prvi bosansko-hercegovački i drugi jadranski kongres ...
prvi bosansko-hercegovački i drugi jadranski kongres ...
prvi bosansko-hercegovački i drugi jadranski kongres ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
FOLIA MEDICA FACULTATIS MEDICINAE UNIVERSITATIS SARAEVIENSIS<br />
Journal of Medical Faculty University of Sarajevo, Bosnia&Herzegovina<br />
Contents<br />
2012;47(1-suppl)<br />
PODIUM LECTURES<br />
APPLIED PHARMACOECONOMICS: HOW PHARMACOECONOMICS CAN BE APPLIED<br />
TO SUPPORT DECISIONS BY DIFFERENT STAKEHOLDERS IN HEALTH CARE?<br />
Zoltán Kaló, Dinko Vitezić . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10<br />
THE ROLE OF PHARMACOECONOMICS AND HEALTH TECHNOLOGY ASSESSMENT<br />
IN ENSURING PATIETNS’ EQUITY RIGHTS<br />
Faris Gavrankapetanović . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12<br />
ENSURING EQUITY AND AVAILABILITY OF HEALTHCARE REGARDING PATIENTS’<br />
RIGHT ON EFFECTIVE, SAFE, QUALITY AND AVAILABLE ESSENTIAL DRUGS IN<br />
FEDERATION OF BOSNIA AND HERZEGOVINA<br />
Rusmir Mesihović, Sanja Ćustović . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13<br />
MEDICINES POLICY IN THE REPUBLIC OF SRPSKA – AVAILABILITY AND EQUALITY<br />
Vanda Marković Peković . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14<br />
REIMBURSEMENT OF EXPENSIVE HOSPITAL DRUGS IN SLOVENIA<br />
Jurij Fürst, Rozeta Hafner . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15<br />
VALUE BASED PRICING – ONGOING HTA REFORM IN THE UK<br />
Petr Hajek . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16<br />
TRANSFERABILITY OF NICE RECOMMENDATIONS TO LOWER INCOME COUNTRIES:<br />
THE CASE OF ONCOLOGY DRUGS<br />
Zoltán Kaló . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17<br />
ADJUSTMENT AND IMPLEMENTATION OF CROATIAN P&R MODEL<br />
Bruna Buble, Tonči Buble, Vesna Bačić Vrca, Dinko Vitezić . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18<br />
HEALTH TECHNOLOGY ASSESSMENT IN SERBIA<br />
Vlad Zah . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19<br />
PRICING POLICY IN MACEDONIA – OVERVIEW ANALYSIS<br />
Marija Gulija, Gordana Damjanovska . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20<br />
THE BLOCKADE OF SCIATIC NERVE AND POSSIBLE CONSEQUENCES<br />
OF INTRANEURAL INJECTIONS<br />
Livio Garattini, Katelijne van de Vooren . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21<br />
IMPACT OF THERAPEUTIC CLASS REFERENCING (JUMBO GROUPS) AS A METHOD<br />
OF GOVERNMENT COST CONTAINMENT MEASURES ON PRESCRIBING BEHAVIOURS<br />
AND CONSEQUENT QUALITY OF PATIENT CARE<br />
Sani Pogorilić, Jelka Drašković, Slobodanka Bolanča . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22<br />
SHOWING THE USE OF DRUGS IN THE CLINICAL CENTER OF MONTENEGRO<br />
AND COMPARISON WITH MODERN PHARMACOTHERAPEUTIC RECOMMENDATIONS<br />
Mirjana Jovanović-Đurašković, Olivera Prodanović . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23
2<br />
COMPARISON OF DRUGS CONSUMPTION IN TWO CROATIAN COUNTY<br />
GENERAL HOSPITALS<br />
Aleksandar Knežević, Mila Basioli, Hana Kalinić Grgorinić . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24<br />
BURDEN OF COMMUNITY ACQUIRED PNEUMONIA<br />
IN CENTRAL EUROPEAN COUNTRIES<br />
Ales Tichopad, C . Roberts, A . Skoczynska, I . Gembula, K . Jahnz-Rozyk . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25<br />
THE ROLE OF HEALTH AUTHORITIES IN PROMOTION OF RATIONAL USE<br />
OF ANTIBIOTICS<br />
Merjem Hadjihamza . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26<br />
PHARMACOECONOMIC ANALYSIS COMPARING THE USE OF CIPROFLOXACIN<br />
AND METRONIDAZOLE VERSUS ERTAPENEM IN PROPHYLAXIS OF MAYOR SURGICAL<br />
PROCEDURES AT THE UNIVERSITY HOSPITAL REBRO<br />
Ivana Čegec, Robert Likic, Ksenija Makar Ausperger, Viktorija Erdeljic, Matea Radacic Aumiler,<br />
Danica Juricic Nahal, Luka Bielen, Iva Kraljickovic, Igor Francetic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27<br />
IMPACT OF CEFTRIAXONE DE-RESTRICTION ON THE COST OF ANTIBIOTIC TREATMENT<br />
Srecko Marusic, Vesna Bacic-Vrca, Jasenka Skrlin, Lado Uglesic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28<br />
IMPACT OF THE PHARMA ECONOMIC ACT ON DIFFUSION OF INNOVATION,<br />
REDUCTION OF COSTS AND PATIENTS’ EQUITY IN THE HUNGARIAN PRESCRIPTION<br />
DRUG MARKET<br />
Rok Hren . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29<br />
ETHICS AS A RISING ISSUE FOR TARGETED THERAPIES: THE METASTATIC<br />
COLORECTAL EXAMPLE<br />
Livio Garattini, Katelijne van de Vooren . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30<br />
IMPLEMENTATION OF BIOLOGICAL THERAPY AND SURGERY IN THE TREATMENT<br />
OF METASTATIC COLORECTAL CANCER: ARE THE COSTS JUSTIFIED?<br />
Renata Dobrila-Dintinjana, Dinko Vitezić . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 31<br />
THE ROLE OF CYTOLOGY IN DETECTION OF SMALL BREAST CANCER – EXPERIENCE<br />
OF UNIVERSITY HOSPITAL FOR TUMOURS, ZAGREB (COST BENEFIT?)<br />
Vesna Ramljak, Iva Bobuš-Kelčec, Merdita Agai, Ljiljana Mayer . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32<br />
COMPARATIVE ANALYSIS OF PATIENT ACCESS TO TARGETED THERAPIES FOR<br />
METASTATIC RENAL CELL CARCINOMA (MRCC) IN SELECTED CEE COUNTRIES<br />
Jasmina Krehić, Novka Agić, Vedrana Raguž . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33<br />
PHARMACOECONOMICS IN PREDICTIVE MEDICINE<br />
Josip Čulig, Marcel Leppee, Nikolina Skaron-Jakobović . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34<br />
THE ECONOMIC COST ANALYSIS OF THE IMPLEMENTATION OF CENTRALIZED<br />
PHARMACY UNIT FOR ANTINEOPLASTIC DRUGS WITH RESPECT TO THE PREMISES,<br />
EQUIPMENT AND TECHNICAL STAFF UNDER THE SUPERVISION OF ONCOLOGY<br />
PHARMACIST<br />
Vesna Pavlica, Damir Vrbanec, Velemir Danko Vrdoljak . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 35<br />
MUSCULOSKELETAL DISORDER - THEIR IMPACT ON WORK ABILITY AND SOCIETAL<br />
COSTS IN POLAND<br />
Magdalena Wladysiuk, Ksenia Zhelthoukhova, Stephen Bevan, Mateusz Haldas . . . . . . . . . . . . . . . . . 36
CASE STUDY IN TRANSPLANTATION AND IMMUNOSUPPRESSANT THERAPY<br />
IN MACEDONIA, THREE YEAR FOLLOW UP<br />
Stevce Acevski, Zoran Sterjev, Vladimir Indov . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37<br />
RARE DISEASES OR DISORDERS, ORPHAN DRUGS AND PATIENTS EQUITY RIGHTS<br />
Jasmina Krehić, Senka Mesihović Dinarević . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38<br />
STEREOLOGICAL ANALYSIS OF TERMINAL VILLI OF HUMAN PLACENTAS<br />
ASSOCIATED WITH EPH GESTOSIS<br />
Dinko Vitezić . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39<br />
TRENDS IN THE UTILIZATION OF CARDIOVASCULAR DRUGS IN CROATIA DURING<br />
THE PERIOD 2007-2010<br />
Viola Macolić-Šarinić, Pero Draganić, Josip Čulig, Marcel Leppée, Marinko Bilušić, Saša Žeželić . . . 40<br />
COMPARATIVE ANALYSIS OF CARDIOVASCULAR DRUGS UTILISATION IN GENERAL<br />
HOSPITAL AND CLINICAL CENTER IN CROATIA AND BOSNIA AND HERZEGOVINA<br />
Mirza Dilić, Aleksandar Knežević, Sanja Sarić-Kužina, Anesa Eminović . . . . . . . . . . . . . . . . . . . . . . . . . . . 41<br />
DIFFERENTIAL DIAGNOSIS OF CLEAR CELL TUMORS<br />
Nenad Vanis, Rusmir Mesihović, Aida Saray . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42<br />
MODELLING THE EUROPEAN BURDEN OF DISEASE ASSOCIATED MALNUTRITION<br />
András Inotai, Mark Nuijten, Eric Roth, Refaat Hegazi, Zoltán Kaló . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43<br />
FROM MORISKY TO HILL-BONE: MEASUREMENT OF ADHERENCE TO MEDICATION<br />
Josip Čulig, Marcel Leppee . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 44<br />
THE COST OF DIABETES MELLITUS IN MACEDONIA<br />
Donka Pankov, Zoran Sterjev, Ljubica Suturkova . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45<br />
COST-EFFECTIVENESS OF INTERVENTIONS TO CONTROL DIABETES MELLITUS<br />
AND PREVENT COMPLICATIONS<br />
Terezija Šarić, Tamara Poljičanin, Željko Metelko . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 46<br />
SYMPTOMATIC THERAPY FOR COLD AND FLU – MACEDONIAN CASE 2011<br />
Stevce Acevski, Vladimir Indov, Zoran Sterjev, Rubin Zareski . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 47<br />
ECONOMIC EVALUATION OF DECREASING PERSISTANT HYPERTENSION WITH RENAL<br />
DENERVATION DEVICE CUTTING COSTS OF HYPERTENSION COMMORBIDITIES IN<br />
UPCOMING CROATIAN PRACTICE<br />
Vanesa Benković, Ranko Stevanović, Ana Ivičević, Marko Matulović, Bojan Jelaković . . . . . . . . . . . . . 48<br />
CODIFFICATION AS A METHOD IN RESEARCH ON ANIMAL MODELS<br />
IN PHARMACOECONOMICAL EFFICIENCY<br />
Iris Broman . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 49<br />
THE ROLE OF PHARMACOECONOMICS IN MEDICINES REIMBURSEMENT<br />
DECISION-MAKING IN BOSNIA AND HERZEGOVINA<br />
Tarik Čatić, Igor Martinović, Begler Begović . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50<br />
EVALUATION OF UTILIZATION OF OLD VERSUS NEWER ANTIEPILEPTIC DRUGS<br />
IN REPUBLIC OF MACEDONIA<br />
Bojana Danilovska, Zoran Sterjev, Ljubica Suturkova . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 51<br />
3
4<br />
DEMENTIA- CAN FORGETFULNESS BE SIGNIFICANT SOCIAL ISSUE?<br />
Vedran Đukić, Nenad Bogdanović . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52<br />
COMPARISON OF COST EFFECTIVENES OF TOTAL HIP AND KNEE ENDOPROTESIS<br />
WITH AND WITHOUT PROLONGED THROMBOEMBOLIC PROPHYLAXIS<br />
Ismet Gavrankapetanović, Faris Gavrankapetanović, Mehmed Jamakosmanović,<br />
Slobodanka Bolanča . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 53<br />
HUMAN PAPILLOMAVIRUS VACCINATION OF BOYS: COST-EFFECTIVENESS ANALYSIS<br />
Rok Hren . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 54<br />
COST-EFFECTIVENESS OF COMBINED TREATMENT OF METFORMIN<br />
AND FENOFIBRATE ON RETINOPATHY PROGRESSION<br />
Rok Hren, Radomir Cerovic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55<br />
EVALUATION OF COST-SAVING OF CLOPIDOGREL PHARMACOGENETIC TESTING<br />
IN PATIENT WITH ATHEROTROMBOTIC DISORDERS FROM R. MACEDONIA<br />
Aleksandra Kapedanovska Nestorovska, Zorica Naumovska, Zoran Sterjev,<br />
Aleksandar Dimovski, Ljubica Suturkova . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56<br />
INFLUENCE OF INCREASED LINEZOLID UTILISATION ON DEVELOPMENT<br />
OF ANTIMICROBIAL RESISTANCE TO LINEZOLID<br />
Aleksandar Knežević, Sanja Sarić-Kužina, Ivanka Matas . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 57<br />
INSTITUTIONAL AND NORMATIVE FRAMEWORK OF DRUG CONTROL COSTS<br />
IN THE REPUBLIC OF MACEDONIA<br />
Kostadinka Kozareva, Ana Petrovska Angelovska . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 58<br />
ANTIDIABETIC DRUG EXPENDITURE IN BOSNIA AND HERZEGOVINA - 2009/2010<br />
Jasmina Krehic, Zelija Velija Asimi . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 59<br />
COST EFFECTIVENESS OF RENAL SYMPATHETIC DENERVATION IN PATIENTS WITH<br />
REFRACTORY HYPERTENSION: DECISION MODELLING OF APPLICABILITY FOR<br />
CROATIAN HEALTH CARE<br />
Robert Likić, Ksenija Makar Aušperger, Viktorija Erdeljić, Matea Radačić Aumiler,<br />
Igor Francetić, Bojan Jelaković . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 60<br />
THE FREQUENCY OF ADMINISTRATION OF ANTIPSYCHOTICS, ANXIOLYTICS<br />
AND ANTIDEPRESSANTS: DESCRIPTION STUDY<br />
Svjetlana Loga-Zec, Damir Celik, Faris Gavrankapetanović, Jasmina Krehić,<br />
Mensura Aščerić, Nedžad Mulabegović . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 61<br />
FINANCIAL IMPACT OF IMPORTED UNAPPROVED DRUGS ON THE HOSPITAL<br />
BUDGET: EXAMPLE OF THE CHILDREN’S HOSPITAL OF THE UNIVERSITY<br />
HOSPITAL CENTRE RIJEKA, CROATIA<br />
Vesna Rosović-Bazijanac, Jasenka Mršić-Pelčić, Dinko Vitezić . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 62<br />
MALNUTRITION IN CROATIA – WHERE ARE WE TODAY AND WHY SHOULD<br />
WE INCLUDE SOCIETAL PERSPECTIVE IN MEASURING “BURDEN OF ILLNESS“?<br />
Ranko Stevanović, Vanesa Benković, Ana Ivičević, Ivana Kolčić, Irena Rojnić Palavra . . . . . . . . . . . . . . 63
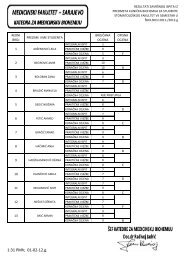
PRVI BOSANSKO-HERCEGOVAČKI I DRUGI<br />
JADRANSKI KONGRES FARMAKOEKONOMIKE<br />
I ISTRAŽIVANJA ISHODA LIJEČENJA<br />
ORGANIZATORI KONGRESA<br />
Udruženje za zdravstvenu ekonomiku i<br />
farmakoekonomska istraživanja u Bosni<br />
i Hercegovini u saradnji sa Sekcijom za<br />
farmakoekonomiku i istraživanje ishoda<br />
liječenja Hrvatskog društva za kliničku<br />
farmakologiju, terapiju i Udruženjem za<br />
farmakoekonomiku i istraživanje ishoda u BIH i<br />
ISPOR Macedonia chapter.<br />
PREDSJEDNICI KONGRESA<br />
Faris Gavrankapetanović<br />
Dinko Vitezić<br />
SEKRETARI KONGRESA<br />
Slobodanka Bolanča<br />
Tarik Ćatić<br />
RIZNIČAR<br />
Sakib Katana<br />
Sanja Sarić-Kužina<br />
ORGANIZACIJSKI ODBOR (predsjedavajući)<br />
Novka Agić (predsjedavajuća)<br />
Mahmut Đapo (predsjedavajući)<br />
Nataša Grubiša (predsjedavajuća)<br />
ORGANIZACIJSKI ODBOR (članovi)<br />
Aldina Ahmetagić (Bosna i Hercegovina)<br />
Tonći Buble (Hrvatska)<br />
Viktorija Erdeljić (Hrvatska)<br />
Jurij Fürst (Slovenija)<br />
Svjetlana Loga Zec (Bosna i Hercegovina)<br />
Zoltan Kalo (Mađarska)<br />
Jasmina Krehić (Bosna i Hercegovina)<br />
Viola Macolić-Šarinić (Hrvatska)<br />
Filipa Markotić (Bosna i Hercegovina)<br />
Lilijana Oruč (Bosna i Hercegovina)<br />
Zoran Sterjev (Makedonija)<br />
Svjetlana Stoisavljević Šatara<br />
(Bosna i Hercegovina)<br />
Nedim Tvrtković (Bosna i Hercegovina)<br />
NAUČNI ODBOR (predsjedavajući)<br />
Igor Francetić<br />
Rusmir Mesihović<br />
Nedžad Mulabegović<br />
Ranko Škrbić<br />
NAUČNI ODBOR (članovi)<br />
Jugoslav Bagatin (Hrvatska)<br />
Elmir Čičkušić (Bosna i Hercegovina)<br />
Livio Garattini (Italija)<br />
Mirjana Huić (Hrvatska)<br />
Aleksandar Knežević (Hrvatska)<br />
Ante Kvesić (Bosna i Hercegovina)<br />
Bakir Mehić (Bosna i Hercegovina)<br />
Ljerka Ostojić (Bosna i Hercegovina)<br />
Zoran Riđanović (Bosna i Hercegovina)<br />
Ljubica Suturkova (Makedonija)<br />
Aziz Šunje (Bosna i Hercegovina)<br />
Veljko Trivun (Bosna i Hercegovina)<br />
Vlad Zah (Srbija)<br />
5
6<br />
FOLIA MEDICA FACULTATIS MEDICINAE UNIVERSITATIS SARAEVIENSIS<br />
Journal of Medical Faculty University of Sarajevo, Bosnia&Herzegovina<br />
Editor-in-Chief<br />
Nedžad Mulabegović<br />
Execute Editor<br />
Maida Rakanović Todić<br />
Editorial Board<br />
Jasminko Huskić<br />
Damir Aganović<br />
Amela Begić<br />
Slavica Ibrulj<br />
Semra Čavaljuga<br />
Nermin Sarajlić<br />
Almira Hadžović Džuvo<br />
Lejla Burnazović Ristić<br />
Radivoj Jadrić<br />
Lectorised by<br />
Dubravko Vaniček<br />
Technical Editor and Print<br />
SaVart Sarajevo<br />
DTP<br />
Narcis Pozderac<br />
Adress of the Editorial board:<br />
71000 Sarajevo, Čekaluša 90<br />
Bosnia & Herzegovina<br />
Phone: 00387 33 226 472<br />
Fax: 00387 33 203 670<br />
Published by<br />
Faculty of Medicine,<br />
University of Sarajevo<br />
www.mf.unsa.ba/folia<br />
ISSN 0352-9630<br />
EBSCO Publishing (EP) USA<br />
http://www.epnet.com<br />
Printed on acid-free paper
Dear Colleagues and friends<br />
On behaf of Scientific Committee of the Association of Health Economics and Pharmacoeconomic<br />
Research in Bosnia and Herzegovina in cooperation with the Section for<br />
Pharmacoeconomi¬cs and Outcomes Research of the Croatian Society for Clinical Pharmacology<br />
and Therapeutics and the Association for Pharmacoeconomics and Outcomes Research<br />
inBIH,<br />
it gives me a great pleasure to welcome you to the First Bosnian-Herzegovinian and Second<br />
Adriatic Congress of the Pharmacoeconomics and Outcomes Research.<br />
We are sure that the plenary lectures, poster presentations and panel discussions will enrich<br />
the scientific atmospfere in the Farmacoeconomic and Health Economic field.<br />
It is our pleasure to list all scientific abstracts in the supllement of<br />
“FOLIA MEDICA FACULTATIS MEDICINAE UNIVERSITATIS SARAEVIENSIS”, indexed<br />
Journal of Medical Faculty University of Sarajevo, Bosnia&Herzegovina.<br />
Warm regards,<br />
Professor Nedžad Mulabegović<br />
Editor in Chief<br />
7
8<br />
Poštovane kolegice i kolege, dragi prijatelji,<br />
Srdačno Vas pozdravljamo i želimo Vam dobrodošlicu u ime organizatora Prvog <strong>bosansko</strong>hercegovačkog<br />
i drugog jadranskog <strong>kongres</strong>a farmakoekonomike i istraživanja ishoda liječenja<br />
koji se održava u Sarajevu od 24. do 26. aprila 2012. godine.<br />
Organizatori Kongresa, Udruženje za zdravstvenu ekonomiku i farmakoekonomska<br />
istraživanja u Bosni i Hercegovini u suradnji sa Sekcijom za farmakoekonomiku i istraživanje<br />
ishoda liječenja Hrvatskog društva za kliničku farmakologiju i terapiju i Udruženjem za farmakoekonomiku<br />
i ispitivanje ishoda u BiH, ove su se godine odlučili za vodilju skupa postaviti<br />
ulogu farmakoekonomike u osiguranju prava jednakosti bolesnika na liječenje.<br />
Nadamo se da će ovaj Kongres nastaviti tradiciju unapređenja rada na regionalnom nivou,<br />
što se već i potvrdilo na osnovu velikog interesovanja sudionika iz zemalja regije, te da će biti<br />
još uspješniji od prethodnog koji je održan u Rovinju, aprila mjeseca 2011. godine. Kongres<br />
će obuhvatiti kroz predavanja, poster prezentacije i organizaciju radionice raznovrsne teme iz<br />
područja razvoja politike zdravstvene zaštite, politike formiranja cijena i uvrštavanja lijekova<br />
