Diagnostic Ultrasound - Abdomen and Pelvis
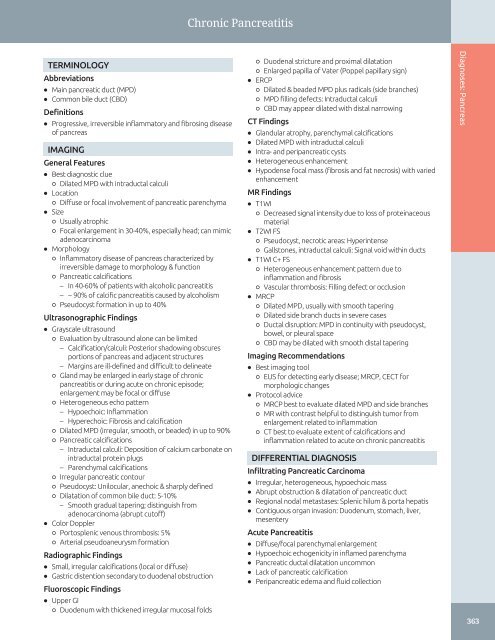
Chronic Pancreatitis TERMINOLOGY Abbreviations • Main pancreatic duct (MPD) • Common bile duct (CBD) Definitions • Progressive, irreversible inflammatory and fibrosing disease of pancreas IMAGING General Features • Best diagnostic clue ○ Dilated MPD with intraductal calculi • Location ○ Diffuse or focal involvement of pancreatic parenchyma • Size ○ Usually atrophic ○ Focal enlargement in 30-40%, especially head; can mimic adenocarcinoma • Morphology ○ Inflammatory disease of pancreas characterized by irreversible damage to morphology & function ○ Pancreatic calcifications – In 40-60% of patients with alcoholic pancreatitis – ~ 90% of calcific pancreatitis caused by alcoholism ○ Pseudocyst formation in up to 40% Ultrasonographic Findings • Grayscale ultrasound ○ Evaluation by ultrasound alone can be limited – Calcification/calculi: Posterior shadowing obscures portions of pancreas and adjacent structures – Margins are ill-defined and difficult to delineate ○ Gland may be enlarged in early stage of chronic pancreatitis or during acute on chronic episode; enlargement may be focal or diffuse ○ Heterogeneous echo pattern – Hypoechoic: Inflammation – Hyperechoic: Fibrosis and calcification ○ Dilated MPD (irregular, smooth, or beaded) in up to 90% ○ Pancreatic calcifications – Intraductal calculi: Deposition of calcium carbonate on intraductal protein plugs – Parenchymal calcifications ○ Irregular pancreatic contour ○ Pseudocyst: Unilocular, anechoic & sharply defined ○ Dilatation of common bile duct: 5-10% – Smooth gradual tapering; distinguish from adenocarcinoma (abrupt cutoff) • Color Doppler ○ Portosplenic venous thrombosis: 5% ○ Arterial pseudoaneurysm formation Radiographic Findings • Small, irregular calcifications (local or diffuse) • Gastric distention secondary to duodenal obstruction Fluoroscopic Findings • Upper GI ○ Duodenum with thickened irregular mucosal folds ○ Duodenal stricture and proximal dilatation ○ Enlarged papilla of Vater (Poppel papillary sign) • ERCP ○ Dilated & beaded MPD plus radicals (side branches) ○ MPD filling defects: Intraductal calculi ○ CBD may appear dilated with distal narrowing CT Findings • Glandular atrophy, parenchymal calcifications • Dilated MPD with intraductal calculi • Intra- and peripancreatic cysts • Heterogeneous enhancement • Hypodense focal mass (fibrosis and fat necrosis) with varied enhancement MR Findings • T1WI ○ Decreased signal intensity due to loss of proteinaceous material • T2WI FS ○ Pseudocyst, necrotic areas: Hyperintense ○ Gallstones, intraductal calculi: Signal void within ducts • T1WI C+ FS ○ Heterogeneous enhancement pattern due to inflammation and fibrosis ○ Vascular thrombosis: Filling defect or occlusion • MRCP ○ Dilated MPD, usually with smooth tapering ○ Dilated side branch ducts in severe cases ○ Ductal disruption: MPD in continuity with pseudocyst, bowel, or pleural space ○ CBD may be dilated with smooth distal tapering Imaging Recommendations • Best imaging tool ○ EUS for detecting early disease; MRCP, CECT for morphologic changes • Protocol advice ○ MRCP best to evaluate dilated MPD and side branches ○ MR with contrast helpful to distinguish tumor from enlargement related to inflammation ○ CT best to evaluate extent of calcifications and inflammation related to acute on chronic pancreatitis DIFFERENTIAL DIAGNOSIS Infiltrating Pancreatic Carcinoma • Irregular, heterogeneous, hypoechoic mass • Abrupt obstruction & dilatation of pancreatic duct • Regional nodal metastases: Splenic hilum & porta hepatis • Contiguous organ invasion: Duodenum, stomach, liver, mesentery Acute Pancreatitis • Diffuse/focal parenchymal enlargement • Hypoechoic echogenicity in inflamed parenchyma • Pancreatic ductal dilatation uncommon • Lack of pancreatic calcification • Peripancreatic edema and fluid collection Diagnoses: Pancreas 363
