Family Medicine
U8UQp U8UQp
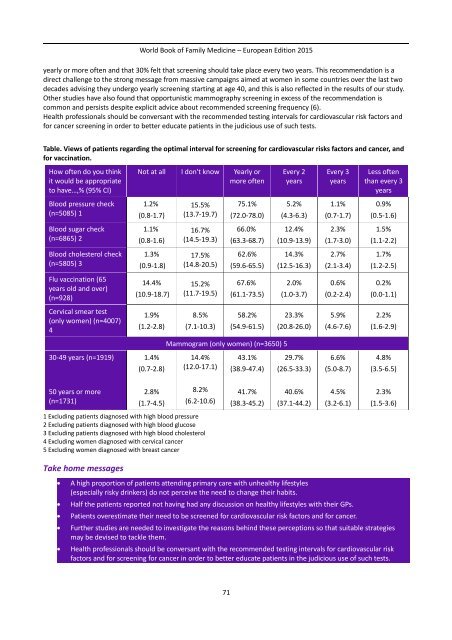
World Book of Family Medicine – European Edition 2015 Carlos Brotons MD, PhD cbrotons@eapsardenya.cat 21 – Prevention and Health Promotion in Clinical Practice Carlos Brotons MD, PhD, on behalf of EUROPREV (European network for prevention and health promotion in GP/FM) Primary health care is a suitable setting for interventions to identify and reduce behavioural risks factors and recommend preventive activities (including immunisations, screening for cardiovascular risk factors and cancer, and counselling). A survey carried out in the year 2000 among 2082 GPs from eleven European countries showed that significant gaps persist between GPs' knowledge and their practice in the use of evidence-based recommendations for health promotion and disease prevention in primary care (1). To complement this GPs’ survey, and in order to explore patients’ views and beliefs on the importance of lifestyle and preventive interventions, another survey was carried out in the year 2008-2009, involving 7947 patients from 22 European countries (2). The results of this survey showed that alcohol drinkers do not see, or fail to admit, that alcohol use is a risky habit that needs to be modified. Less than one third of risky drinkers would like to receive advice concerning alcohol intake from their GPs. It seems that patients are much more conscious about the risk of tobacco, unhealthy diet or sedentary lifestyle than the risk of alcohol. Also, patients reported that they had received less advice (in a discussion initiated by GPs) for alcohol than for tobacco, diet and physical exercise. In another study done in Sweden, only 18% of patients reported that they had received advice at least in one area, with a four-fold variation between the most common type of advice (exercise in 16%) and the rarest type (alcohol in 5%) (3). The view of patients that GPs initiated a discussion on smoking in 63% of cases, eating habits (59% of cases), and physical activity (55%) shows some correlation with the views of GPs in Europe as surveyed in 2000 (1). At that time, GPs declared that they advised smokers to quit in 61 – 71% of cases, and counselled overweight and sedentary patients in 59 – 62% and 54 – 57% of cases respectively. However, in this study patients identified as risky drinkers said that their GPs had only initiated a discussion regarding their alcohol use in 42% while the 2082 doctors participating said they would advise heavy drinkers to reduce consumption in 57 – 64% of cases. Thus while patients and doctors seem to agree regarding the frequency of their discussions on smoking, healthy eating/weight and physical activity, patients seem to have a more negative viewpoint on how often doctors give advice on alcohol use. Table shows the views of patients regarding optimal interval for screening for cardiovascular risk factors and cancer and for vaccination. More than 80% of women think they should be checked for cervical cancer yearly or every two years. However, revised guidelines recommend Pap test screening every three years for women age 30 and older (4). These findings reflect overuse of Pap test screening, which is expensive for the health care system and may result in unnecessary follow-up testing and increased risk for colposcopy-associated illnesses and adverse birth outcomes, as well as distress for patients (5). The survey also showed that 43% of women aged 30-49 thought that screening for breast cancer should be done 70
