2008 Scientific Report
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
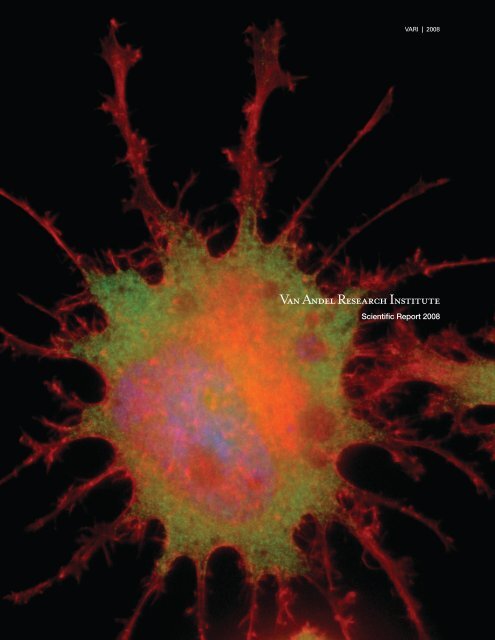
Cover photo: Prostate tumor PC3 cell treated with PI-3K inhibitor. Morphological architecture<br />
of a prostate tumor PC3 cell treated with the phosphoinositol-3 kinase inhibitor LY294002 for 72<br />
hours. PC3 cells were immunostained with phallodin (red) and antibody toward vinculin (green).<br />
Nuclei were stained with Hoechst (blue). In this cell, inhibition of PI-3K produced the formation of<br />
numerous filopodia and microspikes. This is the result of cellular stress, which will eventually lead<br />
to the death of the cell. Photo by Laura Lamb of the Miranti lab.
VARI | <strong>2008</strong><br />
Van Andel Research Institute <strong>Scientific</strong> <strong>Report</strong> <strong>2008</strong>
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Title page illustration: The glucocorticoid receptor. The figure represents the crystal structure<br />
of the glucocorticoid receptor (GR) bound to deacylcortivazol, which is a highly potent ligand<br />
against childhood leukemia. The GR protein chain is shown as ribbons, with helix 1 in blue and the<br />
coactivator helix in red. The deacylcortivazol molecule is shown within the GR structure in green,<br />
with the GR ligand-binding pocket shown by the yellow mesh. Structure by the Xu lab.<br />
Published June <strong>2008</strong>.<br />
Copyright <strong>2008</strong> by the Van Andel Institute; all rights reserved.<br />
Van Andel Institute, 333 Bostwick Avenue, N.E.,<br />
Grand Rapids, Michigan 49503, U.S.A.<br />
ii
VARI | <strong>2008</strong><br />
Director’s Introduction 1<br />
George F. Vande Woude, Ph.D.<br />
Laboratory <strong>Report</strong>s 5<br />
Arthur S. Alberts, Ph.D.<br />
Cell Structure and Signal Integration 6<br />
Brian Cao, M.D.<br />
Antibody Technology 9<br />
Gregory S. Cavey, B.S.<br />
Mass Spectrometry and Proteomics 12<br />
Nicholas S. Duesbery, Ph.D.<br />
Cancer and Developmental Cell Biology 15<br />
Bryn Eagleson, B.S., RLATG<br />
Vivarium and Transgenics Program 20<br />
Kyle A. Furge, Ph.D.<br />
Computational Biology 22<br />
Brian B. Haab, Ph.D.<br />
Cancer Immunodiagnostics 25<br />
Table of Contents<br />
Rick Hay, Ph.D., M.D., F.A.H.A.<br />
Noninvasive Imaging and Radiation Biology<br />
Office of Translational Programs 29<br />
Jeffrey P. MacKeigan, Ph.D.<br />
Systems Biology 34<br />
Cindy K. Miranti, Ph.D.<br />
Integrin Signaling and Tumorigenesis 38<br />
James H. Resau, Ph.D.<br />
Division of Quantitative Sciences<br />
Analytical, Cellular, and Molecular Microscopy<br />
Microarray Technology<br />
Molecular Epidemiology 42<br />
Pamela J. Swiatek, Ph.D., M.B.A.<br />
Germline Modification and Cytogenetics 46<br />
Bin T. Teh, M.D., Ph.D.<br />
Cancer Genetics 51<br />
Steven J. Triezenberg, Ph.D.<br />
Transcriptional Regulation 55<br />
George F. Vande Woude, Ph.D.<br />
Molecular Oncology 59<br />
Craig P. Webb, Ph.D.<br />
Program for Translational Medicine<br />
Tumor Metastasis and Angiogenesis 63<br />
Michael Weinreich, Ph.D.<br />
Chromosome Replication 68<br />
Bart O. Williams, Ph.D.<br />
Cell Signaling and Carcinogenesis 72<br />
H. Eric Xu, Ph.D.<br />
Structural Sciences 76<br />
iii
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Daniel Nathans Memorial Award 80<br />
Harald zur Hausen, M.D., and Douglas R. Lowy, M.D.<br />
Postdoctoral Fellowship Program 82<br />
List of Fellows<br />
Student Programs 84<br />
Grand Rapids Area Pre-College Engineering Program<br />
Summer Student Internship Program<br />
Han-Mo Koo Memorial Seminar Series 88<br />
2007 | <strong>2008</strong> Seminars<br />
Van Andel Research Institute Organization 93<br />
Boards<br />
Office of the Director<br />
VAI Administrative Organization<br />
iv
VARI | <strong>2008</strong><br />
Director’s Introduction
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
George F. Vande Woude<br />
Director’s Introduction<br />
A few short years ago, the Van Andel Research Institute was an idea that many said wouldn’t work—an independent research<br />
institute located in west Michigan with no tie to a major university. Today it is a thriving organization with an excellent reputation,<br />
one that is poised to more than double its size and its contributions to science and human health.<br />
Perhaps this is most evident in our ability to compete for external grants; success in the tight competition for grant funding is an<br />
important measure of our research quality. The National Institutes of Health (NIH) is a major source of research funding in our<br />
disciplines, so I am particularly pleased with the awards our VARI scientists received in the past year.<br />
Steve Treizenberg has received a three-year R01 award from the National Institutes of Health (NIH) for his project, “Chromatin<br />
and Coactivators in HSV-1 Gene Regulation”. Bart Williams also received an R01 award, for five years, for a project titled<br />
“Mouse Models to Characterize the Role of Lrp6 in Metabolic Syndrome”. Finally, Eric Xu received a four-year R01 for his<br />
project titled “Structural and Functional Studies of the Nuclear Receptor PPARg”, and it is important to note that Eric now has<br />
three active R01 grants. Our congratulations go out to Steve, Bart, Eric, and their labs for the rigorous work that went into<br />
making their applications successful.<br />
The Department of Defense also funds cancer research on a competitive application basis. Early in 2007, VARI had three<br />
awards out of 87 projects recommended for funding by the Breast Cancer Research Program, and this was from more than<br />
1,200 proposals that were reviewed. The projects awarded were Kate Eisenmann’s “A Role for Formin-Mediated Cytoskeletal<br />
Regulation in the Mesenchymal-Amoeboid Transition in Breast Cancer Development” (Alberts lab); Carrie Graveel’s “Met<br />
Signaling Promotes Mammary Stem Cell Proliferation” (Vande Woude lab); and Jim Resau’s “Intravital Imaging of Developing<br />
Breast Cancer Lesion of Defined Genomic Profile in a Mouse” (Resau lab). This was clearly an excellent performance.<br />
Showing that this was not an aberration, later in 2007, another three awards were made from the DOD Prostate and Ovarian<br />
Cancer program. The successful proposals were from Kate Eisenmann (again!), for “Diaphanous-related Formins in Ovarian<br />
Cancer Metastasis” (Alberts lab); Laura Lamb, for “Survival Signaling in Prostate Cancer: Role of Androgen Receptor and<br />
Integrins in Regulating Survival” (Miranti lab); and Cindy Miranti for “Mechanisms of KAI1/CD82-induced Prostate Cancer<br />
Metastasis” (Miranti lab).<br />
2
VARI | <strong>2008</strong><br />
We have also been successful in competing for funding from nonfederal sources. Funding was received from the state of<br />
Michigan to support the Good Manufacturing Practices Facility project under the direction of Rick Hay. Craig Webb received<br />
an award for “Establishment of an Innovative Clinical Research Alliance” from the Michigan Strategic Economic Investment &<br />
Commercialization Board. Bin Teh has received awards from the National Foundation for Cancer Research and from the VHL<br />
Family Alliance Fund for Cancer Research; Art Alberts received project funding from the J.P. McCarthy Fund; and Jennifer<br />
Bromberg-White received a fellowship from the Knight’s Templar Foundation. Congratulations to all for a spectacular showing<br />
of top-quality proposals!<br />
On another note, congratulations go out to Brian Haab, who was promoted to Senior <strong>Scientific</strong> Investigator in August 2007.<br />
Brian’s Laboratory of Cancer Immunodiagnostics is working on developing new techniques and new diagnostic markers for<br />
pancreatic cancer, one of the cancers most difficult to treat successfully. Brian has also been elected to a three-year term on<br />
the Board of Directors of the U.S. Human Proteome Organization, which supports and promotes the use of proteomics and<br />
provides information about the proteomes of various species.<br />
We are pleased to announce the formation of VARI International, headed by Bin Tean Teh. VARI International was formed<br />
to organize and formalize the Institute’s international opportunities. Currently, two laboratories with foreign host institutes<br />
are in operation: NCCS–VARI Translational Research Laboratory (headed by Bin Tean Teh) at the National Cancer Centre of<br />
Singapore, and NMU–VARI Antibody Technology Laboratory (headed by Brian Cao) at Nanjing Medical University.<br />
NCCS–VARI is focusing on cancers that are prevalent in Asian countries and on translational cancer research. Since its<br />
establishment at the end of 2006, NCCS–VARI has expanded to include five clinical fellows, three postdoctoral fellows, four<br />
research technicians, and one bioinformatics scientist. We have competed successfully for several research fellowships from<br />
local funding agencies, two scientific papers have been published, and a regional mini-symposium has been organized.<br />
NMU–VARI is developing a variety of murine and human monoclonal antibodies and antibody fragments for potential clinical<br />
diagnostic and therapeutic applications. Since the establishment of NMU-VARI in 2005, six Ph.D. students and four master’s<br />
degree students have been trained, three manuscripts have been published, and four grant applications have been submitted.<br />
Of those grant application submissions, two have been funded (one from U.S. funding, the other from China).<br />
Cooperative/collaborative arrangements at sites in Australia, Sweden, and France are currently being explored. Establishing<br />
such laboratories and determining research projects will take into consideration their ability to synergize and complement<br />
VARI’s mission.<br />
The Program of Translational Medicine under the direction of Craig Webb has established the essential infrastructure and<br />
partnerships that allow VARI to collaborate with other institutions for cutting-edge biomarker-driven clinical research. The<br />
Center for Molecular Medicine, in partnership with Spectrum Health Hospitals, was established to perform molecular-based<br />
diagnostic testing. A community research network of institutions (ClinXus) has also been formed that provides access to<br />
biomarker technologies (molecular and imaging), physician expertise, and patient populations for investigators interested in<br />
clinical research.<br />
The Program of Translational Medicine has also led to the development of a specific personalized medicine protocol in which<br />
genomic technologies are used with the XenoBase bioinformatics tools to identify optimal drug combinations that target the<br />
genotype of tumors from late-stage cancer patients. An expanded trial of 200 patients will open for enrollment in <strong>2008</strong>.<br />
3
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
In June 2007, VARI was awarded full accreditation by the Association for Assessment and Accreditation of Laboratory Animal<br />
Care (AAALAC). This distinction recognizes our institutional commitment to responsible and ethical animal care beyond the<br />
standards required by law. Our success in receiving this accreditation was made possible only through the concerted efforts<br />
of many people, and this achievement is one of which we can all be proud.<br />
Finally in the fall, we presented the Daniel Nathans Memorial Award to Harald zur Hausen and Douglas R. Lowy. Dr. zur Hausen’s<br />
lab identified infection by papillomavirus as the main cause of cervical cancer, and Dr. Lowy’s studies helped lead to a new<br />
way to prepare vaccines that prevent infection by the virus. The importance of this work in terms of improving human health<br />
worldwide is obvious, and we are pleased to have these distinguished researchers join the list of Nathans Award recipients.<br />
In conclusion, 2007 has been a wonderful year for VAI. With the dedication and ceaseless efforts of our scientists and strong<br />
support from our community, we have built a home on “the hill” that is recognized nationwide for its excellence in research. We<br />
continue to exceed even our own expectations and we are eagerly looking forward to the years to come.<br />
4
VARI | <strong>2008</strong><br />
Laboratory <strong>Report</strong>s<br />
5
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Arthur S. Alberts, Ph.D.<br />
Laboratory of Cell Structure and Signal Integration<br />
In 1993, Dr. Art Alberts received his Ph.D. in Physiology and Pharmacology at the University of<br />
California, San Diego School of Medicine, where he studied with Jim Feramisco. Dr. Alberts trained<br />
as a postdoctoral fellow from 1994 to 1997 with Richard Treisman at the Imperial Cancer Research<br />
Fund in London, England, where Dr. Treisman is the current Director. From 1997 through 1999, Dr.<br />
Alberts was an Assistant Research Biochemist in the laboratory of Frank McCormick at the University<br />
of California, San Francisco. In January 2000, Dr. Alberts joined VARI as a <strong>Scientific</strong> Investigator; he<br />
was promoted in 2006 to Senior <strong>Scientific</strong> Investigator. Also in 2006, he established and became the<br />
Director of the Flow Cytometry core facility.<br />
Staff Students Visiting Scientists<br />
Jun Peng, M.D.<br />
Kathryn Eisenmann, Ph.D.<br />
Holly Holman, Ph.D.<br />
Richard A. West, M.S.<br />
Susan Kitchen, B.S.<br />
Kellie Leali<br />
Aaron DeWard, B.S.<br />
Christopher Gorter<br />
Albert Rodriguez<br />
Katja Strunk<br />
Stephen Matheson, Ph.D.<br />
Brad Wallar, Ph.D.<br />
6
VARI | <strong>2008</strong><br />
Research Interests<br />
The Laboratory of Cell Structure and Signal Integration is devoted to understanding how defects in cellular architecture affect<br />
the progression to malignancy and support the tumorigenic platform. The driving hypothesis is that the cytoskeleton does not<br />
only structurally support cell morphology, division, and migration, but with its dynamic nature, it organizes intracellular signaling<br />
networks in order to effectively interpret proliferative and migratory responses to extracellular cues. On a molecular basis, we<br />
are interested in how cells build and control the cytoskeletal assembly machines and how these molecular machines work in<br />
concert within the cell. Through combined molecular, cellular, and genetic approaches, the ultimate goal of the lab is identifying<br />
defective nodes in the networks governing cytoskeletal remodeling in order to improve diagnosis and devising molecular tools<br />
to correct the defective circuits.<br />
Our focus is the role of Rho GTPases in signal transduction networks that control cell proliferation and motility. These highly<br />
conserved molecular switches act within growth factor responses by alternating between GTP- and GDP-bound forms. Upon<br />
GTP binding, Rho proteins undergo a conformational change that allows them to bind to and modulate the activity of effectors<br />
that remodel cell shape, drive motility and division, or alter gene expression patterns.<br />
One set of GTPase effector proteins acts as machines that assemble components of the cytoskeleton. The mammalian<br />
Diaphanous-related formin (mDia) family of actin-nucleating proteins initiate and control the elongation of new actin filaments.<br />
The three conserved mDia proteins (mDia1–3), along with insect Diaphanous protein and their budding yeast counterpart<br />
Bni1p, are canonical members of the formin family. With our discovery of one of the first formin proteins, mDia2, we have taken<br />
a leading role in their characterization.<br />
To study the role of mDia1 in vivo, the murine Drf1 gene was knocked out by conventional gene-targeting methods. Both<br />
Drf1 +/– and Drf1 –/– mice become progressively lympho- and myelodysplastic. Drf1-targeted mice are prone to developing<br />
tumors; cancers observed thus far include various leukemias, monocytosis, and plasmocytomas. Overall, mice lacking one<br />
or both Drf1 alleles phenocopy human myelodysplastic syndrome. Numerous defects in cytoskeletal remodeling have been<br />
observed in immune cells, including impaired T cell adhesion, migration, and the appearance of supernumerary centrosomes,<br />
which are indicative of failed cell division.<br />
These results were published in the Journal of Biological Chemistry and in Cancer Research. In the first paper with lead author<br />
Kate Eisenmann, entitled “T cell responses in mammalian Diaphanous-related formin mDia1 knock-out mice”, we demonstrated<br />
a role for mDia1 in normal immune cell function. Disruption of mDia1 leads to fewer T cells in secondary lymphoid<br />
organs in Drf1-null animals. T cell adhesion, migration, and proliferation upon activation were all impaired in T cells derived<br />
from Drf1-targeted mice. These results pointed to a crucial role for mDia1 in the dynamic regulation of the actin cytoskeleton<br />
in activated T cells.<br />
The second paper, with lead author Jun Peng, “Myeloproliferative defects following targeting of the Drf1 gene encoding the<br />
mammalian Diaphanous-related formin mDia1”, showed that mDia1 also plays an essential role in myelopoiesis. As animals age,<br />
they develop myeloproliferative defects in both the bone marrow and peripheral blood. These observations point to a crucial role<br />
of mDia1 in maintaining myeloid homeostasis, potentially by functioning as a tumor suppressor or susceptibility gene.<br />
7
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Overall, the mDia1 knock-out phenotype resembles human chronic myeloproliferative syndrome (MPS) and myelodysplastic<br />
syndrome (MDS). Both MPS and MDS have been characterized as preleukemic states, with variable lymphopenia, excess<br />
or dysfunctional erythrocytes, chronic myelomonocytic leukemia, ineffective hematopoiesis, and, in some cases, advancing<br />
myelofibrosis. Instances of neutrophilic dermatoses (Sweet syndrome) can also accompany MDS and MPS. MDS is a frequent<br />
hematologic disorder that typically affects older patients and is thought to be a stem cell disorder. Dysplastic features of<br />
the nucleus or cytoplasm, as observed in the mDia1 knock-out mice, and altered cellularity of the bone marrow are also<br />
characteristic of MDS. The effect of Drf1 gene targeting and the resulting mDia1 knock-out suggests that the DRF1 gene for<br />
human mDia1 is affected in MPS, MDS, or other preleukemic pathologies. Ongoing studies are focused on examining if defects<br />
in the human gene encoding mDia1 might be defective in MDS patients.<br />
Recent Publications<br />
From left: Matheson, Rodriguez, West, Strunk, DeWard, Guthrey, Leali, Kitchen, Eisenmann, Alberts<br />
Uma, Kamasani, James B. DuHadaway, Arthur S. Alberts, and George C. Prendergast. In press. mDia function is critical for<br />
the cell suicide program triggered by farnesyl transferase inhibition. Cancer Biology & Therapy.<br />
Sarmiento, Corina, Weigang Wang, Athanassios Dovas, Hideki Yamaguchi, Mazen Sidani, Mirvat El-Sibai, Vera DesMarais,<br />
Holly A. Holman, Susan Kitchen, Jonathan M. Backer, Art Alberts, and John Condeelis. <strong>2008</strong>. WASP family members and<br />
formin proteins coordinate regulation of cell protrusions in carcinoma cells. Journal of Cell Biology 180(6): 1245–1260.<br />
Wang, P., M.R. Bowl, S. Bender, J. Peng, L. Farber, J. Chen, A. Ali, Z. Zhang, A.S. Alberts, R.V. Thakker, A. Shilatifard,<br />
B.O. Williams, and B.T. Teh. <strong>2008</strong>. Parafibromin, a component of the human PAF complex, regulates growth factors and is<br />
required for embryonic development and survival in adult mice. Molecular and Cellular Biology 28(9): 2930–2940.<br />
Dent, Erik W., Adam V. Kwiatkowski, Leslie M. Mebane, Ulrike Philippar, Melanie Barzik, Douglas A. Rubinson, Stephanie<br />
Gupton, J. Edward Van Veen, Craig Furman, Jiangyang Zhang, Arthur S. Alberts, Susumu Mori, and Frank B. Gertler. 2007.<br />
Filopodia are required for cortical neurite initiation. Nature Cell Biology 9(12): 1347–1359.<br />
Eisenmann, Kathryn M., Richard A. West, Dagmar Hildebrand, Susan M. Kitchen, Jun Peng, Robert Sigler, Jinyi Zhang,<br />
Katherine A. Siminovitch, and Arthur S. Alberts. 2007. T cell responses in mammalian Diaphanous-related formin mDia1<br />
knock-out mice. Journal of Biological Chemistry 282(34): 25152–25158.<br />
Gupton, Stephanie L., Katherine Eisenmann, Arthur S. Alberts, and Clare M. Waterman-Storer. 2007. mDia2 regulates actin<br />
and focal adhesion dynamics and organization in the lamella for efficient epithelial cell migration. Journal of Cell Science<br />
120(19): 3475–3487.<br />
Peng, Jun, Susan M. Kitchen, Richard A. West, Robert Sigler, Kathryn M. Eisenmann, and Arthur S. Alberts. 2007. Myeloproliferative<br />
defects following targeting of the Drf1 gene encoding the mammalian Diaphanous-related formin mDia1. Cancer<br />
Research 67(16): 7565–7571.<br />
8
VARI | <strong>2008</strong><br />
Brian Cao, M.D.<br />
Laboratory of Antibody Technology<br />
Dr. Cao obtained his M.D. from Peking University Medical Center, People’s Republic of China, in 1986.<br />
On receiving a CDC fellowship award, he was a visiting scientist at the National Center for Infectious<br />
Diseases, Centers for Disease Control and Prevention in Atlanta (1991–1994). He next served as a<br />
postdoctoral fellow at Harvard (1994–1995) and at Yale (1995–1996). From 1996 to 1999, Dr. Cao was<br />
a Scientist Associate in charge of the Monoclonal Antibody Production Laboratory at the Advanced<br />
BioScience Laboratories–Basic Research Program at the National Cancer Institute, Frederick Cancer<br />
Research and Development Center, Maryland. Dr. Cao joined VARI as a Special Program Investigator<br />
in June 1999 and was promoted to Senior <strong>Scientific</strong> Investigator in July 2006.<br />
Staff<br />
Quliang Gu, Ph.D.<br />
Ping Zhao, M.S.<br />
Tessa Grabinski, B.S.<br />
Students<br />
Guipeng Ding<br />
Jenna Manby<br />
Rui Sun<br />
Ning Xu<br />
Aixia Zhang<br />
9
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Research Interests<br />
Antibodies are primary tools of biomedical science. In basic research, the characterization and analysis of almost any molecule<br />
involves the production of specific monoclonal or polyclonal antibodies that react with it. Antibodies are also widely used in<br />
clinical diagnostic applications. Further, antibodies are making rapid inroads into clinical treatment of a variety of diseases,<br />
driven by technological evolution from chimeric and humanized to fully human antibodies.<br />
Functioning as an antibody production core facility at VARI, our lab’s primary responsibility is to develop state-of-the-art services<br />
and technology platforms for monoclonal antibody (mAb) production and characterization. Our technologies and services<br />
include antigen preparation and animal immunization; peptide design and coupling to protein carriers; immunization with living<br />
or fixed cells; conventional antigen/adjuvant preparation; and immunizing a wide range of antibody-producing models (including<br />
mice, rats, rabbits, and transgenic or knock-out mice). Our work also includes the generation of hybridomas from spleen cells<br />
of immunized mice and rats; hybridoma expansion and subcloning; cryopreservation of hybridomas; mAb isotyping; ELISA<br />
screening of hybridoma supernatants; mAb characterization by immunoprecipitation, immunohistochemistry, immunofluorescence<br />
staining, Western blot, FACS, and in vitro bioassays; conjugation of mAbs to enzymes, biotin/streptavidin, or fluorescent<br />
reporters; and development of detection kits such as sandwich ELISA. We contract our services to biotechnology companies,<br />
producing and purifying mAbs for their research and for diagnostic kit development. Over the last year, this core has finished<br />
14 antibody development projects for researchers and industrial users in Michigan and nationwide.<br />
Michigan’s Core Technology Alliance (CTA), funded by the state government, was created in 2001. The Antibody Technology<br />
Core at VARI and the Hybridoma Core at the University of Michigan in Ann Arbor joined together to form the Michigan Antibody<br />
Technology Core (MATC) and became the seventh core of the CTA in March 2005. The goals of MATC are to provide state-ofthe-art<br />
antibody technologies and services to research scientists; to generate, characterize, produce, and purify a wide variety<br />
of mAbs for clinical diagnostic/therapeutic applications; and to advance biomedical research and development. The Antibody<br />
Technology lab at VARI serves as the core’s hub, and Dr. Brian Cao is the director of MATC.<br />
We also carry out research and collaboration projects, which use both murine mAbs and human antibody fragments generated<br />
in our lab, aimed at developing cancer diagnostic and therapeutic applications.<br />
• Epitope mapping and characterization of a Met-binding peptide using phage-display peptide libraries. This<br />
project is to screen for a specific Met-binding peptide from a random-peptide phage-display library that could<br />
be used as an in vivo imaging agent (and possibly as a therapeutic carrier) when labeled with radioisotopes<br />
or conjugated with chemotherapeutics. A subtractive bio-panning approach on intact cells was used. A<br />
Met-binding peptide was obtained that recognizes the Met extracellular domain under native conditions and<br />
internalizes upon binding to the Met receptor. In vivo imaging showed that the radiolabeled peptide in a<br />
mouse xenograft model had tumor-associated activity. We are modifying this peptide to increase its binding<br />
affinity, and we are screening new Met-binding peptides having higher affinity for future clinical applications.<br />
• Development of highly specific anti-Met mouse mAbs with potential application for clinical immunohistochemical<br />
diagnosis. In collaboration with Beatrice Knudsen’s lab at the Fred Hutchinson Cancer Research Center,<br />
we have developed a monoclonal antibody, designated MET4, with the goal of accurately and reproducibly<br />
measuring MET in formalin-fixed paraffin-embedded (FFPE) tissues. MET4 was selected as the best probe<br />
from a pool of MET-avid monoclonal antibodies, based on its specific staining pattern in FFPE preparations of<br />
normal human prostate tissues. The reliability of MET4 immunohistochemistry was assessed by comparing<br />
MET4-IHC in FFPE cell pellets with immunoblotting analysis, which demonstrated a high avidity of MET4 for<br />
formalin-treated MET. These properties encourage further development of MET4 as a multipurpose molecular<br />
diagnostic reagent to help guide selection of individual patients being considered for treatment with METantagonistic<br />
drugs.<br />
10
VARI | <strong>2008</strong><br />
• Characterization of anti-EGFR and anti-Met human Fab fragments and conjugation with chemotherapeutics<br />
to generate reagents for preclinical studies. In collaboration with the Ministry of Health’s Key Laboratory of<br />
Antibody Technology in Nanjing Medical University, we screened several Fab fragments (from a naïve human<br />
Fab phage library constructed in our lab in late 2004) that specifically recognize Met and EGFR. By modifying<br />
and improving bio-panning strategies, we have selected Fab fragments that recognize the Met and EGFR<br />
extracellular domains in native confirmation with reasonable affinity. These fragments have internalization<br />
properties making them attractive as conjugate reagents for immuno-chemotherapy or immuno-radiation<br />
therapy against cancer. We have conjugated anti-EGFR human Fab to paclitaxel as an immuno-chemotherapy<br />
