Diagnostic Ultrasound - Abdomen and Pelvis
Hepatocellular Carcinoma TERMINOLOGY Abbreviations • Hepatocellular carcinoma (HCC) Definitions • Malignant neoplasm originating from hepatocytes IMAGING General Features • Best diagnostic clue ○ Solid, intrahepatic mass > 1 cmin patient with risk factors such as chronic hepatitis or cirrhosis ○ Portal vein or hepatic vein tumor invasion highly suggestive of HCC • Size ○ Small or large: < 3 cm to> 5 cm ○ Diffuse or infiltrative: Subcentimeter to > 5 cm • Key concepts ○ Most frequent primary visceral malignancy globally – Accounts for 80-90% of all adult primary liver malignancies – Usually arises in cirrhotic liver, due to chronic viral hepatitis (HBV, HCV) or alcoholism ○ 2nd most common malignant liver tumor after hepatoblastoma in children ○ Growth patterns of HCC: 3 major types – Solitary, often large mass – Multinodular or multifocal – Diffuse or infiltrative ○ Metastases to lung, bone, adrenal, lymph node Ultrasonographic Findings • Grayscale ultrasound ○ Hypoechoic: Most common sonographic appearance – Solid tumor – May be surrounded by thin, hypoechoic halo (capsule) ○ Hyperechoic – Indicates fatty metamorphosis/hypervascularity – Simulates hemangioma/focal steatosis □ If risk factors are present and hyperechoic lesion > 1 cm detected, cannot assume hemangioma ○ Mixed echogenicity: More common in larger HCC – Indicates tumor necrosis/fibrosis – Focal fat in some HCCs appear echogenic ○ Background cirrhosis (except for fibrolamellar HCC and hepatitis B) ○ Calcification is rare unless treated ○ Invasion of portal vein & less commonly hepatic vein highly suggestive of HCC ○ Hemoperitoneum if subcapsular or exophytic HCC ruptures ○ Associated signs of portal hypertension: Ascites, splenomegaly, portosystemic collaterals ○ Fibrolamellar carcinoma – Rare, < 1% of all cases of primary liver cancer – Well-defined partially/completely encapsulated mass – Prominent central fibrous scar often with calcification – Intralesional necrosis/hemorrhage – Regional adenopathy and metastases to lung and peritoneum – Typically without chronic liver disease – AFP usually negative or mildly elevated • Pulsed Doppler ○ Arterial feeding vessels with low-resistance waveforms indicate tumor vessels ○ Tumor thrombus with arterial neovascularity • Color Doppler ○ Irregular hypervascularity within neoplasm ○ Tumor thrombus, typically in portal vein, with neovascularity CT Findings • NECT ○ Iso- or hypodense liver mass, occasionally fat content detected – Characterization of lesion not possible on NECT • CECT ○ Characterization and diagnosis of HCC can be made with triphasic CT: Late arterial, portal venous, delayed/equilibrium phase – Late arterial phase: Hyperenhancing compared to background liver – Portal venous phase: Variable enhancement, may be iso-, hypo-, or hyperdense compared to background liver – Delayed or equilibrium phase (3-5 min after contrast injection): "Washout" is characteristic of HCC; lesion hypodense compared to liver □ May see delayed enhancing pseudocapsule MR Findings • T1WI ○ Typically hypointense compared to background liver but may be iso- or hyperintense depending on fat content or necrosis • T2WI ○ Typically slightly hyperintense, similar intensity to spleen • T1WI C+ ○ Late arterial phase: Hyperenhancing compared