Diagnostic Ultrasound - Abdomen and Pelvis
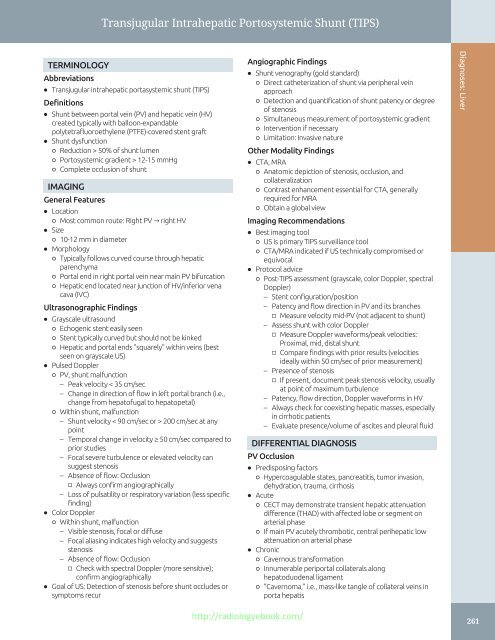
Transjugular Intrahepatic Portosystemic Shunt (TIPS) TERMINOLOGY Abbreviations • Transjugular intrahepatic portasystemic shunt (TIPS) Definitions • Shunt between portal vein (PV) and hepatic vein (HV) created typically with balloon-expandable polytetrafluoroethylene (PTFE)-covered stent graft • Shunt dysfunction ○ Reduction > 50% of shunt lumen ○ Portosystemic gradient > 12-15 mmHg ○ Complete occlusion of shunt IMAGING General Features • Location ○ Most common route: Right PV → right HV • Size ○ 10-12 mm in diameter • Morphology ○ Typically follows curved course through hepatic parenchyma ○ Portal end in right portal vein near main PV bifurcation ○ Hepatic end located near junction of HV/inferior vena cava (IVC) Ultrasonographic Findings • Grayscale ultrasound ○ Echogenic stent easily seen ○ Stent typically curved but should not be kinked ○ Hepatic and portal ends "squarely" within veins (best seen on grayscale US) • Pulsed Doppler ○ PV, shunt malfunction – Peak velocity < 35 cm/sec – Change in direction of flow in left portal branch (i.e., change from hepatofugal to hepatopetal) ○ Within shunt, malfunction – Shunt velocity < 90 cm/sec or > 200 cm/sec at any point – Temporal change in velocity ≥ 50 cm/sec compared to prior studies – Focal severe turbulence or elevated velocity can suggest stenosis – Absence of flow: Occlusion □ Always confirm angiographically – Loss of pulsatility or respiratory variation (less specific finding) • Color Doppler ○ Within shunt, malfunction – Visible stenosis, focal or diffuse – Focal aliasing indicates high velocity and suggests stenosis – Absence of flow: Occlusion □ Check with spectral Doppler (more sensitive); confirm angiographically • Goal of US: Detection of stenosis before shunt occludes or symptoms recur Angiographic Findings • Shunt venography (gold standard) ○ Direct catheterization of shunt via peripheral vein approach ○ Detection and quantification of shunt patency or degree of stenosis ○ Simultaneous measurement of portosystemic gradient ○ Intervention if necessary ○ Limitation: Invasive nature Other Modality Findings • CTA, MRA ○ Anatomic depiction of stenosis, occlusion, and collateralization ○ Contrast enhancement essential for CTA, generally required for MRA ○ Obtain a global view Imaging Recommendations • Best imaging tool ○ US is primary TIPS surveillance tool ○ CTA/MRA indicated if US technically compromised or equivocal • Protocol advice ○ Post-TIPS assessment (grayscale, color Doppler, spectral Doppler) – Stent configuration/position – Patency and flow direction in PV and its branches □ Measure velocity mid-PV (not adjacent to shunt) – Assess shunt with color Doppler □ Measure Doppler waveforms/peak velocities: Proximal, mid, distal shunt □ Compare findings with prior results (velocities ideally within 50 cm/sec of prior measurement) – Presence of stenosis □ If present, document peak stenosis velocity, usually at point of maximum turbulence – Patency, flow direction, Doppler waveforms in HV – Always check for coexisting hepatic masses, especially in cirrhotic patients – Evaluate presence/volume of ascites and pleural fluid DIFFERENTIAL DIAGNOSIS PV Occlusion • Predisposing factors ○ Hypercoagulable states, pancreatitis, tumor invasion, dehydration, trauma, cirrhosis • Acute ○ CECT may demonstrate transient hepatic attenuation difference (THAD) with affected lobe or segment on arterial phase ○ If main PV acutely thrombotic, central perihepatic low attenuation on arterial phase • Chronic ○ Cavernous transformation ○ Innumerable periportal collaterals along hepatoduodenal ligament ○ "Cavernoma," i.e., mass-like tangle of collateral veins in porta hepatis Diagnoses: Liver http://radiologyebook.com/ 261
