Diagnostic Ultrasound - Abdomen and Pelvis
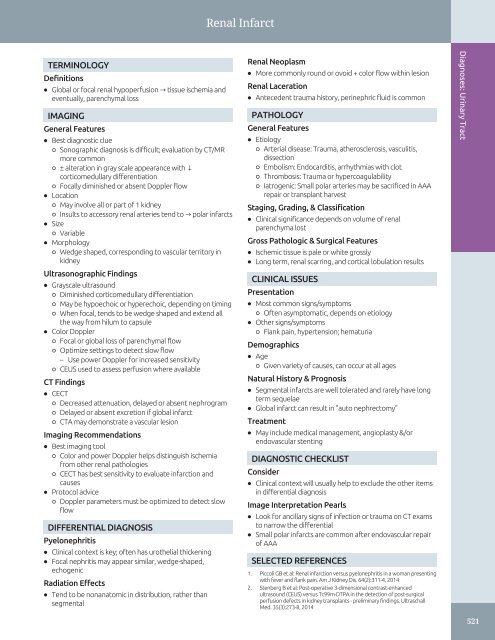
Renal Infarct TERMINOLOGY Definitions • Global or focal renal hypoperfusion → tissue ischemia and eventually, parenchymal loss IMAGING General Features • Best diagnostic clue ○ Sonographic diagnosis is difficult; evaluation by CT/MR more common ○ ± alteration in gray scale appearance with ↓ corticomedullary differentiation ○ Focally diminished or absent Doppler flow • Location ○ May involve all or part of 1 kidney ○ Insults to accessory renal arteries tend to → polar infarcts • Size ○ Variable • Morphology ○ Wedge shaped, corresponding to vascular territory in kidney Ultrasonographic Findings • Grayscale ultrasound ○ Diminished corticomedullary differentiation ○ May be hypoechoic or hyperechoic, depending on timing ○ When focal, tends to be wedge shaped and extend all the way from hilum to capsule • Color Doppler ○ Focal or global loss of parenchymal flow ○ Optimize settings to detect slow flow – Use power Doppler for increased sensitivity ○ CEUS used to assess perfusion where available CT Findings • CECT ○ Decreased attenuation, delayed or absent nephrogram ○ Delayed or absent excretion if global infarct ○ CTA may demonstrate a vascular lesion Imaging Recommendations • Best imaging tool ○ Color and power Doppler helps distinguish ischemia from other renal pathologies ○ CECT has best sensitivity to evaluate infarction and causes • Protocol advice ○ Doppler parameters must be optimized to detect slow flow DIFFERENTIAL DIAGNOSIS Pyelonephritis • Clinical context is key; often has urothelial thickening • Focal nephritis may appear similar, wedge-shaped, echogenic Radiation Effects • Tend to be nonanatomic in distribution, rather than segmental Renal Neoplasm • More commonly round or ovoid + color flow within lesion Renal Laceration • Antecedent trauma history, perinephric fluid is common PATHOLOGY General Features • Etiology ○ Arterial disease: Trauma, atherosclerosis, vasculitis, dissection ○ Embolism: Endocarditis, arrhythmias with clot ○ Thrombosis: Trauma or hypercoagulability ○ Iatrogenic: Small polar arteries may be sacrificed in AAA repair or transplant harvest Staging, Grading, & Classification • Clinical significance depends on volume of renal parenchyma lost Gross Pathologic & Surgical Features • Ischemic tissue is pale or white grossly • Long term, renal scarring, and cortical lobulation results CLINICAL ISSUES Presentation • Most common signs/symptoms ○ Often asymptomatic, depends on etiology • Other signs/symptoms ○ Flank pain, hypertension; hematuria Demographics • Age ○ Given variety of causes, can occur at all ages Natural History & Prognosis • Segmental infarcts are well tolerated and rarely have long term sequelae • Global infarct can result in "auto nephrectomy" Treatment • May include medical management, angioplasty &/or endovascular stenting DIAGNOSTIC CHECKLIST Consider • Clinical context will usually help to exclude the other items in differential diagnosis Image Interpretation Pearls • Look for ancillary signs of infection or trauma on CT exams to narrow the differential • Small polar infarcts are common after endovascular repair of AAA SELECTED REFERENCES 1. Piccoli GB et al: Renal infarction versus pyelonephritis in a woman presenting with fever and flank pain. Am J Kidney Dis. 64(2):311-4, 2014 2. Stenberg B et al: Post-operative 3-dimensional contrast-enhanced ultrasound (CEUS) versus Tc99m-DTPA in the detection of post-surgical perfusion defects in kidney transplants - preliminary findings. Ultraschall Med. 35(3):273-8, 2014 Diagnoses: Urinary Tract 521