to background liver ○ Portal venous phase: Variable but typically hypointense ○ Delayed or equilibrium phase: "Washout" is characteristic of HCC with lesion hypointense to background liver – Hyperintense pseudocapsule typically best seen on delayed or portal venous phase images ○ Hepatobiliary contrast (gadoxetate, Eovist, Primovist): Uptake in hepatocytes related to OATP8 receptor, downregulated in most HCC, up-regulated in focal nodular hyperplasia (FNH) – Pitfall: Up to 10% of HCC can be isointense or hyperintense on hepatobiliary phase Angiographic Findings • Hypervascular tumor ○ Marked neovascularity and AV shunting ○ Large hepatic artery and vascular invasion ○ "Threads and streaks" sign in portal vein tumor thrombus Nuclear Medicine Findings • Hepatobiliary scan: Uptake in 50% http://radiologyebook.com/ Diagnoses: Liver 247
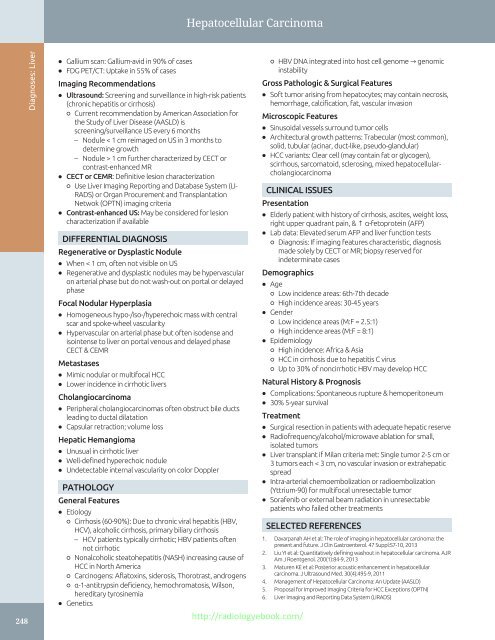
Hepatocellular Carcinoma 248 Diagnoses: Liver • Gallium scan: Gallium-avid in 90% of cases • FDG PET/CT: Uptake in 55% of cases Imaging Recommendations • Ultrasound: Screening and surveillance in high-risk patients (chronic hepatitis or cirrhosis) ○ Current recommendation by American Association for the Study of Liver Disease (AASLD) is screening/surveillance US every 6 months – Nodule < 1 cm reimaged on US in 3 months to determine growth – Nodule > 1 cm further characterized by CECT or contrast-enhanced MR • CECT or CEMR: Definitive lesion characterization ○ Use Liver Imaging Reporting and Database System (LI- RADS) or Organ Procurement and Transplantation Netwok (OPTN) imaging criteria • Contrast-enhanced US: May be considered for lesion characterization if available DIFFERENTIAL DIAGNOSIS Regenerative or Dysplastic Nodule • When < 1 cm, often not visible on US • Regenerative and dysplastic nodules may be hypervascular on arterial phase but do not wash-out on portal or delayed phase Focal Nodular Hyperplasia • Homogeneous hypo-/iso-/hyperechoic mass with central scar and spoke-wheel vascularity • Hypervascular on arterial phase but often isodense and isointense to liver on portal venous and delayed phase CECT & CEMR Metastases • Mimic nodular or multifocal HCC • Lower incidence in cirrhotic livers Cholangiocarcinoma • Peripheral cholangiocarcinomas often obstruct bile ducts leading to ductal dilatation • Capsular retraction; volume loss Hepatic Hemangioma • Unusual in cirrhotic liver • Well-defined hyperechoic nodule • Undetectable internal vascularity on color Doppler ○ HBV DNA integrated into host cell genome → genomic instability Gross Pathologic & Surgical Features • Soft tumor arising from hepatocytes; may contain necrosis, hemorrhage, calcification, fat, vascular invasion Microscopic Features • Sinusoidal vessels surround tumor cells • Architectural growth patterns: Trabecular (most common), solid, tubular (acinar, duct-like, pseudo-glandular) • HCC variants: Clear cell (may contain fat or glycogen), scirrhous, sarcomatoid, sclerosing, mixed hepatocellularcholangiocarcinoma CLINICAL ISSUES Presentation • Elderly patient with history of cirrhosis, ascites, weight loss, right upper quadrant pain, & ↑ α-fetoprotein (AFP) • Lab data: Elevated serum AFP and liver function tests ○ Diagnosis: If imaging features characteristic, diagnosis made solely by CECT or MR; biopsy reserved for