na pozitivnu listu, ispitivanja komparativne učinkovitosti i kliničkih ishoda, kontrole potrošnje<br />
lijekova i istraživanja ekonomskih ishoda, procjene zdravstvenih tehnologija te mnoge druge,<br />
sa posebnim osvrtom na krajnje korisnike, odnosno naše pacijente. Vjerujemo da će dodatnu<br />
korist u okviru Kongresa predstavljati i organizirana radionica pod naslovom Primijenjena farmakoekonomika<br />
u kojoj će biti prikazani principi na osnovu kojih farmakoekonomika postaje<br />
neizostavan alat i pomoć pri donošenju odluka na različitim nivoima u području zdravstvene<br />
zaštite.<br />
Kao predavači i voditelji radionica, uz domaće, sudjelovaće i priznati međunarodni stručnjaci.<br />
Raduje nas i činjenica da će Kongres okupiti stručnjake i sve zainteresirane koji se u regiji<br />
i šire bave farmakoekonomikom, od akademske zajednice, kroz udruženja pa sve do regulatornih<br />
tijela i industrije, uz dodatno nastojanje promoviranja principa integrativnog pristupa<br />
farmakoekonomici, njihovog implementiranja i informiranja šire javnosti.<br />
Zahvaljujemo se Vama kao sudionicima i svima koji su pomogli u realizaciji ovog Kongresa<br />
i želimo Vam ugodan boravak u Sarajevu!<br />
Uz najbolje želje,<br />
Prof. dr. sc. Faris Gavrankapetanović Prof. dr. sc. Dinko Vitezić<br />
Predsjednik Udruženja za zdravstvenu Predsjednik Sekcije za farmakoekonomiku i<br />
ekonomiku i farmakoekonomska istraživanje ishoda liječenja Hrvatskog<br />
istraživanja u BIH društva za kliničku farmakologiju i terapiju
Dear colleagues, dear friends,<br />
We cordially welcome you on behalf of the Organizers of the First Bosnian-Herzegovinian<br />
and Second Adriatic Congress of the Pharmacoeconomics and Outcomes Research to be held<br />
in Sarajevo on 24 to 26 April 2012.<br />
Organizers of the Congress, Association of Health Economics and Pharmacoeconomic<br />
Research in Bosnia and Herzegovina in cooperation with the Section for Pharmacoeconomics<br />
and Outcomes Research of the Croatian Society for Clinical Pharmacology and Therapeutics<br />
and the Association for Pharmacoeconomics and Outcomes Research inBIH, this year, decided<br />
to set up The role of farmacoconomics in ensuring patients’ equity rights as a topic guide.<br />
We hope that this Congress will continue the tradition of advancing this work at regional<br />
level, which is already confirmed on the basis of the great interest of participants from countries<br />
of the region, and that this Congress will be even more successful than the previous one held in<br />
Rovinj, April, 2011. The Congress will cover the lectures, poster presentations and workshops<br />
on various topics in health policy development, pricing policies and the inclusion of drugs on<br />
the positive drug lists, a comparative study of efficiency and clinical outcomes, control of drug<br />
consumption and economic outcomes research, health technology assessment, and many others,<br />
with special reference to end-users - our patients. We believe that the added benefit of this<br />
Congress will be a workshop titled Applied pharmacoeconomics which will show the principles<br />
on which pharmacoeconomics is becoming an indispensable tool and aid in decision making<br />
at various levels in the field of healthcare.<br />
Distinguished international experts will, together with our experts, participate as speakers<br />
and workshop leaders. We are delighted by the fact that the Congress will bring together<br />
experts and all interested professionals dealing with pharmacoeconomics in the region and<br />
beyond, from the academic community, the associations up to the regulatory authorities and<br />
industry, with further efforts to promote the principles of integrative approach to pharmacoeconomics,<br />
implementation of these principles and informing the general public.<br />
We do thank you as participants as well as everyone who helped in realization of this Congress.<br />
Wish you a pleasant stay in Sarajevo!<br />
With best wishes,<br />
Prof. Faris Gavrankapetanović, MD, PhD Prof. Dinko Vitezić, MD, PhD<br />
President, Association for Health Economics and President, Section for Pharmacoeconomics<br />
Pharmacoeconomic Research in Bosnia and and Outcomes Research,Croatian Society for<br />
Herzegovina Clinical Pharmacology and Therapeutics<br />
9
PRE-CONGRESS TRAINING COURSE<br />
Applied pharmacoeconomics: How pharmacoeconomics can be applied to<br />
support decisions by different stakeholders in health care?<br />
Zoltán Kaló 1 , Dinko Vitezić 2<br />
1 Eötvös Loránd University; Syreon Research<br />
Institute, Budapest, Hungary<br />
2 University of Rijeka, School of Medicine and Rijeka<br />
University Hospital Center, Rijeka, Croatia<br />
There is increasing need for improved evidence<br />
base of decisions in all different areas of decisionmaking<br />
in health care. A high-quality economic<br />
evaluation should provide decision-makers with<br />
useful, relevant, and timely information. Stakeholders<br />
both in public and private sectors apply<br />
pharmacoeconomic methods to make better<br />
decisions. Economic evaluations can quantify<br />
costs and consequences of different scenarios<br />
based on the best available scientific evidence,<br />
and can even take into account the uncertainty<br />
related to key assumptions.<br />
In the public sector economic evaluations are<br />
used to justify the basic drug benefit package.<br />
In more and more countries analysis of costeffectiveness<br />
and budget impact is mandated<br />
prior to pricing and reimbursement decisions<br />
of new pharmaceuticals. For reimbursement<br />
and formulary listing purposes, manufacturers<br />
need to convince payers that the drug results in<br />
considerable health benefit in real world; its costeffectiveness<br />
ratio does not exceed the threshold<br />
accepted by the society, and its financing is affordable,<br />
fits into the budget.<br />
Risk sharing agreements are based on health<br />
economic principles. Confidential pricing agreements<br />
in lower income countries can be applied<br />
to adjust the price of medicines to local purchasing<br />
power without influencing the published exfactory<br />
price and so the accessibility of patients<br />
to these drugs in other countries. Introduction<br />
of outcome based risk-sharing schemes can be a<br />
major advancement in the drug reimbursement<br />
strategy of payers. These schemes can help to<br />
reduce the medical uncertainty in coverage decisions<br />
for valuable innovative healthcare tech-<br />
10 Proofreading and translations are in the explicit responsibility of the authors.<br />
nologies. Coverage with evidence development<br />
can fill in the evidence gap especially for orphan<br />
drugs.<br />
Economic evaluation, as part of health technology<br />
assessment is applicable to review full<br />
therapeutic areas with significant budget impact<br />
(e.g. diabetes, oncology, autoimmune diseases),<br />
including the revision of therapeutic guidelines<br />
and financing protocols and delisting of previously<br />
reimbursed pharmaceuticals.<br />
In the private sector pharmacoeconomic evaluations<br />
are applied in pharmaceutical R&D and<br />
marketing decisions. Economically justifiable<br />
price based the target product profile is essential<br />
input variable in the net present value calculation<br />
for go-no go, business development and<br />
licensing decisions. The need for cost-effectiveness<br />
evidence is taken into account in defining<br />
the optimal ex-factory price of new medicines.<br />
Pharmaceutical R&D faces the need for a new<br />
type of strategy: evidence base for registration<br />
and reimbursement has to be created at high scientific<br />
standards. This is a difficult task, as compliance<br />
with the different requirements needs<br />
different approaches. Evidences for registration<br />
have to be achieved with cheap, quick and lowrisk<br />
clinical programme, because R&D resources<br />
are limited, and due to the capped patent protection<br />
period, a shorter clinical development phase<br />
results in a longer return phase. Simple clinical<br />
trials with suboptimal comparators support<br />
these objectives. Evidences for reimbursement<br />
and formulary listing require another approach;<br />
innovators should prove in real-world situation<br />
that their new product is worth public financing<br />
against the best and most widely used alternative
procedures. These clinical trials are longer and<br />
more expensive, as sample size has to be greater<br />
to power these studies adequately. In addition to<br />
efficacy and safety end points, a new type of data<br />
must be collected alongside clinical trials, which<br />
increases the risks and the expected budget of<br />
the R&D programme.<br />
Before the launch of new medicines, a global<br />
health economic dossier is prepared in parallel<br />
with the adaptation of results to most important<br />
countries or markets. Local health economists<br />
prepare country-specific health economic<br />
dossiers in order to obtain reimbursement and<br />
formulary listing in all countries. Health economists<br />
are also involved into the planning and<br />
pharmacoeconomic assessment of major phase<br />
IV and observational studies to extend the economic<br />
evidence base in a constantly changing<br />
clinical and economic environment.<br />
As a consequence of increased utilization of<br />
pharmacoeconomic evaluations in health care<br />
decisions, there is growing demand for trained<br />
health economists. Short courses and post-graduate<br />
university training can fulfill this demand in<br />
Central- Eastern European countries.<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
11
PL 1.1.<br />
The role of pharmacoeconomics and health technology assessment in<br />
ensuring patietns’ equity rights<br />
Faris Gavrankapetanović<br />
Clinical Center University of Sarajevo, Bosnia and<br />
HerzegovinaE-mail: bakic@medfak.ni.ac.rs<br />
Life expectancy and mortality rates in Bosnia<br />
and Herzegovina are comparable to countries<br />
in region, but still lower than EU average and<br />
far away from benchmark EU countries known<br />
to have the best healthcare outcomes (France,<br />
Spain and Italy). Available healthcare resources<br />
are insufficient to meet national healthcare<br />
needs thus different health economic tools for<br />
the rational use of available resources based on<br />
efficiency and patient equity, in the first place<br />
pharmacoeconomics and health technology assessment,<br />
are of highest importance and priority,.<br />
There is also a wide variability in the speed<br />
and magnitude with which valuable innovative<br />
medicines and other new technologies become<br />
available to patients; and then further variability<br />
in uptake of medicines and between disease areas.<br />
Cantonal and Entity Governments are facing<br />
additional difficulties and challenges during the<br />
current financial situation. For that reason, now<br />
more than ever policymakers across the country<br />
need to work together so that all patients are able<br />
to receive the appropriate medical care. We must<br />
create the right regulatory and legal framework<br />
12 Proofreading and translations are in the explicit responsibility of the authors.<br />
in B&H and shift public mindset from healthcare<br />
cost to healthcare value as well as set appropriate<br />
strategies with clear disease priorities in line with<br />
local epidemiology and mortality data. A formal<br />
process of using evidence to evaluate the clinical<br />
efficacy/effectiveness, the cost-effectiveness, and<br />
the broader impact of health technologies on<br />
patients and the health care system is needed to<br />
enhance the functioning of the health care system<br />
as a whole and to incorporate the interests<br />
of patients, health care professionals, payers and<br />
policy makers and manufacturers in such process.<br />
Because good health is basic human aspiration,<br />
patients should be empowered to make informed<br />
choices about access, allocation of funding<br />
and assessments of healthcare value.<br />
In conclusion, decision making in healthcare<br />
is a very complex process requiring simultaneous<br />
consideration of number of factors, among<br />
which pharmacoeconomics and health technology<br />
assessment are the most important for ensuring<br />
patient equity rights in healthcare systems<br />
with limited funding.
Ensuring equity and availability of healthcare regarding patients’ right on<br />
effective, safe, quality and available essential drugs in Federation of Bosnia<br />
and Herzegovina<br />
Rusmir Mesihović, Sanja Ćustović<br />
Ministry of Health of Federation Bosnia and<br />
Herzegovina, Sarajevo, Bosnia and Herzegovina<br />
Endeavoring to find mechanisms of ensuring the<br />
basic package of health insurance for all the citizens<br />
in Federation of Bosnia and Herzegovina<br />
as a part of socially sensitive government plan,<br />
Federal minister of health brings the Decision of<br />
the essential drug list, meaning drugs which are<br />
necessary for providing health insurance in accordance<br />
with the standards of obligatory health<br />
insurance in Federation of Bosnia and Herzegovina<br />
(Official Gazette of the Federation BiH<br />
no. 75/11) with revised prices. The new essential<br />
drug list consists of list A (100% reimbursement)<br />
with 140 different generic drug names, and list<br />
B (different reimbursement) which consists of<br />
85 generic drug names. The decision became effective<br />
on 10 November 2011, and cantons were<br />
obliged to adjust the positive cantonal drug lists<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 2.1.<br />
with the Federal essential drug list within 60<br />
days of the day when the Decision became effective,<br />
but in accordance with the Article 9 of the<br />
Federal Decision, that date has been prolonged,<br />
so the full implementation is expected by the end<br />
of August, 2012. In order to ensure cost-effective<br />
drugs, according to the Decision the prices of<br />
drugs from the positive lists which are higher of<br />
those determined by the Federal Decision will<br />
go down to the level of prices determined by the<br />
Decision, while the prices which are the same or<br />
lower remain the same provided that those drugs<br />
fulfill the general and specific criteria of the item<br />
VII of the Federal Decision. Further efforts will<br />
be made on implementation of pharmacoeconomic<br />
techniques as well as health technology<br />
assessment.<br />
13
PL 2.2.<br />
Medicines Policy in the Republic of Srpska – availability and equality<br />
Vanda Marković Peković<br />
Ministry of Health and Social Welfare<br />
Goal: To present Medicines Policy in the Republic<br />
of Srpska<br />
Materials and Methods: The legislation and<br />
available documents concerning health care system<br />
were used to evaluate the activities regarding<br />
availability of the medicines.<br />
Result. Prime objectives in the area of public<br />
healthcare in the Republic of Srpska are defined<br />
as preservation and improvement of public<br />
health, prolonged life expectancy and improvement<br />
of health related quality of life, amelioration<br />
of differences in health care availability and<br />
utilization, constant upgrade of quality and economic<br />
viability of health services and insurance<br />
against health related financial risks.<br />
Medicines are only one component in the maintenance<br />
and restoration of the health of communities<br />
and individuals, and are segment in the<br />
prevention, diagnosis and treatment of diseases.<br />
If used appropriately, medicines have the potential<br />
to relieve suffering and restore health, which<br />
is why they are placed amongst top priorities in<br />
every health system; otherwise, they waste resources,<br />
fail to achieve the purpose of their use<br />
14 Proofreading and translations are in the explicit responsibility of the authors.<br />
and lead to financial consequences for the society<br />
as a whole. National Medicines Policy (NMP)<br />
as a political and professional document was<br />
adopted in 2006 by the Government. NMP is<br />
harmonized with the WHO policy and provides<br />
for a framework for the coordination of activities<br />
of all stakeholders in the area of medicines.<br />
The overall objective of NMP is to ensure that<br />
the whole population has access to effective, safe<br />
and quality medicines and that these are used in<br />
a rational and cost-effective manner. The overall<br />
objective shall be fulfilled through legislation<br />
and organization, quality, safety and efficacy of<br />
medicines, availability and rational use of medicines.<br />
The NMP is implemented through the<br />
document Medicines Strategy by 2012.<br />
Conclusion: Through the reform of the health<br />
system in general, much effort has been done in<br />
recent years to improve the pharmaceutical sector.<br />
Continuous, efficient and timely provision<br />
of quality, safe and efficient medicines to patient<br />
and health institutions in the Republic of Srpska<br />
ought to be guaranteed both now and in the future.
