Oral Antidiabetic Drugs for Cats - VetLearn.com
Oral Antidiabetic Drugs for Cats - VetLearn.com
Oral Antidiabetic Drugs for Cats - VetLearn.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CE<br />
Vol. 23, No. 7 July 2001 633<br />
Article #2 (1.5 contact hours)<br />
Refereed Peer Review<br />
KEY FACTS<br />
■ Glipizide is the only antidiabetic<br />
agent whose mechanism of<br />
action is directed at the endocrine<br />
pancreas.<br />
■ Acarbose does not reverse any<br />
pathophysiologic derangements<br />
in patients with diabetes. In fact,<br />
the drug is not systemically<br />
absorbed.<br />
■ Of the oral antidiabetic drugs<br />
available <strong>for</strong> cats, glipizide and<br />
acarbose appear to have the<br />
most efficacy and the least<br />
potential <strong>for</strong> toxicity.<br />
<strong>Oral</strong> <strong>Antidiabetic</strong><br />
<strong>Drugs</strong> <strong>for</strong> <strong>Cats</strong><br />
University of Tennessee<br />
Sara M. Cowan, DVM<br />
North Carolina State University<br />
Susan E. Bunch, DVM, PhD, DACVIM<br />
Email <strong>com</strong>ments/questions to<br />
<strong>com</strong>pendium@medimedia.<strong>com</strong><br />
or fax 800-556-3288<br />
ABSTRACT: Diabetes mellitus (DM) is <strong>com</strong>monly diagnosed in cats. In humans, treatment<br />
regimens <strong>for</strong> non–insulin-dependent DM include various <strong>com</strong>binations of dietary modification,<br />
exercise, insulin administration, and one or more oral antidiabetic drugs, which have been extensively<br />
evaluated in humans but not in cats. Glucose toxicity is a phenomenon of chronic hyperglycemia<br />
and must be understood be<strong>for</strong>e interpreting response to any antidiabetic therapy.<br />
This article provides a critical review of the oral antidiabetic drugs glipizide, met<strong>for</strong>min, troglitazone,<br />
and acarbose.<br />
Diabetes mellitus (DM) is a <strong>com</strong>mon endocrine disorder in cats. It is estimated<br />
to affect 1 in 300 cats, 1 with both <strong>for</strong>ms of the disease defined by<br />
the ability of pancreatic beta cells to secrete insulin. 2 Type I DM is characterized<br />
by the destruction of insulin-producing beta cells in the islets of<br />
Langerhans. Type I DM is always insulin dependent; there<strong>for</strong>e, the treatment of<br />
choice is insulin. Type II DM is characterized by defects in glucose-stimulated<br />
insulin secretion by the pancreas and in peripheral tissue sensitivity to and use of<br />
insulin. 3–5 Initially, type II DM is non–insulin-dependent because of the ability<br />
of beta cells to produce some insulin. However, the progression of disease usually<br />
results in insulin dependence. 6<br />
In humans, treatment options <strong>for</strong> type II DM include various <strong>com</strong>binations<br />
of dietary modification, exercise, and administration of one or more oral antidiabetic<br />
drugs with or without insulin. The treatment options <strong>for</strong> type II DM in<br />
cats are not as diverse as those <strong>for</strong> humans <strong>for</strong> the following reasons:<br />
■ It is difficult to discern in cats whether DM is insulin dependent, and most<br />
cats are treated as insulin-dependent diabetics.<br />
■ Diabetic cats with finicky appetites may be difficult to manage with dietary<br />
changes.<br />
■ <strong>Oral</strong> antidiabetic drugs have not been extensively evaluated in cats. (Nevertheless,<br />
understanding their possible role in treating feline diabetics is important<br />
<strong>for</strong> veterinarians. Use of these drugs in cats may be<strong>com</strong>e more <strong>com</strong>monplace,<br />
and clients often have questions regarding their use.)
634 Small Animal/Exotics Compendium July 2001<br />
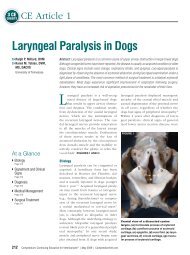
(A) Glipizide<br />
K +<br />
(B)<br />
K +<br />
K +<br />
K +<br />
K +<br />
Closes ATP – K + channel<br />
I<br />
(E) Exocytosis of vesicles<br />
Insulin leaves the pancreas to portal vein<br />
In general, oral antidiabetic drugs act by stimulating<br />
insulin secretion, decreasing hepatic gluconeogenesis,<br />
or improving muscle and adipose tissue sensitivity to<br />
insulin. Because type II DM is a progressive disease 7<br />
that ultimately requires insulin injections and/or multiple<br />
drug therapies, careful patient selection is essential<br />
<strong>for</strong> these drugs to be used successfully.<br />
Due to the high incidence of diabetes, diabetic <strong>com</strong>plications,<br />
problems with long-term insulin use, and<br />
the hospital time and resources spent on managing diabetes<br />
in humans, 8 diabetologists have studied alternatives<br />
to insulin over the past 30 years. Similar investigations<br />
are needed in cats in light of the high euthanasia<br />
rate of diabetic cats (30% to 40%) and the knowledge<br />
gained in humans on the effects of diet, exercise, and<br />
antihyperglycemic drugs on glycemic control.<br />
The following factors are used to evaluate the efficacy<br />
of antidiabetic drugs 9–12 :<br />
■ The difference between pretreatment and posttreatment<br />
fasting blood glucose (FBG) and postprandial<br />
blood glucose (PPBG) concentrations<br />
■ Similar differences in glycosylated hemoglobin (Hb<br />
A 1c) or serum fructosamine concentrations<br />
■ Pretreatment factors serving as positive predictors of<br />
response to therapy<br />
■ Causes of failure to respond<br />
SULFONYLUREAS (GLIPIZIDE)<br />
Sulfonylureas were found to have the potential to<br />
K +<br />
(C) Cell membrane<br />
depolarization<br />
(D)<br />
Ca ++<br />
Ca ++<br />
Ca ++<br />
Figure 1—Mechanism of action of glipizide at the pancreatic<br />
beta cell. Glipizide (A) binds to a receptor on the ATP–<br />
potassium (K + ) channel, which closes it, resulting in reduced<br />
potassium efflux from the cell. An increase in extracellular<br />
potassium (B) causes cell membrane depolarization<br />
(C) and calcium (Ca ++ ) influx (D). An increase in intracellular<br />
calcium is the direct stimulus <strong>for</strong> exocytosis of insulincontaining<br />
vesicles (E).<br />
I<br />
I<br />
treat diabetes over 50 years ago when researchers were<br />
studying their antibiotic effects. 9 Sulfonylureas are<br />
highly protein-bound derivatives of the sulfa antibiotics.<br />
Glipizide is a second-generation sulfonylurea;<br />
first-generation drugs of this class have less potency<br />
