Heartbeat February 2018
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>February</strong> <strong>2018</strong><br />
Sandwell and West Birmingham Hospitals<br />
NHS Trust<br />
The pulse of community health, Leasowes, Rowley Regis, City and Sandwell Hospitals Issue 101<br />
Listening Into Action: Purple Points<br />
give carers and patients a voice Page 3<br />
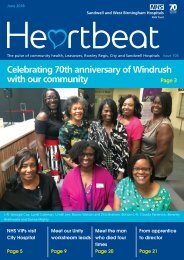
Members of the Trust leadership team and the governance support unit are joined by Ian McGarry, Communications<br />
and Engagement Officer at Healthwatch Sandwell to launch the Purple Points which have gone live this week<br />
Supporting<br />
Over 400 colleagues<br />
Focus on<br />
UK first operation<br />
victims of<br />
undertake<br />
Unity: All you<br />
performed at<br />
domestic abuse<br />
accredited line<br />
need to know<br />
BMEC<br />
manger training<br />
Page 4<br />
Page 6<br />
Page 14-15<br />
Page 17<br />
HB <strong>February</strong> <strong>2018</strong>.indd 1 20/02/<strong>2018</strong> 11:37
Contact us<br />
Communications Team<br />
Ext 5303<br />
swbh.comms@nhs.net<br />
Communications Department<br />
Ground Floor, Trinity House<br />
Sandwell Hospital<br />
Published by<br />
Communications Team<br />
Sandwell and West Birmingham<br />
Hospitals NHS Trust<br />
Designed by<br />
Medical Illustration,<br />
Graphics Team<br />
Sandwell and West Birmingham<br />
Hospitals NHS Trust<br />
Submit an idea<br />
If you’d like to submit an idea<br />
for an article, contact the Editor,<br />
Emily Smith<br />
Ext 5877<br />
emily.smith46@nhs.net<br />
HELLO<br />
Welcome to <strong>February</strong>’s edition<br />
of <strong>Heartbeat</strong>.<br />
This month we focus on the launch<br />
of our Purple Points – a seven<br />
day service which will support<br />
our patients and their families to<br />
resolve any concerns they have<br />
about their care whilst they are still<br />
an inpatient. You can find out more<br />
on page three.<br />
Elsewhere, there is an excellent<br />
article on a UK first operation<br />
performed at BMEC and the centre<br />
spread will tell you everything you<br />
need to know about Unity.<br />
Stay updated<br />
We send out a communications<br />
bulletin via email every day, or you<br />
can follow us on:<br />
FROM THE CHAIR<br />
Purple Points will enable<br />
us to make a difference<br />
straight away<br />
I am really pleased to see this month<br />
the launch of our new Purple Point<br />
phone service, to help patients who<br />
are staying with us as inpatients get<br />
the help that they need immediately.<br />
I am hopeful that this new way for<br />
patients and relatives to raise concerns<br />
about care on our wards will enable us<br />
to make a difference straight away to<br />
people’s experiences. The new phone<br />
service can also be used to record a<br />
thank you or pay a compliment to our<br />
hard-working teams.<br />
The phone service should provide us with<br />
rich feedback on our services and will<br />
help us to understand what really matters<br />
to our patients and their loved ones. Of<br />
course, it is not the only way people can<br />
give feedback. We want to continue to<br />
encourage patients to talk to their ward<br />
teams about their experiences: Purple Point<br />
does not aim to replace that important<br />
interaction. We know, however, from<br />
looking at our complaints and from a useful<br />
report that Healthwatch Sandwell published<br />
after speaking to a number of patients, that<br />
sometimes patients can feel uncomfortable<br />
about raising a concern directly as they<br />
worry that their care will be affected. Purple<br />
Point is one way to help overcome this.<br />
Our Medical Director, David Carruthers, has<br />
made it clear in his support of the service<br />
that people’s care will not be compromised<br />
by speaking up.<br />
The ask for each one of us is to act promptly<br />
when a concern has been raised via our<br />
Purple Point phones. Patients are waiting<br />
for a response so we need to take action<br />
immediately.<br />
Each month our public board meeting<br />
hears from a patient about their experience<br />
of our care. Sometimes these stories are<br />
overwhelmingly positive and it is heartening<br />
to hear how well our teams have looked<br />
after people. At times, their experiences are<br />
less positive than we would like. Over the<br />
past few months we have heard a range<br />
of different patient experiences. From the<br />
frustrations of a deaf patient who wanted<br />
to talk to someone about her needs before<br />
attending an outpatient appointment,<br />
to the patient who was transferred to a<br />
different site late at night. Whilst the clinical<br />
care provided in each of these cases was<br />
appropriate and the right thing to do, how<br />
people feel about their care is strongly<br />
influenced by how their different needs are<br />
taken into account. Being able to adjust our<br />
care of each patient, recognising their needs<br />
and wishes, does have a dramatic impact on<br />
how they feel about their treatment here.<br />
Purple Point aims to help highlight those<br />
small things that we can do to make things<br />
a bit easier for patients, carers, friends and<br />
family members. I am looking forward to<br />
seeing the results.<br />
Richard Samuda – Trust Chairman<br />
Richard Samuda is asking colleagues to act<br />
promptly when a concern has been raised via<br />
the Purple Points<br />
2<br />
HB <strong>February</strong> <strong>2018</strong>.indd 2 20/02/<strong>2018</strong> 11:38
Listening Into Action: Purple Points give<br />
carers and patients a voice<br />
Over the last three years we have<br />
found lots of ways to improve how<br />
we hear from our patients and<br />
make changes as a result. Dr David<br />
Carruthers, our new Medical Director,<br />
is championing the latest organisation<br />
wide project to make it simpler for<br />
patients, friends and families to tell<br />
us what we do well, and what their<br />
worries are.<br />
David told <strong>Heartbeat</strong>: “Feedback must<br />
never mean that a patient feels that their<br />
care is compromised. We know that<br />
people are reluctant to speak up during an<br />
inpatient stay because they feel vulnerable.<br />
All of us need to take away that fear.”<br />
The Purple Point telephones are in place<br />
near our inpatient wards, and went “live”<br />
at the end of <strong>February</strong>. The phones are<br />
staffed seven days a week, and we are<br />
aiming to get action and improvements<br />
happening on each case raised inside a few<br />
hours.<br />
Elaine Newell, our Chief Nurse said: “Purple<br />
Point is a brilliant option but not one that<br />
replaces sorting things out at the bedside.<br />
We want our patients to know the service<br />
is there as a safety net, and we want<br />
relatives and carers to speak up if they are<br />
Communications and Engagement Officer at Healthwatch Sandwell, Ian McGarry, tests out one of our<br />
new Purple Points<br />
CORPORATE & GENERAL NEWS<br />
worried about the care their loved one<br />
is receiving.<br />
“Often that is a communication<br />
problem, but we cannot wait until after<br />
someone leaves our wards to act. All<br />
of us come to work to do a great job,<br />
and so when things seem wrong we<br />
want someone to tell us. Purple Point,<br />
available in multiple languages, gives<br />
local people the chance to do just that.”<br />
A recent study of patient views<br />
conducted by Healthwatch Sandwell<br />
found respondents wanted more ways<br />
to speak up safely. John Clothier, Chair<br />
of Healthwatch Sandwell commented:<br />
“We fully support this new initiative<br />
which, in response to our report<br />
published in 2016, shows that the Trust<br />
listens. This will help patients, relatives<br />
and carers to have their concerns about<br />
treatment and care addressed quickly<br />
and effectively. We wish Purple Point<br />
every success.”<br />
The phone line will be available 9am –<br />
9pm, every day. The Purple Point team,<br />
who are used to helping patients with<br />
complaints and enquiries, will speak to<br />
the caller about their concern and then<br />
make sure that the relevant colleague<br />
is informed so that the issue is resolved<br />
quickly. The team will also check with<br />
the patient that they are happy with<br />
the outcome. Staff members need to<br />
both tackle Purple Point queries rapidly<br />
and take responsibility for talking to the<br />
person raising the concern.<br />
Kam Dhami, Director of Governance<br />
is overseeing implementation of the<br />
Purple Points, she explained that the<br />
project is an NHS first: “Every month<br />
the Trust’s Board hears a patient story.<br />
Many are full of compliments for what<br />
we all do. But some show weaknesses<br />
and errors, typically with missed<br />
opportunities to get it right. This project<br />
is our chance to tackle that. If you get<br />
a call from the team, please take it<br />
seriously and deal with it quickly.<br />
“Often someone has the wrong end<br />
of the stick or needs a little time to<br />
have something explained. That little<br />
bit of time can make all the difference.<br />
Being in hospital is a worrying time for<br />
anyone. This project helps us to reduce<br />
anxiety and spot potential harm. Let’s<br />
embrace it and help our patients to be<br />
part of our safety campaign.”<br />
3<br />
HB <strong>February</strong> <strong>2018</strong>.indd 3 20/02/<strong>2018</strong> 11:38
Routine questions to help support<br />
domestic abuse victims<br />
CORPORATE & GENERAL NEWS<br />
A set of four routine screening<br />
questions are being asked within<br />
A&E and our paediatric department<br />
which are aimed at identifying and<br />
supporting victims of domestic<br />
abuse.<br />
Domestic abuse costs the NHS £1.7<br />
billion a year and nationally one in<br />
four women and one in seven men are<br />
victims of domestic violence, one in five<br />
children are exposed to domestic abuse<br />
and two women every week are killed as<br />
a result of abuse.<br />
In 2015, our organisation introduced<br />
two independent domestic violence<br />
advisors (IDVAs) to work within the<br />
emergency departments at Sandwell<br />
and City Hospitals. It was initially a two<br />
year pilot project, funded by Your Trust<br />
Charity and Black Country Women’s Aid,<br />
although recently the charity has been<br />
able to fund a six month extension of<br />
the service.<br />
<strong>Heartbeat</strong> caught up with IDVAs Sarah<br />
Markland and Rachana Chauhan to find<br />
out more about their important role.<br />
Sarah said: “The purpose of the IDVA<br />
project is to improve assessment and<br />
referral for victims of domestic abuse<br />
and to identify any safeguarding issues<br />
and improve outcomes for children.”<br />
Rachana added: “We have been<br />
working with colleagues in A&E to raise<br />
awareness of domestic abuse and to<br />
train them in the importance of asking<br />
the screening questions, regardless of if<br />
there are any signs.<br />
“Victims of domestic abuse often<br />
present at hospital with other injuries<br />
or with signs of alcohol or drug abuse.<br />
The questions, which should be asked<br />
when the patient is alone so as to not<br />
put them at any risk, can help raise<br />
any issues happening at home that the<br />
patient may need support with.”<br />
“We have access to the Black Country<br />
Women’s Aid database,” explained<br />
Sarah.<br />
“This means that we can check if<br />
there have been any previous referrals<br />
for women who present at A&E with<br />
indications that they are a victim of<br />
domestic violence.”<br />
Rachana said: “We can support patients<br />
who make disclosures by referring<br />
into the multi-agency pathway and<br />
L-R: Rachana Chauhan, IDVA; Sally Tyler, Staff Nurse; Claire Holmes, Domestic Abuse Lead Nurse;<br />
Avnash Nanra, Lyndon Ground Ward Manager and Sarah Markland, IDVA<br />
safeguarding them, and any children who<br />
may be affected whilst they are in hospital.”<br />
In addition to A&E, one area in which the<br />
screening questions are working well is<br />
within paediatrics.<br />
<strong>Heartbeat</strong> spoke to Domestic Abuse Lead<br />
Nurse, Claire Holmes to find out how<br />
training with colleagues on our children’s<br />
wards has already led to some important<br />
interventions for victims of domestic abuse.<br />
“The questions weren’t routinely being<br />
asked on the unit,” explained Claire.<br />
“But we spent time with the team and<br />
explained the importance of asking them<br />
in order to safeguard both adults and<br />
children.”<br />
The questions are now being asked<br />
routinely on every admission when it is safe<br />
to do so.<br />
Claire said: “Colleagues are aware of the<br />
need to protect patients, so they will only<br />
ask the questions when they are on their<br />
own and with no children over the age of<br />
two present. Asking in front of a partner<br />
of family member can potentially place a<br />
victim at more risk.”<br />
Claire said that the training is already<br />
paying off, with the team having identified<br />
and supported some patients who have<br />
been victims.<br />
She said: “A few months ago we had a lady<br />
who had come in with a child aged around<br />
nine months. The morning after they had<br />
arrived, the lady’s make-up had worn off<br />
and a staff nurse noticed she had a black<br />
eye. When it was safe to do so, they asked<br />
the screening questions, but the patient<br />
denied anything untoward was happening<br />
at home.<br />
“Later on, another nurse noticed that she<br />
had what looked like a cigarette burn to<br />
her hand. They notified me and I did some<br />
research via the multi-agency safeguarding<br />
hub. Although they were not known to<br />
children’s services, there was a self-referral<br />
from the lady to Black Country Women’s<br />
Aid.<br />
“The team spoke to her again about<br />
domestic abuse and raised their concerns<br />
over her injuries. This time she did disclose<br />
and we were able to initiate support from<br />
Rachana and Sarah and we made a referral<br />
to children’s services to ensure the child was<br />
safeguarded.<br />
“This all came about because the team put<br />
into practice what they had learned during<br />
their training. They have taken it on board<br />
so well and I can’t thank them enough.<br />
“Health seems to be a safe haven for<br />
people to disclose abuse; they seem to<br />
feel more comfortable in a hospital than in<br />
other settings. Therefore it is vital that we<br />
raise awareness of domestic abuse across<br />
the whole organisation.”<br />
If you are interested in finding out<br />
more and would like to receive<br />
support from the safeguarding team<br />
to implement the screening questions<br />
in your area, please contact Claire on<br />
claire.holmes1@nhs.net.<br />
The four screening<br />
questions are:<br />
1. Do you ever feel afraid at<br />
home?<br />
2. Does a partner, ex-partner or<br />
anyone at home often put you<br />
down, humiliate you or try to<br />
control what you do?<br />
3. Have you ever been hurt or<br />
threatened by a partner or<br />
anyone at home?<br />
4. Could you tell me how or why<br />
you got those injuries?<br />
4<br />
HB <strong>February</strong> <strong>2018</strong>.indd 4 20/02/<strong>2018</strong> 11:38
Charity fundraiser crowned ‘Community<br />
Most Valuable Player’<br />
@SWBHCharity To donate<br />
to the Your Trust Charity text<br />
“SWBH16 £5” to 70070<br />
Sally Gutteridge has been crowned<br />
‘Community Most Valuable Player’ by<br />
Aston Villa Football Club in recognition<br />
of her contribution to the local<br />
community and her ability to inspire<br />
others.<br />
Mum-of-two Sally was nominated by<br />
Amanda Winwood, Your Trust Charity<br />
Fundraising Manager after she raised<br />
£2,526.04 for the charity during 2017 –<br />
despite suffering a stroke and being told<br />
she had a second brain tumour.<br />
“Sally is incredible and we are so glad<br />
she has been recognised for her hard<br />
work,” said Amanda. “She has battled<br />
breast cancer, suffered a stroke and is now<br />
wheelchair bound and living with multiple<br />
brain tumours and liver cancer, but this<br />
doesn’t stop her putting the needs of others<br />
before herself.”<br />
Sally was first diagnosed with breast cancer<br />
four years ago. She had a breast removed<br />
and went into remission. However, in 2016<br />
she started suffering from seizures, and<br />
doctors discovered a tumour on her brain.<br />
Tragedy struck again, when in July 2017<br />
she suffered a stroke, which left her unable<br />
to use her left side. She had to get used to<br />
life in a wheelchair, but continues to have<br />
physiotherapy at Sandwell Hospital. Soon<br />
afterwards she was told the devastating news<br />
that she had another brain tumour. Despite all<br />
of this, her outlook on life remains positive.<br />
Sally decided to fundraise for Your Trust<br />
Charity to give something back to those who<br />
had been caring for her. Much of the funds<br />
she has raised so far came from a 1940s tea<br />
party that she held in October. She also used<br />
this event to showcase her latest project,<br />
Sally’s Sunshine Packs. These are goodie bags<br />
for chemotherapy and end-of-life patients<br />
who are in our care. The packs will contain<br />