Chronic Pancreatitis Diagnoses: Pancreas Intraductal Papillary Mucinous Neoplasm (IPMN) of Pancreas • Low-grade malignancy arising from main pancreatic duct or side branches • Involvement of main pancreatic duct may simulate chronic pancreatitis • Dilated MPD and parenchymal atrophy Groove Pancreatitis • Focal chronic pancreatitis in pancreatoduodenal groove • Sheet-like fibrotic mass between pancreas and thickened duodenal wall • Smooth tapering of distal CBD Autoimmune Pancreatitis • Focal or diffuse enlargement • Narrowed pancreatic duct • Lack of calcifications or fluid collections PATHOLOGY General Features • Etiology ○ Alcohol abuse is most common cause in USA ○ Hyperlipidemia, hyperparathyroidism (hypercalcemia), trauma ○ Idiopathic in up to 40% ○ Gallstones not considered risk factor ○ Pathogenesis: Chronic reflux of pancreatic enzymes, bile, duodenal contents & increased ductal pressure – MPD or terminal duct blockage – Edema, spasm, or incompetent sphincter of Oddi – Periduodenal diverticulum or tumor causing obstruction • Genetics ○ Cystic fibrosis ○ Hereditary pancreatitis: Autosomal dominant with incomplete penetrance • Embryological consideration ○ Pancreas divisum: Minor papilla too small to adequately drain pancreatic secretions, leading to chronic stasis ○ Annular pancreas: Pancreatic ductal obstruction and stasis of secretions Gross Pathologic & Surgical Features • Hard atrophic pancreas with intraductal calculi & dilated MPD • Areas of multiple parenchymal calcifications • Pseudocysts may be seen Microscopic Features • Atrophy & fibrosis of acini with dilated ducts • Mononuclear inflammatory reaction • Occasionally squamous metaplasia of ductal epithelium CLINICAL ISSUES Presentation • Most common signs/symptoms ○ Recurrent attacks of epigastric pain, occasionally radiating to back ○ Diarrhea secondary to exocrine deficiency ○ Weight loss from exocrine dysfunction, pain, or duodenal obstruction • Clinical profile ○ Patient with history of chronic alcoholism, recurrent attacks of epigastric pain, diarrhea, and weight loss ○ Diagnosis usually not made until years following initial onset of symptoms • Labs ○ Serum and fecal markers not sensitive or specific; helpful only in advanced disease ○ Pancreatic exocrine function hormone stimulation tests are helpful in early disease but not widely available Demographics • Age ○ Mean: 5th decade • Gender ○ Males > females • Epidemiology ○ More common in developing countries Natural History & Prognosis • Pseudocyst formation • Diabetes mellitus in ~ 1/3 of patients • Splenic vein thrombosis, portal hypertension • Increased incidence of pancreatic cancer: ~ 4% at 20 years • Increased mortality: 30% at 10 years, 55% at 20 years Treatment • Surgical or endoscopic intervention ○ Ductal & GI obstruction ○ GI bleeding ○ Large pseudocyst or persistently symptomatic • Conservative treatment if no major complication (e.g., pain control, medical therapy for diabetes mellitus, etc.) DIAGNOSTIC CHECKLIST Consider • Differentiate from other conditions that can cause MPD dilatation & glandular atrophy • May be very difficult to distinguish chronic pancreatitis with focal fibrotic enlargement of head from pancreatic adenocarcinoma Image Interpretation Pearls • Glandular atrophy, dilated MPD, and intraductal calculi/parenchymal calcifications are best signs for chronic pancreatitis SELECTED REFERENCES 1. Choueiri NE et al: Advanced imaging of chronic pancreatitis. Curr Gastroenterol Rep. 12(2):114-20, 2010 2. Siddiqi AJ et al: Chronic pancreatitis: ultrasound, computed tomography, and magnetic resonance imaging features. Semin Ultrasound CT MR. 28(5):384-94, 2007 3. Bruno MJ: Chronic pancreatitis. Gastrointest Endosc Clin N Am. 15(1):55-62, viii, 2005 4. Lankisch PG: The problem of diagnosing chronic pancreatitis. Dig Liver Dis. 35(3):131-4, 2003 5. Varghese JC et al: Value of MR pancreatography in the evaluation of patients with chronic pancreatitis. Clin Radiol. 57(5):393-401, 2002 364
