Gastroenterology Today Spring 2022
Gastroenterology Today Spring 2022
Gastroenterology Today Spring 2022
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume 32 No. 1<br />
<strong>Spring</strong> <strong>2022</strong><br />
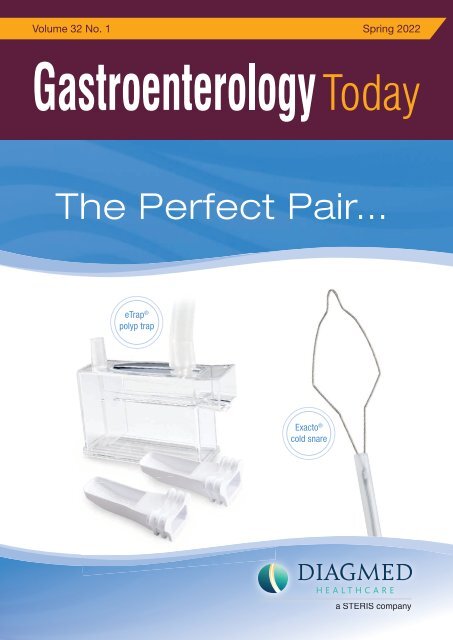
The Perfect Pair...<br />
eTrap ®<br />
polyp trap<br />
Exacto ®<br />
cold snare<br />
a STERIS company
WITH YOUR HELP<br />
We’ve made<br />
<strong>Gastroenterology</strong> a true<br />
7 day NHS service<br />
Join forces with the UK’s largest campaign to see and<br />
treat those NHS patients who need you most. All working<br />
as part of an expert clinical team in outpatient clinics or<br />
undertaking Endoscopy procedures, getting the right care<br />
to those patiently waiting.<br />
Register your support or enquire below.<br />
Together, we can end the wait.<br />
www.ukmedinet.com
CONTENTS<br />
CONTENTS<br />
4 EDITORS COMMENT<br />
6 FEATURE Gastric polyps: a 10-year analysis of 18,496<br />
upper endoscopies<br />
14 FEATURE Endoscopic retrograde appendicitis therapy<br />
versus laparoscopic appendectomy versus open<br />
appendectomy for acute appendicitis: a pilot study<br />
22 FEATURE An extremely dangerous case of acute massive<br />
upper gastrointestinal bleeding: a case report<br />
26 NEWS<br />
31 COMPANY NEWS<br />
This issue edited by:<br />
Hesam Ahmadi Nooredinvand<br />
c/o Media Publishing Company<br />
Greenoaks<br />
Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
ADVERTISING & CIRCULATION:<br />
Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
Tel: 01886 853715<br />
E: info@mediapublishingcompany.com<br />
www.MediaPublishingCompany.com<br />
PUBLISHING DATES:<br />
March, June, September and December.<br />
COPYRIGHT:<br />
Media Publishing Company<br />
Greenoaks<br />
Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
COVER STORY<br />
At Diagmed Healthcare our mission is to provide our Customers with innovative products<br />
to better diagnose, prevent, and treat disease of the gastrointestinal tract. From advanced<br />
polypectomy and GI emergency devices, to procedural infection prevention solutions we<br />
are continuously developing new innovations and technologies.<br />
The perfect pair…<br />
The Exacto ® Cold Snare and eTrap ® Polyp Trap support resection and retrieval of<br />
diminutive polyps.<br />
Clinically proven to achieve a signifi cantly high rate of complete resection, the Exacto cold<br />
snare offers control and placement for a precise, clean cut 1,2 . The Exacto snare supports<br />
the cold snare polypectomy technique and can be used to resect a variety of different<br />
types of polyps in multiple sizes (including diminutive and large) and features the following:<br />
• Features a shield shape design that maximises its width for control and placement<br />
during cold snare polypectomy<br />
• 33% thinner wire diameter than traditional braided wires allowing for stiffness and<br />
fl exibility due to its thin, seven braided wire confi guration<br />
• Reduces polyp “fl y away” from the resection site making it possible tocollect specimen<br />
for pathology 2<br />
Designed by GI nurses, the eTrap polyp trap supports retrieval of multiple specimens,<br />
while safeguarding clinicians and nurses from unnecessary exposure to biomaterials.<br />
• Two removable polyp specimen collector strainer trays allowing for retrieval of multiple<br />
polyps with uninterrupted suction<br />
• A clear magnifying window allows direct visualization of the collected specimen<br />
• A measurement guide designed to aid in specimen sizing<br />
For more information on our complete offering of polypectomy solutions, visit<br />
diagmed.healthcare today.<br />
1) Horiuchi A, Hosoi K. “Prospective, Randomized Comparison of 2 Methods of Cold Snare Polypectomy for Small<br />
Colorectal Polyps.” Gastrointestinal Endoscopy (2015): 1-7.<br />
2) Din S, Ball A. “Cold Snare Polypectomy: Does Snare Type Infl uence Outcomes?” Digestive Endoscopy (2015): 1-6.<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company.<br />
Next Issue Summer <strong>2022</strong><br />
Subscription Information – <strong>Spring</strong> <strong>2022</strong><br />
<strong>Gastroenterology</strong> <strong>Today</strong> is a quarterly<br />
publication currently sent free of charge to<br />
all senior qualifi ed Gastroenterologists in<br />
the United Kingdom. It is also available<br />
by subscription to other interested individuals<br />
and institutions.<br />
UK:<br />
Individuals - £24.00 incl postage<br />
Commercial Organistations - £48.00 incl postage<br />
Overseas:<br />
£72.00 incl Air Mail postage<br />
We are also able to process your<br />
subscriptions via most major credit<br />
cards. Please ask for details.<br />
Cheques should be made<br />
payable to MEDIA PUBLISHING.<br />
Designed in the UK by me&you creative<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
3
EDITORS COMMENT<br />
EDITORS COMMENT<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
“COVID-19<br />
pandemic<br />
appears to<br />
be shifting<br />
towards an<br />
endemic<br />
disease<br />
with most<br />
healthcare<br />
services<br />
gradually<br />
returning<br />
to normal,<br />
the positive<br />
impact of<br />
which will<br />
certainly<br />
be felt by<br />
patients.”<br />
Disruption to the health service during the last couple of years as a result of the<br />
pandemic has undoubtedly had a detrimental impact on certain aspects of patient care.<br />
A recent healthcare survey by Crohn’s and Colitis UK highlights how a delay in diagnosis,<br />
difficulty in accessing specialist advice and disruption to surgery and endoscopy services<br />
have had a negative impact on both physical and mental wellbeing of many patients with<br />
Inflammatory Bowel Disease (IBD).<br />
There is however light at the end of the tunnel. COVID-19 pandemic appears to be shifting<br />
towards an endemic disease with most healthcare services gradually returning to normal,<br />
the positive impact of which will certainly be felt by patients.<br />
We have a number of fascinating articles included in this <strong>Spring</strong> edition of <strong>Gastroenterology</strong><br />
<strong>Today</strong> including,<br />
• Role of Endoscopic Retrograde Appendicitis Therapy (ERAT) as an alternative to surgical<br />
appendectomy in acute uncomplicated appendicitis<br />
• Scientists in Munich explore the mechanism that triggers problematic interaction between<br />
intestinal bacteria and cells in intestinal mucus layer in patients with IBD which could offer<br />
targets for development of new drug therapy<br />
• Coeliac UK highlights the role of the Rare Disease Collaborative Network in supporting<br />
with diagnosis and management of patients with refractory coeliac disease<br />
• Retrospective study looking at the frequency of gastric polyps and their association with<br />
certain factors<br />
• An interesting case report of massive gastrointestinal bleeding secondary to a fish bone!<br />
Hesam Ahmadi Nooredinvand,<br />
St George’s Hospital<br />
4
Prescribe Entocort ® CR by brand<br />
instead of prednisolone<br />
• Rapid induction of remission from 2 weeks with<br />
Entocort ® CR* 1<br />
• ~50% fewer corticosteroid-associated side effects<br />
than prednisolone 2,3<br />
• Unlike Entocort ® CR, prednisolone increases<br />
susceptibility to, and severity of, infections †2,4<br />
• Entocort ® CR is the only controlled-release<br />
oral budesonide indicated for Crohn’s disease 2<br />
Help keep your Crohn’s patients out of hospital...<br />
...and where they want to be<br />
*Remission was defined as a score of ≤150 on the Crohn’s disease activity index.<br />
†Entocort ® CR should be used with caution in patients with infections where the use of glucocorticosteroids may have unwanted effects. 2<br />
ENTOCORT CR 3mg Capsules (budesonide) - Prescribing<br />
Information<br />
Please consult the Summary of Product Characteristics (SmPC) for full<br />
prescribing Information<br />
Presentation: Hard gelatin capsules for oral administration with an<br />
opaque, light grey body and an opaque, pink cap marked CIR 3mg in black<br />
radial print. Contains 3mg budesonide. Indications: Induction of remission<br />
in patients with mild to moderate Crohn’s disease affecting the ileum and/or<br />
the ascending colon. Induction of remission in patients with active<br />
microscopic colitis. Maintenance of remission in patients with microscopic<br />
colitis. Dosage and administration: Active Crohn’s disease (Adults): 9mg<br />
once daily in the morning for up to eight weeks. Full effect achieved in 2-4<br />
weeks. When treatment is to be discontinued, dose should normally be<br />
reduced in final 2-4 weeks. Active microscopic colitis (Adults): 9mg once<br />
daily in the morning. Maintenance of microscopic colitis (Adults): 6mg once<br />
daily in the morning, or the lowest effective dose. Paediatric population: Not<br />
recommended. Older people: No special dose adjustment recommended.<br />
Swallow whole with water. Do not chew. Contraindications:<br />
Hypersensitivity to the active substance or any of the excipients. Warnings<br />
and Precautions: Side effects typical of corticosteroids may occur. Visual<br />
disturbances may occur. If a patient presents with symptoms such as<br />
blurred vision or other visual disturbances they should be considered for<br />
referral to an ophthalmologist for evaluation of the possible causes.<br />
Systemic effects may include glaucoma and when prescribed at high doses<br />
for prolonged periods, Cushing’s syndrome, adrenal suppression, growth<br />
retardation, decreased bone mineral density and cataract. Caution in<br />
patients with infection, hypertension, diabetes mellitus, osteoporosis,<br />
peptic ulcer, glaucoma or cataracts or with a family history of diabetes or<br />
glaucoma. Particular care in patients with existing or previous history of<br />
severe affective disorders in them or their first degree relatives. Caution<br />
when transferring from glucocorticoid of high systemic effect to Entocort<br />
CR. Chicken pox and measles may have a more serious course in patients<br />
on oral steroids. They may also suppress the HPA axis and reduce the stress<br />
response. Reduced liver function may increase systemic exposure. When<br />
treatment is discontinued, reduce dose over last 2-4 weeks. Concomitant<br />
use of CYP3A inhibitors, such as ketoconazole and cobicistat-containing<br />
products, is expected to increase the risk of systemic side effects and<br />
should be avoided unless the benefits outweigh the risks. Excessive<br />
grapefruit juice may increase systemic exposure and should be avoided.<br />
Patients with fructose intolerance, glucose-galactose malabsorption or<br />
sucrose-isomaltase insufficiency should not take Entocort CR. Monitor<br />
height of children who use prolonged glucocorticoid therapy for risk of<br />
growth suppression. Interactions: Concomitant colestyramine may<br />
reduce Entocort CR uptake. Concomitant oestrogen and contraceptive<br />
steroids may increase effects. CYP3A4 inhibitors may increase systemic<br />
exposure. CYP3A4 inducers may reduce systemic exposure. May cause low<br />
values in ACTH stimulation test. Fertility, pregnancy and lactation: Only<br />
to be used during pregnancy when the potential benefits to the mother<br />
outweigh the risks for the foetus. May be used during breast feeding.<br />
Adverse reactions: Common: Cushingoid features, hypokalaemia,<br />
behavioural changes such as nervousness, insomnia, mood swings and<br />
depression, palpitations, dyspepsia, skin reactions (urticaria, exanthema),<br />
muscle cramps, menstrual disorders. Uncommon: anxiety, tremor,<br />
psychomotor hyperactivity. Rare: aggression, glaucoma, cataract, blurred<br />
vision, ecchymosis. Very rare: Anaphylactic reaction, growth retardation.<br />
Prescribers should consult the summary of product characteristics in<br />
relation to other adverse reactions. Marketing Authorisation Numbers,<br />
Package Quantities and basic NHS price: PL 36633/0006. Packs of 50<br />
capsules: £37.53. Packs of 100 capsules: £75.05. Legal category: POM.<br />
Marketing Authorisation Holder: Tillotts Pharma UK Ltd, The Stables,<br />
Wellingore Hall, Wellingore, Lincoln, LN5 0HX. Date of preparation of PI:<br />
February 2020<br />
Adverse events should be reported.<br />
Reporting forms and information can be<br />
found at https://yellowcard.mhra.gov.uk.<br />
Adverse events should also be reported to<br />
Tillotts Pharma UK Ltd. Tel: 01522 813500.<br />
References: 1. Campieri M et al. Gut 1997; 41: 209–214. 2. Entocort ®<br />
CR 3 mg capsules – Summary of Product Characteristics. 3. Rutgeerts<br />
P et al. N Engl J Med 1994; 331: 842–845. 4. Prednisolone 5 mg tablets<br />
– Summary of Product Characteristics.<br />
Date of preparation: August 2021. PU-00572.
