Continuous Renal Replacement Therapy Liverpool SSWAHS
Continuous Renal Replacement Therapy Liverpool SSWAHS
Continuous Renal Replacement Therapy Liverpool SSWAHS
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Liverpool</strong> Health Service<br />
Intensive Care Unit<br />
Self Directed Learning Package:<br />
<strong>Continuous</strong> <strong>Renal</strong> <strong>Replacement</strong> <strong>Therapy</strong><br />
Written by: Nicholas Mifflin & Sharon-Ann Shunker
How to use this package<br />
This package is designed to be used in the clinical area as a self directed<br />
learning tool.<br />
The package is divided into sections. At the end of each section is a self test<br />
to determine how well you have understood the information contained in<br />
that section. You will need to complete the self tests at the end of each<br />
section and ensure that you have mastered the content before moving on to<br />
the next section.<br />
If you have any trouble with the self test, go back over the section and revise<br />
the content. If you are still unsure then you will need to speak with one of<br />
the educators in your area.<br />
The answers to each of the self test questions are contained at the end of the<br />
package. To gain the most benefit from this package attempt the questions<br />
first before seeking this reference.<br />
GOOD LUCK!!!
Learning package objectives<br />
By the completion of this package, the registered nurse will be able to:<br />
1. Define and classify acute renal failure according to its aetiology<br />
2. Identify the signs and symptoms of acute renal failure<br />
3. Discuss the various modalities of renal replacement therapy including<br />
advantages and disadvantages<br />
4. Identify the indications for continuous renal replacement therapy<br />
5. Describe the basic principles of fluid and waste removal involved in<br />
CRRT<br />
6. Describe the various modes of CRRT<br />
7. Recognise the importance of access in CRRT<br />
8. Explain the process for troubleshooting a vascath<br />
9. Differentiate solutions used for CRRT<br />
10. Discuss the safety precautions required for commencing CRRT<br />
11. Differentiate pre dilution from post dilution<br />
12. State the complications of CRRT<br />
13. Describe methods that optimise clearance of fluid and waste<br />
14. Describe methods of prolonging filter life<br />
15. Discuss the indications for ceasing therapy<br />
16. Recognise common reasons for CRRT machine alarms<br />
17. Discuss the nursing management of the patient on CRRT
A Brief Look at <strong>Renal</strong> Anatomy & Physiology<br />
Structures of the <strong>Renal</strong> System:<br />
Adrenal Gland<br />
Kidney<br />
Ureter<br />
Bladder<br />
Urethra<br />
Cross Section of the Kidney:<br />
The renal system is comprised of the<br />
Kidneys and those structures including<br />
the ureters, bladder and urethra that<br />
form the urinary system.<br />
The primary role of the kidneys is to<br />
remove metabolic wastes and maintain<br />
fluid and electrolyte balance. The<br />
kidneys also have a role in:<br />
• Blood Pressure Control<br />
• Red Blood Cell Synthesis<br />
• Bone Metabolism<br />
• Acid- Base Balance<br />
<strong>Renal</strong> dysfunction can negatively impact<br />
on all of these roles. 11<br />
The kidneys are situated in the<br />
retroperitoneum located between T12<br />
and L3 on each side of the vertebral<br />
column. 12<br />
Two layers form them internally. The<br />
outer layer is the Cortex that contains:<br />
• Glomeruli<br />
• Proximal Tubules<br />
• Cortical Portions of Loops of<br />
Henle<br />
• Distal Tubules<br />
• Cortical Collecting Ducts 11,12<br />
The inner layer or Medulla is comprised<br />
of <strong>Renal</strong> Pyramids. The pyramids<br />
contain:<br />
• Medullary portions of Loops of<br />
Henle<br />
• Medullary Portions of Collecting<br />
Ducts 12<br />
Multiple pyramids taper and join<br />
forming a minor calyx. Several<br />
combined make a major calyx. The<br />
major calyces join and enter a funnel<br />
shaped renal pelvis that directs urine<br />
into the ureter. 11
Components of the Nephron:<br />
Urine Formation:<br />
Three processes required for urine formation include:<br />
• Glomerular Filtration<br />
• Tubular Reabsorption<br />
• Tubular Secretion 11,12<br />
Approximately one million nephrons<br />
comprise each kidney. The nephron<br />
consists of:<br />
• Glomerulus<br />
• Bowman Capsule<br />
• Proximal Convoluted Tubule<br />
• Loop of Henle<br />
• Distal Convoluted Tubule<br />
• Collecting Duct 11,12<br />
There are two types of nephron:<br />
• Cortical Nephrons<br />
• Juxtamedullary Nephrons 11<br />
Cortical Nephrons:<br />
• Approximately 85 %<br />
• Perform excretory and regulatory<br />
functions 11<br />
Juxtamedullary Nephrons:<br />
• Approximately 15 %<br />
• Responsible for concentration and<br />
dilution of urine 11<br />
Glomerulus<br />
• Filters fluid and solutes from blood<br />
Proximal Convoluted Tubule<br />
• Reabsorbs Na +, K +, Cl -, HCO3 -, urea, glucose & amino<br />
acids<br />
• Filtrate Continues<br />
Loop of Henle<br />
• Reabsorbs Na +, K + & Cl -<br />
• Blocks reabsorption of H2O<br />
• Dilutes/Concentrates Urine<br />
• Filtrate Continues<br />
Distal Tubule<br />
• Na +, K +, Ca ++, PO4 selectively reabsorbed<br />
• H2O reabsorbed in presence of Antidiuretic Hormone<br />
(ADH)<br />
• Filtrate Continues<br />
Collecting Duct<br />
• Reabsorption similar to distal tubule<br />
• HCO3 - & H - reabsorbed/secreted to acidify urine<br />
• Filtrate leaves hyperosmotic/hypoosmotic depending on<br />
the body’s requirements 11,12
Composition of Urine:<br />
H2O<br />
Electrolytes- Na +, K +, Cl -, HCO3 -<br />
End products of protein metabolism- urea, creatinine, PO4, SO4<br />
End products of nucleic acid metabolism- uric acid<br />
Breakdown products of phosphoric and sulphuric acid<br />
H + ions excreted bound to buffers such as PO4 and NH3 11<br />
<strong>Renal</strong> Anatomy & Physiology in Summary:<br />
• Kidneys filter blood of waste products<br />
• Functional units of the kidneys are called nephrons<br />
• Nephrons consist of a glomerulus, tubule and collecting duct<br />
• Urine is formed through glomerular filtration, tubular reabsorption<br />
and tubular secretion<br />
• Urine moves from the collecting duct via the renal pelvis and ureters<br />
into the bladder, where it is excreted from the body through the<br />
urethra<br />
• Some substances are reabsorbed into the blood and others excreted<br />
into the filtrate
Self Test 1<br />
Q1. State the primary and secondary functions of the kidneys.<br />
Q2. Name the functional units of the Kidneys and list their components.<br />
Q3. Discuss the processes involved in urine formation
Summary of Acute <strong>Renal</strong> Failure<br />
Definition:<br />
Acute renal failure (ARF) is a clinical syndrome, characterised by an<br />
abrupt decline in glomerular filtration rate (GFR). There is a subsequent<br />
retention of metabolic waste products and an inability to maintain<br />
electrolyte and acid-base homeostasis. Regulation of fluid volume is<br />
also affected. 1,7,8,16,18,23<br />
ARF occurs rapidly resulting in fifty percent or more nephrons to lose<br />
