CHORIONIC VILLUS SAMPLING
CHORIONIC VILLUS SAMPLING
CHORIONIC VILLUS SAMPLING
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
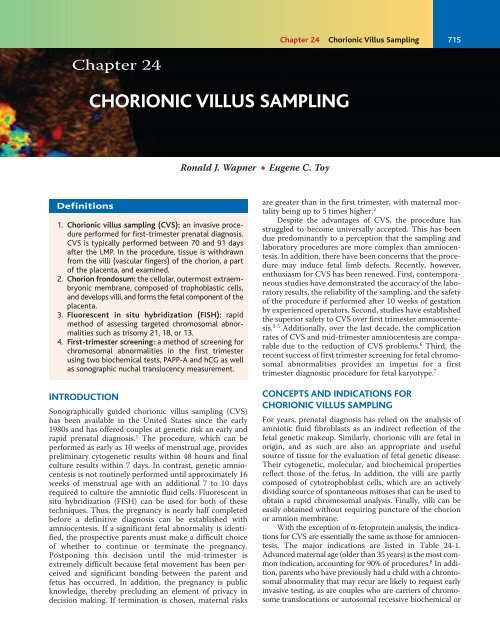
Chapter 24<br />
Definitions<br />
<strong>CHORIONIC</strong> <strong>VILLUS</strong> <strong>SAMPLING</strong><br />
1. Chorionic villus sampling (CVS): an invasive procedure<br />
performed for first-trimester prenatal diagnosis.<br />
CVS is typically performed between 70 and 91 days<br />
after the LMP. In the procedure, tissue is withdrawn<br />
from the villi (vascular fingers) of the chorion, a part<br />
of the placenta, and examined.<br />
2. Chorion frondosum: the cellular, outermost extraembryonic<br />
membrane, composed of trophoblastic cells,<br />
and develops villi, and forms the fetal component of the<br />
placenta.<br />
3. Fluorescent in situ hybridization (FISH): rapid<br />
method of assessing targeted chromosomal abnormalities<br />
such as trisomy 21, 18, or 13.<br />
4. First-trimester screening: a method of screening for<br />
chromosomal abnormalities in the first trimester<br />
using two biochemical tests, PAPP-A and hCG as well<br />
as sonographic nuchal translucency measurement.<br />
INTRODUCTION<br />
Sonographically guided chorionic villus sampling (CVS)<br />
has been available in the United States since the early<br />
1980s and has offered couples at genetic risk an early and<br />
rapid prenatal diagnosis. 1 The procedure, which can be<br />
performed as early as 10 weeks of menstrual age, provides<br />
preliminary cytogenetic results within 48 hours and final<br />
culture results within 7 days. In contrast, genetic amniocentesis<br />
is not routinely performed until approximately 16<br />
weeks of menstrual age with an additional 7 to 10 days<br />
required to culture the amniotic fluid cells. Fluorescent in<br />
situ hybridization (FISH) can be used for both of these<br />
techniques. Thus, the pregnancy is nearly half completed<br />
before a definitive diagnosis can be established with<br />
amniocentesis. If a significant fetal abnormality is identified,<br />
the prospective parents must make a difficult choice<br />
of whether to continue or terminate the pregnancy.<br />
Postponing this decision until the mid-trimester is<br />
extremely difficult because fetal movement has been perceived<br />
and significant bonding between the parent and<br />
fetus has occurred. In addition, the pregnancy is public<br />
knowledge, thereby precluding an element of privacy in<br />
decision making. If termination is chosen, maternal risks<br />
Ronald J. Wapner ● Eugene C. Toy<br />
Chapter 24 Chorionic Villus Sampling<br />
715<br />
are greater than in the first trimester, with maternal mortality<br />
being up to 5 times higher. 2<br />
Despite the advantages of CVS, the procedure has<br />
struggled to become universally accepted. This has been<br />
due predominantly to a perception that the sampling and<br />
laboratory procedures are more complex than amniocentesis.<br />
In addition, there have been concerns that the procedure<br />
may induce fetal limb defects. Recently, however,<br />
enthusiasm for CVS has been renewed. First, contemporaneous<br />
studies have demonstrated the accuracy of the laboratory<br />
results, the reliability of the sampling, and the safety<br />
of the procedure if performed after 10 weeks of gestation<br />
by experienced operators. Second, studies have established<br />
the superior safety to CVS over first trimester amniocentesis.<br />
3-5 Additionally, over the last decade, the complication<br />
rates of CVS and mid-trimester amniocentesis are comparable<br />
due to the reduction of CVS problems. 6 Third, the<br />
recent success of first trimester screening for fetal chromosomal<br />
abnormalities provides an impetus for a first<br />
trimester diagnostic procedure for fetal karyotype. 7<br />
CONCEPTS AND INDICATIONS FOR<br />
<strong>CHORIONIC</strong> <strong>VILLUS</strong> <strong>SAMPLING</strong><br />
For years, prenatal diagnosis has relied on the analysis of<br />
amniotic fluid fibroblasts as an indirect reflection of the<br />
fetal genetic makeup. Similarly, chorionic villi are fetal in<br />
origin, and as such are also an appropriate and useful<br />
source of tissue for the evaluation of fetal genetic disease.<br />
Their cytogenetic, molecular, and biochemical properties<br />
reflect those of the fetus. In addition, the villi are partly<br />
composed of cytotrophoblast cells, which are an actively<br />
dividing source of spontaneous mitoses that can be used to<br />
obtain a rapid chromosomal analysis. Finally, villi can be<br />
easily obtained without requiring puncture of the chorion<br />
or amnion membrane.<br />
With the exception of α-fetoprotein analysis, the indications<br />
for CVS are essentially the same as those for amniocentesis.<br />
The major indications are listed in Table 24-1.<br />
Advanced maternal age (older than 35 years) is the most common<br />
indication, accounting for 90% of procedures. 8 In addition,<br />
parents who have previously had a child with a chromosomal<br />
abnormality that may recur are likely to request early<br />
invasive testing, as are couples who are carriers of chromosome<br />
translocations or autosomal recessive biochemical or
716 Part 3 RISK ASSESSMENT AND THERAPY<br />
Table 24-1<br />
MAJOR INDICATIONS FOR<br />
<strong>CHORIONIC</strong> <strong>VILLUS</strong> <strong>SAMPLING</strong><br />
Maternal age: 35 years or older at estimated date of delivery<br />
Previous child with nondisjunctional chromosome abnormality<br />
Parent is carrier of balanced translocation or other chromosome<br />
disorder<br />
Both parents are carriers of autosomal recessive disease<br />
Women who are carriers of a sex-linked disease<br />
Positive first-trimester screen for trisomy 21 or 18<br />
molecular diseases. First-trimester prenatal diagnosis is often<br />
requested by women who carry sex-linked diseases because<br />
of the 50% recurrence risk in male offspring. Recently, screening<br />
for trisomies 21 and 18 in the first trimester has become<br />
possible by using a combination of biochemical analysis<br />
(pregnancy-associated plasma protein A [PAPP-A] and<br />
human chorionic gonadotropin [hCG]) and measurement of<br />
the fetal nuchal translucency. 7 If the preliminary work<br />
demonstrating almost 90% sensitivity is substantiated, a positive<br />
screen could become a major indication for CVS.<br />
HISTORY OF <strong>CHORIONIC</strong> <strong>VILLUS</strong> <strong>SAMPLING</strong><br />
First-trimester prenatal diagnosis is not a new concept.<br />
The ability to sample and analyze villus tissue was demonstrated<br />
more than 25 years ago by the Chinese who, in an<br />
attempt to develop a technique for fetal sex determination,<br />
inserted a thin catheter into the uterus guided only by tactile<br />
sensation. 9 When resistance from the gestational sac<br />
was felt, suction was applied and small pieces of villi aspirated.<br />
Although this approach seems relatively crude by<br />
today’s standards of ultrasonically guided invasive procedures,<br />
the diagnostic accuracy and low miscarriage rate<br />
demonstrated the feasibility of first-trimester sampling.<br />
In 1968, Hahnemann and Mohr attempted blind transcervical<br />
(TC) trophoblast biopsy in 12 patients using a 6mm-diameter<br />
instrument. 10 Although successful tissue<br />
culture was obtained, half of these subjects subsequently<br />
aborted. In 1973, Kullander and Sandahl used a 5-mmdiameter<br />
fiberoptic endocervoscope with biopsy forceps to<br />
perform TC CVS in patients requesting pregnancy termination.<br />
11 Although tissue culture was successful in approximately<br />
half of the cases, 2 of the subjects subsequently<br />
became septic.<br />
In 1974, Hahnemann described further experience with<br />
first-trimester prenatal diagnosis using a 2.5-mm hysteroscope<br />
and cylindrical biopsy knife. 12 Once again, significant<br />
complications, including inadvertent rupture of the amniotic<br />
sac, were encountered. By this time, the safety of midtrimester<br />
genetic amniocentesis had become well established,<br />
and further attempts at first-trimester prenatal diagnosis were<br />
temporarily abandoned in the Western hemisphere.<br />
Two technological advances occurred in the early<br />
1980s to allow reintroduction of CVS. The first of these<br />
was the development of real-time sonography, making<br />
continuous guidance possible. At the same time, sampling<br />
instruments were miniaturized and refined. In 1982, Kazy<br />
et al reported the first TC CVS performed with real-time<br />
sonographic guidance. 13 That same year, Old reported the<br />
first-trimester diagnosis of β-thalassemia major using DNA<br />
from chorionic villi obtained by sonographically guided TC<br />
aspiration with a 1.5-mm-diameter polyethylene catheter. 14<br />
Using a similar sampling technique, Brambati and Simoni<br />
diagnosed trisomy 21 at 11 weeks of gestation. 15<br />
After these preliminary reports, several CVS programs<br />
were established in both Europe and the United States,<br />
with the outcomes informally reported to a World Health<br />
Organization (WHO)-sponsored registry maintained at<br />
Jefferson Medical College. This registry and single-center<br />
reports were used to estimate the safety of CVS until 1989,<br />
when 2 prospective multicentered studies, 1 from<br />
Canada 16 and 1 from the United States, 17 were published<br />
and confirmed the safety of the procedure.<br />
<strong>CHORIONIC</strong> <strong>VILLUS</strong> <strong>SAMPLING</strong>: THE<br />
PROCEDURE<br />
Procedure-Related Anatomy (Figure 24-1)<br />
Between 9 and 12 weeks after the last menstrual period, the<br />
developing gestation does not yet fill the uterine cavity.<br />
The sac is surrounded by the thick leathery chorionic<br />
membranes within which are both the amniotic cavity and<br />
the extraembryonic coelom. The amniotic cavity contains<br />
the embryo and is enclosed by the thin, whispy, freely<br />
mobile amniotic membrane. The extraembryonic coelom<br />
is located between the amniotic and chorionic membranes,<br />
contains a tenacious mucoid-like substance, and disappears<br />
as the amniotic sac grows toward the chorion and the<br />
2 membranes become juxtaposed.<br />
Before 9 weeks, chorionic villi cover the entire outer surface<br />
of the gestational sac. As growth continues, the developing<br />
sac begins to fill the uterine cavity, and most villi regress<br />
except at the implantation site, where they are associated with<br />
the decidua basalis (see Figure 24-1). Villi in this area rapidly<br />
proliferate to form the chorion frondosum, or fetal component<br />
of the placenta. Between 9 and 12 weeks of gestation, the<br />
villi float freely within the blood of the intervillus space and<br />
are only loosely anchored to the underlying decidua basalis.<br />
Sampling Techniques<br />
Sampling by CVS is generally performed between 70 and 91 days<br />
after the last menstrual period. This window is chosen to minimize<br />
the background spontaneous miscarriage rate that is higher<br />
in early pregnancy, yet still allows sufficient time for results to be<br />
available within the first trimester. The chorion frondosum is<br />
easily localized by ultrasound as a hyperechoic homogeneous<br />
area by this gestational age (Figure 24-2). In addition, fusion of<br />
the amnion and chorion has not yet occurred, thereby decreasing<br />
the risk of amnion rupture during the procedure. Sampling<br />
significantly earlier in gestation may be associated with an<br />
increased risk of fetal abnormalities and should not routinely be<br />
done. 18 Transcervical sampling may be more difficult after 12<br />
weeks of menstrual age due to the increasing distance between<br />
the cervix and placental site as uterine growth continues.<br />
Chorionic villus sampling can be performed by either<br />
the TC or the transabdominal (TA) approach (Figure 24-3).<br />
The techniques are equally safe and efficacious, and the<br />
majority of patients can be sampled by either technique. 19 In
Extraembryonic<br />
border<br />
Amniotic<br />
membrane<br />
most cases, physician or patient preference will dictate<br />
which approach is used; however, in approximately 3% to<br />
5% of patients, clinical circumstances will support one<br />
approach over the other (Table 24-2) requiring operators to<br />
be proficient in both. 19,20 Transcervical CVS is preferred<br />
when the placenta is located on the posterior uterine wall,<br />
whereas TA sampling is particularly useful when the placenta<br />
is implanted in a fundal or high anterior location.<br />
Transcervical sampling has the advantage of minimal<br />
patient discomfort but is somewhat more difficult to learn. 21<br />
Both approaches are best performed by using a 2-person<br />
technique, with one individual performing the sampling and<br />
the other guiding the ultrasound. Communication between<br />
the sonographer and sampler is imperative, and the best<br />
results have come from centers in which a limited number<br />
of samplers and sonographers perform CVS.<br />
Figure 24-2. Sonogram at 10.8 weeks of gestation. The chorion frondosum<br />
(placenta) is located posteriorly and appears as a homogeneous<br />
hyperechoic area.<br />
Yolk sac<br />
Chorion laeve<br />
A<br />
Chapter 24 Chorionic Villus Sampling<br />
Chorion frondosum<br />
20 cc syringe<br />
with 5 cc RPMI<br />
Tenaculum<br />
(optional)<br />
Deciduous border<br />
Figure 24-1. Diagram of first-trimester pregnancy illustrating relevant anatomic landmarks.<br />
3.5 mHz sector transducer<br />
with biopsy guide<br />
Transabdominal chorionic villus sampling<br />
717<br />
20 cc syringe<br />
with 5 cc RPMI<br />
20 G spinal<br />
needle<br />
int diam- .58 mm<br />
Portex<br />
catheter<br />
int. diam<br />
.89 mm<br />
Transcervical chorionic villus sampling<br />
B<br />
Figure 24-3. Diagram illustrating the technique of sonographically<br />
guided chorionic villus sampling: (A) transabdominal sampling and<br />
(B) transcervical sampling.