Reimbursement of expensive hospital drugs in Slovenia<br />
Jurij Fürst, Rozeta Hafner<br />
Health Insurance Institute of Slovenia, Slovenia<br />
Facing economic recession in 2010, Ministry of<br />
Health and Health Insurance Institute of Slovenia<br />
(ZZZS) have amended regulations on pricing<br />
and reimbursement of drugs. In the pricing<br />
regulation, more rigorous measures have been<br />
adopted. In the reimbursement regulation, pharmacoeconomic<br />
part has been renewed and a new<br />
reimbursement and financing model for hospital<br />
drugs has been enacted. A new drug list, called<br />
“hospital list” or “B-list”, was defined.<br />
The new B-list is reserved only for so-called expensive<br />
hospital drugs, defined by a price of 5<br />
000 EUR or more per patient per year. ZZZS follows<br />
the same procedure for both hospital and<br />
prescription drugs. Every drug is evaluated by<br />
both clinical criteria (these include therapeutic<br />
value and relative efficacy) and economic criteria<br />
(these include pharmacoeconomic and budget<br />
impact analysis). To reach an agreement between<br />
ZZZS and marketing authorisation holder about<br />
price is an important part of the procedure.<br />
There are no restrictions; ZZZS is allowed to<br />
sign any type of agreements. For the most expensive<br />
drugs, such as orphan enzyme replacement<br />
therapy, a triple agreement is prepared: the competent<br />
clinic defines clinical criteria for the inclusion<br />
of patients into the treatment, ZZZS and<br />
the pharmaceutical company agree on the way of<br />
financing. In some cases, the clinic has to obtain<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 2.3.<br />
a ZZZS’s consent for every patient. After that,<br />
ZZZS communicates with the pharmaceutical<br />
company to agree upon an additional discount.<br />
For most drugs, a mixed approach with a price<br />
discount and a material rebate or a financial cap<br />
is settled upon. Finally, ZZZS defines a list of<br />
hospitals/clinics to be included in the reimbursement<br />
scheme and a list of therapeutic indications<br />
to be covered.<br />
In order to enable ZZZS to control the use of<br />
B-list drugs, hospitals are required to prepare<br />
monthly reports providing data about all treated<br />
patients. These data should include age, sex, body<br />
surface area, doses, prices, etc. ZZZS reimburses<br />
hospitals for all B-list drugs on a monthly basis.<br />
The new B-list and a broad set of reimbursed<br />
prescription drugs (including low-molecular<br />
weight heparins, intravenous bisphosphonates,<br />
epoetins, drugs for multiple sclerosis, the whole<br />
spectrum of biological drugs for the treatment of<br />
rheumatic and other autoimmune diseases, and<br />
other high-priced drugs) enable high quality and<br />
effective hospital or ambulatory treatment for all<br />
patients without jeopardizing hospital budgets.<br />
A possible “side-effect” of such a “generous” approach<br />
is overuse of expensive drugs. Intensive<br />
cooperation with clinics/hospitals, as well as<br />
education and audits, may ensure a rational use<br />
of drugs.<br />
15
PL 2.4.<br />
Value Based Pricing – ongoing HTA reform in the UK<br />
Petr Hajek<br />
Pfizer Ltd., United Kingdom<br />
UK Government recognizes that there are significant<br />
failings within the system for drug pricing<br />
and access and is proposing reforms which<br />
it says will “provide NHS patients with better<br />
access to effective and innovative treatments at<br />
a price that secures value for the NHS”. These<br />
reforms are encompassed by three key new policies:<br />
1. Cancer Drugs Fund, an interim measure<br />
2011-2013 2. Value-Based Pricing (VBP) from<br />
2014 3. Transform the duties and responsibilities<br />
of NICE (National Institute for Health and Clinical<br />
Excellence), with the body taking on a more<br />
advisory role rather than as ‘gatekeeper’ to medicines.<br />
New structure of NICE will include Cost<br />
Effectiveness Analysis (as in current system) plus<br />
two Expert Panels: Burden of Illness Assessment<br />
and Innovation Assessment. New NICE structure<br />
is mentioned bellow:<br />
16 Proofreading and translations are in the explicit responsibility of the authors.<br />
Basic price Willingness To Pay threshold reflecting<br />
benefits displaced elsewhere in NHS will be<br />
set. New thresholds will be introduced for 1.<br />
Higher price thresholds for medicines that tackle<br />
diseases where there is greater burden of illness,<br />
defined in terms of severity and unmet need. 2.<br />
Higher price threshold for therapeutic innovation<br />
3. Higher price threshold for medicines that<br />
demonstrate wider societal benefits. Under VBP,<br />
new medicines that offer significant health gain,<br />
address unmet need and offer therapeutic innovation<br />
will be advantaged…in the context of limited<br />
resources overall, those that do not, will do<br />
less well than under the current arrangements.
Transferability of NICE recommendations to lower income countries: the<br />
case of oncology drugs<br />
Zoltán Kaló<br />
Health Economics Research Centre, Eötvös Loránd<br />
University Syreon Research Insititute, Budapest,<br />
Hungary<br />
The health burden of malignancies is greater in<br />
Central-Eastern Europe than in Western Europe.<br />
Furthermore, these countries have more limited<br />
health care resources, and therefore transparent<br />
decision criteria for innovative cancer therapies,<br />
including the assessment of cost-effectiveness,<br />
are an absolute necessity. Transferability of good<br />
quality technology assessment reports, especially<br />
those prepared by NICE in the United Kingdom,<br />
could be highly beneficial to prevent duplication<br />
of efforts and save resources for local technology<br />
assessment.<br />
The presentation summarizes key factors influencing<br />
the transferability of NICE recommendations<br />
in oncology for policymakers and<br />
oncologists in Central-Eastern Europe without<br />
personal experience in health technology assessment.<br />
These factors include the incidence and<br />
prevalence of disease, disease progression, unit<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 3.1.<br />
costs, resource utilisation, unmet medical need,<br />
and consistency of NICE recommendations over<br />
time.<br />
In general, NICE recommendations are not<br />
transferable without adjustment of the analyses<br />
to local data. Even if the recommendation is positive,<br />
the conclusion can be still negative in lower<br />
income countries, mainly due to relative price<br />
differences and the significance of the local budget<br />
impact. Technologies with negative NICE<br />
recommendations can be still cost-effective in<br />
Central-Eastern Europe due to the worse health<br />
status and therefore the greater potential health<br />
gain of the targeted population.<br />
The appropriateness of reimbursement decisions<br />
must be improved in Central-Eastern Europe,<br />
but copying NICE recommendations without<br />
local adjustment may do more harm than good.<br />
17
PL 3.2.<br />
Adjustment and Implementation of Croatian P&R Model<br />
Bruna Buble 1 , Tonči Buble 2 , Vesna Bačić Vrca 1 , Dinko Vitezić 3<br />
1Faculty of Pharmacy and Biochemistry, Croatia<br />
2Belupo, Croatia<br />
3University Hospital Centre Rijeka and University of<br />
Rijeka Medical School, Croatia<br />
Actual Croatian “Pricing and Reimbursement”<br />
(P&R) model, introduced in 2001, has been<br />
changed several times until now. It provides an<br />
unique approach to the pricing of drugs from the<br />
basic drug list, financially covered by the Croatian<br />
Institute for Health Insurance - HZZO.<br />
In 2002 the administrative measure of exemption<br />
from co-payments, relating to over 50% of<br />
the insured persons, had the biggest impact on<br />
drug cost augmentation resulting in the annual<br />
growth rate of 25%. In 2007 the system, based<br />
on an external referring drug prices compared<br />
to the 3+2 reference countries (Italy, France, Slovenia<br />
+ Spain, Czech Republic), was completely<br />
defined and implemented. Internal reference<br />
system was set up by defining and implementing<br />
41 therapeutic groups for prescription drugs:<br />
drugs with the same or similar therapeutic effect,<br />
usually defined by the fourth level ATC classifi-<br />
18 Proofreading and translations are in the explicit responsibility of the authors.<br />
cation of drugs. In the period from 2008 to 2010,<br />
consequent drug cost remained unchanged despite<br />
of the augmentation of 7 million prescriptions<br />
and introduction of a number of new drugs<br />
in the drug list. The insured persons can choose<br />
between free medicines from the basic drug list<br />
or more expensive alternative from the supplementary<br />
drug list by paying the difference in<br />
price. Drug producers can also choose between<br />
the reference price covered by basic insurance<br />
and the bigger price when the insured person<br />
pays difference in price.<br />
Using this model, it became unnecessary to relieve<br />
the insured of any co-payments (participation)<br />
while the options for the patient treatment<br />
remained at the same level. Croatian P&R model<br />
provides rational use of drugs and better control<br />
over the cost of drugs within the real possibilities<br />
of the budget.
Health Technology Assessment in Serbia<br />
Vlad Zah<br />
ISPOR Chapter Serbia<br />
This session reviews past and current approaches<br />
to Health Technology Assessment (HTA) in Serbia.<br />
It presents an overview of the product pricing<br />
and reimbursement processes for pharmaceuticals<br />
protected by patents.<br />
The new government regulations published in<br />
May 2011 do take into account necessity for the<br />
new innovative therapy, for the pharmacoeconomic<br />
indicators of justification for the new therapy application,<br />
as well as for the wholesale price of the<br />
new therapy. Over the last five years, there have<br />
been varying approaches utilized by the Serbian<br />
National Insurance Fund (RFZO) to regulate<br />
reimbursement policies and which products belong<br />
to which positive (reimbursement) list.<br />
As with any resources in a down turn, there has<br />
been not enough of health economists (among<br />
others) that could implement HTA effectively.<br />
This has been recognized by various institutions<br />
and the first training camps were open two years<br />
ago to facilitate this.<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 3.3.<br />
During this session attempts will be made to<br />
forecast further development of HTA in Serbia<br />
and its relationship to product pricing and reimbursement.<br />
Being financed predominantly by salaried workers<br />
and the respective level of salaries (70% of<br />
income), RFZO directly depends on the economic<br />
up/down turn. At the end of 2010, there<br />
were 1,626,581 pension beneficiaries, with a slight<br />
(1.4%) year-on-year increase. The ratio of total registered<br />
number of employees and total number of<br />
pensioners was 1.1 / 1.0. In a down turn, financial<br />
liquidity may become one of the issues. Namely, it<br />
can be difficult to collect funds in a timely fashion<br />
and in return this can cause shortages.<br />
During this session attempts will be made to<br />
forecast further development of HTA in Serbia<br />
and its relationship to product pricing and reimbursement.<br />
19
PL 3.4.<br />
Pricing Policy in Macedonia – overview analysis<br />
Marija Gulija, Gordana Damjanovska<br />
AD Dr. Panovski, Macedonia<br />
Defined systematized pricing policy in Macedonia<br />
was introduced through internal and external<br />
reference pricing system for drugs financially<br />
covered by the HIF. Recently, November<br />
2011, new Regulation for “ceiling” prices (unified<br />
prices of all drugs registered in the country)<br />
was enforced by the Bureau of Drugs, Ministry<br />
of Health. The purpose of this Regulation was to<br />
establish unification of ceiling prices of all drugs<br />
on the market in Macedonia. The Regulation<br />
aimed in controlling adjusted unified prices and<br />
stabilization of the pharmaceutical market.<br />
This overview analyses both methodologies developed,<br />
one from the HIF and the other from<br />
the Bureau of Drugs. This overview will try to<br />
provide information of the status of the prices<br />
of drugs on Macedonian pharmaceutical market,<br />
especially drugs financially covered by the<br />
HIF, through direct comparison of the prices of<br />
drugs, their adjustments and correlation.<br />
Performed analysis and comparison showed that<br />
prices of the drugs evaluated differ and are not<br />
20 Proofreading and translations are in the explicit responsibility of the authors.<br />
completely adjusted. Regarding all evaluated<br />
prices of the positive list drugs, significant number<br />
have reference prices higher than the official<br />
unified price. This is due to the differences in the<br />
two methodologies used for calculation of the<br />
prices and they being not previously adjusted<br />
to each other. Having two completely different<br />
methodologies creates problems when the price<br />
has to be used for direct procurement. Thus, if<br />
the reference price is lower than unified price,<br />
than the drug is procured in accordance to the<br />
unified price.<br />
Therefore the system of reference prices established<br />
by the HIF becomes interfered. On the<br />
other hand, unified prices enabled setting of the<br />
prices of expensive drugs on the positive list of<br />
drugs for hospitals. If the country needs and decides<br />
to use this combined pricing policy, then<br />
previous adjustments of methodologies used for<br />
calculation of prices must be completely adapted.
THE BLOCKADE OF SCIATIC NERVE AND POSSIBLE<br />
CONSEQUENCES OF INTRANEURAL INJECTIONS<br />
Livio Garattini, Katelijne van de Vooren<br />
CESAV, Center for Health Economics, ‘Mario Negri’<br />
Institute for Pharmacological Research, Italy<br />
Goal: The main objective of this comparative<br />
analysis was to assess the various co-payments<br />
on drugs applied in selected basket of EU western<br />
countries, either dealing with the problem of<br />
moral hazard or raising revenue.<br />
Materials and methods: We searched the internet<br />
to analyze the various co-payments for pharmaceuticals<br />
by patients in five West European countries;<br />
Germany, Italy, Norway, The Netherlands<br />
and the UK. Furthermore, we analyzed if and<br />
how patients with a lower income were compensated<br />
and protected from excessive expenses<br />
through exemptions.<br />
Results: Even though the situation varied substantially<br />
in the various countries, copayments<br />
were on average low in The Netherlands and the<br />
UK, while patients in Germany, Italy and Norway<br />
have to pay a higher share of out-of-pocket<br />
costs. As to the Netherlands, co-payments are<br />
caused by the difference between reference price<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 4.1.<br />
and actual price set by pharmaceutical companies.<br />
In the UK and in Italy the co-payment consist<br />
of a “lump sum” per prescription, although<br />
the situation is uneven throughout the countries<br />
(e.g. Scotland abolished co-payments, like some<br />
Italian regions), while in Germany and Norway<br />
a fixed proportion on prices has to be paid. In all<br />
countries regressive schemes are applied and patients<br />
with the lowest incomes and children are<br />
mostly exempted.<br />
Conclusion: Copayments exist in all the healthcare<br />
systems analyzed, doesn’t matter if they are<br />
taxation or insurance based. Even though evidence<br />
suggest that co-payments are inequitable,<br />
particularly in times of financial crisis, when<br />
budgets are tight while health care expenses are<br />
growing, increasing out-of-pocket costs is seen<br />
as a solution by health authorities to prevent<br />
overspending.<br />
21
PL 4.2.<br />
Impact of therapeutic class referencing (jumbo groups) as a method of<br />
Government cost containment measures on prescribing behaviours and<br />
consequent quality of patient care<br />
Sani Pogorilić, Jelka Drašković, Slobodanka Bolanča<br />
CARPC – Croatian Association of Research Based<br />
Pharmaceutical Companies<br />
Introduction: Therapeutic reference pricing<br />
(TRP) is a common cost containment measure<br />
used by payers to constrain rising pharmaceutical<br />
expenditure in a way that they are reimbursing<br />
the cost of certain medicine only up to a fixed<br />
maximum amount known as reference price. Patients<br />
are supposed to pay the difference between<br />
the reference price and the actual price. When<br />
such therapeutic classes are very broad and include<br />
both generics and patented medicines, the<br />
system is called jumbo group referencing and as<br />
such represents the most damaging form of reference<br />
pricing for both patients and innovative<br />
pharmaceutical industry.<br />
Materials and Methods: In this research, we have<br />
explored in detail historical pharmaceutical expenditure<br />
patterns using MIDAS, an IMS Health<br />
proprietary database, as well as a variety of secondary<br />
data sources. Croatian trends have been<br />
compared with those of a number of benchmark<br />
countries, categorized either as Peer Countries<br />
(Slovakia, Czech and Hungary) and Aspirational<br />
Countries known to have systems that have been<br />
ensuring excellent healthcare outcomes (France,<br />
Netherlands and Austria).<br />
Results: Jumbo groups account for around half<br />
of Croatian analysis market sales and two thirds<br />
of volume. A comparison of all jumbo grouped<br />
products in Croatia vs. use of those products<br />
in mentioned benchmark countries shows high<br />
consumption (higher volume usage) but low<br />
prices in Croatia. The relative distribution of<br />
products between basic and supplementary<br />
22 Proofreading and translations are in the explicit responsibility of the authors.<br />
lists has remained static over time as well as the<br />
amount of co-pay at approximately 6% of total<br />
Rx sales, although the trend of slow increase of<br />
co-pay for original products has been observed,<br />
but not for generics. Drugs with and without copays<br />
have broadly similar prices, albeit low compared<br />
to other countries. This suggests the level<br />
of co-pay is generally low for drugs on supplementary<br />
list. Jumbo prices have been declining<br />
more than total prices although both are low vs.<br />
Benchmark countries. Prices of generics in jumbo<br />
groups are high compared to originators and<br />
other countries.<br />
Conclusion: This study confirms our hypothesis<br />
that prescribing habits of Croatian physicians<br />
are impacted by jumbo groups as they are<br />
significantly different from those observed in<br />
analyzed benchmark countries. This can negatively<br />
impact quality of treatments, especially for<br />
chronic patients, and undermine equal access to<br />
healthcare while it is most probably not achieving<br />
expected savings as it pulls generic prices up<br />
and originator prices down or shifting them to<br />
supplementary list with co-payment. Patients<br />
are thus oriented towards medicines which may<br />
not be adapted to their needs, resulting in poorer<br />
health outcomes. The best alternative to this unfavourable<br />
cost containment measure is the use<br />
of health technology assessment of medicines<br />
which will enable authorities to adequately reward<br />
healthcare and economic improvements<br />
brought by new products.