function, and as this occurs quickly the body is unable to compensate.<br />
There are three classifications of ARF based on the location of the cause. 23<br />
Prerenal<br />
<strong>Renal</strong> dysfunction is largely related to systemic factors that limit blood flow<br />
and reduce glomerular filtration rate. Examples include:<br />
• Hypotension<br />
• Hypovolaemic shock- dehydration, blood loss<br />
• Cardiogenic shock – post MI<br />
• Septic Shock<br />
• Bilateral renal vascular obstruction- thrombosis 1,8,9,16,18,23<br />
Intrarenal<br />
<strong>Renal</strong> impairment occurs secondary to damage that is sustained at the site<br />
of the nephrons. This may be the result of a number of conditions or<br />
nephrotoxins:<br />
• Acute Tubular Necrosis (ATN)<br />
• Acute Glomerulonephritis<br />
• Acute Pyelonephritis<br />
• Acute Cortical Necrosis<br />
• Malignant Hypertension<br />
• Acute Vasculitis<br />
• Rhabdomyolysis - drugs, trauma<br />
• Nephrotoxins - IV contrast, aminoglycosides 1,8,9,16,18,23<br />
Postrenal<br />
<strong>Renal</strong> failure secondary to obstruction that prevents excretion of urine<br />
• Prostatic Hypertrophy<br />
• <strong>Renal</strong> Calculi<br />
• Tumour<br />
• Blocked Urinary Catheter 1,8,9,16,18,23
Signs & Symptoms<br />
• Fluid and electrolyte abnormalities<br />
• Metabolic acidosis<br />
• Anaemia<br />
• Pruritis secondary to uremic frost<br />
• Nausea & vomiting<br />
• Confusion<br />
• ↓LOC<br />
• Congestive heart failure resulting in acute pulmonary oedema 1,8,16,18,23
Self Test 2<br />
Q1. Define Acute <strong>Renal</strong> Failure<br />
Q2. Describe 3 forms of acute renal failure and the associated causes<br />
Q3. List the signs and symptoms of acute renal failure
<strong>Renal</strong> <strong>Replacement</strong> <strong>Therapy</strong><br />
<strong>Renal</strong> replacement therapy (RRT) is an extracorporeal technique of blood<br />
purification. Blood passes over a semipermeable membrane (filter) allowing<br />
solutes and water to cross over to a collection side. There are various<br />
modalities included under the umbrella of RRT. 19<br />
<strong>Continuous</strong> Modalities (CRRT)<br />
• Haemofiltration<br />
• Haemodialysis<br />
• Haemodiafiltration<br />
• Ultrafiltration<br />
Advantages:<br />
• Better for haemodynamic instability<br />
• Readily accessible<br />
• Effective fluid removal and clearance of solutes<br />
• Can be performed by ICU staff rather than specialised renal nurses<br />
2,4,5,9,17,20<br />
Disadvantages:<br />
• Patient mobilisation is limited<br />
• Access complications<br />
• Anticoagulation<br />
• Reduced blood flow rates secondary to small filters when compared to<br />
IHD 2,4,5,9,17,20<br />
Intermittent Haemodialysis (IHD)<br />
Advantages:<br />
• Quick and effective<br />
• Large amounts of fluid and solutes can be removed over a short<br />
period 5,9<br />
Disadvantages:<br />
• Access Complications- formal access such as A.V. Fistula is<br />
eventually required<br />
• Requires specialised staff and is therefore not readily accessible<br />
• May not be well tolerated by haemodynamically unstable patients<br />
• Intermittent fluid removal with IHD can be associated with fluid<br />
overload and increased electrolytes between treatments 5,9<br />
Peritoneal Dialysis<br />
This form of dialysis utilises the peritoneum as the semipermeable<br />
membrane.<br />
Advantages:<br />
• Comparatively Cheaper<br />
• No anticoagulation required
• No haemodynamic instability 5,9,24<br />
Disadvantages:<br />
• High incidence of peritonitis<br />
• Slow clearance<br />
• Access – Formal access required (Tenkhoff catheter)<br />
• Limitations on patient as it is required frequently 5,9,24
<strong>Continuous</strong> <strong>Renal</strong> <strong>Replacement</strong> <strong>Therapy</strong> (CRRT)<br />
Indications<br />
• Fluid Overload, pulmonary oedema<br />
• Worsening Metabolic Acidosis<br />
• Hyperkalaemia<br />
• Worsening Azotaemia<br />
• Drug overdoses<br />
• Removal of toxins 9<br />
Basic Principles<br />
The basic principles incorporated in the function of CRRT involve:<br />
• Convection<br />
• Diffusion<br />
• Ultrafiltration<br />
• Hydrostatic Pressure 2,4,9,17,20<br />
Terminology<br />
Diffusion<br />
The movement of small and middle molecule solutes from an area of high<br />
concentration to low concentration across a semipermeable-membrane. 5,9<br />
Osmosis<br />
The movement of water from an area of high water concentration to an area<br />
of lower water concentration across a semi-permeable membrane. 5,9<br />
22<br />
22
Ultrafiltration<br />
The movement of water and solutes across a semipermeable membrane by<br />
solvent drag created by convection and hydrostatic pressure. 5,9<br />
Convection<br />
Water flow across a semi-permeable membrane by hydrostatic pressure that<br />
drags solutes with it (the way a waterfall moves pebbles and sand) 9<br />
Hydrostatic Pressure<br />
The force that pushes fluid and solutes across the membrane. The<br />
mechanical blood pump on the dialysis machine creates this. 5,9<br />
Oncotic Pressure<br />
Plasma proteins including albumin, globulin and fibrinogen create the<br />
pulling pressure that favours fluid retention and opposes hydrostatic<br />
pressure. 5,9<br />
Counter Current<br />
The flow of two fluids in opposing directions. The direction of dialysis flows<br />
opposite to that of blood flow maximising the concentration difference<br />
between blood and dialysate. 5<br />
Dialysate<br />
A synthetic solute free solution used to achieve diffusive solute clearance 5<br />
Effluent<br />
Erroneous term used to indicate the solute and solvent discarded form the<br />
patient. 9<br />
<strong>Replacement</strong><br />
Pre or post dilution fluid<br />
Pre-dilution<br />
Administration of the replacement fluid into the circuit prior to the filter 5,9<br />
Post-dilution<br />
Administration of replacement fluid into the circuit after the filter 5,9<br />
22
Modalities<br />
• Slow <strong>Continuous</strong> Ultrafiltration (SCUF)<br />
• <strong>Continuous</strong> Arterio/Venovenous Haemofiltration (CAVH/CVVH)<br />
• <strong>Continuous</strong> Arterio/Venovenous Haemodialysis (CAVHD/CVVHD)<br />
• <strong>Continuous</strong> Arterio/Venovenous Haemodiafiltration<br />
(CAVHDF/CVVHDF)<br />
SCUF<br />
Slow <strong>Continuous</strong> Ultrafiltration is the method used when fluid removal is<br />
the only objective. Dialysate and replacement fluids are not utilised.<br />
Maximum fluid removal is 2000ml/hr. 2,17,20<br />
SCUF System Setup 13<br />
= pump<br />
CAVH/CVVH<br />
<strong>Continuous</strong> Venovenous Haemofiltration uses convective clearance to<br />
remove water and solutes. <strong>Replacement</strong> is used to replace ultrafiltrate.<br />
Maximum fluid removal is 1000ml/hr. 2,17,20<br />
CVVH System Setup 13<br />
= pump
CAVHD/CVVHD<br />
<strong>Continuous</strong> Venovenous Haemodialysis uses diffusion to remove fluid and<br />
solutes. Dialysate is pumped in a counter current to blood flow. Maximum<br />
fluid removal is 1000ml/hr. 2,17,20<br />
CVVHD System Setup 13<br />
= pump<br />
CAVHDF/CVVHDF<br />
<strong>Continuous</strong> Venovenous Haemodiafiltration utilises both convection and<br />
