Advanced Trauma Life Support ATLS Student Course Manual 2018
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
CIRCULATION AND SHOCK 195<br />
breathing<br />
A key factor in evaluating and managing breathing<br />
and ventilation in injured pediatric trauma patients<br />
is the recognition of impaired gas exchange. This<br />
includes oxygenation and elimination of carbon<br />
dioxide resulting from alterations of breathing caused<br />
by mechanical issues such as pneumothorax and lung<br />
injury from contusion or aspiration. In such cases,<br />
apply appropriate countermeasures such as tube<br />
thoracostomy and assisted ventilation.<br />
Breathing and Ventilation<br />
The respiratory rate in children decreases with age. An<br />
infant breathes 30 to 40 times per minute, whereas an<br />
older child breathes 15 to 20 times per minute. Normal,<br />
spontaneous tidal volumes vary from 4 to 6 mL/kg<br />
for infants and children, although slightly larger tidal<br />
volumes of 6 to 8 mL/kg and occasionally as high as<br />
10 mL/kg may be required during assisted ventilation.<br />
Although most bag-mask devices used with pediatric<br />
patients are designed to limit the pressure exerted<br />
manually on the child’s airway, excessive volume<br />
or pressure during assisted ventilation substantially<br />
increases the potential for iatrogenic barotrauma due<br />
to the fragile nature of the immature tracheobronchial<br />
tree and alveoli. When an adult bag-mask device is used<br />
to ventilate a pediatric patient, the risk of barotrauma<br />
is significantly increased. Use of a pediatric bag-mask<br />
is recommended for children under 30 kg.<br />
Hypoxia is the most common cause of pediatric<br />
cardiac arrest. However, before cardiac arrest occurs,<br />
hypoventilation causes respiratory acidosis, which is<br />
the most common acid-base abnormality encountered<br />
during the resuscitation of injured children. With<br />
adequate ventilation and perfusion, a child should be<br />
able to maintain relatively normal pH. In the absence<br />
of adequate ventilation and perfusion, attempting<br />
to correct an acidosis with sodium bicarbonate can<br />
result in further hypercarbia and worsened acidosis.<br />
over-the-needle catheters in infants and small children,<br />
as the longer needle length may cause rather than cure<br />
a tension pneumothorax.<br />
Chest tubes need to be proportionally smaller (see<br />
n TABLE 10-3) and are placed into the thoracic cavity by<br />
tunneling the tube over the rib above the skin incision<br />
site and then directing it superiorly and posteriorly<br />
along the inside of the chest wall. Tunneling is especially<br />
important in children because of their thinner chest<br />
wall. The site of chest tube insertion is the same in<br />
children as in adults: the fifth intercostal space, just<br />
anterior to the midaxillary line. (See Chapter 4: Thoracic<br />
<strong>Trauma</strong>, and Appendix G: Breathing Skills.)<br />
Circulation and Shock<br />
Key factors in evaluating and managing circulation<br />
in pediatric trauma patients include recognizing<br />
circulatory compromise, accurately determining the<br />
patient’s weight and circulatory volume, obtaining<br />
venous access, administering resuscitation fluids<br />
and/or blood replacement, assessing the adequacy of<br />
resuscitation, and achieving thermoregulation.<br />
Recognition of Circulatory<br />
Compromise<br />
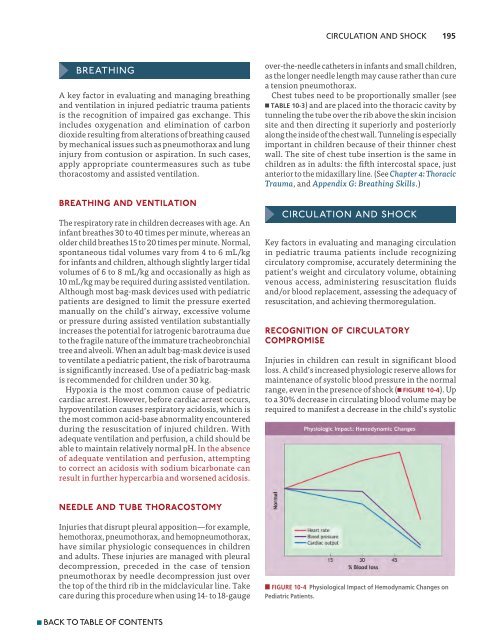
Injuries in children can result in significant blood<br />
loss. A child’s increased physiologic reserve allows for<br />
maintenance of systolic blood pressure in the normal<br />
range, even in the presence of shock (n FIGURE 10-4). Up<br />
to a 30% decrease in circulating blood volume may be<br />
required to manifest a decrease in the child’s systolic<br />
Needle and Tube Thoracostomy<br />
Injuries that disrupt pleural apposition—for example,<br />
hemothorax, pneumothorax, and hemopneumothorax,<br />
have similar physiologic consequences in children<br />
and adults. These injuries are managed with pleural<br />
decompression, preceded in the case of tension<br />
pneumothorax by needle decompression just over<br />
the top of the third rib in the midclavicular line. Take<br />
care during this procedure when using 14- to 18-gauge<br />
n FIGURE 10-4 Physiological Impact of Hemodynamic Changes on<br />
Pediatric Patients.<br />
n BACK TO TABLE OF CONTENTS