Annual Report - Brown University
Annual Report - Brown University
Annual Report - Brown University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
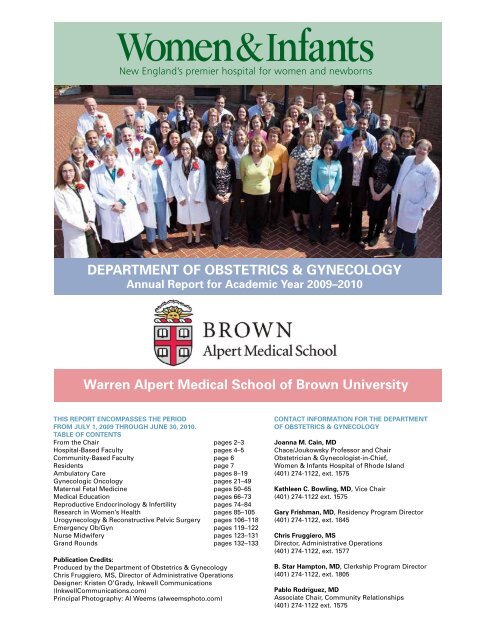
DEPARTMENT OF OBSTETRICS & GYNECOLOGY<br />
<strong>Annual</strong> <strong>Report</strong> for Academic Year 2009–2010<br />
Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong><br />
THIS REPORT ENCOMPASSES THE PERIOD<br />
FROM JULY 1, 2009 THROUGH JUNE 30, 2010.<br />
TABLE OF CONTENTS<br />
From the Chair pages 2–3<br />
Hospital-Based Faculty pages 4–5<br />
Community-Based Faculty page 6<br />
Residents page 7<br />
Ambulatory Care pages 8–19<br />
Gynecologic Oncology pages 21–49<br />
Maternal Fetal Medicine pages 50–65<br />
Medical Education pages 66–73<br />
Reproductive Endocrinology & Infertility pages 74–84<br />
Research in Women’s Health pages 85–105<br />
Urogynecology & Reconstructive Pelvic Surgery pages 106–118<br />
Emergency Ob/Gyn pages 119–122<br />
Nurse Midwifery pages 123–131<br />
Grand Rounds pages 132–133<br />
Publication Credits:<br />
Produced by the Department of Obstetrics & Gynecology<br />
Chris Fruggiero, MS, Director of Administrative Operations<br />
Designer: Kristen O’Grady, Inkwell Communications<br />
(InkwellCommunications.com)<br />
Principal Photography: Al Weems (alweemsphoto.com)<br />
CONTACT INFORMATION FOR THE DEPARTMENT<br />
OF OBSTETRICS & GYNECOLOGY<br />
Joanna M. Cain, MD<br />
Chace/Joukowsky Professor and Chair<br />
Obstetrician & Gynecologist-in-Chief,<br />
Women & Infants Hospital of Rhode Island<br />
(401) 274-1122, ext. 1575<br />
Kathleen C. Bowling, MD, Vice Chair<br />
(401) 274-1122 ext. 1575<br />
Gary Frishman, MD, Residency Program Director<br />
(401) 274-1122, ext. 1845<br />
Chris Fruggiero, MS<br />
Director, Administrative Operations<br />
(401) 274-1122, ext. 1577<br />
B. Star Hampton, MD, Clerkship Program Director<br />
(401) 274-1122, ext. 1805<br />
Pablo Rodriguez, MD<br />
Associate Chair, Community Relationships<br />
(401) 274-1122 ext. 1575
2<br />
NOTE FROM THE CHAIR<br />
I grew up in the pioneering tradition of Western Universities—large, land-grant<br />
based that have as their mission advancing the welfare of the citizens of the<br />
state. It is interesting to now live in the smallest state and be part of a very<br />
special but also private <strong>University</strong>—<strong>Brown</strong>—and perhaps an even more special<br />
institution, a true Women & Infants hospital. Yet, even though private, the mis-<br />
sion of the Alpert School of Medicine and that of WIH is focused on the welfare<br />
of the citizens of the state of RI and southern New England in often more ways<br />
than those Universities dedicated to their state, but also ways that transcend<br />
these borders to touch lives throughout the world in as robust a calling to serve<br />
as formed the Western Universities.<br />
The ESCHUCHE grant—a grant to provide a “curriculum” in health literacy<br />
through the vehicle of Latino Public Radio will not only provide guidance and<br />
education for women and families in RI, but also provide a template for the<br />
entire nation. The work done in MFM to understand H1N1, prematurity, or Ma-<br />
ternal Fetal Medicine Units Network based research helps the large volume of<br />
women served here—and also far beyond. The development of the Center for<br />
Biomarkers and Emerging Technology in Women’s Cancers along with the in-<br />
creasing prominence of the Women’s Cancers’ group as Gynecologic Oncology<br />
Group (GOG) leaders again touches women in the region and far beyond. The<br />
research in Reproductive Endocrinology may provide options for women with<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
cancer to keep their fertility, an option that never existed. Clearly every division<br />
of the Department of Obstetrics and Gynecology is providing care and research<br />
that will improve the lives of women and girls—you only have to read a little<br />
about each to understand that.<br />
Keeping focus on the spiraling benefits of research and education for women<br />
and for the future at a time of great turmoil and competition for scarce re-<br />
sources in medicine will be the true task we face if we are to continue to meet<br />
the great calling to serve that has founded the Department , Women & Infants,<br />
and <strong>Brown</strong>. This will be the task that the generations now and in the future will<br />
have to face with creativity and fortitude. In some ways, we are forging a path<br />
in a new wilderness as broad and uncharted as the western migration and with<br />
as many pitfalls and potential threats. But the vistas and new territories that<br />
will open to us are unimaginable and beautiful beyond words, and the oppor-<br />
tunities to meet our calling in the new world of health care reform even more<br />
critical than ever. Forward ho!<br />
Joanna M. Cain, MD<br />
Chace/Joukowsky Professor and Chair<br />
Obstetrician & Gynecologist-in-Chief,<br />
Women & Infants Hospital of Rhode Island<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 3
ADMINISTRATIVE ROLES WITHIN THE DEPARTMENT<br />
Kathleen C. Bowling, MD<br />
Vice Chairperson,<br />
Department of Ob/Gyn<br />
4<br />
Pablo Rodriguez, MD<br />
Associate Chair,<br />
Community Relationships<br />
PROFESSOR<br />
Eli Adashi, MD<br />
John E. Buster, MD<br />
Joanna Cain, MD<br />
Stephen R. Carr, MD (7/1/2010)<br />
Sandra A. Carson, MD<br />
Donald R. Coustan, MD<br />
Susan Cu-Uvin, MD<br />
(joint appt w/Internal Medicine)<br />
Gary Frishman, MD<br />
Cornelius O. Granai, MD<br />
Deborah Myers, MD<br />
Dwight Rouse, MD<br />
Patrick J. Sweeney, MD, PhD<br />
Katharine Wenstrom, MD<br />
PROFESSOR (JOINT APPT)<br />
Francois I. Luks, MD<br />
(with Surgery & Pediatrics)<br />
Karen Rosene-Montella, MD<br />
(with Internal Medicine)<br />
Raymond O. Powrie, MD<br />
(with Internal Medicine)<br />
CLINICAL PROFESSOR<br />
Diane Angelini, EdD, CNM (7/1/2010)<br />
ASSOCIATE PROFESSOR<br />
Paul DiSilvestro, MD<br />
Richard Moore, MD<br />
Maureen Phipps, MD<br />
Charles Rardin, MD (7/1/2010)<br />
James O’Brien, MD<br />
Medical Director,<br />
Inpatient Obstetrics<br />
DEPARTMENT OF OBSTETRICS AND GYNECOLOGY<br />
HOSPITAL-BASED FACULTY JULY 1, 2009 – JUNE 30, 2010<br />
BROWN APPOINTMENTS<br />
ASSOCIATE PROFESSOR<br />
(CLINICAL)<br />
Robert Berry, MD (Pending)<br />
Robert Legare, MD<br />
ASSOCIATE PROFESSOR<br />
(JOINT APPT)<br />
Don Dizon, MD (7/1/2010)<br />
(with Internal Medicine)<br />
Lucia Larson, MD<br />
(with Internal Medicine)<br />
ASSOCIATE PROFESSOR<br />
(RESEARCH)<br />
Cynthia Rosengard, PhD<br />
CLINICAL ASSOCIATE PROFESSOR<br />
Andrew Blazar, MD<br />
Donna LaFontaine, MD (7/1/10)<br />
Carol Wheeler, MD<br />
ASSISTANT PROFESSOR<br />
Rebecca Allen, MD<br />
Brenna Anderson, MD<br />
Christina Bandera, MD<br />
Laurent Brard, MD<br />
Ed Chien, MD<br />
Sarah Fox, MD<br />
Vinita Goyal, MD<br />
Brittany Star Hampton, MD<br />
Kristen Matteson, MD<br />
Carolyn McCourt, MD<br />
Barbara O’Brien, MD<br />
Gary Wharton, MD<br />
Medical Director,<br />
Surgical Services<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
DEPARTMENT OF OBSTETRICS AND GYNECOLOGY<br />
HOSPITAL-BASED FACULTY JULY 1, 2009 – JUNE 30, 2010<br />
BROWN APPOINTMENTS<br />
ASSISTANT PROFESSOR<br />
(CONTINUED)<br />
Kelly Pagidas, MD<br />
Jared C. Robins, MD<br />
Katina Robison, MD<br />
Ashley Stuckey, MD (8/1/10)<br />
Vivian Sung, MD<br />
Trevor Tejada-Berges, MD<br />
ASSISTANT PROFESSOR<br />
(CLINICAL)<br />
Amy Gottlieb, MD<br />
Tanya Dailey, MD<br />
David Edmonson, MD (7/1/2010)<br />
Robin Gray-Puleo, MD<br />
Amy Snyder, MD<br />
ASSISTANT PROFESSOR<br />
(JOINT APPT)<br />
Margaret Miller, MD<br />
(with Internal Medicine)<br />
CLINICAL ASSISTANT PROFESSOR<br />
Balasubramanian Bhagavath, MD<br />
Cassandra Carberry, MD<br />
Matthew Esposito, MD<br />
Alfredo Gil, MD<br />
Elisabeth Howard, PhD, CNM<br />
Linda A. Hunter, EdD, CNM<br />
James J. O’Brien, MD<br />
Michael J. Paglia, MD<br />
Martha Pizzarello, MD<br />
Beth Plante, MD<br />
Brenda Roy, MD, PhD<br />
Jeannine Witmyer, PhD<br />
CLINICAL ASSISTANT PROFESSOR<br />
(JOINT)<br />
Jennifer S. Gass, MD (with Surgery)<br />
SENIOR TEACHING ASSOCIATE<br />
Anne Cooper, RPN, MS<br />
Edie McConaughey, MSN, CNM<br />
Linda Moulton, RNP, MS (10/1/2010)<br />
Patricia O’Connell, RNC<br />
Janet Singer, MSN, CNM (10/1/2010)<br />
Linda Steinhardt, MS, CNM<br />
Ann Stulik, NP (10/1/2010)<br />
TEACHING ASSOCIATE<br />
Erin Dobson, RNP<br />
Julie Slocum Daley, RN<br />
INSTRUCTOR (CLINICAL)<br />
Moune Jabre-Raughley, MD<br />
Roxanne Vrees, MD<br />
Emily White, MD<br />
CLINICAL INSTRUCTOR<br />
Bachir Sakr, MD<br />
Joanna Schwartz, PhD<br />
ASSISTANT INSTRUCTOR<br />
Aine Clements, MD<br />
Agatha Critchfield, MD<br />
Beth Cronin, MD<br />
Jennifer Kang, MD<br />
Nicole Korbly, MD<br />
Katherine Melzer, MD<br />
Laura Richio, MD<br />
TEACHING FELLOW<br />
Julie Johnson, MD<br />
Nada Kawar, MD<br />
Shannon MacLaughlan, MD<br />
Peter Klatsky, MD<br />
Katrin Kristijandoittir, MD<br />
Sonali Pandya, MD<br />
Matthew Rogalski, MD<br />
Nicole Sprawka, MD<br />
Roman Starikov<br />
Ashley Stuckey, MD<br />
Wendy Vitek, MD<br />
Blair Washington, MD<br />
Kyle Wohlrab, MD<br />
RESEARCH FELLOWS<br />
Stephan Krotz, MD<br />
FELLOWS GRADUATED 6/30/2010<br />
Julie Johnson, MD<br />
Ashley Stuckey, MD<br />
Kyle Wohlrab, MD<br />
RESEARCH ASSOCIATE<br />
Amy S. Cooper, CRN, MSN, RNC<br />
Christina Raker, ScD<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 5
DEPARTMENT OF OBSTETRICS AND GYNECOLOGY<br />
COMMUNITY-BASED JULY 1, 2009 – JUNE 30, 2010<br />
BROWN APPOINTMENTS<br />
6<br />
ASSOCIATE PROFESSOR<br />
Jennifer G. Clarke, MD<br />
Melissa Clarke, MD<br />
CLINICAL ASSOCIATE PROFESSOR<br />
Kathleen Bowling, MD<br />
Terrence Cahill, MD<br />
Wayne Clairborne, MD<br />
Steven Falkenberry, MD<br />
Kathleen Fitzgerald, MD<br />
Tawfik Hawwa, MD<br />
Nabil Khoury, MD (7/1/10)<br />
John Lathrop, MD (Emeritus)<br />
Henry Magendantz, MD<br />
Samir Moubayed, MD (Emeritus)<br />
Frank Pensa, MD<br />
Pablo Rodriguez, MD<br />
Reza Shah-Hosseini (Emeritus)<br />
Marguerite Vigliani, MD<br />
Robert Williams, MD<br />
CLINICAL ASSISTANT PROFESSOR<br />
M. David Beitle, MD<br />
John Bert, MD<br />
Lisa Boyle, MD<br />
Debra Brendel, MD<br />
Cheryl Brodsky, MD<br />
Fred A. Brosco, MD<br />
David Carcieri, MD<br />
Colleen Cavanaugh, MD<br />
Kue Chung Choi, MD<br />
Mauro Colavita, MD<br />
Jeannine Connolly, MD<br />
Joseph DeMartino, MD<br />
Mary C. DeRosa, MD<br />
John DiOrio, MD<br />
Lisa Domagalski, MD<br />
Renee R. Eger, MD<br />
Harris Galkin, MD<br />
Michele Gange, MD<br />
Howard Hall, MD (Emeritus)<br />
Cynthia Hanna, MD<br />
David Harrington, MD<br />
Jennifer Hosmer, MD<br />
Michelle L. Hughes, MD<br />
Marc Jaffe, MD<br />
AnnMarie Jurczak, MD<br />
Erica Klein, MD<br />
Stacey Lievense, MD<br />
Beth Marcaccio, MD<br />
Karen McGoldrick, MD<br />
Kathryn D. McGowan, MD<br />
Carroll Medeiros, MD<br />
John Murphy, MD (Emeritus)<br />
Laura Nevel, MD<br />
J. Douglas Nisbet, II, MD<br />
Maria O’Toole, MD<br />
Michael Pepi, MD<br />
Adrienne Perry, MD<br />
Marilyn Powers, DO<br />
Donald Ramos, MD<br />
Rebecca Randall, MD<br />
Robert Salk, DO<br />
Mark Scott, MD<br />
Jane Sharp, MD<br />
Santina Siena, MD<br />
Meera Simeos, MD<br />
Serena Sposato, MD<br />
Marshall Taylor, MD (Emeritus)<br />
Jacqueline Tetreault, MD<br />
Benjamin Vogel, MD<br />
W. Scott Walker, MD<br />
Gary Wharton, MD<br />
Doreen Wiggins, MD<br />
ASSISTANT PROFESSOR (CLINICAL)<br />
Robert Cohen, DO<br />
CLINICAL INSTRUCTOR<br />
Jennifer Boyle, MD<br />
Constance Brennan, MD<br />
Christine Brousseau, MD<br />
Dilek Cermik, MD<br />
Michael Coppa, MD (2/1/10)<br />
Rebecca Crichton, MD<br />
Suzanne Dambek, MD<br />
Kathryn Davis, MD<br />
Paula DeYoung, MD<br />
Beata DiZoglio, MD<br />
Debra Goldman, MD<br />
Anne Murray, MD<br />
Adelaide Nardone, MD<br />
Gretchen Paranya, MD<br />
Jessica Salak, MD (1/1/10)<br />
Alejandra Turmero, MD<br />
Anne Wold, MD<br />
INSTRUCTOR (ADJUNCT)<br />
Ali, M. F. Moustafa (7/1/2010)<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
BROWN UNIVERSITY/WOMEN & INFANTS HOSPITAL<br />
OF RHODE ISLAND<br />
OBSTETRICS AND GYNECOLOGY RESIDENTS<br />
PGY-1 (2008-2012) MEDICAL SCHOOL<br />
Catherine Albright Columbia <strong>University</strong> College of Physicians and Surgeons<br />
Kathaleen (Gravel) Barker <strong>University</strong> of Connecticut School of Medicine<br />
Lindsay Clark <strong>Brown</strong> Medical School<br />
Luu Doan <strong>University</strong> of California, Los Angeles, David Geffen School of Medicine<br />
Terri Febbraro Albert Einstein College of Medicine/Yeshiva <strong>University</strong><br />
Karen Gibbins Case Western Reserve <strong>University</strong> School of Medicine<br />
Kavita Mishra <strong>University</strong> of California, San Francisco SOM<br />
Dario Roque <strong>University</strong> of Florida School of Medicine<br />
PGY-2 (2007-2011) MEDICAL SCHOOL<br />
Elizabeth (Carlisle) Cappelletti Northwestern <strong>University</strong><br />
Jacquia Fenderson <strong>University</strong> of Rochester School of Medicine<br />
Melanie Greenman Duke <strong>University</strong> School of Medicine<br />
Megan McCoin <strong>University</strong> of Texas Medical School- San Antonio<br />
Jeannine Miranne Albany Medical College<br />
Kristina Mori Tufts <strong>University</strong> School of Medicine<br />
J. Pablo Orezzoli <strong>University</strong> of Buenos Aires School of Medicine<br />
PGY-3 (2006-2010) MEDICAL SCHOOL<br />
Archabald, Karen Yale <strong>University</strong> School of Medicine<br />
Baker, Julie State <strong>University</strong> of New York - Buffalo<br />
Carey, Molly <strong>University</strong> of Pennsylvania<br />
Holman, Laura <strong>University</strong> of Illinois<br />
Jackson, Amanda Medical <strong>University</strong> of South Carolina<br />
Kassis, Nadine Medical <strong>University</strong> of Ohio<br />
McDonnold, Mollie Baylor College of Medicine<br />
McMahon (Reynolds), Megan <strong>University</strong> of Massachusetts<br />
PGY-4 (2005-2009) MEDICAL SCHOOL<br />
Clements, Aine <strong>Brown</strong> Medical School<br />
Critchfield, Agatha <strong>University</strong> of Kentucky College of Medicine<br />
Cronin, Beth <strong>University</strong> of Vermont College of Medicine<br />
Kang, Jennifer <strong>University</strong> of Rochester School of Medicine<br />
Korbly, Nicole <strong>University</strong> of Massachusetts Medical School<br />
Melzer, Katherine State <strong>University</strong> of New York–Buffalo, School of Medicine<br />
Sacco, Laura <strong>University</strong> of Massachusetts Medical School<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 7
A m b u l a t o r y C a r e<br />
MISSION<br />
8<br />
DIVISION OF AMBULATORY CARE<br />
The Division of Ambulatory Care in the Women’s Primary Care Center (WPCC) is dedicated<br />
to the following goals:<br />
1. To provide high quality, comprehensive outpatient services to all women. We offer women’s<br />
Primary Care, Prenatal Care, and Gynecologic Care. In addition, specialty services are<br />
offered in the following areas: Colposcopy, Vulvar Disorders, Chronic Pelvic Pain, complete<br />
Family Planning, Urogynecology, Reproductive Endocrinology, Pediatric Gynecology,<br />
Substance Abuse Counseling and Treatment, Nutritional Counseling, Social Service,<br />
Ultrasound, and Fetal Evaluation.<br />
2. To educate medical students, residents, and other health profession students in women’s<br />
primary care, with emphasis on the screening, diagnosis, treatment, and follow–up of<br />
problems in the ambulatory setting.<br />
3. To conduct research in areas related to women’s primary care and reproductive health issues.<br />
4. To serve as a tertiary outpatient center for patients referred by other primary care providers<br />
for specialized assessment and treatment of substance abuse in pregnancy, cervical dysplasia,<br />
benign vulvar conditions, pediatric gynecology, urogynecology, reproductive endocrinology,<br />
contraception in women with complex medical problems, and chronic pelvic pain.<br />
FACULTY<br />
Patrick J. Sweeney, MD, PhD, Division Director<br />
BS: Loyola <strong>University</strong><br />
MD: St. Louis <strong>University</strong><br />
Residency: Temple <strong>University</strong><br />
MPH: <strong>University</strong> of California, Berkeley<br />
PhD: <strong>University</strong> of Mississippi<br />
Dr. Sweeney is a Professor of Obstetrics and Gynecology and the Director of<br />
the Division of Ambulatory Care with overall responsibility for the administra-<br />
tion of the WPCC. He joined the faculty in 1987 after having served for nine years as the Assistant<br />
Director of Ambulatory Care for the <strong>University</strong> of Tennessee College of Medicine. Early in 1995, Dr.<br />
Sweeney was appointed Associate Chair for the Department of Ob/Gyn, representing the depart-<br />
ment at academic functions when the chair is not available. In addition, he is an Associate Dean of<br />
Medicine for Continuing Medical Education for the <strong>Brown</strong> Medical School. Dr. Sweeney is an ac-<br />
tive member of the American College of Obstetricians and Gynecologists, having been appointed<br />
to several national committees in addition to serving two terms as Treasurer of District I. He is a<br />
reviewer for Obstetrics and Gynecology and serves as an Editorial Board Member for Medicine<br />
and Health - Rhode Island. On April 30, 2010, Dr. Sweeney stepped down to assume the role of<br />
Designated Institutional Official and CME Director at Women & Infants Hospital.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Robert E. Berry, Jr, MD, Incoming Division Director<br />
BA: Williams College<br />
MD: <strong>University</strong> of Virginia School of Medicine<br />
Residency: Tufts <strong>University</strong> Affiliated Hospitals<br />
Dr. Berry is a Clinical Associate Professor of Obstetrics and Gynecology and<br />
the new Director of the Division of Ambulatory Care effective May 1, 2010,<br />
with overall responsibility for the administration of the WPCC. He joined the<br />
faculty in 2010 after having been at the <strong>University</strong> of Massachusetts Medical<br />
School and UMass Memorial hospitals for ten years. He served there as the residency program<br />
director among other capacities. He began his career at Tufts New England Medical Center<br />
where he was a member of the Generalist Division and he served as the clerkship director. His<br />
professional interests include medical education, technology and patient care, and medical<br />
professionalism.<br />
Rebecca H. Allen, MD, MPH<br />
BA: Wesleyan <strong>University</strong><br />
MD: College of Physicians and Surgeons, Columbia <strong>University</strong><br />
MPH: Mailman School of Public Health, Columbia <strong>University</strong><br />
Residency: Brigham and Women’s Hospital/Massachusetts General Hospital,<br />
Harvard <strong>University</strong><br />
Fellowship: Brigham and Women’s Hospital, Harvard <strong>University</strong><br />
Dr. Allen is an Assistant Professor of Obstetrics and Gynecology and Director of Family Plan-<br />
ning for the Women’s Primary Care Center. After completing a fellowship in Family Planning,<br />
she joined the Division of Ambulatory Care in 2007. Dr Allen directs the Department’s Repro-<br />
ductive Health Rotation and the Core Curriculum series in General Gynecology. Since joining<br />
the division her roles have included supervising medical students, residents and nurse prac-<br />
titioners in the WPCC, including the Colposcopy Clinic and Contraception Consult Clinic. She<br />
also coordinates the Rhode Island Hospital Internal Medicine Residency Program Subspecialty<br />
Rotation in Gynecology at the WPCC.<br />
Sarah D. Fox, MD<br />
BS: <strong>Brown</strong> <strong>University</strong><br />
MD: Robert Wood Johnson Medical School<br />
(<strong>University</strong> of Medicine and Dentistry of NJ)<br />
Residency: Allegheny <strong>University</strong>/Allegheny General Hospital<br />
Fellowship: St. George’s Hospital, <strong>University</strong> of London<br />
Dr. Fox is an Assistant Professor of Obstetrics and Gynecology. After completing a fellowship<br />
in Urogynecology and Pelvic Floor Reconstruction, she was in private practice in Rhode Island<br />
and a community-based faculty member at Women & Infants Hospital of Rhode Island for 4<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 9<br />
A m b u l a t o r y C a r e
A m b u l a t o r y C a r e<br />
years. Since joining the division, her roles have included supervising medical students, resi-<br />
dents and nurse practitioners in the Women’s Primary Care Center. She is director of the Col-<br />
poscopy Clinic and also directs a multidisciplinary Virtual Chronic Pelvic Pain clinic with spe-<br />
cialists from Anesthesia, Physiatry, Behavioral Health, Gastroenterology, and Physical Therapy.<br />
In 2004, she received a Kenneth J. Ryan Training Grant in Abortion and Family Planning from<br />
the Kenneth J. Ryan Program and established a family planning curriculum.<br />
10<br />
Amy S. Gottlieb, MD<br />
AB: Harvard <strong>University</strong><br />
MD: <strong>University</strong> of Chicago Pritzker School of Medicine<br />
General Internal Medicine Residency: <strong>Brown</strong> <strong>University</strong>/RI Hospital<br />
Dr. Gottlieb is an Assistant Professor of Medicine and Obstetrics and Gynecology<br />
(Clinical) and the Director of Primary Care Curricula and Consultation in the Women’s Primary<br />
Care Center. Dr. Gottlieb directs the Department’s Ambulatory Care Medicine Rotation and the<br />
Core Curriculum Series in Primary Care Internal Medicine. She also precepts medical students,<br />
residents, and nurse practitioners in the Women’s Primary Care Center and conducts a consul-<br />
tative Internal Medicine clinic. In addition to curriculum development, Dr. Gottlieb’s academic<br />
pursuits include educating health care professionals about violence against women and men-<br />
toring women in medicine. To this end, she is the Chairperson of the Women & Infants Hos-<br />
pital Domestic Violence Task Force, an appointed member of <strong>Brown</strong> Medical School’s Office<br />
of Women in Medicine and Science Advisory Board and its Medical Committee on Academic<br />
Standing, and is Co-Director of MomDocFamily, a nationwide mentoring organization of physi-<br />
cians who are mothers.<br />
Vinita Goyal, MD<br />
BA: <strong>University</strong> of Washington<br />
MD: <strong>University</strong> of Washington School of Medicine<br />
Residency: <strong>University</strong> of Texas Health Science Center at San Antonio<br />
MPH: <strong>University</strong> of North Carolina<br />
Fellowship: <strong>University</strong> of North Carolina<br />
Dr. Goyal is an Assistant Professor of Obstetrics and Gynecology for the Women’s Primary<br />
Care Center. After completing a fellowship in Women’s Health Research, she joined the Divi-<br />
sion of Ambulatory Care in 2009. Since joining the division her roles have included supervising<br />
medical students, residents and nurse practitioners in the WPCC, including the Colposcopy<br />
Clinic and Contraception Consult Clinic. She also directs the Gynecologic Consult Clinic at the<br />
WPCC.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
NURSE PRACTITIONERS<br />
Anne Stulik, MSN, WHCNP<br />
BSN: <strong>University</strong> of RI<br />
MSN: State <strong>University</strong> of New York at Buffalo<br />
Anne Stulik joined the department in 1986 after working for three years as an Ob/<br />
Gyn nurse practitioner for Health Care Plan of Western New York. Previously, she<br />
spent two years as an American Peace Corps volunteer working in women’s health. She com-<br />
pleted her Master’s degree from SUNY Buffalo in 1983 and is certified through the NCC as a<br />
Woman’s Health Care Nurse Practitioner. She has a special interest in adolescents and follows<br />
pregnant teenagers in the WPCC’s adolescent prenatal clinic. Teaching responsibilities include<br />
<strong>Brown</strong> medical students, for which she received a <strong>Brown</strong> <strong>University</strong> Medical School Excellence<br />
in Teaching award.<br />
Patricia O’Connell, MS, WHCNP<br />
BSN: Seattle <strong>University</strong><br />
MS: Boston College<br />
Patricia O’Connell joined the department in 1987 after completing her Masters<br />
program in Women’s Health at Boston College. She is certified as a Women’s<br />
Health Care Nurse Practitioner and as a Nurse Colposcopist. In addition to general obstetric<br />
and gynecologic care, her interests include colposcopy and caring for adolescents. Patricia<br />
teaches <strong>Brown</strong> Medical students, and is a Clinical Preceptor for both the <strong>University</strong> of Rhode<br />
Island and Boston College’s Nurse Practitioner programs. Patricia is a member of the American<br />
Society for Colposcopy and Cervical Pathology and the Association of Reproductive Health<br />
Professionals.<br />
Linda Moulton, MSN, FNP<br />
BA: <strong>Brown</strong> <strong>University</strong><br />
BSN: Newport Hospital School of Nursing<br />
MSN: <strong>University</strong> of RI<br />
Linda Moulton has been a primary care nurse practitioner at the WPCC since<br />
1992. She graduated from <strong>Brown</strong> in 1971 and went on to teach German, mathematics and<br />
ancient history at St. George’s School in Newport, RI and the Shipley School in Bryn Mawr,<br />
PA. After completing her nursing degree in 1983, she worked for four years as a staff nurse at<br />
the Providence VNA. In 1989, she graduated as a family nurse practitioner from URI. She was<br />
certified in colposcopy in 1993 by The <strong>University</strong> of Pennsylvania and Planned Parenthood of<br />
Southeastern Pennsylvania and also has an interest in dermatology. Linda has received numer-<br />
ous excellence in teaching awards since 1992 in her role as a Clinical Instructor for <strong>Brown</strong> med-<br />
ical students. Linda speaks Spanish and German and is a member of the ASCCP and NPRH.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 11<br />
A m b u l a t o r y C a r e
A m b u l a t o r y C a r e<br />
12<br />
Erin Dobson, MSN, FNP<br />
BSN: New York <strong>University</strong><br />
MSN: <strong>University</strong> of RI<br />
After graduating from NYU in 1981, Erin Dobson worked as a staff nurse for ten<br />
years in labor and delivery, surgery and drug and alcohol rehabilitation prior to<br />
obtaining her master’s degree in 1992. She is certified as a family nurse practitioner and joined<br />
the staff at the WPCC in 1992. In addition to her teaching of <strong>Brown</strong> medical students, Erin is a<br />
clinical preceptor for the <strong>University</strong> of Rhode Island Nurse Practitioner program. Erin earned<br />
the Dean’s teaching excellence award last year and has received numerous excellence in teach-<br />
ing awards since 1992.<br />
Paulette Corey, MSN, FNP<br />
BSN: <strong>University</strong> of RI<br />
MSN: <strong>University</strong> of RI<br />
After working in a community health center for three years as well as working in<br />
research at Memorial Hospital with the Women’s Health Initiative, Paulette joined<br />
the department of obstetrics and gynecology in 1995. She has a special interest in STDs and<br />
pregnancy prevention, and while employed at WIH has worked in the Division of Research<br />
performing women’s health research. In the WPCC, Paulette is involved with teaching medical<br />
students and has precepted nurse practitioner students in the past. She is now involved in the<br />
Vulvar Specialty Clinic with a specialty in patients with recurrent vaginitis.<br />
Ann Biderman Cooper, RNP, MS<br />
BS: Skidmore College<br />
MSN: <strong>University</strong> of California, San Francisco<br />
After a number of years working as Nurse practitioner in an OB/GYN practice,<br />
Ann Cooper returned to Women & Infants in 2002 to work with OB Medicine as<br />
a Research nurse and since 2004 at the WPCC as a Nurse practitioner. Following college and a<br />
stint in Boston, Ann worked in San Francisco and completed a Master’s/NP program at UCSF.<br />
She then worked at San Francisco General Hospital as an NP/Research nurse in GYN Infectious<br />
Disease. After moving home to RI in 1979, Ann worked at the Women & Infants Ambulatory<br />
Care Center on Maude Street until 1985. During this time she also served as a Captain in the<br />
US Army Reserves. She is certified as a Women’s Health Care Nurse Practitioner, speaks Span-<br />
ish, and has a special interest in adolescent and refugee health.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Ann Holdredge, CNM, FNP<br />
RN: St. Joseph’s Hospital<br />
BSN: Salve Regina <strong>University</strong><br />
FNP: Northeastern <strong>University</strong><br />
MSN/CNM: <strong>University</strong> of RI<br />
Ann Holdredge returned to the department in 2008 after working as a nurse midwife in a<br />
private Ob/Gyn practice in Rhode Island as well as the Indian Health Services in Gallup, New<br />
Mexico. She has precepted both <strong>Brown</strong> and Yale medical students as well as nurse practitioner<br />
and nurse midwife students from the Universities of RI, Vermont and New Mexico. She has an<br />
interest in cultural aspects in women’s health care.<br />
CLINICAL ACTIVITY: THE WOMEN’S PRIMARY CARE CENTER<br />
The Division of Ambulatory Care conducts a variety of general and specialized outpatient ses-<br />
sions at the Women’s Primary Care Center (WPCC). The WPCC’s volume for 2009 fiscal year<br />
was 33,879 patient encounters. The types of sessions and the times they are held are outlined<br />
in Table 1. Our clinical services include prenatal and postpartum care, family planning, general<br />
gynecology, pre-operative consultation, and primary/preventive health care services such as<br />
immunizations, age-appropriate health screening and annual examinations. Specialty clinics<br />
in colposcopy, vulvar disorders, chronic pelvic pain, contraception for women with complex<br />
medical problems, and early pregnancy termination are also offered. Supervision for clinical<br />
sessions is provided by members of the division as well as by hospital-based and community-<br />
based faculty from the departments of Ob/Gyn and Internal Medicine. Dr. Gottlieb, our general<br />
internist, also conducts regular medicine consultation clinics. Faculty from the subspecialty<br />
of Maternal-Fetal Medicine attends the Diabetic and High Risk prenatal sessions (designated<br />
“GDM” and “MFM” respectively, in Table 1).<br />
Table 1. Ob/Gyn Ambulatory Care Division Outpatient Schedule<br />
Monday Tuesday Wednesday Thursday Friday<br />
AM<br />
PM<br />
• WPCC<br />
• Internal<br />
Medicine<br />
Consult Clinic<br />
• Colposcopy<br />
Test Results<br />
• MFM<br />
• WPCC<br />
• Early Options<br />
Clinic<br />
• WPCC<br />
• Contraception<br />
Consult Clinic<br />
• MFM<br />
• Therapeutic<br />
Abortion Clinic<br />
• Vulvar<br />
• WPCC<br />
• Chronic Pelvic<br />
Pain<br />
• MFM<br />
• Internal<br />
Medicine<br />
Consult Clinic<br />
• WPCC<br />
• Adolescent<br />
Prenatal Clinic<br />
• Yellow Chart<br />
Clinic (MFM)<br />
• WPCC<br />
• Gyn Consult<br />
Clinic<br />
• Gyn Specialty<br />
Clinic<br />
• Colposcopy<br />
• WPCC<br />
• Depo Provera<br />
• MFM<br />
• LEEP<br />
• OR (OR LEEPS,<br />
colpo and<br />
vulvar cases)<br />
• WPCC<br />
• Colposcopy<br />
• Pelvic Pain<br />
• Depo Provera<br />
• Internal<br />
Medicine<br />
Consult Clinic<br />
• WPCC<br />
• WPCC<br />
• Pediatric<br />
Gyn Clinic<br />
• Urogyn<br />
• REI<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 13<br />
A m b u l a t o r y C a r e
A m b u l a t o r y C a r e<br />
The second and third year fellows in the fellowship in Female Pelvic Medicine and Recon-<br />
structive Surgery offer urogynecology services at the WPCC twice monthly which provides<br />
the fellows with more independent clinical care, decision making, and practice management.<br />
Case review is provided by the Division of Urogynecology faculty. Fellows from the Division<br />
of Reproductive Endocrinology and Infertility see patients at the WPCC and address problems<br />
such as infertility, PCOS, menorrhagia, menopausal issues and other endocrine disorders. They<br />
are supervised by the Reproductive Endocrinology and Infertility faculty. The majority of the<br />
patients receiving sub-specialty care are referred by other WPCC providers but our services<br />
are open to all referring providers. A separate session in pediatric and adolescent gynecology<br />
meets weekly and is staffed by faculty from REI and from the community-based practices.<br />
The WPCC is located at 2 Dudley Street on the fifth floor of the Medical Office Center (MOC).<br />
Located one block from the hospital, the MOC is connected to the main hospital building by<br />
a bridge and passageways through Rhode Island Hospital. Our facility includes 18 general<br />
examination rooms and 4 special procedure rooms. One of the rooms is equipped with a ceil-<br />
ing lift to allow safe transfer of patients who need this accommodation. There are eight consult<br />
rooms, a conference room, and offices for nurse practitioners, social workers, and family plan-<br />
ning counselors. Nutritionists are located directly across the hall, and a satellite lab provides<br />
phlebotomy services directly adjacent to the WPCC. The academic offices of the Division of<br />
Ambulatory Care are onsite, allowing faculty immediate access to the clinical area. The WPCC<br />
also has on-site formal ultrasound, staffed by the Department of Radiology, and a fetal evalua-<br />
tion unit.<br />
The WPCC attempts to maintain provider continuity as much as possible. First established<br />
fourteen years ago, the concept of continuity has markedly improved both patient and provider<br />
satisfaction. In the last years, provider continuity occurred during 90% or more of all prenatal<br />
visits. In an attempt to be more responsive to the primary care needs of our patients, we insti-<br />
tuted “walk-in” sessions in the WPCC ten years ago. These appointment slots are reserved for<br />
patients with urgent (but not emergent) complaints for which they would otherwise have to go<br />
to an emergency room.<br />
WPCC nurses staff a ‘nurse line,’ a telephone line to our patients and the community to answer<br />
clinical questions and triage patients’ medical complaints. In the past year, we registered over<br />
10,290 calls. In addition, our Family Planning counselors handled over 5,000 phone calls from<br />
patients requesting information on contraceptive services.<br />
PEDIATRIC AND ADOLESCENT GYNECOLOGY CLINIC<br />
The pediatric and adolescent gynecology clinic began in July of 2006 to serve the needs of the<br />
girls in Rhode Island and Southeastern Massachusetts with gynecologic issues and concerns.<br />
The other focus of the clinic is to provide an educational experience for the Women & Infants<br />
Hospital of Rhode Island obstetrics and gynecology residents. The clinic initially met twice a<br />
month on Friday afternoons, but now meets every Friday afternoon. Attending staff include<br />
14<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Dr. Carol Wheeler (director), Dr. Jackie Tetreault, Dr. Carroll Medeiros, Dr. Suzanne Dambek and<br />
Dr. Evelyne Caron.<br />
Patients have been seen in the clinic as young as infants to as old as 16 years, although in<br />
general the upper age limit is 14 years. The goal has been to focus on the younger child who is<br />
not sexually active. Older girls seeking routine gynecologic care or contraception are referred<br />
to the WPCC or private gynecologists. Several surgical procedures have been done on patients<br />
seen in the clinic, although the bulk of the patients are primarily office based. Follow up care is<br />
provided for girls seen in both the Women & Infants Emergency Room and Hasbro Children’s<br />
Hospital Emergency Room. Problems commonly encountered include pediatric vulvovaginitis,<br />
lichen sclerosis, labial adhesions, pelvic pain, dysfunctional bleeding, dysmenorrhea, congeni-<br />
tal anomalies, ovarian cysts, and amenorrhea. The referring providers have received communi-<br />
cation by letter after every visit. Feedback from the patients has been positive and the residents<br />
have found it to be a valuable educational experience.<br />
RESEARCH ACTIVITY: THE WOMEN’S PRIMARY CARE CENTER<br />
The WPCC is a recruitment site for multiple clinical research studies for faculty and resident re-<br />
search projects. The types of studies conducted range from the Maternal Fetal Medicine Unit’s<br />
Network trials to research in postpartum depression and maternal antidepressant use from the<br />
Center for Women’s Behavioral Health. Research is conducted by most of the divisions of the<br />
Department of Obstetrics and Gynecology and is often performed in concert with the Division<br />
of Research. In addition, the faculty of the Division has conducted studies ranging from mind-<br />
fulness meditation for women with chronic pelvic pain to interventions for pain control during<br />
intrauterine device insertion, and screening for intimate partner violence.<br />
EDUCATIONAL ACTIVITIES<br />
Faculty members in the Division of Ambulatory Care actively participate in the education of<br />
medical students, nurse practitioner students, residents and faculty. As there continues to be<br />
an increasing emphasis on outpatient treatment, future health care professionals need to be<br />
prepared to deal with this trend.<br />
All Ob/Gyn physician faculty members serve as faculty preceptors for medical students during<br />
the 3rd year Ob/Gyn clerkship (BioMed 490) and most participate as lecturers during the clerk-<br />
ship on a variety of topics. In terms of resident education, all faculty members participate in the<br />
gynecology noon conferences, as preceptors, and all give lectures as part of core curriculum.<br />
Other faculty teaching assignments and educational activities include:<br />
Allen, RH<br />
Director and Faculty Lecturer, Core Curriculum Series in General Gynecology, Obstetrics and<br />
Gynecology Residency, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 15<br />
A m b u l a t o r y C a r e
A m b u l a t o r y C a r e<br />
Faculty Preceptor, Rhode Island Hospital Internal Medicine Residency Program Subspecialty<br />
Rotation in Gynecology, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Co-Director for Women’s Reproductive Health, Freedom and Rights Scholarly Concentration,<br />
Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Faculty Mentor: Resident Colposcopy/Vulvar/Gynecology Conference; Obstetrics and Gynecol-<br />
ogy Residency, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Director, Ryan Program for Resident Education in Family Planning, Obstetrics and Gynecology<br />
Residency, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Resident Research Advisor, Obstetrics and Gynecology Residency, Alpert Medical School,<br />
<strong>Brown</strong> <strong>University</strong><br />
Resident Physician Advisor, Department of Obstetrics and Gynecology, Alpert Medical School,<br />
<strong>Brown</strong> <strong>University</strong><br />
Fox, SD<br />
Faculty Mentor, Coordinator: Resident Physician Weekly Colposcopy/Vulvar/Gynecology Con-<br />
ference, Obstetrics and Gynecology Residency, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Medical Student Mentor, Office of Community Health, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Adjunct Assistant Professor in Gender Studies: GNSS0900C – Reproductive Health: Science<br />
and Politics, Freshman Seminar, <strong>Brown</strong> <strong>University</strong><br />
Director, Colposcopy Clinic and Resident Colposcopy Rotation, Obstetrics and Gynecology<br />
Residency, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Faculty Lecturer, Core Curriculum Series in General Gynecology, Obstetrics and Gynecology<br />
Residency, Albert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Gottlieb AS<br />
Director and Faculty Preceptor, Ambulatory Care Rotation, Obstetrics and Gynecology<br />
Residency, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Director and Faculty Lecturer, Core Curriculum Series in Primary Care Internal Medicine,<br />
Obstetrics and Gynecology Residency, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Faculty Supervisor, Primary Care Noon Conference, Obstetrics and Gynecology Residency,<br />
Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
16<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Faculty Lecturer, General Internal Medicine Residency, Alpert Medical School,<br />
<strong>Brown</strong> <strong>University</strong> (Rhode Island Hospital)<br />
Resident Research Advisor, Obstetrics and Gynecology Residency, Alpert Medical School,<br />
<strong>Brown</strong> <strong>University</strong><br />
Research Advisor: Scholarly Concentration Project (Medical Education);<br />
Resident Physician Advisor, Department of Medicine, Alpert Medical School, <strong>Brown</strong> <strong>University</strong><br />
Medical Student Mentor, Office of Women in Medicine, Alpert Medical School,<br />
<strong>Brown</strong> <strong>University</strong><br />
REGIONAL COMMITTEES<br />
Fox SD<br />
Lobbying Team Member, Planned Parenthood of RI<br />
Executive Board of RI National Organization of Women<br />
Program Coordinator of Healthy Kids RI: The Campaign for Comprehensive Sex Education in RI<br />
Gottlieb AS<br />
Chair, Domestic Violence Task Force, Women & Infants Hospital of Rhode Island<br />
Advisory Board, the Office of Women in Medicine, Alpert Medical School of <strong>Brown</strong> <strong>University</strong><br />
Advisory Board, Gender and Sexuality Studies, <strong>Brown</strong> <strong>University</strong><br />
Co-Director, MomDocFamily<br />
NATIONAL COMMITTEES<br />
Fox SD<br />
Board of Directors, International Pelvic Pain Society Chair, Medical Education Committee, Inter-<br />
national Pelvic Pain Society<br />
Gottlieb AS<br />
Invited Member, Women’s Health Task Force, Society of General Internal Medicine<br />
Allen RH<br />
Chair, Contraception Special Interest Group, American Society for Reproductive Medicine<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 17<br />
A m b u l a t o r y C a r e
A m b u l a t o r y C a r e<br />
18<br />
PUBLICATIONS, ABSTRACTS, & PRESENTATIONS<br />
RE BERRY, MD<br />
AWARD<br />
CREOG National Faculty Award for Excellence in Resident Education from the<br />
<strong>University</strong> of Massacusetts.<br />
POSTER PRESENTATION<br />
Tassone,G.M., Moore Simas, T.,Berry, R.E. Jr Gestational Weight Gain – How to ‘Institute’ New<br />
Guidelines. Poster Presentation, American College of Obstetricians and Gynecologists 58th <strong>Annual</strong><br />
Clinical Meeting, San Francisco, CA, 5/2010.<br />
PUBLICATIONS<br />
Moore Simas T , Riza L, Pasquale S, Berry Jr R, Manning M, Tasillo D, Fluid Resuscitation and<br />
Blood Product Replacement in Postpartum Hemorrhage. MedEdPORTAL; 2010. Available from:<br />
http://services.aamc.org/30/mededportal/servlet/s/segment/mededportal/?subid=7919<br />
Tasillo D , Moore Simas T, Riza L, Pasquale S, Berry Jr R, Manning M, Pharmacologic Interventions<br />
in Postpartum Hemorrhage. MedEdPORTAL; 2010. Available from: http://services.aamc.<br />
org/30/mededportal/servlet/s/segment/mededportal/?subid=8024<br />
AS GOTTLIEB, MD<br />
PUBLICATIONS<br />
Kang JA, Gottlieb AS, Raker CA, Aneja SS, Boardman LA. Interpersonal violence inquiry with<br />
standardized health prevention screening. Obstetrics & Gynecology. 2010;115:1159-65.<br />
Aneja S, Gottlieb AS, Feller E. Physician intervention for intimate partner violence. Medicine &<br />
Health/Rhode Island. 2009;92:307-309<br />
Lechner BE, Gottlieb AS, Taylor LE. Effectively mentoring physician-mothers. (Letter) Academic<br />
Medicine. 2009;84:1643-1644.<br />
ABSTRACTS<br />
Taylor J, MacNamara M, Gottlieb AS. MomDocFamily – providing mentoring and support to<br />
physician-mothers. Oral presentation at The Society of Teachers of Family Medicine Northeast<br />
Region Meeting, Rye Brook, New York, November 1, 2009.<br />
MacNamara, M, Gottlieb AS, Taylor J. MomDocFamily – An innovative strategy for physicianmother<br />
workforce development and retention. Seminar at The National Area Health Education<br />
Center (AHEC) Organization 2010 Conference, Las Vegas, Nevada, June 22, 2010.<br />
INVITED LECTURES, WORKSHOPS, AND PANELS<br />
Intimate Partner Violence: A Practical Guide for Clinicians: Recognizing & Assisting Female<br />
Patients Experiencing Partner Abuse” (Speaker). Grand Rounds, Kent Hospital. Warwick, RI.<br />
February 11, 2010.<br />
“Intimate Partner Violence: A Practical Guide for Clinicians: Recognizing & Assisting Female<br />
Patients Experiencing Partner Abuse” (Speaker). Department of Emergency Medicine, Kent<br />
Hospital. Warwick, RI. May 13, 2010.<br />
Domestic Violence” (Panel discussant). Physicians for Human Rights, The Warren Alpert<br />
Medical School of <strong>Brown</strong> <strong>University</strong>. Providence, RI. October 28, 2009.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Mentoring Relationships” (Panel discussant). Careers in Medicine, The Warren Alpert Medical<br />
School of <strong>Brown</strong> <strong>University</strong>. Providence, RI. February 5, 2010.<br />
“Relationships & Medicine” (Panel discussant). Pre-clinical Advising Program, The Warren<br />
Alpert Medical School of <strong>Brown</strong> <strong>University</strong>. Providence, RI. March 3, 2010.<br />
RH ALLEN, MD<br />
PUBLICATIONS<br />
Allen RH, Raker C, Steinauer J, Eastwood KL, Kacmar JE, Boardman LA. Future Abortion ProProvision among United States Graduating Obstetrics and Gynecology Residents, 2004.<br />
Contraception 2010;81:531-6.<br />
Allen RH, O’Brien B. Uses of misoprostol in obstetrics and gynecology. Reviews in Obstetrics<br />
& Gynecology 2009;2:159-168.<br />
Hachey KJ, Allen RH, Nothnagle M, Boardman LA. Requiring human papilloma virus vaccine<br />
for immigrant women. Obstetrics and Gynecology 2009;114:1135-9.<br />
INVITED LECTURES, WORKSHOPS, AND PANELS<br />
Allen, RH. “Hormonal contraception: Pills, patches, rings and other things” Rhode Island Hospital,<br />
Endocrine Division Grand Rounds. Providence, RI. March 31, 2010.<br />
Allen, RH. “Managing Side Effects of Hormonal Contraception” Roundtable Discussion<br />
American Society for Reproductive Medicine 65 th <strong>Annual</strong> Meeting, Atlanta, GA. October 2009.<br />
SD FOX, MD<br />
ABSTRACTS<br />
Chisolm-Straker M, Weinstein S, Fox SD. Abortion Counseling and Informed Consent: A survey<br />
of women’s experiences. National Abortion Federation <strong>Annual</strong> Meeting Philadelphia PA,<br />
4/26/10<br />
INVITED LECTURES, WORKSHOPS, AND PANELS<br />
“Reproductive health and inflammatory bowel disease.” Women & Infants’ Hospital of RI<br />
Inflammatory Bowel Disease Support Group 9/2/09<br />
“Reducing Pain for Patient and Provider: The initial approach to the chronic pelvic pain<br />
patient.” International Pelvic Pain Society <strong>Annual</strong> Meeting, Phoenix, AZ, 10/16/09<br />
“Surgical Management of Chronic Pelvic Pain” International Pelvic Pain Society <strong>Annual</strong><br />
Meeting, Phoenix AZ, 10/16/09<br />
“Chronic Pelvic Pain and Reproductive Health.” <strong>Brown</strong> <strong>University</strong> Scholarly Concentration in<br />
Women’s Reproductive Health and Freedom, 11/12/09<br />
Careers in Women’s Health, Panel Discussion, <strong>Brown</strong> <strong>University</strong> MOMS Program, Providence,<br />
RI, 2/3/10<br />
“Opioids: The Good, the Bad and the Ugly” Luncheon Conference at ACOG <strong>Annual</strong> Clinical<br />
Meeting, San Francisco, CA, 5/18/10<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 19<br />
A m b u l a t o r y C a r e
20<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
DIVISION OF GYNECOLOGIC ONCOLOGY<br />
“THE PROGRAM IN WOMEN’S ONCOLOGY”<br />
The Program in Women’s Oncology is the state’s largest focused cancer program dedicated to<br />
women. Since 1989, the Program in Women’s Oncology has evolved from a series of common–<br />
sense questions. The central and framing question, which continues to drive the Program, is<br />
“What would you want done for your loved ones under those circumstances?” While each of<br />
our desires would undoubtedly vary, in the face of a serious health problem such as cancer,<br />
we would all want for our loved ones the best science–of–medicine (a.k.a. evidence–based<br />