diffusion to remove fluid and solutes. Dialysate and replacement is used.<br />
Maximum fluid removal is 1000ml/hr. 2,17,20<br />
CVVHDF System Setup 13<br />
= pump
CRRT Modality Summary 2,17,20<br />
Mode Filtering Process Removes Indication<br />
Slow <strong>Continuous</strong><br />
Ultra Filtration<br />
(SCUF)<br />
<strong>Continuous</strong><br />
Arterio/Venovenous<br />
Haemofiltration<br />
(CAVH/CVVH)<br />
<strong>Continuous</strong><br />
Arterio/Venovenous<br />
Haemodialysis<br />
(CAVHD, CVVHD)<br />
<strong>Continuous</strong><br />
Arterio/Venovenous<br />
Haemodiafiltration<br />
(CAVHDF/CVVHDF<br />
Convection-<br />
Ultrafiltration<br />
Convection-<br />
Ultrafiltration<br />
Diffusion<br />
Convection &<br />
Diffusion<br />
Fluid, Minimal<br />
solutes<br />
Fluid removal.<br />
Moderate solute<br />
removal. Urea<br />
clearance<br />
approximately 15-<br />
17ml/min<br />
Fluid removal. More<br />
aggressive solute<br />
removal. Urea<br />
clearance<br />
approximately 17-<br />
21ml/min.<br />
Maximum fluid and<br />
solute removal. Urea<br />
clearance<br />
approximately 25-<br />
26ml/min.<br />
NB: There are other forms of CRRT however the above are most<br />
applicable to LHS<br />
Fluid Overload<br />
Heart failure<br />
Moderate electrolyte<br />
imbalances<br />
Oliguria with<br />
parenteral nutrition<br />
or blood<br />
requirements<br />
Septic Shock<br />
Fluid overload with<br />
haemodynamic<br />
instability<br />
Azotaemia<br />
Electrolyte<br />
disturbance and<br />
acidosis<br />
Parenteral nutrition<br />
accompanying fluid<br />
overload<br />
Fluid Overload,<br />
pulmonary oedema<br />
Worsening Metabolic<br />
Acidosis<br />
Hyperkalaemia<br />
Worsening Azotaemia<br />
Drug overdoses<br />
Removal of toxins
Self Test 3<br />
Q1. What is renal replacement therapy?<br />
Q2. List advantages and disadvantages of continuous modalities compared<br />
to other forms of RRT<br />
Q3. List Indications for CRRT<br />
Q4. Describe the basic principles of fluid and solute removal involved in<br />
CRRT.<br />
Q5. Describe the different modes of CRRT.
Vascular Access<br />
Good access that allows high flow rates through the circuit is one of the key<br />
aspects in CRRT that effects blood flow, clearance and filter life.<br />
Catheters<br />
Blood Flow is proportional to the diameter of the catheter- i.e. the wider the<br />
tube the better the blood flow. 3,4 Therefore the largest diameter catheter<br />
should be utilised. Vascaths available in <strong>Liverpool</strong> ICU include.<br />
• Gambro- 13fr ( 15cm &20cm)<br />
• Niagra- 13.5Fr (15cm & 24cm)<br />
• Gambro- 12Fr (15cm & 20cm)<br />
• Arrow Triple Lumen- 12 Fr (20cm)<br />
Lumens are colour coded being red and blue. The red lumen is the arterial<br />
port also known as the access port. This lumen supplies blood from the<br />
patient to the filter. The blue lumen is the venous port also known as the<br />
return port. Blood is returned via this lumen from the filter to the patient.<br />
Differentiating these lumens is necessary when troubleshooting access or<br />
return pressure alarms on the CRRT machines. 5<br />
Catheter Location<br />
Typically the vessels utilised for vascaths are the Internal Jugular, Femoral<br />
and Subclavian veins. The choice of catheter site is dependant on many<br />
factors including:<br />
• Skill of the accessing clinician<br />
• Size of the patient<br />
• Mobility of the patient<br />
• Anticipated Duration of therapy<br />
• Presence of other intravenous lines<br />
• Coagulopathy 3,4<br />
Internal Jugular Vein<br />
Advantages:<br />
• Allows for patient mobility<br />
• Easy to visualise insertion site<br />
Disadvantages:<br />
• Requires Chest Xray prior to use<br />
• Kinking can occur when the patient moves their head<br />
• Sometimes attains insubstantial blood flows secondary to variations<br />
in central filling and intrathoracic pressures. Positive pressure<br />
ventilation can make this more apparent. 3,4,5
Femoral Vein<br />
Advantages:<br />
• Easily accessible by most clinicians<br />
• May allow greater blood flows<br />
Disadvantages:<br />
• Prone to kinking, more so in the obese patient<br />
• Does not allow for patient mobility<br />
• Difficult to visualise and dress insertion site<br />
• Higher incidence of infection secondary to the proximity to intestinal<br />
flora. 3,4,5<br />
Subclavian Vein<br />
Advantages:<br />
• Allows for patient mobility<br />
• Easy to visualise and dress insertion site<br />
Disadvantages:<br />
• Requires Chest Xray prior to use<br />
• Risk of pneumothorax on insertion<br />
• Risk of subclavian stenosis, which can impair suitability for an A-V<br />
fistula on the affected side, if renal failure becomes chronic.<br />
• Sometimes attains insubstantial blood flows secondary to variations<br />
in central filling and intrathoracic pressures. Positive pressure<br />
ventilation can make this more noticeable. 3,4,5<br />
Nursing Care for the Access Device<br />
• Regularly inspect insertion site for signs of infection, haematoma and<br />
bleeding<br />
• Apply standard precautions and aseptic technique whenever<br />
connecting or disconnecting lines to and from the catheter<br />
• Clean catheter and site with 0.5% chlorhexidine once weekly and prn<br />
using an aseptic technique and cover with an occlusive dressing (IV<br />
3000)<br />
• When catheter is not in use lumens should be “Heparin-Locked” to<br />
prevent clotting within the catheter 5<br />
NB: Form more information on care of a vas cath see policy-<br />
management of central venous access devices in appendix<br />
Heparin-Lock for a Vas-Cath<br />
• Apply standard precautions and utilise aseptic technique<br />
• Using 3 ampoules of 5000 units heparin in 1ml (15000 units/3ml)<br />
inject the stated amount (located on each port) of this solution into<br />
the Vas Cath port. Label lumens as Heparin Locked 9,10
Troubleshooting Access Device<br />
Where the CRRT machine exhibits high-pressure alarms the problem may<br />
stem from a malfunctioning catheter. Assess catheter patency as follows:<br />
• Apply standard precautions and utilise aseptic technique<br />
• Aspirate and flush 10ml of blood on the effected lumen to test<br />
resistance to blood flow. Further, flush 10ml 0.9% sterile normal<br />
saline. 22<br />
Where resistance is present, a clot may be obstructing the catheter, but<br />
more likely it is positioned against the vessel wall. Slightly withdrawing or<br />
rotating the catheter may overcome this problem. Where this fails to resolve<br />
the problem the catheter must be changed. 5,9,21<br />
NB: Swapping the lumens- i.e. attaching the access line to the return port<br />
and visa versa may also overcome this problem, however this can result in a<br />
significant reduction in clearance and is therefore not recommended. It can<br />
be used as a temporary measure to overcome access problems. 9
Self Test 4<br />
Q1. What is the importance of adequate access?<br />
Q2. Sate the appropriate name and functions of the red and blue lumens on<br />
a vascath<br />
Q3. What are the three possible sites for vascath insertion? State the<br />
advantages and disadvantages of each.<br />
Q4. How would you troubleshoot a vascath?<br />
Q5. How would you heparin lock a vascath?
