Diagnostic Ultrasound - Abdomen and Pelvis
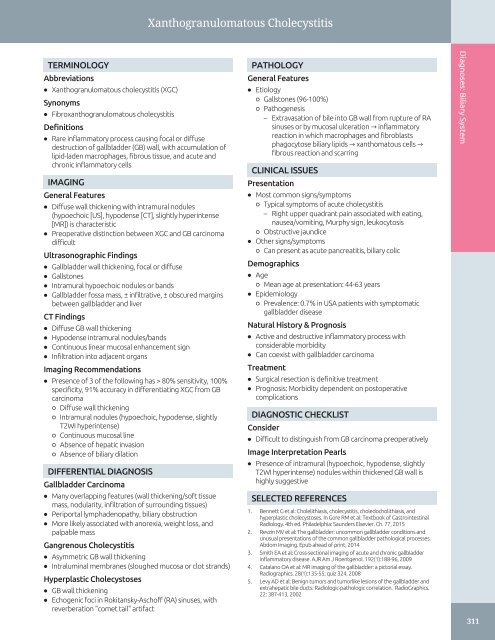
Xanthogranulomatous Cholecystitis TERMINOLOGY Abbreviations • Xanthogranulomatous cholecystitis (XGC) Synonyms • Fibroxanthogranulomatous cholecystitis Definitions • Rare inflammatory process causing focal or diffuse destruction of gallbladder (GB) wall, with accumulation of lipid-laden macrophages, fibrous tissue, and acute and chronic inflammatory cells IMAGING General Features • Diffuse wall thickening with intramural nodules (hypoechoic [US], hypodense [CT], slightly hyperintense [MR]) is characteristic • Preoperative distinction between XGC and GB carcinoma difficult Ultrasonographic Findings • Gallbladder wall thickening, focal or diffuse • Gallstones • Intramural hypoechoic nodules or bands • Gallbladder fossa mass, ± infiltrative, ± obscured margins between gallbladder and liver CT Findings • Diffuse GB wall thickening • Hypodense intramural nodules/bands • Continuous linear mucosal enhancement sign • Infiltration into adjacent organs Imaging Recommendations • Presence of 3 of the following has > 80% sensitivity, 100% specificity, 91% accuracy in differentiating XGC from GB carcinoma ○ Diffuse wall thickening ○ Intramural nodules (hypoechoic, hypodense, slightly T2WI hyperintense) ○ Continuous mucosal line ○ Absence of hepatic invasion ○ Absence of biliary dilation DIFFERENTIAL DIAGNOSIS Gallbladder Carcinoma • Many overlapping features (wall thickening/soft tissue mass, nodularity, infiltration of surrounding tissues) • Periportal lymphadenopathy, biliary obstruction • More likely associated with anorexia, weight loss, and palpable mass Gangrenous Cholecystitis • Asymmetric GB wall thickening • Intraluminal membranes (sloughed mucosa or clot strands) Hyperplastic Cholecystoses • GB wall thickening • Echogenic foci in Rokitansky-Aschoff (RA) sinuses, with reverberation "comet tail" artifact PATHOLOGY General Features • Etiology ○ Gallstones (96-100%) ○ Pathogenesis – Extravasation of bile into GB wall from rupture of RA sinuses or by mucosal ulceration → inflammatory reaction in which macrophages and fibroblasts phagocytose biliary lipids → xanthomatous cells → fibrous reaction and scarring CLINICAL ISSUES Presentation • Most common signs/symptoms ○ Typical symptoms of acute cholecystitis – Right upper quadrant pain associated with eating, nausea/vomiting, Murphy sign, leukocytosis ○ Obstructive jaundice • Other signs/symptoms ○ Can present as acute pancreatitis, biliary colic Demographics • Age ○ Mean age at presentation: 44-63 years • Epidemiology ○ Prevalence: 0.7% in USA patients with symptomatic gallbladder disease Natural History & Prognosis • Active and destructive inflammatory process with considerable morbidity • Can coexist with gallbladder carcinoma Treatment • Surgical resection is definitive treatment • Prognosis: Morbidity dependent on postoperative complications DIAGNOSTIC CHECKLIST Consider • Difficult to distinguish from GB carcinoma preoperatively Image Interpretation Pearls • Presence of intramural (hypoechoic, hypodense, slightly T2WI hyperintense) nodules within thickened GB wall is highly suggestive SELECTED REFERENCES 1. Bennett G et al: Cholelithiasis, cholecystitis, choledocholithiasis, and hyperplastic cholecystoses. In Gore RM et al: Textbook of Gastrointestinal Radiology. 