medicine) but is that all? Surely, we as an Oncology Program must provide the best of medical<br />
science for the patients and families seeking our care, so let’s consider how that’s done first.<br />
Though seemingly straight–forward, in truth, providing the best medical recommendations for<br />
an individual is not easy. “Cancer” is in actuality thousands of different diseases, each with its<br />
own important, distinctive nuances, treatments, and prognoses. Determining what you have<br />
and what are the best medical recommendations for your specific cancer, under your individ-<br />
ual circumstances, is in actuality very important and very difficult to do. The Program in Wom-<br />
en’s Oncology is dedicated to helping patients understand what they have and what science<br />
pertains (a.k.a. – “p–values”) and of those, which medical recommendations are best for them.<br />
It does so through the unique, multi–disciplinary Tumor Board process.<br />
A core value of the Program, the Tumor Board (i.e. a multidisciplinary, prospective process)<br />
assures that the best science of medicine is offered to our patients. The Tumor Board’s charge<br />
is to carefully consider the exact type of malignancy each individual patient has and her overall<br />
medical circumstances. From that evolves the best medical recommendation for them. Once<br />
that recommendation has been conveyed to the patient and fully understood, and assuming<br />
the patient and family concur, the next tumor board question is “Where should that recom-<br />
mendation be carried out?”<br />
The Tumor Board process, the research program and treatment protocols, the best science of<br />
medicine are all extensions of the Program’s answer to the framing question, “What would we<br />
want done for our loved ones under those circumstances?” But, as important as the best “p–<br />
values” of medicine is for patients, is that all we would want for our loved ones facing cancer?<br />
The obvious answer is no, “we would want more”. In addition to the p–values, we want caring,<br />
hope, and other “human values.”<br />
Therefore, in the sequence of questions guiding the Program in Women’s Oncology is the con-<br />
tinuous and always –asked follow–up question, “Can we do more?” Can we do more for the<br />
patient than providing the best possible best science of medicine? Asking these series of ques-<br />
tions, each step along the way, brings the Program’s cancer care/caring to very different places<br />
than would science alone. “P–values,” “H–values”, science, art, and the poetry of life inspire<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 21<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
the Program in the remarkably diverse work that it does on behalf of cancer patients and their<br />
families. The Program now has many excellent and comprehensive services/components…<br />
from MD’s and PhD’s, to surgery, chemotherapy, music, and poetry; all are interpretations of<br />
what we would want done for our loved ones under those circumstances. In the broadest,<br />
most philosophic sense, then, the Program is continually challenged by the simultaneously<br />
unanswerable and introspective question “What matters matter?”<br />
PROGRAM FACULTY<br />
22<br />
Cornelius O. “Skip” Granai III, MD, FACOG, FACS, Division Director<br />
MS: <strong>University</strong> of Vermont<br />
MD: <strong>University</strong> of Vermont<br />
Residency: Tufts<br />
Fellowship: New England Medical Center<br />
Dr. Granai is a Professor of Obstetrics & Gynecology and the Director of the<br />
Gynecologic Oncology Division, as well as Director of the Gynecologic On-<br />
cology Fellowship Program. He is also Vice President of Network Development and Women’s<br />
Cancer at Women & Infants Hospital of Rhode Island. He heads a multidisciplinary team includ-<br />
ing residents, nine gynecologic oncologists, four gynecologic oncology fellows, one breast<br />
fellow, oncology nurses, nurse practitioners, physician’s assistants, social workers, dieticians,<br />
integrative therapy staff, physical therapists, an administrative team and the multi–disciplinary<br />
support of many others including medical students from <strong>Brown</strong> and elsewhere.<br />
Prior to joining Women & Infants Hospital of Rhode Island and <strong>Brown</strong> <strong>University</strong>, he was on<br />
the faculty of Tufts and Harvard <strong>University</strong> and on the staffs of New England Medical Center<br />
and Massachusetts General Hospital where he served as Director of the Gynecologic Oncol-<br />
ogy fellowship program. He is board certified in Obstetrics and Gynecology and Gynecologic<br />
Oncology. He is a fellow of the American College of Surgeons, the Society of Surgical Oncolo-<br />
gists, the Society of Gynecologic Oncology, the New England Association of Gynecologic<br />
Oncologists, and the American Society of Clinical Oncology. Dr. Granai is the Vice President of<br />
the Society for Gynecologic Oncology. He is a member of the International Gynecologic Cancer<br />
Society. Dr. Granai holds the title of Oral Examiner for the American Board of Obstetrics and<br />
Gynecology, for both Ob–Gyn oral boards and the subspecialty Gyn–Oncology boards.<br />
Dr. Granai is the founder of the Integrative Care Program at Women & Infants Hospital of<br />
Rhode Island, which began in 1992. This unique, patient–centered program includes pet thera-<br />
py, massage, reiki, journal writing, yoga, nutrition/weight–loss counseling, personal life history/<br />
writing, music therapy, meditation, hypnotherapy, spa–treatments, acupuncture, art therapy,<br />
and more. He is also the Founder and President of the International Health Foundation, which<br />
provides ongoing, direct health care and educational exchanges in which physicians and nurs-<br />
es from WIH/<strong>Brown</strong> and the Dominican Republic visit each other to provide teaching, clinically<br />
demonstrate surgical techniques, and share ideas on treatment approaches.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Dr. Granai has served as chairman of the Life Enrichment Task Force of the Society of Gyne-<br />
cologic Oncology. Dr. Granai was honored by being voted “Top Doctor for Women” in the<br />
Rhode Island Monthly magazine. Dr. Granai was also honored with being elected as one of the<br />
“Best Doctors in America.” Dr. Granai is a recipient of the Lifetime Achievement Award by the<br />
American Cancer Society. In addition to all of this, Dr. Granai has become an acclaimed, na-<br />
tional speaker, sought after for his real–life medical/surgical experiences, personal experiences,<br />
philosophic, humorous, compassionate and always–dynamic presentations. He has been the<br />
keynote speaker at numerous, national and international conferences and annual meetings.<br />
Christina Bandera, MD<br />
BS: Harvard <strong>University</strong><br />
MD: Johns Hopkins <strong>University</strong><br />
Residency: Brigham and Women’s<br />
Fellowship: <strong>University</strong> of Pennsylvania<br />
Dr. Bandera joined the Program in Women’s Oncology in February 2005 and is Board Certified<br />
in General Obstetrics and Gynecology and Gynecologic Oncology by the American Board of<br />
Obstetrics and Gynecology. She also completed a Fellowship in Robotic Surgery for Gyneco-<br />
logic Oncology. Dr. Bandera’s clinical interests include the surgical and medical management<br />
of gynecologic cancers. She has a special interest in providing minimally invasive surgery. She<br />
has published numerous research articles and chapters regarding gynecologic cancers and<br />
is currently the Gyn Oncology editor for the international journal Gynecologic and Obstetric<br />
Investigation. Dr. Bandera lives in Cranston with her husband Dr. Cedric Priebe.<br />
Laurent Brard, MD, PhD<br />
MD: <strong>University</strong> of Pittsburgh<br />
Residency: Women & Infants Hospital of Rhode Island<br />
Fellowship: Women & Infants Hospital of Rhode Island<br />
Dr. Brard joined our Program in July, 2002. Born in Nantes (France), raised in<br />
Montreal (Canada) and Paris (France), Dr. Brard has received numerous degrees: BSc in Chemi-<br />
cal Engineering from École Supérieure de Chimie Industrielle de Lyon (France), 1987; MSc<br />
in Organic Chemistry from Université Claude Bernard (France), 1987; PhD in Chemistry from<br />
Northwestern <strong>University</strong>, 1991; Post-Doctorate fellowship in Chemistry at Northwestern Uni-<br />
versity, 1992; Post-Doctorate fellowship in Chemistry at <strong>University</strong> of Pennsylvania, 1992-1994;<br />
MD from the <strong>University</strong> of Pittsburgh, 1998. Dr. Brard is a published clinician-scientist with<br />
several patents (some through Women & Infants Hospital of Rhode Island/<strong>Brown</strong> <strong>University</strong>).<br />
Since arriving in Rhode Island, Dr. Brard has continued his academic work with 58 publications,<br />
and 70 abstracts to date. Following the completion of this fellowship in June 2005, he was<br />
selected by a national search process to begin his faculty appointment as Assistant Professor<br />
at the Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong> in the Division of Gynecologic Oncol-<br />
ogy, and Department of Obstetrics and Gynecology. Shortly thereafter, he was selected as one<br />
of four BIRCWH (Building Interdisciplinary Research Careers in Women’s Health) NIH K12 grant<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 23<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
scholars. During his BIRCWH scholarship, he also received a NIH/NINDS R21 grant, an OCRF<br />
Foundation grant and <strong>Brown</strong> <strong>University</strong> Seed grants. After completing his BIRCWH scholar-<br />
ship, he was recently awarded a NIH/NCI R01 five-year grant. He is currently the director of the<br />
Molecular Therapeutics Laboratory, the basic science lab of the division of Gynecology Oncol-<br />
ogy. Among his other accomplishments is a continued commitment to education. Dr. Brard<br />
has received multiple teaching awards from Women & Infants Hospital of Rhode Island and<br />
the Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong> School. Dr. Brard is leaving Women &<br />
Infants effective June 30, 2010.<br />
24<br />
Paul A. DiSilvestro, MD, FACOG, FACS<br />
BA: Dartmouth College<br />
MD: <strong>University</strong> of Vermont<br />
Residency: Women & Infants Hospital of Rhode Island<br />
Fellowship: <strong>University</strong> of Oklahoma.<br />
Dr. DiSilvestro is an Associate Professor in the Department of Obstetrics and Gynecology at<br />
<strong>Brown</strong> <strong>University</strong> School of Medicine. He joined our Program in September, 2003. Dr. DiSilves-<br />
tro is Board certified in Obstetrics and Gynecology and Gynecologic Oncology. He has major<br />
research interest in clinical trials and serves as the Principal Investigator at Women & Infants<br />
Hospital of Rhode Island for the Gynecologic Oncology Group of the National Cancer Institute.<br />
Dr. DiSilvestro has recently been appointed co-chairman of the Ovarian Cancer Committee for<br />
the Gynecologic Oncology Group. He is a member of several professional societies, including<br />
the Society of Gynecologic Oncology. Dr. DiSilvestro is also the chairman of the Institutional<br />
Review Board at Women & Infants Hospital of Rhode Island.<br />
Don S. Dizon, MD<br />
BA: <strong>University</strong> of Rochester<br />
MD: <strong>University</strong> of Rochester School of Medicine<br />
Residency: Yale-New Haven<br />
Fellowship: Cornell <strong>University</strong><br />
Dr. Dizon joined our Program in October, 2003 as Director of Medical Oncology and is an Assis-<br />
tant Professor of Medicine and Obstetrics & Gynecology for <strong>Brown</strong> Medical School; currently<br />
serves as co-director of the Center for Sexuality, Intimacy and Fertility as well as the Director<br />
of Integrative Services. He is board certified in internal medicine and medical oncology. He re-<br />
ceived the American Society of Clinical Oncology Career Development Award in 2002. He was<br />
elected fellow of the American College of Physicians in 2005. He is a member of the American<br />
College of Physicians, the American Society of Clinical Oncologists, American Association for<br />
Cancer Research, Society of Gynecologic Oncologists, The International Gynecologic Cancer<br />
Society, the Society for Integrative Oncology, the National Consortium of Breast Centers and<br />
the International Society for Sexuality and Cancer. In 2006, he became Vice President for the<br />
National Consortium of Breast Centers and will continue as Program Chair for the 2009 <strong>Annual</strong><br />
Meeting. He serves on the Education Committee and as a member of the Speakers’ Bureau for<br />
the International Gynecologic Cancer Society.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Carolyn McCourt, MD<br />
BA: Creighton <strong>University</strong><br />
MD: Creighton <strong>University</strong><br />
Residency: Washington <strong>University</strong> (MO)<br />
Fellowship: Women & Infants Hospital of Rhode Island<br />
Dr. McCourt joined the faculty of the Program in Women’s Oncology as Assistant Professor<br />
in 2008. Dr. McCourt is board certified in Obstetrics and Gynecology. She has major research<br />
interest in clinical trials and serves as the Women & Infants’ site Co-Principal Investigator for<br />
the Gynecologic Oncology Group (GOG), a clinical and basic science research, non-profit orga-<br />
nization supported by the National Cancer Institute. She is a member of several professional<br />
societies, including the Society of Gynecologic Oncology, American College of Surgeons, and<br />
American Society of Clinical Oncology.<br />
Richard Moore, MD, FACOG<br />
MD: <strong>University</strong> of Alberta<br />
Residency: Eastern Virginia School of Medicine<br />
Fellowship: Women & Infants Hospital of Rhode Island /<strong>Brown</strong> <strong>University</strong><br />
Dr. Moore is an Associate Professor in the Department of Obstetrics and Gynecol-<br />
ogy. He is the director of the Center for Biomarkers and Emerging Technologies (CBET) and<br />
an associate director of the Program in Women’s Oncology. Dr. Moore is board certified in<br />
Obstetrics and Gynecology and Gynecologic Oncology. He is a Fellow of the American Board<br />
of Obstetrics and Gynecology and the American College of Surgeons. He is a member of the<br />
Society of Gynecologic Oncologists, the New England Association of Gynecologic Oncolo-<br />
gists and the Society of Surgical Oncologists. Dr. Moore leads the basic science laboratory for<br />
the Program in Women’s Oncology. His Research interests include the development of novel<br />
biomarkers for ovarian and endometrial cancers. His research in ovarian cancer has led to<br />
the clinical development of a novel biomarker (HE4) now used in the management of ovarian<br />
cancer patients world wide. Dr. Moore was also instrumental in the development of the Risk of<br />
Ovarian Malignancy Algorithm (ROMA) used for risk assessment for the diagnosis of ovarian<br />
cancer in women with a pelvic mass. HE4 has recently been cleared by the US FDA for moni-<br />
toring patients with ovarian cancer. Dr. Moore is also one of the pioneers for the use of sentinel<br />
lymph node technology in the treatment of patients with vulva cancer. Dr. Moore has authored<br />
over 30 peer reviewed papers and book chapters.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 25<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
26<br />
Bachir J. Sakr, MD<br />
MD: Lebanese <strong>University</strong><br />
Residency: Detroit Medical Center<br />
Fellowship: <strong>University</strong> of Pittsburgh<br />
Dr. Sakr is a medical oncologist and joined the staff at the Program in Women’s<br />
Oncology in early 2007. Dr. Sakr practiced as a primary care provider and hema-<br />
tology/oncology specialist in Providence for a few years before joining the Program in Wom-<br />
en’s Oncology. He was born in Lebanon and received his medical degree from The Lebanese<br />
<strong>University</strong>. He did clinical rotations in medicine and surgery in Lebanon, before coming to the<br />
United States for his internship and residency. He also completed a fellowship in hematology<br />
and oncology at the <strong>University</strong> of Pittsburgh Medical Center. Fluent in Arabic and French,<br />
Dr. Sakr is certified by the American Board of Internal Medicine in medical oncology<br />
and hematology.<br />
Trevor Tejada–Bergés, MD<br />
BS/MS: McGill <strong>University</strong><br />
MD: McGill <strong>University</strong><br />
Residency: Royal Victory Hospital, McGill <strong>University</strong><br />
Fellowship: Women & Infants Hospital of Rhode Island<br />
Dr. Tejada–Bergés joined the Program in July 2001 as a Gynecologic Oncology fellow. He<br />
completed the Gynecologic Oncology fellowship, and then stayed on to continue a Breast Care<br />
Fellowship. He is now an Assistant Professor of Obstetrics and Gynecology for the Warren<br />
Alpert School of Medicine at <strong>Brown</strong> and cares for patients with both gynecologic malignancies<br />
and breast cancer. He is Board-certified in both Obstetrics and Gynecology and Gynecologic<br />
Oncology. His current clinical interests lie in the field of racial disparities in cancer care and<br />
palliative/end-of-life care. Given his involvement in the field, he was recently invited by the<br />
National Office of Minority Health to participate in the National Partnership for Action to Elimi-<br />
nate Health Disparities. In 2009 he received the APGO award for exceptional teaching by the<br />
medical students at <strong>Brown</strong>. He was also recently recognized by the American Cancer Society<br />
with the Sandra C. Labaree Volunteer Values Award. He is a candidate member of the Society<br />
of Gynecologic Oncologists (SGO), where he serves on the Breast Cancer Task Force, and the<br />
New England Association of Gynecologic Oncologists (NEAGO). He is a member of the Ameri-<br />
can Society of Breast Surgeons (ASBS) and the American Society of Breast Disease (ASBD).<br />
Katina Robison, MD, completed her fellowship and joined the faculty at the<br />
Program in Women’s Oncology as Assistant Professor in July of 2009. She was<br />
chosen as a Women’s Reproductive Health Research Scholar in March of 2009.<br />
She completed her BA in Psychology at San Francisco State <strong>University</strong> in 1996,<br />
followed by her medical doctorate at the <strong>University</strong> of Pittsburgh in 2002. She<br />
completed her Obstetrics and Gynecology residency training and Gynecologic<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Oncology Fellowship at Women & Infants Hospital of Rhode Island in June 2009. As a WRHR<br />
scholar, she is actively involved in clinical research, including a study evaluating barriers to<br />
cervical cancer screening among Southeast Asian women and enrollment will be completed<br />
at the end of this year in a study determining the prevalence of HPV and genotype distribu-<br />
tion among Southeast Asian women in Rhode Island. She also continues to be involved in Dr.<br />
Moore’s prospective sentinel lymph node study in patients with vulvar cancer and has recently<br />
completed a retrospective study evaluating the long-term use of Doxil in women with<br />
recurrent Ovarian Cancer. In addition, she is developing a survivorship database among<br />
women with Gynecologic Malignancies.<br />
FELLOWSHIP TRAINING<br />
Sonali V. Pandya, MD, will complete her Breast Fellowship at Women & Infants Hospital in July<br />
2010. Dr. Pandya completed medical school at Saint George’s <strong>University</strong> School of Medicine<br />
in Grenada, West Indies and graduated in 2004 with a Doctorate in Medicine. After graduating,<br />
she completed a four year residency in General Surgery at Albany Medical Center, Albany NY.<br />
Dr. Pandya was the recipient of the Intern of the Year Award in 2005.<br />
Nada Mufid Kawar, MD, is a second year Fellow in the Program in women’s Oncology. Dr.<br />
Kawar completed medical school at Washington <strong>University</strong> School of Medicine in St. Louis<br />
Missouri and graduated in 2005 with a Doctorate in Medicine. After graduating, she completed<br />
a four year residency in Obstetrics and Gynecology at the <strong>University</strong> of California, San Fran-<br />
cisco. Dr. Kawar was administrative Chief Resident at <strong>University</strong> of California, San Francisco,<br />
from 2008 to 2009.<br />
Katrin Kristjansdottir, MD, is a third year Fellow in the Program in Women’s Oncology. Dr.<br />
Kristjansdottir completed medical school at the <strong>University</strong> of Iceland and graduated in 2001<br />
with a Candidatus Medicinae degree. After graduating, she completed a one-year internship<br />
with the <strong>University</strong> Hospital of Iceland. She then worked as a house officer at the department<br />
of OB/Gyn at the <strong>University</strong> of Iceland Hospital for a year before completing her OB/Gyn resi-<br />
dency at the <strong>University</strong> of Colorado HSC in 2007. After residency, Katrin worked for a year as<br />
an attending at Denver Health and Hospital and was part of the teaching faculty at the Univer-<br />
sity of Colorado HSC during that time.<br />
Shannon MacLaughlan, MD, is the Senior Fellow in the Program in Women’s Oncology. Dr.<br />
MacLaughlan completed her BS degree in biology with a minor in religious studies at Stetson<br />
<strong>University</strong> in DeLand, Florida in 1998. She received her medical doctorate from the <strong>University</strong><br />
of Florida College in Medicine in 2002, and completed her obstetrics and gynecology residency<br />
at Greenville Hospital Systems <strong>University</strong> Medical Center, Greenville, SC in 2006. After gradu-<br />
ation she worked for a year in the Women & Infants’ Hospital triage unit before joining the<br />
Program in 2007. Dr. MacLaughlan is currently conducting a pilot study in collaboration with<br />
The Program in Women’s Oncology Integrative Care Program investigating the use of hypno-<br />
therapy and gabapentin for therapy-induced hot flashes in breast cancer survivors.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 27<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
Ashley Stuckey, MD, completed her combined Gynecologic Oncology and Breast Surgery Fel-<br />
lowship in June 2010 and will be joining the Program in Women’s Oncology in July 2010. Dr.<br />
Stuckey received her B.A. in French from Davidson College in 1996. She received her medical<br />
doctorate in 2001 from Louisiana State <strong>University</strong> Health Sciences Center and then completed<br />
her Obstetrics and Gynecology residency training in June of 2005 at the same institution. She<br />
completed a Pelvic Surgery fellowship at Lahey Clinic in June of 2006. She was the first fellow to<br />
complete the new four-year program focusing on additional training in breast health.<br />
NEW ARRIVALS TO THE DIVISION<br />
Beth Cronin, MD, will begin her Gynecologic Oncology Fellowship at WIH in July 2010.<br />
Dr. Cronin completed medical school at the <strong>University</strong> of Vermont College of Medicine in Burl-<br />
ington VT and graduated in 2006 with a Doctorate in Medicine. After graduating, she completed<br />
a four-year residency in Obstetrics and Gynecology at Women and Infants’/<strong>Brown</strong> <strong>University</strong>. Dr.<br />
Cronin was Administrative Chief Resident at Women and Infants’/<strong>Brown</strong> <strong>University</strong>, from 2009<br />
to 2010. Dr. Cronin was the recipient of the Women and Infants Hospital Excellence in Teach-<br />
ing Awards from 2007 – 2010. She was the recipient of the Professionalism and Humanism in<br />
Women’s Health Award in 2009 and the David H. Nichols Award for Excellence in Pelvic Surgery<br />
in 2010.<br />
Marcia Humphrey Schmidt, MD, will begin her Breast Fellowship at Women & Infants Hospital<br />
in July 2010. Dr. Humphrey Schmidt completed medical school at Upstate Medical <strong>University</strong>,<br />
State <strong>University</strong> of New York and graduated in 2002 with a Doctorate in Medicine. After graduat-<br />
ing, she completed a four-year residency in Obstetrics and Gynecology at Winthrop <strong>University</strong><br />
Hospital, and went on to complete a one-year Fellowship in Pelvic Surgery at Emory <strong>University</strong><br />
School of Medicine, followed by a three-year Gynecologic Oncology Fellowship at the <strong>University</strong><br />
of South Florida.<br />
THE MEDICAL STAFF — BREAST HEALTH CENTER<br />
28<br />
Robert D. Legare, MD<br />
MD: Tufts<br />
Residency: Yale-New Haven<br />
Fellowship: Brigham and Women’s<br />
Dr. Legare is an Associate Professor of Obstetrics and Gynecology (Clinical) at<br />
Women & Infants Hospital of Rhode Island/<strong>Brown</strong> <strong>University</strong>. Dr. Legare was an Associate<br />
Physician at Brigham & Women’s Hospital and Dana-Farber Cancer Institute and an Instructor in<br />
Medicine at Harvard Medical School, 1996 – 1997. As a medical oncologist/hematologist he is an<br />
integral part of both the Gyn-Onc Clinic and the Breast Health Center. Dr. Legare is the Director<br />
of the Breast Health Center and Cancer Risk Assessment and Prevention Program in The Pro-<br />
gram in Women’s Oncology. He is board certified in Medical Oncology, Hematology and Inter-<br />
nal Medicine. He is Instructor for small group sessions, Pathophysiology/Hematology (Bio350),<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
<strong>Brown</strong> <strong>University</strong> School of Medicine. Dr. Legare has received the Dean’s Teaching Excellence<br />
Award from Women & Infants Hospital of Rhode Island/<strong>Brown</strong> <strong>University</strong> from 2000-2009. He is a<br />
member of the American Society of Clinical Oncology, American Society of Hematology, <strong>Brown</strong><br />
<strong>University</strong> Oncology Group and the author of many papers, abstracts and chapters.<br />
Jennifer S. Gass, MD, FACS<br />
MD: <strong>University</strong> of Maryland<br />
Residency: Temple <strong>University</strong> Hospital<br />
Dr. Gass is Chief of Surgery at Women & Infants Hospital of Rhode Island, Director<br />
of the Breast Fellowship at the Breast Health Center, as well as Clinical Assistant<br />
Professor at the Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong> from 1993–present. She is<br />
Board Certified in general surgery. She is on the staff of Women & Infants Hospital of Rhode<br />
Island, Rhode Island Hospital, and Miriam Hospital. In 2002–2003 she attended in the Surgical<br />
Intensive Care Unit at Rhode Island Hospital. She is a member of the American Society of Breast<br />
Surgeons, Rhode Island Medical Women’s Association, Rhode Island Medical Society, American<br />
Medical Women’s Association, Association of Women Surgeons, American College of Surgeons,<br />
American Medical Association, Society of Surgical Oncology, and the New England Surgical So-<br />
ciety. Under Dr. Gass’s supervision, the Women & Infants’ Breast Fellowship received 5 year cer-<br />
tification by the Society of Surgical Oncology. She reviews for the annals of Surgical Oncology,<br />
The Journal of Surgical Oncology, The American Journal of Clinical Oncology, and The Journal<br />
of the American College of Surgeons. She is the program co-chair for the 2010 National Consor-<br />
tium of Breast Centers <strong>Annual</strong> Meeting. She serves on the ethics committee and the board of<br />
Advocates for the American Society of Breast Surgeons and the Breast Program Directors Chair<br />
committee for the Society of Surgical Oncology and the program for American Society of Clinical<br />
Oncologist Breast Meeting. At Women and Infants’ she serves on the CME committee, and the<br />
GYN Review group. At <strong>Brown</strong>, she serves on the Medical School Admissions Committee.<br />
Ekaterini Tsiapali, MD<br />
MD: National <strong>University</strong> of Athens<br />
Residency: East Tennessee State <strong>University</strong><br />
Fellowship: Women & Infants Hospital of Rhode Island<br />
Dr. Tsiapali joined the Program in Women’s Oncology as a General and Breast<br />
surgeon in September 2007. She is a native of Greece, who started her General<br />
Surgery training in Greece (receiving her MD from the National <strong>University</strong> of Athens) and moved<br />
to the US when she was offered a position as a Research Fellow at East Tennessee State Univer-<br />
sity. After a year of bench research on Trauma and Sepsis, she proceeded to complete a General<br />
Surgery Residency. She came to Women and Infants’ in 2006 for her fellowship. Her special inter-<br />
ests include oncoplastic breast surgery and advanced laparoscopy.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 29<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
30<br />
Doreen L. Wiggins, MD, FACOG, FACS<br />
BA: <strong>University</strong> of Rhode Island<br />
MD: <strong>Brown</strong> Medical School<br />
Residency: Women & Infants Hospital of Rhode Island<br />
Fellowship: Women & Infants Hospital of Rhode Island<br />
Dr. Wiggins is part of the Breast Health Center team as a Breast Surgeon. She is an Assistant<br />
Clinical Professor of Obstetrics and Gynecology at <strong>Brown</strong> Medical School. She received a<br />
Teaching Excellence Award presented by <strong>Brown</strong> <strong>University</strong> Medical Students in 1990. She is<br />
a fellow of the American College of Obstetrics and Gynecology. In 2000, she completed train-<br />
ing as a children’s grief counselor at the Dougy Center in Oregon. She has served as the Vice<br />
President of Friend’s Way and volunteered as a facilitator to help children. Dr. Wiggins received<br />
a Partner in Philanthropy Award in 2002 by the Rhode Island Association of Fundraising Profes-<br />
sionals. She is a member of the American Medical Association, the Society of Surgical Oncol-<br />
ogy, the American Society of Breast Surgeons, the American Society of Breast Disease, the<br />
American College of Surgeons, the American Society of Clinical Oncology, and former member<br />
of the Board of Directors of Friend’s Way. Dr. Wiggins was chosen to be one of the 26 cyclists<br />
in the Tour of Hope, a transcontinental bicycling tour by Lance Armstrong to promote cancer<br />
research. Dr Wiggins continues her relationship with the Lance Armstrong Foundation as an<br />
advocate for cancer patients, and was selected to go to Washington, D.C. as part of “Livestrong<br />
Day” and meet with members of Congress in 2005 and 2006. She also represented the Lance<br />
Armstrong Foundation for the American Cancer Society “One Voice Against Cancer (OVAC) in<br />
Washington, DC in June 2008. In July 2006, as a team member she summitted Mt. Shasta (14,<br />
162 ft) in California for the Breast Cancer Fund to raise awareness regarding the environmen-<br />
tal causes of breast cancer. Dr. Wiggins is the Co-Director of the Center for Sexuality, Intimacy<br />
and Fertility through the Program in Women’s Oncology dedicated to helping cancer patients<br />
improve quality of life and provide a much needed resource. Dr. Wiggins coordinates resident<br />
teaching in breast service at <strong>Brown</strong> Medical School and has received excellence in teaching<br />
awards, 2004 through 2008. She was also a course leader for postgraduate course “Breast<br />
Cancer and GYN Patient” at the <strong>Annual</strong> Clinical Meeting of ACOG in May 2008. Dr. Wiggins<br />
resigned from her position in December 2009 to pursue other opportunities.<br />
David A. Edmonson, MD, FACS, joined the staff of the Breast Health Center in<br />
June of 2010. Dr. Edmonson received his B.S. in Biology from Vanderbilt Uni-<br />
versity in Nashville, TN in 1993. He received his medical degree in 1999 from St.<br />
Georges <strong>University</strong> School of Medicine. He completed his general surgery intern-<br />
ship and residency at Albany Medical Center in Albany, NY, and was Chief Resi-<br />
dent in 2004. Dr. Edmonson completed his Fellowship in Surgical Oncology of<br />
the Breast in 2005 at Women and Infants’ Hospital. He is board certified in general surgery. Dr.<br />
Edmonson is also a Fellow of the American College of Surgeons and is a member of numerous<br />
professional societies including the American Society of Breast Surgeons. Dr. Edmonson had<br />
been in private practice in Albany NY prior to returning to Providence. He returns to pursue fur-<br />
ther interests in teaching and research. His interests include genetically-based breast cancers<br />
and the prevention and treatment of lymphedema.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Steven I. Cohen, MD, FACS, joined the staff of the Breast Health Center in 1995. Dr. Cohen is<br />
a Clinical Assistant Professor in the Department of Surgery at <strong>Brown</strong> <strong>University</strong>. He received<br />
his medical degree in 1968 from Downstate Medical Center, Brooklyn, New York. He is board<br />
certified in general surgery. Dr. Cohen is a fellow of the American College of Surgeons and a<br />
member of numerous professional societies.<br />
Arnold H. Herman, MD, FACS, joined the staff of the Breast Health Center in 1995. Dr. Herman<br />
is a Clinical Associate Professor in the Department of Surgery at <strong>Brown</strong> <strong>University</strong>. He received<br />
his medical degree in 1966 from the <strong>University</strong> of Kansas and completed his surgical residency<br />
at Boston <strong>University</strong>. Dr. Herman is board certified in general surgery. He is a fellow of the<br />
American College of Surgeons and a member of numerous professional societies including the<br />
American Society of Breast Surgeons. He is a surveyor for the Commission on Cancer of the<br />
American College of Surgeons.<br />
R. James Koness, MD, joined the staff of the Breast Health Center in June 2004. Dr. Koness<br />
received his B.S. in Biology from Boston College in Chestnut Hill, Massachusetts in 1978 and<br />
his MD from SUNY–Buffalo School of Medicine, Buffalo, New York in 1983. He completed his<br />
internship and residency in general surgery at <strong>Brown</strong> <strong>University</strong> in 1988 and completed his<br />
fellowship in surgical oncology at Roger Williams Medical Center in 1990. He was an Instructor<br />
in Surgery at <strong>Brown</strong> <strong>University</strong> from 1987–1991 and is currently a Clinical Assistant Professor<br />
in the Division of Surgical Oncology, Department of Surgery, <strong>Brown</strong> <strong>University</strong>. Dr. Koness is<br />
a fellow of the American College of Surgeons and is a member of the Rhode Island Chapter of<br />
the American College of Surgeons, New England Surgical Society, Society of Surgical Oncol-<br />
ogy, American Society of Head and Neck Surgeons, and American Society of Breast Surgeons.<br />
Gabriela B. Masko, MD, joined the staff of the Breast Health Center in June 2003. She is cur-<br />
rently Clinical Assistant Professor of Radiation Medicine at <strong>Brown</strong> <strong>University</strong>, Division of Biol-<br />
ogy and Medicine and Clinical Instructor of Radiation Oncology at Tufts <strong>University</strong> School of<br />
Medicine. She received her B.A. in 1980 from Yale <strong>University</strong> and her medical degree in 1984<br />
from Tufts <strong>University</strong> School of Medicine. Dr. Masko is board certified in Radiation Oncology<br />
and a member of several professional societies.<br />
Kathy Radie-Keane, MD, joined the staff of the Breast Health Center in December 2005. She is<br />
currently Clinical Assistant Professor in Radiation Medicine at <strong>Brown</strong> <strong>University</strong>, Division of<br />
Biology and Medicine. She received her B.S., at Emmanuel College, 1980 Boston, MA and her<br />
medical degree in 1986 at Tufts <strong>University</strong> School of Medicine. Dr. Radie-Keane is board certi-<br />
fied in Radiation Oncology and a member of several professional societies.<br />
William M. Sikov, MD, joined the staff of the Breast Health Center in July 2003. He is principal<br />
investigator, CALGB, Rhode Island Hospital and Clinical Assistant Professor of Medicine at<br />
<strong>Brown</strong> <strong>University</strong> School of Medicine. Dr. Sikov received his A.B. in Russian Studies in 1978<br />
from <strong>Brown</strong> <strong>University</strong> and his medical degree in 1982 from Yale <strong>University</strong> School of Medi-<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 31<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
cine. He completed an internship and residency in Internal Medicine at the <strong>University</strong> Health<br />
Center, Pittsburgh, PA, in 1985 and a fellowship in Hematology–Oncology at the New England<br />
Medical Center, Boston, MA, in 1989. Dr. Sikov is board certified in Internal Medicine, Hematol-<br />
ogy, and Medical Oncology. He is a member of numerous professional societies and has major<br />
research interests in the treatment of breast cancer. He chairs the <strong>Brown</strong> <strong>University</strong> Oncology<br />
Group (BRUOG) Breast Cancer Committee.<br />
Rochelle Strenger, MD, is a Clinical Assistant Professor of Medicine at <strong>Brown</strong> <strong>University</strong> School<br />
of Medicine and a Medical Oncologist at the Breast Health Center for over 10 years. She re-<br />
ceived her BA in Biology from Barnard College in 1972 and MS from Columbia <strong>University</strong> in<br />
1978. She received her MD degree from Albert Einstein College of Medicine in 1982 and com-<br />
pleted her Internal Medicine residency at Brigham and Women’s Hospital in Boston in 1985.<br />
She then completed a Research/Clinical fellowship in the Division of Hematology/Oncology at<br />
the same hospital. Dr. Strenger is board certified in Medical Oncology and Internal Medicine.<br />
She is a member of numerous societies. Dr. Strenger was the 2009 recipient of the first Adele<br />
R. Decof Rose award for excellence in patient centered care. She was the recipient of the Amer-<br />
ican Medical Women’s Association Service Award in 1999 and was named RI Women Physician<br />
of the year in 2001. Her major interests are in Women’s Health and Breast Oncology.<br />
Charu Taneja, MD, joined the staff of the Breast Health Center in June 2004. She received her<br />
M.B., B.S. from Maulana Azad Medical College, <strong>University</strong> of Delhi, New Delhi, India in 1989.<br />
Dr. Taneja completed her residency in Surgery at L.N.J.P.N. Hospital, Maulana Azad Medical<br />
College, <strong>University</strong> of Delhi in 1993, and her residency in Surgery at the <strong>University</strong> of Medicine<br />
and Dentistry, New Jersey Medical School in 1999. Dr. Taneja completed her fellowship in Sur-<br />
gical Oncology at Boston <strong>University</strong> – Roger Williams Medical Center in 2001. She is currently<br />
Clinical Assistant Professor in the Department of Surgery, Boston <strong>University</strong> Medical Center,<br />
Boston, Massachusetts and Director of the Breast Health Program at Roger Williams Medical<br />
Center. Dr. Taneja is board certified by the American Board of Surgery. She is a member of the<br />
American College of Surgeons, Society of Surgical Oncology, Association of Women Surgeons,<br />
American Society of Clinical Oncology and Southeastern Surgical Congress.<br />
David E. Wazer, MD, joined the staff of the Breast Health Center in June 2003. He is currently<br />
Joint Professor and Chairman at Tufts <strong>University</strong> School of Medicine and <strong>Brown</strong> Medical<br />
School; Radiation Oncologist–in–Chief at Tufts Medical Center, Rhode Island Hospital, and<br />
Women & Infants Hospital of Rhode Island; and Chief of Radiation Oncology Services, Lifes-<br />
pan Healthcare System. Dr. Wazer received his A.B. (Honors) in 1978 from Holy Cross College<br />
in Worcester, Massachusetts, his Doctor of Medicine degree (Honors) in 1982 from New York<br />
<strong>University</strong> School of Medicine, New York, New York, and his Master of Arts honorary degree in<br />
1999 from <strong>Brown</strong> <strong>University</strong>. Dr. Wazer completed his internship in Medicine in 1983 at Roger<br />
Williams General Hospital, his research fellowship in the Department of Psychiatry Laboratory<br />
of Dr. John Rotrosen, New York <strong>University</strong> School of Medicine in 1984, his residency in Radia-<br />
tion Oncology in 1988 at New England Medical Center/Tufts <strong>University</strong>, and was chief resident<br />
in Radiation Oncology from 1987–1988 at New England Medical Center/Tufts <strong>University</strong>. He is a<br />
member of numerous societies and has major research interests.<br />
32<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
PROGRAM HIGHLIGHTS<br />
Dr. McCourt had a featured article for the Gynecologic Oncology Group section of the Summer<br />
2009 issue of Women and Cancer Magazine (Womenandcancermag.com). The article was titled<br />
Lymphedema and Gynecologic Cancers.<br />
Courtney Dieterich, OSW-C, received her Oncology Social Work certification.<br />
Dr. Granai was the keynote speaker at the First <strong>Annual</strong> Ovarian Cancer Research Fund’s Super Lun-<br />
cheon, hosted by First Lady Suzanne Carcieri, at the <strong>University</strong> Club, Providence RI, on September<br />
9, 2009.<br />
On October 30, 2009, the Breast Health Center held a BHC Fair “Inside the Breast Health Center,<br />
a Place for Health, Wellness and Healing.” Speakers included Dr. Gass, who gave a presentation<br />
titled “New Surgical Options, Including Nipple Sparing Mastectomy and Oncoplastics”; Dr. Legare,<br />
who gave a presentation titled “A Unique Approach to Care”; Dr. Pandya, whose talk was titled “A<br />
Fellow’s Perspective on Care, High-Risk, and Screening; and Lauren Solomon, RD, LDN, who gave<br />
a presentation titled “Nutrition for Breast Health.” Social Work participated, and Integrative Care<br />
Therapies, Promotional Items, and other information on the Breast Health Center were provided.<br />
Dr. Gass was an invited guest speaker at the Festival Ballet “Legacy of Loss”. She gave a presenta-<br />
tion titled “A New Legacy of Knowledge, Choice and Beauty” on October 18 th at the Festival Ballet,<br />
Providence RI.<br />
November 13 – 14, 2009, Dr. Granai and Dr. Moore presented at the 3 rd Asia Pacific Congress: Con-<br />
troversies in Obstetrics, Gynecology, & Infertility, Shangri-La’s Kerry Centre Hotel, Beijing, China. The<br />
conference was attended by over 500 international physicians, healthcare leaders, and administrators.<br />
Dr. Granai participated in the following:<br />
• Invited Speaker: Pelvic mass in pregnancy: When Do We Need to Intervene?<br />
• Dr. Granai served as Chairperson and as a discussant on the following topic: Hot Contro-<br />
versies – Expert Opinion on: Cervical Cancer and Human Papilloma Virus (HPV): Does Vac-<br />
cination Mark the End of Cervical Cancer?<br />
• Dr. Granai was the Keynote Speaker for “VOICES” – Special Entertainment Lecture.<br />
Dr. Moore participated in the following:<br />
• Chairperson – Women and Ovarian Cancer: From Conception to Diagnosis “Early Diagnosis<br />
of Ovarian Cancer Can Improve Prognosis<br />
• Dr. Moore served as a discussant on the following topic: Hot Controversies – Expert Opinion<br />
on: Cervical Cancer and Human Papilloma Virus (HPV): Does Vaccination Mark the End of<br />
Cervical Cancer?<br />
January 12, 2009, Dr. Legare was listed in RI Monthly as one of the Top Docs for Medical Oncology.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 33<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
Dr. Granai was selected as one of America’s Top Doctors for Cancer by Castle Connelly, the na-<br />
tion’s leading source of identifying top doctors for 2009.<br />
Dr. Granai was accepted as a Fellowship Candidate by the American Gynecological and Obstetri-<br />
cal Society (AGOS).<br />
Dr. Brard was appointed as a committee member in Experimental Medicine, Gynecologic Oncol-<br />
ogy Group – January 2010<br />
Dr. Paul Disilvestro was named Co-Chairman of the Ovarian Cancer Committee for the Gyneco-<br />
logic Oncology Group (GOG).<br />
Dr. Granai was voted “Best Doctor in Rhode Island” (Gynecologic Oncology) by Rhode Island<br />
Monthly Magazine, May 2010<br />
On June 29, 2010, Dr. Gass attended the RI American Cancer Society <strong>Annual</strong> Membership Meeting<br />
where she will be inducted as the New Secretary Treasurer for the RI American Cancer Society.<br />
Cain, JM<br />
K12 HD050108-06<br />
10/1/08 – 3/31/15<br />
(Principal Investigator)<br />
$2,200,000 Grant total<br />
Women’s Reproductive Health Research<br />
Career Development Award<br />
1R01CA136491-01A1<br />
Brard L (PI)<br />
6/1/2009- 4/30/2014<br />
NCI/NIH<br />
$ 2,753,225 (TC)<br />
34<br />
GRANTS<br />
Development of an Assay for the Early Detection of Ovarian Cancer.<br />
Ovarian cancer is on of the most lethal cancers affecting women. This is due to the inability to<br />
detect it while still localized to the ovaries. Early detection would result in a 90% survival rate. LPA,<br />
a currently controversial biomarker for ovarian cancer diagnosis, is the subject of this application.<br />
A simple new method for detecting LPA and a fresh approach to validating LPA’s reliability as an<br />
accurate biomarker would emanate from the proposed studies. Role: PI<br />
The Integrative Care Program had a prestigious visit from the RI Foundation, which is now considering<br />
awarding the program a $75,000 grant. Funds would be utilized in part to broaden outreach<br />
and expand education about the potential benefits of integrating complementary approaches<br />
into the cancer care continuum.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
5P41RR001395 - Supplemental<br />
Smith P (PI)<br />
10/01/09 - 09/30/11<br />
NIH/NCRR<br />
BioCurrents Research Center - Mechanisms of Cisplatin Resistance in Ovarian Cancer<br />
The major goals of this project are to understand the genetic and phenotypic differences between<br />
primary and metastatic ovarian cancer growths that may affect therapeutic response. We expect<br />
to genotype each tumor and match the genetic differences to drug response phenotypes including<br />
probing cisplatin sensitivity relative to the regulation of drug efflux systems.<br />
Role: Significant Contributor (Brard L)<br />
RI Research Alliance 2010 Collaborative Research Grants<br />
Brard L (PI)<br />
Submitted October 2009<br />
Genetics of Primary and Metastatic Ovarian Cancer: Towards Personalized Therapies<br />
NCI/NIH R21CA143667-01A1<br />
Brard L (PI)<br />
Submitted November 2009<br />
Cranberry Extracts for the Treatment of Ovarian Cancer.<br />
2010- A Phase II Trial of Belinostat and Carboplatin in Platinum-Resistant Ovarian Cancer (GOG<br />
126-T). Gynecologic Oncology Group, NCI Grant/Contract U10-CA27469.<br />
2010- A Phase I Trial of Intraperitoneal Bortezomib and Carboplatin in Recurrent Ovarian Cancer<br />
(GOG 9924). Gynecologic Oncology Group, NCI Grant/Contract U10-CA27469.<br />
2010- National cancer Institute, Grant R21CA137290-01A2. Social Networks<br />
and Care Planning in Women with Cancer. Amount: $250,000. PI: Melissa A. Clark; Co-PI: Don S.<br />
Dizon.<br />
ORIGINAL PUBLICATIONS IN<br />
PEER-REVIEWED JOURNALS<br />
Sakr B J, Dizon D S, Legare R, Gamage M, Wood R, Colvin G A, Constantinou M, Kennedy<br />
T A, Fenton M, Sikov W M; Women and Infants Hospital, Providence, RI; Alpert Medical<br />
School of <strong>Brown</strong> <strong>University</strong>. Frequent pathologic complete responses in aggressive stages II to<br />
III Breast Cancers with every-4-week Carboplatin and weekly Paclitaxel with or without Trastuzumab:<br />
A <strong>Brown</strong> <strong>University</strong> Oncology Group Study. J Clin Oncol, 2009 Oct 1;27(28):693-700.<br />
Rizack T, Mega A, Legare R, Castillo J. Management of hematological malignancies during<br />
pregnancy. Am J Hematol. 2009 Sept 16;84(12):830-841.<br />
Robison K, MD. Guidance for Cervical Cancer Prevention and Control: LEEP/Cervical Cone. International<br />
Federation of Gynecology & Obstetrics. October 2009<br />
Clements A, Robison K, Granai C O, Margaret M M, Wilbur-Scalia J, and Moore R G. A Case<br />
of Peutz Jeghers Syndrome with Breast Cancer, Bilateral Sex Cord Tumor with Annular Tubules<br />
and Adenoma Malignum caused by STK11 Gene Mutation. International Journal of Gynecologic<br />
Oncology . Dec 2009; 19 (9): 1591-4<br />
