Diagnostic Ultrasound - Abdomen and Pelvis
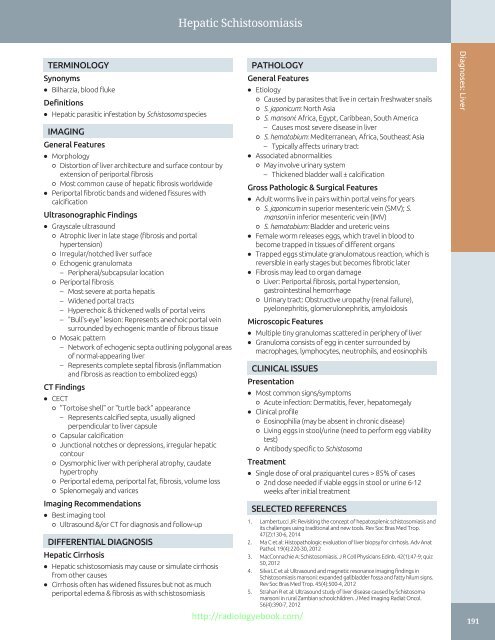
Hepatic Schistosomiasis TERMINOLOGY Synonyms • Bilharzia, blood fluke Definitions • Hepatic parasitic infestation by Schistosoma species IMAGING General Features • Morphology ○ Distortion of liver architecture and surface contour by extension of periportal fibrosis ○ Most common cause of hepatic fibrosis worldwide • Periportal fibrotic bands and widened fissures with calcification Ultrasonographic Findings • Grayscale ultrasound ○ Atrophic liver in late stage (fibrosis and portal hypertension) ○ Irregular/notched liver surface ○ Echogenic granulomata – Peripheral/subcapsular location ○ Periportal fibrosis – Most severe at porta hepatis – Widened portal tracts – Hyperechoic & thickened walls of portal veins – "Bull's-eye" lesion: Represents anechoic portal vein surrounded by echogenic mantle of fibrous tissue ○ Mosaic pattern – Network of echogenic septa outlining polygonal areas of normal-appearing liver – Represents complete septal fibrosis (inflammation and fibrosis as reaction to embolized eggs) CT Findings • CECT ○ "Tortoise shell" or "turtle back" appearance – Represents calcified septa, usually aligned perpendicular to liver capsule ○ Capsular calcification ○ Junctional notches or depressions, irregular hepatic contour ○ Dysmorphic liver with peripheral atrophy, caudate hypertrophy ○ Periportal edema, periportal fat, fibrosis, volume loss ○ Splenomegaly and varices Imaging Recommendations • Best imaging tool ○ Ultrasound &/or CT for diagnosis and follow-up DIFFERENTIAL DIAGNOSIS Hepatic Cirrhosis • Hepatic schistosomiasis may cause or simulate cirrhosis from other causes • Cirrhosis often has widened fissures but not as much periportal edema & fibrosis as with schistosomiasis PATHOLOGY General Features • Etiology ○ Caused by parasites that live in certain freshwater snails ○ S. japonicum: North Asia ○ S. mansoni: Africa, Egypt, Caribbean, South America – Causes most severe disease in liver ○ S. hematobium: Mediterranean, Africa, Southeast Asia – Typically affects urinary tract • Associated abnormalities ○ May involve urinary system – Thickened bladder wall ± calcification Gross Pathologic & Surgical Features • Adult worms live in pairs within portal veins for years ○ S. japonicum in superior mesenteric vein (SMV); S. mansoni in inferior mesenteric vein (IMV) ○ S. hematobium: Bladder and ureteric veins • Female worm releases eggs, which travel in blood to become trapped in tissues of different organs • Trapped eggs stimulate granulomatous reaction, which is reversible in early stages but becomes fibrotic later • Fibrosis may lead to organ damage ○ Liver: Periportal fibrosis, portal hypertension, gastrointestinal hemorrhage ○ Urinary tract: Obstructive uropathy (renal failure), pyelonephritis, glomerulonephritis, amyloidosis Microscopic Features • Multiple tiny granulomas scattered in periphery of liver • Granuloma consists of egg in center surrounded by macrophages, lymphocytes, neutrophils, and eosinophils CLINICAL ISSUES Presentation • Most common signs/symptoms ○ Acute infection: Dermatitis, fever, hepatomegaly • Clinical profile ○ Eosinophilia (may be absent in chronic disease) ○ Living eggs in stool/urine (need to perform egg viability test) ○ Antibody specific to Schistosoma Treatment • Single dose of oral praziquantel cures > 85% of cases ○ 2nd dose needed if viable eggs in stool or urine 6-12 weeks after initial treatment SELECTED REFERENCES 1. Lambertucci JR: Revisiting the concept of hepatosplenic schistosomiasis and its challenges using traditional and new tools. Rev Soc Bras Med Trop. 47(2):130-6, 2014 2. Ma C et al: Histopathologic evaluation of liver biopsy for cirrhosis. Adv Anat Pathol. 