718 Part 3 RISK ASSESSMENT AND THERAPY<br />
Table 24-2<br />
Transcervical Sampling<br />
Transcervical CVS is performed by using a polyethylene<br />
catheter through which a stainless-steel malleable stylet<br />
has been inserted. The stylet fits snugly through the<br />
catheter and provides sufficient rigidity for adequate passage<br />
through the cervix and into the frondosum. The<br />
stylet has a rounded, blunt end that protrudes slightly<br />
beyond the end of the catheter to prevent sharp edges that<br />
may potentially perforate the membranes. The catheter<br />
has a luerlock end to accommodate a syringe. The<br />
Trophcan catheter (Portex Company, Concord, MA,<br />
USA) had been the one most frequently used in the United<br />
States. However, this catheter has recently been removed<br />
from the market by the manufacturer, leaving the catheter<br />
manufactured by the Cook Company (Spencer, IN, USA)<br />
as the only commercially available TC sampling device<br />
(Figure 24-4).<br />
COMPARISON OF TRANSCERVICAL AND TRANSABDOMINAL <strong>CHORIONIC</strong> <strong>VILLUS</strong><br />
<strong>SAMPLING</strong> PROCEDURES<br />
Transcervical Transabdominal<br />
Relative contraindications Cervical polyps, active cervical, or Interceding bowel<br />
vaginal herpes<br />
Ease of learning Somewhat more complex than Adaptation of amniocentesis technique but<br />
transabdominal approach learning curve still required<br />
Sample size Large sample; includes whole villi Smaller sample; includes many small pieces<br />
Patient discomfort Minimal to absent Moderate<br />
Placental location Better for posterior placenta Better for fundal placenta<br />
Figure 24-4. Cook catheter used for transcervical chorionic villus sampling.<br />
Note the general curvature of the distal end, which is aligned with<br />
the notch on the handle. This allows the operator to be aware of the direction<br />
of the curve.<br />
Before performing the CVS procedure, ultrasound<br />
scanning confirms fetal viability and establishes the area of<br />
the chorion frondosum. An approach is mentally mapped<br />
that allows catheter placement parallel to the chorionic<br />
membrane. Uterine contractions may be present and<br />
obstruct or alter the sampling path (Figure 24-5). They<br />
may also alter the appearance and location of the placenta<br />
by pulling it into unusual locations. When contractions<br />
significantly interfere with a proposed sampling path,<br />
delaying the procedure for 15 to 30 minutes until they<br />
abate is suggested. The presence of large placental lakes<br />
should also be noted so they can be avoided, because sampling<br />
through these lakes has been associated with<br />
increased postprocedure bleeding. 22<br />
The maternal bladder should be sufficiently full to<br />
provide an acoustic window through which the vagina,<br />
cervix, and uterus can be visualized. Overfilling makes<br />
retrieval more difficult by increasing patient discomfort<br />
Uterine contraction CVS catheter<br />
Figure 24-5. Transcervical chorionic villus sampling catheter forced<br />
anteriorly by posterior uterine contraction.
and displacing the uterus out of the pelvis, which extends<br />
and fixes the sampling path.<br />
The procedure is performed in the lithotomy position<br />
on a standard examination table with foot stirrups. A<br />
speculum is inserted, and the vagina and cervix are<br />
cleansed with antiseptic solution. The catheter is prepared<br />
by slightly curving its distal 3- to 5-cm part with the<br />
guidewire in place to allow easy insertion through the<br />
cervix. In most cases, only a minimal amount of curvature<br />
is required. The cervical canal is then reimaged by ultrasound,<br />
and the catheter is introduced through the cervix<br />
until loss of resistance at the internal os is felt. Once the<br />
sonographer clearly identifies the catheter tip, it is guided<br />
by real-time sector scanning to the placental site (Figure<br />
24-6A). The catheter is directed by gently maneuvering the<br />
curved periphery of the gestational sac. A greater amount<br />
of upward or downward movement of the tip can be<br />
accomplished by manipulating the speculum to redirect<br />
the angle of approach. Severe bending of the stylet is rarely,<br />
if ever, required, but occasionally use of a single-tooth<br />
tenaculum on the cervix is needed to alter uterine position.<br />
A<br />
B<br />
Figure 24-6. Sonogram illustrating sonographically guided transcervical<br />
chorionic villus sampling at 11.5 weeks of menstrual age. A: The tip of<br />
the catheter is visible at the internal os before farther advancement.<br />
B: The catheter is correctly placed within the corion frondosum parallel<br />
to the chorionic membrane.<br />
Chapter 24 Chorionic Villus Sampling<br />
Insertion of the catheter in the correct tissue plane<br />
between the inner uterine wall and gestational sac is critical<br />
to safe sampling. Although sonographic guidance is<br />
crucial, tactile sensation is equally important. The catheter<br />
can be easily advanced if it is in the proper tissue plane,<br />
whereas resistance is encountered if it is against the chorionic<br />
membrane or uterine wall. A gritty sensation is felt if<br />
the catheter is inserted too deeply into the decidua. Slight<br />
readjustment of the angle of direction corrects the problem.<br />
To ensure an adequate sample, the catheter should be<br />
advanced through the full length of the placenta. The<br />
guidewire is then removed, and a 20-cc syringe containing<br />
approximately 5 cc of a collection medium is attached. The<br />
sample is collected by aspiration using negative pressure as<br />
the catheter is slowly withdrawn. Slight distortion of the<br />
placental surface may be noted sonographically during this<br />
process, and larger villus fragments may be visualized as<br />
they pass through the catheter lumen.<br />
Transabdominal Chorionic Villus Sampling<br />
719<br />
Two techniques for TA sampling are presently used. In the<br />
single-needle approach a 20-gauge spinal needle is used. 23<br />
Alternatively, some operators perform a double-needle<br />
technique that uses an outer guide needle (18-gauge thin<br />
wall or a 16- to 17-gauge standard spinal needle) and a<br />
smaller sampling needle (20 gauge). 24 In general, a 3.5-inchlong<br />
needle is sufficient for most patients, but a 5- or 6-inchlong<br />
needle should be available for very obese women.<br />
With the single-needle technique, a sampling path is<br />
chosen so that the tip of the needle passes within the<br />
chorion frondosum parallel to the chorionic membrane.<br />
Intervening bowel and bladder must be avoided. The needle<br />
tip is first inserted into the myometrium and then redirected<br />
parallel to the membrane (Figure 24-7). As with cervical<br />
sampling, the needle should be passed through as much villus<br />
tissue as possible and remain parallel to the chorionic<br />
membrane to avoid inadvertent puncture (Figure 24-6B).<br />
Once appropriately placed within the placenta, the stylet<br />
is removed and a syringe containing 5 cc of media is<br />
attached. Under continuous suction, 4 or 5 to-and-fro passes<br />
Figure 24-7. Sonogram illustrating transabdominal chorionic villus<br />
sampling. The needle is parallel to the chorionic plate.
720 Part 3 RISK ASSESSMENT AND THERAPY<br />
within the frondosum are made. The needle is then removed<br />
from the abdomen while suction is continued. This “vacuuming”<br />
technique is required to ensure retrieval of sufficient<br />
villus tissue because the diameter of the 20-gauge needle is<br />
slightly smaller than that of a TC catheter.<br />
The 2-needle technique uses a slightly larger-gauge<br />
spinal needle as a trocar, which is inserted into the<br />
myometrium. A thinner (19- to 20-gauge) and longer sampling<br />
needle is passed through the trocar into the chorion<br />
frondosum. The stylet of the sampling needle is then<br />
replaced with a syringe, and sampling is performed as with<br />
a single needle.<br />
Both TA sampling approaches appear to be equally<br />
safe. The 2-needle technique is theoretically less traumatic<br />
because the outer trocar remains still during sampling. It<br />
also has the advantage of allowing the operator to obtain<br />
additional villi by reinserting the sampling needle without<br />
requiring a second skin puncture. The single-needle<br />
approach is quicker, less uncomfortable, able to retrieve<br />
adequate tissue with minimal insertions, and appears to be<br />
the technique that has gained widest acceptance. Both<br />
techniques have a learning curve, and operator experience<br />
does seem to have a bearing on fetal loss rate. 25<br />
Confirmation of Adequate Tissue Retrieval<br />
The presence of adequate villus tissue can usually be confirmed<br />
by visual inspection of the syringe contents, but<br />
occasionally the sample may need to be evaluated under a<br />
dissecting microscope. Samples typically contain a mixture<br />
of predominantly villi with a small amount of maternally<br />
derived decidua. The chorionic villi appear as free-floating,<br />
white structures with fluffy, filiforme branches (Figure 24-<br />
8A). Contaminating decidua tissue has a more amorphous<br />
appearance and lacks distinct branches. Although these 2<br />
tissues can usually be grossly distinguished by virtue of their<br />
respective morphology, confirmation under a dissecting<br />
microscope is required if there is uncertainty that adequate<br />
A B<br />
villi have been retrieved. Microsopically, the villi have a distinctive<br />
branched appearance. Their surface is punctuated<br />
by small buds consisting of an outer syncytiotrophoblast<br />
covering and a core of mitotically active cytotrophoblast<br />
cells (Figure 24-8B). Within the center of each villus is the<br />
mesenchymal core, through which capillaries carrying fetal<br />
blood cells course.<br />
A minimum of 5 mg of villus tissue is required for most<br />
genetic analyses. If insufficient villi are present with the initial<br />
attempt, a second aspiration may be performed without<br />
additional risk. 8 Pregnancy loss rates increase significantly<br />
when more than 2 insertions are required, and may be as<br />
high as 10% if 3 attempts are made. 17,26 Therefore, a third<br />
pass should only be attempted if successful retrieval seems<br />
certain. Before a third attempt, the anatomic relationships<br />
should be reevaluated, interfering contractions should have<br />
abated, and consideration should be given to sampling by<br />
the alternative route. In most experienced centers, more<br />
than 99% of patients can be successfully sampled with 2 or<br />
fewer insertions. In our center, we have not had a failed<br />
procedure in our last 15,000 patients.<br />
Patients may resume normal physical activity after<br />
CVS, although strenuous exercise should be avoided for 24<br />
hours. Sexual abstinence is recommended for a short<br />
period of time to minimize any risk of ascending infection.<br />
Patients may have some mild vaginal bleeding after CVS;<br />
therefore, they should be counseled about this possibility<br />
before sampling.<br />
RISKS ASSOCIATED WITH <strong>CHORIONIC</strong><br />
<strong>VILLUS</strong> <strong>SAMPLING</strong><br />
Bleeding<br />
Vaginal bleeding is uncommon after TA CVS but is seen in<br />
7% to 10% of patients sampled transcervically. Minimal<br />
spotting is a common occurrence and may occur in almost<br />
one-third of women sampled by the TC route. 17 In most<br />
Figure 24-8. A: Photograph of chorionic villus fragments in a Petri dish after collection by chorionic villus sampling. B: Magnified image of chorionic<br />
villus. Note the cytotrophoblastic bud. Within the center of the villus is the mesenchymal core and fetal blood vessels.