McCourt C, Dessi S, Bradley A M, Schwartz J, Brard L, Dizon D S. Is there a taxane-free interval<br />
that predicts response to taxanes as a later-line treatment of recurrent ovarian or primary<br />
peritoneal cancer? Int J Gynecol Cancer, 2009; 19: 343-7.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 35<br />
G y n e c o l o g i c O n c o l o g y
G yy nn e c o l o g i c O nn cc oo l o g y<br />
Gray D L, Dicke J M, Dickerson R, McCourt C, Obibo A O. “Reevaluating humeral length for the<br />
detection of fetal trisomy 21.” J Ultrasound Medicine, 2009; 28:1325-30.<br />
Hensley M, Sill M, Scribner D, <strong>Brown</strong> J, DeBernardo R, Hartenbach E, McCourt C K, Bosscher J,<br />
Gehrig P. “Sunitinib Malate in the treatment of recurrent or persistent uterine leiomyosarcoma:<br />
A Gynecologic Oncology Group phase II study.” Gynecol Oncol, 2009; 115:460-5.<br />
Moore R G, McMeekin S D, <strong>Brown</strong> A K, DiSilvestro P A, Miller C M, Allard J W, Gajewski W,<br />
Kurman R J, Bast R C, Skates S J.: “A Novel Multiple Marker Bioassay Utilizing HE4 and CA125<br />
for the Prediction of Ovarian Cancer in Patients with a Pelvic Mass.” Gynecologic Oncology,<br />
112(1): 40-6, 2009.<br />
Mathews C, Restivo A, Raker C, Weitzen S, DiSilvestro P A: “Willingness of Gynecologic Cancer<br />
Patients to Participate in Clinical Trials.” Gynecologic Oncology, 112(1): 161-5, 2009.<br />
Walker J L, Morrison A, DiSilvestro P A, VonGruenigen V E: “A phase I/II study of extended<br />
field radiation therapy with concomitant paclitaxel and cisplatin chemotherapy in patients with<br />
cervical carcinoma metastatic to the para-aortic lymph nodes: A gynecologic oncology group<br />
study.” Gynecologic Oncology, 112 (1): 78-84, 2009.<br />
Rardin C R, Moore R G, Ward R M, Myers D L. Recurrent thigh abscess with necrotizing fasciitis<br />
from a retained transobturator sling segment. Journal of Minimally Invasive Gynecology, 2009,<br />
16(1), 84-87<br />
Kuroki L, Stuckey A, Hirway P, Raker C, Bandera C, DiSilvestro P A, Granai C O, Legare<br />
R D, Sakr B, Dizon D S. “Addressing clinical trials: Can the Multidisciplinary Tumor Board<br />
improve participation? A study from an academic women’s cancer program”. Article In Press.<br />
G ynecol Oncol 2009<br />
Allard J W and Moore R G. The novel biomarker HE4 improves the sensitivity of CA125 alone<br />
for monitoring and differential diagnosis of ovarian cancer. Clinical Laboratories International,<br />
2009, 3, 20-21<br />
Erekson E A, Sung V W, DiSilvestro P A, Myers D L: “Urinary Symptoms and impact on quality<br />
of life in women following treatment for endometrial cancer.” International Urogynecology<br />
Journal, 20(2): 159-63, 2009.<br />
Shah N, Dizon D S. New generation platinum agents for solid tumors. Future Medicine 2009;<br />
5:33-42.<br />
Schwartz J, Toste B, Dizon D S. Chemotherapy toxicity in gynecologic cancer patients with a<br />
body surface area (BSA) > 2m(2). Gynecol Oncol 2009; 114:53-6.<br />
Dizon D S, Blessing J A, McMeekin D S, Sharma S K, DiSilvestro P A, and Alvarez R D. Ixabepilone<br />
as a second-line treatment in advanced endometrial cancer: Phase II Results of Gynecologic<br />
Oncology Group Trial 129-P. J Clin Oncol 2009; 27:3104-08.<br />
Dizon D S. Quality of life after breast cancer: survivorship and sexuality. The Breast Journal.<br />
2009; 15:500-4.<br />
Dizon D S, Perez K, DiSilvestro P A, Taneja C, Ilson D. Stage IV small bowel carcinoma mimicking<br />
advanced ovarian cancer: case report and review of the literature. American Surgeon 2009;<br />
75:864-5.<br />
Sikov W M, Dizon D S, Strenger R, Legare R D, Theall K P, Graves T A, Gass J S, Kennedy<br />
T A, and Fenton M A. Frequent pathologic complete responses in aggressive stage II-III breast<br />
cancers with q4week carboplatin and weekly paclitaxel + trastuzumab: a <strong>Brown</strong> <strong>University</strong> Oncology<br />
Group study. J Clin Oncology 2009; 27:4693-700.<br />
36<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Dizon D S, Schutzer M E, Politi M, Linkletter C, Miller S, Clark M A. Advance Care Planning<br />
Decisions of Women with Cancer: Provider Recognition and Stability of Choices. J Psychosocial<br />
Oncology 2009; 27:383-95.<br />
Bandera C A and Magrina J F. Robotic surgery in gynecologic oncology. Curr Opin<br />
Obstet and Gynecol 2009,21: 25-30.<br />
Stuckey A, Dizon D S, Scalia Wilbur J, Kent J, Tejada-Berges T, Gass J, Legare R.; Clinical<br />
characteristics and choices regarding risk-reducing surgery in BRCA mutation carriers.“ Gynecol<br />
Obstet Invest. 2010 Jan 21;69(4):270-273 [Epub ahead of print]<br />
Tung N, Wang Y, Collins L C, Kaplan J, Li H, Gelman R, Comander A H, Gallagher B, Fetten K,<br />
Krag K, Stoeckert K A, Legare R D, Sgroi D, Ryan P D, Garber J E, Schnitt S J. Estrogen receptor<br />
positive breast cancers in BRCA1 mutation carriers: clinical risk factors and pathologic<br />
features.; Breast Cancer Res. 2010 Feb 11;12(1):R12; Breast Cancer Res. 2010 Feb 11;12(1):R12.<br />
Krotz S P, Robins J C, Ferruccio T M, Moore R G, Steinhoff M M, Morgan J R, Carson S. In vitro<br />
maturation of oocytes via the pre-fabricated self-assembled artificial human ovary. Journal of<br />
Assisted Reproductive Genetics, Published online: 8/25/2010 DOI 10.1007/s10815-010-9468-6<br />
Kuroki L, Stuckey A, Hirway P, Raker C A, Bandera C, DiSilvestro P A, Granai C O, Legare R<br />
D, Sakr B J,Dizon D S. Addressing clinical trials: can the multidisciplinary tumor board improve<br />
participation? A study from an academic women’s cancers program. Gynecologic Oncology. 2010;<br />
116:295-300.<br />
Penson R, Dizon D S, Cannistra S, Roche M, Krasner C, Berlin S, Horowitz N, DiSilvestro P A,<br />
Matuonis U, Lee H, King M, Campos S: “Phase II Study of Carboplatin, Paclitaxal, and Bevacizumab<br />
with Maintenance Bevacizumab as First-Line Chemotherapy for Advanced Mullerian Tumors.”<br />
Journal of Clinical Oncology, 28(1): 154-59, 2010.<br />
Fleming G, Sill M, Darcy K, McMeeking D, Thigpen J, Adler L, Berek J, Chapman J, DiSilvestro<br />
P A, Horowitz I, Fiorica J: “Phase II Trial of Trastuzumab in Women with Advanced or<br />
Recurrent, HER2-Positive Endometrial Carcinoma: A Gynecologic Oncology Group Study.”<br />
Gynecologic Oncology, 116(1): 15-20, 2010.<br />
Moore R G, MacLaughlan S, Bast R C. Current state of biomarker development for clinical application<br />
in epithelial ovarian cancer. Gynecologic Oncology, 2010, 116, 240-245<br />
Moore R G, MacLaughlan S. Clinical use of Biomarkers for Epithelial Ovarian Cancer. Current<br />
Opinion in Oncology, 2010, 22, 492-497<br />
Moore R G, Jabre-Raughley M, <strong>Brown</strong> A K, Robison K M, Miller M C, Allard W J, Kurman R J,<br />
Bast R C, Skates S J. Comparison of a Novel Multiple Marker Assay Versus the Risk of Malignancy<br />
Index for the Prediction of Epithelial Ovarian Cancer in Patients with a Pelvic Mass. The American<br />
Journal of Obstetrics and Gynecology, 203, 3, 228.e1 – 228.e6doi: 10.1016/j.ajog.2010.03.043<br />
Makhija S, Amler L C, Glenn D, Ueland F, Gold M, Dizon D S, Paton V, Birkner M, Lin C Y, Januario<br />
T, Ng K, Strauss A, Slikowski M, U Matulonis. Clinical Activity of Gemcitabine Plus Pertuzumab<br />
in Platinum-Resistant Ovarian Cancer, Fallopian Tube, or Primary Peritoneal Cancer: Low MRNA<br />
expression of the HER2-Coreceptor HER3 May be Predictive of Pertuzumab Activity. J Clin Oncol<br />
2010; 28:1215-23.<br />
Stuckey A, Dizon D S, Legare R D, Scalia-Wilbur J, Kent J, Tejada-Berges T, Gass J.<br />
Clinical characteristics and choices regarding prophylactic surgery in BRCA mutation carriers.<br />
Gynecologic and Obstetric Investigation. 2010; 69:270-73.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 37<br />
G y n e c o l o g i c O n c o l o g y
G yy nn e c o l o g i c O nn cc oo l o g y<br />
Stuckey A, Dizon D S, Scalia-Wilbur J, Kent J, Tejada-Berges T, Gass J, Legare R et al.<br />
Clinical Characteristics and Choices regarding Risk-reducing Sugery in BRCA Mutation Carriers.<br />
Gynecologic and Obstetric Investigation. 2010;69:270-273.<br />
38<br />
BOOKS AND BOOK CHAPTERS<br />
Cain JM. Principles of Patient Care. Novak’s Gynecology, 15th Edition Berek, J (ed) Lippincott<br />
Williams & Wilkins, 2010.<br />
Dizon D S and Krychman M. Sexuality. In: Principles & Practice of Cancer Rehabilitation. M<br />
Stubblefield, M O’Dell, C Custodio, and T Fitzpatrick, Eds. New York: Demos. 2009.<br />
Krychman M A, Dizon D S, Amsterdam A, Partridge A. Cancer and Dyspareunia. In: Female<br />
Sexual Pain Disorders: Evaluation and Management. Goldstein, Pukall, and Goldstein, Eds.<br />
Towson:Blackwell. In Press, 2009.<br />
Stuckey A, Dizon D S. Choosing Treatments for Recurrent Ovarian Cancer: The Platinum-Free<br />
Interval. In Textbook of Gynaecological Oncology. Eds: A Ayhan, M Gultekin, P Dursun. Turkey:<br />
Gunes Publishing, 2009.<br />
Dizon D S, Tejada-Bergés T, Steinhoff M M, Sung C J, Koelliker S, Khalil H I, O’Conner B, MacAusland<br />
S, Taneja C, Legare R D, and Gass J S. Breast Cancer. In: Principles and Practice of<br />
Gynecologic Oncology, 5 th Edition pp.897-946 RR Barakat, M Markman, ME Randall, EDS.Baltimore:<br />
Lippincott, Williams & Wilkins 2009.<br />
Stuckey A, Dizon D S. Choosing treatments for recurrent ovarian cancer: the platinum-free<br />
interval. The European Society of Gynecologic Oncologists’ Handbook for Fellows in Gynecologic<br />
Oncology. M. Gultekin, Ed. 2009.<br />
Questions and Answers About Human Papilloma Virus. Krychman M A, Dizon D S. Sudbury M<br />
A: Jones and Bartlett, 2010.<br />
DxRx Gynecologic Cancers. Campos S M, Dizon D S, Sudbury M A: Jones and Bartlett, 2010.<br />
Questions and Answers About Uterine Cancer. Duska L R, Dizon D S, Sudbury M A: Jones and<br />
Bartlett, 2010.<br />
DxRx Cervical Cancer: An approach to preinvasive and invasive malignancies of the cervix. Second<br />
Edition. Robison K, Dizon D S, Sudbury M A: Jones and Bartlett, 2010.<br />
OTHER PEER-REVIEWED PUBLICATIONS<br />
Bowling, K, Cain JM. Clinical Educators: How can we meet the expanding need. Women’s<br />
Healthcare, Training the Next Generation of Women’s Healthcare Physicians. Changing Landscape<br />
in Academic Obstetrics and Gynecology. William F. Rayburn/Jay Schulkin (eds) Springer, 2010.<br />
Cain JM, Dickens et al. Bioethics Curriculum in Women’s Reproductive and Sexual Rights. International<br />
Federation of Gynecology and Obstetrics (FIGO), London UK, 2010.<br />
Lange T S, Stuckey A, Robison K, Kim K K, Singh R K, Raker C A, Bard L. “Effect of a Vitamin<br />
D3 derivative (B3CD) with postulated anti-cancer activity in an ovarian cancer animal model”.<br />
Invest New Drugs. 2009 Jul 7.<br />
Singh R, Lange T S, Kim K K, Brard L. “A coumarin derivative (RKS262) inhibits cell-cycle progression,<br />
causes pro-apoptotic signaling and cytotoxicity in ovarian cancer cells”. Invest New<br />
Drugs. 2009 Oct 29. [Epub ahead of print].<br />
Kunz M A, Dizon D S. “Sexuality and intimacy following cancer”. US Obstetrics & Gynecology<br />
2009; 3:21-23.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Dizon D S and Gass J S. “Perspective: Help or harm: Adjuvant therapies for primary invasive<br />
disease and the risk of a second contralateral breast cancer”. Am Journal of Hemat and Oncol<br />
2009; Available at: http://www.ajho.com/Help-or-harm-Adjuvant-therapies-for-primary-invasivedisease-and-the-risk-of-asecond-contralateral-breast-cancer/article/141443/.<br />
Perez K, Gadgil M, Dizon D S. “Sexual ramifications of medical illness”. Clinics of Obstetrics<br />
and Gynecology 2009; 52:691-701.<br />
Lange T S, McCourt C, Singh R K, Kim K K, Singh A P, Luisi B S, Alpturk O, Strongin R, Brard L.<br />
“Apoptotic and chemotherapeutic properties of Iron(III)-salophene in an ovarian cancer animal<br />
model”. Drug Design, Development and Therapy:3 17-26 (2009).<br />
Saulnier Sholler G L, Brard L, Straub J A, Dorf L, Illyene S, Kalkunte S, Bosenberg M, Ashikaga<br />
N, Nishi R. “Nifurtimox Induces Apoptosis of Neuroblastoma Cells in Vitro and in Vivo”. J Pediatr<br />
Hematol Oncol. 31(3):187-193 (2009).<br />
Kawar N, Dizon D S. “Ixabepilone as a second-line treatment in advanced endometrial cancer”.<br />
Asian-Pacific Journal of Hematology and Oncology 2010. Epub online 2/2010.<br />
Moore R G, MacLaughlan S D, Bast R C Jr. “Current state of biomarker development for clinical<br />
application in epithelial ovarian cancer”. Gynecol Oncol. 2010 Feb;116(2):240-5.<br />
Lange T S, Zou Y, Singh R, Kim K, Kristjansdottir K, Saulnier-Sholler G L, Brard L. “Chemotherapeutic<br />
Effect of Calcidiol Derivative B3CD in a Neuroblastoma Xenograft Model”. In Press<br />
Chemical Biology & Drug Design, (April 2010).<br />
Kim K, Lange T S, Singh R, Brard L. “Lipophilic aroylhydrazone chelator HNTMB and its multiple<br />
effects in ovarian cancer cells”. BMC Cancer 10:72 (2010).<br />
Kristjansdottir K, Dizon D S. “HER-Dimerization Inhibitors: Evaluating pertuzumab in women’s<br />
cancers”. Expert Opinion on Biologic Therapy. 2010; 10:243-50.<br />
Dizon D S. “Treatment options for advanced endometrial cancer”. Gynecologic Oncology 2010;<br />
117:373-81.<br />
OTHER NON-PEER REVIEWED PUBLICATIONS<br />
Dwork A J, Christensen J R, Larsen K B, Scalia J, Underwood M D, Arango V, Pakkenberg B,<br />
Lisanby S H. “Unaltered neuronal and glial counts in animal models of magnetic seizure therapy<br />
and electroconvulsive therapy”, Neuroscience. 2009 Dec 29; 164(4):1557-64. Epub 2009 Sep 25.<br />
Moore R G, MacLaughlan S D. “A novel approach for the risk assessment of a pelvic mass for<br />
ovarian cancer”. The Female Patient, September 2009.<br />
Hachey K Dizon D S. “Personalizing chemotherapy through genetic profiling: will pharmacogenomics<br />
help improve and extend life for cancer patients?” Personalized Medicine, 2009; 6:481-4.<br />
Robison K, Dizon D S. “Cervical Cancer RX and DX”. Glasko-Smith-Klein. 2 nd edition 2010<br />
SCHOLARLY WORK IN OTHER MEDIA<br />
Dr. Sakr participated in an interview with Channel 10 on the need for patients to enroll in cancer<br />
research studies on August 3, 2009, Breast Health Center/ Women & Infants Hospital, Providence,<br />
Rhode Island.<br />
Dr. McCourt had a featured article for the Gynecologic Oncology Group section of the Summer<br />
2009 issue of Women and Cancer Magazine (Womenandcancermag.com). The article was titled<br />
Lymphedema and Gynecologic Cancers.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 39<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
Dr. Legare participated in an interview with Channel 10 to discuss the “Hereditary Breast and<br />
Ovarian Cancer: BRCA Testing and Beyond” Symposium; September 24, 2009.<br />
Dr. Sakr participated in an interview with Channel 6, discussing the new guideline and<br />
Recommendation around breast cancer screening on November 7, 2009, Breast Health Center/<br />
Women & Infants Hospital, Providence, Rhode Island.<br />
Dr. Legare was interviewed by the Jewish Voice & Herald for a story on the breast cancer<br />
screening controversy – November 19, 2009<br />
Dr. Legare gave a mammography position statement to <strong>Brown</strong> <strong>University</strong>, WIH, and Pharmawire<br />
– December 2009.<br />
Dr. Sakr interviewed at Channel 10 studios “Special Assignment” on January 7, 2010, discussion<br />
about new mammogram, screening guidelines, Cranston, Rhode Island.<br />
Dr. Legare participated in an interview on breast cancer for HEALTH magazine, a national<br />
publication – January 29, 2010<br />
Dr. Moore participated in a video education taping for The Institute for Continuing Healthcare<br />
Education Regarding Ovarian Cancer Screening and Management to Improve Patient Survival,<br />
Houston TX – February 5, 2010.<br />
Dr. Legare had a commentary in the March issue of the <strong>Brown</strong> Medicine Magazine entitled<br />
“Check Yourself – What to do About Cancer Screening” – March, 2010<br />
LOCAL/REGIONAL<br />
40<br />
ABSTRACTS<br />
Cronin B, Robison K, Moore R, Dizon D S. Long-term use of Pegylated Liposomal Doxorubicin<br />
in recurrent ovarian carcinoma. Oral Presentation at New England Association of Gynecologic<br />
Oncologist <strong>Annual</strong> Conference, Cape Cod 2009.<br />
Fischer A, Kristjansdottir K, MacLaughlan S, Brard L, Brodsky A. Identifying metastatic microRNAs<br />
in ovarian cancer. Ovarian Cancer Research Symposium at <strong>Brown</strong> <strong>University</strong>. February<br />
5, 2010.<br />
Malit B, MacLaughlan S, Dizon D S. Cancer patients and complementary and alternative medicine:<br />
barriers to enrollment in clinical trials. New England Association of Gynecologic Oncologists<br />
(NEAGO) <strong>Annual</strong> Meeting, June 12, 2010, Boothbay Harbor, ME.<br />
Roque D, MacLaughlan S, Tejada-Berges T. Patient death after a core needle biopsy of the<br />
breast: a case report. New England Association of Gynecologic Oncologists (NEAGO) <strong>Annual</strong><br />
Meeting, June 12, 2010, Boothbay Harbor, ME.<br />
Pandya S V, Dizon D S, Gass J S, Hansen K, Raker C “ Management of Intraductal Papiloma<br />
– a clinical dilemma”. New England of Gynecologist Oncology <strong>Annual</strong> Meeting; June 11, 2010,<br />
Boothbay Harbor, ME.(Oral Presentation)<br />
Wu L, Robison K, Eng W, Douangsavanh A, Tejada-Berges T, Clark L, Raker C, S Pinto Granai C<br />
O, Dizon D S. Cervical Cancer Prevention: Participation and knowledge among Asian American<br />
women. Oral presentation at the New England Association of Gynecologic Oncologist <strong>Annual</strong><br />
Conference, BoothBay Harbor, ME, June 2010<br />
Holman L L, Robison K, Lopes V V, Noto R, Steinhoff M, Moore R. A comparison of sentinel<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
lymph node identification between lymphoscintigraphy and sentinel lymph node dissection in<br />
patients with vulvar cancer. Oral presentation at the 30 <strong>Annual</strong> Meeting NEAGO conference in<br />
Booth Bay Harbor, ME, June 2010.<br />
Kawar N M, Kilfoyl K, Raker C, Lomme M, Dizon D S. Class III Beta-Tubulin Expression in Endometrial<br />
Carcinoma. Oral presentation of the 30 th <strong>Annual</strong> Meeting of the New England Association<br />
of Gynecologic Oncologists (NEAGO). June 11-13, 2010, Boothbay Harbor, ME.<br />
Kawar N M, Tsai K, Dizoglio J, Dizon D S, Tsiapali E S. Reconstruction Trends Among Patients<br />
Undergoing Mastectomy for Breast Cancer Treatment or Prophylaxis. Oral presentation of the<br />
30 th <strong>Annual</strong> Meeting of the New England Association of Gynecologic Oncologists (NEAGO). June<br />
11-13, 2010, Boothbay Harbor, ME.<br />
Wu L, Robison K M, Eng W, Douangsavanh A, Tejada-Berges T, Clark L, Raker C, Pinto S, Granai<br />
C O, Dizon D S. Cervical cancer prevention: participation and knowledge among Asian-American<br />
women. New England Association of Gynecologic Oncologist (NEAGO) <strong>Annual</strong> Meeting, June<br />
13, 2010, Boothbay Harbor, ME.<br />
Hollman L L, Robison K M, Lopes V V, Steinhoff M, Moore R G. A comparison of sentinel lymph<br />
node identification between lymphoscintigraphy and sentinel lymph node dissection in patients<br />
with vulvar cancer. New England Association of Gynecologic Oncologists annual meeting, Booth<br />
Bay Harbor, Maine, June 11-13, 2010<br />
Jackson A L, Miller C, Bast R C, Lambert-Messerlian G, Moore R G. Descriptive analysis of HE4<br />
in healthy women, pregnancy and women with benign gynecologic disorders.<br />
New England Association of Gynecologic Oncologists annual meeting, Booth Bay Harbor, Maine,<br />
June 11-13, 2010<br />
Jackson A L, Miller C, Eklund E, Lambert-Messerlian G, Moore R G. A novel biomarker for the<br />
management of patients with epithelial ovarian cancer. New England Association of Gynecologic<br />
Oncologists annual meeting, Booth Bay Harbor, Maine, June 11-13, 2010<br />
Kawar N W, Tsai K, Dizoglio J, Dizon D S, Tsiapali E V. Reconstruction Trends Among Patients<br />
Undergoing Mastectomy for Breast Cancer Treatment of Prophylaxis….30 th <strong>Annual</strong> Meeting<br />
NEAGO conference in Booth Bay Harbor, ME…June 2010<br />
NATIONAL<br />
Sakr B J, Dizon D S, Legare R D, Gamage M, Wood R, Colvin G A, Constatinou M, Kennedy T<br />
A, Fenton M, Sikov W M. Adjuvant therapy after neoadjuvant: Addressing the needs of a highrisk<br />
group. 2009 Breast Cancer Symposium. San Francisco, CA abstr 358. October 7-10, 2009.<br />
Sikov W M. Adjuvant therapy after neaodjuvant treatment: Addressing the needs of a high-risk<br />
group. 2009 Breast Cancer Symposium. San Francisco, CA; abstr 358. October 7-10, 2009.<br />
Wu L, Dizon D S, Santiago E, Hirway P, Koness R J, Gass J S, Taneja C. The incidence of abnormal<br />
pathologic findings in women undergoing elective breast reduction. 2009 Breast Cancer<br />
Symposium. San Francisco, CA; abstr 12. October 7-10, 2009.<br />
Singh A P, Singh R K, Kim K K, Shah S, Brard L, Vorsa N. LC-MS-MS quantification of cyclophosphamide<br />
SMSKCNR cells in absence and presence of cranberry proanthocyanidins. Eastern<br />
Analytical Symposium, November 16-19, 2009, Somerset NJ.<br />
Kent J, Scalia-Wilbur J, Legare R, Development of a Discussion/Education Group for BRCA<br />
Mutation Carriers in a High Risk Clinic: An Assessment of Patient Interest, Expectations, and<br />
Needs. NSGC 28 th <strong>Annual</strong> Education Conference; Abstract Poster presentation, November<br />
2009, Atlanta GA<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 41<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
Ferlatte C, Scalia-Wilbur J, Kent J, Legare R, Patient Perspectives on an Appropriate Time For<br />
Cancer Genetic Counseling and BRCA Testing For Women Diagnosed With Breast Cancer. NSCG<br />
28 th <strong>Annual</strong> Education Conference; Abstract Platform Presentation, November 2009, Atlanta GA<br />
Figueredo N, Gass J S, Dizon D S, LaChance J, Reiker C. “Accuracy of office-based ultrasound<br />
guided needle biopsies performed by dedicated breast surgeons”. Poster, San Antonio Breast<br />
Symposium. December 13, 2009, San Antonio, TX.<br />
Scalia-Wilbur J S, Kent J, Legare R, Uterine Papillary Serous Carcinoma in a BRCA2 Non<br />
Ashkenazi Jewish Founder Mutation Carrier: A Case Study. National Consortium of Breast Cancers<br />
2009 Conference; Poster Presentation, 2009, Las Vegas NV<br />
Hachey K, Scalia-Wilbur J, Kent J, Legare R D, BRCA Carrier Status, Phenotype and Medical<br />
Decision-Making Among Hispanic BRCA Positive Women. National Consortium of Breast Centers<br />
2009 Conference, Abstract Platform Presentation, 2009, Las Vegas NV<br />
Sikov W, Dizon D S, Strenger R, Legare R, Theall K, Graves T, Gass J, Kennedy T, Fenton<br />
M; Frequent Pathologic Complete Responses In Aggressive Stage II-III breast cancers with<br />
q4week carboplatin and weekly paclitaxel ± trastuzumab: a <strong>Brown</strong> <strong>University</strong> Oncology Group<br />
Study, 2009.<br />
Olson C, Dizon D S, Stuckey A, MacLauglin S, Sakr B, Brard L, Legare R D. Outcomes for<br />
Women with Cancer receiving Bevacizumab in an Academic Women’s Oncology Program. SGO<br />
41 st <strong>Annual</strong> Meeting on Women’s Cancer. San Francisco, CA. March 14-17, 2010.<br />
Olson C, Dizon D S, Kristjandottir K, Kawar N, Bandera C, Sakr B, Legare R D, DiSilvestro<br />
P A. Tumor Marker Response in Women Treated with Bevacizumab. SGO 41 st <strong>Annual</strong> Meeting<br />
on Women’s Cancer. San Francisco, CA. March 14-17, 2010.<br />
Stuckey A , Kim K K, Singh R K, Fischer A, Miller D, Hillenmeyer S, Ritz A, Raphael B, Brodsky<br />
A S, Brard L. Developing an Integrated Genomic Approach to Explore the Antitumor Activity of<br />
Vitamin D and Derivatives to Treat Ovarian Cancer. 41st <strong>Annual</strong> Meeting of the Society of Gynecologic<br />
Oncologists, San Francisco, CA, March 14-17, 2010.<br />
Horowitz N, Olawaiye A, Growdon W, Borger D, Dizon D S, Brard L, Matulonis U, MacNeill K,<br />
Roche M, Krasner C. Phase II Trial of Tarceva (erlotinib) in Women with Squamous Cell Carcinoma<br />
of the Vulva. 41st <strong>Annual</strong> Meeting of the Society of Gynecologic Oncologists, San Francisco, CA,<br />
March 14-17, 2010.<br />
Holman L L, Robison K, Lopes V V, Noto R, M. Steinhoff, Moore R. A comparison of sentinel<br />
lymph node identification between lymphoscintigraphy and sentinel lymph node dissection in<br />
patients with vulvar cancer. Poster presentation at the Society of Gynecologic Oncologists. San<br />
Francisco, March 2010.<br />
Robison K, Wu L, Eng W, Douangsavanh A, Tejada-Berges T, Raker C, Pinto S, Dizon D S.<br />
Cervical Cancer Prevention: Participation and knowledge among Asian American women. Poster<br />
presentation at American Society for Colposcopy and Cervical Pathology (ASCCP). Las Vegas,<br />
March 2010.<br />
Chan J K, Kawar N M, Shin J Y, Osann K, Kapp D S, Chen L M. Demographic and Clinical Characteristics<br />
in Women Diagnosed with Uterine Sarcoma. Poster of the 41 st <strong>Annual</strong> Meeting on Women’s<br />
Cancer of The Society of Gynecologic Oncology (SGO). March 14-17, 2010, San Francisco, CA.<br />
Stuckey A, Kim K, Singh R, Ritz R, Fischer A, Hillenmeyer S, Raphael B, Brodsky A, Brard L.<br />
Developing an Integrated Genomic Approach to Explore the Antitumor Activity of Vitamin D and<br />
Derivatives to Treat Ovarian Cancer. Society of Gynecologic Oncology <strong>Annual</strong> Meeting. March<br />
15, 2010, # 396, San Francisco CA<br />
42<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Dizon D S, Myers J, Doan J, Mitra D, Davis K. The Economic Burden of Ovarian Cancer in a<br />
United States Managed Care. SGO 41st <strong>Annual</strong> Meeting on Women’s Cancer. San Francisco,<br />
California. March 14-17, 2010.<br />
Jackson A L, Mathews C, Raker C, Steinhoff M, Bandera C, Dizon D S. Accuracy of Preoperative<br />
and Intraoperative Pathology Findings in Low Grade Endometrial Cancer. SGO 41st <strong>Annual</strong><br />
Meeting on Women’s Cancer. San Francisco, California. March 14-17, 2010.<br />
Horowitz N, Olawaiye A, Growdon W, Borer D, Dizon D S, Brard L, Matulonis U, MacNeill K,<br />
Roche M, Krasner C. Phase II trial of erlotinib (Tarceva) in women with squamous cell carcinoma<br />
of the vulva. SGO 41st <strong>Annual</strong> Meeting on Women’s Cancer. San Francisco, California. March<br />
14-17, 2010. Plenary Presentation.<br />
Dizon D S, Myers J, Doan J, Mitra D, Davis K. The economic burden of ovarian cancer in a US<br />
managed care database. SGO 41st <strong>Annual</strong> Meeting on Women’s Cancer. San Francisco, California.<br />
March 14-17, 2010.<br />
Pandya S, Dizon D S, Gass J S. Should we excise all breast core-biopsy proven papillary lesions?<br />
American Society of Breast Surgeons. Las Vegas, NV. April 28-May 2, 2010.<br />
MacLaughlan S, Fischer A, Kristjansdottir K, Ritz A, Raphael B, Steinhoff M, Brodsky A, Brard<br />
L. Genetics of Primary and Metastatic Ovarian Cancer. 101st <strong>Annual</strong> AACR Meeting, Washington,<br />
DC, April 17- 21, 2010.<br />
MacLaughlan S D, Fischer A, Kristjansdottir K, Ritz A, Raphael B, Steinhoff M, Brodsky A S,<br />
Brard L. Genetics of Primary and Metastatic Ovarian Cancer. American Association for Cancer<br />
Research <strong>Annual</strong> Meeting; April 17-21, 2010, Washington DC<br />
Pandya S V, Dizon D S, Gass J S, Hansen K, “Should we excise all breast core-biopsy proven<br />
papillary lesions?”. Poster, American Society of Breast Surgeons Conference. April 28-May 2,<br />
2010 Las Vegas, NV.<br />
Dizon D S, Gass J S, Legare R D, Sakr B J, Rizack T: Is tumor board relevant submitted for<br />
the 2010 ASCO <strong>Annual</strong> Meeting, June 4-8-2010 Chicago, IL<br />
INTERNATIONAL<br />
Cronin B, Robison K, Moore R, Granai C O, Dizon D S. Long-term use of Pegylated Liposomal<br />
Doxorubicin in recurrent ovarian carcinoma. Poster presentation at European Society of Gynecologic<br />
Oncologists. Belgrade, Serbia. October 2009.<br />
Makhija S, Dizon D S, Walker R A, Amler L, Loecke D, Venturi M, Kaye S. Pertuzumab in low<br />
HER3 mRNA expressing platinum-resistant ovarian cancer. ESGO 2009 Meeting. October 16,<br />
2009. Belgrade, Serbia.<br />
Cronin B, Dizon D S. Long-term use of pegylated liposomal doxorubicin in recurrent ovarian<br />
cancer. ESGO 2009 Meeting. October 16, 2009. Belgrade, Serbia.<br />
Stuckey A, Schwartz J, Dizon D S. Pegylated liposomal doxorubicin in recurrent serous carcinoma<br />
of the uterus. ESGO 2009 Meeting. October 16, 2009. Belgrade, Serbia.<br />
Cronin B, Robison K, Granai C O, Moore R G, Dizon D S. Stopping at progression or at best<br />
response: A study of pegylated liposomal doxorubicin in women with recurrent gynecologic<br />
cancer treated at an academic women’s oncology program. European Society of Gynecologic<br />
Oncologist <strong>Annual</strong> meeting, Belgrade, Serbia, October 11-14, 2009<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 43<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
44<br />
INVITED PRESENTATIONS (LOCAL/REGIONAL)<br />
Cain, JM. Moderator: “Moving into the Future: New Dimensions and Strategies for Women’s<br />
Health Research for the National Institutes of Health.” Providence, RI,<br />
September 2009<br />
Cain, JM. “Safety and Quality Agenda for Ob/Gyn.” Sunshine Seminar, San Juan, Puerto Rico,<br />
February 2010.<br />
Cain, JM. “Management of Ovarian Cancer.” Sunshine Seminar, San Juan, Puerto Rico, February<br />
2010.<br />
Cain, JM. “Cervical Cancer Control: The Challenge and the Hope.” Grand Rounds Presentation:<br />
Weill Cornell Medical College, Lincoln Hospital, Jamaica Hospital, New York, NY, March 2010.<br />
Cain, JM. “10 Key Things Every ER Should Know About Women’s Cancers.” Grand Rounds,<br />
Department of Emergency Medicine, Rhode Island Hospital, Providence, RI, April 2010.<br />
Cain, JM. “Mentors, Mentoring, and Career Strategies for all Settings: Community to Academic.”<br />
ACOG 58th <strong>Annual</strong> Clinical Meeting, San Francisco, CA, May 2010.<br />
Cain, JM. “Who Are We Really? The Future of Obstetrics and Gynecology.”<br />
The 24th <strong>Annual</strong> Resident & Fellow Research Day & Richard E. Hunter, MD Lecture, UMass Memorial<br />
Health Center, <strong>University</strong> of Massachusetts Medical School, Worcester, MA, June 2010.<br />
Ekaterini Tsiapali, MD - “Breast Surgery and Reconstruction” presented at the Breast Cancer<br />
Support Group in the Breast Health Center….July 16, 2009<br />
Richard Moore, MD – “Risk Assessment of a Pelvic Mass for Ovarian Cancer” at Falmouth<br />
Hospital, July 17, 2009<br />
Ekaterini Tsiapali, MD - “Surgical Treatment of Breast Cancer (NSABP B04 and B06)” presented<br />
Breast Educational Rounds to the medical students and fellows…July 17, 2009<br />
Tina Robison, MD - “Mesenchymal Tumors” presented core lecture to the residents and medical<br />
students at WIH. July 17, 2009<br />
Tina Robison, MD - “How to Write an Abstract” presented to the fellows at One Blackstone<br />
Place. August 7, 2009<br />
Skip Granai, MD - “Things Could Be Worse, We Could Always Be A Community Hospital” presented<br />
to Pediatrics Department, WIH; August 12, 2009.<br />
Skip Granai, MD – Speaker, Network Regional Physician Leaders/Advisors Team Meeting “Strategy<br />
Development and Marketing, SWOT Analysis” WIH, August 12, 2009.<br />
Trevor Tejada-Berges, MD - “Why should we care about racial disparities?”- Patient & Advisory<br />
Council meeting- Aug 13, 2009<br />
Tina Robison, MD - “Prevalence of HPV and Type Distribution in Southeast Asian Women Residing<br />
in Rhode Island” presented research proposal to the WRHR committee. August 17, 2009<br />
Skip Granai, MD - Speaker, Network Regional Physician Leaders/Advisors Team Meeting, Women<br />
& Infants Hospital, “Organization and Geography.” August 18. 2009.<br />
Robert Legare, MD – Presented at the “Kick-Off” Breakfast for Making Strides for Breast Cancer<br />
– August 20, 2009<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Robert Legare, MD – presented “Got Milk – Vitamin D and Breast Cancer” at the Breast Health<br />
Lecture Series – September 8, 2009<br />
Skip Granai, MD - Keynote speaker, First <strong>Annual</strong> Ovarian Cancer Research Fund’s Super Luncheon,<br />
hosted by First Lady Suzanne Carcieri, at the <strong>University</strong> Club, Providence, Rhode Island<br />
(September 9, 2009)<br />
Trevor Tejada-Berges, MD - Presented Screening and Management of Breast Cancer “OB GYN<br />
clerkship rotation- Sept 10, 2009<br />
Tina Robison, MD – “Vulva Carcinoma” presented core lecture to the residents and medical<br />
students at WIH. Sept. 11, 2009<br />
Ekaterini Tsiapali, MD – “Oncoplastic Techniques in the Management of Breast Cancer”<br />
presented to the Fellows at WIH September 11, 2009.<br />
Jennifer Scalia-Wilbur, MS - “Hereditary Breast and Ovarian Cancer: BRCA Testing<br />
and Beyond.” Directed, coordinated and lectured at the program’s first symposium,<br />
Women & Infants Hospital, Providence, RI, September 26, 2009.<br />
Jennifer Gass, MD - “Surveillance and Surgical Option for Breast Cancer Risk Reduction”<br />
Speaker at the Hereditary Breast and Ovarian Cancer: BRCA Testing and Beyond, Women & Infants<br />
Hospital, September 26, 2009.<br />
Bachir Sakr, MD – “Use of Tamoxifen (B14 and B12)” presented to the Breast/GYN Fellows at<br />
WIH October 9, 2009.<br />
Don Dizon, MD - You’ve Lost that Loving Feeling: Sexual Health and Breast Cancer Survivors.<br />
Breast Cancer Survivors’ Day. October 15, 2009, Greenfield, MA.<br />
Jennifer Gass, MD - “A New Legacy of Knowledge, Choice and Beauty” Invited speaker: Festival<br />
Ballet Providence Legacy of Loss in recognition of Breast Cancer Awareness Month. Festival<br />
Ballet Providence, Providence, RI, October 18, 2009.<br />
Trevor Tejada-Berges, MD – Presented ”Why Should We Care About Racial/Ethnic Disparities<br />
in Health Care?” Woonsocket MOB <strong>Annual</strong> Community celebration- October 22, 2009<br />
Jennifer Gass, MD – “Sentinel Lymph Node Biopsy” lecture to the Fellows at WIH October 23,<br />
2009.<br />
Jennifer Gass, MD - “New Surgical Option, Including Nipple Sparing Mastectomy and Oncoplastics”<br />
speaker: at Breast Health Center Fair: Inside the Breast Health Center a place for health,<br />
wellness and healing. Women & Infants Hospital, Providence, RI, October 30, 2009.<br />
Robert Legare, MD – presented on breast and ovarian disease at the Women & Infants’<br />
Symposium on “Tsunami of Genetics”; November 7, 2009<br />
Jennifer Scalia-Wilbur, MS - “Identifying Patient with Hereditary Colon Cancer: How it Can<br />
Make a Difference the Tsunami of Genetics in Women’s Health: What you need to know, Rhode<br />
Island Hospital, Providence, RI November 7, 2009.<br />
Jennifer Scalia-Wilbur, MS – didactic lecture to the Fellows on Hereditary Colon Cancer;<br />
November 12, 2009<br />
Ekaterini Tsiapali, MD - “Screening and Management of Breast Cancer” presented to the medical<br />
students at the main hospital on the 3 rd floor conference room. November 13, 2009<br />
Jessica Kent, MS, CGC - “ National Society of Genetic Counselors: AEC 2009 Update Lecture”<br />
Women & Infants’ Hospital, Providence, RI , November 24, 2009.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 45<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
Trevor Tejada-Berges, MD - Presentation on a Core Lecture “Hereditary Breast and Ovarian<br />
Cancer” Women and Infants hospital of RI- Jan 8, 2010<br />
AnnMarie Bradley, RN, BSN, OCN, presented to the staff at Butler Hospital on “Ovarian Cancer<br />
– Progress in Detection, Diagnosis, Staging, and Treatment” – January 13, 2010.<br />
Ekaterini Tsiapali, MD - “BHC Research/Publication” presented to the Fellows at WIH, January<br />
18, 2010<br />
Nada Kawar, MD - Women’s Health Lecture Series: What women should know about Cervix<br />
Cancer. Women & Infants’ Hospital/<strong>Brown</strong> <strong>University</strong>, January 19, 2010.<br />
Robert Legare, MD – RI Hospital Grand Rounds “Breast and Ovarian Cancer Syndrome” – January<br />
28, 2010<br />
Jessica Kent, MS, CGC - “ Hereditary Gynecological Cancer Syndromes” Fellowship Lectures.<br />
Women & Infants’ Hospital, Providence, RI, February 5, 2010.<br />
Paul DiSilvestro, MD – presented at the Ovarian Cancer Research Symposium at <strong>Brown</strong> <strong>University</strong><br />
“Ovarian Cancer Treatment: What Have We Learned, What We Don’t Know.” – February 5, 2010<br />
Ekaterini Tsiapali, MD - presented “Bowel Repair” at the Core Curriculum lecture at WIH,<br />
February 26, 2010<br />
Don Dizon, MD - Ovarian Cancer: Novel Treatments and Current Paradigms. Rhode Island Hospital<br />
Cancer Center Grand Rounds, Rhode Island Hospital, March 11, 2010.<br />
Skip Granai, MD - Invited Speaker, Chemotherapy Certification Course, Women & Infants Hospital,<br />
Providence, RI. April 19 th , 2010.<br />
Trevor Tejada-Berges, MD - Presented: Breast Talk ”Margin Status and DCIS meta Analysis”<br />
at the Fellow Meeting- April 23, 2010<br />
Jessica Kent, MS, CGC - “ Hereditary Colon Cancer Syndromes” Lecturer, Clinical Cancer<br />
Genetics Medical Elective, Alpert Medical School, <strong>Brown</strong> <strong>University</strong>/ Women & Infants’ Hospital,<br />
Providence, RI, April 29, 2010.<br />
Richard Moore, MD – presented “A Novel Biomarker for the Management of Women with<br />
Epithelial Ovarian Cancer” at the American Society of Clinical Lab, Providence RI; May 4, 2010<br />
Ekaterini Tsiapali, MD – presented “Thyroid and Colon Management: to the Woonsocket area<br />
community at the WIH MOB May 4, 2010.<br />
Skip Granai, MD - Keynote speaker at the Oncology Nursing Society Local Chapter, Hasbro<br />
Children’s Hospital, Providence, RI. “We Can Always Dance.” May 5, 2010.<br />
AnnMarie Bradley, RN, BSN, OCN – presented Gynecologic Cancers “We Can Always Dance”<br />
to the Oncology Nursing Society Staff at RIH on May 5, 2010.<br />
Robert Legare, MD – presented a didactic lecture entitled “Hereditary Breast and Ovarian Cancer<br />
Syndromes” to the genetics elective students on May 6, 2010.<br />
Ekaterini Tsiapali, MD – presented at Newport Hospital Grand Rounds “Breast Cancer Screening<br />
and Risk Reduction” on May 7, 2010.<br />
Skip Granai, MD - Keynote Speaker, Program in Women’s Oncology’s Integrative Care Open<br />
House, at South County Common, Wakefield, RI. “If I Were You and You Were Me.” May 8, 2010<br />
46<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Don Dizon, MD – gave a presentation on Breast Screening and Mammography Controversy<br />
Debate at the <strong>Annual</strong> Scientific meeting, Warwick RI; May 13, 2010.<br />
Trevor Tejada-Berges, MD - Presented: “Brining Robotic Surgery To Women & Infants Hospital”-<br />
May 13, 2010<br />
Trevor Tejada-Berges, MD - Core Lecture:”Cervical Caner Diagnosis and Management”- May<br />
14, 2010<br />
Christina Bandera, MD – gave a Robotic Surgery Lecture as part of the Curves Lecture Series,<br />
Attleboro MA; May 14, 2010.<br />
Robert Legare, MD – Westerly Hospital Grand Rounds, “Epithelial Ovarian Cancer: Present<br />
Treatment/Controversies and Future Directions” Westerly Hospital, Westerly RI, May 20, 2010.<br />
Don Dizon, MD – RI Hospital Grand Rounds – “Sex and Intimacy in Female Cancer” – May 20,<br />
2010.<br />
Trevor Tejada-Berges, MD - OB-GYN Clerkship – “Screening and Management of Breast Cancer”<br />
May 27, 2010<br />
Trevor Tejada-Berges, MD – gave a presentation as part of the Curves Lecture Series, Franklin<br />
MA; May 27, 2010<br />
Jennifer Gass, MD - “Breast Cancer in the New Millennium” Staff Development Day, Alpert<br />
School of <strong>Brown</strong> <strong>University</strong>, Providence, Rhode Island, June 3, 2010.<br />
Skip Granai, MD - Invited Speaker, Westerly Hospital, Grand Rounds, “Women’s Cancers: What<br />
are we thinking?” June 6, 2010.<br />
Ekaterini Tsiapali, MD - presented Breast Health Center lecture “Breast Cancer Screening and<br />
the perioperative use of MRI” on June 8, 2010.<br />
Richard Moore, MD – presented “HE4 Update” to the Fall River physicians in North Dartmouth,<br />
MA, on June 10, 2010<br />
AnnMarie Bradley, RN, BSN, OCN – presented “Gynecologic Cancers” to the clinical staff at<br />
William Backus Hospital in CT on June 24, 2010<br />
INVITED PRESENTATIONS (NATIONAL)<br />
Don Dizon, MD - Con: Bevacizumab should be continued indefinitely and utilized with every<br />
drug regimen for recurrence. GOG Summer Symposium, July 16, 2009, Baltimore, MD.<br />
Trevor Tejada-Berges, MD - Presentation” What is the OB/GYN to do?”- Florida Obstetrics and<br />
Gynecologic Society conference, Boca Raton Florida –August 14-15, 2009<br />
Don Dizon, MD - Ovarian Cancer: State of the Art and Current Controversies. <strong>University</strong> of Miami<br />
Sylvester Cancer Center Grand Rounds, September 8, 2009, Miami, FL.<br />
Skip Granai, MD - Keynote speaker, 8 th <strong>Annual</strong> Nixon Lectureship, sponsored by The <strong>University</strong><br />
of Kentucky/Norton Healthcare Foundation, held at the Olmsted, Louisville, KY. “We Can Always<br />
Dance.”(September 21, 2009)<br />
Skip Granai, MD - Keynote speaker, Bassett Healthcare Interdepartmental, Grand Rounds. Clark<br />
Education Building, Bassett Campus, Cooperstown, New York, Wednesday, October 7, 2009. “We<br />
Can Always Dance.” (October, 2009)<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 47<br />
G y n e c o l o g i c O n c o l o g y
G y n e c o l o g i c O n c o l o g y<br />
Don Dizon, MD - Session Co-Chair: Challenges in Survivorship. 2009 ASCO Breast Symposium.<br />
October 8, 2009, San Francisco, CA.<br />
Jennifer Scalia-Wilbur, MS – “Hereditary Breast Cancer: Breast Cancer in Younger Women”<br />
presented at the Breast Cancer in Younger Women Nursing Education Conference, New York,<br />
NY; November 4-5, 2009.<br />
Don Dizon, MD - Moving Beyond Standard of Care: Novel Treatments in Gynecologic Malignancies.<br />
Chemotherapy Foundation Symposium. November 11-13, 2009, New York, NY.<br />
Skip Granai, MD - Invited Speaker, Fall Society of Gynecologic Oncologists Executive Council<br />
Meeting in Washington, DC. “Bringing together the best in Women’s Cancer Care.” (November,<br />
2009)<br />
Skip Granai, MD - Invited speaker, the Society of Gynecologic Oncologist 41 st <strong>Annual</strong> Meeting on<br />
Women’s Cancer, Sunday, March 14 th , Moscone Convention Center, San Francisco, CA. “Incorporating<br />
Breast Care into Clinical Practice – Developing a Breast Fellowship Training Program, 2010.<br />
Skip Granai, MD -Invited Speaker, Vice President <strong>Report</strong> of the Society of Gynecologic Oncologists<br />
Business Meeting, Monday, March 15 th , Moscone Convention Center, San Francisco, CA.<br />
“SGO Strategic Goal Accomplishments”, 2010.<br />
Skip Granai, MD - Invited Speaker, introduced the Society of Gynecologic Oncologists’ President,<br />
David Mutch, MD at the SGO’s Presidential Address Event, Monday, March 15 th , Moscone<br />
Convention Center, San Francisco, CA. SGO’s Presidential Address, 2010.<br />
Don Dizon, MD - Current Strategies in the Treatment of Platinum-Resistant Recurrent Ovarian<br />
Cancer. Clinical Advances in Gynecologic Malignancies. An Industry Satellite Sponsored Symposium<br />
at the Society of Gynecologic Oncologists <strong>Annual</strong> Meeting, March 15, 2010. San Francisco, CA.<br />
Don Dizon, MD - National Consortium of Breast Centers <strong>Annual</strong> Meeting, March 19-24, 2010,<br />
Las Vegas, NV.<br />
1. Session Moderator, Opening Plenary Sessions, March 21, 2010.<br />
2. Golden Girls: The Approach to Breast Health in Women over 70. March 22, 2010.<br />
3. Panelist, Approaching Metastatic Breast Cancer. March 23, 2010<br />
Jennifer Gass, MD - “I want a Bilateral Mastectomy and Urban Unrest: The Breast Center in<br />
Academia” Speaker: at the National Consortium of Breast Centers 20 th <strong>Annual</strong> Interdisciplinary<br />
Breast Center Conference. Los Vegas, NV, March 20-24, 2010.<br />
Trevor Tejada-Berges, MD - Attended Prep Course for Breast Ultrasound and Stereotactic at<br />
American Society of Breast Surgeons, Las Vegas, NV April 29, 2010- Has completed prep course<br />
and has received a certification of completion.<br />
Richard Moore, MD – presented “A Novel Approach to Pelvic Mass Risk Assessment for Ovarian<br />
Cancer” at the Resident Research Day at the <strong>University</strong> of Rochester in NY; May 13, 2010.<br />
Skip Granai, MD - Invited Speaker, Gynecologic Cancer Foundation’s Ovarian Cancer Survivors<br />
Course, at NYU Langone Medical Center, New York, NY. Title: Phenomenal Women: Ovarian Cancer<br />
Survivorship” May 15, 2010.<br />
Skip Granai, MD - Keynote Speaker, <strong>University</strong> of Pennsylvania, Brett Gutsche Lecture. Title:<br />
“We Can Always Dance.” May 20, 2010.<br />
Skip Granai, MD - Keynote Speaker at “The Female Patient” Conference: Current Issues in the<br />
Care of Women – Isla Grand Beach Resort, South Padre Island, Texas. ”We Can Always Dance.”<br />
June 14, 2010.<br />
48<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Skip Granai, MD - Keynote Speaker, “The Female Patient” Conference: Current Issues in the<br />
Care of Women - Isla Grand Beach Resort, South Padre Island, Texas. “Ovarian Masses During<br />
Pregnancy.” June 15, 2010.<br />
INVITED PRESENTATIONS (INTERNATIONAL)<br />
Cain, JM. “Common Cancers Specific to Women: New Developments & Hope.”<br />
Women Deliver Conference (International), Washington, DC, June 2010.<br />
Cain, JM. “Can we eliminate cervical cancer globally.” Women Deliver Conference (International),<br />
Washington, DC June 2010.<br />
Don Dizon, MD - Ville Marie Oncology Center 15th Anniversary Breast Cancer Conference.<br />
Breast Cancer: Progress in prevention, detection, and treatment. August 4, 2009, Montreal, Quebec,<br />
Canada.<br />
1. Current options in chemoprevention. 2. Progress in hormonal and chemotherapy agents.<br />
3. You’ve lost that loving feeling: Sexual health and the breast cancer survivor.<br />
Richard Moore, MD – presentation titled “Tumor Markers in Gynecologic Cancers” at the European<br />
Society of OB-GYN meeting, Rome Italy. September 9-13, 2009.<br />
Tina Robison, MD – Poster presentation “Stopping at Progression or at Best Response: A study<br />
of Pegylated Liposomal Doxorubicin in Women with Recurrent Gynecologic Cancer Treated at<br />
an Academic Women’s Oncology Program” at the European Society of Gynecologic Oncology<br />
meeting, Belgrade, Serbia, October 10-14, 2009<br />
Richard Moore, MD – presented “Pelvic Mass Risk Assessment” at the European Society of<br />
Gynecologic Oncology meeting, Belgrade, Serbia, October 11-14, 2009.<br />
Skip Granai, MD -Invited Speaker: 3 rd Asia Pacific Congress: Controversies in Obstetrics, Gynecology,<br />
& Infertility, Shangri-La’s Kerry Centre Hotel, Beijing, China. Pelvic mass in pregnancy:<br />
When do we need to Intervene? (November, 2009)<br />
Skip Granai, MD - Chairperson/discussant” 3 rd Asia Pacific Congress: Controversies in Obstetrics,<br />
Gynecology, & Infertility, Shangri-La’s Kerry Centre Hotel, Beijing, China (November, 2009)<br />
Skip Granai, MD - Hot Controversies – Expert Opinion on: Cervical Cancer and Human Papilloma<br />
Virus (HPV): Does vaccination mark the end of cervical cancer? Shangri-La’s Kerry Centre<br />
Hotel, Beijing, China (November, 2009)<br />
Skip Granai, MD - Keynote Speaker: 3 rd Asia Pacific Congress: Controversies in Obstetrics, Gynecology,<br />
& Infertility, Shangri-La’s Kerry Centre Hotel, Beijing, China. “Voices” (November, 2009)<br />
Richard Moore, MD – Chairperson – Women and Ovarian Cancer: From Conception to Diagnosis<br />
“Early Diagnosis of Ovarian Cancer Can Improve Prognosis” at 3 rd Asia Pacific Congress:<br />
Controversies in Obstetrics, Gynecology, & Infertility, Shangri-La’s Kerry Centre Hotel, Beijing,<br />
China (November 2009)<br />
Richard Moore, MD – served as a discussant on “Hot Controveries – Expert Opinion on: Cervical<br />
Cancer and Human Papilloma Virus (HPV): Does Vaccination Mark the End of Cervical Cancer?”<br />
at 3 rd Asia Pacific Congress: Controversies in Obstetrics, Gynecology, & Infertility, Shangri-La’s<br />
Kerry Centre Hotel, Beijing, China (November 2009)<br />
Richard Moore, MD – presented “HE4 in Ovarian Cancer,” Istanbul, Turkey<br />
Katrin Kristjansdottir, MD - Development of Tumor Markers In Ovarian Cancer. Grand Rounds.<br />
Landspitali <strong>University</strong> Hospital, Iceland Department of Ob/Gyn. January 21. 2010<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 49<br />
G y n e c o l o g i c O n c o l o g y
M a t e r n a l – F e t a l M e d i c i n e<br />
50<br />
DIVISION OF MATERNAL–FETAL MEDICINE<br />
INTRODUCTION<br />
The mission of the Division of Maternal–Fetal Medicine is: (1) to provide the highest quality<br />
