
groupings). Oncology patients had the highest average spending, of $118,000 per year.<br />
The distribution of spending in the 1% cohort is similar to that of the Medicare 65 and over<br />
population, with 45% of spending being for inpatient, 45% for outpatient, and 10% for<br />
pharmacy services.<br />
Average spending for the top 1% of members with specific chronic conditions was up to<br />
ten-fold the average spending for all members with the same conditions. For example,<br />
members with diabetes averaged $11,858 in annual spending while those in the top 1% cohort<br />
suffering from diabetes averaged $102,465 in annual spending. Similarly, those with chronic<br />
renal failure on average spent $33,801 per year, but those within the top 1% cohort spent over<br />
$150,000 annually.<br />
What is clear from these findings is that health plan management strategies for privately<br />
insured, under age 65 members cannot simply be an extension of Medicare strategies, given<br />
their lower share of expenditure for inpatient service spending, and higher shares for<br />
outpatient and retail pharmacy spending. Out-patient service pricing, use and management are<br />
important to the ability of private payers to manage costs across their membership, particularly<br />
as health exchanges result in large numbers of new entrants to the privately insured<br />
population.<br />
Effective benefits packages will need to fully consider services used by the three high-cost<br />
member segments – those with chronic conditions, cancer, and those with auto-immune or<br />
other specialty diseases.<br />
1. Chronic conditions<br />
Members with chronic conditions are responsible for the majority of healthcare expenditure<br />
in the overall as well as the top 1% spending cohort populations studied. These members and<br />
their plans would benefit from:<br />
• Employer-led wellness efforts<br />
• Prospective outpatient service management and outreach to reduce co-morbidity and<br />
complication risks<br />
• <strong>Health</strong>care payment and delivery model innovations that reward primary care physicians for<br />
coordinating specialty care for chronic care patients and align incentives to facilitate care<br />
coordination across providers<br />
• Care management programs targeting reductions in re-admission rates among members<br />
with conditions such as MI, stroke, diabetes or chronic renal failure, which could lead to<br />
system cost savings and improved member quality of life<br />
Managing health status among health plan members with chronic conditions may result in<br />
cost savings for Medicare into the future, if investment in these individuals reduces or delays<br />
complications.<br />
PAGE 38 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
SUMMARY<br />
US PRIVATE HEALTHCARE SPENDING | INSIGHTS<br />
2. Cancer<br />
Members with cancers remain a small proportion of all members but have high per patient<br />
spending and higher proportions of outpatient spending, including medical drug therapy.<br />
• These patients could benefit from treatment pathway and setting management initiatives<br />
that align incentives among providers for care coordination<br />
• Where possible, providing coverage for self-administered therapies through retail pharmacy<br />
outlets may lead to greater efficiency and better quality of life for members with cancers<br />
• Emerging guidelines around cancer screening and treatment may improve treatment<br />
effectiveness, lower cost, and improve quality of life for patients with different cancers<br />
3. Specialty<br />
In certain disease populations, the increased use of specialty retail drug therapy may lead to<br />
decreased overall member spend.<br />
• Specialty medications dispensed through the traditional or specialty retail pharmacy setting<br />
are a key cost driver and need contracting and utilization management<br />
• At the same time, patients with autoimmune and other specialty conditions had lower<br />
spending and use rates for inpatient services than members with cancers or for chronic<br />
conditions without specialty drugs<br />
• Additionally, members with auto-immune and other specialty conditions in the top 1%<br />
cohort, including MS and RA, had lower overall per member spending, despite higher<br />
shares of retail pharmacy spending<br />
Medicare and private payers face similar challenges managing spending and utilization for drug<br />
therapy administered in an outpatient facility, office or home setting and paid under the<br />
medical benefit. These include:<br />
• Coordinating the management of outpatient medical and retail pharmacy drug use,<br />
spending, and appropriateness<br />
• Evaluating effects of offering specialty medications through the retail or home health<br />
setting, in addition to or instead of in the outpatient facility or office setting, when clinically<br />
possible<br />
Efforts to address healthcare spending levels and ensure optimal care for patients require<br />
detailed understanding from timely and robust information. This analysis is intended to focus<br />
attention on the patient segments, care settings, and treatment options that can best bring<br />
improved health outcomes at lowest cost to those in need. Understanding at a more granular<br />
level the profile, behavior and usage patterns of the privately insured under age 65 health plan<br />
members who will have the greatest overall impact on healthcare costs, is key to the design<br />
and implementation of more effective, efficient care management programs. Addressing the<br />
health needs of this evolving population efficiently will bring significant benefits to the entire<br />
healthcare system. •<br />
1 National <strong>Health</strong> Expenditure Projections 2010-2020. Centers for Medicare & Medicaid Services, Office of the Actuary, National<br />
<strong>Health</strong> Statistics Group. 2010. https://www.cms.gov/nationalhealthexpenddata/downloads/proj2010.pdf<br />
2 Medical Expenditure Panel Survey: Tables of Expenditures by <strong>Health</strong> Care Services. Agency for <strong>Health</strong>care Research and Quality, 2009.<br />
http://www.meps.ahrq.gov/mepsweb/data_stats/quick_tables_results.jsp<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 39
INSIGHTS | IMPLEMENTING HTA IN ASIA PACIFIC<br />
In their efforts to optimize healthcare resources while<br />
improving access to new innovations, more emerging<br />
markets in Asia Pacific are signaling the move to a formal<br />
process for assessing healthcare technologies.<br />
While opportunities beckon for industry to help shape the<br />
landscape, challenges remain for successful implementation<br />
of HTA in the region.<br />
The author<br />
Joe Caputo, BSC<br />
is Regional Principal HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Jcaputo@sg.imshealth.com<br />
PAGE 40 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
IMPLEMENTING HTA IN ASIA PACIFIC | INSIGHTS<br />
Implementing HTA processes in the<br />
emerging markets of Asia Pacific<br />
Critical factors for success<br />
Across the emerging markets of Asia Pacific, government health ministers continue to<br />
emphasize their desire to develop and implement formal pharmacoeconomic guidelines<br />
in their respective countries.<br />
The political desire of many of the region’s authorities to provide broader access to healthcare<br />
for its populations, along with the growing prevalence of non-communicable diseases (NCDs)<br />
such as cancer and diabetes, are placing a strain not only on government budgets but also on the<br />
healthcare infrastructure across Asia Pacific. As in the West, increasing life expectancy is giving<br />
rise to the greater burden associated with ageing populations, while governments struggle to<br />
balance growing costs with a need to expand healthcare provision to all.<br />
APPROACHES TO COST CONTAINMENT<br />
At the heart of any cost-containment strategy is a set of tools, ranging from complex<br />
risk-sharing schemes and health technology assessment (HTA) through to more simplistic<br />
mechanisms, such as prescribing controls and mandatory price cuts. Analysis of<br />
cost-management trends across Asia Pacific, relative to Europe and North America,<br />
suggests a leaning towards less complex approaches (Figure 1 overleaf).<br />
One postulated reason for this is that before being able to even contemplate more sophisticated<br />
initiatives, governments must first address basic infrastructure needs. These include having<br />
sufficient doctors and clinics to diagnose and treat patients or, even more fundamentally,<br />
ensuring the provision of clean water and sanitation – as is the case in Indonesia.<br />
At the same time, there is growing appreciation that cost containment can only be effective<br />
when implemented in a systematic manner. Hence, the use of more complex tools is gaining<br />
in popularity across the region. South Korea and Taiwan already have formal guidelines in<br />
place and are now considered ‘mature’ markets in terms of HTA adoption. However, with<br />
Japan and China, amongst other Asian countries, announcing their intention to develop and<br />
implement pharmacoeconomic assessments, there is an opportunity for industry to engage<br />
with payers and governments to help shape the HTA environment and become a valued<br />
stakeholder in the healthcare process.<br />
CHALLENGING PATH TO IMPLEMENTATION<br />
The caveat, here, is that declaring a wish to establish an HTA process and effectively<br />
implementing that process are two very different things. Success – or otherwise – will be<br />
contingent on a number of factors, including technical expertise, availability of local data,<br />
stakeholder education and last, but not least, transparency of decision making.<br />
• Technical expertise: Lack of technical expertise among the regional and national health<br />
authorities is a key challenge for moving the agenda forward. Many of the region’s<br />
authorities are looking to countries with established approaches and organizations such as<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 41
INSIGHTS | IMPLEMENTING HTA IN ASIA PACIFIC<br />
FIGURE 1: COST CONTAINMENT IN ASIA PACIFIC HAS FOCUSED ON LOW-COMPLEX MEASURES<br />
DECREASING COMPLEXITY OF TOOL<br />
Cost containment<br />
tools FR DE IT ES UK AUS CH IN JP KR TW ID MY PH SG TH VT<br />
VBP/Risk-sharing<br />
agreements<br />
HTA/cost-effectiveness<br />
assessments<br />
Quality/innovation/<br />
therapeutic value rating<br />
Generics promotion<br />
International price<br />
referencing<br />
Spending caps<br />
Patient contributions<br />
Prescribing controls<br />
Mandatory price cuts<br />
EU APAC ASEAN<br />
Most cost-containment tools used are at the relatively low complexity end of the scale<br />
Only recently implemented/limited application FR: France, DE: Germany, IT: Italy, ES: Spain, UK: United Kingdom, AUS: Australia,<br />
CH: China, IN: India, JP: Japan, KR: South Korea, TW: Taiwan, ID: Indonesia,<br />
MY: Malaysia, PH: Philippines, SG: Singapore, TH: Thailand, VT: Vietnam<br />
NICE (National Institute for <strong>Health</strong> and Clinical Excellence) in the UK, for guidance on<br />
the design and implementation of their HTA processes. Even with the relevant expertise in<br />
place, the issue of which therapy areas to prioritize remains a critical question.<br />
• Data availability and real-world evidence: The effective working of an HTA process<br />
relies heavily on local data, be they clinical data in the local population (particularly<br />
important in populations where genetic differences may result in different levels of efficacy),<br />
or healthcare resource use and cost data which will be used to evaluate the costeffectiveness<br />