Transjugular Intrahepatic Portosystemic Shunt (TIPS) 262 Diagnoses: Liver HV Occlusion • Predisposing factors ○ Hypercoagulable states, Budd-Chiari syndrome, myeloproliferative states, birth control pills, tumor invasion (especially hepatocellular carcinoma) • CECT ○ Arterial phase: Normal enhancing caudate lobe, mottled and reticular enhancement in liver periphery – Due to congestion and centrilobular necrosis ○ Venous phase: "Flip-flop" with lower attenuation of caudate lobe and increased density in liver periphery ○ Visualization of thrombi in HV and peridiaphragmatic collateral veins IVC Occlusion • Etiologies ○ Tumor infiltration, hepatocellular carcinoma most common; rarely metastases ○ Congenital web or band ○ Angiosarcoma of IVC PATHOLOGY General Features • Etiology ○ Stenosis usually secondary to intimal fibroplasia within HV – Biliary leak or contamination of shunt may induce intimal hyperplasia • Associated abnormalities ○ Hepatic encephalopathy as portal venous flow bypasses liver Microscopic Features • Intimal hyperplasia within areas of TIPS stenosis CLINICAL ISSUES Presentation • Most common signs/symptoms ○ TIPS malfunction – Signs of worsening portal hypertension with increasing ascites – Variceal hemorrhage Demographics • Epidemiology ○ Maintaining TIPS shunt patency is major problem – Primary patency (no intervention): 1 year = 38-84% – Secondary (assisted) patency: 1 year = 96-100% Natural History & Prognosis • Causes of TIPS failure ○ Technical problems: Malposition, kinks, incomplete deployment, hepatic perforation with hemoperitoneum, or bile leak ○ Venous trauma during stent insertion: Usually HV progresses to fibrosis/stenosis, may result in acute occlusion of PV ○ Neointimal hyperplasia (ameliorated by covered stents) ○ Thrombosis: Coagulopathy, intercurrent illness due to above problems ○ Hepatic arterial injury and arteriovenous fistula http://radiologyebook.com/ ○ Gallbladder injury • Guarded prognosis ○ Maintaining shunt patency ○ Inevitable liver disease progression ○ High risk of cirrhosis-related hepatocellular carcinoma ○ 7-45% 30-day mortality Indications for TIPS • Variceal bleeding refractory to sclerosis/banding • Refractory ascites • Hepatic hydrothorax • Budd-Chiari syndrome • Bridge to liver transplantation Relative Contraindications for TIPS • Hepatobiliary or pancreatic malignancy • Portal venous system thrombosis • Polycystic liver disease • Biliary obstruction • Infectious cholangitis DIAGNOSTIC CHECKLIST Consider • TIPS malfunction on Doppler US ○ If shunt velocity < 90 cm/sec or > 200 cm/sec or PV velocity < 35 cm/sec • Low flow difficult to detect with US ○ Confirm occlusion angiographically (CTA, MRA, shunt venography) SELECTED REFERENCES 1. Engstrom BI et al: Covered transjugular intrahepatic portosystemic shunts: accuracy of ultrasound in detecting shunt malfunction. AJR Am J Roentgenol. 200(4):904-8, 2013 2. Sajja KC et al: Long-term follow-up of TIPS created with expanded polytetrafluoroethylene covered stents. Dig Dis Sci. 58(7):2100-6, 2013 3. Wu Q et al: Transjugular intrahepatic portosystemic shunt using the FLUENCY expanded polytetrafluoroethylene-covered stent. Exp Ther Med. 5(1):263-266, 2013 4. Gazzera C et al: Fifteen years' experience with transjugular intrahepatic portosystemic shunt (TIPS) using bare stents: retrospective review of clinical and technical aspects. Radiol Med. 114(1):83-94, 2009 5. Kim MJ et al: Technical essentials of hepatic Doppler sonography. Curr Probl Diagn Radiol. 38(2):53-60, 2009 6. Bauer J et al: The role of TIPS for portal vein patency in liver transplant patients with portal vein thrombosis. Liver Transpl. 12(10):1544-51, 2006 7. Harrod-Kim P et al: Predictors of early mortality after transjugular intrahepatic portosystemic shunt creation for the treatment of refractory ascites. J Vasc Interv Radiol. 17(10):1605-10, 2006 8. Benito A et al: Doppler ultrasound for TIPS: does it work? Abdom Imaging. 29(1):45-52, 2004 9. Middleton WD et al: Doppler evaluation of transjugular intrahepatic portosystemic shunts. Ultrasound Q. 19(2):56-70; quiz 108 - 10, 2003 10. Bodner G et al: Color and pulsed Doppler ultrasound findings in normally functioning transjugular intrahepatic portosystemic shunts. Eur J Ultrasound. 12(2):131-6, 2000 11. Zizka J et al: Value of Doppler sonography in revealing transjugular intrahepatic portosystemic shunt malfunction: a 5-year experience in 216 patients. AJR Am J Roentgenol. 175(1):141-8, 2000