consultative and patient care pregnancy–related services to health professionals and patients;<br />
(2) to develop new knowledge about physiology, mechanisms of disease and clinical practice<br />
related to pregnancy; (3) to train medical students, residents and fellows to be future leaders in<br />
health care.<br />
FACULTY<br />
Katharine D. Wenstrom, MA, MD, Division Director, joined the staff at Women<br />
& Infants Hospital of Rhode Island as director of the Division of Maternal-Fetal<br />
Medicine and Professor of Obstetrics and Gynecology on July 1, 2009. Dr. Wen-<br />
strom received both her BA and her MD from Case Western Reserve <strong>University</strong><br />
in Cleveland, Ohio, and an MA in Pathology from Columbia <strong>University</strong> in New<br />
York City, New York. She completed her residency training and her fellowship<br />
in Maternal Fetal Medicine at the <strong>University</strong> of Illinois in Chicago, followed by a fellowship in<br />
Medical Genetics at the <strong>University</strong> of Iowa. Dr. Wenstrom has served as president of the Soci-<br />
ety for Maternal-Fetal Medicine, as a member of the executive board of the American College<br />
of Obstetricians and Gynecologists, and as head of the National Institutes of Health Obstetrics<br />
and Maternal-Fetal Biology Subcommittee. She has been editor-in-chief for obstetrics of the<br />
Obstetrical and Gynecological Survey since 2005. Her clinical and research interests include<br />
genetic screening, fetal diagnosis and therapy, and teratology.<br />
Brenna L. Anderson, MD, MS joined the faculty in July, 2006 as Assistant Profes-<br />
sor of Obstetrics and Gynecology. She received her BS from the <strong>University</strong> of RI<br />
and her MD from <strong>Brown</strong> <strong>University</strong>. She completed her Ob/Gyn and MFM train-<br />
ing at the <strong>University</strong> of Pittsburgh. She also received a Master’s degree in clinical<br />
research and completed a fellowship in Reproductive Infectious Diseases and Im-<br />
munology at the <strong>University</strong> of Pittsburgh. Her clinical and research interests focus<br />
on the ante – and intra-partum care of infectious diseases in pregnancy, and she is the chief of<br />
the Reproductive Infectious Diseases consultative service here at WIH. In 2006, Dr. Anderson<br />
was selected for the Women’s Reproductive Health Research (WRHR) Career Development<br />
Program at <strong>Brown</strong> <strong>University</strong>, which supported her investigations of the immune system in<br />
pregnancy. In 2009, she received a K23 Mentored Patient-Oriented Career Development Award<br />
to study mucosal immunity in the acquisition of HIV . Dr. Anderson has served as the leader of<br />
the Infectious Disease Special Interest group for the Society for Maternal Fetal Medicine, and is<br />
currently the alternate PI for the NIH MFMU Network.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Stephen R. Carr, MD joined the faculty in 1988 after completing his Maternal–Fetal<br />
Medicine fellowship here at WIH, and is currently a Professor of Obstetrics and<br />
Gynecology. He graduated from Middlebury College and received his MD from the<br />
<strong>University</strong> of Hawaii. He completed his residency training at the <strong>University</strong> of Il-<br />
linois in Chicago. Dr. Carr’s clinical interests include fetal sonography and invasive<br />
diagnostic and therapeutic techniques. He is the Director of the Prenatal Diagnosis<br />
Center and Maternal–Fetal Medicine Diagnostic Imaging at Women & Infants Hospital of Rhode<br />
Island and Co-Director of the Fetal Treatment Program, a co-operative effort of Women & Infants<br />
Hospital of Rhode Island and Lifespan. His research interests include evaluation and manage-<br />
ment of twin-to-twin transfusion syndrome. Dr. Carr is a Colonel in the Rhode Island Air National<br />
Guard and is Commander of the 143rd Medical Group, and recently returned from a three-month<br />
mission in Afghanistan.<br />
Edward K. S. Chien, MD joined the Division of Maternal–Fetal Medicine in 2004 as<br />
an Assistant Professor of Obstetrics and Gynecology. He graduated from the Uni-<br />
versity of Illinois in Urbana and received his MD from the <strong>University</strong> of Illinois in<br />
Chicago. He completed his residency training in 1992 at the <strong>University</strong> of Michigan<br />
Medical Center. He completed his Maternal Fetal Medicine fellowship at the Univer-<br />
sity of Chicago in 1994, and then undertook a 3 year postdoctoral fellowship in the<br />
laboratory of Graeme I Bell in the Department of Molecular Biology and Biochemistry, funded<br />
through the Reproductive Scientist Development Program as the March of Dimes Fellow. Dr.<br />
Chien joined the faculty at the <strong>University</strong> of Vermont in 2002, where he served as MFM fellow-<br />
ship director After joining the MFM division here at WIH in 2004, Dr. Chien became the Maternal<br />
Fetal Medicine Fellowship director in July of 2005. His research interests focus on understand-<br />
ing the mechanisms responsible for prematurity, focusing on cervical remodeling and maternal<br />
physiology.<br />
Donald R. Coustan, MD joined the faculty as Director of Maternal–Fetal Medicine<br />
in 1981, was appointed Professor of Obstetrics and Gynecology in 1986, and was<br />
Chairman of the Department from 1991 to 2008. After retiring from this role, he<br />
kindly agreed to serve as Interim Division Director of Maternal-Fetal Medicine from<br />
March 2008 until July 1, 2009, when Dr. Katharine Wenstrom assumed the posi-<br />
tion of permanent Division Director. Dr. Coustan continues to be a clinically active<br />
member of the MFM division, providing antenatal care to women with diabetes. His research<br />
interests have been focused on the epidemiology of gestational diabetes and its treatment.<br />
Tanya Dailey, MD joined our division in July 2009 as a clinical Assistant Professor<br />
of Obstetrics and Gynecology. She received her BS degree in Human Physiology<br />
from Boston <strong>University</strong> and completed both medical school and residency at Tufts<br />
New England Medical Center and <strong>University</strong>. She did her Maternal Fetal Medicine<br />
Fellowship here at Women and Infants Hospital, with a thesis on TGF expression<br />
in the pregnant rat cervix and its role in cervical remodeling. Her research interests<br />
include pre-term labor and cervical insufficiency.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 51<br />
M a t e r n a l – F e t a l M e d i c i n e
M a t e r n a l – F e t a l M e d i c i n e<br />
52<br />
Matthew Esposito, MD joined our division in early 2010. He received his BA in<br />
Biology from Williams College and his MD from the <strong>University</strong> of Rochester. After<br />
completing his residency at the <strong>University</strong> of Maryland, he did his Maternal Fetal<br />
Medicine Fellowship here at Women and Infants Hospital. He was then an As-<br />
sistant Professor at the <strong>University</strong> of Massachusetts Memorial Medical System,<br />
where he established himself as an expert in prenatal ultrasound and resident<br />
and medical student teaching. Dr Esposito’s research interests include aspects of cesarean<br />
delivery and clinical problems in obstetrics.<br />
Barbara M. O’Brien, MD joined the faculty in 2007 as Assistant Professor of<br />
Obstetrics and Gynecology. She received her BA from the College of the Holy<br />
Cross and her MD from New York Medical College. She received her OB/GYN and<br />
MFM training at Tufts New England Medical Center. She also completed a Medi-<br />
cal Genetics Fellowship at Tufts New England Medical Center in 2007. She is the<br />
Director of Perinatal Genetics and Co-Director of the Prenatal Diagnosis Center<br />
at Women and Infants Hospital of Rhode Island. She is also the Associate Director of the Core<br />
Clerkship in Ob/Gyn and is in charge of the resident rotation in MFM. Her clinical interests<br />
include fetal sonography, invasive techniques for the diagnosis of chromosomal and genetic<br />
disorders, and the diagnosis and treatment of twin-to-twin transfusion syndrome.<br />
Michael Paglia, MD, PhD joined the faculty in 2005 as a Clinical Assistant Profes-<br />
sor of Obstetrics and Gynecology. He graduated from College of the Holy Cross,<br />
received his MD from the <strong>University</strong> of Pennsylvania and his PhD from Johns<br />
Hopkins Bloomberg School of Public Health with a focus in Health Services Re-<br />
search. At Hopkins he received a Commonwealth Fund Dissertation Award. He<br />
completed both his Ob/Gyn and MFM training at Duke <strong>University</strong> Medical Center.<br />
In November 2009, Dr. Paglia left WIH to become MFM division director at the Geisinger Medi-<br />
cal Center in Wilkes Barre, Pennsylvania. However, he has retained his academic appointment<br />
here and returns several times each month to continue his research, which is focused primarily<br />
on resident education and patient safety issues.<br />
FELLOWS<br />
Julie Johnson, MD received her undergraduate degree from UNC Chapel Hill and her MD from<br />
Wake Forest <strong>University</strong>. After completing her residency at the <strong>University</strong> of South Carolina, she<br />
came to Women and Infants Hospital for her Maternal Fetal Medicine Fellowship. Her research<br />
and clinical interests include fetal cardiac function in growth-restricted pregnancies and mech-<br />
anisms and abnormalities of labor and delivery. She will be joining the Women & Infants’ MFM<br />
division in August, 2010.<br />
Hector Mendez-Figueroa, MD Is the current first year fellow. He received his MD from the Uni-<br />
versidad Nacional Autonoma de Honduras, and completed his residency at Baylor College of<br />
Medicine. His research interests include premature rupture of the membranes and OTC defi-<br />
ciency in pregnancy.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Nicole Sprawka, MD is the third year Maternal Fetal Medicine fellow. She received her under-<br />
graduate degree from the <strong>University</strong> of Texas and her MD from the <strong>University</strong> of Texas South-<br />
western. She completed her residency at Baylor College of Medicine in Houston, Texas. She<br />
is working with the Department of Laboratory and Pathology to study prenatal screening for<br />
chromosomal abnormalities.<br />
Roman Starikov, MD is the current second year fellow. He received his BS from the Univer-<br />
sity of Texas in Austin and his MD from Texas A and M College of Medicine. He completed his<br />
internship at Beth Israel Medical Center in New York City, and his residency at Baystate Medical<br />
Center in Springfield, Massachusetts, after which he spent two years as an Assistant Profes-<br />
sor at Tufts <strong>University</strong> School of Medicine. He is currently studying the relationship between<br />
maternal diabetic control and fetal cardiac defects.<br />
RESEARCH<br />
Brenna Anderson, MD, MS was selected in 2006 for the Women’s Reproductive Health Re-<br />
search (WRHR) Career Development Program at <strong>Brown</strong> <strong>University</strong>, which supported her inves-<br />
tigation of the host immune system in pregnancy, and in 2009 received an NIH K23 Mentored<br />
Patient-Oriented Career Development Award to study mucosal immunity in the acquisition of<br />
HIV. She was also awarded a Center for AIDS Research Developmental grant to study the effect<br />
of treatment of trichomoniasis on genital shedding of HIV in South Africa. She is engaged in<br />
several research studies examining the immune response to HIV infection and other sexually<br />
transmitted infections, as well as normal vaginal immunology and bacteriology. She has also<br />
examined the impact of the novel swine-origin influenza A virus on pregnant women. In 2009<br />
she became the alternate principal investigator for the Maternal–Fetal Medicine Units Network.<br />
This year the Network approved her multicenter study examining the impact of hyperimmune<br />
globulin on the prevention of congenital cytomegalovirus, and she will head the CMV study<br />
subcommittee.<br />
Edward Chien, MD has focused his research on cervical mechanisms of pre–term birth, ex-<br />
amining the molecular remodeling response to mechanical stress and strain. Dr. Chien col-<br />
laborates with bioengineers and investigators at <strong>Brown</strong>, MIT, the <strong>University</strong> of Illinois and<br />
Tufts, evaluating models to understand tissue responses to force. He is examining extracellular<br />
matrix components, including collagen, elastin, and proteoglycans, that provide structural in-<br />
tegrity responsible for resisting mechanical forces. Radiofrequency spectral analysis, molecular<br />
and biochemical techniques are combined to understand how the cervix contributes to suc-<br />
cessful pregnancy outcomes. His research objectives include developing structure/composition<br />
function relationships in cervical tissue and examining the effects of pharmacological agents<br />
known to affect cervical mechanics. Dr. Chien was recently awarded an NIH R03 grant to study<br />
the effects of force and the hormonal environment on the cervical matrix, and has also been<br />
awarded an NIH contract to perform part of the Normal Fetal Growth Study.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 53<br />
M a t e r n a l – F e t a l M e d i c i n e
M a t e r n a l – F e t a l M e d i c i n e<br />
Donald R. Coustan, MD serves as the site principal investigator for the Stillbirth Collaborative<br />
Research Network, which was established to examine the epidemiology, clinical correlates, and<br />
pathogenesis of stillbirth. The network is engaged in the study of a geographically determined<br />
racially mixed population–based sample of 500 to 700 stillbirths and an age-matched sample<br />
of pregnancies productive of liveborn infants. Dr. Coustan also serves as the North American<br />
Regional Director of the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study, an<br />
international observational cohort study of 25,000 gravidas, the results of which are expected<br />
to change the way gestational diabetes is diagnosed throughout the world.<br />
Julie Johnson, MD is joining our faculty in August 2010. Her research interests include normal<br />
and abnormal labor and delivery and treatment of cervical Insufficiency.<br />
Barbara O’Brien, MD has focused her research on various aspects of fetal diagnosis and<br />
therapy. One current project involves using proteomic profiling to identify novel biomarkers<br />
in blood and amniotic fluid from women carrying fetuses with twin-to–twin transfusion syn-<br />
drome, a project made possible by the number of patients with TTTS referred to the <strong>Brown</strong><br />
Fetal Treatment Program. She hypothesizes that there are novel biomarkers in maternal serum<br />
and amniotic fluid, both before and after laser ablation treatment for severe TTTS, that may<br />
both illuminate the etiology and predict the severity of this devastating disorder. Dr. O’Brien<br />
has established collaborations with Dr. Francois Luks, from the Division of Pediatric Surgery,<br />
and Dr. Djuro Josic, Director of Proteomics Core, COBRE Center for Cancer Research Devel-<br />
opment, as well as with colleagues at Yale <strong>University</strong> in order to accomplish this goal. Dr.<br />
O’Brien’s other research interests include novel methods to incorporate teaching of medical<br />
genetics training into resident and fellow training.<br />
Katharine Wenstrom, MA, MD has concentrated her research on perinatal genetics, includ-<br />
ing prenatal screening, the role of MTHFR polymorphisms in the development of cardiac and<br />
neural tube defects, and various aspects of fetal diagnosis and therapy. Her current research<br />
interests include the relationship between folic acid nutriture and post partum depression, and<br />
placental damage after CVS as a possible instigator of preeclampsia.<br />
EDUCATION<br />
The Division contributes to the education of medical and other students enrolled at <strong>Brown</strong><br />
<strong>University</strong>. Maternal–Fetal Medicine faculty members have supported many undergraduate<br />
independent study projects. The Division contributes several lectures and individual advising<br />
of third year clinical clerkship students.<br />
Dr. Chien is the Director of the <strong>Brown</strong> <strong>University</strong>/Women & Infants Hospital of Rhode Island<br />
Fellowship Program in Maternal–Fetal Medicine. During this academic year the Division sup-<br />
ported three fellows in preparation for academic careers in the subspecialty. Our fellows in<br />
2009–10 were: Julie Johnson, MD, Nicole Sprawka, MD, and Roman Starikov, MD. Three quar-<br />
ters of the graduated fellows currently have academic positions. Dr. Johnson completed her<br />
fellowship at the end of June 2010 and will join our Division at Women and Infants Hospital.<br />
54<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Our current fellows are involved in interdisciplinary research involving obstetric outcomes, se-<br />
rum marker screening, preterm labor, and diabetes. The division offers research opportunities<br />
both at the bench and at the bedside.<br />
In addition, the Division supports postgraduate education of residents in Obstetrics and Gyne-<br />
cology. There are 7-week rotations in MFM for PG2 and PG4 residents. Dr. Barbara O’Brien is in<br />
charge of the resident rotations, and is also Associate Program Director of the Residency. The<br />
Division’s clinical conferences include a general obstetrics conference, an MFM case confer-<br />
ence and the Multi–disciplinary Antenatal Diagnosis and Management Conference (MADAM).<br />
Basic orientation in sonography and in amniocentesis for Ob/Gyn residents is offered, and<br />
residents also rotate through the Prenatal Diagnosis Center, where they get additional experi-<br />
ence in prenatal ultrasound.<br />
Medical student preceptors:<br />
MFM faculty served as preceptors for 17 medical students during their core clerkship in Obstet-<br />
rics and Gynecology during 2009-2010 academic year.<br />
Medical school course leadership and participation:<br />
Dr. Barbara O’Brien continued to serve as Associate Director of the Core Clerkship in Obstetrics<br />
and Gynecology this year.<br />
Dr. Carr is course director for the Maternal–Fetal Medicine Clinical Elective Biomed 491, which<br />
accommodated eight medical students this year. MFM faculty provided 24 lectures to students<br />
on the core clerkship over the course of the year.<br />
Resident and fellow lectures:<br />
MFM faculty provided nine core curriculum lectures and three grand rounds lectures to resi-<br />
dents in Obstetrics and Gynecology during the past academic year. In addition, Dr. Brenna<br />
Anderson is a co-director of the resident research curriculum and regularly participates in lec-<br />
tures and journal clubs. Twenty fellow lecture series presentations were made by MFM faculty.<br />
Dr. Carr manages the MADAM conference, held twice monthly. MFM provides a lecture in the<br />
noon resident lecture series once per month. All faculty participate in the majority of the Divi-<br />
sion’s resident conferences.<br />
Perinatal management conference:<br />
Dr. Chien and all MFM fellows have presented at the Perinatal Management Conference Series<br />
of the Neonatology department.<br />
Neonatology core lecture series: September 21-13, 2009<br />
Dr. Chien continued to participate in the didactic teaching program for the neonatology<br />
fellowship program.<br />
Multi–disciplinary antennal diagnosis and management (MADAM) conference:<br />
The <strong>Brown</strong> <strong>University</strong> Program in Fetal Medicine began in 1997. Dr. Carr is one of its co–Direc-<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 55<br />
M a t e r n a l – F e t a l M e d i c i n e
M a t e r n a l – F e t a l M e d i c i n e<br />
tors in addition to Francois Luks, MD, of the Division of Pediatric Surgery at Hasbro Children’s<br />
Hospital. The Program in Fetal Medicine presents the Multidisciplinary Antenatal Diagnosis<br />
and Management conference (MADAM) twice monthly. Of the more than 55,000 patient en-<br />
counters at the Prenatal Diagnosis Center over a five-year span, approximately 1% has been<br />
referred for consultation with pediatric urology, surgery, cardiology, neurosurgery, genetics,<br />
orthopedics or neonatology. During the 2009–2010 academic year, more than 150 cases were<br />
referred to MADAM for consensus recommendations among these represented medical spe-<br />
cialties. The program continues to develop expertise in antenatal diagnosis and management<br />
and in fetal interventions.<br />
The Office of Research on Women’s Health (ORWH) Scientific Workshop on New Dimensions<br />
and Strategies for Women’s Health Research, September 2009<br />
The division of MFM helped to organize and plan this workshop, designed to identify the most<br />
urgent topics for future research in women’s health. Dr. Wenstrom was an invited speaker.<br />
The Tsunami of Genetics–<strong>Brown</strong> Alpert School of Medicine Genetics Course, October 2009<br />
Dr. Barbara O’Brien organized and directed this freestanding CME course on current issues in<br />
genetics for practitioners around the state, and Drs Wenstrom and O’Brien contributed lec-<br />
tures. This course was highly regarded and enthusiastically reviewed.<br />
CLINICAL ACTIVITY<br />
Inpatient Care:<br />
During academic year 2009–2010, the Division managed 834 inpatient admissions to<br />
Women & Infants Hospital of Rhode Island, of which 371 were emergent maternal transfers.<br />
Maternal–Fetal Medicine performed 522 deliveries.<br />
Antenatal Care:<br />
The Division provided antenatal care to patients with a variety of maternal medical complica-<br />
tions and fetal complications. This unit is managed by a nursing professional coordinator with<br />
the help of 2.5 FTE nurses (two of whom are certified diabetes nurse educators) and 2.0 FTE<br />
clerical staff who coordinated 2,368 patient visits for 463 new obstetrical patients (14% more<br />
than last year).<br />
Outpatient Consultation:<br />
During the past academic year, the Division provided 339 non–Prenatal Diagnosis Center (PDC)<br />
outpatient consultations, 282 PDC–based consultations, 64 New Bedford office consultations,<br />
23 Foxboro office consultations, and 9 Norwich consultations for area physicians. The Divi-<br />
sion’s diabetes nurse educators provide gestational diabetes classes and individual education<br />
on the use of a home glucose meter and/or the preparation and self–injection of insulin. A total<br />
of 260 diabetic patients were provided with individual instruction (120% more than last year)<br />
and 274 patients attended classes.<br />
56<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
The Prenatal Diagnosis Center<br />
The Prenatal Diagnosis Center (PDC) is managed by Dr. Stephen Carr, the Director of the Prena-<br />
tal Diagnosis Center and Diagnostic Imaging, and Dr. Barbara O’Brien, the Co-Director. The PDC<br />
opened in March, 1992 providing an integrated array of antenatal diagnostic services, includ-<br />
ing: genetic counseling, MFM and clinical genetics consultation, sonographic evaluation of fetal<br />
functional and anatomic abnormalities, amniocentesis, chorionic villous sampling, biophysical<br />
fetal assessment, and parental testing for diabetes and genetic disorders. During academic year<br />
2009-2010, the PDC provided 6,164 imaging procedures, 2,515 antenatal testing visits, 1,009<br />
genetic counseling visits, 282 MFM consultations, 49 CVS procedures, and 125 amniocenteses.<br />
The PDC employs seven genetic counselors who provide counseling and integrated evaluation<br />
of families and pregnancies at risk for genetically related or other perinatal morbidity. The PDC<br />
is supported by an RN manager, another full–time staff nurse, five administrative coordinators,<br />
an associate division manager, two financial counselors, a medical assistant and three full time<br />
equivalent sonographers, a research sonographer plus a senior ultrasound coordinator.<br />
Off–Campus Consultative and Imaging Services<br />
MFM provides consultative and imaging support to our outlying communities and providers.<br />
These services are offered through our off-site offices in New Bedford, MA and Foxboro, MA<br />
and through contracted service agreements with Charlton Memorial Hospital in Fall River, MA<br />
and at South County Hospital in Wakefield, RI. In April 2010, a new site was opened in Norwich,<br />
CT, which currently provides ultrasound and MFM services 1½ days per week. The New Bedford<br />
office now employs a staff of six sonographers, two secretaries, and an administrative coordina-<br />
tor. The Division supports regular physician and genetic counselor services at all of these sites.<br />
During academic year 2009-2010 these off-sites provided a total of 2,409 imaging procedures,<br />
142 antenatal testing visits, 429 genetic counseling visits, and 96 MFM consultations.<br />
CLINICAL GENETICS SERVICES<br />
Barbara O’Brien joined Women & Infants Hospital of Rhode Island as the MFM Director of Peri-<br />
natal Clinical Genetics in July 2007, providing oversight of the clinical and educational mission<br />
of the Division’s genetics program. Katharine Wenstrom, MD the division director of MFM, is<br />
also a clinical geneticist with a national reputation in prenatal genetics and prenatal diagnosis.<br />
Office Number of Genetic Counseling Sessions<br />
Providence 1009<br />
New Bedford 273<br />
Foxboro 156<br />
Charlton Memorial XX<br />
South County XX<br />
Norwich 11<br />
Total 1986<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 57<br />
M a t e r n a l – F e t a l M e d i c i n e
M a t e r n a l – F e t a l M e d i c i n e<br />
ACTIVE RESEARCH SUPPORT<br />
Anderson BL: Principal Investigator- Center for AIDS Research (CFAR) Developmental Award<br />
“Effect of trichomonas therapy on genital HIV viral burden among African Women.” Funding<br />
Agency: Lifespan/Tufts/<strong>Brown</strong> Center for AIDS Research . Amount: $40,000. Funded: March 1,<br />
2008-2010.<br />
Anderson BL: Principal investigator-Grant number 1 K23 HD062340-01. K23 Mentored Patient-<br />
Oriented Career Development Award: “The role of mucosal immunity in risk of HIV acquisition<br />
during pregnancy” Funding agency: NIH/NICHD. Funded: August 10, 2009-2013.<br />
Chien, EK: Principal Investigator- Grant Number: 1 R03 HD062683-01. Project Title: Effects of<br />
force and hormonal environment on cervical matrix. Award Issue Date: 07/12/2010.<br />
Chien EK: Co-Investigator – (Barbara McFarlin-PI) 1R21 HD058705-01A2 Biochemical, biome-<br />
chanical and morphological properties of quantitative ultrasound. NIH R21 Funding period<br />
9/20/2009-8/31/2011. $300,447-Direct/$433,373-Total.<br />
Chien EK: Advisor-(Fuson Gundogan-PI). Placental development in fetal alcohol syndrome.<br />
NIAAA: K08 AA016783-01. Funding Period 4/1/07-3/20/12.<br />
Chien EK: Advisor-(Beatrice Lechner-PI). The role of Biglycan in reproduction. NICHD: K08<br />
HD054676-01A2. Funding Period 1/8/2009-12/31/13. $100,000/108,000: 500k/540k.<br />
Cu-Uvin S: 1R25TW008102 (Cu-Uvin) 8/10/08-7/31/2011 1.2 calendar months NIH/FIC<br />
$125,000/yr. Interdisciplinary Framework in Global Health at <strong>Brown</strong> <strong>University</strong>.<br />
Cu-Uvin S: 5U01AI066050 (Friedman) 4/1/2006-3/31/2011 1.2 Calendar Months NIH/NIAID<br />
$18,870. S. japonicum and Birth Outcomes: Randomized Controlled Trial.<br />
Cu-Uvin S: 2P30AI042853 (C Carpenter) 9/1/1998-6/30/2012<br />
0.6 Calendar Months. NIH/NIAID $111,526<br />
Lifespan/Tufts/<strong>Brown</strong> Center for AIDS Research<br />
HIV and Women’s Core — Co – Director<br />
Cu-Uvin S: 1U10AI069472 (Tashima) 12/1/06-11/30/2013<br />
0.24 Calendar Months NIH/NIAID $435,000<br />
Adult Therapeutic Clinical Trials Program for HIV/AIDS<br />
Cu-Uvin S: 200-2002-00610 (Carpenter) 9/27/07-9/28/2011<br />
0.3 Calendar Months CDC $424,822<br />
Study to Understand the Natural History of HIV and AIDS in the Era of Effective Therapy (SUN)<br />
58<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
HONORS AND OFFICES<br />
Susan Cu-Uvin, MD<br />
2008-present: Editorial Advisory Board, The Open Infectious Diseases Journal<br />
2008: Member, Institute of Medicine, National Academy of Sciences, Committee<br />
on Women’s Health Research<br />
2009, April: Chair, Special Emphasis Panel Review, ZRG1 AARR-J 40P, Population and<br />
Behavioral Studies in HIV/AIDS<br />
2009, June: Review Panel Special Emphasis Panel Review, ZRG1 BBBP-J (58) and ZRG1<br />
BBBP-L (58) in HIV/AIDS<br />
2009-2013: Member, NIH/NIAID AIDS Research Review Committee<br />
Donald R Coustan, MD<br />
Treasurer, American Gynecological and Obstetrical Society<br />
Katharine D Wenstrom, MD<br />
Editor in Chief for Obstetrics, Obstetrical and Gynecological Survey, 2005 to present<br />
Editorial Board, American Journal of Perinatology, 2001 to present<br />
Advisory Board for Subspecialty Areas, American Journal of Obstetrics and Gynecology,<br />
2002 to present<br />
PEER-REVIEWED PUBLICATIONS<br />
Wenstrom K, Erickson K, Schulkin J. Are generalist Ob-Gyns satisfied with their MFM<br />
consultants? A survey. AJOG 2009;201(6):S202.<br />
Gyamfi, C, Blumenfeld Y, Ramsey P, Foley M, Kilpatrick S, Wenstrom K. The current state of<br />
MFM fellowships: results from the SMFM fellow survey. AJOG 2009;201(6):S47.<br />
Archabald K, Friedman A, Raker C, Anderson BL. Impact of trimester on morbidity of acute<br />
pyelonephritis in pregnancy. Am J Obstet Gynecol, 2009;201:406.e1-4.<br />
Broughton DE, Beigi RH, Switzer GE, Raker CA, Anderson BL. Obstetric Health Care<br />
Workers’ Attitudes and Beliefs Regarding Influenza Vaccination in Pregnancy. Obstet Gynecol,<br />
2009;114(5): 981-987.<br />
Rodriguez E, Raker CA, Paglia MJ, Anderson BL. Assessment of the need for rapid Group B<br />
Streptococcus testing during labor and delivery. Am J Perinat, 2010;27(6): 475-9.<br />
Luks FI, Carr SR, Muratore CS, O’Brien BM, Tracy TF. The pediatric surgeon’s contribution to<br />
in utero treatment of twin-to-twin transfusion syndrome. Annals of Surgery, 250(3):1-7. 2009<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 59<br />
M a t e r n a l – F e t a l M e d i c i n e
M a t e r n a l – F e t a l M e d i c i n e<br />
Aagaard-Tillery KM, Malone FD, Nyberg DA, Porter TF, Cuckle HS, Fuchs K, Sullivan L,<br />
Comstock CH, Saade GR, Eddleman K, Gross S, Dugoff L, Craigo SD, Timor-Tritsch IE, Carr<br />
SR, Wolfe HM, Bianchi DW, D’Alton ME, for the First and Second Trimester Evaluation of Risk<br />
(FASTER) Research Consortium. Role of Second-Trimester Genetic Sonography After Down<br />
Syndrome Screening. Obstetrics & Gynecology. 114(6):1189-1196, December 2009.<br />
Lambert-Messerlian GM, Palomaki GE , Neveux LM, Chien E, Friedman A, Rosene-Montella K,<br />
Hayes M, Canick JA, Early onset preeclampsia and second trimester serum makers. In press<br />
Prenatal Diagnosis 29: 2209-17. 2009.<br />
Chien EK, Jayakrishnan A, Phipps MG, Dailey TL, Raker CA. Racial and ethnic disparity in<br />
male preterm singleton birth. In Press J Reprod Medicine, June 2010.<br />
Ji H, Long V, Briody V; Chien EK. Progesterone modulates integrin α2(itga2) and α11 (itga11) in<br />
the pregnant cervix. Reproductive Sciences, July 2010 In Press.<br />
Coustan DR, Lowe LP, Metzger BE: The hyperglycemia and adverse pregnancy outcome<br />
(HAPO) study: can we use the results as a basis for change? Journal of Maternal-Fetal and<br />
Neonatal Medicine 23:204-209, 2010.<br />
The HAPO Study Cooperative Research Group (Coustan DR, member of writing group):<br />
Hyperglycemia and adverse pregnancy outcome (HAPO) study: associations with maternal<br />
body mass index. British J ObGyn 117:575-584, 2010.<br />
The HAPO Study Cooperative Research Group (Coustan DR, member of writing group):<br />
Hyperglycemia and adverse pregnancy outcome (HAPO) study: preeclampsia, Am J Obstet<br />
Gynecol 202:255e1-7, 2010.<br />
Coustan DR, Lowe LP, Metzger BE: The Hyperglycemia and Adverse Pregnancy Outcome<br />
(HAPO) study: paving the way for new diagnostic criteria for gestational diabetes mellitus. Am<br />
J Obstet Gynecol 202:654e1-6, 2010.<br />
Dudley DJ, Goldenberg R, Conway D, Silver RM, Saade GR, Varner MW, Pinar H, Coustan D,<br />
Bukowski R, Stoll B, Koch MA, Parker CB, Reddy U for the Stillbirth Research Collaborative<br />
Network: A new system for determining the causes of stillbirth. Obstetrics and Gynecology<br />
116:254-260, 2010.<br />
Coustan DR: Finding and treating gestational diabetes – does it help? Nature Reviews:<br />
Endocrinology. 6:540-542, 2010.<br />
Johnson J. Mersilene versus Ethibond suture efficacy and cerclage. Am J Obstet Gynecol<br />
2009; 201(6):S244.<br />
Johnson J, Anderson B, Raker C, Wenstrom K. Elective inductions at term and adverse<br />
neonatal outcomes. Am J Obstet Gynecol 2009; 201(6):S124-5.<br />
Johnson J, Anderson B, Raker C, Wenstrom K. Timing of delivery with placenta previa:<br />
maternal and neonatal outcomes. Am J Obstet Gynecol 2009; 201(6):S74.<br />
Johnson J, Long V, Ji H, Chien E. Strain induces collagen production by cervical stromal<br />
cells. Am J Obstet Gynecol 2009; 201(6):S74-5.<br />
O’Brien BM. Prenatal Management of twin pregnancies: From the Perspective of an MFM/<br />
Geneticist. The Female Patient, 34(12) December 2009.<br />
O’Brien BM, Feltovich HM, Carr SR, Luks FI. Feto-Fetal Transfusion Syndrome in<br />
Monochorionic Quadruplets. Obstet Gynecol 2010; 115 (2) part 2: 470-472.<br />
60<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
O’Brien BM, Wenstrom KD. Down syndrome screening in the First and Second Trimesters of<br />
Pregnancy. US Obstetrics and Gynecology 2010 vol 4, 58-65.<br />
Kassis N, Jayakrishnan A, Sprawka N, Cu-Uvin S, Anderson BL. Hepatotoxicity and<br />
Metabolic Acidosis Manifested as Non-Reassuring Fetal Testing in a Pregnant Woman on<br />
Antiretroviral Therapy. Obstet Gynecol, 2010;116: 515–7.<br />
NON PEER-REVIEWED PUBLICATIONS<br />
Coustan DR: Examining the Evidence: Is metformin more effective than glyburide for treating<br />
gestational diabetes? OBG Management 22:18-21, 2010.<br />
Coustan DR: Diabetes mellitus. Precis: Obstetrics (4th edition) Washington, DC: American<br />
College of Obstetricians and Gynecologists, 2010. Pp. 133-138.<br />
BOOKS AND BOOK CHAPTERS<br />
Wenstrom K. Invasive Fetal Testing: Chorionic Villus Sampling and Amniocentesis.<br />
In: Queenan J, Hobbins, Spong C, eds. Protocols for High-Risk Pregnancies, 5 th edition.<br />
Philadelphia: Wiley-Blackwell, 2010.<br />
Wenstrom K. Cardiac Disease. In: Queenan J, Hobbins, Spong C, eds. Protocols for High-Risk<br />
Pregnancies, 5 th edition. Philadelphia: Wiley-Blackwell, 2010.<br />
Wenstrom KD: Precis XIV Prenatal Diagnosis of Genetic Disorders. American College of<br />
Obstetricians, 2010.<br />
Wenstrom KD: Precis XIV Teratogenic Exposures. American College of Obstetricians, 2010.<br />
Wenstrom KD: Precis XIV Preconception Counseling. American College of Obstetricians,<br />
2010.<br />
Wenstrom KD: Precis XIV Substance Abuse. American College of Obstetricians, 2010.<br />
INVITED PRESENTATIONS (LOCAL)<br />
Wenstrom, KD. Grand Rounds: The Fetal Origins of Adult Disease or Why Obstetrics is the<br />
Most Important Specialty. Women & Infants Hospital, Providence, RI. March 4, 2010.<br />
Anderson BL. RI Association of Nurses in AIDS Care, 6th <strong>Annual</strong> Teaching Day, Warwick, RI,<br />
“Diagnosis and Management of HIV-1 in Pregnancy” September 25, 2009<br />
Anderson BL. Women & Infant’s Hospital Board of Trustees, “Preparedness for pandemic<br />
influenza at Women & Infant’s Hospital” September 29, 2009<br />
Anderson BL. Women & Infant’s Hospital Quality Forum, “Case presentation-peripheral line<br />
infection” December 9, 2009<br />
Anderson BL. Women & Infant’s Hospital Union H1N1 Preparedness Day, “Preparedness for<br />
pandemic influenza at Women & Infant’s Hospital” December 10, 2009.<br />
Chien EK. 14th <strong>Annual</strong> Neonatology-Pediatric conference, Southcoast Hospitals, Nov 4, 2009,<br />
Fall River, MA. Title: PROM at the Borders of Viability<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 61<br />
M a t e r n a l – F e t a l M e d i c i n e
M a t e r n a l – F e t a l M e d i c i n e<br />
Chien EK. Medical Student Lectures: March 8, 2010. Title: Physiology of Labor BIOL 3674<br />
Human Reproduction Growth and Development<br />
Chien EK. Resident Core Lecture: February 5, 2010. Title: IUGR<br />
Chien EK. Neonatal Fellows Core lectures: November 5, 2009. Title: IUGR<br />
Chien EK. MADAM April 16th, 2010. Title: Trisomy 21 and Congenital Heart Disease<br />
Johnson, J. “Thrombophilia and Pregnancy” Women & Infants’ Grand Rounds, Providence RI<br />
December 2009<br />
Johnson J. “Preterm Labor Management and the Use of Magnesium Sulfate for CP<br />
Prophylaxis” St. Luke’s Hospital Grand Rounds, New Bedford MA, December 2009<br />
O’Brien BM. MADAM October 2, 2009. Title: Fetal Abdominal cysts<br />
O’Brien BM. MADAM December 4, 2009. Title: Fetal Patient Round-Up<br />
O’Brien, BM. MADAM January 15, 2010. Title: Fetal Patient Round-Up<br />
O’Brien BM. MADAM February 5, 2010. Title: Selective Termination in TTTS<br />
O’Brien BM. MADAM March 5, 2010- Macrosomia and Overgrowth Syndromes<br />
O’Brien BM. MADAM March 19, 2010 Title: FDA Fetal Surgery Protocol for Diaphragmatic<br />
Hernia<br />
O’Brien BM. MADAM May 7, 2010. Title: Myelomeningocele<br />
O’Brien BM. MADAM June 4, 2010. Title: Fetal Patient Round-Up<br />
O’Brien BM. MADAM June 18, 2010. Title: Fetal Patient Round-Up<br />
O’Brien BM. MADAM August 6, 2010. Title: CCAMs and Other Pulmonary Lesions<br />
O’Brien BM. MADAM October 1, 2010. Title: Fetal Patient Round-Up<br />
Sprawka N. Anticoagulation in Pregnancy. Current Concepts: Issues in Perinatal & Neonatal<br />
Care Conference in Warwick, RI, 2009<br />
Sprawka N. Postpartum Hemorrhage. Intern Lecture Series 2009<br />
Sprawka N. Thalassemia. Maternal Fetal Medicine Resident Lecture 2009<br />
Sprawka N. Elevated Aminotransferases in Pregnancy. Maternal Fetal Medicine Lecture 2009<br />
Sprawka N. Abdominal Wall Defects. Perinatal Management Conference 2009<br />
Sprawka N. Amniotic Band Sequence. Multidisciplinary Antenatal Diagnosis and Management<br />
Conference 2009<br />
Sprawka N. Sacrococcygeal Teratoma. Multidisciplinary Antenatal Diagnosis and Management<br />
Conference 2009<br />
Sprawka N. Intrauterine Growth Restriction. Perinatal Management Conference 2009<br />
62<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Sprawka N. Cleft Lip and Palate. Multidisciplinary Antenatal Diagnosis and Management<br />
Conference 2010<br />
Sprawka N. Prenatal Diagnosis of Skeletal Dysplasias. Perinatal Management Conference<br />
2010<br />
INVITED PRESENTATIONS (NATIONAL)<br />
Wenstrom K. Current Trends and New Direction in Ob/Gyn Seminar: Folic Acid: the Answer to<br />
Everything. Mount Auburn Hospital, Waltham, MA. November 18, 2009.<br />
Anderson BL. Society for Maternal Fetal Medicine, Infectious Disease and Inflammation<br />
Special Interest Group, Leader, 2009-2010.<br />
Anderson BL. Work-in-progress Seminar, Cervicovaginal fluid from pregnant and nonpregnant<br />
women and in vitro HIV suppression, Dartmouth Medical Center, Laboratory of<br />
Charles R. Wira, PhD, January 6, 2010.<br />
Anderson BL. Invited participant in National Institute of Allergy and Infectious Diseases,<br />
Division of Acquired Immunodeficiency Syndrome meeting, “Mucosal Immunity in the Male<br />
and Female Reproductive Tract”, Dartmouth Hitchcock Medical Center, Lebanon, NH, June 30-<br />
July 2, 2010.<br />
Coustan DR. Toward New Criteria for Gestational Diabetes. American Gynecologic and<br />
Obstetrical Society, Chicago, October 2009.<br />
Coustan DR. Gestational Diabetes Update – 2009. New England Obstetrical and Gynecological<br />
Society Fall Meeting, Sturbridge MA, November 2009.<br />
Coustan DR. The independent contribution of BMI to outcomes in the HAPO study. GDM<br />
Pasadena II: An International Conference on Gestational Diabetes. Pasadena, CA April 2010.<br />
(Coustan DR, Metzger BE, Lowe LP, Dyer AE); also moderator of session on pharmacologic<br />
management of GDM.<br />
Coustan DR. Clinical Seminar: Contemporary Approaches to Diabetes in Pregnancy.<br />
American College of Obstetricians and Gynecologists 58th <strong>Annual</strong> Clinical Meeting, San<br />
Francisco, May 2010.<br />
Coustan DR. The evolution of perinatal care: a personal perspective. Sloane Academic<br />
Assembly of graduating residents and fellows, Department of Obstetrics and Gynecology,<br />
Columbia <strong>University</strong> College of Physicians and Surgeons, New York City, June 2010.<br />
Coustan DR. Developing new criteria for gestational diabetes. Rosen Lecture, Sloane<br />
Symposium. Department of Obstetrics and Gynecology, Columbia <strong>University</strong> College of<br />
Physicians and Surgeons, New York, NY. June 2010.<br />
Beck NM, Phornphutkul C, O’Brien B, Abuelo DN. A novel heterozygous deletion and insertion<br />
mutation in COL1A2 in a family with overlapping features of osteogenesis imperfecta and<br />
Ehlers-Danlos syndrome. NSGC AEC, Dallas, TX. October 2010.<br />
INVITED PRESENTATIONS (INTERNATIONAL)<br />
Coustan DR. HAPO Update. 9th World Congress of Perinatal Medicine. Berlin, Germany,<br />
October 2009.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 63<br />
M a t e r n a l – F e t a l M e d i c i n e
M a t e r n a l – F e t a l M e d i c i n e<br />
Sprawka N. Lambert-Messerlian G, Palomaki G, Eklund E, Canick J. The Effect of Oral<br />
Antidiabetic Agents on Maternal Serum Alpha-Fetoprotein Levels in Diabetic Pregnancies. Oral<br />
presentation at the biannual meeting for the International Society for Prenatal Diagnosis in<br />
Amsterdam, Netherlands, 2010.<br />
64<br />
ABSTRACT PRESENTATIONS (NATIONAL)<br />
Wenstrom K, Erickson K, Schulkin J. Are generalist Ob-Gyns satisfied with their MFM<br />
consultants? A survey. Society of Maternal-Fetal Medicine Poster Presentation, Chicago IL,<br />
February 2010.<br />
Gyamfi, C, Blumenfeld Y, Ramsey P, Foley M, Kilpatrick S, Wenstrom K. The current state of<br />
MFM fellowships: results from the SMFM fellow survey. Society of Maternal-Fetal Medicine<br />
Poster Presentation, Chicago IL, 2010.<br />
Anderson BL, Hillier SL, Raker C, Fitzsimmons C, Cu-Uvin S. Maternal inflammatory<br />
mediators are increased as early as the first trimester in low risk pregnancies. Poster<br />
presentation at the 30th <strong>Annual</strong> Meeting of the Society for Maternal Fetal Medicine, February,<br />
2010, Chicago, IL. American Journal of Obstetrics and Gynecology 2009;201(6, Supplement<br />
1):S231.<br />
Johnson JM, Anderson BL. Mersilene Versus Ethibond Suture Efficacy and Cerclage. Poster<br />
presentation at the 30th <strong>Annual</strong> Meeting of the Society for Maternal Fetal Medicine, February,<br />
2010, Chicago, IL. American Journal of Obstetrics and Gynecology 2009;201(6, Supplement<br />
1):S244.<br />
Johnson JM, Anderson BL, Raker C, Wenstrom KD. Timing of delivery with placenta<br />
previa: maternal and neonatal outcomes. Poster presentation at the 30th <strong>Annual</strong> Meeting of<br />
the Society for Maternal Fetal Medicine, February, 2010, Chicago, IL. American Journal of<br />
Obstetrics and Gynecology 2009;201(6, Supplement 1):S74.<br />
Johnson JM, Anderson BL, Raker C, Wenstrom KD. Elective Inductions at Term and Adverse<br />
Neonatal Outcomes. Poster presentation at the 30th <strong>Annual</strong> Meeting of the Society for<br />
Maternal Fetal Medicine, February, 2010, Chicago, IL. American Journal of Obstetrics and<br />
Gynecology 2009;201(6, Supplement 1):S124-5.<br />
Anderson BL, Wira CR, Fitzsimmons C, Ghosh M, Fahey J, Cu-Uvin S. Cervicovaginal fluid<br />
from pregnant and non-pregnant women suppresses HIV infectivity in an in vitro model. Oral<br />
presentation at the 30th <strong>Annual</strong> Meeting of the Society for Maternal Fetal Medicine, February,<br />
2010, Chicago, IL. American Journal of Obstetrics and Gynecology 2009;201(6, Supplement<br />
1):S43.<br />
Matteson KA, McMahon M, Sung VW, Anderson BL, Raker CA, Phipps MG. Development and<br />
evaluation of a formal research curriculum for obstetrics and gynecology residents. Poster<br />
presentation at the 2010 APGO CREOG <strong>Annual</strong> Meeting, March, 2010, Orlando, FL.<br />
Anderson BL for the Eunice Kennedy Shriver National Institute of Child Health and Human<br />
Development, Maternal Fetal Medicine Units Network. The impact of antibiotic therapy on<br />
vaginal flora among women with a positive fetal fibronectin. Poster presentation at the 57th<br />
<strong>Annual</strong> Meeting of the Society for Gynecologic Investigation, March, 2010, Orlando, FL.<br />
McDonnold MA, Friedman A, Raker C, Anderson B. Morbidity Associated with Postpartum<br />
Pyelonephritis as Compared to an Antepartum Population. Poster presentation for the 58th<br />
annual clinical meeting of the American Congress of Obstetricians and Gynecologists, May,<br />
2010, San Francisco, CA.<br />
Anderson BL, Rouse DJ, Fitzsimmons C. Clinical Characteristics of Pregnant Women with<br />
2009 H1N1 Influenza. Poster presentation at the 37th <strong>Annual</strong> Meeting for the Infectious Disease<br />
Society for Obstetrics and Gynecology, Santa Fe, NM, August, 2010.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Anderson BL, Firnhaber C, Liu T, Swarts A, Siminaya M, Cu-Uvin S. Self-Collected Vaginal<br />
Swabs for Trichomoniasis Testing in HIV-infected Women in South Africa. Poster presentation<br />
at the 37th <strong>Annual</strong> Meeting for the Infectious Disease Society for Obstetrics and Gynecology,<br />
Santa Fe, NM, August, 2010.<br />
Anderson BL, Wira CR, Fitzsimmons C, Ghosh M, Fahey J, Cu-Uvin S. Cervicovaginal Fluid<br />
from Third Trimester Pregnant and Non-Pregnant Women Suppresses HIV Infectivity in an In<br />
Vitro Model. Poster presentation at the 37th <strong>Annual</strong> Meeting for the Infectious Disease Society<br />
for Obstetrics and Gynecology, Santa Fe, NM, August, 2010<br />
Critchfield A, Ji H, Long V, Chien EK. Changes in cervical elastin concentration in the pregnant<br />
rat. Society for Maternal Fetal Medicine <strong>Annual</strong> Meeting 2010. Chicago, IL. Am J Obstet<br />
Gynecol 201:S74-75:2010.<br />
Johnson J, Long V, Ji H, Chien EK. Strain induces collagen production by cervical stromal<br />
cells. Society for Maternal Fetal Medicine <strong>Annual</strong> Meeting 2010. Chicago, IL. Am J Obstet<br />
Gynecol 201:S84:2010.<br />
Ji H, Long V, Chien EK. Mechanical stretch modulates extracellular matrix remodeling<br />
and MAP kinase pathway activation in rat cervical stromal cells. Society for Gynecologic<br />
Investigation <strong>Annual</strong> Meeting, Orlando, FL. March 2010. Reprod Sciences 17(3):74A, 2010.<br />
Ji H, Briody V, Noh J-H, Chien EK. Integrin α2 is modulated by stretch in rat cervical stromal<br />
cells. Society for Maternal Fetal Medicine <strong>Annual</strong> Meeting 2011, San Francisco, CA. (Accepted)<br />
Yogev Y, Chen R, Hod M, Coustan D, Oats JJN, Metzger B, Lowe L, Dyer AR, Trimble,<br />
Hadden D, Persson B for the HAPO Study Cooperative Research Group: Associations with<br />
preeclampsia: lessons from the hyperglycemia and adverse pregnancy outcome (HAPO) study.<br />
Society for Maternal-Fetal Medicine 30th <strong>Annual</strong> Meeting, Chicago, February 2010.<br />
Johnson J. Mersilene versus Ethibond suture efficacy and cerclage. Society of Maternal-Fetal<br />
Medicine Poster Presentation, Chicago IL, February 2010.<br />
Johnson J, Anderson B, Raker C, Wenstrom K. Elective inductions at term and adverse<br />
neonatal outcomes. Society of Maternal-Fetal Medicine Poster Presentation, Chicago IL,<br />
February 2010.<br />
Johnson J, Anderson B, Raker C, Wenstrom K. Timing of delivery with placenta previa:<br />
maternal and neonatal outcomes. Society of Maternal-Fetal Medicine Poster Presentation,<br />
Chicago IL, February 2010.<br />
Johnson J, Long V, Ji H, Chien E. Strain induces collagen production by cervical stromal<br />
cells. Society of Maternal-Fetal Medicine Poster Presentation, Chicago IL, February 2010.<br />
Sprawka N, Timmins, A, Sangi-Haghpeykar, H, Mathieson, K, Coonrod, D. Troponin I Levels in<br />
Mild and Severe Preeclampsia. <strong>Annual</strong> meeting for the Society of Maternal Fetal Medicine in<br />