and higher polarity, are less lipid soluble, and have not<br />
been examined <strong>for</strong> use in cats. Sulfonylureas are well<br />
absorbed from the gastrointestinal (GI) tract. There<br />
are some weakly active or inactive metabolites produced<br />
in the liver. The liver and kidney clear sulfonylureas;<br />
hepatic inactivation is the primary route of<br />
clearance. 10<br />
The sulfonylureas are the only class of antihyperglycemic<br />
drug with a direct mechanism of action at the<br />
pancreatic beta cell. 11 The insulinotropic effect of sulfonylureas<br />
is depicted in Figure 1.<br />
Other effects of sulfonylureas have also been described.<br />
13 There is in vitro evidence <strong>for</strong> a decrease in<br />
hepatic gluconeogenesis, an increased number of insulin<br />
receptors in tissues of action, and increased<br />
postinsulin receptor activity. 12<br />
Efficacy<br />
Humans<br />
In humans with type II diabetes, glipizide decreases<br />
the FBG level by 60 to 70 mg/dl and the Hb A 1c by<br />
1.5% to 2%, 12 which is similar to the efficacy of insulin.<br />
7 In humans, factors that predict a positive response<br />
to sulfonylureas include diabetes diagnosed<br />
within the past 5 years, hyperglycemia in the range of<br />
220 to 240 mg/dl, adequate beta-cell function as measured<br />
by a high fasting C-peptide level, and no history<br />
of exogenous insulin treatment. 10,14 The likelihood of<br />
response to glipizide treatment is inversely correlated<br />
with the degree of blood glucose elevation at the start<br />
of therapy. 7 There<strong>for</strong>e, carefully selecting patients with<br />
mildly to moderately elevated fasting and postprandial<br />
glucose levels <strong>for</strong> glipizide therapy is re<strong>com</strong>mended and<br />
may improve efficacy.<br />
Failure of humans to respond to therapy as evidenced<br />
by an unacceptably minimal decrease in glucose<br />
concentrations after 3 months of therapy is related<br />
to patient factors (non<strong>com</strong>pliance, coexisting<br />
disease), drug factors (use of medications that antagonize<br />
insulin action or secretion, inadequate drug<br />
dosage), and disease progression. 12 A 6-year follow-up<br />
of humans treated with sulfonylureas showed that only<br />
5% (33 of 660) maintained normoglycemia. This attests<br />
to the nature of type II DM as a progressive disease<br />
and the eventual need <strong>for</strong> multidrug therapy, including<br />
insulin. 7
Compendium July 2001 Small Animal/Exotics 635<br />
<strong>Cats</strong><br />
The data on efficacy of glipizide in cats is <strong>com</strong>plicated<br />
by the uncertainty of the underlying diabetic state<br />
(type II versus type I DM) and the absence of blinded,<br />
placebo-controlled prospective clinical trials. The first<br />
study of glipizide in cats examined its effect on serum<br />
insulin and glucose concentrations in 10 healthy cats. 15<br />
Mean serum insulin concentration increased <strong>for</strong> 1 hour<br />
after glipizide administration, and mean serum glucose<br />
concentration decreased within 15 minutes of glipizide<br />
administration, with the lowest concentration at 60<br />
minutes and duration of effect up to 120 minutes. In a<br />
1993 study of 20 cats, Nelson and colleagues found improved<br />
clinical signs and blood glucose concentrations<br />
in 65% (13 of 20) of cats with DM that were treated<br />
with glipizide. 16a This included five cats that were considered<br />
<strong>com</strong>plete responders based on resolution of<br />
clinical and laboratory indices of diabetes by the fourth<br />
week of therapy. Eight cats considered to be partial responders<br />
did have resolution of clinical signs but remained<br />
hyperglycemic (greater than 200 mg/dl) and<br />
glucosuric.<br />
In 1997, Feldman and coworkers monitored glycemic<br />
control in feline diabetics treated with only glipizide <strong>for</strong><br />
50 weeks. 16b Glycemic control was achieved in 44% (22<br />
of 50) of cats. These cats were further classified as <strong>com</strong>plete<br />
responders (14%), partial responders (12%), transient<br />
diabetics (12%), and transient responders (6%).<br />
However, three of these cats had long-term treatment<br />
failure, reducing the overall success rate to 38%. Results<br />
of long-term follow-up in a number of these diabetic<br />
cats supported the presence of type II DM and its progressive<br />
nature. The relationship between the degree and<br />
duration of hyperglycemia prior to therapy and the likelihood<br />
of response to glipizide in cats is unknown. Other<br />
predictive factors <strong>for</strong> determining response to therapy<br />
in cats are also unknown. There<strong>for</strong>e, conservative patient<br />
selection promotes a better success rate when using<br />
glipizide in cats. Guidelines <strong>for</strong> patient selection as well<br />
as therapeutic protocols have been described. 10,17–19<br />
Side Effects<br />
Humans<br />
In humans, adverse effects of sulfonylureas are typically<br />
mild and reversible upon discontinuation of drug<br />
administration. The most important side effect of therapy<br />
is hypoglycemia, which is estimated to occur in 2%<br />
to 4% of humans treated <strong>for</strong> type II DM with a sulfonylurea.<br />
For <strong>com</strong>parison, the incidence of hypoglycemia<br />
due to insulin therapy is the same. 12 Other<br />
<strong>com</strong>mon side effects include cutaneous rashes and GI<br />
disturbance, while less <strong>com</strong>mon side effects include<br />
mild thrombocytopenia, mild hemolytic anemia, and<br />
high liver enzyme activity. 20<br />
Risk factors that predispose humans to adverse effects<br />
include decreased glomerular filtration rate, hepatic<br />
insufficiency, mild DM (mean serum glucose concentration<br />
of 140 mg/dl), and the simultaneous use of<br />
drugs that interact with the pharmacokinetics of sulfonylureas<br />
(e.g., aspirin, trimethoprim, H 2-blockers,<br />
warfarin, β-adrenergic blockers, sympatholytic drugs,<br />
thiazides, loop diuretics, corticosteroids). 12,20–22<br />
<strong>Cats</strong><br />
The incidence of side effects due to glipizide in cats<br />
was 16% in 50 cats treated <strong>for</strong> 50 weeks. 16 Commonly<br />
reported side effects are high liver enzyme activity, hepatotoxicity,<br />
anorexia, and vomiting, all of which may<br />
resolve with temporary discontinuation of the drug.<br />