4th ed. Philadelphia: Saunders Elsevier. Ch. 77, 2015 2. Revzin MV et al: The gallbladder: uncommon gallbladder conditions and unusual presentations of the common gallbladder pathological processes. Abdom Imaging. Epub ahead of print, 2014 3. Smith EA et al: Cross-sectional imaging of acute and chronic gallbladder inflammatory disease. AJR Am J Roentgenol. 192(1):188-96, 2009 4. Catalano OA et al: MR imaging of the gallbladder: a pictorial essay. Radiographics. 28(1):135-55; quiz 324, 2008 5. Levy AD et al: Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: Radiologic-pathologic correlation. RadioGraphics. 22: 387-413, 2002 Diagnoses: Biliary System 311
Porcelain Gallbladder Diagnoses: Biliary System TERMINOLOGY • Intramural calcification of gallbladder wall, uncommon manifestation of chronic cholecystitis IMAGING • Type of calcification determines the ultrasound appearance ○ Thick diffuse GB wall calcification (complete) ○ Segmental GB wall calcification (incomplete) • Set focus to maximize depiction of high-amplitude echoes and dense posterior acoustic shadowing • Look for soft tissue mass in gallbladder or fossa, indicating presence of GB carcinoma TOP DIFFERENTIAL DIAGNOSES • Gallstone-filled gallbladder or large gallstone ○ Wall-echo-shadow (WES) complex appearance ○ Mobile stones may be positional ○ Dense, clean posterior acoustic shadowing (should not see posterior wall) KEY FACTS • Emphysematous cholecystitis ○ Echogenic crescent in gallbladder ○ Irregular (dirty) posterior acoustic shadowing • Hyperplastic cholecystosis ○ Diffuse or focal GB wall thickening, echogenic foci with "comet tail" artifacts ○ No posterior acoustic shadowing PATHOLOGY • Associated with gallstones in 95% CLINICAL ISSUES • Risk of gallbladder cancer: 0-5% ○ Complete type: No risk, mucosa entirely denuded ○ Incomplete type: Mucosal metaplasia → dysplasia • Prophylactic cholecystectomy is appropriate for healthy patients • Nonoperative approach can be considered in patients with significant comorbidity (Left) Grayscale US shows a thin, hyperechoic semilunar line in the GB fossa with dense posterior acoustic shadowing ſt in a 67-year-old woman who presented with chronic intermittent biliary pain as an example of complete calcification. (Right) Curvilinear diffuse, thin calcifications are shown in the RUQ of the same patient, in the expected location and shape of the gallbladder. (Courtesy American Institute for Radiologic Pathology archives, Case ID #2133052.) (Left) Discontinuous hyperechoic foci in the anterior ſt and posterior GB wall, with variable shadowing , in a 67-yearold woman with RUQ pain after eating; an example of incomplete calcification. (Right) Punctate mural calcifications ſt in a 61-yearold obese man, an example of incomplete calcification. Gallstones found at pathology are not shown. (Courtesy American Institute for Radiologic Pathology archives, Case IDs #2674992, #642.) 312
- Page 282 and 283: Transjugular Intrahepatic Portosyst
- Page 284 and 285: Transjugular Intrahepatic Portosyst
- Page 286 and 287: Portal Vein Occlusion TERMINOLOGY A
- Page 288 and 289: Portal Vein Occlusion (Left) Color
- Page 290 and 291: Budd-Chiari Syndrome TERMINOLOGY Ab
- Page 292 and 293: Budd-Chiari Syndrome (Left) Color D
- Page 294 and 295: Portal Vein Gas TERMINOLOGY Abbrevi
- Page 296 and 297: Liver Transplant Portal Vein Stenos
- Page 298 and 299: Liver Transplant Biliary Stricture
- Page 300 and 301: PART II SECTION 2 Biliary System In
- Page 302 and 303: Approach to Biliary Sonography hosp
- Page 304 and 305: Approach to Biliary Sonography (Lef