cases, the bleeding is self-limited and the pregnancy outcome<br />
is excellent. However, a subchorionic hematoma<br />
may be visualized immediately after sampling in up to 4%<br />
of TC samples. 27 The hematoma usually disappears before<br />
the 16th week of pregnancy and is only rarely associated<br />
with adverse outcome. Of the more than 15,000 CVS procedures<br />
performed in our center, we have never needed to<br />
terminate a pregnancy or admit a patient for excessive<br />
postprocedural bleeding.<br />
Cases of heavy bleeding and resulting hematoma formation<br />
occur from accidental placement of the TC<br />
catheter into the vascular decidua basalis underlying the<br />
chorion frondosum. In extreme cases, the development of<br />
the hematoma can actually be seen on ultrasound. In most<br />
of these cases, a gritty feeling indicates penetration into the<br />
decidual layer. Careful attention to the feel of the catheter<br />
and avoidance of unnecessary manipulation can prevent<br />
most of these hemorrhagic episodes and minimize this<br />
complication.<br />
Infection<br />
Since the initial development of TC CVS, there has been<br />
concern that transvaginal passage of an instrument would<br />
introduce vaginal flora into the uterus. This possibility was<br />
confirmed by cultures that isolated bacteria from up to 30%<br />
of catheters used for CVS. 28-30 However, in clinical practice,<br />
the incidence of post-CVS chorioamnionitis is low. 16,17,31,32<br />
In a recently published US study of more than 2000 cases of<br />
TC CVS, infection was suspected as a possible etiology of<br />
pregnancy loss in only 0.3% of cases. 17 Infection after TA<br />
CVS also occurs and has been demonstrated, at least in<br />
some cases, to be secondary to bowel flora introduced by<br />
inadvertent puncture by the sampling needle.<br />
In our own series of more than 15,000 procedures in<br />
which prophylactic antibodies are not used, we have not<br />
observed any cases of chorioamnionitis requiring uterine<br />
evacuation. Our incidence of periabortion chorioamnionitis<br />
was 0.08% for both TC and TA sampling; this rate is<br />
about the same as that seen in series of spontaneous abortions<br />
that have not been sampled. 33,34 At present, because<br />
of the clinically low incidence of post-CVS chorioamnionitis,<br />
routine pre-CVS vaginal or cervical cultures for any<br />
organism other than gonococcus is not indicated.<br />
Early in the development of TC CVS, 2 lifethreatening<br />
pelvic infections were reported. 35,36 Each<br />
initially presented with a mild prodrome of maternal myalgias<br />
and low-grade fever without localized adnexal or uterine<br />
tenderness and subsequently led to maternal sepsis.<br />
Both occurred early in the respective center’s experience,<br />
and in both the same catheter was used for repeat insertions.<br />
Since these reports, a practice of using a new sterile<br />
catheter for each insertion has been universally adopted,<br />
with only exceedingly rare reports of serious infectious<br />
complications.<br />
Ruptured Membranes<br />
Acute rupture of the membranes, documented by either<br />
obvious gross fluid leakage or a decrease in measurable<br />
amnionic fluid on ultrasound evaluation, is a very rare<br />
Chapter 24 Chorionic Villus Sampling<br />
complication of CVS. 17,37 In our own experience, acute<br />
rupture of the membranes has not occurred. Experimental<br />
attempts to rupture membranes intentionally with a TC<br />
catheter have confirmed that the chorion can withstand<br />
significant punishment without perforation.<br />
Gross rupture of the membranes days to weeks after<br />
the procedure is acknowledged as a possible post-CVS<br />
complication. Delayed rupture can result from either<br />
mechanical injury to the chorion at the time of sampling<br />
with rupture from exposure of the amnion, or chronic irritation<br />
or inflammation from a hematoma on low-grade<br />
infection, allowing exposure of the amnion to subsequent<br />
damage or infection. One group reported a 0.3% incidence<br />
of delayed rupture of the membranes after CVS, 32 a rate<br />
confirmed by Brambati et al. 27<br />
Unexplained mid-trimester oligohydramnios has been<br />
suggested as a rare complication of TC CVS and may occur<br />
from delayed chorioamnion rupture with slow leakage of<br />
amniotic fluid. 37 These cases are frequently associated with<br />
postprocedure bleeding and an elevated maternal serum<br />
α-fetoprotein (MSAFP). Operator experience will<br />
markedly reduce the risk of this complication, probably by<br />
decreasing hematoma formation with its potential to serve<br />
as either a nidus for a smoldering infection or a chemical<br />
irritant of the membranes.<br />
Elevated MSAFP<br />
An acute rise in MSAFP after CVS has been consistently<br />
reported, implying a detectable degree of fetal maternal<br />
bleeding. 38-40 The elevation is transient, occurs more frequently<br />
after TA CVS, and appears to be dependent on the<br />
quantity of tissue aspirated. 40 Some studies have also<br />
demonstrated a correlation between the degree of elevation<br />
and the incidence of pregnancy loss. 41 Levels will drop<br />
to normal ranges by 16 to 18 weeks, which allows neural<br />
tube defect (NTD) serum screening to proceed according<br />
to usual prenatal protocols.<br />
Rh Isoimmunization<br />
In Rh-negative women, the otherwise negligible fetal<br />
maternal bleeding that follows CVS accrues special importance<br />
because Rh-positive cells in volumes as low as 0.1 mL<br />
have been shown to cause Rh sensitization. 42 Because all<br />
women with even a single pass of a catheter or needle<br />
show detectable rises in MSAFP, it seems prudent that<br />
all Rh-negative nonsensitized women undergoing CVS<br />
receive Rho (D) immunoglobulin subsequent to the<br />
procedure.<br />
The potential for a CVS-induced maternal-to-fetal<br />
transfusion to worsen already existing Rh immunization<br />
has been described, suggesting that sampling sensitized<br />
patients represents a contraindication to the procedure. 43<br />
Pregnancy Loss<br />
721<br />
Multiple reports from individual centers have demonstrated<br />
the safety and low pregnancy loss rates after CVS. 8,44-51 In<br />
experienced centers, the rate of miscarriage from the time<br />
of CVS until 28 weeks of gestation is approximately 2%
722 Part 3 RISK ASSESSMENT AND THERAPY<br />
to 3%. 19 However, to determine the incidence of procedureinduced<br />
pregnancy loss, adjustments for the relatively<br />
high background loss at this gestational age must be<br />
made.<br />
First-trimester spontaneous abortion in women not<br />
undergoing CVS is a common event, occurring in 1 in<br />
every 6 clinically recognized pregnancies. 52 However, miscarriage<br />
rates after ultrasound confirmation of a viable gestation<br />
are expected to be less. Simpson et al reported that,<br />
when ultrasound confirmation of fetal viability was noted<br />
at 8 weeks, 3.2% of 220 women with a mean age of 30 years<br />
aborted. 53 Christiaens and Stoutenbeek noted a 3.3% fetal<br />
loss rate in 274 women with proven fetal viability at 10<br />
weeks. 54 Because the majority of women undergoing CVS<br />
are older than 35 years and the spontaneous miscarriage<br />
rate increases with advancing maternal age, this variable<br />
must also be considered. Wilson et al found a total fetal<br />
loss rate after proven viability by first-trimester ultrasonography<br />
of 1.4% in women younger than 30 years, 2.6%<br />
in those between 30 and 34 years old, and 4.3% in women<br />
older than 35 years. 55 It appears that the best estimate of<br />
the background spontaneous miscarriage rate in a population<br />
of women similar to those undergoing CVS is approximately<br />
2% to 3%. Although this rate is similar to the postprocedure<br />
loss rate in other centers, a randomized clinical trial<br />
is necessary to quantify the procedure-induced risk precisely.<br />
Unfortunately, no randomized comparison of sampled<br />
with unsampled patients is likely; however, comparisons to<br />
amniocentesis have been performed.<br />
Because the background loss rate is higher in the firsttrimester<br />
than in the second, any comparison of CVS to<br />
second-trimester amniocentesis must enroll all patients<br />
before the gestational age at which CVS is performed. The<br />
total loss rates can then be compared. All losses must be<br />
included, whether from a spontaneous miscarriage or an<br />
induced termination for abnormal results. This approach<br />
eliminates any bias that may occur when comparing procedures<br />
performed at significantly different gestational ages,<br />
and also takes into account cytogenetically abnormal<br />
embryos that miscarry before an amniocentesis, which<br />
would be electively terminated after CVS.<br />
The largest demonstrations of data evaluating the relative<br />
safety of CVS and amniocentesis come from 3 recent<br />
collaborative reports. In 1989, the Canadian Collaborative<br />
CVS-Amniocentesis Clinical Trial Group reported its experience<br />
with a prospective, randomized trial comparing TC<br />
CVS with second-trimester amniocentesis. 16 During the<br />
study period, patients across Canada were only able to<br />
undergo CVS in conjunction with the randomized protocol.<br />
There were 7.6% fetal losses (spontaneous abortions,<br />
induced abortions, and late losses) in the CVS group and<br />
7.0% in the amniocentesis group. Thus, in desired pregnancies,<br />
an excess loss rate of 0.6% for CVS over amniocentesis<br />
was obtained; this difference was not statistically significant.<br />
Two months after the publication of the Canadian<br />
experience, the first American collaborative report<br />
appeared. 17 This study was a prospective, although nonrandomized,<br />
trial of more than 2200 women who chose<br />
either TC CVS or second-trimester amniocentesis.<br />
Patients in both groups were recruited in the firsttrimester<br />
of pregnancy. As in the Canadian study, advanced<br />
maternal age was the primary indication for prenatal testing.<br />
When the loss rates were adjusted for slight group<br />
differences in maternal and gestational ages at enrollment,<br />
an excess pregnancy loss rate of 0.8% referable to CVS over<br />
amniocentesis was calculated, which was not statistically<br />
significant.<br />
Whereas both North American trials showed no statistical<br />
difference in pregnancy loss when CVS was compared<br />
with amniocentesis, a prospective, randomized collaborative<br />
comparison of more than 3200 pregnancies sponsored<br />
by the European MRC Working Party on the Evaluation of<br />
CVS demonstrated a 4.6% greater pregnancy loss rate after<br />
CVS (95% confidence interval [CI], 1.6% to 7.5%). 36 This<br />
difference reflected more spontaneous deaths before 28<br />
weeks of gestation (2.9%), more terminations of pregnancy<br />
for chromosomal anomalies (1.0%), and more neonatal<br />
deaths (0.3%) in the CVS group.<br />
The factors responsible for the discrepant results<br />
between the European and North American studies<br />
remain uncertain, but it is probable that inadequate operator<br />
experience with CVS accounted for a large part of this<br />
difference. Whereas the US trial consisted of 7 centers and<br />
the Canadian trial 11 centers, the European trial included<br />
31 sampling sites. There were, on average, 325 cases per<br />
center in the US study, 106 in the Canadian study, and only<br />
52 in the European trial. Although no significant change in<br />
pregnancy loss rate was demonstrated during the course of<br />
the European trial, it appears that the learning curve for<br />
both TC and TA CVS may exceed 400 or more cases. 56,57<br />
Operators having performed fewer than 100 cases may<br />
have 2 or 3 times the postprocedure loss rate of operators<br />
who have performed more than 1000 procedures.<br />
The consensus of the recent literature indicates that<br />
with experienced operators, the procedural complication<br />
rates with CVS and amniocentesis is comparable; however,<br />
CVS is more difficult to learn. 5<br />
There have been similar comparisons between CVS and<br />
early amniocentesis, defined as amniocentesis performed<br />
before 14 weeks of gestation. In these comparisons of 2 firsttrimester<br />
procedures, consideration of gestational age differences<br />
is not necessary. Nicolaides et al compared TA CVS<br />
with amniocentesis performed between 10 and 13 weeks and<br />
gestation. 58 In this prospective comparison, the spontaneous<br />
loss rate was significantly higher after early amniocentesis<br />
(5.3%) than after CVS (2.3%). Also, a significant increase in<br />
the incidence of talipes equinovarus was seen after early<br />
amniocentesis. In another recent comparison, Sundberg et al<br />
randomized patients to either amniocentesis between 11 and<br />
13 weeks or TA CVS between 10 and 12 weeks. 3 Although<br />
the initial end point of this trial was intended to be pregnancy<br />
loss, the trial was stopped early because of an increased risk<br />
of talipes equinovarus in the early amniocentesis group.<br />
Although the power of the trial to compare fetal loss rates<br />
was limited by the incomplete sample, no significant difference<br />
was demonstrated. The amniocentesis loss rate, however,<br />
was 0.6% higher. Leakage of amniotic fluid after sampling<br />
occurred significantly more frequently after amniocentesis.<br />
Overall, the higher loss rates, increased risk of fluid<br />
leakage, and subsequent club foot deformity with early<br />
amniocentesis suggest that CVS is the preferred technique<br />
for first-trimester sampling.