FEATURE<br />
GASTRIC POLYPS: A 10-YEAR<br />
ANALYSIS OF 18,496 UPPER<br />
ENDOSCOPIES<br />
Haythem Yacoub 1,2* , Norsaf Bibani 1,2 , Mériam Sabbah 1,2 , Nawel Bellil 1,2 , Asma Ouakaa 1,2 , Dorra Trad 1,2 and Dalila Gargouri 1,2<br />
Yacoub et al. BMC <strong>Gastroenterology</strong> (<strong>2022</strong>) 22:70 https://doi.org/10.1186/s12876-022-02154-8<br />
Abstract<br />
Background/aims<br />
Gastric polyps (GPs) are usually asymptomatic lesions of the upper<br />
gastrointestinal tract observed in 1–3% of esophagogastroduodenoscopies<br />
(EGD). Most GPs are benign. The aim of this study was to precise the<br />
frequency of different types of gastric polyps in our population, and to<br />
analyze their possible association with other factors.<br />
Materials and methods<br />
A total of 18,496 consecutive patients undergoing EGD over a<br />
10-year period (between 2007 and 2018) in a tertiary hospital were<br />
retrospectively reviewed. Eighty-six patients diagnosed with gastric<br />
polyps were analysed. Demographics, medical history of the patients,<br />
and indication for gastroscopy were collected. Morphological,<br />
histological characteristics of polyps, and therapeutic management data<br />
were also collected.<br />
fundic gland are the most common in our country. The high frequency of<br />
Helicobacter pylori infection in our patients and in our area may explain<br />
the high frequency of HP.<br />
Keywords<br />
Stomach, Polyp, Polypectomy, Endoscopic mucosal resection<br />
Introduction<br />
Gastric polyps (GPs) are defined as luminal projections above<br />
the plane of the adjacent mucosa regardless of its histological<br />
type [1]. Gastric polyps are usually discovered incidentally during<br />
esophagogastroduodenoscopies (EGD) and their prevalence is<br />
estimated from 0.5 to 23% of all upper gastrointestinal endoscopies [2].<br />
Some polyps can occasionally present with bleeding, anemia, or gastric<br />
outlet obstruction [3].<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
Results<br />
GPs were found in 86 out of 18,496 (0.46%) reviewed EGD,<br />
corresponding to a total of 141 polyps. There were 64 female (74.4%)<br />
and 22 male patients (25.6%) with a sex ratio (M/F) of 0.34. The<br />
average age was 58.1 years. One hundred and forty one polyps were<br />
included, and histopathology was obtained on 127 GPs. The most<br />
common location was the fundus (59.6%) and 48.9% were smaller than<br />
5 mm. The polyp was unique in 75.6% of cases. According to Paris<br />
classification, 80% of the polyps were sessile (Is). Hyperplastic polyps<br />
were the most common (55.9%), followed by sporadic fundic gland<br />
polyps observed in 23 patients (18.1%), 7 (5.5%) were adenomas and<br />
4 (3.1%) were neuroendocrine tumors type 1. The following factors<br />
were associated with hyperplastic polyps: anemia (p =0.022), single<br />
polyp (p=0.025) and size≥5 mm (p=0.048). Comparing hyperplastic<br />
polyps’ biopsies to resected polyps, no difference was found in the<br />
evolutionary profile of the 2 groups. A size less than 10 mm (p =0.013)<br />
was associated with fundic gland polyps. Sixty polyps (47.2%) were<br />
treated by cold forceps, 19 (15%) treated by a mucosal resection and<br />
15 (11.8%) with diathermic snare. Five procedural bleeding incidents<br />
were observed (3.9%). Only the use of anticoagulant treatment was<br />
associated with a high bleeding risk (p=0.005). The comparative<br />
histological study between specimens of biopsied GPs and endoscopic<br />
polypectomy led to an overall agreement of 95.3%.<br />
Conclusion<br />
In our study, the GPs frequency was 0.36%. Hyperplastic polyps and<br />
The majority of polyps are benign (> 85% of cases). The risk of<br />
malignancy or malignant transformation of gastric polyps depends on<br />
their histological nature. GPs have been associated with multiple factors,<br />
such as H. pylori infection for hyperplastic polyps and adenomas,<br />
proton-pump inhibitor (PPI) use for fundic gland polyps [4, 5].<br />
The aim of this study was to precise the frequency of different types of<br />
gastric polyps in our population and to analyze their possible association<br />
with other factors to evaluate the results of curative endoscopic<br />
resection of gastric polyps and to study the evolutionary status of<br />
unresected gastric polyps.<br />
Methods<br />
Study design<br />
A retrospective study in which all consecutive patients with GPs were<br />
enrolled was performed at a tertiary-level hospital (Habib Thameur<br />
Hospital of Tunis) from 2008 to 2017. A total of 18,496 consecutive<br />
EGD over a 10-year period were retrospectively reviewed. Eightysix<br />
patients diagnosed with gastric polyps were analysed. Follow-up<br />
gastroscopies performed on the same patient were not excluded. This<br />
study was performed according to the Declaration of Helsinki, following<br />
the guidelines for good clinical practice. Habib Thameur Hospital ethics<br />
committee approved the study protocol.<br />
6<br />
*Correspondence: yacoubhaythem@hotmail.com<br />
1<br />
<strong>Gastroenterology</strong> and Hepatology Department, Habib Thameur Hospital, Tunis, Tunisia<br />
©The Author(s) <strong>2022</strong>
FEATURE<br />
All cases of gastric polyps were identified from endoscopy reports.<br />
All data regarding patients were obtained from the electronic medical<br />
record. Demographic data (sex, age), relevant pathological history<br />
(colorectal cancer or hereditary polyposis syndrome, colon polyp,<br />
cirrhosis), routine hemograms, as well as data related to the EGD<br />
indication of gastroscopy, number and size of GPs, location, histological<br />
type, and the presence of chronic gastritis or H. pylori infection using<br />
the Hematoxylin eosin staining) were collected. The polyp size was<br />
estimated by comparing it with the opening size of the used biopsy<br />
forceps. In patients with multiple polyps, we collected the endoscopic<br />
characteristics of the four largest polyps. GP recurrence following<br />
resection were also collected (number, location, size, histological type<br />
and, recurrence interval after polypectomy) Patients whose hemoglobin<br />
levels were less than 13 g/dl in males and 12 g/dl in females were<br />
considered with anemia.<br />
was based on endoscopic findings; the most common localization<br />
for gastric polyps was the fundus, followed by the antrum and the<br />
corpus (Table 2).<br />
Histopathologic diagnosis of polyps was obtained for 127 polyps.<br />
The histological study showed hyperplastic polyps in 71 of the polyps<br />
(55.9%), followed by fundic gland polyps (n=23, 18.1%) (Table 3). The<br />
“other” category included pancreatic heterotopias, lipoma and polypoid<br />
foveolar hyperplasia.<br />
H. pylori infection identification was carried out with the hematoxylin<br />
eosin staining in 64 patients (patients with gastric mucosa<br />
abnormalities). H. pylori infection was detected in 45 patients<br />
(62.3%). H. pylori was positive in 30 of the 49 (61.2%) of patients with<br />
hyperplastic polyps.<br />
Ethics approval and consent to participate<br />
This study was performed according to the Declaration of Helsinki,<br />
following the guidelines for good clinical practice. “Habib Thameur<br />
Hospital ethics committee” approved the study protocol. All methods<br />
were carried out in accordance with relevant guidelines and regulations.<br />
Informed consent to participate in the study was obtained from<br />
participants.<br />
Statistical analysis<br />
The data were analyzed on the Statistical Package for the Social<br />
Sciences (SPSS) version 23, IBM SPSS Inc.; Chicago, IL, USA). Results<br />
for the continuous variables that followed a normal distribution were<br />
expressed as mean±standard deviation and range while variables that<br />
did not follow a normal distribution were presented in median and the<br />
interquartile range.<br />
For comparisons, Student’s t-test was used for quantitative variables.<br />
A univariate analysis was conducted to identify the possible associated<br />
factors with the different histological types of GPs. A multivariate analysis<br />
was carried out with variables that achieved statistical significance. The<br />
level of statistical significance was established with a p value ≤ 0.05.<br />
The factors independently associated with hyperplastic polyps were<br />
the presence of anemia, being a single polyp, and sized≥5 mm. The<br />
associated variable for fundic gland polyps, was only size 70 years. Age distribution of the patients with<br />
GPs was summarized in Fig. 1.<br />
More than the three-quarters of the patients had single polyps.<br />
The average polyp diameter was 6 mm (range: 2–30 mm). The<br />
diameters of the polyps were < 5 mm in 69 of cases (48.9%), 5–9<br />
mm in 53 (37.6%) patients, 10–19 mm in 15 (10.7%) patients,<br />
and ≥ 20 mm in 4 (2.8%) patients (Table 2). The location of GPs<br />
Age (median years),(range, years) 58.1 ± 15.4, (18–84)<br />
Gender<br />
Male 22 (25.6)<br />
Female 64 (74.4)<br />
Personal history<br />
GERD 26 (30.2)<br />
Anemia 36 (44.2)<br />
Colon polyps 2 (2.3)<br />
Cirrhosis 11 (12.8)<br />
Gastrectomy 3 (3.5)<br />
Hereditary polyposis syndrome 0 (0)<br />
Indication<br />
Epigastric pain 30 (34.9)<br />
Dyspepsia 16 (18.6)<br />
Anemia 21 (24.4)<br />
UGIB 2 (2.3)<br />
Monitoring of PHT 13 (15.1)<br />
Other 4 (4.7)<br />
GP gastric polyps, GERD gastro-esophageal reflux disease, PHT portal<br />
hypertension, UGIB upper gastrointestinal bleeding<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
7
FEATURE<br />
Anticoagulant or anti-aggregating medication was significantly correlated<br />
with the onset of bleeding (p=0.002).<br />
Twenty-one polyps were biopsied and then resected. A comparison of<br />
the histological results between biopsy specimen and polypectomy was<br />
made.<br />
Adenomas analysis showed a 100% agreement between primary and<br />
final results. The agreement rate was 93% for hyperplastic polyps<br />
(13 polyps out of 14). The comparative histological study between<br />
specimens of biopsied GPs and endoscopic polypectomy led to an<br />
overall agreement of 95.3% (Table 7).<br />
Discussion<br />
One hundred and twenty-seven specimens, corresponding to eightysix<br />
patients, of the total of 18,496 upper gastrointestinal endoscopic<br />
procedures, taken from gastric polypoid lesions (0.46%) were reported.<br />
In the literature, a great variability was observed in the prevalence of<br />
GPs, ranging from 0.5 to 6.35% [2, 6, 7]. In our study, the prevalence<br />
of GPs is lesser than reported in literature. This can be explained by<br />
the fact that follow-up EGD performed on the same patient was not<br />
excluded.<br />
This is the first study that evaluates the GPs frequency in Tunisia. In our<br />
study, we found that the most common symptoms in patients with GPs<br />
were epgastric pain and anemia. We also found that GPs were localized<br />
mostly in the fundus, and mostly Is according to Paris classification and<br />
the hyperplastic type was the most common.<br />
Table 2 Morphological and histological characteristics of the<br />
141 polyps<br />
Parameter n (%)<br />
Table 2 Morphological and histological characteristics of the<br />
Patient with GPs 86 (100)<br />
141 polyps<br />
Single 65 (75.6)<br />
Parameter Multiple n (%) 21 (24.4)<br />
Location<br />
Patient with GPs 86 (100)<br />
Fundus 51 (59.3)<br />
Single 65 (75.6)<br />
Body 5 (5.8)<br />
Multiple 21 (24.4)<br />
Antrum 28 (32.6)<br />
Location<br />
Multiple location 2 (2.3)<br />
Fundus 51 (59.3)<br />
Size in mm<br />
Body 5 (5.8)<br />
1–4 mm 69 (48.9)<br />
Antrum 28 (32.6)<br />
5–9 mm 53 (33.6)<br />
Multiple location 2 (2.3)<br />
10–14 mm 8 (5.7)<br />
Size in mm<br />
15–19 mm 7 (5)<br />
1–4 mm 69 (48.9)<br />
> 20 mm 4 (2.8)<br />
5–9 mm 53 (33.6)<br />
Paris classification<br />
10–14 mm 8 (5.7)<br />
Ip 17 (12)<br />
15–19 mm 7 (5)<br />
Is 112 (80)<br />
> 20 mm 4 (2.8)<br />
IIa 11 (8)<br />
Paris classification<br />
IIb, IIc 0 (0)<br />
Ip 17 (12)<br />
Is GP gastric polyps<br />
112 (80)<br />
IIa 11 (8)<br />
IIb, IIc 0 (0)<br />
Hyperplastic polyps and fundic gland polyps together make up to 90%<br />
GP gastric polyps<br />
[6,7,8] followed by adenomas and other histological type, which are<br />
much less common. These rates are similar to those observed in our<br />
population with a predominance of hypeplastic type.<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
Fig. 1 The age distribution of patients with gastric polyps<br />
Fig. 1 The age distribution of patients with gastric polyps<br />
8
FEATURE<br />
Table Table 3 3 Histological analysis analysis of the of the 127 127 GP GP<br />
Table Table 5 5 Univariate analysis analysis of of associated factors factors with with fundic fundic<br />
Table 3 Histological analysis of the 127 GP<br />
gland Tablepolyps 5 Univariate analysis of associated factors with fundic<br />
Histological Table 3 type Histological type analysis of the 127 GP<br />
gland<br />
n (%) n (%) Tablepolyps 5 Univariate (n=127) analysis of associated factors with fundic<br />
gland polyps (n=127)<br />
Histological type n (%)<br />
Parameter gland polyps (n=127)<br />
Histological type n (%)<br />
Fundic Fundic gland gland polyps polyps Non-fundic p value p value<br />
Hyperplastic 71 (55.9) 71 (55.9)<br />
Parameter Fundic gland polyps gland Non-fundic gland polyps polyps<br />
Parameter Fundic gland polyps Non-fundic p value p value<br />
Fundic Hyperplastic Fundic Hyperplastic gland gland polyps polyps 23 71 (18.1) (55.9) 23 71 (18.1) (55.9)<br />
n (%) n (%) gland n (%) gland n (%) polyps polyps<br />
Adenoma Fundic Adenoma Fundic gland gland polyps polyps 237 (5.5) (18.1) 237 (5.5) (18.1)<br />
n (%) n (%) n (%) n (%)<br />
Age Age (years) (years) 53.3 53.3 ± 21.3 ± 21.3 58.8±14.1 0.303 0.303<br />
Adenoma Neuroendocrine Adenoma neoplasia neoplasia 47 (3.1) (5.5) 47 (3.1) (5.5)<br />
Age Gender (years) 53.3 ± 21.3 58.8±14.1 0.303 0.289<br />
Xanthelasmaneoplasia 14 (0.8) (3.1) 1 (0.8) Age Gender (years) 53.3 ± 21.3 58.8±14.1 0.289 0.303<br />
Neuroendocrine neoplasia 4 (3.1)<br />
Male Gender Male 1 (11.1) 19 (27.5) 0.289<br />
Xanthelasma Inflammatory fibroid fibroid polyp polyp 91 (7.2) (0.8) 9 (7.2) Gender 1 (11.1) 19 (27.5) 0.289<br />
Xanthelasma 1 (0.8)<br />
Male Female 18 (11.1) (88.9) 19 50 (27.5) (72.5)<br />
No Inflammatory true No true polyp polyp fibroid polyp 79 (5.5) (7.2) 7 (5.5) Male Female 18 (11.1) (88.9) 19 50 (27.5) (72.5)<br />
Inflammatory fibroid polyp 9 (7.2)<br />
Female 8 (88.9) 50 (72.5) 0.170<br />
Other No true Other polyp 57 (3.9) (5.5) 5 (3.9) Female Single/multiple 8 (88.9) 50 (72.5) 0.170<br />
No true polyp 7 (5.5)<br />
Single/multiple 5 (55.6) 53 (76.8)<br />
GP Other gastric polyps<br />
5 (3.9)<br />
Single/multiple 5 (55.6) 53 (76.8) 0.170 0.170<br />
GP Other gastric polyps<br />
5 (3.9)<br />
Single Multiple Single Multiple 54 (55.6) (44.4) 54 (55.6) (44.4) 53 16 (76.8) (23.2) 53 16 (76.8) (23.2)<br />
GP gastric GP gastric polyps polyps<br />
GERDMultiple 4 (44.4) 4 (44.4) 16 (23.2) 16 (23.2) 0.7 0.7<br />
Table Table 4 4 Univariate analysis analysis of of associated factors factors with with<br />
GERDYes GERD 5 (55.6) 5 (55.6) 20 (29) 20 (29) 0.7 0.7<br />
Table hyperplastic Table 4 Univariate 4 polyps Univariate polyps (n analysis = (n 127) analysis = 127) of of associated associated factors factors with with Yes No Yes No 54 (55.6) (44.4) 54 (55.6) (44.4) 20 49 (29) (71) 20 49 (29) (71)<br />
hyperplastic polyps (n = 127)<br />
Parameter hyperplastic polyps Hyperplastic (n = 127) polyps polyps Non-<br />
Nonhyperplastic<br />
p value p value No Anemia No Anemia 4 (44.4) 4 (44.4) 49 (71) 49 (71) 0.115 0.115<br />
p value Yes Anemia 8 (88.9) 43 (62.3) 0.115<br />
Parameter Hyperplastic polyps Nonhyperplastic<br />
polyps<br />
Parameter Hyperplastic polyps Nonhyperplastic<br />
Yes No Yes No 81 (88.9) (11.1) 81 (88.9) (11.1) 43 26 (62.3) (37.7) 43 26 (62.3) (37.7)<br />
p value<br />
Yes Anemia 8 (88.9) 43 (62.3) 0.115<br />
polyps<br />
n (%) n (%) n polyps (%) polyps n (%)<br />
No Location No Location 1 (11.1) 1 (11.1) 26 (37.7) 26 (37.7)<br />
n (%) n (%) n (%) n (%)<br />
Age Age (years) (years) 57.7 57.7 ± 13.4 ± 13.4 58.8 58.8 ± 17.4 ± 17.4 0.7 0.7 Fundus Location Fundus Location 23 (100) 23 (100) 56 (53.9) 56 (53.9)<br />
Age Gender Age Gender (years) (years) 57.7 57.7 ± 13.4 ± 13.4 58.8 58.8 ± 17.4 ± 17.4 0.7<br />
0.7<br />
Fundus Non Fundus Non fundus fundus 23 0 (0) (100) 23 0 (0) (100) 56 48 (53.9) (46.1) 56 48 (53.9) (46.1)<br />
Male Gender Male Gender 12 (24.5) 12 (24.5) 8 (27.6) 8 (27.6) 0.7 0.7<br />
Non Size Non Size in fundus mm in fundus mm 0 (0) 0 (0) 48 (46.1) 48 (46.1) 0.013 0.013<br />
MaleFemale 37 12 (75.5) (24.5) 37 12 (75.5) (24.5) 21 8 (27.6) (72.4) 21 8 (27.6) (72.4)<br />
< Size 5 mm < Size in 5 mm in mm 14 (60.9) 14 (60.9) 55 (53) 55 (53) 0.013 0.013<br />
Female Single/multiple Female 37 (75.5) 37 (75.5) 21 (72.4) 21 (72.4) 0.05 0.05 < ≥5 mm < ≥5 mm 14 9 (39.1) (60.9) 14 9 (39.1) (60.9) 55 49 (53) (47) 55 49 (53) (47)<br />
Single/multiple Single/multiple 40 (81.6) 40 (81.6) 11 (38) 11 (38) 0.05 0.05<br />
≥Paris 5 mm ≥Paris 5 mm classification 9 (39.1) 9 (39.1) 49 (47) 49 (47)<br />
Multiple Single Multiple Single 940 (18.4) (81.6) 940 (18.4) (81.6) 18 11 (62) (38) 18 11 (62) (38)<br />
Ip Paris Ip Paris classification classification 3 (13) 3 (13) 12 (11.5) 12 (11.5) 0.524 0.524<br />
GERD Multiple GERD Multiple 9 (18.4) 9 (18.4) 18 (62) 18 (62) 0.7 0.7 Ip Is Ip Is 316 (13) (69.5) 316 (13) (69.5) 12 85 (11.5) (81.7) 12 85 (11.5) (81.7) 0.524 0.273 0.524 0.273<br />
GERDYes GERD 15 (30.6) 15 (30.6) 10 (34.5) 10 (34.5) 0.7 0.7<br />
Is IIa Is IIa 16 4 (17.5) (69.5) 16 4 (17.5) (69.5) 85 7 (6.8) (81.7) 85 7 (6.8) (81.7) 0.273 0.105 0.273 0.105<br />
No Yes No Yes 34 15 (69.4) (30.6) 34 15 (69.4) (30.6) 19 10 (65.5) (34.5) 19 10 (65.5) (34.5)<br />
IIa IIb, IIc IIa IIb, IIc 40 (17.5) (0) 40 (17.5) (0) 70 (6.8) (0) 70 (6.8) (0) 0.105 – 0.105 –<br />
Anemia No Anemia No 34 (69.4) 34 (69.4) 19 (65.5) 19 (65.5) < 10 < –3 10 –3 GP: IIb, IIc gastric GP: IIb, IIc gastric polyps, polyps, GERD: GERD: 0 (0) 0 gastro-esophageal (0) reflux reflux disease 0 (0) disease 0 (0) – –<br />
Yes Anemia Yes Anemia 28 (57.2) 28 (57.2) 3 (10.3) 3 (10.3) < 10 < –3<br />
10 –3 Significant GP: gastric Significant GP: gastric polyps, p value polyps, p value GERD: < 0.05 GERD: < 0.05 are in gastro-esophageal are bold in bold reflux reflux disease disease<br />
No Yes Yes No 21 28 (42.8) (57.2) 21 28 (42.8) (57.2) 26 3 (10.3) (89.7) 26 3 (10.3) (89.7)<br />
Significant Significant p value p value < 0.05 < 0.05 are in are bold in bold<br />
Location No Location No 21 (42.8) 21 (42.8) 26 (89.7) 26 (89.7) 0.009 0.009<br />
Table Table 6 Risk 6 Risk value value for the for the significant variables variables in the in the multivariate<br />
Antrum Location Antrum Location 34 (47.9) 34 (47.9) 43 (76.8) 43 (76.8) 0.009 0.009<br />