reagent and investigated its in vitro anti-tumor efficacy using cell proliferation and apoptosis assays. We will<br />
further explore its in vivo anti-tumor efficacy in xenograft or orthotopic animal models, and we will label this<br />
Fab fragment with radioisotopes to evaluate its potential as an immuno-radiation reagent for in vivo imaging<br />
diagnosis and immuno-radiation therapy.<br />
From left: Zhao, Sun, Nelson, Ding, Grabinski, Cao<br />
Recent Publications<br />
Wang, Xin, Jin Zhu, Ping Zhao, Yongjun Jiao, Ning Xu, Tessa Grabinski, Chao Liu, Cindy K. Miranti, Tao Fu, and Brian B. Cao.<br />
2007. In vitro efficacy of immuno-chemotherapy with anti-EGFR human Fab-Taxol conjugate on A431 epidermoid carcinoma<br />
cells. Cancer Biology & Therapy 6(6): 980–987.<br />
Zhao, Ping, Tessa Grabinski, Chongfeng Gao, R. Scot Skinner, Troy Giambernardi, Yanli Su, Eric Hudson, James Resau,<br />
Milton Gross, George F. Vande Woude, Rick Hay, and Brian Cao. 2007. Identification of a Met-binding peptide from a phage<br />
display library. Clinical Cancer Research 13(20): 6049–6055.<br />
11
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Gregory S. Cavey, B.S.<br />
Laboratory of Mass Spectrometry and Proteomics<br />
Mr. Cavey received his B.S. degree from Michigan State University in 1990. Prior to joining VARI he was<br />
employed at Pharmacia in Kalamazoo, Michigan, for nearly 15 years. As a member of a biotechnology<br />
development unit, he was group leader for a protein characterization core laboratory. More recently<br />
as a research scientist, he was principal in the establishment and application of a state-of-the-art<br />
proteomics laboratory for drug discovery. Mr. Cavey joined VARI as a Special Program Investigator in<br />
July 2002.<br />
Staff<br />
Paula Davidson, M.S.<br />
Caryn Lehner, M.S.<br />
Student<br />
Matthew McElliott<br />
12
VARI | <strong>2008</strong><br />
Research Interests<br />
Through recent advancements in technology, mass spectrometry–based proteomics is now an important and widespread tool<br />
in basic and clinical research. In 2005, VARI purchased a Waters Q-Tof mass spectrometry system that remains at the cutting<br />
edge of many research applications. This equipment allows us to provide routine mass spectrometry services and to develop<br />
new services such as protein profiling for biomarker discovery and protein phosphorylation analysis.<br />
Protein identification analysis and protein molecular weight determination are routine services performed on sub-microgram<br />
amounts of material to address a wide variety of biological questions. Protein identification via mass spectrometry is mainly<br />
used to identify novel protein-protein interactions and can be performed on proteins in SDS-PAGE gels or proteins in solutions.<br />
Molecular weight determination of protein solutions is typically employed to confirm the expression and purification of recombinant<br />
proteins to be used as reagents in x-ray crystallographic experiments or drug screening/cell-based assays.<br />
Our research emphasis is on 1) developing liquid chromatography–mass spectrometry (LC-MS) protein profiling analysis for<br />
systems biology research and biomarker discovery and 2) improving methods for identifying and quantifying phosphorylation<br />
of proteins.<br />
LC-MS protein profiling<br />
Liquid chromatography–mass spectrometry is used at most major research institutions to analyze complex protein mixtures<br />
for systems biology research and biomarker discovery. Our lab collaborates with Waters Corporation, a major manufacturer<br />
of mass spectrometry and HPLC equipment, to evaluate and improve existing methods while applying LC-MS to the research<br />
efforts at VARI and to those of external clients. Our LC-MS system employs a novel data acquisition method unique to Waters<br />
mass spectrometers, termed LC-MS E , whereby quantitative and qualitative data are collected in a single analysis. Protein<br />
samples are first digested into peptides using trypsin and then analyzed by reverse-phase nanoscale LC-MS. Recording<br />
peptide mass, HPLC retention time, and intensity as measured in the mass spectrometer, we digitize the data to allow comparisons<br />
across samples. Quantitation is based on the measurement and subsequent comparison of the chromatographic peak<br />
area for each peptide across samples. Qualitative protein identification data is collected in a multiplexed, non-intensity-biased<br />
fashion concurrent with quantitative data. One current pilot project is a time-course analysis of protein secretion (secretome)<br />
from mouse 3T3-L1 preadipocytes as they differentiate in response to treatment with dexamethasone-insulin or with the PPARg<br />
antagonist rosiglitasone; a second is the study of the secretome of a cell line model of hypoxia. In addition to mechanismof-action<br />
studies, our goal is to use LC-MS to discover candidate biomarkers of disease. Current research efforts focus on<br />
sample processing techniques to reproducibly fractionate highly complex samples such as blood plasma, tissue, and urine to<br />
allow quantitative analysis. Replicate LC-MS analysis of carefully chosen samples and multivariate data analysis will allow us to<br />
differentiate between normal biological variation and disease.<br />
Protein phosphorylation analysis<br />
Mapping post-translational modifications of proteins such as phosphorylation is an important yet difficult undertaking. In<br />
cancer research, phosphorylation regulates many protein pathways that could serve as targets for drug therapy. In recent<br />
years, mass spectrometry has emerged as a primary tool in determining site-specific phosphorylation and relative quantitation.<br />
Phosphorylation analysis is complicated by many factors, but principally by the low-stoichiometry modifications that<br />
may regulate pathways: we are sometimes dealing with 0.01% or less of phosphorylated protein among a large excess of a<br />
nonphosphorylated counterpart.<br />
13
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
As with most mass spectrometry–based methods, mapping phosphorylation sites on proteins begins by enzymatically digesting<br />
protein into peptides using trypsin, Lys-C, Staph V8, or chymotrypsin. Peptides are separated by nanoscale reverse-phase<br />
HPLC and analyzed by on-line electrospray ionization on a quadrupole time-of-flight (Q-Tof) mass spectrometer. Samples<br />
are analyzed using the MS E data acquisition mentioned above. MS E toggles the collision energy in the mass spectrometer<br />
between high and low every second throughout the analytic run. Low-collision-energy data acquisition allows peptide mass<br />
to be recorded at high sensitivity with high mass accuracy to implicate phosphorylation based on mass alone. The peptide<br />
intensity measured in the mass spectrometer is also recorded and used for relative quantitation in time course studies. During<br />
high-collision-energy acquisition, all peptides are fragmented to identify the protein(s) from which the peptides were liberated by<br />
enzyme digestion and to locate specific phosphorylated amino acids. MS E differs from other mass spectrometry approaches<br />
because fragmentation occurs for all peptides, not just for the most abundant peptides. We are currently using this method on<br />
several in vitro phosphorylation projects, but our goal is to extend these analyses to in vivo systems to identify novel kinase or<br />
phosphatase substrates.<br />
External Collaborators<br />
Gary Gibson, Henry Ford Hospital, Detroit, Michigan<br />
Michael Hollingsworth, Eppley Cancer Center, University of Nebraska, Omaha<br />
Waters Corporation<br />
Core Technology Alliance (CTA)<br />
This laboratory participates in the CTA as a member of the Michigan Proteomics Consortium.<br />
From left: Cavey, Lehner, Davidson<br />
14
VARI | <strong>2008</strong><br />
Nicholas S. Duesbery, Ph.D.<br />
Laboratory of Cancer and Developmental Cell Biology<br />
Nick Duesbery received a B.Sc. (Hon.) in biology (1987) from Queen’s University, Canada, and both his<br />
M.Sc. (1990) and Ph.D. (1996) degrees in zoology from the University of Toronto, Canada, under the<br />
supervision of Yoshio Masui. Before his appointment as a <strong>Scientific</strong> Investigator at VARI in April 1999,<br />
he was a postdoctoral fellow in the laboratory of George Vande Woude in the Molecular Oncology<br />
Section of the Advanced BioScience Laboratories–Basic Research Program at the National Cancer<br />
Institute, Frederick Cancer Research and Development Center, Maryland. Dr. Duesbery was promoted<br />
to Senior <strong>Scientific</strong> Investigator and appointed Deputy Director for Research Operations in 2006.<br />
Staff<br />
Jennifer Bromberg-White, Ph.D.<br />
Philippe Depeille, Ph.D.<br />
Yan Ding, Ph.D.<br />
John Young, M.S.<br />
Jaclyn Lynem, B.S.<br />
Elissa Boguslawski<br />
Laura Holman<br />
Students<br />
Chih-Shia Lee, M.S.<br />
Naomi Asantewa-Sechereh<br />
Michelle Dawes<br />
Lisa Orcasitas<br />
Jennifer Wilcox<br />
15
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Research Interests<br />
Many malignant sarcomas such as fibrosarcomas are refractory to available treatments. However, sarcomas possess unique<br />
vascular properties which indicate they may be more responsive to therapeutic agents that target endothelial function.<br />
Mitogen-activated protein kinase kinases (MKKs) have been shown to play an essential role in the growth of carcinomas, and<br />
we hypothesize that signaling through multiple MKK pathways is also essential for sarcomas. One objective of our research<br />
is to define the role of MKK signaling in the growth and vascularization of human sarcomas and to determine whether agents<br />
such as anthrax lethal toxin (LeTx), a proteolytic inhibitor of MKKs, can form the basis of a novel and innovative approach to<br />
the treatment of human sarcoma.<br />
In the past year, we have made fascinating discoveries that bring us closer to achieving that objective. Yan Ding and Philippe<br />
Depeille, postdoctoral fellows in the lab, with the assistance of Elissa Boguslawski, our xenograft technician, had earlier shown<br />
that MKKs are active in soft-tissue sarcomas (including Kaposi sarcoma, fibrosarcoma, malignant fibrous histiocytoma, and<br />
leiomyosarcoma) and that LeTx can inhibit the in vitro tumorigenic potential of these cells. We believed that the anti-tumoral<br />
properties of LeTx primarily stemmed from its ability to substantially decrease the release of many growth factors—notably<br />
the pro-angiogenic vascular endothelial growth factor (VEGF)—from tumor cells, leading to a reduction in tumor growth and<br />
vascularization. However, our work this year has changed the way we envision this.<br />
As an alternative approach to test the requirement for MKK signaling in fibrosarcoma vascularization in vivo, we established a<br />
collaboration with Rick Hay (Laboratory of Noninvasive Imaging and Radiation Biology) to monitor tumor perfusion in xenografts<br />
using ultrasound imaging in conjunction with injecting contrast ultrasound microbubbles. We found that inhibition of MKK<br />
signaling by LeTx caused a rapid and dramatic decrease in tumor perfusion (Figure 1). Follow-up histologic analysis in collaboration<br />
with James Resau (Laboratory of Analytical, Cellular, and Molecular Microscopy) showed this decrease in tumor perfusion<br />
was caused by increased extravasation, i.e., tumor blood vessels became leaky (Figure 2). This was unexpected, since<br />
published studies have shown that withdrawal of VEGF leads to a regression of neovascularization over the course of weeks,<br />
not hours. Our failure to observe similar changes in normal endothelium indicates that the survival requirements for normal and<br />
tumor endothelium are distinct. Taken together, our results indicate that while MKK activity is required for tumor cell proliferation,<br />
it also plays an important role in tumor vascular function. Further studies are required to delineate the events leading to<br />
loss of vascular function, as well as the relative contributions of tumor, stromal, and endothelial cells in this response.<br />
Figure 1<br />
Figure 1. Ultrasound analysis of the<br />
effects of acute MKK inhibition on<br />
tumor blood flow. HT-1080 fibrosarcoma<br />
xenograft tumors (approximately 100 mm 3<br />
in diameter) were treated with 1 standard<br />
dose of either LeTx or inactive LeTx by i.v.<br />
injection. Tumor perfusion was evaluated<br />
by ultrasound imaging enhanced with<br />
contrast microbubbles either immediately<br />
prior to treatment or 24 h after treatment.<br />
The contrast signals, displayed in the<br />
images as green spots, are proportional<br />
to the number of microbubbles within the<br />
region of interest, which in turn reflects the<br />
included volume of flowing blood.<br />
16
VARI | <strong>2008</strong><br />
Currently, Jenn Bromberg-White, a postdoctoral fellow, is following up these studies with an investigation into the roles these<br />
same pathways play in other neovascular diseases such as acute macular degeneration. Chih-Shia Lee, a graduate student,<br />
is performing a detailed study of the individual contributions of MKK pathways to melanoma survival, and Jaclyn Lynem, our<br />
laboratory technician, is investigating the molecular basis of LF inactivation of MKK. Finally, in our longstanding collaboration<br />
with Arthur Frankel, Director of the Scott & White Cancer Research Institute in Texas, we are moving forward with preclinical<br />
testing of the therapeutic potential of LeTx in the treatment of malignant melanoma.<br />
Figure 2<br />
Figure 2. The effect of acute MKK inhibition on xenograft morphology. Mice bearing HT-1080 xenograft tumors<br />
were injected i.v. with inactive LeTx (A) or LeTx (B, C). Twenty-four hours later, tumor (A, B) and kidney (C) tissues were<br />
formalin-fixed, paraffin-embedded, sectioned, and stained using hemotoxylin and eosin. Images were obtained at 20X;<br />
bars represent 50 μm.<br />
From left: Ding, Duesbery, Holman, Boguslawski, Lynem, Lee, Bromberg-White<br />
17
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Recent Publications<br />
Bromberg-White, J.L., and N.S. Duesbery. In press. Biological and biochemical characterization of anthrax lethal factor, a<br />
proteolytic inhibitor of MEK signaling pathways. Methods in Enzymology.<br />
Kuo, S.R., M.C. Willingham, S.H. Bour, E.A. Andreas, S.K. Park, C. Jackson, N.S. Duesbery, S.H. Leppla, W.J. Tang, and<br />
A.E. Frankel. In press. Anthrax toxin-induced shock in rats is associated with pulmonary edema and hemorrhage. Microbial<br />
Pathogenesis.<br />
Alfano, Randall W., Stephen H. Leppla, Shihui Liu, Thomas H. Bugge, Nicholas S. Duesbery, and Arthur E. Frankel. <strong>2008</strong>.<br />
Potent inhibition of tumor angiogenesis by the matrix metalloproteinase–activated anthrax lethal toxin: implication for broad<br />
anti-tumor efficacy. Cell Cycle 7(6): 745–749.<br />
Ding, Yan, Elissa A. Boguslawski, Bree D. Berghuis, John J. Young, Zhongfa Zhang, Kim Hardy, Kyle Furge, Eric Kort,<br />
Arthur E. Frankel, Rick V. Hay, James H. Resau, and Nicholas S. Duesbery. <strong>2008</strong>. Mitogen-activated protein kinase kinase<br />
signaling promotes growth and vascularization of fibrosarcoma. Molecular Cancer Therapeutics 7(3): 648–658.<br />
Huang, Dan, Yan Ding, Wang-Mei Luo, Stephanie Bender, Chao-Nan Qian, Eric Kort, Zhong-Fa Zhang, Kristin VandenBeldt,<br />
Nicholas S. Duesbery, James H. Resau, and Bin Tean Teh. <strong>2008</strong>. Inhibition of MAPK kinase signaling pathways suppressed<br />
renal cell carcinoma growth and angiogenesis in vivo. Cancer Research 68(1): 81–88.<br />
Rouleau, Cecile, Krishna Menon, Paula Boutin, Cheryl Guyre, Hitoshi Yoshida, Shiro Kataoka, Michael Perricone, Srinivas<br />
Shankara, Arthur E. Frankel, Nicholas S. Duesbery, George F. Vande Woude, Hans-Peter Biemann, and Beverly A. Teicher.<br />
<strong>2008</strong>. The systemic administration of lethal toxin achieves a growth delay of human melanoma and neuroblastoma xenografts:<br />
assessment of receptor contribution. International Journal of Oncology 32(4): 739–748.<br />
Depeille, Philippe, John J. Young, Elissa A. Boguslawski, Bree D. Berghuis, Eric J. Kort, James H. Resau, Arthur E. Frankel,<br />
and Nicholas S. Duesbery. 2007. Anthrax lethal toxin inhibits growth of and vascular endothelial growth factor release from<br />
endothelial cells expressing the human herpes virus 8 viral G protein–coupled receptor. Clinical Cancer Research 13(19):<br />
5926–5934.<br />
Young, John J., Jennifer L. Bromberg-White, Cassandra R. Zylstra, Joseph T. Church, Elissa Boguslawski, James H. Resau,<br />
Bart O. Williams, and Nicholas S. Duesbery. 2007. LRP5 and LRP6 are not required for protective antigen–mediated internalization<br />
or lethality of anthrax lethal toxin. PLoS Pathogens 3(3): e27.<br />
18
VARI | <strong>2008</strong><br />
MET expression in breast cancer cells<br />
This image was from a breast cancer project funded by DOD IDEA grant with J. Resau as PI. MET is a protein found overexpressed in many<br />
cancers. The image shows MET and Her2neu overlaid onto a Nomarski–DIC (differential interference contrast) background of the tissue<br />
structure (gray). The holes are where adipose tissue was removed or cleared in histology processing. Her2neu was localized with a DAKO<br />
polyclonal antibody (green) and MET was localized with a monoclonal antibody (red). Yellow results from the combination of both green and red<br />
costaining or colocalization. This was selected as an Image of Distinction in the Nikon Small World 2007 Competition. Photo by James Resau.<br />
19
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Bryn Eagleson, B.S., RLATG<br />
Vivarium and Transgenics Program<br />
Bryn Eagleson began her career in laboratory animal services in 1981 with Litton Bionetics at the<br />
National Cancer Institute’s Frederick Cancer Research and Development Center (NCI–FCRDC) in<br />
Maryland. In 1983, she joined the Johnson & Johnson Biotechnology Center in San Diego, California. In<br />
1988, she returned to NCI–FCRDC, where she continued to develop her skills in transgenic technology<br />
and managed the transgenic mouse colony. In 1999, she joined VARI as the Vivarium Director and<br />
Transgenics Special Program Manager.<br />
Technical Staff<br />
Lisa DeCamp, B.S.<br />
Dawna Dylewski, B.S.<br />
Audra Guikema, B.S., L.V.T.<br />
Tristan Kempston, B.S.<br />
Angie Rogers, B.S.<br />
Elissa Boguslawski, RALAT<br />
20<br />
Animal Caretaker Staff<br />
Sylvia Marinelli, Team leader<br />
Crystal Brady<br />
Jarred Grams<br />
Samuel Johnson<br />
Rishard Moody<br />
Janelle Post<br />
Tina Schumaker<br />
Bobbie Vitt
VARI | <strong>2008</strong><br />
Research Interests<br />
The goal of the vivarium and the transgenics program is to develop, provide, and support high-quality mouse modeling services<br />
for the Van Andel Research Institute investigators, Michigan Technology Tri-Corridor collaborators, and the greater research<br />
community. We use two Topaz Technologies software products, Granite and Scion, for integrated management of the vivarium<br />
finances, the mouse breeding colony, and the Institutional Animal Care and Use Committee (IACUC) protocols and records.<br />
Imaging equipment, such as the PIXImus mouse densitometer and the ACUSON Sequoia 512 ultrasound machine, is available<br />
for noninvasive imaging of mice. Also provided by the vivarium technical staff are an extensive xenograft model development<br />
and analysis service, rederivation, surgery, dissection, necropsy, breeding, and health-status monitoring.<br />
Transgenics<br />
Fertilized eggs contain two pronuclei, one that is derived from the egg and contains the maternal genetic material and one<br />
derived from the sperm that contains the paternal genetic material. As development proceeds, these two pronuclei fuse,<br />
the genetic material mixes, and the cell proceeds to divide and develop into an embryo. Transgenic mice are produced by<br />
injecting small quantities of foreign DNA (the transgene) into a pronucleus of a one-cell fertilized egg. DNA microinjected into a<br />
pronucleus randomly integrates into the mouse genome and will theoretically be present in every cell of the resulting organism.<br />
Expression of the transgene is controlled by elements called promoters that are genetically engineered into the transgenic<br />
DNA. Depending on the selection of the promoter, the transgene can be expressed in every cell of the mouse or in specific cell<br />
populations such as neurons, skin cells, or blood cells. Temporal expression of the transgene during development can also<br />
be controlled by genetic engineering. These transgenic mice are excellent models for studying the expression and function of<br />
the transgene in vivo.<br />
From left to right, standing: Dylewski, Guikema, Grams, Schumaker, Rogers, Eagleson, Brady, Marinelli, Vitt, Post, Jason, Boguslawski, DeCamp<br />
From left to right, kneeling: Kempston, Moody, Johnson<br />
21
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Kyle A. Furge, Ph.D.<br />
Laboratory of Computational Biology<br />
Dr. Furge received his Ph.D. in biochemistry from the Vanderbilt University School of Medicine in 2000.<br />
Prior to obtaining his degree, he worked as a software engineer at YSI, Inc., where he wrote operating<br />
systems for embedded computer devices. Dr. Furge did his postdoctoral work in the laboratory of<br />
George Vande Woude. He became a Bioinformatics Scientist at VARI in June of 2001 and a <strong>Scientific</strong><br />
Investigator in May of 2005.<br />
Staff<br />
Karl Dykema, B.A.<br />
Students<br />
Jeff Klomp, B.S.<br />
Theresa Gipson<br />
Craig Johnson<br />
22
VARI | <strong>2008</strong><br />
Research Interests<br />
As high-throughput technologies such as DNA sequencing, gene and protein expression profiling, DNA copy number analysis,<br />
and single nucleotide polymorphism genotyping become more available to researchers, extracting the most significant biological<br />
information from the large amount of data produced by these technologies becomes increasingly difficult. Computational<br />
disciplines such as bioinformatics and computational biology have emerged to develop methods that assist in the storage,<br />
distribution, integration, and analysis of these large data sets. The Computational Biology laboratory at VARI currently focuses<br />
on using mathematical and computer science approaches to analyze and integrate complex data sets in order to develop a<br />
better understanding of how cancer cells differ from normal cells at the molecular level. In addition, members of the lab provide<br />
assistance in data analysis and other computational projects on a collaborative and/or fee-for-service basis.<br />
In the past year the laboratory has contributed to several gene expression microarray analysis projects ranging from mechanisms<br />
of oncogene transformation to the identification of genes associated with drug sensitivity. For example, in recent work<br />
led by the Laboratory of Molecular Oncology, we combined cytogenetic, phenotypic, and gene expression profiling data to help<br />
elucidate the role of chromosomal abnormalities during tumor cell progression. We also worked closely with the Laboratory of<br />
Cancer Genetics in the development of gene expression–based models for the diagnosis and prognosis of renal cell carcinoma.<br />
Moreover, we and other groups have demonstrated that several types of biological information, in addition to relative transcript<br />
abundance, can be derived from high-density gene expression profiling data. Taking advantage of this additional information<br />
can lead to the rapid development of plausible computational models of disease development and progression.<br />
Changes in DNA copy number result in dramatic changes in gene expression within the abnormal region and are detectable<br />
by examining the population of mRNAs generated from the genes that map to each chromosome. Additionally, activation of<br />
certain oncogenes or inactivation of certain tumor suppressor genes can produce context-independent gene signatures that<br />
can be detected in a gene expression profile. For example, genes that are up-regulated by overexpression of RAS in breast<br />
epithelial cells also tend to be overexpressed in other samples having activated RAS signaling, such as lung tumors that<br />
contain activating RAS mutations. We have invested a reasonable portion of the past several years developing and evaluating<br />
computational methods to predict deregulated signal transduction pathways and chromosomal abnormalities using gene<br />
expression data. We have worked closely with the Laboratory of Cancer Genetics on computational models to describe the<br />
development and progression of renal cell carcinoma. An example of the successful application of this analytic approach is in<br />
the examination of gene expression profiling data derived from papillary renal cell carcinoma (RCC).<br />
23
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Computational analysis of gene expression data derived from papillary RCC revealed that a transcriptional signature indicative<br />
of MYC pathway activation was present in high-grade papillary RCC, but not other high-grade RCCs. Predictions of chromosomal<br />
gains and losses were also generated from the gene expression data, and it was demonstrated that the presence<br />
of the MYC signature was coincident with a predicted amplification of chromosome 8q. Because the c-MYC gene maps to<br />
chromosome 8q, a computational model was developed such that amplification of chromosome 8q occurs in the high-grade<br />
papillary tumors, which leads to c-MYC overexpression and activation of the MYC pathway. The importance of MYC activation<br />
was confirmed by both pharmacological and siRNA inhibition of active MYC signaling in a cell line model of high-grade papillary<br />
RCC. These results highlight the effectiveness of using gene expression profiling data to build integrative computational models<br />
of tumor development and progression.<br />
From left: Furge, Johnson, Klomp, Dykema<br />
Recent Publications<br />
Camparo, P., V. Vasiliu, V. Molinié, J. Couturier, K. Dykema, D. Petillo, K.A. Furge, E.M. Comperat, M. Laé, R. Bouvier,<br />
L. Boccon-Gibbod, Y. Denoux, S. Ferlicot, E. Forest, G. Fromont, et al. In press. Renal translocation carcinomas: clinicopathological,<br />
immunohistochemical, and gene expression profiling analysis of 31 cases with a review of the literature. American<br />
Journal of Surgical Pathology.<br />
Ding, Yan, Elissa A. Boguslawski, Bree D. Berghuis, John J. Young, Zhongfa Zhang, Kim Hardy, Kyle Furge, Eric Kort,<br />
Arthur E. Frankel, Rick V. Hay, James H. Resau, and Nicholas S. Duesbery. <strong>2008</strong>. Mitogen-activated protein kinase kinase<br />
signaling promotes growth and vascularization of fibrosarcoma. Molecular Cancer Therapeutics 7(3): 648–658.<br />
Gao, ChongFeng, Kyle Furge, Julie Koeman, Karl Dykema, Yanli Su, Mary Lou Cutler, Adam Werts, Pete Haak, and<br />
George F. Vande Woude. 2007. Chromosome instability, chromosome transcriptome, and clonal evolution of tumor cell<br />
populations. Proceedings of the National Academy of Sciences U.S.A. 104(21): 8995–9000.<br />
24
VARI | <strong>2008</strong><br />
Brian B. Haab, Ph.D.<br />
Laboratory of Cancer Immunodiagnostics<br />
Dr. Haab obtained his Ph.D. in chemistry from the University of California at Berkeley in 1998. He then<br />
