Diagnostic Ultrasound - Abdomen and Pelvis
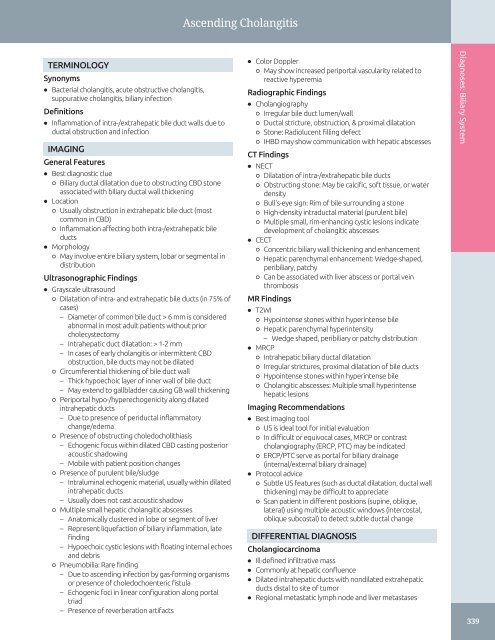
Ascending Cholangitis TERMINOLOGY Synonyms • Bacterial cholangitis, acute obstructive cholangitis, suppurative cholangitis, biliary infection Definitions • Inflammation of intra-/extrahepatic bile duct walls due to ductal obstruction and infection IMAGING General Features • Best diagnostic clue ○ Biliary ductal dilatation due to obstructing CBD stone associated with biliary ductal wall thickening • Location ○ Usually obstruction in extrahepatic bile duct (most common in CBD) ○ Inflammation affecting both intra-/extrahepatic bile ducts • Morphology ○ May involve entire biliary system, lobar or segmental in distribution Ultrasonographic Findings • Grayscale ultrasound ○ Dilatation of intra- and extrahepatic bile ducts (in 75% of cases) – Diameter of common bile duct > 6 mm is considered abnormal in most adult patients without prior cholecystectomy – Intrahepatic duct dilatation: > 1-2 mm – In cases of early cholangitis or intermittent CBD obstruction, bile ducts may not be dilated ○ Circumferential thickening of bile duct wall – Thick hypoechoic layer of inner wall of bile duct – May extend to gallbladder causing GB wall thickening ○ Periportal hypo-/hyperechogenicity along dilated intrahepatic ducts – Due to presence of periductal inflammatory change/edema ○ Presence of obstructing choledocholithiasis – Echogenic focus within dilated CBD casting posterior acoustic shadowing – Mobile with patient position changes ○ Presence of purulent bile/sludge – Intraluminal echogenic material, usually within dilated intrahepatic ducts – Usually does not cast acoustic shadow ○ Multiple small hepatic cholangitic abscesses – Anatomically clustered in lobe or segment of liver – Represent liquefaction of biliary inflammation, late finding – Hypoechoic cystic lesions with floating internal echoes and debris ○ Pneumobilia: Rare finding – Due to ascending infection by gas-forming organisms or presence of choledochoenteric fistula – Echogenic foci in linear configuration along portal triad – Presence of reverberation artifacts • Color Doppler ○ May show increased periportal vascularity related to reactive hyperemia Radiographic Findings • Cholangiography ○ Irregular bile duct lumen/wall ○ Ductal stricture, obstruction, & proximal dilatation ○ Stone: Radiolucent filling defect ○ IHBD may show communication with hepatic abscesses CT Findings • NECT ○ Dilatation of intra-/extrahepatic bile ducts ○ Obstructing stone: May be calcific, soft tissue, or water density ○ Bull's-eye sign: Rim of bile surrounding a stone ○ High-density intraductal material (purulent bile) ○ Multiple small, rim-enhancing cystic lesions indicate development of cholangitic abscesses • CECT ○ Concentric biliary wall thickening and enhancement ○ Hepatic parenchymal enhancement: Wedge-shaped, peribiliary, patchy ○ Can be associated with liver abscess or portal vein thrombosis MR Findings • T2WI ○ Hypointense stones within hyperintense bile ○ Hepatic parenchymal hyperintensity – Wedge shaped, peribiliary or patchy distribution • MRCP ○ Intrahepatic biliary ductal dilatation ○ Irregular strictures, proximal dilatation of bile ducts ○ Hypointense stones within hyperintense bile ○ Cholangitic abscesses: Multiple small hyperintense hepatic lesions Imaging Recommendations • Best imaging tool ○ US is ideal tool for initial evaluation ○ In difficult or equivocal cases, MRCP or contrast cholangiography (ERCP, PTC) may be indicated ○ ERCP/PTC serve as portal for biliary drainage (internal/external biliary drainage) • Protocol advice ○ Subtle US features (such as ductal dilatation, ductal wall thickening) may be difficult to appreciate ○ Scan patient in different positions (supine, oblique, lateral) using multiple acoustic windows (intercostal, oblique subcostal) to detect subtle ductal change DIFFERENTIAL DIAGNOSIS Cholangiocarcinoma • Ill-defined infiltrative mass • Commonly at hepatic confluence • Dilated intrahepatic ducts with nondilated extrahepatic ducts distal to site of tumor • Regional metastatic lymph node and liver metastases Diagnoses: Biliary System 339