Liver enzyme activity may return to normal despite<br />
continued administration of glipizide, suggesting that<br />
elevated liver enzyme activity may be seen with or<br />
without underlying hepatotoxicity. GI side effects resolve<br />
or improve by administering the drug with food.<br />
Based on current in<strong>for</strong>mation, the incidence of hypoglycemia<br />
(usually asymptomatic) ranges between 12%<br />
to 15%. 7,16b The incidence of mild hypoglycemia may<br />
be underestimated due to the subtle clinical signs associated<br />
with its occurrence. 10<br />
BIGUANIDES (METFORMIN)<br />
Met<strong>for</strong>min is a biguanide antihyperglycemic agent.<br />
The active <strong>com</strong>ponent, guanidine, is found naturally in<br />
animal and plant material and explains the medieval<br />
European practice of administering <strong>com</strong>ponents of the<br />
French lilac flower (Galega officinalis) to diabetic patients.<br />
23 Unlike glipizide, it is not highly protein bound<br />
or metabolized. To date, there are two reports of met<strong>for</strong>min<br />
pharmacokinetics in cats. The mean oral<br />
bioavailability in six healthy adult cats was found to be<br />
48%. 24 The peak plasma concentration occurs between<br />
1 and 3 hours after oral administration. 24,25 Ninety percent<br />
of the drug is excreted in the urine within 12<br />
hours of administration. 26<br />
Because met<strong>for</strong>min improves insulin sensitivity in peripheral<br />
tissues, it is not effective in the absence of insulin.<br />
27 Whereas glipizide results in an increase in<br />
serum insulin concentration to lower blood glucose,<br />
met<strong>for</strong>min results in a decrease in serum insulin concentration.<br />
In humans and rats, therapeutic concentrations of<br />
met<strong>for</strong>min in the liver result in improved insulin-induced<br />
suppression of hepatic gluconeogenesis, which<br />
correlates with decreases in FBG concentrations. 12,26
636 Small Animal/Exotics Compendium July 2001<br />
Also, glucagon-induced gluconeogenesis is reduced. In<br />
myocytes, met<strong>for</strong>min increases the activity of the insulin<br />
receptor tyrosine kinase and enhances the number<br />
and activity of the glucose-transporter-4. Uptake of<br />
glucose by muscle, muscle glycogen <strong>for</strong>mation, and<br />
glucose oxidation are all increased. 28 In adipose tissue,<br />
met<strong>for</strong>min increases the uptake and oxidation of glucose<br />
and increases the binding of insulin to its receptors.<br />
26 The antilipolytic action of insulin is thereby reduced,<br />
causing weight loss even when diet and exercise<br />
are held constant. 27 This benefit in obese patients is in<br />
contrast to insulin and glipizide therapy, which increases<br />
insulin concentrations. 28 Met<strong>for</strong>min has no effect<br />
on insulin production or secretion at the pancreatic<br />
beta cell.<br />
Efficacy<br />
Humans<br />
When used as monotherapy in humans, the FBG level<br />
decreases by a mean of 60 to 70 mg/dl and the Hb<br />
A 1c concentration by a mean of 3%. 7,12,24,26–30 When<br />
<strong>com</strong>pared with other therapies (insulin, glipizide), met<strong>for</strong>min<br />
causes a greater decrease in the PPBG concentration<br />
<strong>com</strong>pared with the FBG concentration.<br />
When used in <strong>com</strong>bination therapy with a sulfonylurea<br />
in humans, the FBG decreases by 63 mg/dl more<br />
than with sulfonylurea alone. 7,31 When patients with<br />
poorly controlled type II DM on insulin were treated<br />
with met<strong>for</strong>min, Hb A 1c concentrations were significantly<br />
lower <strong>com</strong>pared with placebo and there was improved<br />
glycemic control with the use of 30% less insulin.<br />
10,30 This indicates that the hypoglycemic effect of<br />
met<strong>for</strong>min is additive to that of sulfonylureas and insulin<br />
in humans, a concept that has not been studied in<br />
cats.<br />
Primary treatment failure, defined as failure to<br />
achieve glycemic control at the onset of therapy, occurs<br />
at an overall incidence of 12% in humans. 7,10 As with<br />
most patients, the incidence of secondary treatment<br />
failure (failure to maintain target glycemic levels after<br />
an initial positive response) with met<strong>for</strong>min increases<br />
with duration of therapy because of the progressive nature<br />
of type II DM.<br />
<strong>Cats</strong><br />
Recently, 25 five newly diagnosed diabetic cats and one<br />
acromegalic diabetic cat that was on insulin therapy<br />
were given met<strong>for</strong>min (10 mg sid to 50 mg bid PO).<br />
Clinical signs, blood glucose, serum fructosamine, and<br />
Hb A 1c values did not improve after 7 weeks in three<br />
cats. There was no improvement in the cat with diabetes<br />
and acromegaly. One cat developed ketoacidosis, and<br />
one was found dead (cause unknown) 2 weeks after ini-<br />
BOX 1<br />
Chronic Hyperglycemia: A Brief Review<br />
Chronic hyperglycemia causes pancreatic beta cells<br />
to be desensitized to glucose, resulting in impaired<br />
insulin secretion. In addition, there is relative insulin<br />
resistance in peripheral tissues. Insulin receptors can<br />
move beneath the cell membrane as a result of chronic<br />
hyperglycemia, and the glucose transport systems<br />
be<strong>com</strong>e dysfunctional. 4 The end result is a low serum<br />
insulin concentration with hyperglycemia (this is in<br />
contrast to insulin resistance, characterized by a<br />
very high insulin concentration ac<strong>com</strong>panying<br />
hyperglycemia). Glucose-induced desensitization<br />
of the pancreas and peripheral tissues is reversible.<br />
Glucose toxicity is the term used <strong>for</strong> an irreversible<br />
state of beta-cell dysfunction and resembles type I<br />
DM because the pancreas be<strong>com</strong>es unresponsive after<br />
stimulation by insulin secretagogues despite its ability<br />
to produce insulin. There<strong>for</strong>e, results of insulin<br />
secretory tests to distinguish type I from type II DM<br />
in cats are inconsistent partly because of the effects of<br />
glucose-induced desensitization and glucose toxicity. 3<br />
A clinically useful way of distinguishing type I from<br />
type II DM in cats may be to evaluate response to<br />
treatment with antidiabetic drugs.<br />