San Diego, CA, 2009<br />
Kassis N, Heard A, Sprawka N, Cu-Uvin S, Anderson B. Antiretroviral Induced Hepatotoxicity<br />
Presenting as Non-Reassuring Fetal Testing. <strong>Annual</strong> meeting for Infectious Diseases Society for<br />
Obstetrics and Gynecology Montreal, QC 2009<br />
Sprawka N, Lambert-Messerlian G, Palomaki G, Canick J. The Effect of Oral Hypoglycemic<br />
Agents on Maternal Serum Alpha-Fetoprotein Levels in Diabetic Pregnancies. <strong>Annual</strong> meeting<br />
for the Society of Maternal Fetal Medicine in Chicago, IL, 2010.<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 65<br />
M a t e r n a l – F e t a l M e d i c i n e
M e d i c a l E d u c a t i o n<br />
CLERKSHIP PROGRAM<br />
66<br />
MEDICAL EDUCATION<br />
B. Star Hampton, MD, Clerkship Director<br />
Dr. Hampton, Assistant Professor of Obstetrics and Gynecology and a member of<br />
the Division of Urogynecology and Reconstructive Pelvic Surgery, continues her<br />
role as Director of the Obstetrics and Gynecology Core Clerkship for the Alpert<br />
School of Medicine of <strong>Brown</strong> <strong>University</strong>.<br />
Barbara M. O’Brien, MD, Associate Clerkship Director<br />
Dr. O’Brien, Assistant Professor of Obstetrics and Gynecology and a member of<br />
the Division of Maternal Fetal Medicine, continues her active role as the Associate<br />
Director.<br />
The core clerkship continues to flourish, as evidenced by improved overall evalu-<br />
ations of the clerkship as well as an increase in numbers of students interested in pursing<br />
Ob/Gyn residencies. The 2009 match saw eight Alpert Medical Students successfully pursue<br />
Ob/Gyn residencies, and the coming year has even more interested.<br />
This year students began to be assigned time on Maternal Fetal Medicine, rotating with that<br />
service for two mornings during their time on labor and delivery. This afforded students expo-<br />
sure to patients with high-risk pregnancies, and allowed students to be part of the team for a<br />
short time. Students felt this was a valuable addition to their learning experience, and stated<br />
they only wished they had more time with the team.<br />
Students continue to be taught according to APGO medical student learning objectives. Exist-<br />
ing lecture content is continuously reviewed and revised based on these learning objectives as<br />
well as student feedback. Students are encouraged to utilize resources provided by APGO such<br />
as uWise shelf exam review questions, which are recognized with favorable comments.<br />
Outpatient community based faculty preceptorships continue to provide students with ad-<br />
ditional outpatient experience and exposure to physicians in the community. Students spend<br />
one half day session in their preceptor’s office, gaining valuable exposure to the “daily life” of<br />
a community-based faculty member. Comments from both students and physicians alike are<br />
very favorable.<br />
The RIME method to classify students into one of four categories, namely <strong>Report</strong>er, Interpreter,<br />
Manager, and Educator is still utilized for mid-clerkship review of each student. The clerkship<br />
directors meet with each student at mid-clerkship to review individual comments and classifi-<br />
cation, as well as student self assessment and goals. In addition, a “patient passport” is used<br />
in an effort to review student clinical exposure and experience. Review of students’ clinical<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
experience reveals excellent scope and breadth. Dr. Hampton and Dr. O’Brien also meet with<br />
students at the end of each clerkship to discuss how to improve the experience, and changes<br />
are made according to student suggestions.<br />
Outstanding resident and faculty involvement in student teaching continues to be encouraged<br />
and facilitated. Directors meet with residents during resident business meetings to address any<br />
student concerns or changes. Residents continue to have an important role in medical student<br />
orientation, with residents reviewing ward expectations, scrubbing, gowning and gloving,<br />
instrument recognition, and knot tying. Quality of teaching scores continue to increase as rated<br />
by the students at the end of the clerkship.<br />
Students have the option to participate in Dr. Pablo Rodriguez’ Latino radio show, “Nuestro<br />
Salud.” This unique experience allows students the opportunity to present a case they have<br />
prepared for their classmates and explain it to a lay, Latino population. This enables the stu-<br />
dents to improve not only their communication skills but also their health literacy skills. The<br />
student interest group is also active on the <strong>Brown</strong> campus. Activities throughout the year<br />
include “Deliver a Baby Week” as well as application and interview primers for students inter-<br />
ested in Ob/Gyn.<br />
OB/GYN RESIDENCY PROGRAM<br />
Gary Frishman, MD continues in his role as both the Residency<br />
Program Director and the Associate Division Director in the Divi-<br />
sion of Reproductive Endocrinology and Infertility. Roxanne Vrees,<br />
MD is the Associate Residency Program Director and continues her<br />
work in Triage.<br />
Eight residents graduated from the program with six entering fel-<br />
lowship programs (two at Women & Infants), one entering private practice and one entering<br />
the Indian Health Service on the Navajo Nation reservation.<br />
In 2010, four hundred sixty-four candidates applied to the <strong>Brown</strong> Ob/Gyn Residency Program.<br />
We interviewed eighty to fill the eight intern positions for the 2010-2011 academic year. The<br />
total number of residents in the four-year program is 32.<br />
We have increased our formalized didactic experiences with scheduled talks every day on<br />
rounds with both the obstetric and gynecologic services. A new Pediatric Outcomes multi-dis-<br />
ciplinary conference has been added to the noon conference schedule. The new PGY 1 resi-<br />
dents receive special dedicated lecture topics in the fall geared towards their needs and level<br />
of training.<br />
The program has moved to a new web-based recording system for resident duty hours.<br />
We are implementing new educational formats including a posted question on the labor floor<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 67<br />
M e d i c a l E d u c a t i o n
M e d i c a l E d u c a t i o n<br />
for medical students, residents, and nursing staff to respond to as well as a fetal monitor strip<br />
review for obstetric rounds.<br />
We have two new rotations having added a new “swing shift” block with last year’s third-year<br />
class to facilitate residents’ ability to leave the hospital and stay within duty hours on busy servic-<br />
es as well as, with this year, a new “float” rotation in the fourth year class which provides them<br />
the opportunity and ability to rotate in areas in which they feel that they have specific interest or<br />
feel the need for additional exposure to (examples include the wound clinic at Kent Hospital, hav-<br />
ing a session at the Women’s Day Hospital, additional ultrasound exposure at the PDC, etc.).<br />
Under the direction of Dr. Pagidas, we have implemented a new ultrasound curriculum integrat-<br />
ing Maternal Fetal Medicine, Triage, Reproductive Endocrinology, etc.) with the ultimate goal of<br />
having residents being able to apply for AIUM certification upon graduation.<br />
In addition to the annual dinner held for the PGY 2 class with the Fellowship Directors (at which<br />
time informal discussions are held about the subspecialties and fellowships), we have added a<br />
dinner with Generalist Faculty to offer complementary information about going into Private Prac-<br />
tice.<br />
We had our second annual “mini-boot camp” given by our residents for the graduating <strong>Brown</strong><br />
Medical Students going into Ob/Gyn at any Residency Program around the country. This provides<br />
our students with a jump start prior to starting internship. Topics reviewed include writing orders,<br />
performing an endometrial biopsy, rupturing membranes and placing a scalp clip, etc.<br />
SAPHIER FAMILY LECTURE IN OBSTETRICS AND GYNECOLOGY<br />
Established in 2007 by Carl J. Saphier ‘88 MD’92 to support an annual lecture focused on issues<br />
related to Women’s Health, including Maternal Fetal Medicine, Reproductive Endocrinology and<br />
Fertility, Urogynecology, and Women’s Oncology.<br />
<strong>Brown</strong> and the World: Engaging HIV-Infected Women<br />
Susan Cu-Uvin, MD<br />
The Miriam Hospital, Providence, RI<br />
Director, Global Health Initiative, <strong>Brown</strong> <strong>University</strong><br />
Professor, Ob/Gyn and Medicine, The Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong><br />
8:30 a.m. Research Paper Presentations<br />
68<br />
Ob/Gyn Residents and Fellows<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
RESIDENT/FELLOW RESEARCH DAY<br />
Guest Judge: Susan Cu-Uvin, MD<br />
The Miriam Hospital, Providence, RI<br />
Director, Global Health Initiative, <strong>Brown</strong> <strong>University</strong><br />
Professor, Ob/Gyn and Medicine, The Warren Alpert Medical School of<br />
<strong>Brown</strong> <strong>University</strong><br />
Judges: Joanna M. Cain, MD, Obstetrician and Gynecologist-in-Chief<br />
Gary N. Frishman, MD, Residency Program Director<br />
Moderator: Kristen A. Matteson, MD, MPH<br />
Presenting Residents<br />
Karen L. Archabald, MD, Resident in Obstetrics and Gynecology: Anemia and chorioamnionitis<br />
at term<br />
Julie A. Baker, MD, PhD, Resident in Obstetrics and Gynecology: Association between mater-<br />
nal-fetal attachment and quitting smoking with pregnancy recognition<br />
Molly S. Carey, MD, Resident in Obstetrics and Gynecology: An observational study of pain<br />
with IUD insertion<br />
Laura L. Holman, MD, Resident in Obstetrics and Gynecology: A comparison of sentinel<br />
lymph node identification between lymphoscintigraphy and sentinel lymph node dissection<br />
in patients with vulvar cancer<br />
Amanda L. Jackson, MD, Resident in Obstetrics and Gynecology: A novel biomarker for the<br />
management of patients with epithelial ovarian cancer<br />
Nadine Kassis, MD, Resident in Obstetrics and Gynecology: Effect of surgical therapy on<br />
improving physical activity levels in women with stress urinary incontinence<br />
Mollie A. McDonnold, MD, Resident in Obstetrics and Gynecology: Neurologic outcomes<br />
associated with polyhydramnios<br />
Megan D. McMahon, MD, Resident in Obstetrics and Gynecology: The effect of obesity on peri-<br />
operative outcomes of laparoscopic hysterectomy<br />
Presenting Fellows<br />
Sonali Pandya, MD, Fellow in Breast Health: Should we excise all breast core-biopsy proven<br />
papillary lesions?<br />
Ashley Stuckey, MD, Fellow in Gynecologic Oncology: Developing an integrated genomic ap-<br />
proach to explore the antitumor activity of vitamin D and derivatives to treat ovarian cancer<br />
Julie M. Johnson, MD, Fellow in Maternal Fetal Medicine: Mersilene versus Ethibond suture<br />
efficacy and cerclage<br />
Kyle J. Wohlrab, MD, Fellow in Urogynecology: The association between regional anesthesia<br />
and acute postoperative urinary retention in women undergoing outpatient midurethral slings.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 69<br />
M e d i c a l E d u c a t i o n
M e d i c a l E d u c a t i o n<br />
FACULTY AND RESIDENT AWARDS<br />
UNDERGRADUATE MEDICAL EDUCATION TEACHING AWARDS<br />
APGO Excellence-in-Teaching Award<br />
Christina Bandera, MD<br />
Top Community-based Faculty Teacher of the Year Awards<br />
Kathleen Bowling, MD<br />
Frank Pensa, MD<br />
Pablo Rodriguez, MD<br />
Meera Simoes, MD<br />
Jackie Tetreault, MD<br />
Top Hospital-based Faculty Teacher of the Year Awards<br />
Amy Gottlieb, MD<br />
Michael Paglia, MD<br />
Maureen Phipps, MD<br />
Charles Rardin, MD<br />
Vivian Sung, MD<br />
Top Fellow Teacher of the Year Award<br />
Kyle Wohlrab, MD<br />
Top Resident Teacher of the Year Award<br />
Megan McMahon, MD<br />
Top Specialty Nursing Faculty Teacher of the Year Award<br />
Ann Holdredge, CNM, NP<br />
Top Community-based Faculty Excellence-in-Teaching Awards<br />
Dave Beitle, MD<br />
Jennifer Boyle, MD<br />
Kathleen Bowling, MD<br />
Paula DeYoung, MD<br />
Michele Gange, MD<br />
Fred Hawwa, MD<br />
70<br />
Tolga Kokturk, MD<br />
Frank Pensa, MD<br />
Pablo Rodriguez, MD<br />
Meera Simoes, MD<br />
Jackie Tetreault, MD<br />
Marguerite Vigliani, MD<br />
Hospital-based Faculty Excellence-in-Teaching Awards<br />
Rebecca Allen, MD<br />
Christina Bandera, MD<br />
Andrew Blazar, MD<br />
Cassandra Carberry, MD<br />
Steve Carr, MD<br />
Donald Coustan, MD<br />
Paul DiSilvestro, MD<br />
Sarah Fox, MD<br />
Gary Frishman, MD<br />
Amy Gottlieb, MD<br />
Star Hampton, MD<br />
Donna LaFontaine, MD<br />
Kristen Matteson, MD<br />
Barbara O’Brien, MD<br />
Michael Paglia, MD<br />
Maureen Phipps, MD<br />
Charles Rardin, MD<br />
Pablo Rodriguez, MD<br />
Vivian Sung, MD<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y<br />
Trevor Tejada Berges, MD
Specialty Nursing Faculty<br />
Excellence-in-Teaching Awards<br />
Diane Angelini, EdD, CNM<br />
Anne Cooper, RNP<br />
Paulette Corey, RNP<br />
Erin Dobson, RNP<br />
Elisabeth Howard, PhD, CNM<br />
Linda Hunter, EdD, CNM<br />
Edie McConaughey, CNM<br />
Linda Moulton, RNP<br />
Patricia O’Connell , RNP<br />
Janet Singer, MSN, CNM<br />
Linda Steinhardt, MS, FNP-C, CNM<br />
Anne Stulik, RNP<br />
Resident Excellence-in-Teaching Awards<br />
Catherine Albright, MD<br />
Karen Archibald, MD<br />
Elizabeth Cappelletti, MD<br />
Molly Carey, MD<br />
Beth Cronin, MD<br />
Luu Doan, MD<br />
Terri Febbraro, MD<br />
Amanda Jackson, MD<br />
Jennifer Kang, MD<br />
Nadine Kassis, MD<br />
Mollie McDonnold, MD<br />
Megan McCoin, MD<br />
Katherine Melzer, MD<br />
Jeannine Miranne, MD<br />
Kavita Mishra, MD<br />
Katina Mori, MD<br />
Michaela Onstad, MD<br />
Pablo Orezzoli, MD<br />
Dario Roque, MD<br />
RESIDENT MEDICAL EDUCATION TEACHING AWARDS<br />
CREOG Excellence-in-Teaching Award<br />
Donald R. Coustan, MD<br />
Top Community-based Faculty Teacher of the Year Awards<br />
Terrence Cahill, MD<br />
Rebecca Crichton, MD<br />
Kathryn Davis, MD<br />
Cynthia Hanna, MD<br />
Tawfik Hawwa, MD<br />
Top Hospital-based Faculty Teacher of the Year Awards<br />
Donald Coustan, MD<br />
Robyn Gray, DO<br />
Kristen Matteson, MD<br />
Barbara O’Brien, MD<br />
Charles Rardin, MD<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 71<br />
M e d i c a l E d u c a t i o n
M e d i c a l E d u c a t i o n<br />
Top Fellow Teacher of the Year Awards<br />
Kyle Wohlrab, MD<br />
Wendy Vitek, MD<br />
Top Specialty Nursing Faculty Teacher of the Year Awards<br />
Elisabeth Howard, CNM<br />
Edie McConaughey, CNM<br />
Community-based Faculty Excellence-in-Teaching Awards<br />
David Beitle, MD<br />
Kathleen Bowling, MD<br />
Christine Brousseau, MD<br />
Terrence Cahill, MD<br />
Wayne Clairborne, MD<br />
Jeannine Connolly, MD<br />
Rebecca Crichton, MD<br />
Kathryn Davis, MD<br />
Joseph DeMartino, MD<br />
Beata DiZoglio, MD<br />
72<br />
Stephen Falkenberry, MD<br />
Alfredo Gil, MD<br />
Cynthia Hanna, MD<br />
Tawfik Hawwa, MD<br />
Janet Lefkowitz, MD<br />
Carol Manning, MD<br />
Carol Medeiros, MD<br />
Frank Pensa, MD<br />
Marilyn Powers, MD<br />
Gary Wharton, MD<br />
Hospital-based Faculty Excellence-in-Teaching Awards<br />
Brenna Anderson, MD<br />
Bala Bhagavath, MD<br />
Andrew Blazar, MD<br />
Joanna Cain, MD<br />
Donald Coustan, MD<br />
Gary Frishman, MD<br />
Robyn Gray, DO<br />
B. Star Hampton, MD<br />
Donna LaFontaine, MD<br />
Kristen Matteson, MD<br />
Fellow Excellence-in-<br />
Teaching Awards<br />
Nada Kawar, MD<br />
Peter Klatsky, MD<br />
Katrin Kristjansdottir, MD<br />
Blair Washington, MD<br />
Kyle Wohlrab, MD<br />
Wendy Vitek, MD<br />
Deborah Myers, MD<br />
Barbara O’Brien, MD<br />
Kelly Pagidas, MD<br />
Maureen Phipps, MD<br />
Charles Rardin, MD<br />
Moune Jabre Raughley, MD<br />
Vivian Sung, MD<br />
Trevor Tejada-Berges, MD<br />
Roxanne Vrees, MD<br />
Katharine Wenstrom, MD<br />
Specialty Nursing Faculty Excellence-in-<br />
Teaching Awards<br />
Diane Angelini, EdD, CNM<br />
Elisabeth Howard, PhD, CNM<br />
Linda Hunter, EdD, CNM<br />
Edie McConaughey, CNM<br />
Janet Singer, CNM<br />
Linda Steinhardt, MS, FNP-C, CNM<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
RESIDENT AWARDS FROM FACULTY<br />
David H. Nichols Award for Excellence in Pelvic Surgery<br />
Beth Cronin, MD<br />
Excellence in Resident Research Award<br />
Mollie McDonnold, MD<br />
The Outstanding Resident Award for Professionalism and Humanism in Women’s Health<br />
Megan McMahon, MD<br />
Chief Administrative Resident Awards<br />
Beth Cronin, MD and Laura Richio, MD<br />
AAGL Special Resident in Minimally Invasive Gynecology<br />
Nicole Korbly, MD<br />
SLS Outstanding Laparoendoscopic Resident Surgeon<br />
Nadine Kassis, MD<br />
AWARDS FROM CHIEF RESIDENTS<br />
The “Life Saver” Award<br />
Robyn Gray, DO<br />
Mentorship Award<br />
Kathleen Bowling, MD<br />
Community-based Faculty Awards<br />
Terrence Cahill, MD<br />
Beata DiZoglio, MD<br />
Lisa Domagalski, MD<br />
Tawfik Hawwa, MD<br />
Carol Manning, MD<br />
Gary Wharton, MD<br />
Hospital-based Faculty Awards<br />
Bala Bhagavath, MD<br />
Paul DiSilvestro, MD<br />
Star Hampton, MD<br />
Kristen Matteson, MD<br />
Barbara O’Brien, MD<br />
Maureen Phipps, MD<br />
Special Recognition Awards<br />
Wendy Bergren, RN<br />
Cynthia DiBlasi, RN<br />
Dita Lubera, RN<br />
Barbara McCaffrey<br />
Karen Newberg<br />
Noemia Norberg, RN<br />
Sue Pirri<br />
Ana Santos<br />
Chrystal Smith<br />
Pat Vest<br />
Fellow of Excellence Award<br />
Kyle Wohlrab, MD<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 73<br />
M e d i c a l E d u c a t i o n
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y<br />
74<br />
DIVISION OF REPRODUCTIVE<br />
ENDROCRINOLOGY AND INFERTILITY<br />
MISSION: CARING, SHARING, QUERYING<br />
Caring for patients during their reproductive lifespan, sharing educational aspects to students<br />
of reproduction, and querying through research aspects of reproductive medicine embodies<br />
the mission of the Division of Reproductive Endocrinology and Infertility. The Center for Repro-<br />
duction and Infertility is the clinical service of the division encompassing patients with prob-<br />
lems involving endocrinology of the reproductive system, lactation, and pregnancy; infertility,<br />
in vitro fertilization [IVF], and surgical repair to restore reproductive function; reproductive<br />
anomalies; the menopause; pediatric gynecology, and disorders of puberty, ovulatory function,<br />
hirsutism, and galactorrhea.<br />
FACULTY<br />
Sandra Ann Carson, MD, Division Director<br />
MD: Northwestern <strong>University</strong><br />
Residency: Prentice Women’s Hospital, Northwestern <strong>University</strong><br />
Fellowship: <strong>University</strong> of Chicago<br />
Dr. Carson joined the division in 2007 as its director and a Professor of Ob-<br />
stetrics and Gynecology. She came from Baylor College of Medicine where<br />
she directed the Programs in Advanced Reproduction. Her research in ecto-<br />
pic pregnancy, unexplained infertility and polycystic ovarian disease has been supported for<br />
over 15 years by the National Institutes of Health. She has served as President of the American<br />
Society of Reproductive Medicine, Vice President of the American College of Obstetricians and<br />
Gynecologists and Secretary-Treasurer of the Society of Gynecologic Investigation. Currently<br />
she is Editor-in-Chief of Sexuality, Reproduction and Menopause. She is an Associate Editor of<br />
The American Journal of Obstetrics and Gynecology. She is the Vice President of the American<br />
Board of Obstetrics and Gynecology and is the Chairman of the Reproductive Endocrinology<br />
and Infertility subspecialty division of the Board. Dr. Carson was appointed as Chair of the<br />
Reproductive Health Drugs Advisory Committee of the Food and Drug Administration. She<br />
has served as a consultant to both the FDA’s Center for Devices and Radiological Health and<br />
the President’s Council on Bioethics. She is co-chairman of the Committee to Protect Women<br />
Who Serve as Oocyte Donors for Stem Cell Research of the California Institute of Regenerative<br />
Medicine.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Gary Frishman, MD, Associate Division Director<br />
MD: Columbia <strong>University</strong><br />
Residency: Pennsylvania Hospital<br />
Fellowship: <strong>University</strong> of Connecticut<br />
Dr. Frishman joined the division in 1991 as Assistant Professor and is now a full Professor. He<br />
is Associate Division Director. Dr. Frishman also serves as Residency Program Director for the<br />
Obstetrics and Gynecology Residency at Women & Infants Hospital of Rhode Island/<strong>Brown</strong><br />
<strong>University</strong>. He is board certified in Ob/Gyn and in Reproductive Endocrinology and Infertility<br />
and is a Board Examiner for the American Board of Obstetrics and Gynecology. Dr. Frishman<br />
has a major interest and focus on teaching, having won multiple <strong>Brown</strong> <strong>University</strong> and Na-<br />
tional (APGO and CREOG) teaching awards. He has held numerous leadership roles at <strong>Brown</strong><br />
Medical School including writing the Dean’s letter for medical students applying for an Ob/Gyn<br />
residency and running the second year PathoPhysiology course. He currently lectures at both<br />
the graduate and undergraduate level. He created and runs two unique LISTSERVs. AcadOb-<br />
Gyn is a nationwide LISTSERV, with over 800 subscribers, which addresses issues in resident<br />
and medical student education. AAGL-Endo-Issues, with over 3650 international members<br />
from over 25 countries, is devoted to topics related to Minimally Invasive Gynecologic Mini-<br />
mally Invasive Surgery. Dr. Frishman is a Contributing Editor to The Journal of Minimally Inva-<br />
sive Gynecology and is on the International Editorial Board of The Obstetrician and Gynaecolo-<br />
gist. He has served twice as Vice President for the New England Fertility Society. Dr. Frishman<br />
is currently Vice President of the Society for Reproductive Surgeons.<br />
John E. Buster, MD, Associate Division Director, Tufts Medical Center<br />
Assistant Fellowship Director<br />
MD: <strong>University</strong> of California, Los Angeles<br />
Residency: Harbor General Hospital, <strong>University</strong> of California, Los Angeles<br />
Fellowship: <strong>University</strong> of California, Los Angeles<br />
Dr. Buster joined the Division in 2007 as Professor of Obstetrics and Gynecology. He practices<br />
principally at the Women and Infants’ Center for Reproduction and Infertility site at the Tufts<br />
Medical Center in Boston. After 30 years as an REI Division Director, Dr. Buster has proven well-<br />
suited for administrative duties in the Fellowship program. Dr. Buster is best known for having<br />
led the team of researchers that developed a process for recovering and transplanting embryos<br />
from female donors to recipients that led to the first donated embryo human pregnancies and<br />
births in 1984. More uncommon knowledge is that he developed the first direct radioimmu-<br />
noassay for DHEA-S and uncongugated estriol in pregnancy plasma. He was also among the<br />
first to describe, to exploit, and to publish extensively on the use of methotrexate for medical<br />
treatment of ectopic pregnancy. More recently, Dr. Buster conducted studies and published<br />
extensively on the use of transdermal testosterone to treat women with hypoactive sexual<br />
desire disorder, an approach with wide acceptance and in use throughout Europe and gaining<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 75<br />
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y<br />
acceptance in the United States. Most recently, Dr. Buster served as lead investigator and first<br />
author in the pivotal paper describing the first experience with an estradiol spray that deliv-<br />
ers low doses of estrogen for effective treatment of vasomotor symptoms in post menopausal<br />
women. This spray was approved by the FDA in 2007, was launched in 2008, and is currently in<br />
use throughout the United States where it is known as Evamist®.<br />
76<br />
Balasubramanian Bhagavath, MD<br />
Team Leader: Director of Endoscopic Training and Credentialing;<br />
Associate Director of Third Party Reproduction<br />
MD: Madras Medical College<br />
Residency: Medical College of Georgia, Georgia<br />
Fellowship: <strong>University</strong> of Texas Southwestern Medical Center<br />
Dr. Bhagavath joined the division in 2007 as Clinical Assistant Professor of Obstetrics and<br />
Gynecology after completing his fellowship in Texas. He is at present the only REI surgeon in<br />
the Rhode Island region (Rhode Island/southeastern Massachusetts/Eastern Connecticut) who<br />
performs robot-assisted surgeries. He is actively involved in student and resident education.<br />
He is the Course Director for OBG-494, an elective in Reproductive Endocrinology for fourth<br />
year medical students. He has been named an APGO Educational Scholar for 2010 and current-<br />
ly directs the APGO LISTSERV. As Director of Endoscopic Training and Credentialing, he runs<br />
the bi-annual endoscopy training course for the OB/Gyn residents. Dr. Bhagavath is a leader<br />
in the efforts to build a Simulation Center at WIH. His clinical and research interests include<br />
anomalies of the reproductive tract, premature ovarian failure, fertility preservation and egg<br />
donation.<br />
Andrew Blazar, MD<br />
Team Leader: Clinical Outreach<br />
MD: Tufts <strong>University</strong> School of Medicine<br />
Residency: Pennsylvania Hospital, <strong>University</strong> of Pennsylvania<br />
Fellowship: Karolinska Hospital in Stockholm, Sweden<br />
Dr. Blazar joined the division in 1994 after 30 years in clinical practice. He was the first direc-<br />
tor of the Infertility Clinic at Women & Infants Hospital of Rhode Island. Dr. Blazar’s research<br />
focuses on factors affecting IVF outcomes, particularly as related to hormone response and<br />
hydrosalpinx. His teaching responsibilities include directing an elective course in “Women’s<br />
Health Issues.” He directs the divisional clinical outreach efforts and oversees feasibility of<br />
satellite activities and is a Clinical Associate Professor of Obstetrics and Gynecology.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Kelly Pagidas, MD<br />
Team Leader: Director of Preimplantation Genetic Diagnosis<br />
MD: McGill <strong>University</strong> School of Medicine<br />
Residency: McGill <strong>University</strong>, Montreal, Canada<br />
Fellowship: McGill <strong>University</strong><br />
Dr. Pagidas joined the division in 1998. Her research interests include ovarian physiology, IVF<br />
outcomes, recurrent pregnancy loss, reproductive genetics and mechanisms underlying aneu-<br />
ploidy in embryos. She directs the longitudinal course for 2nd year <strong>Brown</strong> medical students. Dr.<br />
Pagidas founded and directs the program in Preimplantation Genetic Diagnosis (PGD) and is<br />
the Medical Director of Preimplantation Genetic Diagnosis both at Women and Infants and Tufts<br />
Medical Center. Dr. Pagidas is an examiner for the endocrinology oral certification examination.<br />
She is an Assistant Professor of Obstetrics and Gynecology at <strong>Brown</strong> and Tufts <strong>University</strong>.<br />
Beth Plante, MD<br />
MD: <strong>University</strong> of Massachusetts Medical School<br />
Residency: Women & Infants Hospital of Rhode Island,<br />
<strong>Brown</strong> <strong>University</strong> Medical School<br />
Fellowship: <strong>University</strong> of North Carolina<br />
Dr. Plante joined the division in 2010 as a Clinical Assistant Professor of Obstetrics and Gynecol-<br />
ogy after completing a fellowship at the <strong>University</strong> of North Carolina. She is an avid clinician<br />
and educator at the Division’s sites in Massachusetts as well as Providence. She is investigating<br />
alterations in bio-markers during the menstrual cycle.<br />
Jared Robins, MD<br />
Team Leader: In Vitro Oocyte Maturation<br />
MD: State <strong>University</strong> of New York at Stony Brook<br />
Residency: Albert Einstein College of Medicine<br />
Fellowship: <strong>University</strong> of Cincinnati<br />
Dr. Robins joined the division in 2007 as an Assistant Professor of Obstetrics and Gynecology<br />
after a 5-year tenure as a Women’s Reproductive Health Research scholar at the <strong>University</strong> of<br />
Cincinnati. Dr. Robins leads the In Vitro Maturation (IVM) Program and the international training<br />
program in IVM which has trained physicians in this country and also from Asia and Europe. He<br />
was elected to the Society for Gynecological Investigation in 2010. His investigation is focused<br />
on the effect of hypoxia on trophoblast interaction and differentiation prior to implantation. In<br />
addition, he directs the clinical program in in vitro maturation of oocytes and oocyte cryopreser-<br />
vation for women choosing to preserve their fertility.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 77<br />
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y<br />
78<br />
Carol Wheeler, MD<br />
Team Leader: Third Party Reproduction, Pediatric/Adolescent Gynecology Clinic<br />
MD: Jefferson Medical College. Residency: Wright State <strong>University</strong>, Dayton, Ohio<br />
Fellowship: <strong>University</strong> of Pennsylvania<br />
Dr. Wheeler joined the division in 1990 from the faculty at Tulane <strong>University</strong>,<br />
New Orleans, Louisiana. After being in private practice for four years, she rejoined the division<br />
faculty in 2006. Dr. Wheeler is a Clinical Associate Professor of Obstetrics and Gynecology. She<br />
founded the division’s third party reproduction program and is actively involved in student and<br />
resident education serving as the director of the resident rotation in reproductive endocrinol-<br />
ogy. Her research interests include menopause in different ethnic groups and she was a co<br />
investigator on the Women’s Health Initiative, the largest study of menopause in the United<br />
States. She chairs the Bioethics committee at Women & Infants Hospital of Rhode Island. She<br />
developed and directs the pediatric/adolescent gynecology clinic in the WPCC. She leads the<br />
ASRM mentoring program for the Women’s Council. She serves on the Editorial Board of<br />
Sexuality, Reproduction and Menopause.<br />
Jeannine Witmyer, PhD, HCLD(ABB)<br />
IVF Laboratory Director. PhD: Boston College<br />
Dr. Witmyer is a Clinical Assistant Professor of Obstetrics and Gynecology as well<br />
as the Laboratory Director of the In Vitro Maturation Training Program. She joined<br />
the division in 2007 as IVF Laboratory Director of the embryology labs at both<br />
Tufts Medical Center and Women & Infants Hospital of Rhode Island after a 21-year tenure as a<br />
Laboratory Supervisor at Boston IVF. She has worked in the field of clinical embryology since<br />
1980 and was part of the clinical team responsible for the first IVF birth in Norfolk, VA. She was<br />
a member of the Harvard research team deriving 17 new human embryonic stem cell lines in<br />
2004. Her research interests include sperm nuclear proteins, embryo morphology, oocyte/em-<br />
bryo culture, and oocyte cryopreservation.<br />
CARING:<br />
WOMEN AND INFANTS’ CENTER FOR REPRODUCTION AND INFERTILITY<br />
The Center for Reproduction and Infertility is the clinical arm of the division which includes the<br />
in vitro fertilization program, oocyte donation, gestational surrogacy, intracytoplasmic sperm<br />
injection, fertility cryopreservation, preimplantation genetic diagnosis and management of<br />
patients referred to the division with reproductive health problems. The division is well known<br />
to partner with patients’ obstetrician-gynecologists from the local community and the nation to<br />
provide state-of-the art clinical care in problems requiring subspecialty expertise. The Center<br />
recently moved to 90 Plain Street in Providence where patient consultations and IVF–related<br />
procedures are performed. The new Center was designed specifically for the reproductive<br />
medicine program, highlighting intimacy in couples’ care. In addition, the Tufts Medical Center<br />
serves as a northern branch of the Center.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Satellite offices of the Center for Reproduction and Infertility span three states. The Center offers<br />
monitoring and patient consultation in Woonsocket, East Greenwich, and South Kingstown,<br />
Rhode Island; Fall River, Foxboro, Melrose, and Swansea, Massachusetts, and in<br />
Putnam, Connecticut.<br />
SHARING:<br />
EDUCATIONAL FUNCTIONS<br />
The Educational program of the Division of Reproductive Endocrinology and Infertility at Wom-<br />
en & Infants Hospital of Rhode Island spans geography and chronology. In 2000, the division de-<br />
veloped an affiliation with the Division of Reproductive Endocrinology at Tufts Medical School,<br />
in Boston, Massachusetts. The combined Divisions now provide a regional network of clinical<br />
care and education in Reproductive Medicine across New England. Beginning with second<br />
year medical students, the Division participates in Biomed 351 Integrated Pathophysiology and<br />
Pharmacology course at Alpert Medical School, <strong>Brown</strong> <strong>University</strong>. At both <strong>Brown</strong> and Tufts, the<br />
division teaches the third and fourth year medical students in the Obstetrics and Gynecology<br />
core clerkship (Biomed 331A); and <strong>Brown</strong> fourth year students through our 4th year electives in<br />
Reproductive Medicine (Biomed 342A) and Reproductive Health (Biomed 496). Division faculty<br />
serve as preceptors for <strong>Brown</strong> medical students and residents. All physicians in the Division<br />
teach medical students and residents, while caring for patients during office hours and in the<br />
operating room. Dr. Frishman directs the residency in obstetrics and gynecology. The faculty<br />
consistently are highly rated preceptors and lecturers.<br />
Peter Klatsky, MD, MPH<br />
MD: The Mount Sinai School of Medicine—New York, New York<br />
MPH: Columbia <strong>University</strong>—New York, NY<br />
Residency: <strong>University</strong> of California, San Francisco<br />
Dr. Klatsky joined the division in July 2008 as a clinical and research fellow. He is currently in-<br />
vestigating novel, minimally-invasive approaches to evaluate genetic expression in developing<br />
oocytes and embryos. His clinical research interests include fibroids, predictors of success and<br />
long term safety outcomes in women using assisted reproduction technologies. During residen-<br />
cy, he received honors for his endoscopic surgical skills as well as his clinical research on the<br />
effect of fibroids on reproductive outcomes. He enjoys clinical teaching and mentoring residents<br />
at a community reproductive endocrinology clinic. In his spare time, he provides volunteer care<br />
to women at the Rhode Island Free Clinic.<br />
Wendy Vitek, MD<br />
MD: <strong>University</strong> of Rochester School of Medicine & Dentistry<br />
Residency: Magee-Womens Hospital, <strong>University</strong> of Pittsburgh Medical Center<br />
Dr. Vitek joined the Division in July 2009 as a clinical and research fellow. Her research interests<br />
include folliculogenesis, tissue engineering and fertility preservation. She enjoys teaching medi-<br />
cal students and residents and has received teaching awards during residency and fellowship.<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 79<br />
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y<br />
QUERYING:<br />
RESEARCH IN REPRODUCTIVE MEDICINE<br />
The division’s research endeavors have long focused around in vitro fertilization, its outcome<br />
measures and pre-implantation genetic diagnosis. The addition of Drs. Carson, Buster and<br />
Robins have broadened the research focus to include trophoblast culture, oocyte maturation,<br />
fertility cryopreservation and the effect of reproductive toxicants on oocyte development.<br />
Programs to initiate clinical research using recombinant growth factors in the stimulation of<br />
ovarian follicles have begun. New indications for drugs in ovation induction offer patients op-<br />
portunities to participate in protocols which may enhance otherwise dismal chances of preg-<br />
nancy. The division’s efforts to stimulate oocyte development in women who have been turned<br />
away from other programs offer patients with “terminal infertility” a chance to be a parent<br />
while simultaneously contributing to the forefront of our knowledge of ovarian function.<br />
Partnerships with basic scientists at the Alpert Medical School have been developed in an effort<br />
to create a three-dimensional ovarian culture system. This system will explore all aspects of<br />
oocyte development and the effect of reproductive toxicants. This knowledge will be extended<br />
to environmental toxins and issues involved in oocyte cryopreservation as well as issues in<br />
standard oocyte culture at the time of in vitro fertilization<br />
HIGHLIGHTS<br />
CARING<br />
• The Division moved to new offices designed specifically for the reproductive endocrinology<br />
80<br />
patient needs.<br />
• One clinical satellite was added to the division’s clinical outreach network:<br />
Fall River, Massachusetts.<br />
• Drs. Buster, Carson and Robins were named to the list of Best Doctors in America.<br />
SHARING<br />
• Dr. Carson was appointed Vice President of the American Board of Obstetrics<br />
and Gynecology.<br />
• Dr. Carson was appointed Chair of FDA Advisory Committee for Reproductive<br />
Health Drugs.<br />
• Dr. Robins leads an international education program for in vitro maturation, hosting and<br />
training physicians from Asia, Europe and the Middle East.<br />
QUERYING<br />
• The Division was awarded a $1 million research contract to investigate a new drug for<br />
in-vitro fertilization.<br />
• Dr. Robins was awarded research funding through the Women & Infants Hospital of Rhode<br />
Island COBRE grant by the NICHD.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
PEER-REVIEWED PUBLICATIONS<br />
Carson SA, Wiggins D. Female Sexual Health and Its Dysfunction. Clinical OB/GYN<br />
(submitted 2009)<br />
Legro RS, Schlaff WD, Diamond MP, Coutifaris C, Casson PR, Brzyski RG, Christman GM, Trussell<br />
JC, Krawetz SA, Snyder PJ, Ohl D, Carson SA, Steinkampf MP, Carr BR, McGovern PG, Cataldo NA,<br />
Gosman GG, Nestler JE, Myers ER, Santoro N, Eisenberg E, Zhang M, Zhang H. Total testosterone<br />
assays in women with polycystic ovary syndrome: precision and correlation with hirsutism. J Clin<br />
Endocrinol Metab (submitted May 2010)<br />
Klatsky PC, Carson SA, Wessel GM. Detection of oocyte mRNA in starfish polar bodies. Mol Reprod<br />
Dev. 2010 May;77(5):386.<br />
Buster JE. Transdermal menopausal hormone therapy: delivery through skin changes the rules.<br />
Expert Opin. Pharmacother 2010 11(9):1-12.<br />
Melzer K, Klatsky PC, Krotz S, Robins J, Carson SA. In Vitro Fertilization Protocols in Poor<br />
Responders: A comparison of outcomes in patients repeating the same protocol versus switching<br />
protocols. ASRM October 2009<br />
Wessel GM, Reich A, Klatsky PC. Use of Sea Stars to Study Basic Reproductive Processes. Systems<br />
Bio in Reprod Med. In press 2010.<br />
Pagidas K, Carson SA, McGovern PG, Barnhart HX, Myers ER, Legro RS, Diamond MP, Carr BR,<br />
Schlaff WD, Coutifaris C, Steinkampf MP, Cataldo NA, Nestler JE, Gosman G, Giudice LC. Body<br />
mass index and intercourse compliance for the National Institute of Child Health and Human<br />
Development-Reproductive Medicine Network. Fertil Steril. 2009 Jun 19.<br />
Pagidas K, Carson SA, McGovern PG, Barnhart HX, Myers ER, Legro RS, Diamond MP, Carr BR,<br />
Schlaff WD, Coutifaris C, Steinkampf MP, Cataldo NA, Nestler JE, Gosman G, Giudice LC. Intercourse<br />
compliance, ovulation, and treatment success in the National Institute of Child Health and<br />
Human Development-Reproductive Medicine Network’s Pregnancy in Polycystic Ovary Syndrome<br />
(PPCOS) Trial. for the National Institute of Child Health and Human Development–Reproductive<br />
Medicine Network. Fertil Steril. 2009 Jun 19<br />
Plante BJ, Kannan A, Bagchi MK, Yuan L, Young SL. Cyclic regulation of transcription factor C/<br />
EBPβ in human endometrium. Reprod Biol Endocrinol 2009;7:15.<br />
Plante BJ, Cooper GS, Baird DD, Steiner AZ. The impact of smoking on antimullerian hormone<br />
levels in women ages 38-50 years. Menopause (in press).<br />
Plante BJ, Moldenhauer J, Landy C, Beamon C, Steiner AZ. Maternal Antimullerian Hormone and<br />
Fetal Aneuploidy. Journal of Assisted Reproduction and Genetics (in press).<br />
Erb TM, Vitek WS, Wakim, ANG. Gonadotropin-releasing hormone agonist or human chorionic<br />
gonadotropin for final oocyte maturation in an oocyte donor program. Fertil Steril 2010;93(2):374-8<br />
BOOKS AND BOOK CHAPTERS<br />
Carson SA, Wiggins D (eds). Clinical Obstetrics and Gynecology: Sexuality and Sexual Dysfunction.<br />
Lippincott Williams & Wilkins, 2009.<br />
Krotz S, Carson SA. Ectopic Pregnancy. Biennial Review of Infertility, Chapter 5 (in press, 2009)<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 81<br />
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y<br />
82<br />
INVITED PRESENTATIONS (LOCAL)<br />
Carson SA. “Unexplained Infertility,” RESOLVE of the Bay State, Providence, RI, June 15, 2009.<br />
Carson SA. “Moving Into the Future: New Dimensions and Strategies for Women’s Health Research,”<br />
Co-Chair, Working Group on Adolescent Health, Office of Women’s Health of the National<br />
Institutes of Health U.S. Department of Health and Human Services National Conference,<br />
Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong>/Women & Infants Hospital of Rhode Island,<br />
Providence, RI, September 21, 2009.<br />
Carson SA. “Sexual Issues and Reproductive Options, including Preimplantation Genetic Diagnosis<br />
(PGD),” Women & Infants Hospital of Rhode Island/American Cancer Society Symposium<br />
on Hereditary Breast and Ovarian Cancer, Providence, RI, September 26, 2009.<br />
Carson SA. “Making the Choice of Gonadotropins,” Beth Israel Deaconess/Boston IVF REI Lecture<br />
Series, Boston, MA, October 13, 2009.<br />
Carson SA. “An Update on Female Sexual Response,” Endocrine Grand Rounds, Rhode Island<br />
Hospital, Providence, RI, January 20, 2010.<br />
Carson SA. “An Update on Female Sexual Response,” Grand Rounds, Memorial Hospital of<br />
Rhode Island, Pawtucket, RI, January 21, 2010.<br />
Carson SA. “An Update on Female Sexual Response,” Pelvic Floor Disorders Conference,<br />
Women & Infants Hospital of Rhode Island, Providence, RI, March 13, 2010.<br />
Carson SA. “An Update on Female Sexual Dysfunction,” Grand Rounds, Massachusetts General<br />
Hospital, Boston MA, May 6, 2010.<br />
Carson SA. “Take Down the Heat of Hot Flashes,” Sisterhood meeting, Temple Sinai, Cranston<br />
RI, June 2, 2010.<br />
INVITED PRESENTATIONS (NATIONAL)<br />
Carson SA. “REI Certification and Maintenance of Certification,” American Society of Reproductive<br />
Medicine Fellows Retreat, Park City, UT, August 2, 2009.<br />
Carson SA. “Update on Female Sexual Dysfunction,” Albert Einstein School of Medicine Grand<br />
Rounds, Bronx, NY, September 15, 2009.<br />
Carson SA. Clark L, Carson SA, Wheeler CA, Bhagavath B. Poster Presentation: Role Of Routine<br />
Monitoring Of Hepatic And Renal Function Prior To Methotrexate Treatment For Ectopic Pregnancy.<br />
American Society of Reproductive Medicine (ASRM) <strong>Annual</strong> Meeting, Atlanta, GA, October<br />
17-21, 2009.<br />
Carson SA. “Helping Your Patients Avoid Obesity,” Grand Rounds, ChristianaCare <strong>Annual</strong> Resident<br />
Symposium, Newark, DE, March 24, 2010.<br />
Carson SA. “An Update on the Medical Treatment of Ectopic Pregnancy,” ChristianaCare <strong>Annual</strong><br />
Resident Symposium, Newark, DE, March 24, 2010.<br />
Carson SA. “An Update on Female Sexual Dysfunction,” ChristianaCare <strong>Annual</strong> Resident Symposium,<br />
Newark, DE, March 24, 2010.<br />
Carson SA. “The Transformational Impact of the Pill Over 50 Years,” Panelist selected by Today’s<br />
Woman with Gloria Steinem and Jocelyn Elders, ACOG <strong>Annual</strong> Clinical Meeting, San Francisco<br />
CA, May 17, 2010.<br />
Carson SA. “Female Sexuality and Psychological Well-Being,” Post-Graduate Course, ACOG <strong>Annual</strong><br />
Clinical Meeting, San Francisco CA, May 18, 2010.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
INVITED PRESENTATIONS (INTERNATIONAL)<br />
Carson SA. “Helping Your Patient Avoid Obesity,” 60th Mexican Congress of Gynecology and<br />
Obstetrics, Cancun, Mexico, November 3, 2009.<br />
Carson SA. “But Doctor, I Really Don’t Eat That Much,” 60th Mexican Congress of Gynecology<br />
and Obstetrics, Cancun, Mexico, November 3, 2009.<br />
Carson SA. “An Update on Female Sexual Dysfunction,” 60th Mexican Congress of Gynecology<br />
and Obstetrics, Cancun, Mexico, November 4, 2009.<br />
Carson SA. “Cryopreservation of Gametes and Ovaries,” 3rd Asian Pacific Congress on Controversies<br />
in Obstetrics, Gynecology & Infertility, Beijing, China, November 13, 2009.<br />
Carson SA. “Preservation of Fertility: Conservative Management of the Artificial Ovary,”<br />
Keynote Lectures (Women and Ovarian Cancer: From Conception to Diagnosis Capsule), 3rd<br />
Asian Pacific Congress on Controversies in Obstetrics, Gynecology & Infertility, Beijing, China,<br />
November 13, 2009.<br />
Carson SA. “Hot Controversies: Expert Opinions on Controversial Topics,” Panel Discussions,<br />
3rd Asian Pacific Congress on Controversies in Obstetrics, Gynecology & Infertility, Beijing,<br />
China, November 13, 2009.<br />
ABSTRACT PRESENTATIONS (NATIONAL)<br />
Herbst S, Pauls R, Millheiser L, Carson SA, Parmer J, Willson C, Stern R, Chen B. Safety and<br />
efficacy of radiofrequency treatment for vaginal laxity-nonsurgical functional vaginal rejuvenation.<br />
30th <strong>Annual</strong> Meeting, American Urogynecologic Society, Hollywood, FL, September 2009.<br />
Melzer KE, Klatsky PC, Krotz S, Carson SA, Robins JC. In vitro fertilization (IVF) protocols in<br />
poor responders: a comparison of patients remaining on the same stimulation. 65th <strong>Annual</strong> Meeting,<br />
American Society for Reproductive Medicine, Atlanta, GA, September 2009, Abstract #O-189.<br />
Krotz SP, Carson SA, Tomey C, Witmyer J, Buster JE. Environmental phthalates and bisphenol<br />
A do not preferentially accumulate in human follicular fluid. 65th <strong>Annual</strong> Meeting, American<br />
Society for Reproductive Medicine, Atlanta, GA, September 2009, Abstract #P-183.<br />
Klatsky PC, Witmyer J, Robins J, Wessel GM, Carson SA. Evidence of oocyte specific gene<br />
expression from polar body analysis. 65th <strong>Annual</strong> Meeting, American Society for Reproductive<br />
Medicine, Atlanta, GA, September 2009, Abstract #P-452.<br />
Clark L, Carson S, Wheeler C, Bhagavath B. Role of routine monitoring of hepatic and renal<br />
function prior to single-dose methotrexate treatment for ectopic pregnancy. Accepted for presentation<br />
at the 65th <strong>Annual</strong> Meeting of the American Society for Reproductive Medicine, November<br />
2009, Atlanta, GA<br />
Blazar A. Poster presentation at ASRM 65th <strong>Annual</strong> Meeting.” Serum Anti Mullerian Hormone<br />
(AMH) Concentration Declines During IVF Cycles.” Atlanta, GA. October 2009.<br />
Blazar A. Oral presentation at ASRM 65th <strong>Annual</strong> Meeting. “Anti Mullerian Hormone (AMH)<br />
Levels at the Onset of IVF Predict Outcome Better Than Patient Age or Prior FSH Levels.” Atlanta,<br />
GA. October 2009<br />
Klatsky PC, Witmyer J, Hackett R, Robins JC, Wessel G, Carson SA. Analysis of oocyte<br />
gene expression in polar bodies. ASRM October 2009.<br />
Klatsky PC, Witmyer J, Carson SA, Robins J. Routine Extended Culture Identifies Different<br />
Embryos for Freezing and Does Not Reduce Cryopreservation Rate. ASRM October 2009.<br />
Balthazar U, Plante BJ, Lessey BA, Wang W, Taylor RN, Bagchi MK, Young SL. “Secretory-phase<br />
regulation of human endometrial GPR30 expression.” Society of Gynecologic Investigation 57th<br />