analysis Table analysis Table 6 Risk 6 Risk value value for the for the significant significant variables variables in the in the multivariate multivariate<br />
Non Antrum Non Antrum antrum antrum 37 34 (52.1) (47.9) 37 34 (52.1) (47.9) 13 43 (23.2) (76.8) 13 43 (23.2) (76.8)<br />
analysis<br />
Size Non Size in antrum mm in mm 37 (52.1) 13 (23.2) 0.002 0.002 Variable Variable analysis<br />
Non antrum 37 (52.1) 13 (23.2)<br />
Odds Odds ratio ratio 95% 95% CI CI p value p value<br />
< Size 5 mm < Size in 5 mm in mm 30 (42.3) 30 (42.3) 39 (69.6) 39 (69.6) 0.002 0.002<br />
Variable Variable Hyperplastic polyps polyps<br />
Odds Odds ratio ratio 95% 95% CI CI p value p value<br />
≥< 5 mm ≥< 5 mm 41 30 (47.7) (42.3) 41 30 (47.7) (42.3) 17 39 (30.4) (69.6) 17 39 (30.4) (69.6)<br />
Anemia Hyperplastic Anemia Hyperplastic polyps polyps 4.28 4.28 (1.39–13.17) 0.022 0.022<br />
Paris ≥ 5 mm Paris ≥ 5 mm classification 41 (47.7) 41 (47.7) 17 (30.4) 17 (30.4)<br />
Single Anemia Anemia Single 2.85 4.282.85 (1.39–13.17) (0.95–8.59) (1.39–13.17) 0.025 0.022 0.025 0.022<br />
Ip Paris Ip Paris classification classification 10 (14) 10 (14) 5 (8.9) 5 (8.9) 0.371 0.371<br />
Size≥5 Single Size≥5 Single mm mm 2.851.85 (0.95–8.59) (1.29–2.67) (0.95–8.59) 0.048 0.025 0.048 0.025<br />
Is Ip Is Ip 58 10 (81.7) (14) 58 10 (81.7) (14) 43 5 (8.9) (76.8) 43 5 (8.9) (76.8) 0.496 0.371 0.496 0.371 Fundic Size≥5 Fundic Size≥5 mmgland polyps polyps 1.85 1.85 (1.29–2.67) (1.29–2.67) 0.048 0.048<br />
IIa Is IIa Is 358 (4.3) (81.7) 358 (4.3) (81.7) 843 (14.3) (76.8) 843 (14.3) (76.8) 0.055 0.496 0.055 0.496 Size Fundic Size Fundic < 5gland mm < 5gland mm polyps polyps 2.31 2.31 (1.37–4.11) < 0.001 < 0.001<br />
IIb, IIa IIc IIb, IIa IIc 03 (0) (4.3) 03 (0) (4.3) 08 (0) (14.3) 08 (0) (14.3) – 0.055 – 0.055 Size GP gastric GP Size < 5gastric mm < polyps, 5 mm polyps, GERD GERD gastro-esophageal 2.31 2.31 (1.37–4.11) reflux (1.37–4.11) reflux disease disease < 0.001 < 0.001<br />
GP IIb, gastric IIc GP IIb, gastric IIcpolyps, polyps, GERD GERD 0 (0) 0 gastro-esophageal (0) reflux reflux disease 0 disease (0) 0 (0) – –<br />
GP gastric GP gastric polyps, polyps, GERD GERD gastro-esophageal reflux reflux disease disease<br />
Significant GP gastric Significant GP gastric polyps, p value polyps, p value GERD < 0.05 GERD < 0.05 are gastro-esophageal in are bold in bold reflux reflux disease disease<br />
Significant Significant p value p value < 0.05 < 0.05 are in are bold in bold<br />
are the most common [9,10,11,12,13]. It has been suggested that<br />
the prevalence of hyperplastic polyps could be related to the high<br />
Argüello et al. reported the frequency of GP as 42.8% for<br />
hyperplastic polyps, and 37.7% for fundic gland polyps. The<br />
mean age of the patients was 65.6 years and 38% were males<br />
[9]. Carmack et al. found the incidence of GP as 6.3% in 121.564<br />
EGD. Fundic gland polyps were the most frequent polyp type,<br />
which accounted for 77% of all polyps of all polyps [6]. Fundic<br />
gland polyps were the second most common type (18.1%) of GPs<br />
lesions in our study. In the majority of series, hyperplastic polyps<br />
prevalence of H. pylori infection in our population (62.3%). Freeman<br />
et al. reported tendency of fundic gland polyps to arise in H. pylori<br />
-free stomachs [14] (OR 0.007, 95% CI 0.003–0.015). The same<br />
findings were also reported in Carmack et al. study (OR 0.007,<br />
95% CI 0.003–0.016) [6]. Fundic gland polyps tend also to arise<br />
in patients who receive long-course PPI treatment [14, 15]. The<br />
widespread of PPIs use and the low H. Pylori infection rate may be<br />
the most important reasons behind the large frequency of fundic<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
9
FEATURE<br />
gland polyps reported in American studies [6, 14]. Although in three<br />
Spanish series, hyperplastic polyps were the most common which<br />
is comparable to our study [8, 9, 16].<br />
Hyperplastic polyps are associated with chronic gastritis such<br />
as H. pylori gastritis, and particularly autoimmune gastritis.<br />
Patients with hyperplastic polyp have an increased risk of gastric<br />
adenocarcinoma [1, 17, 18].<br />
In our study, adenomas were detected in seven patients (5.5%).<br />
The majority of cases we reported were low-grade intestinal-type.<br />
These polyps constitute less than 10% and have a malignant<br />
potential. They are more common in communities where gastric<br />
cancer is frequent [19]. Malignant potential of adenomas is variable<br />
(6.8% − 55.3%) [20]. Risk factors for malignancy transformation are:<br />
high-grade dysplasia, and size of the lesion [19].<br />
It has been reported that between 16 and 37.5% of cases, and<br />
despite the endoscopic appearance of a polyp, the final histological<br />
study shows normal mucosa [6, 16]. In our study the percentage of<br />
biopsies with normal mucosa was 5.5%.<br />
Although the majority of GP do not cause symptoms, they can be<br />
the cause of bleeding and gastric obstruction. Frequently, GP are<br />
detected during EGD performed to study gastrointestinal symptoms<br />
not attributable to polyps or asymptomatic patients examined for<br />
other reasons [6, 21].<br />
In our study, an association between hyperplastic polyps and<br />
anemia, single polyps and size > 5 mm. It has been described in<br />
the literature between anaemia and hyperplastic polyps, while the<br />
gastrointestinal reflux was associated with fundic gland polyps [22].<br />
A total of 94 polyps were resected with snare. Five patients had<br />
hemorrhage requiring endoscopic treatment and bleeding was<br />
60<br />
53<br />
Table 7 Agreement between polypectomy and biopsy<br />
specimen in different histological types<br />
Histological type<br />
Biopsy<br />
Polypectomy<br />
Table 7 Agreement between<br />
specimen (n)<br />
polypectomy<br />
(n)<br />
and biopsy<br />
specimen Adenomas in different histological types<br />
Histological With low grade typedysplasia Biopsy 4 Polypectomy<br />
4<br />
With high grade dysplasia specimen 1 (n) (n) 1<br />
Fundic gland polyps<br />
Adenomas<br />
1 1<br />
Hyperplastic polyps<br />
With low grade dysplasia<br />
13<br />
4<br />
14<br />
4<br />
Type I neuroendoscrine tumor<br />
With high grade dysplasia<br />
1<br />
1<br />
1<br />
1<br />
Inflammatory mucosa<br />
Fundic gland polyps<br />
1<br />
1<br />
0<br />
1<br />
Hyperplastic polyps 13 14<br />
Type I neuroendoscrine tumor 1 1<br />
controlled Inflammatory by mucosa endoscopic procedures. 1 Perforation did 0not occur in<br />
any of our patients. In the literature, bleeding as a complication of<br />
gastric polypectomy was reported in 3.5% [23].<br />
Relationship between long-term PPIs use and fundic gland polyps’<br />
occurring has not yet been fully established. Jalving et al. [4] found<br />
in their study a significant association only in the subgroup of<br />
patients treated with PPI for over 1 year. Our data do not support a<br />
relationship between PPI and fundic gland polyps.<br />
In patients with GP, evaluating H. pylori infection state by obtaining<br />
biopsies of the surrounding gastric mucosa is recommended and<br />
treatment is required if present [24, 25].<br />
Hyperplastic polyps should be biopsied according to the British<br />
society of gastroenterology and an examination of the whole<br />
stomach should be made. H pylori infection should be detected and<br />
eradicated when present [24]. GP of the non-adenomatous type<br />
are at a low risk of malignant transformation, therefore endoscopic<br />
resection is not necessary.<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
50<br />
60<br />
53<br />
40<br />
50<br />
30<br />
40<br />
14 14<br />
20<br />
7<br />
30<br />
10<br />
14<br />
1<br />
14<br />
20<br />
7<br />
0<br />
10<br />
Cold snare Hot snare<br />
1<br />
EMR<br />
Monoblock Piece-meal<br />
0<br />
Fig. 2 The distribution of polypectomy. EMR endoscopic mucosal resection<br />
Cold snare Hot snare EMR<br />
Monoblock Piece-meal<br />
Fig. 2 The distribution of polypectomy. EMR endoscopic mucosal resection<br />
5<br />
5<br />
10
FEATURE<br />
Guidelines on management of hyperplastic polyps, recommend<br />
resection of polyps greater than 5 mm [26, 27].<br />
Complete removal of the adenoma should be performed when safe to<br />
do according to the British recommendations [24].<br />
Polypectomy is not required for sporadic fundic gland polyps. Biopsy of<br />
probable fundic gland polyps is recommended to exclude dysplasia. In<br />
patients with multiple fundic gland polyps who are under 40 years-old,<br />
or where biopsies specimens show dysplasia, colonoscopy should be<br />
performed to exclude familial adenomatous polyposis [24].<br />
Szaloki et al. reported that there were important disagreements in 12<br />
cases of examined forceps biopsy specimens. In 14 neoplastic, and<br />
1 hyperplastic polyps, the degree of dysplasia seen on histological<br />
examination of the forceps biopsy specimens differed from that<br />
observed for the resected specimens. Complete agreement between<br />
the histological results on ectomized polyp, and the forceps biopsy<br />
was observed in only 55.3% of the cases [28]. In our study, Adenomas<br />
analysis showed a 100% agreement between primary and final results.<br />
The agreement rate was 93% for hyperplastic polyps (13 polyps out of<br />
14). The overall agreement was of 95.3%.<br />
Ethics approval and consent to participate<br />
This study was performed according to the Declaration of Helsinki,<br />
following the guidelines for good clinical practice. “Habib Thameur<br />
Hospital ethics committee” approved the study protocol. All methods<br />
were carried out in accordance with relevant guidelines and regulations.<br />
Informed consent to participate in the study was obtained from<br />
participants.<br />
Consent for publication<br />
Not applicable.<br />
Competing interests<br />
The authors declare that they have no competing interests.<br />
Author details<br />
1<br />
<strong>Gastroenterology</strong> and Hepatology Department, Habib Thameur<br />
Hospital, Tunis, Tunisia. 2 Faculty of Medicine of Tunis, El Manar<br />
University, Tunis, Tunisia.<br />
Received: 8 July 2021 Accepted: 7 February <strong>2022</strong><br />
Published online: 19 February <strong>2022</strong><br />
Our study included the greatest number of EGD with patients diagnosed<br />
with GP in our country.<br />
Conclusion<br />
Gastric polyps’ frequency in our study was low (0.46%). Hyperplastic<br />
polyps are the most common gastric polyps in our country. In case of<br />
single polyps, biopsies are recommended to rule out a diagnosis of<br />
adenoma or hyperplastic polyps with dysplasia. Good knowledge of<br />
practical guidelines is important for the management of GP.<br />
Acknowledgements<br />
Not applicable.<br />
Authors’ contributions<br />
H.Y.: concept, design, definition of intellectual content, literature<br />
search, manuscript preparation, manuscript editing, manuscript review.<br />
N.B.: concept, design, definition of intellectual content, manuscript<br />
preparation, manuscript review. M.S.: definition of intellectual content,<br />
manuscript preparation. N.B.: design. A.O.: design, manuscript<br />
review. D.T.: manuscript review. D.G.: definition of intellectual content,<br />
manuscript review. All authors read and approved the final manuscript.<br />
Funding<br />
Not applicable.<br />
Availability of data and materials<br />
The data that support the findings of this study are available on<br />
request from the corresponding author, [HY]. The data are not publicly<br />
available due to [restrictions e.g. their containing information that could<br />
compromise the privacy of research participants].<br />
Declarations<br />
References<br />
1. Lesur G. Gastric polyps: how to recognize? Which to resect?<br />
Gastroenterol Clin Biol. 2009;33(4):233–9.<br />
2. Voutilainen M, Mantynen T, Kunnamo I, Juhola M, Mecklin JP,<br />
Farkkila M. Impact of clinical symptoms and referral volume on<br />
endoscopy for detecting peptic ulcer and gastric neoplasms. Scand<br />
J Gastroenterol. 2003;38(1):109–13.<br />
3. Barbosa SHB, Lazaro GCF, Franco LM, Valenca JTJ, Nobre<br />
SMA, Souza M. Agreement between different pathologists in<br />
histopathologic diagnosis of 128 gastric polyps. Arq Gastroenterol.<br />
2017;54(3):263–6.<br />
4. Jalving M, Koornstra JJ, Wesseling J, Boezen HM, Jong DE,<br />
Kleibeuker SJH. Increased risk of fundic gland polyps during<br />
long-term proton pump inhibitor therapy. Aliment Pharmacol Ther.<br />
2006;24:1341–8.<br />
5. Elhanafi S, Saadi M, Lou W, Mallawaarachchi I, Zuckerman AM,<br />
Othman MO. Gastric polyps: a association with Heli-cobacter<br />
pylori status and the pathology of the surrounding mucosa, a cross<br />
sectional study. World J Gastrointest Endosc. 2015;7:995–1002.<br />
6. Carmack SW, Genta RM, Schuler CM, Saboorian MH. The current<br />
spectrum of gastric polyps: a 1-year national study of over 120,000<br />
patients. Am J Gastroenterol. 2009;104(6):1524–32.<br />
7. Morais DJ, Yamanaka A, Zeitune JM, Andreollo NA. Gastric polyps:<br />
a retrospective analysis of 26,000 digestive endoscopies. Arq<br />
Gastroenterol. 2007;44(1):14–7.<br />
8. Garcia Alonso FJ, Marti Mateos RM, Gonzalez Martin JA, Foruny<br />
JR, Vazquez Sequeiros E, Boixeda de Miquel D. Gastric polyps:<br />
analysis of endoscopic and histological features in our center. Rev<br />
Esp Enferm Dig. 2011;103(8):416–20.<br />
9. Argüello Viúdez L, Córdova H, Uchima H, Sánchez Montes C, Ginès<br />
À, Araujo I, et al. Gastric polyps: retrospective analysis of 41,253<br />
upper endoscopies. Gastroenterol Hepatol. 2017;40(8):507–14.<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
11
FEATURE<br />
10. Bassene ML, Diallo S, Thioubou MA, Diallo A, Gueye MN, Diouf ML.<br />
Gastric polyps in a digestive endoscopy center in Dakar. Open J<br />
Gastroenterol. 2017;7(10):279–86.<br />
11. Olmez S, Sayar S, Saritas B, Savas AY, Avcioglu U, Tenlik I, et<br />
al. Evaluation of patients with gastric polyps. North Clin Istanb.<br />
2018;5(1):41–6.<br />
12. Ljubicic N, Kujundzic M, Roic G, Banic M, Cupic H, Doko M, et al.<br />
Benign epithelial gastric polyps-frequency, location, and age and sex<br />
distribution. Coll Antropol. 2002;26(1):55–60.<br />
13. Sivelli R, Del Rio P, Bonati L, Sianesi M. Gastric polyps: a clinical<br />
contribution. Chir Ital. 2002;54(1):37–40.<br />
14. Freeman HJ. Proton pump inhibitors and an emerging epidemic<br />
of gastric fundic gland polyposis. World J Gastroenterol.<br />
2008;14:1318–20.<br />
15. Raghunath AS, O’Morain C, McLoughlin RC. Review article: the<br />
long-term use of proton-pump inhibitors. Aliment Pharmacol Ther.<br />
2005;22(11):55–63.<br />
16. Macenlle García R, Bassante Flores LA, Fernández Seara J. Pólipos<br />
gástricos epiteliales. Estudio retrospectivo 1995–2000. Rev Clin<br />
Esp. 2003;203(8):368–72.<br />
17. Abraham SC, Singh VK, Yardley JH, Wu TT. Hyperplastic polyps of<br />
the stomach: associations with histologic patterns of gastritis and<br />
gastric atrophy. Am J Surg Pathol. 2001;25(4):500–7.<br />
18. Scoazec JY. Les polypes gastriques: pathologie et génétique. Ann<br />
Pathol. 2006;26(3):173–99.<br />
19. Hattori T. Morphological range of hyperplastic polyps and<br />
carcinomas arising in hyperplastic polyps of the stomach. J Clin<br />
Pathol. 1985;38(6):622–30.<br />
20. Stolte M. Clinical consequences of the endoscopic diagnosis of<br />
gastric polyps. Endoscopy. 1995;27:32–7.<br />
21. Gencosmanoglu R, Sen Oran E, Kurtkaya Yapicier O, Avsar E, Sav<br />
A, Tozun N. Gastric polypoid lesions: analysis of 150 endoscopic<br />
polypectomy specimens from 91 patients. World J Gastroenterol.<br />
2003;9(10):2236–9.<br />
22. Sonnenberg A, Genta RM. Prevalence of benign gastric polyps in a<br />
large pathology database. Digest Liver Dis. 2015;47:164–9.<br />
23. Russo A, Sanfi lippo G, Magnano A, La Malfa M, Belluardo N.<br />
Complications de la polypectomie endoscopique gastrique et<br />
duodénale expérience italienne. Acta Endosc. 1986;16(5):251.<br />
24. Goddard AF, Badreldin R, Pritchsard DM, Walker MM, War-ren B. on<br />
behalf of the British Society of <strong>Gastroenterology</strong>. The management<br />
of gastric polyps. Gut. 2010;59:1270–6.<br />
25. Sharaf RN, Shergill AK, Odze RD, Krinsky ML, Fukami N, Jain R, et<br />
al. ASGE Standards of Practice Committee. Endoscopic mucosal<br />
tissue sampling. Gastrointest Endosc. 2013;78:216–24.<br />
26. Evans JA, Chandrasekhara V, Chathadi KV, Decker GA, Early DS,<br />
Fisher DA, et al. ASGE guideline: the role of endoscopy in the<br />
management of premalignant and malignant conditions of the<br />
stomach. Gastrointest Endosc. 2015;82:1–8.<br />
27. Han AR, Sung CO, Kim KM, Park C, Min B, Lee JH, et al.<br />
Theclinicopathological features of gastric hyperplastic polyps with<br />
neoplastic transformations: a suggestion of indication for endoscopic<br />
polypectomy. Gut Liver. 2009;3:271–5.<br />
28. Szaloki T, Toth V, Tiszlavicz L, Czako L. Flat gastric polyps: results<br />
of forceps biopsy, endoscopic mucosal resection, and long-term<br />
follow-up. Scand J Gastroenterol. 2006;41(9):1105–9.<br />
Publisher’s Note<br />
<strong>Spring</strong>er Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affi liations.<br />
WHY NOT WRITE FOR US?<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
<strong>Gastroenterology</strong> <strong>Today</strong> welcomes the submission of<br />
clinical papers and case reports or news that<br />
you feel will be of interest to your colleagues.<br />
Material submitted will be seen by those working within all<br />
UK gastroenterology departments and endoscopy units.<br />
All submissions should be forwarded to info@mediapublishingcompany.com<br />
If you have any queries please contact the publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
12
FASTER DIAGNOSIS OF GASTRIC CANCER<br />
FEATURE<br />
Gastric cancer is typically diagnosed at a very late stage,<br />
leading to a poor prognosis for the patient, and the strain<br />
on healthcare services through the COVID-19 pandemic<br />
has only made things worse. However, detection of precancerous<br />
conditions – such as atrophic gastritis (AG) and<br />
gastric intestinal metaplasia (GIM) – before endoscopy could<br />
potentially support diagnostic pathways, allowing doctors<br />
in primary care to identify and prioritise patients for whom<br />
endoscopy would be useful, streamlining NHS resources and<br />
improving patient outcomes.<br />
What are AG and GIM?<br />
AG is a chronic inflammatory condition of the gastric mucosa.<br />
It can be an autoimmune disorder, but most commonly arises<br />
following prolonged inflammation caused by Helicobacter<br />
pylori<br />
infection. This disrupts the mucus barrier that helps<br />
to protect the cells of the stomach lining from digestive<br />
juices, causing them to be slowly destroyed. AG significantly<br />
increases the risk of stomach cancer, with 18 % of cases<br />
progressing to cancer within 10 years. However, studies<br />