items such as puzzle books, a journal, sweets,<br />
wet wipes, shampoo and tissues.<br />
Sally said of these packs: “They will mean so<br />
YOUR TRUST CHARITY<br />
much to patients. I remember seeing<br />
others undergoing treatment who were<br />
there by themselves. I just thought it<br />
would have been so nice for them to<br />
have something that they could take<br />
home, that was useful.<br />
“I decided to join forces with Your Trust<br />
Charity because it meant I could really<br />
give something back to the people who<br />
have been caring for me. By working<br />
with the charity, I can see where this<br />
money is going and how it is helping<br />
patients. It is more personal to me. I<br />
want to raise more than £3,000 and<br />
I would like to keep building on this<br />
figure.”<br />
Sally was handed the Aston Villa Community Most Valuable Player award on the pitch at the game<br />
versus Burton Albion on 3 <strong>February</strong><br />
Family donate cash to critical care to<br />
say thanks for outstanding care<br />
The family of a patient have shown<br />
their gratitude for the care he received<br />
at City Hospital by donating £200 to the<br />
critical care unit.<br />
Trevor Gabb, from Hereford, was rushed to<br />
the hospital after suffering respiratory arrest<br />
in November. The 77-year-old had been<br />
at an event in Birmingham when tragedy<br />
struck. Sadly, doctors were unable to save<br />
him, and he died eight days later.<br />
However, his wife Ann and son Andrew,<br />
were so touched by the support and care<br />
Trevor was given that they asked mourners<br />
at his funeral to donate money so they<br />
could give it to the Your Trust Charity critical<br />
care fund.<br />
“We wanted to make this donation because<br />
of the absolutely unbelievable care that the<br />
nursing staff and doctors gave to my dad<br />
during his final days,” said Andrew, also<br />
from Hereford.<br />
“They also were really supportive to us as<br />
well. My mum stayed at the hospital with<br />
him, because of the distance, and they were<br />
very accommodating towards her. It really<br />
made a difference to us and we wanted<br />
to show our gratitude by making this<br />
donation.”<br />
Trevor was treated by Dr Santhana Kannan,<br />
Consultant for Anaesthesia and Critical<br />
Care during his time in the hospital.<br />
Andrew added: “All the nursing staff were<br />
very good and we nicknamed Dr Kannan<br />
‘Dr Nice’ because of how caring he was.”<br />
Dr Kannan said: “The team are very grateful<br />
to the family of Mr Gabb for their kind<br />
donation. To say that Mrs Gabb is a very<br />
sweet person is quite an understatement.<br />
It was really exceptional that under difficult<br />
circumstances, the family took the time<br />
to provide detailed written feedback and<br />
remembered the individual staff by their<br />
names. Instances like these make working<br />
in critical care all worth it.”<br />
5<br />
HB <strong>February</strong> <strong>2018</strong>.indd 5 20/02/<strong>2018</strong> 11:38
6<br />
Over 400 colleagues on their way to<br />
becoming accredited managers<br />
CORPORATE & GENERAL NEWS<br />
L-R: Acting Matron Surgical Services, Jo<br />
Mansell and Senior Charge Nurse AMU,<br />
Mike Beech have both attended the<br />
accredited line manger training<br />
We have approximately 750 line<br />
managers within our organisation<br />
and over half of them are already<br />
on their way to becoming ‘SWBH<br />
accredited managers’ and by the end<br />
of March <strong>2018</strong>, every line manager<br />
will have been through our internal<br />
training programme.<br />
Bethan Downing, Deputy Director of<br />
Organisation Development spoke to<br />
<strong>Heartbeat</strong> about the exciting accredited<br />
manager programme.<br />
“Everyone in our organisation, who is<br />
a manager, regardless of whether they<br />
manage one person or a team of people,<br />
is required to become an accredited<br />
manager,” said Bethan.<br />
“We introduced the programme as<br />
we recognise that good managers<br />
are key to developing people in our<br />
organisation and that we had a range<br />
of managers with lots of differing levels<br />
of experience, who had entered the<br />
world of people management through<br />
a range of different routes. Some of our<br />
managers have formal qualifications<br />
and others have developed their skills<br />
through on the job learning, both of<br />
which are fine and add to our diversity<br />
of experiences and learning, but we<br />
needed all our managers to have a<br />
common understanding of how we<br />
need to manage our people consistently<br />
to ensure we create and retain the best<br />
workforce we can.<br />
“We hadn’t really done anything like this<br />
before. Our managers are very busy people<br />
and we wanted to give them something<br />
that helped them meet new people, learn<br />
through experiences and also update<br />
themselves on best practice in managing<br />
people.<br />
Each manager will undertake five core<br />
modules in Year 1, which started in January<br />
this year and will run until the end of<br />
March, following which any new managers<br />
entering our organisation will also attend the<br />
accredited manager modules.”<br />
The five core accredited manager modules<br />
are:<br />
• Module 1 - Aspiring to excellence<br />
PDR<br />
• Module 2 - Managing health and<br />
wellbeing<br />
• Module 3 - Recruiting and<br />
retaining talented people<br />
• Module 4 - Managing your resources<br />
• Module 5 - Managing your<br />
responsibilities<br />
Bethan added: “After achieving the five core<br />
modules, line managers will be presented<br />
with their accredited manager passport<br />
which will enable them to demonstrate the<br />
skills they have learned through the training.<br />
“It will also form part of their PDR as they<br />
can discuss with their own manager how<br />
they are utilising the skills they learnt from<br />
the training. They can also discuss the next<br />
steps in their management journey and book<br />
onto the next phase of training which will<br />
be individually tailored to them, some of the<br />
new modules which are available from April<br />
include resilience training and coaching for<br />
managers.<br />
“So far we have seen 100 managers in<br />
some of the sessions and the range of<br />
experience levels and areas they work in has<br />
really enabled depth of conversation and<br />
learning. They have been able to network<br />
with each other and learn from people who<br />
may have experienced similar challenges to<br />
themselves.”<br />
The training is being run entirely internally,<br />
with the organisation making use of subject<br />
experts amongst colleagues.<br />
“We are using our internal experts to deliver<br />
the training,” said Bethan.<br />
“Not only does that mean we avoid<br />
using expensive companies to deliver the<br />
training, it also means that we really can<br />
share the expertise that we have within the<br />
organisation and that the learning is about<br />
Over 400 managers have attended the<br />
accredited line manager programme sessions<br />
us specifically.<br />
“It also gives the subject experts who are<br />
presenting the opportunity to apply their<br />
knowledge in a different way to their day to<br />
day job.”<br />
One line manager who has completed all<br />
five modules is Mike Beech, Senior Charge<br />
Nurse on City AMU. He told <strong>Heartbeat</strong>: “I<br />
really enjoyed the accredited line manager<br />
sessions. I learned a lot of new things, but<br />
it also acted as a good refresher of things I<br />
have learned in the past.<br />
“The sessions were interesting and<br />
interactive and it was great to share ideas<br />
and knowledge with other managers from<br />
across the organisation. As we work in such<br />
a busy environment, it’s not often you have<br />
the opportunity to come together so it was<br />
great to have the chance to do so.<br />
“I am looking forward to putting my new<br />
learning into practice.”<br />
If you are a manager and you have<br />
not already completed or booked<br />
onto the accredited manager<br />
programme modules, please ensure<br />
you book on to a session before the<br />
end of March.<br />
The training takes two days and<br />
each module is delivered in half a<br />
day. It is recommended that you<br />
complete modules 2 and 3 before<br />
4 and 5. You should have already<br />
complete module 1- Aspiring to<br />
Excellence PDR, however if you<br />
are a manager of people and have<br />
not attended the training there<br />
are dates available until the end of<br />
March.<br />
You can book your accredited<br />
manager modules via ESR or e-mail<br />
swbh.leadership@nhs.net<br />
PDR training can also be booked via<br />
ESR or email swbh.pdr@nhs.net<br />
HB <strong>February</strong> <strong>2018</strong>.indd 6 20/02/<strong>2018</strong> 11:38
Safe space provides confidential<br />
meeting place for LGBT colleagues<br />
Colleagues from lesbian, gay, bisexual<br />
and trans (LGBT) communities can now<br />
meet and talk confidentially in a new<br />
‘safe space’ provided by our workplace.<br />
It is the first time that such a space has<br />
been offered to colleagues within our<br />
organisation. Colleagues are welcome to<br />
use the space which has a breakout area,<br />
tables, chairs and hot refreshments.<br />
Head of Diversity and Inclusion, Stuart<br />
Young said: “We are delighted that the<br />
Trust has supported the provision of such a<br />
vital space for LGBT colleagues.<br />
“We have taken the lead from higher<br />
education institutions, the majority of which<br />
have had to provide LGBT space spaces<br />
on their campuses. We found that when<br />
colleagues move from university and in<br />
to the workplace, the loss of a safe space<br />
can be difficult, particularly if they are not<br />
out. Our safe space allows continuity and<br />
support.<br />
“The space provides some useful resources<br />
about sexual health information from<br />
our organisation, a Birmingham based<br />
organisation called Umbrella and the<br />
Terrence Higgins Trust.”<br />
Head of Diversity and Inclusion, Stuart Young is<br />
pictured in the new LGBT safe space<br />
There is open access to the safe space seven<br />
days a week. For further information email<br />
Swbh.lgbt@nhs.net<br />
Celebrating LGBT History Month<br />
This year our workplace has for the second<br />
CORPORATE & GENERAL NEWS<br />
consecutive year been celebrating and<br />
supporting LGBT History Month which<br />
nationally commemorated the:<br />
• 40th anniversary of the murder by<br />
shooting of Harvey Milk, the USA’s<br />
first out-gay elected councillor<br />
• 40th anniversary of the rainbow<br />
flag - launched in 1978,<br />
although sadly its creator Gilbert<br />
Baker passed away last year.<br />
Are you free during the second<br />
May Bank Holiday weekend?<br />
The LGBT staff network is calling<br />
for volunteers, both LGBT<br />
colleagues and allies to help at<br />
this year’s Birmingham –Pride on<br />
Saturday 26 May. Colleagues will<br />
be in the parade and helping out<br />
on the stall. If you can help email<br />
Swbh.lgbt@nhs.net<br />
Improvement Corner: Single<br />
improvement methodology training<br />
Each month we are highlighting the<br />
projects that are currently being<br />
undertaken by our improvement team.<br />
Our latest feature is single improvement<br />
methodology training – a programme<br />
introduced to give colleagues an<br />
overview of project management.<br />
Our organisation has a 2020 vision<br />
to become the best integrated care<br />
organisation in the NHS. The scale, pace and<br />
complexity of delivering this programme<br />
in conjunction with configuring services in<br />
line with the new Midland Metropolitan<br />
Hospital is unprecedented in our history<br />
with many programmes and projects being<br />
implemented.<br />
<strong>Heartbeat</strong> caught up with Improvement<br />
Team Project Manager, Janice Nelson to find<br />
our more.<br />
Janice said: “There was an identified need<br />
to upskill colleagues and standardise the<br />
approach in managing and delivering<br />
projects.<br />
“The single improvement methodology<br />
training introduces a standardised approach<br />
to project management. The training<br />
consists of two modules that have been<br />
developed to teach health professionals<br />
improvement methods with an increasing<br />
focus on improving healthcare in order to<br />
ensure higher quality, greater access and<br />
better value for money.”<br />
The unique, specially designed course, which<br />
is delivered by members of the improvement<br />
team, provides a great way to get the skills<br />
you need in the following ways:<br />
• Understand what makes a project<br />
successful and how to avoid pitfalls<br />
• Understand the three elements of<br />
single improvement methodology<br />
• An introduction to PDSA cycle – Plan,<br />
Do, Study, Act<br />
• An introduction to project<br />
documentation<br />
• Understanding roles within a project<br />
team.<br />
Module 1 is a half day study involving theory<br />
and an opportunity to complete project<br />
documentation.<br />
Module 2 is a full study day applying theory<br />
to practice. This day is full of fun elements<br />
where students undertake the different<br />
project roles within a project team and<br />
deliver a project.<br />
Deputy Director of Governance, Allison<br />
Binns, has attended the training. She said:<br />
“The single improvement methodology<br />
training was really good.<br />
“It has given me a great appreciation of<br />
making a plan and communicating it, but<br />
then understanding the plans need to be<br />
fluid to manage unforeseen changes that<br />
often crop up during the lifecycle of a<br />
project.<br />
“I learnt that it is ok to put a hard stop on<br />
what is happening as it gives time to reevaluate<br />
and communicate any changes,<br />
which often delivers better results than just<br />
proceeding anyway.”<br />
If you would like further information<br />
on elements of the training courses,<br />
please email swb-tr.SWBH-TEAM-<br />
TheImprovementTeam@nhs.net<br />
7<br />
HB <strong>February</strong> <strong>2018</strong>.indd 7 20/02/<strong>2018</strong> 11:38
Supported internship programme is<br />
breaking down workplace stereotypes<br />
CORPORATE & GENERAL NEWS<br />
Eager and enthusiastic is what you get<br />
when you first meet Ethan Motterham.<br />
The 20 year old has come on leaps and<br />
bounds since he joined our organisation<br />
in September 2017.<br />
Lead Administrator, Lea Brown recalls the<br />
first day Ethan came to work. “He was very<br />
shy. He walked over and sat beside me and<br />
hunched down by the desk as he didn’t<br />
want to be noticed by others in the office.”<br />
Fast forward five months and Ethan is a<br />
completely changed character. He is always<br />
laughing, eager to help and has become<br />
the heart and soul of the learning and<br />
development administration team.<br />
Ethan came to our organisation as part<br />
of a pilot with Sandwell College, which<br />
sees students placed for 30 weeks on a<br />
supported internship in a bid to develop<br />
their skills and help them to get work<br />
ready. Two other students have been<br />
placed in finance and recruitment as part<br />
of the scheme - they will all complete their<br />
placements in June.<br />
Lawrence Kelly is the Learning Works<br />
Centre Co-ordinator who explained<br />
more. “This scheme demonstrates our<br />
commitment to breaking down workplace<br />
stereotypes and the great achievements<br />
that can be achieved with support from our<br />
colleagues.<br />
“The success of the pilot is due to the<br />
measures we put in place together with<br />
Sandwell College to ensure the students<br />
have the right support to enable them<br />
to flourish in a work environment. The<br />
Ethan Motterham enjoyed his look around<br />
theatres<br />
students have personal challenges but are<br />
supported well by Steve Clarke who is a job<br />
coach on the supported interns scheme at<br />
the college.”<br />
Steve is based at Trinity House, Sandwell<br />
Hospital where he supports all three<br />
students. He said: “My role is a supportive<br />
one which sees me ensuring the students<br />
understand how to undertake their tasks.<br />
I will normally spend time with them each<br />
morning to go through their tasks and I<br />
touch base throughout the day. While they<br />
needed me around more often when they<br />
first started, all three students have become<br />
Changes to waiting list initiative<br />
payments to streamline services<br />
more independent over the months.”<br />
So what does Ethan make of his experience<br />
in our organisation so far? “I love it,” he<br />
beamed. “Everyone is really nice to me and<br />
they are not strict!<br />
“When I first started I found the work<br />
really challenging but with support<br />
from Steve and Shima Siddiqa, Assistant<br />
Administrator, my confidence began to<br />
grow. I have learned many new tasks<br />
including photocopying, putting training<br />
packs together and CD burning. I can also<br />
now input data.<br />
“I am very interested in the work of the<br />
Trust and was delighted when Lea arranged<br />
for me to look around an operating<br />
theatre. Terry January, Theatres Deputy<br />