Showing the use of drugs in the Clinical Center of Montenegro and<br />
comparison with modern pharmacotherapeutic recommendations<br />
Mirjana Jovanović-Đurašković, Olivera Prodanović<br />
Agency for Medicines and Medical Devices of<br />
Montenegro, Montenegro<br />
Goal: Analysis of the use of drugs is an important<br />
segment of clinical pharmacotherapy<br />
because it may indicate the need and ways to<br />
rationalize therapy. The aim of this study is to<br />
analyze it, which will enable more realistic look<br />
at the relationship between therapeutic practice<br />
proposed by doctrinal views and modern therapeutic<br />
practice that is specifically implemented<br />
in the selected area.<br />
Materials and Methods: The data source was the<br />
Clinical Center of Montenegro Pharmacy report<br />
on issued drugs. The use of drugs was expressed<br />
as the number of defined daily doses (DDD) per<br />
1,000 bed days (BD). After obtaining the results<br />
shown in tables and charts, made a retrospective<br />
analysis, we used a descriptive-analytical<br />
method.<br />
Results: In the reporting period, the most common<br />
groups of drugs have proven to be remedies<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 4.3.<br />
for diseases of blood and blood-forming organs<br />
(25.52%), in second place were drugs for the digestive<br />
tract and metabolism (21.91%), in the<br />
third to the nervous system drugs (17.34%), and<br />
the fourth - systemic antiinfectives (12.01%).<br />
Conclusion: Research on consumption and use<br />
of drugs is extremely important because it may<br />
indicate the need for rationalization of therapy,<br />
as well as the direction in which we are to make,<br />
and also the education of doctors in prescribing<br />
medications adjusted to the modern principles<br />
of pharmacotherapy. This research pointed to<br />
certain changes in the use of drugs in the Clinical<br />
Center of Montenegro in 2010. compared to<br />
research done in 2004, and that is necessary to<br />
make additional educational efforts to establish<br />
more regular access to the choice of drugs.<br />
23
PL 4.4.<br />
Comparison of drugs consumption in two Croatian county general<br />
hospitals<br />
Aleksandar Knežević1, Mila Basioli1, Hana Kalinić Grgorinić2<br />
1 General hospital Zadar, Croatia<br />
2 General hospital Pula, Croatia<br />
Comparison of drugs consumption in two Croatian<br />
county general hospitals<br />
Goal of study: To analyze drug consumption in<br />
two Croatian county general hospitals similar in<br />
size, expected level of health care and patients<br />
catchment areas.<br />
Materials and methods: We analyzed total drug<br />
consumption in HRK and particulary first twenty<br />
drugs (Top 20) which share about 50% of total<br />
drug consumption during 5 years (2007th to<br />
2011th).<br />
Results: In 2007, General Hospital Pula spent<br />
on drugs 27.296.962 HRK of which the Top 20<br />
13.956.483 HRK (51%). In the same year, General<br />
Hospital Zadar spent on drugs 28.985.189<br />
HRK and 16.132.925 HRK for Top 20 (56%).<br />
Values for 2011: General Hospital Pula a total of<br />
HRK 33.272.104, and Top 20 18.456.304 HRK<br />
(55%), General Hospital Zadar total of HRK<br />
43.040.099 and Top 20 22.702.476 HRK (53%).<br />
During the observation period total drugs consumption<br />
in General Hospital Pula increased<br />
24 Proofreading and translations are in the explicit responsibility of the authors.<br />
by 22%, and in Zadar General Hospital by 48%.<br />
Consumption of Top 20 increased by 32% in<br />
General Hospital Pula and in Zadar General<br />
Hospital by 41%. General Hospital Pula has a<br />
catchment area of about 160.000 inhabitants,<br />
506 beds contracted and 156.641 realised patient<br />
days, in 2011. Zadar General Hospital has<br />
a catchment area of about 200.000 inhabitants,<br />
483 contracted beds and 133.927 realised patient<br />
days in 2011. In 2011 General Hospital Zadar,<br />
although with 17%less realised patient days,<br />
spent 29% more for drugs in HRK.<br />
Conclusion: Differences between drug consumption<br />
in two compared hospitals can be explained<br />
by higher level of service in General Hospital<br />
Zadar or greater development of certain specialties,<br />
but also with more patients oriented toward<br />
that hospital. Of course, there is a possibility that<br />
the pharmacotherapy in General Hospital Pula is<br />
more rational than in Zadar. It certainly requires<br />
further investigation.
Burden of community acquired pneumonia in Central European countries<br />
Ales Tichopad 1 , C. Roberts 2 , A. Skoczynska 3 , I. Gembula 1 , K. Jahnz-Rozyk 4<br />
1 CEEOR, Prague, Czech Republic<br />
2 Pfizer, New York, USA<br />
3 National Medicines Institute, Warsaw, Poland<br />
4 Military Institute of Medicine, Warsaw, Poland<br />
Objectives: Older adults are in an increased risk<br />
of respiratory infections including community<br />
acquired pneumonia (CAP). The former socialistic<br />
countries of the central Europe form a<br />
unique region with specific health care and epidemiology<br />
characteristics, and where the local<br />
evidence on the underlying epidemiology in elderly<br />
is scarce. The objective of this study was to<br />
estimate the incidence and the case fatality rates<br />
(CFR) of CAP in adults ≥50 years of age in the<br />
Czech Republic (CR), Hungary (HU), Poland<br />
(PL) and Slovakia (SK).<br />
Methods: The incidence and the CFR for hospitalised<br />
CAP were estimated using the national<br />
surveillance systems (PL, CR, SK) and national<br />
insurance records (HU). National retrospective<br />
patient chart reviews (CZ, SK) were used to estimate<br />
the non-hospitalised CAP incidence as a<br />
portion of the hospitalised CAP. In PL we used<br />
national surveillance data and in HU the national<br />
insurance fund records to estimate outpatient<br />
CAP incidence.<br />
Results: Hospitalised CAP incidence per 100,000<br />
person years was 457 in CR, 879 in HU 879, 364<br />
in PL, and 524 in SK. The CFR per 100 cases of<br />
hospitalised CAP was estimated as 21 in CR; 20<br />
in SK; and 18 both in PL and HU. Non-hospitalised<br />
CAP incidence per 100,000 person years<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 5.1.<br />
was 710 in CR, 3551 in HU, 316 in PL, and 598<br />
in SK. Compared with adults 50-64 years of age,<br />
the incidence of hospitalised CAP were 2.3 fold<br />
higher in those 65-74, 5.2 fold higher in 75-84<br />
and 10.8 fold higher in those ≥85, manifesting<br />
an exponential trend. By contrast, the incidence<br />
of non-hospitalised CAP was generally flat or declining<br />
with age, representing a higher likelihood<br />
of hospitalisation with increasing age. The total<br />
number of hospitalisations and deaths in CR,<br />
HU, PL, and SK were 17,473 and 3,686; 23,652<br />
and 4,796; 35,895 and 7,325; 6,321 and 1,497) In<br />
Poland, for example, adults over 65 represent approximately<br />
14% of the study population, while<br />
they account for 80% of deaths from CAP).<br />
Conclusion: The morbidity and mortality of hospitalised<br />
CAP increases sharply with advancing<br />
age, signalling a likely increasing public health<br />
problem as the population ages over time. In HU,<br />
where the primary incidence data were provided<br />
by the national insurance fund, substantially<br />
larger incidence was calculated in both types of<br />
CAP with strikingly high number of outpatient<br />
CAP cases. This may be mainly due to different<br />
coding practice. Nevertheless, CAP poses a<br />
significant burden in all four countries among<br />
adults ≥50 years of age.<br />
25
PL 5.2.<br />
The role of health authorities in promotion of rational use of antibiotics<br />
Merjem Hadjihamza<br />
Drug Bureau - Ministry of Health, Skopje, Macedonia<br />
Health care systems and health policies differ<br />
from country to country and they reflect the economic,<br />
social and even political situation of each<br />
country. The main goal of any Health authority<br />
should be creating and implementing of policies<br />
which will promote the public health, provide<br />
quality health services at all levels of health care<br />
and ensure the access of drugs with proven quality<br />
and safety for the whole population.<br />
Rational use of antibiotics is of high relevance in<br />
improving health care and it has emerged as a<br />
global challenge imposed due to adverse findings<br />
about their use.<br />
WHO estimates that more than half of all medicines<br />
are prescribed, dispensed or sold inappropriately,<br />
and that half of all patients fail to take<br />
them correctly. This incorrect use may take the<br />
form of overuse, underuse and misuse of prescription<br />
or non-prescription medicines.<br />
What should be done to prevent irrational use of<br />
antibiotics?<br />
26 Proofreading and translations are in the explicit responsibility of the authors.<br />
First it must be determined exactly what in practice<br />
means irrational use of antibiotics, what are<br />
the reasons and consequences of irrational use,<br />
who are the involved parties and finally, which<br />
mechanisms must be established in order to promote<br />
rational use of antibiotics. Having in mind<br />
the scientific, social and regulatory dimension of<br />
this phenomenon, Ministry of Health of Republic<br />
of Macedonia have undertaken many activities<br />
i.e. published EBM guidelines, Continual medical<br />
education for health professionals is ongoing process<br />
since year 2000, last year it has been endorsed<br />
National strategy for control of antimicrobial resistance<br />
for 2012-2016. Organizing trainings on<br />
rational use of antibiotics with population based<br />
groups is foreseen in future. It may be conluded<br />
that raising the awareness of all stakeholders regarding<br />
rationale use of antibiotics is very important,<br />
it will for sure fight antimicrobial resistance<br />
and improve public health, decrease antibiotics<br />
expenditure and save health budget.
Pharmacoeconomic analysis comparing the use of ciprofloxacin and<br />
metronidazole versus ertapenem in prophylaxis of mayor surgical<br />
procedures at the University Hospital Rebro<br />
Ivana Čegec, Robert Likic, Ksenija Makar Ausperger, Viktorija Erdeljic, Matea<br />
Radacic Aumiler, Danica Juricic Nahal, Luka Bielen, Iva Kraljickovic, Igor Francetic<br />
University Hospital Center Zagreb, Zagreb, Croatia<br />
Goal: At the University Hospital Rebro (Zagreb;<br />
Croatia), combination of ciprofloxacin 2x400mg<br />
I.V. and metronidazole 3x500mg I.V. is a usual<br />
antimicrobial prophylaxis for mayor surgical<br />
procedures. Our aim was to compare daily cost<br />
of that practice versus ertapenem 1x1gr I.V.<br />
Materials and Methods: We collected pricing<br />
data concerning the usual daily doses of ciprofloxacin<br />
plus metronidazole combination and ertapenem,<br />
infusion system as well as nursing time<br />
for one day of therapy and compared them.<br />
Results: One day of therapy with ciprofloxacin<br />
and metronidazole combination costs 429.29kn<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 5.3.<br />
(57.2 €) while one day of therapy with ertapenem<br />
is priced at 374.334kn (49.9€).<br />
Conclusion: Therapy with ertapenem is significantly<br />
cheaper (13% less on a daily basis) in<br />
comparison to ciprofloxacin and metronidazole<br />
combination. Considering the ertapenem’s broad<br />
spectrum of antibacterial activity, pharmacokinetic<br />
and pharmacodynamic characteristics as<br />
well as its lower cost of treatment, this therapeutic<br />
option should be given priority in antimicrobial<br />
prophylaxis for mayor surgical procedures at<br />
the University Hospital Rebro.<br />
27
PL 5.4.<br />
Impact of Ceftriaxone De-restriction on the Cost of Antibiotic Treatment<br />
Srecko Marusic 1 , Vesna Bacic-Vrca 2 , Jasenka Skrlin 3 , Lado Uglesic 4<br />
1 Department of Clinical Pharmacology, University<br />
Hospital Dubrava, Zagreb, Croatia<br />
2 Department of Clinical Pharmacy, University<br />
Hospital Dubrava, Zagreb, Croatia<br />
3 Department of Clinical Microbiology and Hospital<br />
Infections, University Hospital Dubrava, Zagreb,<br />
Croatia<br />
4 Pfizer Croatia d.o.o., Zagreb, Croatia<br />
Goal: In 2008, cefuroxime was the only second<br />
generation cephalosporin available in Croatia<br />
and responsible for largest share of antibiotics<br />
cost at the University Hospital Dubrava, Zagreb.<br />
The market price of ceftriaxone, which was included<br />
in the list of antibiotics with restricted<br />
use, was about 40% lower then the market price<br />
of cefuroxime. As a cost-saving measure ceftriaxone<br />
was removed from the list of restricted<br />
antibiotics in May 2008 and started to be used<br />
as first-line antibiotic. The aim of this study is<br />
comparison of total antibiotic cost and cephalosporins<br />
and carbapenems costs before and after<br />
intervention.<br />
Materials and methods: Data on antibiotic use<br />
were obtained monthly from the computerized<br />
hospital pharmacy database. These data are expressed<br />
as the costs of antibiotics in Croatian<br />
kunas per 1000 bed days. The observed period<br />
was 2 years before intervention and 2 years after<br />
intervention.<br />
28 Proofreading and translations are in the explicit responsibility of the authors.<br />
Results: Total antibiotic cost did not change significantly.<br />
Cost of cefuroxime and ceftriaxone<br />
showed expected changes, cefuroxime cost decreased<br />
and ceftriaxone cost increased. Carbapenems<br />
cost increased significantly.<br />
Conclusion: Total antibiotic cost did not decrease<br />
in post-intervention period due to increase<br />
in carbapenems cost. Increase in the use<br />
of third-generation cephalosporins led to increase<br />
in ESBL-positive pathogens and increased<br />
use of carbapenems. Beside costs, this can have<br />
negative epidemiological impact in creating hospital<br />
situations with pathogens producing ESBLs<br />
and carbapenemases with very limited possibility<br />
for efficient therapy. Therefore, a reduction in<br />
use of third-generation cephalosporins and their<br />
replacement with different types of antibiotics<br />
seems necessary.
Impact of the Pharma Economic Act on diffusion of innovation, reduction<br />
of costs and patients’ equity in the Hungarian prescription drug market<br />
Rok Hren<br />
University of Ljubljana, Slovenia<br />
Sažetak: In this study, we examined the impact<br />
of Pharma Economic Act (PEA), which was introduced<br />
in Hungary in 2007. The motivation to<br />
analyze this particular legislative measure within<br />
a single mid-size country is in its comprehensiveness<br />
and in its unique approach toward marketing<br />
authorization holders (MAHs). Moreover,<br />
recent economic crisis is making such a »laboratory<br />
of cost-containment tools« attractive for authorities<br />
and payers not only among the Central<br />
and Eastern European (CEE) countries, but also<br />
among Western (e.g., EU-15) jurisdictions. Final<br />
reason for the analysis is availability of detailed<br />
data on Hungarian prescription drug market,<br />
which are provided to the public by the authorities.<br />
Controlling prescription drugs spending is<br />
fraught with difficulties, and particularly notable<br />
are examples of GP Fundholding scheme in the<br />
UK and prescribing drug budgets in Germany.<br />
Difficulties arise due to multifactorial reasons<br />
for pharmaceutical expenditure growth, which<br />
are usually addressed only partially with national<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 6.1.<br />
prescription drug policies. Typically, the authorities/payers<br />
introduce two groups of policies: one<br />
group on the so-called demand side (e.g., physicians,<br />
pharmacists, and patients), and one group<br />
on the supply-side (e.g., MAHs). International<br />
reference pricing has been widely embraced by<br />
authorities/payers as a particular supply-side<br />
tool geared toward regulating prices of primarily<br />
branded drugs.<br />
Hungarian authorities / payers with PEA took different<br />
approach and included, among a plethora<br />
of other measures, strong mechanisms to control<br />
volume on the supply side, with MAHs being responsible<br />
to cover any overshoot of the pre-agreed<br />
volume. In that sense, PEA is unique among CEE<br />
jurisdictions, however, at its conception there were<br />
serious warnings that the austerity act may jeopardize<br />
innovation and could even lead to withdrawals<br />
of breakthrough branded drugs. Accordingly, we<br />
are here specifically evaluating the effect of PEA<br />
on both dynamic and static efficiencies and also<br />
on equity, which has been historically a controversial<br />
issue in Hungary.<br />
29
PL 6.2.<br />
Ethics as a rising issue for targeted therapies: the metastatic colorectal<br />
example<br />
Livio Garattini, Katelijne van de Vooren<br />
CESAV, Center for Health Economics, ‘Mario Negri’<br />
Institute for Pharmacological Research, Italy<br />
Goal: The number of new biological agents (BAs)<br />
registered with an indication related to cancer<br />
treatment is flourishing and the cost of these<br />
treatments is rising dramatically, making the<br />
situation potentially unsustainable for healthcare<br />
services. As an interesting example to draw lessons,<br />
we focus here on bevacizumab (BV) and<br />
cetuximab (CX), the first two BAs approved for<br />
metastatic colorectal cancer (mCRC).<br />
Materials and methods: We reviewed full economic<br />
evaluations (FEEs) on BV or CX to analyze<br />
their results, the literature search was done<br />
on the PubMed international database to select<br />
FEEs on BV and CX published in English since<br />
January 2004. Finally, we selected eight articles.<br />
Results: Despite frequently arguable estimates<br />
based on indirect efficacy, only one of the eight<br />
FEEs reviewed estimated the addition of CX was<br />
cost-effective in a virtual subgroup of patients,<br />
albeit with flawed methods.<br />
Conclusion: Most Western European countries<br />
reimburse BV and CX for mCRC, though<br />
30 Proofreading and translations are in the explicit responsibility of the authors.<br />
both clinical and economic evidence seems very<br />
weak. The underlying question, hardly made explicit,<br />
is whether national health authorities are<br />
prepared to spend an increasing share of healthcare<br />
budgets on very expensive end-of-life treatments,<br />
their impact on life expectancy (a few<br />
additional months at best) and QoL (enhanced<br />
mainly by patients’ hopes) being doubtful and<br />
their cost-effectiveness hardly ever proved. Assessing<br />
these treatments highlights the problems<br />
raised by market failure in health care, where a<br />
“third party payer” funds treatments prescribed<br />
by a physician for a patient who can hardly be<br />
expected to behave as a rational consumer.<br />
At present, the fullest approach to decisions on<br />
reimbursement of new technologies with sustainable<br />
costs is expected to be the multidisciplinary<br />
“health technology assessment” (HTA).<br />
Unfortunately, although ethics is an acknowledged<br />
part of HTA, there is scant evidence that<br />
ethical issues are commonly addressed.