tiating met<strong>for</strong>min administration. One cat achieved improved<br />
glycemic control <strong>for</strong> 5 months and then developed<br />
acute pancreatitis and loss of glycemic control.<br />
There are no other published data on the efficacy of<br />
met<strong>for</strong>min in cats. It has been speculated that many cats<br />
suffer from glucose toxicity as a result of chronic hyperglycemia<br />
(Box 1); there<strong>for</strong>e, improving insulin sensitivity<br />
in peripheral tissues by using met<strong>for</strong>min may provide<br />
little benefit in cats with glucose toxicity.<br />
Side Effects<br />
Humans<br />
The overall incidence of adverse effects of met<strong>for</strong>min<br />
treatment in humans is 20% to 30%. The most <strong>com</strong>mon<br />
effects are diarrhea, nausea, abdominal pain, and a<br />
metallic taste. 28 Side effects can be minimized by taking<br />
met<strong>for</strong>min with food and by slowly increasing the dose<br />
in small increments once therapy is initiated. 10,27<br />
Hypoglycemia is a rare occurrence in humans treated<br />
with met<strong>for</strong>min alone because the drug does not increase<br />
insulin secretion. An un<strong>com</strong>mon yet potentially<br />
fatal adverse effect of met<strong>for</strong>min therapy documented<br />
in humans is lactic acidosis, with an estimated incidence<br />
of 0.027 to 0.06 cases per 1000 patient-years. 12,28<br />
Met<strong>for</strong>min precipitates lactic acidosis by promoting the
Compendium July 2001 Small Animal/Exotics 637<br />
conversion of ingested carbohydrate to lactate by the<br />
intestinal mucosa, which is subsequently absorbed and<br />
metabolized by the liver. 10 Incriminating met<strong>for</strong>min as<br />
the sole cause of all lactate elevations is <strong>com</strong>plicated because<br />
obesity and diabetes also slightly raise blood lactate<br />
concentrations. 26<br />
In most patients suffering from met<strong>for</strong>min-associated<br />
lactic acidosis, predisposing factors include concurrent<br />
renal insufficiency, liver disease, or other major illness<br />
causing tissue hypoperfusion or hypoxia. 10,12,26 The<br />
risk of death from met<strong>for</strong>min-induced lactic acidosis<br />
(50%) is similar to that of severe hypoglycemia in sulfonylurea-treated<br />
patients. 26<br />
There are infrequent reports of drug interactions<br />
with met<strong>for</strong>min. In humans, cimetidine causes an elevation<br />
of plasma met<strong>for</strong>min by <strong>com</strong>petition <strong>for</strong> renal<br />
tubular secretion. 28<br />
<strong>Cats</strong><br />
There is little in<strong>for</strong>mation on the adverse effects of<br />
met<strong>for</strong>min in cats. In cats, the drug appears to be excreted<br />
primarily by glomerular filtration. 24 The effects<br />
of cimetidine on plasma met<strong>for</strong>min concentration in<br />
cats are unknown.<br />
In one study, six healthy male cats received met<strong>for</strong>min<br />
(25 mg sid <strong>for</strong> 7 days, then 25 mg bid <strong>for</strong> 14<br />
days) and two cats received placebo. All six cats receiving<br />
met<strong>for</strong>min, but neither cat receiving the placebo,<br />
developed a <strong>com</strong>bination of inappetence, weight loss,<br />
and/or intermittent vomiting. 25 In another study, six<br />
healthy adult cats were given 25 mg met<strong>for</strong>min IV and<br />
PO. There was no mention of adverse effects (e.g.,<br />
vomiting). 24<br />
THIAZOLIDINEDIONES (TROGLITAZONE)<br />
Thiazolidinediones were discovered by Japanese scientists<br />
almost 2 decades ago as they were studying <strong>com</strong>pounds<br />
to serve as hypolipidemic drugs. 32 One analogue,<br />
troglitazone, was approved <strong>for</strong> human use by the<br />
FDA in 1997. Troglitazone is rapidly absorbed (its<br />
bioavailability is 40% to 50%), and food increases the<br />
absorption. 33 In humans, troglitazone undergoes<br />
metabolism by sulfation, glucuronidation, and oxidation<br />
into active conjugates. Hepatic impairment causes<br />
plasma concentrations of troglitazone to increase. 33 Despite<br />
proven efficacy, its suitability as a first-line drug to<br />
treat type II DM has been questioned because of the<br />
risk of severe liver dysfunction. 34,35<br />
Like met<strong>for</strong>min, troglitazone enhances peripheral insulin<br />
sensitivity and thereby lowers both glucose and<br />
insulin levels. Troglitazone reduces the expression of<br />
specific genes responsible <strong>for</strong> producing the regulatory<br />
enzymes of hepatic gluconeogenesis, thereby slowing<br />
the rate of hepatic gluconeogenesis. 36 In muscle and fat,<br />
thiazolidinediones cause an increase in intracellular glucose<br />
transport, which increases glucose metabolism and<br />
decreases peripheral demand <strong>for</strong> insulin. 10,12,37 Troglitazone<br />
has no effect on insulin production or secretion at<br />
the pancreatic beta cell.<br />
Efficacy<br />
Humans<br />
Clinical trials show that troglitazone achieves longterm<br />
(up to 2 years) glycemic control in humans. 32,33,35,37<br />
To date, six trials examining troglitazone as the sole<br />
agent <strong>for</strong> treating type II DM showed a mean decrease<br />
in FBG of 34 mg/dl and in Hb A 1c of 0.6%. 12 There<strong>for</strong>e,<br />
troglitazone is not as efficacious as monotherapy<br />
when <strong>com</strong>pared with other classes of antidiabetic drugs.<br />
Primary treatment failure occurs in 25% of humans<br />
with type II DM treated with troglitazone alone. 12,35<br />
Troglitazone is more effective in patients with the syndrome<br />
of insulin resistance, where serum insulin concentrations<br />
are very high. This is in keeping with the<br />
described mechanism of action in peripheral tissues<br />
(enhancing insulin sensitivity). Combination therapy<br />
with met<strong>for</strong>min is not re<strong>com</strong>mended because troglitazone<br />
and met<strong>for</strong>min have similar mechanisms of action<br />
and do not show <strong>com</strong>plementary effects as do met<strong>for</strong>min<br />
and a sulfonylurea or troglitazone and a sulfonylurea.<br />
<strong>Cats</strong><br />
There is no published in<strong>for</strong>mation on the efficacy of<br />
troglitazone in cats.<br />
Side Effects<br />
Humans<br />
Troglitazone-related adverse effects occurred in one<br />