indeterminate cases Demographics • Age ○ Low incidence areas: 6th-7th decade ○ High incidence areas: 30-45 years • Gender ○ Low incidence areas (M:F = 2.5:1) ○ High incidence areas (M:F = 8:1) • Epidemiology ○ High incidence: Africa & Asia ○ HCC in cirrhosis due to hepatitis C virus ○ Up to 30% of noncirrhotic HBV may develop HCC Natural History & Prognosis • Complications: Spontaneous rupture & hemoperitoneum • 30% 5-year survival Treatment • Surgical resection in patients with adequate hepatic reserve • Radiofrequency/alcohol/microwave ablation for small, isolated tumors • Liver transplant if Milan criteria met: Single tumor 2-5 cm or 3 tumors each < 3 cm, no vascular invasion or extrahepatic spread • Intra-arterial chemoembolization or radioembolization (Yttrium-90) for multifocal unresectable tumor • Sorafenib or external beam radiation in unresectable patients who failed other treatments PATHOLOGY General Features • Etiology ○ Cirrhosis (60-90%): Due to chronic viral hepatitis (HBV, SELECTED REFERENCES HCV), alcoholic cirrhosis, primary biliary cirrhosis – HCV patients typically cirrhotic; HBV patients often not cirrhotic ○ Nonalcoholic steatohepatitis (NASH) increasing cause of HCC in North America ○ Carcinogens: Aflatoxins, siderosis, Thorotrast, androgens ○ α-1-antitrypsin deficiency, hemochromatosis, Wilson, hereditary tyrosinemia • Genetics http://radiologyebook.com/ 1. Davarpanah AH et al: The role of imaging in hepatocellular carcinoma: the present and future. J Clin Gastroenterol. 47 Suppl:S7-10, 2013 2. Liu YI et al: Quantitatively defining washout in hepatocellular carcinoma. AJR Am J Roentgenol. 200(1):84-9, 2013 3. Maturen KE et al: Posterior acoustic enhancement in hepatocellular carcinoma. J Ultrasound Med. 30(4):495-9, 2011 4. Management of Hepatocellular Carcinoma: An Update (AASLD) 5. Proposal for Improved Imaging Criteria for HCC Exceptions (OPTN) 6. Liver Imaging and Reporting Data System (LIRADS)
- Page 218 and 219: Hepatic Cyst TERMINOLOGY Synonyms
- Page 220 and 221: Hepatic Cyst (Left) Transverse and
- Page 222 and 223: Biliary Hamartoma TERMINOLOGY Synon
- Page 224 and 225: Biliary Hamartoma (Left) Ultrasound
- Page 226 and 227: Caroli Disease TERMINOLOGY Synonyms
- Page 228 and 229: Caroli Disease (Left) Oblique abdom
- Page 230 and 231: Biloma TERMINOLOGY Definitions •
- Page 232 and 233: Biliary Cystadenoma/Carcinoma TERMI
- Page 234 and 235: Biliary Cystadenoma/Carcinoma (Left
- Page 236 and 237: Pyogenic Hepatic Abscess TERMINOLOG
- Page 238 and 239: Pyogenic Hepatic Abscess (Left) Obl
- Page 240 and 241: Amebic Hepatic Abscess TERMINOLOGY
- Page 242 and 243: Amebic Hepatic Abscess (Left) Longi
- Page 244 and 245: Hepatic Echinococcus Cyst TERMINOLO
- Page 246 and 247: Hepatic Echinococcus Cyst (Left) Ob
- Page 248 and 249: Hepatic Diffuse Microabscesses TERM
- Page 250 and 251: Peribiliary Cyst TERMINOLOGY Synony
- Page 252 and 253: Ciliated Hepatic Foregut Cyst TERMI
- Page 254 and 255: Hepatic Cavernous Hemangioma TERMIN
- Page 256 and 257: Hepatic Cavernous Hemangioma (Left)
- Page 258 and 259: Hepatic Cavernous Hemangioma (Left)
- Page 260 and 261: Focal Nodular Hyperplasia TERMINOLO
- Page 262 and 263: Focal Nodular Hyperplasia (Left) Tr
- Page 264 and 265: Hepatic Adenoma TERMINOLOGY Synonym
- Page 266 and 267: Hepatic Adenoma (Left) Transverse t