Implementation of biological therapy and surgery in the treatment of<br />
metastatic colorectal cancer: Are the costs justified?<br />
Renata Dobrila-Dintinjana, Dinko Vitezić<br />
University of Rijeka Medical School and Department<br />
of Oncology and Radiotherapy, University Hospital<br />
Centre Rijeka, Rijeka, Croatia<br />
Colorectal cancer (CRC) is a disease of high incidence<br />
and mortality (700 000 deaths annually<br />
in the world), and it is the third cause of cancer<br />
deaths in the Western world. Despite prevention<br />
programs on global and national level at the time<br />
of diagnosis about 25% of patients have metastatic<br />
disease, and approximately 50% of patients<br />
will develop metastatic disease. Although the<br />
tendency to perceive the occurrence of CRC in<br />
younger age groups this cancer is still a disease<br />
of old age group patients (70-75 years). Modern<br />
methods of treatment with chemotherapy and<br />
biological therapy significantly prolonged survival,<br />
but such treatment in developed countries is increasingly<br />
becoming an important financial issue<br />
for healthcare systems. The current challenge for<br />
oncologists and the healthcare systems is how to integrate<br />
a new set of biological therapy into clinical<br />
practice and for this purpose it is necessary to apply<br />
health technology assessment (HTA).<br />
The fact is that the patients undergoing radical<br />
surgery have a chance for prolonged survival<br />
and, according to some authors, for complete<br />
cure. In the first postoperative year recurrences<br />
of the disease in 60% or more of patients may<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 6.3.<br />
be expected. Operating costs of treatment are<br />
high and in combination with systemic therapy<br />
is a marked impact on health systems around the<br />
world.<br />
It is therefore clear why screening programs are<br />
carried out in spite of unclear evidence about the<br />
usefulness thereof. The ultimate goal of screening<br />
is to reduce morbidity and mortality, and the<br />
diagnosis of the disease at an early stage, as a rule<br />
does not justify the screening process. The possibility<br />
that the disease could be detected in earlier<br />
stages and diminished mortality is a sufficient<br />
ground to pursue global and national screening<br />
programs, although there are not enough scientific<br />
facts which indicate a clear benefit for the<br />
general population.<br />
OTA and POHEM screening models showed<br />
that the 10-year mortality can be reduced by<br />
17.9% per year and the cost for the life-saved<br />
year is from US$ 12,000 to 13,500. The most effective<br />
is the screening of individuals aged 50-74<br />
years. However, it has not been proved that these<br />
results can be reproduced in the general population.<br />
The colorectal cancer screening costs are<br />
higher than for cervical and breast cancer.<br />
31
PL 6.4.<br />
The role of cytology in detection of small breast cancer – experience of<br />
University Hospital for Tumours, Zagreb (cost benefit?)<br />
Vesna Ramljak, Iva Bobuš-Kelčec, Merdita Agai, Ljiljana Mayer<br />
Clinical Hospital Center “Sestre milosrdnice”,<br />
University Clinic for Tumors, Zagreb, Croatia<br />
Aim: University Hospital for Tumours is highly<br />
specialised oncological centre. The majority of<br />
breast cancer patients in Croatia are surgically<br />
treated here; more than 3500 woman were operated<br />
in last 5 years. The aim was to evaluate the<br />
role of cytology in detection tumours less than<br />
1cm in size. Long time follow-up indicates much<br />
better prognosis for such patients than those<br />
with tumours larger than 1cm.<br />
Materials and methods: We analysed group of<br />
patients cytologicaly diagnosed as breast cancer<br />
and treated in our institution during 2011.<br />
US guided FNAB was performed and cytological<br />
diagnosis implied cancer in all cases. Final<br />
histological report included tumour size and<br />
differentiation grade, involvement of axillary<br />
lymph nodes, estrogen and progesteron receptors,<br />
HER-2 and Ki-67. Separate analysis was<br />
performed for T1a and T1b group of patients.<br />
Results and conclusion: There was no difference<br />
between groups in patients age, 59,2 vs. 59 years<br />
. As expected differentiation grade was low in<br />
both groups in more than 90% of patients. In<br />
32 Proofreading and translations are in the explicit responsibility of the authors.<br />
majority of patients axillary lymph nodes were<br />
not involved, (93% and 84%). High expression<br />
of HER-2 (3+) was found in 3,3% of patients<br />
in T1a group, and in 7,1 % of patients in T1b<br />
group. HER-2 was negative in 70% of T1a cases<br />
and 80% of T1b cases. Mean (range) of Ki-67 expression<br />
was 19% (3-54) for T1a group, and 12%<br />
(1-14) for T1b group. Early cytological recognition<br />
of cancer provided a group of patients with<br />
excellent prognostic factors. Adjuvant therapy<br />
is planned based on prognostic factors. In this<br />
group of patients’ majority received adjuvant<br />
hormonal therapy – estrogen receptor antagonists<br />
(tamoxifen) or aromatase inhibitors. In<br />
only small proportion of patients adjuvant chemotherapy<br />
was indicated. Our results show high<br />
value of cytology in detection of small breast<br />
cancer. Detection of small cancer enables us to<br />
reduce treatment to surgery, radiotherapy and<br />
hormonal adjuvant therapy with expected high<br />
cure rates, low rates of treatment complications,<br />
good quality of life after treatment, and declining<br />
costs.
Comparative analysis of patient access to targeted therapies for metastatic<br />
renal cell carcinoma (mRCC) in selected CEE countries<br />
Jasmina Krehić 1 , Novka Agić 2 , Vedrana Raguž 3<br />
1 Clinical Centre of the University Sarajevo, Bosnia<br />
and Herzegovina<br />
2 Institute for Health Insurance and Reinsurance of<br />
the Federation of Bosnia and Herzegovina, Bosnia<br />
and Herzegovina<br />
3 Pfizer Croatia, Zagreb, Croatia<br />
Goal: Our goal was to analyze differences in<br />
patient access to targeted therapies for metastatic<br />
renal cell carcinoma (mRCC) between two<br />
nonEU countries, Bosnia and Herzegovina and<br />
Croatia, on one hand, and Slovenia as an EU<br />
member state, on the other.<br />
Materials and Methods: We performed a study<br />
using the officially published data from relevant<br />
national institutions in order to determine first<br />
registration lags and reimbursement lags of<br />
new targeted therapies for mRCC indication in<br />
Bosnia & Herzegovina and Croatia as opposed<br />
to Slovenia. Data collection was limited to six<br />
targeted agents that have come into EU market<br />
since 2005: sorafenib, bevacizumab, temsirolimus,<br />
sunitinib, everolimus and pazopanib.<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 6.5.<br />
Results: There are considerable variations and<br />
inequities between selected three countries in<br />
patient access to targeted therapies for mRCC.<br />
As a country with all six targeted agents registered<br />
and reimbursed, Slovenia is a leader. Croatia<br />
and Bosnia & Herzegovina lag behind Slovenia<br />
in registration and reimbursement for these<br />
selected agents..<br />
Conclusion: A patient access to targeted therapy<br />
for mRCC is of clinical importance, knowing the<br />
fact that this new therapy prologs lives and improves<br />
quality of life. Our analysis indicates that<br />
delay in the registration and reimbursement of<br />
new drugs in one country prevents the patients<br />
living with life-threatening disease from receiving<br />
the most effective and safest treatments available<br />
in another country.<br />
33
PL 6.6.<br />
Pharmacoeconomics in Predictive Medicine<br />
Josip Čulig, Marcel Leppee, Nikolina Skaron-Jakobović<br />
Zagreb Institute of Public Health, Zagreb, Croatia<br />
A genomic-based prediction of common diseases<br />
is still not very informative, and is with little predictive<br />
power, despite increasing developments<br />
in genomic research. Risk assessment based on<br />
a genetic profile is correct when a genetic predisposition<br />
is the only risk factor for a disease or<br />
drug therapy. The impact on the health care budget<br />
might be significant because of the high cost<br />
of predictive-genetic testing. Pharmaco-economic<br />
tools could prove to be useful in assisting<br />
decision-makers on this subject. The pharmacogenomic<br />
biomarkers have already demonstrated<br />
superior impact in improving drug efficacy and<br />
avoiding drug toxicity. As an example of an<br />
implementation personalised therapy, we have<br />
analysed the introduction of new medication in<br />
a selected group of patients with non-small cell<br />
lung cancer (NSCLC). It is a biologically aggressive<br />
type of cancer and the leading cause of cancer<br />
death in men and women. Many tumours,<br />
including those of the lungs, show increased<br />
34 Proofreading and translations are in the explicit responsibility of the authors.<br />
activity of the epidermal growth factor receptor<br />
(EGFR). Various clinical trials have shown that<br />
patients with advanced NSCLC and EGFR mutations<br />
had significant benefits from gefitinib therapy,<br />
while patients without these mutations did<br />
not. A budget impact analysis (BIA) compared<br />
the cost of gefitinib (190.151 HRK, Croatian national<br />
currency, per patient) and the cost of standard<br />
chemotherapy (188.724 HRK). There are<br />
some advantages to gefitinib therapy: prolonged<br />
time of progression; a higher degree of survival<br />
in the first line (51%); received in 10 cycles (10<br />
months) compared to the reference scenario (6<br />
cycles); fewer side effects (a difference in cost<br />
of 311 HRK to 4 072 HRK per patient); no cost<br />
administration of the drug (per os administration<br />
of medication); better quality of life (higher<br />
QALY); and other. It is important to establish the<br />
real cost of the standard procedure in advanced<br />
NSLC, including genetic testing.
The economic cost analysis of the implementation of centralized pharmacy<br />
unit for antineoplastic drugs with respect to the premises, equipment and<br />
technical staff under the supervision of oncology pharmacist<br />
Vesna Pavlica 1 , Damir Vrbanec 2 , Velemir Danko Vrdoljak 1<br />
1 Clinical Hospital Center „Sestre milosrdnice“,<br />
University Clinic for Tumors, Zagreb, Croatia<br />
2 Clinical Hospital Center Zagreb, Croatia<br />
Goal:this paper presents the results of long-term<br />
cooperation between the onclogy pharmacist,<br />
oncologists and technical support staff, as well as<br />
the economic and safety justification of the implementation.<br />
This refers to patient safety, related<br />
to the reduction in the frequency of medication<br />
error and staff safety that manipulates antineoplastic<br />
drugs and the safety of hospital settings.<br />
Material and methods: all relevant data was collected<br />
by means of the standardized ESOP questionnaire<br />
from various hospitals in Croatia and<br />
by analysis of different project documents.<br />
Results: results obtained were statistically processed<br />
and indicate the need for permanent education<br />
and cooperation between health workers<br />
and technical support staff, which is of utmost<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 6.7.<br />
importance. The results are the first sistematically<br />
collected data related to the manipulation<br />
of antineoplastic drugs in the republic of Croatia.<br />
Conclusion: antineoplastic drugs are cytotoxic,<br />
teratogenic, mutagenic and embryotoxic and<br />
should be subjected to a special preparation and<br />
manipulation procedures, especially in view of<br />
their cost. In most countries in the world, and<br />
in the EU in particular, their preparation takes<br />
place under a strict control of oncology pharmacists<br />
and under precisely determined spatial and<br />
technical conditions. From the data analysis we<br />
conclude that a pharmacist needs to specialize in<br />
this pharmacy field and take an active role in the<br />
promotion of knowledge, thus becoming a part<br />
of the health care oncology team.<br />
35
PL 7.1.<br />
Musculoskeletal disorder - their impact on work ability and societal costs in<br />
Poland<br />
Magdalena Wladysiuk, Ksenia Zhelthoukhova, Stephen Bevan, Mateusz Haldas<br />
CEESTAHC - Central and Eastern European Society<br />
of Technology Assessment in Health, Poland<br />
Fundamental changes need to occur in the way<br />
policy-makers, medical professionals, employers<br />
and even individuals themselves approach<br />
the management of long-term conditions. Fit for<br />
work project was conducted in Poland in 2011 to<br />
estimated social burden of MSD (musculoskeletal<br />
disorders) and their on work ability (direct<br />
and indirect cost).<br />
Results: Musculoskeletal conditions incurred<br />
costs of almost 330 million Euros in sickness absence<br />
and another 470 million Euros in costs of<br />
disability in 2009. Up to 874 million Euros were<br />
spent on the welfare benefits of the work disabled<br />
with only 38 million Euros put to preventative<br />
rehabilitation. In 2010 total direct costs of<br />
the conditions of musculoskeletal system added<br />
up to 937 million Euros, of which only 223 Euros<br />
were spent on preventative health care. The<br />
36 Proofreading and translations are in the explicit responsibility of the authors.<br />
average age of the recipients of the rehabilitation<br />
benefits in Poland was 46 years meaning that<br />
increasingly more individuals of prime working<br />
age require support for managing their longterm<br />
conditions. At least 12 per cent of registered<br />
unemployed people in Poland do not seek work<br />
due to poor health condition.<br />
The evidence presented in this report illustrates<br />
that a large proportion of working age people in<br />
oland are, or will be, directly affected by musculoskeletal<br />
conditions (MSDs) in the coming<br />
years. This an have very significant social and<br />
economic consequences for these individuals<br />
and their families, it can impede the productive<br />
capacity of the total workforce and parts of<br />
Polish industry, and it can raw heavily on the<br />
resources of both the health system and the benefits<br />
regime.
Case study in transplantation and immunosuppressant therapy in<br />
Macedonia, three year follow up<br />
Stevce Acevski 1 , Zoran Sterjev 2 , Vladimir Indov 1<br />
1 Alkaloid AD Skopje, Skopje, Macedonia<br />
2 Faculty of Pharmacy, Skopje, Macedonia<br />
The aim is to present situation with organ transplantation<br />
and immunosuppressant therapy in<br />
Macedonia. Immunosuppressant therapy is essential<br />
for patients after transplantation, in order<br />
to suppress immune response, to prevent rejection<br />
of grafts or transplants. In Macedonisloan<br />
healthcare system there are tree active transplantation<br />
procedures, kidney, liver and bone marrow.<br />
Kidney transplantation is active for 15 years<br />
and there are more of 160 live patients. Annually<br />
10 – 20 kidney`s are transplanted. All transplanted<br />
patients are started initially with immunosuppressive<br />
therapy, and take lifelong doses. Bone<br />
marrow transplantation is active for 11 years and<br />
total 215 patients are transplanted, annually 20<br />
– 25. One third of are allogenic (other donor)<br />
transplantations, which by the protocol get immunosuppressant<br />
therapies, mostly cyclosporine<br />
and mycophenolate mofetil, for the first six<br />
months. Liver transplantation is active in Macedonia<br />
since 2011, only one child is transplanted.<br />
According to protocols was initially treated with<br />
tacrolimus.<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 7.2.<br />
Twelve immunosuppressant products are registered<br />
in Macedonia of which two cyclosporine,<br />
two antithymocyte immunoglobulin, four mycophenolate<br />
mofetil, tacrolimus, daclizumab, basiliximab<br />
and everolimus, of which six are not marketed<br />
at all. Five generics are on reimbursement<br />
list of HIF, but only three of them are marketed.<br />
In 2009 for immunosuppressant therapy was<br />
spend 593.000 Euro 1.15% of total budget spend<br />
for medicines. Spending in 2010 decreased to<br />
522.000 Euro or 12 % less than previous year,<br />
0.86% of total budget for medicines. Promoted<br />
use of new immunosuppressive drugs such as<br />
tacrolimus and sirolimus were main factor for<br />
increased spending for immunosuppressant<br />
therapy in 2011 to 590.000 Euro, or 13% more<br />
compared to 2010 or 0.99% of total budget for<br />
medicines.<br />
Nevertheless continuous price reduction of<br />
the medicines, positive trend in number of<br />
transplantation\’s and implementing use of new<br />
immunosuppressant drugs are main factors in increased<br />
spending for immunosuppressant therapy.<br />
37
PL 7.3.<br />
Rare diseases or disorders, orphan drugs and patients equity rights<br />
Jasmina Krehić 1 , Senka Mesihović Dinarević 1<br />
1Clinical Centre University of Sarajevo, Sarajevo,<br />
Bosnia and Herzegovina<br />
The term “rare diseases” or “rare disorders” by<br />
definition is different in different parts of world.<br />
In Europe it is defined as life-threatening or very<br />
serious conditions that are rare and affect not<br />
more than 5 in 10,000 persons, in US those are<br />
diseases/disorders that affect fewer than 200,000<br />
people and WHO defines an incidence of 0.65-<br />
1/1000. \’\’Orphan\’\’ medicinal products are<br />
intended for diagnosing, preventing or treating<br />
rare diseases/disorders. Although pharmaceutical<br />
companies are consistantly developing new<br />
drugs, people with rare diseases/disorders are<br />
not in focus of their their interes beause numbers<br />
of those patients are small as well as potential<br />
market for orphan drugs. But, Article 25.1<br />
of the Universal Declaration of Human Rights<br />
states:“everyone has the right to health and well<br />
being and especially to medical care and social<br />
services”. So, the right to health protection is universal,<br />
and ethial issues rising from this Delaration<br />
clearly oblige governments to ensure pres-<br />
38 Proofreading and translations are in the explicit responsibility of the authors.<br />
ence of orphan drugs in the drug market. Regulatory<br />
agencies in the European Union and the<br />
United States have thus established Committee<br />
on Orphan Medicinal Products and Office of Orphan<br />
Product Development (OOPD) to facilitate<br />
the development of orphan drugs. Regardless<br />
of existance of such departments in European<br />
Medicines Agency (EMEA) and Food and Drug<br />
Administration (FDA) orphan drugs still have<br />
to pass through all preclinical and clinical trials<br />
to prove their efficacy and safety. At the end an<br />
expensive drug with very rectricted market is developed.<br />
For that reason access to orphan drugs<br />
should be facilitated by the whole community<br />
– from governments, pharmaceutical industry,<br />
health funds and patient associations. In Western<br />
Balkan countries should be developed an shared<br />
network for rare diseases register, strengthened<br />
cooperation of patient associatioans, education,<br />
early diagnosis as well as the influence on research<br />
and health funds and governments.