19(4):220-30, 2012 3. MacConnachie A: Schistosomiasis. J R Coll Physicians Edinb. 42(1):47-9; quiz 50, 2012 4. Silva LC et al: Ultrasound and magnetic resonance imaging findings in Schistosomiasis mansoni: expanded gallbladder fossa and fatty hilum signs. Rev Soc Bras Med Trop. 45(4):500-4, 2012 5. Strahan R et al: Ultrasound study of liver disease caused by Schistosoma mansoni in rural Zambian schoolchildren. J Med Imaging Radiat Oncol. 56(4):390-7, 2012 http://radiologyebook.com/ Diagnoses: Liver 191
Venoocclusive Disease Diagnoses: Liver TERMINOLOGY • Hepatic venous outflow obstruction due to occlusion of terminal hepatic venules and sinusoids • Synonym: Hepatic sinusoidal obstruction syndrome IMAGING • Hepatosplenomegaly, ascites, gallbladder wall thickening • Narrowing of hepatic veins • Color Doppler ultrasound ○ Elevated hepatic arterial velocity > 100 cm/s ○ Slow portal venous velocity (< 10 cm/s) or hepatofugal flow TOP DIFFERENTIAL DIAGNOSES • Graft-vs.-host disease • Budd-Chiari syndrome • Portal vein thrombosis • Portal hypertension • Opportunistic infection KEY FACTS PATHOLOGY • Injury to hepatic venous endothelium • Progresses to deposition of fibrinogen + factor VIII within venule and sinusoidal walls • Progressive venular obstruction, centrilobular hemorrhagic necrosis • Sclerosis of venular wall and intense collagen deposition in sinusoids and venules CLINICAL ISSUES • Occurs most frequently following hematopoietic cell transplantation ○ Responsible for 5-15% of deaths in population with VOD • Signs and symptoms of liver failure with painful hepatomegaly, jaundice, peripheral edema, unexplained weight gain • Clinical and laboratory features of VOD usually begin within 3 weeks of transplantation (Left) Color Doppler US of the liver shows hepatofugal flow in the main portal vein ſt in a patient with venoocclusive disease (VOD) after bone marrow transplant for AML. Note edematous appearance of the liver and hypertrophied hepatic artery . (Right) On pulsed Doppler US in the same patient, peak systolic velocity measured at the common hepatic artery is elevated to 168 cm/s, confirming high flow state of the hepatic artery related to hepatic arterial buffer response to hepatofugal portal flow. (Left) Grayscale ultrasound of liver shows markedly edematous and an enlarged liver resulting in narrowed hepatic veins st and smallcaliber inferior vena cava ſt in this patient with VOD. A small right pleural effusion is also evident. (Right) Grayscale ultrasound shows diffuse gallbladder wall thickening ſt and sludge in this patient with VOD. Gallbladder wall thickening in isolation is a nonspecific finding. However, in combination with other sonographic findings of VOD, is supportive of this diagnosis. 192 http://radiologyebook.com/
- Page 162 and 163: Uterus ARTERIES OF UTERUS AND ADJAC
- Page 164 and 165: Uterus NORMAL VARIATIONS, UTERINE P
- Page 166 and 167: Uterus UTERINE VARIATIONS WITH AGE
- Page 168 and 169: Uterus CYCLIC CHANGES OF ENDOMETRIU
- Page 170 and 171: Uterus FALLOPIAN TUBE Anatomy: Pelv
- Page 172 and 173: Cervix GRAPHICS OF CERVIX ANATOMY A
- Page 174 and 175: Cervix TRANSVAGINAL ULTRASOUND OF C
- Page 176 and 177: Cervix CHANGES OF CERVIX DURING PRE
- Page 178 and 179: Vagina GRAPHICS OF NORMAL VAGINAL A
- Page 180 and 181: Vagina Urinary bladder TRANSVERSE U
- Page 182 and 183: Vagina SPECTRAL WAVEFORM OF VAGINAL
- Page 184 and 185: Ovaries Mesosalpinx LIGAMENTOUS SUP