- Page 270 and 271: Hepatocellular Carcinoma (Left) Tra
- Page 272 and 273: Hepatocellular Carcinoma (Left) Tra
- Page 274 and 275: Hepatic Metastases TERMINOLOGY Defi
- Page 276 and 277: Hepatic Metastases (Left) Transvers
- Page 278 and 279: Hepatic Lymphoma TERMINOLOGY Defini
- Page 280 and 281: Hepatic Lymphoma (Left) Transverse
- Page 282 and 283: Transjugular Intrahepatic Portosyst
- Page 284 and 285: Transjugular Intrahepatic Portosyst
- Page 286 and 287: Portal Vein Occlusion TERMINOLOGY A
- Page 288 and 289: Portal Vein Occlusion (Left) Color
- Page 290 and 291: Budd-Chiari Syndrome TERMINOLOGY Ab
- Page 292 and 293: Budd-Chiari Syndrome (Left) Color D
- Page 294 and 295: Portal Vein Gas TERMINOLOGY Abbrevi
- Page 296 and 297: Liver Transplant Portal Vein Stenos
- Page 298 and 299: Liver Transplant Biliary Stricture
- Page 300 and 301: PART II SECTION 2 Biliary System In
- Page 302 and 303: Approach to Biliary Sonography hosp
- Page 304 and 305: Approach to Biliary Sonography (Lef
- Page 306 and 307: Approach to Biliary Sonography (Lef
- Page 308 and 309: Cholelithiasis TERMINOLOGY Synonyms
- Page 310 and 311: Cholelithiasis (Left) Longitudinal
- Page 312 and 313: Cholelithiasis (Left) Abdominal rad
- Page 314 and 315: Echogenic Bile TERMINOLOGY Synonyms
- Page 316 and 317: Echogenic Bile (Left) Transverse ul
Hepatocellular Carcinoma<br />
248<br />
Diagnoses: Liver<br />
• Gallium scan: Gallium-avid in 90% of cases<br />
• FDG PET/CT: Uptake in 55% of cases<br />
Imaging Recommendations<br />
• <strong>Ultrasound</strong>: Screening <strong>and</strong> surveillance in high-risk patients<br />
(chronic hepatitis or cirrhosis)<br />
○ Current recommendation by American Association for<br />
the Study of Liver Disease (AASLD) is<br />
screening/surveillance US every 6 months<br />
– Nodule < 1 cm reimaged on US in 3 months to<br />
determine growth<br />
– Nodule > 1 cm further characterized by CECT or<br />
contrast-enhanced MR<br />
• CECT or CEMR: Definitive lesion characterization<br />
○ Use Liver Imaging Reporting <strong>and</strong> Database System (LI-<br />
RADS) or Organ Procurement <strong>and</strong> Transplantation<br />
Netwok (OPTN) imaging criteria<br />
• Contrast-enhanced US: May be considered for lesion<br />
characterization if available<br />
DIFFERENTIAL DIAGNOSIS<br />
Regenerative or Dysplastic Nodule<br />
• When < 1 cm, often not visible on US<br />
• Regenerative <strong>and</strong> dysplastic nodules may be hypervascular<br />
on arterial phase but do not wash-out on portal or delayed<br />
phase<br />
Focal Nodular Hyperplasia<br />
• Homogeneous hypo-/iso-/hyperechoic mass with central<br />
scar <strong>and</strong> spoke-wheel vascularity<br />
• Hypervascular on arterial phase but often isodense <strong>and</strong><br />
isointense to liver on portal venous <strong>and</strong> delayed phase<br />
CECT & CEMR<br />
Metastases<br />
• Mimic nodular or multifocal HCC<br />
• Lower incidence in cirrhotic livers<br />
Cholangiocarcinoma<br />
• Peripheral cholangiocarcinomas often obstruct bile ducts<br />
leading to ductal dilatation<br />
• Capsular retraction; volume loss<br />
Hepatic Hemangioma<br />
• Unusual in cirrhotic liver<br />
• Well-defined hyperechoic nodule<br />