of different treatment options relative to the current standard of care. Hence,<br />
the growing demand for real-world evidence (RWE) to support HTA submissions.<br />
For the emerging Asian markets, the need for RWE in itself brings another set of challenges.<br />
Local databases are scarce; even when they exist they tend not to be readily available. They<br />
are invariably limited in scope, restricted to a particular locality or condition, or provide<br />
only a sub set of relevant information (eg, diagnosis but no test results). Traditionally not<br />
collected for research purposes, data are neither gathered nor coded in a consistent manner,<br />
meaning that databases cannot necessarily be combined to give an accurate bigger picture.<br />
This reality reflects the relatively early stage of HTA programs across the region; however, it<br />
will have to change in the future, with greater investment in databases and generation of<br />
RWE evidence fast becoming a priority.<br />
PAGE 42 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
IMPLEMENTING HTA IN ASIA PACIFIC | INSIGHTS<br />
THE TIME IS NOW<br />
• Stakeholder education and understanding: Stakeholder awareness will also be critical<br />
to the success of any HTA process. Experience from Europe has taught us that the role of<br />
HTA differs from country to country. Factor in the complex and diverse nature of Asian<br />
markets and this is also likely to be the case across Asia Pacific.<br />
Stakeholder understanding of the role of HTA for each country will be a key factor,<br />
although this also represents an opportunity for Asia Pacific to learn from Europe’s<br />
experience and fast forward through the learning process.<br />
• Transparency: Finally, any HTA process that is implemented will need to be transparent in<br />
its decision making and influence. One of the criticisms leveled at authorities by industry<br />
currently is that even in cases where manufacturers are invited or permitted to submit<br />
pharmacoeconomic data there is a lack of transparency as to how this data is actually used.<br />
When the sweeping price cuts announced on a regular basis by health ministers are added<br />
into the mix, the industry could be forgiven for weighing up the benefits and risks of<br />
complying with the process.<br />
Despite the obvious challenges, some would argue that the time for HTA has arrived in<br />
Asia Pacific. Implemented correctly, it can play a role in the future of the region, not only as a<br />
key component of cost containment but also as a pivotal enabler for the efficient use of<br />
resources, as governments look to provide broader access to affordable healthcare for all.<br />
In this regard, Asian markets can learn from the experience of countries in Europe, whilst<br />
industry can also take the opportunity to help shape their healthcare strategy and become a<br />
key stakeholder in that process. Should they choose to ignore the lessons from addressing<br />
growth in costs and demand for healthcare in Europe, Asia Pacific may well face a decade of<br />
potentially painful development. •<br />
For the emerging Asian markets, the need for RWE in itself brings another set of challenges.<br />
Data are neither gathered nor coded in a consistent manner, meaning that databases cannot<br />
necessarily be combined to give an accurate bigger picture. It will have to change in the future,<br />
with greater investment in databases and generation of RWE evidence fast becoming a priority.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 43
INSIGHTS | PHARMACOGENOMICS<br />
The full potential of pharmacogenomics may still be to come<br />
but as its role in healthcare continues to evolve, there are<br />
new priorities to consider and address – including a deeper<br />
understanding of the impact and implications for real-world<br />
evidence generation.<br />
The authors<br />
Jacco Keja, PHD<br />
is Regional Principal HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Jkeja@nl.imshealth.com<br />
Maartje Smulders, MSC, MPH<br />
is Director HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Msmulders@nl.imshealth.com<br />
PAGE 44 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
PHARMACOGENOMICS | INSIGHTS<br />
Pharmacogenomics comes of age<br />
Imperatives for a real-world evidence strategy<br />
On completion of the Human Genome Project in the early 2000s, pharmacogenomics (PGx)<br />
was hailed as the research area that would transform the pharmaceutical landscape;<br />
knowledge about the effects of DNA variation in man would revolutionize research and<br />
development (R&D) and approaches to diagnosing, treating and even preventing diseases.<br />
Now, ten years on, it seems those expectations may have been too high.<br />
In other words, PGx has not so far delivered the revolutionary outcomes that were promised.<br />
With hindsight, this is perhaps not surprising given the complexity of general health, drug<br />
response and toxicity and the way in which they vary by not only genotype presentation and<br />
manifestation, but also environmental factors.<br />
INCREASING VISIBILITY<br />
Notwithstanding the slower than anticipated progress to date, there is no doubt that in the<br />
coming decade, PGx will be more visible in research and clinical applications. It has the<br />
potential to accelerate drug discovery and development by identifying better drug targets, and<br />
to establish preferred segmented patient populations, thereby improving safety, efficacy and<br />
effectiveness profiles in clinical practice. Accordingly, the number of useful biomarkers for<br />
predicting drug response is expected to increase rapidly both in quantity and quality. 1,2 In fact,<br />
some currently available biomarkers are already integrated into drug label inserts by the US<br />
FDA and European Medicines Agency (eg, HercepTest, TPMT test) and are required for<br />
reimbursement. Overall, PGx is now a reality of doing business. Clear progress is being made,<br />
especially in the field of cancer.<br />
A number of factors have been influential in the development of PGxs. These have been well<br />
elaborated by Garrison, et al, including public policy issues and the challenges in linking<br />
pharmacogenomics-based diagnostics and drugs for personalized medicine. 3,4,5 This article<br />
focuses on two critical success factors for PGx: coping with the (perhaps negatively-perceived)<br />
impact of associated increased market segmentation; and the consequent increased need for<br />
more detailed and complex patient-centric data.<br />
DOES PHARMACOGENOMICS LEAD TO DECREASED MARKET POTENTIAL?<br />
The prevailing view in the pharmaceutical industry has been that many executives, marketing<br />
and sales people held back on PGx – a resistance that was possibly driven by concerns about<br />
PGx reducing market size and cases where it had negatively affected commercial success.<br />
Consider, for example, the many drug withdrawals that may have been a direct result of<br />
pharmacogenomic differences among small patient sub-populations (eg, Seldane ® , Baycol ® ,<br />
Redux ® , Rezulin ® ), and the potential of poor responders to negatively impact overall safety<br />
and efficacy in product development.<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 45
INSIGHTS | PHARMACOGENOMICS<br />
However, perceptions have been evolving since then, amid growing recognition that PGx has<br />
the potential to impact product market size in a number of ways – both good and bad (Figure<br />
1). As Bernard has observed in analyzing the myths of PGx, the introduction of PGx testing<br />
may yield loss of market share (A, B, C). On the other hand, it may drive an increase in share<br />
as a result, for example, of: earlier market approvals enabled by faster identification of drug<br />
targets and responsive patients during R&D (D); recruitment of patients from less effective<br />
competing products (E); identification of patients who refused treatment due to efficacy/safety<br />
concerns (F); and potential for higher pricing or reimbursement advantage for drugs that, with<br />
the test, can identify the patients who will respond favorably (J) 6 .<br />
FIGURE 1: MARKETING A GENERIC TEST WITH A PRODUCT CAN PRODUCE BOTH SHARE LOSS AND GAIN, POTENTIALLY<br />
RESULTING IN A MARKET SHARE INCREASE<br />
Product X’s Market<br />
Share without<br />
Pharmacogenomics<br />
Y<br />
Market Share = Y<br />
Share Loss<br />
Share Gain<br />
Earlier market<br />
introduction with<br />
faster approvals<br />
Recruitment of<br />
patients from less<br />
effective drugs<br />
D<br />
Adverse event risk<br />
E<br />
Non responders<br />
Product X’s Market<br />
Share with<br />
Pharmacogenomics<br />
Increased use in<br />
diagnosed but<br />
untreated patients<br />
Potential for higher<br />
pricing reimbursement<br />
for best-in-class drug<br />
Expansion of<br />
treatment to new<br />
subgroup/diseases<br />
Earlier/<br />
preventive<br />
use<br />
Enhanced<br />
patient<br />
compliance<br />
Thus, by monitoring PGx development and thoroughly analyzing the potential impact of PGx<br />
early, an appropriate assessment of commercial impact can be made. It is imperative that this<br />
type of evaluation is undertaken prior to Phase II development. One key question to address is<br />
the potential for higher pricing and improved reimbursement to be enabled by a PGx<br />
approach. It is here that health economics and outcomes research plays a quintessential role.<br />
PAGE 46 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH<br />
A<br />
B<br />
Low responders<br />
C<br />
F<br />
Y<br />
Market Share = Y - (A+B+C+) + (D+E+F+G+H+I+J)<br />
Source: Bernard S., The 5 myths of pharmacogenomics. Pharmaceutical Executive, 2003; October 1: 70-78<br />
J<br />
G<br />
I<br />
H
PHARMACOGENOMICS | INSIGHTS<br />
DO WE NEED DATA?<br />
PGx has the potential to establish preferred segmented patient populations, thereby improving<br />
safety, efficacy and effectiveness profiles in clinical practice. Here, the need for real-world<br />
evidence (RWE) is implicit.<br />
In the EU and US, changing safety regulations, risk management procedures and<br />
reimbursement requirements already require RWE and hence access to patient-centric<br />
longitudinal data. These data enable follow-up of patients over time to understand disease<br />
progression, (drug) treatment and associated outcomes, as well as safety. With advancements in<br />
PGx, the need for more detailed and complex patient-centric data will grow even further.<br />
Manufacturers should look to establishing RWE plans early in drug development and<br />
anticipate on co-development of RWE programs to collect, or enable a certain level of access<br />
to, the complex patient-centric data that are needed.<br />
The challenge is that access to real-life patient-centric data in general is limited for industry,<br />
due to privacy regulations, security systems, laws and public opinion. This is even more the<br />
case for genotypic information. Additionally, acceptance of and requirements for data use vary<br />
among countries, due to differing systems infrastructure, regulations and stakeholder trust.<br />
Furthermore, the fragmentation of data sources necessitates linkage of multiple data assets<br />
– calling for bespoke and well-governed approaches. Consider the example of oncology.<br />
PGx IN ONCOLOGY<br />
Data content considerations in oncology are challenging; for robust observational<br />
pharmacoepidemiology and pharmacovigilance research to support payer and regulatory<br />
requirements successfully, there are multiple data issues to address:<br />
• Longitudinal and patient-centric<br />
• Sufficiently large<br />
• Covering all population ages (not just >65)<br />