served as a postdoctoral fellow in the laboratory of Patrick Brown in the Department of Biochemistry<br />
at Stanford University. Dr. Haab joined VARI as a Special Program Investigator in May 2000, became a<br />
<strong>Scientific</strong> Investigator in 2004, and was promoted to Senior <strong>Scientific</strong> Investigator in 2007.<br />
Staff Students Visiting Scientists<br />
Songming Chen, Ph.D.<br />
Yi-Mi Wu, Ph.D.<br />
Derek Bergsma, B.S.<br />
Sara Forrester, B.S.<br />
Andrew Porter, B.S.<br />
Tingting Yue, B.S.<br />
Alex Turner<br />
Krysta Collins<br />
Carrie Fiebig<br />
Adam Granger<br />
Lee Heeringa<br />
Kevin Maupin<br />
Randi VanOcker<br />
David Nowack, Ph.D.<br />
25
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Research Interests<br />
C-reactive protein<br />
C-reactive protein (CRP) is a crucial component of the body’s innate immune system. CRP is involved in the recognition and<br />
removal of pathogens and dying cells and in the signaling that controls inflammation. While CRP is crucial to the maintenance<br />
of health, recent research has demonstrated a possible involvement of CRP in the development of diseases associated with<br />
inflammation. A more complete understanding of CRP functions in normal and disease-associated inflammation could have<br />
valuable therapeutic implications.<br />
We have used a novel method developed in our laboratory, called Antibody Array Interaction Mapping (AAIM), to uncover<br />
possible additional roles for CRP in inflammation and disease. A protein’s function is determined in part by its interactions with<br />
other proteins, and identifying and measuring changes in those interactions are keys to understanding protein functions. Current<br />
methods of detecting protein-protein interactions—such as immunoprecipitation, mass spectrometry, yeast two-hybrid assay,<br />
and protein arrays—are not suitable for measuring changes over multiple samples and may require purified proteins instead<br />
of native, biological samples. AAIM complements these methods by allowing quantitative, high-throughput comparisons of<br />
protein-protein interaction levels in biological samples. We produce multiple, identical arrays containing antibodies targeting a<br />
variety of proteins that might interact with each other. A native, nondenatured biological sample such as serum is incubated on<br />
each array, and proteins in the sample are captured by the antibodies according to their specificities. After unbound proteins<br />
are washed away, each array is probed with a detection antibody that corresponds to one of the capture antibodies, and the<br />
detection antibodies localize on the array wherever their targets are found. The pattern of binding of the detection antibodies<br />
can reveal potential protein-protein interactions.<br />
Using this tool, we have discovered several novel protein-protein interactions in human serum, including previously unknown<br />
interactions between CRP and other inflammation-related proteins. The finding of a subset of CRP circulating in complex<br />
with inflammatory mediators suggests previously unrecognized functions or sites of action for CRP. An intriguing aspect of<br />
this bound form of CRP is that it appears to be conformationally different than the freely circulating form. The bound CRP<br />
is structurally altered in a way that produces potent biological effects distinct from those of normal CRP. We have shown a<br />
biological context for the bound form of CRP; now we are seeking to determine how the functions of this bound CRP differ<br />
from those of free CRP and how abnormal levels of bound CRP might be involved in inflammation-related pathologies. We also<br />
are characterizing the components of circulating multiprotein complexes involving CRP and characterizing the details of those<br />
interactions. AAIM has been a valuable tool for the discovery and ongoing study of these multiprotein complexes, especially<br />
using monoclonal antibodies with defined specificities for various regions and forms of CRP. Other proteomics methods,<br />
performed in the collaboration with the Mass Spectrometry and Proteomics lab at VARI, facilitate this work.<br />
Glycosylation in pancreatic cancer<br />
The development of biomarkers for the accurate and early diagnosis of pancreatic cancer has been challenging. Many of the<br />
candidate biomarkers are either elevated in other conditions or only in later-stage disease, leading to unacceptably low specificity<br />
and sensitivity. A common molecular feature of pancreatic cancer is alteration of the carbohydrate structures (glycans) that<br />
are attached to certain proteins. Glycan alterations can appear at a higher rate than changes in protein abundance, and certain<br />
glycan structures may be unique to particular disease states, even at early stages of cancer development. Thus, the detection<br />
of particular glycans on specific proteins may form the basis of improved pancreatic cancer biomarkers.<br />
26
VARI | <strong>2008</strong><br />
The key to developing improved markers is the ability to reproducibly measure specific glycans on specific proteins. Many of<br />
the carbohydrate structures on proteins in normal and cancer tissues have been characterized using mass spectrometry and<br />
enzymatic methods. Those methods are valuable for defining structures, but they do not have the precision or throughput<br />
necessary to look at changes in levels between samples, which is necessary to assess biomarker potential. A new method<br />
developed in our laboratory provides the means to obtain more detailed information on glycan variation. We use lectins—<br />
proteins that bind specific glycan structures—and glycan-binding antibodies to probe the levels of particular glycans on the<br />
proteins captured by antibody arrays. This method provides the important feature of allowing comparison between samples of<br />
the levels of particular glycans on specific proteins so that we can assess their diagnostic potential. A product based on this<br />
technology is now available from GenTel Biosciences (Madison, WI).<br />
The class of proteins called mucins shows particularly high levels of glycan alteration in pancreatic cancer. Mucins are longchain,<br />
heavily glycosylated proteins on epithelial cell surfaces that have roles in cell protection, interaction with the extracellular<br />
space, and regulation of extracellular signaling. Altered carbohydrates on mucins can affect critical processes in cancer such<br />
as cell migration or extracellular signaling to the immune system. We have extensively characterized the glycan variations on<br />
mucins secreted into the blood of pancreatic cancer patients. In some cases, the levels of certain mucin glycans are altered in<br />
cancer patients more often than the levels of the core proteins (Figure 1a). As a result, detection of the glycans performed better<br />
as a biomarker than detection of the core proteins (Figure 1b). The efficient analysis of many samples and glycan structures<br />
was made possible by the ability to run dozens of samples on a single microscope slide. A device based on that technology,<br />
which partitions microscope slides for efficient sample processing, is available from The Gel Company (San Francisco, CA).<br />
Our work shows the promise of this approach and points to key directions for further developing biomarkers of pancreatic<br />
cancer. Our research now focuses on the goals of identifying the protein carriers of cancer-associated glycans, of identifying<br />
the most important cancer-associated glycans and the reagents to detect them, and of applying these discoveries to pancreatic<br />
cancer diagnostics (Figure 1c).<br />
Figure 1<br />
In addition, we are seeking to better<br />
understand the origins of glycan alterations<br />
and the functional contribution of<br />
these molecules to pancreatic cancer<br />
development and progression.<br />
Figure 1. Pancreatic cancer biomarker development. a) Comparison of glycan versus protein detection. The level of the MUC5ac<br />
core protein in serum samples from cancer patients and healthy subjects, determined using monoclonal antibody (mAb) sandwich assays,<br />
is indicated along the vertical axis. The level of glycan CA 19-9 on MUC5ac, determined using a mAb to capture MUC5ac and another<br />
antibody to detect CA 19-9 on the captured protein, is indicated along the horizontal axis. b) Receiver-operator characteristic curve<br />
analysis comparing the biomarker performance of core protein versus glycan detection. Each curve gives the sensitivity (rate of true<br />
positive detection) and the specificity (rate of true negative detection) for discriminating cancer subjects from control subjects at various<br />
thresholds of discrimination. “AUC” is area-under-the-curve, indicating the total discriminating ability of each marker. c) Cluster analysis.<br />
The glycan measurements along the vertical axis were taken in the samples indicated along the horizontal axis; the color of each square<br />
is the level of each measurement (see the color bar). The rows and columns were ordered (clustered) by similarity, showing consistently<br />
increased levels in the cancer patients.<br />
27
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
External Collaborators<br />
Philip Andrews, Irwin Goldstein, Gilbert Omenn, and Diane Simeone, University of Michigan, Ann Arbor<br />
Randall Brand, University of Pittsburgh, Pennsylvania<br />
William Catalona, Northwestern University, Evanston, Illinois<br />
Terry Du Clos, University of New Mexico, Albuquerque<br />
Ziding Feng and Samir Hanash, Fred Hutchinson Cancer Research Center, Seattle, Washington<br />
Michael A. Hollingsworth, University of Nebraska, Omaha<br />
Raju Kucherlapati, Harvard Medical School, Boston, Massachusetts<br />
Anna Lokshin, University of Pittsburgh, Pennsylvania<br />
Alan Partin, Johns Hopkins University, Baltimore, Maryland<br />
Lawrence A. Potempa, Immtech Pharmaceuticals, Vernon Hills, Illinois<br />
Robert Vessella, University of Washington, Seattle<br />
From left: Yue, Wu, VanOcker, Bergsma, Nelson, Porter, Haab<br />
Recent Publications<br />
Chen, Songming, Tom LaRoche, Darren Hamelinck, Derek Bergsma, Dean Brenner, Diane Simeone, Randall E. Brand, and<br />
Brian B. Haab. 2007. Multiplexed analysis of glycan variation on native proteins captured by antibody microarrays. Nature<br />
Methods 4(5): 437–444.<br />
Forrester, Sara, Kenneth E. Hung, Rork Kuick, Raju Kucherlapati, and Brian B. Haab. 2007. Low-volume, high-throughput<br />
sandwich immunoassays for profiling plasma proteins in mice: identification of early-stage systemic inflammation in a mouse<br />
model of intestinal cancer. Molecular Oncology 1(2): 216–225.<br />
Forrester, Sara, Ji Qiu, Leslie Mangold, Alan Partin, David Misek, Brett Phinney, Douglas Whitten, Philip Andrews, Eleftherios<br />
Diamandis, Gilbert S. Omenn, Samir Hanash, and Brian B. Haab. 2007. An experimental strategy for quantitative analysis of<br />
the humoral immune response to prostate cancer antigens using natural protein microarrays. Proteomics – Clinical Applications<br />
1(5): 494–505.<br />
Li, Zheng, Shireesh Srivastava, Xuerui Yang, Sheenu Mittal, Paul Norton, James Resau, Brian Haab, and Christina Chan. 2007.<br />
A hierarchical approach employing metabolic and gene expression profiles to identify the pathways that confer cytotoxicity in<br />
HepG2 cells. BMC Systems Biology 1: 15 pp.<br />
28
VARI | <strong>2008</strong><br />
Rick Hay, Ph.D., M.D., F.A.H.A.<br />
Laboratory of Noninvasive Imaging and Radiation Biology<br />
Office of Translational Programs<br />
Dr. Hay earned a Ph.D. in pathology (1977) and an M.D. (1978) at the University of Chicago and the<br />
Pritzker School of Medicine. He became a resident in anatomic pathology and then a postdoctoral<br />
research fellow in the University of Chicago Hospitals and Clinics. Following a postdoctoral fellowship at<br />
the Biocenter/University of Basel (Switzerland), he returned to the University of Chicago as an Assistant<br />
Professor in the Department of Pathology and Associate Director of the Section of Autopsy Pathology<br />
from 1984 to 1992. He moved to the University of Michigan Medical Center in 1992 as a clinical fellow<br />
in the Division of Nuclear Medicine and became Chief Fellow in 1993. From 1994 to 1997 he was a<br />
staff physician, and from 1995 to 1997 the Medical Director in the Department of Nuclear Medicine<br />
at St. John Hospital and Medical Center in Detroit. He joined VARI in 2001 as a Senior <strong>Scientific</strong><br />
Investigator. In 2002 he was named Assistant to the Director for Clinical Programs, and in 2003 was<br />
appointed Deputy Director for Clinical Programs.<br />
Staff<br />
Laboratory Staff<br />
Visiting Scientist<br />
Students<br />
Visiting Scientists<br />
Physician-Scientist In Training<br />
Troy Giambernardi, Ph.D.<br />
Kim Hardy, M.A., RT(R), RDMS<br />
Natalie Kent, B.S.<br />
Jose Toro, B.S.<br />
Nigel Crompton, Ph.D., D.Sc.<br />
Matthew Steensma, M.D.<br />
Students<br />
Alaa Abughoush<br />
Sara Kunz<br />
Jennifer Vogal<br />
Consultants<br />
Helayne Sherman, M.D., Ph.D., F.A.C.C.<br />
Milton Gross, M.D., F.A.C.N.P.<br />
29
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Research Interests<br />
The Laboratory of Noninvasive Imaging & Radiation Biology is devoted both to noninvasive imaging (i.e., depicting anatomic<br />
structures and physiology in living organisms without surgery) and to radiation biology (evaluating the consequences of external<br />
and internal radiation exposure in living organisms).<br />
The lab’s work follows three common themes:<br />
• Developing and using laboratory models that address medical imaging and radiation exposure problems<br />
• Advancing technology in imaging and radiation biology, including novel agents, probes, and reporters; new<br />
strategies for tackling research problems; and new instrumentation<br />
• Pursuing two-way translation between the laboratory and the clinical setting, i.e., using examples of human<br />
disease to design and improve laboratory model systems for study, as well as moving new discoveries from<br />
the laboratory benchtop to clinical use<br />
We depend heavily upon sophisticated instruments and equipment, including nuclear imaging cameras; planar and tomographic<br />
(3-D) X-ray units; clinical and research ultrasonography units; fluorescence detection systems; and cell and organism irradiation<br />
capability. Because of the equipment- and expertise-intensive nature of our projects, we could not succeed without the help of<br />
our valued collaborators. Our laboratory operates state-of-the-art noninvasive instruments for imaging mice, including a Vevo<br />
770 high-resolution micro-ultrasound imaging system (VisualSonics) and a nanoSPECT/CT imaging unit (BioScan).<br />
We are pursuing two major collaborative projects in the area of radiation biology:<br />
• Nigel Crompton of Cornerstone University co-directs an effort to predict the sensitivity of a patient’s normal<br />
tissues to irradiation being administered for treatment of cancer. This project is made possible through collaboration<br />
with the radiation oncology service at Saint Mary’s Health Care and with the West Michigan Center<br />
for Family Health, both in Grand Rapids. For this project, a sample of the patient’s blood is drawn before<br />
radiation therapy. That blood sample is then irradiated under precise conditions of exposure, treated with<br />
fluorescent molecules that detect certain blood cells (lymphocytes), and analyzed by fluorescence-activated<br />
cell sorting (FACS) for evidence of lymphocyte death. We have also been investigating the effects of patient<br />
age, gender, and administered radiation dose on the lymphocyte response, and we are now working to<br />
determine the molecular basis for patient-to-patient variability. The midpoint results of our five-year clinical trial<br />
are being presented this year at the annual meeting of the American Society of Clinical Oncology.<br />
• In collaboration with Drs. Weiwen Deng, Aly Mageed, and Anthony Senagore of DeVos Children’s Hospital/<br />
Spectrum Health, we are exploring a new approach for treating graft-versus-host disease in mice undergoing<br />
bone marrow transplantation, with planned extension to human patients in the near future.<br />
30
VARI | <strong>2008</strong><br />
Our major project in nuclear medicine is to develop and bring into clinical use radioactive antibodies and smaller molecules that<br />
attach to the Met receptor tyrosine kinase, collectively designated Met-avid radiopharmaceuticals (MARPs). Met plays a key<br />
role in causing cancers to become more aggressive, so that they spread to nearby tissues (invasion) and/or travel through the<br />
bloodstream or lymph channels to distant organs (metastasis). We previously showed that both large and small MARPs are<br />
useful for nuclear imaging of Met-expressing human tumors (xenografts) grown under the skin of immunodeficient mice. We<br />
are currently translating MARP-based imaging into mice with orthotopic xenografts (see below), as well as undertaking studies<br />
in additional animal species in order to gain governmental approval for the first MARP testing in humans.<br />
Finally, to support our internal and external collaborators, we operate a multimodality noninvasive imaging program for evaluating<br />
the growth, molecular expression, and response to therapy of aggressive human tumor xenografts grown subcutaneously<br />
or orthotopically in immunodeficient mice. Employing a combination of high-resolution ultrasound with and without contrast<br />
agents, planar and tomographic nuclear imaging, and CT imaging, we are studying tumors of the brain, adrenals, soft connective<br />
tissue, and bone. From studies using this imaging program, one paper (Ding et al. <strong>2008</strong>) has been published; two<br />
manuscripts have been submitted for publication; and three more are being prepared.<br />
External Collaborators<br />
Our lab depends critically on intramural and extramural collaborations to address our research themes. Current extramural<br />
collaborators include scientists and physicians at the Department of Veterans Affairs Healthcare System and the University of<br />
Michigan Medical Center, both in Ann Arbor; Cornerstone University, West Michigan Heart, P.C., DeVos Children’s Hospital/<br />
Spectrum Health, St. Mary’s Health Care, and West Michigan Center for Family Health, all in Grand Rapids; the University of<br />
Illinois in Champaign-Urbana; and VisualSonics, Inc., in Toronto.<br />
Recent Publications<br />
Gross, M.D., and R.V. Hay. In press. Molecular imaging of adrenal disease. Molecular Endocrinology.<br />
Ding, Yan, Elissa A. Boguslawski, Bree D. Berghuis, John J. Young, Zhongfa Zhang, Kim Hardy, Kyle Furge, Eric Kort, Arthur<br />
E. Frankel, Rick V. Hay, James H. Resau, and Nicholas S. Duesbery. <strong>2008</strong>. Mitogen-activated protein kinase kinase signaling<br />
promotes growth and vascularization of fibrosarcoma. Molecular Cancer Therapeutics 7(3): 648–658.<br />
Zhao, Ping, Tessa Grabinski, Chongfeng Gao, R. Scot Skinner, Troy Giambernardi, Yanli Su, Eric Hudson, James Resau, Milton<br />
Gross, George F. Vande Woude, Rick Hay, and Brian Cao. 2007. Identification of a Met-binding peptide from a phage display<br />
library. Clinical Cancer Research 13(20): 6049–6055.<br />
31
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Office of Translational Programs<br />
The Office of Translational Programs (OTP) is the administrative home for activities overseen by the Deputy Director for Clinical<br />
Programs. The role of OTP is to promote and facilitate collaborative programs involving the Van Andel Research Institute and<br />
other institutions in the realm of translational medicine. These programs include development of translational infrastructure,<br />
research project coordination, medical-scientific education oversight, and community outreach.<br />
OTP accomplishments during our past year include the following:<br />
• Serving as the administrative home for a new cGMP facility. With funding from the state of Michigan and the<br />
federal Health Resources and Services Administration, VARI and Grand Valley State University have partnered<br />
to build and operate Grand River Aseptic Pharmaceutical Packaging (GR-APP), a current Good Manufacturing<br />
Practices (cGMP) facility that will package pharmaceuticals for early-phase clinical trials commissioned by<br />
academic and commercial investigators, primarily in Michigan and the Midwest. Construction of GR-APP at<br />
140 Front Street is complete, and operations will begin in mid <strong>2008</strong>.<br />
• Overseeing VARI’s participation in activities of the Michigan Cancer Consortium (MCC). As an active member of<br />
the MCC, VARI is committed to participating in statewide and regional community-based programs to reduce<br />
the burden of cancer in Michigan.<br />
• Coordinating research rotations for physicians-in-training. In collaboration with the Grand Rapids Medical<br />
Education and Research Center (MERC), OTP schedules each first-year general surgery resident to spend one<br />
month working in a research laboratory at VARI. This program has been well received by both residents and<br />
VARI investigators. Custom-tailored rotations of variable duration at VARI can also be arranged for physiciansin-training.<br />
For example, Matt Steensma, M.D., is pursuing a one-year laboratory research fellowship with<br />
funding through the Orthopaedic Research and Education Foundation under joint mentorship by Dr. Hay and<br />
by Dr. David Rispler at MERC.<br />
Staff<br />
Rick Hay, Ph.D., M.D., F.A.H.A.<br />
Troy Carrigan<br />
Jean Chastain<br />
32
VARI | <strong>2008</strong><br />
mTOR staining of transitional cell carcinoma<br />
A pseudofluorescent image captured with the CRi Nuance imaging system of phospho-mTOR immunohistochemical staining of a human<br />
transitional cell carcinoma. The sample shows high expression of phospho-mTOR in the tumor cells (red) among normal interstitial tissue.<br />
The cellular nuclei are stained blue. The tissue was prepared by Chao-Nan Qian of the Teh laboratory and imaged by Kristin VandenBeldt of<br />
the Resau laboratory.<br />
33
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Jeffrey P. MacKeigan, Ph.D.<br />
Laboratory of Systems Biology<br />
Dr. MacKeigan received his Ph.D. in microbiology and immunology at the University of North Carolina<br />
Lineberger Comprehensive Cancer Center in 2002. He then served as a postdoctoral fellow in the<br />
laboratory of John Blenis in the Department of Cell Biology at Harvard Medical School. In 2004, he<br />
joined Novartis Institutes for Biomedical Research in Cambridge, Massachusetts, as an investigator<br />
and project leader in the Molecular and Developmental Pathways expertise platform. Dr. MacKeigan<br />
joined VARI in June 2006 as a <strong>Scientific</strong> Investigator.<br />
Staff<br />
Brendan Looyenga, Ph.D.<br />
Christina Ludema, B.S.<br />
34<br />
Students<br />
Katie Sian, B.S.<br />
Natalie Wolters, B.S.<br />
Joe Church<br />
Halley Crissman<br />
Alyse DeHaan<br />
Sara Herman<br />
Geoff Kraker<br />
Matthew McElliott
VARI | <strong>2008</strong><br />
Research Interests<br />
The primary focus of the Systems Biology laboratory is identifying and understanding the genes and signaling pathways that,<br />
when mutated, contribute to the pathophysiology of cancer. We take advantage of RNA interference (RNAi) and novel proteomic<br />
approaches to identify the enzymes that control cell growth, proliferation, and survival. For example, after screening the human<br />
genome for more than 600 kinases and 200 phosphatases—called the “kinome” and “phosphatome”, respectively—that act<br />
with chemotherapeutic agents in controlling apoptosis, we identified several essential kinases and phosphatases whose roles<br />
in cell survival were previously unrecognized. We are asking several questions. How are these survival enzymes regulated at<br />
the molecular level? What signaling pathway(s) do they regulate? Does changing the number of enzyme molecules present<br />
inhibit waves of compensatory changes at the cellular level (system-level changes)? What are the system-level changes after<br />
reduction or loss of each gene?<br />
Novel modulators of chemotherapeutic sensitization<br />
Kinases and phosphatases play an integral role in balancing the survival and apoptotic signals within a cell. In an attempt to<br />
define proteins with a major role in these processes, we tested an RNAi library against all known kinases and phosphatases<br />
in the human genome and assayed various phenotypes, including sensitization to apoptosis and chemoresistance. A group<br />
of apoptosis sensitizers was identified whose siRNA knock-out conferred a marked increase in cell survival as well as a<br />
striking chemoresistant phenotype (Figure 1). One of these proteins, MK-STYX, resembles the dual-specificity phosphatases<br />
implicated in MAP kinase signaling, but it is catalytically inactive due to a cysteine-to-serine mutation at its active site. When<br />
MK-STYX is knocked down via RNAi, the cells display a profound decrease in apoptosis; MK-STYX-overexpressing cells,<br />
on the other hand, are sensitized to apoptotic signals. We propose that MK-STYX could function as a dead phosphatase,<br />
sequestering potential phosphoproteins that promote survival. Through further experiments, we plan to characterize MK-STYX<br />
and elucidate its mechanism of apoptotic sensitization; these studies may identify a survival signal that would constitute a novel<br />
target for chemotherapy.<br />
Figure 1<br />
Figure 1. Human kinase and phosphatase<br />
siRNA library screen. HeLa<br />
cells were transfected with siRNAs<br />
directed against all known and putative<br />
human phosphatases and kinases.<br />
Cells were incubated for 72 h to allow<br />
target knockdown, and apoptosis was<br />
measured by a DNA-fragmentation<br />
ELISA. The graph shows relative<br />
apoptosis for 600 kinase and 200<br />
phosphatase siRNA targets.<br />
35
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Monitoring cellular signaling<br />
Phosphatidylinositol-3-kinase (PI3K) phosphorylates the 3´ ring position of phosphatidylinositol to generate lipid products<br />
important for signal transduction, membrane trafficking, and other cellular processes. The identification of PI3Ks as key players<br />
in cellular functions ranging from vesicular trafficking to cell survival merits further study to identify factors acting immediately upand<br />
downstream of these lipid kinases, as well as characterizing the phosphatase regulating these molecular pathways. Roles<br />
for PI3K isoforms in amino acid sensing and in signaling through the mTOR pathway, as well as in autophagy, have also recently<br />
emerged. Note that these functions of PI3Ks might not merely rely on their lipid kinase activity, since they are large enzymes<br />
that could also serve as platforms for the assembly of protein complexes. Understanding is needed of the mechanisms of PI3K<br />
signaling involved in these various cellular functions.<br />
Parkinson disease–associated genes in cancer<br />
Renal cell carcinoma (RCC) is an aggressive cancer that is highly metastatic and refractory to all forms of systemic cancer<br />
therapy. Using bioinformatic analysis and over 150 RCC tumor samples, we have identified Parkinson disease–associated (PD)<br />
kinases as a novel molecular constituent of the renal tubule epithelium whose expression is specifically down-regulated during<br />