<strong>Annual</strong> Meeting, Orlando, Florida, March 2010.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 83<br />
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y
R e p r o d u c t i v e E n d o c r i n o l o g y & I n f e r t i l i t y<br />
Balthazar U, Plante BJ, Lessey BA, Young SL. “Elevated mid-secretory endometrial GPR30<br />
expression in women with endometriosis.” Society of Gynecologic Investigation 57th <strong>Annual</strong><br />
Meeting, Orlando, Florida, March 2010.<br />
Underhill LA, Shaw SK, Robins JC. Cellular growth parameters are altered when embryos are<br />
cultured under physiologic conditions. Presented at the <strong>Annual</strong> Meeting of the American Society<br />
for Reproductive Medicine, Atlanta, GA, 2009. (Oral Abstract).<br />
Melzer KE, Klatsky PC, S Krotz, Carson SA, Robins JC. In vitro fertilization (ivf) protocols in<br />
poor responders: a comparison of patients remaining on the same stimulation protocol with those<br />
that switched protocols. Presented at the <strong>Annual</strong> Meeting of the American Society for Reproductive<br />
Medicine, Atlanta, GA, 2009. (Oral Abstract).<br />
Robins JC, Krueger P, Underhill LA. Oxygen tension affects the proliferation and differentiation<br />
of trophoblast stem cells by altering the expression of the fibroblast growth factor receptor gene.<br />
Presented at the <strong>Annual</strong> Meeting of the American Society for Reproductive Medicine, Atlanta,<br />
GA. (Oral Abstract).<br />
Blazar AS, Krotz SP, Messerlian G, Hackett R, Robins JC. Anti mullerian hormone (amh)<br />
levels at the onset of ivf predict outcome better than patient age or prior fsh levels. Presented at<br />
the <strong>Annual</strong> Meeting of the American Society for Reproductive Medicine, Atlanta, GA, 2009. (Oral<br />
Abstract).<br />
Blazar AS, Krotz SP, Messerlian G, Hackett R, Robins JC. Anti mullerian hormone (amh)<br />
levels decline during ivf cycles. Presented at the <strong>Annual</strong> Meeting of the American Society for<br />
Reproductive Medicine, Atlanta, GA, 2009. (Poster)<br />
Underhill LA, Robins JC, Witmyer J, Pagidas K. The effect of oxygen tension pre and post<br />
preimplantation genetic diagnosis biopsy on embryo quality. Presented at the <strong>Annual</strong> Meeting<br />
of the American Society for Reproductive Medicine, Atlanta, GA, 2009.<br />
Clark L, Carson S, Wheeler C, Bhagavath B. Role of routine monitoring of hepatic and renal<br />
function prior to single-dose methotrexate treatment for ectopic pregnancy. Presented at the 65th<br />
<strong>Annual</strong> Meeting of the American Society for Reproductive Medicine, November 2009, Atlanta, GA.<br />
Krotz SP, Carson SA, Tomey J, Witmyer J, Buster JE. (2009) Environmental phthalates and<br />
bisphenol A do not preferentially accumulate in human follicular fluid. Poster Presentation at<br />
ASRM in Atlanta, GA, October 2009.<br />
Underhill LA, Robins JC, Witmyer J, Pagidas K. (2009) The effect of oxygen tension pre and<br />
post preimplantation genetic diagnosis biopsy on embryo quality. Poster Presentation at ASRM<br />
in Atlanta, GA, October 2009.<br />
Klatsky PC, Witmyer J, Robins JC, Wessel GM, Carson SA. (2009) Evidence of oocyte specific<br />
gene expression from polar body analysis. Poster Presentation at ASRM in Atlanta, GA, October<br />
2009.<br />
Legro RS, Schlaff WD, Diamond MP, Coutifaris C, Casson PR, Brzyski RG, Christman GM, Trussell<br />
JC, Krawetz SA, Snyder PJ, Ohl D, Carson SA, Steinkampf MP, Carr BR, McGovern PG, Cataldo<br />
NA, Gosman GG, Nestler JE, Myers ER, Santoro N, Eisenberg E, Zhang M, Zhang H. Total Testosterone<br />
Assays in Polycystic Ovary Syndrome: Is There a Gold Standard?. ENDO 2010, 92nd<br />
<strong>Annual</strong> Meeting & Expo, San Diego CA, June 19-22, Abstract #850038.<br />
84<br />
EDITORIALS<br />
Carson SA. Sexuality, Reproduction & Menopause, Editorials<br />
Respect Repairs Demoralization. Vol. 7, No. 3, August 2009<br />
Relationship vs. Responsibility. Vol. 7, No. 4, October 2009<br />
Are All Those Pins Really Necessary? Vol. 8, No. 1, February 2010<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
DIVISION OF RESEARCH IN WOMEN’S HEALTH<br />
MISSION<br />
The mission of the Division of Research is to improve women’s health through developing in-<br />
novative research and interdisciplinary collaborations as well as providing research support for<br />
diverse women’s health investigators. By providing expertise in research methodology, data-<br />
base management and statistical analysis, the division works towards the goal of developing<br />
new knowledge and transforming this knowledge into practical information that can be shared<br />
with health care providers and the community.<br />
FACULTY<br />
Maureen G. Phipps, MD, MPH, Division Director and Vice-chair for Research<br />
BS: Boston College<br />
MD: <strong>University</strong> of Vermont<br />
MPH: <strong>University</strong> of Michigan<br />
Residency: Women & Infants Hospital of Rhode Island<br />
Fellowship: Robert Wood Johnson Clinical Scholars Program,<br />
<strong>University</strong> of Michigan<br />
Dr. Maureen Phipps, Associate Professor of Obstetrics and Gynecology and Community Health<br />
at the Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong>, is the Vice-chair for Research and Di-<br />
vision Director for the Research Division for the Department of Obstetrics and Gynecology. Dr.<br />
Phipps also directs the <strong>Brown</strong> <strong>University</strong>/ Women & Infants Hospital of Rhode Island National<br />
Center of Excellence in Women’s Health. Dr. Phipps joined the Department of Obstetrics and<br />
Gynecology in 2001 and has served as Division Director since 2007. Her research and academic<br />
activities involve collaborations across departments, hospitals and state agencies. Dr. Phipps is<br />
the principal investigator for several on-going interdisciplinary research projects and collabo-<br />
rates with investigators locally and nationally. She is an affiliate member of the <strong>Brown</strong> Univer-<br />
sity Institute for Community Health Promotion and the Center for AIDS Research. Dr. Phipps<br />
also participates in numerous community outreach activities and mentors undergraduate,<br />
graduate, medical students and residents on issues of career development and research. Her<br />
research areas include adolescent pregnancy, pregnancy outcomes, postpartum depression,<br />
prenatal care, contraception, and outcome disparities in women’s health.<br />
Dr. Phipps serves on multiple local and national committees. Dr. Phipps chairs the Rhode<br />
Island Task Force on Preterm Births which is co-sponsored by the Rhode Island Department<br />
of Health, the March of Dimes and Women & Infants Hospital of Rhode Island. Dr. Phipps also<br />
serves on numerous local committees including the RI PRAMS (Pregnancy Risk Assessment<br />
Monitoring System) Steering Committee, the <strong>Brown</strong> <strong>University</strong> Office of Women in Medicine<br />
Advisory Committee and the Rhode Island March of Dimes Board of Directors. Nationally, Dr.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 85<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
Phipps serves as Chair of the American College of Obstetricians and Gynecologists’ Committee<br />
on Underserved Women, Associate Editor for the American Journal of Obstetrics & Gynecology,<br />
a member of the National Institutes of Health National Children’s Study Steering Committee, an<br />
examiner for the American Board of Obstetrics and Gynecology and a member of the National<br />
Board of Medical Examiners Biostatistics and Epidemiology Task Force.<br />
Dr. Phipps is the Principal Investigator of the NIMH-funded project, Preventing Postpartum De-<br />
pression in Adolescent Mothers (R34 MH077588), a clinical trial to prevent postpartum depres-<br />
sion in adolescent mothers. Dr. Phipps is the Co-PI for the NICHD-funded <strong>Brown</strong> <strong>University</strong>/<br />
Women & Infants Hospital National Children’s Study Center with responsibility for co-directing<br />
both the Providence County, Rhode Island and Bristol County, Massachusetts sites for this<br />
national collaborative project with Dr. Stephen Buka. Dr. Phipps is involved, as Co-investigator,<br />
in Reducing ETS Exposure of Pregnant Women and Newborns (RO1 HL070947) a project to<br />
develop an innovative intervention (tailored “take-home” videotape) to help pregnant women<br />
maximize their pregnancy outcome and their new infant’s health through reduction in exposure<br />
to environmental tobacco smoke (ETS) and to study the feasibility and efficacy of this interven-<br />
tion compared with a usual care group. Dr. Phipps is also Co-Investigator in the project Preven-<br />
tion of Postpartum Weight Retention (R01 DK071667) a clinical trial to evaluate an intervention<br />
to prevent excess weight gain during pregnancy and weight retention postpartum. In addition,<br />
Dr. Phipps has experience with Community-Academic Partnership research and is currently the<br />
PI for the project Improving Health and Science Literacy in a Latino Community (R03 HD05900).<br />
The overall goal of this project is to increase science and health literacy in the Latino community<br />
by delivering a science and health curriculum to a Spanish-speaking radio audience.<br />
Over the past year, Dr. Phipps was honored by membership in the American Gynecological and<br />
Obstetrical Society (AGOS) as well as with the Rhode Island Health Mothers, Healthy Babies<br />
2010 Silver Rattle Award. Dr. Phipps was also awarded a Faculty Teacher of the Year Award and<br />
Excellence-in-Teaching Award for Undergraduate Medical Education; and a Faculty Award from<br />
the Graduating Chief Residents and an Excellence-in-Teaching Award for Resident Education.<br />
86<br />
Kristen A. Matteson, MD, MPH<br />
BS: The Pennsylvania State <strong>University</strong><br />
MD: Tufts <strong>University</strong> School of Medicine<br />
MPH: <strong>Brown</strong> <strong>University</strong><br />
Residency: Baystate Medical Center, Tufts <strong>University</strong> School of Medicine<br />
Dr. Kristen Matteson, Assistant Professor of Obstetrics and Gynecology, is a member of the<br />
Division of Research. Dr. Matteson successfully transitioned from the Women’s Reproductive<br />
Health Research (WRHR) Scholars Program in September 2008 to her own NICHD-funded K23<br />
mentored career development award, “A Comprehensive Patient Based Outcome Measure for<br />
Heavy Menstrual Bleeding.” Dr. Matteson started the WRHR Program in January 2006 follow-<br />
ing training in the <strong>Brown</strong>/ WIH T32 Research Fellowship in Clinical Trials and Epidemiology<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
program. During her fellowship training, Dr. Matteson also earned a Masters in Public Health<br />
degree through the <strong>Brown</strong> Program in Public Health. Dr. Matteson presented her research on<br />
Abnormal Uterine Bleeding (AUB) at the First International Congress on Abnormal Uterine<br />
Bleeding held by the American Association of Gynecologic Laparoscopists and the Society for<br />
Endoscopic Gynecologists of Italy, the <strong>Annual</strong> Congress on Women’s Health, and the <strong>Annual</strong><br />
Clinical Meeting of the American College of Obstetricians and Gynecologists. Recognizing her<br />
expertise on AUB, she was invited by the Society of Gynecologic Surgeons Systematic Review<br />
Group to serve as their clinician-researcher expert on abnormal uterine bleeding and associ-<br />
ated patient-based outcomes measures.<br />
Dr. Matteson is an emerging leader in women’s health and research design. She is the co-<br />
ordinating director for the Resident Research Curriculum and the Women’s Health Fellows<br />
Workshop in Clinical Research Design. In addition, Dr. Matteson has been rewarded for her<br />
outstanding teaching skills, most notably being awarded the CREOG (Counsel on Residency<br />
Education in Obstetrics and Gynecology) Excellence in Teaching Award (National Recogni-<br />
tion Award) in 2009. Dr. Matteson is sought after as an advisor and mentor for residents and<br />
medical students for which she has been consistently awarded outstanding teacher of the year<br />
awards since 2006. With her strong leadership and research skills in women’s health, Dr. Mat-<br />
teson is committed to continuing mentoring students, residents, fellows and faculty.<br />
This year, Dr. Matteson was awarded with a Faculty Excellence-in-Teaching Award for Under-<br />
graduate Medical Education, a Faculty Teacher of the Year Award for Resident Education, a<br />
Faculty Excellence-in-Teaching Award for Resident Education, a Faculty Award from the Gradu-<br />
ating Chief Residents, and the first prize poster at the 2010 APGO CREOG <strong>Annual</strong> Meeting in<br />
Orlando, Florida.<br />
Dwight J. Rouse, MD, MSPH joined the Divisions of Maternal-Fetal Medicine<br />
and Research in September of 2009 as Professor. He graduated from Harvard,<br />
received his MD from the <strong>University</strong> of Illinois (Chicago), completed a residency<br />
at the <strong>University</strong> of Iowa and a fellowship at the <strong>University</strong> of Alabama (Birming-<br />
ham.) From 1994 to 2009 he was a faculty member in the Division of Maternal-<br />
Fetal Medicine at UAB, where he was promoted to Professor in 2003. Dr. Rouse<br />
is the <strong>Brown</strong>/WIH Principal Investigator for the Eunice Kennedy Shriver NICHD Maternal Fetal<br />
Medicine Units (MFMU) Network. His research is focused on clinical obstetrics, particularly<br />
labor management. Through the MFMU he has led studies on the prevention of prematurity<br />
in twins, and the prevention of cerebral palsy with magnesium sulfate. He is an author of the<br />
23rd edition of Williams Obstetrics, and a past member of the editorial board of Obstetrics and<br />
Gynecology.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 87<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
88<br />
Cynthia Rosengard, PhD, MPH<br />
BA: <strong>University</strong> of Vermont<br />
MA: <strong>University</strong> of Connecticut<br />
PhD: <strong>University</strong> of Connecticut<br />
MPH: <strong>Brown</strong> <strong>University</strong><br />
Post-doctoral fellowship: <strong>University</strong> of California, San Francisco<br />
Dr. Cynthia Rosengard, Associate Professor of Obstetrics and Gynecology and Medicine,<br />
received her Ph.D. in Clinical Psychology from the <strong>University</strong> of Connecticut in 1994. Subse-<br />
quently, she completed a two-year post-doctoral fellowship in Psychology and Medicine and<br />
Adolescent Medicine at the <strong>University</strong> of California, San Francisco and served on the faculty of<br />
the Pacific Graduate School of Psychology in Palo Alto, California for five years. She joined the<br />
Research Unit of the Division of General Internal Medicine at Rhode Island Hospital in Sep-<br />
tember, 2001. In December of 2002, she was awarded a career development award from the<br />
National Institute of Mental Health entitled “Partner-specific Factors in Adolescent Sexual Be-<br />
havior.” In September of 2006, she was awarded an independent investigator award from the<br />
National Institute on Drug Abuse entitled “Partner-specific HIV Risk Reduction for Drug Using<br />
Incarcerated Adolescents.” Dr. Rosengard serves as Co-Investigator on three additional proj-<br />
ects with colleagues – all related to adolescent HIV risk behaviors and/or pregnancy. In May of<br />
2005, Dr. Rosengard completed work on her masters of public health program and received<br />
her MPH from <strong>Brown</strong> <strong>University</strong>. In November of 2008, Dr. Rosengard joined the Division of<br />
Research, Department of Obstetrics and Gynecology at Women & Infants Hospital.<br />
Dr. Rosengard’s adolescent health research focuses on investigations of the influences on<br />
adolescent sexual decision-making and behavior. Her current research examines the factors<br />
that influence sexual behavior within different types of sexual partnerships and assesses these<br />
associations separately for adolescent boys and girls. Her ultimate goal is to develop inter-<br />
ventions that will decrease the incidence of STDs and unplanned pregnancies in adolescents.<br />
Through her program of research, she plans to develop sexual risk reduction interventions that<br />
will include important attitudes, values, and expectancies found to influence partner-specific<br />
sexual decision-making in adolescents. Future research on a broader range of influential fac-<br />
tors (i.e., family, peer, community, and culture) and additional emphasis on the development of<br />
targeted risk prevention interventions (e.g., targeting sexually inexperienced adolescents) are<br />
a part of her long-term plan of research.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Jennifer Clarke, MD, MPH<br />
BA: Cornell <strong>University</strong><br />
MD: Cornell <strong>University</strong><br />
MPH: <strong>Brown</strong> <strong>University</strong><br />
Dr. Jennifer Clarke, Associate Professor of Medicine and Obstetrics and Gynecology, received<br />
her medical degree from Cornell <strong>University</strong> and completed her residency in General Inter-<br />
nal Medicine at Rhode Island Hospital. After residency she completed a two-year fellowship<br />
in women’s health and has been performing her clinical work at the women’s division of the<br />
Rhode Island Department of Corrections since 1998. Dr. Clarke’s research has focused on the<br />
reproductive health needs of incarcerated women. She completed an NIH-funded K23 career<br />
development award and is the Principal Investigator of project CARE funded by NICHD, a proj-<br />
ect designed to evaluate the effectiveness of motivational interviewing for family planning for<br />
women leaving prison. She is also the Principal Investigator of “Project WISE” a NIDA funded<br />
study to prevent relapse to smoking after release from prison. Dr. Clarke also received a grant<br />
from the Rhode Island Foundation to evaluate “Prevalence of Obesity and Weight Change<br />
among Incarcerated Women in RI”. Additionally, Dr. Clarke is a Co-Investigator on a multi-<br />
center trial of substance abuse treatment for people leaving prison (CJ-DATS).<br />
Melissa A. Clark, PhD<br />
BA: Hanover College<br />
MS: <strong>University</strong> of Illinois<br />
PhD: <strong>University</strong> of Illinois<br />
Dr. Melissa A. Clark, Associate Professor of Community Health and Obstetrics and Gynecology,<br />
is a survey methodologist with interests in survey design and data collection methodologies.<br />
Dr. Clark is the Associate Director for the Center for Population Health and Clinical Epidemiol-<br />
ogy where she directs primary data collection activities. Her research interests are in women’s<br />
health issues, and particularly the role that psychosocial factors play in health behaviors<br />
among middle-aged and older women. A consistent theme in Dr. Clark’s work is to better un-<br />
derstand the individual, social, and environmental barriers and facilitators to health and well-<br />
being among individuals who have traditionally experienced disparities in overall health status<br />
and access to high quality health care. She is the Principal Investigator of a project concerning<br />
social networks and advance care planning among women with recurrent cancer. She is also<br />
the Principal Investigator of the data collection cores of two program project grants. In addi-<br />
tion, she is the Study Director for the Providence County site of the National Children’s Study.<br />
She recently completed a series of studies about the experiences of unmarried heterosexual<br />
and sexual minority women with health care. In the past year, Dr. Clark was awarded the<br />
Dean’s Teaching Excellence Award, Alpert Medical School of <strong>Brown</strong> <strong>University</strong>.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 89<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
Susan Cu–Uvin, MD<br />
BS: <strong>University</strong> of the Philippines<br />
MD: <strong>University</strong> of the Philippines<br />
Ob/Gyn Residency: Philippine General Hospital, <strong>University</strong> of the Philippines<br />
HIV/AIDS Fellowship: The Miriam Hospital, <strong>Brown</strong> Medical School<br />
Dr. Susan Cu-Uvin, Professor of Obstetrics and Gynecology and Medicine, is the Director of<br />
the Global Health Initiative at <strong>Brown</strong> <strong>University</strong>. She is also the Director of the Women and<br />
AIDS Core, for the Center for AIDS Research (CFAR) at <strong>Brown</strong> <strong>University</strong>. She was the Director<br />
of the Miriam Immunology Center until 2009. She was the Chair of the Women’s Health Com-<br />
mittee of the Adult AIDS Clinical Trials Group (AACTG) from 2003-2006. She served on the<br />
Institute of Medicine’s Committee on Perinatal Transmission of HIV to investigate interventions<br />
to decrease vertical transmission of HIV within the United States. She currently serves on the<br />
IOM Committee on Women’s Health Research and Committee on HIV Testing and Care. She<br />
is a member of the Public Health Service Task Force/Perinatal Antiretroviral Guidelines Work-<br />
ing Group, Office of AIDS Research Advisory Council, and the NIH advisory committee on HIV<br />
related research in microbicides and the HPV Working Group, USPHS/IDSA Guidelines for the<br />
Prevention and Treatment of Opportunistic Infections. She recently chaired the NIH advisory<br />
committee on HIV related research in women and girls. She is also a member of the Global<br />
Microbicide Project scientific advisory group. She is a member of the Fogarty Executive Com-<br />
mittee at <strong>Brown</strong> <strong>University</strong> and has been a very active mentor for international trainees in<br />
HIV/AIDS care and research (Philippines, Cambodia, India, Kenya, and Indonesia). She is the<br />
recipient of the First <strong>Annual</strong> Ladies’ Home Journal Health Breakthrough Awards, the Constance<br />
B. Wofsy Women’s Health Investigator Award from the AIDS Clinical Trials Group and voted RI<br />
Woman Physician of the Year in 2007.<br />
Dr. Cu-Uvin is the Principal Investigator of an RO1 to assess antiviral therapy and HIV in the<br />
female genital tract (AI40350), and was Co-Principal Investigaor of an RO3 to assess HIV-1 geni-<br />
tal tract shedding among Cambodian women (TW6981), and a World AIDS Foundation grant<br />
to establish a HIV women’s clinic in Cambodia and provide training to Cambodian health care<br />
professionals for research readiness for future projects related to HIV in women. She is the<br />
Principal Investigator of a Fogarty supplement to compare conventional Pap smear and visual<br />
inspection with acetic acid as a cervical cancer screening tool of HIV infected women in West-<br />
ern Kenya. She is a Co-Investigator of the CDC funded study to understand the natural history<br />
of HIV and AIDS in the era of highly active antiretroviral therapy (SUN). She has a K24 Mid-<br />
Career Investigator Award in Patient Oriented Research. She has been a Co-Investigator and<br />
participated in multiple sub studies and study groups of the CDC sponsored HIV Epidemiology<br />
Research Study (HERS), a study on the natural history of HIV in North American women. She<br />
was a Co-Investigator of the NICHD-sponsored WHS 001 to investigate the impact of menstrual<br />
cycle and hormonal variations on HIV genital tract shedding.<br />
90<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
David C. Dove, PhD<br />
BA: <strong>University</strong> of Miami<br />
PhD: George Washington <strong>University</strong><br />
Post-doctoral fellowship: Rhode Island Hospital<br />
Dr. David Dove, a psychologist, received his Ph.D. in Clinical Psychology from George Wash-<br />
ington <strong>University</strong> in 2005. Subsequently, he completed a post-doctoral fellowship in Mental<br />
Health and HIV Prevention at the Alpert Medical School of <strong>Brown</strong> <strong>University</strong>. Dr. Dove joined<br />
the Division of Research, Department of Obstetrics and Gynecology in November 2008. His<br />
post-doctoral research focused on sexual risk reduction among adolescents, including the<br />
identification of cultural factors and the development of culturally tailored interventions. An ad-<br />
ditional line of research investigated the clinical needs and sociodemographic characteristics of<br />
black gay and bisexual men in community-based mental health treatment. Currently, Dr. Dove<br />
is working with Dr. Rosengard directing a team evaluating a sexual risk reduction intervention<br />
with at-risk substance-using adolescents involved in the juvenile justice system and conduct-<br />
ing a web-based longitudinal assessment of alternative school students’ sexual behavior and<br />
substance use.<br />
Christina Raker, ScD<br />
AB: Vassar College<br />
ScM, ScD: Department of Epidemiology, Harvard School of Public Health<br />
Dr. Christina Raker joined the Division of Research as a research statistician in March, 2006.<br />
Prior to joining the division, she was involved in the design and analysis of case-control and<br />
longitudinal studies of oncogenic viral infections in community-based populations. In addi-<br />
tion, she has research experience in virology, immunology, and genetic epidemiology. Her<br />
current interests include the application of epidemiologic and biostatistical methods in clinical<br />
research. Dr. Raker is involved in research design and analysis for members of the Department<br />
of Obstetrics and Gynecology, including faculty, fellows and residents. She lectures in the Fel-<br />
low’s Course in Clinical Research Design and the Resident Research Curriculum.<br />
EDUCATIONAL FUNCTIONS<br />
Medical Students<br />
Drs. Phipps and Matteson participate in teaching of undergraduate and medical students by<br />
serving as preceptors for medical students in the Obstetrics and Gynecology core clerkship,<br />
undergraduate students undertaking an independent study semester course—Reproductive<br />
Epidemiologic Research, and medical students in the Community Health Clerkship. In addition,<br />
Drs. Phipps and Matteson provide hands–on clinical instruction to medical students through<br />
their work in triage, the Women’s Primary Care Center, labor and delivery and the operating<br />
room. Didactic sessions with the medical students often focus on Cervicitis, Vaginitis and Sexu-<br />
ally Transmitted Infections.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 91<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
Residents<br />
Drs. Phipps and Matteson provide teaching through clinical work in the triage unit, the Wom-<br />
en’s Primary Care Center, labor and delivery, and the operating room. Didactic sessions with<br />
obstetrics and gynecology residents include: Cervicitis, Vaginitis and Sexually Transmitted<br />
Infections; Abnormal Uterine Bleeding: First Trimester Bleeding; Adolescent Pregnancy; Clini-<br />
cal Research Design and Methods; Research Ethics; Biostatistics; Study Design; and Evidence–<br />
Based Medicine. In September 2006, Drs. Matteson, Phipps, Sung and Anderson launched the<br />
newly developed Obstetrics and Gynecology Resident Research Curriculum. The two-year cur-<br />
riculum covers research design, database development, analysis, statistics, ethics, and critical<br />
appraisal of the medical literature, career development and resident research project develop-<br />
ment. Two sessions per month during core curriculum are dedicated to the resident research<br />
curriculum. One of these sessions includes a didactic seminar with the following session<br />
including a journal club review that complements the didactic session. The course is undergo-<br />
ing evaluation, including pre-course, mid-course and final assessments.<br />
Dr. Matteson is the coordinating director for the Resident Research Curriculum and the Resi-<br />
dent Research requirement. She organizes and directs the annual Resident Research Day that<br />
is coordinated with the annual Departmental Saphire Lecture. The Division of Research sup-<br />
ports resident research projects throughout the year including research design and develop-<br />
ment, database development, statistical support, abstract development, as well as oral and<br />
poster presentation preparation.<br />
Fellows<br />
The Women’s Health Fellows Workshop on Clinical Research Design, directed by Dr. Matteson,<br />
successfully completed its ninth consecutive year. Initiated in 2002, this popular two-week<br />
course involves clinical fellows from the Departments of Obstetrics and Gynecology, Neo-<br />
natology, Internal Medicine, Pathology, Pediatrics and Emergency Medicine. The curriculum<br />
includes sessions on study design methodology, data base management, statistics, ethics,<br />
academic promotion, grant writing and research proposal development.<br />
Women’s Reproductive Health Research Scholars (WRHR)<br />
(NIH-funded K12 program)<br />
The <strong>Brown</strong> <strong>University</strong> / Women & Infants Hospital WRHR program was initially funded in 2005<br />
and was recently awarded an additional 5 years of NIH funding allowing for new scholar ap-<br />
pointments through 2015. The purpose of the <strong>Brown</strong> / WIH WRHR program is to train the next<br />
generation of women’s health translational researchers that have the expertise and research<br />
skills to develop innovative research in women’s reproductive health from basic science to<br />
clinical applications relevant to public health. The overarching goal of the <strong>Brown</strong> / WIH WRHR<br />
program is to provide a supportive and stimulating research environment that enables well-<br />
qualified, junior faculty physician-scientists to develop into well-funded leaders in women’s<br />
reproductive health research with expertise in clinical translational research. The training pro-<br />
gram involves a tailored research and career development plan that works through intensive<br />
multidisciplinary mentoring, didactic seminars and practical hands-on research investigation.<br />
92<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
The career objectives for each scholar are focused on: acquiring the necessary knowledge and<br />
research skills in relevant scientific areas as well as key areas in women’s health and transla-<br />
tional research; professional development including management and leadership skills; and,<br />
developing the foundation for an independent research career through an intensive mentored<br />
research experience. Scholars are expected to actively write grants to the level of R01, or<br />
program project grants as they transition through and beyond the program and to continue to<br />
mentor and interact with the program even after independent funding is achieved.<br />
WRHR Program leadership<br />
• Joanna Cain, MD, Principal Investigator<br />
• Maureen G. Phipps, MD, MPH, Program Director<br />
Current WRHR scholar:<br />
• Katina Robison, MD Program in Women’s Oncology (March 30, 2009 to present)<br />
Previous WRHR scholars:<br />
• Brenna Anderson, MD, MS Division of Maternal-Fetal Medicine<br />
(July 1, 2006 to August 10, 2009)<br />
• Kristen Matteson, MD, MPH, Division of Research (January 1, 2006 – August 31, 2008)<br />
• Vivian Sung, MD, MPH Division of Urogynecology (July 1, 2006 – June 15, 2009)<br />
NATIONAL CENTER OF EXCELLENCE IN WOMEN’S HEALTH<br />
The <strong>Brown</strong> <strong>University</strong> National Center of Excellence in Women’s Health has been led by Dr.<br />
Maureen Phipps since 2003. <strong>Brown</strong> <strong>University</strong> and Women & Infants Hospital of Rhode Island<br />
were designated as a National Center of Excellence in Women’s Health by the U.S. Department<br />
of Health and Human Services in October of 2003. The mission of the CoE has been focused<br />
on improving health and health care for all women by working with academic and community<br />
partners and collaborating with public and private health care providers throughout the state.<br />
Although the national program ended in September 2007, the commitment to continue to work<br />
toward the mission and goals has continued. The CoE was successful because of the dedicated<br />
network of partners located throughout Rhode Island working on initiatives that include:<br />
• Enhancing the professional development of women residents, fellows and faculty leading<br />
to academic promotion and positions of leadership throughout the university;<br />
• Promoting education, training and advancement of women in nursing and allied health<br />
professions;<br />
• Improving the medical curriculum in women’s health throughout the medical school<br />
residency and post graduate programs, with an emphasis on diversity and cultural issues;<br />
• Enhancing collaborative efforts of women’s health researchers statewide, regionally<br />
and nationally;<br />
• Providing community health education, outreach and health services to diverse groups<br />
of women;<br />
• Improving quality and access to care for women of all ages, emphasizing the specific needs<br />
of underserved and vulnerable populations of women.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 93<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
CoE Outstanding Faculty Mentor Award: Established in 2005, the Outstanding Faculty Men-<br />
tor Award recognizes faculty members throughout the <strong>Brown</strong> Community who have been<br />
instrumental in the career development of junior faculty pursuing careers in women’s health<br />
and leadership. The faculty members are nominated by their mentees and selected by the CoE<br />
leadership team.<br />
In 2010, two faculty members received this prestigious award:<br />
• Caron Zlotnick, PhD, Professor, Department of Psychiatry & Human Behavior at the Warren<br />
94<br />
Alpert Medical School of <strong>Brown</strong> <strong>University</strong> and Director of Research for Women’s<br />
Behavioral Health at Women & Infants Hospital (October, 2009)<br />
• Donald R. Coustan, MD, Professor of Obstetrics & Gynecology at the Warren Alpert<br />
Medical School of <strong>Brown</strong> <strong>University</strong> and Women & Infants Hospital, Division of<br />
Maternal-Fetal Medicine (March, 2010)<br />
Innovations in Women’s Health Research Seed Grant: The Center of Excellence Innovations<br />
in Women’s Health Seed Grant program was established in 2005 to support activities neces-<br />
sary to advance interdisciplinary projects in women’s health and gender-based research and<br />
education. The goal of the program is to support high quality projects to help attract external<br />
funding from federal and foundation sources. The program requires that proposals have a<br />
realistic potential for future success in attracting external support. Funds should be applied to<br />
pilot research necessary to advance such proposals. These funds are not intended to supple-<br />
ment ongoing NIH funded projects, but rather to stimulate new research and interdisciplinary<br />
collaborations. In consultation with an ad hoc committee of faculty advisors, awards are made<br />
by the <strong>Brown</strong> <strong>University</strong> National Center of Excellence in Women’s Health (CoE). On-going sup-<br />
port for the program has been received from numerous medical school departments and the<br />
dean’s office. Since the inception of the program in 2005, fourteen Research Seed Grants and<br />
two Education Seed Grants have been awarded.<br />
The 2010 Innovations in Women’s Health Research Seed Grant include:<br />
Title: A polymorphic variant at survivin 129 is a novel biomarker for breast cancer<br />
Principal Investigator: Rachel Altura (Pediatrics)<br />
<strong>Brown</strong> Collaborators: Carmen Marsit (Pathology), Evgeny Yakirevich (Pathology)<br />
Title: Susceptibility genes for polycystic ovarian syndrome in Somoan and<br />
American Somoan women<br />
Principal Investigator: Geralyn Lambert-Messerlian (Pathology)<br />
<strong>Brown</strong> Collaborators: Stephen McGarvey (Community Health)<br />
Other Collaborators: Ranjan Deka (Cincinnati, Genotyping lab), Margrit Urbanek<br />
(Northwestern, Medicine)<br />
Title: Role of sleep and circadian rhythm disruption in postpartum depression<br />
Principal Investigator: Katherine Sharkey (Medicine)<br />
<strong>Brown</strong> Collaborator: Teri Pearlstein (Psychiatry & Human Behavior)<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
RESEARCH ACTIVITIES<br />
The goal of the Division of Research is to develop and support original research which will lead<br />
to improved patient and community outcomes. The Division of Research works to increase<br />
grant funding in the Department of Obstetrics and Gynecology, support publication of the<br />
research activities in the Department, enhance the careers of junior investigators and provide<br />
support for clinical investigators in the Department of Obstetrics and Gynecology. The work of<br />
the Division of Research is driven by collaboration, education, training and investigator support.<br />
The backgrounds of the multidisciplinary staff members in the Division of Research include<br />
nursing, epidemiology, statistics, psychology, database development, business management,<br />
public health research coordination, and research support.<br />
The Division of Research in Women’s Health provides the following services to members of the<br />
Department of Obstetrics and Gynecology and Women and Infants: 1) consultation regarding<br />
epidemiology, methodology, project planning, biostatistics, publishing, and grant applications;<br />
2) data management and entry; 3) statistical analyses; 4) expertise in project coordination; and<br />
5) outcomes measurement and research. The George Anderson Outcomes Unit, established in<br />
1997, is integrated within the Division of Research. The Outcomes Unit focuses its efforts on<br />
patient–oriented outcomes research in the Department of Obstetrics and Gynecology, and the<br />
hospital. The integration of these services maximizes the efficiency of both the Division and the<br />
Outcomes Unit. By providing essential services for the department and the hospital, the Division<br />
has encouraged clinical investigation and increased the NIH grant support to the Department of<br />
Obstetrics and Gynecology.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 95<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
96<br />
GRANTS<br />
Clarke JG: NIH NICHD “Empowering Women to Make Contraceptive Choices While Incarcerated.”<br />
(PI: J Clarke) $1,484,579 grant total. 6/1/08-5/31/13.<br />
Clarke JG: NIH NIDA “Sustaining Tobacco Abstinence after Incarceration.” (PI: J Clarke)<br />
$908,875 grant total. 8/15/09-7/31/11.<br />
Clark MA: NIH NCI “Understanding Reversed Race/Ethnic Associations with Cancer Screening<br />
Tests” (PI: Rakowski) Co-Investigator for project. $125,387 direct costs, 4/07 − present.<br />
Clark MA: NIH NIA “Older Latina Women. Marital Status and Cancer Screening” (PI: Wasserman)<br />
Co-Investigator for project. $11,366 direct costs, 3/07 − present.<br />
Clark MA: NIH NCI “Methods and Measures Core (PI) and Social Contexts and Patterns of<br />
Young Adult Smoking (Co-I) (PI: Rende) “Renewal of the Transdisciplinary Tobacco Use in Research<br />
Centers”. (PI: Niaura) (P50-CA04012), $424,535 direct costs, 10/04 − present.<br />
Clark MA: NIH NIA “Primary Data Collect Core (Core PI), Program Project Grant, “Long-Term<br />
Care in America” (PI: V Mor) $1,333,093 direct costs, 9/2007− present.<br />
Clark MA: NIH NICHD “The National Children’s Study—Providence and Bristol County Sites”.<br />
(PI: S Buka, Co-PI M Phipps), Co-Investigator and Operations Manager for project. $1,495,650<br />
(Providence) and $424,829 (Bristol) direct costs, 9/07 − present.<br />
Clark MA: Subcontract to Providence VA “A Computer Adaptive Test to Measure Community<br />
Reintegration.” (PI: L Resnik) Co-Investigator for project. $102,594 direct costs, 3/08 − present.<br />
Clark MA: NIH NCI “Classification Tree Analysis to Enhance Targeting for Cancer Screening<br />
Programs.” (PI: W Rakowski), $103,750 direct costs, 1/10 – present.<br />
Clark MA: Subcontract (PI for subcontract) “Video-Based HIV Testing for Latinos.” (PI: R Merchant),<br />
$18,806 direct costs, 3/10 – present.<br />
Clark MA: NIH NCI “Social Networks and Care Planning for Women with Cancer.” (PI) $116,971<br />
direct costs, 4/10 - present.<br />
Cu-Uvin S: NIAID K24 AI066884-05. “Antiviral Therapy and HIV in the Genital Tract of Women.”<br />
(PI: S Cu-Uvin) $136,653 yr; 8/15/05-6/30/10.<br />
Cu-Uvin S: NIAID R01 5U01AI6605. “S.japonicum and Birth Outcomes: Randomized Controlled<br />
Trial.” (PI: A Friedman) Co-Investigator. $18,870 yr; 4/1/06-3/31/11.<br />
Cu-Uvin S: NIH FIC “Interdisciplinary Framework in Global Health at <strong>Brown</strong> <strong>University</strong>.” (PI: S<br />
Cu-Uvin) $125,000 yr; 8/10/08-7/31/11.<br />
Cu-Uvin S: NIH NIAID “HIV and Women’s Core.” Lifespan/Tufts/<strong>Brown</strong> Center for AIDS Research<br />
(PI: Carpenter) Co-Director, $111,526 yr, 9/1/98-6/30/12.<br />
Cu-Uvin S: NIH NIAID “Adult Therapeutic Clinical Trials Program for HIV/AIDS.” (PI: Tashima)<br />
$435,000 yr, 12/1/06-11/30/13.<br />
Cu-Uvin S: CDC “Study to Understand the Natural History of HIV and AIDS in the Era of Effective<br />
Therapy (SUN).” (PI: Carpenter) $424,822 yr, 9/27/07-9/28/11.<br />
Cu-Uvin S: NIH NIAID “Molecular T. Vaginalis Host Interactions in Relevance to Inflammatory<br />
Sequelae.” (PI: Fichorova) 29,992 yr, 7/1/09-6/30/13.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Matteson KA: NIH NICHD “Mentored Patient-Oriented Research Career Development Award<br />
- A Comprehensive Patient Based Outcome Measure for Heavy Menstrual Bleeding.” (1K23<br />
HD057957 (Matteson)). PI. $739,932 grant total. 9/1/08-9/31/13.<br />
Phipps MG: NIH NIDDK “Prevention of Postpartum Weight Retention.” (R01DK071667 (Phelan)).<br />
Site PI, Co-Investigator for project. $1,369,059 grant total. 9/11/06-08/31/10.<br />
Phipps MG: NIH NICHD “Improving Health and Science Literacy in a Latino Community (ES-<br />
CUCHE).” (1R01 3 HD05900-02 (Phipps and Rodriquez)) PI. $56,686 grant total. 9/25/08-8/31/10.<br />
Phipps MG: NIH NICHD “<strong>Brown</strong> <strong>University</strong>/Women and Infants National Children’s Study<br />
(Providence County, Rhode Island).” (HH SN 267200700032C ( Buka and Phipps)). PI. $5,420,356<br />
grant total. 9/27/07-9/26/12.<br />
Phipps MG: NIH NICHD “<strong>Brown</strong> <strong>University</strong>/Women and Infants National Children’s Study (Bristol<br />
County, Massachusetts).” (HH SN 275200800017C (Buka and Phipps)). PI. $4,287,866 grant<br />
total. 9/30/08-9/29/13.<br />
Phipps MG: NIH NICHD “<strong>Brown</strong> <strong>University</strong>/Women and Infants Women’s Reproductive Health<br />
Research Career Development.” (2K12 HD0501080-06 Cain)). PD. $2,200,000 Grant total.<br />
9/27/05-3/31/15.<br />
Phipps MG: NIEHS “Formative Center for the Evaluation of Environmental Impacts on Fetal<br />
Development: Tissue Procurement Core.” Site PI. $114,047 (Subcontract) 12/1/09-2/1/12.<br />
Rouse DJ: ( PI) and Anderson BL (Alternate Principal Investigator) Cooperative Multicenter Maternal<br />
Fetal Medicine Units Network. NICHD. PHS#5-U10 – HD40500-05. 9/6/05-3/31/10.<br />
INVITED PRESENTATIONS (LOCAL)<br />
Clarke JG: “Introduction to Research.” Resident Noon Conference. <strong>Brown</strong> <strong>University</strong> School<br />
of Medicine, Memorial Hospital of Rhode Island, Pawtucket, Rhode Island, September 2009.<br />
Clarke JG:“A 25 Year Old Pregnant Incarcerated Women.” OB-Gyn Grand Rounds Beth<br />
Israel Deaconess Medical Center, Boston, Massachusetts, January 2010.<br />
Clarke JG: Panelist, “The Life of a Clinician Researcher.” <strong>Brown</strong> <strong>University</strong>, The Office of<br />
Women in Medicine, Providence, Rhode Island, February 2010.<br />
Cu-Uvin S: Special Health Concerns of HIV Infected Women, 6th <strong>Annual</strong> Teaching Day:<br />
“Focusing on HIV and Women.” Association of Nurses in AIDS Care, Radisson Hotel,<br />
Providence, Rhode Island, September 2009.<br />
Cu-Uvin S: “<strong>Brown</strong> and the World: Engaging HIV Infected Women.” Saphier Family Lecture<br />
in Obstetrics and Gynecology, Women and Infants Hospital, Providence, Rhode Island,<br />
May 2010.<br />
Cu-Uvin S: “Gender Issues in HIV.” 14 th <strong>Annual</strong> Meeting, HIV Update, Contemporary Issues<br />
and Management, Harvard Medical School and Beth Israel Deaconess Medical Center. Seaport<br />
Hotel, Boston, Massachusetts, June 2010.<br />
Cu-Uvin S: Course Director: “Women, HIV and Rhode Island’s New Testing Law.” Providence<br />
Hilton Hotel, Providence, Rhode Island, June 2010.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 97<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
Phipps MG: “Understanding Adolescent Pregnancy: Policy, Data and Research.” The<br />
Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong>, Department of Pediatrics Grand Rounds,<br />
Providence, Rhode Island, August 2009.<br />
Phipps MG: “Translational Research in Women’s Health, From Basic Science to Bedside to<br />
Community.” New Dimensions and Strategies for Women’s Health Research for the National<br />
Institutes of Health. Office of Research in Women’s Health Strategy Conference and Public<br />
Hearing. Hosted by <strong>Brown</strong> <strong>University</strong> and Women & Infants Hospital, Providence, Rhode<br />
Island, September 2009.<br />
Phipps MG: “Rhode Island Task Force on Premature Births: 2009 Progress <strong>Report</strong>.” 2009<br />
Rhode Island March of Dimes Prematurity Summit. Providence, Rhode Island, November 2009.<br />
INVITED PRESENTATIONS (NATIONAL)<br />
Cu-Uvin S: “Clinical Parameters Essential to Methodology and Interpretation of Mucosal<br />
Responses.” Mucosal Immunity in the Male and Female Reproductive Tract and The<br />
Prevention of HIV Transmission Meeting, Dartmouth-Hitchcock Medical Center, Lebanon,<br />
New Hampshire, July 2010.<br />
Cu-Uvin S: “Vulnerable Populations: Why Can’t We Protect Men and Women from HIV with<br />
the Knowledge we Have?” Mucosal Immunity in the Male and Female Reproductive Tract and<br />
The Prevention of HIV Transmission Meeting, Dartmouth-Hitchcock Medical Center, Lebanon,<br />
New Hampshire, July 2010.<br />
Matteson KA: “Hysterectomy Compared to Other Therapies for Abnormal Uterine Bleeding.<br />
Why Should we Care?” Part of the Systematic Review Group panel at the meeting for the<br />
Society for Gynecologic Surgeons, Tucson, Arizona, April 2010.<br />
Phipps MG: “Understanding Adolescent Pregnancy: Policy, Data and Research.” <strong>University</strong><br />
of Wisconsin, Department of Obstetrics and Gynecology Grand Rounds, Madison, Wisconsin,<br />
August 2009.<br />
Phipps MG: “The Rhode Island Task Force on Premature Birth.” Symposium on Quality<br />
Improvement to Prevent Prematurity. Sponsored by March of Dimes, American College of<br />
Obstetricians and Gynecologists, American Academy of Pediatrics, American College of Nurse-<br />
Midwives, Association of Women’s Health, Obstetrics and Neonatal Nurses. Arlington, Virginia,<br />
October 2009.<br />
Phipps MG: “Adolescent Pregnancy: Policy, Data and Research.” Guest Consultant for<br />
Resident Graduation Day Albany Medical College, Department of Obstetrics, Gynecology and<br />
Reproductive Sciences, Albany, New York, June 2010.<br />
Rouse DJ. Current Trends and New Direction in Ob/Gyn Seminar: MgSO4 for the Prevention<br />
of CP. Mount Auburn Hospital, Waltham, MA. November 18, 2009.<br />
Bates E, Rouse DJ, Chapman V, Mann ML, Carlo W, Tita A. Fetal lung maturity testing before<br />
39 weeks and neonatal outcomes. Society of Maternal-Fetal Medicine Poster Presentation,<br />
Chicago IL, February 2010.<br />
Rouse DJ. Spring Postgraduate Course. <strong>University</strong> of Michigan Department of Obstetrics and<br />
Gynecology, Detroit, MI. April 2010.<br />
Rouse DJ. Resident Research Symposium. <strong>University</strong> of South Carolina School of Medicine,<br />
Columbia, SC. June 2010.<br />
Rouse DJ. Sloane Symposium. Department of Obstetrics and Gynecology, Columbia<br />
<strong>University</strong> College of Physicians and Surgeons, New York, NY. June 2010.<br />
98<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
INVITED PRESENTATIONS (INTERNATIONAL)<br />