Lead Practitioner took me around and he<br />
was really good at explaining everything<br />
to me. You can see in my photo, I had to<br />
wear scrubs and keep my hands sanitised<br />
with gel.<br />
“I will miss everyone when I have to leave.<br />
They are all very helpful and kind to me.”<br />
Lea added: “I speak on behalf of the team<br />
when I say I have thoroughly enjoyed<br />
working with Ethan over the past few<br />
months. It would be a shame to see him go<br />
when his placement ends in June. I would<br />
definitely be up for taking on a new intern.<br />
This is a wonderful part of the job where<br />
you really get to help someone learn a skill<br />
and be ready for the workplace. It has been<br />
a very fulling experience for me.”<br />
Would your team be interested in the<br />
supported internship scheme?<br />
For more information email Steve<br />
Clarke: Steve.Clarke@sandwell.ac.uk<br />
As part of the ongoing drive to review<br />
costs across the organisation, we are<br />
working to reduce the number of<br />
waiting list initiatives being carried out<br />
each year, through robust job planning<br />
and management of planned activity.<br />
We are also reviewing the amount<br />
being paid for these lists to reduce costs<br />
and also to ensure a more consistent<br />
approach across all groups and teams,<br />
be they additional outpatient clinics or<br />
theatre lists.<br />
Therefore, with effect from 1 March, the<br />
arrangements for waiting list initiative lists<br />
will change for all non-medical colleagues.<br />
All professionally registered staff – such<br />
as staff nurses and radiographers – will<br />
continue to receive the £100 payment for<br />
each approved four hour list worked.<br />
For lists which are three hours or less the<br />
rate will be £75 for the session.<br />
All un-registered colleagues including<br />
healthcare assistants, admin staff and<br />
technicians will be booked on via the Trust<br />
bank for any additional lists and will be<br />
paid at the standard bank rates which are<br />
available on Connect.<br />
Any rates currently paid above £100 to<br />
registered colleagues will cease with effect<br />
from 1 March and those carrying out<br />
work on additional lists will receive the flat<br />
payment of £100.<br />
If you have any queries or concerns about<br />
this please contact your Group Senior<br />
Management Team in the first instance.<br />
8<br />
HB <strong>February</strong> <strong>2018</strong>.indd 8 20/02/<strong>2018</strong> 11:38
Bethan learns about healthcare in India<br />
Kind-hearted Bethan Downing has<br />
revealed how she devoted her time to<br />
helping patients and children in India<br />
during a three-week long volunteering<br />
project.<br />
Bethan, Deputy Director of Organisational<br />
Development, flew out to New Delhi where<br />
she saw first-hand how healthcare services<br />
are run. <strong>Heartbeat</strong> caught up with Bethan<br />
following her return from India to find out<br />
more about her trip.<br />
“I took part in a range of the volunteering<br />
projects, which were supporting some of<br />
the poorest people in India,” said Bethan.<br />
“The aim of the projects is to provide a<br />
sustainable solution to improving health,<br />
wellbeing and education in very poor<br />
communities. Many of the projects are<br />
directly supporting slum communities<br />
including; clinics, schools, community<br />
centres and orphanages.<br />
“I volunteered in two orphanages and just<br />
loved it! Spending time with the children<br />
was so uplifting for me. The simplicity of<br />
time and offering love and support has such<br />
a huge impact.<br />
“I met one child in an orphanage who had<br />
a disability and could not walk. He valued<br />
his education so much and his English was<br />
better than mine and at the age of 12! He<br />
gave me a lesson in physics that I will never<br />
forget. His outlook on life was to embrace<br />
it, learn, grow and enjoy it – he taught me<br />
so much!”<br />
One of the things that stood out for Bethan<br />
was how resourceful the people were with<br />
very little and sometimes nothing.<br />
She said: “I watched the children play and<br />
the games are so creative and just require<br />
imagination. I watched the GP who is also<br />
the pharmacist see many patients in a clinic.<br />
She had very limited equipment to diagnose<br />
and is very reliant on her experience and<br />
asking the right questions to get to the<br />
diagnosis rather than having access to a<br />
suite of diagnostic equipment.”<br />
Beth Downing, Deputy Director of<br />
Organisation Development spent time in an<br />
Indian orphanage<br />
CORPORATE AND<br />
GENERAL NEWS<br />
Bethan said that the trip has had a<br />
positive effect on her and made her<br />
look at life a bit differently. She is also<br />
planning to keep supporting the charity<br />
she volunteered with.<br />
“It’s incredible to see how having<br />
less changes your focus and in a way<br />
takes away the complexity of having<br />
lots of choices in lots of different life<br />
scenarios,” said Bethan.<br />
“I came home and pretty much the<br />
first thing I did was empty my house of<br />
everything I haven’t used and re-stocked<br />
the local charity shop – it felt so good!”<br />
“We tend to have lots of material things<br />
but my observation is that having less is<br />
sometimes having more.”<br />
Bethan added: “Although the project<br />
has achieved some amazing results,<br />
they are at the point now where they<br />
can maintain the great work they have<br />
been doing. But they are struggling to<br />
see a sustainable way to scale up what<br />
they do to help more orphans and more<br />
communities. This is something I hope<br />
to be able to support the charity with<br />
moving forward.”<br />
Snail mail to email: The move to digital<br />
delivery of letters<br />
The wait for appointment letters,<br />
referrals and results, amongst other<br />
correspondence is often frustrating for<br />
patients who are keen to progress their<br />
care and get on with their lives. Waiting<br />
a couple of days for a letter can seem<br />
like an eternity when your health or the<br />
health of a loved one is involved.<br />
Whilst process changes have taken place<br />
within our organisation to reduce the time<br />
it takes for letters to be written and sent<br />
to patients, until now we have had little<br />
influence over the time taken for letters<br />
to progress through the postal system.<br />
However, a team made up of colleagues<br />
from across our organisation have been<br />
tasked with developing a means for patients<br />
to receive their letters by email.<br />
The new system which is currently under<br />
development looks to centralise both the<br />
printing and distribution of letters, moving<br />
away from individual departments printing<br />
and posting their own letters to a central<br />
print and distribution function where<br />
patients are able to opt to have their letters<br />
delivered by post or by email.<br />
Deputy Chief Operating Officer for Planned<br />
Care, Liam Kennedy is leading the project.<br />
He said: “Putting patients in control of how<br />
they receive letters and correspondence<br />
from our organisation is one of our priorities<br />
this year, as technology has evolved and<br />
patients have access to smartphones,<br />
the need for us to be able to deliver<br />
correspondence promptly has become vital.<br />
“Annually we send out over 1.8 million<br />
letters which can take between two to three<br />
days to reach patients. Not only is this slow<br />
and time consuming, it’s also extremely<br />
costly – we spend over £800,000 on print<br />
and postage.<br />
“We have found that patients are keen to<br />
communicate over email as opposed to<br />
printed letters, so now is the ideal time to<br />
develop this function.<br />
“The new system is scheduled for<br />
completion in Summer <strong>2018</strong> and will<br />
complement, Unity, our new electronic<br />
patient record and the Winscribe digital<br />
dictation and speech recognition system,<br />
completing an end to end digital workflow,<br />
enabling colleagues to easily access patient<br />
data, compose correspondence and deliver it<br />
digitally at the click of a button.”<br />
For more information regarding the<br />
plans to develop email correspondence<br />
please contact Liam Kennedy, Deputy<br />
Chief Operating Officer, Planned Care on<br />
liam.kennedy@nhs.net<br />
9<br />
HB <strong>February</strong> <strong>2018</strong>.indd 9 20/02/<strong>2018</strong> 11:38
Making adjustments to support<br />
colleagues at work<br />
CORPORATE & GENERAL NEWS<br />
Conflict Resolution Trainer, Richard<br />
Burnell has recently been appointed<br />
Chair of our disability and long term<br />
conditions staff network. In this<br />
issue of <strong>Heartbeat</strong>, he has bravely<br />
shared his story to raise awareness<br />
of the importance of supporting<br />
those with a disability or long term<br />
condition within our organisation.<br />
Richard, who joined us in 2009 was<br />
diagnosed with bipolar disorder in 2011,<br />
this means he experiences periods of<br />
depression and periods of hypomania.<br />
“My condition is what they call rapid<br />
cycling bipolar,” Richard told <strong>Heartbeat</strong>.<br />
“This means that my mood can<br />
change from one day to the next,<br />
and sometimes I can suffer bouts<br />
of depression and then hypomania<br />
within the same day. When I am in the<br />
depression cycle, I have chronic anxiety –<br />
I have sweaty palms, dry mouth and feel<br />
really fatigued.<br />
“The best way I can describe mania is<br />
feeling really excited all of the time and<br />
doing everything in double speed. It<br />
can create a lot of stress as you end up<br />
saying yes to everything and then being<br />
unable to complete what you have said<br />
you will do.”<br />
When he was first diagnosed, Richard<br />
struggled to understand his diagnosis.<br />
“I was embarrassed,” he said. “I thought<br />
that it was a form of weakness and I was<br />
worried about how I would continue to<br />
do my job. I did a lot of teaching in the<br />
mornings, and this seemed to be when I<br />
was at my worst.”<br />
He knew that he couldn’t go on without<br />
talking to his line manager.<br />
“When I made the decision to talk to John<br />
(Rigby) I was incredibly nervous, but he was<br />
brilliant. I said ‘John, I have been diagnosed<br />
with a mental health condition, but I don’t<br />
want anyone to know.’<br />
“Straight away, John found us a private<br />
room so that I would feel safe to discuss my<br />
issues. He just said ‘what can I do to help?’<br />
and from that moment on he has been<br />
incredibly supportive of me.”<br />
Together Richard and John came up with<br />
a plan which would support Richard to<br />
manage his illness and his work better. John<br />
suggested that Richard could be flexible<br />
with his start times.<br />
“I explained that mornings were the worst<br />
time for me,” said Richard.<br />
“So we agreed that I could take a flexible<br />
approach to my work hours and start at<br />
10am and work through to 6pm. John<br />
also sets my monthly targets, but is flexible<br />
on how I achieve them. He understands<br />
that I will achieve a lot more on a good<br />
day as opposed to when I am suffering a<br />
particularly bad day.”<br />
“John also gives me adequate notice of<br />
any changes that may be happening. He<br />
understands that it could affect me if he<br />
drops something on me suddenly.”<br />
Richard now handles his illness a lot better<br />
than when he was first diagnosed and<br />
recognises the part that John has played in<br />
this.<br />
He said: “I could never have got to this<br />
point without John’s support. He is<br />
understanding of my illness and shows<br />
confidence in me to perform well in my job<br />
with some slight adjustments.”<br />
Richard is delighted to have been<br />
appointed chair of the disability and long<br />
term conditions staff network and he<br />
is hoping to encourage colleagues who<br />
may be struggling themselves to have the<br />
courage to seek support from either the<br />
network or their line manager.<br />
“The network is there to advise both the<br />
organisation and individual colleagues,”<br />
Richard said to <strong>Heartbeat</strong>.<br />
He added: “I would like to encourage<br />
colleagues to speak up if they are<br />
experiencing any issues relating to a<br />
disability or long term condition. There is<br />
no need to feel embarrassed or ashamed.<br />
Talking things through with your manager<br />
can help you to understand the impact<br />
on your role and put strategies in place to<br />
support you.”<br />
John is delighted to see Richard doing<br />
so well now. He said: “There is a stigma<br />
attached to mental health that should not<br />
be there; it is an illness along with many<br />
other illnesses that can be managed in the<br />
workplace with time and understanding.<br />
“I am glad that Richard had the confidence<br />
in me to speak out so that we could<br />
together devise a plan that supports him<br />
and gives the organisation an effective<br />
member of staff.”<br />
If you would like to speak to someone<br />
regarding a disability or long term<br />
condition, please contact either Richard<br />
(richard.burnell@nhs.net) or Stuart<br />
Young, Head of Diversity and Inclusion<br />
(stuartyoung1@nhs.net).<br />
L-R: John Rigby, Mandatory Training Manager has made adjustments at work to support Richard Burnell, Conflict Resolution Trainer<br />
10<br />
HB <strong>February</strong> <strong>2018</strong>.indd 10 20/02/<strong>2018</strong> 11:38
Huge honours for two clinical<br />
colleagues<br />
Professor Elizabeth Hughes has been<br />
awarded an honorary fellowship of the<br />
Royal College of General Practitioners<br />
Two of our clinical colleagues have<br />
recently been awarded fellowships<br />
from the Royal College of General<br />
Practitioners (RCGP) and the Royal<br />
Pharmaceutical Society.<br />
Consultant Chemical Pathologist, Professor<br />
Elizabeth Hughes, who is also a Regional<br />
Dean and Director of Education and<br />
Quality within Health Education England,<br />
was awarded an honorary fellowship by<br />
the RCGP in recognition of her work in<br />
supporting and developing general practice,<br />
including the development of innovative<br />
roles within primary care.<br />
Professor Helen Stokes-Lampard, Chairman<br />
of the RCGP said: “Liz is someone who<br />
really understands primary care and was<br />
committed to ensuring the highest quality<br />
education for doctors and other healthcare<br />
professionals to ensure the best possible<br />
care for patients.”<br />
Professor Hughes, who was presented with<br />
her award by President of the RCGP, Dr<br />
Terry Kemple was delighted to receive the<br />
honour. She said: “It is a huge honour for<br />
me to receive an honorary fellowship for<br />
the RCGP. It is the highest award that the<br />
college can give to a person who is not a GP<br />
and only three to five are given out per year,<br />
so naturally I am delighted.”<br />
Emma Graham-Clarke, Consultant<br />
Pharmacist in Critical Care, was one of<br />
27 new fellows appointed by the Royal<br />
Pharmaceutical Society (RPS) at the end of<br />
last year. The RPS stated: “Being appointed<br />
a fellow of the RPS is one of the highest<br />
honours that can be bestowed upon society<br />
members. It recognised the distinction<br />
members have attained in a particular<br />
aspect or aspects of their pharmacy career.”<br />
Nominations for fellows are submitted by<br />
members and have to be supported by two<br />
Connected communications at<br />
your fingertips<br />
CORPORATE & GENERAL NEWS<br />
other people, before being reviewed by<br />
a panel.<br />
Liz, Emma was delighted to receive the<br />
award: “I received a letter in the post<br />
which stated the panel’s decision was<br />
that I should become a fellow of the RPS<br />
for distinction in the field of pharmacy –<br />
I was both shocked and delighted!<br />
“The fact that nominations and support<br />
comes from my fellow professionals<br />
makes it all the more special.”<br />
Emma Graham-Clark has been appointed as<br />
fellow of the Royal Pharmaceutical Society<br />
Are you one of the many colleagues<br />
who spend most of their time on their<br />
feet, away from your desk and rarely<br />
able to login to a computer? Feeling left<br />
out and unaware of developments in<br />
our organisation?<br />
We will soon be launching an app which will<br />
be enable you to access all of the important<br />
information currently available on Connect<br />
but most importantly, on your phone and<br />
available wherever you are.<br />
Whether you’re keen to keep up to date<br />
with corporate communications, eager<br />
to know what is going on in a specific<br />
department or looking for a means to<br />
share your news with colleagues, the new<br />
MyConnect app is set to revolutionise<br />
communication within our organisation.<br />
Unveiling the MyConnect app, Ruth Wilkin<br />
Director of Communications said: “I’m<br />
delighted to launch the new MyConnect<br />
app as it finally gives all colleagues a means<br />
to keep up to date with developments in<br />
our organisation.<br />
“Most importantly, colleagues who wouldn’t<br />
easily have access to desktops and laptops<br />