Ascending Cholangitis Diagnoses: Biliary System Pancreatic Ductal Carcinoma • Infiltrative hypoechoic mass in pancreatic head • Dilatation of intra- and extrahepatic bile ducts and pancreatic ducts • Vascular encasement • Regional nodal and liver metastases Primary Sclerosing Cholangitis (PSC) • Segmental strictures, beaded and pruned ducts • Involves both intrahepatic & extrahepatic ducts • End-stage: Lobular liver, hypertrophy, and atrophy Recurrent Pyogenic Cholangitis (RPC) • Intra-/ and extrahepatic biliary pigmented stones • Lateral segment of left lobe and posterior segment of right lobe are more commonly involved • Presence of multifocal intrahepatic ductal strictures with segmental dilatation • Clinical information of ethnic origin and recurrent attacks of cholangitis help in suggesting etiology Other Forms of Secondary Cholangitis • AIDS-related cholangitis • Chemotherapy-induced cholangitis • Ischemic cholangitis PATHOLOGY General Features • Etiology ○ Pathogenesis: Stone/stricture → obstruction → bile stasis → increased biliary pressure → infection ○ Source of infection: Usually ascending from duodenum; rarely hematogenous ○ Risk factors – Choledocholithiasis and hepatolithiasis (most common) – Biliary stricture: In setting of PSC or malignancy – Biliary stents: Can act as nidus of infection – Choledochal surgery – Recent manipulation: ERCP, PTC – Sphincter of Oddi dysfunction or stenosis ○ Bacteriology – Escherichia coli, Klebsiella, Enterococcus species, Enterobacter species – Anaerobes in mixed infections • Associated abnormalities ○ Gallstone disease Staging, Grading, & Classification • Severity of disease ○ Mild: Responsive to antibiotics and supportive therapy ○ Moderate: Not responsive to medical therapy, but no organ dysfunction ○ Severe: Organ dysfunction Microscopic Features • Acute inflammatory infiltrates involving ductal mucosa/submucosa • Periductal aggregates of leukocytes with edema • Liquefied necrosis in cholangitic abscesses CLINICAL ISSUES Presentation • Most common signs/symptoms ○ Charcot triad: RUQ pain, fever, jaundice • Other signs/symptoms ○ Septicemia, septic shock ○ Lethargy, mental confusion – Especially in elderly patients • Lab data ○ Increased WBC count & bilirubin levels ○ Increased alkaline phosphatase and GGT ○ Transaminitis ○ Positive blood cultures in toxic phase Demographics • Age: More common in middle age or elderly • Epidemiology: Most common type of cholangitis in Western countries Natural History & Prognosis • Complications: Cholangitic liver abscesses & septicemia, portal vein thrombosis • Majority improve with antibiotic treatment • High mortality if not decompressed • Overall mortality significantly improved with antibiotic treatment and biliary decompression Treatment • Antibiotics to cover gram-negative organisms • Biliary decompression for uncontrolled sepsis and failed medical therapy ○ ERCP: Sphincterotomy + stone extraction, internal stent ○ PTC: External biliary drainage via percutaneous transhepatic biliary drainage (PTBD) ○ Surgical decompression: Fulminant cases and failed nonoperative decompression DIAGNOSTIC CHECKLIST Consider • Correlate with clinical & laboratory data to achieve accurate imaging interpretation ○ Due to overlap in US features of various cholangitis Image Interpretation Pearls • Biliary ductal dilatation and thickening related to obstructing choledocholithiasis in appropriate clinical setting SELECTED REFERENCES 1. Spârchez Z et al: Role of contrast enhanced ultrasound in the assessment of biliary duct disease. Med Ultrason. 16(1):41-7, 2014 2. Kiriyama S et al: TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 20(1):24-34, 2013 3. Patel NB et al: Multidetector CT of emergent biliary pathologic conditions. Radiographics. 33(7):1867-88, 2013 4. Eun HW et al: Assessment of acute cholangitis by MR imaging. Eur J Radiol. 81(10):2476-80, 2012 5. Kim SW et al: Diagnostic performance of multidetector CT for acute cholangitis: evaluation of a CT scoring method. Br J Radiol. 85(1014):770-7, 2012 340
