Universal Newborn Hearing Screening introduced to NICU infants in ...
Universal Newborn Hearing Screening introduced to NICU infants in ...
Universal Newborn Hearing Screening introduced to NICU infants in ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
THE NEW ZEALAND<br />
MEDICAL JOURNAL<br />
Vol 117 No 1206 ISSN 1175 8716<br />
<strong>Universal</strong> <strong>Newborn</strong> <strong>Hear<strong>in</strong>g</strong> <strong>Screen<strong>in</strong>g</strong> <strong><strong>in</strong>troduced</strong> <strong>to</strong> <strong>NICU</strong><br />
<strong><strong>in</strong>fants</strong> <strong>in</strong> Canterbury Prov<strong>in</strong>ce, New Zealand<br />
Mark Flynn, Nicola Aust<strong>in</strong>, Traci Schmidtke Flynn, Rodney Ford, Liz Buckland<br />
Abstract<br />
Aims <strong>Universal</strong> <strong>Newborn</strong> <strong>Hear<strong>in</strong>g</strong> <strong>Screen<strong>in</strong>g</strong> (UNHS) is be<strong>in</strong>g implemented<br />
worldwide as an effective method of early identification of hear<strong>in</strong>g loss. The impact<br />
of delayed detection of sensor<strong>in</strong>eural hear<strong>in</strong>g loss is a major lifelong impairment. The<br />
aim of the study was <strong>to</strong> assess the feasibility of <strong>in</strong>troduc<strong>in</strong>g universal newborn hear<strong>in</strong>g<br />
screen<strong>in</strong>g over the 12-month period <strong>in</strong> the Neonatal Intensive Care Unit (<strong>NICU</strong>) at<br />
Christchurch Women’s Hospital, and <strong>to</strong> assess the costs, and resources required.<br />
Methods <strong>Universal</strong> <strong>Newborn</strong> <strong>Hear<strong>in</strong>g</strong> <strong>Screen<strong>in</strong>g</strong> was conducted over a 12 month<br />
period <strong>in</strong> the Neonatal Service of Christchurch Women’s Hospital. Throughout the<br />
implementation period, data were collected <strong>to</strong> moni<strong>to</strong>r and benchmark aga<strong>in</strong>st<br />
World’s best practice.<br />
Results Dur<strong>in</strong>g the 12 months of the study, 435 babies were screened for hear<strong>in</strong>g loss<br />
<strong>in</strong> the Neonatal Service at Christchurch Women’s Hospital. Of these babies, 19<br />
(4.37%) were referred for diagnostic ‘audi<strong>to</strong>ry bra<strong>in</strong>stem response’ ABR test<strong>in</strong>g <strong>to</strong><br />
confirm hear<strong>in</strong>g loss. Two babies were confirmed with hear<strong>in</strong>g loss, with only one<br />
baby exhibit<strong>in</strong>g a known risk fac<strong>to</strong>r for deafness. This resulted <strong>in</strong> a positive predictive<br />
<strong>in</strong>dex of 10.53%.<br />
Conclusions This study highlights that UNHS can be implemented efficiently and<br />
cost-effectively with<strong>in</strong> the Neonatal Service of a New Zealand Hospital. The results<br />
were consistent with best practice, and show the benefits of UNHS aga<strong>in</strong>st ‘at risk’<br />
screen<strong>in</strong>g. The ultimate success of this study will be <strong>in</strong> the implementation of UNHS<br />
across New Zealand.<br />
Early detection and management of hear<strong>in</strong>g loss is crucial for the developmental<br />
period for audi<strong>to</strong>ry, speech, and language acquisition. Numerous studies demonstrate<br />
that early diagnosis and <strong>in</strong>tervention (before 6 months of age) of hear<strong>in</strong>g impairment<br />
is effective <strong>in</strong> allow<strong>in</strong>g children with congenital hear<strong>in</strong>g loss <strong>to</strong> acquire age<br />
appropriate cognitive and spoken language skills. 1–4 In recent years, the technology<br />
and expertise has developed <strong>to</strong> allow screen<strong>in</strong>g <strong>to</strong> detect hear<strong>in</strong>g loss <strong>in</strong> newborn<br />