to access news and information on Connect<br />
will now have the ability to access this<br />
through an app as well as being able to setup<br />
alerts and notifications.”<br />
The MyConnect app is compatible with both<br />
iPhones and Android handsets, and will<br />
be available to download from the Apple<br />
Appstore as well as the Google Playstore.<br />
Details on when you can download and<br />
access the MyConnect app will be shared<br />
through the Communications Bulletin.<br />
If you have any questions on how the app<br />
will work or if you would like to be able to<br />
share your content through the app, contact<br />
Subtan Mahmood, Internal Communications<br />
Manager on Subtan.Mahmood@nhs.net or<br />
extension 4840.<br />
11<br />
HB <strong>February</strong> <strong>2018</strong>.indd 11 20/02/<strong>2018</strong> 11:38
Youngsters are ready to get creative for<br />
Midland Met<br />
CORPORATE & GENERAL NEWS<br />
Excited schoolchildren were<br />
invited to the launch of the<br />
Midland Metropolitan Hospital’s<br />
art competition which will see the<br />
winning designs immortalised within<br />
the children’s department of the new<br />
building.<br />
Youngsters and teachers from schools<br />
across Sandwell and West Birmingham<br />
attended the event, held at The<br />
Education Centre at Sandwell Hospital<br />
last month.<br />
They were tasked with creating<br />
superheroes, explorers and astronomers<br />
for the walls of the new £350 million<br />
hospital, and spread the word about the<br />
competition to their fellow pupils.<br />
The competition is being run by Your<br />
Trust Charity.<br />
In total, six characters will be featured.<br />
They will be male and female versions of<br />
superheroes, astronomers and explorers.<br />
The astronomers will be in a children’s<br />
ward, the explorers will be painted onto<br />
the walls in the children’s outpatients<br />
department, whilst the superheroes<br />
will feature in the paediatric emergency<br />
department and also within the other<br />
children’s wards.<br />
The designs will flow throughout their<br />
allocated department.<br />
Logan Heard, aged seven, who attends<br />
Ferndale School, in Great Barr, said he has<br />
already started work on his design.<br />
The youngster, who came dressed as<br />
Batman to the launch, said: “I love<br />
drawing and I’ve got an idea for the<br />
character I want to create.”<br />
His mum Amber added: “Logan spent a<br />
lot of time in hospital as he was diagnosed<br />
with a Wilms Tumour. He is now in<br />
remission, but this is his way of giving<br />
something back to the NHS which has<br />
helped him so much.”<br />
Ruth Billingham, Assistant Head Teacher<br />
at Holyhead Primary Academy in<br />
Wednesbury, was also at the event. She<br />
said: “This is a great way of involving<br />
children in the creation of their hospital. I<br />
think there will be many youngsters eager<br />
to take part in this competition and we<br />
will be passing on the details through an<br />
assembly.”<br />
Would-be explorer Rubyrose Millard,<br />
from Mesty Croft Primary School, also in<br />
Wednesbury, added: “I like drawing or<br />
doing anything that is creative. I think the<br />
idea of us designing our own characters for<br />
the new hospital is good as we know what<br />
will make children feel better if they were<br />
poorly in hospital.”<br />
Amanda Winwood, Membership Academy<br />
Manager for Your Trust Charity, said: “The<br />
launch was a huge success and the children<br />
who attended were very keen on getting<br />
straight to work in creating their characters.<br />
“It was lovely to see how enthusiastic they<br />
were. The teachers who attended were also<br />
happy to promote the competition.<br />
“The competition is also open to the<br />
children of colleagues, so please do<br />
encourage your little ones to get drawing.<br />
“It’ll be a real privilege for the winners to<br />
see their own creations up on the walls of<br />
Midland Met.”<br />
The closing date for competition is 29<br />
March. To enter please contact Amanda<br />
Winwood on amanda.winwod@nhs.net<br />
or extension 4847.<br />
L-R: Logan Heard (7) Rubyrose Millard (10) and Erin Oakley (5) all donned their costumes for the launch of the Midland Met art competition<br />
Free NHS Health Checks now available<br />
across our sites<br />
Health checks are now being offered<br />
for free at City, Sandwell and Rowley<br />
Hospitals.<br />
Checks include height measurement,<br />
weight, blood pressure, pulse, cholesterol,<br />
glucose as well as lifestyle questionnaires.<br />
Health and Wellbeing Manager, Jenny<br />
Wright said: “We are delighted to be<br />
working with Mytime Active to offer these<br />
free health checks to colleagues. The<br />
checks are for any colleague aged between<br />
40 and 74 and aim to help prevent heart<br />
disease, stroke, diabetes, kidney disease and<br />
dementia.”<br />
The health checks will be provided subject<br />
to eligibility criteria. Appointments are for<br />
approximately 30 minutes and must be<br />
booked with Jatinder Sekhon on extension<br />
3306. Evening appointments are available<br />
and checks can also be delivered in wards<br />
and departments.<br />
12<br />
HB <strong>February</strong> <strong>2018</strong>.indd 12 20/02/<strong>2018</strong> 11:38
When terror strikes…colleagues test<br />
our major incident plan<br />
A devastating and bloody scene at<br />
New Square Shopping Centre in West<br />
Bromwich set the scene for a wide scale<br />
test of our emergency response earlier<br />
this month. With a ‘terrorist attack’<br />
striking at the heart of our population<br />
going about their normal business, we<br />
were forced to swing into major incident<br />
response.<br />
The Civil Contingency Act 2004 requires our<br />
organisation to carry out a major incident test<br />
once every three years, testing our plans and<br />
capturing any learning in a safe environment,<br />
so we can be ready to respond effectively if<br />
the worst should happen.<br />
Departments across the organisation were<br />
put to the test, including security, theatres,<br />
emergency department teams, pharmacy,<br />
communications and management.<br />
Strategic command was set up and led by<br />
Chief Informatics Officer, Mark Reynolds,<br />
while tactical command was run by<br />
Deputy Chief Nurse, Paul Hooton. The<br />
communications team played a dual role,<br />
being both poacher and gamekeeper, with<br />
team members advising both strategic and<br />
tactical commands on communications<br />
‘Casualty’ Mike Beech, Senior Charge Nurse<br />
on AMU is treated at A&E<br />
strategy while others took on the role of a<br />
particularly aggressive TV crew.<br />
Colleagues from across the organisation<br />
volunteered to take the role of casualty<br />
with Siân Davies, Speech and Language<br />
Therapy Assistant commenting: “It was<br />
really interesting to see how effectively the<br />
team coped when faced with an influx of<br />
casualties. It was a great way to spend my<br />
Sunday morning.”<br />
Community Midwife, Amanda Jowett<br />
agreed, she said: “My son Jenson and I<br />
took part as casualties, as Jenson is fond<br />
of drama at school and this gave him a<br />
great opportunity to act. But the serious<br />
side is seeing how our organisation<br />
has plans in place to switch smoothly<br />
into major incident mode. That is very<br />
CORPORATE & GENERAL NEWS<br />
reassuring to see.”<br />
Phil Stirling, Emergency Planning Officer<br />
said: “We regularly test our plans on a<br />
smaller scale, but this was our big one. It<br />
could be the difference between life and<br />
death for some if we do not get it right,<br />
so we must ensure that we have the<br />
right procedures in place to deal with an<br />
attack of this kind and on this scale.<br />
“During the exercise we saw how<br />
quickly a scenario can escalate, and<br />
how important it is that the situation is<br />
handled very carefully, so our patients,<br />
visitors and colleagues are protected.<br />
“Observers from NHS England watched<br />
the event unfold and judged our<br />
response to be correct, making the<br />
exercise a success.<br />
“Many thanks to colleagues who took<br />
part and to the volunteers (many of our<br />
own team) who gave up their morning<br />
to come in and help us.”<br />
Introducing Unity Digital Champions<br />
As our organisation gears up for<br />
the implementation of Unity (our<br />
new electronic patient record) there<br />
is a range of training taking place,<br />
which will ensure that colleagues<br />
understand how Unity will be used<br />
within their role and department.<br />
Over 500 colleagues, from all parts of<br />
the organisation have signed up to be<br />
digital champions. These colleagues will<br />
offer support during key parts of the<br />
journey to Unity going live, including<br />
full dress rehearsal and cutover. They<br />
will receive two training sessions, one<br />
which will give an overall introduction to<br />
Unity and the second part will look more<br />
specifically at how different roles will<br />
interact with the system.<br />
<strong>Heartbeat</strong> caught up with two digital<br />
champions from Lyndon 5, Ward<br />
Clerk, Jayne Fergusson and Discharge<br />
Coordinator, Anne Parker to find out<br />
more about the training.<br />
“The training was really good,” Anne<br />
told <strong>Heartbeat</strong>.<br />
“We had an overview of the new system<br />
– we looked at it both from a nurse’s<br />
perspective and a doctor’s perspective.”<br />
Jayne added: “In the next session we will<br />
be looking more specifically at all the roles<br />
which will be using the system, so that we<br />
are able to support our colleagues once it<br />
has gone live.”<br />
Both Anne and Jayne believe that the<br />
introduction of Unity will make a real<br />
difference to both colleagues and patients.<br />
“Everybody involved in the care of the<br />
patient will be able to see all of their<br />
information in one place,” said Anne.<br />
“It will bring everything together,” said<br />
Jayne. “Unity will make us work much better<br />
in unison.”<br />
Another lot of training which will be<br />
launching soon is the early adopter training.<br />
These sessions are for colleagues who will be<br />
involved in the full dress rehearsal (FDR) of<br />
Unity which will take place over three weeks<br />
from 9 – 27 April.<br />
During week two (16-20 April) of the<br />
FDR, colleagues will use the system in a<br />
live setting. This means a small number of<br />
nurses/midwives, healthcare assistants and<br />
ward clerks will work with both our current<br />
systems and Unity at the same time.<br />
In order for FDR to be successful, we need<br />
L-R: Ward Clerk, Jayne Fergusson and Discharge<br />
Coordinator, Anne Parker have both attended<br />
digital champion training<br />
in colleagues who will be using it during<br />
the week to book onto the early adopter<br />
training. All areas must ensure they identify<br />
a nurse (or midwife), HCA and a ward clerk<br />
to be part of the training and book them on.<br />
These should be colleagues who are rostered<br />
for 16-20 April.<br />
Full details of the early adopter training<br />
sessions can be found on the back page<br />
of this month’s edition of <strong>Heartbeat</strong>.<br />
13<br />
HB <strong>February</strong> <strong>2018</strong>.indd 13 20/02/<strong>2018</strong> 11:38
Focus on<br />
New electronic patient record will unify clinical records<br />
enabling consistency of care<br />
Later this year many of our clinical systems will change to Unity.<br />
This significant change to the way we work brings a range of<br />
benefits including:<br />
• Providing one integrated IT solution supporting a range of<br />
best practice care from acute to emergency<br />
• Improvement in the legibility of health records.<br />
When Unity has been successfully launched and is being widely<br />
used it will bring about even more benefits including:<br />
• Reduction in missed appointments<br />
• Prevention of duplicate investigations and repetition of<br />
patient information.<br />
<strong>Heartbeat</strong> caught up with Chief Informatics Officer, Mark<br />
Reynolds who explained more.<br />
“The new electronic patient record has been named Unity as it<br />
will unify clinical records so we are able to work together in an<br />
integrated way,” said Mark. “Unity will replace electronic systems<br />
including CDA, eBMS, PatientFirst and iCM and importantly, will<br />
Unity<br />
will be used by<br />
over<br />
5,500<br />
Unity is coming to you – be prepared<br />
colleagues<br />
enable the delivery of consistency of care across our services.<br />
January saw the completion of the first stage of integration<br />
testing and the move to the second stage.<br />
“During stage two we test that the system works with our other<br />
IT, processes and procedures,” added Mark. “We will complete<br />
the second stage at the end of <strong>February</strong> and will use the month<br />
of March for any final bug fixing. We’ve also started to train<br />
colleagues who will take the lead with Unity, known as digital<br />
champions.”<br />
In April, Mark’s team is also planning for a full dress rehearsal<br />
(FDR) of Unity - a test of Unity in our clinical services to identify<br />
issues and drive out risk before the go-live.<br />
“During FDR, technical teams will carry out the full breadth of<br />
their activities (apart from switching any systems off),” said Mark.<br />
“For operational teams it’s an opportunity to verify that Unity<br />
works in a business as usual context.<br />
“We’ve agreed that FDR will occur from 9 to 27 April. During<br />
the week commencing 16 April clinical colleagues across the<br />
organisation will use Unity alongside existing clinical systems.”<br />
This is an exciting time for our workplace as we get ready<br />
for this change. For the launch of Unity to be successful<br />
we all must ensure we are prepared. To help with this, a<br />
readiness checklist has been produced as guide to support<br />
teams. The checklist contains the main information and<br />
actions that departments need to take in order to be<br />
ready for Unity. Each ward/department/team will receive<br />
their own checklist.<br />
Team readiness checklist<br />
The checklist belongs to your department, so assign someone within<br />
your team to be in charge of it and store it somewhere safe. How you<br />
get your checks is up to you. You may ask different team members<br />
to focus on a particular area or set up a small group to work through<br />
them all. Accountability for progress with readiness preparation and<br />
associated reporting sits with the ward/department manager.<br />
Getting ready for Unity should be a team effort – the checklist is an<br />
excellent way of engaging colleagues, stimulating discussion about<br />
Unity and starting to address people’s questions and concerns.<br />
You won’t be able to complete each check straight away – many<br />
are tied to particular phases of the project so may not be available<br />
immediately.<br />
Your personal checklist<br />
The success of Unity is dependent upon all of us. You need to:<br />
• Ensure you have basic IT skills<br />
• Ensure you have a network login in your name – generic logins<br />
will not be supported by Unity<br />
• When requested promptly register for digital champion and end<br />
user training - it is expected that 5,500 colleagues will be trained<br />
so it’s important this goes well.<br />
• Attend the training – it will be difficult to reschedule later on as<br />
courses will be busy<br />
• Participate in discussions about Unity in teams and directorates<br />
• Keep up to date with the information published on the Trust in<br />
Digital section on Connect.<br />
The checklists will be issued at day two of the digital<br />
champion training, but are also available to download from<br />
the Trust in Digital page on Connect.<br />
Did you know?<br />
• Computers are updated<br />
regularly to ensure they<br />
are safe and secure. Your<br />
computer will receive<br />
updates overnight even if it<br />
is shutdown, however it must<br />
be plugged in and switched<br />
on at the wall. We will wake<br />
it up remotely, update it and<br />
then shut it down again.<br />
Please do not turn off wall<br />
sockets.<br />
• The most common calls<br />
to the IT helpdesk are for<br />
password resets yet with a<br />
little prep you can reset your<br />
own passwords. For email<br />
passwords see the guide at<br />
http://bit.ly/2xUS0sN. For<br />
log on passwords to access<br />
the network you can use the<br />
SpecOps password reset tool.<br />
To register, go to<br />
http://bit.ly/2xXqxqp.<br />
• Informatics will provide<br />
additional computers to<br />
support Unity. The team<br />
rolled out 50 new computers<br />
on wheels in early <strong>February</strong><br />
and have another 160<br />
being built. Floor plans for<br />
each clinical area showing<br />
equipment to be provided<br />
have been published on<br />
Connect.<br />
Sandwell and West<br />
Birmingham Hospitals<br />
NHS Trust<br />
Lots of information is available on Connect including<br />
an overview of Unity, quickstart guides, videos and<br />
information on training. If you want to know more it’s<br />
a good place to start. If you have a question, please<br />
contact swbh.trustindigital@nhs.net.<br />
HB <strong>February</strong> <strong>2018</strong>.indd 14-15 20/02/<strong>2018</strong> 11:38