• Tumor staging, grading and patient wellbeing<br />
• Biomarkers<br />
• Exposure (drug treatment, including chemotherapy, radiotherapy, surgery)<br />
• Outcomes as mortality and hospitalizations<br />
continued on next page<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 47
INSIGHTS | PHARMACOGENOMICS<br />
Taking the aforementioned considerations into account, much of the relevant data is actually<br />
already routinely collected in practice. However, the sources are fragmented. Consequently,<br />
often de novo data collection projects are being developed which provide the full and<br />
complete information that is needed. However, these are expensive and time consuming.<br />
An alternative is the linkage of several routine databases (+/- ad hoc data collection). In this<br />
case, linking pathology and/or (pharmaco-) genomics databases, cancer registries and<br />
administrative healthcare or claims databases would provide an ultimately comprehensive RWE<br />
platform allowing for robust pharmacoepidemiology and pharmacovigilance research in<br />
oncology (Figure 2). In Europe, pathology and laboratory databases and cancer registries<br />
provide more details on diagnosis (eg, staging, histological classification, receptor status, etc);<br />
administrative healthcare databases (EMR) and to a certain extent claims data, generally<br />
provide <strong>insights</strong> into treatment and (co-) morbidities; pathology databases provide more<br />
information on, for example, biomarkers to the extent that they are used in real-world<br />
practice.<br />
In terms of the patient population segmentation driven by PGx, sample size is an important<br />
consideration and often limiting factor in pharmacoepidemiology and pharmacovigilance. To<br />
increase sample size, multiple national databases would need to be harmonized and integrated.<br />
The importance of managing the heterogeneity of underlying healthcare systems, coding and<br />
treatment pathways, and technical aspects (hardware limits) must be taken into account,<br />
particularly in relation to biobanks and PGx databases given their extensive size.<br />
FIGURE 2: LINKING FRAGMENTED DATA SOURCES COVERING CANCER CARE<br />
Pathology<br />
Cancer<br />
register<br />
Genotypic<br />
data<br />
PATIENT CORE<br />
Rx (community<br />
& in-patient)<br />
Microbiology Hospitalizations<br />
Mortality Clinical Lab<br />
PAGE 48 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH<br />
GP
PHARMACOGENOMICS | INSIGHTS<br />
INITIATIVES AND TRENDS<br />
The good news is that many different initiatives are ongoing at national and international<br />
level. Specifically in PGx, biobanks and PGx databases are being developed and becoming<br />
more open to research by third parties, in some cases providing industry with a seat at the<br />
table. A good example of such collaborative effort is the Biotech Cluster Rhine-Neckar<br />
(http://www.biorn.org/biorn-start/).<br />
There are multiple ongoing national and international biobank harmonization and linking<br />
initiatives in the EU and US. Several multi-country consortia exist, whose overall aim is<br />
(stimulating) pooling of data, including the development of harmonized measures and<br />
standardized computing infrastructures to enable the effective pooling of the data.<br />
Examples include BioSHaRE (http://www.bioshare.eu/), BBMRI (http://www.bbmri.eu)<br />
and PharmGKB. 7 Further, in response to recent calls for the development of common<br />
principles applying to data access and use, several networks are working on an international<br />
data-sharing Code of Conduct, for example, the global Public Population Project in Genomics<br />
(P³G; http://www.p3gobservatory.org), the European Network for Genetic and Genomic<br />
Epidemiology (ENGAGE) and the Centre for <strong>Health</strong>, Law and Emerging Technologies<br />
(HeLEX) in the EU. 8<br />
PLAN FOR ACTION<br />
It is clear that these advancements in PGx impact early drug and commercial strategy<br />
development. This calls for an early and thorough analysis of potential PGx implications even<br />
before Phase II development, and the development of appropriate plans for RWE generation.<br />
These plans need to incorporate the co-development of RWE programs to collect, or enable a<br />
certain level of access to the complex patient-centric data required. This early anticipation is<br />
already implicit for “normal” product development, but takes on even greater significance<br />
with the introduction of PGx given the even greater complexity of the data requirements and<br />
the need for co-development of diagnostics and treatment interventions.<br />
It goes without saying that industry must take partnered control of RWE to improve its access<br />
to and understanding of valuable information, even more so in PGx. Positive advancements<br />
have seen various different initiatives established in which the industry has a role to play. To a<br />
growing extent, data sharing is regarded as an ethical and scientific imperative that advances<br />
knowledge and thereby respects the contributions of the participants. Increased public trust,<br />
which is increasingly translated through broad consents and efforts in harmonization of data<br />
privacy are also positive trends. Perhaps the downside is that biobank and pharmacogenomic<br />
data access (and if feasible, linkages) will take much time investment in building relationships<br />
and establishing well-managed governance and access models which ensure platform quality<br />
and integrity and are in-line with data standards. Now is the time to start investing in<br />
these partnerships. •<br />
This article partially draws on a recent MSc. Thesis “Is the pharmaceutical industry ready to make its choice for PGx?” by Jorien van Luling, Erasmus University, 2012, working<br />
under Dr Keja’s supervision.<br />
1 Sim SC, Ingelman-Sundberg M. Pharmacogenomic biomarkers: New tools in current and future drug therapy. Trends Pharmacol Sci. 2011, Feb; 32(2): 72-81.<br />
2 Sim SC, Altman R B, Ingelman-Sundberg M. Databases in the area of pharmacogenetics. Human Mutation. 2011, May; 32(5): 526-31. Epub 5 April 2011.<br />
3 Garrison LP Jr, Finley Austin MJ. Linking pharmacogenetics-based diagnostics and drugs for personalized medicine. <strong>Health</strong> Affairs, 2006; 25(5): 1281-90.<br />
4 Garrison LP Jr, et al. A review of public policy issues in promoting the development and commercialization of pharmacogenomic applications: Challenges<br />
and implications. Drug Metabolism Reviews, 2008; 40(2): 377-401.<br />
5 Garrison LP. Will pharmacogenomics disrupt the U.S. <strong>Health</strong> Care System? No. Public <strong>Health</strong> Genomics, 2009; 12(3): 185-90.<br />
6 Bernard S. The 5 Myths of Pharmacogenomics, Pharmaceutical Executive, 2003; Oct 1: 70-78.<br />
7 McDonagh EM, Whirl-Carrillo M, Garten Y, Altman RB, Klein TE. From pharmacogenomic knowledge acquisition to clinical applications: The<br />
PharmGKB as a clinical pharmacogenomic biomarker resource.” Biomarkers in Medicine, 2011, Dec; 5(6): 795-806.<br />
8 Knoppers BM, et al. Towards a data sharing Code of Conduct for international genomic research. Genome Medicine, 2011; 3: 46.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 49
PROJECT FOCUS | <strong>IMS</strong> CORE BUDGET IMPACT MODEL<br />
Sophisticated,<br />
user-centric modeling<br />
solutions are bringing<br />
new possibilities for<br />
uniformly analyzing<br />
the budget impact of<br />
technologies across<br />
multiple stakeholder<br />
settings<br />
The authors<br />
Julie Munakata, MS<br />
is Principal HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Jmunakata@us.imshealth.com<br />
Cheryl Prasad Ferrufino, MS<br />
is Senior Consultant HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Cferrufino@us.imshealth.com<br />
Developing payer-relevant<br />
pharmacy budget impact<br />
analyses in OAB<br />
Budget impact analyses (BIA) are increasingly required by national<br />
regulatory agencies and managed care organizations to estimate the<br />
financial consequences of adopting and diffusing a new healthcare<br />
intervention within a particular setting of care. They may be planneutral<br />
(eg, nationally representative data in the US for an Academy<br />
of Managed Care Pharmacy dossier) or customized, based on a<br />
particular plan’s characteristics (eg, state-level commercial data<br />
for field-based discussions). By enabling critical <strong>insights</strong> into the<br />
impact of a drug or technology on a healthcare budget over time,<br />
they are a source of key information for healthcare decision makers.<br />
Recent advancements in health economic modeling are now<br />
broadening the scope of these analyses to provide a consolidated<br />
solution for multiple stakeholders.<br />
REQUIREMENT FOR STAND ALONE TOOL<br />
A leading pharmaceutical manufacturer based in the US, was<br />
interested in developing a stand-alone tool that would enable it to<br />
determine and communicate the pharmacy budget impact of adding<br />
and/or increasing the uptake of a previously launched treatment for<br />
overactive bladder (OAB) within a health plan’s formulary. OAB, a<br />
chronic and embarrassing condition characterized by urinary urgency<br />
with or without urge incontinence, is a considerable health concern<br />
with an estimated prevalence of 16%-17% among adults in the US. 1<br />
It is often under diagnosed and under treated – despite the<br />
availability of pharmacotherapy – and can significantly impact<br />
quality of life, making strategies to improve its management and<br />
outcomes important.<br />
The proposed tool was primarily intended for use by the company’s<br />
field-based account managers and internal health outcomes<br />
specialists. It was further being considered as a possible leavebehind<br />
for clients. In order to be fit for purpose, it would need to<br />
fulfill several key criteria:<br />
• A streamlined, “uncluttered” user interface<br />
• Transparent and logical presentation of data inputs and calculations<br />
• Populated with data sourced from syndicated databases to<br />
promote company-wide consistency and familiarity in modeling<br />
approach, and create efficiencies for model updates and training<br />
• Functionality to allow custom input overrides and scenario analyses<br />
• Clear within-model documentation of methods, assumptions<br />
and references<br />
PAGE 50 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
<strong>IMS</strong> CORE BUDGET IMPACT MODEL | PROJECT FOCUS<br />
FIGURE 1: <strong>IMS</strong> CORE BUDGET IMPACT MODEL: LANDING AND RESULTS SCREENS<br />
• <strong>IMS</strong> benchmark<br />
• Medi-Span<br />
• First DataBank<br />
ADVANCED MODELING SOLUTION<br />
In approaching <strong>IMS</strong> HEOR for help, the company found an<br />
expert team with proven capabilities in evidence-based and<br />
user-centric, advanced design modeling solutions. These were<br />
backed by in-depth market knowledge, <strong>insights</strong> from worldclass<br />
data assets and relevant stakeholder networks, and<br />
access to the <strong>IMS</strong> CORE Budget Impact Model.<br />
Developed in MS Excel and in accordance with local and national<br />
guidelines for BIAs, the <strong>IMS</strong> CORE Budget Impact Model is an<br />
interactive, flexible, multi-use and standardized framework<br />
enabling pharmacy budget impact analyses (Figure 1).<br />
The model is designed to be an efficient turnkey modeling<br />
solution – packaged and delivered pre-populated with userspecified<br />
default values, such as therapy area and products<br />
of interest, geographic coverage, method of payment, etc.<br />
All model screens are presented in a logical fashion and<br />