Preparation for <strong>Therapy</strong><br />
Orders & Equipment<br />
• Obtain a complete and correctly filled order for CRRT using the ICU<br />
CRRT prescription form. NB: Pre dilution or Post dilution set<br />
• Obtain equipment according to ICU protocol <strong>Continuous</strong> <strong>Renal</strong><br />
<strong>Replacement</strong> <strong>Therapy</strong> (CRRT) using the PRISMA MACHINE. NB:<br />
equipment for the PRISMA FLEX is identical except for the required<br />
set, compatible warming line and one extra bag of GAMBRO or<br />
HEMOSOL solution as ordered.<br />
Please read and become familiar with this protocol in conjunction<br />
with this package. (See appendix)<br />
Preparation of Fluids<br />
Losses in ultrafiltrate through CVVH and CVVHDF require replacing.<br />
<strong>Replacement</strong> fluid should be a balanced electrolyte solution that will offset<br />
the convective loss of electrolytes and plasma water during haemofiltration.<br />
As stated earlier, replacement fluid is a pre or post dilution fluid. The fluids<br />
available for such purpose in <strong>Liverpool</strong> ICU include HEMOSOL and<br />
GAMBRO. These fluids are also used as dialysate in modalities where<br />
diffusive clearance is also involved (CVVHDF, CVVHD). 3 To maintain acidbase<br />
balance, it is necessary for these fluids to contain base that will provide<br />
a buffer. Typically lactate serves this purpose as it is converted to<br />
bicarbonate in the liver. 4, GAMBRO is the fluid that contains lactate as<br />
its buffer.<br />
Lactate free solutions also exist where bicarbonate must be added<br />
immediately prior to use. 4, HEMOSOL is considered lactate free and thus<br />
requires the addition of bicarbonate prior to use. This is accomplished by<br />
breaking the seal within the bag to mix the solutions together.<br />
HEMOSOL is the fluid of choice where the patient is severely acidotic or<br />
suffering liver dysfunction that would prevent the metabolism of lactate to<br />
bicarbonate. Utilising GAMBRO in this circumstance may contribute to a<br />
worsening acidosis.<br />
Specific to Dialysate<br />
Both GAMBRO and HEMOSOL solutions require addition of KCL when used<br />
as dialysate. KCL is added to these fluids to reduce loss K + of through<br />
diffusion.<br />
NB: KCL is only added to these fluids when patient’s K + level is<br />
Procedure<br />
• GAMBRO- Add 15mmol K + to 5L (already contains 5mmol K +/ 5L)<br />
• HEMOSOL- Add 20mmol K + to 5L (Contains no K + )<br />
Addition of K + in these quantities will make a final concentration of 4mmol<br />
K + /L. 9<br />
Priming The Circuit<br />
Both PRISMA and PRISMA FLEX machines contain on screen step by step<br />
instructions for setting up and priming the circuit. For further information<br />
on priming the PRISMA machine consult ICU protocol, <strong>Continuous</strong> <strong>Renal</strong><br />
<strong>Replacement</strong> <strong>Therapy</strong> (CRRT) using the PRISMA MACHINE. Further<br />
information regarding the same processes for the PRISMA FLEX can be<br />
found in the operator’s manual located on the back of the machine. Failing<br />
this, please consult a senior staff member or educator that may assist you.<br />
Access<br />
Once the circuit is primed and ready to connect, 5ml of blood should be<br />
aspirated and discarded to remove heparin from the line. The vascath<br />
should then be checked for patency as described earlier in troubleshooting<br />
access device. It is important that therapy with a good circuit not be<br />
commenced on inadequate access. Circuits are expensive and poor access<br />
will significantly reduce its functional duration. Always apply aseptic<br />
technique when accessing catheter. 9
Commencing <strong>Therapy</strong><br />
Providing access is adequate, access and return lines can be connected to<br />
the corresponding lumens of the vascath using standard precautions and<br />
aseptic technique. A full breakdown of this procedure is located in ICU<br />
protocol <strong>Continuous</strong> <strong>Renal</strong> <strong>Replacement</strong> <strong>Therapy</strong> (CRRT) using the PRISMA<br />
MACHINE.<br />
Connecting Patient to CRRT (Running pt on)<br />
• Once patient is connected select desired flow rates for Dialysate,<br />
<strong>Replacement</strong>, Blood Pump Speed, Ultrafiltrate/Fluid removal<br />
according to order (Commence blood pump at 80-100ml/hr and<br />
increase as tolerated by patient)<br />
• Assess patient’s haemodynamic status<br />
• Commence therapy<br />
• Administer 2500 units heparin bolus via the red port on the access<br />
line. Omit heparin bolus if patient is coagulopathic or has been on<br />
CRRT in the last 4 hours.<br />
• Monitor patient for haemodynamic instability for 15-30 minutes post<br />
commencing therapy. Patient may experience a transient drop in<br />
blood pressure, that will therefore require adjustment of pump speed<br />
to compensate, depending on the sensitivity of the patient. 9,21<br />
Safety<br />
• CRRT Machine should be plugged into an isolated power socket<br />
• When commencing therapy, colloid on a pump giving set should be<br />
connected to patient’s intravenous access<br />
• 10mg Metaraminol (Aramine) should be drawn up and readily<br />
available. 10mg of Aramine is prepared in 20ml of 0.9% sodium<br />
chloride. This in conjunction with colloid is precautionary, should the<br />
patient become hypotensive. If the patient is on inotropes, Aramine<br />
may not be necessary as blood pressure can be controlled with the<br />
existing inotropic drugs. 9,21<br />
Pre-dilution or Post-dilution<br />
Pre-dilution involves administering replacement fluid prior to the filter. This<br />
thereby reduces the viscosity of blood and hematocrit and in effect may aid<br />
in preventing filter clotting. Unfortunately this method also dilutes the<br />
concentration of solute in plasma, which can negatively impact on clearance.<br />
In order to optimise clearance of solutes, replacement rate must be<br />
increased in order to increase the rate of ultrafiltration. 3,9<br />
Post-dilution therefore involves administering replacement fluid after the<br />
filter. This does not dilute solutes in plasma, however the ability for optimal<br />
clearance is lost when blood viscosity is not reduced and high flow rates are<br />
then difficult to achieve. With reduced blood flow comes reduced<br />
ultrafiltration. Utilising filters with larger surface areas in conjunction with<br />
this method may improve clearance. 9
Complications<br />
• Hypotension that may result from aggressive fluid removal<br />
• Electrolyte imbalances<br />
• Cardiac Arrhythmias<br />
• Anaemia secondary to haemolysis of red blood cells<br />
• Thrombocytopaenia secondary to platelet aggregation in filter<br />
• Hypothermia secondary to extracorporeal blood circulation<br />
• Coagulopathy secondary to over heparinisation<br />
• Infection (line sepsis)<br />
• Heparin induced thrombocytopaenia 2,9,17,21
Self Test 5<br />
Q1. What is the purpose of dialysate and replacement fluids?<br />
Q2. State the two fluids available at <strong>Liverpool</strong> ICU for CRRT, including the<br />
major difference and the preparations required.<br />
Q3. How do you prepare the vascath prior to commencing CRRT with a new<br />
circuit?<br />
Q4. List the safety aspects of connecting and commencing therapy.<br />
Q5. Differentiate pre dilution from post dilution including benefits and<br />
disadvantages.<br />
Q6. List the complications of CRRT.