Measles: How to<br />
Stay Safe<br />
The best protection is<br />
Measles is on the rise –<br />
2 doses of the safe,<br />
effective MMR<br />
vaccine at 1 year of<br />
are you protected? age, and 3 years, 4<br />
CORPORATE & GENERAL NEWS<br />
Measles is a highly infectious viral<br />
illness that can be very unpleasant<br />
and sometimes lead to serious<br />
complications. It used to be fairly<br />
uncommon in the UK due to the<br />
effectiveness of vaccination, but<br />
unfortunately it is now on the rise<br />
again.<br />
months<br />
Subsequent studies have found no link<br />
between the vaccine and autism.”<br />
In order to be protected If you have against not had measles, a<br />
person requires two doses, you of the cancombined<br />
get them free from<br />
MMR vaccine, which also protects you<br />
your GP surgery<br />
against mumps and rubella. The vaccines<br />
are given one month apart.<br />
“Many people are unsure if they have had<br />
Know the<br />
the two vaccines,” explained Tracy.<br />
symptoms!<br />
“And we have also Keep found people that withmany of<br />
our colleagues are symptoms not fully away protected,<br />
<strong>Heartbeat</strong> spoke to Tracy Lees,<br />
which puts them, from their others colleagues and our<br />
Occupational Health and Wellbeing Nurse patients at risk.<br />
Manager to find out more. “There has “Measles is highly infectious, a cough or a<br />
been a rise in measles in the UK over the sneeze can spread the measles virus over a<br />
last few months,” said Tracy.<br />
wide area. If you Call come ahead into before contact with it<br />
going to A&E<br />
“In fact, the West Midlands is one of and are not protected, the chances are that<br />
or your GP<br />
five hotspot areas for outbreaks. One you will be infected.<br />
of the main reasons for the rise in cases “My question to colleagues is – are you<br />
is that there is a cohort of people who protected? If not, please contact your GP or<br />
didn’t receive the vaccine as children due occupational health to find out – it is better<br />
to the concerns about its link to autism, to be safe and check than to contract<br />
following a study in 1998 by Dr Andrew measles.<br />
Wakefield.<br />
“If you have not received both does of the<br />
“The work of Dr Wakefield has since been vaccine, please contact us as soon as you<br />
completely discredited and he has been are able to and we can arrange an<br />
struck off as a doctor in the UK.<br />
STOP<br />
Symptoms<br />
of Measles<br />
Rash<br />
Temperature<br />
Runny Nose<br />
Red Eyes<br />
Cough<br />
appointment for you. If there are a number<br />
of you in the department, we can arrange<br />
for a nurse to come to you to administer<br />
the vaccine.”<br />
For any further concerns or questions<br />
on the MMR vaccination please contact<br />
the occupational health service on<br />
extension 3306.<br />
To: Medical Illustration<br />
Shout out is a way for colleagues<br />
to be recognised for their excellent<br />
work, delivering first class<br />
healthcare to our patients.<br />
If you believe a member of your team,<br />
or someone from elsewhere in the<br />
organisation deserves a mention please<br />
visit Connect to give them a shout out.<br />
They may have gone out of their way<br />
to help you with something or you may<br />
have witnessed them make a difference<br />
to a patient or colleague.<br />
To: Tracey Dixon<br />
Tracey is a community staff nurse<br />
working in the Mesty North district<br />
nurse team. She is a fantastic role model<br />
and has an excellent rapport with<br />
patients. She quickly gains trust and<br />
patients love her down to earth and no<br />
nonsense ways. Her unique skills get the<br />
best out of patients and they often ask<br />
‘when is Tracey coming?’ One student<br />
commented at a careers fair recently: ‘I<br />
want to be like Tracey!’<br />
From: Beverley Callaghan<br />
The team is always friendly, provides<br />
customer focused, high quality and<br />
innovative services e.g. graphic design,<br />
electronic forms and printing which<br />
are not only effective but ‘warm’ and<br />
audience friendly – thank you!<br />
From: Essie Li<br />
To: Joanne Brookes<br />
We were very fortunate to have her<br />
contribute to the high turnover of<br />
patients who required x-ray. A fine<br />
addition to the portering team which<br />
can be a thankless job. It’s not always<br />
straightforward getting a patient from<br />
A to B. Hope you feel appreciated.<br />
From: Happy Radiographers<br />
To: Mary Causer and D15 Team<br />
Thank you to Mary Causer and<br />
colleagues on D15 for the support they<br />
provided to the team on D16 during<br />
a particularly difficult day earlier<br />
this month. Their acts of kindness<br />
made a huge difference and is much<br />
appreciated.<br />
From: Elaine Newell<br />
To: Nicola Ager<br />
We wanted to say a big thank you to<br />
Nicola for holding the fort before our<br />
new manager was appointed. Also,<br />
for all her hard work facilitating the<br />
opening of our newly refurbished<br />
library at Sandwell.<br />
From: Library Services Team<br />
To: Dr Josie White<br />
Went above and beyond in discharging<br />
a patient who was extremely vulnerable<br />
and homeless!! Showed exceptional<br />
compassion and selflessness ensuring<br />
the lady was discharged safely.<br />
From: Hayley Barnes<br />
To: Adam Wylie and Rob Kemp<br />
They helped make an office move an<br />
exceptionally smooth process, even<br />
when I was requesting additional ad<br />
hoc jobs on the day.<br />
From: Sam Banwell<br />
16<br />
HB <strong>February</strong> <strong>2018</strong>.indd 16 20/02/<strong>2018</strong> 11:38
Patient becomes UK-first after<br />
undergoing pioneering eye op<br />
SURGICAL SERVICES<br />
Patient Daniyaal Farooq, with Mr Imran Masood<br />
A 20-year-old man has become the first<br />
in the UK to undergo a sight-saving<br />
operation at Birmingham and Midland<br />
Eye Centre (BMEC).<br />
Daniyaal Farooq, from Yardley, was<br />
diagnosed with glaucoma after he was<br />
plagued with excruciating headaches and<br />
blurred vision which affected his work. The<br />
pressure in his eyes was dangerously high<br />
and he was close to going completely blind<br />
in his left eye.<br />
However, quick-thinking Daniyaal booked<br />
himself in for an eye test and was ordered<br />
by his optician to go to the emergency<br />
department at BMEC.<br />
Once there, he was diagnosed with<br />
glaucoma – which is rare in a person<br />
as young as Daniyaal. In a follow up<br />
appointment with Mr Imran Masood,<br />
Consultant Ophthalmic Surgeon, he was<br />
told that he would need to undergo an<br />
operation in his left eye, followed by his<br />
right.<br />
But instead of the risky Trabeculotomy<br />
procedure, Mr Masood suggested a<br />
more advanced and minimally invasive<br />
technique – GATT (Gonioscopic Abinterno<br />
Transluminal Trabeculotomy) surgery.<br />
The operation was carried out on Daniyaal<br />
in November, and he became the first<br />
patient in the UK to undergo the procedure.<br />
“When I first started getting the headaches,<br />
I thought I’d simply be told to wear<br />
glasses,” Daniyaal explained.<br />
“I never thought I’d become the first<br />
patient in the country to have a unique<br />
operation for a condition that normally<br />
affects older people.<br />
“When I was told I had glaucoma I was very<br />
shocked as no one in my family has it. But it<br />
explained why the headaches were so bad<br />
and my vision was blurry. There was still<br />
time to save the sight in my left eye, if I had<br />
this operation.”<br />
Glaucoma occurs when the drainage<br />
channels in the eye become blocked<br />
How the GATT procedure works:<br />
The usual method to tackle<br />
Daniyaal’s problem would involve a<br />
Trabeculectomy, which would bypass<br />
the eyes normal drainage system<br />
creating drainage under the upper<br />
eyelid. This surgery carries some<br />
risk which is increased in younger<br />
patients. These include bleeding<br />
during surgery, and in particular<br />
dangerously low pressure after the<br />
procedure.<br />
GATT surgery is a minimally invasive<br />
procedure where a tiny catheter<br />
is passed into Schlemm’s canal<br />
(The eye’s natural drainage canal).<br />
resulting in an increase in the eyepressure.<br />
If not treated, the pressure<br />
can damage the optic nerve and this<br />
can lead to permanent blindness in the<br />
affected eye.<br />
Mr Masood explained: “It is very rare for<br />
someone of Daniyaal’s age to have this<br />
condition and there was a significant risk<br />
of him becoming completely blind.<br />
“A typical surgical procedure would be<br />
a Trabeculectomy but it can be a risky<br />
operation particularly in young patients.<br />
It can result in the pressure in the eye<br />
going too low, resulting in loss of<br />
vision and the patient requiring further<br />
operations.<br />
“However, in Texas, in the United<br />
States surgeons have been carrying<br />
out Gonioscopy-Assisted Transluminal<br />
Trabeculotomy (GATT), for a few years<br />
and had published a paper citing its<br />
benefits in young patients.<br />
“It is a procedure with minimal risk.<br />
Daniyaal’s surgery went well in his left<br />
eye and we were able to save his sight.<br />
There were no side effects and we then<br />
carried out the same procedure in his<br />
right eye in January. He is doing really<br />
well.”<br />
Daniyaal added: “I don’t get the<br />
headaches anymore and my vision is<br />
better. I could have gone blind had I not<br />
acted in time, and I would advise anyone<br />
else suffering from the same symptoms<br />
as myself, to get checked out. I was<br />
lucky that my sight was saved, thanks to<br />
Mr Masood and the team at BMEC.”<br />
The canal is dilated and then the<br />
catheter is removed by pulling it<br />
through the abnormal wall of the<br />
canal thus opening the wall and<br />
allowing the fluid free access into<br />
Schlemm’s canal.<br />
This lowers the eye pressure and<br />
prevents blindness. A significant<br />
advantage of this operation is<br />
that it takes 15 minutes compared<br />
to about 60-90 minutes for the<br />
Trabeculectomy. The complication<br />
rate is very low with minimal impact<br />
on the vision following surgery.<br />
17<br />
HB <strong>February</strong> <strong>2018</strong>.indd 17 20/02/<strong>2018</strong> 11:38
Appeal for knitted boobs to help train<br />
breastfeeding support volunteers<br />
WOMEN’S AND CHILD HEALTH<br />
The infant feeding team are<br />
appealing for knitters to get creative<br />
by making breasts which will be<br />
used to help train up breastfeeding<br />
support volunteers.<br />
As well as a call for the knitted breasts,<br />
the team are also after newborn size<br />
dolls with soft bodies. They will be used<br />
to demonstrate the various ways of<br />
breastfeeding to the volunteers who will<br />
be on an eight week course learning<br />
how to support new mums.<br />
Louise Thompson, Infant Feeding Coordinator,<br />
said: “We will be increasing<br />
the amount of support that new mums<br />
have after they have just given birth<br />
at our hospital. We are doing this by<br />
carrying out an eight week training<br />
course which will ensure they learn all<br />
the basics of breastfeeding and peer<br />
support.<br />
“We know that breastfeeding is the<br />
healthiest way to feed your baby but<br />
eight out of 10 mums stop doing this<br />
before they want to. However, by<br />
carrying out this training, it means we<br />
will be able to give further help to mums<br />
on postnatal wards, so they can continue<br />
breastfeeding for as long as they want<br />
L-R: Infant Feeding Team Midwife, Kirsty Dunning, Volunteer Karen Gayle and Infant Feeding<br />
Coordinator, Louise Thompson<br />
to. The role will also support our midwives.”<br />
Louise added: “We will also give<br />
information on safe responsive bottle<br />
feeding for women who have made an<br />
informed decision to feed this way.”<br />
The volunteers will be based at our<br />
maternity department, which is housed at<br />
City Hospital, along with the midwifery-led<br />
birthing unit Serenity.<br />
Louise added: “The course will run for eight<br />
weeks and we already have quite a few<br />
volunteers who want to take part. Other<br />
areas we will cover are how to spot signs<br />
of effective feeding, and helping a mum<br />
to feel confident and know where to get<br />
support if they encounter difficulties.<br />
“We are looking for enthusiastic volunteers<br />
to complete the training and who can<br />
commit to volunteering a few hours a<br />
week. Breastfeeding experience is desirable<br />
but not essential.”<br />
If you would like to knit breasts for the<br />
team, or become a breastfeeding support<br />
volunteer, please contact Louise Thompson<br />
on 07982 242941.<br />
Streamlining surgical service is<br />
improving the patient journey<br />
SURGICAL SERVICES<br />
Being booked in for surgery can<br />
be an anxious and stressful time<br />
for patients who are unaware of<br />
the many pathways, processes and<br />
assessments involved, which often<br />
differ between specialties and<br />
departments.<br />
Tackling this issue head-on, a group of<br />
leaders from surgical services have been<br />
tasked with future proofing the group,<br />
reviewing all of the processes currently<br />
in place, with a view to unify and<br />
standardise the service for all patients.<br />
Embracing the challenge, the taskforce<br />
have focussed their efforts on the first port<br />
of call for most patients, the booking and<br />
scheduling of pre-operative assessments and<br />
total controlled infusions.<br />
To find out more about the changes<br />
to surgical services, <strong>Heartbeat</strong> caught<br />
up with Leann Coughlan. Directorate<br />
General Manager for Theatres, Pain and<br />
Anaesthetics. She said: “The booking of<br />
planned surgical activity differs across our<br />
organisation. This unfortunately leads to an<br />
inconsistent service and varied journeys for<br />
patients.<br />
“The variations in service also make it<br />
difficult for colleagues to support each other<br />
across specialties without having an indepth<br />
knowledge of each other’s respective<br />
processes.<br />
“The complex nature of all of the processes<br />
also has an effect on patients where we see<br />
multiple DNAs and cancellations due to poor<br />
booking and scheduling.“<br />
Keen to highlight plans for the future, Leann<br />
outlined where the future proofing plans<br />
would take surgical services, saying: “When<br />
our changes are implemented, we will have<br />
a more effective booking system which looks<br />
at the whole patient journey and implements<br />
standardised processes and practice across<br />
the group.<br />
“The changes aren’t simply an effort to<br />
improve efficiency, they’re a change from our<br />
traditional way of working to a new holistic<br />
approach which focuses on the needs and<br />
wants of the patients, ensuring they can<br />
be booked in for safe, effective and timely<br />
surgery.”<br />
18<br />
HB <strong>February</strong> <strong>2018</strong>.indd 18 20/02/<strong>2018</strong> 11:38
Tammy gets national news coverage<br />
after she lands new role<br />
National industry magazine The Nursing<br />
Standard put the spotlight on one of<br />
our colleagues in <strong>February</strong>, to find<br />
out more about her role within our<br />
organisation. Tammy Davies, Group<br />
Director of Primary Care and Community<br />
and Therapies, was featured in the<br />
publication’s section – the 60 Second<br />
Interview.<br />
Here’s the article in full:<br />
After qualifying as a nurse in 2001 Tammy<br />
worked in critical care and then coronary<br />
care, including as a palliative care heart<br />
failure nurse specialist. In 2015 she was<br />
appointed lead nurse in palliative and end of<br />
life care at Birmingham’s City Hospital before<br />
taking up her current role last year.<br />
Q. What are your main work<br />
responsibilities?<br />
Professional leadership for a range of<br />
specialist and community nurses and the<br />
quality, safety and experience of patients<br />
and carers.<br />
Q. How did you get your job?<br />
I was initially asked to take the interim<br />
position following the departure of the<br />
previous post holder. I thoroughly enjoyed<br />
the role and accepted the permanent<br />
position in December 2017.<br />
Q. Who are your clients/patients?<br />
Adult patients with a range of acute, chronic<br />
or life limiting illnesses cared for in the<br />
community setting.<br />
Q. What do you love about your job?<br />
The ability to develop services and improve<br />
quality of care and the experience of our<br />
patients. In addition I love supporting junior<br />
colleagues in developing their skills and<br />
careers.<br />
Q. What do you find most difficult?<br />
Lack of time – there are not enough hours<br />
in the day!<br />
Q. What is your top priority at work?<br />
To develop services that I would be happy<br />
for any of my own relatives to experience<br />
and to be a visible and supportive role<br />
model.<br />
Q. How have you developed your skills<br />
in this role?<br />
By having a role model who I can constantly<br />
learn from, but also by listening to feedback<br />
from patients and carers.<br />