World Book of Family Medicine – European Edition 2015 yearly or more often and that 30% felt that screening should take place every two years. This recommendation is a direct challenge to the strong message from massive campaigns aimed at women in some countries over the last two decades advising they undergo yearly screening starting at age 40, and this is also reflected in the results of our study. Other studies have also found that opportunistic mammography screening in excess of the recommendation is common and persists despite explicit advice about recommended screening frequency (6). Health professionals should be conversant with the recommended testing intervals for cardiovascular risk factors and for cancer screening in order to better educate patients in the judicious use of such tests. Table. Views of patients regarding the optimal interval for screening for cardiovascular risks factors and cancer, and for vaccination. How often do you think it would be appropriate to have…,% (95% CI) Not at all I don't know Yearly or more often Every 2 years Every 3 years Less often than every 3 years Blood pressure check (n=5085) 1 1.2% (0.8-1.7) 15.5% (13.7-19.7) 75.1% (72.0-78.0) 5.2% (4.3-6.3) 1.1% (0.7-1.7) 0.9% (0.5-1.6) Blood sugar check (n=6865) 2 1.1% (0.8-1.6) 16.7% (14.5-19.3) 66.0% (63.3-68.7) 12.4% (10.9-13.9) 2.3% (1.7-3.0) 1.5% (1.1-2.2) Blood cholesterol check (n=5805) 3 1.3% (0.9-1.8) 17.5% (14.8-20.5) 62.6% (59.6-65.5) 14.3% (12.5-16.3) 2.7% (2.1-3.4) 1.7% (1.2-2.5) Flu vaccination (65 years old and over) (n=928) 14.4% (10.9-18.7) 15.2% (11.7-19.5) 67.6% (61.1-73.5) 2.0% (1.0-3.7) 0.6% (0.2-2.4) 0.2% (0.0-1.1) Cervical smear test (only women) (n=4007) 4 1.9% (1.2-2.8) 8.5% (7.1-10.3) 58.2% (54.9-61.5) 23.3% (20.8-26.0) 5.9% (4.6-7.6) 2.2% (1.6-2.9) Mammogram (only women) (n=3650) 5 30-49 years (n=1919) 1.4% (0.7-2.8) 14.4% (12.0-17.1) 43.1% (38.9-47.4) 29.7% (26.5-33.3) 6.6% (5.0-8.7) 4.8% (3.5-6.5) 50 years or more (n=1731) 2.8% (1.7-4.5) 8.2% (6.2-10.6) 41.7% (38.3-45.2) 40.6% (37.1-44.2) 4.5% (3.2-6.1) 2.3% (1.5-3.6) 1 Excluding patients diagnosed with high blood pressure 2 Excluding patients diagnosed with high blood glucose 3 Excluding patients diagnosed with high blood cholesterol 4 Excluding women diagnosed with cervical cancer 5 Excluding women diagnosed with breast cancer Take home messages A high proportion of patients attending primary care with unhealthy lifestyles (especially risky drinkers) do not perceive the need to change their habits. Half the patients reported not having had any discussion on healthy lifestyles with their GPs. Patients overestimate their need to be screened for cardiovascular risk factors and for cancer. Further studies are needed to investigate the reasons behind these perceptions so that suitable strategies may be devised to tackle them. Health professionals should be conversant with the recommended testing intervals for cardiovascular risk factors and for screening for cancer in order to better educate patients in the judicious use of such tests. 71
- Page 19 and 20: World Book of Family Medicine - Eur
- Page 21 and 22: World Book of Family Medicine - Eur
- Page 23 and 24: World Book of Family Medicine - Eur
- Page 25 and 26: World Book of Family Medicine - Eur
- Page 27 and 28: World Book of Family Medicine - Eur
- Page 29 and 30: World Book of Family Medicine - Eur
- Page 31 and 32: World Book of Family Medicine - Eur
- Page 33 and 34: World Book of Family Medicine - Eur
- Page 35 and 36: World Book of Family Medicine - Eur
- Page 37 and 38: World Book of Family Medicine - Eur
- Page 39 and 40: World Book of Family Medicine - Eur