include informational, user-input (population, market share,<br />
drug prices and contracting), results and sensitivity analyses<br />
screens. Users are able to select default data sources and<br />
assumptions and override all inputs to perform exploratory<br />
scenario analyses.<br />
User Requirements<br />
• Therapy area<br />
• Products of interest<br />
1 DATA EXTRACTION<br />
2 CONFIGURATION<br />
• <strong>IMS</strong> Core BIM<br />
• Custom features<br />
• Geographic coverage<br />
• Method of payment<br />
• Etc…<br />
STAKEHOLDER-RELEVANT ANALYSES<br />
<strong>IMS</strong> benchmark data permit a view of retail pharmacy<br />
utilization and cost trends at national, state, or local<br />
(Metropolitan Statistical Area) level based on the <strong>IMS</strong><br />
National Prescription Audit, the industry-standard source<br />
of national prescription activity in the US. In addition, drug<br />
and cost inputs for the model may be sourced from First<br />
DataBank and/or Medi-Span. Key metrics may be shown by<br />
method of payment (commercial, Medicare, Medicaid) in<br />
addition to geography, and include total prescriptions,<br />
average price per prescription and quantity, and patient copay<br />
averages. Such granularity offers the user an opportunity<br />
to configure targeted analyses for clients with similar<br />
underlying policy or demographic characteristics.<br />
BRIDGING A CRITICAL GAP<br />
DELIVERY<br />
• Targeted analyzer<br />
• Stakeholder bridge<br />
Co-developed by <strong>IMS</strong> HEOR and the Payer Solutions unit of<br />
<strong>IMS</strong> <strong>Health</strong>, the <strong>IMS</strong> CORE Budget Impact Model has been<br />
specifically designed to be used by manufacturers and payers<br />
alike and is the first of its kind to bridge the critical gap<br />
between payers and manufacturers. Through their work with<br />
<strong>IMS</strong>, the client gained a simple, easy-to-use tool that could<br />
be custom-configured by geographic region and payment<br />
methods, enabling up-to-date, relevant and impactful<br />
analytics and insight to inform OAB therapy options within<br />
their targeted health plans. •<br />
1 Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, Hunt TL. Prevalence and burden of overactive bladder in the United States.<br />
World J Urol, 2003;20(6):327-336.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 51<br />
3
PROJECT FOCUS | DATA LINKAGE IN ONCOLOGY<br />
Advanced techniques<br />
linking multiple<br />
patient-level data sets<br />
allow <strong>insights</strong> across<br />
the spectrum of care<br />
for robust,<br />
comprehensive<br />
real-world evidence<br />
The author<br />
Jerrold Hill, PHD, MS<br />
is Director HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Jhill@us.imshealth.com<br />
Enabling rigorous outcomes<br />
research with an EMR<br />
oncology data platform<br />
The growing requirement for pharmaceutical manufacturers to<br />
demonstrate the value and safety of pharmaceutical and other medical<br />
technologies is increasing the need for research based on real-world<br />
evidence (RWE). The use of large, anonymized patient-level databases,<br />
based on electronic medical records (EMR), health plan and other<br />
medical claims data, has been rising significantly as a consequence.<br />
While these datasets allow important and unique <strong>insights</strong> into drug<br />
effectiveness and utilization patterns, they are typically not linked<br />
across service provision in a way that captures the total patient<br />
experience. This is particularly relevant in fast-evolving areas like<br />
oncology where complex pathways and changing treatment<br />
preferences can confound a true understanding of real-world practice.<br />
Innovative approaches that are able to integrate existing data<br />
sources through sophisticated linkage methodologies are key to<br />
overcoming these limitations. For one US biotechnology corporation,<br />
this technique proved pivotal to providing RWE for demonstrating<br />
product value within the broader context of current care in oncology.<br />
CAPTURING REAL-WORLD OUTCOMES<br />
The company, a market leader in developing innovative new cancer<br />
therapies, faced increased demands for RWE across its oncology<br />
product portfolio. However, the disparate and clinically sparse nature<br />
of patient EMR data in oncology across the US was challenging its<br />
ability to capture real-world outcomes or track utilization patterns<br />
in this field. Keen to find a practical solution, it approached <strong>IMS</strong><br />
HEOR for help in developing and building a comprehensive data<br />
acquisition, integration, warehousing, and analytics platform to<br />
explore treatment patterns, drug usage and clinical outcomes in the<br />
real-world setting – without compromising patient confidentiality.<br />
UNIQUE, COMPREHENSIVE RESOURCE<br />
The development of the EMR oncology data platform took <strong>IMS</strong><br />
through a lengthy and rigorous process of firstly pinpointing data<br />
gaps within existing data resources, next identifying and evaluating<br />
new data resources, and ultimately curating and linking external<br />
claims and registry data to existing data sources. The resulting data<br />
warehouse and research platform incorporated and linked EMR,<br />
insurance claims, tumor registry, death, biospecimen, and more.<br />
Today, the EMR oncology data platform contains more than 540,000<br />
patient records, with a history from 2004. Data are sourced from 65<br />
oncology/hematology clinics across more than 30 States in America,<br />
encompassing about 550 treating providers. Approximately 60,000<br />
patients are observed in the database every month.<br />
The clinical data available are extensive, spanning: cancer staging;<br />
TNM values; patient demographics; lab results; injectables and oral<br />
PAGE 52 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
DATA LINKAGE IN ONCOLOGY | PROJECT FOCUS<br />
FIGURE 1: EMR ONCOLOGY PLATFORM FIVE-YEAR PROGRAM OF DEVELOPMENT<br />
2006<br />
• Client identifies<br />
need to build an<br />
oncologyspecific<br />
EMR data<br />
repository<br />
2007<br />
• Request for<br />
proposals<br />
• Contract for<br />
platform building<br />
awarded<br />
to <strong>IMS</strong><br />
• Project initiated<br />
by <strong>IMS</strong> at end<br />
of year<br />
2008<br />
• Aggregate EMR<br />
data feeds<br />
• Privacy & advisory<br />
boards held<br />
• Design &<br />
delivery of<br />
standard reports<br />
• Analysis &<br />
publications to<br />
support FDA &<br />
CMS negotiations<br />
• Evaluation of<br />
data gaps<br />
• Plans for filling<br />
gaps<br />
medications (including chemo-therapeutic and hormonal<br />
drugs); dosing; treatment intervals; disease progression;<br />
vitals; drug regimens; and radiation treatments, including<br />
sites radiated. Linked to patient-level medical claims,<br />
prescription drug claims and hospital data they provide<br />
information on the full spectrum of patient care.<br />
FULLY-INTEGRATED SOLUTION<br />
In the five years since its inception, the EMR oncology data<br />
platform has served as a fully-integrated data solution,<br />
allowing the company to quickly, easily and comprehensively<br />
address ad-hoc real-world clinical and economic questions from<br />
payers and regulators as well as internal customers (Figure 1).<br />
WIDE-RANGING APPLICATIONS<br />
Outputs leveraging the EMR oncology platform data have formed<br />
the basis of various custom research studies and standard<br />
tracking reports developed by <strong>IMS</strong> to support the company’s<br />
oncology portfolio, particularly in the use of erythropoiesisstimulating<br />
agents (ESAs) for chemotherapy-induced anemia<br />
(CIA) – a common complication of cancer treatment.<br />
Typically, data afforded by the platform data have not been<br />
available in other sources, such as health insurance claims data<br />
sets, enabling unique real-world evidence for negotiations on<br />
product labeling at the FDA Oncologic Drugs Advisory<br />
Committee (ODAC) and on reimbursement decisions at CMS.<br />
Analyses include cost-effectiveness, comparative effectiveness,<br />
trends in practice patterns, physician adherence to product<br />
label instructions, impacts of FDA and Centers for Medicare and<br />
Medicaid Services (CMS) policies on product use, and patient<br />
risks (eg, transfusion risk in chemotherapy patients).<br />
The use of patient hemoglobin data, for example, has<br />
provided important <strong>insights</strong> into the real-life costs and<br />
effects of treatment for CIA as well as enabling the company<br />
2009<br />
• Gap projects<br />
initiated<br />
• Evaluation of<br />
new data<br />
• Licensing of new<br />
data<br />
• Design & delivery<br />
of more reports<br />
• Launch of<br />
multiple research<br />
projects<br />
2010<br />
• Gap projects<br />
complete<br />
• Licensing of 6<br />
new linkable data<br />
feeds<br />
• Projection of<br />
platform to US<br />
treated<br />
population<br />
• Platform linked<br />
to death records<br />
& claims data<br />
provider tumor<br />
registry<br />
22 Poster/Podium presentations and 13 peer-reviewed papers<br />
2011<br />
• Transition of<br />
platform to<br />
client<br />
• Evaluation and<br />
analysis of<br />
patient<br />
subpopulation<br />
data<br />
• Launch of<br />
platform-based<br />
research projects<br />
• 88 reports<br />
designed &<br />
delivered to<br />
clients<br />
to demonstrate significant benefits for its ESA, including:<br />
• Lower cost compared to the alternative ESA therapy<br />
• Fewer associated healthcare visits as a result of a less<br />
frequent dosing schedule<br />
• Increased likelihood of enabling chemotherapy and ESA<br />
therapy on the same visit<br />
A further study showing that physicians administered the<br />
product at hemoglobin levels consistent with label<br />
instructions also found that following FDA restrictions on<br />
indications for the product, and CMS restrictions on<br />
reimbursement, red blood transfusion rates increased in<br />
patients receiving chemotherapy – with significant<br />
implications for cost, outcomes and quality of life.<br />
Research findings from these and other studies using data<br />
from the EMR oncology platform have been communicated in<br />
peer-reviewed journals and disseminated in more than 20<br />
poster or podium presentations at professional conferences<br />
such as ISPOR, American Society of Clinical Oncology (ASCO),<br />
Hematology/Oncology Pharmacy Association (HOPA),<br />
Multinational Association of Supportive Care in Cancer<br />
(MASCC) and Association of Schools of Public <strong>Health</strong> (ASPH).<br />
KEY DECISION SUPPORT<br />
Collaborating with <strong>IMS</strong> on the development of the EMR<br />
oncology data platform has provided the company with the<br />
means to generate fast, accurate answers to key clinical<br />
research, health economic and commercialization questions,<br />
as well as improving standardization of processes and<br />
reducing costs internally. In enabling the development of<br />
robust RWE in oncology through the associated research<br />
program it has been instrumental in providing value messages<br />
for payers and physicians and informing the broader medical<br />
community on key issues in cancer care. •<br />
ACCESSPOINT - ISSUE 4 PAGE 53
PROJECT FOCUS | METASTATIC COLORECTAL CANCER<br />
Retrospective cohort<br />
analyses of physiciansurvey<br />
data can<br />
enable value<br />
messages based on<br />
real-world evidence of<br />
current patterns of<br />
practice<br />
The author<br />
Elise Pelletier, MS<br />