babies. Early detection will also lead <strong>to</strong> earlier fitt<strong>in</strong>g of advanced hear<strong>in</strong>g <strong>in</strong>struments<br />
comb<strong>in</strong>ed with <strong>in</strong>tensive services target<strong>in</strong>g communication development.<br />
Latest New Zealand figures for the year 2002 5 <strong>in</strong>dicate that the average age of<br />
detection of hear<strong>in</strong>g loss is 35 months. Unfortunately, these figures do not <strong>in</strong>dicate<br />
what percentage of children with hear<strong>in</strong>g impairment were hear<strong>in</strong>g impaired at birth.<br />
As 84% of permanent childhood hear<strong>in</strong>g impairment is evident at birth, we conclude<br />
that the vast majority of children (for whom permanent hear<strong>in</strong>g impairment was<br />
detected) have been hear<strong>in</strong>g impaired s<strong>in</strong>ce birth. Further <strong>in</strong>vestigation of the New<br />
Zealand Deafness notification data reveals that, s<strong>in</strong>ce 1982, the average age of<br />
diagnosis has <strong>in</strong>creased steadily and predictably at the rate of almost 1 month each<br />
NZMJ 26 November 2004, Vol 117 No 1206 Page 1 of 9<br />
URL: http://www.nzma.org.nz/journal/117-1206/1183/ © NZMA
year, whereas <strong>in</strong> most other countries the average age of diagnosis of deafness has<br />
been <strong>in</strong> steady decl<strong>in</strong>e.<br />
The reason for this higher age of detection of deafness <strong>in</strong> New Zealand is due <strong>to</strong><br />
reliance on the previous gold standard of screen<strong>in</strong>g babies present<strong>in</strong>g with one or<br />
more ‘high-risk’ <strong>in</strong>dica<strong>to</strong>rs for deafness. Despite the positive rationale beh<strong>in</strong>d the use<br />
of high-risk registers, an abundance of research no longer supports this method as<br />
effective for early identification of deafness. 6–9 As approximately 10% of all<br />
newborns fall with<strong>in</strong> these risk fac<strong>to</strong>rs for deafness, 10 there are large numbers of<br />
newborns <strong>to</strong> screen and lengthy wait<strong>in</strong>g lists for audiology services. Unfortunately,<br />
over 50% of children with a severe/profound congenital hear<strong>in</strong>g loss are not identified<br />
due <strong>to</strong> the fact that they fail <strong>to</strong> exhibit any of the high-risk <strong>in</strong>dica<strong>to</strong>rs. 5,11<br />
Reports that such programmes typically complete diagnostic evaluations on only 25-<br />
50% of this targeted population 12 are similarly concern<strong>in</strong>g, although a New Zealand<br />
programme reports a higher rate of 84%. 13 The <strong>in</strong>effectiveness of us<strong>in</strong>g risk fac<strong>to</strong>rs <strong>to</strong><br />
identify a subpopulation for further screen<strong>in</strong>g is illustrated by the fact that <strong>in</strong><br />
New Zealand there is no significant difference <strong>in</strong> age of detection for those children<br />
who had a risk fac<strong>to</strong>r versus those who do not. 5 Despite the use of high-risk registers,<br />
the goal of detection of deafness before 3 months of age has never been achieved<br />
us<strong>in</strong>g this method of screen<strong>in</strong>g and has a number of serious limitations.<br />
Technology exists <strong>to</strong> quickly and efficiently test the hear<strong>in</strong>g of all babies. Several<br />
large studies overseas exam<strong>in</strong><strong>in</strong>g universal hear<strong>in</strong>g screen<strong>in</strong>g have been conducted<br />
us<strong>in</strong>g au<strong>to</strong>mated ‘audi<strong>to</strong>ry bra<strong>in</strong>stem response’ (ABR) or ‘o<strong>to</strong>acoustic emissions’<br />
(OAE) followed by diagnostic audiology <strong>to</strong> confirm the results.<br />
