Diagnostic Ultrasound - Abdomen and Pelvis
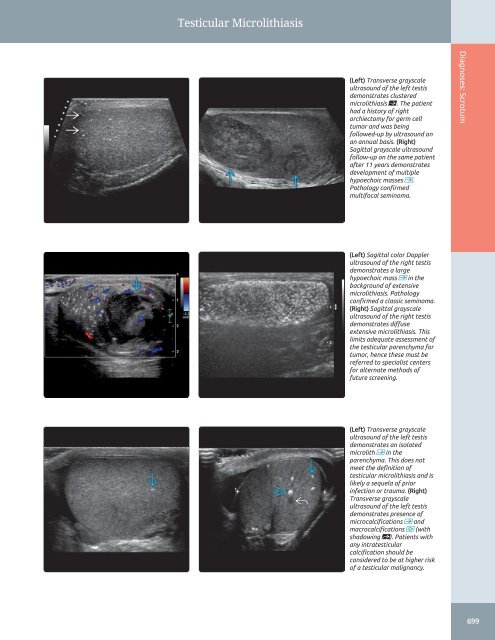
Testicular Microlithiasis (Left) Transverse grayscale ultrasound of the left testis demonstrates clustered microlithiasis ſt. The patient had a history of right orchiectomy for germ cell tumor and was being followed-up by ultrasound on an annual basis. (Right) Sagittal grayscale ultrasound follow-up on the same patient after 11 years demonstrates development of multiple hypoechoic masses . Pathology confirmed multifocal seminoma. Diagnoses: Scrotum (Left) Sagittal color Doppler ultrasound of the right testis demonstrates a large hypoechoic mass in the background of extensive microlithiasis. Pathology confirmed a classic seminoma. (Right) Sagittal grayscale ultrasound of the right testis demonstrates diffuse extensive microlithiasis. This limits adequate assessment of the testicular parenchyma for tumor, hence these must be referred to specialist centers for alternate methods of future screening. (Left) Transverse grayscale ultrasound of the left testis demonstrates an isolated microlith in the parenchyma. This does not meet the definition of testicular microlithiasis and is likely a sequela of prior infection or trauma. (Right) Transverse grayscale ultrasound of the left testis demonstrates presence of microcalcifications and macrocalcifications (with shadowing st). Patients with any intratesticular calcification should be considered to be at higher risk of a testicular malignancy. 699
Testicular Torsion/Infarction Diagnoses: Scrotum TERMINOLOGY • Spontaneous or traumatic twisting of testis & spermatic cord within scrotum, resulting in vascular occlusion/infarction IMAGING • Absent or decreased abnormal testicular blood flow on color Doppler US • Findings vary with duration and degree of rotation of cord • Unilateral in 95% of patients • Role of spectral Doppler is limited; may be helpful to detect partial torsion; in partial torsion of 360° or less, spectral Doppler may show diminished diastolic arterial flow • Spiral twist of spermatic cord cranial to testis and epididymis causing torsion knot or whirlpool pattern of concentric layers KEY FACTS PATHOLOGY • Varying degrees of ischemic necrosis & fibrosis depending on duration of symptoms • Undescended testes have an increased risk of torsion • Intravaginal torsion: Common type, most frequently occurs at puberty CLINICAL ISSUES • Acute scrotal/inguinal pain; swollen, erythematous hemiscrotum without recognized trauma • Reducing time lag between onset of symptoms and time of surgical or manual detorsion is of utmost importance in preserving viable testis • Nonviable testicle usually removed; higher risk of subsequent torsion on contralateral side • Venous obstruction occurs 1st, followed by obstruction of arterial flow, which leads to testicular ischemia (Left) Graphic shows spiral twist st of the spermatic cord with torsion, leading to venous congestion and compromised blood supply to the testis ſt. (Right) Sagittal power Doppler ultrasound of the left testis in a young male with intermittent symptoms of left testicular pain demonstrates a large focal avascular heterogeneous area consistent with infarct that is likely secondary to intermittent torsion. (Left) Transverse color Doppler ultrasound of the testis in a young male with an acute painful scrotum for 48 hours shows a heterogeneous avascular testis with cystic areas st, consistent with an infarcted testis with necrosis secondary to torsion. (Right) Sagittal color Doppler ultrasound superior to the left testis in a young male with acute painful scrotum shows a whirlpool sign secondary to a twisted spermatic cord. Patient was manually detorsed followed by bilateral orchidopexy. 700
- Page 670 and 671: Appendicitis (Left) Axial ultrasoun
- Page 672 and 673: Appendicitis (Left) Axial ultrasoun
- Page 674 and 675: Appendiceal Mucocele TERMINOLOGY De
- Page 676 and 677: Appendiceal Mucocele (Left) Sagitta
- Page 678 and 679: Intussusception TERMINOLOGY Definit
- Page 680 and 681: Intussusception (Left) Transverse t
- Page 682 and 683: Epiploic Appendagitis TERMINOLOGY A