Optimising Clearance<br />
Regardless of which CRRT machine is being used, optimising clearance is<br />
dependant on two factors. These include improving diffusion and<br />
convection/ultrafiltration.<br />
Improving Diffusion<br />
Using filters with larger surface areas is one means of improving diffusion. 6<br />
Currently <strong>Liverpool</strong> ICU stock consists of M100 and ST 100 filter sets. The<br />
M100 circuits incorporate an AN69 hollow fiber filter. These filters are<br />
comprised of Acrylonitrile and sodium methallyl sulfonate copolymer and<br />
have a surface area of 0.9m 2. The ST 100 sets are similar but have a surface<br />
area of 1.0 m 2. The filter is comprised of identical materials, however also<br />
includes the surface treatment agent polyethylene imine. 14 This surface<br />
treatment aims to encourage heparin binding during priming that can<br />
ultimately reduce heparin requirements for anticoagulation of the circuit.<br />
This may also benefit patients who require heparin free dialysis. 15<br />
A second means of improving diffusion involves utilising an appropriate<br />
dialysate fluid. Eg. Withholding addition of KCL to dialysate fluid when the<br />
patient is hyperkalaemic so that serum potassium concentration remains<br />
higher than that in the dialysate. K + will therefore be filtered off the patient<br />
from an area of high to low concentration.<br />
Improving Convection/Ultrafiltration<br />
Improving convection/ultrafiltration is largely accomplished through high<br />
flow rates (Dialysate, <strong>Replacement</strong>, Ultrafiltration & Blood Pump). As<br />
mentioned earlier pre dilution assists in achieving higher flow rates by<br />
reducing the viscosity of blood and hematocrit. Location and care of the<br />
vascath is also shown to influence flow considerably. 6,9
Prolonging Filter Life<br />
Prolonging filter life simply refers to preventing the filter clotting and<br />
maintaining its functional ability to remove fluid and waste. Factors that<br />
prolong filter life include:<br />
• High blood flow rates<br />
• Pre dilution and warming of fluid<br />
• Adequate Access<br />
• Anticoagulation 3,4,9<br />
Anticoagulation<br />
• On priming the circuit 5000 units of heparin should be added to each<br />
1L bag of warmed normal saline<br />
• Unless the patient is coagulopathic or has been on CRRT in the past 4<br />
hours, 2500 units of heparin should be administered as a bolus, via<br />
the red pre filter port of the access line, as therapy is commenced.<br />
• A heparin infusion of 15000 units in 50ml 0.9% sodium chloride can<br />
be administered according to ICU HEPARIN SODIUM protocol for<br />
anticoagulation of the dialysis circuit via the designated anticoagulant<br />
line of the circuit.<br />
• Aim for a pre filter APTT (from pre filter port or arterial line/patient)<br />
between 30-40 seconds. 10<br />
NB: If patient is coagulopathic run heparin free CRRT- refer to<br />
protocol for further precautions.<br />
NB: Full information for anticoagulation of the dialysis circuit is available in<br />
ICU HEPARIN SODIUM protocol. Please read and become familiar with this<br />
protocol in conjunction with this package. (See appendix)<br />
Discontinuing CRRT (Running Patient Off)<br />
Refers to ending therapy either temporarily or permanently<br />
Indications<br />
• When indications for CRRT are no longer present<br />
• When return pressures are elevated associated with filter clotting<br />
• When alarms are indicating poor clearance<br />
• For procedures in theatre or CT 21
Procedure<br />
1. Observe standard precautions and aseptic technique. Use sterile gloves<br />
when disconnecting lines from the Vascath.<br />
2. Press 'stop' and choose to ‘end treatment’. The PRISMA will then prompt<br />
you to return blood to the patient after providing the following:<br />
• Attach a secondary giving set to 500mL bag of normal saline, add<br />
three-way tap to the end of this line and prime.<br />
• Connect the red ‘access’ line of the PRISMA circuit to the three-way<br />
tap, using aseptic technique.<br />
• Return blood by following on screen prompts<br />
• Remove circuit as per onscreen prompts.<br />
3. Flush each lumen of the Vascath with 10mL normal saline.<br />
4. Heparin Lock as per protocol<br />
NB: If only a temporary disconnection and filter is still viable then connect<br />
both lines to a three-way tap. Circuit can then be reconnected to patient as<br />
normal when recommencing therapy. 21
Self Test 6<br />
Q1. What factors need to be manipulated in order to optimise clearance?<br />
Q2. Describe methods of optimising clearance.<br />
Q3. List four factors that can prolong filter life.<br />
Q4. When would anticoagulation NOT be used?<br />
Q5. What are the indications for terminating therapy?
Common Alarms & Troubleshooting<br />
There are various alarms that occur on both CRRT machines available in<br />
<strong>Liverpool</strong> ICU. The most common are discussed. Troubleshooting options are<br />
available in operator’s manual and instruction cards attached to each<br />
machine. On screen prompts are also issued when alarms are triggered.<br />
Access Pressure High<br />
Possible Triggers include:<br />
• Red clamps closed<br />
• Blocked or kinked vascath secondary to clot or position<br />
• Blocked or kinked access line<br />
• High blood flow rate<br />
• High airway pressures<br />
• Patient coughing 9,13<br />
Return Pressure High<br />
Possible Triggers include:<br />
• Blue clamps closed<br />
• Blocked or kinked vascath secondary to clot or position<br />
• Blocked or kinked return line<br />
• High airway pressures<br />
• Filter Clotting/Clotted 9,13<br />
Treatment obviously involves correcting the above problems. Where<br />
filter clotting is a possibility blood should be returned ASAP<br />
Access or Return Disconnect<br />
Triggered by low pressure in either of the lines. May indicate disconnection<br />
somewhere in the circuit. Check that all lines are connected securely.<br />
Air in Blood<br />
Possible Triggers include:<br />
• Fluid level in bubble trap below sensor<br />
• Air in circuit<br />
• Incomplete priming<br />
• Return line not installed in Air detector<br />
• Dirty sensor<br />
• Leaking connection 9,13<br />
NB: This alarm must not be bypassed. It is a protective mechanism<br />
against the possibility of air embolism. Do not override until<br />
troubleshooting procedures in operator’s manuals have been fully<br />
followed. 9,13
There are many alarms that may be triggered during CRRT. If in doubt follow<br />
the on screen prompts or refer to the operator’s manual for guidance. Most<br />
alarms that occur will be related to the following:<br />
• Vascath obstruction due to position of patient<br />
• Access or return lines kinking or clotting<br />
• Bag placement on scales is incorrect<br />
• Clotting of the filter/circuit<br />
• Poorly placed blood leak detector<br />
• Air in the circuit<br />
• Periodic self test failure 9,13<br />
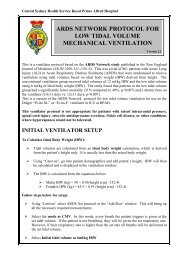
Diaphragm Reposition Procedure<br />
Performed if pod is accidentally<br />
removed or machine alarms<br />
indicating problem<br />
-ve Pods (Access & Effluent)<br />
• Stop Pump<br />
• Clamp line above & below<br />
pod<br />
• Remove pod & clean port<br />
• Inject maximum of 1cc<br />
normal saline into pod using<br />
20 g needle<br />
• Reinstall pod<br />
• Resume therapy<br />
+ve Pods (Filter & Return)<br />
• Same as above<br />
• Aspirate maximum of 1cc<br />
13<br />
13
Summary of Nursing Care for the Patient on CRRT<br />
• <strong>Continuous</strong> monitoring of haemodynamic parameters<br />
• Pressure area care and hygiene needs<br />
• Optimise blood pressure prior to commencing therapy<br />
• Colloid and Metaraminol precautions when running patient on<br />
• When anticoagulation is running an initial APTT should be checked 4<br />
hours after commencing therapy. 6 hourly APTT is attended thereafter<br />
and heparin infusion titrated according to protocol<br />
• Electrolytes, urea and creatine (EUC) and calcium, magnesium and<br />
phosphate (CMP) should be checked 2 hours after commencing<br />
therapy. 6 hourly EUC/CMP thereafter. Where electrolytes need<br />
replacing, do so in accordance with ICU electrolyte protocols.<br />
• Strict monitoring of fluid balance to prevent excessive fluid losses<br />
when removing fluid- this should monitored hourly and documented<br />
on CRRT observation chart to prevent incorrect fluid removal<br />
secondary to scale malfunction.<br />
• Attend CRRT observation chart monitoring pressures in particular<br />
that may warn of filter clotting or access problems<br />
• Monitor Vascath site for signs of infection. Clean and dress as<br />
required as earlier described.<br />
• Monitor patient’s temperature and actively warm using a bear hugger<br />
blanket if necessary<br />
• Maintain standard precautions and aseptic technique when priming,<br />
connecting, disconnecting the circuit. This also applies when<br />
changing fluids or disposing of ultrafiltrate<br />
• As with all intensive care patients the MFASTHUG pneumonic should<br />
be followed- i.e. Mouth care, Feeding, Analgaesia, Sedation,<br />
Thromboembolism prophylaxis, Elevated bed head, Stress ulcer<br />
prophylaxis and Glucose control + Gut- aperients etc 2,5,8,17,20
Self Test 7<br />
Q1. List the common triggers for alarms on the CRRT machines.<br />
Q2. How would you reposition the diaphragms on both positive and<br />
negative pressure pods when required?<br />
Q3. What nursing care is necessary for the patient undergoing CRRT?