- Page 232 and 233: Biliary Cystadenoma/Carcinoma TERMI
- Page 234 and 235: Biliary Cystadenoma/Carcinoma (Left
- Page 236 and 237: Pyogenic Hepatic Abscess TERMINOLOG
- Page 238 and 239: Pyogenic Hepatic Abscess (Left) Obl
- Page 240 and 241: Amebic Hepatic Abscess TERMINOLOGY
- Page 242 and 243: Amebic Hepatic Abscess (Left) Longi
- Page 244 and 245: Hepatic Echinococcus Cyst TERMINOLO
- Page 246 and 247: Hepatic Echinococcus Cyst (Left) Ob
- Page 248 and 249: Hepatic Diffuse Microabscesses TERM
- Page 250 and 251: Peribiliary Cyst TERMINOLOGY Synony
- Page 252 and 253: Ciliated Hepatic Foregut Cyst TERMI
- Page 254 and 255: Hepatic Cavernous Hemangioma TERMIN
- Page 256 and 257: Hepatic Cavernous Hemangioma (Left)
- Page 258 and 259: Hepatic Cavernous Hemangioma (Left)
- Page 260 and 261: Focal Nodular Hyperplasia TERMINOLO
- Page 262 and 263: Focal Nodular Hyperplasia (Left) Tr
- Page 264 and 265: Hepatic Adenoma TERMINOLOGY Synonym
- Page 266 and 267: Hepatic Adenoma (Left) Transverse t
- Page 268 and 269: Hepatocellular Carcinoma TERMINOLOG
- Page 270 and 271: Hepatocellular Carcinoma (Left) Tra
- Page 272 and 273: Hepatocellular Carcinoma (Left) Tra
- Page 274 and 275: Hepatic Metastases TERMINOLOGY Defi
- Page 276 and 277: Hepatic Metastases (Left) Transvers
- Page 278 and 279: Hepatic Lymphoma TERMINOLOGY Defini
- Page 280 and 281: Hepatic Lymphoma (Left) Transverse
- Page 284 and 285: Transjugular Intrahepatic Portosyst
- Page 286 and 287: Portal Vein Occlusion TERMINOLOGY A
- Page 288 and 289: Portal Vein Occlusion (Left) Color
- Page 290 and 291: Budd-Chiari Syndrome TERMINOLOGY Ab
- Page 292 and 293: Budd-Chiari Syndrome (Left) Color D
- Page 294 and 295: Portal Vein Gas TERMINOLOGY Abbrevi
- Page 296 and 297: Liver Transplant Portal Vein Stenos
- Page 298 and 299: Liver Transplant Biliary Stricture
- Page 300 and 301: PART II SECTION 2 Biliary System In
- Page 302 and 303: Approach to Biliary Sonography hosp
- Page 304 and 305: Approach to Biliary Sonography (Lef
- Page 306 and 307: Approach to Biliary Sonography (Lef
- Page 308 and 309: Cholelithiasis TERMINOLOGY Synonyms
- Page 310 and 311: Cholelithiasis (Left) Longitudinal
- Page 312 and 313: Cholelithiasis (Left) Abdominal rad
- Page 314 and 315: Echogenic Bile TERMINOLOGY Synonyms
- Page 316 and 317: Echogenic Bile (Left) Transverse ul
- Page 318 and 319: Gallbladder Cholesterol Polyp TERMI
- Page 320 and 321: Gallbladder Cholesterol Polyp (Left
- Page 322 and 323: Acute Calculous Cholecystitis TERMI
- Page 324 and 325: Acute Calculous Cholecystitis (Left
- Page 326 and 327: Acute Acalculous Cholecystitis TERM
- Page 328 and 329: Acute Acalculous Cholecystitis (Lef
- Page 330 and 331: Chronic Cholecystitis TERMINOLOGY D
Transjugular Intrahepatic Portosystemic Shunt (TIPS)<br />
TERMINOLOGY<br />
Abbreviations<br />
• Transjugular intrahepatic portasystemic shunt (TIPS)<br />
Definitions<br />
• Shunt between portal vein (PV) <strong>and</strong> hepatic vein (HV)<br />
created typically with balloon-exp<strong>and</strong>able<br />
polytetrafluoroethylene (PTFE)-covered stent graft<br />
• Shunt dysfunction<br />
○ Reduction > 50% of shunt lumen<br />
○ Portosystemic gradient > 12-15 mmHg<br />
○ Complete occlusion of shunt<br />
IMAGING<br />
General Features<br />
• Location<br />
○ Most common route: Right PV → right HV <br />
• Size<br />
○ 10-12 mm in diameter<br />