suggest that in some cases the progression of AG can be<br />
halted, and even improved, reinforcing the importance of early<br />
diagnosis and monitoring. 1<br />
GIM is common in cases of AG and occurs when the cells<br />
of the stomach lining are replaced with cells similar to the<br />
lining of the intestines. Again, H. pylori is often implicated in<br />
this process, which predisposes individuals to intestinal-type<br />
gastric adenocarcinoma and neuroendocrine tumours (NETs).<br />
Patients with GIM are often over 50 years of age, and the risk<br />
is further increased by factors such as smoking or having a<br />
first-degree relative with gastric cancer.<br />
Challenges of diagnosis<br />
The current gold standard for diagnosing AG and GIM is<br />
gastroscopy with targeted biopsies, which relies on referral<br />
of patients from primary care. However, AG and GIM are often<br />
asymptomatic – or present with very general symptoms such as<br />
stomach pain, loss of appetite, nausea or vomiting, anaemia and<br />
stomach ulcers – making them hard to detect. Tests for<br />
H. pylori infection, along with blood tests for levels of<br />
pepsinogens and gastrin-17, may help to identify some patients<br />
for whom a referral would be beneficial. However, current<br />
practice is not to actively look for AG and GIM cases before<br />
endoscopy, and so patients may remain undiagnosed in primary<br />
care for prolonged periods if they do not qualify for referral.<br />
Rapid detection of AG and GIM<br />
GastroPanel from BIOHIT is a simple, non-invasive blood test<br />
that can be used in primary care settings for effective diagnosis<br />
of AG and GIM. It gives detailed information on the structure<br />
and function of the stomach mucosa, by quantifying pepsinogen<br />
I, pepsinogen II and gastrin-17, and can also differentiate the<br />
cause of AG by identifying IgG antibodies to H. pylori. Using<br />
GastroPanel in targeted groups of at-risk patients could help to<br />
direct referrals more effectively. As well as detecting cancers<br />
at an earlier and more curable stage, reducing the number of<br />
gastroscopies in lower risk patients would reduce both the cost<br />
and volume burden on healthcare resources, without adversely<br />
affecting patient care.<br />
For more information about GastroPanel<br />
contact: info@biohithealthcare.co.uk<br />
1 . Kong YJ, Yi HG, Dai JC, Wei MX. Histological changes of gastric mucosa after Helicobacter pylori eradication: A systematic review and meta-analysis. World J Gastroenterol 2014; 20(19): 5903-5911<br />
For the early diagnosis<br />
of gastric cancer risk<br />
Reduce endoscopy waiting lists and<br />
improve the diagnostic pathway for<br />
patients, through an earlier, faster<br />
and more cost-effective approach.<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
www.biohithealthcare.co.uk<br />
13
FEATURE<br />
ENDOSCOPIC RETROGRADE APPENDICITIS<br />
THERAPY VERSUS LAPAROSCOPIC<br />
APPENDECTOMY VERSUS OPEN APPENDECTOMY<br />
FOR ACUTE APPENDICITIS: A PILOT STUDY<br />
Zhemin Shen 1 , Peilong Sun 1*† , Miao Jiang 2† , Zili Zhen 1 , Jingtian Liu 1 , Mu Ye 1 and Weida Huang 1<br />
Shen et al. BMC <strong>Gastroenterology</strong> (<strong>2022</strong>) 22:63 https://doi.org/10.1186/s12876-022-02139-7<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
14<br />
Abstract<br />
Background<br />
An increasing number of studies have shown the merits of endoscopic<br />
retrograde appendicitis therapy (ERAT) in diagnosing and treating acute<br />
uncomplicated appendicitis. However, no related prospective controlled<br />
studies have been reported yet. Our aim is to assess the feasibility and<br />
safety of ERAT in the treatment of acute uncomplicated appendicitis.<br />
Methods<br />
In this open-label, randomized trial, participants were randomly allocated<br />
to the ERAT group, laparoscopic appendectomy (LA) group and open<br />
appendectomy (OA) group. The primary outcome was the clinical success<br />
rate of the treatment. Intention-to-treat analysis was used in the study.<br />
Results<br />
The study comprised of 99 patients, with 33 participants in each<br />
group. The clinical success rate was 87.88% (29/33), 96.97% (32/33)<br />
and 100% (33/33) in the ERAT, LA and OA group, respectively. In the<br />
ERAT group, 4 patients failed ERAT due to difficult cannulation. In LA<br />
group, 1 patient failed because of abdominal adhesion. There were no<br />
significant differences among the three treatment groups regarding the<br />
clinical success rate (P=0.123). The median duration of follow-up was<br />
22 months. There were no significant differences (P =0.693) among the<br />
three groups in terms of adverse events and the final crossover rate of<br />
ERAT to surgery was 21.21% (7/33).<br />
Conclusion<br />
ERAT can serve as an alternative and efficient method to treat acute<br />
uncomplicated appendicitis.<br />
Trial registration The study is registered with the WHO Primary Registry-<br />
Chinese Clinical Trial Registry (ChiCTR1900025812).<br />
Keywords<br />
Acute appendicitis, Endoscopic retrograde appendicitis therapy,<br />
Appendectomy, Randomized controlled trial<br />
Introduction<br />
Acute appendicitis is one of the most common causes of acute<br />
abdominal pain clinically [1]. Appendectomy has long been standard<br />
treatment for acute appendicitis. However, there are a series of potential<br />
*Correspondence: sunpeilong@fudan.edu.cn<br />
†<br />
Peilong Sun and Miao Jiang contributed equally in the trial<br />
1<br />
Department of General Surgery, Jinshan Hospital, Fudan University, Shanghai, China<br />
©The Author(s) <strong>2022</strong><br />
postoperative complications, such as postoperative bleeding, wound<br />
infection and intestinal obstruction [2, 3], and the overall complication<br />
rate has been reported to be 8.2–31.4% [1]. Moreover, negative<br />
appendectomy is also a nonnegligible problem [4]. As previous studies<br />
suggested that perforation may not be an inevitable consequence of<br />
acute appendicitis, there is a division of opinions on performing surgery<br />
on patients with acute uncomplicated appendicitis [5]. Thus, developing<br />
a safe and efficient nonoperative method has been an agenda for<br />
treating acute uncomplicated appendicitis.<br />
Endoscopic retrograde appendicitis therapy (ERAT) was firstly<br />
reported by Liu et al. as being inspired by endoscopic retrograde<br />
cholangiopancreatography (ERCP) [6]. ERAT is a novel, nonoperative and<br />
minimally invasive method of treating acute uncomplicated appendicitis.<br />
Recently, there has been additional studies of the use of ERAT for<br />
treating acute uncomplicated appendicitis [7,8,9]. The results of these<br />
3 trials indicated the clinical value of ERAT, including both diagnostic<br />
and therapeutic aspects. Thus, ERAT has the potential to become an<br />
alternative treatment method for acute appendicitis, especially in patients<br />
who are deemed as high-risk candidates for surgery. However, these<br />
previous studies were all retrospective, and no prospective study has<br />
been reported yet. To address this issue, we conducted a prospective<br />
randomized controlled trial to compare ERAT with laparoscopic<br />
appendectomy (LA) and open appendectomy (OA), and evaluated the<br />
feasibility and safety of ERAT in treating acute uncomplicated appendicitis.<br />
Method<br />
Patients<br />
The period of patient enrollment was between January 2018 and August<br />
2019. A prospective, open-label, randomized controlled study was<br />
conducted at Jinshan Hospital, Fudan University. Patients diagnosed<br />
with acute uncomplicated appendicitis were enrolled in the study.<br />
The inclusion criteria were as follows: (1) patient age over 18 years and<br />
under 80 years; (2) Alvarado score >5 [1]; (3) suspicious (or could not<br />
be excluded) acute appendicitis diagnosed by an abdominal CT scan,<br />
which was indicated by a dilated appendix with a diameter greater than<br />
6 mm, a thickened cecal wall, and periappendiceal fat inflammation, with<br />
or without an appendicolith [10].<br />
Exclusion criteria were as follows: (1) suspected acute complicated<br />
appendicitis with perforation or gangrene; (2) appendiceal diameter
FEATURE<br />
Fig. 1 Procedures of endoscopic retrograde appendicitis therapy (ERAT). a Congestion and edema around the mucosa of appendix orifice. b The<br />
endoscopic retrograde appendicography (ERA) fluoroscopy showed filling defect in the appendix lumen (arrows), which indicated the presence<br />
of appendicoliths. c Cannulation of catheter along the guidewire with sand-like appendicoliths excretion and pus drainage inside the appendix<br />
lumen, confirming acute appendicitis. d Retracting the appendicoliths by the extraction basket. e After appendicolith being retracted, the appendix<br />
lumen was fully filled with contrast media under ERA. f Stenting for keeping pus drainage<br />
greater than 15 mm, which usually indicates malignancy [11]; (3)<br />
patients under the age of 18 years or over 80 years; (4) patients<br />
with the following contradictions for receiving colonoscopy, surgery<br />
or anesthesia: (a) severe cardiopulmonary insufficiency, psychiatric<br />
dysfunction or coma; (b) acute diffuse peritonitis, which is defined<br />
as diffuse abdominal tenderness, rebound tenderness and muscular<br />
tension; (c) acute gastroenteritis (dysentery, explosive ulcerative colitis);<br />
(d) concurrent menses; (e) intestinal obstruction; (f) acute gastrointestinal<br />
hemorrhage; (g) recent gastrointestinal or pelvic operation or<br />
radiotherapy; (h) allergy to contrast medium; (i) hemorrhagic tendency<br />
because of long-term use of corticosteroids or anticoagulant treatment;<br />
(5) patients undergoing any other clinical trial.<br />
Written informed consent was obtained from all participants. The study<br />
was conducted according to the Declaration of Helsinki and approved<br />
by the Ethics Committee of Jinshan Hospital, Fudan University (No.<br />
2017–24) on May 17th, 2017. The study is registered with the WHO<br />
Primary Registry-Chinese Clinical Trial Registry (ChiCTR1900025812)<br />
(09/09/2019).<br />
Randomization was conducted by a computer-generated randomization<br />
number (1:1:1) by statisticians. The final allocation was concealed in<br />
an opaque envelope. The allocation was reported to the doctors and<br />
patients immediately prior to the intervention.<br />
Preintervention preparation<br />
All patients intravenously received antibiotic treatment (1.5 g cefuroxime<br />
with 100 ml normal saline, 0.5% metronidazole 100 ml) immediately<br />
after being clinically diagnosed. In the ERAT group, the patients orally<br />
took 328.8 g polyethylene glycol (PEG) electrolyte solution with 2000 ml<br />
water before ERAT for bowel preparation. When the excrement became<br />
a clear liquid, the patients were well prepared to undergo ERAT.<br />
ERAT procedure<br />
Similar to that in previous studies [7,8,9], the ERAT procedure was<br />
performed as follows (Fig. 1):<br />
First, a full and careful examination of the large intestine was performed<br />
by a colonoscope (CF-H260AI, Olympus, Japan) with a transparent cap.<br />
Then, the colonoscope was located to the appendiceal orifice to check<br />
the appendiceal mucosa to determine whether there was inflammation<br />
or any other abnormalities. With the help of a transparent cap, the tip<br />
of the catheter (BDC-12/55–7/1810/55–7/18, Micro-Tech Co. Ltd.,<br />
Nanjing, China) was placed in the appendiceal orifice, and a 0.035-inch<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
15
FEATURE<br />
guidewire (MTN-BM-89/45-A, Micro-Tech Co. Ltd., Nanjing, China) was<br />
gently and deeply inserted into the appendiceal lumen over the catheter.<br />
Finally, the catheter moved forward into the appendiceal lumen along<br />
the guidewire. To make a definite diagnosis, the appendiceal lumen<br />
was filled with contrast medium (ioversol) for endoscopic retrograde<br />
appendicography (ERA) fluoroscopy. Next, the appendiceal lumen was<br />
flushed repeatedly with gentamicin (240,000 units with 100 ml normal<br />
saline) and 0.5% metronidazole 100 ml to clear pus and other infectious<br />
contents, such as sand-like appendicoliths. Then, an extraction basket<br />
(SEB-A- 30/55–7/200, Micro-Tech Co., Ltd., Nanjing, China) was used<br />
to extract the remaining appendicoliths if necessary. Finally, a plastic<br />
stent (SPSOF7-7, Cook, USA) was placed routinely in the appendiceal<br />
orifice to maintain pus drainage.<br />
Surgical treatment<br />
All operations were performed by surgeons from a same team. In the<br />
LA group, the three-port technique (umbilical, 10 mm; suprapubic, 5<br />
mm; right lower abdomen, 10 mm) was chosen. In the OA group, a<br />
McBurney muscle-splitting incision technique was used.<br />
and CRP level; the duration of diet resumption; the length of hospital<br />
stay (LOS); the total cost of the primary hospital stay; adverse events<br />
during follow-up period and final crossover rate of ERAT to surgery.<br />
Definition<br />
The clinical success of ERAT is defined as successful appendix<br />
cannulation with complete resolution of symptoms and normalization<br />
of inflammatory markers, including WBC count, neutrophil percentages<br />
and CRP. Difficult appendix cannulation is defined as failure to achieve<br />
successful appendix cannulation within 15 min. The assessment of<br />
abdominal pain degree is based on visual analog scales (VAS). In the<br />
VAS, scores of 0 and 10 represent no pain and most severe pain,<br />
respectively. Complete relief of abdominal pain refers to a VAS score of<br />
0.<br />
The diagnostic criteria of acute appendicitis by ERAT mainly consist<br />
of ERA fluoroscopy images, inflammation of the appendiceal mucosa<br />
observed under endoscopy and the presence of pus or appendicoliths<br />
inside the appendiceal lumen [8].<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
16<br />
Postintervention management<br />
After ERAT or surgery was performed, patients were sent back to the<br />
ward and monitored carefully. Patients continued to receive antiinflammatory<br />
therapy when necessary. In the ERAT group, patients<br />
were given a soft diet later on the same day and resumed a normal diet<br />
when the soft diet was tolerated. In the LA and OA groups, a soft diet<br />
was started 24 h after surgery, and a normal diet was given when the<br />
soft diet was completely tolerated. All patients were asked about their<br />
clinical presentation every day. Routine blood tests, including the white<br />
blood cell (WBC) count, neutrophil percentages and C-reactive protein<br />
(CRP) level, were performed on day 1, 3, and 5 in a similar fashion after<br />
ERAT or surgery. Patients were discharged when all symptoms were<br />
completely relieved and inflammatory markers (including the WBC count,<br />
neutrophil percentages, and CRP level) returned to normal. If ERAT<br />
failed or abdominal pain persisted after ERAT, LA or OA was performed<br />
immediately.<br />
Follow-up<br />
Fourteen days after ERAT, all patients in the ERAT group were scheduled<br />
for outpatient services to inform doctors of their symptoms after<br />
discharge. Patients then received an abdominal X-ray to check the<br />
status of the stent. If the stent was not discharged spontaneously with<br />
defecation, colonoscopy was recommended to retrieve the stent.<br />
Follow-up was performed by telephone interview every 3 months for<br />
the first half year, and then every 6 months till November 2020. In<br />
the ERAT group, recurrence of abdominal pain or appendicitis after<br />
ERAT, including the relevant treatment, was mainly investigated. In the<br />
LA group and OA group, the survey mainly included postoperative<br />
complications such as wound infection, persistent incision pain and<br />
intestinal obstruction. Follow-up was performed until the end of the<br />
study period.<br />
Outcomes<br />
The primary outcome was the clinical success of the treatment. The<br />
secondary outcomes were as follows: the duration of complete relief of<br />
abdominal pain and body temperature; the duration of normalization of<br />
inflammatory markers including the WBC count; neutrophil percentages<br />
In the ERAT group, adverse events mainly indicated the recurrence of<br />
acute appendicitis. In the LA and OA groups, adverse events suggested<br />
postoperative complications.<br />
Statistical analysis<br />
As this was a pilot trial, we did not perform a power calculation. On the<br />
basis of our yearly caseload of approximately 240 cases and estimated<br />
recruitment of one fifth of eligible cases, we aimed to enroll at least<br />
96 patients within a 2-year period. Qualitative data are expressed as<br />
numbers (n) and percentages (%) and were compared by using the χ 2<br />
test or Fisher’s exact test when appropriate.<br />
Quantitative data are expressed as the mean ±standard deviation<br />
(SD) or median with 25th and 75th percentiles, as appropriate. For<br />
normally distributed quantitative data (such as age, temperature, WBC<br />
count), one-way analysis of variance (ANOVA) was used to compare<br />
the differences among the three groups. For nonnormally distributed<br />
quantitative data (neutrophil percentages, CRP, Alvarado scores, VAS<br />
scores, the duration of normalization of inflammatory markers, the<br />
duration of normal diet and body temperature, total cost and length of<br />
hospitalization), the Kruskal–Wallis test followed by all pairwise multiple<br />
comparisons was used to detect statistical significance. Bonferroni’s<br />
correction was used for multiple hypothesis testing. The data were<br />
analyzed by IBM SPSS software version 22 (SPSS, Chicago, Illinois,<br />
USA). A P value
FEATURE<br />
Fig. 2 Trial profile<br />
Appendicoliths were present in 12 patients (36.36%) in the ERAT group,<br />
16 patients (48.48%) in the LA group and 11 patients (33.33%) in the<br />
OA group. There were no significant differences in appendicoliths among<br />
the three groups (p =0.516).<br />
Treatment success rate and efficacy of ERAT<br />
Table 2 shows the clinical outcomes of the three groups. Successful<br />
treatment was achieved in 29 patients (87.88%) in the ERAT group,<br />
32 patients (96.97%) in the LA group and 33 patients (100%) in the<br />
OA group. No significant differences were observed among the three<br />
groups (P=0.123). Among the three groups, ERAT failed in four patients<br />
(12.12%) due to difficult cannulation, and LA was performed in these<br />
patients later on the same day, with uneventful recoveries. All these<br />
four patients were found appendicoliths before ERAT. Appendicoliths<br />
of the other 8 patients who were found to have appendicoliths by CT<br />
scan were removed by ERAT. Stents were placed in 29 patients with<br />
successful ERAT. In the LA group, a 63-year-old patient failed LA due<br />