is Director HEOR, <strong>IMS</strong> <strong>Health</strong><br />
Epelletier@us.imshealth.com<br />
Informing optimal treatment<br />
strategies in advanced<br />
colorectal cancer in Europe<br />
Pharmaceutical manufacturers face a growing need to generate,<br />
analyze and apply real-world evidence (RWE) to support value<br />
demonstrations for their products and ensure optimal use in<br />
treatment protocols. This is particularly valid in crowded therapy<br />
areas like oncology, where scientific breakthroughs are expanding<br />
treatment options and the range of indications they can address,<br />
but where new agents must compete for inclusion in complex<br />
regimens, often involving multiple modalities, including surgery.<br />
The ability to determine and demonstrate added value within the<br />
context of current and emerging practice patterns is key to ensuring<br />
optimal outcomes – and successful product differentiation.<br />
Anonymized patient-level databases, which track the treatment<br />
experience of large patient cohorts over time, afford unique<br />
glimpses into the real-world use of medicines and, importantly, the<br />
implications of attributes associated with different interventions.<br />
When one leading biopharmaceutical manufacturer needed help in<br />
generating RWE in Europe for its new monoclonal antibody (mAB)<br />
for metastatic colorectal cancer (mCRC), the retrospective analysis<br />
of physician-survey patient-level data in <strong>IMS</strong> LifeLink Oncology<br />
Analyzer proved pivotal to identifying value differentiators based<br />
on the relative safety profile of its competitors.<br />
UNDERSTANDING THE IMPACT OF ATTRIBUTES<br />
In Europe, CRC is the most common newly diagnosed cancer and the<br />
second leading cause of death from cancer. 1 Between 15-25% of<br />
newly identified CRC patients present with metastatic disease, and<br />
up to 50% of all CRC patients will eventually develop metastases. 2<br />
Consequently, high numbers of patients seek treatment for mCRC,<br />
where prolonged survival/prevention of tumor progression,<br />
reduction of associated symptoms, and/or maintenance of quality<br />
of life are the key goals. 3 After many years of limited therapeutic<br />
options for mCRC, recent advances in systemic approaches, including<br />
new combination chemotherapies and targeted treatment with mABs<br />
combined with chemotherapy, have significantly improved the<br />
ability to achieve these outcomes.<br />
The company, a key player in oncology, wanted to explore the value<br />
of its mAB, which was indicated for second-line treatment of mCRC,<br />
but lacked sufficient post-launch experience to study the drug’s<br />
performance in the real world. However, by understanding the use<br />
of other targeted agents and the distribution of chemotherapy<br />
backbones, it could better determine the potential patient segment<br />
for a first-line indication. One significant adverse effect of a<br />
PAGE 54 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
METASTATIC COLORECTAL CANCER | PROJECT FOCUS<br />
FIGURE 1: SURGERY BY PURPOSE: PATIENTS WITH AT LEAST ONE SURGERY FOR ANY PURPOSE AND FOR DIAGNOSTIC, CURATIVE AND<br />
PALLIATIVE PURPOSE, BY COUNTRY<br />
45%<br />
40%<br />
35%<br />
30%<br />
25%<br />
20%<br />
15%<br />
10%<br />
5%<br />
0%<br />
36.3%<br />
12.8% 15.7%<br />
11.5%<br />
competing mAB was serious wound-healing complications,<br />
causing treatment discontinuation for a period of 5-8 weeks<br />
prior to surgery and 28 days after. Keen to understand the<br />
limitations this imposed and thereby better communicate the<br />
benefits of a product without this safety issue, the company<br />
approached <strong>IMS</strong> for help. Through the course of working with<br />
the HEOR team on several economic evaluations leveraging<br />
<strong>IMS</strong> LifeLink Oncology Analyzer, it had come to rely on the<br />
quality and rigor of the analyses and the power of the<br />
underlying data.<br />
EXPLORING THE EVIDENCE<br />
35.2%<br />
9.2%<br />
20.5%<br />
8.4%<br />
France<br />
Germany<br />
Total patients with at least 1 surgery for any purpose<br />
(curative, palliative, diagnostic)<br />
38.4%<br />
Source: Zhao A, Pelletier E, Barber B, Bhosle M, Wang S, Klingman D, Gao S Major surgery in patients with metastatic colorectal cancer in Western Europe.<br />
J Gastrointest Cancer, Epub 2011, Nov 29.<br />
Given the potential connection between surgical events and<br />
treatment for mCRC, and to better understand the<br />
implications of interruptions in therapy, the <strong>IMS</strong> team set<br />
out to establish the prevalence of major surgery following a<br />
diagnosis of mCRC.<br />
The retrospective cohort study used physician-survey data<br />
from the <strong>IMS</strong> LifeLink Oncology Analyzer database for mCRC<br />
patients in France, Germany, Italy, Spain and the UK. This<br />
includes information on patients with all types and stages of<br />
cancer treated by a panel of nearly 2,300 physicians at<br />
hospitals, private clinics and other cancer care centers across<br />
Europe, the US and Japan. Physicians provide case histories<br />
on a quarterly basis for the last 5-25 patients they have seen,<br />
without including the same patient’s details twice in any 12month<br />
period. The database records include full treatment<br />
history from diagnosis to current treatment, including all<br />
major surgical procedures (MSP), with patients segmented by<br />
13.4%<br />
Italy Spain UK<br />
Total patients with at least 1 surgery for curative purposes<br />
Total patients with at least 1 surgery for palliative purposes<br />
Total patients with at least 1 surgery for diagnostic purposes<br />
diagnosis, stage and line of therapy. Both physician<br />
recruitment and data collection meet exacting quality standards.<br />
All patients aged 21 years and over at the time of<br />
mCRC diagnosis were included, and MSPs were examined<br />
descriptively by the purpose and location of surgery.<br />
UNDERSTANDING THE IMPLICATIONS<br />
The study identified at least one MSP for any purpose<br />
in 30.5% (UK),35.2% (Germany), 35.6% (Spain), 36.3% (France),<br />
and 38.4% (Italy) of patients, indicating that major surgery<br />
is highly prevalent in the mCRC population, and thus has a<br />
significant role to play in meeting the goals of mCRC<br />
treatment (Figure 1).<br />
KEY VALUE DIFFERENTIATOR<br />
The results of the analysis 4 enabled the company to<br />
demonstrate, based on RWE, the importance of considering<br />
the role of pharmacological treatment options and their<br />
potential to interfere with both the use of surgery and<br />
surgical outcomes when evaluating treatment strategies for<br />
mCRC. With an additional study conducted by <strong>IMS</strong> indicating<br />
that nearly half of patients with mCRC in western Europe<br />
(with the exception of the UK) receive mAB therapy as part<br />
of their pharmacological treatment, 5 the company was able<br />
to further quantify the implications of the results. The<br />
findings have been disseminated to the broader medical<br />
community in several peer-reviewed publications and at<br />
leading conferences. •<br />
1 Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer, 2010:46(4):765-781.<br />
2 Kindler HL, Shulman KL. Metastatic colorectal cancer. Curr Treat Options Oncol, 2001;2:459-71.<br />
3 Van Cutsem E, Nordinger B, Cervantes A. Advanced colorectal cancer: ESMO clinical practice guidelines for treatment. Ann Oncol, 2010; 21 (Suppl 5):v93-7.<br />
4 Zhao Z, Pelletier E, Barber B, Bhosle M, Wang S, Klingman D, Gao S. Major surgery in patients with metastatic colorectal cancer in Western Europe. J<br />
Gastrointest Cancer, Epub 2011, Nov 29.<br />
5 Zhao Z, Pelletier E, Barber B, et al. Current chemotherapy and monoclonal antibody use patterns in metastatic colorectal cancer in Western Europe.<br />
35th EMSO Congress, Milan Italy, 8-12 October 2010.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 55<br />
19.4%<br />
7.3%<br />
35.6%<br />
10.3%<br />
20.5%<br />
5.7%<br />
30.5%<br />
14.1%<br />
10.8%<br />
7.2%
<strong>IMS</strong> HEOR | OVERVIEW<br />
Enabling your real-world success<br />
<strong>IMS</strong> offers a spectrum of world-class expertise in <strong>Health</strong> Economics & Outcomes Research<br />
(HEOR) and real-world evidence (RWE) to deliver the local excellence you need.<br />
In a future where healthcare efficiency and quality are measured through the lens of ‘real-world’<br />
<strong>insights</strong>, external validity demands a focus on the right data sources, best-in-class research and<br />
actionable communication.<br />
<strong>IMS</strong> is committed to helping you succeed:<br />
• Largest multi-disciplinary team of HEOR experts, based in 18 countries worldwide<br />
• Credible scientific voice and deep therapy area knowledge, captured in 200+ publications each year<br />
• Market leadership in developing and adapting robust economic models<br />
• Most advanced capabilities in RWE management and analysis leveraging relevant <strong>IMS</strong> proprietary<br />
and other key data assets<br />
• Proven expertise in generating and communicating RWE to advance stakeholder engagement at all levels<br />
<strong>IMS</strong> is a leading independent provider of outcomes research, economic modeling,<br />
RWE and market access solutions leveraging relevant <strong>IMS</strong> and other key data assets.<br />
Our unique, data-agnostic market position can help you develop and support the evidence<br />
required to engage global and local healthcare stakeholders, with deep <strong>insights</strong> into product<br />
safety, efficacy, cost, value for money and affordability.<br />
Outcomes Research<br />
• Evidence generation<br />
• Late-phase studies<br />
• Patient-Reported Outcomes (PROs)<br />
• Database studies<br />
• Epidemiology<br />
• Risk management<br />
<strong>Health</strong> Economic Modeling<br />
• <strong>Health</strong> economic evaluations<br />
• Core models & local adaptations<br />
• Budget impact<br />
• Meta-analyses<br />
• Indirect comparisons<br />
• <strong>IMS</strong> CORE Diabetes Model<br />
Market Access<br />
• Value development planning<br />
• Market access strategy<br />
• Core value dossiers & local adaptations<br />
• HTA readiness<br />
• Value communication<br />
• Reimbursement submissions<br />
Real-World Evidence Solutions<br />
• Data sourcing & validation<br />
• Data integration & linking<br />
• Data management & curation<br />
• Platform development<br />
• Customized analytics & reporting<br />
• Evidence planning<br />
Datasets<br />
Largest collection of scientifically validated,<br />
anonymized patient-level data assets:<br />
• <strong>Health</strong> plan claims<br />
• Longitudinal Rx<br />
• Electronic medical records<br />
• Hospital disease<br />
• Oncology<br />
• Diabetes<br />
Technology<br />
• Platform engines<br />
• Data warehouse/data marts<br />
• Encryption systems & linking technology<br />
• Meta-data repository<br />
• User interface & sophisticated<br />
analytics library<br />
• Electronic data capture<br />
PAGE 56 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
Global scope, local expertise<br />
<strong>IMS</strong> HEOR experts are located in 18 countries worldwide and they have published on<br />
projects completed in more than 50 countries on all continents.<br />
YOUR PRIMARY CONTACTS:<br />
Dr. Xavier Badier<br />
Senior Principal HEOR<br />
<strong>IMS</strong> <strong>Health</strong><br />
Doctor Ferran 25-27<br />
08034 Barcelona<br />
Spain<br />
Tel: +34 93 749 63 00<br />
Xbadia@es.imshealth.com<br />
<strong>IMS</strong> HEOR office locations<br />
NORTH AMERICA<br />
REGIONAL HEADQUARTERS<br />