Cu-Uvin S: “HIV and Women.” Presented at the 2010 HIV/AIDS Nursing Symposium, Chennai,<br />
India, January 2010.<br />
Matteson KA: “Structuring the Menstrual History.” Part of the Abnormal Uterine Bleedin<br />
panel at XIX World Congress of FIGO, Cape Town, South Africa, October 2009.<br />
ABSTRACT PRESENTATIONS (LOCAL)<br />
Clark MA. Homegrown: Experiences and Reflections on the Challenges and Rewards of Using<br />
Community-Based Learning. <strong>Brown</strong> <strong>University</strong> Swearer Center & Sheridan Center, Providence,<br />
Rhode Island, 2009.<br />
van den Berg JJ, Lopez R, Dove DC, Morrow KM, Stein LAR, and Rosengard C. Teenspeak:<br />
The Language of Inner-city Adolescents’ Sexual Behaviors and Sexual Relationships. Presented<br />
at the CFAR Social and Behavioral Sciences Research Network National Scientific Meeting,<br />
Boston, Massachusetts, October 2009.<br />
ABSTRACT PRESENTATIONS (NATIONAL)<br />
Waxman, MJ, Merchant RC, Clark MA, Maher JG, Celada,MT, Beckwith CG, Liu T, Simmons<br />
EA, and Mayer KH. Will the 2006 CDC HIV testing recommendations reduce stigma and increase<br />
HIV testing? 2009 CDC National HIV Prevention Conference, Atlanta, Georgia, 2009.<br />
Merchant RC, Waxman MJ, Clark MA, Maher JC, Celada MT, Beckwith CG, Liu,T, Simmons<br />
EA, and Mayer KH. Do patients and clinicians have ethical concerns about the 2006 CDC HIV<br />
testing recommendations? 2009 CDC National HIV Prevention Conference, Atlanta, Georgia,<br />
2009.<br />
Sung VW, Williams DA, Rogers RG, Myers DL, Marques F, and Clark MA. Content validity of<br />
the “PROMIS” framework in women with urinary incontinence. <strong>Annual</strong> Meeting of the American<br />
Urogynecologic Society, Hollywood Florida, 2009.<br />
Rakowski W, and Clark MA. Unwanted sex and partner violence: mammography and pap<br />
testing in the 2006 BRFSS. <strong>Annual</strong> meeting of the Society of Behavioral Medicine. Montreal,<br />
Canada, 2009.<br />
Politi MC, Clark MA, Ombao H, and Légaré F. The impact of a mismatch between patients’ and<br />
providers’ reactions to uncertainty on patients’ breast health decisions and decision satisfaction.<br />
<strong>Annual</strong> Meeting of the Society for Medical Decision Making, Hollywood, California, 2009.<br />
Rogers ML, Clark MA,Rakowski W, and Linkletter CD. Racial and ethnic differences in onschedule<br />
mammography screening: results from the Behavioral Risk Factor Surveillance System.<br />
<strong>Annual</strong> Meeting of the American Association of Public Opinion Research, Chicago, Illinois,<br />
2010.<br />
Anderson BL, Cu-Uvin S, Raker C, Hillier SL. Subtle perturbations of genital microflora alter<br />
immunity among low risk pregnant women. Oral presentation at the 36 th <strong>Annual</strong> Scientific<br />
Meeting of the Infectious Diseases Society for Obstetrics and Gynecology, Montreal, Canada,<br />
August 2009.<br />
Kassis N, Jayakrishnan A, Sprawka N, Cu-Uvin S, Anderson BL. Hepatotoxicity and metabolic<br />
acidosis manifested as non-reassuring fetal testing in a pregnant women on antiretroviral<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 99<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
therapy. Poster presentation at the 36 th <strong>Annual</strong> Scientific Meeting of the Infectious Diseases<br />
Society for Obstetrics and Gynecology, Montreal, Canada, August 2009.<br />
Nijhawan A, McManus J, Liu T, Delong A, Chapman S, Rapoza K, Kurpewski J, Caliendo A,<br />
Cu-Uvin S. The effect of acyclovir on CD4 count and CD4 percent slope in HIV-1/HSV-2 co-infected<br />
women taking HAART. <strong>Annual</strong> IDSA Meeting, Philadelphia, Pennsylvania, October 2009.<br />
McManus J, Nijhawan A, Liu T, Delong A, Chapman S, Rapoza K, Kurpewski J, Caliendo A,<br />
Cu-Uvin S. The effect of acyclovir on prevalence of bacterial vaginosis in HIV-1/HSV-2 co-infected<br />
women taking HAART. <strong>Annual</strong> IDSA Meeting, Philadelphia, Pennsylvania, October 2009.<br />
Anderson BL, Wira CR, Fitzsimmons C, Ghosh M, Fahey J, Cu-Uvin S. Cervicovaginal fluid<br />
from pregnant and non-pregnant women suppresses HIV infectivity in an in vitro model.<br />
Oral presentation at the 30 th <strong>Annual</strong> Meeting of the Society for Maternal Fetal Medicine,<br />
Chicago, Illinois, February, 2010. American Journal of Obstetrics and Gynecology 2009;201(6,<br />
Supplement 1):S43.<br />
Anderson BL, Hillier SL, Raker C, Fitzsimmons C, Cu-Uvin S. Maternal inflammatory mediators<br />
are increased as early as the first trimester in low risk pregnancies. Poster presentation at the<br />
30 th <strong>Annual</strong> Meeting of the Society for Maternal Fetal Medicine, Chicago, Illinois, February,<br />
2010. American Journal of Obstetrics and Gynecology 2009;201(6, Supplement 1):S231.<br />
van den Berg JJ, Lopez R, Dove DC, Morrow KM, Stein LAR, and Rosengard C. African<br />
American and Latino/a adolescents’ sexual relationship perceptions and motivations. Presented<br />
at the <strong>Annual</strong> Meeting of the American Psychological Association Conference, Toronto,<br />
Canada, August 2009.<br />
van den Berg JJ, Lopez R, Dove DC, Morrow KM, Stein LAR, and Rosengard C. Participantidentified<br />
intervention components and facilitator characteristics for an HIV risk reduction<br />
program among incarcerated adolescents. Presented at the <strong>Annual</strong> Meeting of the American<br />
Public Health Association Conference, Philadelphia, Pennsylvania, November 2009.<br />
Li S, Dove DC, van den Berg JJ, Lopez R, Audet D, Morrow KM, Stein LAR, and Rosengard C.<br />
Sexual health learning and partner communication about sexually transmitted disease/HIV risk:<br />
Incarcerated adolescents’ perspectives. Presented at the <strong>Annual</strong> Meeting of the Society for<br />
Adolescent Medicine, Toronto, Canada, April 2010.<br />
Critchfield AR, Matteson KA, Lievense S, Raker CR. Intrapartum Group B Streptococcus<br />
Prophylaxis in patients who report a penicillin allergy: has there been an improvement in<br />
adherence to the 2002 CDC Guidelines? Oral presentation at the Infectious Disease Society of<br />
Obstetrics and Gynecology, Montreal, Quebec, Canada, August 2009.<br />
Carey M, Matteson KA, Masterton D, Raker CR. Misoprostol for non-viable first trimester<br />
pregnancies – Can patients accurately determine spontaneous miscarriage completion? Oral<br />
presentation at the American Society for Reproductive Medicine, Atlanta, Georgia, October<br />
2009.<br />
Matteson KA, Anderson BL, Sung VW, Raker CA, McMahon M, Phipps MG. Development<br />
and evaluation of a formal research curriculum for obstetrics and gynecology. Poster<br />
Presentation at the APGO CREOG <strong>Annual</strong> Meeting, Orlando, Florida, March 2010.<br />
Matteson KA, Phipps MG, Peipert JF. Developing a workshop on research design for clinical<br />
fellows. Poster Presentation at the APGO CREOG <strong>Annual</strong> Meeting, Orlando, Florida, Awarded<br />
First Prize, March 2010.<br />
Phipps MG, Rodriguez P. Improving health and science literacy in a Latino Community.<br />
National Institutes of Health Partners in Research Investigator Workshop. Bethesda, Maryland,<br />
October 2009.<br />
100<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Sung VW, Raker CA, Myers DL, and Clark MA. Ambulatory care for female pelvic floor<br />
disorders in the United States. <strong>Annual</strong> Meeting of the Society of Gynecologic Surgeons, New<br />
Orleans, Louisiana, 2009.<br />
ABSTRACT PRESENTATIONS (INTERNATIONAL)<br />
Harwell J, Lim K, DeLong A, Srey P, Thay S, Tharpe L, Ingersoll J, Caliendo A, Cu-Uvin S.<br />
Changes in plasma (PVL) and genital tract (GTVL) HIV-1 viral loads in Cambodian women<br />
initiating generic antiretroviral therapy. International Conference on AIDS in Asia and Pacific,<br />
Bali, Indonesia, August 2009.<br />
PEER REVIEWED PUBLICATIONS<br />
Havens JR, Leukefeld C, Oser CB, Staton-Tindall M, Knudsen HK, Mooney J, Duvall J,<br />
Clarke JG, Frisman L, Surratt H and Inciardi J. An Examination of Protocol Performance and<br />
Adherence among Criminal Justice Involved Women Prisoners Receiving an HIV Intervention.<br />
Journal of Experimental Criminology 5(3):245, 2009.<br />
Stein MD, Caviness CM, Anderson BJ, Hebert M, Clarke JG. A brief alcohol intervention for<br />
hazardously drinking incarcerated women. Addiction 105(3):466-75, 2010.<br />
Clarke JG, Phipps MG, Tong I, Rose J, Gold M. Timing of conception for pregnant women<br />
returning to jail. Journal of Correctional Health Care 16(2):133-8, 2010.<br />
Nijhawan AE, Salloway R, Nunn AS, Poshkus M, Clarke JG. Preventive healthcare for<br />
underserved women: results of a prison survey. Journal of Womens Health (Larchmt) 19(1):17-<br />
22, 2010.<br />
Politi MC, Clark MA, Armstrong G, McGarry KA, and Sciamanna CN. Patient-provider communication<br />
about sexual health among unmarried middle-aged and older women. Journal of<br />
General Internal Medicine 24(4):511-516, 2009.<br />
Pasick R, Burke N, Barker J, Joseph G, Bird J, Otero-Sabogal R, Nuason N, Stewart S, Rakowski<br />
W, Clark MA, Washington P, and Guerra C. Behavioral theory in a diverse society: like a compass<br />
on mars. Health Education and Behavior 36:11S-35S, 2009.<br />
Burke N, Bird J, Clark MA, Rakowski W, Guerra C, Barker J, and Pasick R. Social and cultural<br />
meaning of Sself-efficacy. Health Education and Behavior 36:111S-128S, 2009.<br />
Clough-Gorr KM, Rakowski W, Clark MA, and Silliman RA. The Getting-Out-of-Bed (GoB)<br />
measure of motivation and life outlook in older adults: development and initial psychometric<br />
evaluation in a sample of older breast cancer survivors. Journal of Psycho-Oncology 27(4):454-<br />
468, 2009.<br />
Merchant RC, Clark MA, Langan TJ, Seage GR, Mayer KH, and DeGruttola VG. Effectiveness<br />
of increasing emergency department patients’ self-perceived risk for being HIV infected<br />
through audio-computer self-interview (ACASI)-based feedback about reported HIV risk behaviors.<br />
Academic Emergency Medicine 16:1143-1155, 2009.<br />
Dizon DS, Schutzer ME, Politi M, Linkletter C, Miller S, and Clark MA. Advance care planning<br />
decisions of women with cancer: Provider recognition and stability of choices. Journal of Psychosocial<br />
Oncology 27(4):383-395, 2009.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 101<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
Rakowski W, Clark, MA, Rogers ML, and Weitzen S. Investigating reversals of association for<br />
utilization of recent mammography among Hispanic and non-Hispanic black women. Cancer<br />
Causes and Control 20:1483-1495, 2009.<br />
Schneider K, Lapane K, Clark MA, and Rakowski W. Using small area estimation to describe<br />
county-level disparities in mammography. Preventing Chronic Disease: Public Health Research,<br />
Practice and Policy 6(4):A125, 2009.<br />
Clark MA, Rogers ML, Wen X, Wilcox V, McCarthy-Barnett K, Panarace J, Manning C, Allen S,<br />
and Rakowski W. Repeat mammography among unmarried women with and without a disability.<br />
Women’s Health Issues 19:415-424. 2009.<br />
Fennell ML, Feng Z, Clark MA, and Mor V. Disparities in nursing home use and performance:<br />
The case of elderly U.S. Hispanics. Health Affairs 29(1):65-73, 2010.<br />
Merchant RC, Freelove SM, Langan TJ, Clark, MA, Mayer KH, Seage GR, and DeGruttola VG.<br />
The relationship of reported HIV risk and history of HIV testing among emergency department<br />
patients. Postgraduate Medicine 122(1):61-74, 2010.<br />
Miller EA, Mor V, and Clark MA. Reforming long-term care in the United States: findings from<br />
a national survey of specialists. The Gerontologist 50(2):238-252, 2010.<br />
Rakowski W, Wyn R, Breen N, Meissner H, and Clark MA. Prevalence and correlates of recent<br />
and repeat mammography among California women ages 55-79. Cancer Epidemiology<br />
34(2):168-177,2010.<br />
Kahler CW, Leventhal AM, Daughters SB, Clark MA, Colby SM, Ramsey SE, Boergers J,<br />
Abrams DB, Niaura R, and Buka SL. Relationships of personality and psychiatric disorders to<br />
multiple domains of smoking motives and dependence in middle-aged adults. Nicotine & Tobacco<br />
Research 12(4):381-389, 2010.<br />
Cohen A, Lopez A, Marder S, Safane N, and Clark MA. Lessons from an Introductory Public<br />
Health Course. Academic Exchange Quarterly 14(1): 158-163, 2010.<br />
Kojic EM, Wang CC, Firth JA, Gopalakrishnan G, Cu-Uvin S. Special care issues of women living<br />
with HIV/AIDS. Medicine Health RI 92(7):229-30, 2009.<br />
Gillani FS, Zaller ND, Zeller K, Rich JD, Cu-Uvin S, Flanigan TP, Carpenter CC. Changes in<br />
demographics and risk factors among persons living with HIV in an academic medical center<br />
from 2003-2007. Medicine Health RI 92(7):237-40, 2009.<br />
Moreira C, Venkatesh KK, DeLong A, Liu T, Kurpewski J, Ingersoll J, Caliendo AM, Cu-Uvin S.<br />
Effect of treatment of asymptomatic bacterial vaginosis on HIV-1 shedding in the genital tract<br />
among women on antiretroviral therapy: a pilot study. Clinical Infectious Diseases 15;49(6):991-<br />
2, 2009.<br />
Mitchell C, Moreira C, Fredricks D, Paul K, Caliendo AM, Kurpewski J, Ingersoll J, Cu-Uvin S.<br />
Detection of fastidious vaginal bacteria in women with HIV infection and bacterial vaginosis.<br />
Infectious Diseases in Obstetrics and Gynecology 2009;2009:236919.<br />
Ghosh M, Shen Z, Fahey JV, Cu-Uvin S, Mayer K, Wira CR. Trappin-2/Elafin: a novel innate<br />
anti-human immunodeficiency virus-1 molecule of the human female reproductive tract. Immunology<br />
129(2):207-19, 2010.<br />
Ghosh M, Fahey JV, Shen Z, Lahey T, Cu-Uvin S, Wu Z, Mayer K, Wright PF, Kappes JC,<br />
Ochsenbauer C, Wira CR. Anti-HIV activity in cervical-vaginal secretions from HIV-positive<br />
and -negative women correlate with innate antimicrobial levels and IgG antibodies. PLoS One<br />
29;5(6):e11366, 2010.<br />
102<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Theiler RN, Farr SL, Karon JM, Paramsothy P, Viscidi R, Duerr A, Cu-Uvin S, Sobel J, Shah K,<br />
Klein RS, Jamieson DJ. High-risk human papillomavirus reactivation in human immunodeficiency<br />
virus-infected women: risk factors for cervical viral shedding. Obstetrics and Gynecology<br />
115(6):1150-8, 2010.<br />
Matteson KA, Boardman L, Clark MA, Munro MG. Abnormal uterine bleeding: A review of<br />
patient-based outcome measures. Fertility and Sterility 92(1):205-16, 2009.<br />
Matteson KA, Phipps MG, Raker C, Sacco LJ, Jackson AL. Discussion: ’Laparoscopic versus<br />
vaginal hysterectomy for benign pathology’ by Candiani et al. American Journal of Obstetrics<br />
and Gynecology 200(4):e1-6, 2009.<br />
Einarsson JI, Matteson KA, Schulkin J, Chavan NR, Sangi-Haghpeykar K. Minimally invasive<br />
hysterectomies - A survey on attitudes and barriers among practicing gynecologists. Journal of<br />
Minimum Invasive Gynecology 17(2):167-175, 2010.<br />
Matteson KA, Clark MA. Questioning our Questions: Do frequently asked questions adequately<br />
cover the aspects of women’s lives most affected by abnormal uterine bleeding?<br />
Opinions of women with abnormal uterine bleeding participating in focus groups. Women and<br />
Health 50(2):195-211, 2010.<br />
Pregler J, Freund KM, Kleinman M, Phipps MG, Fife RS, Gams B, Núñez AE, Seaver R, Lazarus<br />
CJ, Raymond NC, Uijtdehaage S, Guiton G, David M, Gabeau GV, Geller S, Meekma K, Moore<br />
C, Robertson C, Sarto G. The heart truth professional education campaign on women and heart<br />
disease: needs assessment and evaluation results. The Journal of Women’s Health 8(10):1541-<br />
7, 2009.<br />
Sung VW, Raker CA, Myers DL, and Clark MA. Ambulatory care related to female pelvic<br />
floor disorders in the United States, 1995-2006. American Journal of Obstetrics and Gynecology<br />
201(5):508.e1-6, 2009.<br />
Stein MD, Anderson BJ, Caviness CM, Rosengard C, Kiene S, Friedmann P, Clark JG.<br />
Relationship of alcohol use and sexual risk taking among hazardously drinking incarcerated<br />
women: an event-level analysis. Journal of Study on Alcohol and Drugs 70(4):508-15, 2009.<br />
Grobman W, Lai Y, Landon M, Spong C, Leveno K, Rouse DJ, et al. Can a prediction model for<br />
vaginal birth also predict the probability of morbidity related to a trial of labor? Am J Obstet<br />
Gynecol 2009;200:56.e1-6.<br />
Caritis SN, Rouse DJ, Peaceman AM, et al. Prevention of preterm birth in triplets: An<br />
evaluation of 17-alpha hydroxyprogesterone caproate. Obstet Gynecol 2009;113:285-292.<br />
Tita AT, Rouse DJ. Progesterone for the prevention of preterm birth: An evolving intervention.<br />
Am J Obstet Gynecol 2009;200:219-224.<br />
Tita AT, Rouse DJ, Saade G, et al. Evolving concepts in antibiotic prophylaxis for cesarean<br />
delivery: a systematic review. Obstet Gynecol 2009;113:675-682.<br />
Doyle LW, Crowther CA, Middleton P, Marret S, Rouse DJ. Magnesium sulphate for women<br />
at risk of preterm birth for neuroprotection of the fetus. Cochrane Database of Systematic<br />
Reviews 2009, Issue 1. Art. No.: CD004661. DOI: 10.1002/14651858.CD004661.pub3.<br />
Newman RB, Momirova V, Dombrowski MP, Schatz M, Wise R, Landon M, Rouse DJ, et al. The<br />
Effect of Active and Passive Household Cigarette Smoke Exposure on Pregnant Women with<br />
Asthma. Chest 2010;137:601-8.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 103<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
R e s e a r c h i n W o m e n ’ s H e a l t h<br />
Landon, MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, Wapner RJ, Varner MW,<br />
Rouse DJ, et al. A Multicenter, Randomized Trial of Treatment for Mild Gestational Diabetes.<br />
New Engl J Med 2009; 361:1339-48.<br />
Dinsmoor MJ, Gilbert S, Landon MB, Rouse DJ, et al. Perioperative Antibiotic Prophylaxis for<br />
Nonlaboring Cesarean Delivery. Obstet Gynecol 2009;114:752-6.<br />
Grobman WA, Lai Y, Landon MB, Spong CY, Leveno KJ, Rouse DJ, et al. Does Information<br />
Available at Admission for Delivery Improve Prediction of Vaginal Birth after Cesarean? Amer<br />
J Perinatol 2009;26:693-701.<br />
Rouse DJ, Weiner S, Bloom SL, et al. Second-stage labor duration in nulliparous women:<br />
relationship to maternal and perinatal outcomes. AJOG 2009;201:357.el-7.<br />
Gyamfi C, Horton AL, Momirova V, Rouse DJ, et al. The effect of 17-alpha<br />
hydroxyprogesterone caproate on the risk of gestational diabetes in singleton or twin<br />
pregnancies. AJOG 2009;201:392.el-5.<br />
Killam WP, Tambatamba BC, Chintu N, Rouse DJ, Stringer E, Bweupe M, Yu Y, Stringer JS.<br />
Antiretroviral therapy in antenatal care to increase treatment initiation in HIV-infected pregnant<br />
women: a stepped-wedge evaluation. J AIDS 2010:24:85-91.<br />
Cormier C, Landon M, Lai Y, Spong C, Rouse DJ, et al. White’s Classification of Maternal<br />
Diabetes and Vaginal Birth After Cesarean Delivery Success in Women Undergoing a Trial of<br />
Labor. Obstet Gynecol 2010;115:1:60-4.<br />
Bates E, Rouse DJ, Chapman V, Mann ML, Carlo W, Tita A. Fetal lung maturity testing before<br />
39 weeks and neonatal outcomes. Society of Maternal-Fetal Medicine Poster Presentation,<br />
Chicago IL, February 2010.<br />
Harper M, Thom E, Klebanoff M, Thorp J Jr., Sorokin Y, Varner M, Wapner R, Caritis S, Iams<br />
J, Carpenter M, Peaceman A, Mercer B, Sciscione A, Rouse DJ, et al. Omega-3 Fatty Acid<br />
Supplementation to Prevent Recurrent Preterm Birth: A Randomized Controlled Trial. Obstet<br />
Gynecol 2010;115:2.1:234-42.<br />
Biggio J Jr, Chapman V, Neely C, Cliver S, Rouse DJ. Fetal Anomalies in Obese Women: The<br />
Contribution of Diabetes. Obstet Gynecol 2010;115:2.1:290-6.<br />
Contag SA, Clifton RG, Bloom SL, Spong CY, Varner MW, Rouse DJ, et al. Neonatal Outcomes<br />
and Operative Vaginal Delivery Versus Cesarean Delivery. Am J Perinatol 2010;27:493-9.<br />
Refuerzo JS, Momirova V, Peaceman AM, Sciscione A, Rouse DJ, et al. Neonatal Outcomes<br />
in Twin Pregnancies Delivered Moderately Preterm, Late Preterm, and Term .Am J Perinatol<br />
2010;27:537-42.<br />
Schatz M, Dombrowski MP, Wise R, Lai Y, Landon M, Newman RB, Rouse DJ, et al. The<br />
relationship of asthma-specific quality of life during pregnancy to subsequent asthma and<br />
perinatal morbidity. J Asthma 2010; 47:46-50.<br />
Moldenhauer JS, Lai Y, Schatz M, Wise R, Landon MB, Newman RB, Rouse DJ, et al. Influence<br />
of maternal asthma and asthma severity on newborn morphometry. J Asthma. 2010 Mar;<br />
47(2):145-9.<br />
Sorokin Y, Romero R, Mele L, Wapner RJ, Iams JD, Dudley DJ, Spong CY, Peaceman AM,<br />
Leveno KJ, Harper M, Caritis SN, Miodovnik M, Mercer BM, Thorp JM, O’Sullivan MJ, Ramin<br />
SM, Carpenter MW, Rouse DJ, Sibai B. Maternal Serum Interleukin-6, C-Reactive Protein, and<br />
Matrix Metalloproteinase-9 Concentrations as Risk Factors for Preterm Birth
Hashima JN, Lai Y, Wapner RJ, Sorokin Y, Dudley DJ, Peaceman A, Spong CY, Iams JD, Leveno<br />
KJ, Harper M, Caritis SN, Varner M, Miodovnik M, Mercer BM, Thorp JM, O’Sullivan MJ, Ramin<br />
SM, Carpenter M, Rouse DJ, Sibai B. The effect of maternal body mass index on neonatal<br />
outcome in women receiving a single course of antenatal corticosteroids. Am J Obstet Gynecol<br />
2010;202:263.e1-5.<br />
Ramirez MM, Gilbert S, Landon MB, Rouse DJ, et al. Mode of Delivery in Women with<br />
Antepartum Fetal Death and Prior Cesarean Delivery. Am J Perinatol 2010. PMID: 20486068.<br />
Bakhshi T, Landon MB, Lai Y, Spong CY, Rouse DJ, et al. Maternal and Neonatal Outcomes<br />
of Repeat Cesarean Delivery in Women with a Prior Classical versus Low Transverse Uterine<br />
Incision. Am J Perinatol 2010. PMID: 20458666.<br />
Durnwald CP, Momirova V, Rouse DJ, et al. Second trimester cervical length and risk of<br />
preterm birth in women with twin gestations treated with 17-alpha hydroxyprogesterone<br />
caproate. J Matern Fetal Neonatal Med 2010. PMID: 20441408.<br />
Clark EA, Mele L, Wapner RJ, Spong CY, Sorokin Y, Peaceman A, Iams JD, Leveno KJ,<br />
Harper M, Caritis SN, Miodovnik M, Mercer BM, Thorp JM, Ramin SM, Carpenter M, Rouse<br />
DJ. Association of fetal inflammation and coagulation pathway gene polymorphisms with<br />
neurodevelopmental delay at age 2 years. Am J Obstet Gynecol 2010;83.e1-83.e10.<br />
Saleem S, Rouse DJ, et al. Chlorhexidine vaginal and infant wipes to reduce perinatal<br />
mortality and morbidity: a randomized controlled trial. Obstet Gynecol. 2010;115:1225-32.<br />
Wylie BJ, Gilbert S, Landon MB, Spong CY, Rouse DJ, et al. Comparison of transverse and<br />
vertical skin incision for emergency cesarean delivery. Obstet Gynecol. 2010;115:1134-40.<br />
Rouse DJ. Magnesium sulfate for the prevention of cerebral palsy. Am J Obstet Gynecol 2009;<br />
200: 610-612.<br />
BOOKS AND BOOK CHAPTERS<br />
Tita AN, Rouse DJ. Obstetric Management of Labor and Vaginal Delivery. In: Chestnut DH, ed.<br />
Obstetric Anesthesia: Principles and Practice, 4 th edition. Philadelphia: Mosby, 2009.<br />
Figueroa D, Rouse DJ. Location, Mode of Delivery and Intrapartum Issues for the Preterm<br />
Gestation. In: Berghella V, ed. Preterm Birth: Prevention and Management. Philadelphia: Wiley-<br />
Blackwell, 2010.<br />
Rouse DJ, Prevention of Cerebral Palsy. In: Queenan JT, Hobbins JC, and Spong CY, eds.<br />
Protocols for High-Risk Pregnancies, 5 th edition. Hoboken: Wiley-Blackwell, 2010.<br />
Hauth JC, Cunningham FG, Rouse DJ. Use of Magnesium in Obstetrics. ACOG Update (Audio)<br />
2009; 34: #7.<br />
Rouse, DJ. Editor, Williams Obstetrics, 23 rd edition. McGraw-Hill, 2009.<br />
EDITORIALS<br />
Rouse DJ, Hirtz D, Thom E. Reply to Mittendorf and Pryde. N Engl J Med 2009; 360: 190.<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 105<br />
R e s e a r c h i n W o m e n ’ s H e a l t h
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y<br />
MISSION<br />
106<br />
DIVISION OF UROGYNECOLOGY<br />
AND RECONSTRUCTIVE PELVIC SURGERY<br />
The Division of Urogynecology and Reconstructive Pelvic Surgery (URPS) is also known as<br />
the Center for Women’s Pelvic Medicine and Reconstructive Surgery. It is a tertiary care center<br />
whose faculty are subspecialty fellowship-trained in Female Pelvic Medicine and Reconstruc-<br />
tive Surgery; thus they have expertise in the diagnosis and treatment of pelvic floor disorders<br />
such as urinary incontinence, pelvic organ prolapse, defecatory dysfunction, interstitial cystitis,<br />
and fistulas. The mission of the Division of URPS is to:<br />
1. Provide diagnosis and therapy for women with voiding and bowel dysfunction and<br />
abnormalities of the pelvic floor<br />
2. Serve as a referral source of experts for reproductive tract anomalies e.g. Mullerian<br />
agenesis, minimally invasive reconstructive surgery including robotics, sacral stimulators<br />
for chronic urge incontinence and urinary retention, urethral injection materials and<br />
transvaginal systems for prolapse repair<br />
3. Provide education and training for the public, students, post graduate trainees and fellows<br />
in urogynecology<br />
4. Advance the research and science of urogynecologic and pelvic floor conditions<br />
5. Outreach to those with devasting urinary fistulas in underserved areas of the world<br />
The main office location is at 695 Eddy Street with outreach offices at the Medical Office Build-<br />
ings at South County Commons in Wakefield, East Greenwich and Woonsocket, RI.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
FACULTY–PHYSICIAN<br />
Deborah L. Myers, MD, FACOG, Division Director<br />
MD: State <strong>University</strong> of New York at Stony Brook<br />
Medical-Surgical Internship: Rhode Island Hospital<br />
Ob/Gyn Residency: Women & Infants Hospital of Rhode Island<br />
Fellowship: <strong>University</strong> of Connecticut<br />
Dr. Myers joined the Division of Urogynecology and Reconstructive Pelvic<br />
Surgery in 1992. She is board certified in Obstetrics and Gynecology and a<br />
fellow of ACOG. As Division Director, Dr. Myers leads the Division in its continued mission of<br />
patient care, education and research. Dr. Myers was promoted to Professor of Obstetrics and<br />
Gynecology in July 2009. Dr. Myers has particular expertise in the condition of interstitial cysti-<br />
tis. She oversees the RI Network for Pelvic Floor Disorders providers and meetings. She is the<br />
Medical Director of The Program in Women’s Physical Therapy.<br />
Dr. Myers serves on various hospital committees and several search committees for new<br />
faculty. She is a member of the Women’s Health Council of RI. Under her guidance, the Divi-<br />
sion has grown in faculty, space, clinical services and research. The Division now has its own<br />
urogynecologic research coordinator and research assistant, thus growing the Divisions’ ability<br />
to participate in multi-centered trials. Dr. Myers is the site PI for the BRIDGES trial – Bringing<br />
simple urge incontinence diagnosis and treatment to providers.<br />
Dr. Myers’ teaching efforts at Women & Infants Hospital of Rhode Island are primarily work-<br />
shop-based learning. Dr. Myers received teachers an excellence in teaching award for Under-<br />
graduate Education. Nationally, Dr. Myers is the President-elect of the American Urogyneco-<br />
logic Society (AUGS), chairs the AUGS governance task force and is board of director liaison<br />
for the Health Policy committee. Dr. Myers continues to serve on the Subcommittee on Urogy-<br />
necology of the Committee on Gynecologic Practice of ACOG, and as an oral examiner for the<br />
American Board of Obstetrics and Gynecology. For the NIH / NICCD, she continues as a mem-<br />
ber of the Data and Safety Monitoring Board for the Urinary Incontinence Treatment Network<br />
and the Advisory Board for the Pelvic Floor Disorders Network. She continues to serve as a re-<br />
viewer for national journals. Dr. Myers continues to lecture both nationally and locally. She was<br />
the course director for the Women & Infants conference entitled Pelvic Floor Disorders: The<br />
Team Approach held March 2010. She also lectured at 42nd <strong>Annual</strong> Matt Weis Symposium, at<br />
St John’s Mercy Medical Center, in St Louis MO. She presented an “Update on Neuromodula-<br />
tion” and “Obesity and the Pelvic Floor.”<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 107<br />
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y<br />
108<br />
Charles R. Rardin, MD, FACOG<br />
MD: <strong>University</strong> of Rochester<br />
Residency: Beth Israel Deaconess Hospital<br />
Fellowship: Mount Auburn Hospital, Harvard Medical School Affiliated Hospitals<br />
Dr. Rardin joined the Division of Urogynecology and Reconstructive Pelvic Sur-<br />
gery in 2003. He is an Assistant Professor of Obstetrics and Gynecology. He is board certified<br />
in Obstetrics and Gynecology and a fellow of ACOG. He is the Director of the fellowship In<br />
Female Pelvic Medicine and Reconstructive Surgery (FPM&RS). Dr Rardin remains the leader<br />
in endoscopic surgery for the fellowship; he oversees the minimally invasive, laparoscopic and<br />
robotic training for the fellows. He continues to be the leader in Rhode Island and Southeastern<br />
New England for robotically-assisted pelvic reconstructive surgery, including sacral colpopexy<br />
for advanced pelvic organ prolapse. He serves on the Women and Infants Hospital Resident<br />
Evaluation Committee, Surgical Services Council, and Quality Council, and on the Robotic Sur-<br />
gical Services Steering Committee.<br />
Dr. Rardin’s research continues to evaluate prenatal risk factors for development of perineal<br />
trauma during childbirth, and the use of peripheral neuromodulation for voiding dysfunction<br />
and bladder overactivity. Dr Rardin is the Rhode Island site PI for a multi-centered surgical<br />
trial –SECURiTy, evaluating different sling devices for incontinence. He remains a reviewer for<br />
several journals.<br />
Dr Rardin’s teaching skills continue to be recognized. Over this past year he received the<br />
Women and Infants’ Hospital Excellence in Teaching Award, and Top Full-Time Faculty Teacher<br />
of the Year in both Undergraduate Medical Education and Resident Medical Education. Dr. Rar-<br />
din serves on the Postgraduate Referral Committee at Alpert Medical School of <strong>Brown</strong> Univer-<br />
sity, and serves as Advisor for medical students seeking residency in OB/Gyn. He continues to<br />
give grand rounds lectures locally and nationally. His presentations have involved roundtable<br />
discussions and hands – on – cadaver courses on laparoscopic (AAGL) and minimally invasive<br />
techniques. He is the Program Chair of the AUGS Female Pelvic Medicine for the Office-Based<br />
Provider Course, and the Program Chair for AAGL Postgraduate Course entitled “When Lapa-<br />
roscopy is Not Enough”. He will be serving as faculty for the upcoming AUGS Postgraduate<br />
Course “Masters of Surgery.”<br />
Nationally, Dr. Rardin continues to serve as website editor and director of the Information<br />
Technology Sub–committee on of the Public Relations Committee of the American Urogynecol-<br />
ogy Society. He is now on the program committee for AUGS. For the American Association of<br />
Gynecologic Laparoscopists, he serves the Publication Committee and its Video Review com-<br />
mittee for the scientific program. He is also on the Education Committee of the Society of Gy-<br />
necologic Surgeons. At the <strong>Annual</strong> Clinical Meeting of the American College of Obstetricians &<br />
Gynecologists, he presented the clinical seminar “Innovations in Pelvic Surgery: Old Standards<br />
vs. Kit-based Newcomers”. He speaks regularly on the indications and complications, and<br />
medicolegal implications for the use of mesh on pelvic reconstructive surgery<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Vivian W. Sung, MD, MPH<br />
MD: Tufts <strong>University</strong> School of Medicine<br />
Residency: Magee-Women’s Hospital / <strong>University</strong> of Pittsburgh Medical Center<br />
Fellowship: Women & Infants Hospital of Rhode Island/ <strong>Brown</strong> Medical School<br />
Dr. Sung joined the Division of Urogynecology and Reconstructive Pelvic Surgery<br />
in 2006. She is board certified in Obstetrics and Gynecology and a fellow of ACOG. Dr. Sung is<br />
currently an Assistant Professor of Obstetrics and Gynecology. She completed a dual fellow-<br />
ship in Female Pelvic Medicine and Reconstructive Pelvic Surgery and the John Evrard Fel-<br />
lowship in Epidemiology and Clinical Trials at Women and Infants Hospital in 2006, and transi-<br />
tioned off of the NICHD Women’s Reproductive Health Research (K 12 WRHR) program in 2009.<br />
Her research is now supported by a K23 career development award through the NICHD (2009-<br />
2014) and an American Urogynecologic Society Foundation Grant (2008-2010), and is focused<br />
on patient-reported outcomes for female pelvic floor disorders. She is site Co-investigator as<br />
well as a member of the Steering Committee and Executive Committee for the BRIDGES study,<br />
a multi-center randomized trial and site PI for the Informed Consent Evaluation project, a multi-<br />
center prospective cohort study. Her research skills and achievements are nationally recog-<br />
nized. She served as served as Co-Chair for the Society of Gynecologic Surgeons Systematic<br />
Review Writing Group from 2006-2009. Dr Sung is now the Chair for the Research Committee<br />
of the Society of Gynecologic Surgeons and a member of the Research Committee for the<br />
American Urogynecologic Society. She serves on the Senior Advisory Board for the Fellow’s<br />
Pelvic Research Network of the Society of Gynecologic Surgeons and is on the Board of Direc-<br />
tors for the National Association for Continence. She is highly productive on a research level<br />
and serves as the Division of Urogynecology Research Director. She oversees the Division’s<br />
research team, which includes a research nurse coordinator, 1-2 research assistants, and 1 re-<br />
search intern at any given time with numerous ongoing multi-center studies. Dr. Sung remains<br />
involved in teaching and mentorship and is the mentor for many resident research projects.<br />
B. Star Hampton, MD, FACOG<br />
MD: Mount Sinai School of Medicine<br />
Residency: New York <strong>University</strong> School of Medicine<br />
Fellowship: New York <strong>University</strong> School of Medicine<br />
Dr. Hampton joined the Division of Urogynecology and Reconstructive Pelvic<br />
Surgery in 2006. She is board certified in Obstetrics and Gynecology and a fellow of ACOG.<br />
She is currently Assistant Professor of Obstetrics and Gynecology at <strong>Brown</strong> Medical School. Dr<br />
Hampton’s primary academic focus is education. Dr. Hampton is the Director of the Core Clerk-<br />
ship in Obstetrics and Gynecology at Warren Alpert School of Medicine of <strong>Brown</strong> <strong>University</strong><br />
and remains a small group leader for Biomed 351 Human Reproduction, Growth and Develop-<br />
ment Pathophysiology. Her teaching expertise is sought after. This past year she presented<br />
the “Mentoring” seminar at the Clinical Faculty Teaching Workshop, Alpert Medical School.<br />
She presented a roundtable at the National APGO Faculty Development Seminar “Students<br />
teaching students: covering APGO Educational Objectives during the Ob/Gyn clerkship”. Dr.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 109<br />
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y<br />
Hampton was awarded the Dean’s Excellence in Teaching Award for her teaching in the Ob/Gyn<br />
Core Clerkship, and had the honor to be elected Faculty Marshall for the Alpert Medical School<br />
Commencement by the graduating class. She received Excellence in Teaching Awards for both<br />
undergraduate and resident education, as well as the Full-time Faculty award from Chief Resi-<br />
dents. She completed the APGO Educational Scholar and Leader program. Dr Hampton serves<br />
on the Education Council and was co-leader of the Parental Leave Task Force at Women and<br />
Infants. Dr. Hampton was elected to and currently serves on the Postgraduate Referral Commit-<br />
tee for Alpert Medical School. She was elected to and is a member of the Education Committee<br />
of the American Urogynecologic Society.<br />
Dr. Hampton’s recent research has been centered in education. She completed her project<br />
“Using interactive computer modules with dynamic animation for individual-based learning<br />
of female pelvic anatomy and female pelvic floor dysfunction” which led to two publications.<br />
Within her subspecialty of urogynecology, she has presented a roundtable discussion on New<br />
Approaches to Pelvic Floor Repair as well as a Clinical Seminar on Innovation in Pelvic Surgery<br />
at the ACOG annual meeting. She presented on Stress Urinary Incontinence at the RI Network<br />
for PFDs conference at Women and Infants Hospital, and gave grand rounds on Urinary Incon-<br />
tinence at Backus Hospital. She has collaborated with radiology on MRI imaging of the pelvic<br />
floor which led to a publication “Imaging pelvic floor disorders: trend towards comprehensive<br />
MR imaging” in the American Journal of Roentgenology. She is an editorial reviewer for In-<br />
ternational Urogynecology Journal and European Journal of Obstetrics and Gynecology and<br />
Reproductive Biology.<br />
110<br />
Cassandra L. Carberry MD MS<br />
MD: <strong>University</strong> of Texas Health Science Center at San Antonio School of Medicine<br />
Residency: New York <strong>University</strong> School of Medicine<br />
Fellowship: New York <strong>University</strong> School of Medicine<br />
Master of Science: New York <strong>University</strong> School of Medicine<br />
Dr. Carberry joined the Division of Urogynecology and Reconstructive Pelvic Surgery in 2009.<br />
She is board certified in Obstetrics and Gynecology. Dr Carberry is Clinical Assistant Professor<br />
of Obstetrics and Gynecology. She completed her fellowship in Female Pelvic Medicine and Re-<br />
constructive Surgery in 2009 at New York <strong>University</strong> School of Medicine. While in fellowship she<br />
also enrolled in a Master of Science Degree program, and in May 2010 was awarded a Master of<br />
Science in Clinical Investigation, completing her thesis on “Desire for Information and Decision-<br />
making in Women with Pelvic Floor Disorders.” Her academic focus is patient outcomes. As<br />
a fellow, she was active in the Fellows’ Pelvic Research Network (sponsored by the Society of<br />
Gynecologic Surgeons), gaining valuable experience in conducting multi-center clinical research<br />
and co-authoring publications. Since completing fellowship, she has become an active member<br />
of the Systematic Review Group of The Society of Gynecologic Surgeons. She is an editorial<br />
reviewer for the Journal of Sexual Medicine.<br />
Dr. Carberry is Course Leader, for ObG-492, Clinical Urogynecology and Pelvic Reconstructive<br />
Surgery, MS4 Elective, for Alpert Medical School of <strong>Brown</strong> <strong>University</strong>. She also oversees men-<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
tors, educates and develops curricula for all outside residents rotating from Family Practice,<br />
Internal Medicine, and Women’s Health, fellows from Women’s Gastroenterology and Geriat-<br />
rics, as well as OB/GYN residents from other hospitals interested in fellowship in Female Pelvic<br />
and Reconstructive Surgery. She is a committed teacher, regularly precepting and providing<br />
lectures for third year medical students, as well as mentoring OB/GYN residents. She received<br />
recognition for Excellence in Teaching for the ObG-490 Core Clerkship in 2010. She has given<br />
Grand Rounds at various hospitals in Southern New England. Dr Carberry is the Division’s<br />
outreach point person for the northern RI region seeing patients at the Woonsocket Medical<br />
Office Building. She is interested in expanding clinical care as well as community outreach and<br />
education.<br />
NURSE PRACTITIONER<br />
Sarah M Collins, MSN, APRN-BC, completed her Masters in Nursing / Nurse Prac-<br />
titioner degree at Simmons College in Boston, MA. She attended undergraduate<br />
study at Bridgewater State College in Bridgewater, MA and earned a BS in Psy-<br />
chology. She joined the Division in December 2008. She has expertise in non-sur-<br />
gical management of urinary incontinence, pelvic prolapse, and interstitial cys-<br />
titis. Prior to her joining the Division, Sarah was a Nurse practitioner at the Beth<br />
Israel Deaconess Medical Center – Joslin Center in Needham, MA. Sarah has had experience in<br />
education as she was Assistant Professor of Nursing at the Caritas Laboure College in Boston<br />
MA. She has had expertise in alternative teaching techniques using video and simulation.<br />
Sarah also has research experience as she was a research nurse practitioner/ clinical research<br />
coordinator at the Boston Medical Center, Androgen Clinical Research Unit in Boston from<br />
2005-2006. As natural progression, she is research personnel of the Division’s BRIDGES trial.<br />
She also is a member of the National Association of Nurse Practitioners in Women’s Health,<br />
American Urogynecolologic Society, International Pelvic Pain Society, Interstitial Cystitis As-<br />
sociation and Interstitial Cystitis Network.<br />
CLINICAL ACTIVITY<br />
Referrals to the Division come from over 500 physicians’ offices. The majority of patients<br />
seen at the Division of Urogynecology and Reconstructive Pelvic Surgery are by referral from<br />
colleagues over a wide geographic area, principally, RI and Southern Massachusetts. The<br />
increased demand for clinical services has led to the Division’s growth. Dr Cassandra Carberry<br />
joined the faculty in August 2009 and Dr Kyle Wohlrab will join in July 2010. Dr Wohlrab com-<br />
pleted his fellowship in FPM&RS at Women & Infants and will be active in resident teaching<br />
and robotics. With the increase in faculty and research, the Division’s clinical area underwent<br />
renovation to increase exam rooms and incorporate research offices and research clinical<br />
space. Academic offices are located at 45 Willard. Patients are sent for diagnosis and definitive<br />
therapy by the Division’s attending physicians, with surgery conducted at Women & Infants<br />
Hospital of Rhode Island. Particular effort is made to maintain the referring physician’s special<br />
relationship with the patient as an integral part of the collaborative therapeutic decision.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 111<br />
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y<br />
The Division has had office hours at the Women & Infants Hospital of Rhode Island South<br />
County Commons offsite; services have expanded to the East Greenwich and Woonsocket<br />
Medical Office Buildings. Future outreach is planned into Eastern Connecticut and Massachu-<br />
setts to ensure that women and their providers have convenient access to tertiary urogyneco-<br />
logic services.<br />
The basic philosophy of the Division is to discuss all means of therapy (conservative and<br />
surgical) and to tailor therapy individually. A full range of therapeutic modalities is offered,<br />
including exercise programs, behavior modification, vaginal devices, pharmacological therapy<br />
as well as surgery. As evidence of its commitment to a broad base of therapeutic options, the<br />
Division’s oversight of the physical therapy department for pelvic floor musculature rehabilita-<br />
tion therapy has led to increased growth. Providers from not only the local area, but also the<br />
New England region, refer to the division’s pelvic rehabilitation services thus demonstrating an<br />
increased need for this type of service.<br />
Fiscal Year 2005 2006 2007 2008 2009<br />
Outpatient surgery 142 172 213 234 285<br />
Inpatient surgery 207 182 239 261 249<br />
Urodynamics 975 989 1257 1101 1167<br />
New patient consults 777 787 1155 1148 1211<br />
The faculty at the Division keeps current with the use of graft and synthetic materials for re-<br />
construction, mid urethral retropubic sling tapes and transoburator tapes, mini – slings, ure-<br />
thral injection materials, placement of sacral stimulators for neuromodulation and minimally<br />
invasive/ laparoscopic techniques and robotics. Although urinary incontinence comprises the<br />
preponderance of pelvic floor dysfunction, to a lesser frequency, but equally important, pelvic<br />
floor dysfunction may involve the lower intestinal tract. Appropriate diagnosis and manage-<br />
ment of rectal abnormalities are pursued with collaboration of the Women’s Gastroenterology<br />
service at Women & Infants Hospital of Rhode Island and with Colorectal Surgery services<br />
at the RI Hospital and Miriam Hospital. Patients with rectal compartment abnormalities are<br />
studied with ultrasound, anal manometry, and pelvic nerve conduction studies. The increased<br />
recognition of the utility of pelvic floor MRI to assist in evaluation of complex pelvic floor dis-<br />
orders has also led to increased demand for this imaging study from the Department of Radiol-<br />
ogy. The Rhode Island Network for Pelvic Floor Disorders has been established under Women<br />
& Infants Hospital launched by a successful CME conference held March 2010. The conference<br />
had both educational sessions for patients and providers, showcasing the interdisciplinary<br />
pelvic floor network. The RI Network for PFDs enhances providers’ ability to evaluate, diagnose<br />
and treat women with complex pelvic floor disorders. Regular monthly meetings continue<br />
amongst the providers for discussion of complex patients. All related disciplines (urogynecol-<br />
ogy, gastrointestinal, radiology, female urology, physical therapy and colo-rectal) participate in<br />
the monthly meetings.<br />
112<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
EDUCATION<br />
The educational activities of the staff of the Division of U&RPS are diverse and deeply involved<br />
on a number of fronts – the public, medical students, residency training, fellowship and col-<br />
leagues.<br />
Teaching to the lay public is supported by participation and efforts of the members of the Divi-<br />
sion staff and the public relations staff of the hospital. Locally, faculty have presented at Wom-<br />
en and Infants’ Patient Information sessions, presented to local senior groups, and appeared<br />
in newspaper articles, and radio and television spots to provide information on pelvic muscle<br />
disorders. This awareness has led to an increased consciousness in the lay community and<br />
increased demand for formalized evaluation.<br />
Education efforts at Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong> occur at various levels.<br />
The Division of Urogynecology faculty teach 2nd year students during the Human Reproduc-<br />
tion Growth and Development section of the Integrated Medical Sciences Course on campus.<br />
The faculty and fellows in the Division serve as preceptors for the 3rd year medical students<br />
during their core clerkship in Ob/ Gyn. As part of the core curriculum in Ob/Gyn the third year<br />
medical students are taught an appreciation of the differential diagnosis of urinary inconti-<br />
nence. An elective for fourth year students in pelvic surgery/ urogynecology is offered to the<br />
students at <strong>Brown</strong> as well as students from other medical schools.<br />
Resident training is very much an active part of the teaching portfolio. A series of compre-<br />
hensive lectures in Urogynecology and Reconstructive Pelvic Surgery is part of the residency<br />
core curriculum, given on a recurring two-year cycle. Chief residents (PGY4) rotate through the<br />
division for 7–8 weeks. During that time they participate in all the activities of the Division, in<br />
the consultation room, the operating room as well as in the diagnostic laboratory. Here they re-<br />
ceive hands–on instruction in evaluation, management and longitudinal postoperative follow–<br />
up. Residents at the PGY-3 level from other Ob/ Gyn programs do electives in urogynecology<br />
often leading them to pursue and procure fellowship positions. Second year resident rotation<br />
in the division is 2 ½ days per week with exposure to both office and the operating room. The<br />
PGY2 and PGY4 residents also participate in the Division’s “fellow’s clinic” one half day per<br />
month giving them direct patient care responsibilities in diagnosis and management of urogy-<br />
necologic patients.<br />
The faculty of the Division of Urogynecology and Pelvic Reconstructive Surgery run and par-<br />
ticipate in various “hands–on”/skills workshops. As part of the PGY-1 orientation week- our<br />