Answers<br />
Self Test1<br />
Q1. State the primary and secondary functions of the kidneys.<br />
The primary role of the kidneys is to remove metabolic wastes and maintain<br />
fluid and electrolyte balance. The kidneys also have a role in Blood Pressure<br />
Control, Red Blood Cell Synthesis, Bone Metabolism and Acid- Base<br />
Balance.<br />
Q2. Name the functional units of the Kidneys and list their<br />
components.<br />
The functional units of the kidneys are known as nephrons. The nephron<br />
consists of a Glomerulus, Bowman Capsule, Proximal Convoluted Tubule,<br />
Loop of Henle, Distal Convoluted Tubule and Collecting Duct.<br />
Or<br />
Glomerulus, tubule and collecting duct.<br />
Q3. Discuss the processes involved in urine formation<br />
Three process involved in urine formation include Glomerular Filtration,<br />
Tubular Reabsorption and Tubular Secretion. Glomerular filtration occurs<br />
as blood passes through the glomerulus being filtered of fluid and solutes.<br />
Tubular reabsorption and secretion occurs progressively through the areas<br />
of the tubule. Fluid, electrolytes and waste products are excreted as filtrate<br />
depending on the body’s requirements.<br />
Self Test2<br />
Q1. Define Acute <strong>Renal</strong> Failure<br />
Acute renal failure (ARF) is a clinical syndrome, characterised by an abrupt<br />
decline in glomerular filtration rate (GFR). There is a subsequent retention of<br />
metabolic waste products and an inability to maintain electrolyte and acidbase<br />
homeostasis. Regulation of fluid volume is also affected.<br />
Q2. Describe 3 forms of acute renal failure and the associated causes<br />
Prerenal ARF is largely related to systemic factors that limit blood flow and<br />
reduce glomerular filtration rate. Related causes may include hypotension,<br />
hypovolaemic shock, cardiogenic shock, septic shock and thrombosis that<br />
results in bilateral renal vascular obstruction.<br />
Intrarenal ARF is the result of damage sustained at the site of the nephrons.<br />
This could be secondary to a number of conditions or nephrotoxins<br />
including: Acute tubular necrosis, acute glomerulonephritis, acute cortical<br />
necrosis, malignant hypertension, acute vasculitis, rhabdomyolysis, IV<br />
contrast and aminoglycosides.
Post renal ARF occurs secondary to obstruction that prevents excretion of<br />
urine. This may relate to prostatic hypertrophy, renal calculi, tumour or<br />
blocked urinary catheter.<br />
Q3. List the signs and symptoms of acute renal failure<br />
• Fluid and electrolyte abnormalities<br />
• Metabolic acidosis<br />
• Anaemia<br />
• Pruritis secondary to uremic frost<br />
• Nausea & vomiting<br />
• Confusion<br />
• ↓LOC<br />
• Congestive heart failure resulting in acute pulmonary oedema<br />
Self Test 3<br />
Q1. What is renal replacement therapy?<br />
<strong>Renal</strong> replacement therapy (RRT) is an extracorporeal technique of blood<br />
purification. Blood passes over a semipermeable membrane (filter) allowing<br />
solutes and water to cross over to a collection side. There are various<br />
modalities included under the umbrella of RRT.<br />
Q2. List advantages and disadvantages of continuous modalities<br />
compared to other forms of RRT<br />
Advantages:<br />
• Better for haemodynamic instability<br />
• Readily accessible<br />
• Effective fluid removal and clearance of solutes<br />
• Can be performed by ICU staff rather than specialised renal nurses<br />
Disadvantages:<br />
• Patient mobilisation is limited<br />
• Access complications<br />
• Anticoagulation<br />
• Reduced blood flow rates secondary to small filters when compared to<br />
IHD<br />
Q3. List Indications for CRRT<br />
• Fluid Overload, pulmonary oedema<br />
• Worsening Metabolic Acidosis<br />
• Hyperkalaemia<br />
• Worsening Azotaemia<br />
• Drug overdoses<br />
• Removal of toxins
Q4. Describe the basic principles of fluid and solute removal involved in<br />
CRRT.<br />
Diffusion involves the movement of small and middle molecule solutes from<br />
an area of high concentration to low concentration across a semipermeablemembrane.<br />
Convection occurs with water flow across a semi-permeable<br />
membrane by hydrostatic pressure that drags solutes with it (the way a<br />
waterfall moves pebbles and sand). Ultrafiltration is the movement of fluid<br />
and solutes across a semipermeable membrane secondary to convection or<br />
hydrostatic pressure. Positive pressure pushes the fluid across where<br />
negative pressure pulls the fluid across. The force that pushes fluid and<br />
solutes across the membrane is known as hydrostatic pressure. The<br />
mechanical blood pump on the dialysis machine creates this.<br />
Q5. Describe the different modes of CRRT.<br />
Slow <strong>Continuous</strong> Ultrafiltration utilises convection and ultrafiltration to<br />
remove fluid. It is indicated for fluid overload. SCUF does not require<br />
dialysate or replacement fluids.<br />
<strong>Continuous</strong> Venovenous Haemofiltration incorporates convection and<br />
ultrafiltration to remove fluid and moderate solutes. <strong>Replacement</strong> fluid is<br />
used. This modality is indicated for moderate electrolyte imbalances, oliguria<br />
whilst receiving TPN or blood and for patients in septic shock.<br />
<strong>Continuous</strong> Venovenous Haemodialysis filters via diffusion. Fluid is removed<br />
together with more aggressive solute removal. <strong>Replacement</strong> fluid is not used.<br />
CVVHD is warranted for fluid overload with haemodynamic instability,<br />
Azotaemia, electrolyte disturbances and acidosis.<br />
<strong>Continuous</strong> Venovenous Haemodiafiltration uses both diffusive and<br />
convective processes. Both replacement and dialysate solutions are used for<br />
maximum fluid and solute removal. This mode of CRRT is indicated for fluid<br />
overload, pulmonary oedema, worsening metabolic acidosis, hyperkalaemia<br />
worsening Azotaemia, drug overdoses and removal of toxins<br />
Self Test 4<br />
Q1. What is the importance of adequate access?<br />
Good access that allows high flow rates through the circuit is one of the key<br />
aspects in CRRT that effects blood flow, clearance and filter life.<br />
Q2. State the appropriate name and functions of the red and blue<br />
lumens on a vascath<br />
The red lumen is the arterial port also known as the access port. This lumen<br />
supplies blood from the patient to the filter. The blue lumen is the venous
port also known as the return port. Blood is returned via this lumen from<br />
the filter to the patient.<br />
Q3. What are the three possible sites for vascath insertion? State the<br />