fourth of patients using troglitazone either as monotherapy<br />
or in <strong>com</strong>bination with a sulfonylurea. 34,35–38<br />
Liver-related death occurs in 1 of 100,000 humans. 35<br />
This has raised questions regarding the role of troglitazone<br />
in the repertoire of antidiabetic drugs; there<strong>for</strong>e,<br />
troglitazone is no longer re<strong>com</strong>mended by the FDA as<br />
monotherapy. 12 The causative mechanism of hepatotoxicity<br />
is unknown but may represent idiosyncratic injury<br />
as a result of aberrant metabolism, resulting in the accumulation<br />
of hepatotoxic metabolites. 39<br />
Troglitazone may cause expansion of the plasma volume;<br />
5% of patients receiving the drug experience edema.<br />
Its use is contraindicated in patients with New<br />
York Heart Association class III or IV cardiac status. 12,38
638 Small Animal/Exotics Compendium July 2001<br />
<strong>Cats</strong><br />
There are no published data on adverse effects of<br />
troglitazone in cats.<br />
α-GLUCOSIDASE INHIBITORS (ACARBOSE)<br />
α-Glucosidase inhibitors delay glucose absorption<br />
from the GI tract. Acarbose, an α-glucosidase inhibitor,<br />
is an oligosaccharide extracted from the bacterium<br />
Actinomyces. It was first developed as a starch blocker<br />
<strong>for</strong> obesity. Acarbose was introduced in the United<br />
States in 1995 and has recently been studied <strong>for</strong> use in<br />
domestic animals. 40,41<br />
Dietary control of blood glucose through stringent<br />
dietary regimens has been the proposed foundation of<br />
early therapy <strong>for</strong> human diabetes, but non<strong>com</strong>pliance<br />
with eating small, frequent meals is high. 7,10 Similarly,<br />
owners of diabetic cats are often unable to provide<br />
small, frequent meals. Appropriate dietary therapy <strong>for</strong><br />
diabetic cats is outlined elsewhere. 19<br />
Acarbose inhibits the α-glucosidases, which include<br />
enzymes produced in the brush border of the small intestine.<br />
Sucrase, maltase, isomaltase, glucoamylase, lactase,<br />
and others function to digest oligosaccharides and<br />
disaccharides (<strong>com</strong>plex carbohydrates) into monosaccharides<br />
(glucose), which are subsequently absorbed<br />
through the small intestine. 42 Acarbose <strong>com</strong>petitively<br />
and reversibly inhibits these enzymes, delaying the hydrolysis<br />
of <strong>com</strong>plex carbohydrates without affecting the<br />
absorption of the glucose molecule. 10 Carbohydrate absorption<br />
then shifts to more distal parts of the intestines.<br />
43 Carbohydrates that reach the large intestine<br />
are metabolized by colonic bacteria into fatty acids <strong>for</strong><br />
absorption.<br />
Acarbose does not cause a malabsorptive state; rather,<br />
it slows the digestive and absorptive processes. The end<br />
result is a blunted entry of glucose into the systemic<br />
circulation, thus reaching the pancreatic beta cell at<br />
lower blood concentrations. 44,45 Acarbose does not decrease<br />
hepatic glucose output or reverse any pathophysiologic<br />
derangements in patients with diabetes. In fact,<br />
the drug is not systemically absorbed.<br />
Efficacy<br />
Humans<br />
Human studies with acarbose have documented a<br />
decrease in PPBG concentrations and glucosuria <strong>for</strong><br />
up to 3 years irrespective of con<strong>com</strong>itant therapy.<br />
10,42,44–48 This occurs in both insulin- and non–insulin-dependent<br />
DM, which may have implications<br />
<strong>for</strong> veterinary medicine because discriminating between<br />
type I and type II DM would not be a factor in<br />
deciding whether or when to prescribe the drug. When<br />
used alone in humans, acarbose decreased the FBG<br />
level by only 25 to 30 mg/dl, the PPBG level by 40 to<br />
50 mg/dl, and the Hb A 1c concentration by 0.5% to<br />
1.2%. 49–51 Although less potent than insulin, glipizide,<br />
or met<strong>for</strong>min, acarbose is prescribed as initial and adjunctive<br />
therapy in obese patients. Acarbose does not<br />
affect the absorption of other antidiabetic drugs. It is<br />
not re<strong>com</strong>mended <strong>for</strong> patients with normal or decreased<br />
body condition. 50<br />
<strong>Cats</strong><br />
The efficacy of acarbose in cats is not established. Because<br />
acarbose works by interfering with starch digestion<br />
and absorption, its effectiveness needs to be studied<br />
in cats in light of their low carbohydrate intake<br />
when <strong>com</strong>pared with humans. 12 Recently, seven obese<br />
diabetic cats (five on insulin therapy) were evaluated <strong>for</strong><br />
the effects of acarbose (12.5 mg PO bid with meals)<br />
and a high-protein diet on glycemic control. Insulin administration<br />
was discontinued in four of five cats during<br />
the course of the 4-month study. Improved serum<br />
fructosamine and FBG concentrations as well as improved<br />
attitude <strong>com</strong>pared with pretreatment values<br />
were noted in six cats. 41<br />
Side Effects<br />
Humans/Dogs<br />
Up to 30% of humans experience mild and transient<br />
GI side effects from acarbose that diminish despite continued<br />
drug use. Bloating with abdominal dis<strong>com</strong><strong>for</strong>t,<br />
flatulence, and diarrhea have been reported. 45,52–55 In<br />
five healthy dogs fed a high-fiber diet and given 200<br />
mg acarbose daily, four dogs developed soft to watery<br />
stools and two dogs lost weight during the study. 40<br />
To minimize the incidence of GI side effects, acarbose<br />
therapy should be initiated with a low dose and<br />
gradually increased to reach the minimally effective<br />
dose. 48 Food must be present in the bowel with acarbose<br />
<strong>for</strong> the drug to have its effect, but side effects may<br />
occur regardless of the presence or absence of food.<br />
Other adverse effects are dose dependent and include<br />
high liver enzyme activities and abnormal results of liver<br />
function tests. These abnormalities resolve when the<br />
drug is discontinued. Hypoglycemia does not occur as a<br />
direct result of acarbose therapy. However, if hypoglycemia<br />
occurs due to concurrent administration of<br />
other antidiabetic drugs (insulin, glipizide), pure glucose<br />
should be ingested. 52–55<br />
<strong>Cats</strong><br />
The appropriate dose <strong>for</strong> cats has not been established.