Maxon et al 14 reported a study of 50,000 <strong><strong>in</strong>fants</strong> screened over a 4-year period, with<br />
measures of sensitivity and specificity compar<strong>in</strong>g favourably with other objective<br />
measures of proven efficacy. Additionally, the Wessex UNHS Trial Group 15<br />
conducted a controlled study of 21,279 babies f<strong>in</strong>d<strong>in</strong>g 1.6% of babies screen<strong>in</strong>g<br />
positive for hear<strong>in</strong>g loss with an overall positive predictive <strong>in</strong>dex of 6.7%.<br />
Techniques such as au<strong>to</strong>mated ABR and OAE are sensitive and specific <strong>to</strong> the<br />
identification of moderate-<strong>to</strong>-profound hear<strong>in</strong>g losses allow the identification of<br />
hear<strong>in</strong>g loss with<strong>in</strong> the neonatal period rather than at 2 or 3 years of age. The aim of<br />
this study was <strong>to</strong> assess the <strong>in</strong>troduction of UNHS of newborns admitted <strong>to</strong> the <strong>NICU</strong><br />
at Christchurch Women’s Hospital.<br />
Methods<br />
From mid-July 2001 <strong>to</strong> mid-July 2002, all babies admitted <strong>to</strong> the Neonatal Service at Christchurch<br />
Women’s Hospital were offered the opportunity <strong>to</strong> undertake a hear<strong>in</strong>g screen<strong>in</strong>g us<strong>in</strong>g the GSI-70<br />
o<strong>to</strong>acoustic emissions screener. The GSI-70 utilises a fully au<strong>to</strong>matic dis<strong>to</strong>rtion product o<strong>to</strong>acoustic<br />
emissions (DPOAE) screen<strong>in</strong>g algorithm, which provides either a ‘PASS’ or ‘REFER’ result at 2000,<br />
4000, and 6000Hz.<br />
In l<strong>in</strong>e with <strong>in</strong>ternational guidel<strong>in</strong>es, a two-stage screen<strong>in</strong>g programme was implemented with each<br />
child who failed the <strong>in</strong>itial screen be<strong>in</strong>g re-screened before discharge. 16 This method has been shown <strong>to</strong><br />
be effective <strong>in</strong> reduc<strong>in</strong>g the false positive rate <strong>to</strong> as low as 1%–2% <strong>in</strong> established programmes. 14,16<br />
False positive rates are largely from fluid <strong>in</strong> the middle ear and small ear canal size, so the o<strong>to</strong>acoustic<br />
emission test<strong>in</strong>g was conducted once the baby was at 34 weeks gestational age and older than 48 hours.<br />
Of the 688 babies admitted <strong>to</strong> the Neonatal Intensive Care Unit, 438 babies (64%) were eligible <strong>to</strong><br />
participate <strong>in</strong> the study by meet<strong>in</strong>g the 48-hour stay criteria. As there was no UNHS screen<strong>in</strong>g <strong>in</strong> the<br />
well baby nursery, those babies who were discharged at younger than 48 hours (36%) were followed<br />
NZMJ 26 November 2004, Vol 117 No 1206 Page 2 of 9<br />
URL: http://www.nzma.org.nz/journal/117-1206/1183/ © NZMA
through the normal ‘at risk’ screen<strong>in</strong>g procedures if a risk fac<strong>to</strong>r was evident. As UNHS has not<br />
become a standard of care procedure, the parents were offered the procedure as an optional screen<strong>in</strong>g<br />
by the research nurse. Only three families chose not <strong>to</strong> undertake UNHS test<strong>in</strong>g. As this was a pilot<br />
programme, for the first 6 months of the trial, all babies who had a risk fac<strong>to</strong>r for deafness were also<br />
referred <strong>to</strong> Christchurch Hospital for a diagnostic ABR. The 435 babies who were screened represented<br />
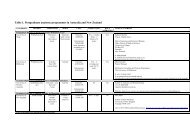
the ethnic diversity <strong>in</strong> Christchurch City region when compared with the 2001 Census 17 (Table 1).<br />
Table 1. Self def<strong>in</strong>ed ethnic group of the children’s parents<br />
Self def<strong>in</strong>ed ethnic group of parents Number %<br />