- Page 310 and 311: Cholelithiasis (Left) Longitudinal
- Page 312 and 313: Cholelithiasis (Left) Abdominal rad
- Page 314 and 315: Echogenic Bile TERMINOLOGY Synonyms
- Page 316 and 317: Echogenic Bile (Left) Transverse ul
- Page 318 and 319: Gallbladder Cholesterol Polyp TERMI
- Page 320 and 321: Gallbladder Cholesterol Polyp (Left
- Page 322 and 323: Acute Calculous Cholecystitis TERMI
- Page 324 and 325: Acute Calculous Cholecystitis (Left
- Page 326 and 327: Acute Acalculous Cholecystitis TERM
- Page 328 and 329: Acute Acalculous Cholecystitis (Lef
- Page 330 and 331: Chronic Cholecystitis TERMINOLOGY D
- Page 332 and 333: Xanthogranulomatous Cholecystitis T
- Page 334 and 335: Porcelain Gallbladder TERMINOLOGY A
- Page 336 and 337: Hyperplastic Cholecystosis (Adenomy
- Page 338 and 339: Hyperplastic Cholecystosis (Adenomy
- Page 340 and 341: Gallbladder Carcinoma TERMINOLOGY A
- Page 342 and 343: Gallbladder Carcinoma (Left) Sagitt
- Page 344 and 345: Biliary Ductal Dilatation IMAGING G
- Page 346 and 347: Choledochal Cyst TERMINOLOGY Synony
- Page 348 and 349: Choledochal Cyst (Left) Longitudina
- Page 350 and 351: Choledocholithiasis TERMINOLOGY Abb
- Page 352 and 353: Choledocholithiasis (Left) A single
- Page 354 and 355: Biliary Ductal Gas TERMINOLOGY Syno
- Page 356 and 357: Cholangiocarcinoma TERMINOLOGY Syno
- Page 358 and 359: Cholangiocarcinoma (Left) Ultrasoun
- Page 362 and 363: Ascending Cholangitis (Left) Longit
- Page 364 and 365: Recurrent Pyogenic Cholangitis TERM
- Page 366 and 367: Recurrent Pyogenic Cholangitis (Lef
- Page 368 and 369: AIDS-Related Cholangiopathy TERMINO
- Page 370 and 371: PART II SECTION 3 Pancreas Introduc
- Page 372 and 373: Approach to Pancreatic Sonography C
- Page 374 and 375: Approach to Pancreatic Sonography (
- Page 376 and 377: Acute Pancreatitis TERMINOLOGY Abbr
- Page 378 and 379: Acute Pancreatitis (Left) Transvers
- Page 380 and 381: Pancreatic Pseudocyst TERMINOLOGY D
- Page 382 and 383: Pancreatic Pseudocyst (Left) Transv
- Page 384 and 385: Chronic Pancreatitis TERMINOLOGY Ab
- Page 386 and 387: Chronic Pancreatitis (Left) Transve
- Page 388 and 389: Mucinous Cystic Pancreatic Tumor TE
- Page 390 and 391: Mucinous Cystic Pancreatic Tumor (L
- Page 392 and 393: Serous Cystadenoma of Pancreas TERM
- Page 394 and 395: Serous Cystadenoma of Pancreas (Lef
- Page 396 and 397: Intraductal Papillary Mucinous Neop
- Page 398 and 399: Intraductal Papillary Mucinous Neop
- Page 400 and 401: Intraductal Papillary Mucinous Neop
- Page 402 and 403: Pancreatic Ductal Carcinoma TERMINO
- Page 404 and 405: Pancreatic Ductal Carcinoma (Left)
- Page 406 and 407: Pancreatic Neuroendocrine Tumor TER
- Page 408 and 409: Pancreatic Neuroendocrine Tumor (Le
Ascending Cholangitis<br />
TERMINOLOGY<br />
Synonyms<br />
• Bacterial cholangitis, acute obstructive cholangitis,<br />
suppurative cholangitis, biliary infection<br />
Definitions<br />
• Inflammation of intra-/extrahepatic bile duct walls due to<br />
ductal obstruction <strong>and</strong> infection<br />
IMAGING<br />
General Features<br />
• Best diagnostic clue<br />
○ Biliary ductal dilatation due to obstructing CBD stone<br />
associated with biliary ductal wall thickening<br />
• Location<br />
○ Usually obstruction in extrahepatic bile duct (most<br />
common in CBD)<br />
○ Inflammation affecting both intra-/extrahepatic bile<br />
ducts<br />
• Morphology<br />
○ May involve entire biliary system, lobar or segmental in<br />
distribution<br />
Ultrasonographic Findings<br />
• Grayscale ultrasound<br />
○ Dilatation of intra- <strong>and</strong> extrahepatic bile ducts (in 75% of<br />