advantages and disadvantages of each.<br />
Internal Jugular Vein<br />
Advantages:<br />
• Allows for patient mobility<br />
• Easy to visualise insertion site<br />
Disadvantages:<br />
• Requires Chest Xray prior to use<br />
• Kinking can occur when the patient moves their head<br />
• Sometimes attains insubstantial blood flows secondary to variations<br />
in central filling and intrathoracic pressures. Positive pressure<br />
ventilation can make this more apparent.<br />
Femoral Vein<br />
Advantages:<br />
• Easily accessible by most clinicians<br />
• May allow greater blood flows<br />
Disadvantages:<br />
• Prone to kinking, more so in the obese patient<br />
• Does not allow for patient mobility<br />
• Difficult to visualise and dress insertion site<br />
• Higher incidence of infection secondary to the proximity to intestinal<br />
flora.<br />
Subclavian Vein<br />
Advantages:<br />
• Allows for patient mobility<br />
• Easy to visualise and dress insertion site<br />
Disadvantages:<br />
• Requires Chest Xray prior to use<br />
• Risk of pneumothorax on insertion<br />
• Risk of subclavian stenosis, which can impair suitability for an A-V<br />
fistula on the affected side, if renal failure becomes chronic.<br />
• Sometimes attains insubstantial blood flows secondary to variations<br />
in central filling and intrathoracic pressures. Positive pressure<br />
ventilation can make this more apparent.<br />
Q4. How would you troubleshoot a vascath?<br />
Using aseptic technique, assess catheter patency by aspirating and flushing<br />
10ml of blood on the effected lumen to test resistance to blood flow. Further,<br />
flush 10ml 0.9% sterile normal saline. Where resistance is present, a clot
may be obstructing the catheter, but more likely it is positioned against the<br />
vessel wall. Slightly withdrawing or rotating the catheter may overcome this<br />
problem. Where this fails to resolve the problem the catheter must be<br />
changed. The lumens may be swapped, however this is only a temporary<br />
measure as there is a loss in clearance.<br />
Q5. How would you heparin lock a vascath?<br />
• Apply standard precautions and utilise aseptic technique<br />
• Using 3 ampoules of 5000 units heparin in 1ml (15000 units/3ml)<br />
inject the stated amount (located on each port) of this solution into<br />
the Vas Cath port. Label lumens as Heparin Locked<br />
Self Test 5<br />
Q1. What is the purpose of dialysate and replacement fluids?<br />
Dialysate fluid is used as a means to encourage diffusive clearance.<br />
<strong>Replacement</strong> fluid is a pre or post dilution fluid used to replace losses in<br />
ultrafiltrate.<br />
Q2. State the two fluids available at <strong>Liverpool</strong> ICU for CRRT, including<br />
the major difference and the preparations required.<br />
GAMBRO is the fluid that contains lactate as its buffer. HEMOSOL is<br />
considered lactate free and thus requires the addition of bicarbonate prior to<br />
use. This is accomplished by breaking the seal within the bag to mix the<br />
solutions together. Both GAMBRO and HEMOSOL solutions require addition<br />
of KCL when used as dialysate. 15mmol K + is added to 5L of GAMBRO.<br />
20mmol K + is added to 5L of HEMOSOL. Both make a final concentration of<br />
4mmol K + /L. KCL is added to these fluids to reduce loss K + of through<br />
diffusion.<br />
Q3. How do you prepare the vascath prior to commencing CRRT with a<br />
new circuit?<br />
Once the circuit is primed and ready to connect, 5ml of blood should be<br />
aspirated and discarded to remove heparin from the line. Assess catheter<br />
patency by aspirating and flushing 10ml of blood on the effected lumen to<br />
test resistance to blood flow. Further, flush 10ml 0.9% sterile normal saline.<br />
Q4. List the safety aspects of connecting and commencing therapy.<br />
• CRRT Machine should be plugged into an isolated power socket<br />
• When commencing therapy, colloid on a pump giving set should be<br />
connected to patient’s intravenous access<br />
• 10mg Metaraminol (Aramine) should be drawn up and readily<br />
available. This in conjunction with colloid is precautionary, should<br />
the patient become hypotensive. Inotropes can be titrated for control<br />
of hypotension, if the patient is on them rather than utilising<br />
Aramine.
Q5. Differentiate pre dilution from post dilution including benefits and<br />
disadvantages.<br />
Pre-dilution involves administering replacement fluid prior to the filter. This<br />
thereby reduces the viscosity of blood and hematocrit and in effect may aid<br />
in preventing filter clotting. Unfortunately this method also dilutes the<br />
concentration of solute in plasma, which can negatively impact on clearance<br />
by reducing the diffusion gradient. In order to optimise clearance of solutes,<br />
replacement rate must be increased in order to increase the rate of<br />
ultrafiltration.<br />
Post-dilution therefore involves administering replacement fluid after the<br />
filter. This does not dilute solutes in plasma, however the ability for optimal<br />
clearance is lost when blood viscosity is not reduced and high flow rates are<br />
then difficult to achieve. With reduced blood flow comes reduced<br />
ultrafiltration. Utilising filters with larger surface areas in conjunction with<br />
this method may improve clearance.<br />
Q6. List the complications of CRRT.<br />
• Hypotension that may result from aggressive fluid removal<br />
• Electrolyte imbalances<br />
• Cardiac Arrhythmias<br />
• Anaemia secondary to haemolysis of red blood cells<br />
• Thrombocytopaenia secondary to platelet aggregation in filter<br />
• Hypothermia secondary to extracorporeal blood circulation<br />
• Coagulopathy secondary to over heparinisation<br />
• Infection<br />
• Heparin induced thrombocytopaenia<br />
Self Test 6<br />
Q1. What factors need to be manipulated in order to optimise<br />
clearance?<br />
Regardless of which CRRT machine is being used, optimising clearance is<br />
dependant on two factors. These include improving diffusion and<br />
convection/ultrafiltration.<br />
Q2. Describe methods of optimising clearance.<br />
Using filters with larger surface areas and appropriate dialysate fluid can<br />
optimise diffusive clearance. Improving clearance via<br />
convection/ultrafiltration is largely accomplished through high flow rates<br />
(Dialysate, <strong>Replacement</strong>, Ultrafiltration & Blood Pump). Pre dilution assists<br />
in achieving higher flow rates by reducing the viscosity of blood and<br />
hematocrit. Location and care of the vascath is also shown to influence flow<br />
considerably.