to extensive abdominal adhesion caused by surgical reduction for<br />
intussusception 3 years ago. The patient was later converted to OA<br />
successfully.<br />
Among 29 patients who underwent successful ERAT, most achieved<br />
complete abdominal pain relief immediately after the procedure. The<br />
duration of normalization of inflammatory markers, including the WBC<br />
count, neutrophil percentages and CRP level, did not significantly differ<br />
among the ERAT, LA and OA groups (P =0.351, P=0.607, P=0.147,<br />
respectively). The overall cost in the LA group was significantly<br />
higher (P
FEATURE<br />
Table 1 Basic characteristics<br />
ERAT group (n=33) LA group (n=33) OA group<br />
(n=33)<br />
P value<br />
Age, mean (SD), years 44.12±16.95 43.24±15.41 45.45±18.04 0.866<br />
Male, n (%) 18 (54.55) 17 (51.52) 19 (57.58) 0.967<br />
Abdominal surgery history, n (%) 8 (24.24) 8 (24.24) 7 (21.21) > 0.999<br />
Symptoms<br />
Migrated right lower abdominal pain, n (%) 29 (87.88) 22 (66.67) 25 (75.76) 0.142<br />
Nausea, n (%) 22 (66.67) 23 (69.70) 17 (51.52) 0.285<br />
Vomiting, n (%) 5 (15.15) 4 (12.12) 9 (27.27) 0.345<br />
Anorexia, n (%) 33 (100) 32 (96.97) 32 (96.97) > 0.999<br />
Fever, n (%) 18 (54.55) 13 (39.39) 17 (51.52) 0.532<br />
Temperature (℃) 37.37±0.77 37.13±0.57 37.22±0.58 0.317<br />
Signs<br />
Right lower abdominal tenderness, n (%) 33 (100) 33 (100) 33 (100)<br />
Rebound tenderness, n (%) 17 (51.52) 15 (45.45) 20 (57.58) 0.654<br />
Laboratory examination<br />
WBC count (× 10 9 /L) 11.78±3.84 11.87±3.80 13.64±3.87 0.091<br />
Neutrophil percentages, median (25th, 75th percentile) 0.84 (0.78, 0.87) 0.81 (0.76,0.85) 0.83 (0.76, 0.90) 0.233<br />
CRP (mg/L) 0.749<br />
0–20 18 (54.6) 20 (60.6) 25 (75.76)<br />
21–50 7 (21.2) 7 (21.2) 6 (18.18)<br />
> 50 8 (24.2) 6 (18.2) 2 (6.06)<br />
CT scan<br />
Local Cecal Wall thickening, n (%) 4 (12.12) 0 (0) 1 (3.03) 0.123<br />
Periappendiceal fat inflammation, n (%) 25 (75.76) 27 (81.82) 29 (87.88) 0.496<br />
Intraluminal appendicolith, n (%) 12 (36.36) 16 (48.48) 11 (33.33) 0.516<br />
Alvarado scores, median (25th, 75th percentile) 8 (7, 9) 8 (6, 9) 8 (7, 9) 0.127<br />
VAS scores, median (25th,75th percentile) 6 (5, 7) 7 (6, 7) 6 (6, 7) 0.054<br />
ERAT, endoscopic retrograde appendicitis therapy; LA, laparoscopic appendectomy; OA, open appendectomy; SD, standard deviation; WBC, white blood cell; CRP,<br />
C-reactive protein; VAS, visual analog scale<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
9 patients only received colonoscopy for one time. Moreover, for the 4<br />
patients who failed ERAT, they also received two-times intervention since<br />
they underwent both ERAT and LA. Table 3 summarizes the adverse<br />
events which arose in the three groups. No significant differences<br />
(P =0.693) were found among the three treatment groups. In the ERAT<br />
group, three patients (9.09%) reported right lower abdominal pain and<br />
were diagnosed with recurrent acute appendicitis. The recurrence time<br />
was 4, 6 and 11 months, respectively. Two of them were found to have<br />
intraluminal appendicoliths during primary hospitalization. These three<br />
patients received LA later at the same day. Thus, there were totally 7<br />
patients in the ERAT group who crossed over to the LA group, and<br />
the final crossover rate is 21.21% (7/33). In the LA group, one patient<br />
(3.03%) was found to have a fluid collection around the ileocecal<br />
junction and the fluid collection gradually diminished later on. In the<br />
OA group, three patients (9.09%) were found to have postoperative<br />
complications. Two of them exhibited wound infections within one<br />
month after surgery. Another patient complained of occasional incision<br />
pain one month after OA, especially on rainy days.<br />
Discussion<br />
In this pilot RCT, we have shown that ERAT is feasible and safe for<br />
treating acute uncomplicated appendicitis. Overall, nearly 25% of<br />
patients accepted to participate the trial, suggesting the potential<br />
clinical extension of ERAT since it is a brand-new treating method and<br />
no patient has ever heard of it before. Appendicoliths and infection are<br />
considered as important causes of acute appendicitis and ERAT could<br />
treat acute uncomplicated appendicitis by appendicolith extraction, pus<br />
drainage and intraluminal pressure reduction to relieve the syndromes<br />
and ultimately treat acute appendicitis [7, 12, 13]. Although this pilot trial<br />
was not adequately powered to detect differences in treatment efficacy,<br />
the results are useful to inform future clinical application of ERAT.<br />
Although there are some complications associated to colonoscopy,<br />
the adverse event rates were less than 1% and 0.2% for bleeding and<br />
perforation respectively and there were no any adverse events related<br />
to colonoscopy among the patients underwent ERAT treatment in our<br />
study [14]. Moreover, ERAT compares favorably with the results of<br />
surgery in terms of the postintervention recovery of patients. Regarding<br />
the period of body temperature normalization, inflammatory markers<br />
(including the WBC count, neutrophil percentages and CRP level)<br />
and the length of hospitalization, our data did not indicate significant<br />
differences among the three groups (P =0.194, P=0.351, P=0.607,<br />
P=0.147, P=0.054, respectively), which showed that the clinical<br />
efficacy of ERAT was similar to that of surgery. As for different surgical<br />
methods, LA showed a similar clinical efficacy as OA, while LA yielded<br />
18
FEATURE<br />
Table 2 Clinical outcome<br />
ERAT group<br />
(n = 33)<br />
LA group<br />
(n=33)<br />
OA group<br />
(n=33)<br />
P value ERAT-LA ERAT-OA LA-OA<br />
Treatment Success, n (%) 29 (87.88) 32 (96.97) 33 (100) 0.123<br />
Definite acute uncomplicated appendicitis, n (%) 33 (100) 33 (100) 33 (100)<br />
Appendicoliths removal, n (%) 8 (66.67) NA NA<br />
Stent d rainage, n(%) 29 (87.88) NA NA<br />
Failed cannulation, n (%) 4 (12.12) NA NA<br />
Transferred to surgery, n (%) 4 (12.12) NA NA<br />
Normalization of WBC count, days 0.351<br />
0–1 16 12 17<br />
1–3 5 12 9<br />
> 3 2 0 2<br />
Normalization neutrophil percentages, days 0.607<br />
0–1 15 11 7<br />
1–3 11 14 19<br />
> 3 4 2 2<br />
Normalization of CRP, days 0.147<br />
0–1 3 1 3<br />
1–3 5 10 2<br />
> 3 7 2 3<br />
Normalization of temperature, median (25th, 75th 2 (1, 3) 1 (1, 2) 2 (1, 3) 0.194<br />
percentile), days<br />
LOS, median (25th, 75th percentile), days 5 (4, 6) 4 (3, 5) 4 (3, 5) 0.054<br />
Total cost, median (25th, 75th percentile), RMB 10,983.25<br />
(10,210.26,<br />
13,028.25)<br />
14,517.22<br />
(12,991.05,<br />
15,528.25)<br />
8246.82<br />
(6819.71,<br />
9530.22)<br />
< 0.001 0.001 < 0.001 < 0.001<br />
ERAT, endoscopic retrograde appendicitis therapy; LA, laparoscopic appendectomy; OA, open appendectomy; NA, not applicable; WBC, white blood cell; CRP,<br />
C-reactive protein; LOS, length of hospital stay<br />
Table 3 Follow-up<br />
ERAT group<br />
(n=33)<br />
LA group<br />
(n=33)<br />
OA group (n=33)<br />
P value<br />
Stent discharged, n (%) 29 (87.88) NA NA<br />
Spontaneously discharged, n (%) 9 (31.03) NA NA<br />
Retrieved, n (%) 20 (68.97) NA NA<br />
Adverse events, n (%) 3 (9.09) 1 (3.03) 3 (9.09) 0.693<br />
Recurrence, n (%) 3 (9.09) NA NA<br />
Patients with appendicolith at first admission, n (%) 2 (6.06) NA NA<br />
Patients without appendicolith at first admission, n (%) 1 (3.03) NA NA<br />
Crossover rate (%) 21.21 3.03 NA<br />
Complications<br />
Wound infection, n (%) NA 0 2 (6.06)<br />
Abdominal or incisional pain, n (%) NA 0 1 (3.03)<br />
Abdominal fluid collection, n (%) NA 1 (3.03) 0<br />
Obstructive symptoms, n (%) NA 0 0<br />
ERAT, endoscopic retrograde appendicitis therapy; LA, laparoscopic appendectomy; OA, open appendectomy; NA, not applicable<br />
fewer complications, although there was no statistical significance<br />
(P =0.693) in the current study. OA, as the traditional treatment method,<br />
is the most reliable therapy for acute appendicitis. However, OA seems<br />
to cause more adverse events, such as wound infection, which reduces<br />
the quality of life of patients.<br />
protect beneficial or commensal microorganisms from contamination<br />
with pathogenic organisms [15]. In addition, evidence has shown that<br />
appendectomy may slightly increase the incidence of Crohn’s disease<br />
[16]. In patients with acute uncomplicated appendicitis, ERAT may<br />
preserve the function of the appendix with a satisfactory therapeutic<br />
effect. To some extent, ERAT may be essential for intestinal immune<br />
A previous study suggested that the appendix could preserve and function, which is another strength of the treatment.<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
19
FEATURE<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
Difficult biliary cannulation is defined as the inability to achieve selective<br />
cannulation within 10 min or 5 attempts by a recent ERCP guideline<br />
[17]. Taking the ERCP guideline as a reference, in our study, we set<br />
the difficult appendix cannulation time to within 15 min regardless of<br />
the number of cannulation attempts. In the present study, 4 patients<br />
(12.12%) failed ERAT treatment. All of these failures were due to difficult<br />
cannulation caused by a swollen mucosa and narrow lumen of the<br />
appendix. In these patients, the guidewire failed to pass through the<br />
swollen and convoluted appendiceal lumen. Unfortunately, difficult<br />
appendiceal cannulation remains an unsolved issue. We believe that<br />
there may be two ways to assist appendiceal cannulation in this<br />
situation. One is to find new equipment that can overcome the severe<br />
edema of the appendix mucosa. The other is to prolong the pre-ERAT<br />
duration to acquire more sufficient anti-inflammatory effect by antibiotics<br />
and thereby maximally reduce the inflammation of the appendiceal<br />
mucosa. However, the second method would definitely increase the<br />
overall hospitalization duration of patients. Subsequent studies will be<br />
conducted to address difficult appendiceal cannulation. In the current<br />
study, 4 patients who failed ERAT were found to have appendicoliths.<br />
However, the reason of failure was due to the mucosal edema instead<br />
of the obstruction of the appendicoliths. Apart from the 4 patients,<br />
the other 8 patients with appendicoliths had a smooth recovery by<br />
receiving ERAT alone. Hence, appendicolith should not be considered<br />
as a contraindication of ERAT. Same as previous study [18], we think<br />
the key to remove appendicoliths was based on the quality of the stone<br />
and the technique of the endoscopist. A fragile stone, regardless of<br />
its size, is more likely to be removed by the combination of irrigation<br />
and extraction basket. If the stone is hard and large, the success of<br />
retraction is more dependent on the experience and the technique of<br />
the endoscopist. When a giant and irregular appendicolith is observed,<br />
it is also feasible to squeeze the appendix and let the stone fall into<br />
the intestine cavity. After that, the appendicolith can be removed via<br />
the intestine by a stone basket. Previous studies showed that the<br />
recurrence rates of acute appendicitis patients treated with ERAT ranges<br />
from 6.1 to 15% [7,8,9]. In the present study, 3 patients (9.09%) had<br />
recurrent appendicitis. This recurrence rate was consistent with previous<br />
findings. The recurrence of acute appendicitis may be associated with<br />
the appendiceal morphology since long and curved appendix is also<br />
risk factor of acute appendicitis. Other factors, such as genetic and<br />
environmental factors, may also have impact on recurrence. The final<br />
crossover rate of ERAT group was 21.21%, which means more than 3/4<br />
of all patients recovered successfully by receiving ERAT alone and those<br />
who crossed over to surgery did not experience any adverse outcomes<br />
due to the delay in appendectomy. However, the final crossover rate<br />
may be underestimated due to short-term follow-up period and a<br />
long-term follow-up is needed to be done in the future. Moreover, in a<br />
previous study, spontaneous discharge of the stents was considered as<br />
an adverse event [9]. However, in current study, the stents of 9 patients<br />
spontaneously discharged and these 9 patients did not show symptoms<br />
during the 14-day period. Thus, from our point of views, if the patients<br />
do not show any discomfort, spontaneous discharge of the stents<br />
should be considered as a benefit and convenience since these patients<br />
will not have to undergo colonoscope a second time.<br />
Another advantage of ERAT is its ability to facilitate a precise diagnosis<br />
of acute appendicitis. Generally, endoscopy can serve as a diagnostic<br />
tool for numerous diseases, such as ulcerative colitis and Crohn’s<br />
disease [19, 20]. A previous study indicated that colonoscopy can<br />
diagnose acute appendicitis with 100% sensitivity and 99% specificity<br />
[21]. Li et al. further described the key points of diagnosing acute<br />
appendicitis by ERAT by observing both the appendiceal mucosa<br />
morphology and the appendiceal lumen imaging by fluoroscopy [8].<br />
In our study, 33 patients with acute uncomplicated appendicitis in<br />
the ERAT group were all confirmed by ERAT. In the future, ERAT may<br />
become an essential diagnostic method for patients suspicious for acute<br />
appendicitis who have atypical clinical manifestations.<br />
One feature of our study was that an abdominal CT scan was performed<br />
in all participants. Although CT scan is not a necessary diagnostic<br />
criterion for acute appendicitis, using CT can enhance the accuracy of<br />
diagnosing acute appendicitis and minimize the negative appendicitis<br />
rate. Similar to this view, some previous trials showed that their study<br />
design was limited due to the lack of CT scans performed in suspicious<br />
patients [7]. Based on former experiences, all participants had to be<br />
examined by abdominal CT scan in our study. Thus, we could accurately<br />
enroll the patients with acute uncomplicated appendicitis in our trial by<br />
both clinical manifestation and CT scan confirmation.<br />
The study has several limitations. First, the success rate of ERAT largely<br />
depends on the skills of endoscopists. Although our endoscopists are<br />
experienced doctors, the lack of ERAT guidelines was still the main<br />
problem when faced with difficult cannulation. Second, since this was<br />
an RCT, we tried to perform ERAT on the first day of hospital admission,<br />
which was similar to the timing of emergency surgery. The downside of<br />
this strategy is that it may cause insufficient anti-inflammatory treatment<br />
in patients, which may increase the difficulty of appendiceal cannulation.<br />
Third, in the current study, the power was not calculated and the study<br />
is more likely to commit a type II error. However, in this pilot study,<br />
the safety and feasibility of ERAT were preliminarily estimated. Thus,<br />
future studies involved with larger sample size are needed to be done.<br />
Fourth, a double-blinded trial cannot be conducted due to the nature<br />
of the study. Last, the need to prepare for colonoscopy in patients with<br />
abdominal pain requires further study and is another limitation of the<br />
study.<br />
In conclusion, ERAT was demonstrated to be a feasible and safe<br />
treatment for acute uncomplicated appendicitis. However, difficult<br />
appendiceal cannulation and acute appendicitis recurrence are the main<br />
problems that remain to be solved. In the future, large-scale multicenter<br />
RCTs are needed to further address the current challenges.<br />
Abbreviations<br />
ERAT: Endoscopic retrograde appendicitis therapy; LA: Laparoscopic<br />
appendectomy; OA: Open appendectomy; PEG: Polyethylene glycol;<br />
SD: Standard deviation; ERA: Endoscopic retrograde appendicography;<br />
WBC: White blood cell; CRP: C-reactive protein; LOS: Length of<br />
hospital stay; VAS: Visual analog scales; ANOVA: Analysis of variance;<br />
ITT: Intention-to-treat; CT: Computed tomography; RCT: Randomized<br />
controlled trial; EMR: Endoscopic mucosal resection<br />
Acknowledgements<br />
We would like to thank American Journal Experts (https://www.aje.com/)<br />
for English language editing. We also appreciate all members from the<br />
Department of General Surgery, Jinshan hospital, Fudan University, for<br />
helping with the study.<br />
20
FEATURE<br />
Authors’ contributions<br />
PLS and MJ proposed the study and were accountable for all aspects of<br />
the work. ZMS contributed to the article in the aspects of drafting work<br />
as well as collecting, analyzing and interpreting the data; ZLZ, JTL, MY<br />
and WDH all made essential contribution to the manuscript. All authors<br />
read and approved the final manuscript.<br />
Funding<br />
This study was supported by Project of Shanghai Municipal Health<br />
Commission of China (No. 201740041). All the funding was used to<br />
conduct this trial.<br />
Availability of data and materials<br />
The datasets supporting the conclusions of this article are available in the<br />
the ResMan original data sharing platform (IPD sharing platform) of the<br />
Chinese Clinical Trial Registry, which can be viewed at the following website:<br />
http://www.medresman.org.cn/pub/cn/proj/projectshow.aspx?proj=5600.<br />
We expect to release the original data on December <strong>2022</strong>.<br />
Declarations<br />
Ethics approval and consent to participate<br />
All procedures performed in studies involving human participants<br />
were in accordance with the ethical standards of Ethics Committee of<br />
Jinshan Hospital, Fudan University (No. 2017-24) on May 17th, 2017<br />
and also with the 1964 Helsinki declaration and its later amendments<br />
or comparable ethical standards. The experimental protocol was also<br />
approved by Shanghai Municipal Health Commission and Project of<br />
Shanghai Municipal Health Bureau in China (No. 201740041). Written<br />
informed consent was obtained from all participants. The study is<br />
registered with the WHO Primary Registry-Chinese Clinical Trial Registry<br />
(ChiCTR1900025812).<br />
Consent for publication<br />
Not applicable.<br />
Competing interests<br />
The authors declare that they have no competing interest.<br />
Author details<br />
1<br />
Department of General Surgery, Jinshan Hospital, Fudan University,<br />
Shanghai, China. 2 Department of <strong>Gastroenterology</strong>, Jinshan Hospital,<br />
Fudan University, Shanghai, China.<br />
Received: 29 June 2021 Accepted: 3 February <strong>2022</strong><br />
Published online: 13 February <strong>2022</strong><br />
References<br />
1. Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute<br />