cases)<br />
– Diameter of common bile duct > 6 mm is considered<br />
abnormal in most adult patients without prior<br />
cholecystectomy<br />
– Intrahepatic duct dilatation: > 1-2 mm<br />
– In cases of early cholangitis or intermittent CBD<br />
obstruction, bile ducts may not be dilated<br />
○ Circumferential thickening of bile duct wall<br />
– Thick hypoechoic layer of inner wall of bile duct<br />
– May extend to gallbladder causing GB wall thickening<br />
○ Periportal hypo-/hyperechogenicity along dilated<br />
intrahepatic ducts<br />
– Due to presence of periductal inflammatory<br />
change/edema<br />
○ Presence of obstructing choledocholithiasis<br />
– Echogenic focus within dilated CBD casting posterior<br />
acoustic shadowing<br />
– Mobile with patient position changes<br />
○ Presence of purulent bile/sludge<br />
– Intraluminal echogenic material, usually within dilated<br />
intrahepatic ducts<br />
– Usually does not cast acoustic shadow<br />
○ Multiple small hepatic cholangitic abscesses<br />
– Anatomically clustered in lobe or segment of liver<br />
– Represent liquefaction of biliary inflammation, late<br />
finding<br />
– Hypoechoic cystic lesions with floating internal echoes<br />
<strong>and</strong> debris<br />
○ Pneumobilia: Rare finding<br />
– Due to ascending infection by gas-forming organisms<br />
or presence of choledochoenteric fistula<br />
– Echogenic foci in linear configuration along portal<br />
triad<br />
– Presence of reverberation artifacts<br />
• Color Doppler<br />
○ May show increased periportal vascularity related to<br />
reactive hyperemia<br />
Radiographic Findings<br />
• Cholangiography<br />
○ Irregular bile duct lumen/wall<br />
○ Ductal stricture, obstruction, & proximal dilatation<br />
○ Stone: Radiolucent filling defect<br />
○ IHBD may show communication with hepatic abscesses<br />
CT Findings<br />
• NECT<br />
○ Dilatation of intra-/extrahepatic bile ducts<br />
○ Obstructing stone: May be calcific, soft tissue, or water<br />
density<br />
○ Bull's-eye sign: Rim of bile surrounding a stone<br />
○ High-density intraductal material (purulent bile)<br />
○ Multiple small, rim-enhancing cystic lesions indicate<br />
development of cholangitic abscesses<br />
• CECT<br />
○ Concentric biliary wall thickening <strong>and</strong> enhancement<br />
○ Hepatic parenchymal enhancement: Wedge-shaped,<br />
peribiliary, patchy<br />
○ Can be associated with liver abscess or portal vein<br />
thrombosis<br />
MR Findings<br />
• T2WI<br />
○ Hypointense stones within hyperintense bile<br />
○ Hepatic parenchymal hyperintensity<br />
– Wedge shaped, peribiliary or patchy distribution<br />
• MRCP<br />
○ Intrahepatic biliary ductal dilatation<br />
○ Irregular strictures, proximal dilatation of bile ducts<br />
○ Hypointense stones within hyperintense bile<br />
○ Cholangitic abscesses: Multiple small hyperintense<br />
hepatic lesions<br />
Imaging Recommendations<br />
• Best imaging tool<br />
○ US is ideal tool for initial evaluation<br />
○ In difficult or equivocal cases, MRCP or contrast<br />
cholangiography (ERCP, PTC) may be indicated<br />
○ ERCP/PTC serve as portal for biliary drainage<br />
(internal/external biliary drainage)<br />
• Protocol advice<br />
○ Subtle US features (such as ductal dilatation, ductal wall<br />
thickening) may be difficult to appreciate<br />
○ Scan patient in different positions (supine, oblique,<br />
lateral) using multiple acoustic windows (intercostal,<br />
oblique subcostal) to detect subtle ductal change<br />
DIFFERENTIAL DIAGNOSIS<br />
Cholangiocarcinoma<br />
• Ill-defined infiltrative mass<br />
• Commonly at hepatic confluence<br />
• Dilated intrahepatic ducts with nondilated extrahepatic<br />
ducts distal to site of tumor<br />
• Regional metastatic lymph node <strong>and</strong> liver metastases<br />
Diagnoses: Biliary System<br />
339