Perinephric Hematoma Diagnoses: Urinary Tract TERMINOLOGY • Hemorrhagic collection in perinephric spaces: Subcapsular, perirenal, anterior and posterior pararenal IMAGING • Avascular solid or cystic masses in 1 or more perinephric spaces • Echogenicity of blood changes over time • Sonographic features vary over time ○ Acute: Highly echogenic perinephric mass ○ Subacute: Partial liquefaction, echogenic debris, retractile clot with thick septa ○ Chronic: May be almost anechoic • Useful to assess perfusion in compressed kidney • Sometimes reveals etiologies such as pseudoaneurysm TOP DIFFERENTIAL DIAGNOSES • Lymphoma infiltration • Cystic lymphangioma KEY FACTS • Perinephric abscess PATHOLOGY • Causes include trauma, renal biopsy, renal cyst or tumor rupture, anticoagulation, aneurysm rupture CLINICAL ISSUES • Treatment varies with etiology • Hematoma without underlying significant pathology usually resolves spontaneously • Flank pain, often severe, palpable mass, shock • Diminished hematocrit may prompt evaluation • Subcapsular hematoma may cause hypertension DIAGNOSTIC CHECKLIST • Must identify underlying etiology in spontaneous perinephric hematoma to exclude malignancy (Left) Transverse color Doppler US of a 6 year old after stent placement shows a grossly enlarged renal contour st due to large echogenic perinephric hematoma. The relatively hypoechoic kidney is seen in the center of the mass , demonstrating how hyperechoic acute blood can obscure normal structures. (Right) Transverse color Doppler US shows a large, spontaneous perinephric hematoma with mixed echogenicity . Note occult RCC must be considered in spontaneous hemorrhage. (Left) Longitudinal US in a young man with left flank pain after collision during a soccer game illustrates a thick, irregular soft tissue rind of blood surrounding the left kidney. (Right) CT confirms an extensive perinephric hematoma in the same patient, with associated renal lacerations . 522
- Page 492 and 493: Cystic Disease of Dialysis TERMINOL
- Page 494 and 495: Cystic Disease of Dialysis (Left) L
- Page 496 and 497: Multilocular Cystic Nephroma TERMIN
- Page 498 and 499: Acute Pyelonephritis TERMINOLOGY Ab
- Page 500 and 501: Acute Pyelonephritis (Left) Longitu
- Page 502 and 503: Renal Abscess TERMINOLOGY Definitio
- Page 504 and 505: Emphysematous Pyelonephritis TERMIN
- Page 506 and 507: Emphysematous Pyelonephritis (Left)
- Page 508 and 509: Pyonephrosis TERMINOLOGY Definition
- Page 510 and 511: Xanthogranulomatous Pyelonephritis
- Page 512 and 513: Tuberculosis, Urinary Tract TERMINO
- Page 514 and 515: Tuberculosis, Urinary Tract (Left)
- Page 516 and 517: Renal Cell Carcinoma TERMINOLOGY Ab
- Page 518 and 519: Renal Cell Carcinoma (Left) Longitu
- Page 520 and 521: Renal Metastases IMAGING General Fe
- Page 522 and 523: Renal Angiomyolipoma TERMINOLOGY Ab
- Page 524 and 525: Renal Angiomyolipoma (Left) Longitu
- Page 526 and 527: Upper Tract Urothelial Carcinoma TE
- Page 528 and 529: Upper Tract Urothelial Carcinoma (L
- Page 530 and 531: Renal Lymphoma TERMINOLOGY Abbrevia
- Page 532 and 533: Renal Lymphoma (Left) Longitudinal
- Page 534 and 535: Renal Artery Stenosis TERMINOLOGY A
- Page 536 and 537: Renal Artery Stenosis (Left) Obliqu
- Page 538 and 539: Renal Vein Thrombosis TERMINOLOGY A
- Page 540 and 541: Renal Vein Thrombosis (Left) Longit
- Page 544 and 545: Perinephric Hematoma TERMINOLOGY De
- Page 546 and 547: Prostatic Hyperplasia TERMINOLOGY A
- Page 548 and 549: Prostatic Hyperplasia (Left) Axial
- Page 550 and 551: Prostatic Carcinoma TERMINOLOGY Abb
- Page 552 and 553: Prostatic Carcinoma (Left) Transver
- Page 554 and 555: Prostatic Carcinoma (Left) Transver
- Page 556 and 557: Bladder Carcinoma TERMINOLOGY Defin
- Page 558 and 559: Bladder Carcinoma (Left) Transverse
- Page 560 and 561: Ureterocele TERMINOLOGY Definitions
- Page 562 and 563: Ureterocele (Left) Transabdominal l
- Page 564 and 565: Bladder Diverticulum TERMINOLOGY Ab
- Page 566 and 567: Bladder Diverticulum (Left) Transab
- Page 568 and 569: Bladder Calculi TERMINOLOGY Synonym
- Page 570 and 571: Schistosomiasis, Bladder TERMINOLOG
- Page 572 and 573: PART II SECTION 6 Kidney Transplant
- Page 574 and 575: Approach to Sonography of Renal All
- Page 576 and 577: Approach to Sonography of Renal All
- Page 578 and 579: Approach to Sonography of Renal All
- Page 580 and 581: Allograft Hydronephrosis TERMINOLOG
- Page 582 and 583: Allograft Hydronephrosis (Left) Lon
- Page 584 and 585: Perigraft Fluid Collections TERMINO
- Page 586 and 587: Perigraft Fluid Collections (Left)
- Page 588 and 589: Transplant Renal Artery Stenosis TE
- Page 590 and 591: Transplant Renal Artery Stenosis (L
Renal Infarct<br />
TERMINOLOGY<br />
Definitions<br />