• Undetectable internal vascularity on color Doppler<br />
○ HBV DNA integrated into host cell genome → genomic<br />
instability<br />
Gross Pathologic & Surgical Features<br />
• Soft tumor arising from hepatocytes; may contain necrosis,<br />
hemorrhage, calcification, fat, vascular invasion<br />
Microscopic Features<br />
• Sinusoidal vessels surround tumor cells<br />
• Architectural growth patterns: Trabecular (most common),<br />
solid, tubular (acinar, duct-like, pseudo-gl<strong>and</strong>ular)<br />
• HCC variants: Clear cell (may contain fat or glycogen),<br />
scirrhous, sarcomatoid, sclerosing, mixed hepatocellularcholangiocarcinoma<br />
CLINICAL ISSUES<br />
Presentation<br />
• Elderly patient with history of cirrhosis, ascites, weight loss,<br />
right upper quadrant pain, & ↑ α-fetoprotein (AFP)<br />
• Lab data: Elevated serum AFP <strong>and</strong> liver function tests<br />
○ Diagnosis: If imaging features characteristic, diagnosis<br />
made solely by CECT or MR; biopsy reserved for<br />
indeterminate cases<br />
Demographics<br />
• Age<br />
○ Low incidence areas: 6th-7th decade<br />
○ High incidence areas: 30-45 years<br />
• Gender<br />
○ Low incidence areas (M:F = 2.5:1)<br />
○ High incidence areas (M:F = 8:1)<br />
• Epidemiology<br />
○ High incidence: Africa & Asia<br />
○ HCC in cirrhosis due to hepatitis C virus<br />
○ Up to 30% of noncirrhotic HBV may develop HCC<br />
Natural History & Prognosis<br />
• Complications: Spontaneous rupture & hemoperitoneum<br />
• 30% 5-year survival<br />
Treatment<br />
• Surgical resection in patients with adequate hepatic reserve<br />
• Radiofrequency/alcohol/microwave ablation for small,<br />
isolated tumors<br />
• Liver transplant if Milan criteria met: Single tumor 2-5 cm or<br />
3 tumors each < 3 cm, no vascular invasion or extrahepatic<br />
spread<br />
• Intra-arterial chemoembolization or radioembolization<br />
(Yttrium-90) for multifocal unresectable tumor<br />
• Sorafenib or external beam radiation in unresectable<br />
patients who failed other treatments<br />
PATHOLOGY<br />
General Features<br />
• Etiology<br />
○ Cirrhosis (60-90%): Due to chronic viral hepatitis (HBV,<br />
SELECTED REFERENCES<br />
HCV), alcoholic cirrhosis, primary biliary cirrhosis<br />
– HCV patients typically cirrhotic; HBV patients often<br />
not cirrhotic<br />
○ Nonalcoholic steatohepatitis (NASH) increasing cause of<br />
HCC in North America<br />
○ Carcinogens: Aflatoxins, siderosis, Thorotrast, <strong>and</strong>rogens<br />
○ α-1-antitrypsin deficiency, hemochromatosis, Wilson,<br />
hereditary tyrosinemia<br />
• Genetics<br />
http://radiologyebook.com/<br />
1. Davarpanah AH et al: The role of imaging in hepatocellular carcinoma: the<br />
present <strong>and</strong> future. J Clin Gastroenterol. 47 Suppl:S7-10, 2013<br />
2. Liu YI et al: Quantitatively defining washout in hepatocellular carcinoma. AJR<br />
Am J Roentgenol. 200(1):84-9, 2013<br />
3. Maturen KE et al: Posterior acoustic enhancement in hepatocellular<br />
carcinoma. J <strong>Ultrasound</strong> Med. 30(4):495-9, 2011<br />
4. Management of Hepatocellular Carcinoma: An Update (AASLD)<br />
5. Proposal for Improved Imaging Criteria for HCC Exceptions (OPTN)<br />
6. Liver Imaging <strong>and</strong> Reporting Data System (LIRADS)