European<br />
European/Maori<br />
European/Pacific peoples<br />
European/Asian<br />
Maori<br />
Pacific peoples<br />
Asian<br />
Other ethnicity<br />
Results<br />
NZMJ 26 November 2004, Vol 117 No 1206 Page 3 of 9<br />
URL: http://www.nzma.org.nz/journal/117-1206/1183/ © NZMA<br />
366<br />
12<br />
3<br />
1<br />
27<br />
6<br />
10<br />
10<br />
84.14%<br />
2.76%<br />
0.69%<br />
0.23%<br />
6.21%<br />
1.38%<br />
2.30%<br />
2.30%<br />
In <strong>to</strong>tal, 435 babies underwent the UNHS screen<strong>in</strong>g (Figure 1); of those 389 (89.4%)<br />
passed the screen<strong>in</strong>g on first test. Of the 46 babies that required a second screen<strong>in</strong>g<br />
(10.6%), 19 babies failed the second screen and were referred for diagnostic ABR.<br />
The reason for babies fail<strong>in</strong>g the first screen and pass<strong>in</strong>g the second screen was due <strong>to</strong><br />
<strong>in</strong>ternal noise at test<strong>in</strong>g, rema<strong>in</strong><strong>in</strong>g birth fluid, or small ear canals mak<strong>in</strong>g test<strong>in</strong>g<br />
difficult.<br />
The 19 babies (4.37%) who did not pass the retest were referred for a diagnostic ABR<br />
at Christchurch Hospital timed for 1 month past their due date. The diagnostic ABR<br />
confirmed that two babies had a moderate-<strong>to</strong>-severe bilateral sensor<strong>in</strong>eural hear<strong>in</strong>g<br />
loss. Importantly, one of these babies had no risk fac<strong>to</strong>rs for deafness while the other<br />
had hear<strong>in</strong>g loss as part of a congenital syndrome which would have been detected<br />
through the at risk hear<strong>in</strong>g screen<strong>in</strong>g programme. In the first 6 months of the trial,<br />
<strong><strong>in</strong>fants</strong> with a risk fac<strong>to</strong>r for deafness were tested with both OAE screen<strong>in</strong>g and<br />
diagnostic ABR. None of the <strong><strong>in</strong>fants</strong> who passed the OAE screen failed the diagnostic<br />
ABR procedure.<br />
Two of the babies unfortunately did not attend the diagnostic appo<strong>in</strong>tment after<br />
obta<strong>in</strong><strong>in</strong>g a refer result from the screen<strong>in</strong>g and follow-up, despite a follow-up letter<br />
and phone call. As both ‘at risk’ screen<strong>in</strong>g and UNHS programmes have the same<br />
difficulty with follow-up once an <strong>in</strong>fant has left the hospital, it is crucial that medical<br />
practitioners and Plunket nurses rema<strong>in</strong> vigilant for childhood deafness.
Figure 1. Block diagram of the hear<strong>in</strong>g screen<strong>in</strong>g procedure along with numbers<br />
of children pass<strong>in</strong>g and fail<strong>in</strong>g at each stage<br />
DPOAE= dis<strong>to</strong>rtion product o<strong>to</strong>acoustic emissions; ABR= audi<strong>to</strong>ry bra<strong>in</strong>stem response.<br />
Exam<strong>in</strong>ation of risk fac<strong>to</strong>rs <strong>in</strong>dicated that 118 (27.1%) babies had one or more<br />
significant risk fac<strong>to</strong>rs for deafness (Table 2) which would have resulted <strong>in</strong> referral<br />
for a diagnostic ABR. Where there was more than one risk fac<strong>to</strong>r, the most significant<br />
fac<strong>to</strong>r was allocated (eg, birth weight < 1500g). This number (27.1%) is significantly<br />
above the 10% of babies with risk fac<strong>to</strong>rs <strong>in</strong> the general population and highlights the<br />
<strong>in</strong>creased risk of deafness for babies admitted <strong>to</strong> a Neonatal unit.<br />
The undertak<strong>in</strong>g of UNHS screen<strong>in</strong>g resulted <strong>in</strong> a reduction <strong>in</strong> the number of referrals<br />
from 118 babies <strong>to</strong> only 19 babies. A reduction <strong>in</strong> referral rates has the carry-on<br />