the progression of papillary RCC (Figure 2). These PD kinases are highly expressed in the brain and kidney and have been<br />
previously linked to familial Parkinson disease. Activating mutations in these genes sensitize cells to oxidative stress and lead<br />
to increased death of neural cells, implying that these genes may function as a sensor of oxidative stress in the renal epithelium<br />
and induce cell death pathways in response to toxic levels of reactive oxygen species. Selective loss of each gene in more<br />
aggressive and metastatic RCC tumors suggests that this protein may also be a tumor suppressor. The goal of this project is to<br />
define the relationship between oxidative stress management and malignant tumor progression in the kidney, with a particular<br />
emphasis on the role of kinase signaling. This project is a collaboration with VARI’s Kyle Furge and Bin Teh.<br />
Figure 2<br />
Figure 2. PD genes are located<br />
within a conserved RCC amplicon<br />
on chromosome 12. Expression<br />
profiles from more than 150 normal and<br />
RCC tissue samples were obtained by<br />
microarray analysis with the Affymetrix<br />
HGU-133 Plus 2.0 chip.<br />
36
VARI | <strong>2008</strong><br />
Colorectal cancer<br />
Chemoresistance is a therapeutic problem that severely limits successful treatment of most human cancers. This is particularly<br />
true of colorectal cancer, in which the development of resistance is common: most anti-cancer regimens are ineffective, with<br />
the five-year survival rates for late-stage colorectal cancer being only 8%. How colorectal cancer resistance develops is largely<br />
unknown, and the response to therapy varies based on individual patient tumors. With this in mind, how can we prevent cancer<br />
emergence or progression at the level of individual tumors? Recent studies have shown that a large percentage of colorectal<br />
tumors have mutations in a key gene, for class I PI3K. While mutations play an important causative role in colorectal cancer, it<br />
is currently unclear how these mutations can be exploited as drug targets and whether we can develop targeted cancer agents<br />
based on the gene. We have ongoing projects to determine the molecular pathways (and genes) that can be used to prevent<br />
progression of precancerous lesions to colorectal cancer. Further, we are defining each pathway activation in each patient’s<br />
tumor and comparing the pathways with a novel chemopreventive agent against PI3K/mTOR.<br />
Graded MAPK signaling and switch-like c-Fos induction<br />
We also take a systems biology approach to understanding two key molecular pathways, Ras/MAPK and PI3K/mTOR. One<br />
project in the lab involves the question of whether the evolutionarily conserved pathways exhibit a switch-like or a graded<br />
response in mammalian cells. Ultrasensitive switch-like responses control cell-fate decisions in many biological settings, and<br />
the regulation of kinase activity is one way in which such behavior can be initiated. Signaling molecules switch between two<br />
discontinuous, stable states with no intermediate; this is referred to as a bistable response. Given the irreversible, all-or-none<br />
nature of many cell behaviors, including cell cycle control and apoptosis, significant effort has been focused on identifying the<br />
cellular mechanisms underlying bistability.<br />
Recent Publications<br />
From left: Wolters, Nelson, MacKeigan, Looyenga, DeHaan, Church, Crissman,<br />
Sian, McElliott<br />
Elis, W., E. Triantafellow, N.M. Wolters, K.R. Sian, G. Caponigro, J. Borawski, L.A. Gaither, L.O. Murphy, P. Finan, and J.P.<br />
MacKeigan. <strong>2008</strong>. Downregulation of class II PI3Ka expression below a critical threshold induces apoptotic cell death.<br />
Molecular Cancer Research 6(4): 614–623.<br />
Wolters, N.M., and J.P. MacKeigan. <strong>2008</strong>. From sequence to function: using RNAi to elucidate mechanisms of human<br />
disease. Cell Death and Differentiation 15(5): 809–819.<br />
37
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Cindy K. Miranti, Ph.D.<br />
Laboratory of Integrin Signaling and Tumorigenesis<br />
Dr. Miranti received her M.S. in microbiology from Colorado State University in 1982 and her Ph.D. in<br />
biochemistry from Harvard Medical School in 1995. She was a postdoctoral fellow in the laboratory<br />
of Joan Brugge at ARIAD Pharmaceuticals, Cambridge, Massachusetts, from 1995 to 1997 and in<br />
the Department of Cell Biology at Harvard Medical School from 1997 to 2000. Dr. Miranti joined<br />
VARI as a <strong>Scientific</strong> Investigator in January 2000. She is also an Adjunct Assistant Professor in the<br />
Department of Physiology at Michigan State University and an Assistant Professor in the Van Andel<br />
Education Institute.<br />
Staff<br />
Kristin Saari, M.S.<br />
Lia Tesfay, M.S.<br />
Veronique Schulz, B.S.<br />
38<br />
Students<br />
Jelani Zarif, M.S.<br />
Laura Lamb, B.S.<br />
Susan Spotts, B.S.<br />
Erica Bechtel<br />
Eric Graf<br />
Fraser Holleywood<br />
Gary Rajah
VARI | <strong>2008</strong><br />
Research Interests<br />
Our laboratory is interested in understanding the mechanisms by which integrin receptors, interacting with the extracellular<br />
matrix, regulate cell processes involved in the development and progression of cancer. Using tissue culture models, biochemistry,<br />
molecular genetics, and mouse models, we are defining the cellular and molecular events involved in integrin-dependent<br />
adhesion and downstream signaling that are important for prostate tumorigenesis and metastasis.<br />
Integrins are transmembrane proteins that serve as receptors for extracellular matrix (ECM) proteins. By interacting with the<br />
ECM, integrins stimulate intracellular signaling transduction pathways that regulate cell shape, proliferation, migration, survival,<br />
gene expression, and differentiation. Integrins do not act autonomously, but “crosstalk” with receptor tyrosine kinases (RTKs)<br />
to regulate many of these cellular processes. Studies in our lab indicate that integrin-mediated adhesion to ECM proteins<br />
activates epidermal growth factor receptors EGFR/ErbB2 and the HGF/SF receptor c-Met. Integrin-mediated activation of<br />
these RTKs is ligand-independent and required for the activation of a subset of intracellular signaling molecules in response to<br />
cell adhesion.<br />
The prostate gland and cancer<br />
Tumors that develop in cells of epithelial origin, i.e., carcinomas, represent the largest tumor burden in the United States.<br />
Prostate cancer is the most frequently diagnosed cancer in American men and the second leading cause of cancer death in<br />
men. Patients who present at the time of diagnosis with androgen-dependent and organ-confined prostate cancer are relatively<br />
easy to cure through radical prostatectomy or localized radiotherapy. However, patients with aggressive and metastatic<br />
disease have fewer options. Androgen ablation can significantly reduce the tumor burden in these patients, but the potential for<br />
relapse and the development of androgen-independent cancer is high. Currently there are no effective treatments for patients<br />
who reach this stage of disease.<br />
In the human prostate gland, a3b1 and a6b4 integrins on epithelial cells bind to the ECM protein laminin 5 in the basement<br />
membrane. In tumor cells, however, the a3 and b4 integrin subunits disappear—as does laminin 5—and the tumor cells<br />
express primarily a6b1 and adhere to a basement membrane containing laminin 10. There is also an increase in expression of<br />
the RTKs EGFR and c-Met in the tumor cells. Two fundamental questions in our lab are whether the changes in integrin and<br />
matrix interactions that occur in tumor cells are required for or help to drive the survival of tumor cells, and whether crosstalk<br />
with RTKs is important for cell survival.<br />
Integrins and RTKs in prostate epithelial cell survival<br />
How integrin engagement of different ECMs regulates survival pathways in normal and tumor cells is poorly understood. We<br />
have previously demonstrated that integrin-induced activation of EGFR in normal primary prostate epithelial cells is required for<br />
survival of these cells on their endogenous matrix, laminin 5. The ability of EGFR to support integrin-mediated cell survival on<br />
laminin 5 is mediated through a3b1 integrin and requires signaling downstream to Erk. Surprisingly, we found that the death<br />
induced by inhibition of EGFR in normal primary prostate cells is not mediated through or dependent on classical caspasemediated<br />
apoptosis. The presence of an autophagic survival pathway, regulated by adhesion to matrix, prevents the induction<br />
of caspases when EGFR is inhibited. Suppression of autophagy is sufficient to induce caspase activation and apoptosis in<br />
laminin 5–adherent primary prostate epithelial cells. Thus, adhesion of normal cells to matrix regulates survival through at least<br />
two mechanisms, crosstalk with EGFR and Erk and maintenance of an autophagic survival pathway.<br />
We have begun studies to determine how integrins regulate cell survival through autophagy. When we block expression of<br />
the RTK c-Met in primary prostate epithelial cells adherent to laminin 5, they also die. In this case death is due to classical<br />
caspase-mediated apoptosis. Since autophagy must be inhibited in these cells to induce apoptosis, these results suggest<br />
that c-Met may regulate autophagy. Future studies in our lab are aimed at deciphering this pathway and determining how this<br />
pathway is altered during tumor progression.<br />
39
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Role of androgen receptor in integrin-mediated survival<br />
All primary and metastatic prostate cancers express the intracellular steroid receptor for androgen (AR). In the normal gland,<br />
the AR-expressing cells do not interact with the ECM in the basement membrane; however, all AR-expressing tumor cells do<br />
adhere to the ECM in the basement membrane. In normal cells, AR expression suppresses growth and promotes differentiation,<br />
but in tumor cells AR expression promotes cell growth and is required for cell survival. The mechanisms that lead to<br />
the change from growth inhibition and differentiation to growth promotion and survival are unknown. Our hypothesis is that<br />
adhesion to the ECM by the tumor cells is responsible for driving the change in AR function by initiating crosstalk between AR<br />
and integrins.<br />
When prostate tumor cells are placed in culture, they lose expression of AR. The reason for this is not clear, but it may have<br />
to do with loss of the appropriate ECM-containing basement membrane. When we introduce AR into prostate tumor cells, it<br />
actually suppresses their growth and induces cell death. However, if we place the AR-expressing tumor cells on laminin (the<br />
ECM found in tumors), these cells no longer die. We have determined that AR expression results in increased expression of<br />
a6b1 integrin, the receptor for laminin. Thus, AR-expressing tumor cells are likely to survive better when they remain adherent<br />
to the laminin-rich ECM that is present in the prostate gland. Survival under these conditions appears to depend on the<br />
ability of AR to enhance expression of the laminin receptor, a6b1 integrin; we are currently determining how AR regulates the<br />
expression of this integrin.<br />
Role of CD82 and integrin signaling in prostate cancer metastasis<br />
Death from prostate cancer is due to the development of metastatic disease, which is difficult to control. The mechanisms<br />
involved in progression to metastatic disease are not understood. One approach we are taking is to characterize genes that<br />
are specifically associated with metastatic prostate cancer. CD82/KAI1 is a metastasis suppressor gene whose expression<br />
is specifically lost in metastatic cancer, but not in primary tumors. Interestingly, CD82/KAI1 is known to associate with both<br />
integrins and RTKs. Our goal has been to determine how loss of CD82/KAI1 expression promotes metastasis by studying the<br />
role of CD82/KAI1 in integrin and RTK crosstalk.<br />
We have found that reexpression of CD82/KAI1 in metastatic tumor cells suppresses laminin-specific migration and invasion<br />
via suppression of both integrin- and ligand-induced activation of the RTK c-Met. Interestingly, c-Met is often overexpressed in<br />
metastatic prostate cancer. Thus, CD82/KAI1 normally acts to regulate signaling through c-Met such that upon CD82 loss in<br />
tumor cells, signaling through c-Met is increased, leading to increased invasion. We are currently determining the mechanism<br />
by which CD82/KAI1 down-regulates c-Met signaling. So far our investigations indicate that c-Met and CD82 do not directly<br />
interact, and CD82 may act to suppress c-Met signaling indirectly by dispersing the c-Met aggregates on metastatic tumor cells<br />
into monomers, thus blocking signaling. We are developing mutants of CD82 to determine which part of the CD82 molecule is<br />
required for suppression of c-Met activity. In addition, we have determined that reexpression of CD82 in tumor cells induces a<br />
physical association between CD82 and a related family member, CD9. Loss of CD9 prevents CD82 from suppressing c-Met.<br />
We are currently determining whether CD82/CD9 association with integrins is required to suppress c-Met.<br />
We have also initiated several mouse studies to demonstrate the importance of CD82 in regulating metastasis in vivo. Using<br />
orthotopic injection of wild-type or CD82-expressing metastatic prostate tumor cells directly into the prostate, we found that<br />
CD82 also suppresses metastasis in vivo. The ability of some prostate cancer cells to metastasize depends on activation of<br />
c-Met. Using mice that are able to specifically activate c-Met, we have been able to demonstrate that these tumor cells will<br />
only metastasize when c-Met is active. Under these conditions, reexpression of CD82 completely suppresses metastasis.<br />
In addition, we have generated mice in which CD82 expression is specifically lost in the epithelial cells of the prostate gland.<br />
These mice will be crossed to mice that develop only primary tumors to determine if the loss of CD82 is sufficient to induce<br />
prostate cancer metastasis.<br />
40
VARI | <strong>2008</strong><br />
External Collaborators<br />
Beatrice Knudsen, Fred Hutchinson Cancer Research Center, Seattle, Washington<br />
Valeri Vasioukin, Fred Hutchinson Cancer Research Center, Seattle, Washington<br />
Andries Zijlstra, Vanderbilt University, Nashville, Tennessee<br />
From left, standing: Bechtel, Rajah, Graf, Zarif, Holleywood, Spotts:<br />
seated: Schulz, Miranti, Guthrey, Tesfay, Saari, Lamb<br />
Recent Publications<br />
Edick, Mathew J., Lia Tesfay, Laura E. Lamb, Beatrice S. Knudsen, and Cindy K. Miranti. 2007. Inhibition of integrin-mediated<br />
crosstalk with epidermal growth factor receptor/Erk or Src signaling pathways in autophagic prostate epithelial cells induces<br />
caspase-independent death. Molecular Biology of the Cell 18(7): 2481–2490.<br />
Tolbert, W. David, Jennifer Daugherty, Chongfeng Gao, Qian Xie, Cindy Miranti, Ermanno Gherardi, George Vande Woude, and<br />
H. Eric Xu. 2007. A mechanistic basis for converting a receptor tyrosine kinase agonist to an antagonist. Proceedings of the<br />
National Academy of Sciences U.S.A. 104(37): 14592–14597.<br />
Wang, Xin, Jin Zhu, Ping Zhao, Yongjun Jiao, Ning Xu, Tessa Grabinski, Chao Liu, Cindy K. Miranti, Tao Fu, and Brian B. Cao.<br />
2007. In vitro efficacy of immuno-chemotherapy with anti-EGFR human Fab-Taxol conjugate on A431 epidermoid carcinoma<br />
cells. Cancer Biology & Therapy 6(6): 980–987.<br />
41
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
James H. Resau, Ph.D.<br />
Division of Quantitative Sciences<br />
Laboratory of Analytical, Cellular, and Molecular Microscopy<br />
Laboratory of Microarray Technology<br />
Laboratory of Molecular Epidemiology<br />
Dr. Resau received his Ph.D. from the University of Maryland School of Medicine in 1985. He has been<br />
involved in clinical and basic science imaging and pathology-related research since 1972. Between<br />
1968 and 1994, he was in the U.S. Army (active duty and reserve assignments) and served in Vietnam.<br />
From 1985 until 1992, Dr. Resau was a tenured faculty member at the University of Maryland School of<br />
Medicine, Department of Pathology. Dr. Resau was the Director of the Analytical, Cellular and Molecular<br />
Microscopy Laboratory in the Advanced BioScience Laboratories–Basic Research Program at the<br />
National Cancer Institute, Frederick Cancer Research and Development Center, Maryland, from 1992<br />
to 1999. He joined VARI as a Special Program Senior <strong>Scientific</strong> Investigator in June 1999 and in 2003<br />
was promoted to Deputy Director. In 2004, Dr. Resau assumed as well the direction of the Laboratory<br />
of Microarray Technology to consolidate the imaging and quantification of clinical samples in a CLIAtype<br />
research laboratory program. In 2005, Dr. Resau was made the Division Director of the quantitative<br />
laboratories (pathology-histology, microarray, proteomics, epidemiology, and bioinformatics), and in<br />
2006 he was promoted to Distinguished <strong>Scientific</strong> Investigator.<br />
Staff<br />
Eric Kort, M.D.<br />
Brendan Looyenga, Ph.D.<br />
Bree Berghuis, B.S., HTL<br />
(ASCP), QIHC<br />
Eric Hudson, B.S.<br />
Angie Jason, B.S.<br />
Paul Norton, B.S.<br />
Ken Olinger, B.S.<br />
David Satterthwaite, B.S.<br />
Kristin VandenBeldt, B.S.<br />
JC Goolsby<br />
42<br />
Students<br />
Pete Haak, B.S.<br />
Heather Born<br />
Danielle Burgenske<br />
Janell Carruthers<br />
Halley Crissman<br />
Sara Herman<br />
Wei Luo<br />
Bryan Mendez<br />
Tarrick Mussa<br />
Sara Ramirez<br />
Aleesa Schlientz<br />
Huong Tran<br />
Yarong Yang<br />
Visiting Scientist<br />
Yair Andegeko
VARI | <strong>2008</strong><br />
Research Interests<br />
The Division of Quantitative Sciences includes the laboratories of Analytical, Cellular, and Molecular Microscopy (ACMM), the<br />
Laboratory of Microarray Technology, the Laboratory of Computational Biology, the Laboratory of Molecular Epidemiology,<br />
and the Laboratory of Mass Spectrometry and Proteomics. The Division’s laboratories use objective measures to define<br />
pathophysiologic events and processes.<br />
The ACMM laboratory has programs in pathology, histology, and imaging to describe and visualize changes in cell, tissue,<br />
or organ structure. Our imaging instruments allow us to visualize cells and their components with striking clarity, and enable<br />
researchers to determine where in a cell specific molecules are located. An archive of pathology tissues in paraffin blocks (Van<br />
Andel Tissue Repository) is being accumulated with the cooperation of local hospitals, and the data on the samples is being<br />
converted to computerized files in collaboration with Tom Barney from VAI-IT. The lab also carries out research that will improve<br />
our ability to quantify images. We are able to image using either fluorescent (e.g., FITC, GFP) or chromatic agents (e.g., DAB,<br />
H&E) and separate the components using our confocal, Nuance, or Maestro instruments.<br />
The Laboratory of Microarray Technology provides gene expression analysis using Agilent commercially prepared arrays as<br />
well as “home-brewed” cDNA microarrays. In 2007 we produced and used 305 cDNA microarrays and 150 custom protein<br />
microarrays. We also used 107 Agilent arrays to genomically characterize a variety of tissues and samples, including archived<br />
human blood samples from newborns.<br />
Hauenstein Parkinson’s Center<br />
Throughout 2007 we continued our collaboration with the Hauenstein Parkinson’s Center, collecting blood samples and controls<br />
from 154 individuals. Mutations in the parkin gene in a set of families with more than one generation affected by Parkinson<br />
disease are being studied by DNA sequence analysis and will be correlated to gene expression data from microarray analysis.<br />
Identification of novel Parkinson-modifying genes with siRNA screening<br />
Small interfering RNA (siRNA) technology allows the specific knockdown of any mRNA/protein pair. Combined with information<br />
from the human genome, this technology has given rise to libraries of siRNAs targeted to every known or predicted gene in the<br />
genome. Under the direction of VARI’s Jeff MacKeigan, postdoctoral fellow Brendon Looyenga has begun to use a subset of<br />
the siRNA library developed by Qiagen to individually target several classes of enzymes having pharmaceutical potential. We<br />
are searching for genes involved in Parkinson disease that may be drug targets for rationally designed therapies.<br />
We are attempting to identify molecules that attenuate oxidative stress–induced toxicity in dopaminergic neurons; our initial<br />
focus is on phosphatases and kinases. To date we have screened all of the phosphatases in the human genome and have<br />
identified several potential candidates that regulate neuronal cell death in response to 6-hydroxydopamine, a toxic compound<br />
used to induce oxidative stress in Parkinson research. We are validating these initial screening studies and are planning the<br />
assays required to screen all kinases in the human genome as well. We hope to extend these studies to include nuclear<br />
hormone receptors and G protein–coupled receptors.<br />
Mouse models of Parkinson disease<br />
James Resau and Brendan Looyenga are generating novel rodent models of dopaminergic cell loss in the brain in collaboration<br />
with VARI’s Bart Williams. A key tool for these studies is the transgenic dopamine-transporter/cre (DAT-cre) mouse line, which<br />
specifically expresses the cre recombinase in dopaminergic neurons of the brain. The DAT-cre mice will allow us to address<br />
the response of such neurons to specific gene deletions and additions; projects based on the DAT-cre mouse model include<br />
the following.<br />
43
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
• Imaging and isolation of primary dopaminergic neurons from mouse brain. Brendan Looyenga has performed<br />
a genetic cross between the DAT-cre strain and ROSA26 reporter strain to generate mice that specifically<br />
express the LacZ reporter gene in dopaminergic neurons. The DAT-cre/ROSA26 mice will permit us to visualize<br />
and quantify live dopaminergic neurons in vivo. With these mice we will assess the effect of cytotoxic agents<br />
(e.g., MMTP, rotenone, or 6-hydroxydopamine) on the number of dopaminergic cells, and more importantly,<br />
assess the ability of mice to recover from these insults. These studies will provide insight into the regenerative<br />
capacity of the brain when dopaminergic neurons are lost or injured. The DAT-cre/ROSA26 mice will also<br />
provide a source of highly pure dopaminergic neurons for in vitro studies.<br />
• Dopaminergic cell regeneration as a function of age. The relationship between age and the likelihood of<br />
developing Parkinson disease is well established, though the causal nature of this relationship is unclear. One<br />
hypothesis is that the capacity of the brain to regenerate damaged neurons decreases with age, consistent<br />
with a gradual loss of brain stem cells that give rise to new dopaminergic neurons. To test this hypothesis in a<br />
mammalian system, we will cross DAT-cre and puDTK mice, the latter specifically expressing herpes simplex<br />
virus thymidine kinase (hsvTK) in cells that contain cre recombinase. Cells expressing hsvTK are sensitive<br />
to ganciglovir (G418) and undergo programmed cell death after systemic treatment. Using the DAT-cre/<br />
puDTK model, we will eliminate dopaminergic neurons at various ages and assess the regenerative potential<br />
of these mice. These studies will provide information about the value of therapies intended to stimulate the<br />
endogenous regenerative capacity of the brain in Parkinson disease patients.<br />
• Effect of hypoxia-inducible factor signaling on dopaminergic cell survival. Dopaminergic neurons are exquisitely<br />
sensitive to oxidative stress (reactive oxygen species), which can lead to cell death by direct mechanisms,<br />
such as damage to important cellular biomolecules, and indirect ones, such as the induction of cell death<br />
pathways. The latter mechanism may be offset by cell survival pathways, which increase the threshold signal<br />
intensity required to induce cell death. Because Parkinson disease is characterized by increased oxidative<br />
stress in dopaminergic neurons, therapies that increase cell survival pathways in these neurons may be broadly<br />
applicable to decrease cell death in patients.<br />
Other highlights<br />
Our GRAPCEP mentorship program continues for an eighth year and is now funded by Schering Plough. This year we had<br />
three students from GRAPCEP. Dr. Resau is a member of the graduate school committee that established the VAEI Graduate<br />
School, which will increase our research and educational opportunities. Also in 2007, Jim Resau had an image selected as one<br />
of the Nikon Small World top 100 images (see p.19), and Bree Berghuis, working with Carrie Graveel, had an image of cMet<br />
staining selected for the June <strong>2008</strong> Ventana Calendar.<br />
From left: Olinger, Luo, Hudson, Jason, Carruthers, Berghuis, Resau, Goolsby, Ramirez, Kort,<br />
VandenBeldt, Looyenga<br />
44
VARI | <strong>2008</strong><br />
Recent Publications<br />
Haak, P., J. Busik, E. Kort, M. Tikhonenko, N. Paneth, and J. Resau. In press. Archived unfrozen neonatal blood spots are<br />
amenable to quantitative gene expression analysis. Neonatology.<br />
Ding, Yan, Elissa A. Boguslawski, Bree D. Berghuis, John J. Young, Zhongfa Zhang, Kim Hardy, Kyle Furge, Eric Kort,<br />
Arthur E. Frankel, Rick V. Hay, James H. Resau, and Nicholas S. Duesbery. <strong>2008</strong>. Mitogen-activated protein kinase kinase<br />
signaling promotes growth and vascularization of fibrosarcoma. Molecular Cancer Therapeutics 7(3): 648–658.<br />
Huang, Dan, Yan Ding, Wang-Mei Luo, Stephanie Bender, Chao-Nan Qian, Eric Kort, Zhong-Fa Zhang, Kristin VandenBeldt,<br />
Nicholas S. Duesbery, James H. Resau, and Bin Tean Teh. <strong>2008</strong>. Inhibition of MAPK kinase signaling pathways suppressed<br />
renal cell carcinoma growth and angiogenesis in vivo. Cancer Research 68(1): 81–88.<br />
Baldus, Stephan E., Eric J. Kort, Peter Schirmacher, Hans P. Dienes, and James H. Resau. 2007. Quantification of MET<br />
and hepatocyte growth factor/scatter factor expression in colorectal adenomas, carcinomas and non-neoplastic epithelia by<br />
quantitative laser scanning microscopy. International Journal of Oncology 31(1): 199–204.<br />
Depeille, Philippe, John J. Young, Elissa A. Boguslawski, Bree D. Berghuis, Eric J. Kort, James H. Resau, Arthur E. Frankel, and<br />
Nicholas S. Duesbery. 2007. Anthrax lethal toxin inhibits growth of and vascular endothelial growth factor release from endothelial<br />
cells expressing the human herpes virus 8 viral G protein–coupled receptor. Clinical Cancer Research 13(19): 5926–5934.<br />
Li, Zheng, Shireesh Srivastava, Xuerui Yang, Sheenu Mittal, Paul Norton, James Resau, Brian Haab, and Christina Chan. 2007.<br />
A hierarchical approach employing metabolic and gene expression profiles to identify the pathways that confer cytotoxicity in<br />
HepG2 cells. BMC Systems Biology 1: 15 pp.<br />
Lindemann, K., J. Resau, J. Nährig, E. Kort, B. Leeser, K. Anneke, A. Welk, J. Schäfer, G. F. Vande Woude, E. Lengyel, and<br />