• Global or focal renal hypoperfusion → tissue ischemia <strong>and</strong><br />
eventually, parenchymal loss<br />
IMAGING<br />
General Features<br />
• Best diagnostic clue<br />
○ Sonographic diagnosis is difficult; evaluation by CT/MR<br />
more common<br />
○ ± alteration in gray scale appearance with ↓<br />
corticomedullary differentiation<br />
○ Focally diminished or absent Doppler flow<br />
• Location<br />
○ May involve all or part of 1 kidney<br />
○ Insults to accessory renal arteries tend to → polar infarcts<br />
• Size<br />
○ Variable<br />
• Morphology<br />
○ Wedge shaped, corresponding to vascular territory in<br />
kidney<br />
Ultrasonographic Findings<br />
• Grayscale ultrasound<br />
○ Diminished corticomedullary differentiation<br />
○ May be hypoechoic or hyperechoic, depending on timing<br />
○ When focal, tends to be wedge shaped <strong>and</strong> extend all<br />
the way from hilum to capsule<br />
• Color Doppler<br />
○ Focal or global loss of parenchymal flow<br />
○ Optimize settings to detect slow flow<br />
– Use power Doppler for increased sensitivity<br />
○ CEUS used to assess perfusion where available<br />
CT Findings<br />
• CECT<br />
○ Decreased attenuation, delayed or absent nephrogram<br />
○ Delayed or absent excretion if global infarct<br />
○ CTA may demonstrate a vascular lesion<br />
Imaging Recommendations<br />
• Best imaging tool<br />
○ Color <strong>and</strong> power Doppler helps distinguish ischemia<br />
from other renal pathologies<br />
○ CECT has best sensitivity to evaluate infarction <strong>and</strong><br />
causes<br />
• Protocol advice<br />
○ Doppler parameters must be optimized to detect slow<br />
flow<br />
DIFFERENTIAL DIAGNOSIS<br />
Pyelonephritis<br />
• Clinical context is key; often has urothelial thickening<br />
• Focal nephritis may appear similar, wedge-shaped,<br />
echogenic<br />
Radiation Effects<br />
• Tend to be nonanatomic in distribution, rather than<br />
segmental<br />
Renal Neoplasm<br />
• More commonly round or ovoid + color flow within lesion<br />
Renal Laceration<br />
• Antecedent trauma history, perinephric fluid is common<br />
PATHOLOGY<br />
General Features<br />
• Etiology<br />
○ Arterial disease: Trauma, atherosclerosis, vasculitis,<br />
dissection<br />
○ Embolism: Endocarditis, arrhythmias with clot<br />
○ Thrombosis: Trauma or hypercoagulability<br />
○ Iatrogenic: Small polar arteries may be sacrificed in AAA<br />
repair or transplant harvest<br />
Staging, Grading, & Classification<br />
• Clinical significance depends on volume of renal<br />
parenchyma lost<br />
Gross Pathologic & Surgical Features<br />
• Ischemic tissue is pale or white grossly<br />
• Long term, renal scarring, <strong>and</strong> cortical lobulation results<br />
CLINICAL ISSUES<br />
Presentation<br />
• Most common signs/symptoms<br />
○ Often asymptomatic, depends on etiology<br />
• Other signs/symptoms<br />
○ Flank pain, hypertension; hematuria<br />
Demographics<br />
• Age<br />
○ Given variety of causes, can occur at all ages<br />
Natural History & Prognosis<br />
• Segmental infarcts are well tolerated <strong>and</strong> rarely have long<br />
term sequelae<br />
• Global infarct can result in "auto nephrectomy"<br />
Treatment<br />
• May include medical management, angioplasty &/or<br />
endovascular stenting<br />
DIAGNOSTIC CHECKLIST<br />
Consider<br />
• Clinical context will usually help to exclude the other items<br />
in differential diagnosis<br />
Image Interpretation Pearls<br />
• Look for ancillary signs of infection or trauma on CT exams<br />
to narrow the differential<br />
• Small polar infarcts are common after endovascular repair<br />
of AAA<br />
SELECTED REFERENCES<br />
1. Piccoli GB et al: Renal infarction versus pyelonephritis in a woman presenting<br />
with fever <strong>and</strong> flank pain. Am J Kidney Dis. 64(2):311-4, 2014<br />
2. Stenberg B et al: Post-operative 3-dimensional contrast-enhanced<br />
ultrasound (CEUS) versus Tc99m-DTPA in the detection of post-surgical<br />
perfusion defects in kidney transplants - preliminary findings. Ultraschall<br />
Med. 35(3):273-8, 2014<br />
Diagnoses: Urinary Tract<br />
521