STEREOLOGICAL ANALYSIS OF TERMINAL VILLI OF HUMAN<br />
PLACENTAS ASSOCIATED WITH EPH GESTOSIS<br />
Dinko Vitezić<br />
University of Rijeka Medical School and University<br />
Hospital Centre Rijeka, Rijeka, Croatia<br />
Hypertension is a major risk factor for stroke,<br />
myocardial infarction, heart failure, chronic kidney<br />
disease, peripheral vascular disease, cognitive<br />
decline and premature death. Treatment of<br />
hypertension is of utmost importance in prevention<br />
of morbidity and premature mortality. This<br />
is the reason why antihypertensive drugs are the<br />
most frequently prescribed and costly drugs in<br />
most of the countries (Croatia as well). Clinical<br />
guidelines for hypertension treatment are important<br />
for adequate drugs usage and among them<br />
European guidelines (ESH-ECS), United States<br />
guidelines (JNC-7) and England and Wales<br />
guidelines (NICE) are the most influential. Pharmacoeconomic<br />
issues are included in JNC-7 and<br />
especially in NICE guidelines, while ESH-ECS<br />
guidelines are strictly clinical with no pharmacoeconomic<br />
aspect. The NICE analysis and different<br />
studies showed that treating hypertension<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 7.4.<br />
is highly cost-effective and the result is improved<br />
health outcomes. Major drug classes resulted in<br />
overall cost savings when compared to no treatment<br />
because of the reduction in cardiovascular<br />
events, which led to savings that compensate the<br />
relatively low cost of drugs. Certain savings are<br />
gained because the absolute difference in costs<br />
between angiotensin converting enzyme inhibitors,<br />
angiotensin receptor blockers, calcium<br />
channel blockers and thiazide-type diuretics is<br />
now much smaller than it was according to previous<br />
analyses. Further, usage of low cost generic<br />
drugs could make the impact on savings more<br />
significant.<br />
Adequate usage of antihypertensives, according<br />
to clinical guidelines, has positive pharmacoeconomic<br />
impact (besides obviously clinical), but it<br />
would be necessary to perform analyses locally<br />
to measure dimensions of this savings.<br />
39
PL 7.5.<br />
Trends in the utilization of cardiovascular drugs in Croatia during the<br />
period 2007-2010<br />
Viola Macolić-Šarinić, Pero Draganić, Josip Čulig, Marcel Leppée, Marinko Bilušić,<br />
Saša Žeželić<br />
ISPOR chapter Croatia, Zagreb, Croatia<br />
Goal: A comprehensive insight into drug utilization<br />
as an economic and a public health issue<br />
can only be acquired in the context of the overall<br />
state of health of the respective population.<br />
The goal is to investigate the utilization trends of<br />
cardiovascular drugs in Croatia during the 2007-<br />
2010 period, with an emphasis on the most common<br />
pharmacological/therapeutic subgroups.<br />
This will be compared with the number of patients<br />
admitted to hospital because of cardiovascular<br />
events.<br />
Materials and methods: The Croatian Agency for<br />
Medicinal Products and Medical Devices collected<br />
and analyzed data of drug utilization in<br />
Croatia. The data was used to calculate the number<br />
of defined daily doses (DDD) and DDD per<br />
1000 inhabitants per day (DDD/1000/day), in<br />
the period 2007-2010, using Anatomical-Therapeutic-Chemical<br />
methodology (ATC). A Public<br />
Health Institute is analyzing the data obtained<br />
from hospital statistics.<br />
40 Proofreading and translations are in the explicit responsibility of the authors.<br />
Results: The utilization of all cardiovascular drugs<br />
increased by 47, 55% (from 248, 88 DDD/1000/<br />
day in 2007 to 367, 23 DDD/1000/day in 2010),<br />
while the total cost increased by 13, 09% (from<br />
863,601,721 HRK in 2007 to 976,657,904 HRK<br />
in 2010). The utilization of the lipid modifying<br />
agents (C10) increased the most (78, 93%), followed<br />
by agents acting on the renin-angiotensin<br />
system (57, 51%). The calcium channel blockers<br />
(28, 46%) were next. The total number of hospital<br />
admissions for cardiovascular diseases decreased<br />
from 84,413 in 2007 to 81,575 in 2010.<br />
Conclusion: The utilization of cardiovascular<br />
drugs increased significantly during the 2007-<br />
2010 period. In the same period, the number of<br />
hospital admissions of patients with main cardiovascular<br />
events (3, 4%) has decreased. A further<br />
analysis of this co-founder is needed.
Comparative analysis of cardiovascular drugs utilisation in General<br />
Hospital and Clinical Center in Croatia and Bosnia and Herzegovina<br />
Mirza Dilić 1 , Aleksandar Knežević 2 , Sanja Sarić-Kužina 3 , Anesa Eminović 1<br />
1 Clinical Center University of Sarajevo, Sarajevo,<br />
Bosnia and Herzegovina<br />
2 General Hospital Zadar, Zadar, Croatia<br />
3 Pfizer Croatia, Zagreb, Croatia<br />
Goal: Our goal was to analyze and compare the<br />
cardiovascular (CV) drugs utilisation in General<br />
Hospital Zadar (GHZ) and Clinical Center University<br />
of Sarajevo (KCUS).<br />
Materials and methods: Data were collected<br />
from hospital pharmacies for the period of 2009-<br />
2011. The drug utilisation in GHZ was expressed<br />
in DDD/100 bed-days (BD) and in KCUS was<br />
expressed in number of tablets/pills.<br />
Results: In the observed period, the utilisation<br />
of fibrinolitc drugs (alteplaze, streptokinase) in<br />
GHZ was negligible which correlates with development<br />
of interventional cardiology there.<br />
The low-molecular weight heparins utilisation<br />
was quite high. Looking at the ATC groups, the<br />
most used beta blocker was atenolol, lacidipine<br />
among Ca-channel antagonists, isosorbidemononitrate<br />
among nitrates, ramipril among<br />
ACE-inhibitors, losartan among sartans, atorvastatin<br />
among statins, amiodaron among antiarrythmics,<br />
methyldigoxin among inotropic drugs<br />
and furosemide among diuretics. In KCUS the<br />
most used drugs were: carvedilol among betablockers,<br />
amlodipine among Ca-channel antago-<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 7.6.<br />
nists, glyceril-trinitrate among nitrates, lisinopril<br />
among ACE-inhibitors, atorvastatin among<br />
statins, amiodarone among antiarrhytmics,<br />
methyldigoxin among inotropic drugs and furosemide<br />
among diuretics. The utilisation of streptokinase<br />
is still stable and alteplaze utilisation is<br />
increasing. The sharp growth of enoxaparine was<br />
observed as well.<br />
Conclusion: Because the data from GHZ and<br />
KCUS were collected using different methodologies,<br />
their comparison was quite difficult. Nevertheless,<br />
the data are showing trends in CV drugs<br />
utilisation in both institutions, which are preconditioned<br />
by type and number of procedures<br />
in patient treatment, tradition, economic factors<br />
as well as the influence of pharmaceutical companies.<br />
According to the principles of evidence<br />
based medicine, the utilisation of beta-blockers<br />
and Ca-channel antagonists in KCUS is optimal<br />
as well as the utilisation of ACE-inhibitors, sartans<br />
and nitrates in GHZ. In other ATC groups<br />
there is no difference among hospitals and most<br />
used drugs are the optimal ones. Our analysis<br />
indicates the differences in CV drugs utilisation<br />
among two hospitals which could be better explained<br />
by using unique methodology.<br />
41
PL 8.1.<br />
DIFFERENTIAL DIAGNOSIS OF CLEAR CELL TUMORS<br />
Nenad Vanis 1 , Rusmir Mesihović 1 , Aida Saray 1<br />
1 Clinical Center University of Sarajevo, Sarajevo,<br />
Bosnia and Herzegovina<br />
Many diseases are associated with loss of appetite<br />
or inability to ordinary intake food. The<br />
consequence of long-term or even short –term<br />
inability to intake food leads to the damage of<br />
tissue and organ function. Loss of tissue, which<br />
is accelerated through metabolic effects of inflammatory<br />
mediators, is a feature that is identified<br />
as a clinical malnutrition. The aim of this paper<br />
is to offer a major guide for malnutrition risk<br />
detection, proposing several standards that are<br />
practical for general use in patients and healthcare<br />
workers.<br />
Methodology and subjects: This systematically<br />
planned, descriptive, two years (2008 to 2010)<br />
prospective clinical study included a total of<br />
2200 patients hospitalized in the Clinical Center<br />
of the University Sarajevo. Subjects were hospitalized<br />
patients with clear diagnose who came<br />
for assessing the nutritional status and prevalence<br />
of hospital malnutrition.<br />
Results: According MUST test malnutrition<br />
was detected in 58%, and the test relies more<br />
42 Proofreading and translations are in the explicit responsibility of the authors.<br />
on subjective assessment of the patient and is<br />
not acceptable for general screening. According<br />
to NRS 2002 test, malnutrition was detected<br />
in total of 52.04% patients who were placed in<br />
other clinics. This test is convenient because the<br />
answers with formulation as “yes” or “no” are<br />
acceptable for the patient and final screening is<br />
simple. According to the MNA test malnutrition<br />
is detected in total of 55.3% patients but the<br />
test is not suitable because answers are more subjective<br />
and not acceptable for the patient as well<br />
as for physician.<br />
Conclusion: More than 55% subjects were detected<br />
as proven clinical malnutrition with all<br />
three tests. The greatest risk of malnutrition<br />
among internal medicine diseases have oncologic<br />
patients. BMI should be routinely done on the<br />
first examination. NRS 2002 test is suitable and<br />
acceptable tfor patient.<br />
Keywords: Prevalence, Hospital malnutrition,<br />
screening
Modelling the European Burden of Disease Associated Malnutrition<br />
András Inotai 1 , Mark Nuijten 2 , Eric Roth 3 , Refaat Hegazi 4 , Zoltán Kaló 1,5<br />
1 Syreon Research Institute, Budapest, Hungary<br />
2 Ars Accessus Medica; Erasmus University<br />
Rotterdam, Rotterdam, Netherlands<br />
3 Department of Surgery, Medical University of<br />
Vienna, Vienna, Austria<br />
4 Abbott Nutrition, Columbus, Ohio, USA<br />
5 Eötvös Loránd University, Budapest, Hungary<br />
Background: Disease associated malnutrition<br />
(DAM) is a frequent but often unrecognised<br />
problem, even in the developed world. DAM is<br />
associated with increased morbidity, number<br />
and severity of complications arising from the<br />
primary disease and, consequently, increased<br />
utilisation of health care services and decreased<br />
quality of life (QoL).<br />
Objective: To estimate the health and economic<br />
burden of DAM in Europe.<br />
Design: An Excel spreadsheet model was developed<br />
to estimate direct incremental health care<br />
costs and health burden (including increased<br />
mortality and reduced QoL expressed in lost<br />
quality adjusted life years [QALYs]). The monetary<br />
value of health loss was calculated by multiplying<br />
lost QALYs with explicit or implicit cost<br />
effectiveness thresholds. Ten primary diseases<br />
were incorporated into the model: stroke, coronary<br />
heart disease, breast cancer, colorectal cancer,<br />
head and neck cancer, chronic obstructive<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 8.2.<br />
pulmonary disease, dementia, depression, musculoskeletal<br />
disorders and chronic pancreatitis.<br />
Results: The direct financial burden of DAM is<br />
over 31 billion EUR annually. DAM is responsible<br />
for 5.7 million lost life years and 9.1 million<br />
QALYs. The total monetary value of health<br />
and financial burden of DAM exceeds 305 billion<br />
EUR in ten primary diseases. Conclusions:<br />
In Europe, DAM is a considerable health and financial<br />
burden and represents a significant contribution<br />
to the total burden of disease, estimated<br />
by World Health Organization to be 255 million<br />
disability adjusted life years (DALYs) annually in<br />
Europe. The model highlights the necessity and the<br />
importance of further economically relevant studies<br />
in the medical nutritional area as potential inputs<br />
for future economic models. Therefore, policy<br />
makers should support programmes to extend the<br />
clinical and economic evidence base of nutritional<br />
care, with the ultimate aim of reducing the resource<br />
burden associated with malnutrition.<br />
43
PL 8.3.<br />
From Morisky to Hill-Bone: measurement of adherence to medication<br />
Josip Čulig, Marcel Leppee<br />
Andrija Stampar Institute of Public Health, Zagreb,<br />
Croatia<br />
Goal: Adherence to medication is measured in<br />
several ways.<br />
Materials and Methods: Direct methods include<br />
measuring the concentration of drug or metabolite<br />
in the body (blood, urine, biological markers)<br />
and those are the most accurate, but also<br />
very expensive and complex. Therefore, the most<br />
commonly used indirect methods are patient<br />
and clinician report, pill counting system, electronic<br />
medication monitors, rates of prescription<br />
refills, patient diaries and patient self-reports or<br />
questionnaires as the most important ways of<br />
measuring adherence. Self-report measures have<br />
the benefits of being cheap, easy to administer,<br />
non-intrusive, and able to provide information<br />
on attitudes and beliefs about medication. Potential<br />
limitations to self-report are that ability<br />
to understand the items, and willingness to disclose<br />
information can affect response accuracy<br />
and thus questionnaire validity.<br />
Results: The best known and most widely usable<br />
scale for research adherence is MAQ (Medication<br />
Adherence Questionnaire) by Morisky,<br />
which has several advantages: identifies barri-<br />
44 Proofreading and translations are in the explicit responsibility of the authors.<br />
ers to nonadherence, is the shortest scale, easiest<br />
to score and very adaptable for various groups<br />
of medication. SEAMS (Self-Efficacy for Appropriate<br />
Medication Use Scale) is a 13-question<br />
scale, more complex than the previous one.<br />
BMQ (Brief Medication Questionnaire) consists<br />
of four main question headings (regimen, belief,<br />
recall and access screen) and multiple subquestions.<br />
MARS (Medication Adherence Rating<br />
Scale) is a 10-question scale focused mainly on<br />
psychiatric populations. ARMS (Adherence to<br />
Refills and Medication Scale) is a valid and reliable<br />
medication adherence 14-question scale<br />
when used in a chronic disease population, with<br />
good performance characteristics even among<br />
low-literacy patients. The Hill-Bone Compliance<br />
Scale address barriers and self-efficacy and<br />
focuses on hypertensive patients. Some scale are<br />
modified depending on the disease or kinds of<br />
medication.<br />
Conclusion: No gold-standard medication adherence<br />
scale exists, but MAQ is most adaptable<br />
at the point of care and across populations.
The cost of diabetes mellitus in Macedonia<br />
Donka Pankov, Zoran Sterjev, Ljubica Suturkova<br />
ISPOR-Skopje, regional ISPOR chapter from<br />
Republic of Macedonia, Skopje, Macedonia<br />
Diabetes as a chronic disease is associated with<br />
economic and social influence on the health system.<br />
The aim of our study was to estimate the direct<br />
cost of providing health care to patients with<br />
Diabetes in R.Macedonia, to asses the economic<br />
impact of complications on the costs of diabetes<br />
and costs for treatment of diabetes and other<br />
unrelated health costs.The costs of diabetes and<br />
its complication were obtained retrospectively<br />
as an economic evaluation which derived costs<br />
from national DRG values and from official price<br />
lists for outpatient care in Macedonia.Тhere<br />
are 23 Medical Diagnostic categories (MDC)<br />
which are used by Macedonian Health Insurance<br />
Found (FZO). The annual costs caused by<br />
diabetes patients in Macedonia in 2010, which<br />
includes inpatient treatment and medication, is<br />
approcsimately 15 million Euros. The ambulato-<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
PL 8.4.<br />
ry treatment, laboratory and the other costs are<br />
not included. Diabetes medication (insulin, oral<br />
antidiabetic drugs) accounted to 8,79 million euros,<br />
hospital costs amount to 5,5 million euros<br />
in 2010 and 6,23 million in 2011. The analysis<br />
of the costs for 2010 and 2011 show that 50%<br />
of the total costs are allocated for treatment of<br />
CVC, 12% are allocated for treating direct moderate<br />
and severe complication of diabetes (ketoacidosies<br />
and etc), 10% are due to stroke and the<br />
other complication of the nervous system, 3% of<br />
the costs are related with kidney complications,<br />
2% for eye complications, 4% for diabetic foot<br />
and the rest of the costs are related with the other<br />
17 MDC. In conclusion, diabetes has a high costs<br />
to society. Because of the high cost of treating<br />
diabetes and its complications, preventive measures<br />
should be implemented.<br />
45
PL 8.5.<br />
Cost-Effectiveness of Interventions to Control Diabetes Mellitus and<br />
Prevent Complications<br />
Terezija Šarić, Tamara Poljičanin, Željko Metelko<br />
Promeritus savjetovanje d.o.o., Zagreb, Croatia<br />
Objective: To estimate the incremental cost-effectiveness<br />
of intensive glycemic control (relative<br />
to conventional control), intensified hypertension<br />
control and reduction in serum cholesterol<br />
level for patients with type 2 diabetes.<br />
Methods: In the Markov framework, a series of<br />
patient cohorts diagnosed as having diabetes<br />
progressed through the model. The model is<br />
based on the assumption that the natural history<br />
of type 2 diabetes and its complications<br />
and comorbidities can be described by a series<br />
of discrete health states that represent the microvascular<br />
and neuropathic complications of<br />
type 2 diabetes (retinopathy, nephropathy, and<br />
neuropathy) and the two major comorbidities<br />
(stroke and coronary heart disease). Cohorts<br />
were followed-up along the disease paths for 10<br />
years. Health resource use and associated medical<br />
costs are analyzed by type of diabetes complication<br />
and health resource category.<br />
Results: Based on use of resources driven by trial<br />
protocol, the incremental cost-effectiveness of<br />
46 Proofreading and translations are in the explicit responsibility of the authors.<br />
intensive glycemic control, intensified hypertension<br />
control and reduction in serum cholesterol<br />
level was cost saving. Although the standard<br />
treatment cost increased moderately, the complications<br />
cost dropped significantly. Over 10<br />
years, average undiscounted total savings for<br />
direct medical costs were estimated to be 273,5<br />
mil EUR. Interventions directly affected cumulative<br />
incidence of complications by reducing the<br />
transition probabilities for complications. A very<br />
large proportion of the reduction in direct medical<br />
cost was attributable to a decrease in hospitalization<br />
expenditure. For patients with stroke and<br />
coronary heart disease hospitalization represents<br />
the largest proportion of total cost.<br />
Conclusion: This study has confirmed that better<br />
disease monitoring and complication prevention<br />
would save substantial resources. Economic data<br />
on the costs of diabetes are essential to motivate<br />
decisions that can reduce the national burden of<br />
the disease and to optimize resource allocation.