N. Harbeck. 2007. Differential expression of c-Met, its ligand HGF/SF and HER2/neu in DCIS and adjacent normal breast<br />
tissue. Histopathology 51(1): 54–62.<br />
Ott, Mickey, Alan T. Davis, Wayne VanderKolk, James H. Resau, David H. DeHeer, Clifford B. Jones, Chad Stouffer, and<br />
Edward W. Kubek. 2007. The protective effect of the blood brain barrier from systemic cytokines in an animal femur fracture<br />
model. Journal of Trauma 63(3): 591–595.<br />
Whitwam, T., M.W. VanBrocklin, M.E. Russo, P.T. Haak, D. Bilgili, J.H. Resau, H.-M. Koo, and S.L. Holmen. 2007. Differential<br />
oncogenic potential of activated RAS isoforms in melanocytes. Oncogene 26(31): 4563–4570.<br />
Young, John J., Jennifer L. Bromberg-White, Cassandra R. Zylstra, Joseph T. Church, Elissa Boguslawski, James H. Resau,<br />
Bart O. Williams, and Nicholas S. Duesbery. 2007. LRP5 and LRP6 are not required for protective antigen–mediated internalization<br />
or lethality of anthrax lethal toxin. PLoS Pathogens 3(3): e27.<br />
Zhao, Ping, Tessa Grabinski, Chongfeng Gao, R. Scot Skinner, Troy Giambernardi, Yanli Su, Eric Hudson, James Resau, Milton<br />
Gross, George F. Vande Woude, Rick Hay, and Brian Cao. 2007. Identification of a Met-binding peptide from a phage display<br />
library. Clinical Cancer Research 13(20): 6049–6055.<br />
45
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Pamela J. Swiatek, Ph.D., M.B.A.<br />
Laboratory of Germline Modification and Cytogenetics<br />
Dr. Swiatek received her M.S. (1984) and Ph.D. (1988) degrees in pathology from Indiana University.<br />
From 1988 to 1990, she was a postdoctoral fellow at the Tampa Bay Research Institute. From<br />
1990 to 1994, she was a postdoctoral fellow at the Roche Institute of Molecular Biology in the<br />
laboratory of Tom Gridley. From 1994 to 2000, Dr. Swiatek was a research scientist and Director of<br />
the Transgenic Core Facility at the Wadsworth Center in Albany, N.Y., and an Assistant Professor in<br />
the Department of Biomedical Sciences at the State University of New York at Albany. She joined<br />
VARI as a Special Program Investigator in August 2000. She has been the chair of the Institutional<br />
Animal Care and Use Committee since 2002 and is an Adjunct Assistant Professor in the College<br />
of Veterinary Medicine at Michigan State University. Dr. Swiatek received her M.B.A. in 2005 from<br />
Krannert School of Management at Purdue University, and in 2006 she was promoted to Senior<br />
<strong>Scientific</strong> Investigator.<br />
Staff<br />
Sok Kean Khoo, Ph.D.,<br />
Associate Laboratory Director<br />
Kellie Sisson, B.S.<br />
Julie Koeman, B.S., CLSp(CG)<br />
Laura Mowry, B.S.<br />
Diana Lewis<br />
Student<br />
Katie Koelzer<br />
46
VARI | <strong>2008</strong><br />
Research Interests<br />
The Germline Modification and Cytogenetics lab is a full-service lab that functions at the levels of service, research, and<br />
teaching to develop, analyze, and maintain mouse models of human disease. Our lab applies a business philosophy to core<br />
service offerings for both the VARI community and external entities. Our mission is to support mouse model and cytogenetics<br />
research with scientific innovation, customer satisfaction, and service excellence.<br />
Gene targeting<br />
Mouse models are produced using gene-targeting technology, a well-established, powerful method for inserting specific<br />
genetic changes into the mouse genome. The resulting mice can be used to study the effects of these changes in the complex<br />
biological environment of a living organism. The genetic changes can include the introduction of a gene into a specific site in<br />
the genome (gene “knock-in”) or the inactivation of a gene already in the genome (gene “knock-out”). Since these mutations<br />
are introduced into the reproductive cells known as the germline, they can be used to study the developmental aspects of gene<br />
function associated with inherited genetic diseases.<br />
The germline modification lab can also produce mouse models in which the gene of interest is inactivated in a target organ<br />
or cell line instead of in the entire animal. These models, known as conditional knock-outs, are particularly useful in studying<br />
genes that, if missing, cause the mouse to die as an embryo. The lab can produce mutant embryos that have a wild-type<br />
placenta using tetraploid embryo technology, which is useful when the gene-targeted mutation prevents implantation of the<br />
mouse embryo in the uterus. We also assist in the development of embryonic stem (ES) or fibroblast cell lines from mutant<br />
embryos, to allow for in vitro studies of the gene mutation.<br />
Our gene-targeting service encompasses three major procedures: DNA electroporation, clone expansion and cryopreservation,<br />
and microinjection. Gene targeting is initiated by mutating the genomic DNA of interest and inserting it into ES cells via<br />
electroporation. The mutated gene integrates into the genome and, by a process called homologous recombination, replaces<br />
one of the two wild-type copies of the gene in the ES cells. Clones are identified, isolated, and cryopreserved, and genomic<br />
DNA is extracted from each clone and delivered to the client for analysis. Correctly targeted ES cell clones are thawed,<br />
established into tissue culture, and cryopreserved in liquid nitrogen. Gene-targeting mutations are introduced by microinjection<br />
of the pluripotent ES cell clones into 3.5-day-old mouse embryos (blastocysts). These embryos, containing a mixture of<br />
wild-type and mutant ES cells, develop into mice called chimeras. The offspring of chimeras that inherit the mutated gene are<br />
heterozygotes possessing one copy of the mutated gene. The heterozygous mice are bred together to produce “knock-out<br />
mice” that completely lack the normal gene and have two copies of the mutant gene.<br />
Embryo/sperm cryopreservation<br />
We provide cryopreservation services for archiving and reconstituting valuable mouse strains. These cost-effective procedures<br />
decrease the need to continuously breed valuable mouse models, and they provide added insurance against the loss of custom<br />
mouse lines due to disease outbreak or a catastrophic event. Mouse embryos at various stages of development, as well as<br />
mouse sperm, can be cryopreserved and stored in liquid nitrogen; they can be thawed and used, respectively, by implantation<br />
into the oviducts of recipient mice or by in vitro fertilization of oocytes.<br />
47
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Cytogenetics<br />
Our lab also directs the VARI cytogenetics core, which uses advanced molecular techniques to identify structural and numerical<br />
chromosomal aberrations in mouse, rat, and human cells. Tumor, fibroblast, blood, or ES cells can be grown in tissue culture,<br />
growth-arrested, fixed, and spread onto glass slides. Karyotyping of chromosomes using Leishman- or Giemsa-stained<br />
(G-banded) chromosomes is our basic service; spectral karyotyping (SKY) analysis of metaphase chromosome spreads in 24<br />
colors can aid in detecting subtle and complex chromosomal rearrangements. Fluorescence in situ hybridization (FISH) analysis,<br />
using indirectly or directly labeled bacterial artificial chromosome (BAC) or plasmid probes, can also be performed on metaphase<br />
spreads or on interphase nuclei derived from tissue touch preps or nondividing cells. Sequential staining of identical metaphase<br />
spreads using FISH and SKY can help identify the integration site of a randomly integrated transgene. Recently, FISH has been<br />
widely used to validate microarray data by confirming amplification/gain or deletion/loss of chromosomal regions of interest.<br />
Speed congenics<br />
Congenic mouse strain development traditionally involves a series of backcrosses, transferring a targeted mutation or genetic<br />
region of interest from a mixed genetic donor background to a defined genetic recipient background (usually an inbred strain).<br />
This process requires about ten generations (2.5 to 3 years) to attain 99.9% of the recipient’s genome. Since congenic mice<br />
have a more defined genetic background, phenotypic characteristics are less variable and the effects of modifier genes can be<br />
more pronounced.<br />
Speed congenics, also called marker-assisted breeding, uses DNA markers in a progressive breeding selection to accelerate<br />
the congenic process. For high-throughput genotyping, we use the state-of-the-art Sentrix BeadChip technology from<br />
Illumina, which contains 1,449 mouse single nucleotide polymorphisms (SNPs). These SNPs are strain-specific and cover the<br />
10 most commonly used inbred mouse strains for optimal marker selection. The client provides the genomic DNA of male<br />
mice from the second, third, and fourth backcross generations for genotyping. The males having the highest percentage of<br />
the recipient’s genome from each generation are identified, and these mice are bred by the client. Using speed congenics,<br />
99.9% of congenicity can be achieved in five generations (about 1.5 years).<br />
Michigan Animal Model Consortium<br />
The VARI Germline Modification and Cytogenetics lab directs the Michigan Animal Model Consortium (MAMC), one of the ten<br />
Core Technology Alliance (CTA) collaborative core facilities. The MAMC labs were developed with funding from the Michigan<br />
Economic Development Corporation and provide efficient mouse modeling services to researchers studying human diseases.<br />
MAMC’s long-term goal is to offer a comprehensive<br />
set of cutting-edge services that, through continuous<br />
enhancements and development, will define<br />
our organization as a single point-of-service site<br />
for animal models research. Centralized provision<br />
of services maximizes research productivity and<br />
decreases time to discovery; it is in demand<br />
by academia, and also by pharmaceutical and<br />
biotechnology companies, which are increasingly<br />
looking to outsource to service centers. Through<br />
its well-organized service structure and staff of<br />
experts, MAMC supports the growth of the life<br />
science industry in Michigan, which is congruent<br />
with the CTA goals.<br />
From left: Sisson, Swiatek, Khoo, Koeman, Lewis, Mowry<br />
48
VARI | <strong>2008</strong><br />
MAMC service offerings<br />
Animal model development<br />
• Mouse transgenics. Transgenic technology is used to produce genetically engineered mice expressing foreign<br />
genes and serving as models for human disease research. Microinjection delivers the foreign DNA into the<br />
pronucleus of a one-cell fertilized egg. This service uses various strains of laboratory mice, with production of<br />
three transgenic founder mice guaranteed from each procedure.<br />
• Gene targeting. By transfecting mouse embryonic stem cells with inactivating, homologous DNAs, target<br />
gene expression can be shut down. Genetically engineered mice are produced by microinjecting mutant stem<br />
cells into mouse embryos and breeding the progeny to mutant homozygosity. This service is provided using<br />
129 or C57BL/6 embryonic stem cells.<br />
• Xenotransplantation. Human cancer cells are injected into immunodeficient mice to produce human-derived<br />
tumors. Protocols are designed to test anti-tumor treatment regimens that can lead to prognostic, diagnostic,<br />
or therapeutic procedures for humans.<br />
Animal model analysis<br />
• Cytogenetics. Mouse and rat chromosomal abnormalities and genetic loci are visually observed using Giemsa<br />
stain, SKY, or FISH techniques.<br />
• Necropsy. Mice are dissected postmortem and tissues are fixed for histological analysis, with necropsy<br />
reports generated using voice-recognition software.<br />
• Histology. Histological sections are prepared from mouse tissues using microtomes and cryostats; they are<br />
processed and stained using automated instruments and then are microscopically analyzed.<br />
• Veterinary pathology. A board-certified veterinary pathologist holding the D.V.M. and Ph.D. degrees provides<br />
expert microscopic analysis and project consultation.<br />
• DNA isolation. DNA is isolated from mouse tail biopsies using the AutogenPrep 960 instrument.<br />
Animal model maintenance and preservation<br />
• Mouse rederivation. All mouse strains entering the specific pathogen–free breeding facility are rederived to<br />
specific pathogen–free status using embryo transfer techniques.<br />
• Animal technical services. Veterinary services such as injections, measurements, mating set-up, and tail<br />
biopsies are performed by the animal technician staff.<br />
• Contract breeding. Wild-type mouse strains and genetically engineered animal models are maintained for<br />
research purposes by breeding the strains in a specific pathogen–free environment.<br />
• Embryo/sperm cryopreservation. Genetically engineered mice are preserved for archival purposes, disease<br />
control, genetic stability, and economic efficiency using germplasm cryopreservation techniques.<br />
• Cancer model repository. Mouse cancer models of research interest are maintained through breeding strategies.<br />
49
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Lipid signaling in osteosarcoma<br />
A cell-based RNAi screen of human genes identified regulators of lipid signaling. Shown is an osteosarcoma cell marked by a lipid-binding domain<br />
fused to enhanced green fluorescent protein (green) and with the nucleus Hoechst-stained (blue); imaging was by fluorescence microscopy.<br />
Photo by Katie Sian of the MacKeigan lab.<br />
50
VARI | <strong>2008</strong><br />
Bin T. Teh, M.D., Ph.D.<br />
Laboratory of Cancer Genetics<br />
Dr. Teh obtained his M.D. from the University of Queensland, Australia, in 1992, and his Ph.D. from<br />
the Karolinska Institute, Sweden, in 1997. Before joining the Van Andel Research Institute, he was an<br />
Associate Professor of Medical Genetics at the Karolinska Institute. Dr. Teh joined VARI as a Senior<br />
<strong>Scientific</strong> Investigator in January 2000. His research mainly focuses on kidney cancer, and he is<br />
currently on the Medical Advisory Board of the Kidney Cancer Association. Dr. Teh was promoted to<br />
Distinguished <strong>Scientific</strong> Investigator in 2005.<br />
Staff<br />
Students<br />
Visiting Scientist<br />
Chao-Nan (Miles) Qian, M.D., Ph.D.<br />
Peng-Fei Wang, M.D., Ph.D.<br />
Eric Kort, M.D.<br />
Daisuke Matsuda, M.D.<br />
Jindong Chen, Ph.D.<br />
Leslie Farber, Ph.D.<br />
Dan Huang, Ph.D.<br />
Yan Li, Ph.D.<br />
David Petillo, Ph.D.<br />
Racheal Zhang, Ph.D.<br />
Zhongfa (Jacob) Zhang, Ph.D.<br />
Stephanie Bender, M.S.<br />
Wangmei Luo, M.S.<br />
Robert Antecki, B.S.<br />
Elizabeth Block, B.S.<br />
Stephanie Kloostra, B.S.<br />
Aaron Massie, B.S.<br />
Sabrina Noyes, B.S.<br />
Michael Westphal, B.S.<br />
Michael Avallone<br />
Lindsay Barnett<br />
Kristin Buzzitta<br />
Bill Wondergem<br />
Laura Lowe Furge, Ph.D.<br />
51
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Research Interests<br />
Kidney cancer, or renal cell carcinoma (RCC), is the tenth most common cancer in the United States (51,000 new cases and<br />
more than 13,000 deaths a year). Its incidence has been increasing, a phenomenon that cannot be accounted for by the wider<br />
use of imaging procedures. We have established a comprehensive and integrated kidney research program, and our major<br />
research goals are 1) to identify the molecular signatures of different subtypes of kidney tumors, both hereditary and sporadic,<br />
and to understand how genes function and interact in giving rise to the tumors and their progression; 2) to identify and develop<br />
diagnostic and prognostic biomarkers for kidney cancer; 3) to identify and study novel and established molecular drug targets<br />
and their sensitivity and resistance; and 4) to develop animal models for drug testing and preclinical bioimaging.<br />
Our program to date has established a worldwide network of collaborators; a tissue bank containing fresh-frozen tumor pairs<br />
(over 1,500 cases) and serum; and a gene expression profiling database of 600 tumors, with long-term clinical follow-up<br />
information for half of them. Our program includes molecular subclassification using microarray gene expression profiling and<br />
bioinformatic analysis, generation of RCC mouse models, and more recently, molecular therapeutic studies.<br />
RCC genomics<br />
We have been using high-density single nucleotide polymorphism (SNP) arrays to genotype RCC samples, and by combing<br />
this data and the gene expression data (see below), we have identified the candidate chromosomal regions and genes that are<br />
involved in different subsets of tumors.<br />
Gene expression profiling and bioinformatics<br />
To date, we have studied over 600 RCC specimens. We are currently focusing on analysis and data mining. Clinically, we<br />
continue to subclassify the tumors by correlation with clinicopathological information, including rarer forms of RCC such as<br />
translation-related papillary RCC, mixed epithelial and stromal tumors, and adult Wilms. We are also in the process of trying to<br />
understand the underlying molecular signatures of some of the so-called unclassified group of tumors for which the histological<br />
diagnosis is “unknown”. Our database has proven to be very useful in RCC research, since we can obtain differential expression<br />
data for any gene in seconds.<br />
Mouse models of kidney cancer and molecular therapeutic studies<br />
We have generated several kidney-specific conditional knock-outs including APC, PTEN, and VHL. The first two knock-outs<br />
give rise to renal cysts and tumors including urothelial cancer of the renal pelvis, whereas the VHL knock-out remains neoplasiafree;<br />
double knock-outs are also being studied. We have successfully generated nine xenograft RCC models via subcapsular<br />
injection that have characteristic clinical features and outcomes. Tumors and serum have been harvested for a baseline data<br />
set. We are currently performing in vitro and in vivo studies on several new drugs for kidney cancer.<br />
52
VARI | <strong>2008</strong><br />
Targeted therapeutic studies<br />
We have focused on several targets we identified using gene expression profiling studies. In vitro and in vivo studies are being<br />
performed to verify these targets and their role in therapeutics. These include cell-cycle, proliferation, and migration assays to assess<br />
the cellular effects of these genes. In vivo studies are performed to understand the involvement of blood vessels in drug response.<br />
External Collaborators<br />
We have extensive collaborations with researchers and clinicians in the United States and overseas.<br />
From left: Teh, Antecki, Li, Furge, Huang, Kort, Noyes, Block, Petillo, Zhang, Matsuda, Chen, Kloostra<br />
Recent Publications<br />
Camparo, P., V. Vasiliu, V. Molinié, J. Couturier, K. Dykema, D. Petillo, K.A. Furge, E.M. Comperat, M. Laé, R. Bouvier, L.<br />
Boccon-Gibbod, Y. Denoux, S. Ferlicot, E. Forest, G. Fromont, et al. In press. Renal translocation carcinomas: clinicopathological,<br />
immunohistochemical, and gene expression profiling analysis of 31 cases with a review of the literature. American<br />
Journal of Surgical Pathology.<br />
Chuang, Shang-Tian, Kurt T. Patton, Kristian T. Schafernak, Veronica Papavero, Fan Lin, Robert C. Baxter, Bin Tean Teh, and<br />
Ximing J. Yang. <strong>2008</strong>. Over expression of insulin-like growth factor binding protein 3 in clear cell renal cell carcinoma. Journal<br />
of Urology 179(2): 445–449.<br />
Huang, Dan, Yan Ding, Wang-Mei Luo, Stephanie Bender, Chao-Nan Qian, Eric Kort, Zhong-Fa Zhang, Kristin VandenBeldt,<br />
Nicholas S. Duesbery, James H. Resau, and Bin Tean Teh. <strong>2008</strong>. Inhibition of MAPK kinase signaling pathways suppressed<br />
renal cell carcinoma growth and angiogenesis in vivo. Cancer Research 68(1): 81–88.<br />
53
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Morris, M.R., D. Gentle, M. Abdulrahman, N. Clarke, M. Brown, T. Kishida, M. Yao, B.T. Teh, F. Latif, and E.R. Maher. <strong>2008</strong>.<br />
Functional epigenomics approach to identify methylated candidate tumour suppressor genes in renal cell carcinoma. British<br />
Journal of Cancer 98(2): 496–501.<br />
Selvarajan, S., L-H. Sii, A. Lee, G. Yip, B-H. Bay, M-H. Tan, B.T. Teh, and P-H. Tan. <strong>2008</strong>. Parafibromin expression in breast<br />
cancer: a novel marker for prognostication? Journal of Clinical Pathology 61(1): 64–67.<br />
Wang, Pengfei, Michael R. Bowl, Stephanie Bender, Jun Peng, Leslie Farber, Jindong Chen, Asif Ali, ZhongFa Zhang,<br />
Arthur S. Alberts, Rajesh V. Thakker, Ali Shilatifard, Bart O. Williams, and Bin Tean Teh. <strong>2008</strong>. Parafibromin, a component<br />
of the human PAF complex, regulates growth factors and is required for embryonic development and survival in adult mice.<br />
Molecular and Cellular Biology 28(9): 2930–2940.<br />
Yang, Ximing J., Ming Zhou, Ondrej Hes, Steven Shen, Rongshan Li, Jose Lopez, Rajal B. Shah, Yu Yang, Shang-Tian Chuang,<br />
Fan Lin, Maria M. Tretiakova, Eric J. Kort, and Bin Tean Teh. <strong>2008</strong>. Tubulocystic carcinoma of the kidney: clinicopathological<br />
and molecular characterization. American Journal of Surgical Pathology 32(2): 177–187.<br />
Al-sarraf, Nael, Johanne Nørvig Reiff, Jane Hinrichsen, Shaukat Mahmood, Bin Tean Teh, Eilish McGovern, Pierre De Meyts,<br />
Kenneth J. O’Byrne, and Steven G. Gray. 2007. DOK4/IRS-5 expression is altered in clear cell renal cell carcinoma.<br />
International Journal of Cancer 121(5): 992–998.<br />
Daly, Adrian F., Jean-François Vanbellinghen, Sok Kean Khoo, Marie-Lise Jaffrain-Rea, Luciana A. Naves, Mirtha A. Guitelman,<br />
Arnaud Murat, Philippe Emy, Anne-Paule Gimenez-Roqueplo, Guido Tamburrano, Gérald Raverot, Anne Barlier, Wouter De<br />
Herder, Alfred Penfornis, Enrica Ciccarelli, et al. 2007. Aryl hydrocarbon receptor interacting protein gene mutations in familial<br />
isolated pituitary adenomas: analysis in 73 families. Journal of Clinical Endocrinology and Metabolism 92(5): 1891–1896.<br />
Haven, C.J., M. van Puijenbroek, M.H. Tan, B.T. Teh, G.J. Fleuren, T. van Wezel, and H. Morreau. 2007. Identification of MEN1<br />
and HRPT2 somatic mutations in paraffin-embedded (sporadic) parathyroid carcinomas. Clinical Endocrinology 67(3): 370–376.<br />
Yao, Xin, Chao-Nan Qian, Zhong-Fa Zhang, Min-Han Tan, Eric J. Kort, James H. Resau, and Bin Tean Teh. 2007. Two distinct<br />
types of blood vessels in clear cell renal cell carcinoma have contrasting prognostic implications. Clinical Cancer Research<br />
13(1): 161–169.<br />
54
VARI | <strong>2008</strong><br />
Steven J. Triezenberg, Ph.D.<br />
Laboratory of Transcriptional Regulation<br />
Dr. Triezenberg received his bachelor’s degree in biology and education at Calvin College in Grand<br />
Rapids, Michigan. His Ph.D. training in cell and molecular biology at the University of Michigan was<br />
followed by postdoctoral research in the laboratory of Steven L. McKnight at the Carnegie Institution of<br />
Washington. Dr. Triezenberg was a faculty member of the Department of Biochemistry and Molecular<br />
Biology at Michigan State University for more than 18 years, where he also served as associate director<br />
of the Graduate Program in Cell and Molecular Biology. Dr. Triezenberg was recruited to VAI to serve<br />
as the founding Dean of the Van Andel Institute Graduate School and as a <strong>Scientific</strong> Investigator in the<br />
Van Andel Research Institute, arriving in May 2006.<br />
Staff<br />
Glen Alberts, B.S.<br />
Jennifer Klomp, M.S.<br />
Xu Lu, Ph.D.<br />
Student<br />
Sebla Kutluay, B.S.<br />
Sarah DeVos<br />
55
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Research Interests<br />
The genetic information encoded in DNA must first be copied, in the form of RNA, before it can be translated into the proteins<br />
that do most of the work in a cell. Some genes must be expressed more or less constantly throughout the life of any eukaryotic<br />
cell. Others must be turned on (or turned off) in particular cells either at specific times or in response to a specific signal or<br />
event. Thus, regulation of gene expression is a key determinant of cell function. Our laboratory explores the mechanisms that<br />
regulate the first step in that flow, transcription, using infection by herpes simplex virus and the acclimation of plants to cold<br />
temperature as experimental contexts.<br />
Transcriptional activation in herpes simplex virus infection<br />
Herpes simplex virus type 1 (HSV-1) causes the common cold sore or fever blister. The initial lytic infection by HSV-1 results in<br />
the obvious symptoms, typically in or around the mouth. After the initial infection, HSV-1 finds its way into nerve cells, where<br />
the virus can hide in a latent mode for long times—essentially for the lifetime of the host. Occasionally, some event (such as<br />
emotional stress or damage to the nerve from a sunburn or a root canal operation) will cause the latent virus to reactivate,<br />
producing new viruses and recurrence of the cold sore.<br />
The DNA genome of HSV-1 encodes approximately 80 different proteins. The virus does not have its own machinery for<br />
expressing those genes, so it diverts the gene expression machinery of the host cell. That process is triggered by a viral<br />
regulatory protein designated VP16, whose function is to stimulate transcription of the first viral genes to be expressed (the<br />
immediate-early, or IE, genes). In the prevailing model for the mechanism of transcriptional activation, the activation domain of<br />
an activating protein (such as VP16) can bind to the host cell RNA polymerase II or to its accessory proteins. In this manner,<br />
VP16 recruits or tethers these accessory proteins to the genes that are to be activated.<br />
Chromatin-modifying coactivators<br />
Eukaryotic DNA is typically packaged as chromatin, in which the DNA is wrapped around “spools” of histone proteins, and<br />
these spools are arranged into higher-order structures. This packaging creates an impediment to transcription, during which<br />
RNA polymerase must separate the two strands of DNA. The impediment is overcome with the help of chromatin-modifying<br />
coactivator proteins; some chemically alter the histones and others remove the histones so that RNA polymerase can access<br />
the DNA. VP16 can recruit various coactivator proteins to target genes, and results from our lab have clearly indicated that<br />
VP16 can recruit certain coactivators to IE genes during lytic infection. We have also shown that some histone proteins do<br />
associate with viral DNA, although perhaps not to the same extent as with cellular DNA.<br />
Yet, the fact that coactivators are present on viral DNA is not sufficient evidence that they play a significant role in transcriptional<br />
activation. We have tested whether particular coactivators are necessary for effective expression of HSV-1 IE genes during lytic<br />
infection, using siRNA knockdown of certain coactivators or using mutant cell lines having disrupted expression or activity of<br />
a coactivator. We were surprised to find that viral genes were expressed efficiently regardless of what we did to diminish the<br />
coactivator activity. These results indicate that our initial hypothesis was wrong; the coactivators, although present, are not<br />
required for viral gene expression during lytic infection. Another possibility is that the coactivators are required to reactivate the<br />
