Diagnostic Ultrasound - Abdomen and Pelvis
Transplant Renal Artery Stenosis TERMINOLOGY Abbreviations • Transplant renal artery stenosis (TRAS) Definitions • Narrowing of the transplant renal artery (TRA) IMAGING General Features • Best diagnostic clue ○ Focal elevation of peak systolic velocity (PSV) with poststenotic turbulence • Location ○ Most commonly at arterial anastomosis ○ Can occur anywhere along transplant artery or there may be diffuse involvement ○ In iliac artery proximal to renal artery graft (pseudo TRAS) • Surgical anatomy ○ End of graft artery-to-side of external iliac artery most common – Performed in living donor and cadaveric grafts ○ Patch of donor aorta along with single or multiple renal arteries anastomosed with recipient external iliac artery – Cadaveric graft only ○ End of graft artery-to-end of internal iliac artery or branch uncommon – Living donor or cadaveric graft Ultrasonographic Findings • Grayscale ultrasound ○ Appearance usually normal • Color Doppler ○ Color aliasing at area of stenosis ○ Soft tissue vibration adjacent to stenosis • Spectral Doppler ○ Direct criteria: Elevated PSV in stenotic area > 250-300 cm/sec – Wide range of PSV in normal graft arteries: 60-200 cm/sec ○ Renal artery to iliac PSV ratio > 1.8-3.5 ○ Sensitivity 87-94%, specificity 86-100 for > 50% stenosis ○ Moderate to severe post-stenotic turbulence ○ Indirect criteria: tardus parvus intrarenal waveforms = slow systolic upstroke and decreased peak velocity – Quantified by acceleration index, acceleration time, and resistive index (RI) □ Prolonged systolic acceleration time > 0.1 s and decreased acceleration index < 3 m/s² □ Low RI < 0.5 – Acceleration index and acceleration time less specific than PSV of main renal artery and should not be used as signs of TRAS in isolation – Note that sensitivity and specificity depend on specific Doppler criteria ○ More proximal stenosis such as common iliac or external iliac stenosis may cause tardus parvus in main renal artery and intrarenal arteries • Ideal screening modality • Contrast-enhanced US ○ Fast and noninvasive evaluation of graft perfusion ○ Time for contrast arrival and rate of inflow correlate with degree of stenosis ○ Use is not limited by renal function Nuclear Medicine Findings • Isotope renography: Lower sensitivity (75%( and specificity (67%) for TRAS • Prolonged tracer transit using MAG3 CT Findings • CTA ○ Comprehensive vascular evaluation including iliac arteries and aorta ○ 3-dimensional images with high spatial resolution, can be rotated for optimal angle ○ Accurate, noninvasive ○ Limited by nephrotoxicity, streak artifact from metal MR Findings • MRA ○ Comprehensive vascular evaluation ○ 3-dimensional images which can be manipulated for optimal angle ○ High sensitivity (67-100%) and high specificity (75-100%) ○ No radiation or nephrotoxic iodinated contrast agents – However, limited by risk of nephrogenic systemic fibrosis when renal function is abnormal ○ Artifacts from surgical clips and metal prostheses may lead to overestimate of stenosis or nondiagnostic study • Nonenhanced MRA techniques increasing in diagnostic value and accuracy ○ For patients with abnormal glomerular filtration rate in whom gadolinium based contrast agents are best avoided Angiographic Findings • Catheter angiography is gold standard but is invasive with potential complications • Confirms stenosis (> 50% stenosis on angiography considered significant) • Pull back pressure gradient across stenosis > 10-20 mmHg suggests significant stenosis • Carbon dioxide angiography useful to limit amount of iodinated contrast • Endovascular intervention can be performed Imaging Recommendations • Best imaging tool ○ Color, power, spectral Doppler US is screening modality for TRAS • Protocol advice ○ Careful attention to Doppler angle to ensure accurate PSV measurements ○ Optimization of pulse repetition frequency and gain is essential DIFFERENTIAL DIAGNOSIS Abrupt Renal Artery Curves and Kinks • Curves and kinks can elevate peak velocity without stenosis Diagnoses: Kidney Transplant 567
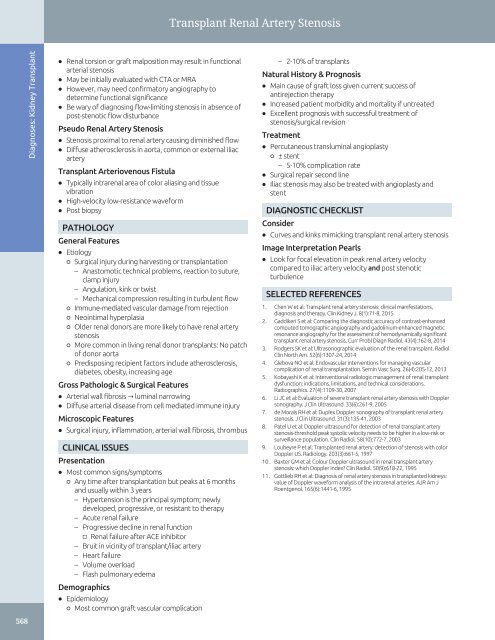