Symptomatic therapy for cold and flu – Macedonian case 2011<br />
Stevce Acevski 1 , Vladimir Indov 1 , Zoran Sterjev 2 , Rubin Zareski 2<br />
1 Alkaloid AD Skopje Macedonia<br />
2 Faculty of Pharmacy, Skopje, Macedonia<br />
Market of pharmaceutical products for treatment<br />
of cold and fly in R. Macedonia as globally,<br />
increases in its volume of sales. In this study<br />
we evaluated the utilization of combination of<br />
the products for cold and fly, prepared in form<br />
of sachets, ready for preparing hot or cold drink,<br />
with major recommendations 48 – 72 hours<br />
treatment, taken every 6 – 8 hours. We analyzed<br />
utilization of following combinations: 500<br />
mg acitysalicilic acid plus 30 mg pseudoefedrin<br />
registered and marketed since 2009, 1000 mg<br />
paracetamol and 12.2 mg phenylephrine hydrochloride<br />
registered and marketed since 2010, and<br />
500 mg paracetamol, 25 mg feniramine maleat<br />
and 200 mg ascorbic acid with additional forms<br />
with same active ingredients but without sugar<br />
registered and marketed for more than 10 years.<br />
The sale of the three top brand products in 2011<br />
showed that 4.042.780 doses of combined prod-<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
P 01<br />
ucts for symptomatic therapy products were sold<br />
or by the recommendation almost 500.000 times<br />
Macedonian patients treated itself with combine<br />
therapy for relieve of symptom’s of cold and fly.<br />
This is almost 25% of all population. Market<br />
share of the evaluated three products were as follows:<br />
500 mg acitysalicilic acid plus 30 mg pseudoefedrin<br />
0.71%, 1000 mg paracetamol and 12.2<br />
mg phenylephrine hydrochloride 33.39% and<br />
500 mg paracetamol, 25 mg feniramine maleat<br />
and 200 mg ascorbic acid with 65.90 %.<br />
We could conclude that 500 mg paracetamol,<br />
25 mg feniramine maleat and 200 mg ascorbic<br />
acid dominated on the market of pharmaceutical<br />
products for symptomatic treatment of cold<br />
and fly, but 1000 mg paracetamol and 12.2 mg<br />
phenylephrine hydrochloride rapidly increases<br />
its sales and builds up its market share, and treats<br />
dominating position.<br />
47
P 02<br />
Economic evaluation of decreasing persistant hypertension with renal<br />
denervation device cutting costs of hypertension commorbidities in<br />
upcoming Croatian practice<br />
Vanesa Benković 1 , Ranko Stevanović 1 , Ana Ivičević 1 , Marko Matulović 2 ,<br />
Bojan Jelaković 3<br />
1 Croatian Society for Pharmacoeconomics and<br />
Health Economics Zagreb, Croatia<br />
2 Medtronic Zagreb, Croatia<br />
3 Department for nephrology and arterial<br />
hypertension, Clinical Hospital Centre Zagreb,<br />
Croatia<br />
Goal: to assess cost saving of decrease in persistant<br />
hypertension using renal denervation, a<br />
novel a catheter-based procedure<br />
Materials and Methods: using RCT data on decreasing<br />
commorbidities of hypertension and<br />
Framingham risk score a model is set to establish<br />
and structure cost in cardiovascular, cerebrovascular<br />
and renal commorbidities. Cost savings in<br />
commorbidities is assessed in Croatian setting<br />
using current prices and DRG tariffs. Epideimology<br />
data is taken from existing research such as<br />
registries and Croatian Health Survey.<br />
Results and Conclusion: Hypertension is a<br />
major risk factor for stroke, ischemic heart disease,<br />
heart failure, end stage renal disease and<br />
peripheral arterial disease. Renal denervation<br />
with the Symplicity Catheter System is a new<br />
catheter-based procedure for treatment-resistant<br />
48 Proofreading and translations are in the explicit responsibility of the authors.<br />
hypertension. Treatment-resistant hypertensive<br />
patients currently have no additional treatment<br />
options; they represent a significant unmet clinical<br />
need. Using one time renal denervation may<br />
significantly decrease systolic blood presure<br />
(SBP) - up to 32 mmHG SBP in six months, with<br />
sustainable effect. Decreasing the SBP is associated<br />
with decrease in incidence of ischaemic<br />
heart disease, renal failure, cerebrovascular insult<br />
and correlated mortality. As they all negatively<br />
impact quality of life they also increase the<br />
economic burden of the disease. The novel renal<br />
denervation procedure brings excellent options<br />
for unmet need in persistant hypertension and<br />
decreases cost in hospitalizations, drugs and rehabilitation<br />
from the budget holder and the hospital<br />
perspective.
Codiffication as a method in research on animal models in<br />
pharmacoeconomical efficiency<br />
Iris Broman<br />
School of Medicine Osijek, Osijek, Croatia<br />
Contemporary research on animal models embraces<br />
a wide pallet of models, research approaches<br />
and subjects of interests. In order to<br />
improve the insight of the results of these activities<br />
and reduce repetitions or mistakes during<br />
the process, rationalize the need of the animal<br />
use, we recommend codification as a method in<br />
the practical approach. Codification can be reduced,<br />
by certain definition, to the formal method<br />
in legislative techniques, that can be separated<br />
from legal authorities. On the other side, there is<br />
no use in gathering data and regulations unless<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
P 03<br />
they are placed in the practical order and if they<br />
are not fulfilling each other with means of purpose.<br />
(If the codification gets applied unsightly,<br />
it makes the base of a quality management). Research<br />
on animal models is conducted globally.<br />
Besides the rigid definition of science, it enters<br />
the field of the global economy, international<br />
legislation, environment protection and others.<br />
Codification, as a method, helps the variety of<br />
groups of interests, more organized, easier and<br />
practical link.<br />
49
P 04<br />
The role of pharmacoeconomics in medicines reimbursement decisionmaking<br />
in Bosnia and Herzegovina<br />
Tarik Čatić, Igor Martinović, Begler Begović<br />
Society for Pharmacoeconomics and Outcomes<br />
Research in Bosnia and Herzegovina - ISPOR BH<br />
Regional Chapter, Sarajevo, Bosnia and Herzegovina<br />
Goal: Pharmacoeconomics is relatively new concept<br />
for Bosnia and Herzegovina health care decision<br />
makers. Education in this field is not sufficient,<br />
and it ismain reason for lack of experts in<br />
this field. Decision on reimbursement of medicines<br />
and other technologies are made on different<br />
levels due to decentralised health system<br />
and by different stakeholders (Entities/Cantonal<br />
Health Insurance Funds-HIF, Hospitals, Ministries<br />
of Health-MoH). Objective of this survey<br />
was skreening of current situation and understanding<br />
of pharmacoeocnomics principles,<br />
process and implementation in decision making<br />
proces among key stakeholders.<br />
Materials and Methods: A nine-question survey<br />
has been distibuted to 50 stakeholders involved<br />
in reimbursement decisions. Survey include<br />
questions on current process of reimbursement<br />
decisions, existance of pharmacoeconomic criteria,<br />
and reasons for de-listing of reimbursed<br />
medicines with two months deadline.<br />
Results and Conclusions: Overall response rate<br />
was 30%; 50% (6/12) of MoH, 42% (5/12) HIFs<br />
50 Proofreading and translations are in the explicit responsibility of the authors.<br />
and 17% (4/24) Hospitals respond. 73% respondents<br />
use criteria for decisions on drug reimbursement.<br />
Mostly used criteria are expert opinions<br />
(47%) and pharmacoeconomic studies provided<br />
by the manufacturer (40%), 33% base decision<br />
on price. Most of respondents use mixed<br />
criteria. Official bodies in form of commission<br />
are established in 7 institutinons, mostly in MoH<br />
and HIFs. This bodies consist of physitians and<br />
pharmacists, and only 2 of respondents include<br />
economicst into these bodies. Similar situation<br />
is observed in case od medical devices and<br />
other technologies reimbursement decisions.<br />
De-listing is recorded in 40% respondents but<br />
main reason was production discontinuation.<br />
Although the response rate is low, it allows conclusions<br />
that correlate with the experience and<br />
current practices. There is a need for a systematic<br />
approach to HTA and adoption of clearer criteria<br />
for reimbursement decision-making. Establishing<br />
HTA bodies consisted of trained professionals<br />
would improve the reimbursement decisions<br />
and make it more transparent.
Evaluation of utilization of old versus newer antiepileptic drugs in Republic<br />
of Macedonia<br />
Bojana Danilovska, Zoran Sterjev, Ljubica Suturkova<br />
ISPOR –Skopje, regional ISPOR chapter from<br />
Republic of Macedonia, Skopje, Macedonia<br />
Goal: New, ‘second generation’ antiepileptic<br />
drugs (AEDs) which have entered the marketplace<br />
since 1990 are currently taken by approximately<br />
16% of patients with epilepsy worldwide.<br />
Concerning the efficacy of these drugs in comparison<br />
to the older ones, they are generally<br />
considered to have equal efficacy. In some conditions<br />
are slightly more efficacious but the differences<br />
in price are still very big. In the present<br />
study we evaluated and compared utilization and<br />
cost of “old” and “newer AEDs” which are present<br />
in reimbursement drug list in R.Macedonia,<br />
for the period 2009-2010.<br />
Materials and methods: We used official data obtained<br />
from Health Insurance Found of Republic<br />
of Macedonia (FZO) and defined daily dose<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
P 05<br />
(DDD), as a method for drug use evaluation,<br />
defined by WHO Collaborating Centre for Drug<br />
Statistics Methodology.<br />
Results: Carbamazpine (CBZ) was commonly<br />
prescribed antiepileptic drug in comparison with<br />
other AEDs (0,00053DDD/1000 people per day<br />
in 2009 and 0,00074 DDD/1000 people per day<br />
in 2010). The FZO cost for AEDs 2009 v.s. 2010<br />
was: 268915 v.s. 278257 euros for CBZ, 314821<br />
v.s. 365101euros for Valproic acid (VAL), 116433<br />
v.s. 100361 euros for Lamotrigine and 313522 v.s.<br />
184875 euros for Topiramate.<br />
Conclusion: The trend of utilization of the standard<br />
AEDs in Macedonia showed that the old<br />
AEDs are stiil therapy of choice for treatment of<br />
epilepsy.<br />
51
P 06<br />
DEMENTIA- can forgetfulness be significant social issue?<br />
Vedran Đukić 1 , Nenad Bogdanović 2<br />
1 Pfizer Croatia, Zagreb, Croatia<br />
2 Pfizer Primary Care Business Unit Europe, London,<br />
UK; Karolinska Institutet, Stockholm Sweden<br />
Goal: Our goal was to evaluate costs that are<br />
generated for diagnosis, treatment and care of<br />
dementia patients and are resources adequately<br />
allocated in Croatia and Bosnia Herzegovina<br />
comparing to the European Union countries.<br />
Materials and Methods: Data were collected<br />
from several available pharmacoeconomical<br />
analysis and epidemiological studies.<br />
Results: Diagnosis, treatment and care of dementia<br />
patients represent significant cost for<br />
every society, especially in highly developed and<br />
emerging countries.<br />
52 Proofreading and translations are in the explicit responsibility of the authors.<br />
Conclusion: Amount of money spent in EU<br />
countries is around 22.000€ per year and per<br />
patient, while in Croatia it is around 13.000€. In<br />
Bosnia and Herzegovina difference is even bigger.<br />
Based on current predictions, number of<br />
patients with dementias, including Alzheimer’s<br />
disease, will be tripled until 2050. Current disease<br />
awareness, early diagnosis, treatment and<br />
care options are not fully explored so there are<br />
still unmet needs for those patients which can<br />
improve quality of life and reduce costs.
Comparison of cost effectivenes of total hip and knee endoprotesis with and<br />
without prolonged thromboembolic prophylaxis<br />
Ismet Gavrankapetanović 1 , Faris Gavrankapetanović 1 , Mehmed Jamakosmanović 1 ,<br />
Slobodanka Bolanča 2<br />
1 Clinical Center University of Sarajevo, Sarajevo,<br />
Bosnia and Herzegovina<br />
2 Pfizer Croatia, Zagreb, Croatia<br />
Total hip (THR) and knee replacement (TKR)<br />
surgeries are known to be highly successful and<br />
cost effective treatments for degenerative joint<br />
diseases in large number of elderly patients who<br />
are at increased risk of deep venous thrombosis<br />
and venous thromboembolism (VTE), including<br />
pulmonary embolism (PE). VTE is one of the<br />
most common complications among patients<br />
undergoing orthopaedic surgery, and a leading<br />
cause of preventable mortality after elective orthopaedic<br />
surgery. In the absence of prophylaxis,<br />
it has been estimated that 40-60% of patients<br />
will develop venographically-detected deep vein<br />
thrombosis (DVT), seven to 14 days after major<br />
orthopaedic surgery. The overall mortality<br />
risk after hip arthroplasty has been reported as<br />
0.7% with a baseline risk of DVT in the absence<br />
of prophylaxis of 44% and an incidence of pul-<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
P 07<br />
monary embolism of 3%. Although the overall<br />
mortality is not as significant as that reported for<br />
THR with the incidence of fatal and non-fatal PE<br />
probably less than 1%, the baseline risk for DVT<br />
including asymptomatic DVT may be as high as<br />
60%.<br />
In this study in addition to clinical efficacy we<br />
also considered complications of VTE and its<br />
prophylaxis (e.g. bleeding, PE).<br />
Our findings and recommendations are consistent<br />
with those observed in scientific literature<br />
relevant health technology reports and have<br />
been included in our hospitals treatment guidelines:<br />
combination of mechanical and prolonged<br />
pharmacological treatment of patients at high<br />
risk for DVT and PE together with early mobilisation<br />
and discharge has been assessed to be the<br />
most cost efficient in terms of QALYs gained.<br />
53
P 08<br />
Human papillomavirus vaccination of boys: cost-effectiveness analysis<br />
Rok Hren<br />
University of Ljubljana, Ljubljana, Slovenia<br />
The objective of the study was to analyze costeffectiveness<br />
of a human papillomavirus (HPV)<br />
vaccination of boys at age 12 against oropharyngeal<br />
carcinoma and anogenital warts. Due to<br />
availability of the data, we applied the Markov<br />
model to the conditions of potential national<br />
immunisation program in the United Kingdom.<br />
Comparison of HPV vaccination of boys at age<br />
12 vs. no vaccination resulted in ICER exceeding<br />
100,000 GBP per QALY. The outcome was sensitive<br />
to the vaccination costs, the probability of<br />
developing oropharyngeal carcinoma and anogenital<br />
warts, and proportion of oropharyngeal<br />
carcinoma attributable to infection with types<br />
54 Proofreading and translations are in the explicit responsibility of the authors.<br />
HPV-16 and HPV-18. When comparing quadrivalent<br />
and bivalent vaccines, resulting ICER<br />
was 5,205 GPB per QALY. Our results indicate<br />
that HPV vaccination of boys with quadrivalent<br />
vaccine is at present deemed not cost-effective,<br />
i.e., ICER exceeds willingness-to-pay threshold<br />
of 30,000 GBP per QALY. Comparison of quadrivalent<br />
and bivalent vaccines revealed that the<br />
additional benefits of protection against anogenital<br />
warts would favour quadrivalent vaccine as<br />
the vaccination choice. An increase in incidence<br />
of HPV-positive oropharyngeal carcinoma and<br />
anogenital warts, and reduction of vaccination<br />
costs could substantially reduce ICER.
Cost-effectiveness of combined treatment of metformin and fenofibrate on<br />
retinopathy progression<br />
Rok Hren 1 , Radomir Cerovic 2<br />
1 University of Ljubljana, Ljubljana, Slovenia<br />
2 National Insurance Fund, Belgrade, Serbia<br />
Goal: To evaluate the cost-effectiveness of intensive<br />
glycemic control (metformin) combined<br />
with fenofibrate in its impact on retinopathy<br />
progression compared to the treatment with<br />
metformin only in patients with type 2 diabetes.<br />
Design: Markov decision model of retinopathy<br />
progression.<br />
Population: 40-year old patient with type 2 diabetes<br />
followed for 29 years.<br />
Main outcome measures: Risk of visual impairment;<br />
incremental cost-effeciveness ratio (ICER)<br />
for the two treatment options: one combining<br />
metformin and fenofibrate, and one using solely<br />
metformin.<br />
Results: Combined tretament of metformin and<br />
fenofibrate resulted in ICER of -133.06 GBP<br />
per QALY which means that the intervention is<br />
not only effective but is also potentially saving<br />
money to the National Health Service; tretament<br />
solely with metformin is therefore dominated.<br />
Conclusions: Results of our study suggest that<br />
patients suffering from type 2 diabetes will re-<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
P 09<br />
ceive from additional treatment with fenofibrate<br />
substantial benefits of protection against<br />
early microvascular complications related to<br />
retinopathy, including blindness. The favorable<br />
cost-effectiveness of intensive glycemic control<br />
combined with fenofibrate will likely be further<br />
increased if other major microvascular complications<br />
(e.g., non-traumatic amputations) and<br />
macrovascular complications (e.g., total cardiovascular<br />
events) of type 2 diabetes are taken into<br />
account.<br />
What this study adds? Our study is one of the<br />
first to compare cost-effectiveness of combined<br />
treatment of metformin and fenofibrate with<br />
current intensive glycemic control using solely<br />
metformin in its impact on retinopathy progression.<br />
Our study also provides evidence which<br />
may be useful in shaping the current clinical<br />
practice in the United Kingdom and European<br />
Union.<br />
55
P 10<br />
Evaluation of cost-saving of Clopidogrel pharmacogenetic testing in patient<br />
with atherotrombotic disorders from R. Macedonia<br />
Aleksandra Kapedanovska Nestorovska, Zorica Naumovska, Zoran Sterjev,<br />
Aleksandar Dimovski, Ljubica Suturkova<br />
Faculty of Pharmacy, Skopje, Macedonia<br />
The CYP2C19*2 variant is related with reduced<br />
clopidogrel therapy responsiveness in patients<br />
with atherotrombotic disorders (ATD), increased<br />
adverse cardiovascular event (ACE)<br />
rates, poorer cardiovascular outcomes and attenuated<br />
therapy benefits. The aim of this study<br />
is evaluation of the cost of CYP2C19*2 genetic<br />
testing for reducing the incidence of clopidrogel<br />
ACE rates in ATD patients from R. Macedonia. A<br />
total of 67 patients with ATD, treated with standard<br />
clopidogrel induction/maintenance therapy<br />
(600 mg/75 mg) were included in this study.<br />
All patients were randomized in to two patient’s<br />
subgroups: responders, N= 38 (57%) , who did<br />
not developed any ACE and non - responders<br />
group, N=29 (43%), who developed ACE during<br />
the follow up period. National hospital DRG<br />
discharge codes were used to determinate the<br />
costs of hospitalization for ACE during exposure<br />
56 Proofreading and translations are in the explicit responsibility of the authors.<br />
to clopidogrel therapy or after. The cost of PGx<br />
testing was calculated according to the standard<br />
protocols for CYP2C19*2 pharmacogenetic testing<br />
in the Center for biomolecular pharmaceutical<br />
analyses (CBMA) at the Faculty of Pharmacy<br />
in Skopje and is 50 euros/per patient. The cost<br />
of clopidogrel therapy per patient in R. Macedonia<br />
is approximately 390 EUR per year. The cost<br />
of ACEs related to therapy failure range from<br />
226 to 5910 EUR per patient depending on the<br />
type of ACE. Clopidogrel therapy cost for nonresponder<br />
patient group in our study was 3510<br />
EUR. Additionally, estimation of 6554 EUR is<br />
the minimal cost of hospital treatment for nonresponder<br />
patients. Using PGx testing will allow<br />
us to predict the treatment phenotype of patients<br />
and the cost of those analyses in our group of 67<br />
patients is estimated to be 3350 EUR. The use of<br />
this genetic testing is economically justified.