benefit that it decreases the length of the wait<strong>in</strong>g list for audiological referrals. In<br />
summary, the positive predictive value of UNHS was significantly greater than ‘at<br />
risk’ screen<strong>in</strong>g with a positive predictive value of hav<strong>in</strong>g a hear<strong>in</strong>g loss of 10.53%<br />
compared <strong>to</strong> 0.85% for babies referred through the at risk program.<br />
NZMJ 26 November 2004, Vol 117 No 1206 Page 4 of 9<br />
URL: http://www.nzma.org.nz/journal/117-1206/1183/ © NZMA
Table 2. Details of the risk fac<strong>to</strong>rs for the 188 babies with one or more<br />
identifiable risk fac<strong>to</strong>rs for deafness<br />
Pr<strong>in</strong>cipal risk fac<strong>to</strong>r Percentage<br />
Significant family his<strong>to</strong>ry<br />
In utero <strong>in</strong>fection<br />
Craniofacial abnormalities<br />
Birth weight
isk of a greater than mild sensor<strong>in</strong>eural hear<strong>in</strong>g loss. The major outcome is the early<br />
identification of hear<strong>in</strong>g loss at 3-4 months of age which allows early <strong>in</strong>troduction of<br />
amplification devices (hear<strong>in</strong>g aids or cochlear implants) and early <strong>in</strong>tervention <strong>to</strong><br />
beg<strong>in</strong>. The New Zealand Deafness Database <strong>in</strong>dicates strongly that the current<br />
identification of children through ‘at risk’ screen<strong>in</strong>g clearly does not achieve this goal.<br />
Two children were confirmed with hear<strong>in</strong>g loss through the UNHS screen<strong>in</strong>g. One<br />
child presented identifiable risk fac<strong>to</strong>rs (congenital syndrome). For this child, the<br />
benefit of UNHS over ‘at risk’ screen<strong>in</strong>g was a reduction <strong>in</strong> wait<strong>in</strong>g list time for a<br />
diagnostic ABR (J Gooley, personal communication, 2002). Conversely, the child<br />
with no risk fac<strong>to</strong>rs for deafness was detected at least 2 years earlier than would have<br />
occurred through the standard ‘at risk’ screen<strong>in</strong>g measures. 5 Earlier detection of<br />
deafness leads <strong>to</strong> improved outcomes <strong>in</strong> terms of audi<strong>to</strong>ry, speech, language, and<br />
educational development. 4 Based on the data presented, the positive predictive <strong>in</strong>dex<br />
for ‘at risk’ screen<strong>in</strong>g was 0.86% with one child missed child who had a hear<strong>in</strong>g<br />
impairment. Conversely, the positive predictive <strong>in</strong>dex for the neonatal screen<strong>in</strong>g<br />
programme was much higher at 10.53% and all hear<strong>in</strong>g impaired children were<br />
identified.<br />
There is some concern that despite a higher positive predictive <strong>in</strong>dex a significant<br />
majority of children who need <strong>to</strong> be retested or referred for further evaluation have no<br />
hear<strong>in</strong>g impairment. The argument has been that the screen<strong>in</strong>g and referral of many<br />
<strong><strong>in</strong>fants</strong> with normal hear<strong>in</strong>g is potentially harmful <strong>to</strong> maternal bond<strong>in</strong>g and family<br />
function. 18 To answer this question, a large study by Watk<strong>in</strong> et al 19 reported that<br />
anxiety <strong>to</strong>wards the screen<strong>in</strong>g was low and that there was no significant difference <strong>in</strong><br />
anxiety state of the retest group versus the control group.<br />
Despite this observation, it is crucial that the attitudes and anxiety of the family are<br />
considered proactively by follow<strong>in</strong>g such recommendations as perform<strong>in</strong>g the screen<br />
<strong>in</strong> the mother’s room, mak<strong>in</strong>g screen<strong>in</strong>g available at a later stage for the small<br />