Q. What has been your most formative<br />
career experience?<br />
Developing the palliative care service – this<br />
enabled me to gain an insight into new<br />
ways of working by learning from third<br />
sector organisations and to see beyond the<br />
healthcare model.<br />
Q. If you hadn’t become a nurse, what<br />
would you have done instead?<br />
I can’t imagine doing anything else – I love<br />
being a nurse and have enjoyed every role I<br />
have done.<br />
Q. What will be your next career move?<br />
My current role is very new and so my main<br />
aim is to consolidate my current knowledge<br />
and ensure that our community services are<br />
sustainable and fit for purpose.<br />
New duty radiologist system to<br />
streamline processes in imaging<br />
A new process, which will improve the<br />
way emergency patients and inpatients<br />
are managed by the imaging department<br />
was introduced earlier this month. The<br />
duty radiologist system will streamline<br />
the requesting process and reduce the<br />
number of calls needed to arrange a scan<br />
for a patient.<br />
Imaging Group Director, Dr Sarah Yusuf<br />
explained more: “Our new duty radiologist<br />
system means that one radiologist will take all<br />
the calls on that particular day, with a contact<br />
number on each site.<br />
“They will be responsible for vetting all the<br />
requests for emergency and inpatients, as well<br />
as vetting and protocolling the outpatients<br />
in priority order. This speeds up the booking<br />
process.<br />
“Whilst this means that colleagues on the<br />
wards do not have to ring for every scan, it also<br />
means that our other radiologists can report on<br />
scans without getting interrupted.“ Colleagues<br />
should request an x-ray or scan on iCM,<br />
ensuring that adequate clinical information is<br />
provided. The request will then be accepted,<br />
protocolled and scheduled without you having<br />
to discuss the case.<br />
“We aim to complete the vetting and<br />
scheduling process for urgent cases within 30<br />
minutes of receiving the request, and as soon<br />
possible for ED,” said Sarah.<br />
“Colleagues should remember to check the<br />
CRIS status before calling the departments for<br />
an update.<br />
“We are confident that this new system will<br />
PRIMARY CARE<br />
COMMUNITY & THERAPIES<br />
Q. What is the best lesson nursing<br />
has taught you?<br />
Showing compassion and being kind<br />
is more important than any other<br />
skill, whilst developing a successful<br />
team improves patient care and job<br />
satisfaction.<br />
Q. What career advice would you<br />
give your younger self?<br />
Enjoy every moment and embrace new<br />
experiences – everything is a learning<br />
experience.<br />
Tammy Davies, Group Director of Primary<br />
Care and Community and Therapies,<br />
features in The Nursing Standard this<br />
month<br />
IMAGING<br />
be a positive change for the imaging<br />
team, as well as for colleagues across the<br />
hospital and also for our patients.”<br />
The new system will allow the imaging team<br />
more time to report on scans<br />
19<br />
HB <strong>February</strong> <strong>2018</strong>.indd 19 20/02/<strong>2018</strong> 11:38
Delight as district nurse is honoured by<br />
the Queen’s Nursing Institute<br />
PRIMARY CARE, COMMUNITIES<br />
AND THERAPIES<br />
The Queen’s Nursing Institute (QNI)<br />
is a registered charity, dedicated<br />
to improving the nursing care of<br />
people in the home and community.<br />
They achieve this through a national<br />
network of Queen’s Nurses, who are<br />
committed to learning, leadership<br />
and high standards of practice and<br />
patient care.<br />
Val Hutchinson, District Nurse Clinical<br />
Lead at Friar Park, has recently been<br />
named one of only 32 Queen’s Nurses<br />
in the whole of the West Midlands.<br />
<strong>Heartbeat</strong> caught up with her to find out<br />
what this prestigious title means.<br />
She explained: “The title of ‘Queen’s<br />
Nurse’ is available to individual nurses<br />
who have demonstrated a high level of<br />
commitment to patient care and nursing<br />
practice.<br />
“Nurse, health visitors and midwives<br />
working in the community are eligible<br />
to apply, provided they have at least five<br />
years’ experience.”<br />
The title of ‘Queen’s Nurse’ gives<br />
special recognition of an individual’s<br />
commitment to their profession and<br />
signals their enduring commitment to<br />
Val Hutchison, District Nurse Clinical Lead has<br />
been named as a Queen’s Nurse<br />
providing the best care for patients and<br />
being a role model for colleagues.<br />
Eligible individuals apply personally<br />
to become a ‘Queen’s Nurse’ and are<br />
supported by both their manager and at<br />
least two patients. Applications are then<br />
reviewed by a specialist panel with the<br />
applicant informed via writing if they have<br />
been successful or not.<br />
“I applied in April 2017,” said Val. “I found<br />
out I had been successful in August and<br />
I attended a presentation in October. The<br />
event took place in the Royal Garden Hotel<br />
in London and I was presented with the<br />
‘Queen’s Nurse Award’ by Professor Jean<br />
White, Chief Nursing Officer for Wales.”<br />
So what made Val apply to become a<br />
‘Queen’s Nurse?’<br />
“I wanted to be part of the initiative to<br />
promote community nursing,” said Val.<br />
“I share the same vision as the QNI in that<br />
I believe people are entitled to the best<br />
possible care, by the right skillfully trained<br />
nurse.<br />
“I also felt that becoming a ‘Queen’s Nurse<br />
would assist in my development as a leader.<br />
As a district nurse clinical lead, I lead a small<br />
team of community staff - my leadership<br />
style is developing all the time and I receive<br />
positive feedback from them, but I felt that<br />
the QNI could help me further my skills.<br />
“I love my role as a district nurse and I have<br />
an immense amount of pride in the work<br />
that we do. Being awarded the title of<br />
‘Queen’s Nurse’ is the ultimate accolade and<br />
I feel honoured to have been given it.”<br />
Val’s line manager, District Nurse Team<br />
Leader, Sue Knight is extremely proud of her<br />
achievement. She said: “Val is so dedicated<br />
to all patients in her care and is extremely<br />
supportive of family members.<br />
“I have only ever received compliments and<br />
never complaints in respect of the input Val<br />
gives. She is thorough and hard-working,<br />
often working over her shift to go that<br />
extra mile and does so without asking for<br />
recognition.<br />
“In summary, if I or my family needed the<br />
services of a district nurse, I would want Val<br />
Hutchinson to walk through the door.”<br />
Histopathology recruits to<br />
continue excellent service<br />
PATHOLOGY<br />
During the past six months<br />
histopathology has welcomed 10 new<br />
members to their team based at City<br />
Hospital. <strong>Heartbeat</strong> caught up with<br />
Deputy Director of Operations, Diane<br />
Edwards to find out more about the<br />
new recruits.<br />
“We had lost a number of highly skilled and<br />
experienced colleagues recently due to the<br />
period of uncertainty in pathology across the<br />
midlands at the moment,” said Diane.<br />
“However, it is testament to our active<br />
recruitment process that we have been<br />
able to bring in these new members of the<br />
team. We have successfully appointed two<br />
senior biomedical scientists and have been<br />
able to give opportunities to newly qualified<br />
biomedical science degree students to kickstart<br />
their careers.”<br />
Diane explained more about the role of the<br />
senior biomedical scientists. She said: “They<br />
will be involved in using advanced dissection<br />
techniques to prepare specimens for<br />
diagnosis. These are tissue samples which<br />
are taken during operations in theatre.<br />
“They will also play a big role in helping to<br />
train their junior colleagues.<br />
“The newly qualified degree students<br />
will now undertake a two year training<br />
programme within the department to<br />
become biomedical scientists.”<br />
One of these new starters, Rahel Haile, told<br />
<strong>Heartbeat</strong>: “I’m so happy to be offered this<br />
role. This is my first job after I finished my<br />
master’s degree and I’m really grateful to be<br />
given this opportunity to start my career.<br />
“Everyone in the team has been so friendly<br />
and kind to me. I have already learned so<br />
much from the job and I couldn’t wait to<br />
learn and gain more experience.”<br />
As well as clinical appointments, there has<br />
also been some additions to the office team<br />
within the histopathology department.<br />
“We have also had a new medical secretary<br />
and a multi-disciplinary team co-ordinator<br />
who have joined our office team,” said<br />
Diane.<br />
“In addition to this we have appointed two<br />
undergraduate students from Birmingham<br />
University to assist in the decommissioning<br />
of our archives prior to the opening of<br />
Midland Metropolitan Hospital.<br />
“All the new members of our team have<br />
settled well and have made a great start.<br />
I am confident that they will be an asset<br />
to us moving forwards and together<br />
we will continue to provide an excellent<br />
histopathology services for our patients,<br />
clinicians and GPs.”<br />
20<br />
HB <strong>February</strong> <strong>2018</strong>.indd 20 20/02/<strong>2018</strong> 11:38
Picture book is having an impact on<br />
sickle cell youngsters<br />
MEDICINE AND<br />
EMERGENCY CARE<br />
other and can rely on each other to talk<br />
to or just be there.<br />
“If the transition process is not right,<br />
it can lead to a poor experience for<br />
patients. I first came to City Hospital<br />
when I was 16. I had suffered a crisis and<br />
was taken to the emergency department.<br />
It was scary and confusing as I knew no<br />
one and was unfamiliar with the hospital.<br />
I eventually got to know everyone in<br />
the SCAT team and others who are<br />
responsible for my care and I’m very<br />
fortunate to have a great team of carers<br />
around me.”<br />
The transition project is currently going<br />
through a consultation process with a<br />
view to launching in the summer.<br />
Jenica Leah’s book ‘My Friend Jen’ is available from Amazon and other book stores<br />
Her name is Jen, and the story book ‘My<br />
Friend Jen’ tells how a four year old girl<br />
manages when she is diagnosed with the<br />
blood disorder, sickle cell anaemia.<br />
‘My Friend Jen’ was penned by first time<br />
self-published author, Jenica Leah, a sickle cell<br />
sufferer who has been a patient at our Sickle<br />
Cell and Thalassaemia (SCAT) unit at City<br />
Hospital for nearly 12 years.<br />
Published in 2016, the book has been well<br />
received and Jenica has won some accolades<br />
along the way including being named<br />
Inspirational Young Author at the BEX Live<br />
Enterprise and Community Awards.<br />
She said: “The idea of the book came to me<br />
because there is no literature out there to help<br />
young people with sickle cell. I was diagnosed<br />
as a baby and throughout my childhood it<br />
was very difficult to explain to my friends<br />
why I was always unwell and missing school.<br />
There wasn’t even an easy definition out there<br />
that could simply tell someone else what was<br />
wrong with me.”<br />
‘My Friend Jen’ initially started off as a poem<br />
but gradually became a book once Jenica<br />
realised that there was a need for a book with<br />
good and simple advice about sickle cell.<br />
She added: “I realised this would be a perfect<br />
opportunity for me to talk about the condition<br />
and how it affects Jen, as well as give advice<br />
on how to stay well and healthy in a fun and<br />
informative way. The book shows that Jen can<br />
do anything that other little boys and girls can<br />
do, apart from this one thing that makes her a<br />
little different.<br />
“I have been surprised by the reaction to<br />
the book. I have been fortunate to appear<br />
on radio and TV both here and abroad to<br />
talk about my condition and why my book<br />
is important. It’s good to see young people<br />
and their families reading ‘My Friend Jen’ and<br />
learning about my condition.”<br />
Helping young people to transition<br />
Jenica is part of a group of sickle cell sufferers<br />
working with the SCAT unit and Your Trust<br />
Charity to deliver a project that will help<br />
young people with their move from paediatric<br />
to adult care.<br />
“This project is really dear to my heart and I<br />
am delighted to work with Your Trust Charity<br />
to help it come to fruition,” Jenica explained.<br />
“Moving from children to adult care is a<br />
significant change for young people. The<br />
project will allow them to visit the SCAT unit<br />
and the hospital as a whole so they are aware<br />
of where the key services are.<br />
“We will also provide advice on the nonmedical<br />
challenges that come with sickle<br />
cell. Sickle cell can be a lonely disease, it is<br />
particularly helpful if young people know one<br />
Eddie Edmead, Major Grants Manager,<br />
Your Trust Charity said: “The project<br />
has benefitted tremendously from the<br />
dedicated support of clinical leads Liz<br />
Green and Amanda Tembedza (SCAT<br />
team), and is led by Jenica and Sadeh –<br />
who are both pro-active young people<br />
who are living with sickle cell.<br />
“They are the project’s advocates and our<br />
health champions!”<br />
As well as working on the transition<br />
project, Jenica also volunteers at the<br />
SCAT unit, providing one to one advice to<br />
young sufferers.<br />
Sickle cell disease is the name for<br />
a group of inherited conditions<br />
that affect the red blood cells. It<br />
mainly affects people of African,<br />
Caribbean, Middle Eastern,<br />
Eastern Mediterranean and Asian<br />
origin. In the UK, it’s particularly<br />
common in people with an<br />
African or Caribbean family<br />
background.<br />
People with sickle cell disease<br />
produce unusually shaped<br />
red blood cells that can cause<br />
problems because they don’t live<br />
as long as healthy blood cells and<br />
they can become stuck in blood<br />
vessels.<br />
Sickle cell disease is a serious<br />
and lifelong condition, although<br />
long-term treatment can help<br />
manage many of the problems<br />
associated with it.<br />
‘My Friend Jen’ is available at<br />
Amazon and other book stores.<br />
21<br />
HB <strong>February</strong> <strong>2018</strong>.indd 21 20/02/<strong>2018</strong> 11:38
NHS Hero - Nuhu Usman<br />
MEDICINE AND<br />
EMERGENCY CARE<br />
Our organisation is full of<br />
remarkable, motivated people,<br />
who give a lot to the communities<br />
we serve. Since 2014, we have<br />
been recognising our quiet heroes<br />
who come from a wide variety of<br />
backgrounds, and do a wide variety<br />
of jobs across our organisation. Each<br />
week we shine a spotlight on one<br />
of those heroes, and following an<br />
interview by our press office the<br />
Sandwell Chronicle publishes these<br />
inspirational stories.<br />
In this edition of <strong>Heartbeat</strong>, the spotlight<br />
is on our Clinical Director for Emergency<br />
Care, Dr Nuhu Usman.<br />
He’s one of the medics who will be<br />
responsible for the clinical development<br />
of Europe’s biggest accident &<br />
emergency departments. Dr Usman has<br />
told how merging two A&Es into one<br />
at the new “super hospital” Midland<br />
Metropolitan, in Smethwick, is his next<br />
big challenge.<br />
“When the Midland Metropolitan<br />
Hospital opens it will have the biggest<br />
emergency department in Europe,”<br />
explained Dr Usman, who began working at<br />
our organisation nine years ago.<br />
“Getting emergency care settled into the<br />
new hospital and merging two A&Es into<br />
one is definitely a huge task. It will be a<br />
100-bed development serving the people of<br />
Sandwell and West Birmingham.<br />
“We will also be creating a new urgent care<br />
centre on the Sandwell site.”<br />
Dad-of-two Dr Usman, from Sutton<br />
Coldfield, is also in charge of ensuring the<br />
emergency departments at both Sandwell<br />
and City Hospital are running well.<br />
He added: “In my role along with support<br />
from my team, we try to make sure patients<br />
get the treatment they need and in a timely<br />
manner.”<br />
During his nine years here, Dr Usman,<br />
48, has helped to create the ambulatory<br />
care unit, which is based at both sites and<br />
relieves the pressure on A&E. In fact, it is<br />
this work that Dr Usman cites as his career<br />
highlight to date. “I am very proud of our<br />
ambulatory care unit. We set up units at<br />
both City and Sandwell back in 2012. At<br />
the time there wasn’t any space for these<br />
units but with support from our Chief<br />
Executive, Toby Lewis, we made room and<br />
since then it has developed successfully and<br />
is now working very well.”<br />
It’s no surprise that helping people is Nuhu’s<br />
ultimate goal. He added: “Patients drive<br />
and motivate me at work. I think one of the<br />
most satisfying things is seeing a patient<br />
leaving the hospital looking well. I enjoy<br />
talking to patients especially those who are<br />
elderly. Seeing the brightness in their eyes<br />