- Page 334 and 335: Porcelain Gallbladder TERMINOLOGY A
- Page 336 and 337: Hyperplastic Cholecystosis (Adenomy
- Page 338 and 339: Hyperplastic Cholecystosis (Adenomy
- Page 340 and 341: Gallbladder Carcinoma TERMINOLOGY A
- Page 342 and 343: Gallbladder Carcinoma (Left) Sagitt
- Page 344 and 345: Biliary Ductal Dilatation IMAGING G
- Page 346 and 347: Choledochal Cyst TERMINOLOGY Synony
- Page 348 and 349: Choledochal Cyst (Left) Longitudina
- Page 350 and 351: Choledocholithiasis TERMINOLOGY Abb
- Page 352 and 353: Choledocholithiasis (Left) A single
- Page 354 and 355: Biliary Ductal Gas TERMINOLOGY Syno
- Page 356 and 357: Cholangiocarcinoma TERMINOLOGY Syno
- Page 358 and 359: Cholangiocarcinoma (Left) Ultrasoun
- Page 360 and 361: Ascending Cholangitis TERMINOLOGY S
- Page 362 and 363: Ascending Cholangitis (Left) Longit
- Page 364 and 365: Recurrent Pyogenic Cholangitis TERM
- Page 366 and 367: Recurrent Pyogenic Cholangitis (Lef
- Page 368 and 369: AIDS-Related Cholangiopathy TERMINO
- Page 370 and 371: PART II SECTION 3 Pancreas Introduc
- Page 372 and 373: Approach to Pancreatic Sonography C
- Page 374 and 375: Approach to Pancreatic Sonography (
- Page 376 and 377: Acute Pancreatitis TERMINOLOGY Abbr
- Page 378 and 379: Acute Pancreatitis (Left) Transvers
- Page 380 and 381: Pancreatic Pseudocyst TERMINOLOGY D
- Page 382 and 383: Pancreatic Pseudocyst (Left) Transv
- Page 386 and 387: Chronic Pancreatitis (Left) Transve
- Page 388 and 389: Mucinous Cystic Pancreatic Tumor TE
- Page 390 and 391: Mucinous Cystic Pancreatic Tumor (L
- Page 392 and 393: Serous Cystadenoma of Pancreas TERM
- Page 394 and 395: Serous Cystadenoma of Pancreas (Lef
- Page 396 and 397: Intraductal Papillary Mucinous Neop
- Page 398 and 399: Intraductal Papillary Mucinous Neop
- Page 400 and 401: Intraductal Papillary Mucinous Neop
- Page 402 and 403: Pancreatic Ductal Carcinoma TERMINO
- Page 404 and 405: Pancreatic Ductal Carcinoma (Left)
- Page 406 and 407: Pancreatic Neuroendocrine Tumor TER
- Page 408 and 409: Pancreatic Neuroendocrine Tumor (Le
- Page 410 and 411: Solid Pseudopapillary Neoplasm TERM
- Page 412 and 413: Solid Pseudopapillary Neoplasm (Lef
- Page 414 and 415: PART II SECTION 4 Spleen Introducti
- Page 416 and 417: Approach to Splenic Sonography sple
- Page 418 and 419: Approach to Splenic Sonography (Lef
- Page 420 and 421: Approach to Splenic Sonography (Lef
- Page 422 and 423: Splenomegaly TERMINOLOGY Abbreviati
- Page 424 and 425: Splenomegaly (Left) US in a 92-year
- Page 426 and 427: Splenic Cyst TERMINOLOGY Definition
- Page 428 and 429: Splenic Cyst (Left) Grayscale US of
- Page 430 and 431: Splenic Tumors TERMINOLOGY Definiti
- Page 432 and 433: Splenic Tumors (Left) Longitudinal
Chronic Pancreatitis<br />
TERMINOLOGY<br />
Abbreviations<br />
• Main pancreatic duct (MPD)<br />
• Common bile duct (CBD)<br />
Definitions<br />
• Progressive, irreversible inflammatory <strong>and</strong> fibrosing disease<br />
of pancreas<br />
IMAGING<br />
General Features<br />
• Best diagnostic clue<br />
○ Dilated MPD with intraductal calculi<br />
• Location<br />
○ Diffuse or focal involvement of pancreatic parenchyma<br />
• Size<br />
○ Usually atrophic<br />
○ Focal enlargement in 30-40%, especially head; can mimic<br />
adenocarcinoma<br />
• Morphology<br />
○ Inflammatory disease of pancreas characterized by<br />
irreversible damage to morphology & function<br />
○ Pancreatic calcifications<br />
– In 40-60% of patients with alcoholic pancreatitis<br />
– ~ 90% of calcific pancreatitis caused by alcoholism<br />
○ Pseudocyst formation in up to 40%<br />