- Page 186 and 187: Ovaries Transvaginal transducer NOR
- Page 188 and 189: Ovaries Ovarian artery SPECTRAL WAV
- Page 190 and 191: Ovaries CYCLIC CHANGES OF OVARY Ana
- Page 192 and 193: Ovaries CYCLIC CHANGES OF INTRAOVAR
- Page 194 and 195: Liver Transplant Hepatic Artery Ste
- Page 196 and 197: Approach to Hepatic Sonography (Lef
- Page 198 and 199: Approach to Hepatic Sonography (Lef
- Page 200 and 201: Acute Hepatitis TERMINOLOGY Definit
- Page 202 and 203: Acute Hepatitis (Left) Transverse g
- Page 204 and 205: Hepatic Cirrhosis TERMINOLOGY Defin
- Page 206 and 207: Hepatic Cirrhosis (Left) Longitudin
- Page 208 and 209: Hepatic Steatosis TERMINOLOGY Synon
- Page 210 and 211: Hepatic Steatosis (Left) Transverse
- Page 214 and 215: Venoocclusive Disease TERMINOLOGY A
- Page 216 and 217: Venoocclusive Disease (Left) Graysc
- Page 218 and 219: Hepatic Cyst TERMINOLOGY Synonyms
- Page 220 and 221: Hepatic Cyst (Left) Transverse and
- Page 222 and 223: Biliary Hamartoma TERMINOLOGY Synon
- Page 224 and 225: Biliary Hamartoma (Left) Ultrasound
- Page 226 and 227: Caroli Disease TERMINOLOGY Synonyms
- Page 228 and 229: Caroli Disease (Left) Oblique abdom
- Page 230 and 231: Biloma TERMINOLOGY Definitions •
- Page 232 and 233: Biliary Cystadenoma/Carcinoma TERMI
- Page 234 and 235: Biliary Cystadenoma/Carcinoma (Left
- Page 236 and 237: Pyogenic Hepatic Abscess TERMINOLOG
- Page 238 and 239: Pyogenic Hepatic Abscess (Left) Obl
- Page 240 and 241: Amebic Hepatic Abscess TERMINOLOGY
- Page 242 and 243: Amebic Hepatic Abscess (Left) Longi
- Page 244 and 245: Hepatic Echinococcus Cyst TERMINOLO
- Page 246 and 247: Hepatic Echinococcus Cyst (Left) Ob
- Page 248 and 249: Hepatic Diffuse Microabscesses TERM
- Page 250 and 251: Peribiliary Cyst TERMINOLOGY Synony
- Page 252 and 253: Ciliated Hepatic Foregut Cyst TERMI
- Page 254 and 255: Hepatic Cavernous Hemangioma TERMIN
- Page 256 and 257: Hepatic Cavernous Hemangioma (Left)
- Page 258 and 259: Hepatic Cavernous Hemangioma (Left)
- Page 260 and 261: Focal Nodular Hyperplasia TERMINOLO
Hepatic Schistosomiasis<br />
TERMINOLOGY<br />
Synonyms<br />
• Bilharzia, blood fluke<br />
Definitions<br />
• Hepatic parasitic infestation by Schistosoma species<br />
IMAGING<br />
General Features<br />
• Morphology<br />
○ Distortion of liver architecture <strong>and</strong> surface contour by<br />
extension of periportal fibrosis<br />
○ Most common cause of hepatic fibrosis worldwide<br />
• Periportal fibrotic b<strong>and</strong>s <strong>and</strong> widened fissures with<br />
calcification<br />
Ultrasonographic Findings<br />
• Grayscale ultrasound<br />
○ Atrophic liver in late stage (fibrosis <strong>and</strong> portal<br />
hypertension)<br />
○ Irregular/notched liver surface<br />
○ Echogenic granulomata<br />
– Peripheral/subcapsular location<br />
○ Periportal fibrosis<br />
– Most severe at porta hepatis<br />
– Widened portal tracts<br />
– Hyperechoic & thickened walls of portal veins<br />
– "Bull's-eye" lesion: Represents anechoic portal vein<br />
surrounded by echogenic mantle of fibrous tissue<br />
○ Mosaic pattern<br />
– Network of echogenic septa outlining polygonal areas<br />
of normal-appearing liver<br />
– Represents complete septal fibrosis (inflammation<br />
<strong>and</strong> fibrosis as reaction to embolized eggs)<br />
CT Findings<br />
• CECT<br />
○ "Tortoise shell" or "turtle back" appearance<br />
– Represents calcified septa, usually aligned<br />
perpendicular to liver capsule<br />
○ Capsular calcification<br />
○ Junctional notches or depressions, irregular hepatic<br />