Transplant Renal Artery Stenosis 568 Diagnoses: Kidney Transplant • Renal torsion or graft malposition may result in functional arterial stenosis • May be initially evaluated with CTA or MRA • However, may need confirmatory angiography to determine functional significance • Be wary of diagnosing flow-limiting stenosis in absence of post-stenotic flow disturbance Pseudo Renal Artery Stenosis • Stenosis proximal to renal artery causing diminished flow • Diffuse atherosclerosis in aorta, common or external iliac artery Transplant Arteriovenous Fistula • Typically intrarenal area of color aliasing and tissue vibration • High-velocity low-resistance waveform • Post biopsy PATHOLOGY General Features • Etiology ○ Surgical injury during harvesting or transplantation – Anastomotic technical problems, reaction to suture, clamp injury – Angulation, kink or twist – Mechanical compression resulting in turbulent flow ○ Immune-mediated vascular damage from rejection ○ Neointimal hyperplasia ○ Older renal donors are more likely to have renal artery stenosis ○ More common in living renal donor transplants: No patch of donor aorta ○ Predisposing recipient factors include atherosclerosis, diabetes, obesity, increasing age Gross Pathologic & Surgical Features • Arterial wall fibrosis → luminal narrowing • Diffuse arterial disease from cell mediated immune injury Microscopic Features • Surgical injury, inflammation, arterial wall fibrosis, thrombus CLINICAL ISSUES Presentation • Most common signs/symptoms ○ Any time after transplantation but peaks at 6 months and usually within 3 years – Hypertension is the principal symptom; newly developed, progressive, or resistant to therapy – Acute renal failure – Progressive decline in renal function □ Renal failure after ACE inhibitor – Bruit in vicinity of transplant/iliac artery – Heart failure – Volume overload – Flash pulmonary edema Demographics • Epidemiology ○ Most common graft vascular complication – 2-10% of transplants Natural History & Prognosis • Main cause of graft loss given current success of antirejection therapy • Increased patient morbidity and mortality if untreated • Excellent prognosis with successful treatment of stenosis/surgical revision Treatment • Percutaneous transluminal angioplasty ○ ± stent – 5-10% complication rate • Surgical repair second line • Iliac stenosis may also be treated with angioplasty and stent DIAGNOSTIC CHECKLIST Consider • Curves and kinks mimicking transplant renal artery stenosis Image Interpretation Pearls • Look for focal elevation in peak renal artery velocity compared to iliac artery velocityandpost stenotic turbulence SELECTED REFERENCES 1. Chen W et al: Transplant renal artery stenosis: clinical manifestations, diagnosis and therapy. Clin Kidney J. 8(1):71-8, 2015 2. Gaddikeri S et al: Comparing the diagnostic accuracy of contrast-enhanced computed tomographic angiography and gadolinium-enhanced magnetic resonance angiography for the assessment of hemodynamically significant transplant renal artery stenosis. Curr Probl Diagn Radiol. 43(4):162-8, 2014 3. Rodgers SK et al: Ultrasonographic evaluation of the renal transplant. Radiol Clin North Am. 52(6):1307-24, 2014 4. Glebova NO et al: Endovascular interventions for managing vascular complication of renal transplantation. Semin Vasc Surg. 26(4):205-12, 2013 5. Kobayashi K et al: Interventional radiologic management of renal transplant dysfunction: indications, limitations, and technical considerations. Radiographics. 27(4):1109-30, 2007 6. Li JC et al: Evaluation of severe transplant renal artery stenosis with Doppler sonography. J Clin Ultrasound. 33(6):261-9, 2005 7. de Morais RH et al: Duplex Doppler sonography of transplant renal artery stenosis. J Clin Ultrasound. 31(3):135-41, 2003 8. Patel U et al: Doppler ultrasound for detection of renal transplant artery stenosis-threshold peak systolic velocity needs to be higher in a low-risk or surveillance population. Clin Radiol. 58(10):772-7, 2003 9. Loubeyre P et al: Transplanted renal artery: detection of stenosis with color Doppler US. Radiology. 203(3):661-5, 1997 10. Baxter GM et al: Colour Doppler ultrasound in renal transplant artery stenosis: which Doppler index? Clin Radiol. 50(9):618-22, 1995 11. Gottlieb RH et al: Diagnosis of renal artery stenosis in transplanted kidneys: value of Doppler waveform analysis of the intrarenal arteries. AJR Am J Roentgenol. 165(6):1441-6, 1995