Compendium July 2001 Small Animal/Exotics 639<br />
CONCLUSION<br />
The mechanism of action, efficacy, and side effects of<br />
the oral antidiabetic drugs glipizide, met<strong>for</strong>min, troglitazone,<br />
and acarbose have been extensively studied in<br />
humans but not in cats. On the basis of limited data,<br />
glipizide and acarbose appear to have the most efficacy<br />
and the least potential <strong>for</strong> toxicity when <strong>com</strong>pared with<br />
met<strong>for</strong>min and troglitazone. Careful patient selection is<br />
important. <strong>Oral</strong> antidiabetic drugs may be appropriate<br />
<strong>for</strong> cats that are in good overall health with early or<br />
mild clinical signs of diabetes and those with owners<br />
who are unwilling or unable to administer insulin injections.<br />
There are <strong>com</strong>plications 56 and many uncertainties<br />
regarding the current use of oral antidiabetic<br />
agents in cats. They should not be used in cats with evidence<br />
of diabetic <strong>com</strong>plications (e.g., ketoacidosis, infection,<br />
any concurrent disease).<br />
Although the difficulty in differentiating between<br />
type I and II DM in cats <strong>com</strong>plicates the ideal treatment<br />
plan <strong>for</strong> each patient, it is clear that not every<br />
newly diagnosed diabetic cat requires exogenous insulin.<br />
Hyperglycemia in cats with type II DM may be a<br />
reflection of impaired insulin secretion from the pancreas,<br />
increased hepatic glucose output, decreased peripheral<br />
insulin sensitivity, and intestinal glucose ab-<br />
sorption. If so, therapy would ideally revolve around<br />
correcting these abnormalities by the use of dietary<br />
changes, oral antidiabetic agents, insulin, or a <strong>com</strong>bination<br />
of these treatments. 4,10,12,18,32,57–59<br />
Some cats that are exquisitely sensitive to insulin may<br />
benefit from a diet change and the use of an oral agent<br />
without insulin. Other cats that are well maintained<br />
with insulin and then be<strong>com</strong>e unregulated may represent<br />
the progressive nature of type II diabetes; these cats<br />
may also benefit from the addition of drugs (e.g., glipizide<br />
or acarbose alone or with insulin). More in<strong>for</strong>mation<br />
is needed on the use of <strong>com</strong>bination therapy in<br />
cats and the efficacy and/or toxicity of met<strong>for</strong>min and<br />
troglitazone. Initial observations have not been encouraging.<br />
The reason <strong>for</strong> the apparent lack of efficacy <strong>com</strong>pared<br />
with that in humans remains unknown but may<br />
be related to low serum insulin concentrations associated<br />
with glucose toxicity.<br />
Improving recognition of type II DM in cats and further<br />
study of oral antidiabetic agents are important <strong>for</strong><br />
managing the unique characteristics of feline diabetes.<br />
To date, clinical trial data are insufficient in both human<br />
and veterinary medicine <strong>for</strong> determining the optimal<br />
insulin <strong>for</strong>mulation and optimal <strong>com</strong>binations and<br />
dosages of oral agents. 59 We hope that future research
640 Small Animal/Exotics Compendium July 2001<br />
will provide clues to the many unanswered questions<br />
regarding glycemic control in cats.<br />
REFERENCES<br />
1. Feldman EC, Nelson RW: Diabetes mellitus, in Feldman<br />
EC, Nelson RW (eds): Canine and Feline Endocrinology and<br />
Reproduction, ed 2. Philadelphia, WB Saunders Co, 1996,<br />
pp 339–391.<br />
2. Kirk CA, Feldman EC, Nelson RW: Diagnosis of naturally<br />
acquired type-I and type-II diabetes mellitus in cats. Am J<br />
Vet Res 54:463–467, 1993.<br />
3. Nelson RW, Griffey SM, Feldman EC, Ford SL: Transient<br />
clinical diabetes mellitus in cats: 10 Cases (1989–1991). J<br />
Vet Intern Med 13:28–35, 1999.<br />
4. DeFronzo RA, Bonadonna RC, Ferrannini E: Pathogenesis<br />
of NIDDM: A balanced overview. Diabetes Care 15:318–<br />
368, 1992.<br />
5. Pimenta W, Korytkowski M, Mitra A, et al: Pancreatic Bcell<br />
dysfunction as the primary genetic lesion in NIDDM.<br />
JAMA 273:1855–1861, 1995.<br />
6. Johnson KH, O’Brien TD, Betsholtz C, Westermark P: Islet<br />
amyloid, islet-amyloid polypeptide, and diabetes mellitus. N<br />
Engl J Med 321:513–518, 1989.<br />
7. Turner RC, Cull CA, Frighi V, Homan RR: The UK Prospective<br />
Diabetes Study Group (UKPDS). JAMA 281:2005–<br />
2012, 1999.<br />
8. Rubin RJ, Altman WM, Mendelson DN: Health care expenditures<br />
<strong>for</strong> people with diabetes mellitus, 1992. J Clin<br />
Endocrinol Metab 78:809, 1994.<br />
9. Melander A: Clinical pharmacology of sulfonylureas.<br />
Metabolism 28:12–16, 1987.<br />
10. Bressler R, Johnson DG: Pharmacological regulation of<br />
blood glucose levels in non-insulin-dependent diabetes mellitus.<br />
Arch Intern Med 157:836–848, 1997.<br />
11. Malaisse WJ, Lebrun P: Mechanism of sulfonylurea-induced<br />
insulin release. Diabetes Care 13:9–17, 1990.<br />
12. DeFronzo RA: Pharmacologic therapy <strong>for</strong> type 2 diabetes<br />
mellitus. Ann Intern Med 131:281–303, 1999.<br />
13. Lebovitz HE, Melander A: Sulfonylureas: Basic aspects and<br />
clinical uses, in Alberti KG, Zimmet P, DeFronzo RA (eds):<br />
International Textbook of Diabetes Mellitus, ed 2. New York,<br />
J Wiley, 1997, pp 817–840.<br />
14. Blaum CS, Velez L, Hiss RG, Halter JB: Characteristics related<br />
to poor glycemic control in type II DM patients in<br />
<strong>com</strong>munity practice. Diabetes Care 20:7–11, 1997.<br />
15. Miller AB, Nelson RW, Kirk CA, et al: Effect of glipizide on<br />
serum insulin and glucose concentrations in healthy cats. Res<br />
Vet Sci 52:177–181, 1992.<br />
16a.Nelson RW, Feldman EC, Ford SL, Roemer OP: Effect of<br />
an orally administered sulfonylurea, glipizide, <strong>for</strong> treatment<br />
of diabetes mellitus in cats. JAVMA 203:821–827, 1993.<br />
16b.Feldman EC, Nelson RW, Feldman MS: Intensive 50-week<br />