viral genes from the latent or quiescent state, and we will test that hypothesis during the coming year.<br />
56
VARI | <strong>2008</strong><br />
Can a curry spice block herpes infections?<br />
Curcumin, the bright yellow component of the curry spice turmeric, affects eukaryotic cells in several ways. Another laboratory<br />
had reported that curcumin could block the histone acetyltransferase activity of two coactivator proteins, p300 and CBP.<br />
Because we had shown that VP16 can recruit p300 and CBP to viral IE gene promoters, we tested whether curcumin would<br />
block viral IE gene expression and thus block HSV infection. Indeed, curcumin has dramatic effects on IE gene expression and<br />
substantial effects on virus infection; however, subsequent experiments indicate that this effect is not mediated by the p300 and<br />
CBP proteins. For example, the effects on viral infection were observed using lower curcumin concentrations than those required<br />
to substantially inhibit global histone H3 acetylation. Moreover, we detected no effect of curcumin on the presence of H3 at viral<br />
gene promoters or on the acetylation of H3 at those promoters. These results suggest that curcumin affects VP16-mediated<br />
recruitment of RNA polymerase II to IE gene promoters by a mechanism independent of p300/CBP histone acetyltransferase<br />
activity. We conclude that curcumin does block herpes infections, but we don’t yet know the mechanism by which it does so.<br />
Gene activation during cold acclimation of plants<br />
Although plants and their cells obviously have very different forms and functions than animals and their cells, the mechanisms<br />
used for expressing genetic information are quite similar. About ten years ago, we applied our emerging interest in<br />
chromatin-modifying coactivators to an interesting question in plant biology. Some plants, including the popular experimental<br />
organism Arabidopsis, can sense low but nonfreezing temperature in a way that provides protection from subsequent freezing<br />
temperatures. This process is known as cold acclimation. Michael Thomashow, an MSU plant scientist, identified genes that<br />
are expressed during this process and a transcription factor that activates these genes in response to low temperature. We<br />
have collaborated with the Thomashow laboratory to explore the mechanisms involved. We have characterized one particular<br />
histone acetyltransferase, termed GCN5, and two of its accessory proteins, ADA2a and ADA2b. Mutations in the genes<br />
encoding these coactivator proteins result in diminished expression of cold-regulated genes. Moreover, histones located at<br />
these cold-regulated genes become more highly acetylated during initial stages of cold acclimation. However, contrary to our<br />
expectations, the GCN5 and ADA2 proteins are not responsible for this cold-induced acetylation. In fact, we’ve tested several<br />
other Arabidopsis histone acetyltransferases, and none (on their own) seem solely responsible for this acetylation. It seems<br />
likely that redundant mechanisms are at work, such that when we disrupt one pathway, another pathway compensates.<br />
We are also collaborating with groups in Greece and Pennsylvania to explore the distinct biological activities of the two ADA2<br />
proteins. Although the two proteins have very similar sequences and both are expressed throughout the plant, mutations in the<br />
genes encoding these two proteins have very different phenotypes. The ada2b mutants are very short, have smaller cells than<br />
normal, and are sterile. In contrast, the ada2a mutants seem quite normal in most attributes (Figure 1). Plants with mutations in both<br />
ADA2a and ADA2b are strikingly similar to plants with mutations in GCN5. We suspect that GCN5 can partner with either ADA2a or<br />
ADA2b and that these two distinct complexes affect different sets of genes and thus different developmental and stress response<br />
pathways. This work may help us understand whether the mechanisms by which plants express their genes can be effectively<br />
modulated so as to protect crop plants from loss in yield or viability due to environmental stresses such as low temperature.<br />
Figure 1<br />
Figure 1. Growth of Arabidopsis plants, wild<br />
type and mutants.<br />
57
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
External Collaborators<br />
Kanchan Pavangadkar and Michael F. Thomashow, Michigan State University, East Lansing<br />
Amy S. Hark, Muhlenberg College, Allentown, Pennsylvania<br />
Kostas Vlachonasios, Aristotle University of Thessaloniki, Greece<br />
From left: Lu, Alberts, Kutluay, Triezenberg, Klomp<br />
Recent Publications<br />
Kutluay, Sebla B., James Doroghazi, Martha E. Roemer, and Steven J. Triezenberg. <strong>2008</strong>. Curcurmin inhibits herpes<br />
simplex virus immediate-early gene expression by a mechanism independent of p300/CBP histone acetyltransferase<br />
activity. Virology 373(2): 239–247.<br />
Shooltz, Dean D., Glen L. Alberts, and Steven J. Triezenberg. <strong>2008</strong>. One-step affinity purification of recombinant TATA binding<br />
proteins utilizing a modular protein interaction partner. Protein Expression and Purification 59(2): 297–301.<br />
58
VARI | <strong>2008</strong><br />
George F. Vande Woude, Ph.D.<br />
Laboratory of Molecular Oncology<br />
Dr. Vande Woude received his M.S. (1962) and Ph.D. (1964) from Rutgers University. From 1964–<br />
1972, he served first as a postdoctoral research associate, then as a research virologist for the U.S.<br />
Department of Agriculture at Plum Island Animal Disease Center. In 1972, he joined the National<br />
Cancer Institute as Head of the Human Tumor Studies and Virus Tumor Biochemistry sections and,<br />
in 1980, was appointed Chief of the Laboratory of Molecular Oncology. In 1983, he became Director<br />
of the Advanced Bioscience Laboratories–Basic Research Program at the National Cancer Institute’s<br />
Frederick Cancer Research and Development Center, a position he held until 1998. From 1995, Dr.<br />
Vande Woude first served as Special Advisor to the Director, and then as Director for the Division of<br />
Basic Sciences at the National Cancer Institute. In 1999, he was recruited to become the founding<br />
Director of the Van Andel Research Institute.<br />
Staff<br />
Laboratory Staff<br />
Student<br />
Guest Researchers<br />
Qian Xie, M.D., Ph.D.<br />
Yu-Wen Zhang, M.D., Ph.D.<br />
Chongfeng Gao, Ph.D.<br />
Carrie Graveel, Ph.D.<br />
Dafna Kaufman, M.Sc.<br />
Angelique Berens, B.S.<br />
Jack DeGroot, B.S.<br />
Curt Essenburg, B.S.<br />
Betsy Haak, B.S.<br />
Liang Kang, B.S.<br />
Rachel Kuznar, B.S.<br />
Benjamin Staal, B.S.<br />
Ryan Thompson, B.S.<br />
Yanli Su, A.M.A.T.<br />
Alysha Kett<br />
David Wenkert, M.D.<br />
Yuehai Shen, Ph.D.<br />
Edwin Chen, B.S.<br />
59
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Laboratory of Molecular Oncology<br />
The Laboratory of Molecular Oncology is focused on understanding the numerous and diverse roles that Met and HGF/SF play<br />
in malignant progression and metastasis. Our work involves a wide variety of cancers, animal models, and drug therapies. The<br />
combination of studies, coupled with our examination of Met signaling, will lead to a greater understanding of tumor progression<br />
and new knowledge for developing and delivering novel targeted therapies.<br />
Clonal selection of proliferative and invasive cells in metastasis<br />
Malignant progression leads to metastasis, which is the primary cause of death due to cancer. Metastasis begins with proliferating<br />
tumor cells that become invasive and detach from the primary tumor mass, invading the extracellular matrix, entering the<br />
bloodstream or lymphatic vessels, and establishing metastases or secondary tumors as proliferating colonies at distant sites.<br />
Because phenotypic switching between proliferation and invasion is critical to malignant progression, we use in vitro and in vivo<br />
methods to select subclones of glioblastoma tumor cells that are either highly proliferative or highly invasive.<br />
The molecular signaling pathways that accompany phenotypic switching change dramatically in response to HGF/SF. We<br />
discovered that invasive cells signal through the Ras/MAPK pathway, while the c-myc pathway is highly expressed in<br />
proliferative clones. Using gene expression analysis, spectral karyotyping (SKY), and fluorescent in situ hybridization (FISH),<br />
we observed that subtle and specific changes in chromosome content ratio are virtually the same as the changes in<br />
the chromosome transcriptome ratio, showing that major changes in gene expression are mediated by gains or losses in<br />
chromosome content. Importantly, a significant number of the genes whose expression change is greater than twofold are<br />
functionally consistent with changes in the proliferative or invasive phenotypes. Our results imply that chromosome instability<br />
can provide the diversity of gene expression that allows a tumor to switch between proliferative and invasive phenotypes during<br />
tumor progression.<br />
Met Induces mammary tumors in mice and is associated with human basal breast cancers<br />
We are also investigating the role that the MET oncogene plays in breast cancer progression and metastasis through a novel<br />
mouse model of mutationally activated Met. We discovered that mutationally activated Met induces a high incidence of<br />
mammary tumors in mice. These mammary tumors have several unique pathological characteristics and contain high levels of<br />
extrachromosomal Met amplification. In addition, all of the tumors lack progesterone receptor expression and only half express<br />
ErbB2. These characteristics are similar to those of aggressive forms of human breast cancer and led us to examine how Met<br />
is associated with the various human breast cancer subtypes.<br />
Recently, gene expression studies have identified several distinct breast cancer subtypes that correlate with clinical outcome.<br />
These molecular subtypes include three main groups of estrogen receptor (ER)–negative tumors (basal, ErbB2, and normallike/unclassified)<br />
and at least two types of ER-positive tumors (luminal A and luminal B). A study of Met expression data<br />
from existing human breast cancer datasets indicated that Met was significantly expressed in basal-like cancers relative to<br />
nonbasal cancers. To further examine Met expression patterns in human breast cancer, we used a human breast cancer tissue<br />
microarray containing 139 patient samples (in collaboration with Dr. Matthew Ellis and associates, Washington University). High<br />
Met staining was associated with the basal and ErbB2 subtypes and was inversely associated with the luminal subtypes. To<br />
confirm this observation, Met expression was compared to ER status and was found to negatively correlate with ER expression.<br />
These results show that Met protein levels are increased in the majority of breast cancer cases, but that the protein levels are<br />
highest in the more aggressive basal subtypes. Therefore, Met can be a novel therapeutic target for those patients with the<br />
most aggressive tumors and, currently, the fewest therapeutic options.<br />
60
VARI | <strong>2008</strong><br />
Noninvasive imaging of glioblastoma progression in a novel mouse model<br />
One major deficiency of the existing glioblastoma tumor cell lines used in mouse orthotopic models is in their lack of invasiveness.<br />
We have determined that the invasive phenotype of human glioblastoma cells is greatly enhanced in cells that develop<br />
extensive metastatic foci in the lungs, skeletal muscle, and lymph nodes after tail vein injection. Importantly, all individual<br />
infiltrative cells express Met, indicating that Met would be an effective target for inhibiting glioblastoma growth and invasion.<br />
One of the cell lines, when inoculated orthotopically, displays extensive infiltrative growth into normal mouse brain tissue. The<br />
brain tumor growth generates necrosis with pseudopalisades and closely resembles malignant glioblastoma in humans. In this<br />
model, osteolysis occurs at the inoculation site and, as a result, the tumor grows both intra- and extracranially. This growth<br />
pattern provides a transcranial acoustic window, allowing observation of tumor growth and vascularization with high resolution<br />
micro-ultrasound. Such observation allows real time monitoring of orthotopic brain tumor growth, for assessing intracranial<br />
tumor vascularity and for evaluating the therapeutic efficacy of antitumor agents. We determined that increases in the opening<br />
of the skull are proportional to tumor growth, and therefore ultrasound provides a surrogate measurement of tumor growth.<br />
With this cell line, we can measure tumor growth orthotopically in the brain, subcutaneously as tumor xenografts, and as<br />
metastatic growth in experimental lung metastases assays. We have shown that an anti-HSP90 drug, the geldanamycin<br />
derivative 17-(allylamino)-17-demethoxygeldanamycin (17AAG), inhibits tumor growth in all three model systems.<br />
The role of Mig-6 in Met signaling and tumor suppression<br />
Mig-6 is one of several feedback regulators that we have found is rapidly induced by HGF/SF-Met signaling, as well as by other<br />
receptor tyrosine kinases such as EGFR. Mig-6 is a scaffolding adaptor protein that upon induction can negatively regulate<br />
EGFR and Met signaling. Mig-6 is located on human chromosome 1p36, a locus that is frequently associated with many<br />
human cancers. We have discovered that Mig-6 may function as a tumor suppressor, because mutations in the MIG-6 gene<br />
have been observed in human lung cancers, and disruption of Mig-6 in mice leads to lung, gallbladder, and bile duct cancers.<br />
Mig-6 may also play an important role in stress response and tissue homeostasis, as mice having a Mig-6 deficiency develop<br />
degenerative joint diseases that might be triggered by mechanical joint stress. We are currently investigating how Mig-6<br />
regulates EGFR and Met signal transduction and what role Mig-6 may play in the development and progression of cancer and<br />
of degenerative joint disease.<br />
External Collaborators<br />
Donald Bottaro and Benedetta Peruzzi, National Cancer Institute, Bethesda, Maryland<br />
Sandra Cottingham, Spectrum Health Hospitals, Grand Rapids, Michigan<br />
Francesco DeMayo, Baylor College of Medicine, Houston, Texas<br />
Ermanno Gherardi, MRC Center, Cambridge, England<br />
Sherri Davies and Matthew Ellis, Washington University, St. Louis, Missouri<br />
Beatrice Knudsen, Fred Hutchinson Cancer Research Center, Seattle, Washington<br />
Ernest Lengyel and Ravi Salgia, University of Chicago, Illinois<br />
Patricia LoRusso, Karmanos Cancer Institute, Detroit, Michigan<br />
Alnawaz Rehemtulla, Brian Ross, and Richard Simon, University of Michigan, Ann Arbor<br />
Ilan Tsarfaty, Tel Aviv University, Israel<br />
Robert Wondergem, East Tennessee State University, Johnson City<br />
61
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
From left, back row: Graveel, DeGroot, Haak, Vande Woude, Gao, Staal, Kaufman, Essenburg, Zhang<br />
front row: Kang, Nelson, Su, Xie, Berens, Thompson<br />
Recent Publications<br />
Knudsen, B., and G.F. Vande Woude. In press. Showering c-Met-dependent cancers with drugs. Current Opinion in<br />
Genetics and Development.<br />
Rouleau, Cecile, Krishna Menon, Paula Boutin, Cheryl Guyre, Hitoshi Yoshida, Shiro Kataoka, Michael Perricone,<br />
Srinivas Shankara, Arthur E. Frankel, Nicholas S. Duesbery, George F. Vande Woude, Hans-Peter Biemann, and<br />
Beverly A. Teicher. <strong>2008</strong>. The systemic administration of lethal toxin achieves a growth delay of human melanoma and<br />
neuroblastoma xenografts: assessment of receptor contribution. International Journal of Oncology 32(4): 739–748.<br />
Zhao, Ping, Tessa Grabinski, Chongfeng Gao, R. Scot Skinner, Troy Giambernardi, Yanli Su, Eric Hudson, James Resau,<br />
Milton Gross, George F. Vande Woude, Rick Hay, and Brian Cao. 2007. Identification of a Met-binding peptide from a<br />
phage display library. Clinical Cancer Research 13(20): 6049–6055.<br />
Zhang, Yu-Wen, and George F. Vande Woude. 2007. Mig-6, signal transduction, stress response and cancer. Cell Cycle<br />
6(5): 507–513.<br />
Tolbert, W. David, Jennifer Daugherty, Chongfeng Gao, Qian Xie, Cindy Miranti, Ermanno Gherardi, George Vande<br />
Woude, and H. Eric Xu. 2007. A mechanistic basis for converting a receptor tyrosine kinase agonist to an antagonist.<br />
Proceedings of the National Academy of Sciences U.S.A. 104(37): 14592–14597.<br />
Lindemann, K., J. Resau, J. Nährig, E. Kort, B. Leeser, K. Anneke, A. Welk, J. Schäfer, G. F. Vande Woude, E. Lengyel,<br />
and N. Harbeck. 2007. Differential expression of c-Met, its ligand HGF/SF and HER2/neu in DCIS and adjacent normal<br />
breast tissue. Histopathology 51(1): 54–62.<br />
Gao, ChongFeng, Kyle Furge, Julie Koeman, Karl Dykema, Yanli Su, Mary Lou Cutler, Adam Werts, Pete Haak, and<br />
George F. Vande Woude. 2007. Chromosome instability, chromosome transcriptome, and clonal evolution of tumor cell<br />
populations. Proceedings of the National Academy of Sciences U.S.A. 104(21): 8995–9000.<br />
62
VARI | <strong>2008</strong><br />
Craig P. Webb, Ph.D.<br />
Program for Translational Medicine<br />
Laboratory of Tumor Metastasis and Angiogenesis<br />
Dr. Webb received his Ph.D. in cell biology from the University of East Anglia, England, in 1995. He<br />
then served as a postdoctoral fellow in the laboratory of George Vande Woude in the Molecular<br />
Oncology Section of the Advanced BioScience Laboratories–Basic Research Program at the National<br />
Cancer Institute, Frederick Cancer Research and Development Center, Maryland (1995–1999). Dr.<br />
Webb joined VARI as a <strong>Scientific</strong> Investigator in October 1999; he now also oversees the Program<br />
for Translational Medicine.<br />
Staff<br />
Visiting Scentists<br />
Visiting Scientists<br />
Students<br />
David Cherba, Ph.D.<br />
Jessica Hessler, Ph.D.<br />
Jeremy Miller, Ph.D.<br />
David Monsma, Ph.D.<br />
Emily Eugster, M.S.<br />
Sujata Srikanth, M.Phil.<br />
Dawna Dylewski, B.S.<br />
Brian Hillary, B.A.<br />
Marcy Ross, B.S.<br />
Stephanie Scott, B.S.<br />
Danielle Welch, B.S.<br />
Katherine Koehler<br />
Richard Leach, M.D.<br />
David Reinhold, Ph.D.<br />
Molly Dobb<br />
Hailey Hines<br />
Catherine Perrin<br />
James Smith, Jr.<br />
63
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Research Interests<br />
Molecular biomarkers are widely expected to revolutionize the current trial-and-error practice of medicine by enabling a more<br />
predictive discipline in which therapies target the molecular constitution of individual patients and their disease. This concept is<br />
often termed “personalized medicine”. Biomarkers are being widely evaluated for their ability to assess disease risk, detect and<br />
monitor disease over time, accurately identify disease stage, approximate prognosis, and predict optimal targeted treatments.<br />
The Program for Translational Medicine was launched in 2006 to extend the Institute’s translational research capabilities, with<br />
a focus on the development of molecular biomarker strategies with clinical implications. The program’s activities have focused<br />
on building the critical translational infrastructure and technologies, the fostering of clinical and industrial partnerships, and<br />
the coordination of the multidisciplinary project teams required to implement molecular-based approaches in medicine. The<br />
Program of Translational Medicine, with its multidisciplinary partners, strives to create an efficient pipeline between the clinic and<br />
the research laboratory for efficient discovery and clinical application of novel biomarker strategies. We also work to increase<br />
the readiness of the community to implement advances in molecular medicine, benefiting human health and promoting West<br />
Michigan as a leader in biomarker research.<br />
Translational informatics<br />
To accelerate the implementation of personalized medicine, the consolidation and real-time analysis of standardized molecular<br />
and clinical/preclinical data is critical. Thus, much of our effort over the past several years has focused on the development of<br />
an integrated informatics solution known as the XenoBase BioIntegration Suite (XB-BIS; see http://xbtransmed.com). XB-BIS<br />
supports essential features of data management, data analysis, knowledge management, and reporting within an integrated<br />
framework, enabling the efficient exchange of information between the basic research laboratory and the clinic (Figure 1).<br />
XB-BIS has recently been licensed to industrial and academic partners with an interest in biomarker research, drug development,<br />
and the development of molecular-based diagnostics.<br />
Figure 1<br />
Figure 1. The XenoBase BioIntegration<br />
Suite (XB-BIS). The suite serves as a portal<br />
and common interface for consolidating<br />
clinical, preclinical, and molecular data, and<br />
it incorporates analytical, visualization, and<br />
reporting tools, which have historically been<br />
used in isolation. XB-BIS allows for the<br />
bidirectional flow of real-time data,<br />
information, and extracted knowledge<br />
between the multiple clinical and laboratory<br />
research components of a translational<br />
project.<br />
64
VARI | <strong>2008</strong><br />
Community partnerships<br />
Productive partnerships are pivotal to our efforts in biomarker research and personalized medicine. In the Center for<br />
Molecular Medicine (CMM, http://www.commex.org), the Van Andel Institute and Spectrum Health Hospitals have created a<br />
CLIA-certified/CAP-accredited clinical diagnostics laboratory for biomarker qualification and the development of associated<br />
diagnostic assays. CMM offers cutting-edge molecular diagnostic tests, and also performs fee-for-service genomics and<br />
proteomics work for commercial firms. Under Dr. Daniel Farkas, a national leader in molecular diagnostics, CMM provides<br />
access to molecular technologies of today that will become central to our personalized medicine initiatives in the future.<br />
ClinXus (http://www.clinxus.org) was developed to coordinate the West Michigan translational research enterprise. ClinXus<br />
was awarded a Michigan 21st Century Jobs Fund grant to support early-stage development and operations, and it was recently<br />
recognized for its efforts to develop biomarker strategies in translational studies by membership in the Predictive Safety and<br />
Testing Consortium (PSTC) of the Critical Path Institute. The PSTC brings pharmaceutical companies together to share and<br />
validate each other’s safety testing methods under advisement of the FDA and the European Medicines Agency. Membership<br />
in this prestigious consortium will help ensure that West Michigan remains at the forefront of biomarker research and development<br />
and will further the community’s rapidly emerging life sciences and healthcare industry.<br />
Predictive therapeutics protocol<br />
Translational research represents the interface where hypotheses advance to studies that ultimately provide definitive information<br />
for a clinical decision. A fundamental challenge in clinical cancer research remains how to make best use of current<br />
biomarker technologies, advances in computational biology, the expanding pharmacopeia, and a rapidly expanding knowledge<br />
of disease networks to deliver targeted treatments to cancer patients with optimal therapeutic index. Our research is focused<br />
on developing, testing, and refining biomarker-driven analytical methods to systematically predict combinations of drugs that<br />
target the perturbed molecular systems within a tumor. We have also begun to consider means by which such information<br />
should be conveyed to the treating physician in support of medical decision-making.<br />
We recently completed a feasibility study of 50 late-stage pediatric and adult cancer patients: tumor-derived gene expression<br />
profiles were analyzed to identify potential drugs to target perturbed molecular components of each patient’s specific tumor.<br />
With patient consent, tumor biopsies are collected, qualified by pathology, and processed within the CMM to generate a<br />
standardized gene expression profile for the tumor. These molecular data are uploaded into XB-BIS along with pertinent clinical<br />
data, and these are compared with other patient samples. Deregulated patterns of gene expression are identified and analyzed<br />
within XB-BIS to identify drugs that have predicted efficacy based upon the genomic data. A report scoring a series of drugs<br />
for predicted efficacy is generated within XB-BIS, and this is conveyed to the treating physician in an actionable and electronic<br />
format for consideration in treatment planning. The process from patient consent to molecular report must be completed in 10<br />
days, which provides significant workflow challenges. In parallel, a series of tumor grafts is established in immune-compromised<br />
mice, and these appear to closely resemble the human disease at the phenotypic and genotypic level. This resource is being<br />
used to test biomarker-driven predictive models (and the identified drugs) in a more systematic fashion and to evaluate novel<br />
targeted agents in partnership with industrial sponsors. Over the long term, the treatments are captured within XB-BIS together<br />
with critical outcome variables, allowing the predictive analytical methods to be refined and optimized.<br />
Anecdotal signs of success in a handful of patients have provided the impetus to launch a follow-up study with an expanded<br />
population of 220 patients and a more rigorous statistical design. In conjunction with our laboratory efforts to isolate, characterize,<br />
and target the putative cancer stem-cell subpopulation of metastatic tumors, biomarker-driven approaches that identify a<br />
rational treatment regimen targeting the molecular composition of the patient’s tumor hold promise for the future treatment of<br />
metastatic and refractory malignancies.<br />
65
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
From left: Koehler, Eugster, Miller, Webb, Monsma, Ross, Srikanth, Hines, Cherba, Scott, Dylewski<br />
External Collaborators<br />
Academic Surgical Associates, Advanced Radiology Services, Cancer & Hematology Centers of Western Michigan, P.C.,<br />
DeVos Children’s Hospital, Digestive Disease Institute, Grand Valley Medical Specialists, Grand Valley State University,<br />
MMPC, Saint Mary’s Health Care, Spectrum Health, and West Michigan Heart, all of Grand Rapids, Michigan<br />
Barbara Ann Karmanos Institute, and Henry Ford Hospital, Detroit, Michigan<br />
GeneGo, Inc., and Oncology Care Associates, St. Joseph, Michigan<br />
Jasper Clinical Research & Development, Inc. and ProNAi Therapeutics, Kalamazoo, Michigan<br />
Johns Hopkins University, Baltimore, Maryland<br />
M.D. Anderson Cancer Center, Houston, Texas<br />
Mary Crowley Cancer Center, Dallas, Texas<br />
Michigan State University, East Lansing, Michigan<br />
New York University, New York City<br />
Pfizer (Ann Arbor, Michigan; Saint Louis, Missouri; Groton, Connecticut)<br />
Schering-Plough Research Institute, New Jersey<br />
TGEN, Phoenix, Arizona<br />
University of Michigan, Ann Arbor<br />
University of California, San Francisco<br />
Recent Publications<br />