PREGNANCY LOSS: TRANSCERVICAL VERSUS<br />
TRANSABDOMINAL <strong>CHORIONIC</strong> <strong>VILLUS</strong><br />
<strong>SAMPLING</strong><br />
Randomized trials have compared the TC and TA<br />
approaches. 19,57,59-61 The US collaborative CVS project performed<br />
a randomized, prospective study and found no difference<br />
in the postprocedure pregnancy loss rates between the<br />
2 approaches (TC, 2.5%; TA, 2.3%). 19 Equally important was<br />
that the overall post-CVS loss rate in the study (2.5%) was<br />
0.8% lower than that in the initial US study, which compared<br />
CVS with second-trimester amniocentesis. Because 0.8% was<br />
the quantitative difference in loss rates between amniocentesis<br />
and CVS in the original study, this finding suggests that,<br />
when centers become equivalently experienced, amniocentesis<br />
and CVS may have the same risk of pregnancy loss.<br />
Smidt-Jensen et al, pioneers of TA CVS, added additional<br />
information to the comparative safety of the procedures.<br />
61 In a prospective, randomized study, they found no<br />
difference in pregnancy loss between TA CVS and secondtrimester<br />
amniocentesis, but did demonstrate an increased<br />
risk for TC CVS, the procedure for which their center was<br />
least experienced. Chueh et al, in a retrospective review of<br />
more than 9000 CVS procedures, showed that in their center<br />
TC CVS had a slightly greater risk of pregnancy loss<br />
than TA sampling. 62 It appears safe to speculate that fetal<br />
loss rates between TC and TA sampling will be similar in<br />
most centers once equivalent expertise is gained with<br />
either approach. Integration of both methods into the program<br />
of any single center will offer the most complete,<br />
practical, and safe approach to first-trimester diagnosis.<br />
Table 24-3<br />
Chapter 24 Chorionic Villus Sampling<br />
RISK OF FETAL ABNORMALITIES AFTER<br />
<strong>CHORIONIC</strong> <strong>VILLUS</strong> <strong>SAMPLING</strong><br />
723<br />
It has recently been suggested that CVS may be associated<br />
with the occurrence of specific fetal malformations. The first<br />
suggestion of this was reported by Firth et al 63 In a series of<br />
539 CVS-exposed pregnancies, they identified 5 infants with<br />
severe limb abnormalities, all of which came from a cohort of<br />
289 pregnancies sampled at 66 days of gestation or less. Four<br />
of these infants had the unusual and rare oromandibularlimb<br />
hypogenesis syndrome, and the fifth had a terminal<br />
transverse limb reduction defect. Oromandibular-limb<br />
hypogenesis syndrome occurs with a birth prevalence of 1<br />
per 175,000 live births, 64 and limb reduction defects occur in<br />
1 per 1690 births. 65 Therefore, the occurrence of these<br />
abnormalities in more than 1% of CVS-sampled cases raised<br />
strong suspicion of an association. In this initial report, all of<br />
the limb abnormalities followed TA sampling performed<br />
between 55 and 66 days of gestation.<br />
Subsequent to this initial report, others added supporting<br />
cases to this list. Using the Italian multicenter birth defects<br />
registry, Mastroiacovo et al reported, in a case control study,<br />
an odds ratio of 11.3 (CI 5.6 to 2.13) for transverse limb<br />
abnormalities after first-trimester CVS. 66 When stratified by<br />
gestational age at sampling, pregnancies sampled before 70<br />
days had a 19.7% increased risk of transverse limb reduction<br />
defects, whereas patients sampled later did not demonstrate a<br />
significantly increased risk. Other single-center and case control<br />
studies, however, have been inconclusive about an association<br />
of CVS with limb reduction defects, with the majority<br />
demonstrating no increased risk (Table 24-3).<br />
STUDIES EVALUATING THE ASSOCIATION OF <strong>CHORIONIC</strong> <strong>VILLUS</strong> <strong>SAMPLING</strong> (CVS) AND LIMB<br />
REDUCTION DEFECT (LRD): PROCEDURES PERFORMED AFTER 63 DAYS<br />
No Association Association<br />
n Post-CVS n Post-CVS<br />
Reference Liveborns n LRDs Reference Liveborns n LRDs<br />
Jahoda et al. 120 3973 3 Burton et al. 131 394 4<br />
Halliday et al. 121 2071 3* Mastroiacovo et al. 132 2759 3<br />
Canadian group 13 905 0 Bissonnette et al. 129‡ 507 5<br />
Schloo et al. 122 3120 2<br />
Monni et al. 123 2752 2<br />
Blakemore et al. 124 3709 3<br />
Silver et al. 125 1048 1 ∗<br />
Mahoney et al. 126 4588 8 ∗∗<br />
Jackson et al. 127 12,863 5<br />
Smidt-Jensen et al. 128 2624 0<br />
Bissonnette et al. 129‡ 269 0<br />
Case Control Studies OR CI OR CI<br />
Dolk et al. 130 1.8 0.7–5 Mastroiacovo and Botto 133 19 9–37<br />
Williams et al. 73 Williams et al. 73<br />
Overall LRD 1.7 0.4–6 Terminal Digital LRD 6.4 1.1–38<br />
Transverse LRD 4.7 0.8–28<br />
∗ Uncertain association: There was no statistical increase in LRDs, but absolute incidence was higher than general risk.<br />
† Includes known syndromal defects.<br />
‡ Single report comparing two sampling sites.<br />
§ Less than 76 days. CI, confidence interval; OR, odds ratio.
724 Part 3 RISK ASSESSMENT AND THERAPY<br />
There is support of the notion that CVS may increase<br />
the risk of limb defects when sampling is performed before<br />
63 days of gestation. Most notably, Brambati et al, an<br />
extremely experienced group who have reported no<br />
increased risk of limb defects in patients sampled after 9<br />
weeks, have reported a 1.6% incidence of severe limb<br />
reduction defects when patients were sampled at 6 and 7<br />
weeks. 67 This rate decreased to 0.1% for sampling at 8 to 9<br />
weeks. Hsieh et al, in a report of the Taiwan CVS experience,<br />
reported 29 cases of limb reduction defects after CVS<br />
from September 1990 until June 1992; 4 cases had<br />
oromandibular-limb hypogenesis syndrome. 68 There were<br />
2 remarkable aspects of this report. First, although the gestational<br />
age at sampling was not known with certainty in<br />
all cases, the majority were performed at less than 63 days<br />
after the last menstrual period. Second, very inexperienced<br />
community-based operators performed the cases with<br />
limb reduction defects, whereas no defects were seen from<br />
the major centers. This experience suggests that very early<br />
sampling with excessive placental trauma may be etiologic<br />
in some reports of post-CVS limb reduction defects.<br />
The question continues to be debated of whether CVS<br />
sampling after 70 days has the potential of causing more<br />
subtle defects, such as shortening of the distal phalanx or<br />
nail hypoplasia. 69 At present, there are few data to substantiate<br />
this concern. On the contrary, most experienced centers<br />
performing CVS after 10 weeks have not seen an<br />
increase in limb defects of any type. A recent review of<br />
more than 200,000 CVS procedures reported to the WHO<br />
registry was reported and demonstrated no increase in the<br />
overall incidence of limb reduction defects after CVS or in<br />
any specific type or pattern of defect. 70 In a similar review<br />
of more than 65,000 procedures performed in 10 of the<br />
most experienced centers in the world, no increase in limb<br />
reduction defects was identified. 71<br />
Mechanisms by which early CVS could potentially<br />
lead to fetal malformations continue to be disputed.<br />
Placental thrombosis with subsequent fetal embolization<br />
has been raised as a potential etiology, but is unlikely<br />
because fetal clotting factors appear to be insufficient at<br />
this early gestational age. Inadvertent entry into the<br />
extraembryonic coelom with resulting amnionic bands has<br />
also been raised as a potential mechanism, but appears<br />
unlikely as well, because actual bands have not been<br />
observed in the majority of the cases. In addition, many of<br />
the cases of oromandibular-limb hypogenesis syndrome<br />
had internal central nervous system anomalies that cannot<br />
be accounted for by fetal entanglement or compression.<br />
Uterine vascular disruption appears to be the most<br />
plausible mechanism at present. 64 In this hypothesis, CVS<br />
causes placental injury or vasospasm that subsequently<br />
results in underperfusion of the fetal peripheral circulation.<br />
After the initial insult, there may be subsequent rupture of<br />
the thin-walled vessels of the damaged distal embryonic circulation,<br />
leading to further hypoxia, necrosis, and eventual<br />
resorption of preexisting limb structures. A similar mechanism<br />
leading to limb defects has been demonstrated in animal<br />
models after uterine vascular clamping, maternal<br />
cocaine exposure, or even simple uterine palpation. 71,72<br />
In a recent report, Quintero et al added additional<br />
information about a possible etiology. 73,74 Using TA<br />
embryoscopic visualization of the first-trimester embryo,<br />
they demonstrated the occurrence of fetal facial, head, and<br />
thoracic ecchymotic lesions after traumatically induced<br />
detachment of the placenta with subchorionic hematoma<br />
formation. No changes in fetal heart rate were seen.<br />
Although these lesions consistently appeared after major<br />
physical trauma to the placental site, they were not able to<br />
be produced by the passage of a standard CVS catheter.<br />
Any theory of CVS-induced limb defects must consider<br />
that there are different stages of fetal sensitivity and<br />
should demonstrate a correlation between the severity of<br />
the defects and the gestational age at sampling. Firth et al<br />
recently presented evidence that appears to illustrate that<br />
sampling before 9 weeks of gestation induces the most<br />
severe and proximally located fetal limb defects. 75 These<br />
severe defects are not seen after later CVS. Alternatively,<br />
Froster and Jackson reviewed the severity of the post-CVS<br />
limb defects reported to the WHO registry and found no<br />
such correlation. 70<br />
At the present time, patients planning to have CVS<br />
can be counseled that there is no increased risk of severe<br />
limb defects if CVS is performed after 70 days of gestation.<br />
76 They should be made aware of the present controversy<br />
concerning more subtle defects and reassured that<br />
this has not been seen in most experienced centers. If such<br />
a risk does exist, the magnitude based on case control studies<br />
can be estimated to be no higher than 1 in 3000. 76<br />
Ideally, centers performing CVS should have aggressive<br />
follow-up systems in place and be capable of giving<br />
patients information about the rate of congenital abnormalities<br />
in their center. Sampling before 10 weeks of gestation<br />
should be limited to very exceptional cases, and these<br />
patients must be informed of a 1% or higher risk of limb<br />
77-90 124-137<br />
reduction defects.<br />
PERINATAL RISKS AND IMPACT ON<br />
LONG-TERM DEVELOPMENT OF THE INFANT<br />
No increases in preterm labor, premature rupture of the<br />
membranes, small-for-gestational-age infants, maternal<br />
morbidity, or other obstetric complications have occurred in<br />
sampled patients. 91 Although the Canadian collaborative<br />
study showed an increased perinatal mortality in CVS sampled<br />
patients, with the greatest imbalance being beyond 28<br />
weeks, no obvious recurrent event was identified. 16 To date,<br />
no other studies have seen a similar increase in perinatal loss.<br />
Long-term infant follow-up has been performed by<br />
Chinese investigators, who evaluated 53 children from<br />
their initial placental biopsy experience of the 1970s. All<br />
were reported in good health, with normal development<br />
and school performance. 92<br />
LABORATORY ASPECTS OF <strong>CHORIONIC</strong><br />
<strong>VILLUS</strong> <strong>SAMPLING</strong><br />
CVS is now considered a reliable method of prenatal diagnosis,<br />
but early in its development incorrect results were<br />
reported. 93-95 The major sources of these errors included<br />
maternal cell contamination and misinterpretation of
mosaicism confined to the placenta. Today, genetic evaluation<br />
of chorionic villi provides a high degree of success<br />
and accuracy, in particular with regard to the diagnosis of<br />
common trisomies. 96,97 In 1990, the US collaborative study<br />
reported a 99.7% rate of successful cytogenetic diagnosis,<br />
with 1.1% of the patients requiring a second diagnostic<br />
test, such as amniocentesis or fetal blood analysis to further<br />
interpret the results. 96 In most cases, the additional<br />
testing was required to delineate the clinical significance of<br />
mosaic or other ambiguous results (76%), and laboratory<br />
failure (21%) and maternal cell contamination (3%) also<br />
required follow-up testing. Continued experience has<br />
almost eliminated maternal cell contamination as a source<br />
of clinical errors. In addition, we now have a better understanding<br />
of the biology of the placenta so that confined placental<br />
mosaicism no longer leads to incorrect diagnosis,<br />
but provides us with information predictive of pregnancy<br />
outcome and can serve as a clue to the presence of uniparental<br />
disomy. Therefore, an understanding of villus<br />
morphology and CVS laboratory techniques is required to<br />
provide correct clinical interpretation.<br />
Chorionic villi have 3 major components: (1) an outer<br />
layer of hormonally active and invasive syncytiotrophoblast,<br />
(2) a middle layer of cytotrophoblast from which<br />
syncytiotrophoblast is derived, and (3) an inner mesodermal<br />
core containing blood, capillaries for oxygen, and<br />
nutrient exchange (Figure 24-8B). After collection, the villi<br />
are cleaned of any adherent decidua and then exposed to<br />
trypsin to digest and separate the cytotrophoblast from the<br />
underlying mesodermal core. The cytotrophoblast has a<br />
high mitotic index, with many spontaneous mitoses available<br />
for immediate chromosomal analysis. The liquid suspension<br />
containing the cytotrophblast is either dropped<br />
immediately onto a slide for analysis or may undergo a<br />
Syncytiotrophoblast<br />
Mesenchymal core<br />
Cytotrophoblastic<br />
cell column<br />
Cytotrophoblast<br />
A B<br />
Chapter 24 Chorionic Villus Sampling<br />
725<br />
short incubation. 98-100 This “direct” chromosomal preparation<br />
can provide preliminary results within 2 to 3 hours.<br />
However, most laboratories now use overnight incubation<br />
to improve karyotype quality and thus report results within<br />
2 to 4 days (Figure 24-9). The remaining villus core is placed<br />
in tissue culture and is typically ready for harvest and chromosome<br />
analysis within 1 week. 101 The direct method has<br />
the advantage of providing a rapid result and minimizing<br />
the decidual contamination, whereas tissue culture is better<br />
for interpreting discrepancies between the cytotrophoblast<br />
and the actual fetal state. Ideally, both the direct and culture<br />
methods should be used because they each evaluate slightly<br />
different tissue sources. Abnormalities in either may have<br />
clinical implications. However, the direct preparation is<br />
labor intensive, adds additional cost, and is not routinely<br />
available in some laboratories.<br />
MATERNAL CELL CONTAMINATION<br />
Chorionic villus samples typically contain a mixture of placental<br />
villi and maternally derived decidua. Although specimens<br />
are thoroughly washed and inspected under a<br />
microscope after collection, some maternal cells may<br />
remain and grow in the culture. As a result, 2 cell lines, one<br />
fetal and the other maternal, may be identified. In other<br />
cases, the maternal cell line may completely overgrow the<br />
culture, thereby leading to diagnostic errors including<br />
incorrect sex determination8,102-104 and potentially to falsenegative<br />
diagnoses, although there are no published<br />
reports of the latter. Direct preparations of chorionic villi<br />
are generally thought to prevent maternal cell contamination,<br />
100, 103 whereas long-term culture has a contamination<br />
rate ranging from 1.8% to 4%. 104 Because, in contrast to<br />
cytotrophoblast, maternal decidua has a low mitotic index,<br />
Mesenchymal<br />
core<br />
Villus<br />
culture<br />
Villus tissue<br />
trypsin<br />
Cytotrophoblast<br />
suspension<br />
Direct<br />
preparation<br />
Figure 24-9. A: Diagram of normal villus architecture. B: Diagram outlining the laboratory technique for chorionic<br />
villus sampling direct chromosomal preparation and villus culture.