Influence of increased linezolid utilisation on development of antimicrobial<br />
resistance to linezolid<br />
Aleksandar Knežević 1 , Sanja Sarić-Kužina 2 , Ivanka Matas 3<br />
1 General Hospital Zadar, Zadar, Croatia<br />
2 Pfizer Croatia d.o.o., Zagreb, Croatia<br />
3 Institute of Public Health, Zadar, Croatia<br />
Goal: Our goal was to evaluate the influence of<br />
increased linezolid utilisation on the development<br />
of resistance to the drug in General Hospital<br />
Zadar.<br />
Materials and Methods: Data were collected from<br />
hospital pharmacy and microbiology laboratory<br />
for the period of 2005-2011. The utilisation of linezolid<br />
in GHZ was expressed in DDD/100 beddays<br />
(BD). The susceptibility of MRSA, MSSA,<br />
Pneumococcus and Enterococcus isolates to linezolid<br />
was tested regularly.<br />
Results: In the period from 2005-2011, the utilisation<br />
of linezolid increased from 0.002 to 0.353<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
P 11<br />
in DDD/100 BD, i.e. 176 times, but at the same<br />
time resistance to linezolid was not observed.<br />
Conclusion: Although resistance to linezolid had<br />
been rarely reported in literature, our evaluation<br />
confirms that in spite of huge increase in utilisation<br />
of linezolid, this drug remains the reliable<br />
therapy of infections caused by susceptible bacteria.<br />
The fact that linezolid was all the time on<br />
the list of “reserve antibiotics” probably contributes<br />
to this. It shows also that the use of relatively<br />
expensive drug can be cost-effective because it<br />
enables effective therapy without or very small<br />
possibility of failure.<br />
57
P 12<br />
Institutional and normative framework of drug control costs in the<br />
Republic of Macedonia<br />
Kostadinka Kozareva, Ana Petrovska Angelovska<br />
Bayer doo Ljubljana, Representative office Skopje,<br />
Skopje, Macedonia<br />
One of the main goals of every healthcare system<br />
is to provide quality, timely and accessible<br />
healthcare services for the population. The analyzis<br />
show that health and pharmaceutical costs<br />
in the last 30 years grow significantly more than<br />
GDP growth. And therefore there is a need for<br />
effective control of health care and pharmaceutical<br />
costs by payers for healthcare and pharmaceutical<br />
services.<br />
Goal: The goal of the paper is to make analysis<br />
of institutional and normative framework as an<br />
important prerequisite for the implementation<br />
of the specific model of control mechanisms of<br />
drug costss.<br />
Material and methods: This study used several<br />
methods: the historical method, used to analyze<br />
the historical development of pharmacoeconomic<br />
theory and practice in the Republic of<br />
Macedonia; normative method is applied in research<br />
and analysis of the legal framework upon<br />
58 Proofreading and translations are in the explicit responsibility of the authors.<br />
which to realize the essence of individual control<br />
mechanisms of drug costs, content analysis<br />
is used as a method of research which wants to<br />
build a systematic record of experienced communication<br />
as one aspect of social life.<br />
Results: The analysis shows that in recent years<br />
Republic of Macedonia has introduced a number<br />
of normative solutions by which there have been<br />
implemented numerous control mechanisms of<br />
drug costs.<br />
Conclusion: From the analysis of the established<br />
control mechanisms for drug costs in the RM,<br />
we can conclude that Macedonia in the past few<br />
years has achieved considerable success with the<br />
implementation of a series of control mechanisms,<br />
which led to a significant reduction in<br />
drug costs, but there is still open room for further<br />
improvement of the existing model in order<br />
to increase the quality of care and to protect citizens<br />
from the additional financial costs.
Antidiabetic drug expenditure in Bosnia and Herzegovina - 2009/2010<br />
Jasmina Krehic 1 , Zelija Velija Asimi 2<br />
1 Department for Clinical Pharmacology, Clinical<br />
Centre of the University Sarajevo, Sarajevo, Bosnia<br />
and Herzegovina<br />
2 Clinic for Endocrinology and Diabetes, Clinical<br />
Centre of the University Sarajevo, Sarajevo, Bosnia<br />
and Herzegovina<br />
Objective: To compare drug expenditure for diabetes<br />
in Bosnia and Herzegovina (B&H) comparing<br />
years 2009 and 2010.<br />
Methods: Research was based on data published<br />
in latest official annual reports from national<br />
Drug Agency of B&H and official reports from<br />
The World Bank. Analysis was performed for all<br />
available drugs from ATC A10 group. ATC A10<br />
groups from 2nd to 5th level were identified, calculated<br />
and compared between two years – 2009<br />
and 2010.<br />
Results: In 2009, total drug expenditure in<br />
B&H was 238.852.446,5 EUR compared to<br />
269.015.061,8 EUR in 2010 (increase of 11,2%).<br />
A10 group was at high, fifth place in total drug<br />
expenditure with 12.512.110,6 EUR (5,24%)<br />
share in 2009 and in 2010 A10 group moved<br />
up at third place in (total) with 19.900.252,8<br />
EUR share (7,4%). Portion of A10A group at<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
P 13<br />
3rd ATC level of total antidiabetic drug expenditure<br />
was 7.531.246,9 EUR (60,2%) and A10B<br />
was 4.980.863,7 EUR (39,8%) in 2009 (ratio<br />
A10A:A10B = 1,5) while in 2010 that ratio was<br />
14.291.116,5 EUR (71,8%) for A10A group and<br />
5.609.136,3 EUR (28,2%) for A10B group, 2,5<br />
respectively. In the same time GDP in B&H decreased<br />
from 17 billion US$ in 2009 to 16,5 billion<br />
US$.<br />
Conclusion: Our results show that total drug expenditure<br />
in B&H significantly increased in 2010<br />
year with regard to 2009 as well as total drug<br />
expenditure for diabetes. Some changes can be<br />
explained with withdrawal of some A10A and<br />
A10B group drugs from market, but such alarming<br />
increase of antidiabetic drug expenditure requires<br />
attention of all health authorities regarding<br />
development of national diabetes guidelines.<br />
59
P 14<br />
Cost effectiveness of renal sympathetic denervation in patients with<br />
refractory hypertension: decision modelling of applicability for Croatian<br />
health care<br />
Robert Likić, Ksenija Makar Aušperger, Viktorija Erdeljić, Matea Radačić Aumiler,<br />
Igor Francetić, Bojan Jelaković<br />
University Hospital Center Zagreb, Zagreb, Croatia<br />
Goal: Renal sympathetic hyperactivity contributes<br />
to the severity of hypertension and significantly<br />
determines treatment resistance, accelerating<br />
clinical course and increasing risk of<br />
stroke,, heart failure, myocardial infarction and<br />
chronic kidney disease. Catheter based renal<br />
sympathetic denervation (RSD) has recently<br />
been shown to effectively reduce blood pressure<br />
in up to 84% patients with refractory hypertension.<br />
We assessed decision modelling scenarios<br />
for cost effective application of this novel therapeutic<br />
method in Croatian health care.<br />
Materials and methods: Data regarding the prevalence<br />
of complications of hypertension were<br />
collected from the literature. Costs of hospital<br />
treatments and pharmacotherapy were obtained<br />
from the Croatian Institute’s for Health Insurance<br />
online Cezih and DTS gruper databases as<br />
well as the Institute’s online drug lists. Pricing for<br />
the RSD catheter electrodes was provided by the<br />
supplier. TreeAge Pro 2011 software suite was<br />
used for decision modelling.<br />
Results: Two decision three models were constructed.<br />
The first compared the cost effective-<br />
60 Proofreading and translations are in the explicit responsibility of the authors.<br />
ness of standard care with associated complications<br />
of refractory hypertension with that of the<br />
RSD. The second model additionally took into<br />
account the costs associated with rehabilitation<br />
and diminished quality of life following debilitating<br />
events caused by refractory hypertension.<br />
Both scenarios suggest RSD is not immediately<br />
cost effective, however depending on the model,<br />
it should be considered in patients with treatment<br />
resistant hypertension lasting between 2.5<br />
years (model 2) and/or 7 years (model 1).<br />
Conclusion: Catheter based renal sympathetic<br />
denervation can safely be used to substantially<br />
reduce blood pressure in treatment-resistant hypertensive<br />
patients. Based on current pricing of<br />
equipment for RSD and on the performed modelling,<br />
this new therapeutic approach should be<br />
considered in patients with treatment resistant<br />
hypertension lasting between 2.5 years (model<br />
2) and/or 7 years (model 1). Our results confirm<br />
that RSD should be indicated only in truly resistant<br />
hypertensives, and decision should be made<br />
only by experienced hypertensiologists.
The frequency of administration of antipsychotics, anxiolytics and<br />
antidepressants: description study<br />
Svjetlana Loga-Zec 1 , Damir Celik 2 , Faris Gavrankapetanović 2 , Jasmina Krehić 2 ,<br />
Mensura Aščerić 3 , Nedžad Mulabegović 1<br />
1 Institute of Pharmacology, Clinical Pharmacology<br />
and Toxicology, Faculty of Medicine, University of<br />
Sarajevo, Bosnia and Herzegovina<br />
2 Clinical Centre of the University Sarajevo, Bosnia<br />
and Herzegovina<br />
3 Department for pharmacology and toxicology,<br />
Faculty of Medicine, University of Tuzla, Bosnia and<br />
Herzegovina<br />
Goal: To determine the frequency of administration<br />
of antipsychotics, anxiolytics and antidepressants<br />
at the Clinical Center University of<br />
Sarajevo (KCUS), within the Mental Health Care<br />
Policy in the Federation of Bosnia and Herzegovina.<br />
Materials and methods: A retrospective study<br />
was conducted for the period 2009-2011 and as<br />
a source of data we used databases of Pharmacy<br />
of KCUS. The descriptive statistics was used,<br />
counts and percentages were reported. Statistical<br />
analysis was performed by using the SPSS 19.0<br />
software.<br />
Results: The total number of administrated antipsychotics<br />
in 2009 was 33 637, in 2010 and 2011<br />
was higher (59 593 and 54 973; respectively).<br />
The most commonly administered antipsychotics<br />
were: haloperidol (24.9%), sulpiride (24.1%),<br />
promazine (20.4%), chlorpromazine (17.5%),<br />
levomepromazine (11.1%), risperidone (1.3%)<br />
and fluphenazine (0.7%). The total number of<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
P 15<br />
administrated anxiolytics in 2009 was 18 500,<br />
in 2010 and 2011 was twice higher (37 930 and<br />
40 910; respectively). Out of the total number of<br />
administrated anxiolytics, the most commonly<br />
administered were: midazolam (41.6%), nitrazepam<br />
(32.0%), alprazolam (22.6%), bromazepam<br />
(3.3%), and diazepam (0.5%). The total number<br />
of administrated antidepressants in 2009 was 14<br />
762, in 2010 and 2011 was almost twice higher<br />
(28 552 and 27 846; respectively). The most commonly<br />
administered antidepressants were: sertraline<br />
(32.5%), paroxetine (27.8%), fluoxetine<br />
(20.1%), amitriptiline (8.9%), clomipramine<br />
(8.2%), and maprotiline (2.5%).<br />
Conclusion: The rational usage of psychotropic<br />
medicines requires multiple strategies such as<br />
psychosocial interventions and the existence of<br />
Mental Health Care\’s policy formulation to define<br />
goals related to participation of patients and<br />
doctors in decision making processes in order to<br />
improve the usage of psychotropic medicines.<br />
61
P 16<br />
Financial impact of imported unapproved drugs on the hospital budget:<br />
example of the Children’s Hospital of the University Hospital Centre Rijeka,<br />
Croatia<br />
Vesna Rosović-Bazijanac, Jasenka Mršić-Pelčić, Dinko Vitezić<br />
University Hospital Centre Rijeka and University of<br />
Rijeka Medical School, Croatia<br />
Goal: The aim of our study is to analyse the financial<br />
impact on the hospital budget of imported<br />
drugs (“interventional import”), not approved<br />
in Croatia.<br />
Materials and methods: The data were collected<br />
from the Pharmacy of the Children’s Hospital<br />
of the University Hospital Centre Rijeka during<br />
2011. This is a hospital with120 beds, treating<br />
population to 18 years of age. Descriptive<br />
analyses were performed and the financial data<br />
are presented in Euros (€) regarding the whole<br />
amount of purchased drugs. We classified drugs<br />
into three groups i.e. the first group are drugs<br />
included on the Hospital drug list (HDL) of the<br />
Croatian National Health Insurance under a generic<br />
name, the second group are the necessary<br />
drugs which are not on the HDL, and in the third<br />
group are parenteral solutions which are now<br />
imported, but previously made in the Hospital<br />
Pharmacy.<br />
Results: The Children’s hospital treatment includes<br />
13.21% of drugs which are not approved,<br />
but are now imported as necessary for treatment<br />
and the total cost is 101,306.20 €. Top five drugs<br />
in the first group (35 in total) are asparaginase,<br />
62 Proofreading and translations are in the explicit responsibility of the authors.<br />
pulmonary surfactants, cefotaxime, cloxacillin<br />
and ampicillin and the total cost is 70,818.17 €,<br />
which is 9.24% of total costs. The second group<br />
includes 42 drugs (the first five are sodium phenylbutyrate,<br />
gonadorelin, nystatin, colistin and allergens<br />
for Prick testing) and the total cost was<br />
30,488.03 € (3.98% of total cost). The third group<br />
includes magnesium sulphate 20% (now 50%),<br />
glucose 25 and 50% (now 40%), sodium benzoate<br />
10% (now sodium phenylbutyrate), sodium<br />
chloride 5.84% (now 10%) and potassium chloride<br />
7.45%. Our analysis shows that the average<br />
price of the imported solutions is approximately<br />
ten times greater than the one we used to make<br />
in the Hospital Pharmacy.<br />
Conclusion: The results show that a considerable<br />
amount of money is spent on imported unapproved<br />
drugs, i.e. two monthly drug budgets of<br />
the Children’s hospital. The process of approval<br />
is probably expensive and the financial gain for<br />
pharmaceutical companies could not compensate<br />
it, but it is necessary to find a new way how<br />
to make this process easier and prices of imported<br />
drugs less costly (defined prices).
Malnutrition in Croatia – where are we today and why should we include<br />
societal perspective in measuring “burden of illness“?<br />
Ranko Stevanović 1 , Vanesa Benković 1 , Ana Ivičević 1 , Ivana Kolčić 2 ,<br />
Irena Rojnić Palavra 1<br />
1 Croatian Society for Pharmacoeconomics and<br />
Health Economics, Zagreb, Croatia<br />
2 Medical Faculty, University of Split, Split, Croatia<br />
Goal: to identify current status of health care related<br />
cost attributable to malnutrition in Croatia.<br />
To emphasize the importance of concealed societal<br />
costs in today’s budget holder perspective, to<br />
set platform model for estimating cost of illness<br />
in the region.<br />
Materials and methods: increasing efforts are being<br />
made to estimate the cost of malnutrition in<br />
many European countries including setting up<br />
costing structure based on co morbidities (oncology,<br />
palliative care, gastroenterology diseases),<br />
interviews with key opinion leaders, interviews<br />
with nurses for homecare and other care<br />
providers. Also, cost of illness methodology and<br />
interviewing stakeholders in malnutrition diagnostics<br />
should be used to assess present state and<br />
tackle societal costs.<br />
Results and conclusion: Malnutrition is common,<br />
yet under-recognized and under-treated<br />
condition in the community, in long-term care<br />
and in hospitals in Croatia. Untreated malnutrition<br />
has adverse effects on clinical outcomes<br />
Proofreading and translations are in the explicit responsibility of the authors.<br />
P 17<br />
including impaired gastrointestinal, cardiac, pulmonary,<br />
renal, skin, immune and mental function.<br />
In clinical practice, malnutrition delays<br />
recovery from illness or injury, causes muscle<br />
loss and weakening, increases risk for complications<br />
such as infections and pressure ulcers,<br />
predisposes to depression and reduced quality<br />
of life, and increases risk for death. Overall costs<br />
for health care can be 2-3 folds higher among<br />
malnourished patient compared to their nourished<br />
peers. To be able to fully account for cost<br />
of malnutrition in Croatia, a societal perspective<br />
should be maintained<br />
to enable true values and estimation of costs a<br />
holistic approach must be taken when considering<br />
economic evaluation. The costs may be incurred<br />
in one setting whilst the benefit appears<br />
in another sector.<br />
Further one implementation of ‘academic’ guidelines<br />
and national programs to indentify patients<br />
at risk is needed to achieve improved outcomes<br />
and optimal use of resources.<br />
63
PRVI BOSANSKO-HERCEGOVAČKI I DRUGI<br />
JADRANSKI KONGRES FARMAKOEKONOMIKE<br />
I ISTRAŽIVANJA ISHODA LIJEČENJA<br />
24. - 26. april 2012.<br />
Sarajevo, Bosna i Hercegovina<br />
Pokrovitelji kogresa su:<br />
Ministarstvo zdravlja Republike Hrvatske<br />
Ministar, Prof.dr. Rajko Ostojić, dr. med.<br />
Ministarstvo zdravstva Federacije Bosne i Hercegovine<br />
Ministar, Prof.dr.Rusmir Mesihović, dr.med.<br />
Ministarstvo zdravlja i socijalne zaštite Republike Srpske<br />
Ministar, Prof.dr.Ranko Škrbić, dr.med.
Zlatni sponzor<br />
PFIZER<br />
Brončani sponzori<br />
ELI LILLY NOVO NORDISK HEMOFARM<br />
Sponzor