contour<br />
○ Dysmorphic liver with peripheral atrophy, caudate<br />
hypertrophy<br />
○ Periportal edema, periportal fat, fibrosis, volume loss<br />
○ Splenomegaly <strong>and</strong> varices<br />
Imaging Recommendations<br />
• Best imaging tool<br />
○ <strong>Ultrasound</strong> &/or CT for diagnosis <strong>and</strong> follow-up<br />
DIFFERENTIAL DIAGNOSIS<br />
Hepatic Cirrhosis<br />
• Hepatic schistosomiasis may cause or simulate cirrhosis<br />
from other causes<br />
• Cirrhosis often has widened fissures but not as much<br />
periportal edema & fibrosis as with schistosomiasis<br />
PATHOLOGY<br />
General Features<br />
• Etiology<br />
○ Caused by parasites that live in certain freshwater snails<br />
○ S. japonicum: North Asia<br />
○ S. mansoni: Africa, Egypt, Caribbean, South America<br />
– Causes most severe disease in liver<br />
○ S. hematobium: Mediterranean, Africa, Southeast Asia<br />
– Typically affects urinary tract<br />
• Associated abnormalities<br />
○ May involve urinary system<br />
– Thickened bladder wall ± calcification<br />
Gross Pathologic & Surgical Features<br />
• Adult worms live in pairs within portal veins for years<br />
○ S. japonicum in superior mesenteric vein (SMV); S.<br />
mansoni in inferior mesenteric vein (IMV)<br />
○ S. hematobium: Bladder <strong>and</strong> ureteric veins<br />
• Female worm releases eggs, which travel in blood to<br />
become trapped in tissues of different organs<br />
• Trapped eggs stimulate granulomatous reaction, which is<br />
reversible in early stages but becomes fibrotic later<br />
• Fibrosis may lead to organ damage<br />
○ Liver: Periportal fibrosis, portal hypertension,<br />
gastrointestinal hemorrhage<br />
○ Urinary tract: Obstructive uropathy (renal failure),<br />
pyelonephritis, glomerulonephritis, amyloidosis<br />
Microscopic Features<br />
• Multiple tiny granulomas scattered in periphery of liver<br />
• Granuloma consists of egg in center surrounded by<br />
macrophages, lymphocytes, neutrophils, <strong>and</strong> eosinophils<br />
CLINICAL ISSUES<br />
Presentation<br />
• Most common signs/symptoms<br />
○ Acute infection: Dermatitis, fever, hepatomegaly<br />
• Clinical profile<br />
○ Eosinophilia (may be absent in chronic disease)<br />
○ Living eggs in stool/urine (need to perform egg viability<br />
test)<br />
○ Antibody specific to Schistosoma<br />
Treatment<br />
• Single dose of oral praziquantel cures > 85% of cases<br />
○ 2nd dose needed if viable eggs in stool or urine 6-12<br />
weeks after initial treatment<br />
SELECTED REFERENCES<br />
1. Lambertucci JR: Revisiting the concept of hepatosplenic schistosomiasis <strong>and</strong><br />
its challenges using traditional <strong>and</strong> new tools. Rev Soc Bras Med Trop.<br />
47(2):130-6, 2014<br />
2. Ma C et al: Histopathologic evaluation of liver biopsy for cirrhosis. Adv Anat<br />
Pathol. 19(4):220-30, 2012<br />
3. MacConnachie A: Schistosomiasis. J R Coll Physicians Edinb. 42(1):47-9; quiz<br />
50, 2012<br />
4. Silva LC et al: <strong>Ultrasound</strong> <strong>and</strong> magnetic resonance imaging findings in<br />
Schistosomiasis mansoni: exp<strong>and</strong>ed gallbladder fossa <strong>and</strong> fatty hilum signs.<br />
Rev Soc Bras Med Trop. 45(4):500-4, 2012<br />
5. Strahan R et al: <strong>Ultrasound</strong> study of liver disease caused by Schistosoma<br />
mansoni in rural Zambian schoolchildren. J Med Imaging Radiat Oncol.<br />
56(4):390-7, 2012<br />
http://radiologyebook.com/<br />
Diagnoses: Liver<br />
191