200 Campus Drive<br />
Collegeville, PA 19426<br />
USA<br />
Tel: +1 610 244 2000<br />
UNITED STATES<br />
1725 Duke Street<br />
Suite 510<br />
Alexandria, VA 22314<br />
USA<br />
Tel: +1 703 837 5150<br />
The Arsenal on the Charles<br />
311 Arsenal Street<br />
Watertown, MA 02472<br />
USA<br />
Tel: +1 800 783 6362<br />
CANADA<br />
303 Terry Fox Drive<br />
Suite 300<br />
Ottawa K2K 3J1, Ontario<br />
Canada<br />
Tel: +1 613 599 0711<br />
LATIN AMERICA<br />
REGIONAL HEADQUARTERS<br />
Insurgentes Sur # 2375<br />
5th Floor, Col. Tizapan<br />
Mexico City D.F. - C.P. 01090<br />
Mexico<br />
Tel: + 52 (55) 50 62 52 00<br />
ext 5269<br />
Dr. Jacco Keja<br />
Senior Principal HEOR<br />
<strong>IMS</strong> <strong>Health</strong><br />
210 Pentonville Road<br />
London N1 9JY<br />
United Kingdom<br />
Tel: +31 (0) 631 693 939<br />
Jkeja@nl.imshealth.com<br />
EUROPE<br />
REGIONAL HEADQUARTERS<br />
210 Pentonville Road<br />
London N1 9JY<br />
United Kingdom<br />
Tel: +44 (0)20 3075 4800<br />
BELGIUM<br />
Medialaan 38<br />
1800 Vilvoorde<br />
Belgium<br />
Tel: +32 2 627 3211<br />
FRANCE<br />
91 rue Jean Jaurès<br />
92807 Puteaux cedex<br />
France<br />
Tel: +33 1 41 35 1000<br />
GERMANY<br />
Erika-Mann-Str. 5<br />
80636 München<br />
Germany<br />
Tel: +49 89 457912 6400<br />
ITALY<br />
Viale Certosa 2<br />
20155 Milano<br />
Italy<br />
Tel: +39 02 69 78 6721<br />
Adam Lloyd<br />
Senior Principal HEOR<br />
<strong>IMS</strong> <strong>Health</strong><br />
210 Pentonville Road<br />
London N1 9JY<br />
United Kingdom<br />
Tel: +44 (0)20 3075 4800<br />
Alloyd@uk.imshealth.com<br />
SPAIN<br />
Dr Ferran, 25-27<br />
08034 Barcelona<br />
Spain<br />
Tel: +34 93 749 63 00<br />
SWEDEN<br />
Sveavägen 155/Plan9<br />
11346 Stockholm<br />
Sweden<br />
Tel: +46 8 508 842 00<br />
SWITZERLAND<br />
Theaterstr. 4<br />
4051 Basle<br />
Switzerland<br />
Tel: +41 61 204 5071<br />
UNITED KINGDOM<br />
210 Pentonville Road<br />
London N1 9JY<br />
United Kingdom<br />
Tel: +44 (0)20 3075 4800<br />
ASIA PACIFIC<br />
REGIONAL HEADQUARTERS<br />
10 Hoe Chiang Road<br />
Keppel Towers #23-01/02<br />
Singapore 089315<br />
Tel: +65 6227 3006<br />
LOCATIONS | <strong>IMS</strong><br />
Dr. Michael Nelson<br />
Senior Principal HEOR<br />
<strong>IMS</strong> <strong>Health</strong><br />
1725 Duke Street, Suite 510<br />
Alexandria, VA 22314<br />
USA<br />
Tel: +1 703 837 5150<br />
Mnelson@us.imshealth.com<br />
AUSTRALIA<br />
Level 5, Charter Grove<br />
29 - 57 Christie Street<br />
St Leonards, NSW 2065<br />
Australia<br />
Telephone: +61 2 9805 6800<br />
CHINA<br />
7/F Central Tower<br />
China Overseas Plaza<br />
Jianguomenwai Avenue,<br />
Chaoyang District<br />
Beijing 100001<br />
China<br />
Tel: +86 10 8567 4255<br />
SOUTH KOREA<br />
9F Handok Building<br />
735 Yeoksam1-dong<br />
Kangnam-ku Seoul<br />
135-755<br />
S. Korea<br />
Tel: +82 2 3459 7307<br />
FOR FURTHER INFORMATION: email HEORinfo@uk.imshealth.com or visit www.imshealth.com/heor<br />
TAIWAN<br />
8th Floor<br />
No 2, Tun Hwa South Road<br />
Section 1<br />
Taipei 10506<br />
Taiwan<br />
ROC<br />
Tel: +886 2 2721 5337<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 57
<strong>IMS</strong> | EXPERTISE<br />
Expertise in depth<br />
<strong>IMS</strong> has one of the largest global teams of experts in HEOR, RWE and market access of<br />
any organization in the world.<br />
Our senior team<br />
We apply unrivalled experience and specialist expertise to help our clients meet the demands of an<br />
increasingly complex global, regional and local pharmaceutical landscape.<br />
Our highly-qualified, multi-disciplinary consultants and researchers have proven skills and<br />
capabilities across all key therapy areas. Spanning industry, consulting, government and academia,<br />
their expertise reflects a global grasp, local experience and a unique, inside market perspective.<br />
The strength of our ability to support<br />
clients in healthcare decision making<br />
for health economics, outcomes research,<br />
RWE and market access, is built on<br />
the quality of our global team.<br />
Renée J. G. Arnold, PHARM D<br />
• Dr. Renée Arnold is Principal HEOR at <strong>IMS</strong> <strong>Health</strong> with particular expertise in the use of technology to<br />
collect and/or model real-world data to facilitate rational decision making by healthcare practitioners<br />
and policy makers.<br />
• Renée was previously President and CEO, Arnold Consultancy & Technology where she developed and<br />
oversaw outcomes research for the pharmaceutical, biotech and device industries as well as federal<br />
government programs. Her distinguished career in health economics and outcomes research includes<br />
roles as President and co-founder of Pharmacon International, Center for <strong>Health</strong> Outcomes Excellence<br />
and Senior VP and Medical Director at William J Bologna International.<br />
• Founding member and former Chair of the Education Committee of ISPOR, Renée has several adjunct<br />
appointments and is the author of numerous articles on pharmacoeconomics and cost-containment<br />
strategies. She holds a Doctor of Pharmacy degree from the University of Southern California in Los Angeles.<br />
Xavier Badia, MD, MPH, PHD<br />
• Dr. Xavier Badia is Senior Principal HEOR at <strong>IMS</strong> <strong>Health</strong> with extensive experience in all areas of<br />
outcomes research.<br />
• A founder of <strong>Health</strong> Outcomes Research Europe, Xavier has extensive experience in consulting and<br />
research outcomes, patient-reported outcomes, and effectiveness and cost-effectiveness<br />
evaluations. A respected scientific speaker and member of EuroQol since 1993, he serves on several<br />
international advisory and editorial boards and has published over 150 peer-reviewed papers.<br />
• Xavier holds an MD, a PhD in Medicine, and a Master’s in Public <strong>Health</strong> and <strong>Health</strong> Economics from<br />
the University of Barcelona.<br />
PAGE 58 <strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH
EXPERTISE | <strong>IMS</strong><br />
Karin Berger, MBA<br />
• Karin Berger is Principal HEOR at <strong>IMS</strong> <strong>Health</strong> with a particular focus on outcomes research, patientreported<br />
outcomes, and cost-effectiveness evaluation analyses at a national and international level.<br />
• Formerly Managing Director of MERG (Medical Economics Research Group), an independent German<br />
organization providing health economics services to the pharmaceutical industry, university<br />
hospitals and European Commission, Karin has more than 14 years experience in the health<br />
economics arena. She lectures at several universities, has published extensively in peer-reviewed<br />
journals, and regularly presents at economic and medical conferences around the world.<br />
• Karin graduated as Diplom-Kaufmann (German MBA equivalent) from the Bayreuth University,<br />
Germany, with a special focus on health economics.<br />
Christopher M. Blanchette, PHD, MS, MA<br />
• Dr. Chris Blanchette is Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, with extensive experience in retrospective database<br />
research and observational studies with particular emphasis on respiratory diseases.<br />
• Chris was previously Director of Clinical & Outcomes Research at the Lovelace Respiratory Research<br />
Institute, where he led a team of 50 people conducting clinical research, biostatistics, and<br />
outcomes research programs. He also spent time in market access and R&D health economics at<br />
GlaxoSmithKline, most recently as Director for <strong>Health</strong> Data Analytics, and was formerly a researcher<br />
at the Premier Hospital Alliance and Agency for <strong>Health</strong>care Research and Quality.<br />
• In addition to serving in leadership positions for ISPOR and several respiratory disease associations,<br />
Christopher is on the editorial board of the Journal of Medical Economics and advisory board of<br />
Current Medical Research and Opinion. He holds a PhD in Pharmaceutical <strong>Health</strong> Services Research<br />
and an MS in Epidemiology from the University of Maryland, and an MA in Medical Sociology from<br />
the University of North Carolina.<br />
Nevzeta Bosnic, BA<br />
• Nevzeta Bosnic is Principal at <strong>IMS</strong> Brogan, where she manages projects to meet the broad spectrum<br />
of client needs in the Canadian pharmaceutical market.<br />
• Formerly Director of Economic Consulting at Brogan Inc, Nev has led many strategic consulting,<br />
policy and data analyses for pharmaceutical clients, government bodies and academic institutions in<br />
Canada. She has extensive knowledge of public and private drug plans across the country and<br />
in-depth expertise and experience on the drug reimbursement process.<br />
• Nev holds a Bachelor’s degree in Business Economics from the School of Economics and Business at<br />
the University of Sarajevo, Bosnia-Herzegovina.<br />
Joe Caputo, BSC<br />
• Joe Caputo is Regional Principal HEOR at <strong>IMS</strong> <strong>Health</strong> leveraging more than 15 years experience in<br />
the pharmaceutical sector to help clients address the challenges of global reimbursement and<br />
market access throughout the drug development program. He has led numerous projects involving<br />
payer research, value dossiers, local market access models and HTA submissions.<br />
• With a background that spans industry roles in drug development, sales & marketing and UK &<br />
global health outcomes, and consulting in health economics, Joe has wide-ranging knowledge of<br />
the drug development process at both local and international level and a unique understanding of<br />
evidence gaps in light of reimbursement and market access requirements.<br />
• Joe holds a BSc in Applied Statistics and Operational Research from Sheffield Hallam University, UK.<br />
Frank-Ulrich Fricke, PHD, MSC<br />
• Dr. Frank-Ulrich Fricke is Principal HEOR at <strong>IMS</strong> <strong>Health</strong> and Professor for <strong>Health</strong> Economics, Georg-<br />
Simon-Ohm University of Applied Sciences, Nuremberg in Germany, with a focus on health economic<br />
evaluations, market access strategies and health policy.<br />
• Formerly a Managing Director of Fricke & Pirk GmbH, and previously Head of <strong>Health</strong> Economics at<br />
Novartis Pharmaceuticals, Frank-Ulrich has conducted health economic evaluations across a wide<br />
range of therapeutic areas, developing a wealth of experience in pricing, health affairs and health<br />
policy. As a co-founder of the NIG 21 association, he has forged strong relationships with health<br />
economists, physicians and related researchers working in the German healthcare system.<br />
• Frank-Ulrich holds a PhD in Economics from the Bayreuth University, and an MBA equivalent from<br />
the Christian-Albrechts-University, Kiel.<br />
ACCESSPOINT • VOLUME 2 ISSUE 4 PAGE 59
<strong>IMS</strong> | EXPERTISE<br />
David Grant, MBA<br />
• David Grant is Senior Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, specializing in reimbursement and market<br />
access, environmental analysis, prospective and retrospective data collection and<br />
communications for product support.<br />
• A co-founder and former Director of Fourth Hurdle, David’s experience spans 10 years in health<br />
economics and outcomes research consulting, and 15 years in the pharmaceutical industry,<br />
including roles in clinical research, new product marketing and health economics in the U.K.<br />
and Japan.<br />
• David holds a degree in Microbiology and an MBA from the London Business School.<br />
Jacco Keja, PHD<br />