Ultrasonographic Findings<br />
• Grayscale ultrasound<br />
○ Evaluation by ultrasound alone can be limited<br />
– Calcification/calculi: Posterior shadowing obscures<br />
portions of pancreas <strong>and</strong> adjacent structures<br />
– Margins are ill-defined <strong>and</strong> difficult to delineate<br />
○ Gl<strong>and</strong> may be enlarged in early stage of chronic<br />
pancreatitis or during acute on chronic episode;<br />
enlargement may be focal or diffuse<br />
○ Heterogeneous echo pattern<br />
– Hypoechoic: Inflammation<br />
– Hyperechoic: Fibrosis <strong>and</strong> calcification<br />
○ Dilated MPD (irregular, smooth, or beaded) in up to 90%<br />
○ Pancreatic calcifications<br />
– Intraductal calculi: Deposition of calcium carbonate on<br />
intraductal protein plugs<br />
– Parenchymal calcifications<br />
○ Irregular pancreatic contour<br />
○ Pseudocyst: Unilocular, anechoic & sharply defined<br />
○ Dilatation of common bile duct: 5-10%<br />
– Smooth gradual tapering; distinguish from<br />
adenocarcinoma (abrupt cutoff)<br />
• Color Doppler<br />
○ Portosplenic venous thrombosis: 5%<br />
○ Arterial pseudoaneurysm formation<br />
Radiographic Findings<br />
• Small, irregular calcifications (local or diffuse)<br />
• Gastric distention secondary to duodenal obstruction<br />
Fluoroscopic Findings<br />
• Upper GI<br />
○ Duodenum with thickened irregular mucosal folds<br />
○ Duodenal stricture <strong>and</strong> proximal dilatation<br />
○ Enlarged papilla of Vater (Poppel papillary sign)<br />
• ERCP<br />
○ Dilated & beaded MPD plus radicals (side branches)<br />
○ MPD filling defects: Intraductal calculi<br />
○ CBD may appear dilated with distal narrowing<br />
CT Findings<br />
• Gl<strong>and</strong>ular atrophy, parenchymal calcifications<br />
• Dilated MPD with intraductal calculi<br />
• Intra- <strong>and</strong> peripancreatic cysts<br />
• Heterogeneous enhancement<br />
• Hypodense focal mass (fibrosis <strong>and</strong> fat necrosis) with varied<br />
enhancement<br />
MR Findings<br />
• T1WI<br />
○ Decreased signal intensity due to loss of proteinaceous<br />
material<br />
• T2WI FS<br />
○ Pseudocyst, necrotic areas: Hyperintense<br />
○ Gallstones, intraductal calculi: Signal void within ducts<br />
• T1WI C+ FS<br />
○ Heterogeneous enhancement pattern due to<br />
inflammation <strong>and</strong> fibrosis<br />
○ Vascular thrombosis: Filling defect or occlusion<br />
• MRCP<br />
○ Dilated MPD, usually with smooth tapering<br />
○ Dilated side branch ducts in severe cases<br />
○ Ductal disruption: MPD in continuity with pseudocyst,<br />
bowel, or pleural space<br />
○ CBD may be dilated with smooth distal tapering<br />
Imaging Recommendations<br />
• Best imaging tool<br />
○ EUS for detecting early disease; MRCP, CECT for<br />
morphologic changes<br />
• Protocol advice<br />
○ MRCP best to evaluate dilated MPD <strong>and</strong> side branches<br />
○ MR with contrast helpful to distinguish tumor from<br />
enlargement related to inflammation<br />
○ CT best to evaluate extent of calcifications <strong>and</strong><br />
inflammation related to acute on chronic pancreatitis<br />
DIFFERENTIAL DIAGNOSIS<br />
Infiltrating Pancreatic Carcinoma<br />
• Irregular, heterogeneous, hypoechoic mass<br />
• Abrupt obstruction & dilatation of pancreatic duct<br />
• Regional nodal metastases: Splenic hilum & porta hepatis<br />
• Contiguous organ invasion: Duodenum, stomach, liver,<br />
mesentery<br />
Acute Pancreatitis<br />
• Diffuse/focal parenchymal enlargement<br />
• Hypoechoic echogenicity in inflamed parenchyma<br />
• Pancreatic ductal dilatation uncommon<br />
• Lack of pancreatic calcification<br />
• Peripancreatic edema <strong>and</strong> fluid collection<br />
Diagnoses: Pancreas<br />
363