726 Part 3 RISK ASSESSMENT AND THERAPY<br />
it is highly desirable for laboratories to offer a direct chromosomal<br />
preparation and a long-term culture on all samples<br />
of chorionic villus. Even in culture, the contaminating<br />
cells are easily identified as maternal and should not lead to<br />
clinical errors. Interestingly, for reasons still uncertain,<br />
maternal cell contamination occurs more frequently in<br />
specimens retrieved by the TC route. 104<br />
Contamination of samples with significant amounts of<br />
maternal decidual tissue is almost always due to small sample<br />
size, making selection of appropriate tissue difficult. In<br />
experienced centers in which adequate quantities of villi<br />
are available, this problem has disappeared. Choosing only<br />
whole, clearly typical villus material and discarding any<br />
atypical fragments, small pieces, or fragments with adherent<br />
decidua will avoid confusion. 105 Therefore, if the initial<br />
aspiration is small, a second pass should be performed<br />
rather than risk inaccurate results. When proper care is<br />
taken and good cooperation and communication exists<br />
between the sampler and the laboratory, even small<br />
amounts of contaminating maternal tissue can be absent.<br />
Fluorescent in situ hybridization (FISH) for common<br />
chromosomal abnormalities can be helpful in reaching a<br />
rapid diagnosis (within hours) without the concern for<br />
maternal contamination.<br />
CONFINED PLACENTAL MOSAICISM<br />
The second major source of potential diagnostic error<br />
associated with CVS is mosaicism confined to the placenta.<br />
Although the fetus and placenta have a common ancestry,<br />
chorionic villus tissue will not always reflect fetal genotype.<br />
96,106 Although there was concern that this might<br />
invalidate CVS as a prenatal diagnostic tool, subsequent<br />
investigations have led to a clearer understanding of villus<br />
biology so that accurate clinical interpretation is now possible.<br />
This understanding has also revealed new information<br />
about the etiology of pregnancy loss, discovered a new<br />
cause of intrauterine growth retardation, and clarified the<br />
basic mechanism of uniparental disomy.<br />
Discrepancies between the cytogenetics of the placenta<br />
and fetus occur because the cells contributing to the chorionic<br />
villi become separate and distinct from those forming<br />
the embryo in early development. Specifically, at approximately<br />
the 32- to 64-cell stage, only 3 to 4 become compartmentalized<br />
into the inner cell mass (ICM) to form the<br />
embryo, and the remainder become precursors of the<br />
extraembryonic tissues. 107 Mosaicism can then occur<br />
through 2 possible mechanisms. 108 An initial meiotic error<br />
in one of the gametes can lead to a trisomic conceptus that<br />
normally would spontaneously abort. However, if one of the<br />
early aneuploid precursor cells loses one of the chromosomes<br />
contributing to the trisomic set during subsequent<br />
mitotic divisions, the embryo can be “rescued” by reduction<br />
of a portion of its cells to disomy. This will result in a mosaic<br />
morula, with the percentage of normal cells dependent on<br />
the cell division at which rescue occurred. More abnormal<br />
cells will be present when correction is delayed to the second<br />
or a subsequent cell division. Because the majority of<br />
cells in the morula proceed to the trophoblast cell lineage<br />
(processed by the direct preparation), it is highly probable<br />
that that lineage will continue to contain a significant number<br />
of trisomic cells. Alternatively, because only a small number<br />
of cells are incorporated into the ICM, involvement of the<br />
fetus will depend on the chance distribution of the aneuploid<br />
progenitor cells. Involvement of the mesenchymal<br />
core of the villus, which also evolves from the ICM, is similarly<br />
dependent on this random cell distribution.<br />
Noninvolvement of the fetal cell lineage will produce confined<br />
placental mosaicism (CPM) in which the trophoblast<br />
and perhaps the extraembryonic mesoderm will have aneuploid<br />
cells, but the fetus will be euploid.<br />
Alternatively, mitotic postzygotic errors can produce<br />
mosaicism, with the distribution and percentage of aneuploid<br />
cells in the morula or blastocyst dependent on the timing<br />
of nondisjunction. If mitotic errors occur early in the<br />
development of the morula, they may segregate to the ICM<br />
and have the same potential to produce an affected fetus as<br />
do meoitic errors. Mitotic errors occurring after primary cell<br />
differentiation and compartmentalization has been completed<br />
lead to cytogenetic abnormalities in only one lineage.<br />
Meiotic rescue can lead to uniparental disomy (UPD).<br />
This occurs because the original trisomic cell contained 2<br />
chromosomes from one parent and 1 from the other. After<br />
rescue, there is a theoretical 1 in 3 chance that the resulting<br />
pair of chromosomes came from the same parent,<br />
which is called uniparental disomy. UPD may have clinical<br />
consequences if the chromosomes involved carry<br />
imprinted genes in which expression is based on the parent<br />
of origin. For example, Prader-Willi syndrome may result<br />
from uniparental maternal disomy for chromosome 15.<br />
Therefore, a CVS diagnosis of confined placental<br />
mosaicism for trisomy 15 may be the initial clue that UPD<br />
could be present and lead to an affected child. 109,110<br />
Because of this, all cases in which CVS reveals trisomy 15<br />
(either complete or mosaic) should be evaluated for UPD<br />
by subsequent amniotic fluid analysis. In addition to chromosome<br />
15, chromosomes 7, 11, 14, and 22 are felt to be<br />
imprinted and require follow-up. 111<br />
Recently, there has been evidence that confined placental<br />
mosaicism (unassociated with UPD) can alter placental<br />
function and lead to fetal growth failure or perinatal<br />
death. 108,112-117 The exact mechanism by which abnormal<br />
cells within the placenta alter fetal growth or lead to fetal<br />
death is unknown. However, the effect may be limited to<br />
specific chromosomes. For example, CPM for chromosome<br />
16 leads to severe intrauterine growth restriction,<br />
prematurity, or perinatal death, with fewer than 30% of<br />
pregnancies resulting in normal full-term infants appropriate<br />
for gestational age. 118-125<br />
CVS mosaic results require diligent follow-up by<br />
amniocentesis or fetal sampling to determine their clinical<br />
significance because, in most cases, if the mosaic results<br />
are confined to the placenta, fetal development will be normal.<br />
However, if the mosaic cell line also involves the fetus,<br />
there may be significant phenotypic consequences.<br />
Mosaicism occurs in about 1% of all CVS samples<br />
97, 104<br />
,121,122 but is confirmed in the fetus in only 10% to 40% of<br />
these cases. The probability of fetal involvement appears to<br />
be related to the tissue source in which the aneuploid cells<br />
were detected and the specific chromosome involved. 110<br />
Mesenchymal core culture results are more likely than<br />
direct preparation to reflect a true fetal mosaicism.