faculty participate in the “surgical skills” lab. During the third year of residency, the faculty and<br />
fellows under the direction of Dr. Myers, provide a three hour educational session on teaching<br />
pelvic anatomy using clay models. This novel teaching lab has been shown to be effective and<br />
fun in learning pelvic anatomy. The faculty and fellows also work under the direction of Diane<br />
Angelini, PhD, Program in Midwifery, in a “hands on” training session for 3rd and 4th degree<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 113<br />
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y<br />
episiotomy repair for the incoming 3rd year residents and a refresher session for 4th year<br />
residents using a beef–tongue model. In the spring, a fresh frozen cadaver workshop, directed<br />
at repair of urological and intestinal injuries (PGY-3) and an anatomy teaching of the human<br />
female pelvis is provided (PGY-4) residents. Under the direction of Drs. Hampton and Rardin,<br />
faculty and fellows serve as preceptors. Dr Rardin participates in the endoscopy lab work-<br />
shops. Residents each year rate these workshops highly.<br />
Many other specialties under the direction of Dr Carberry rotate through the Division, gleaning<br />
experience and exposure to problems of urinary incontinence and pelvic prolapse: residents in<br />
Women’s Health and fellows in Geriatric Medicine from RI Hospital, Family Medicine and Inter-<br />
nal Medicine residents from Memorial Hospital. A Fellowship training experience is provided<br />
for the fellows in the Division of Gastroenterology.<br />
To support the efforts of the Division in clinical care, teaching and research, a philanthropic<br />
campaign, the “Grateful Patient” was developed and implemented.<br />
FELLOWSHIP TRAINING<br />
In 1998, the fellowship program in Female Pelvic Medicine and Pelvic Reconstructive Surgery<br />
was approved, and recertified in 2002, 2005 and most recently 2010. There are currently 38 cer-<br />
tified fellowship programs in Female Pelvic Medicine and Reconstructive Pelvic Surgery. The<br />
Division has graduated 10 fellows:<br />
Peter Rosenblatt, MD (1995) Assistant Professor of Ob/Gyn, Director Division of Urogynecol-<br />
ogy, Mount Auburn Hospital, Harvard Medical School Affiliated Hospitals, Cambridge, MA.<br />
Christine LaSala, MD (1997) Clinical Associate Professor of Ob/Gyn, Director of the Division of<br />
Urogynecology, Hartford Hospital, <strong>University</strong> of Connecticut, Hartford, CT.<br />
Lily Arya, MD (2000) Assistant Professor of Ob/Gyn, Director of the Division of Urogynecology<br />
and the Fellowship in Female Pelvic Medicine & Reconstructive Surgery, <strong>University</strong> of Pennsyl-<br />
vania, Philadelphia, PA.<br />
Jeffrey Clemons MD, LTC, MC (2002) Chief, Urogynecology and Pelvic Reconstructive Surgery,<br />
Chief, Gynecology Madigan Army Medical Center, Tacoma, WA.<br />
Vivian Aguilar, MD (2003) Director, Fellowship in Urogynecology and Reconstructive Pelvic<br />
Surgery, Department of Ob/Gyn, Cleveland Clinic Florida, Weston, FL.<br />
Eric Sokol, MD (2005) Assistant Professor of Ob/Gyn, Co–Director of the Division of Urogyne-<br />
cology and Reconstructive Pelvic Surgery, Stanford <strong>University</strong>, Palo Alto, CA.<br />
114<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Vivian W Sung, MD, MPH (2006) Assistant Professor of Ob Gyn, Leader in Research Training,<br />
Division of Urogynecology and Reconstructive Pelvic Surgery, <strong>Brown</strong> Medical School,<br />
Providence, RI.<br />
Renee Ward, MD (2005–2008), Assistant Professor of Ob/Gyn, Division of Gynecology, Vander-<br />
bilt <strong>University</strong>, Nashville TN.<br />
Elisabeth A. Erekson, MD (2006–2009), Assistant Professor of Ob/Gyn, Yale <strong>University</strong>, New<br />
Haven CT.<br />
Kyle J. Wohlrab, MD (2007-2010), Clinical Assistant Professor of Ob/Gyn, Division of Urogyne-<br />
cology and Reconstructive Pelvic Surgery, Alpert Medical School of <strong>Brown</strong> <strong>University</strong>, Provi-<br />
dence, RI.<br />
Blair B. Washington, MD, MHA (2008-2011) will be the Division’s 3rd year fellow in Female<br />
Pelvic Medicine & Reconstructive Surgery. Dr. Washington completed her MD and MHA at the<br />
<strong>University</strong> of Washington School of Medicine (2002) and then a general surgery internship at<br />
Howard <strong>University</strong> (2003). She completed her residency in Obstetrics and Gynecology at The<br />
Stamford Hospital, Columbia <strong>University</strong> College of Physicians and Surgeons (2008). She has<br />
been recognized as an effective educator and received the graduate medical education Fellow<br />
Excellence in Teaching Award in June 2010. Dr. Washington also serves as a preceptor for the<br />
students in the OB/Gyn core clerkship, preceptor for Gyn morning report, and a preceptor for<br />
the division’s educational workshops and the department’s endoscopy course. With regard to<br />
research, Dr. Washington was awarded Best Manuscript at the 2009 meeting of the American<br />
Urogynecologic Society for her evaluation of the ambulatory costs of female pelvic floor dis-<br />
orders. She has also published this year on the association between prolapse and defecatory<br />
dysfunction, the association between obesity and prolapse and the costs of ambulatory care<br />
related to female pelvic floor disorders in the United States. Dr. Washington’s research inter-<br />
ests focus on access to health care.<br />
Peter C Jeppson, MD (2010-2013) will be the Division’s 1st year fellow in Female Pelvic Medi-<br />
cine & Reconstructive Surgery. Dr Jeppson graduated from Saint Louis <strong>University</strong> Health<br />
Sciences Center, Saint Louis, MO in 2006 and completed residency in Ob/Gyn at Case Western<br />
Reserve <strong>University</strong> MetroHealth Medical Center/Cleveland Clinic in 2010, where he was se-<br />
lected to be the chief administrative resident. During residency Dr Jeppson was recognized for<br />
his teaching efforts – he was awarded the Bayer HealthCare Pharmaceuticals Best PGY2 Ob/<br />
Gyn Teaching Resident. In 2009 was awarded the Arnold P. Gold Foundation, an award for hu-<br />
manism and excellence in teaching. He has a long track record of teaching at all levels- he was<br />
an arithmetic and reading teacher for elementary students, as well as college level chemistry<br />
teaching assistant and medical student anatomy instructor. Dr Jeppson has traveled on out-<br />
reach missions to Guatemala. His research interests have been in pelvic pain syndromes and<br />
robotic outcomes.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 115<br />
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y<br />
Nicole B. Korbly, MD (2010-2013) will be the Division’s 1st year fellow in Female Pelvic Medi-<br />
cine & Reconstructive Surgery. Dr Korbly graduated AOA from <strong>University</strong> of Massachusetts<br />
Medical School, Worcester MA in 2006. She completed her OB/Gyn residency at Women and<br />
Infants Hospital (2010). Dr Korbly has a strong interest in research. Prior to medical school, Dr<br />
Korbly worked as a research coordinator at the Massachusetts General Hospital in the Depart-<br />
ment of Psychiatry. She also spent a summer (1998) at the NIH as a research coordinator in the<br />
Department of Child Psychiatry. During residency she served as the resident representative for<br />
WIH IRB. Her research pursuits in the field of urogynecology have been investigating the effect<br />
of pelvic floor physical therapy on QOL, sexual function and body image in women with pelvic<br />
floor disorders.<br />
RESEARCH/PUBLICATIONS<br />
The Division continues to make yearly presentations at the AUGS (American Urogynecologic<br />
Society) scientific meetings since 1997 and at the SGS (Society of Gynecologic Surgeons)<br />
annual meetings since 2000. The Division’s leader in research, Dr Vivian W Sung MD MPH,<br />
urogynecologic research coordinator, Ann Meers, RN and research assistant, Felisha Marques,<br />
all enhance the Divisions’ ability to participate in national multi-centered trials and perform its<br />
own larger prospective studies. This establishment of research personnel is an investment in<br />
the future of the Division’s research and reputation.<br />
Lowenstein L, Gamble T, Sanses T, Van Raalte H, Carberry CL, Jakus S, Kambiss S, McAchran<br />
S, Pham T, Aschkenazi S, Hoskey K, Kenton K for the Fellows’ Pelvic Research Network. Sexual<br />
Function is Related to Body Image Perception in Women with Pelvic Organ Prolapse.<br />
J Sex Med 2009 Aug;6(8):2286-91.<br />
Erekson EA, Weitzen S, Sung VW, Raker C, Myers DL. Socioeconomic indicators and hysterec-<br />
tomy status in the United States, 2004. J Reprod Med 2009 Sep;54(9):553-8.<br />
Sung VW, Hampton BS. Epidemiology of pelvic floor dysfunction. Obstet Gynecol Clin North<br />
Am, 2009;Sep 36(3):421-43.<br />
Sung VW, Raker CA, Myers DL, Clark MA. Ambulatory related care related to female pelvic<br />
floor disorders in the United States 1995- 2006. Am J Obstet Gynecol. 2009 Nov; 201(5):508.<br />
PMCID: PMC2784092.<br />
Sung VW, Joo K, Marques F, Myers DL. Patient-reported outcomes after combined surgery<br />
for pelvic floor disorders in older compared to younger women. Am J Obstet Gynecol. 2009<br />
Nov;201(5):534. PMCID: PMC2783851.<br />
Hampton BS, Erekson EA, “Antibiotic prophylaxis for short-term post-operative transurethral<br />
Foley catheter use in women after sub-urethral sling,” J Pelv Med Surg, Nov/Dec 2009;<br />
15:427-443.<br />
116<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Hampton BS, Ward RM, Idrissa A, “Attitudes and expectations of women undergoing vaginal<br />
fistula repair in Niger,” J Pelv Med Surg, Nov/Dec 2009; 15:441-447.<br />
Lowenstein L, Gamble T, Sanses T, Van Raalte H, Carberry CL, Jakus S, Pham T, Nguyen A,<br />
Hoskey K, Kenton K. Changes in Sexual Function after Treatment for Prolapse Are Related to<br />
Improvement in Body Image Perception. J Sex Med. 2010 Feb;7(2 Pt 2):1023-8.<br />
Sung VW, Raker C, Myers DL, Clark MA. Treatment decision- making and information -seeking<br />
preferences in women with pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct. Int<br />
Urogynecol J Pelvic Floor Dysfunct. 2010 Apr 28. [Epub ahead of print]<br />
Washington BB, Erekson EA, Kassis NC, Myers DL. The association between obesity and stage<br />
II or greater prolapse. Am J Obstet Gynecol. 2010 May;202(5):503.e1-4.<br />
Woodfield CA, Krishnamoorthy S, Hampton BS, Brody JM, “Imaging pelvic floor disorders:<br />
trend towards comprehensive MR imaging,” AJR Am J Roentgenol. 2010 Jun;194(6):1640-9.<br />
Review.<br />
Hampton BS, Sung VW. Improving medical student knowledge of female pelvic floor dysfunc-<br />
tion and anatomy: a randomized trial. Am J Obstet Gynecol. 2010 Jun; 202(6):601.e1-8.<br />
ACTIVE GRANTS<br />
K23HD060665-01 (Sung, PI) 6/15/09-6/15/14<br />
NIH-NICHD<br />
Patient-reported outcomes in functioning for female pelvic floor disorders<br />
Role: PI<br />
Career development award focused on developing and testing a comprehensive question-<br />
naire for patient functioning in female pelvic floor disorders utilizing traditional and innovative<br />
survey methods and item response theory psychometrics. The questionnaire framework will<br />
be guided by the NIH-PROMIS framework and the patient perspective. Provides 75% protected<br />
time for research and career development.<br />
American Urogynecologic Society Foundation Grant (Sung, PI) 12/16/08-12/31/10<br />
Application of the Patient-<strong>Report</strong>ed Outcomes Measurement Information System (PROMIS) to<br />
Female Pelvic Floor Disorders<br />
Role: PI<br />
To determine the face and content validity of the National Institutes of Health PROMIS system<br />
and the feasibility and usability of computerized-adaptive testing for collecting patient-reported<br />
outcomes in women with urinary incontinence.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 117<br />
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y
U r o g y n e c o l o g y & R e c o n s t r u c t i v e<br />
P e l v i c S u r g e r y<br />
BRIDGES (Bringing Simple Urge Incontinence Diagnosis and Treatment to Providers)<br />
(<strong>Brown</strong>, PI)<br />
Role: Site PI Myers, Co- PI Sung<br />
Multi-center study evaluating the effect of fesoterodine to placebo in the treatment of urge<br />
urinary incontinence.<br />
Informed Consent Process for Women Undergoing Surgery for Stress Incontinence<br />
(Rogers, PI)<br />
Role: Site PI Sung<br />
Multi-center study evaluating patient knowledge, understanding and recall of the surgical<br />
informed consent process before and after midurethral sling treatment for stress<br />
urinary incontinence.<br />
Foundation for Female Health Awareness<br />
2009 - present<br />
SECURiTy; Role: site PI Rardin<br />
A randomized trial comparing the Tension-Free Vaginal Tape (TVT) procedure with the TVT-<br />
SECUR for the surgical treatment of stress urinary incontinence.<br />
AWARDS<br />
Washington BB, Raker C, Sung VW. Medicare Costs and Private Payer Charges for the Ambu-<br />
latory Care of Female Pelvic Floor Disorders in 2006. (Oral Presentation) American Urogyne-<br />
cologic Society 30th <strong>Annual</strong> Clinical Meeting in Hollywood, FL. September 24th to 26th, 2009.<br />
Best Manuscript, American Urogynecologic Society Outstanding Science Award.<br />
Carson SA. “An Update on Female Sexual Response,” Pelvic Floor Disorders Conference,<br />
Women & Infants Hospital of Rhode Island, Providence, RI, March 13, 2010.<br />
Carson SA. “An Update on Female Sexual Dysfunction,” Grand Rounds, Massachusetts General<br />
Hospital, Boston MA, May 6, 2010.<br />
Carson SA. “Take Down the Heat of Hot Flashes,” Sisterhood meeting, Temple Sinai, Cranston<br />
RI, June 2, 2010.<br />
118<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
EMERGENCY OB/GYN<br />
Donna M. LaFontaine, MD, Director<br />
BA: Holy Cross College<br />
MD: <strong>University</strong> of Massachusetts<br />
Ob/Gyn Residency: Women & Infants Hospital of Rhode Island<br />
Dr. Donna Lafontaine is the Director of the Division of Emergency Obstetrics<br />
and Gynecology and a Clinical Assistant Professor at the Warren Alpert School of Medicine<br />
at <strong>Brown</strong> <strong>University</strong>. She came to the Triage Unit in 2003 and her professional goals include<br />
improving the quality of care as well as the efficiency of care in the OB/GYN Triage Unit. She<br />
coordinated efforts to start a Sexual Assault Nurse Examiner Program at Women and Infants,<br />
currently the only hospital in Rhode Island offering these resources to patients. Dr. LaFontaine<br />
participates in the teaching of medical students and residents and serves as preceptor for<br />
BioMed 331A (Ob/Gyn core clerkship). Dr. LaFontaine coordinates and directs the experience<br />
of the visiting residents from the RIH Emergency Medicine Residency and Kent Emergency<br />
Medicine Residency.<br />
Alfredo Gil, MD<br />
BS: Florida International <strong>University</strong><br />
MD: Howard <strong>University</strong> College of Medicine<br />
Ob/Gyn Residency: Thomas Jefferson <strong>University</strong> Hospital<br />
Dr. Alfredo Gil, Clinical Assistant Professor if Obstetrics and Gynecology at War-<br />
ren Alpert Medical School of <strong>Brown</strong> <strong>University</strong>, joined the Division of Emergency Obstetrics<br />
and Gynecology as a full time attending in March 2010. A member of the Women & Infants<br />
community faculty since 2004, and a private attending with a local practice, Dr. Gil brings an in-<br />
terest and expertise in minimally invasive gynecologic surgery and treatment of incontinence.<br />
He also continues as an active member of the Clinic Attending Service.<br />
Robyn Gray-Puleo, D.O.<br />
BA: Wheaton College<br />
MD: <strong>University</strong> of New England College of Osteopathic Medicine<br />
Ob/Gyn Residency: Christiana Care Health System<br />
Dr. Robyn Gray-Puleo has been a member of the Women & Infants physician staff<br />
since 2004 as a private attending and participant in the Clinic Attending Service. A Fellow of<br />
the American College of Obstetrics and Gynecology, she joined the Division of Emergency Ob-<br />
stetrics and Gynecology in August 2008. Her expertise is in general obstetrics and gynecology<br />
with an interest in pediatric and adolescent gynecology.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 119<br />
E m e r g e n c y O b / G y n
E m e r g e n c y O b / G y n<br />
120<br />
Moune Jabre-Raughley, MD<br />
BA: Boston <strong>University</strong><br />
MD Boston <strong>University</strong><br />
Ob/Gyn Residency: Women & Infants Hospital of Rhode Island<br />
Dr. Moune Jabre-Raughley graduated from residency in June 2009 and joined the<br />
staff of the Division of Emergency Obstetrics and Gynecology in July of the same year. Flu-<br />
ent in Arabic and French, Dr Jabre-Raughley has an interest in global health and international<br />
medicine. She is also a Fellow of the American College of Obstetrics and Gynecology.<br />
Martha Pizzarello, MD<br />
BA: Boston College<br />
MD: Georgetown <strong>University</strong> School of Medicine<br />
Ob/Gyn Residency: Tufts-New England Medical Center<br />
Dr. Martha Pizzarello, Clinical Assistant Professor of Obstetrics and Gynecology at<br />
Warren Alpert Medical School of Medicine at <strong>Brown</strong> <strong>University</strong>, serves as an attending physi-<br />
cian in the Division of Emergency Obstetrics and Gynecology and participates in the Clinic At-<br />
tending Service. A Fellow of the American College of Obstetrics and Gynecology, Dr. Pizzarello<br />
comes to Women & Infants Hospital of Rhode Island from the Vincent Obstetrics and Gynecol-<br />
ogy Service at Massachusetts General Hospital where she served as an Instructor at Harvard<br />
Medical School. Her interests and expertise are in general obstetrics, colposcopy and female<br />
sexual dysfunction.<br />
Brenda Roy, MD<br />
BS: Queen’s <strong>University</strong>, Ontario, Canada<br />
MD: <strong>University</strong> of Toronto, Ontario, Canada<br />
Ob/Gyn Residency: McGill <strong>University</strong>, Quebec, Canada<br />
Dr. Brenda Roy joined the Division of Emergency Obstetrics and Gynecology as<br />
a part time attending physician in September 2008. Trained in Canada, Dr. Roy has an inter-<br />
est in laparoscopic and robotic surgery, and is also involved in a training program with a local<br />
private physician to hone her surgical skills. She is appointed as a Clinical Assistant Professor<br />
of Obstetrics and Gynecology, Warren Alpert Medical School.<br />
Amy Laura Snyder, MD<br />
BA: <strong>University</strong> of Michigan<br />
MD: <strong>University</strong> of Connecticut<br />
Ob/Gyn Residency: <strong>University</strong> of Connecticut Health Center & Hartford Hospital<br />
Dr Amy Snyder, a Fellow of the American College of Obstetrics and Gynecology,<br />
comes to the division of Emergency Obstetrics and Gynecology from a private practice in West<br />
Hartford, CT. Certified through the American Institute for Ultrasound in Medicine, she is also an<br />
active participant in the clinic coverage system.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Roxanne Vrees, MD<br />
BA: <strong>Brown</strong> <strong>University</strong><br />
MD: <strong>Brown</strong> <strong>University</strong><br />
Ob/Gyn Residency: Women & Infants Hospital of Rhode Island<br />
Dr. Roxanne Vrees came to the Division of Emergency Obstetrics and Gynecology<br />
as an attending in September 2008 after practicing with a local physician group since complet-<br />
ing her residency. As a graduate of the Women & Infants residency program, Roxanne brings<br />
a keen understanding of the day to day activities of the residency and how to best integrate<br />
teaching into the hectic pace of an emergency room. She is an active participant in the Clinic<br />
Attending Service and member of the Medical Records Task Force.<br />
Emily White, MD<br />
BS: George Washington <strong>University</strong><br />
MD: State <strong>University</strong> of NY at Brooklyn College of Medicine<br />
MPH: Columbia <strong>University</strong><br />
Ob/Gyn Residency: Women & Infants Hospital of Rhode Island<br />
Dr. Emily White joined the Division of Emergency Obstetrics and Gynecology<br />
in October 2009 after working in private practice in New York for two years. A Fellow of the<br />
American College of Obstetricians and Gynecologists, Dr. White returns to Women and Infants<br />
with an interest in quality improvement and organizational efficiency. As a graduate of the<br />
residency program here, she brings an in-depth understanding of the role of residents in the<br />
Emergency/Triage area and will focus on improved efficiency in patient flow and documenta-<br />
tion. Dr. White is also an active participant in the Clinic Attending Service.<br />
The Triage unit is the operating unit of the Division of Emergency Obstetrics and Gynecology,<br />
the only division of this type in the nation. The primary goal is to provide acute care for obstet-<br />
rical and gynecologic urgent and emergent problems, 24 hours each day, 7 days a week. The<br />
facilities include 12 exam rooms with capacity to care for obstetric and gynecologic patients.<br />
The increase in the number of attending physicians has had a major positive impact on the ef-<br />
ficiency of care provided in the unit and has expanded the teaching opportunities to 24/7. The<br />
Emergency Ob/Gyn Unit provides teaching rotations in emergency obstetric and gynecologic<br />
care to residents and fellows from Kent Hospital Emergency Medicine Residency, Rhode Island<br />
Hospital Emergency Medicine Residency, and Rhode Island Pediatric Medicine Fellowship, as<br />
well as <strong>Brown</strong> medical students. Plans are underway to expand patient care space and to im-<br />
prove patient flow through the unit.<br />
The Triage unit provides state-of-the-art ultrasound equipment and collaborates with radiol-<br />
ogy for other needed radiologic procedures. The Triage unit works in collaboration with other<br />
hospital clinical care units including labor and delivery, antepartum units, operating room, and<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 121<br />
E m e r g e n c y O b / G y n
E m e r g e n c y O b / G y n<br />
in-patient gynecology floors. The triage team also facilitates follow-up for patients seen in the<br />
unit to their primary physicians.<br />
The Triage unit saw 30,006 in fiscal year 2007; 30,544 in fiscal year 2008; and 28,925 in fiscal<br />
year 2009. Recent initiatives include the introduction of Sepsis, Stroke, Chest Pain and DKA<br />
protocols, dedicated attending coverage 24/7, and the implementation of an Automatic Urine<br />
Reflux plan which has greatly reduced the number of patients returning with worsening uri-<br />
nary symptoms.<br />
122<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
MISSION<br />
NURSE MIDWIFERY<br />
To support the educational goals of <strong>Brown</strong> <strong>University</strong> medical students and obstetric residents<br />
at Women & Infants Hospital (WIH) of Rhode Island regarding basic knowledge and skill acqui-<br />
sition in both obstetric triage and low–risk intrapartum services.<br />
To augment the clinical services provided by obstetric residents within the Department of Ob/<br />
Gyn by providing timely and expert care within the obstetric service, i.e., labor–delivery, oper-<br />
ating room, obstetric triage and gestational diabetic clinic.<br />
To advance the academic preeminence of the Department of Ob/Gyn by participating in<br />
national and international presentations, as well as publications and research projects<br />
advancing the specialty of midwifery.<br />
FACULTY<br />
Diane J. Angelini, EdD CNM FACNM FAAN, Director<br />
Clinical Associate Professor<br />
EdD: Boston <strong>University</strong><br />
CNM: State <strong>University</strong> of New York at Downstate<br />
MSN: <strong>University</strong> of Pittsburgh<br />
BSN: Fitchburg State College<br />
Diane served as Director of both the midwifery practice and educational<br />
programs at LA County–USC for five years as well as the Director of Mid-<br />
wifery at Brigham and Women’s Hospital in her role as Nursing Administrator. She was Interim<br />
Director for the <strong>University</strong> of RI Nurse Midwifery Educational Program from 1993–1994. She<br />
has edited two books and published numerous articles. She is Senior Editor for the Journal of<br />
Perinatal and Neonatal Nursing and Associate Editor, Journal Watch Women’s Health Journal.<br />
She is a reviewer for the Journal of Midwifery and Women’s Health and served as Educational<br />
Consultant for the same journal from 1998-2007. She is recertified as a Nurse Executive Ad-<br />
vanced (NEA-BC). She was elected a Fellow to both the American College of Nurse Midwives<br />
and the American Academy of Nursing. She has 34 years midwifery experience.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 123<br />
N u r s e M i d w i f e r y
N u r s e M i d w i f e r y<br />
124<br />
Elisabeth D. Howard, PhD, CNM<br />
Clinical Assistant Professor<br />
PhD: Vanderbilt <strong>University</strong><br />
CNM: Yale <strong>University</strong><br />
MSN: Yale <strong>University</strong><br />
BA: William Smith College (New York)<br />
From 1985 to 1988, Liz worked as Information Coordinator, Counselor in Family Planning and<br />
Director of Family Health Education. From 1991 to 1995, she worked as a Nurse Midwife at<br />
Parkland Memorial Hospital in Texas, Martin Luther King, Jr. Family Clinic in Texas and Ma-<br />
ternal Infant Care Project in Tennessee. From 1995 to June 2004, she served as Instructor and<br />
Midwifery Practice Director at Vanderbilt <strong>University</strong> School of Nursing in Nashville, Tennessee.<br />
Liz is a reviewer for the Journal of Midwifery and Women’s Health. She serves as the American<br />
College of Nurse-Midwives’ delegate for the National Quality Forum. Currently, she is special<br />
guest editor for the Journal of Perinatal and Neonatal Nursing’s forthcoming issue on perinatal<br />
bereavement. She has 19 years midwifery experience.<br />
Linda Hunter, EdD, CNM<br />
Clinical Assistant Professor<br />
EdD: <strong>University</strong> of Vermont<br />
CNM: <strong>University</strong> of RI<br />
MS: <strong>University</strong> or RI<br />
BS: <strong>University</strong> of RI; BA: Mohegan Community College<br />
From 1982 to 1995 Linda worked as an RN in the emergency room, labor and delivery and as a<br />
staff educator at WIH. Since receiving her master’s degree, she has worked in a private practice<br />
in New London Connecticut for 7 years and then joined the faculty practice of the <strong>University</strong> of<br />
Vermont. From 2002 to 2007, Linda worked in a hospital based nurse-midwifery practice and<br />
held faculty appointments in the College of Medicine the College of Nursing and Health Sci-<br />
ences, where she remains an Adjunct Instructor. She is a peer reviewer for both the Journal<br />
of Midwifery and Women’s Health and the Journal of Obstetric, Gynecologic, and Neonatal<br />
Nursing. She actively participated in the classroom and clinical education of nursing and medi-<br />
cal students and has lectured extensively on a variety of women’s health topics. Linda has 15<br />
years midwifery experience.<br />
Edie P. McConaughey, MSN, CNM<br />
Senior Clinical Teaching Associate<br />
MS: <strong>University</strong> of RI; CNM: <strong>University</strong> of RI<br />
BS: <strong>University</strong> of RI; BA: <strong>University</strong> of RI<br />
Edie worked at Women and Infants’ Hospital, prior to her midwifery experience,<br />
where she was responsible for nursing staff education for both Labor and Deliv-<br />
ery and High Risk Antepartum Units. Her midwifery experience includes working in RI for both<br />
a large HMO OB/Gyn group and a private OB/Gyn practice for a total of seven years. In these<br />
settings, she was involved with the clinical education of both midwifery and medical students.<br />
Edie is a peer reviewer for the Journal of Midwifery and Women’s Health. She has 15 years<br />
midwifery experience.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
Janet E. Singer, MSN, CNM<br />
Senior Clinical Teaching Associate<br />
MSN: Yale <strong>University</strong><br />
CNM: Yale <strong>University</strong><br />
BSN: Columbia <strong>University</strong><br />
BA: Harvard College<br />
For six years, Janet was a nurse midwife in private midwifery practice in the Greater Boston<br />
area, where she was involved in the education of midwifery and medical students, as well as<br />
family practice residents. Janet serves as President of the Board of the Abortion Access Proj-<br />
ect. She lectures widely on issues surrounding abortion care. She has worked for IPAS on a<br />
project providing Technical Assistance and Mentoring to hospitals interested in offering outpa-<br />
tient management of early pregnancy loss and/or abortion to their patients. As Senior Clinical<br />
Advisor to the Women’s Dignity Project, she has assisted in research on vesico-vaginal fistula<br />
in women from Tanzania. Janet has been appointed Assistant Core Clerkship Director of Mid-<br />
wifery Didactics at Women & Infants’ Hospital. Janet is a reviewer for the Journal of Midwifery<br />
and Women’s Health. She has 19 years midwifery experience.<br />
Linda Steinhardt, MS, CNM, FNP–C<br />
Senior Clinical Teaching Associate<br />
Post Master’s Certificate in Teaching. <strong>University</strong> of Pennsylvania<br />
MS: Pace <strong>University</strong><br />
CNM: <strong>University</strong> of Medicine and Dentistry of New Jersey<br />
FNP–C: Pace <strong>University</strong>; BA: Bard College<br />
Linda was a Family Nurse Practitioner for nine years at St. Luke’s/Roosevelt Hospital and in the<br />
Student Health Services at the Fashion Institute of Technology in NYC. In 1991, she continued<br />
her education as a CNM. She has worked as a CNM at St. Luke’s/Roosevelt Hospital and the<br />
Bronx Municipal Hospital Center in New York City, and as faculty at UMDNJ/St. Mary Hospital<br />
Center Family Practice Residency program in New Jersey. For the three years prior to coming<br />
to <strong>Brown</strong>, Linda was in private practice as a CNM affiliated with St. Vincent’s Medical Center<br />
in NYC. Linda coordinates the midwifery gestational diabetic (GDM) clinic. She has 20 years<br />
midwifery experience.<br />
Sylvia Ross, MSN, CNM<br />
MSN: <strong>University</strong> of Pennsylvania<br />
CNM: <strong>University</strong> of Pennsylvania<br />
BSN: <strong>University</strong> of New Hampshire<br />
Sylvia worked in the Midwifery section at WIH from 1993 to 1996 and then again<br />
recently joined the group in March of 2010. Currently, Sylvia is a PhD student at<br />
the <strong>University</strong> of Rhode Island. Her interest is in interprofessional clinical education. Since re-<br />
ceiving her midwifery degree, Sylvia has been in private OB/GYN practice in Rhode Island and<br />
is currently on the faculty at Rhode Island College School of Nursing as an Assistant Professor.<br />
Sylvia has 16 years midwifery experience.<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 125<br />
N u r s e M i d w i f e r y
N u r s e M i d w i f e r y<br />
CLINICAL ACTIVITIES<br />
Inpatient Service: Labor and Delivery<br />
Midwifery faculty provide clinical management, consultation and teaching in labor and deliv-<br />
ery Monday through Friday. Consultation and supervision are provided for medical students<br />
and obstetric residents in the clinic management of labor and delivery on the low risk obstetric<br />
service. Midwifery faculty provide direct clinical services to women by sharing in the care of all<br />
women presenting in labor on the low–risk obstetric service.<br />
Inpatient Service: OR 1st Assist — C-Sections<br />
Two midwifery faculty are credentialed to function as first-assistants in the operating room for<br />
C-Sections. This expanded midwifery role provides for part time 1st assist coverage during<br />
the week (for assistance with primary and repeat cesarean sections). Two 4 hour sessions are<br />
covered weekly by midwives for 1st assist.<br />
Inpatient Service: Postpartum Rounds<br />
Starting in May 2010, midwifery faculty are now the attending provider, rounding on all clinic<br />
patients in the low-risk obstetric service, Monday – Friday.<br />
Ambulatory Service: Obstetric Triage<br />
Midwifery faculty staff the obstetric triage unit, caring for women who primarily present with<br />
obstetric complaints. They provide direct clinical care to pregnant women and provide clinical<br />
teaching to obstetric interns and Rhode Island Hospital (RIH) Emergency Room residents. They<br />
assist PGY–1 residents in the acquisition of various skills including: use of the microscope,<br />
sterile speculum and vaginal exams, fetal assessment, limited sonography (including amniotic<br />
fluid index, biophysical profile, biometry), Leopold’s maneuvers, and evaluation of women<br />
with preterm labor, bleeding, pre–eclampsia, post–term pregnancy, bleeding and intrauterine<br />
growth restriction as well as other obstetric complaints.<br />
Ambulatory Service: Gestational Diabetic (GDM) Clinic<br />
Every Tuesday afternoon, GDM clinic is staffed by one midwifery faculty member with Mater-<br />
nal Fetal Medicine (MFM) consultation available. This clinic is a referral clinic for antepartum<br />
GDM patients from Women & Infants Hospital and from Providence Health Centers. Midwives<br />
work collaboratively with MFM in this setting.<br />
MIDWIFERY PRODUCTIVITY STATISTICS<br />
126<br />
FY 2008 FY 2009 FY 2010<br />
Births 334 334 265<br />
OB Triage Visits 3334 3359 2162<br />
1st Assist C-Sections 28 15 42<br />
Gestational Diabetic Clinic Visits 417 428 318<br />
*Inpatient Postpartum Visits — — 507<br />
*Initiated May 2010<br />
(completed thru June 2010)<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
TEACHING RESPONSIBILITIES<br />
Medical Students<br />
The midwifery faculty assist in core clinical education for third year medical students from<br />
<strong>Brown</strong> Medical School. These students perform history and physical exams, and participate in<br />
labor and birth experiences under the guidance of the midwifery faculty. Simulations for episi-<br />
otomy and laceration repair, mechanisms of labor and hand maneuvers for delivery to enhance<br />
skill acquisition are practiced while on the labor unit. This is in preparation for actual experi-<br />
ences with patients as well as to prepare for the OSCE skill stations at the end of the rotation<br />
in which the midwives participate as proctors. Six hours of lecture time are provided by the<br />
CNMs during the six–week rotation. Midwives are responsible for approximately 3–5 medical<br />
students per week on labor and delivery.<br />
OB/GYN Residents<br />
During the eight weeks the PGY-1 residents are on the low risk OB service, midwifery faculty<br />
assist them with labor management, birth experiences, procedural skills, use of local and<br />
pudendal anesthesia, episiotomy and laceration repair and verify accuracy of vaginal examina-<br />
tions. At the completion of approximately 30 births, each PGY-1 resident is assessed for com-<br />
petency with: hand maneuvers for delivery, episiotomy/laceration and repair and accuracy of<br />
vaginal examinations. They are assessed for competency with basic ultrasound skills as well as<br />
with selected clinical scenarios in the triage setting. Numerous educational workshops are held<br />
yearly for residents by the midwifery faculty.<br />
Midwifery faculty serve as primary consultants for the PGY-2 experiences during their labor<br />
and delivery rotation. Expanded suturing and clinical decision making skills are emphasized,<br />
along with a specific reading list.<br />
MIDWIFERY / RESIDENT WORKSHOPS<br />
PGY–1 Workshop<br />
The PGY-1 Resident Orientation is a full day program given to all PGY-1 interns at the begin-<br />
ning of residency. The content consists of intrapartum seminars and skill sessions addressing<br />
clinical dexterity and beginning level clinical management of pregnant women in labor and<br />
delivery. The skill and simulation sessions include: abdominal assessment, vaginal exams, rup-<br />
ture of membranes, prolapsed cord, use of fetal scalp electrode, intrauterine pressure catheter,<br />
amnioinfusion, electronic fetal monitoring, local anesthesia, cutting and repair of episiotomy/<br />
lacerations, hand maneuvers for birth (including management of nuchal cord, meconium and<br />
shoulder dystocia), third stage management and postpartum hemorrhage.<br />
PGY–2 Advanced Skills Workshop<br />
An advanced clinical skills workshop for the PGY-2 residents is conducted each year. This<br />
advanced skills workshop covers a case based approach to fetal heart rate (FHR) monitoring<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 127<br />
N u r s e M i d w i f e r y
N u r s e M i d w i f e r y<br />
and advanced interpretation of FHR strips, as well as clinical management of non–reassuring<br />
FHR tracings. The workshop also covers shoulder dystocia, postpartum hemorrhage, alterna-<br />
tive birthing positions, and principles of effective clinical teaching in the birth setting. Clinically,<br />
midwives are available on labor and delivery to review labor management and clinical deci-<br />
sion–making with PGY-2 residents.<br />
PGY–3 Workshop<br />
This advanced skills workshop is a collaborative effort between Midwifery and the Uro–Gyn Di-<br />
vision under Dr. Deb Myers. A clinical simulation lab is set up to demonstrate repair of medio-<br />
lateral episiotomy, as well as 3rd and 4th degree laceration repair. Didactic material on perineal<br />
anatomy and physiology is provided.<br />
PGY-4 Workshop for New Leaders<br />
This is a 2½ hour workshop focusing on leadership skills for chief residents. This workshop is<br />
guided by the SynecticsTM process of using creative problem solving techniques. Leadership<br />
scenarios are included in the workshop to role play leadership issues commonly encountered<br />
by chief residents in their leadership role. Follow-up on leadership aspects are reviewed with<br />
all new obstetric chief residents during their senior rotation as low-risk OB chief.<br />
RIH – ER Resident Workshop<br />
In collaboration with the RIH Emergency Department, the midwives have continued to develop<br />
and coordinate educational training experiences for the ED residents’ in managing selected<br />
obstetric emergencies. This year, the midwifery faculty will be providing a didactic<br />
and practicum training session for the ED interns focusing on pelvic exam techniques and<br />
specimen collection for selected obstetric and gynecology clinical scenarios. Using standard-<br />
ized patients, this session will also help prepare the ED interns for their upcoming clinical rota-<br />
tions at WIH.<br />
RESIDENT MENTORING PROGRAM<br />
PGY-1 Mentoring Program<br />
Each June, midwifery faculty assume the role of mentors for the incoming PGY-1 residents.<br />
Each new resident is assigned a midwife faculty person during the first year. The faculty meets<br />
with him/her on a regular basis tracking clinical experiences and adjustments to the resident<br />
role, especially while rotating on the low–risk obstetric service. Obstetric noon conferences for<br />
interns are coordinated through the midwifery faculty preceptor who assumes responsibility<br />
for assisting interns with noon conference planning and presentation skills.<br />
128<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
EDUCATIONAL ACTIVITIES<br />
Midwives are actively involved in multiple educational activities with medical student and resi-<br />
dent education. These include the following:<br />
Diane J. Angelini:<br />
Resident Core Curriculum Lecture: “Management of Shoulder Dystocia”<br />
Core Clerkship Lecture: “Intrapartum I and II”<br />
Coordinator: PGY–3 Workshop<br />
Participating Workshop Faculty: PGY–1, PGY–3<br />
Elisabeth D. Howard:<br />
Resident Core Curriculum Lecture: “First Stage Labor Management”<br />
Core Clerkship Lecture: “Intrapartum I and II”<br />
Core Clerkship Lecture: “Electronic Fetal Monitoring: The Basics”<br />
Coordinator: PGY–2 Workshop<br />
Participating Workshop Faculty: PGY–1, PGY–2, RIH ED Resident Workshop<br />
Linda A. Hunter:<br />
Resident Core Curriculum Lecture: “Analgesia and Anesthesia in Labor.”<br />
Core Clerkship Lecture “Intrapartum I and II”<br />
Core Clerkship Lecture “Electronic Fetal Monitoring: Basics”<br />
Coordinator: RIH ED Resident Workshop<br />
Participating Workshop Faculty: PGY-1, PGY-2, RIH ED Resident Workshop<br />
Credentialed 1st Assist C-Sections<br />
Edie McConaughey:<br />
Resident Core Curriculum Lecture: “Third Stage Labor” and “Complex Fetal Monitoring Cases”<br />
Core Clerkship Lecture “Intrapartum I and II”<br />
Core Clerkship Lecture “Electronic Fetal Monitoring: The Basics”<br />
Midwifery Faculty, Gestational Diabetic Clinic – with MFM Division<br />
Coordinator: PGY–1 Workshop<br />
Participating Workshop Faculty: PGY–1, Workshop for New Leaders<br />
Credentialed 1st Assist C-Sections<br />
Janet E. Singer:<br />
Resident Core Curriculum Lecture: “Surviving a Malpractice Trial”<br />
Core Clerkship Lecture: “Termination of Pregnancy”<br />
Core Clerkship Lecture “Intrapartum I and II”<br />
Participating Workshop Faculty: PGY–1, PGY–2, Workshop for New Leaders<br />
(continued)<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 129<br />
N u r s e M i d w i f e r y
N u r s e M i d w i f e r y<br />
Linda A. Steinhardt:<br />
Resident Core Curriculum Lecture: “Second Stage Labor”<br />
Core Clerkship Lecture “Intrapartum I and II”<br />
Midwifery Faculty Coordinator, Gestational Diabetic Clinic – Tuesday PM with MFM Division<br />
Coordinator: Workshop for New Leaders<br />
Participating Workshop Faculty: PGY–1, Workshop for New Leaders<br />
Sylvia P. Ross:<br />
Core Clerkship Lecture: “Intrapartum I and II”<br />
Participating Workshop Faculty: PGY-1<br />
130<br />
HONORS/AWARDS<br />
Angelini: Guest Editor, Journal of Midwifery and Women’s Health, 2009<br />
Hunter: Reappointed Peer Reviewer, Journal of Midwifery and Women’s Health, 2009<br />
Singer: Appointed to Senior Clinical Teaching Associate, 2009<br />
McConaughey: Nurse Faculty of the Year Award, 2010<br />
Howard: Nurse Faculty of the Year Award, 2010<br />
NATIONAL PRESENTATIONS<br />
Hunter L. Invited Speaker, “Women’s Health Care within an Inclusive Gender Model”<br />
“Reducing Inappropriate Inductions of Labor” American College of Nurse Midwives (ACNM)<br />
55 th <strong>Annual</strong> Meeting Washington, DC, June 2010.<br />
Ross S. Invited Speaker “Paving the Path: Midwives Teaching Nursing at the Baccalaureate<br />
Level” American College of Nurse Midwives (ACNM) 55th <strong>Annual</strong> Meeting, Washington, DC,<br />
June 2010.<br />
Singer J. Invited Speaker “Caring for Families with Fetal and Neonatal Loss” and<br />
“Bleeding in Pregnancy” Massachusetts Nursing Association, Lawrence, MA , May 2010.<br />
Angelini D. Invited Speaker “Safety Parameters in OB Triage”, “Triage Case Studies”,<br />
“Delivery Complications” 27 th <strong>Annual</strong> Obstetric Nursing Conference, Las Vegas, NV, April 2010.<br />
Howard, E. Invited Speaker “Preconceptual Counseling and “Management of Perinatal<br />
Depression and Substance Abuse and Depression” St. Thomas Hospital Risk Management<br />
Conference, Nashville, TN - 2009.<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
LOCAL PRESENTATIONS<br />
Steinhardt L, McConaughey E, Hunter L. Invited Speakers “Developing a Workshop for New<br />
Leaders” Breakout Session, Warren Alpert Medical School of <strong>Brown</strong> <strong>University</strong> Clinical Faculty<br />
Workshop, Women and Infants’ Hospital, April 2010.<br />
INTERNATIONAL PRESENTATIONS<br />
McConaughey E. Invited Speaker “Midwives as Educators of Medical Students and Residents:<br />
Results of a National Survey” 29 th <strong>Annual</strong> International Nursing and Midwifery Research<br />
Conference, Royal College of Surgeons in Ireland, Dublin, Ireland, February 2010.<br />
PUBLICATIONS<br />
McConaughey E, Howard E. Nurse Midwifery and Medical Education: Results of a National<br />
Survey. Journal of Midwifery and Women’s Health. 2009; 54: 268-274.<br />
Hunter L, Angelini D, Singer J. Levonorgestrel Emergency Contraception: An Update for<br />
Providers. Sexuality, Reproduction and Menopause. 2009; 7 (4): Available from<br />
http://www.srm-ejournal.com/article.asp?AID=8002.<br />
Angelini D. A National Survey of the Midwifery Directors Role in Academic Midwifery<br />
Practice Involved in Medical Education in the US. Journal of Midwifery and Women’s<br />
Health. 2009; 54 (4): 275-281.<br />
Angelini D, Stevens E, MacDonald A, Wiener S, Wieczorek B. Obstetric Triage: Models and<br />
Trends in Resident Education by Midwives. Journal of Midwifery and Women’s Health.<br />
2009; 54 (4): 294-300.<br />
OTHER<br />
Howard E, McConaughey E. “Midwives as Educators of Medical Students and Residents:<br />
Results of a National Survey.” 2009. ReachMD – Podcast Interview. The Channel for<br />
Medical Professionals. Available: http://reachmd.com.<br />
Howard E. “Midwives in Medicine”. Providence Business News. 2010.<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 131<br />
N u r s e M i d w i f e r y
G r a n d R o u n d s<br />
132<br />
WOMEN & INFANTS HOSPITAL OF RHODE ISLAND<br />
OB/GYN GRAND ROUNDS SCHEDULE 2009-2010<br />
July 2009<br />
9 Peter Rosenblatt, MD<br />
Current and Future Treatments for Fecal Incontinence<br />
16 Brenna Anderson, MD<br />
Hot Topics in Reproductive Infectious Disease<br />
30 Stephan Krotz, MD<br />
Ovarian Aging and Fertility<br />
August 2009<br />
13 Nicole Korbly, MD<br />
Cesarean Scar Pregnancy<br />
Jennifer Kang, MD<br />
Alcohol Use and Abuse in Pregnancy<br />
27 Kyle Wohlrab, MD<br />
Complications in Urogynecologic Surgery<br />
September 2009<br />
3 Eve Espey, MD<br />
Strike While the Iron is Hot: Postpartum and Postabortal Contraception<br />
10 Stephan Rubin, MD<br />
Hereditary Ovarian Cancer: Molecular Genetics and Clinical Implications<br />
17 Donna LaFontaine, MD<br />
Some Observations on the Practice of Obstetrics/Gynecology in Kosovo<br />
October 2009<br />
1 Colleen Pelletier<br />
Surgical Consent<br />
8 Stephen Bogdewic, PhD<br />
Organizational Culture: The Key to Success<br />
15 Roxanne Gardner, MD<br />
Forming Your Hands for Practice:<br />
The Role of Simulation in Obstetrics and Gynecology<br />
November 2009<br />
5 Brenna Anderson, MD<br />
Update on Pandemic Influenza<br />
Aine Clements, MD<br />
Updates in Ovarian Torsion<br />
12 Nils Bergman, MD<br />
Perinatal Neuroscience and Skin-to-Skin Contact”<br />
D e p a r t m e n t o f O b s t e t r i c s & G y n e c o l o g y
December 2009<br />
3 Julie Johnson, MD<br />
Thrombophilia and Pregnancy<br />
January 2010<br />
7 Raymond Powrie, MD<br />
Medical Causes of Maternal Mortality and What to do About Them<br />
14 Agatha Critchfield, MD<br />
Pitocin Protocols<br />
Katherine Melzer, MD<br />
Bariatric Surgery: Impact on Fertility, Contraception and Pregnancy<br />
28 Brenna Anderson, James A. O’Brien, MD, Raymond Powrie, MD<br />
New Protocols for Postpartum Hemorrhage; New Protocols for Anticoagulation<br />
February 2010<br />
4 Peter Klatsky, MD<br />
Uterine Fibroids and Reproductive Outcomes: From Implantation to Delivery<br />
March 2010<br />
4 Katharine Wenstrom, MD<br />
The Fetal Origins of Adult Disease – Why Obstetrics is the Most Important Specialty<br />
11 Gary Frishman, MD<br />
Hysteroscopy from the Office to the Operating Room<br />
25 Beth Cronin, MD and Laura Richio, MD<br />
Robotics in Gynecologic Surgery: A Debate<br />
April 2010<br />
1 Gregory Dubel, MD<br />
Uterine Artery Embolization for Symptomatic Fibroids: Where Do We Stand in 2010?<br />
8 John Buster, MD<br />
Two Million Babies, 30 Years…What is Next in Reproductive Medicine?<br />
May 2010<br />
6 Lori Boardman, MD<br />
Contemporary Management of the Pap Test: Navigating Practice Guidelines<br />
20 Charles Rardin, MD<br />
Update in Minimally-Invasive Urogynecology<br />
27 Susan Cu-Uvin, MD<br />
<strong>Brown</strong> and the World: Engaging HIV-Infected Women<br />
June 2010<br />
3 Ashley Stuckey, MD<br />
Breast Cancer Screening<br />
10 Jo Shapiro, MD<br />
Apology and Disclosure<br />
A n n u a l R e p o r t 2 0 0 9 – 2 0 1 0 133<br />
G r a n d R o u n d s