appendicitis: modern understanding of pathogenesis, diagnosis,<br />
and management. Lancet. 2015;386(10000):1278–87.<br />
2. National Surgical Research Collaborative. Multicentre observational<br />
study of performance variation in provision and outcome of<br />
emergency appendicectomy. Br J Surg. 2013;100:1240–52.<br />
3. Ahmed HO, Muhedin R, Boujan A, Aziz AHS, Abdulla AM, Hardi RA,<br />
et al. A five-year longitudinal observational study in morbidity and<br />
mortality of negative appendectomy in Sulaimani teaching Hospital/<br />
Kurdistan Region/Iraq. Sci Rep. 2020;10:2028.<br />
4. Andersson RE. The natural history and traditional management of<br />
appendicitis revisited: spontaneous resolution and predominance<br />
of prehospital perforations imply that a correct diagnosis is more<br />
important than an early diagnosis. World J Surg. 2007;31:86–92.<br />
5. Flum DR. Clinical practice. Acute appendicitis—appendectomy or<br />
the “antibiotics first” strategy. N Engl J Med. 2015;372:1937–43.<br />
6. Liu BR, Song JT, Han FY, Li H, Yin JB. Endoscopic retrograde<br />
appendicitis therapy: a pilot minimally invasive technique (with<br />
videos). Gastrointest Endosc. 2012;76:862–6.<br />
7. Liu BR, Ma X, Feng J, Yang Z, Qu B, Feng ZT, et al. Endoscopic<br />
retrograde appendicitis therapy (ERAT): a multicenter retrospective<br />
study in China. Surg Endosc. 2015;29:905–9.<br />
8. Li Y, Mi C, Li W, She J. Diagnosis of acute appendicitis by<br />
endoscopic retrograde appendicitis therapy (ERAT): combination of<br />
colonoscopy and endoscopic retrograde appendicography. Dig Dis<br />
Sci. 2016;61:3285–91.<br />
9. Ye LP, Mao XL, Yang H, He BL, Zhu LH, Zhang Y. Endoscopic<br />
retrograde appendicitis techniques for the treatment of patients with<br />
acute appendicitis. Z Gastroenterol. 2018;56:899–904.<br />
10. Gaitini D. Imaging acute appendicitis: state of the art. J Clin Imaging<br />
Sci. 2011;1:49.<br />
11. Pickhardt PJ, Levy AD, Rohrmann CA Jr, Kende AI. Primary<br />
neoplasms of the appendix manifesting as acute appendicitis: CT<br />
findings with pathologic comparison. Radiology. 2002;224:775–81.<br />
12. Williams SN, Bulstrode CJK, O’Connell PR. The vermiform<br />
appendix. In: Bailey & Love’s short practice of surgery. 26th ed.<br />
Boca Raton: CRC Press; 2013. p. 1201–2.<br />
13. Liang MK, Andersson RE, Jaffe BM, Berger HD, et al. The appendix.<br />
In: Brunicardi FC, Andersen DK, Billiar TR, et al., editors. Schwartz’s<br />
principles of surgery. 9th ed. New York: McGraw-Hill; 2010. p. 1074–5.<br />
14. Su YK, Kim HS, Hong JP. Adverse events related to colonoscopy:<br />
global trends and future challenges. World J Gastroenterol.<br />
2019;25(02):190–204.<br />
15. Randal Bollinger R, Barbas AS, Bush EL, Lin SS, Parker W. Biofilms<br />
in the large bowel suggest an apparent function of the human<br />
vermiform appendix. J Theor Biol. 2007;249:826–31.<br />
16. Kaplan GG, Pedersen BV, Andersson RE, Sands BE, Korzenik<br />
J, Frisch M. The risk of developing Crohn’s disease after an<br />
appendectomy: a population-based cohort study in Sweden and<br />
Denmark. Gut. 2007;56:1387–92.<br />
17. Liao WC, Angsuwatcharakon P, Isayama H, Dhir V, Devereaux B,<br />
Khor CJ, et al. International consensus recommendations for difficult<br />
biliary access. Gastrointest Endosc. 2017;85:295–304.<br />
18. Song MY, Liu ZH, Zhao LX, Liu BR. Endoscopic retrograde<br />
appendicitis therapy for treating a giant hard appendicolith<br />
embedded in the appendiceal orifice: a case report. Asian J Surg.<br />
2020;44(2):488–9.<br />
19. Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long<br />
MD. ACG clinical guideline: ulcerative colitis in adults. Am J<br />
Gastroenterol. 2019;114:384–413.<br />
20. Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB,<br />
Sands BE. ACG clinical guideline: management of crohn’s disease in<br />
adults. Am J Gastroenterol. 2018;113:481–517.<br />
21. Chang HS, Yang SK, Myung SJ, Jung HY, Hong WS, Kim JH, et al.<br />
The role of colonoscopy in the diagnosis of appendicitis in patients<br />
with atypical presentations. Gastrointest Endosc. 2002;56:343–8.<br />
Publisher’s Note<br />
<strong>Spring</strong>er Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affiliations.<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
21
FEATURE<br />
AN EXTREMELY DANGEROUS CASE OF<br />
ACUTE MASSIVE UPPER GASTROINTESTINAL<br />
BLEEDING: A CASE REPORT<br />
Zhiqiang Yi 1† , Cheng Chen 2† , Biguang Tuo 1 , Taolang Li 3 and Xuemei Liu 1*<br />
Yi et al. BMC <strong>Gastroenterology</strong> (<strong>2022</strong>) 22:67 https://doi.org/10.1186/s12876-022-02138-8<br />
Abstract<br />
Background<br />
Upper gastrointestinal (GI) bleeding is a severe acute disease of<br />
gastroenterology department. Fish bone is the most common foodrelated<br />
foreign body. However, fish bone piercing the esophagus,<br />
causing the mediastinal abscess that corroded the left subclavian artery,<br />
resulting delayed but high-risk massive upper gastrointestinal bleeding<br />
is very rare.<br />
Case presentation<br />
A 54-year-old man was admitted to the hospital with a chief complaint<br />
of hematemesis for 2 h. The color of hematemesis was bright red, and<br />
the volume was over 1000 ml. He also had symptoms of palpitations,<br />
fatigue and sweating. He had been on long-term glucocorticoids or<br />
nonsteroidal anti-inflammatory drugs (NSAIDs) for gout for 3 years<br />
before admission, had no previous history of liver disease or GI bleeding<br />
disease, and had a history of drinking.<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
Case presentation<br />
We report a 54-year-old man who was diagnosed with delayed but<br />
high-risk massive upper GI bleeding that was the result of a fish bone<br />
piercing the esophagus, causing a mediastinal abscess that corroded<br />
the left subclavian artery. He was saved effectively by early and timely<br />
multidisciplinary collaboration.<br />
Conclusion<br />
A fish bone-caused mediastinal abscess that corrodes the left<br />
subclavian artery and induces delayed but high-risk massive upper GI<br />
bleeding is very rare. In addition to routine consideration of upper GI<br />
bleeding, medical history, endoscopy and CT are helpful for achieving<br />
a diagnosis. Importantly, early and timely multidisciplinary collaboration<br />
can effectively save critically ill patients.<br />
Keywords<br />
Delayed but high-risk massive upper gastrointestinal bleeding, Fish<br />
bone, Mediastinal abscess, Left subclavian artery (LSA), Early and timely<br />
multidisciplinary collaboration<br />
Background<br />
Upper gastrointestinal (GI) bleeding is a severe acute disease<br />
associated with four main causes, namely, esophageal variceal<br />
bleeding, peptic ulcer (PU) bleeding, gastric cancer bleeding<br />
and acute erosive hemorrhagic gastritis, and prompt diagnosis<br />
and treatment are mandatory [1, 2]. In adults, a fish bone is the<br />
most common food-related foreign body [3, 4]. A fish bone can<br />
unfortunately pierce the left subclavian artery (LSA) and cause a<br />
pseudoaneurysm in rare cases, resulting in an LSA esophageal<br />
fistula [3, 5]. Arterioesophageal fistula are rare, but they can cause<br />
massive life-threatening bleeding [6, 7]. Here, we report an adult<br />
case of a mediastinal abscess corroding the LSA, resulting in<br />
delayed but high-risk massive upper GI bleeding.<br />
On admission, the patient’s vital signs included a temperature of 36.4 °C,<br />
blood pressure of 80/50 mmHg, and heart rate of 135 bpm. Laboratory<br />
data showed routine blood tests: hemoglobin 72 g/L (normal, 130–175<br />
g/L), white blood cells 13.41×10 9 /l (normal, 4–10*10 9 /L), total platelets<br />
60×10 9 (normal, 100–300*10 9 /L); C-reactive protein 159.90 mg/l<br />
(normal 0–8 mg/L); blood gas analysis: oxygen partial pressure 79.3<br />
mmHg, CO 2<br />
partial pressure 30.8 mmHg, pH value 7.281; and normal<br />
liver and renal function and coagulation tests. Therefore, GI hemorrhage<br />
was first considered, and esomeprazole was administered. Computed<br />
tomography (CT) on admission showed a visible breach on the left side<br />
of the esophageal wall, a low-density lesion was found between the<br />
esophageal wall and the LSA, and the demarcation from the esophageal<br />
wall and subclavian artery was unclear (Fig. 1). Because the patient had<br />
no history of foreign body ingestion, we initially considered esophageal<br />
diverticula with bleeding potential. However, the patient still presented<br />
with repeated hematemesis with a large volume of bright red blood;<br />
his vital signs could not be maintained, and he developed progressive<br />
unconsciousness 30 min after admission to the hospital. We applied<br />
a multidisciplinary approach; critical care doctors were included in the<br />
treatment, and a member of the Department of Anesthesiology performed<br />
an urgent consultation. Tracheal intubation-assisted respiration, aspiration<br />
prevention, and anti-shock therapy were applied, and 6 units of red blood<br />
cells were transfused. Additionally, urgent esophagogastroduodenoscopy<br />
was performed in the operating room, which indicated active and massive<br />
bleeding from the esophageal wall (Fig. 2). However, due to massive<br />
bleeding, this patient suffered from two cardiac arrests, so a detailed<br />
endoscopic examination could not be performed.<br />
Urgent thoracotomy through the median sternal incision was performed<br />
immediately, and an abscess cavity 4 cm in size was detected between<br />
the LSA and the left common carotid artery. A stench of putrefaction<br />
accompanied by a large gush of blood was present when the abscess<br />
cavity was opened. The active bleeding point was found in the posterior<br />
lateral wall of the LSA with a 3 mm rupture. During the repair of the LSA<br />
and clean-up of the abscess cavity, an esophageal fistula was detected<br />
and repaired on the other side of the abscess cavity. However, no foreign<br />
22<br />
*Correspondence: onlyoneliuxuemei@163.com<br />
†<br />
Zhiqiang Yi and Cheng Chen contributed equally and shared first authorship<br />
1<br />
Department of <strong>Gastroenterology</strong>, Affiliated Hospital of Zunyi Medical University, Zunyi 563003, Guizhou Province, China<br />
©The Author(s) <strong>2022</strong>
FEATURE<br />
Fig. 1 Image from CT scan. CT showed that the local soft tissue<br />
was Fig. thickened 1 Image in the from esophagus CT scan. CT at the showed cervicothoracic that the local junction, soft tissue<br />
and was a gaseous thickened cavity in was the esophagus present on at the the left cervicothoracic posterior wall of junction, the<br />
esophagus and a gaseous (red arrow), cavity approaching was present the on left the subclavian left posterior artery wall (white of the<br />
arrow). esophagus Esophageal (red breach arrow), was approaching detected (black the left arrow) subclavian artery (white<br />
arrow). Esophageal breach was detected (black arrow)<br />
body was observed (Fig. 3a, b). With prompt and effective treatment, the<br />
patient recovered. Revisiting family history indicated that chest pain and<br />
discomfort occurred in this patient after eating fish 4 days prior.<br />
Discussion and conclusions<br />
Fig. 2 Image from the emergent endoscopy. Active and massive<br />
bleeding Fig. 2was Image detected from from the emergent the esophageal endoscopy. wall by Active emergent and massive<br />
endoscopy bleeding was detected from the esophageal wall by emergent<br />
endoscopy<br />
There are generally four main causes of upper GI bleeding, namely,<br />
esophageal variceal bleeding, PU-caused bleeding, gastric cancercaused<br />
bleeding and acute erosive hemorrhagic gastritis [1, 2].<br />
In addition, there are also reports of NSAIDs causing esophageal<br />
mucosal damage. These drugs may cause mucosal damage by<br />
reducing the cytoprotective effect of prostaglandins on the mucosa<br />
or aggravating reflux esophagitis [8, 9]. The clinical manifestations of<br />
these patients are usually retrosternal pain, sore throat and dysphagia<br />
[9]. Esophageal bleeding caused by NSAIDs is a rare nonfatal bleeding,<br />
mostly secondary to superficial esophageal ulcer oozing, and some<br />
bleeding can even be discovered during endoscopy [10, 11]. However,<br />
Fig. 3 Image from the surgical operation. a The abscess cavity (white arrow) was located between the left subclavian artery (black arrow) and the<br />
left common carotid artery (blue arrow). b Schematic diagram of surgical anatomy<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
23
FEATURE<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
in the present case, the patient’s condition progressed so rapidly and<br />
dangerously that the challenge was to determine the cause of the<br />
bleeding and how to treat it. Based on medical history, physiological<br />
signs, examination and treatment, this case of delayed but high-risk<br />
massive upper GI bleeding was the result of a fish bone piercing<br />
the esophagus, causing the mediastinal abscess that corroded the<br />
LSA. Fistulas between the subclavian artery and esophagus are rare<br />
but can rapidly become life-threatening [12, 13]. Clinically, among<br />
arterial-esophageal fistulas caused by esophageal foreign bodies,<br />
the proportion of LSA esophageal fistulas is only 2% [3]. Most<br />
mediastinal abscesses are related to infections of deep sternal wounds,<br />
esophageal perforations, or descending necrotizing mediastinitis [14,<br />
15]. Mediastinal abscess directly caused by taking glucocorticoids<br />
has not been reported. It may be a contributing factor to the formation<br />
of abscesses after mediastinal infection. Glucocorticoids have many<br />
complex quantitative and qualitative immunosuppressive effects,<br />
which can induce cellular immune deficiency and may increase the<br />
susceptibility of the host to various viruses, bacteria, fungi and parasites<br />
[16]. The patient’s risk of infection increases with increasing treatment<br />
dose and treatment time. In patients exposed to low doses, even if the<br />
cumulative dose is high, the risk of infection is often low. In addition, the<br />
host’s underlying disease status also determines the changes in the risk<br />
of infection in clinical practice [17]. Therefore, in this case, we believe<br />
that the patient’s long-term use of glucocorticoids is not an independent<br />
risk factor for mediastinal abscess.<br />
Generally, fish bones or sharp foreign bodies can directly pierce the large<br />
arteries in the mediastinum, causing fatal upper GI bleeding. For example,<br />
some case reports have reported sharp foreign bodies such as fish<br />
bones or chicken bones piercing the esophagus and mediastinal artery<br />
[3, 18, 19]. Because the symptoms are initially not serious, they are often<br />
ignored by patients and their families. Once the foreign body leaves the<br />
artery, the patient will die suddenly due to acute upper GI bleeding [3, 18].<br />
If the patient seeks medical attention in time and the foreign body does<br />
not break away from the artery, the patient can be successfully cured by<br />
surgery [19]. In contrast, in this rare case, the mediastinal abscess that<br />
resulted from puncture of the esophagus by the fishbone corroded the<br />
LSA, causing delayed but high-risk arterial hemorrhage.<br />
This case suggests that in addition to routine consideration of upper GI<br />
bleeding, medical history, endoscopy and CT are helpful for achieving<br />
a diagnosis. Importantly, early and timely multidisciplinary collaboration<br />
can effectively save critically ill patients. Emergency thoracotomy<br />
remains a life-saving treatment.<br />
Abbreviations<br />
GI: Gastrointestinal; NSAIDs: Nonsteroidal anti-inflammatory drugs; LSA:<br />
Left subclavian artery; CT: Computed tomography; PU: Peptic ulcer.<br />
Acknowledgements<br />
The authors are grateful to Prof. Hua Zhang and Jiaxing Zhu<br />
(Department of <strong>Gastroenterology</strong>, Affiliated Hospital of Zunyi Medical<br />
University, Zunyi, Guizhou Province, China) for study support.<br />
Authors’ contributions<br />
ZQY collected and interpreted the data; ZQY and XML drafted the<br />
manuscript; CC established the surgical plan; BGT analyzed the<br />
radiological images; TLL and XML designed the study and revised<br />
the draft; and XML supervised the study. All the authors listed have<br />
approved the enclosed manuscript.<br />
Funding<br />
This research was supported by the National Natural Science<br />
Foundation of China (81860103 and 82070536 to X.M.L., 81660098<br />
and 82160505 to T.L.L., 81960532 to C.C., and 82073087 to B.G.T.),<br />
the Guizhou Province International Science and Technology Cooperation<br />
(<strong>Gastroenterology</strong>) Base (Qian Ke He Platform Talents-HZJD [2021] 001<br />
to X.M.L.), the Guizhou Province Science Plan Program (Qian Ke He<br />
Foundation-ZK [2021] General 461 to T.L.L.), the Cultivation of high-level<br />
innovative talents in Guizhou Province [“Thousand” level] (fzc120200615<br />
to T.L.L.), the 15851 Talent Projects of Zunyi City (2018 to T.L.L.), and<br />
the Guizhou Province Science and Technology Plan (No. Qiankehe<br />
Support [2021] General 073 to C.C.).<br />
Availability of data and materials<br />
All information about the patient came from the Affiliated Hospital of<br />
Zunyi Medical University. The data used and analyzed during the current<br />
study are included in this article.<br />
Declarations<br />
Ethics approval and consent to participate<br />
The study was reviewed and approved by the Ethics Committee of the<br />
Affiliated Hospital of Zunyi Medical University.<br />
Consent for publication<br />
Written informed consent was obtained from the patient for publication<br />
of this report and any accompanying images. A copy of the written<br />
consent is available upon request.<br />
Competing interests<br />
The authors declare that they have no competing interests.<br />
Author details<br />
1<br />
Department of <strong>Gastroenterology</strong>, Affiliated Hospital of Zunyi Medical<br />
University, Zunyi 563003, Guizhou Province, China. 2 Department of<br />
Thoracis Surgery, Affiliated Hospital of Zunyi Medical University, Zunyi,<br />
Guizhou Province, China. 3 Department of Thyroid and Breast Surgery,<br />
Affiliated Hospital of Zunyi Medical University, Zunyi, Guizhou Province,<br />
China.<br />
Received: 27 August 2021 Accepted: 3 February <strong>2022</strong><br />
Published online: 15 February <strong>2022</strong><br />
References<br />
1. Gralnek I, Dumonceau J, Kuipers E, Lanas A, Sanders D, Kurien<br />
M, et al. Diagnosis and management of nonvariceal upper<br />
gastrointestinal hemorrhage: European Society of Gastrointestinal<br />
Endoscopy (ESGE). Guideline. 2015;47(10):a1-46.<br />
2. Gralnek I, Stanley A, Morris A, Camus M, Lau J, Lanas A, et al.<br />
Endoscopic diagnosis and management of nonvariceal upper<br />