- Page 538 and 539: Renal Vein Thrombosis TERMINOLOGY A
- Page 540 and 541: Renal Vein Thrombosis (Left) Longit
- Page 542 and 543: Renal Infarct TERMINOLOGY Definitio
- Page 544 and 545: Perinephric Hematoma TERMINOLOGY De
- Page 546 and 547: Prostatic Hyperplasia TERMINOLOGY A
- Page 548 and 549: Prostatic Hyperplasia (Left) Axial
- Page 550 and 551: Prostatic Carcinoma TERMINOLOGY Abb
- Page 552 and 553: Prostatic Carcinoma (Left) Transver
- Page 554 and 555: Prostatic Carcinoma (Left) Transver
- Page 556 and 557: Bladder Carcinoma TERMINOLOGY Defin
- Page 558 and 559: Bladder Carcinoma (Left) Transverse
- Page 560 and 561: Ureterocele TERMINOLOGY Definitions
- Page 562 and 563: Ureterocele (Left) Transabdominal l
- Page 564 and 565: Bladder Diverticulum TERMINOLOGY Ab
- Page 566 and 567: Bladder Diverticulum (Left) Transab
- Page 568 and 569: Bladder Calculi TERMINOLOGY Synonym
- Page 570 and 571: Schistosomiasis, Bladder TERMINOLOG
- Page 572 and 573: PART II SECTION 6 Kidney Transplant
- Page 574 and 575: Approach to Sonography of Renal All
- Page 576 and 577: Approach to Sonography of Renal All
- Page 578 and 579: Approach to Sonography of Renal All
- Page 580 and 581: Allograft Hydronephrosis TERMINOLOG
- Page 582 and 583: Allograft Hydronephrosis (Left) Lon
- Page 584 and 585: Perigraft Fluid Collections TERMINO
- Page 586 and 587: Perigraft Fluid Collections (Left)
- Page 590 and 591: Transplant Renal Artery Stenosis (L
- Page 592 and 593: Transplant Renal Artery Thrombosis
- Page 594 and 595: Transplant Renal Vein Thrombosis TE
- Page 596 and 597: Renal Transplant Arteriovenous (AV)
- Page 598 and 599: Renal Transplant Pseudoaneurysm TER
- Page 600 and 601: Renal Transplant Rejection IMAGING
- Page 602 and 603: Delayed Renal Graft Function TERMIN
- Page 604 and 605: PART II SECTION 7 Adrenal Gland Adr
- Page 606 and 607: Adrenal Hemorrhage TERMINOLOGY Abbr
- Page 608 and 609: Adrenal Hemorrhage (Left) Longitudi
- Page 610 and 611: Myelolipoma TERMINOLOGY Definitions
- Page 612 and 613: Myelolipoma (Left) Longitudinal US
- Page 614 and 615: Adrenal Adenoma TERMINOLOGY Synonym
- Page 616 and 617: Adrenal Adenoma (Left) Longitudinal
- Page 618 and 619: Adrenal Cyst TERMINOLOGY Definition
- Page 620 and 621: Pheochromocytoma TERMINOLOGY Defini
- Page 622 and 623: Pheochromocytoma (Left) Longitudina
- Page 624 and 625: Adrenal Carcinoma TERMINOLOGY Synon
- Page 626 and 627: Adrenal Carcinoma (Left) Transverse
- Page 628 and 629: PART II SECTION 8 Abdominal Wall/Pe
- Page 630 and 631: Approach to Sonography of Abdominal
- Page 632 and 633: Approach to Sonography of Abdominal
- Page 634 and 635: Abdominal Wall Hernia TERMINOLOGY D
- Page 636 and 637: Abdominal Wall Hernia (Left) Transv
Transplant Renal Artery Stenosis<br />
568<br />
Diagnoses: Kidney Transplant<br />
• Renal torsion or graft malposition may result in functional<br />
arterial stenosis<br />
• May be initially evaluated with CTA or MRA<br />
• However, may need confirmatory angiography to<br />
determine functional significance<br />
• Be wary of diagnosing flow-limiting stenosis in absence of<br />
post-stenotic flow disturbance<br />
Pseudo Renal Artery Stenosis<br />
• Stenosis proximal to renal artery causing diminished flow<br />
• Diffuse atherosclerosis in aorta, common or external iliac<br />
artery<br />
Transplant Arteriovenous Fistula<br />
• Typically intrarenal area of color aliasing <strong>and</strong> tissue<br />
vibration<br />
• High-velocity low-resistance waveform<br />
• Post biopsy<br />
PATHOLOGY<br />
General Features<br />
• Etiology<br />
○ Surgical injury during harvesting or transplantation<br />
– Anastomotic technical problems, reaction to suture,<br />
clamp injury<br />
– Angulation, kink or twist<br />
– Mechanical compression resulting in turbulent flow<br />