and the gratitude that someone is spending<br />
time with them is very rewarding.<br />
“One of my most memorable occasions<br />
at work is when we had a wedding on<br />
the ward. A patient was supposed to get<br />
married but her dad was in hospital. One<br />
of our matrons helped to arrange the<br />
wedding in the hospital instead. It was such<br />
a wonderful ceremony and it was all very<br />
sweet.”<br />
When Dr Usman isn’t busy working, he likes<br />
to escape by going on long walks with his<br />
wife and children.<br />
So who is his own hero? “It has to be<br />
Nye Bevan, the MP who spearheaded the<br />
establishment of the NHS. It is inspiring that<br />
he had the courage to do it. The country<br />
had just come out of a war and was not<br />
prosperous but he still had the vision to<br />
create a health system that meant free care<br />
for all. He really is a remarkable person.”<br />
January <strong>2018</strong> staff<br />
lottery results<br />
2nd £112.35<br />
Kathleen McGrath<br />
(ticket number 446)<br />
1st £187.25<br />
Theresa Duru<br />
(ticket number 207)<br />
3rd £74.90<br />
Sally Harrison<br />
(ticket number 318)<br />
Don’t forget that the Trust Charity Lottery costs just £1<br />
a month and anyone who works for the Trust can join.<br />
Payment is deducted from your wages each month.<br />
Nuhu Usman, Clinical Director for Emergency Care<br />
To take part e-mail amanda.winwood@nhs.net<br />
22<br />
HB <strong>February</strong> <strong>2018</strong>.indd 22 20/02/<strong>2018</strong> 11:38
Sandwell and West Birmingham Hospitals<br />
NHS Trust<br />
It’s Your<br />
Voice –<br />
have your<br />
say<br />
Your Voice survey gives you a greater say in<br />
decision making, changes that affect you and<br />
is also a great way of getting your ideas heard.<br />
Your feedback tells managers and leaders<br />
about what it is like to work here and what can<br />
be improved, and provides timely data about<br />
whether actions taken as a result are making a<br />
difference. You should have received an email<br />
asking you to take part. If you have not had an<br />
invitation, you can still have your say via this link.<br />
http://www.myonlinesurvey.co.uk/SRXKAN/<br />
You have until 16 March to complete the survey.<br />
HB <strong>February</strong> <strong>2018</strong>.indd 23 20/02/<strong>2018</strong> 11:38
Claire Hubbard,<br />
Director of Nursing for Medicine and Emergency Care<br />
Attracted to the SWBH family on seeing<br />
our outstanding rating for being caring,<br />
Project 2000 nurse Claire Hubbard has<br />
come from Birmingham Women’s and<br />
Children’s NHS Foundation Trust to<br />
take on her new role in Medicine and<br />
Emergency Care.<br />
She explained: “I started my training back<br />
in 1992, qualifying in ’95, before taking<br />
up my first role in Harefield Hospital on the<br />
outskirts of London, I had the privilege of<br />
working alongside Professor Sir Magdi Yacoub<br />
– the founder and Director of Research at<br />
the Harefield Heart Science Centre, on the<br />
cardiothoracic transplant unit.<br />
“As an only child growing up I aspired to be<br />
a solicitor and my first job was an accounts<br />
clerk. Fate led me in a totally different<br />
direction and I applied for nursing during the<br />
implementation of Project 2000, which saw<br />
nurse training change to move out of schools<br />
of nursing and into the university classroom.<br />
It is a decision I have never regretted, as I<br />
feel I have found my true passion, in caring<br />
for others. I am inspired by random acts of<br />
kindness, patient and staff experience and my<br />
ideology majors on compassion. I am looking<br />
forward to working in a team that values<br />
safety and quality, as my Master’s degree is in<br />
Quality and Service Improvement.<br />
“Alongside my sons Max (16) and Ollie (14),<br />
last year I climbed Snowdon to raise money<br />
for a patient experience initiative regarding<br />
privacy and dignity, so I’m looking forward to<br />
investigating opportunities within Your Trust<br />
Charity to do something similar here.”<br />
Claire Hubbard has joined us from<br />
Birmingham Women’s and Children’s NHS<br />
Foundation Trust<br />
Wave goodbye to…<br />
Dave ‘the bloodhound’ Johnson<br />
Dave Johnson will be a familiar face<br />
to many around Sandwell Hospital, as<br />
he has spent over 41 years working in<br />
receipts and distribution, walking miles<br />
around the hospital each day to deliver<br />
parcels to departments.<br />
Dave first reported for duty on 25 October<br />
1976 at West Bromwich and District Hospital<br />
which was in Edward Street. His role was to<br />
be part of the commission team, ready for<br />
the opening of Sandwell General Hospital.<br />
Dave told <strong>Heartbeat</strong>: “One of my first tasks<br />
was to furnish all the flats in Hallam Close<br />
Nurses’ Home, which is situated at the<br />
bottom of Hallam Street staff car park and is<br />
now used by apprentices.<br />
“I filled all the flats with furniture, even<br />
down to the cutlery and the kettles.<br />
“I remember being in the new hospital<br />
when it was still a building site. The<br />
contractors were finishing off and the only<br />
people around were me and security. I had<br />
an old chunky walkie talkie, which needed a<br />
holder, but it wouldn’t even reach security,<br />
so I used to have to walk closer to them to<br />
get any reception!”<br />
Dave has seen many people come and go<br />
during his many years at the hospital, and it<br />
is the people (not the trolley pushing!) that<br />
he will miss most.<br />
He said: “People here are wonderful – I will<br />
really miss them. I won’t miss pushing those<br />
metal trolleys all over the place though!”<br />
Dave Hobbs, Receipts and Distribution Team<br />
Leader said Dave will be really missed.<br />
“He is the most dependable person I know.<br />
He’s always here – he hardly ever has a day<br />
off sick.<br />
“I call him the bloodhound as he always<br />
manages to track down lost parcels. If<br />
we get a call saying something had been<br />
misplaced – I would always put Dave on the<br />
case and he would always find it!<br />
“He will be really missed – he is like part of<br />
the furniture here but we wish him well in<br />
his retirement.”<br />
As if almost 42 years working in the hospital<br />
wasn’t enough, Dave plans to spend some<br />
of his retirement here too as he is hoping to<br />
register with the volunteer service.<br />
“Hopefully you will see me about in a yellow<br />
t-shirt!” said Dave.<br />
“I know this place like the back of my hand<br />
so I am hoping to join the volunteers to help<br />
direct patients around.”<br />
Aside from volunteering, Dave plans to<br />
use his retirement to reignite a love of<br />
photography and take up model making.<br />
Dave Johnson is retiring after over 41 years<br />
service to the NHS<br />
24<br />
HB <strong>February</strong> <strong>2018</strong>.indd 24 20/02/<strong>2018</strong> 11:38
Letters, of less than 200 words please, can be sent to the Communications Department,<br />
Trust Headquarters, Sandwell Hospital or by email to swb-tr.SWBH-GM-<strong>Heartbeat</strong>@nhs.net<br />
YOUR RIGHT TO BE HEARD<br />
25<br />
Why can’t we access electric<br />
car charging points?<br />
Dear <strong>Heartbeat</strong>,<br />
I was so happy to read in the previous issue<br />
of <strong>Heartbeat</strong>, the Trust’s commitment to<br />
sustainability, with the introduction of electric<br />
charging points. Having just purchased a<br />
hybrid car I registered and looked forward<br />
to being able to use the points once at<br />
work. Unfortunately I have been constantly<br />
disappointed when arriving to find both<br />
car parking areas meant for the sole use<br />
of charging, occupied by cars not using<br />
the facility. I then have to go through the<br />
rigmarole of contacting security to see if<br />
the car is registered (who I’m sure now look<br />
forward to my persistent early morning call),<br />
leaving notes on cars to contact me once they<br />
vacate, or constantly checking back during my<br />
break or lunch sometimes to no avail.<br />
I know new things take time to bed in, but<br />
could we make the area more clear what they<br />
are for, maybe a different colour parking area,<br />
place warnings on the vehicles.<br />
Also, the way in which we are charged for<br />
the use of the points seems somewhat unfair<br />
with an additional charge for just docking<br />
the charger! Hopefully these are just teething<br />
problems and we will see improvements<br />
(including the cost) as the system is bedded in.<br />
Thank you.<br />
Dear Colleague,<br />
I’m pleased to hear that you have<br />
purchased a hybrid vehicle and sorry to<br />
hear that you have experienced issues<br />
when attempting to access the designated<br />
electric vehicle charging bays.<br />
On the issue of accessing the spaces, we<br />
have ordered new signage that states<br />
‘Electric Vehicles Only Charing Point.<br />
Maximum stay 3 hours. Vehicles must be<br />
on charge’. This signage will allow our<br />
security team to issue a Parking Charge<br />
Notice (PCN) on vehicles parked in these<br />
spaces illegally. We will also be painting<br />
the bays so there is clearer definition.<br />
With regards to the cost of charging, we<br />
have tried to keep costs for users to a<br />
minimum. We also want to ensure that the<br />
cost of charging vehicles on site is cheaper<br />
than petrol or diesel. We fully support<br />
colleagues travelling by sustainable<br />
modes, including low emissions vehicles<br />
and were successful in receiving some<br />
external funding to cover some of the<br />
installation costs. A discounted rate for<br />
using the charge points has been applied<br />
to colleagues when registering here:<br />
https://www.cpsgenie.com/ds/Register/For/<br />
NHSWBS. Once registered, you will have<br />
access to a 24/7 customer helpline (hence<br />
the transaction fee). The organisation<br />
has to pay for the electricity we consume.<br />
If there is any surplus income, this will<br />
be used to fund the maintenance of the<br />
charge points and future low emission<br />
vehicles infrastructure.<br />
If this issue persists or should you have any<br />
further questions, please feel free to get<br />
in contact.<br />
Kind regards,<br />
Fran Silcocks<br />
Sustainability Officer<br />
Shuttle bus frustrations<br />
Dear <strong>Heartbeat</strong>,<br />
I use the shuttle bus early morning to get to<br />
work in Sandwell but there are loads of times<br />
that the driver is late or doesn’t turn up.<br />
On Tuesday 23 January I was there at the<br />
shuttle waiting area at 6.31am to catch the<br />
6.40am bus. I waited there and at around<br />
6.40am I rang the transport services and a lady<br />
answered my call and said ‘The driver is here<br />
but he’s sorting himself and he will be there<br />
and you have to wait.’<br />
So I waited and the driver still didn’t turn up. I<br />
had to wait for the 7am bus to go to Sandwell<br />
and in the end I was late for my shift by 25<br />
minutes.<br />
Looking forward for your response.<br />
Staff nurse<br />
Dear Colleague,<br />
I can only apologise for the cancellation of<br />
the 6.30am shuttle bus service on Tuesday<br />
23 January. The driver rostered for that<br />
early morning service rang in sick so we<br />
had to organise a replacement driver.<br />
Unfortunately this could not be done in<br />
time to meet the 6.30am service.<br />
Although the vehicles are serviced and<br />
regularly maintained there have also<br />
been a couple of times when the shuttle<br />
bus has broken down. Contingencies<br />
are in place with the rental company to<br />
provide a replacement vehicle, however<br />
there is sometimes a delay whilst the<br />
arrangements are made and the vehicle<br />
delivered.<br />
Kind Regards,<br />
Steve Clarke<br />
Deputy Director – Facilities<br />
Why is Rowley the forgotten<br />
hospital?<br />
Dear <strong>Heartbeat</strong>,<br />
I am sending this letter in relation to the<br />
catering and food facilities at Rowley Regis<br />
Hospital. As usual we hear lots of things<br />
that are happening at City and Sandwell<br />
but Rowley is not really involved in the<br />
developments. It sometimes feels as though<br />
this is the forgotten hospital.<br />
At present the catering restaurant is open<br />
until 2pm (Monday to Friday only). I am on a<br />
shift today until 8pm, and there is no catering<br />
facilities, the machine which supplies minimal<br />
choice of food is out of order. Therefore, there<br />
is nothing available for all the staff who are on<br />
duty once the canteen closes at 2pm.<br />
We then have to result to driving out to<br />
the nearest shops or take away outlets. Are<br />
there any plans for the times to increase for<br />
the canteen and to be better services during<br />
the weekend? Also if there are going to be<br />
machines – could they be working, and have a<br />
good selection to choose from?<br />
Kind regards,<br />
Nursing staff from Rowley<br />
Dear Colleagues,<br />
Thank you for your comments. I have<br />
looked into the issues raised and can<br />
confirm that the snack vending machine<br />
is scheduled for repair on Tuesday 13<br />
<strong>February</strong>.<br />
Unfortunately the repair has taken longer<br />
than we would have liked due to a delay<br />
in the replacement parts becoming<br />
available. Hopefully, on reading my<br />
response, you will have already noticed<br />
that the machine is now stocked with our<br />
new sandwich and wrap products, along<br />
with other snack items, which I hope you<br />
are enjoying.<br />
In relation to the opening hours, there<br />
are no plans to increase the hours of<br />
the Coffee Pot as unfortunately there is<br />
just not enough customers to warrant<br />
extending the hours.<br />
Kind regards,<br />
Jane Owen<br />
Trust Catering Manager<br />
Dear Colleague<br />
Rowley Regis Hospital is certainly not a<br />
“forgotten” hospital. Over the past two<br />
years we have made a lot of changes to<br />
RRH to bring in more outpatient activity,<br />
clinics and diagnostics. It remains a vital<br />
part of our Trust and our provision of<br />
services to people in the community.<br />
Kind regards,<br />
Toby Lewis, Chief Executive<br />
HB <strong>February</strong> <strong>2018</strong>.indd 25 20/02/<strong>2018</strong> 11:38
YOUR RIGHT TO BE HEARD<br />
Why the bank rate change for<br />
bands 2 and 3?<br />
Dear <strong>Heartbeat</strong>,<br />
Can someone please explain why it is that the<br />
bank rate of pay for band 2 and 3 staff has<br />
been reduced and not any of the band 5 and<br />
upwards? Where is the fairness in this?<br />
Band 2 and 3 staff are now to get the same<br />
rate of pay, yet their workload increases. We<br />
are expected to do various tasks, but not get<br />
anymore pay. Our workload is as important as<br />
the qualified staff.<br />
We hear all the so called ‘appreciation’ for the<br />
hard work that is done in these very trying<br />
times with all the cuts, sickness and pressure<br />
that are in the trust at the moment, where is<br />
the gratitude shown to band 2/3 staff?<br />
I think it is very disheartening that our rate<br />
has been cut. There are too many managers in<br />
this organisation, some, as far as I can see, do<br />
absolutely nothing that warrants them getting<br />
astronomical salaries. Why don’t you cut their<br />
salary and employ more staff, instead of, yet<br />
again making the lower paid, hardworking<br />
staff suffer. Band 2/3 staff work really hard<br />
but get no acknowledgement in the form of<br />
money to reflect this.<br />
Anon<br />
Dear Colleague,<br />
We reviewed our bank rates at the<br />
end of last year as part of our planned<br />
approach to reduce our pay spend. You’ll<br />
no doubt be aware from our corporate<br />
communications that we are having to<br />
make some tough choices to ensure we<br />
manage within our affordable levels of<br />
spend, and this is one such example.<br />
We did not make the decision lightly and<br />
ensured that our rates remain competitive<br />
with other NHS banks and agency rates.<br />
We also remain committed to paying the<br />
living wage foundation minimum rate of<br />
pay.<br />
Whilst we recognise and value the<br />
contribution that our bank workers<br />
provide to the organisation our preference<br />
is to reduce our pay expenditure by<br />
reducing our reliance on temporary spend,<br />
thereby protecting as far as possible our<br />
permanent employees.<br />
As you say we didn’t reduce band 5 nurse<br />
pay this time around, but nurse rates of<br />
pay were reduced earlier in the year, so<br />
whilst not undertaken at the same time,<br />
all non-medical staff groups have now<br />
been reviewed.<br />
Obviously exercises such as this will always<br />
be unpopular but are a necessary and<br />
important step if we are to reduce our pay<br />
spend to the levels required in the next<br />
financial year, and minimise the impact on<br />
our permanent employees.<br />
Managers play a vital role in the smoothrunning<br />
of our organisation. We have<br />
made changes to manager bank rates too<br />
as well as putting stops on non-clinical<br />
bank and agency work. We have one of<br />
the lowest manager to employee ratio in<br />
the West Midlands and we keep this under<br />
constant review.<br />
Kind regards,<br />
Raffaela Goodby<br />