- Page 306 and 307: Approach to Biliary Sonography (Lef
- Page 308 and 309: Cholelithiasis TERMINOLOGY Synonyms
- Page 310 and 311: Cholelithiasis (Left) Longitudinal
- Page 312 and 313: Cholelithiasis (Left) Abdominal rad
- Page 314 and 315: Echogenic Bile TERMINOLOGY Synonyms
- Page 316 and 317: Echogenic Bile (Left) Transverse ul
- Page 318 and 319: Gallbladder Cholesterol Polyp TERMI
- Page 320 and 321: Gallbladder Cholesterol Polyp (Left
- Page 322 and 323: Acute Calculous Cholecystitis TERMI
- Page 324 and 325: Acute Calculous Cholecystitis (Left
- Page 326 and 327: Acute Acalculous Cholecystitis TERM
- Page 328 and 329: Acute Acalculous Cholecystitis (Lef
- Page 330 and 331: Chronic Cholecystitis TERMINOLOGY D
- Page 334 and 335: Porcelain Gallbladder TERMINOLOGY A
- Page 336 and 337: Hyperplastic Cholecystosis (Adenomy
- Page 338 and 339: Hyperplastic Cholecystosis (Adenomy
- Page 340 and 341: Gallbladder Carcinoma TERMINOLOGY A
- Page 342 and 343: Gallbladder Carcinoma (Left) Sagitt
- Page 344 and 345: Biliary Ductal Dilatation IMAGING G
- Page 346 and 347: Choledochal Cyst TERMINOLOGY Synony
- Page 348 and 349: Choledochal Cyst (Left) Longitudina
- Page 350 and 351: Choledocholithiasis TERMINOLOGY Abb
- Page 352 and 353: Choledocholithiasis (Left) A single
- Page 354 and 355: Biliary Ductal Gas TERMINOLOGY Syno
- Page 356 and 357: Cholangiocarcinoma TERMINOLOGY Syno
- Page 358 and 359: Cholangiocarcinoma (Left) Ultrasoun
- Page 360 and 361: Ascending Cholangitis TERMINOLOGY S
- Page 362 and 363: Ascending Cholangitis (Left) Longit
- Page 364 and 365: Recurrent Pyogenic Cholangitis TERM
- Page 366 and 367: Recurrent Pyogenic Cholangitis (Lef
- Page 368 and 369: AIDS-Related Cholangiopathy TERMINO
- Page 370 and 371: PART II SECTION 3 Pancreas Introduc
- Page 372 and 373: Approach to Pancreatic Sonography C
- Page 374 and 375: Approach to Pancreatic Sonography (
- Page 376 and 377: Acute Pancreatitis TERMINOLOGY Abbr
- Page 378 and 379: Acute Pancreatitis (Left) Transvers
- Page 380 and 381: Pancreatic Pseudocyst TERMINOLOGY D
Xanthogranulomatous Cholecystitis<br />
TERMINOLOGY<br />
Abbreviations<br />
• Xanthogranulomatous cholecystitis (XGC)<br />
Synonyms<br />
• Fibroxanthogranulomatous cholecystitis<br />
Definitions<br />
• Rare inflammatory process causing focal or diffuse<br />
destruction of gallbladder (GB) wall, with accumulation of<br />
lipid-laden macrophages, fibrous tissue, <strong>and</strong> acute <strong>and</strong><br />
chronic inflammatory cells<br />
IMAGING<br />
General Features<br />
• Diffuse wall thickening with intramural nodules<br />
(hypoechoic [US], hypodense [CT], slightly hyperintense<br />
[MR]) is characteristic<br />
• Preoperative distinction between XGC <strong>and</strong> GB carcinoma<br />
difficult<br />
Ultrasonographic Findings<br />
• Gallbladder wall thickening, focal or diffuse<br />
• Gallstones<br />
• Intramural hypoechoic nodules or b<strong>and</strong>s<br />
• Gallbladder fossa mass, ± infiltrative, ± obscured margins<br />
between gallbladder <strong>and</strong> liver<br />
CT Findings<br />
• Diffuse GB wall thickening<br />
• Hypodense intramural nodules/b<strong>and</strong>s<br />
• Continuous linear mucosal enhancement sign<br />
• Infiltration into adjacent organs<br />
Imaging Recommendations<br />
• Presence of 3 of the following has > 80% sensitivity, 100%<br />
specificity, 91% accuracy in differentiating XGC from GB<br />
carcinoma<br />