Q3. List four factors that can prolong filter life.<br />
• High blood flow rates<br />
• Pre dilution and warming of fluid<br />
• Adequate Access<br />
• Anticoagulation<br />
Q4. When would anticoagulation NOT be used?<br />
Anticoagulation is not used if the patient is coagulopathic. A heparin bolus<br />
is not given if the patient has had CRRT within the last 4 hours.<br />
Q5. What are the indications for terminating therapy?<br />
• When indications for CRRT are no longer present<br />
• When return pressures are elevated associated with filter clotting<br />
• When alarms are indicating poor clearance<br />
• For procedures in theatre or CT<br />
Self Test 7<br />
Q1. List the common triggers for alarms on the CRRT machines.<br />
• Vascath obstruction due to position of patient<br />
• Access or return lines kinking or clotting<br />
• Bag placement on scales is incorrect<br />
• Clotting of the filter/circuit<br />
• Poorly placed blood leak detector<br />
• Air in the circuit<br />
• Periodic self test failure<br />
Q2. How would you reposition the diaphragms on both positive and<br />
negative pressure pods when required?<br />
If the pump has not stopped with an alarm, it should first be stopped. Apply<br />
clamps above and below the affected pod. Remove the pod and clean the<br />
port. If the pod is negative (Access & Effluent), inject a maximum of 1cc<br />
normal saline using a 20g needle into the pod. Conversely, if the pod is<br />
positive then a maximum of 1cc should be aspirated from the pod. Following<br />
this step the pod can be reinstalled into the appropriate port and therapy<br />
resumed.<br />
Q3. What nursing care is necessary for the patient undergoing CRRT?<br />
• <strong>Continuous</strong> monitoring of haemodynamic parameters<br />
• Pressure area care and hygiene needs<br />
• Optimise blood pressure prior to commencing therapy
• Colloid and Metaraminol precautions when running patient on<br />
• When anticoagulation is running an initial APTT should be checked 4<br />
hours after commencing therapy. 6 hourly APTT is attended thereafter<br />
and heparin infusion titrated according to protocol<br />
• Electrolytes, urea and creatine (EUC) and calcium, magnesium and<br />
phosphate (CMP) should be checked 2 hours after commencing<br />
therapy. 6 hourly EUC/CMP thereafter. Where electrolytes need<br />
replacing, do so in accordance with ICU electrolyte protocols.<br />
• Strict monitoring of fluid balance to prevent excessive fluid losses<br />
when removing fluid- this should monitored hourly and documented<br />
on CRRT observation chart to prevent incorrect fluid removal<br />
secondary to scale malfunction.<br />
• Attend CRRT observation chart monitoring pressures in particular<br />
that may warn of filter clotting or access problems<br />
• Monitor Vascath site for signs of infection. Clean and dress as<br />
required as earlier described.<br />
• Monitor patient’s temperature and actively warm using a bear hugger<br />
blanket if necessary<br />
• Maintain standard precautions and aseptic technique when priming,<br />
connecting, disconnecting the circuit. This also applies when<br />
changing fluids or disposing of ultrafiltrate<br />
• As with all intensive care patients the MFASTHUG pneumonic should<br />
be followed- i.e. Mouth care, Feeding, Analgaesia, Sedation,<br />
Thromboembolism prophylaxis, Elevated bed head, Stress ulcer<br />
prophylaxis and Glucose control + Gut- aperients etc
References<br />
1. Agraharkar, M., Gupta, R., Agraharkar, A., & Workeneh, B.T. (2006).<br />
Acute renal failure, [Online]. Available:<br />
http://www.emedicine.com/med/topic1595.htm [2006,<br />
September 13].<br />
2. Astle, S. (2001). A new direction for dialysis. RN. 64(7), 56-60, 62<br />
3. Baldwin, I., Bridge, N., Elderkin, T. (1998). Nursing issues, practices<br />
and perspectives for the management of continuous renal<br />
replacement therapy in the intensive care unit. In Bonett, J.,<br />
Hattley, S., & Bastick, M. <strong>Continuous</strong> renal replacement<br />
information package. A quick guide to CRRT. (pp1-41) Gosford:<br />
NSCCH.<br />
4. Bellomo, R., Baldwin, I., Ronco, C. (2001). Atlas of haemofiltration. In<br />
Bonett, J., Hattley, S., & Bastick, M. <strong>Continuous</strong> renal replacement<br />
information package. A quick guide to CRRT. (pp1-41) Gosford:<br />
NSCCH.<br />
5. Bonett, J., Hattley, S., & Bastick, M. (2005). <strong>Continuous</strong> renal<br />
replacement information package. A quick guide to CRRT. (pp1-<br />
41) Gosford: NSCCH.<br />
6. Brunet, S., Leblanc, M., Geadah, M., Parent, D., Courteau, S., &<br />
Cardinal, J. (1999). Diffusive and convective solute clearances<br />
during continuous renal replacement therapy at various<br />
dialysate and ultrafiltration flow rates. Am J Kidney Dis. 34,<br />
486-492.<br />
7. Cannon, J.D. (2004). Recognizing chronic renal failure…the sooner<br />
the better. Nursing, 2004, 34(1), 50-53.<br />
8. Campbell, D. (2003). How acute renal failure puts the brakes on<br />
kidney function. Nursing 2003. 33(1), 59-64.<br />
9. Castro, P., & Shunker, S. (No date). <strong>Continuous</strong> renal replacement<br />
therapy. Workshop handout. <strong>Liverpool</strong>: LHS.<br />
10. Crawley, T. Shunker, S. & Edgtton-Winn, M. (2004). Heparin sodium.<br />
ICU protocol. <strong>Liverpool</strong>: LHS.
11. Glann, J.K. (2002). <strong>Renal</strong> disorders and therapeutic management. In<br />
Urden, L.D., Stacy K.M., Lough, M.E. (Eds). Thelan’s critical<br />
care nursing- diagnosis and management. (pp745-777). St<br />
louis: Mosby.<br />
12. Henke, K. (2003). <strong>Renal</strong> physiology. Dimensions of Critical Care<br />
Nursing 22(3), 125-132.<br />
13. Hospal. (2000). Prisma system operator’s manual, Gambro Dasco<br />
14. Hospal. (No date) <strong>Renal</strong> intensive care- PRISMA. Filter instruction<br />
Guide, Gambro.<br />
15. Hospal (No date). AN69ST membrane- the bioactive membrane<br />
[Online]. Available: http://193.15.174.148/index.html.<br />
16. Kaplan, A.A. (2003). <strong>Renal</strong> failure. In F.S. Bongard, & D.Y. Sue.<br />
Current critical care diagnosis & treatment (2 nd Ed.). [Online].<br />
Available:<br />
http://online.statref.com/TOC/TOC.aspx?FxId=5&SessionId=7<br />
A4937EMGZBYBIEJ<br />
17. Kaplow, R., & Barry, R. (2002). <strong>Continuous</strong> renal replacement<br />
therapies: a more gentle blood filtering technique allows for<br />
fewer complications. American Journal of Nursing. 102(11), 26-<br />
33.<br />
18. Lameire, N., Van Biesen, W., & Vanholder, R. (2005). Acute renal<br />
failure. The Lancet. 365(9457), 417.<br />
19. Medtel. (No date). Kimal- <strong>Continuous</strong> renal replacement therapy<br />
workbook. In Bonett, J., Hattley, S., & Bastick, M. <strong>Continuous</strong><br />
renal replacement information package. A quick guide to CRRT.<br />
(pp1-41) Gosford: NSCCH.<br />
20. Paton, M. (2003). <strong>Continuous</strong> renal replacement therapy: slow but<br />
steady. Nursing 2003. 33(6), 48-50<br />
21. Sommer, N., Edgtton-Winn, M., & Shunker, S. (2004). <strong>Continuous</strong><br />
renal replacement therapy (CRRT) using the prisma machine.<br />
ICU protocol. <strong>Liverpool</strong>: LHS
22. Toltec International. (2006). How haemodialysis works. [online]<br />
Available: http://www.toltec.biz/how_hemodialysis_works.htm<br />
(December, 2006).<br />
23. Ward, K. (2005). Kidneys don’t fail me now. Nursing Made Incredibly<br />
Easy. 3(2), 18-26<br />
24. Zabat, E. (2003), When your patient needs peritoneal dialysis. Nursing 2003,<br />
33(8), 52-54.
Appendix