gastrointestinal hemorrhage (NVUGIH): European Society of<br />
Gastrointestinal Endoscopy (ESGE). Guideline Update 2021.<br />
2021;53(3):300–32.<br />
24
FEATURE<br />
3. Zhao S, Tinzin L, Deng W, Tong F, Shi Q, Zhou Y. Sudden<br />
unexpected death due to left subclavian artery-esophageal fistula<br />
caused by fish bone. J Forensic Sci. 2019;64(6):1926–8.<br />
4. Wang X, Zhao J, Jiao Y, Wang X, Jiang D. Upper gastrointestinal<br />
foreign bodies in adults: a systematic review. Am J Emerg Med.<br />
2021;50:136–41.<br />
5. Stringari C, Sbraga P, Zaraca F. Endovascular treatment of a left<br />
subclavian pseudoaneurysm induced by ingestion of a foreign body.<br />
Ann Vasc Surg. 2013;27(5):672.e677-672.611.<br />
6. Hollander JE, Quick G. Aortoesophageal fistula: a comprehensive<br />
review of the literature. Am J Med. 1991;91(3):279–87.<br />
7. Millar A, Rostom A, Rasuli P, Saloojee N. Upper gastrointestinal<br />
bleeding secondary to an aberrant right subclavian arteryesophageal<br />
fistula: a case report and review of the literature. Can J<br />
Gastroenterol. 2007;21(6):389–92.<br />
8. Noffsinger AE. Update on esophagitis: controversial and<br />
underdiagnosed causes. Arch Pathol Lab Med. 2009;133(7):1087–95.<br />
9. Zografos GN, Georgiadou D, Thomas D, Kaltsas G, Digalakis M.<br />
Drug-induced esophagitis. Dis Esophagus. 2009;22(8):633–7.<br />
10. Kikendall JW, Friedman AC, Oyewole MA, Fleischer D, Johnson<br />
LF. Pill-induced esophageal injury. Case reports and review of the<br />
medical literature. Dig Dis Sci. 1983;28(2):174–82.<br />
11. Kim SH, Jeong JB, Kim JW, Koh S-J, Kim BG, Lee KL, et al. Clinical<br />
and endoscopic characteristics of drug-induced esophagitis. World<br />
J Gastroenterol. 2014;20(31):10994–9.<br />
12. Kim S, Jeon KN, Bae K. Aberrant left subclavian artery-esophageal<br />
fistula in a patient with a prolonged use of nasogastric tube: a case<br />
report and literature review. Diagnostics (Basel). 2021;11(2):195.<br />
13. Oliveira E, Anastácio M, Marques AJ. Aberrant right subclavian<br />
artery-esophageal fistula: massive upper gastrointestinal<br />
hemorrhage secondary to prolonged intubation. Braz J Anesthesiol.<br />
2016;66(3):318–20.<br />
14. Pastene B, Cassir N, Tankel J, Einav S, Fournier PE, Thomas P, et<br />
al. Mediastinitis in the intensive care unit patient: a narrative review.<br />
Clin Microbiol Infect. 2020;26(1):26–34.<br />
15. Martínez Vallina P, Espinosa Jiménez D, Hernández Pérez L, Triviño<br />
RA. Mediastinitis. Arch Bronconeumol. 2011;47(Suppl 8):32–6.<br />
16. Lionakis MS, Kontoyiannis DP. Glucocorticoids and invasive fungal<br />
infections. Lancet. 2003;362(9398):1828–38.<br />
17. Cutolo M, Seriolo B, Pizzorni C, Secchi ME, Soldano S, Paolino S,<br />
et al. Use of glucocorticoids and risk of infections. Autoimmun Rev.<br />
2008;8(2):153–5.<br />
18. Russo SS, Taff ML, Ratanaproeksa O, Spitz WU. Sudden death<br />
resulting from chicken bone perforation of the esophagus. Am J<br />
Forensic Med Pathol. 1986;7(3):263–5.<br />
19. Jiang D, Lu Y, Zhang Y, Hu Z, Cheng H. Aortic penetration due to a<br />
fish bone: a case report. J Cardiothorac Surg. 2020;15(1):292.<br />
Publisher’s Note<br />
<strong>Spring</strong>er Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affiliations.<br />
Find out more at www.calprotectin.co.uk<br />
[Figure 1: Edwards et al. ECCO 2021 P518]<br />
Improved Compliance for Faecal Calprotectin<br />
The BÜHLMANN IBDoc ® enables<br />
faecal calprotectin testing<br />
by patients at home, using<br />
their smartphone to read the<br />
results. It facilitates remote<br />
monitoring, patient privacy, rapid<br />
implementation of appropriate<br />
treatment pathways and<br />
prioritisation of valuable resources.<br />
The IBDoc is loved by the clinical<br />
teams and patients with 85%<br />
of respondents in a recent<br />
survey preferring it to standard<br />
lab testing, and another study<br />
showing improved compliance.<br />
Dr Pushpakaran Munuswamy from<br />
Basildon and Thurruck NHS Trust said:<br />
“Using the IBDoc has increased<br />
the engagement from both<br />
the patients and the clinical<br />
team, and the speed ofv the<br />
results really makes a big<br />
impact in decision making<br />
and patient management.”<br />
Patient feedback has also been great:<br />
“I don’t think they could have<br />
made the test any easier to<br />
be honest - if you have been<br />
offered a chance to use the<br />
IBDoc just give it a go, taking<br />
the sample isn’t a big deal and<br />
the results come through really<br />
quickly which is all that matters.”<br />
Contact us today to see how<br />
the IBDoc can have a positive<br />
impact on your IBD service.
NEWS<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
Healthcare survey highlights<br />
the impact of the pandemic<br />
on IBD patient care<br />
Over 7,000 people responded to the<br />
Crohn’s & Colitis UK Healthcare Survey,<br />
providing an insight into how IBD patients<br />
experienced healthcare during 2021.<br />
The responses showed that health services<br />
have continued to be disrupted by the<br />
coronavirus pandemic and there’s been a big<br />
impact on patient care. Difficulties accessing<br />
GPs, specialists, medicines, tests, and<br />
procedures have led to delays in diagnosis,<br />
flares, and complications for people with<br />
Crohn’s and Colitis. Mental wellbeing,<br />
relationships, and ability to work have also<br />
been affected.<br />
Ruth Wakeman, Director of Services,<br />
Advocacy & Evidence at Crohn’s & Colitis<br />
UK says: ‘The results of the Healthcare<br />
Survey highlight that the pandemic has<br />
exacerbated existing issues with resourcing<br />
of IBD services, which need to be addressed,<br />
but also some opportunities as services<br />
have adapted to the pandemic. We are<br />
very grateful for the care and support that<br />
healthcare professionals continue to give<br />
to people with Crohn’s and Colitis in such<br />
difficult circumstances.’<br />
The results showed that whilst huge efforts<br />
had been made to deliver excellent care for<br />
people with Crohn’s and Colitis, prioritisation<br />
and investment are vital to tackle increasingly<br />
long waits for care. The recent Getting it Right<br />
First Time (GIRFT) gastroenterology report<br />
called for more proactive management of IBD,<br />
with the aim of reducing admissions. It also<br />
highlighted improvements that could be made<br />
to triage to speed up diagnosis and early<br />
treatment.<br />
This survey, which was conducted between<br />
August and October 2021, asked questions<br />
about experiences of healthcare during the<br />
previous 6-12 months. It builds on previous<br />
surveys by Crohn’s & Colitis UK, including<br />
the Life in Lockdown Survey in 2020 and IBD<br />
Patient Survey in 2019, all contributing to<br />
build a comprehensive view of healthcare over<br />
the last 3 years.<br />
What people with living with Crohn’s and<br />
Colitis said<br />
Diagnosis<br />
Many said that getting a diagnosis during<br />
the pandemic has been difficult, with 29% of<br />
respondents diagnosed during the previous<br />
12 months reporting that this had taken<br />
over a year. This is an increase from 26% in<br />
2019. Respondents also reported that it had<br />
taken longer for treatment to start following<br />
diagnosis. 41% said it took more than two<br />
weeks for treatment to start, compared to<br />
2019 when only 24% reported waiting more<br />
than two weeks for treatment.<br />
Access to healthcare professionals<br />
The results also showed that people found<br />
it harder to get through to IBD teams for<br />
specialist advice, with 27% of those who tried<br />
to contact their advice line saying they did not<br />
get a response by the end of the next working<br />
day.<br />
This was in addition to 41% of those who had<br />
needed care from their GP during the previous<br />
6 months saying they had been unable to get<br />
the care they needed. Furthermore, 29% had<br />
not been able to get the help they needed from<br />
urgent care services.<br />
Access to medicines, tests and procedures<br />
The results indicate a particularly big disruption<br />
to surgery and colonoscopy. 29% reported<br />
cancelled surgery and 24% cancelled<br />
colonoscopies, with many still waiting for a<br />
new date.<br />
Additionally, 18% had experienced disruption<br />
to getting medication.<br />
Impact of difficulties accessing health<br />
services or treatment<br />
22% of those who have needed health<br />
services or treatment during the previous 6<br />
months said that difficulties accessing this had<br />
resulted in a flare of their condition. In addition<br />
to this, 24% reported that their mental health<br />
had been affected. Respondents relayed<br />
how this has led to time off work, affected<br />
relationships and ability to do everyday tasks.<br />
Changes to how patients access care<br />
The survey found that 72% of those who had<br />
needed outpatient appointments during the<br />
previous 6 months had mostly had these by<br />
telephone, with only 3% having mostly video<br />
appointments. Only 13% were offered a<br />
choice. Comments highlighted the benefits of<br />
remote appointments, but also preferences for<br />
some face-to-face appointments. Whichever<br />
method was used, quality of care and a<br />
personalised approach were considered<br />
important.<br />
Quality of care<br />
Despite the challenges during this period, 56%<br />
felt that their quality of care was the same as<br />
before the pandemic, with a small proportion<br />
(4%) considering it was better.<br />
More information about the survey can be<br />
found on the Crohn’s & Colitis UK website. If<br />
you’re an IBD Nurse Specialist or Healthcare<br />
Professional working in IBD, you may want<br />
to use these results alongside your service’s<br />
IBD UK Benchmarking reports as your service<br />
refocuses, adapts, and redesigns for the<br />
future. If you would like to seek feedback and<br />
involve your IBD patients in service redesign,<br />
the charity also has a Patient Engagement<br />
Toolkit, also available on their website which<br />
may be helpful.<br />
Cause of inflammatory<br />
bowel disease discovered<br />
Interaction between gut bacteria and<br />
mucus layer cells<br />
Chronic inflammatory bowel disease (IBD)<br />
is becoming increasingly widespread. Until<br />
now, however, the underlying causes of<br />
the inflammation responses were unclear.<br />
Scientists at the Technical University<br />
of Munich (TUM) have now identified a<br />
mechanism that triggers a problematic<br />
interaction between intestinal bacteria and<br />
cells in the intestinal mucus layer in XLP2,<br />
a condition associated with IBD. The team<br />
believes that the results can be applied to<br />
other intestinal diseases and could offer<br />
approaches to the development of new<br />
drugs.<br />
The billions of bacteria living in the human<br />
gut – known collectively as the microbiome<br />
– are of enormous importance. They help<br />
with digestion, among other functions.<br />
Consequently, the immune system in the gut<br />
must be extremely well regulated: It should<br />
fight only harmful pathogens without attacking<br />
useful microorganisms. However, this fine<br />
balance can be disrupted by various factors.<br />
A defect in the gene XIAP, which causes<br />
the rare disease XLP2, results in chronic<br />
inflammation of the bowels in 30 percent of all<br />
26
NEWS<br />
Dr Monica Yabal<br />
cases, among other symptoms. Babies with this<br />
genetic defect often display serious symptoms<br />
such as diarrhea, abdominal pain, weakness<br />
and weight loss soon after birth. Until now,<br />
scientists have been unable to understand the<br />
underlying mechanism or discover effective<br />
treatments – apart from stem cell transplants,<br />
which involve a high risk of mortality.<br />
Overreaction of the innate immune system<br />
Working with organoids – intestinal cells in a<br />
Petri dish – and animal experiments, a team<br />
headed by Dr. Monica Yabal, Adam Wahida and<br />
Madeleine Müller of the Institute for Molecular<br />
Immunology and the Clinic of Hematology<br />
and Oncology of TUM’s university hospital,<br />
Klinikum rechts der Isar, has now identified the<br />
mechanism behind the inflammation response<br />
and learned how it becomes chronic. “The<br />
innate immune system overreacts to microbes<br />
in the gut,” says Yabal. The immune system in<br />
healthy people eliminates bacteria that cause<br />
illness and then returns to its resting state. But<br />
in some XLP2 patients, a fatal chain reaction<br />
begins:<br />
Every person has toll-like receptors (TLRs) that<br />
use unique structures such as molecules in the<br />
cell wall to identify harmful microbes. When a<br />
TLR binds a molecule, the signaling substance<br />
TNF and its TNFR1 and TNFR2 receptors<br />
activate the immune system to eliminate the<br />
pathogen. However, this does not work properly<br />
in XLP2 patients. Instead, the binding of TNF to<br />
the TNFR1 receptor on cells known as Paneth<br />
cells causes these cells to die, resulting in a<br />
vicious circle. That is because the Paneth cells<br />
in the gut mucus layer produce antimicrobial<br />
substances and thus ensure a bacterial balance<br />
in the intestines. The loss of those cells changes<br />
the composition of the microbiome. Beneficial<br />
bacteria such as clostridia are attacked and can<br />
no longer perform their Publication:<br />
regulatory role. This Adam Wahida, Madeleine Müller, Andreas<br />
again activates the Hiergeist, Bastian Popper, Katja Steiger,<br />
immune system. Caterina Branca, Markus Tschurtschenthaler,<br />
Thomas Engleitner, Sainitin Donakonda,<br />
New drugs<br />
Jordy De Coninck, Rupert Öllinger, Marie K.<br />
could stop the Pfautsch, Nicole Müller, Miguel Silva, Sinem<br />
inflammation<br />
Usluer, Erik Thiele Oberg, Jan P. Böttcher,<br />
response<br />
Nicole Pfarr, Martina Anton, Julia B. Slotta-<br />
“We believe that this Huspenina, Andreas G. Nerlich, Tobias Madl,<br />
principle might also Marijana Basic, André Bleich, Geert Berx,<br />
be applicable to other Jürgen Ruland, Percy A. Knolle, Roland<br />
inflammatory bowel Rad, Timon E. Adolph, Peter Vandenabeele,<br />
diseases and not only Hirokazu Kanegane, André Gessner, Philipp<br />
in XLP2 patients,” says J. Jost, Monica Yabal. XIAP restrains TNFdriven<br />
intestinal inflammation and dysbiosis by<br />
Prof. Percy Knolle,<br />
the Director of the promoting innate immune responses of Paneth<br />
Institute for Molecular Immunology at TUM. and dendritic cells (2021) Science Immunology,<br />
Malfunctioning Paneth cells have also been Vol 6, Issue 65. DOI: 10.1126/sciimmunol.<br />
observed in many patients with inflammatory abf7235.<br />
bowel diseases with various causes.<br />
More information:<br />
These insights might open up important The study was funded by the European<br />
avenues for the development of new drugs. Research Council (ERC), the German Research<br />
Patients with chronic bowel inflammation Foundation (DFG), the Austrian Research<br />
have been treated for many years with drugs Promotion Agency (FFG) and the German<br />
that inhibit the TNF ScheBo_Gastro<strong>Today</strong>_Aug_2020 Center for Multi-Ad_Address_Change<br />
Infection Research (FFG).<br />
receptors. However,<br />
these molecules are<br />
not very specific<br />
and deactivate both<br />
TNFR1 and TNFR2.<br />
“Our experiments<br />
show that it would<br />
be better if we had a<br />
selective inhibitor for<br />
the TNFR1 receptor,”<br />
says Yabal. It also<br />
remains unclear<br />
why some people<br />
respond very well<br />
to this treatment<br />
while others show<br />
no response at<br />
all. Consequently,<br />
the team would<br />
now like to turn<br />
its attention to the<br />
adaptive immune<br />
system, which<br />
learns throughout an<br />
individual’s lifetime<br />
through contact<br />
with pathogens<br />
and forms special<br />
antigens, and also<br />
study its special role<br />
in the gut.<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
27
NEWS<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
Go with the Flow!<br />
How the Rare Disease Collaborative<br />
Network can support you in diagnosis and<br />
management of refractory coeliac disease<br />
Woodward JM 1 , Soilleux E 1 , Passmore R 2 ,<br />
Sanders D 3<br />
Coeliac disease that is refractory to the<br />
withdrawal of gluten from the diet is rare,<br />
and as a result prone to both over and under<br />
diagnosis. Two types are described: ‘Type 1’ is<br />
indistinguishable from non-responsive coeliac<br />
disease (1) and may be due to the individual<br />
being highly sensitized to trace amounts of<br />
gluten remaining in the diet that would not<br />
affect most people with the condition. ‘Type 2’<br />
refractory coeliac disease (RCD2) progresses<br />
to an aggressive T-cell lymphoma in as many<br />
as 67% of cases over 5 years (2). RCD2 is<br />
distinguished from non-responsive coeliac<br />
disease or RCD1 by the abnormal clonal<br />
increase of an unusual population of intestinal<br />
intra-epithelial lymphocytes (IELs) characterized<br />
by the presence of the T-cell marker CD3<br />
within the cytoplasm but not on the surface of<br />
the cell (3). These cells also usually lack the<br />
normal expression of another surface marker,<br />
CD8. However, immunohistochemistry for T-cell<br />
markers or polymerase chain reaction (PCR) for<br />
T-cell receptor clonality are unreliable diagnostic<br />
tests for RCD2 (3,4), whereas flow cytometry<br />
to identify individual IELs isolated from fresh<br />
intestinal biopsies is definitive (figure 1a).<br />
It is important to distinguish RCD1 from other<br />
causes of non-responsive coeliac disease<br />
and from RCD2 as specific treatments exist<br />
– for instance, the use of topical steroids or<br />
azathioprine for RCD1 and cladribine and<br />
autologous stem cell transplantation for<br />
RCD2. In 2018, NHS England designated<br />
Sheffield and Cambridge as the two national<br />
centres in the first ever UK Rare Disease<br />
Collaborative network in order to refine<br />
diagnostic and therapeutic techniques, and<br />
to develop a national database in order to<br />
further the understanding of the conditions<br />
and facilitate trials of treatment (5,6). The<br />
ongoing development of flow cytometry of<br />
intra-epithelial lymphocytes in the network<br />
has unexpectedly also demonstrated the<br />
utility of this technique in the diagnosis of<br />
coeliac disease itself (7). A characteristic<br />
change in the IEL composition occurs<br />
following the development of coeliac disease<br />
(8) and remains regardless of normalization<br />
of duodenal histology and serological tests<br />
on institution of a gluten free diet. Hence IEL<br />
flow cytometry is the only existing accessible<br />