○ Diffuse wall thickening<br />
○ Intramural nodules (hypoechoic, hypodense, slightly<br />
T2WI hyperintense)<br />
○ Continuous mucosal line<br />
○ Absence of hepatic invasion<br />
○ Absence of biliary dilation<br />
DIFFERENTIAL DIAGNOSIS<br />
Gallbladder Carcinoma<br />
• Many overlapping features (wall thickening/soft tissue<br />
mass, nodularity, infiltration of surrounding tissues)<br />
• Periportal lymphadenopathy, biliary obstruction<br />
• More likely associated with anorexia, weight loss, <strong>and</strong><br />
palpable mass<br />
Gangrenous Cholecystitis<br />
• Asymmetric GB wall thickening<br />
• Intraluminal membranes (sloughed mucosa or clot str<strong>and</strong>s)<br />
Hyperplastic Cholecystoses<br />
• GB wall thickening<br />
• Echogenic foci in Rokitansky-Aschoff (RA) sinuses, with<br />
reverberation "comet tail" artifact<br />
PATHOLOGY<br />
General Features<br />
• Etiology<br />
○ Gallstones (96-100%)<br />
○ Pathogenesis<br />
– Extravasation of bile into GB wall from rupture of RA<br />
sinuses or by mucosal ulceration → inflammatory<br />
reaction in which macrophages <strong>and</strong> fibroblasts<br />
phagocytose biliary lipids → xanthomatous cells →<br />
fibrous reaction <strong>and</strong> scarring<br />
CLINICAL ISSUES<br />
Presentation<br />
• Most common signs/symptoms<br />
○ Typical symptoms of acute cholecystitis<br />
– Right upper quadrant pain associated with eating,<br />
nausea/vomiting, Murphy sign, leukocytosis<br />
○ Obstructive jaundice<br />
• Other signs/symptoms<br />
○ Can present as acute pancreatitis, biliary colic<br />
Demographics<br />
• Age<br />
○ Mean age at presentation: 44-63 years<br />
• Epidemiology<br />
○ Prevalence: 0.7% in USA patients with symptomatic<br />
gallbladder disease<br />
Natural History & Prognosis<br />
• Active <strong>and</strong> destructive inflammatory process with<br />
considerable morbidity<br />
• Can coexist with gallbladder carcinoma<br />
Treatment<br />
• Surgical resection is definitive treatment<br />
• Prognosis: Morbidity dependent on postoperative<br />
complications<br />
DIAGNOSTIC CHECKLIST<br />
Consider<br />
• Difficult to distinguish from GB carcinoma preoperatively<br />
Image Interpretation Pearls<br />
• Presence of intramural (hypoechoic, hypodense, slightly<br />
T2WI hyperintense) nodules within thickened GB wall is<br />
highly suggestive<br />
SELECTED REFERENCES<br />
1. Bennett G et al: Cholelithiasis, cholecystitis, choledocholithiasis, <strong>and</strong><br />
hyperplastic cholecystoses. In Gore RM et al: Textbook of Gastrointestinal<br />
Radiology. 4th ed. Philadelphia: Saunders Elsevier. Ch. 77, 2015<br />
2. Revzin MV et al: The gallbladder: uncommon gallbladder conditions <strong>and</strong><br />
unusual presentations of the common gallbladder pathological processes.<br />
Abdom Imaging. Epub ahead of print, 2014<br />
3. Smith EA et al: Cross-sectional imaging of acute <strong>and</strong> chronic gallbladder<br />
inflammatory disease. AJR Am J Roentgenol. 192(1):188-96, 2009<br />
4. Catalano OA et al: MR imaging of the gallbladder: a pictorial essay.<br />
Radiographics. 28(1):135-55; quiz 324, 2008<br />
5. Levy AD et al: Benign tumors <strong>and</strong> tumorlike lesions of the gallbladder <strong>and</strong><br />
extrahepatic bile ducts: Radiologic-pathologic correlation. RadioGraphics.<br />
22: 387-413, 2002<br />
Diagnoses: Biliary System<br />
311