Cherba, D., and C.P. Webb. In press. Systems biology of personalized medicine. In Bioinformatics for Systems Biology, second<br />
ed., Stephen Krawetz, ed. Humana Press.<br />
Littman, B., J. Thompson, and C.P. Webb. In press. Where are we heading/What do we really need? In Biomarkers in Drug<br />
Development, Michael Bleavins, Ramin Rahbari, Malle Jurima-Romet, and Claudio Carini, eds. New York: Wiley.<br />
Webb, C.P. In press. Personalized medicine: the need for system integration in the design of targeted therapies. In Computational<br />
and Systems Biology: Applications and Methods, Richard Mazzarella, ed.<br />
66
VARI | <strong>2008</strong><br />
Differentiating prostate epithelial cells<br />
Prostate epithelial cells (PECs) were treated with keratinocyte growth factor and dihydrotestosterone to induce differentiation. PECs are positive<br />
for integrin beta 1 (green) and laminin 5 (red), while differentiated cells are negative for both. Nuclei were stained with Hoechst (blue). By forcing<br />
the cells to differentiate, cells that cannot be isolated for cell culture under normal conditions can be studied, allowing for improved understanding<br />
of normal prostate biology. Photo by Laura Lamb of the Miranti lab.<br />
67
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Michael Weinreich, Ph.D.<br />
Laboratory of Chromosome Replication<br />
Dr. Weinreich received his Ph.D. in biochemistry from the University of Wisconsin–Madison in 1993. He<br />
then was a postdoctoral fellow in the laboratory of Bruce Stillman, Director of the Cold Spring Harbor<br />
Laboratory, New York, from 1993 to 2000. Dr. Weinreich joined VARI as a <strong>Scientific</strong> Investigator in<br />
March 2000.<br />
Staff<br />
Dorine Savreux, Ph.D.<br />
FuJung Chang, M.S.<br />
Carrie Gabrielse, B.S.<br />
68<br />
Students<br />
Ying-Chou Chen, M.S.<br />
Charles Miller, B.S.<br />
Anthony Gaca<br />
Christina Gourlay<br />
Louise Haste<br />
Christina Untersperger
VARI | <strong>2008</strong><br />
Research Interests<br />
We are studying how cells accurately replicate their DNA, a process that begins at specific DNA sequences termed replication<br />
origins. Various genome-wide approaches have identified from 320 to 420 possible replication origins in budding yeast,<br />
the model organism we study. In G1 phase, each origin assembles approximately 40 polypeptides in a temporally defined<br />
order, culminating in the initiation of DNA replication at the G1/S phase boundary. The first stage of this process is called<br />
pre-replicative complex assembly and requires the origin recognition complex (ORC), Cdc6p, and Cdt1p. ORC directly binds<br />
to DNA and then recruits Cdt1p and Cdc6p during early G1 phase. These three proteins cooperate to load the MCM DNA<br />
helicase at origins in an ATP-dependent reaction. Cyclin-dependent kinases and the Cdc7p-Dbf4p kinase then catalyze<br />
the association of additional proteins with the MCM helicase, ultimately causing the initiation of bi-directional DNA synthesis<br />
(Figure 1). In our lab we are studying how Cdc6p-ATP functions to load the MCM helicase within a chromatin context in<br />
budding yeast. We also are studying the Cdc7p-Dbf4p kinase in both yeast and human cells.<br />
We previously discovered that deletion of SIR2, encoding a histone deacetylase, rescued the temperature sensitivity of several<br />
mutants that were defective in pre-RC assembly, including a cdc6-4 mutant. We screened the replication origins on chromosomes<br />
III and VI to identify those origins that were inhibited by SIR2 and identified five SIR2-sensitive origins: ARS305, ARS315,<br />
ARS317, ARS603, and ARS606. We determined the detailed structure of two origins on chromosome III and found that these<br />
origins contain inhibitory elements distal to the ORC binding site. By utilizing data from another group that mapped stably<br />
positioned nucleosomes on chromosome III, we found that these inhibitory elements were positioned within stably bound nucleosomes.<br />
Furthermore, the positioned nucleosomes were very close to or overlapping the site of pre-RC assembly. Origins<br />
that were not inhibited by SIR2 did not have nearby nucleosomes in this region. Since genetically, SIR2 inhibited origins through<br />
the inhibitory element, we suggest that the acetylation state of this nucleosome affects pre-RC assembly. We do not know<br />
whether Sir2p is acting directly at these inhibitory sites or indirectly by regulating another gene, but we put forth the following<br />
model to explain our findings (Figure 2). Because pre-RC assembly occurs on naked DNA and because nucleosomes within<br />
the origin inhibit pre-RC assembly, some origins may exist within a nucleosome environment that is not optimal for pre-RC<br />
assembly. In those cases, either a particular modification of a nearby nucleosome or a protein that binds to the nucleosome<br />
in a SIR2-dependent manner inhibits pre-RC assembly. Since Sir2p was previously thought to only act at very specific heterochromatic<br />
regions in the genome, we are interested to discover exactly how Sir2p acts at these euchromatic sites.<br />
Figure 1<br />
Figure 1. The stages of replication initiation. In the first stage, a multi-subunit complex called the prereplicative<br />
complex (pre-RC) is assembled at replication origins. This complex consists of ORC, Cdt1p, Cdc6p,<br />
and the MCM helicase. In the second stage, Cdc7p-Dbf4p and Cdk kinases activate the MCM helicase,<br />
resulting in origin unwinding and the association of DNA polymerases at the origin.<br />
69
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Figure 2<br />
Figure 2. Model for SIR2-<br />
mediated inhibition of DNA<br />
replication. A) Schematic of the<br />
ARS315 element that contains an<br />
inhibitory sequence element (I S )<br />
downstream of the site for pre-RC<br />
assembly. B) The I S element<br />
positions a nucleosome close to<br />
B2, which is inhibitory for pre-RC<br />
assembly. Deletion of SIR2 or<br />
mutation of the I S element allows<br />
repositioning of the nucleosome to<br />
allow pre-RC assembly.<br />
Cdc7p-Dbf4p is a two-subunit protein kinase required for initiating DNA replication after MCM helicase loading. The Cdc7p<br />
kinase subunit binds Dbf4p, which activates its kinase activity. Although Cdc7p-Dbf4p is required to promote DNA replication,<br />
it also has an undefined role in the repair of certain DNA lesions. In order to define the amino acids required for its roles in DNA<br />
replication and repair, we are analyzing Dbf4p using a mutational approach. We found that the Dbf4p N-terminus is dispensable<br />
for DNA replication, but it encodes functions that participate in the repair of DNA lesions and the firing of late-replication origins.<br />
An N-terminal BRCT-like motif may mediate these activities. It is also possible that Dbf4p maintains replication fork stability by<br />
targeting Cdc7p kinase to stalled replication forks. Interestingly, these are separable activities from Dbf4p’s essential role in<br />
promoting initiation of DNA replication. In addition, we have identified two regions within Dbf4p—a C-terminal Zn-finger motif<br />
and a separate region—that mediate binding to and activation of the Cdc7p kinase. The C-terminal region is also not essential<br />
for Dbf4p activity, but loss of this region dramatically lowers Cdc7p kinase activity.<br />
We also are studying the human Cdc7-Dbf4 protein kinase. We previously raised monoclonal antibodies that recognize both<br />
human subunits and used these to screen human cancer cell lines and primary human tumors for HsCdc7-Dbf4 abundance.<br />
Although both subunits are expressed at very low levels in normal cycling cells (and are perhaps absent in post-mitotic cells),<br />
they are up-regulated in a substantial number of tumor cell lines. HsCdc7 protein is also highly expressed in some primary<br />
breast and colon tumors. By screening expression data from a panel of more than 650 primary human tumors, we also found<br />
that CDC7 and DBF4 mRNA expression are coordinately up-regulated in many tumors of diverse origin. Similarly, we screened<br />
several primary tumors and tumor cell lines for gene copy changes in CDC7 and DBF4. We found that the DBF4 gene copy<br />
number is often elevated in those cells expressing higher levels of Cdc7-Dbf4 kinase.<br />
Because HsCdc7 is an essential kinase for DNA replication, its increased expression level in some tumors and tumor cell<br />
lines may reflect higher rates of cellular proliferation. However, we find no correlation between doubling time and Cdc7-Dbf4<br />
expression in the NCI60 tumor cell lines. Furthermore, several published studies suggest that increased Cdc7-Dbf4 expression<br />
can inhibit the growth of rodent cell lines but has no effect on the growth of human cells. We suggest that since HsCdc7-Dbf4<br />
is likely involved in other aspects of chromosome metabolism (e.g., DNA repair) and functions in the S-phase checkpoint, its<br />
increased expression in some tumor cell lines may offer an advantage for handling the chromosome instability that occurs in<br />
many human tumors. Our aim is to understand the mechanism(s) that allow increased expression of Cdc7-Dbf4 kinase in<br />
tumor cells and to investigate its phenotypic effects.<br />
70
VARI | <strong>2008</strong><br />
From left: Savreux, Gabrielse, Chang, Miller, Chen, Weinreich<br />
External Collaborators<br />
Angelika Amon, Massachusetts Institute of Technology, Cambridge<br />
Catherine Fox, University of Wisconsin–Madison<br />
Carol Newlon, University of Medicine and Dentistry of New Jersey, Newark<br />
Alain Verreault, University of Montreal, Quebec, Canada<br />
Recent Publications<br />
Crampton, Amber, FuJung Chang, Donald L. Pappas, Jr., Ryan L. Frisch, and Michael Weinreich. <strong>2008</strong>. An ARS element<br />
inhibits DNA replication through a SIR2-dependent mechanism. Molecular Cell 30(2): 156–166.<br />
71
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Bart O. Williams, Ph.D.<br />
Laboratory of Cell Signaling and Carcinogenesis<br />
Dr. Williams received his Ph.D. in biology from Massachusetts Institute of Technology in 1996. For<br />
three years, he was a postdoctoral fellow at the National Institutes of Health in the laboratory of Harold<br />
Varmus, former Director of NIH. Dr. Williams joined VARI as a <strong>Scientific</strong> Investigator in July 1999 and<br />
was promoted to Senior <strong>Scientific</strong> Investigator in 2006.<br />
Staff<br />
Charlotta Lindvall, M.D., Ph.D.<br />
Kyle VanKoevering, B.S.<br />
Cassandra Zylstra, B.S.<br />
Students<br />
Tristan Kempston<br />
Audrey Sanders<br />
Brent Vanderhart, B.S.<br />
72
VARI | <strong>2008</strong><br />
Research Interests<br />
Our laboratory is interested in understanding how alterations in the Wnt signaling pathway cause human disease. Specifically, we<br />
have focused our efforts on the functions of the Wnt co-receptors, Lrp5 and Lrp6. Wnt signaling is an evolutionarily conserved<br />
process that functions in the differentiation of most tissues within the body. Given its central role in growth and differentiation, it<br />
is not surprising that alterations in the pathway are among the most common events associated with human cancer. In addition,<br />
several other human diseases, including osteoporosis, have been linked to altered regulation of this pathway.<br />
We also work on understanding the role of Wnt signaling in bone formation. Our interest is not only from the perspective of<br />
normal bone development, but also in trying to understand whether aberrant Wnt signaling plays a role in the predisposition of<br />
some common tumor types (for example, prostate, breast, lung, and renal tumors) to metastasize to and grow in bone. The<br />
long-term goal of this work is to provide insights useful in developing strategies to lessen the morbidity and mortality associated<br />
with skeletal metastasis.<br />
Wnt signaling in normal bone development<br />
Mutations in the Wnt receptor Lrp5 have been causally linked to alterations in human bone development. We have characterized<br />
a mouse strain deficient for Lrp5 and shown that it recapitulates the low-bone-density phenotype seen in human patients<br />
deficient for Lrp5. We have further shown that mice carrying mutations in both Lrp5 and the related Lrp6 protein have even<br />
more-severe defects in bone density.<br />
To test whether Lrp5 deficiency causes changes in bone density due to aberrant signaling through b-catenin, we created mice<br />
carrying an osteoblast-specific deletion of b-catenin (OC-cre;b-catenin-flox/flox mice). In collaboration with Tom Clemens of<br />
the University of Alabama at Birmingham, we found that alterations of Wnt/b-catenin signaling in osteoblasts lead to changes<br />
in the expression of RANKL and osteoprotegerin (OPG). Consistent with this, histomorphometric evaluation of bone in the mice<br />
with osteoblast-specific deletions of either Apc or b-catenin revealed significant alterations in osteoclastogenesis.<br />
We are addressing how other genetic alterations linked to Wnt/b-catenin signaling affect bone development and osteoblast<br />
function. We have generated mice with conditional alleles of Lrp6 and Lrp5 that can be inactivated via cre-mediated recombination,<br />
and we will assess the roles of these genes at different stages of osteoblast differentiation. Finally, we are<br />
working to determine what other signaling pathways may impinge on b-catenin signaling to control osteoblast differentiation<br />
and function.<br />
Wnt signaling in mammary development and cancer<br />
We are also addressing the relative roles of Lrp5 and Lrp6 in Wnt1-induced mammary carcinogenesis. A deficiency in Lrp5<br />
dramatically inhibits the development of mammary tumors, and a germline deficiency for Lrp5 or Lrp6 results in delayed<br />
mammary development. Because Lrp5-deficient mice are viable and fertile, we have focused our initial efforts on these mice.<br />
In collaboration with Caroline Alexander’s laboratory, we have found dramatic reductions in the number of mammary progenitor<br />
cells in these mice, and we are examining the mechanisms underlying this reduction. We have also found that Lrp6 plays a key<br />
role in mammary development, and we are focusing on the mechanisms underlying this unique role. Finally, we are defining<br />
the relative roles of b-catenin and mTOR signaling in the initiation and progression of Wnt1-induced mammary tumors. We are<br />
particularly interested in the role(s) of these pathways in regulating the proliferation of normal mammary progenitor cells, as well<br />
as of tumor-initiating cells.<br />
73
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Wnt signaling in metabolic syndrome<br />
Several studies have linked mutations in Lrp5 and/or Lrp6 to the development of diabetes, dyslipedemias, and hypertension in<br />
humans and mice. We are exploring the roles of these genes in this context by creating mice carrying conditional deletions in<br />
hepatocytes or in adipocytes and evaluating their phenotypes.<br />
Wnt signaling in prostate development and cancer<br />
Two hallmarks of advanced prostate cancer are the development of skeletal osteoblastic metastasis and the ability of the tumor<br />
cells to become independent of androgen for survival. The association of Wnt signaling with bone growth, plus the fact that<br />
b-catenin can bind to the androgen receptor and make it more susceptible to activation with steroid hormones other than DHT,<br />
make Wnt signaling an attractive candidate for explaining some phenotypes associated with advanced prostate cancer. We<br />
have created mice with a prostate-specific deletion of the Apc gene. These mice develop fully penetrant prostate hyperplasia<br />
by four months of age, and these tumors progress to frank carcinomas by seven months. We have found that these tumors<br />
initially regress under androgen ablation but show signs of androgen-independent growth some months later.<br />
General mechanisms of Wnt signaling<br />
There are many levels of regulating the reception of Wnt signals. The completion of the Human Genome Project has shown<br />
that there are 19 different genes encoding Wnt proteins, 9 encoding Frizzled proteins, and the genes encoding Lrp5 and Lrp6.<br />
In addition, there are several proteins that can inhibit Wnt signaling by binding to components of the receptor complex and<br />
interfering with normal signaling, including the Dickkopfs (Dkks) and the Frizzled-related proteins (FRPs). One of the long-term<br />
goals of our laboratory is to understand how specificity is generated for the different signaling pathways, with a specific focus<br />
on understanding the molecular functions of Lrp5 and Lrp6.<br />
VARI mutant mouse repository<br />
With support from the Institute, our laboratory maintains a repository of mutant mouse strains to support the general development<br />
of animal models of human disease. We distribute these strains at a nominal cost to interested laboratories.<br />
From left: Vanderhart, Zylstra, Sanders, Lindvall, Williams, VanKoevering<br />
74
VARI | <strong>2008</strong><br />
External Collaborators<br />
Bone development<br />
Mary Bouxsein, Beth Israel Deaconness Medical Center, Boston, Massachusetts<br />
Thomas Clemens, University of Alabama–Birmingham<br />
David Ornitz and Fanxin Long, Washington University, St. Louis, Missouri<br />
Matthew Warman, Harvard University, Boston, Massachusetts<br />
Prostate cancer<br />
Wade Bushman and Ruth Sullivan, University of Wisconsin–Madison<br />
Mammary development<br />
Caroline Alexander, University of Wisconsin–Madison<br />
Yi Li, Baylor Breast Center, Houston, Texas<br />
Mechanisms of Wnt signaling<br />
Kathleen Cho, University of Michigan, Ann Arbor<br />
Kang-Yell Choi, Yansei University, Seoul, South Korea<br />
Eric Fearon, University of Michigan, Ann Arbor<br />
Silvio Gutkind, National Institute of Dental and Craniofacial Research, Bethesda, Maryland<br />
Kun-Liang Guan, University of California, San Diego<br />
Malathy Shekhar, Wayne State University, Detroit, Michigan<br />
Aaron Zorn, University of Cincinnati<br />
Recent Publications<br />
Robinson, D.R., C.R. Zylstra, and B.O. Williams. In press. Wnt signaling and prostate cancer. Current Drug Targets.<br />
Shekhar, Malathy P.V., Brigitte Gerard, Robert J. Pauley, Bart O. Williams, and Larry Tait. <strong>2008</strong>. Rad6B is a positive regulator of<br />
b-catenin stabilization. Cancer Research 68(6): 1741–1750.<br />
Wang, Pengfei, Michael R. Bowl, Stephanie Bender, Jun Peng, Leslie Farber, Jindong Chen, Asif Ali, ZhongFa Zhang,<br />
Arthur S. Alberts, Rajesh V. Thakker, Ali Shilatifard, Bart O. Williams, and Bin Tean Teh. <strong>2008</strong>. Parafibromin, a component<br />
of the human PAF complex, regulates growth factors and is required for embryonic development and survival in adult mice.<br />
Molecular and Cellular Biology 28(9): 2930–2940.<br />
Hinoi, Takao, Aytekin Akyol, Brian K. Theisen, David O. Ferguson, Joel K. Greenson, Bart O. Williams, Kathleen R. Cho, and<br />
Eric R. Fearon. 2007. Mouse model of colonic adenoma-carcinoma progression based on somatic Apc inactivation. Cancer<br />
Research 67(20): 9721–9730.<br />
Lindvall, Charlotta, Wen Bu, Bart O. Williams, and Yi Li. 2007. Wnt signaling, stem cells, and the cellular origin of breast cancer.<br />
Stem Cell Reviews 3(2): 157–168.<br />
Wu, Rong, Neali Hendrix-Lucas, Rork Kuick, Yali Zhai, Donald R. Schwartz, Aytekin Akyol, Samir Hanash, David E. Misek, Hidetaka<br />
Katabuchi, Bart O. Williams, Eric R. Fearon, and Kathleen R. Cho. 2007. Mouse model of human ovarian endometroid adenocarcinoma<br />
based on somatic defects in the Wnt b-catenin and PI3K/Pten signaling pathways. Cancer Cell 11(4): 321–333.<br />
Young, John J., Jennifer L. Bromberg-White, Cassandra R. Zylstra, Joseph T. Church, Elissa Boguslawski, James H. Resau, Bart<br />
O. Williams, and Nicholas S. Duesbery. 2007. LRP5 and LRP6 are not required for protective antigen–mediated internalization<br />
or lethality of anthrax lethal toxin. PLoS Pathogens 3(3): e27.<br />
75
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
H. Eric Xu, Ph.D.<br />
Laboratory of Structural Sciences<br />
Dr. Xu went to Duke University and the University of Texas Southwestern Medical Center, where he<br />
earned his Ph.D. in molecular biology and biochemistry. Following a postdoctoral fellowship with Carl<br />
Pabo at MIT, he moved to GlaxoWellcome in 1996 as a research investigator of nuclear receptor drug<br />
discovery. Dr. Xu joined VARI as a Senior <strong>Scientific</strong> Investigator in July 2002 and was promoted to<br />
Distinguished <strong>Scientific</strong> Investigator in March 2007.<br />
Staff<br />
Students<br />
Visiting Scientist<br />
Abhishek Bandyopadhyay, Ph.D.<br />
Jiyuan Ke, Ph.D.<br />
Schoen Kruse, Ph.D.<br />
Raghu Malapaka, Ph.D.<br />
Karsten Melcher, Ph.D.<br />
Augie Pioszak, Ph.D.<br />
David Tolbert, Ph.D.<br />
Yong Xu, Ph.D.<br />
Chenghai Zhang, Ph.D.<br />
X. Edward Zhou, Ph.D.<br />
Jennifer Daugherty, B.S.<br />
Amanda Kovach, B.S.<br />
Naomi Parker, B.S.<br />
Kelly Powell, B.S.<br />
Cee Wah Chan<br />
Aoife Conneely<br />
Xiang Gao<br />
Mien Nguyen<br />
Rachel Talaski<br />
Peipei Zhong<br />
Ross Reynolds, Ph.D.<br />
76
VARI | <strong>2008</strong><br />
Research Interests<br />
Our laboratory uses multidisciplinary approaches to study the structures and functions of protein complexes that play key<br />
roles in major signaling pathways. Currently we are focusing on three families of proteins: nuclear hormone receptors, the Met<br />
tyrosine kinase receptor, and G protein–coupled receptors, because beyond their fundamental roles in biology, these proteins<br />
are important drug targets for many human diseases.<br />
Nuclear hormone receptors<br />
The nuclear hormone receptors form a large family comprising ligand-regulated and DNA-binding transcription factors. The<br />
family includes receptors for classic steroid hormones such as estrogen, progesterone, androgens, and glucocorticoids, as<br />
well as receptors for peroxisome proliferator activators, vitamin D, vitamin A, and thyroid hormones. These classic receptors<br />
are among the most successful targets in the history of drug discovery: every receptor has one or more cognate synthetic<br />
ligands being used as medicines. The nuclear receptors also include a class of “orphan” receptors for which no ligand has<br />
been identified. In the last several years, we have developed the following projects centering on the structural biology of<br />
nuclear receptors.<br />
Peroxisome proliferator–activated receptors<br />
The peroxisome proliferator–activated receptors (PPARa, d, and g) are key regulators of glucose and fatty acid homeostasis<br />
and as such are important therapeutic targets for treating cardiovascular disease, diabetes, and cancer.<br />
We have determined crystal structures of each PPAR’s ligand-binding domain (LBD) bound to diverse ligands<br />
including fatty acids, the lipid-lowering fibrate drugs, and a new generation of anti-diabetic drugs, the glitazones.<br />
We have also determined the crystal structures of these receptors bound to coactivators or co-repressors. We are<br />
developing approaches to the structures of large PPAR fragment/DNA complexes.<br />
Human glucocorticoid and mineralocorticoid receptors<br />
The human glucocorticoid receptor (GR) and mineralocorticoid receptor (MR) are classic steroid hormone<br />
receptors that are key to a wide spectrum of human physiology, including immune/inflammatory responses,<br />
metabolic homeostasis, and control of blood pressure. Both are well-established drug targets. GR ligands such<br />
as dexamethasone (Dex) and fluticasone propionate (FP) are used to treat asthma, leukemia, and autoimmune<br />
diseases; MR ligands such as spironolactone and eplerenone are used to treat hypertension and heart failure.<br />
The discovery of highly potent and more-selective ligands for GR and MR is an important goal of pharmaceutical<br />
research.<br />
We have determined a crystal structure of the GR LBD bound to dexamethasone and the MR LBD bound to<br />
corticosterone, both of which are in complex with a coactivator peptide motif. These structures provide a detailed<br />
basis for the specificity of hormone recognition and coactivator assembly by GR and MR. Currently we are<br />
studying receptor-ligand interactions by crystallizing GR and MR with various steroid or nonsteroid ligands. In<br />
collaboration with Brad Thompson and Raj Kumar at the University of Texas Medical Branch at Galveston, we are<br />
also extending our studies to the structure of a large GR fragment bound to DNA.<br />
77
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
The human androgen receptor<br />
The androgen receptor (AR) is the central molecule in the development and progression of prostate cancer, and<br />
as such it serves as the molecular target of anti-androgen therapy. However, most prostate cancer patients<br />
develop resistance to such therapy, mainly due to mutations in this hormone receptor that alter its three-dimensional<br />
structure and allow AR to escape repression. This hormone-independent cancer is highly aggressive and is<br />
responsible for most deaths from prostate cancer. In this project, we are aiming to determine the structures of<br />
mutated AR proteins that alter the response to anti-hormone therapy. In collaboration with Donald MacDonnell at<br />
Duke University, we are working on the crystal structure of the full-length AR/DNA complex.<br />
Orphan nuclear receptors<br />
We have focused on structural characterization of two orphan receptors: constitutive androstane receptor (CAR) and<br />
steroidogenic factor-1 (SF-1). The CAR structure reveals a compact LBD fold containing a small pocket that is only<br />
half the size of the pocket in PXR, a receptor closely related to CAR. The constitutive activity of CAR appears to be<br />
mediated by a novel linker helix between the C-terminal AF-2 helix and helix 10. On the other hand, SF-1 is regarded<br />
as a ligand-independent receptor, but its LBD structure reveals the presence of a phospholipid ligand in a surprisingly<br />
large pocket; more than twice the size of the pocket in the mouse LRH-1, a closely related receptor. The bound<br />
phospholipid is readily exchanged and modulates SF-1 interactions with coactivators. Mutations designed to reduce<br />
the size of the SF-1 pocket or to disrupt hydrogen bonds formed with the phospholipid abolish the SF-1/coactivator<br />
interactions and reduce SF-1 transcriptional activity. These findings establish that SF-1 is a ligand-dependent receptor<br />
and suggest an unexpected link between nuclear receptors and phospholipid signaling pathways.<br />
The Met tyrosine kinase receptor<br />
MET is a tyrosine kinase receptor that is activated by hepatocyte growth factor/scatter factor (HGF/SF). Aberrant activation of<br />
the MET receptor has been linked to the development and metastasis of many types of solid tumors and correlates with poor<br />
clinical prognosis. HGF/SF has a modular structure with an N-terminal domain, four kringle domains, and an inactive serine<br />
protease domain. The structure of the N-terminal domain with a single kringle domain (NK1) has been determined. Less is<br />
known about the structure of the MET extracellular domain; thus, the molecular basis of the MET receptor–HGF/SF interaction<br />
and the activation of MET signaling by this interaction remains poorly understood. In collaboration with George Vande Woude<br />
and Ermanno Gherardi, we are developing this project to solve the crystal structure of the MET receptor/HGF complex.<br />