percentage (4%) of mothers who have significant anxiety, and ensur<strong>in</strong>g that it is<br />
always communicated that the test is a screen<strong>in</strong>g and referral procedure not a<br />
pass/fail. 19<br />
In terms of <strong>in</strong>ternational benchmarks, the implementation of the programme <strong>in</strong><br />
Canterbury matched those recommended for established programmes. Overall, 4.35%<br />
of babies were referred for follow-up test<strong>in</strong>g which is <strong>in</strong> l<strong>in</strong>e with the American<br />
Academy of Paediatrics 20 recommendation of
up. Additionally, 14% of permanent childhood hear<strong>in</strong>g impairment is acquired after<br />
birth (eg, men<strong>in</strong>gitis or cy<strong>to</strong>megalovirus). 6<br />
To quickly detect acquired deafness, it is critical that UNHS programmes do not<br />
remove the need for vision and hear<strong>in</strong>g test<strong>in</strong>g (VHT) <strong>in</strong> schools or other detection<br />
pathways such as suspicion by family members or through regular screen<strong>in</strong>gs by the<br />
family doc<strong>to</strong>r and the Plunket nurse. 5<br />
For the study, DPOAEs were chosen as the technique of choice as it was anticipated<br />
that most children would be admitted <strong>in</strong><strong>to</strong> the neonatal service for longer than 48<br />
hours and is quicker and cheaper <strong>to</strong> perform than au<strong>to</strong>mated ABR. Unfortunately, this<br />
assumption was <strong>in</strong>correct <strong>in</strong> that 250 babies (36.3%) were discharged from the unit<br />
before 48 hours and as such were unable <strong>to</strong> be tested. These babies were then<br />
screened through us<strong>in</strong>g ‘at risk’ screen<strong>in</strong>g. This effect of missed babies due <strong>to</strong> early<br />
discharge would become even greater if test<strong>in</strong>g with OAEs was conducted also <strong>in</strong> the<br />
well baby nursery, where babies are often discharged before 48 hours of age.<br />
While test<strong>in</strong>g with OAE is cheaper <strong>in</strong> terms of capital equipment cost, we recommend<br />
that for a larger programme <strong>in</strong>volv<strong>in</strong>g all live births au<strong>to</strong>mated ABR be used <strong>in</strong><br />
conjunction with OAE as the system of choice. The use of au<strong>to</strong>mated ABR<br />
technology has the advantages of reduced false positive rate with test<strong>in</strong>g <strong>in</strong> the first<br />
few days of a baby’s life, and the ability <strong>to</strong> detect the 3.5% of hear<strong>in</strong>g impaired<br />
children who have audi<strong>to</strong>ry neuropathy, 11 although these advantages must be weighed<br />
up aga<strong>in</strong>st the <strong>in</strong>creased time and equipment cost of au<strong>to</strong>mated ABR test<strong>in</strong>g.<br />
It is crucial that New Zealand take a national approach <strong>to</strong> the development of UNHS<br />
which has begun with Project HEIDI (<strong>Hear<strong>in</strong>g</strong> Impairment Early Detection and<br />
Intervention) and the establishment of a UNHS trial programme <strong>in</strong> Waika<strong>to</strong> Prov<strong>in</strong>ce.<br />
Althrough projects such as these we can demonstrate that deafness can be detected<br />
quickly and reliably <strong>in</strong> newborn babies. Early detection leads <strong>to</strong> the fitt<strong>in</strong>g of<br />
advanced digital hear<strong>in</strong>g <strong>in</strong>struments and/or cochlear implants and beg<strong>in</strong>n<strong>in</strong>g the<br />
crucial audi<strong>to</strong>ry, speech, language, and/or sign language <strong>in</strong>tervention required <strong>to</strong><br />
ensure that the child with a hear<strong>in</strong>g impairment has every chance <strong>to</strong> develop alongside<br />