Director of People and Organisation<br />
Development<br />
Why don’t we offer transport<br />
for outpatient appointments?<br />
Dear <strong>Heartbeat</strong>,<br />
I would just like to ask why when we are a<br />
provider of care 24/7 that if a patient has an<br />
outpatient appointment after 3pm on a week<br />
day or an appointment of a weekend, patient<br />
transport won’t bring the patient into their<br />
appointment.<br />
Patient transport have staff that work up<br />
to 8pm weekdays and work Saturdays and<br />
Sundays but still patients with outpatient<br />
appointments will not be bought into the<br />
hospital and have to re-arrange which is not<br />
always possible due to the times the specific<br />
clinics run.<br />
Surely the system needs up dating so patients<br />
are not having to cancel appointments after<br />
3pm and are able to come to clinics that run<br />
on a weekend.<br />
This is not good patient care and the<br />
managers of patient transport need to put<br />
the needs of the patients first and upgrade<br />
and extend the hours of the service they are<br />
offering.<br />
Thank you.<br />
Dear Colleague,<br />
The patient transport service is a finite<br />
resource which provides transport for<br />
patients across all sites within the Trust<br />
and in the community. As well as the<br />
outpatient service, their work schedule<br />
comprises of discharges to assist in<br />
patient flow, cross site transfers, inter-site<br />
transfers (City), transfers to other hospitals<br />
and ED after treatments.<br />
Transport arrangements for outpatients<br />
with appointments after 3pm would be<br />
difficult to schedule as the majority of<br />
patient discharges take place after this<br />
time and the remaining crews are off-site<br />
taking earlier outpatients appointments<br />
home and the evening crews are all<br />
concentrated on patient discharges.<br />
There is also a reduced service on a<br />
weekend, again with all crews scheduled<br />
to undertake in-patient discharges or<br />
transfers.<br />
The costs of the service have to be<br />
managed within budget, the controls are<br />
necessary to ensure the maximum overall<br />
output for both the outpatients and<br />
inpatient service.<br />
Kind regards,<br />
Steve Clarke<br />
Deputy Director – Facilities<br />
Action against smoking is<br />
needed now<br />
Dear <strong>Heartbeat</strong>,<br />
Imagine a consultant lighting a cigarette while<br />
examining a patient. Or perhaps ashtrays<br />
should be placed on wards so that patients<br />
can smoke while they wait to be seen.<br />
Both are situations that will not happen. So<br />
why does the Trust feel that is acceptable to<br />
maintain a smoking shelter so close to offices.<br />
Each and every day my colleagues and I are<br />
exposed to the effects of secondary smoke<br />
and noise.<br />
The Trust has a responsibility to protect the<br />
health of its workforce - just as we have taken<br />
on the responsibility to care for and support<br />
our patients.<br />
We don’t need debate. We need action.<br />
Thank you<br />
Dear Colleague,<br />
Thank you for your letter. The issue of<br />
smoking on our sites is one that we will<br />
stop completely once we move into the<br />
new Midland Metropolitan Hospital<br />
and rationalise our remaining estate,<br />
becoming smoke-free. I am sorry that you<br />
are being affected by second hand smoke<br />
from one of our designated smoking<br />
shelters. I would be happy to see if we<br />
can relocate the shelter to avoid smoke<br />
getting into your office space. Perhaps<br />
you could email me so I can look at the<br />
particular shelter you are referring to?<br />
tobylewis@nhs.net<br />
Best wishes<br />
Toby Lewis<br />
Chief Executive<br />
26<br />
HB <strong>February</strong> <strong>2018</strong>.indd 26 20/02/<strong>2018</strong> 11:38
This month Toby writes about…listening more<br />
and listening better<br />
TobyLewis_SWBH<br />
TOBY’S LAST WORD<br />
The front-page of <strong>Heartbeat</strong> this month ought to make us all<br />
proud to be part of this organisation.<br />
We are visibly and unambiguously providing<br />
relatives, friends, family, colleagues and<br />
patients with the chance to speak up, seven<br />
days a week and in multiple local languages.<br />
Over the coming month you will see all sorts<br />
of publicity and explanation for the new<br />
Purple Point system. Please give it some<br />
of your precious time – when a call comes<br />
through from the team fielding calls we all<br />
need to know what we are being asked to do<br />
- of course we are being asked to respond,<br />
but also to find time to go and listen to the<br />
person raising a concern. Very often that<br />
concern may be solely about communication<br />
or more explanation being needed. Yet if we<br />
really want to make carers, in particular, part<br />
of the care pathway, then that is precisely<br />
what we are going to need to become<br />
experts in. Let’s start simply. The next time<br />
you work through the notes or records of an<br />
inpatient, ask yourself this: Is it clear who is a<br />
family member or neighbour? Who is the key<br />
point of contact?<br />
That partnership with friends and family is<br />
something we have been emphasising since<br />
we started to work with John’s Campaign,<br />
which supports relatives sleeping on our<br />
wards overnight, as is commonplace on<br />
children’s wards. It is part of what we do<br />
with Age-Well in providing a befriending<br />
service, now expanded into our Sapphire<br />
project.<br />
The big expansion of our volunteering<br />
service and pilot status as a HelpForce aligned<br />
organisation, are all about how we involve<br />
and engage local people in the care that we<br />
provide. We have a huge amount to learn<br />
through that, about the resources available<br />
in our local community to better support<br />
patients at home. As we look to double<br />
the number of patients we discharge each<br />
weekend, and thereby make Mondays not a<br />
“double” day, we need to know who we can<br />
rely upon for isolated patients living alone.<br />
By 2020, of course, we will have made two<br />
more huge changes in how we relate to<br />
friends and family:<br />
• The Midland Met wards, in the main,<br />
will be based around patient-led<br />
kitchens. Building on the pioneering<br />
work done on our stroke wards around<br />
breakfast clubs, we want to change<br />
the therapeutic model where we can,<br />
to make it normal to cook and eat at<br />
a time of the patients’ choosing, like<br />
they would at home. This is a big<br />
change – and one designed to tackle<br />
institutionalisation. Part of the work in<br />
our Trust, and across the NHS, to end<br />
so-called PJ Paralysis. I know that when<br />
Paula Gardner joins us in April as our<br />
new chief nurse this will be one of the<br />
first issues that she focuses on.<br />
• And in a little while, we will implement<br />
our Unity Patient Portal (PatientHub).<br />
This will give patients the ability to<br />
log into their care records from home.<br />
Taking a look at the work we do,<br />
understanding their condition better,<br />
and of course understanding the daily<br />
care that inpatients receive. There are all<br />
sorts of reasons to want to improve our<br />
record keeping, as we work across multi<br />
professional teams. But this too will<br />
push us to get this right.<br />
In <strong>2018</strong> however the listening drive is not<br />
confined to patients and their relatives. It is<br />
also part of how we want the Trust to change<br />
for you, and by your actions. Hundreds of<br />
managers are presently graduating from<br />
our accredited manager programme. That<br />
creates a manager’s passport for working<br />
here, with some key expectations of each<br />
of us – including expectations about how<br />
we manage our line reports and teams. In<br />
<strong>2018</strong>-19 all line managers will take part in a<br />
360-degree feedback exercise in which we<br />
gather data on what people who work for<br />
us think we do well, and could improve. The<br />
executive team are doing just this right now,<br />
as we work towards our next away time.<br />
Your Voice continues, as a big part of our<br />
work to gather your ideas and views. Please<br />
do contribute to it when it comes your<br />
way. But like any feedback it is as good as<br />
what we do with it and your confidence<br />
that something is done. It is the same with<br />
incident reports. Each morning they are<br />
studied and the SIs – serious incidents – go<br />
through a very detailed process all the way<br />
into the board and beyond. We are making<br />
changes now, for example, to what happens<br />
to patients in resus if their care is delated. I<br />
am sure there is more we could do to work<br />
with amber incidents. Ben Mears, Nuhu<br />
Usman, Liz Miller and I met just last week<br />
to look at security issues in relation to ED<br />
and AMU. This is all information that each<br />
directorate and group is working with, as<br />
well as individual line managers. The new, or<br />
now nearly new, executive quality committee<br />
is looking to make sure that there is a thriving<br />
structure at local level to assess, learn from<br />
and act on feedback and information on<br />
safety and governance.<br />
You may, or may not, have heard of Hadiza<br />
Bawa-Garba. She was, is, a paediatrician<br />
who latterly worked at Leicester Royal. One<br />
of our colleagues, David Nicholl, is part of<br />
a campaign to get her readmitted to the<br />
medical register. The GMC has removed<br />
her from that after her conviction for gross<br />
negligence manslaughter. Her case has given<br />
rise to grave concern across the service, and<br />
within our Trust, about how we learn from<br />
error, and hear properly concerns about<br />
things that have or could go wrong. Her<br />
case is relevant to all of us, because we work<br />
in teams, and need to take responsibility<br />
for each other. Individual accountability<br />
will always be a feature of care, but our<br />
best care is provided across teams, often<br />
teams who only know each other a little.<br />
From March we will make it, as part of<br />
our CQC Improvement Plan, mandatory to<br />
undertake pre shift assessments of the skills<br />
of new, bank and agency colleagues. The<br />
data on that work will be collated and as<br />
necessary used to feedback to agencies and<br />
to individuals about their work. Dr. Bawa<br />
Garba was though a substantive member<br />
of NHS staff. Her reflections on the tragic<br />
death of her patient were used – in my view<br />
unacceptably - to critique her in court and at<br />
tribunal. In our Trust we want a culture of<br />
learning, where anyone feels able to speak<br />
honestly about mistakes. And one where<br />
senior staff, clinical or otherwise, always<br />
expect to be asked to help, or just to listen.<br />
I published in a recent Friday message a note<br />
from David Carruthers, our Medical Director,<br />
on precisely that theme, and I want to<br />
reiterate here that everyone who works in our<br />
Trust should feel encouraged to contact those<br />
around and above them day or night. In<br />
changing our own Trust management system<br />
out of hours, which we did in <strong>February</strong>, we<br />
are looking to both empower and support<br />
colleagues providing care - especially when<br />
care is provided with the support of people<br />
on call from home. Listening, whether in<br />
the moment, or in looking at trends and<br />
themes being reported by you, protects us<br />
all, and our ability to hear emerging concerns<br />
is a key bridge between our successful<br />
safety plan implementation and the quality<br />
improvement work that David will lead in<br />
<strong>2018</strong>.<br />
27<br />
HB <strong>February</strong> <strong>2018</strong>.indd 27 20/02/<strong>2018</strong> 11:38
Unity early adopter training March and April <strong>2018</strong><br />
These sessions are for colleagues who will be involved in the full dress rehearsal (FDR) of Unity which will<br />
take place in April. If you have been nominated as an early adopter by your manager you must book on as<br />
soon as possible.<br />
FOR DATE TIMES LOCATION<br />
Drs/Consultants<br />
Course length 2 days<br />
FOR DATE TIMES LOCATION<br />
Nurses/HCAs<br />
Course length 2.5 days<br />
19/03/<strong>2018</strong> 9am - 4pm<br />
Training Room 2,<br />
Sandwell Hospital<br />
Part 1<br />
04/04/<strong>2018</strong> 9am - 4pm<br />
Training Room 2,<br />
Sandwell Hospital<br />
Part 1<br />
20/03/<strong>2018</strong> 9am - 4pm<br />
Training Room 2,<br />
Sandwell Hospital<br />
Part 2<br />
05/04/<strong>2018</strong> 9am - 4pm<br />
Training Room 2,<br />
Sandwell Hospital<br />
Part 2<br />
21/03/<strong>2018</strong> 9am - 4pm<br />
IT Library, City<br />
Hospital<br />
Part 1<br />
06/04/<strong>2018</strong> 9am - 12pm<br />
Training Room 2,<br />
Sandwell Hospital<br />
Part 3<br />
Nurses/HCAs<br />
22/03/<strong>2018</strong> 9am - 4pm IT Library, City Hospital Part 2<br />
26/03/<strong>2018</strong> 9am - 4pm<br />
27/03/<strong>2018</strong> 9am - 4pm<br />
Education Centre<br />
Room 5, Sandwell<br />
Hospital<br />
Education Centre<br />
Room 5, Sandwell<br />
Hospital<br />
Part 1<br />
Part 2<br />
28/03/<strong>2018</strong> 9am - 4pm IT Library, City Hospital Part 1<br />
29/03/<strong>2018</strong> 9am - 4pm IT Library, City Hospital Part 2<br />
03/04/<strong>2018</strong> 9am - 4pm<br />
04/04/<strong>2018</strong> 9am - 4pm<br />
Education Centre<br />
Room 5, Sandwell<br />
Hospital<br />
Education Centre<br />
Room 5, Sandwell<br />
Hospital<br />
Part 1<br />
Part 2<br />
05/04/<strong>2018</strong> 9am - 4pm IT Library, City Hospital Part 1<br />
06/04/<strong>2018</strong> 9am - 4pm IT Library, City Hospital Part 2<br />
Course length 2.5 days<br />
19/03/<strong>2018</strong> 9am - 4pm<br />
20/03/<strong>2018</strong> 9am - 4pm<br />
21/03/<strong>2018</strong> 9am - 12pm<br />
21/03/<strong>2018</strong> 9am - 4pm<br />
22/03/<strong>2018</strong> 9am - 4pm<br />
23/03/<strong>2018</strong> 9am - 12pm<br />
26/03/<strong>2018</strong> 9am - 4pm<br />
27/03/<strong>2018</strong> 9am - 4pm<br />
28/03/<strong>2018</strong> 9am - 12pm<br />
27/03/<strong>2018</strong> 9am - 4pm<br />
28/03/<strong>2018</strong> 9am - 4pm<br />
29/03/<strong>2018</strong> 9am - 12pm<br />
03/04/<strong>2018</strong> 9am - 4pm<br />
04/04/<strong>2018</strong> 9am - 4pm<br />
05/04/<strong>2018</strong> 9am - 12pm<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Training Room 2,<br />
Sandwell Hospital<br />
Training Room 2,<br />
Sandwell Hospital<br />
Training Room 2,<br />
Sandwell Hospital<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Training Room 2,<br />
Sandwell Hospital<br />
Training Room 2,<br />
Sandwell Hospital<br />
Training Room 2,<br />
Sandwell Hospital<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Part 1<br />
Part 2<br />
Part 3<br />
Part 1<br />
Part 2<br />
Part 3<br />
Part 1<br />
Part 2<br />
Part 3<br />
Part 1<br />
Part 2<br />
Part 3<br />
Part 1<br />
Part 2<br />
Part 3<br />
Therapists (AHP)<br />
Ward Clerks<br />
Capacity Managers<br />
Pharmacists<br />
Course length 1 day<br />
19/03/<strong>2018</strong> 9am - 4pm IT Library, City Hospital<br />
20/03/<strong>2018</strong> 9am - 4pm IT Library, City Hospital<br />
22/03/<strong>2018</strong> 9am - 4pm<br />
23/03/<strong>2018</strong> 9am - 4pm<br />
Training Room 1,<br />
Sandwell Hospital<br />
Training Room 1,<br />
Sandwell Hospital<br />
26/03/<strong>2018</strong> 9am - 4pm IT Library, City Hospital<br />
27/03/<strong>2018</strong> 9am - 4pm IT Library, City Hospital<br />
28/03/<strong>2018</strong> 9am - 4pm<br />
29/03/<strong>2018</strong> 9am - 4pm<br />
Training Room 1,<br />
Sandwell Hospital<br />
Training Room 1,<br />
Sandwell Hospital<br />
03/04/<strong>2018</strong> 9am - 4pm IT Library, City Hospital<br />
04/04/<strong>2018</strong> 9am - 4pm IT Library, City Hospital<br />
05/04/<strong>2018</strong> 9am - 4pm<br />
06/04/<strong>2018</strong> 9am - 4pm<br />
Course length 1 day<br />
20/03/<strong>2018</strong> 9am - 4pm<br />
22/03/<strong>2018</strong> 9am - 4pm<br />
26/03/<strong>2018</strong> 9am - 4pm<br />
27/03/<strong>2018</strong> 9am - 4pm<br />
03/04/<strong>2018</strong> 9am - 4pm<br />
04/04/<strong>2018</strong> 9am - 4pm<br />
Course length 1 day<br />
19/03/<strong>2018</strong> 9am - 4pm<br />
28/03/<strong>2018</strong> 9am - 4pm<br />
05/04/<strong>2018</strong> 9am - 4pm<br />
Course length 1 day<br />
21/03/<strong>2018</strong> 9am - 4pm<br />
27/03/<strong>2018</strong> 9am - 4pm<br />
Training Room 1,<br />
Sandwell Hospital<br />
Training Room 1,<br />
Sandwell Hospital<br />
Training Room 1,<br />
Sandwell Hospital<br />
Anne Gibson IT Suite,<br />
City Hospital<br />
Post Graduate Centre,<br />
Room 5, City Hospital<br />
Training Room 1,<br />
Sandwell Hospital<br />
Training Room 1,<br />
Sandwell Hospital<br />
Post Graduate Centre,<br />
Room 5, City Hospital<br />
Post Graduate Centre,<br />
Room 5, City Hospital<br />
Education Centre<br />
Room 8, Sandwell<br />
Hospital<br />
Post Graduate Centre,<br />
Room 5, City Hospital<br />
Post Graduate Centre,<br />
Room 5, City Hospital<br />
Post Graduate Centre,<br />
Room 5, City Hospital<br />
To book on the Unity early adopter training email swbh.informaticsbookings@nhs.net<br />
HB <strong>February</strong> <strong>2018</strong>.indd 28 20/02/<strong>2018</strong> 11:38