○ Immune-mediated vascular damage from rejection<br />
○ Neointimal hyperplasia<br />
○ Older renal donors are more likely to have renal artery<br />
stenosis<br />
○ More common in living renal donor transplants: No patch<br />
of donor aorta<br />
○ Predisposing recipient factors include atherosclerosis,<br />
diabetes, obesity, increasing age<br />
Gross Pathologic & Surgical Features<br />
• Arterial wall fibrosis → luminal narrowing<br />
• Diffuse arterial disease from cell mediated immune injury<br />
Microscopic Features<br />
• Surgical injury, inflammation, arterial wall fibrosis, thrombus<br />
CLINICAL ISSUES<br />
Presentation<br />
• Most common signs/symptoms<br />
○ Any time after transplantation but peaks at 6 months<br />
<strong>and</strong> usually within 3 years<br />
– Hypertension is the principal symptom; newly<br />
developed, progressive, or resistant to therapy<br />
– Acute renal failure<br />
– Progressive decline in renal function<br />
□ Renal failure after ACE inhibitor<br />
– Bruit in vicinity of transplant/iliac artery<br />
– Heart failure<br />
– Volume overload<br />
– Flash pulmonary edema<br />
Demographics<br />
• Epidemiology<br />
○ Most common graft vascular complication<br />
– 2-10% of transplants<br />
Natural History & Prognosis<br />
• Main cause of graft loss given current success of<br />
antirejection therapy<br />
• Increased patient morbidity <strong>and</strong> mortality if untreated<br />
• Excellent prognosis with successful treatment of<br />
stenosis/surgical revision<br />
Treatment<br />
• Percutaneous transluminal angioplasty<br />
○ ± stent<br />
– 5-10% complication rate<br />
• Surgical repair second line<br />
• Iliac stenosis may also be treated with angioplasty <strong>and</strong><br />
stent<br />
DIAGNOSTIC CHECKLIST<br />
Consider<br />
• Curves <strong>and</strong> kinks mimicking transplant renal artery stenosis<br />
Image Interpretation Pearls<br />
• Look for focal elevation in peak renal artery velocity<br />
compared to iliac artery velocity<strong>and</strong>post stenotic<br />
turbulence<br />
SELECTED REFERENCES<br />
1. Chen W et al: Transplant renal artery stenosis: clinical manifestations,<br />
diagnosis <strong>and</strong> therapy. Clin Kidney J. 8(1):71-8, 2015<br />
2. Gaddikeri S et al: Comparing the diagnostic accuracy of contrast-enhanced<br />
computed tomographic angiography <strong>and</strong> gadolinium-enhanced magnetic<br />
resonance angiography for the assessment of hemodynamically significant<br />
transplant renal artery stenosis. Curr Probl Diagn Radiol. 43(4):162-8, 2014<br />
3. Rodgers SK et al: Ultrasonographic evaluation of the renal transplant. Radiol<br />
Clin North Am. 52(6):1307-24, 2014<br />
4. Glebova NO et al: Endovascular interventions for managing vascular<br />
complication of renal transplantation. Semin Vasc Surg. 26(4):205-12, 2013<br />
5. Kobayashi K et al: Interventional radiologic management of renal transplant<br />
dysfunction: indications, limitations, <strong>and</strong> technical considerations.<br />
Radiographics. 27(4):1109-30, 2007<br />
6. Li JC et al: Evaluation of severe transplant renal artery stenosis with Doppler<br />
sonography. J Clin <strong>Ultrasound</strong>. 33(6):261-9, 2005<br />
7. de Morais RH et al: Duplex Doppler sonography of transplant renal artery<br />
stenosis. J Clin <strong>Ultrasound</strong>. 31(3):135-41, 2003<br />
8. Patel U et al: Doppler ultrasound for detection of renal transplant artery<br />
stenosis-threshold peak systolic velocity needs to be higher in a low-risk or<br />
surveillance population. Clin Radiol. 58(10):772-7, 2003<br />
9. Loubeyre P et al: Transplanted renal artery: detection of stenosis with color<br />
Doppler US. Radiology. 203(3):661-5, 1997<br />
10. Baxter GM et al: Colour Doppler ultrasound in renal transplant artery<br />
stenosis: which Doppler index? Clin Radiol. 50(9):618-22, 1995<br />
11. Gottlieb RH et al: Diagnosis of renal artery stenosis in transplanted kidneys:<br />
value of Doppler waveform analysis of the intrarenal arteries. AJR Am J<br />
Roentgenol. 165(6):1441-6, 1995