You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Low</strong> <strong>Back</strong> <strong>Pain</strong>: Clinical Practice Guidelines<br />
even when still experiencing pain, and (6) the importance of<br />
improvement in activity levels, not just pain relief.<br />
PROGRESSIVE ENDURANCE EXERCISE AND FITNESS<br />
ACTIVITIES<br />
Presently, most national guidelines for patients<br />
with chronic low back pain endorse progressive<br />
aerobic exercise with moderate to high levels of<br />
evidence. 5,20,46,56,265 High-intensity exercise has also been demonstrated<br />
to have a positive effect on patients with chronic<br />
low back pain. 47,68,225,246-248,275,277 I<br />
The samples of these studies<br />
included patients with long-term duration of symptoms that<br />
were primarily confined to the lumbopelvic region without<br />
generalized pain complaints.<br />
Patients with low back pain and related generalized pain are<br />
believed to have increased neural sensitivity to afferent stimuli,<br />
including proprioception and movement. This sensitizing<br />
process has been termed central sensitization. 44,229,320 Along<br />
with underlying psychosocial factors, deficits in aerobic fitness,<br />
91,162,274,299,322 and tissue deconditioning, this sensitizing<br />
process is believed to impact a person’s functional status and<br />
pain perception. Aerobic fitness has been hypothesized to be<br />
an important component of reducing pain and improving/<br />
maintaining function of these patients.<br />
I<br />
Findings in patients with generalized pain complaints<br />
have demonstrated altered central pain<br />
processing, supporting that these patients should<br />
a40 | april 2012 | volume 42 | number 4 | journal of orthopaedic & sports physical therapy<br />
be managed at lower-intensity levels of training. 228,229 Endurance<br />
exercise has been demonstrated to have a positive effect<br />
on global well-being (standardized mean difference [SMD],<br />
0.44; 95% CI: 0.13, 0.75), physical functioning (SMD, 0.68;<br />
95% CI: 0.41, 0.95), and pain (SMD, 0.94; 95% CI: –0.15,<br />
2.03) associated with fibromyalgia syndrome. 40 Excessively<br />
elevated levels of exercise intensity may be responsible for<br />
increased symptom complaints due to increases in immune<br />
activation with release of proinflammatory cytokines, 208<br />
blunted increases in muscular vascularity leading to widespread<br />
muscular ischemia, 93 and inefficiencies in the endogenous<br />
opioid and adrenergic pain-inhibitory mechanism. 281<br />
Clinicians should consider (1) moderate- to high-<br />
A intensity exercise for patients with chronic low<br />
back pain without generalized pain, and (2) incorporating<br />
progressive, low-intensity, submaximal fitness and<br />
endurance activities into the pain management and health<br />
promotion strategies for patients with chronic low back pain<br />
with generalized pain.<br />
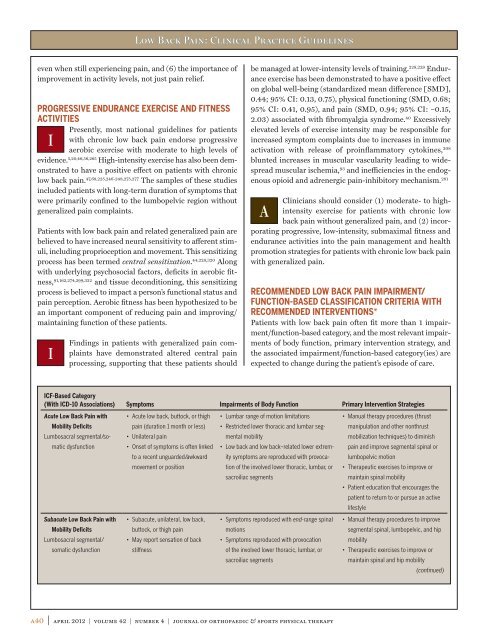
RECOMMENDED LOW BACK PAIN IMPAIRMENT/<br />
FUNCTION-BASED CLASSIFICATION CRITERIA WITH<br />
RECOMMENDED INTERVENTIONS*<br />
Patients with low back pain often fit more than 1 impairment/function-based<br />
category, and the most relevant impairments<br />
of body function, primary intervention strategy, and<br />
the associated impairment/function-based category(ies) are<br />
expected to change during the patient’s episode of care.<br />
ICF-Based Category<br />
(With ICD-10 Associations) Symptoms Impairments of Body Function Primary Intervention Strategies<br />
Acute <strong>Low</strong> <strong>Back</strong> <strong>Pain</strong> with<br />
Mobility Deficits<br />
Lumbosacral segmental/so-<br />
matic dysfunction<br />
Subacute <strong>Low</strong> <strong>Back</strong> <strong>Pain</strong> with<br />
Mobility Deficits<br />
Lumbosacral segmental/<br />
somatic dysfunction<br />
• Acute low back, buttock, or thigh<br />
pain (duration 1 month or less)<br />
• Unilateral pain<br />
• Onset of symptoms is often linked<br />
to a recent unguarded/awkward<br />
movement or position<br />
• Subacute, unilateral, low back,<br />
buttock, or thigh pain<br />
• May report sensation of back<br />
stiffness<br />
• Lumbar range of motion limitations<br />
• Restricted lower thoracic and lumbar seg-<br />
mental mobility<br />
• <strong>Low</strong> back and low back–related lower extrem-<br />
ity symptoms are reproduced with provoca-<br />
tion of the involved lower thoracic, lumbar, or<br />
sacroiliac segments<br />
• Symptoms reproduced with end-range spinal<br />
motions<br />
• Symptoms reproduced with provocation<br />
of the involved lower thoracic, lumbar, or<br />
sacroiliac segments<br />
• Manual therapy procedures (thrust<br />
manipulation and other nonthrust<br />
mobilization techniques) to diminish<br />
pain and improve segmental spinal or<br />
lumbopelvic motion<br />
• Therapeutic exercises to improve or<br />
maintain spinal mobility<br />
• Patient education that encourages the<br />
patient to return to or pursue an active<br />
lifestyle<br />
• Manual therapy procedures to improve<br />
segmental spinal, lumbopelvic, and hip<br />
mobility<br />
• Therapeutic exercises to improve or<br />
maintain spinal and hip mobility<br />
(continued)