evaluation of glipizide administration in 50 cats with previously<br />
untreated diabetes mellitus. JAVMA 210:772–777,<br />
1997.<br />
17. Garcia JL, Bruyette DS: Using oral hypoglycemic agents to<br />
treat diabetes mellitus in cats. Vet Med 736–742, 1998.<br />
18. Greco DS: Treatment of non–insulin-dependent diabetes<br />
mellitus with oral hypoglycemic agents. Proc 15 th ACVIM<br />
Forum:252–254, 1997.<br />
19. Behrend EN, Greco DS: Treatment of feline diabetes mellitus:<br />
Overview and therapy. Compend Contin Educ Pract Vet<br />
22:423–438, 2000.<br />
20. Heine RJ: Role of sulfonylureas in NIDDM: Part II—The<br />
cons. Horm Metab Res 28:522–526, 1996.<br />
21. Lebovitz HE, Melander A: Sulfonylureas: Basic aspects and<br />
clinical uses, in Alberti KG, Zimmet P, DeFronzo RA (eds):<br />
International Textbook of Diabetes Mellitus, ed 2. New York,<br />
J Wiley, 1997, pp 745–772.<br />
22. Seltzer HS: Drug-induced hypoglycemia: A review of 1418<br />
cases. Endocrinol Metab Clin North Am 18:163–183, 1989.<br />
23. Bailey CJ, Day C: Traditional plant medicines as treatments<br />
<strong>for</strong> diabetes. Diabetes Care 12:553–564, 1989.<br />
24. Michels GM, Boudinot FD, Ferguson DC, Hoenig M:<br />
Pharmacokinetics of the antihyperglycemic agent met<strong>for</strong>min<br />
in cats. Am J Vet Res 60:738–742, 1999.<br />
25. Spann D, Nelson R, et al: Evaluation of met<strong>for</strong>min in<br />
healthy and diabetic cats. Proc 18 th ACVIM Forum:722, 2000.<br />
26. Baily CJ, Turner RC: Met<strong>for</strong>min. N Engl J Med 334:<br />
574–578, 1996.<br />
27. Stumvoll M, Nurjhan N, Perriello G, et al: Metabolic effects<br />
of met<strong>for</strong>min in non–insulin-dependent diabetes mellitus.<br />
N Engl J Med 333:550–554, 1995.<br />
28. Melchior WR, Jaber LA: Met<strong>for</strong>min: An antihyperglycemic<br />
agent <strong>for</strong> treatment of type II diabetes. Ann Pharmacother<br />
30:158–164, 1996.<br />
29. Johansen K: Efficacy of met<strong>for</strong>min in the treatment of<br />
NIDDM. Meta-analysis. Diabetes Care 22:33–37, 1999.<br />
30. Aviles SL, Sindling J, Raskin P: Effects of met<strong>for</strong>min in patients<br />
with poorly controlled, insulin-treated type 2 diabetes<br />
mellitus. A randomized, double-blind, placebo-controlled<br />
trial. Ann Intern Med 131:182–188, 1999.<br />
31. Groop LC, Bonadonna RC, Del Prato S, et al: Glucose and<br />
free fatty acid metabolism in non–insulin-dependent diabetes<br />
mellitus. Evidence <strong>for</strong> multiple sites of insulin resistance.<br />
J Clin Invest 84:205–213, 1989.<br />
32. Kuehnle HF: New therapeutic agents <strong>for</strong> the treatment of<br />
NIDDM. Exp Clin Endocrinol Diabetes 104:93–101, 1996.<br />
33. Loi CM, Young M, et al: Clinical pharmacokinetics of<br />
troglitazone. Clin Pharmacokinet 37:91–104, 1999.<br />
34. Wagenaar LJ, Kuck EM, Hoekstra JB: Troglitazone. Is it all<br />
over? Neth J Med 55:4–12, 1999.<br />
35. Plosker GL, Faulds D: Troglitazone: A review of its use in<br />
the management of type 2 diabetes mellitus. <strong>Drugs</strong> 57:409–<br />
438, 1999.<br />
36. Davies GF, Khandelwal RL, Roesler WJ: Troglitazone inhibits<br />
expression of the phosphoenolpyruvate carboxykinase<br />
gene by an insulin-independent mechanism. Biochim Biophys<br />
Acta 1451:122–131, 1999.<br />
37. Buysschaert M, Bobbioni E, Starkie M, Frith L: Troglitazone<br />
in <strong>com</strong>bination with sulfonylurea improves glycemic<br />
control in Type 2 diabetic patients inadequately controlled<br />
by sulfonylurea therapy alone. Troglitazone Study Group.<br />
Diabetes Med 16:147–153, 1999.<br />
38. Hirsch IB, Kelly J, Cooper S: Pulmonary edema associated<br />
with troglitazone therapy [letter]. Arch Intern Med 159:<br />
1811, 1999.<br />
39. Fukano M, Amano S, et al: Subacute hepatic failure associated<br />
with a new antidiabetic agent, troglitazone: A case report<br />
with autopsy examination. Human Pathol 31:250–253,<br />
2000.<br />
40. Robertson J, Nelson R, Kass P, Neal L: Effects of the alphaglucosidase<br />
inhibitor acarbose on postprandial serum glucose<br />
and insulin concentrations in healthy dogs. Am J Vet Res<br />
60:541–545, 1999.<br />
41. Mazzaferro EM, Greco DS, Turner SJ: Treatment of feline
Compendium July 2001 Small Animal/Exotics 641<br />
diabetes mellitus with a high-protein diet and acarbose. Proc<br />
18 th ACVIM Forum:722, 2000.<br />
42. Kelley DE, Bidot P, Freedman Z, et al: Efficacy and safety of<br />
acarbose in insulin-treated patients with type 2 diabetes. Diabetes<br />
Care 21:2056–2061, 1998.<br />
43. Vierhapper H, Bratusch-Marrain A, Waldausl W: Alphaglucoside<br />
hydrolase inhibition in diabetes. Lancet 2:1386,<br />
1978.<br />
44. Walton RJ, Sherif IT, Noy GA, et al: Improved metabolic<br />
profiles in insulin-treated diabetic patients given an alphaglucosidehydrolase<br />
inhibitor. BMJ 1:220–221, 1979.<br />
45. Coniff RF, et al: A double-blind placebo-controlled trial<br />
evaluating the safety and efficacy of acarbose <strong>for</strong> the treatment<br />
of patients with insulin-requiring type II diabetes. Diabetes<br />
Care 18:928–932, 1995.<br />
46. Holamn RR, Cull CA, Turner RC: A randomized doubleblind<br />
trial of acarbose in type 2 diabetes shows improved<br />
glycemic control over 3 years (UK Prospective Diabetes<br />
Study 44). Diabetes Care 22:960–964, 1999.<br />
47. Mertes G: Efficacy and safety of acarbose in the treatment of<br />
type 2 diabetes: Data from a 2-year surveillance study. Diabetes<br />
Res Clin Pract 40:63–70, 1998.<br />
48. Mooradian AD, Albert SG, et al: Dose-response profile of<br />
acarbose in older subjects with type 2 diabetes. Am J Med<br />
Sci 319(5):334–337, 2000.<br />
49. Chiasson JL, Josse RG, Hunt JA, et al: The efficacy of acarbose<br />
in the treatment of patients with non–insulin-dependent<br />
diabetes mellitus. Ann Intern Med 121:928–935, 1994.<br />
50. Scheen AJ: Clinical efficacy of acarbose in diabetes mellitus:<br />
A critical review of controlled trials. Diabetes Metab 24:<br />