his/her peers with normal hear<strong>in</strong>g. New Zealand, with an average age of detection of<br />
35 months, is, however, far beh<strong>in</strong>d World’s best standard of practice.<br />
This is a concern as the technology and expertise exists <strong>to</strong> screen the 55,000 babies<br />
born <strong>in</strong> New Zealand each year, diagnose deafness before 4 weeks of age and have the<br />
child fitted with appropriate amplification and <strong>in</strong>tegrated <strong>in</strong><strong>to</strong> an early <strong>in</strong>tervention<br />
programme before 6 months of age. The <strong>in</strong>cidence of permanent congenital hear<strong>in</strong>g<br />
loss currently stands at approximately 3 per 1000 live births, 5 a rate more frequent<br />
than any other health condition for which newborn screen<strong>in</strong>g is already required <strong>in</strong><br />
this country. 21,22 The question now for New Zealand is ‘when will universal hear<strong>in</strong>g<br />
screen<strong>in</strong>g become a national focus?’.<br />
Author <strong>in</strong>formation: Mark C Flynn, Senior Lecturer, University of Canterbury,<br />
Christchurch; Nicola Aust<strong>in</strong>, Neona<strong>to</strong>logist, Canterbury District Health Board,<br />
Christchurch; Traci Schmidtke Flynn, Research Fellow, University of Canterbury,<br />
Christchurch; Rodney P K Ford, Associate Professor, Community Paediatrician,<br />
Canterbury District Health Board, Christchurch; Liz Buckland, Research Nurse,<br />
Canterbury District Health Board, Christchurch<br />
NZMJ 26 November 2004, Vol 117 No 1206 Page 7 of 9<br />
URL: http://www.nzma.org.nz/journal/117-1206/1183/ © NZMA
Correspondence: Dr Mark C Flynn, Oticon A/S, Strandvejen 58, 2900 Hellerup,<br />
Denmark. Fax: (+45) 39 27 79 00; email: mcf@oticon.dk<br />
References:<br />
1. Mauk GW, Behrens TR. His<strong>to</strong>rical, political, and technological context associated with early<br />
identification of hear<strong>in</strong>g loss. Sem<strong>in</strong>ars <strong>in</strong> <strong>Hear<strong>in</strong>g</strong>. 1993;14:1–17.<br />
2. Carney AE, Moeller MP. Treatment efficacy: <strong>Hear<strong>in</strong>g</strong> loss <strong>in</strong> children. Journal of Speech,<br />
Language and <strong>Hear<strong>in</strong>g</strong> Research. 1998;41:S61–S84.<br />
3. Yosh<strong>in</strong>aga-Itano C, Apuzzo ML. The development of deaf and hard of hear<strong>in</strong>g children<br />
identified early through the high-risk registry. American Annal of the Deaf. 1998;143:416-24.<br />
4. Yosh<strong>in</strong>aga-Itano C, Sedey AL, Coulter DK, Mehl AL. Language of early- and later-identified<br />
children with hear<strong>in</strong>g loss. Pediatrics. 1998;102:1161–71.<br />
5. National Audiology Centre. New Zealand deafness notification data: January-December 2002.<br />
Auckland: National Audiology Centre; 2003.<br />
6. Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S. A critical review of the<br />
role of neonatal hear<strong>in</strong>g screen<strong>in</strong>g <strong>in</strong> the detection of congenital hear<strong>in</strong>g impairment. Health<br />
Technology Assessment. 1997;1:1–177.<br />
7. Friedland DR, Fahs MC, Catalano PJ. A cost-effectiveness analysis of the high risk register<br />
and audi<strong>to</strong>ry bra<strong>in</strong>stem response. International Journal of Pediatric O<strong>to</strong>rh<strong>in</strong>olaryngology.<br />
1996;38:115–30.<br />
8. Mauk GW, White KR, Mortensen LB, Behrens TR. The effectiveness of screen<strong>in</strong>g programs<br />
based on high-risk characteristics <strong>in</strong> early identification of hear<strong>in</strong>g impairment. Ear and<br />
<strong>Hear<strong>in</strong>g</strong>. 1999:312–9.<br />
9. White KR, Vohr BR, Behrens TR. <strong>Universal</strong> newborn hear<strong>in</strong>g screen<strong>in</strong>g us<strong>in</strong>g transient<br />