In a recent review, Phillips et al demonstrated that<br />
autosomal mosaicism involving common trisomies (ie, 21,<br />
18, and 13) was confirmed in the fetus in 19% of cases,<br />
whereas uncommon trisomies involved the fetus in only<br />
3%. 123 When sex chromosome mosaicism was found in the<br />
placenta, the abnormal cell line was confirmed in the fetus<br />
in 16% of cases. When a nonfamilial marker chromosome<br />
was involved, it was confirmed in the fetus in more than<br />
one-fourth of cases, whereas mosaic polyploidy was confirmed<br />
in only 1 of 28 cases. Chromosomal structural<br />
abnormalities were confirmed in 8.6% of cases.<br />
When placental mosaicism is discovered, amniocentesis<br />
is frequently performed to elucidate the extent of fetal<br />
involvement. When mosaicism is limited to the direct<br />
preparation only, amniocentesis appears to correlate perfectly<br />
with fetal genotype. 123 However, when a mosaicism is<br />
observed in tissue culture, both false-positive and falsenegative<br />
amniocentesis results occur. In these cases, amniocentesis<br />
will predict the true fetal karyotype in approximately<br />
94% of cases. 123 Most importantly, these discrepancies<br />
may involve the common autosomal trisomies. There<br />
have been 3 cases reported of mosaic trisomy 21 on villus<br />
culture and a normal amniotic fluid analysis, followed by a<br />
fetus or newborn with mosaic aneuploidy. 96<br />
At present, the following clinical recommendations<br />
may be used to assist in the evaluation of CVS mosaicism.<br />
Analysis of CVS samples should, if possible, include both<br />
direct preparation and tissue culture. Although the direct<br />
preparation is less likely to be representative of the fetus,<br />
its use will minimize the likelihood of maternal cell contamination,<br />
and if culture fails, a nonmosaic normal direct<br />
preparation result can be considered conclusive, although<br />
rare cases of false-negative results for trisomies 21 and 18<br />
have been reported. 124-128 If mosaicism is found on either<br />
culture or direct preparation, follow-up amniocentesis<br />
should be offered. Under no circumstances should a decision<br />
to terminate a pregnancy be based entirely on a CVS<br />
mosaic result. For CVS mosaicism involving sex chromosome<br />
abnormalities, polyploidy, marker chromosomes,<br />
structural rearrangements, and uncommon trisomies, the<br />
patient can be reassured if amniocentesis results are<br />
euploid and detailed ultrasonographic examination is normal.<br />
However, no guarantees should be made and, as<br />
described above, in certain cases testing for UPD will be<br />
indicated. If common trisomies 21, 18, and 13 are involved,<br />
amniocentesis should be offered, but the patient must be<br />
advised of the possibilities of a false-negative result.<br />
Follow-up may include detailed ultrasonography, fetal<br />
blood sampling, or fetal skin biopsy. At present, the predictive<br />
accuracy of these additional tests is uncertain.<br />
BIOCHEMICAL AND DNA PROCEDURES<br />
Most biochemical and molecular diagnoses that can be<br />
made from amnionic fluid or cultured amniocytes can also<br />
be made from chorionic villi. In many cases, the results will<br />
be available more rapidly and more efficiently by using<br />
villi, because sufficient enzyme or DNA is present in villus<br />
samples to allow direct analysis rather than wait for tissue<br />
culture. For example, the analysis of Tay-Sachs disease can<br />
be performed in less than 30 minutes using fresh villi. 129<br />
Chapter 24 Chorionic Villus Sampling<br />
727<br />
A discussion of individual biochemical or molecular<br />
diagnoses is beyond the scope of this chapter and is<br />
impractical because techniques are changing so rapidly. A<br />
registry of diagnoses performed by CVS is kept and<br />
updated through the WHO by Dr Hans Galjaard in<br />
Rotterdam, The Netherlands, and a published summary of<br />
the early worldwide experience is available. 130<br />
It cannot be assumed that biochemical or molecular<br />
results from villus tissue will always be a true reflection of<br />
the fetal state. Recently, misdiagnosis of the peroxisomal<br />
disorder, X-linked adrenoleukodystrophy, from cultured<br />
villus cells has been reported. 131 In addition, tests requiring<br />
determination of DNA methylation status, such as that for<br />
fragile X, 132 are also not always reliable in villus tissue. This<br />
does not, however, preclude CVS from making these prenatal<br />
diagnoses because other molecular approaches can<br />
be used. It does emphasize that all tests on villus tissue<br />
must be validated by testing sufficient numbers of affected<br />
and unaffected pregnancies before being used clinically.<br />
Because of the rarity and unique aspects of most biochemical<br />
and molecular disorders, specific diagnoses are usually<br />
performed by only a few laboratories. Before performing a<br />
CVS, the clinician should contact the center analyzing the<br />
tissue so that the details of testing can be discussed.<br />
<strong>CHORIONIC</strong> <strong>VILLUS</strong> <strong>SAMPLING</strong> IN MULTIPLE<br />
GESTATIONS<br />
Chorionic villus sampling is a safe and effective approach to<br />
examining twins. Not only does it provide results early in<br />
pregnancy, but, if discordancy is discovered, the medical<br />
and psychological difficulties encountered with selective<br />
termination can be minimized. However, it can be technically<br />
more demanding because it requires an experienced<br />
operator and sonographer. The ideal time to perform a twin<br />
CVS is similar to that for singletons. Ultrasound initially<br />
identifies placental locations, determines chorionicity, and<br />
confirms fetal sizes and viability. Sampling of each sac is<br />
independently performed by either a TC or TA approach,<br />
with separate passes of a new sampling instrument for each<br />
attempt. Because no unique marker is available to ensure<br />
that the samples have been retrieved from distinct placentas,<br />
it is imperative that insertion of the instrument into<br />
each frondosum is certain. Longitudinal and transverse<br />
scanning planes should be used to ensure proper location.<br />
If any doubt exists, a repeat procedure is required, but with<br />
increased experience, the need for repeat procedure is<br />
rare. 133<br />
Contamination of one sample with villi from the other<br />
sac is possible and occurs most commonly when retrieval<br />
is performed near the dividing membrane, or if a needle or<br />
catheter is dragged through one frondosum while sampling<br />
another. When the chorions appear fused, sampling<br />
near the cord insertion sites, with avoidance of the area of<br />
confluence of the 2 placentas, should prevent contamination<br />
and ensure sampling of each fetus. A combination of<br />
TC and TA sampling can minimize co-twin contamination<br />
by ensuring unique sampling paths. For example, if both<br />
chorion frondosa are situated along the anterior uterine<br />
wall, the lower one can be sampled transcervically and the
728 Part 3 RISK ASSESSMENT AND THERAPY<br />
upper transabdominally without contaminating either<br />
sample. Despite meticulous sampling techniques, co-twin<br />
contamination occurs in up to 4% of cases 120 but is rarely<br />
of clinical concern. If the cytogenetic laboratory is aware of<br />
the presence of a multiple gestation, the presence of both<br />
normal and aneuploid cells in the sample will be correctly<br />
interpreted. The possibility of contamination is of greater<br />
consequence if sampling is being performed for biochemical<br />
analysis, where a small amount of contaminating tissue<br />
could lead to an incorrect diagnosis. For this reason,<br />
instead of pooling a sample, we recommend analyzing<br />
individual villi when biochemical studies are to be performed.<br />
An experienced sampler and an aware and knowledgeable<br />
laboratory are extremely important in such cases.<br />
The need to map the placental location clearly and<br />
accurately is mandatory, because the risk of discordant<br />
results is higher early in the pregnancy and selective termination<br />
may be required. The relative positions of the placentas<br />
will remain stable over the time frame that results<br />
are obtained, so that identification of the affected fetus can<br />
usually be determined even 2 or 3 weeks after the procedure.<br />
However, if there is uncertainty, a repeat CVS with<br />
direct villus analysis can confirm the position immediately<br />
before the termination.<br />
Procedure-related loss rates after CVS sampling of<br />
twins are well studied. In experienced centers, no<br />
increased procedure-related loss risks are seen compared<br />
with second trimester amniocentesis. 133,134 Table 24-4<br />
presents overall pregnancy loss rates to 28 weeks of 1.6% to<br />
2.8% in sampled twins. When compared with a contemporaneously<br />
sampled group of patients choosing either CVS<br />
or second trimester amniocentesis, we found no difference<br />
in the overall risk of pregnancy loss (2.9% amniocentesis vs<br />
3.2% CVS). There was, however, a slightly increased risk of<br />
losing one fetus in the group sampled by amniocentesis. 133<br />
The choice of the appropriate technique for sampling<br />
twins depends on a number of factors including locally<br />
available skill and expertise. In centers in which amniocentesis<br />
and CVS are both available, CVS may be the preferred<br />
approach because it provides results 1 month sooner, thus<br />
providing earlier reassurance. When discordant results are<br />
encountered, complications and loss rates are decreased<br />
Table 24-4<br />
SAFETY OF <strong>CHORIONIC</strong> <strong>VILLUS</strong><br />
<strong>SAMPLING</strong> (CVS) WITH TWINS<br />
COMPARED WITH AMNIOCENTESIS<br />
Success Pregnancy Loss<br />
n Rate Rate to 28 Weeks<br />
CVS<br />
Wapner et al. 115∗ 440 † 100% 2.8%<br />
Pergament et al. 116 128 99.2% 2.4%<br />
Brambati et al. 119 66 100% 1.6%<br />
Amniocentesis<br />
Wapner et al. 115∗ 73 100 2.9%<br />
∗ Contemporaneously collected comparison of CVS with amniocentesis in a<br />
single center.<br />
† Additional cases added since original publication.<br />
when selective termination is performed before 16 weeks<br />
of gestation. 135<br />
<strong>CHORIONIC</strong> <strong>VILLUS</strong> <strong>SAMPLING</strong> AND<br />
MULTIFETAL PREGNANCY REDUCTION<br />
Multifetal pregnancy reduction (MFPR) to improve perinatal<br />
outcome is an unfortunate but accepted part of reproductive<br />
medicine. As with selective termination, MFPR is<br />
most safely performed in the first-trimester. 136 Therefore, in<br />
high-order gestations at increased risk for a genetic abnormality,<br />
CVS before a reduction can avoid the potential need<br />
for a later selective termination. The CVS can be performed<br />
between 10 and 11.5 weeks of gestation, and a rapid karyotype<br />
can be available within 24 to 48 hours, after which the<br />
MFPR is performed. Villus mesenchymal core tissue culture<br />
is also performed, but results are usually not available<br />
for 7 to 10 days. Because of the small increased risk of confined<br />
placental mosaicism with the direct preparation,<br />
awaiting culture results when time allows is suggested. The<br />
positions of the sampled fetuses will be the same when the<br />
patient returns for the MFPR. In most cases, only the 2<br />
fetuses most likely to remain after the MFPR are sampled.<br />
If an abnormality is identified, an additional fetus can be<br />
sampled at the time of the MFPR and the patient can return<br />
if this is also abnormal. Of 745 MFPR reductions performed<br />
at our center, 254 had an initial CVS. Abnormal chromosomal<br />
results were present in approximately 2.5% of pregnancies,<br />
and the abnormal fetus was terminated as part of the<br />
reduction procedure. The pregnancy loss rate to 24 weeks<br />
of gestation of those having a preceding CVS was 5.5% versus<br />
5.6% in those having only MFPR. This encouraging outcome<br />
is similar to that described by Brambati et al137 in<br />
which the cohort of patients undergoing CVS before MFPR<br />
demonstrated no increased risk of pregnancy loss, prematurity,<br />
or small-for-gestational-age infants.<br />
SUMMARY<br />
Chorionic villus sampling is a safe technique for firsttrimester<br />
prenatal diagnosis of genetic disorders. Real-time<br />
sonography and technologic advances of sampling instruments<br />
have been critical in establishing a safe technique for<br />
retrieving villus tissue for genetic analysis. Clinical trials<br />
suggest that CVS carries a low risk of pregnancy loss, which<br />
is comparable to that of second-trimester amniocentesis.<br />
An understanding of the laboratory techniques and human<br />
embryology is essential in avoiding diagnostic errors related<br />
to confined placental mosaicism.<br />
To maximize outcome, CVS should be performed by<br />
an experienced team of physicians, ultrasonographers, and<br />
genetic laboratory technicians. Before initiating a CVS<br />
program, operators should have considerable experience<br />
in the placement of the catheter, which can be achieved<br />
either in a formal training program with observation of 50<br />
procedures followed by close hands-on supervision of<br />
another 100 cases, 8 or by supervised practice on pregnancies<br />
undergoing subsequent abortion. In addition, it is<br />
advisable to limit the number of ultrasonographers
assigned to assist in this procedure, because sampling success<br />
is equally dependent on skillful ultrasound guidance.<br />
Similar to the physician retrieving the villi, the guiding<br />
sonographer should be knowledgeable in the didactics of<br />
CVS sampling and should obtain adequate hands-on training<br />
before beginning work in this area. This can be<br />
achieved in a formal training program or by visiting centers<br />
performing this procedure. 8 In this setting, CVS will<br />
continue to be an important, reliable, and safe contributor<br />
to prenatal genetic diagnosis.<br />
KEY POINTS<br />
1. Chorionic villus sampling has a low complication rate<br />
comparable to mid-trimester amniocentesis in experienced<br />
hands. The learning curve is more difficult with<br />
CVS.<br />
2. CVS is the preferable method of fetal aneuploidy testing<br />
in the first trimester.<br />
3. CVS is generally performed after 9 completed weeks<br />
of gestation. In this setting, there does not seem to be<br />
an increased risk of limb reduction defects.<br />
4. CVS may be performed either transabdominally or<br />
transcervically.<br />
5. Caution should be exercised in the interpretation of a<br />
mosaic of chromosomal findings from CVS.<br />
6. The complications of CVS include miscarriage, bleeding,<br />
rupture of membranes, and infection.<br />
REFERENCES<br />
1. American College of Obsetetricians and Gynecologists. Invasive<br />
prenatal testing for aneuploidy. ACOG Practice Bulletin 88,<br />
Washington, DC: Dec 2007.<br />
