Kompendium 2020 Forschung & Klinik
Das Kompendium 2020 der Universitätsklinik für Orthopädie und Unfallchirurgie von MedUni Wien und AKH Wien (o. Univ.-Prof. R. Windhager) stellt einen umfassenden Überblick über die medizinsichen Leistungen und auch die umfangreichen Forschungsfelder dar. Die Veröffentlichungen zeigen die klinische Relevanz und innovative Ansätze der einzelnen Forschungsrichtungen. Herausgeber: Universitätsklinik für Orthopädie und Unfallchirurgie MedUni Wien und AKH Wien Prof. Dr. R. Windhager ISBN 978-3-200-07715-7
Das Kompendium 2020 der Universitätsklinik für Orthopädie und Unfallchirurgie von MedUni Wien und AKH Wien (o. Univ.-Prof. R. Windhager) stellt einen umfassenden Überblick über die medizinsichen Leistungen und auch die umfangreichen Forschungsfelder dar. Die Veröffentlichungen zeigen die klinische Relevanz und innovative Ansätze der einzelnen Forschungsrichtungen.
Herausgeber: Universitätsklinik für Orthopädie und Unfallchirurgie
MedUni Wien und AKH Wien
Prof. Dr. R. Windhager
ISBN 978-3-200-07715-7
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
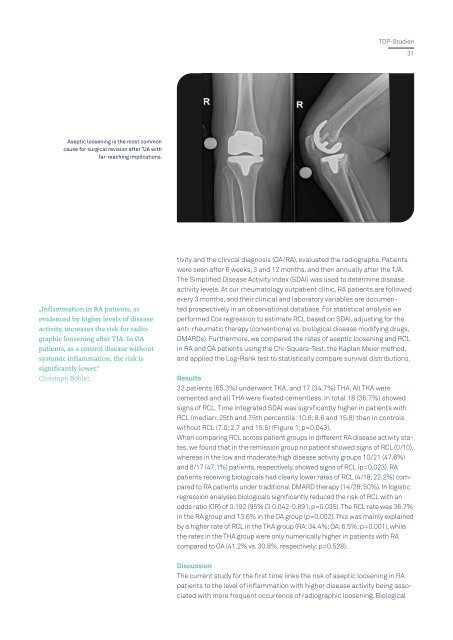
TOP-Studien<br />
31<br />
Aseptic loosening is the most common<br />
cause for surgical revision after TJA with<br />
far-reaching implications.<br />
„Inflammation in RA patients, as<br />
evidenced by higher levels of disease<br />
activity, increases the risk for radiographic<br />
loosening after TJA. In OA<br />
patients, as a control disease without<br />
systemic inflammation, the risk is<br />
significantly lower.“<br />
Christoph Böhler<br />
tivity and the clinical diagnosis (OA/RA), evaluated the radiographs. Patients<br />
were seen after 6 weeks, 3 and 12 months, and then annually after the TJA.<br />
The Simplified Disease Activity Index (SDAI) was used to determine disease<br />
activity levels. At our rheumatology outpatient clinic, RA patients are followed<br />
every 3 months, and their clinical and laboratory variables are documented<br />
prospectively in an observational database. For statistical analysis we<br />
performed Cox regression to estimate RCL based on SDAI, adjusting for the<br />
anti-rheumatic therapy (conventional vs. biological disease modifying drugs,<br />
DMARDs). Furthermore, we compared the rates of aseptic loosening and RCL<br />
in RA and OA patients using the Chi-Square-Test, the Kaplan Meier method,<br />
and applied the Log-Rank test to statistically compare survival distributions.<br />
Results<br />
32 patients (65.3%) underwent TKA, and 17 (34.7%) THA. All TKA were<br />
cemented and all THA were fixated cementless. In total 18 (36.7%) showed<br />
signs of RCL. Time integrated SDAI was significantly higher in patients with<br />
RCL (median; 25th and 75th percentile: 10.8; 8.6 and 15.8) than in controls<br />
without RCL (7.0; 2.7 and 15.5) (Figure 1; p=0.043).<br />
When comparing RCL across patient groups in different RA disease activity states,<br />
we found that in the remission group no patient showed signs of RCL (0/10),<br />
whereas in the low and moderate/high disease activity groups 10/21 (47.6%)<br />
and 8/17 (47.1%) patients, respectively, showed signs of RCL (p=0.023). RA<br />
patients receiving biologicals had clearly lower rates of RCL (4/18; 22.2%) compared<br />
to RA patients under traditional DMARD therapy (14/28; 50%). In logistic<br />
regression analyses biologicals significantly reduced the risk of RCL with an<br />
odds ratio (OR) of 0.192 (95% CI 0.042-0.891; p=0.035). The RCL rate was 36.7%<br />
in the RA group and 13.6% in the OA group (p=0.002). This was mainly explained<br />
by a higher rate of RCL in the TKA group (RA: 34.4%; OA: 6.5%; p=0.001), while<br />
the rates in the THA group were only numerically higher in patients with RA<br />
compared to OA (41.2% vs. 30.8%, respectively; p=0.528).<br />
Discussion<br />
The current study for the first time links the risk of aseptic loosening in RA<br />
patients to the level of inflammation with higher disease activity being associated<br />
with more frequent occurrence of radiographic loosening. Biological