• Dr. Jacco Keja is Senior Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, drawing on deep expertise in global market<br />
access, operational and strategic pricing, and health economics and outcomes research.<br />
• Jacco’s background includes four years as global head of pricing, reimbursement, health outcomes<br />
and market access consulting services at a large clinical research organization and more than<br />
13 years experience in the pharmaceutical industry, including senior-level international and global<br />
roles in strategic marketing, pricing and reimbursement and health economics.<br />
• Jacco holds a PhD in Biology (Neurophysiology) from Vrije Universiteit in Amsterdam, a Masters in<br />
Medical Biology, and an undergraduate degree in Biology, both from Utrecht. He is also visiting<br />
Professor at the Institute of <strong>Health</strong> Policy & Management at Erasmus University, Rotterdam.<br />
Rob Kotchie, MCHEM, MSC<br />
• Rob Kotchie is Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, with particular expertise in health economics,<br />
outcomes research, evidence-based medicine and real-world evidence.<br />
• Previously with ZS Associates, Rob specializes in the design and roll-out of global<br />
pharmacoeconomic models, the production of health technology assessment dossiers and the use of<br />
retrospective database analytics. He has a strong focus on the areas of cardiovascular medicine,<br />
oncology, respiratory and mental health, in addition to organizational design and market access<br />
capability assessments.<br />
• Rob holds a first class honors degree in Chemistry from the University of Oxford and an MSc in<br />
International <strong>Health</strong> Policy & <strong>Health</strong> Economics from the London School of Economics.<br />
Mark Lamotte, MD<br />
• Dr. Mark Lamotte is Principal HEOR at <strong>IMS</strong> <strong>Health</strong> with responsibility for the content and quality<br />
of all health economic evaluations conducted by his team.<br />
• A physician by training (cardiology), Mark spent a number of years in medical practice before<br />
joining Rhône-Poulenc Rorer as Cardiovascular Medical Advisor and later becoming Scientific<br />
Director at the Belgian research organization, HEDM. He has since worked on more than 150<br />
projects, involving expert interviews, patient record reviews, extensive modeling and report<br />
writing across a wide range of therapy areas, and authored many peer-reviewed publications.<br />
• Mark holds an MD from the Free University of Brussels (Vrije Univeristeit Brussel, Belgium) and<br />
is fluent in Dutch, French, English and Spanish.<br />
Won Chan Lee, PHD<br />
• Dr. Won Chan Lee is Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, specializing in prospective and retrospective<br />
health economics research.<br />
• Over the course of his career, Won has completed numerous international economic evaluations<br />
employing a variety of analytical methods across a range of diseases and geographies. His expertise<br />
includes econometric database analysis, quality of life assessment and advanced economic modeling<br />
to establish the economic and humanistic value of new and existing therapeutic interventions.<br />
• Won holds a Master’s in Economics from the University of Grenoble II, and a PhD in Economics from<br />
the Graduate Center of the City University of New York.<br />
PAGE Page PAGE 60 60 <strong>IMS</strong> <strong>IMS</strong> HEALTH HEALTH ECONOMICS ECONOMICS & & OUTCOMES OUTCOMES RESEARCH<br />
RESEARCH
EXPERTISE | <strong>IMS</strong><br />
Claude Le Pen, PHD<br />
• Dr. Claude Le Pen is a member of the strategic committee of <strong>IMS</strong> <strong>Health</strong> and Professor of <strong>Health</strong><br />
Economics at Paris-Dauphine University, providing expert economic advisory services to the<br />
consulting practice.<br />
• A renowned economist, leading academic, and respected public commentator, Claude has served<br />
as an appointed senior member of several state commissions in the French Ministry of <strong>Health</strong> and<br />
is an expert for a number of parliamentary bodies, bringing a unique perspective and unparalleled<br />
<strong>insights</strong> into the economic evaluation of pharmaceutical technologies at the highest level.<br />
• Claude studied Business Administration in HEC Business School in Paris and holds a PhD in<br />
Economics from Panthéon-Sorbonne University.<br />
Adam Lloyd, MPHIL, BA<br />
• Adam Lloyd is Senior Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, with a particular focus on economic modeling<br />
and the global application of economic tools to support the needs of local markets.<br />
• A former founder and Director of Fourth Hurdle, and previously Senior Manager of Global <strong>Health</strong><br />
Outcomes at GlaxoWellcome, Adam has extensive experience leading economic evaluations of prelaunched<br />
and marketed products, developing submissions to NICE and the SMC, decision-analytic<br />
and Markov modeling, and in the use of health economics in reimbursement and marketing in<br />
continental Europe.<br />
• Adam holds an MPhil in Economics, and a BA (Hons) in Philosophy, Politics and Economics from the<br />
University of Oxford.<br />
Charles Makin, MS, MBA, MM, BS<br />
• Charles Makin is Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, focusing on naturalistic trials, adherence<br />
interventions, chart abstractions, patient-reported outcomes and other studies involving<br />
primary data collection.<br />
• During a career that includes senior roles at the United<strong>Health</strong> Group and Wellpoint, Charles has<br />
led numerous studies involving database analyses, economic modeling, multi-country patient<br />
registries, systematic literature reviews and survey-based research.<br />
• Charles holds a BS in Pharmacy from the University of Pune, India, an MS in Pharmacy<br />
Administration from Purdue University, Indiana, U.S. and an MBA in Marketing Management and<br />
a Master’s in Management, both from Goldey Beacom College, Delaware, U.S.<br />
Frédérique Maurel, MS, MPH<br />
• Frédérique Maurel is Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, with a particular focus on observational research<br />
and health economics studies.<br />
• A skilled consultant and project manager, Frédérique has extensive experience in the economic<br />
evaluation of medical technologies gained in roles at ANDEM, Medicoeconomie, and AREMIS<br />
Consultants.<br />
• Frédérique holds a Masters degree in Economics – equivalent to an MS – and completed a postgraduate<br />
degree equivalent to an MPH with a specialization in <strong>Health</strong> Economics at the University<br />
of Paris-Dauphine (Paris IX) as well as a degree in Industrial Strategies at the Pantheon-Sorbonne<br />
University (Paris I).<br />
Joan McCormick, MBA<br />
• Joan McCormick is Principal at <strong>IMS</strong> Brogan, leading a team providing strategic advice to<br />
companies with new products coming to market and ongoing consultation on the rules for<br />
existing drugs post launch.<br />
• Formerly Head of Price Regulation Consulting at Brogan Inc, Joan has supported many major<br />
pharmaceutical companies with the preparation of pricing submissions to the Patented<br />
Medicine Prices Review Board (PMPRB), gaining extensive <strong>insights</strong> into the operation of the<br />
Canadian pharmaceutical market.<br />
• Joan holds a Bachelor’s degree in Life Sciences from Queen’s University in Kingston, Canada,<br />
and an MBA from the University of Ottawa, Canada.<br />
ACCESSPOINT AccessPoint ACCESSPOINT - • Issue VOLUME 3 2 ISSUE 4 PAGE Page 61<br />
61
<strong>IMS</strong> | EXPERTISE<br />
Dana Morlet-Vigier, MD<br />
• Dr. Dana Morlet-Vigier is Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, applying in-depth expertise and extensive<br />
experience in pharmaceutical pricing, reimbursement and market access to help clients meet the<br />
growing challenges of today’s increasingly complex product launch process.<br />
• A medical doctor and INSEAD executive, Dana’s background spans 15 years in pharmaceuticals and<br />
includes roles in R&D, commercial, market access, strategy and government affairs at<br />
GlaxoSmithKline, Organon and 3M Pharma. She has worked on numerous pricing and reimbursement<br />
negotiations and designed and implemented national and international Phase II, III and IV studies<br />
across a wide range of therapy areas.<br />
• Dana holds an MD from Bucharest Medical University, Romania and the Paris-Cochin Faculty, Paris, France.<br />
Julie Munakata, MS<br />
• Julie Munakata is Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, with a particular focus on global economic<br />
modeling, value development planning, and survey data analysis.<br />
• An accomplished researcher and author of more than 25 original articles, Julie has extensive<br />
experience in managing clinical trials, health economic studies and decision analytic modeling work,<br />
gained in senior roles at ValueMedics Research LLC, the VA <strong>Health</strong> Economics Resource Center and<br />
Stanford Center for Primary Care & Outcomes Research, and Wyeth Pharmaceuticals.<br />
• Julie holds an MS in <strong>Health</strong> Policy and Management from the Harvard School of Public <strong>Health</strong> and a<br />
BS in Psychobiology from the University of California, Los Angeles.<br />
Michael Nelson, PHARM D<br />
• Dr. Michael Nelson is Senior Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, with particular expertise in retrospective<br />
database research, prospective observational research, health program evaluation, and costeffectiveness<br />
analysis.<br />
• During a career that includes leadership roles in HEOR at PharmaNet, i3 Innovus, SmithKline<br />
Beecham, and DPS/United<strong>Health</strong> Group, Mike has gained extensive experience in health<br />
information-based product development, formulary design, drug use evaluation, and disease<br />
management program design and implementation.<br />
• A thought leader in health economics for more than 20 years, Mike holds a doctorate in Pharmacy<br />
and a Bachelor of Science degree, both from the University of Minnesota College of Pharmacy. He<br />
also served as an adjunct clinical faculty member at the University of Minnesota whilst in clinical<br />
pharmacy practice.<br />
Olaf Pirk, MD, PHD<br />
• Dr. Olaf Pirk is Senior Scientific Consultant to <strong>IMS</strong> <strong>Health</strong> and previously Principal HEOR at <strong>IMS</strong><br />
<strong>Health</strong>, with a particular focus on health technology assessment, healthcare system research,<br />
health policy and health economic modeling across a range of countries and therapeutic areas.<br />
• Formerly a Managing Director of Fricke & Pirk GmbH, Olaf has considerable pharmaceutical<br />
industry experience gained in roles within health economics, pricing, health policy, marketing<br />
and clinical research. As a co-founder of the NIG 21 association, he has forged strong<br />
relationships with health economists, physicians and related researchers working in the German<br />
healthcare system.<br />
• Olaf holds an MD and PhD in Medicines from the Medical University of Lübeck.<br />
Jon Resnick, MBA<br />
• Jon Resnick is Vice President Real-World Evidence Solutions at <strong>IMS</strong> <strong>Health</strong>, leading the<br />
company’s global real-world evidence (RWE) business, including the development of RWE<br />
strategy, offerings, collaborations and foundational technologies to meet the RWE needs of<br />
healthcare stakeholders.<br />
• A former Legislative Research Assistant in Washington DC and member of the Professional<br />
<strong>Health</strong> and Social Security staff for the US Senate Committee on Finance, Jon has 10 years<br />