2. Grimes DA, Schultz KF. Morbity and mortality from second<br />
trimester abortion. J Repro Med 1985;30:505-14.<br />
3. Sundberg K, Bang J, Smidt-Jensen S, et al. Randomized study of risk<br />
of fetal loss related to early amniocentesis versus chorionic villus<br />
sampling. Lancet 1997;350:697-703.<br />
4. CEMAT Group. Randomized trial to assess safety and fetal outcomes<br />
of early and midtrimester amniocentesis. Lancet 1998;351:<br />
1435.<br />
5. Evans MI, Andriole S. Chorionic villus sampling and amniocentesis<br />
in 2008. Curr Opin Obstet Gynecol 2008;20(1):164-8.<br />
6. Caughey AB, Hopkins LM, Norton ME. Chorionic villus sampling<br />
compared with amniocentesis and the difference in the rate of pregnancy<br />
loss. Obstet Gynecol 2006;18:612-6.<br />
7. Spencer K, Souter V, Tul N, et al. A screening program for trisomy<br />
21 at 10-14 weeks using fetal nuchal translucency, maternal serum<br />
free B-human chorionic gonadotrophin and pregnancy-assoicarted<br />
plasma protein A. Ultrasound Obstet Gynecol 1991;13:231-7.<br />
8. Boehm FH, Salyer SL, Dev VG, et al. Chorionic villus sampling: quality<br />
control-m-A continuous improvement model. Am J Obstet<br />
Gynecol 1993;168:1766-77.<br />
9. Department of Obstetrics and Gynecology. Tietung Hospital of<br />
Anshan Iron and Steel Co. Anshan, China. Fetal sex prediction by<br />
sex chromatin of chorionic villi cells during early pregnancy.<br />
Chinese Med J 1975;1:117.<br />
10. Hahnemann N, Mohr J. Genetic diagnosis in the embryo by means<br />
of biopsy from extraembryonic membranes. Bull Eur Soc Hum<br />
Genet 1968;2:23-9.<br />
11. Kullander S, Sandahl B. Fetal chromosome analysis after transcervical<br />
placental biopsies during early pregnancy. Acta Obstet Gynecol<br />
Scand 1973;52:355-9.<br />
Chapter 24 Chorionic Villus Sampling<br />
729<br />
12. Hahnemann N. Early prenatal diagnosis: a study of biopsy techniques<br />
and cell culturing from extraembryonic membranes. Clin<br />
Genet 1974;6:294-306.<br />
13. Kazy Z, Rozovsky I, Bakhaey V. Chorion biopsy in early pregnancy:<br />
a method of early prenatal diagnosis for inherited disorders. Prenat<br />
Diagn 1982;2:39-45.<br />
14. Old J. First trimester fetal diagnosis for haemoglobinopathies: three<br />
cases. Lancet 1982;2:1413-6.<br />
15. Brambati B, Simoni G. Diagnosis of fetal trisomy 21 in first<br />
trimester. Lancet 1983;1:586.<br />
16. Canadian Collaborative CVS-Amniocentesis Clinical Trial Group.<br />
Multicentre randomized clinical trial of chorion villus sampling and<br />
amniocentesis. Lancet 1989;i:1.<br />
17. Rhoads GG, Jackson IG, Schlesselman SE, et al. The safety and efficacy<br />
of chorionic villus sampling for early prenatal diagnosis of cytogenetic<br />
abnormalities. N Engl J Med 1989;320:609-9.<br />
18. Committee on Genetics. ACOG Committee Opin 1995;160.<br />
19. Jackson LG, Zachary JM, Fowler SE, et al. Randomized comparison<br />
of transcervical and transabdominal chorionic villus sampling. N<br />
Engl J Med 1992;327:594-8.<br />
20. Silver RK, MacGregor SN, Sholl JS, et al. Initiating a chorionic villus<br />
sampling program. Relying on placental location as the primary<br />
determinant of the sampling route. J Reprod Med 1990;<br />
35:964-8.<br />
21. Brambati B, Oldrini A, Lanzani A. Transabdominal and transcervical<br />
chorionic villus sampling: efficiency and risk evaluation of<br />
2,411 cases. Am J Med Genet 1990;35: 160-4.<br />
22. Liu DT, Agbaje R, Preston C, Savage J. Intraplacental sonolucent<br />
spaces: Incidences and relevance to chorionic villus sampling.<br />
Prenat Diagn 1991;11:805.<br />
23. Brambati B, Oldrini A, Lanzani A. Transabdominal chorionic villus<br />
sampling: a freehand ultrasound-guided technique. Am J Obstet<br />
Gynecol 1987;157:134.<br />
24. Smidt-Jensen S, Hahnemann N. Transabdominal chorionic villus<br />
sampling for fetal genetic diagnosis. Technical and obstetric evaluation<br />
of 100 cases. Prenat Diagn 1988;8:7.<br />
25. Silver RK, MacGregor SN, Sholl JS, Hobart ED, Waldee JK. An evaluation<br />
of the chorionic villus sampling learning curve. Am J Obstet<br />
Gynecol 1990;163:917-22.<br />
26. Jackson LG, Wapner RJ. Risks of chorionic villus sampling. Clin<br />
Obstet Gynecol 1987;1:513.<br />
27. Brambati B, Oldrini A, Ferrazzi E, et al. Chorionic villus sampling: an<br />
analysis of the obstetric experience of 1000 cases. Prenat Diagn<br />
1987;7:157-69.<br />
28. Brambati B, Matarrelli M, Varotto F. Septic complications after<br />
chorionic villus sampling. Lancet 1987;i(8543):1212a.<br />
29. Wass D, Bennett MJ. Infection and chorionic villus sampling. Lancet<br />
1985;ii:338.<br />
30. Scialli AR, Neugebauer DL, Fabro SE. Microbiology of the endcervix<br />
in patients undergoing chorionic villus sampling. In: Fracearo M,<br />
Simoni G, Brambati B, eds. First Trimester Fetal Diagnosis. Berlin:<br />
Springer-Verlag, 1985:69-73.<br />
31. Brambati B, Varotti F. Infection and chorionic villus sampling.<br />
Lancet 1985;ii:609.<br />
32. Hogge WA, Schonberg SA, Golbus MS. Chorionic villus sampling:<br />
experience of the first 1000 cases. Am J Obstet Gynecol 1986;154:1249.<br />
33. Gilmore DH, McNay MB. Spontaneous fetal loss rate in early pregnancy.<br />
Lancet 1985;i:107.<br />
34. Wilson RD, Kendrick V, Witmann BK. Risks of spontaneous abortion<br />
in ultrasonographically normal pregnancies. Lancet 1984;ii:920.<br />
35. Barela A, Kleinman GE, Golditch IM, et al. Septic shock with renal<br />
failure after chorionic villus sampling. Am J Obstet Gynecol<br />
1986;154:1120.<br />
36. Blakemore KJ, Mahoney MJ, Hobbins JC. Infection and chorionic<br />
villus sampling. Lancet 1985;2:339.<br />
37. Cheng EY, Luth DA, Hickok D, et al. Transcervical chorionic villus<br />
sampling and midtrimester oligohydramnios. Am J Obstet Gynecol<br />
1991;165:1063.<br />
38. Blakemore KJ, Baumgarten A, Schoenfeld-Dimaio M, et al. Rise in<br />
maternal serum alpha-fetoprotein concentration after chorionic villus<br />
sampling. Lancet 1985;ii:339.<br />
39. Bramabati B, Guercilena S, Bonacchi I, et al. Fetomaternal transfusion<br />
after chorionic villus sampling: clinical implications. Hum<br />
Reprod 1986;1:37.
730 Part 3 RISK ASSESSMENT AND THERAPY<br />
40. Shulman LP, Meyers CM, Simpson JL, et al. Fetomaternal transfusion<br />
depends on amount of chorionic villi aspirated but not on<br />
method of chorionic villus sampling. Am J Obstet Gynecol<br />
1990;162:1185.<br />
41. Smidt-Jensen S, Philip J, Zachary J, et al. Implications of maternal<br />
serum alpha-fetoprotein elevation caused by transabdominal and<br />
transcervical CVS. Prenat Diagn 1994;14:35-46.<br />
42. Zipursky A, Israels LG. The pathogenesis and prevention of Rh<br />
immunization. Can Med Assoc J 1967;97:1245-57.<br />
43. Moise KJ, Carpenter RJ. Increased severity of fetal hemolytic disease<br />
with known Rhesus alloimmunization after first trimester transcervical<br />
chorionic villus biopsy. Fetal Diagn Ther 1990;5:76.<br />
44. Clark BA, Bissonnette J, Olson SB, et al. Pregnancy loss in a small<br />
chorionic villus sampling series. Am J Obstet Gynecol 1989;161:301.<br />
45. Green JE, Dorfman A, Jones SL, et al. Chorionic villus sampling:<br />
experience with an initial 940 cases. Obstet Gynecol 1988;71:208.<br />
46. Gustavii B, Claesson V, Kristoffersson U, et al. Risk of miscarriage<br />
after chorionic biopsy is probably not higher than after amniocentesis.<br />
Lakartidningen 1989;86:4221.<br />
47. Jahoda MGJ, Pijpers L, Reuss A, et al. Evaluation of transcervical<br />
chorionic villus sampling with a completed follow-up of 1550 consecutive<br />
pregnancies. Prenat Diagn 1989;9:621.<br />
48. Young SR, Shipley CF, Wade RV, et al. Single-center comparison of<br />
results of 1000 prenatal diagnoses with chorionic villus sampling<br />
and 1000 diagnoses with amniocentesis. Am J Obstet Gynecol<br />
1991;165:255.<br />
49. Hogge WA, Schonberg SA, Golbus MS. Chorionic villus sampling:<br />
experience of the first 1000 cases. Am J Obstet Gynecol 1986;154:1<br />
249-52.<br />
50. Jackson LG. CVS Newslett 1988;25-7.<br />
51. Wade RV, Young SR. Analysis of fetal loss after transcervical chorionic<br />
villus sampling: a review of 719 patients. Am J Obstet Gynecol<br />
1989;161:513-9.<br />
52. Warburton D, Fraser FC. Spontaneous abortion risks in man: data<br />
from reproductive histories collected in a medical genetics unit.<br />
Hum Genet 1964;16:1-25.<br />
53. Simpson JL, Mills ML, Holmes LB, et al. Low fetal loss rates after<br />
ultrasound-proved viability in early pregnancy. JAMA 1987;258:<br />
2555-7.<br />
54. Christiaens GC, Stoutenbeeck P. Spontaneous abortion in proven<br />
intact pregnancies. Lancet 1984;2:571-2.<br />
55. Wilson RD, Kendrick V, Wirtman BP, et al. Spontaneous abortion<br />
and pregnancy outcome after normal first-trimester ultrasound<br />
examination. Obstet Gynecol 1986;67:352-5.<br />
56. Saura R, Gauthier B, Taine L, et al. Operator experiences and fetal<br />
loss rate in transabdominal CVS. Prenat Diagn 1994;14:70.<br />
57. Wapner RJ, Barr MA, Heeger S, et al. Chorionic villus sampling: a<br />
10-year, over 13,000 consecutive case experience (abstract).<br />
Presented at the First Annual Meeting of the American College of<br />
Medical Genetics, Orlando, Florida, March 1994.<br />
58. Nicolaides K, Brizot M de L, Patel F, Snijders R. Comparison of<br />
chorionic villus sampling and amniocentesis for fetal karyotyping at<br />
10-13 weeks’ gestation. Lancet 1994;344(8920):435.<br />
59. Brambati B, Lanzani A, Tului L. Transabdominal and transcervical<br />
chorionic villus sampling: efficacy and risk evaluation of 2411 cases.<br />
Am J Hum Genet 1990;35:160.<br />
60. Brambati B, Terzian E, Tognoni G. Randomized clinical trial of<br />
transabdominal versus transcervical chorionic villus sampling methods.<br />
Prenat Diagn 1991;11:285.<br />
61. Smidt-Jensen S, Permin M, Philip J. Sampling success and risk by<br />
transabdominal chorionic villus sampling, transcervical chorionic<br />
villus sampling and amniocentesis: a randomized study. Ultrasound<br />
Obstet Gynecol 1991;1:86.<br />
62. Chueh JT, Goldberg JD, Wohlfered MM, Golbus MS. Comparison of<br />
transcervical and transabdominal chorionic villus sampling loss<br />
rates in nine thousand cases from a single center. Am J Obstet<br />
Gynecol 1995;173:1277.<br />
63. Firth HV, Boyd P, Chamberlain P, et al. Severe limb abnormalities<br />
after chorion villus sampling at 56-66 days gestation. Lancet<br />
1991;337:726.<br />
64. Hoyme F, Jones KL, Van Allen MI, et al. Vascular pathogenesis of<br />
transverse limb reduction defects. J Pediatr 1982;101:839.<br />
65. Foster-Iskenius U, Baird P. Limb reduction defects in over 1,000,000<br />
consecutive live births. Teratology 1989;39:127.<br />
66. Mastroiacovo P, Botto LD, Cavalcanti DP. Limb anomalies following<br />
chorionic villus sampling: a registry based case control study. Am J<br />
Med Genet 1992;44:856-63.<br />
67. Brambati B, Simoni G, Traui M. Genetic diagnosis by chorionic villus<br />
sampling before 8 gestational weeks: efficiency, reliability, and<br />
risks on 317 completed pregnancies. Prenat Diagn 1992;12:784-99.<br />
68. Hsieh FJ, Shyu MK, Sheu BC, et al. Limb defects after chorionic villus<br />
sampling. Obstet Gynecol 1995;85:84.<br />
69. Burton BK, Schultz CJ, Burd LI. Spectrum of limb disruption defects<br />
associated with chorionic villus sampling. Pediatrics 1993;91:989-93.<br />
70. Froster UG, Jackson L. Limb defects and chorionic villus sampling:<br />
results from an international registry. 1992-1994. Lancet 1996;<br />
347(9000):489.<br />
71. Brent RL. Relationship between uterine vascular clamping, vascular<br />
disruption syndrome and cocaine teratology. Teratology 1990;41:<br />
757.<br />
72. Webster W, Brown-Woodman T. Cocaine as a cause of congenital<br />
malformations of vascular origin: experimental evidence in the rat.<br />
Teratology 1990;41:689.<br />
73. Quintero R, Romero R, Mahoney M, et al. Fetal haemorrhagic<br />
lesions after chorionic villus sampling. Lancet 1992;339:193.<br />
74. Quintero RA, Romero R, Mahoney MJ, et al. Embryoscopic demonstration<br />
of hemoagic lesions on the human embryo after placental<br />
tauma. Am J Obstet Gynecol 1993;168:756-9.<br />
75. Firth HV, Boyd PA, Chamberlain PF, et al. Analysis of limb reduction<br />
defects in babies exposed to chorionic villus sampling. Lancet<br />
1994;343(8905):1069.<br />
76. Olney RS, Khoury MJ, Alo CJ, et al. Increased risk for transverse digital<br />
deficiency after chorionic villus sampling: results of the United<br />
States Multistate Case-Control Study. 1988-1992. Teratology<br />
1995;5(1):20-9.<br />
77. Williams J, Medearis AL, Bear MD, et al. Chorionic villus sampling<br />
is associated with normal fetal growth. Am J Obstet Gynecol 1987;<br />
157:708.<br />
78. Jahoda MGJ, Brandenberg H, Cohen-Overbeek TE, et al. Terminal<br />
transverse limb defects and early chorionic villus sampling: evaluation<br />
of 4,300 cases with completed follow-up. Am J Med Genet<br />
1993;46:483.<br />
79. Halliday J, Lumley J, Sheffield LJ, et al. Limb deficiencies, chorion<br />
villus sampling, and advanced maternal age. Am J Med Genet<br />
1993;47:1096.<br />
80. Schloo R, Miney P, Holzgreve W, et al. Distal limb deficiency following<br />
chorionic villus sampling? Am J Med Genet 1992;42:404.<br />
81. Monni G, Ibba RM, Lai R, et al. Limb-reduction defects and chorion<br />
villus sampling. Lancet 1991;337:1091.<br />
82. Blakemore K, Filkins K, Luthy DA, et al. Cook Obstetrics and<br />
Gynecology Catheter Multicenter Chorionic Villus Sampling Trial:<br />
Comparison of birth defects with expected rates. Am J Obstet<br />
Gynecol 1993;169:1022.<br />
83. Silver RK, Macgregor SN, Muhlbach LH, et al. Congenital malformations<br />
subsequent to chorionic villus sampling: outcome analysis<br />
of 1048 consecutive procedures. Prenat Diagn 1994;14:421.<br />
84. Mahoney MJ for the USNICHD Collaborative CVS Study Group.<br />
Limb abnormalities and chorionic villus sampling. Lancet<br />
1991;37:1422.<br />
85. Jackson LG, Wapner RJ, Brambati B. Limb abnormalities and chorionic<br />
villus sampling. Lancet 1991;337:1423.<br />
86. Smidt-Jensen S, Permin M, Philip J, et al. Randomized comparison<br />
of amniocentesis and transabdominal and transcervical chorionic<br />
villus sampling. Lancet 1992;340:1237.<br />
87. Bissonnette JM, Busch WL, Buckmaster JG, et al. Factors associated<br />
with limb anomalies after chorionic villus sampling (letter). Prenat<br />
Diagn 1993;13:1163-5.<br />
88. Dolk H, Bertrend F, Lechat MF. Chorionic villus sampling and limb<br />
abnormalities. The EUROCAT Working Group. Lancet 1992;<br />
339:876.<br />
89. Burton BK, Schulz CH, Burd LI. Limb anomalies associated with<br />
chorionic villus sampling. Obstet Gynecol 1992;79:726.<br />
90. Mastroiacovo P, Tozzi AE, Agosti S, et al. Transverse limb reduction<br />
defects after chorion villus sampling: a retrospective cohort study.<br />
Prenat Diagn 1993;13:1051.<br />
91. Mastroiacovo P, Botto LD. Chorionic villus sampling and transverse<br />
limb deficiencies: maternal age is not a confounder. Am J Med<br />
Genet 1994;53:182.