311–320, 1998.<br />
51. Hanefeld M: The role of acarbose in the treatment of noninsulin-dependent<br />
diabetes mellitus. J Diabetes Complications<br />
12:228–237, 1998.<br />
52. Odawara M, Bannai C, Saitoh T, et al: Potentially lethal<br />
ileus associated with acarbose treatment <strong>for</strong> NIDDM [letter].<br />
Diabetes Care 20:1210–1211, 1997.<br />
53. Scorpiglione N, Belfiglio M, Carinci F, et al: The effectiveness,<br />
safety and epidemiology of the use of acarbose in the<br />
treatment of patients with type II diabetes mellitus. A model<br />
of medicine-based evidence. Eur J Clin Pharmacol 55:239–<br />
249, 1999.<br />
54. Riccardi G, Giacco R, Parillo M, et al: Efficacy and safety of<br />
acarbose in the treatment of type I diabetes mellitus: A<br />
placebo-controlled, double-blind, multicentre study. Diabetes<br />
Med 16:228–232, 1999.<br />
55. Ranganath L, Norris F, Morgan L, et al: Delayed gastric<br />
emptying occurs following acarbose administration and is a<br />
further mechanism <strong>for</strong> its antihyperglycemic effect. Diabetes<br />
Med 15:120–124, 1998.<br />
56. Nelson RW, Feldman EC: Complications associated with<br />
insulin treatment of diabetes mellitus, in Kirk RW, Bonagura<br />
JD (eds): Current Veterinary Therapy XIII. Philadelphia,<br />
WB Saunders Co, 1999, pp 354–357.<br />
57. Greco DS: Treatment of non–insulin-dependent diabetes<br />
mellitus in cats using oral hypoglycemic agents, in Kirk RW,<br />
Bonagura JD (eds): Current Veterinary Therapy XIII.<br />
Philadelphia, WB Saunders Co, 1999, pp 350–354.<br />
58. American Diabetes Association: Standards of medical care<br />
<strong>for</strong> patients with diabetes mellitus. Diabetes Care<br />
17:616–623, 1994.<br />
59. Buse J: Combining insulin and oral agents. Am J Med 108<br />
(Suppl 6a):235–325, 2000.<br />
ARTICLE<br />
CE<br />
#2 CE TEST<br />
The article you have read qualifies <strong>for</strong> 1.5 contact<br />
hours of Continuing Education Credit from<br />
the Auburn University College of Veterinary<br />
Medicine. Choose the best answer to each of the fol-<br />
lowing questions; then mark your answers on the<br />
postage-paid envelope inserted in Compendium.<br />
1. Which of the following is not a result of glucose toxicity?<br />
a. desensitization of the pancreatic beta cell to glucose<br />
b. dysfunctional glucose transport systems in peripheral<br />
tissues<br />
c. movement of peripheral insulin receptors beneath<br />
the cell membrane<br />
d. low serum insulin concentration<br />
e. depletion of liver glycogen stores<br />
2. Insulin resistance is characterized by _____ serum insulin<br />
concentration and _____ blood glucose.<br />
a. high; low<br />
b. high; high<br />
c. low; high<br />
d. low; normal<br />
e. low; low<br />
3. The direct physiologic stimulus <strong>for</strong> insulin secretion<br />
by the pancreatic beta cell is<br />
a. closing of the ATP–potassium channel.<br />
b. hypoglycemia.<br />
c. intracellular calcium influx.<br />
d. intracellular potassium influx.<br />
e. opening of the ATP–potassium channel.<br />
4. In humans, the likelihood of response to glipizide is<br />
improved by selecting patients with<br />
a. mild to moderate hyperglycemia.<br />
b. marked hyperglycemia.<br />
c. insulin resistance.<br />
d. a history of ketoacidosis.<br />
e. ketonuria.<br />
5. All of the following are reported adverse effects of glipizide<br />
therapy in cats except<br />
a. jaundice.<br />
b. vomiting.<br />
c. hypoglycemia.<br />
d. constipation.<br />
e. high liver enzyme activity.<br />
6. To which class of drugs does met<strong>for</strong>min belong?<br />
a. α-glucosidase inhibitors<br />
b. biguanides
642 Small Animal/Exotics Compendium July 2001<br />
c. sulfonylureas<br />
d. thiazolidinediones<br />
e. glycosylated proteins<br />
7. Which of the following are mechanisms by which<br />
met<strong>for</strong>min lowers the blood glucose concentration?<br />
a. improved insulin-induced suppression of hepatic<br />
gluconeogenesis<br />
b. increased stimulation of insulin secretion by the<br />
pancreas<br />
c. enhanced number and activity of glucose transporters<br />
into myocytes<br />
d. increased uptake and oxidation of glucose in adipose<br />
tissue<br />
e. a, c, and d<br />
8. Troglitazone is not <strong>com</strong>monly used in cats because<br />
a. clinical trials have shown that it does not lower<br />
blood glucose concentrations in cats as it does in<br />
humans.<br />
b. it causes profound hypoglycemia in cats.<br />
c. it causes renal toxicity in cats.<br />
d. its efficacy and toxicity in cats is unknown.<br />
e. it cannot be used con<strong>com</strong>itantly with insulin.<br />
9. In a study of seven obese diabetic cats evaluated <strong>for</strong> the<br />
effects of acarbose,<br />
a. insulin administration could not be discontinued in<br />
any of the cats due to refractory hyperglycemia during<br />
acarbose administration.<br />
b. the cats did not tolerate acarbose administration<br />
due to the metallic taste reported in humans.<br />
c. serum fructosamine and FBG concentrations were<br />
improved <strong>com</strong>pared with pretreatment values in<br />
most of the cats.<br />
d. the drug resulted in <strong>com</strong>plete resolution of clinical<br />
signs of DM in all seven cats.<br />
e. long-term follow up on all seven cats showed<br />
glycemic control on acarbose alone after 1 year.<br />
10. Which of the following statements regarding acarbose<br />
administration is true?<br />
a. Acarbose must be taken on an empty stomach in<br />
order to have an affect.<br />
b. Compared with glipizide, met<strong>for</strong>min, and troglitazone,<br />
acarbose has the most profound effect in lowering<br />
the blood glucose concentration.<br />
c. The use of acarbose is not suitable <strong>for</strong> insulin-dependent<br />
DM (type I).<br />
d. Therapeutic serum concentrations of acarbose are<br />
met by tid administration.<br />
e. GI side effects in humans are usually transient and<br />
diminish despite continued use.