consulting experience at <strong>IMS</strong>. He was most recently responsible for leading the European<br />
management consulting team and global HEOR business teams of 300 colleagues, advising<br />
clients on a wide range of strategic, pricing and market access issues.<br />
• Jon holds an MBA from the Kellogg School of Management, Northwestern University, with a<br />
major in Management & Strategy, Finance, <strong>Health</strong> Industry Management and Biotechnology.<br />
PAGE Page PAGE 62 62 <strong>IMS</strong> <strong>IMS</strong> HEALTH HEALTH ECONOMICS ECONOMICS & & OUTCOMES OUTCOMES RESEARCH<br />
RESEARCH
EXPERTISE | <strong>IMS</strong><br />
Vernon Schabert, PHD<br />
• Dr. Vernon Schabert is Senior Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, with a particular focus on the<br />
assessment and validation of patient-reported outcomes (PRO) instruments, retrospective<br />
analyses of claims and survey databases, and primary data collection surveys.<br />
• A founder and former President of Integral <strong>Health</strong> Decisions, Inc, Vernon has extensive<br />
experience in conducting claims analyses, creating custom administrative databases,<br />
developing business intelligence software, and leading national quality research projects,<br />
gained in roles with Thomson Reuters, Strategic <strong>Health</strong>care Programs LLC, and CIGNA<br />
<strong>Health</strong>Care. His expertise spans numerous disease areas and diverse topics including medication<br />
adherence, in-patient safety and outcomes in post-acute care.<br />
• Vernon holds a PhD in Personality and Social Psychology from Stanford University and a BA in<br />
Psychology from Princeton University.<br />
Núria Lara Surinach, MD, MSC<br />
• Dr. Núria Lara is Principal HEOR at <strong>IMS</strong> <strong>Health</strong>, with a particular focus on the design and coordination<br />
of local and international observational and patient-reported outcomes studies.<br />
• A former practicing GP and clinical researcher, Núria’s experience spans roles in outcomes research<br />
at the Institute of Public <strong>Health</strong> in Barcelona and in Catalan <strong>Health</strong> Authorities, and consulting<br />
positions within the pharmaceutical and medical device industries focusing on medical regulatory<br />
and pricing affairs, pharmacoeconomics and market access strategies.<br />
• Núria holds an MD (specializing in Family and Community Medicine in Barcelona), and a Master’s in<br />
Public <strong>Health</strong> from the London School of Hygiene and Tropical Medicine and London School of Economics.<br />
Christian Thielscher, MD, MBA, PHD<br />
• Dr. Christian Thielscher is Principal HEOR at <strong>IMS</strong> <strong>Health</strong> and Professor for <strong>Health</strong> Economics at<br />
the FOM University in Germany, with expertise in clinical medicine, health economics, strategic<br />
consulting, business administration and innovative service development.<br />
• Christian began his career in medical practice before moving into healthcare consulting at<br />
McKinsey, where he established one of the first disease management programs in Germany. He<br />
later founded GHX Europe where his work included developing the “health card” and the first<br />
German internet-based hospital guide.<br />
• Founding president of the DGFM eV and editor of ‘Medizinökonomie’, Christian’s current research<br />
interests include quality in medicine and healthcare business management and marketing. He<br />
holds an MD from Bonn University, an MBA, and a PhD in Economics from the University of<br />
Frankfurt am Main, Germany.<br />
Massoud Toussi, MD, MSC, PHD<br />
• Dr. Massoud Toussi is Medical Director HEOR at <strong>IMS</strong> <strong>Health</strong> with particular expertise in<br />
methodological and operational aspects of clinical research to assure the quality of interventional,<br />
observational and database studies.<br />
• Previously Head of Global Clinical Research Operations at Cegedim, Massoud has also worked at the<br />
French High Authority for <strong>Health</strong> and various CROs as Project Lead, Scientific Manager and<br />
Operations Director. His experience includes defining and elaborating a new service process in drug<br />
safety signal detection and transmission.<br />
• Massoud holds an MD from Mashad University in Iran, an MSc in Medical Informatics and<br />
Communication Technology from Paris IV, a PhD in Medical Informatics from Paris XIII University<br />
and a diploma in Transcultural Psychiatry from Paris Nord University.<br />
Arnaud Troubat, PHARM D, MBA, MHEM<br />
• Dr. Arnaud Troubat is Principal HEOR at <strong>IMS</strong> <strong>Health</strong>. He has extensive consulting experience and<br />
special expertise in the development of registration dossiers and market access strategies<br />
across a large number of therapeutic areas.<br />
• A pharmacist by training, Arnaud began his career at the French pharmaceutical industry<br />
association (LEEM), supporting members in understanding and interpreting the changing<br />
economical environment in France. He then spent a number of years in pharmaceutical affairs<br />
at ICI, leading regulatory work on registration submissions and reimbursement strategies,<br />
before subsequently moving into consulting. Most recently, he was Director at Carré-Castan<br />
Consultants, managing a team working for a wide range of pharmaceutical companies.<br />
• Arnaud holds a Doctor of Pharmacy degree and an MBA from IAE Paris and a Master’s in <strong>Health</strong><br />
Economics and Management from Paris-Dauphine University.<br />
ACCESSPOINT AccessPoint ACCESSPOINT - • Issue VOLUME 3 2 ISSUE 4 PAGE Page 63<br />
63
<strong>IMS</strong> | MEETINGS<br />
Conferences and events<br />
The global HEOR team at <strong>IMS</strong> <strong>Health</strong> play an active role in the HEOR community at<br />
events and conferences around the world and we look forward to meeting you and<br />
sharing our latest research at forthcoming meetings this year:<br />
Conference City Country Date<br />
ASCO Chicago US Jun 1-5<br />
ISPOR Washington US Jun 2-6<br />
Mount Hood 2012 Challenge Baltimore US Jun 7-8<br />
American Diabetes Association (ADA) Philadelphia US Jun 8-12<br />
HTAi Bilbao Spain Jun 23-27<br />
ISPE Barcelona Spain Aug 23-26<br />
ISPOR Taipei Taiwan Sept 2-4<br />
European Association for<br />
Study of Diabetes (EASD)<br />
Society of Medical<br />
Decision Making (SMDM)<br />
Berlin Germany Oct 1-5<br />
Phoenix US Oct 17-20<br />
ISPOR Berlin Germany Nov 3-7<br />
Visit us online<br />
<strong>IMS</strong> <strong>Health</strong> Economics & Outcomes Research web pages<br />
are at www.imshealth.com/heor<br />
PAGE Page PAGE 64 64 <strong>IMS</strong> <strong>IMS</strong> HEALTH HEALTH ECONOMICS ECONOMICS & & OUTCOMES OUTCOMES RESEARCH<br />
RESEARCH
Powering a patient perspective<br />
LIFELINK | <strong>IMS</strong><br />
Pharmaceutical companies worldwide rely on LifeLink to power patient-centered<br />
decisions – from the first exploratory questions that drive clinical development to<br />
tactical sales planning for mature brands.<br />
They are recognizing significant benefits, such as:<br />
• Better global decision making through consistent <strong>insights</strong> across all brands and across the<br />
product lifecycle<br />
• Improved internal alignment with consistent patient segments defined across Research &<br />
Development and Commercial functions<br />
• Enhanced communication with healthcare payers and other stakeholders through the use of a<br />
consistent patient view and common language<br />
• Faster and more accurate views across three key dimensions: patients, payers and prescribers<br />
• Confidence working with a partner who is committed to driving new metrics for new business models<br />
<strong>IMS</strong> has made extensive investments in anonymized patient-level data in markets around the world.<br />
Today, we capture information for more than 260 million patient lives - for unparalleled real-world<br />
treatment <strong>insights</strong>.<br />
Through the global <strong>IMS</strong> LifeLink program, we provide a powerful patient lens to drive focus and<br />
alignment across your business, deepening your understanding of critical patient, physician and<br />
payer dynamics. LifeLink allows you to identify the right patient segments early on, in order to gain<br />
competitive advantage in today’s complex environment.<br />
We make a patient-centered perspective easy – by integrating patient-level intelligence into our<br />
industry leading offerings and giving you expert consultants who apply it to your key issues.<br />
LifeLink provides the <strong>insights</strong> of primary research with the benefits of secondary: lower cost,<br />
repeatable, faster, larger sample size.<br />
<strong>IMS</strong> LifeLink has everything you need to succeed in a patient-centered universe.<br />
AN UNPARALLELED ARRAY OF ANONYMIZED PATIENT-LEVEL DATA WORLDWIDE<br />
CANADA<br />
• Longitudinal Rx<br />
• Drug Plan Claims<br />
(Oncology, hospital)<br />
UNITED STATES<br />
• Longitudinal Rx<br />
• <strong>Health</strong> Plan Claims<br />
• Oncology Analyzer<br />
• Electronic Medical Records<br />
(Oncology, ambulatory)<br />
• Medical Encounters<br />
• Hospital Charge Detail Master<br />
EUROPE<br />
• Longitudinal Rx<br />
(Belgium, France, Germany, Italy,<br />
Netherlands, Sweden, UK)<br />
• Electronic Medical Records<br />
(France, Germany, Italy, UK)<br />
• Oncology Analyzer<br />
(France, Germany, Italy, Netherlands,<br />
Spain, Turkey, UK)<br />
• Hospital Disease Database<br />
(Belgium)<br />
• Longitudinal Patient Database<br />
(Sweden)<br />
ASIA PACIFIC<br />
• Oncology Analyzer<br />
(China, Japan, South Korea,<br />
Taiwan)<br />
• Longitudinal Rx<br />
(Japan, South Korea)<br />
AUSTRALIA<br />
• Longitudinal Rx<br />
ACCESSPOINT AccessPoint ACCESSPOINT - • Issue VOLUME 3 2 ISSUE 4 PAGE Page 65<br />
65
<strong>IMS</strong> HEALTH ECONOMICS & OUTCOMES RESEARCH<br />
is based in 18 countries worldwide with regional headquarters in:<br />
EUROPE & WORLDWIDE<br />
210 Pentonville Road<br />
London N1 9JY<br />
United Kingdom<br />
Tel: +44 (0)20 3075 4800<br />
HEORinfo@uk.imshealth.com<br />
www.imshealth.com/heor<br />
ABOUT <strong>IMS</strong><br />
THE AMERICAS<br />
1725 Duke Street<br />
Suite 510<br />
Alexandria, VA 22314<br />
USA<br />
Tel: +1 (703) 837 5150<br />
<strong>IMS</strong> <strong>Health</strong> is the leading provider of information services for the healthcare industry around the world. The company<br />
draws on its global technology infrastructure and unique combination of in-depth, sophisticated analytics, on-shore and<br />
off-shore commercial services, and consulting platforms to help clients better understand the performance and value of<br />
medicines. With a presence in 100+ countries and more than 55 years of industry experience, <strong>IMS</strong> <strong>Health</strong> serves leading<br />
decision makers in healthcare, including pharmaceutical manufacturers and distributors, providers, payers, government<br />
agencies, policymakers, researchers and the financial community. Additional information is available at<br />
www.imshealth.com<br />
© 2012 <strong>IMS</strong> <strong>Health</strong> Incorporated and its affiliates. All rights reserved.<br />
Trademarks are registered in the United States and in various other countries.<br />
LATIN AMERICA<br />
Insurgentes Sur # 2375<br />
5th Floor<br />
Col. Tizapan<br />
México D.F. - C.P. 01090<br />
Tel: + 52 (55) 50 62 52 00<br />
ASIA PACIFIC<br />
10 Hoe Chiang Road<br />
Keppel Towers # 23-01/02<br />
Singapore 089315<br />
Tel: +65 6412 7365<br />
HEORAP0512