- Page 684 and 685: Epiploic Appendagitis (Left) Graysc
- Page 686 and 687: Diverticulitis TERMINOLOGY Definiti
- Page 688 and 689: Diverticulitis (Left) Acute diverti
- Page 690 and 691: Crohn Disease TERMINOLOGY Synonyms
- Page 692 and 693: Crohn Disease (Left) Long-axis ultr
- Page 694 and 695: Crohn Disease (Left) Long-axis ultr
- Page 696 and 697: Large Bowel Malignancy TERMINOLOGY
- Page 698 and 699: Large Bowel Malignancy (Left) Hepat
- Page 700 and 701: PART II SECTION 10 Scrotum Introduc
- Page 702 and 703: Approach to Scrotal Sonography (Lef
- Page 704 and 705: Testicular Germ Cell Tumors TERMINO
- Page 706 and 707: Testicular Germ Cell Tumors (Left)
- Page 708 and 709: Gonadal Stromal Tumors, Testis TERM
- Page 710 and 711: Gonadal Stromal Tumors, Testis (Lef
- Page 712 and 713: Testicular Lymphoma/Leukemia TERMIN
- Page 714 and 715: Epidermoid Cyst TERMINOLOGY Synonym
- Page 716 and 717: Tubular Ectasia of Rete Testis TERM
- Page 718 and 719: Testicular Microlithiasis TERMINOLO
- Page 722 and 723: Testicular Torsion/Infarction TERMI
- Page 724 and 725: Testicular Torsion/Infarction (Left
- Page 726 and 727: Undescended Testis TERMINOLOGY Syno
- Page 728 and 729: Epididymitis/Orchitis TERMINOLOGY S
- Page 730 and 731: Epididymitis/Orchitis (Left) Sagitt
- Page 732 and 733: Scrotal Trauma TERMINOLOGY Definiti
- Page 734 and 735: Scrotal Trauma (Left) Transverse gr
- Page 736 and 737: Hydrocele TERMINOLOGY Definitions
- Page 738 and 739: Spermatocele/Epididymal Cyst TERMIN
- Page 740 and 741: Adenomatoid Tumor TERMINOLOGY Defin
- Page 742 and 743: Varicocele TERMINOLOGY Definitions
- Page 744 and 745: Non-Ovarian Cystic Masses Hydrosalp
- Page 746 and 747: Approach to Sonography of the Femal
- Page 748 and 749: Nabothian Cyst TERMINOLOGY Synonyms
- Page 750 and 751: Nabothian Cyst (Left) Longitudinal
- Page 752 and 753: Cervical Carcinoma IMAGING General
- Page 754 and 755: Cervical Carcinoma (Left) Longitudi
- Page 756 and 757: Cervical Carcinoma (Left) Longitudi
- Page 758 and 759: Adenomyosis TERMINOLOGY Synonyms
- Page 760 and 761: Adenomyosis (Left) Longitudinal tra
- Page 762 and 763: Leiomyoma TERMINOLOGY Abbreviations
- Page 764 and 765: Leiomyoma (Left) Transvaginal ultra
- Page 766 and 767: Leiomyoma (Left) Transverse transab
- Page 768 and 769: Uterine Anomalies TERMINOLOGY Abbre
Testicular Microlithiasis<br />
(Left) Transverse grayscale<br />
ultrasound of the left testis<br />
demonstrates clustered<br />
microlithiasis ſt. The patient<br />
had a history of right<br />
orchiectomy for germ cell<br />
tumor <strong>and</strong> was being<br />
followed-up by ultrasound on<br />
an annual basis. (Right)<br />
Sagittal grayscale ultrasound<br />
follow-up on the same patient<br />
after 11 years demonstrates<br />
development of multiple<br />
hypoechoic masses .<br />
Pathology confirmed<br />
multifocal seminoma.<br />
Diagnoses: Scrotum<br />
(Left) Sagittal color Doppler<br />
ultrasound of the right testis<br />
demonstrates a large<br />
hypoechoic mass in the<br />
background of extensive<br />
microlithiasis. Pathology<br />
confirmed a classic seminoma.<br />
(Right) Sagittal grayscale<br />
ultrasound of the right testis<br />
demonstrates diffuse<br />
extensive microlithiasis. This<br />
limits adequate assessment of<br />
the testicular parenchyma for<br />
tumor, hence these must be<br />
referred to specialist centers<br />
for alternate methods of<br />
future screening.<br />
(Left) Transverse grayscale<br />
ultrasound of the left testis<br />
demonstrates an isolated<br />
microlith in the<br />
parenchyma. This does not<br />
meet the definition of<br />
testicular microlithiasis <strong>and</strong> is<br />
likely a sequela of prior<br />
infection or trauma. (Right)<br />
Transverse grayscale<br />
ultrasound of the left testis<br />
demonstrates presence of<br />
microcalcifications <strong>and</strong><br />
macrocalcifications (with<br />
shadowing st). Patients with<br />
any intratesticular<br />
calcification should be<br />
considered to be at higher risk<br />
of a testicular malignancy.<br />
699