• Morphology<br />
○ Typically follows curved course through hepatic<br />
parenchyma<br />
○ Portal end in right portal vein near main PV bifurcation<br />
○ Hepatic end located near junction of HV/inferior vena<br />
cava (IVC)<br />
Ultrasonographic Findings<br />
• Grayscale ultrasound<br />
○ Echogenic stent easily seen<br />
○ Stent typically curved but should not be kinked<br />
○ Hepatic <strong>and</strong> portal ends "squarely" within veins (best<br />
seen on grayscale US)<br />
• Pulsed Doppler<br />
○ PV, shunt malfunction<br />
– Peak velocity < 35 cm/sec<br />
– Change in direction of flow in left portal branch (i.e.,<br />
change from hepatofugal to hepatopetal)<br />
○ Within shunt, malfunction<br />
– Shunt velocity < 90 cm/sec or > 200 cm/sec at any<br />
point<br />
– Temporal change in velocity ≥ 50 cm/sec compared to<br />
prior studies<br />
– Focal severe turbulence or elevated velocity can<br />
suggest stenosis<br />
– Absence of flow: Occlusion<br />
□ Always confirm angiographically<br />
– Loss of pulsatility or respiratory variation (less specific<br />
finding)<br />
• Color Doppler<br />
○ Within shunt, malfunction<br />
– Visible stenosis, focal or diffuse<br />
– Focal aliasing indicates high velocity <strong>and</strong> suggests<br />
stenosis<br />
– Absence of flow: Occlusion<br />
□ Check with spectral Doppler (more sensitive);<br />
confirm angiographically<br />
• Goal of US: Detection of stenosis before shunt occludes or<br />
symptoms recur<br />
Angiographic Findings<br />
• Shunt venography (gold st<strong>and</strong>ard)<br />
○ Direct catheterization of shunt via peripheral vein<br />
approach<br />
○ Detection <strong>and</strong> quantification of shunt patency or degree<br />
of stenosis<br />
○ Simultaneous measurement of portosystemic gradient<br />
○ Intervention if necessary<br />
○ Limitation: Invasive nature<br />
Other Modality Findings<br />
• CTA, MRA<br />
○ Anatomic depiction of stenosis, occlusion, <strong>and</strong><br />
collateralization<br />
○ Contrast enhancement essential for CTA, generally<br />
required for MRA<br />
○ Obtain a global view<br />
Imaging Recommendations<br />
• Best imaging tool<br />
○ US is primary TIPS surveillance tool<br />
○ CTA/MRA indicated if US technically compromised or<br />
equivocal<br />
• Protocol advice<br />
○ Post-TIPS assessment (grayscale, color Doppler, spectral<br />
Doppler)<br />
– Stent configuration/position<br />
– Patency <strong>and</strong> flow direction in PV <strong>and</strong> its branches<br />
□ Measure velocity mid-PV (not adjacent to shunt)<br />
– Assess shunt with color Doppler<br />
□ Measure Doppler waveforms/peak velocities:<br />
Proximal, mid, distal shunt<br />
□ Compare findings with prior results (velocities<br />
ideally within 50 cm/sec of prior measurement)<br />
– Presence of stenosis<br />
□ If present, document peak stenosis velocity, usually<br />
at point of maximum turbulence<br />
– Patency, flow direction, Doppler waveforms in HV<br />
– Always check for coexisting hepatic masses, especially<br />
in cirrhotic patients<br />
– Evaluate presence/volume of ascites <strong>and</strong> pleural fluid<br />
DIFFERENTIAL DIAGNOSIS<br />
PV Occlusion<br />
• Predisposing factors<br />
○ Hypercoagulable states, pancreatitis, tumor invasion,<br />
dehydration, trauma, cirrhosis<br />
• Acute<br />
○ CECT may demonstrate transient hepatic attenuation<br />
difference (THAD) with affected lobe or segment on<br />
arterial phase<br />
○ If main PV acutely thrombotic, central perihepatic low<br />
attenuation on arterial phase<br />
• Chronic<br />
○ Cavernous transformation<br />
○ Innumerable periportal collaterals along<br />
hepatoduodenal ligament<br />
○ "Cavernoma," i.e., mass-like tangle of collateral veins in<br />
porta hepatis<br />
Diagnoses: Liver<br />
http://radiologyebook.com/<br />
261