G protein–coupled receptors<br />
G protein–coupled receptors (GPCRs) form the largest family of receptors in the human genome; they are receptors for diverse<br />
signals carried by photons, ions, small chemicals, peptides, and hormones. These receptors account for over 40% of drug<br />
targets, but the structure of these receptors remains a challenge because they are seven-transmembrane molecules. Currently,<br />
there is only one reported GPCR structure, for an inactive form of bovine rhodopsin. From our standpoint, GPCRs are similar<br />
to nuclear hormone receptors with respect to regulation by protein-ligand and protein-protein interactions. Due to their importance,<br />
we have decided to take on studies of the structural basis of ligand binding in, and activation of, GPCRs. Currently, we<br />
are focusing on hormone recognition by Class B GPCRs, and we have recently determined the first structure of parathyroid<br />
hormone bound to the extracellular domain of its receptor.<br />
78
VARI | <strong>2008</strong><br />
External Collaborators<br />
Doug Engel, University of Michigan, Ann Arbor<br />
Ermanno Gherardi, University of Cambridge, United Kingdom<br />
Steve Kliewer, University of Texas Southwestern Medical Center, Dallas<br />
David Mangelsdorf, University of Texas Southwestern Medical Center, Dallas<br />
Donald MacDonnell, Duke University, Durham, North Carolina<br />
Stoney Simmons, National Institutes of Health, Bethesda, Maryland<br />
Scott Thacher, Orphagen Pharmaceuticals, San Diego, California<br />
Brad Thompson and Raj Kumar, University of Texas Medical Branch at Galveston<br />
Ming-Jer Tsai, Baylor College of Medicine, Houston, Texas<br />
From left, standing: Kruse, Chan, Zhou, Pioszak, Bandyopadhyay, Zhang, Zhong, Ke, Malapaka, Y. Xu,<br />
Melcher, Tolbert;<br />
seated: Guthrey, Parker, Conneely, Kovach, Powell, H.E. Xu<br />
Recent Publications<br />
Pioszak, Augen A., and H. Eric Xu. <strong>2008</strong>. Molecular recognition of parathyroid hormone by its G protein-coupled receptor.<br />
Proceedings of the National Acadamy of Sciences U.S.A. 105(13): 5034–5039.<br />
Suino-Powell, Kelly, Yong Xu, Chenghai Zhang, Yong-guang Tao, W. David Tolbert, Stoney S. Simons, Jr., and H. Eric Xu. <strong>2008</strong>.<br />
Doubling the size of the glucocorticoid receptor ligand binding pocket by deacylcortivazol. Molecular and Cellular Biology<br />
28(6): 1915–1923.<br />
Guo, Dongsheng, Joy Sarkar, Kelly Suino-Powell, Yong Xu, Kojiro Matsumoto, Yuzhi Jia, Songtao Yu, Sonal Khare, Kasturi Haldar,<br />
M. Sambasiva Rao, Jennifer E. Foreman, Satdarshan P.S. Monga, Jeffrey M. Peters, H. Eric Xu, and Janardan K. Reddy. 2007.<br />
Induction of nuclear translocation of constituitive androstane receptor by peroxisome proliferator–activated receptor a synthetic<br />
ligands in mouse liver. Journal of Biological Chemistry 282(50): 36766–36776.<br />
Tolbert, W. David, Jennifer Daugherty, Chongfeng Gao, Qian Xie, Cindy Miranti, Ermanno Gherardi, George Vande Woude, and<br />
H. Eric Xu. 2007. A mechanistic basis for converting a receptor tyrosine kinase agonist to an antagonist. Proceedings of the<br />
National Academy of Sciences U.S.A. 104(37): 14592–14597.<br />
79
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Daniel Nathans Memorial Award<br />
80
VARI | <strong>2008</strong><br />
Daniel Nathans Memorial Award<br />
The Daniel Nathans Memorial Award was established in memory of Dr. Daniel Nathans, a distinguished member of our scientific<br />
community and a founding member of VARI’s Board of <strong>Scientific</strong> Advisors. We established this award to recognize individuals<br />
who emulate Dan and his contributions to biomedical and cancer research. It is our way of thanking and honoring him for his<br />
help and guidance in bringing Jay and Betty Van Andel’s dream to reality. The Daniel Nathans Memorial Award was announced<br />
at our inaugural symposium, “Cancer & Molecular Genetics in the Twenty-First Century”, in September 2000.<br />
Award Recipients<br />
2000 Richard D. Klausner, M.D.<br />
2001 Francis S. Collins, M.D., Ph.D.<br />
2002 Lawrence H. Einhorn, M.D.<br />
2003 Robert A. Weinberg, Ph.D.<br />
2004 Brian Druker, M.D.<br />
2005 Tony Hunter, Ph.D., and Tony Pawson, Ph.D.<br />
2006 Harald zur Hausen, M.D., and Douglas R. Lowy, M.D.<br />
Dr. Harald zur Hausen (left) and Dr. Douglas R. Lowy (right) with Dr. George Vande Woude, who<br />
presented the Nathans Awards.<br />
81
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Postdoctoral Fellowship Program<br />
82
VARI | <strong>2008</strong><br />
Postdoctoral Fellowship Program<br />
The Van Andel Research Institute provides postdoctoral training opportunities to Ph.D. scientists beginning their research careers.<br />
The fellowships help promising scientists advance their knowledge and research experience while at the same time supporting<br />
the research endeavors of VARI. The fellowships are funded in three ways: 1) by the laboratories to which the fellow is assigned;<br />
2) by the VARI Office of the Director; or 3) by outside agencies. Each fellow is assigned to a scientific investigator who oversees<br />
the progress and direction of research. Fellows who worked in VARI laboratories in 2007 and early <strong>2008</strong> are listed below.<br />
Abhishek Bandyopadhyay<br />
University of Cambridge, U.K.<br />
VARI mentor: Eric Xu<br />
Jennifer Bromberg-White<br />
Pennsylvania State University College of<br />
Medicine, Hershey<br />
VARI mentor: Nicholas Duesbery<br />
Philippe Depeille<br />
University of Montpellier, France<br />
VARI mentor: Nicholas Duesbery<br />
Yan Ding<br />
Peking Union Medical College, China<br />
VARI mentor: Nicholas Duesbery<br />
Kathryn Eisenmann<br />
University of Minnesota, Minneapolis<br />
VARI mentor: Arthur Alberts<br />
Leslie Farber<br />
George Washington University,<br />
Washington, D.C.<br />
VARI mentor: Bin Teh<br />
Quliang Gu<br />
Sun Yat-sen University of Medicine,<br />
Guangzhou, China<br />
VARI mentor: Brian Cao<br />
Carrie Graveel<br />
University of Wisconsin – Madison<br />
VARI mentor: George Vande Woude<br />
Jessica Hessler<br />
University of Michigan, Ann Arbor<br />
VARI mentor: Craig Webb<br />
Holly Holman<br />
University of Glasgow, U.K.<br />
VARI mentor: Arthur Alberts<br />
Dan Huang<br />
Peking Union Medical College, China<br />
VARI mentor: Bin Teh<br />
Schoen Kruse<br />
University of Colorado, Boulder<br />
VARI mentor: Eric Xu<br />
Yan Li<br />
Peking Union Medical College, China<br />
VARI mentor: Bin Teh<br />
Brendon Looyenga<br />
University of Michigan, Ann Arbor<br />
VARI mentor: James Resau<br />
Xu Lu<br />
University of Texas Health Sciences Center,<br />
San Antonio<br />
VARI mentor: Steven Triezenberg<br />
Venkata Malapaka<br />
Western Michigan University, Kalamazoo<br />
VARI mentor: Eric Xu<br />
Daisuke Matsuda<br />
Kitasato University, Japan<br />
VARI mentor: Bin Teh<br />
Augen Pioszak<br />
University of Michigan, Ann Arbor<br />
VARI mentor: Eric Xu<br />
Daniel Robinson<br />
University of California, Davis<br />
VARI mentor: Bart Williams<br />
Dorine Savreux<br />
Virology University, France<br />
VARI mentor: Michael Weinreich<br />
Peng Fei Wang<br />
Fourth Military Medical University,<br />
Shannxi, China<br />
VARI mentor: Bin Teh<br />
Yi-Mi Wu<br />
National Tsin-Hua University, Taiwan<br />
VARI mentor: Brian Haab<br />
Yong Xu<br />
Shanghai Institute of Materia Medica,<br />
China<br />
VARI mentor: Eric Xu<br />
Chenghai Zhang<br />
Virus Institute of the CDC, China<br />
VARI mentor: Eric Xu<br />
Xiaoyin Zhou<br />
University of Alabama – Birmingham<br />
VARI mentor: Eric Xu<br />
From left: Eisenmann, Kruse, Bromberg-White, Pioszak, Malapaka, Lu, Zhang, Looyenga, Xu<br />
83
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Student Programs<br />
84
VARI | <strong>2008</strong><br />
Grand Rapids Area Pre-College Engineering Program<br />
The Grand Rapids Area Pre-College Engineering Program (GRAPCEP) is administered by Davenport University and jointly<br />
sponsored and funded by Schering Plough and VARI. The program is designed to provide selected high school students,<br />
who have plans to major in science or genetic engineering in college, with the opportunity to work in a research laboratory. In<br />
addition to research methods, the students also learn workplace success skills such as teamwork and leadership. The four<br />
2007 GRAPCEP students were<br />
Bryan Mendez (Resau/Duesbery)<br />
Creston High School<br />
Tarrick Mussa (Resau/Duesbery)<br />
Creston High School<br />
Aleesa Schlientz (Resau/Duesbery)<br />
Creston High School<br />
Jennifer Vogal (Hay)<br />
Creston High School<br />
From left: Mussa, Schlientz, Vogal, Mendez<br />
85
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Summer Student Internship Program<br />
The VARI student internships were established to provide college students with an opportunity to work with professional researchers<br />
in their fields of interest, to use state-of-the-art equipment and technologies, and to learn valuable people and presentation<br />
skills. At the completion of the 10-week program, the students summarize their projects in an oral presentation.<br />
From January 2007 to March <strong>2008</strong>, VARI hosted 74 students from 22 colleges and universities in formal summer internships under<br />
the Frederik and Lena Meijer Student Internship Program and in other student positions during the year. An asterisk (*) indicates<br />
a Meijer student intern.<br />
Anderson University, Indiana<br />
James Smith, Jr. (Webb)<br />
Aquinas College, Grand Rapids, Michigan<br />
Elizabeth Block (Teh)<br />
Krysta Collins* (Haab)<br />
Christina Gourley (Weinreich)<br />
Sara Kunz* (Hay)<br />
Mien Nguyen* (Xu)<br />
Audrey Sanders (Williams)<br />
Randi VanOcker (Haab)<br />
Calvin College, Grand Rapids, Michigan<br />
Christopher Gorter* (Alberts)<br />
Lee Heeringa (Haab)<br />
Alysha Kett* (Vande Woude)<br />
Geoff Kraker (MacKeigan)<br />
Bill Wondergem (Teh)<br />
Central Michigan University, Mount Pleasant<br />
Lindsay Barnett (Teh)<br />
Sarah DeVos* (Triezenberg)<br />
Ferris State University, Big Rapids, Michigan<br />
Carrie Fiebig (Haab)<br />
Grand Rapids Community College, Michigan<br />
Wei Luo (Resau)<br />
Albert Rodriguez (Alberts)<br />
Grand Valley State University, Allendale, Michigan<br />
Alaa Abughoush (Hay)<br />
Erica Bechtel* (Miranti)<br />
Janell Carruthers (Resau)<br />
Molly Dobb (Webb)<br />
Eric Graf (Miranti)<br />
Craig Johnson (Furge)<br />
Tristan Kempston* (Williams)<br />
Kevin Maupin (Haab)<br />
Lisa Orcasitas (Duesbery)<br />
Gary Rajah (Miranti)<br />
Sara Ramirez (Resau)<br />
Kalamazoo College, Kalamazoo, Michigan<br />
Adam Granger (Haab)<br />
Marquette University, Milwaukee, Wisconsin<br />
Michael Avallone (Teh)<br />
McGill University, Montreal, Quebec, Canada<br />
Halley Crissman (Resau/MacKeigan)<br />
Michigan State University, East Lansing<br />
Heather Born (Resau)<br />
Ying-Chou Chen, M.S. (Weinreich)<br />
Michelle Dawes (Duesbery)<br />
Aaron DeWard, B.S. (Alberts)<br />
Anthony Gaca* (Weinreich)<br />
Pete Haak, B.S. (Resau)<br />
Sebla Kutluay, B.S. (Triezenberg)<br />
Laura Lamb, B.S. (Miranti)<br />
Chih-Shia Lee, M.S. (Duesbery)<br />
Charles Miller, B.S. (Weinreich)<br />
Katie Sian, B.S. (MacKeigan)<br />
Susan Spotts, B.S. (Miranti)<br />
Rachel Talaski (Xu)<br />
Jelani Zarif, M.S. (Miranti)<br />
Nanjing Medical University, China<br />
Guipeng Ding (Cao)<br />
Ning Xu (Cao)<br />
Aixia Zhang (Cao)<br />
Northern Illinois University, DeKalb<br />
Yarong Yang (Resau)<br />
Spring Arbor University, Michigan<br />
Jenna Manby* (Cao)<br />
Sun Yat-sen University, Guangzhou, China<br />
Rui Sun (Cao)<br />
86
VARI | <strong>2008</strong><br />
Kneeling, left to right: Church, Smith, Gaca, Kempston, Gorter, Koelzer, Buzzitta, Devos<br />
Standing, left to right: Crissman, Firestone, Manby, Dawes, Hines, Avallone, Born, Kunz, Wilcox, Burgenske, Bechtel, Block, Barnett,<br />
VanKoevering, Nguyen, Gao, Talaski, McElliott, Herman<br />
University of Bath, United Kingdom<br />
Naomi Asantewa-Sechereh (Duesbery)<br />
Cee Wah Chen (Xu)<br />
Aoife Conneely (Xu)<br />
Louise Haste (Weinreich)<br />
Fraser Holleywood (Miranti)<br />
Christina Untersperger (Weinreich)<br />
University of Illinois, Champaign-Urbana<br />
Huong Tran (Resau)<br />
University of Mannheim, Germany<br />
Katja Strunk (Alberts)<br />
University of Michigan, Ann Arbor<br />
Alyse DeHaan* (MacKeigan)<br />
Xiang Gao (Xu)<br />
Theresa Gipson* (Furge)<br />
Sara Herman* (Resau/MacKeigan)<br />
Hailey Hines (Webb)<br />
Katie Koelzer* (Swiatek)<br />
Matthew McElliott* (Cavey/MacKeigan)<br />
Catherine Perrin* (Webb)<br />
Kyle VanKoevering (Williams)<br />
Jennifer Wilcox* (Duesbery)<br />
University of Notre Dame, South Bend, Indiana<br />
Kristin Buzzitta* (Teh)<br />
Joe Church (MacKeigan)<br />
University of Ulster, Northern Ireland<br />
Peipei Zhong (Xu)<br />
University of Wisconsin – Green Bay<br />
Danielle Burgenske (Resau)<br />
Other Van Andel Institute Interns<br />
Aquinas College, Grand Rapids, Michigan<br />
Tanja Barunovic (Grants and Contracts)<br />
Davenport University, Grand Rapids, Michigan<br />
Randall Edler (Information Technology)<br />
Philip Straatsma (Information Technology)<br />
Ferris State University, Big Rapids, Michigan<br />
Eric Firestone (Facilities)<br />
Grand Valley State University<br />
Andy Schmidt (Finance)<br />
University of Michigan, Ann Arbor<br />
Mitchell Zoerhoff (Communications)<br />
87
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Han-Mo Koo Memorial Seminar Series<br />
88
VARI | <strong>2008</strong><br />
Han-Mo Koo Memorial Seminar Series<br />
This seminar series is dedicated to the memory of Dr. Han-Mo Koo, who was a VARI <strong>Scientific</strong> Investigator from 1999 until his<br />
passing in May of 2004.<br />
January 2007<br />
Moses Lee, Hope College<br />
“Regulation of the topoisomerase IIα gene using polyamides that bind to the inverted CCAAT<br />
box present in the promoter”<br />
February<br />
Raj Kumar, University of Texas Medical Branch<br />
“Structure and functions of the steroid receptors”<br />
David Kimelman, University of Washington<br />
“Tales of tails: the importance of Bmp signaling in embryogenesis”<br />
Arthur L. Haas, Louisiana State University<br />
“ISG15 and ubiquitin as antagonistic regulators of cell transformation”<br />
March<br />
S. Stoney Simons, Jr., National Institutes of Health<br />
“A systems biology approach to steroid hormone action: towards a quantitative understanding<br />
of whole cell responses to steroid hormones”<br />
John D. Shaughnessy, Jr., University of Arkansas for Medical Sciences<br />
“Using genomics to better understand the biology and clinical course of multiple myeloma”<br />
Melanie H. Cobb, University of Texas Southwestern Medical Center<br />
“MAP kinase signaling in pancreatic beta cells”<br />
April<br />
Christopher G. Wood, M.D. Anderson Cancer Center<br />
“Redefining the role of surgery for renal cell carcinoma in the era of targeted therapy”<br />
Jules J. Berman, Writer/consultant<br />
“New trends in biomedical informatics”<br />
89
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
May<br />
Shiv Greval, National Cancer Institute<br />
“Heterochromatin: a versatile platform of the genome”<br />
Ermanno Gherardi, MRC Centre<br />
“Structure/function of HGF/SF and MET”<br />
Caroline Alexander, University of Wisconsin–Madison<br />
“Stem cells and cancer”<br />
David A. Cheresh, University of California, San Diego<br />
“Signaling mechanism in angiogenesis and metastasis”<br />
June<br />
Bruce R. Ksander, Schepens Eye Research Institute<br />
“A gene therapy to prevent the growth and spread of uveal melanomas”<br />
August<br />
Peggy Farnham, University of California, Davis<br />
“Using ChIP-chip to characterize mechanisms of transcriptional repression in pluripotent and<br />
differentiated mammalian cells”<br />
Daniel D. Von Hoff, Translational Genomics Research Institute<br />
“The oncologists’ 6th vital sign—a context of vulnerability”<br />
Arul M. Chinnaiyan, University of Michigan<br />
“Recurrent gene fusions in prostate cancer: a new class of biomarkers and therapeutic targets”<br />
Eddy Arnold, Rutgers University<br />
“Engineering of high-resolution HIV-1 reverse transcriptase crystals and the concept of strategic<br />
flexibility in evading drug resistance”<br />
90
VARI | <strong>2008</strong><br />
September<br />
Michael Glotzer, University of Chicago<br />
“Dividing the spoils—positioning the plane of cell division”<br />
Andries Zijlstra, Vanderbilt University<br />
“Intravital imaging of tumor cell motility: the role of migration in metastasis”<br />
Harald zur Hausen, German Cancer Research Institute<br />
The Daniel Nathans Memorial <strong>Scientific</strong> Lecture: “Mechanisms of viral oncogenesis”<br />
The Daniel Nathans Memorial Lay Lecture: “Infectious causes of human cancer”<br />
Douglas R. Lowy, National Cancer Institute<br />
The Daniel Nathans Memorial <strong>Scientific</strong> Lecture: “Preventing cervical cancer by HPV vaccination and<br />
other approaches”<br />
The Daniel Nathans Memorial Lay Lecture: “Prevention and treatment of cancers caused<br />
by infections”<br />
Michael Ohh, University of Toronto<br />
“HIF-centric tumour suppressor model of VHL”<br />
October<br />
Atul Butte, Stanford University<br />
“Exploring genomic medicine using translational bioinformatics”<br />
Phil Hieter, University of British Columbia<br />
“Chromosome instability in yeast and cancer”<br />
Dimiter S. Dimitrov, National Cancer Institute<br />
“Human monoclonal antibodies against viruses and cancer”<br />
Robert L. Nussbaum, University of California, San Francisco<br />
“Molecular genetic approach to Parkinson disease”<br />
91
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
November<br />
Timothy P. Cripe, Children’s Hospital Medical Center, Cincinnati<br />
“Got herpes? Developing oncolytic virus therapy for pediatric cancer”<br />
Gary D. Stoner, Ohio State University<br />
“A food-based approach to the prevention of G.I. tract cancers”<br />
Stephen P. Bell, Massachusetts Institute of Technology<br />
“A G1 checkpoint coordinating origin selection and cell cycle progression”<br />
Diane M. Simeone, University of Michigan<br />
“Pancreatic cancer stem cells”<br />
G. David Roodman, University of Pittsburgh<br />
“Paget’s disease: virus or gene?”<br />
February <strong>2008</strong><br />
David N. Zachs, University of Michigan<br />
“Photoreceptor survival during disease: life hanging in the balance”<br />
Anthony J. Senagore, Spectrum Health<br />
“Economic issues in translational medicine”<br />
March<br />
Robert M. Strieter, University of Virginia<br />
“CXC chemokines in angiogenesis and metastases of cancer”<br />
Graham J. Burton, University of Cambridge<br />
“Trophoblast invasion in human pregnancy: functions, mechanisms, and regulation”<br />
Valeri I. Vasioukhin, Fred Hutchinson Cancer Research Center<br />
“Mechanisms of prostate cancer initiation and progression”<br />
92
VARI | <strong>2008</strong><br />
Van Andel Research Institute Organization<br />
93
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
David L. Van Andel,<br />
Chairman and CEO, Van Andel Institute<br />
VARI Board of Trustees<br />
David L. Van Andel, Chairman and CEO<br />
James Fahner, M.D.<br />
Fritz M. Rottman, Ph.D.<br />
Board of <strong>Scientific</strong> Advisors<br />
The Board of <strong>Scientific</strong> Advisors advises the CEO and the Board of Trustees, providing recommendations and suggestions<br />
regarding the overall goals and scientific direction of VARI. The members are<br />
Michael S. Brown, M.D., Chairman<br />
Richard Axel, M.D.<br />
Joseph L. Goldstein, M.D.<br />
Tony Hunter, Ph.D.<br />
Phillip A. Sharp, Ph.D.<br />
<strong>Scientific</strong> Advisory Board<br />
The <strong>Scientific</strong> Advisory Board advises the VARI Director, providing recommendations and suggestions specific to the ongoing<br />
research, especially in the areas of cancer, genomics, and genetics. It also coordinates and oversees the scientific review<br />
process for the Institute’s research programs. The members are<br />
Alan Bernstein, Ph.D.<br />
Joan Brugge, Ph.D.<br />
Webster Cavenee, Ph.D.<br />
Frank McCormick, Ph.D.<br />
94
VARI | <strong>2008</strong><br />
Office of the Director<br />
George F. Vande Woude, Ph.D.<br />
Director<br />
Deputy Director<br />
for Clinical Programs<br />
Rick Hay, Ph.D., M.D.<br />
Deputy Director<br />
for Special Programs<br />
James H. Resau, Ph.D.<br />
Deputy Director<br />
for Research Operations<br />
Nicholas S. Duesbery, Ph.D.<br />
Director<br />
for Research Administration<br />
Roberta Jones<br />
Administrator<br />
to the Director<br />
Michelle Bassett<br />
Science Editor<br />
David E. Nadziejka<br />
Administrative Assistants<br />
From left, Lewis, Koehler, Spears,<br />
Holman, Chastain, Guthrey, Noyes,<br />
Nelson, Rappley, Jason, Koo, Resau<br />
Not present: Novakowski<br />
95
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Van Andel Institute Administrative Organization<br />
The organizational units listed below provide administrative support to both the Van Andel Research Institute and the Van Andel<br />
Education Institute.<br />
Executive<br />
David Van Andel, Chairman and CEO<br />
Steven R. Heacock, Chief Administrative Officer and<br />
General Counsel<br />
R. Jack Frick, Chief Financial Officer<br />
Christy Goss, Executive Assistant<br />
Ann Schoen, Executive Assistant<br />
Laura Lohr<br />
Business Development<br />
Jerry Callahan, Ph.D., Vice President<br />
Brent Mulder, Ph.D.<br />
Thomas DeKoning<br />
Jennifer McGrail<br />
Linda Chamberlain, Ph.D., consultant<br />
Communications and Development<br />
Joseph P. Gavan, Vice President<br />
Jaime Brookmeyer<br />
Tim Hawkins<br />
Sarah Lamb<br />
Sarah Smedes<br />
Laurie Ward<br />
Facilities<br />
Samuel Pinto, Manager<br />
Michelle Bies<br />
Jeff Cooling<br />
Jason Dawes<br />
Ken De Young<br />
Shelly King<br />
Tracy Lewis<br />
Dave Marvin<br />
Karen Pittman<br />
Richard Sal<br />
Richard Ulrich<br />
Pete VanConant<br />
Jeff Wilbourn<br />
Finance<br />
Timothy Myers, Controller<br />
Cory Cooper<br />
Sandi Essenburg<br />
Stephanie Green<br />
Richard Herrick<br />
Keri Jackson<br />
Angela Lawrence<br />
Laura Lohr<br />
Heather Ly<br />
Susan Raymond<br />
Jamie VanPortfleet<br />
Mitchell Zoerhoff<br />
Glassware and Media Services<br />
Richard M. Disbrow, C.P.M., Manager<br />
Bob Sadowski<br />
Marlene Sal<br />
Grants and Contracts<br />
Carolyn W. Witt, Director<br />
Anita Boven<br />
Nicole Doppel<br />
Sara O’Neal<br />
David Ross<br />
Human Resources<br />
Linda Zarzecki, Director<br />
Margie Hoving<br />
Stephanie Koelewyn<br />
Pamela Murray<br />
Angela Plutschouw<br />
96
VARI | <strong>2008</strong><br />
Information Technology<br />
Bryon Campbell, Ph.D., Chief Information Officer<br />
David Drolett, Manager<br />
Bill Baillod<br />
Tom Barney<br />
Phil Bott<br />
Nathan Bumstead<br />
Brad Covell<br />
Charles Grabinski<br />
Kenneth Hoekman<br />
Kimberlee Jeffries<br />
Jason Kotecki<br />
Thad Roelofs<br />
Russell Vander Mey<br />
Candy Wilkerson<br />
Investments Office<br />
Kathleen Vogelsang, Director<br />
Benjamin Carlson<br />
Ted Heilman<br />
Procurement Services<br />
Richard M. Disbrow, C.P.M., Manager<br />
Heather Frazee<br />
Chris Kutchinski<br />
Shannon Moore<br />
Amy Poplaski<br />
John Waldon<br />
Security<br />
Kevin Denhof, CPP, Chief<br />
Amy Davis<br />
Sean Mooney<br />
Maria Straatsma<br />
Chris Wilson<br />
Contract Support<br />
Sarah Lowen, Librarian<br />
(Grand Valley State University)<br />
Jim Kidder, Safety Manager<br />
(Michigan State University)<br />
97
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
Van Andel Institute<br />
Van Andel Institute Board of Trustees<br />
David Van Andel, Chairman<br />
Peter C. Cook<br />
Ralph W. Hauenstein<br />
Michael Jandernoa<br />
John C. Kennedy<br />
Board of <strong>Scientific</strong> Advisors<br />
Michael S. Brown, M.D., Chairman<br />
Richard Axel, M.D.<br />
Joseph L. Goldstein, M.D.<br />
Tony Hunter, Ph.D.<br />
Phillip A. Sharp, Ph.D.<br />
Van Andel Research Institute<br />
Board of Trustees<br />
David Van Andel, Chairman<br />
James Fahner, M.D.<br />
Fritz M. Rottman, Ph.D.<br />
Chief Executive Officer<br />
David Van Andel<br />
Van Andel Education Institute<br />
Board of Trustees<br />
David Van Andel, Chairman<br />
Donald W. Maine<br />
Gordon Van Harn, Ph.D.<br />
Gordon Van Wylen, Sc.D.<br />
Van Andel Research Institute<br />
Director<br />
George Vande Woude, Ph.D.<br />
Chief Administrative Officer<br />
and General Counsel<br />
Steven R. Heacock<br />
VP Communications<br />
and Development<br />
Joseph P. Gavan<br />
Van Andel Education Institute<br />
Director<br />
Gordon Van Harn, Ph.D.<br />
Chief Financial Officer<br />
R. Jack Frick<br />
98
VARI | <strong>2008</strong><br />
Van Andel Research Institute<br />
DIRECTOR – George Vande Woude, Ph.D.<br />
Deputy Directors<br />
Clinical Programs Rick Hay, Ph.D., M.D.<br />
Special Programs James Resau, Ph.D.<br />
Research Operations Nick Duesbery, Ph.D.<br />
Director for Research Administration<br />
Roberta Jones<br />
SCIENTIFIC ADVISORY BOARD<br />
Alan Bernstein, Ph.D.<br />
Joan Brugge, Ph.D.<br />
Webster Cavenee, Ph.D.<br />
Frank McCormick, Ph.D.<br />
BASIC SCIENCE<br />
SPECIAL PROGRAMS<br />
Cancer Cell Biology<br />
Brian Haab, Ph.D.<br />
Cancer Immunodiagnostics<br />
George Vande Woude, Ph.D.<br />
Molecular Oncology<br />
Craig Webb, Ph.D.<br />
Tumor Metastasis & Angiogenesis<br />
Signal Transduction<br />
Art Alberts, Ph.D.<br />
Cell Structure & Signal Intergration<br />
Cindy Miranti, Ph.D.<br />
Integrin Signaling & Tumorigenesis<br />
DNA Replication & Repair<br />
Michael Weinreich, Ph.D.<br />
Chromosome Replication<br />
Animal Imaging<br />
Rick Hay, Ph.D., M.D.<br />
Noninvasive Imaging<br />
& Radiation Biology<br />
Animal Models<br />
Nicholas Duesbery, Ph.D.<br />
Cancer & Developmental Cell Biology<br />
Bart Williams, Ph.D.<br />
Cell Signaling & Carcinogenesis<br />
Cancer Genetics<br />
Bin Teh, M.D., Ph.D.<br />
Cancer Genetics<br />
Structural Biology<br />
Eric Xu, Ph.D.<br />
Structural Sciences<br />
Systems Biology<br />
Jeffrey MacKeigan, Ph.D.<br />
Systems Biology<br />
Gene Regulation<br />
Steven Triezenberg, Ph.D.<br />
Transcriptional Regulation<br />
Dean of VAI Graduate School<br />
Brian Cao, M.D.<br />
Antibody Technology<br />
Pamela Swiatek, Ph.D., M.B.A.<br />
Germline Modification<br />
and Cytogenetics<br />
Bryn Eagleson, A.A.<br />
Transgenics and Vivarium<br />
Bin Teh, M.D., Ph.D.<br />
Sequencing<br />
Art Alberts, Ph.D.<br />
Flow Cytometry<br />
Division of Quantitative Sciences<br />
James Resau, Ph.D.<br />
James Resau, Ph.D.<br />
Analytical, Cellular,<br />
& Molecular MIcroscopy<br />
James Resau, Ph.D.<br />
Microarray Technology<br />
Kyle Furge, Ph.D.<br />
Computational Biology<br />
Greg Cavey, B.S.<br />
Mass Spectrometry and<br />
Proteomics<br />
James Resau, Ph.D.<br />
Molecular Epidemiology<br />
99
Van Andel Research Institute | <strong>Scientific</strong> <strong>Report</strong><br />
The Van Andel Institute and/or its affiliated organizations (VARI and VAEI), through its responsible managers, recruits, hires, upgrades, trains,<br />
and promotes in all job titles without regard to race, color, religion, sex, national origin, age, height, weight, marital status,<br />
disability, pregnancy, or veteran status, except when an accommodation is unavailable or it is a bona fide occupational qualification.<br />
Printed by Spectrum Graphics, Inc.<br />
100