evoked o<strong>to</strong>acoustic emissions: Results of the Rhode Island hear<strong>in</strong>g assessment project.<br />
Sem<strong>in</strong>ars <strong>in</strong> <strong>Hear<strong>in</strong>g</strong>. 1993;14:18–29.<br />
10. Hayes D, Northern JL. Infants and <strong>Hear<strong>in</strong>g</strong>. San Diego (CA): S<strong>in</strong>gular Press; 1996.<br />
11. Mehl AL, Thomson V. The Colorado newborn hear<strong>in</strong>g screen<strong>in</strong>g project, 1992-1999: on the<br />
threshold of effective population-based universal newborn hear<strong>in</strong>g screen<strong>in</strong>g. Pediatrics.<br />
2002;109(1):E7.<br />
12. White KR. <strong>Universal</strong> newborn hear<strong>in</strong>g screen<strong>in</strong>g us<strong>in</strong>g transient evoked o<strong>to</strong>acoustic<br />
emissions: Past, present, and future. Sem<strong>in</strong>ars <strong>in</strong> <strong>Hear<strong>in</strong>g</strong>. 1996;17:171–83.<br />
13. Eden D, Ford RP, Hunter MF, et al. Audiological screen<strong>in</strong>g of neonatal <strong>in</strong>tensive care unit<br />
graduates at high risk of sensor<strong>in</strong>eural hear<strong>in</strong>g loss. N Z Med J. 2000;113:182–3.<br />
14. Maxon AB, White KR, Behrens TR, Vohr BR. Referral rates and cost efficiency <strong>in</strong> a universal<br />
newborn hear<strong>in</strong>g screen<strong>in</strong>g program us<strong>in</strong>g transient evoked o<strong>to</strong>acoustic emissions. J Am Acad<br />
Audiol. 1995;6:271–7.<br />
15. Controlled trial of universal neonatal screen<strong>in</strong>g for early identification of permanent childhood<br />
hear<strong>in</strong>g impairment. Wessex <strong>Universal</strong> Neonatal <strong>Hear<strong>in</strong>g</strong> <strong>Screen<strong>in</strong>g</strong> Trial Group. Lancet.<br />
1998;352:1957–64.<br />
16. Clemens CJ, Davis SA. M<strong>in</strong>imiz<strong>in</strong>g false-positives <strong>in</strong> universal newborn hear<strong>in</strong>g screen<strong>in</strong>g: a<br />
simple solution. Pediatrics. 2001;107:E29.<br />
17. Statistics New Zealand. 2001 Census of Population and Dwell<strong>in</strong>gs. Well<strong>in</strong>g<strong>to</strong>n: Statistics New<br />
Zealand; 2002.<br />
18. Bess FH, Paradise JL. <strong>Universal</strong> hear<strong>in</strong>g screen<strong>in</strong>g for <strong>in</strong>fant hear<strong>in</strong>g impairment: not simple,<br />
not risk free, not necessarily beneficial, and not presently justified. Paediatrics.1994;93:330–4.<br />
19. Watk<strong>in</strong> PM, Baldw<strong>in</strong> M, Dixon R, Beckman A. Maternal anxiety and attitudes <strong>to</strong> universal<br />
neonatal hear<strong>in</strong>g screen<strong>in</strong>g. Br J Audiol.1998;32:27–37.<br />
NZMJ 26 November 2004, Vol 117 No 1206 Page 8 of 9<br />
URL: http://www.nzma.org.nz/journal/117-1206/1183/ © NZMA
20. Year 2000 position statement: pr<strong>in</strong>ciples and guidel<strong>in</strong>es for early hear<strong>in</strong>g detection and<br />
<strong>in</strong>tervention programs. Jo<strong>in</strong>t Committee on Infant <strong>Hear<strong>in</strong>g</strong>, American Academy of Audiology,<br />
American Academy of Pediatrics, American Speech-Language-<strong>Hear<strong>in</strong>g</strong> Association, and<br />
Direc<strong>to</strong>rs of Speech and <strong>Hear<strong>in</strong>g</strong> Programs <strong>in</strong> State Health and Welfare Agencies. Pediatrics<br />
2000;106:798–817.<br />
21. Mehl AL, Thomson V. <strong>Newborn</strong> hear<strong>in</strong>g screen<strong>in</strong>g: the great omission. Pediatrics.<br />
1998;101:E4.<br />
22. Flynn MC, Pope B. New acoustical measures for the early detection of deafness <strong>in</strong> newborn<br />
babies. NZ Acoustics. 2001;14:32–37.<br />
NZMJ 26 November 2004, Vol 117 No 1206 Page 9 of 9<br />
URL: http://www.nzma.org.nz/journal/117-1206/1183/ © NZMA