92. Angue H, Bingru Z, Hong W. Long-term follow-up results after<br />
aspiration of chorionic villi during early pregnancy. In: Fraccaro M,<br />
Simoni G, Brambati B, eds. First Trimester Fetal Diagnosis. New<br />
York: Springer, 1995:1.<br />
93. Martin AO, Simpson JL, Rosinksy BJ, et al. Chorionic villus sampling<br />
in continuing pregnancies II: cytogenetic reliability. Am J Obstet<br />
Gynecol 1986;154:1653-62.<br />
94. Simoni G, Gimelli G, Cuoco C, et al. Discordance between prenatal<br />
cytogenetic diagnosis after chorionic villi sampling and chromosomal<br />
constitution of the fetus. In: Fraccaro M, Simoni G, Brambati B,<br />
eds. First Trimester Fetal Diagnosis. Heidelberg: Springer-Verlag,<br />
1985:137-43.<br />
95. Cheung SW, Crane JP, Beaver HA, et al. Chromosome mosaicism<br />
and maternal cell contamination in chorionic villi. Prenat Diagn<br />
1987;7:535-42.<br />
96. Ledbetter DH, Martin AO, Verlinsky Y, et al. Cytogenetic results of<br />
chorionic villus sampling: high success rate and diagnostic accuracy<br />
in the United States collaborative study. Am J Obstet Gynecol<br />
1990;162:495.<br />
97. Mikkelsen M, Ayme S. Chromosomal findings in chorionic villi. In:<br />
Vogel F, Sperling K, eds. Human Genetics. Heidelberg: Springer-<br />
Verlag, 1987:597.<br />
98. Simoni G, Brambati B, Danesino C, et al. Efficient direct chromosome<br />
analyses and enzyme determinations from chorionic villi samples<br />
in the first trimester of pregnancy. Hum Genet 1983;63:349.<br />
99. Ford JH, Jahnke AB. Handling of chorionic villus for direct chromosome<br />
studies. Lancet 1983;2:1491.<br />
100. Gregson NM, Seabright N. Handling of chorionic villi for direct<br />
chromosome studies. Lancet 1983;2:1491.<br />
101. Chang HC, Jones OW, Masui H. Human amniotic fluid cells grown<br />
in a hormone-supplemented medium: suitability for prenatal diagnosis.<br />
Proc Natl Acad Sci U S A 1982;79:4795.<br />
102. Hogge WA, Schonberg SA, Golbus MS. Prenatal diagnosis by chorionic<br />
villus sampling: lessons of the first 600 cases. Prenat Diagn<br />
1985;5:393.<br />
103. Williams J, Madearis AL, Chun WH, et al. Maternal cell contamination<br />
in cultured chorionic villi: comparison of chromosome<br />
Q-polymorphisms derived from villi, fetal skin, and maternal lymphocytes.<br />
Prenal Diagn 1987;7:315.<br />
104. Ledbetter DH, Zachary JL, Simpson MS, et al. Cytogenetic results<br />
from the U.S. collaborative study on CVS. Prenat Diagn 1992;12:317.<br />
105. Elles RG, Williamson R, Niazi D, et al. Absence of maternal contamination<br />
of chorionic villi used for fetal gene analysis. N Engl J Med<br />
1983;308:1433.<br />
106. Karkut I, Zakrzewski S, Sperling K. Mixed karyotypes obtained by<br />
chorionic villi analysis: mosaicism and maternal contamination. In:<br />
Fraccaro M, Simoni G, Brambati B, eds. First Trimester Fetal<br />
Diagnosis. Heidelberg: Springer-Verlag, 1985:144-6.<br />
107. Markert C, Petters R. Manufactured hexaparenteral mice show that<br />
adults are derived from three embryonic cells. Science 1978;202:56.<br />
108. Wolstenholine J. Confined placental mosaicism for trisomies 2, 3, 7,<br />
8, 9, 16, and 22: their incidence, likely origins, and mechanisms for<br />
cell lineage compartmentalization. Prenat Diag 1996;16:511.<br />
109. Cassidy SB, Lai LW, Erickson RP, et al. Trisomy 15 with loss of the<br />
paternal 15 as a cause of Prader-Willi syndrome due to maternal disomy.<br />
Am J Hum Genet 1992;51:701.<br />
110. Purvis-Smith SG, Sayille T, Manass S, et al. Uniparental disomy 15<br />
resulting from “correction” of an initial trisomy 15. Am J Hum<br />
Genet 1992;50:1348.<br />
111. Ledbetter DH, Engel E. Uniparental disomy in humans: development<br />
of an imprinting map and its implications for prenatal diagnosis.<br />
Hum Mol Genet 1995;4:1757-64.<br />
112. Kalousek DK, Dill FJ, Pantzar T, et al. Confined chorionic mosaicism<br />
in prenatal diagnosis. Hum Genet 1987;77:163.<br />
113. Johnson A, Wapner RJ, Davis GH, et al. Mosaicism in chorionic villus<br />
sampling: an association with poor perinatal outcome. Obstet<br />
Gynecol 1990;75:573.<br />
Chapter 24 Chorionic Villus Sampling<br />
731<br />
114. Wapner RJ, Simpson MS, Golbus MS, et al. Chorionic mosaicism:<br />
association with fetal loss but not with adverse perinatal outcome.<br />
Prenat Diagn 1992;12:347.<br />
115. Goldberg JD, Proter AE, Golbus MS. Current assessment of fetal<br />
losses as a direct consequence of chorionic villus sampling. Am J<br />
Med Genet 1990;35:174.<br />
116. Kalousek DK, Howard-Pebbles PN, Olson SB, et al. Confirmation of<br />
CVS mosaicism in term placentae and high frequency of intrauterine<br />
growth retardation association with confined placental<br />
mosaicism. Prenat Diagn 1991;11:743.<br />
117. Worton RG, Stern RA. Canadian collaborative study of mosaicism in<br />
amniotic fluid cell cultures. Prenat Diagn 1984;4:131.<br />
118. Kalousek DK, Langlois S, Barrett I, et al. Uniparental disomy for<br />
chromosome 16 in humans. Am J Hum Genet 1993;52:8.<br />
119. Post JG, Nijhuis JG. Trisomy 16 confined to the placenta. Prenat<br />
Diagn 1992;12:1001.<br />
120. BENN P. Trisomy 16 and trisomy 16 mosaicism: a review. Am J Med<br />
Genet 1998;79:121-33.<br />
121. Vejerslev LO, Mikkelsen M. The European collaborative study on<br />
mosaicism in chorionic villus sampling: data from 1986-1987. Prenal<br />
Diagn 1989;9:575.<br />
122. Breed ASPM, Mantingh A, Vosters R, et al. Follow-up and pregnancy<br />
outcome after a diagnosis of mosaicism in CVS. Prenat Diagn<br />
1991;11:577.<br />
123. Phillips OP, Tharapel AT, Lerner JL, et al. Risk of fetal mosaicism<br />
when placental mosaicism is diagnosed by chorionic villus sampling.<br />
Am J Obstet Gynecol 1996;174:850.<br />
124. Bartels I, Hansmann I, Holland U, et al. Down syndrome at birth not<br />
detected by first trimester chorionic villus sampling. Am J Med<br />
Genet 1989;34:606.<br />
125. Lilford RJ, Caine A, Linton G, et al. Short-term culture and falsenegative<br />
results for Down’s syndrome on chorionic villus sampling.<br />
Lancet 1991;337:861.<br />
126. Miny P, Basaran S, Holzgreve W, et al. False-negative cytogenetic<br />
result in direct preparations after CVS. Prenat Diagn 1988;8:633.<br />
127. Simoni G, Fraccaro M, Gimelli G, et al. False-positive and falsenegative<br />
findings on chorionic villus sampling. Prenat Diagn<br />
1987;7:671.<br />
128. Martin AO, Elias S, Rosinsky B, et al. False-negative findings on<br />
chorion villus sampling. Lancet 1986;2:391.<br />
129. Grebner EE, Jackson LG. Prenatal diagnosis for Tay-Sachs disease<br />
using chorionic villus sampling. Prenat Diagn 1985;5:313.<br />
130. Galjaard H. Biochemical analyses of chorionic villi: a worldwide survey<br />
of first trimester fetal diagnosis of inborn errors of metabolism.<br />
In: Fraccaro M, Simoni G, Brambati B, eds. First Trimester Fetal<br />
Diagnosis. Berlin: Springer-Verlag, 1985:205.<br />
131. Gray RG, Green A, Cole T, et al. A misdiagnosis of X-linked<br />
adrenoleukodystrophy in cultured chorionic villus cells by the measurement<br />
of very long chain fatty acids. Prenat Diagn 1995;15:486.<br />
132. Castellvi-Bel S, Mila M, Solor A, et al. Prenatal diagnosis of fragile X<br />
syndrome: expansion and methylation of chorionic villus samples.<br />
Prenat Diagn 1995;15:801.<br />
133. Wapner RJ, Johnson A, Davis G, et al. Prenatal diagnosis in twin gestations:<br />
a comparison between second trimester amniocentesis and first<br />
trimester chorionic villus sampling. Obstet Gynecol 1993;82:49-56.<br />
134. Pergament E, Schulman J, Copeland K, et al. The risk of and efficacy<br />
of chorionic villus sampling in multiple gestations. Prenat Diagn<br />
1992;12:377-84.<br />
135. Evans MI, Goldberg J, Horenstein J, et al. Selective termination for<br />
structural chromosomal and mendelian anomalies: International<br />
experience. Obstet Gynecol 1999;180:S31.<br />
136. Evans MI, Wapner RJ, Carpenter R, et al. International collaboration<br />
on multifetal pregnancy reduction: dramatically improved outcomes<br />
with increased experience. Obstet Gynecol 1999;180:S28.<br />
137. Brambati B, Tului L, Lanzana A, et al. First trimester gentic diagnosis<br />
in multiple pregnancies: principles and potential pitfalls. Prenat<br />
Diagn 1991;11:767-74.