test capable of confirming or refuting the<br />
diagnosis of coeliac disease in a patient<br />
following a strict gluten free diet. Referrals<br />
to the national centres remain lower than the<br />
expected prevalence of RCD (6) and indicates<br />
ongoing failure to recognize the condition. The<br />
following case studies demonstrate the utility<br />
of referral to the specialist national centres.<br />
Coeliac UK<br />
have developed<br />
resources on<br />
refractory and<br />
non-responsive<br />
coeliac disease<br />
to support<br />
you and your<br />
patients, scan<br />
the QR code to<br />
find out more.<br />
Case 1. Misdiagnosis of coeliac disease.<br />
A 20-year old woman contacted Coeliac UK<br />
for advice. Following a period of chronic<br />
fatigue she presented to her GP who found a<br />
very high anti-TTG antibody titre in her serum.<br />
Indirect immunofluorescence was negative for<br />
anti-endomysial antibodies. Following referral<br />
to her local gastroenterologist she underwent<br />
a gastroscopy and duodenal biopsies which<br />
were reported as showing equivocal features<br />
but consistent with coeliac disease. She<br />
was commenced on a gluten free diet which<br />
marginally improved her symptoms, however<br />
on follow up her anti-TTG titres remained<br />
high and she was repeatedly told by her<br />
hospital team that this meant that she was<br />
continuing to ingest gluten, which was a cause<br />
of significant anxiety for her and contributed<br />
to her fatigue. The patient was advised to<br />
request a second opinion from a tertiary<br />
centre. Further blood tests at the national<br />
centre revealed a negative anti-TTG titre<br />
and non-compatible HLA (human leucocyte<br />
antigen) haplotype for coeliac disease (9).<br />
Duodenal biopsies were reported as showing<br />
mild peptic duodenitis and flow cytometry<br />
revealed no evidence of coeliac disease (fig<br />
1a). Following reassurance that she did not<br />
have coeliac disease she was able to tolerate<br />
a normal diet without symptoms. This case<br />
demonstrates the variability of anti-TTG assays<br />
between laboratories, and the potential flaws<br />
of current diagnostic techniques.<br />
Case 2. Delayed diagnosis of RCD2.<br />
A previously fit and well 56-year old man<br />
presented via his GP to the local hospital<br />
following a business trip to the tropics with<br />
diarrhoea. A strong family history of coeliac<br />
disease was elicited, and duodenal biopsies<br />
at gastroscopy demonstrated sub-total villous<br />
atrophy, however anti-TTG antibodies were<br />
negative. He was therefore considered not<br />
to have coeliac disease and was treated<br />
empirically for tropical parasitic infections.<br />
However, his symptoms progressed and 12<br />
months later he was reinvestigated and found<br />
to have ongoing severe villous atrophy in the<br />
duodenum with thickening of the distal jejunum<br />
on magnetic resonance enterography. He was<br />
referred to one of the national tertiary centres<br />
for enteroscopy and biopsy of the thickened<br />
jejunum in order to make a diagnosis. An<br />
experienced clinician considered the possibility<br />
of RCD2 and lymphoma and instead carried<br />
out a gastroscopy and duodenal biopsy with<br />
flow cytometry the day after receiving the<br />
referral. The flow cytometry demonstrated<br />
a large population of atypical IELs lacking<br />
surface CD3 (fig 1b) in keeping with RCD2<br />
and a presumptive diagnosis of enteropathy<br />
associated lymphoma was made. Within<br />
3 weeks of referral he was admitted for<br />
establishment of home parenteral nutrition<br />
and underwent laparotomy and resection<br />
of the tumour, which was confirmed as a T<br />
cell lymphoma. He subsequently underwent<br />
CHOP chemotherapy and autologous<br />
haematopoeitic stem cell transplant. In his<br />
case earlier consideration of the diagnosis of<br />
RCD and referral to a national centre could<br />
have led to preventative treatment prior to<br />
developing lymphoma.<br />
Case 3. Overdiagnosis and overtreatment.<br />
A 37-year old woman presented to her GP<br />
in 2013 with diarrhoea and weight loss. A<br />
positive anti-tissue transglutaminase (TTG)<br />
antibody titre led to referral to the local<br />
gastroenterologist and a diagnosis was<br />
confirmed by the presence of sub-total<br />
villous atrophy on duodenal biopsy. She<br />
was commenced on a gluten free diet.<br />
However, in 2016 the presence of ongoing<br />
symptoms led to a repeat endoscopy which<br />
demonstrated persistent villous atrophy in<br />
the duodenal biopsies. She was told by her<br />
local gastroenterologist that she had refractory<br />
coeliac disease and that she needed to start<br />
on steroids and azathioprine as she was<br />
otherwise at risk of developing lymphoma. At<br />
this stage she sought a referral for a second<br />
28
NEWS<br />
Figure 1a Figure 1b Figure 1c<br />
opinion through one of the national tertiary<br />
centres. An experienced clinician elicited a<br />
history of a shared kitchen with potential for<br />
gluten contamination during food preparation,<br />
and that the patient was consuming foods<br />
that were labelled as ‘may contain traces of<br />
gluten’. It was recommended that she did<br />
not start steroids or azathioprine but made<br />
the necessary changes to her lifestyle and<br />
attend for a repeat duodenal biopsy after a<br />
further 9 months. At endoscopy the patient<br />
reported complete resolution of her symptoms,<br />
biopsies were reported as entirely normal<br />
while flow cytometry confirmed the underlying<br />
diagnosis of coeliac disease (figure 1c). She<br />
therefore avoided potentially harmful treatment,<br />
considerable health anxiety and achieved rapid<br />
resolution of her condition following referral.<br />
Notably the referral came from herself via her<br />
GP, not the local gastroenterologist.<br />
Figure 1. Typical duodenal IEL flow cytometry<br />
plots for a non-coeliac individual (a), a<br />
patient with RCD2 (b), and a patient with<br />
coeliac disease (c). Each dot on the plot<br />
represents a separate cell, immunostained<br />
for surface CD3 (y-axis) and cytoplasmic CD3<br />
(x-axis). In addition, CD3+ T cells bearing the<br />
gamma-delta type of TCR are in dark blue,<br />
those with the alpha-beta TCR are in light<br />
blue. Clearly defined population of IELs are<br />
apparent based on the lack of expression of<br />
CD3 (green), the expression of surface and<br />
cytoplasmic CD3 (light and dark blue), or just<br />
cytoplasmic CD3 (orange). Note that RCD1 is<br />
not distinguishable from coeliac disease using<br />
any available diagnostic tests (including flow<br />
cytometry) (reference 2), whereas populations<br />
of CD3+ and gamma delta TCR positive<br />
cells are clearly increased in coeliac disease<br />
compared to normal.<br />
References<br />
1. Rubio-Tapia A, Murray JA. Classification<br />
and management of refractory coeliac<br />
disease. Gut 2010 Apr;59(4):547-57.<br />
2. Nijeboer P, van Wanrooij, van Gils T, et<br />
al. Lymphoma development and survival<br />
in refractory coeliac disease type II:<br />
histological response as a prognostic<br />
factor. United European Gastroenterol J<br />
2017; 5(2): 208-217<br />
3. Woodward JM. Improving outcomes of<br />
refractory Celiac Disease: current and<br />
emerging treatment strategies. Clinical<br />
and Experimental <strong>Gastroenterology</strong> 2016;<br />
9: 225-236<br />
4. Liu H, Brais R, Lavergne-Slove A, et al.<br />
Continual monitoring of intraepithelial<br />
lymphocyte immunophenotype and clonality<br />
is more important than snapshot analysis<br />
in the surveillance of refractory coeliac<br />
disease. Gut. 2010 Apr;59(4):452-60.<br />
5. https://www.coeliac.org.uk/about-us/<br />
media-centre/news/first-rare-diseasecollaborative-network-on-refractorycoeliac/<br />
6. Baggus E, Urwin H, Watson S, Woodward<br />
JM, Sanders DS. How to manage<br />
adult coeliac disease: The perspective<br />
from the NHS England Rare Diseases<br />
Collaborative Network for Non-Responsive<br />
and Refractory Coeliac Disease. Frontline<br />
Gastroenterol. 2019 Aug 8;11(3):235-242<br />
7. Basu K, Creasey H, Bruggemann N,<br />
Stevens J, Bloxham DM, Woodward<br />
JM. The diagnosis of coeliac disease<br />
by flow cytometry of intraepithelial<br />
lymphocytes – a new ‘gold standard’?<br />
Frontline <strong>Gastroenterology</strong> 2021 epub<br />
ahead of print http://dx.doi.org/10.1136/<br />
flgastro-2021-101838<br />
8. Mayassi T, Ladell K, Gudjonson H, et<br />
al. Chronic inflammation permanently<br />
reshapes tissue-resident immunity in celiac<br />
disease. Cell 2019;176:967–81.<br />
9. Abadie V, Sollid LM, Barreiro LB, et al.<br />
Integration of genetic and immunological<br />
insights into a model of celiac disease<br />
pathogenesis. Annu Rev Immunol.<br />
2011;29:493-525<br />
1<br />
NHS Refractory Coeliac Disease Rare<br />
Disease Collaborative Network<br />
Box 133<br />
Addenbrooke’s Hospital<br />
Hills Road<br />
Cambridge CB2 0QQ<br />
01223-596231<br />
(jeremy.woodward@nhs.net)<br />
*Corresponding author<br />
2<br />
Coeliac UK<br />
Apollo Centre,<br />
Desborough Road<br />
High Wycombe<br />
HP11 2QW<br />
3<br />
NHS Refractory Coeliac Disease Rare<br />
Disease Collaborative Network<br />
Academic unit of gastroenterology,<br />
Royal Hallamshire Hospital,<br />
Sheffield S10 2JF<br />
(david.sanders1@nhs.net)<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
29
NEWS<br />
Mother thanks doctors for<br />
saving her and unborn baby<br />
A Herefordshire mother has thanked<br />
clinicians at University Hospitals of North<br />
Midlands NHS Trust (UHNM) for life-saving<br />
treatment she received.<br />
Pregnant Lucy Rossiter was initially thought<br />
to have irritable bowel syndrome (IBS) after<br />
suffering for months with stomach pain, but<br />
doctors in Hereford later found she had a bile<br />
duct infection which posed a serious risk to her<br />
and her baby.<br />
“My doctors contacted Royal Stoke University<br />
Hospital in Stoke-on-Trent and the entire<br />
endoscopy team got together and agreed<br />
that the necessary procedure could be carried<br />
out at Stoke and would be scheduled for the<br />
following morning.<br />
“When I arrived at Stoke I was in terrible pain<br />
and almost unable to stand, let alone walk.<br />
I would have given anything to stop the pain<br />
and make me feel better.<br />
“I found the endoscopy team ready and<br />
waiting for me at Royal Stoke. Everybody I<br />
came into contact with was aware of who I<br />
was and exactly why I was there.<br />
The team were able to remove the bile duct<br />
stone which was causing Lucy’s infection and<br />
affecting her liver function.<br />
Dr Hebbar said: “Lucy’s was an extremely<br />
complicated case, made more challenging<br />
by the fact that she was pregnant. The<br />
endoscopic procedure to remove the stone<br />
in the bile duct involves using X-ray to assess<br />
the location of the stone and understand<br />
the anatomy. In a pregnant lady in her first<br />
trimester, the radiation is a significant risk to<br />
the baby. An additional risk of this particular<br />
procedure is pancreatitis - especially so<br />
in young women - because the bile duct<br />
and pancreas are close to each other. This<br />
complication can be serious and even fatal.<br />
34-year-old Lucy, a primary school teacher<br />
from Kingsland in Herefordshire, was seven<br />
weeks’ pregnant when her condition began to<br />
rapidly deteriorate.<br />
“When I left after having my procedure,<br />
everybody was amazed that I could not only<br />
stand but also walk out of hospital, the pain was<br />
gone instantly. The change was just incredible<br />
“Unfortunately other trusts were unable to<br />
accept Lucy’s case because of the complexity<br />
involved, so we were contacted.<br />
Doctors at Hereford County Hospital scoured<br />
the country to find clinicians with the expert<br />
knowledge needed to treat the mother-of-two.<br />
UHNM’s endoscopy team were contacted<br />
and made such a difference to my condition, it<br />
was as if someone had turned a tap off. William<br />
commented that it was like a different person<br />
who walked out of Royal Stoke.<br />
“When I was ill I was having flare-ups a good<br />
“If we had not done the procedure, there was<br />
clearly a significant risk to Lucy because of<br />
the infection but at the same time, we did not<br />
want to put the baby at any risk because of the<br />
procedure.”<br />
and Lucy was taken to Royal Stoke University<br />
Hospital for care.<br />
Lucy said: “I started to experience abdominal<br />
pains in early May 2020. My GP suspected I<br />
had IBS but over time various remedies proved<br />
to be ineffective and the flare-ups increased<br />
few times a week, so trying to look after my<br />
daughter Poppy was really hard. Now I have a<br />
controlled diet but I can live more normally.<br />
“I need to have my gall bladder removed and<br />
might have to always be a bit more restricted in<br />
what I eat, but I feel I will be able to manage it.<br />
The team performed an endoscopic<br />
ultrasound, which helps to identify internal<br />
structures and can assess the pancreas and<br />
bile duct in detail. Using this, they were able<br />
to identify the location and size of the bile duct<br />
stone and successfully remove it.<br />
in intensity and frequency and on a number of<br />
occasions I had to go to hospital.<br />
“I had been living with these symptoms for about<br />
12 months and during this time I discovered I<br />
“Dr Hebbar and his team at Royal Stoke<br />
were incredible. The care that I had, their<br />
professionalism, just everything. I cannot thank<br />
them enough.<br />
Dr Hebbar continued: “As it turned out, we<br />
did not need to use any x-ray in the end, so<br />
the procedure was completed and the stone<br />
removed with no risk to the baby.<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
was pregnant with my second child, Thomas.<br />
“In April 2021 me and my partner William<br />
became very worried. Not only did my<br />
symptoms continue to get worse but I now<br />
also had our unborn baby to worry about.<br />
“Events finally came to a head one night when<br />
I was in severe pain, vomiting and unable to<br />
stand. William called 111 and I was bluelighted<br />
to Hereford County Hospital. I then<br />
spent the next few days as an inpatient waiting<br />
for a diagnosis. It was horrible, I was desperate<br />
to get home so that I could see my daughter.<br />
“Eventually I was able to get home but my liver<br />
function continued to get worse and I was<br />
back in hospital in May, where my condition<br />
deteriorated rapidly.<br />
“Now I can get back to a more normal life.<br />
We’re quite an active family and we like the<br />
outdoors, we like spending time at the coast,<br />
we spend quite a lot of time with our extended<br />
family. We’ve got holidays booked as well.<br />
When I was ill I couldn’t really enjoy them, so<br />
it’s nice to have something to look forward to.<br />
“I am very grateful to all the NHS for working<br />
together to help me.”<br />
Lucy lives with her partner William Wood, 37,<br />
and is mum to two-year-old daughter Poppy<br />
and new baby Thomas.<br />
Consultant gastroenterologist Dr Srisha<br />
Hebbar and his team cared for Lucy at Royal<br />
Stoke University Hospital.<br />
“Lucy was able to travel back to Hereford the<br />
same day and was discharged the next day.”<br />
30
COMPANY NEWS<br />
INNOVATIVE SHUTTLEPOUCH WINS<br />
FLEXIBLE PLASTIC PACK OF THE YEAR<br />
Alpha Laboratories Ltd. (Eastleigh, UK) and shuttlepac Ltd.<br />
(Telford, UK) are delighted to announce that the unique and<br />
innovative ShuttlePouch has been awarded Flexible Plastic<br />
Pack of the Year in the 2021 UK Packaging Awards.<br />
Developed by shuttlepac, ShuttlePouch provides a compliant UN3373<br />
sample packaging solution that protects users from exposure to<br />
biological samples during transit and on arrival at the laboratory. It<br />
addresses the needs of users, radically improving ease of use and<br />
reducing the cost of packing and shipping sample tubes, compared with<br />
using conventional methods. In addition, ShuttlePouch contains up to<br />
83% less plastic than other standard specimen pouches (an average<br />
of 73% reduction across the range of pouches available), making it the<br />
more environmentally friendly option.<br />
The ShuttlePouch range of leak proof pouches is designed to carry<br />
individual 95kPa pressure differential certifi ed blood or urine specimen<br />
tubes (or any similar sized specimen tube). They include absorbent<br />
material already inside the pouch for convenient compliance to UN3373<br />
packaging requirements.<br />
The pouches also feature a transparent front so the tube and label<br />
are clearly visible. An easy to open tear area facilitates processing<br />
when the samples arrive at the lab.<br />
The ShuttlePouch range is exclusive to Alpha Laboratories in the<br />
UK and Ireland, and provides a powerful, cost effective solution to<br />
the clinical and diagnostic market.<br />
Each leak proof pouch is printed with easy-to-follow instructions<br />
showing how to pack and seal the specimen tube. Simply add a<br />
rigid outer packaging box for a complete and compliant UN3373<br />
solution.<br />
In addition, the 95kPa pressure differential compliant ShuttlePouch<br />
is certified for transport by air (IATA). With all the features described<br />
above, they can be used with any leak free tube for transport by<br />
road or air.<br />
Please visit www.UN3373.co.uk for further information or contact Alpha<br />
Laboratories on 0800 38 77 32 or email marketing@alphalabs.co.uk<br />
WHY NOT WRITE FOR US?<br />
<strong>Gastroenterology</strong> <strong>Today</strong> welcomes the submission of<br />
clinical papers and case reports or news that<br />
you feel will be of interest to your colleagues.<br />
Material submitted will be seen by those working within all<br />
UK gastroenterology departments and endoscopy units.<br />
All submissions should be forwarded to info@mediapublishingcompany.com<br />
If you have any queries please contact the publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
31
Helicobacter Test INFAI ®<br />
The most used 13 C-urea breath test for the<br />
diagnosis of Hp-infection worldwide<br />
• more than 4.5 million INFAI tests performed in Europe<br />
• approved for children from the ages of 3 to 11<br />
• special INFAI test for patients with dyspepsia taking PPIs<br />
• cost-effective CliniPac Basic version for hospital use<br />
INFAI Institute for Biomedical Analysis & NMR Imaging, INFAI UK Ltd<br />
Innovation Centre, University Science Park, University Road, Heslington, YORK YO10 5DG, UK<br />
Phone +44 1904 435 228 - Fax +44 1904 435 229 - mail: info@infai.co.uk - Visit us at www.infai.com