- Page 41 and 42: World Book of Family Medicine - Eur
- Page 43 and 44: World Book of Family Medicine - Eur
- Page 45 and 46: References: World Book of Family Me
- Page 47 and 48: World Book of Family Medicine - Eur
- Page 49 and 50: World Book of Family Medicine - Eur
- Page 51 and 52: Original Abstract World Book of Fam
- Page 53 and 54: World Book of Family Medicine - Eur
- Page 55 and 56: World Book of Family Medicine - Eur
- Page 57 and 58: World Book of Family Medicine - Eur
- Page 59 and 60: World Book of Family Medicine - Eur
- Page 61 and 62: World Book of Family Medicine - Eur
- Page 63 and 64: World Book of Family Medicine - Eur
- Page 65 and 66: World Book of Family Medicine - Eur
- Page 67 and 68: World Book of Family Medicine - Eur
- Page 69: World Book of Family Medicine - Eur
- Page 73 and 74: World Book of Family Medicine - Eur
- Page 75 and 76: World Book of Family Medicine - Eur
- Page 77 and 78: World Book of Family Medicine - Eur
- Page 79 and 80: World Book of Family Medicine - Eur
- Page 81 and 82: Original abstract World Book of Fam
- Page 83 and 84: World Book of Family Medicine - Eur
- Page 85 and 86: World Book of Family Medicine - Eur
- Page 87 and 88: World Book of Family Medicine - Eur
- Page 89 and 90: World Book of Family Medicine - Eur
- Page 91 and 92: World Book of Family Medicine - Eur
- Page 93 and 94: Original Abstract World Book of Fam
- Page 95 and 96: World Book of Family Medicine - Eur
- Page 97 and 98: World Book of Family Medicine - Eur
- Page 99 and 100: World Book of Family Medicine - Eur
- Page 101 and 102: World Book of Family Medicine - Eur
- Page 103 and 104: World Book of Family Medicine - Eur
- Page 105 and 106: World Book of Family Medicine - Eur
- Page 107 and 108: References World Book of Family Med
- Page 109 and 110: World Book of Family Medicine - Eur
- Page 111 and 112: World Book of Family Medicine - Eur
- Page 113 and 114: World Book of Family Medicine - Eur
- Page 115 and 116: World Book of Family Medicine - Eur
- Page 117 and 118: World Book of Family Medicine - Eur
- Page 119 and 120: World Book of Family Medicine - Eur
World Book of <strong>Family</strong> <strong>Medicine</strong> – European Edition 2015<br />
yearly or more often and that 30% felt that screening should take place every two years. This recommendation is a<br />
direct challenge to the strong message from massive campaigns aimed at women in some countries over the last two<br />
decades advising they undergo yearly screening starting at age 40, and this is also reflected in the results of our study.<br />
Other studies have also found that opportunistic mammography screening in excess of the recommendation is<br />
common and persists despite explicit advice about recommended screening frequency (6).<br />
Health professionals should be conversant with the recommended testing intervals for cardiovascular risk factors and<br />
for cancer screening in order to better educate patients in the judicious use of such tests.<br />
Table. Views of patients regarding the optimal interval for screening for cardiovascular risks factors and cancer, and<br />
for vaccination.<br />
How often do you think<br />
it would be appropriate<br />
to have…,% (95% CI)<br />
Not at all I don't know Yearly or<br />
more often<br />
Every 2<br />
years<br />
Every 3<br />
years<br />
Less often<br />
than every 3<br />
years<br />
Blood pressure check<br />
(n=5085) 1<br />
1.2%<br />
(0.8-1.7)<br />
15.5%<br />
(13.7-19.7)<br />
75.1%<br />
(72.0-78.0)<br />
5.2%<br />
(4.3-6.3)<br />
1.1%<br />
(0.7-1.7)<br />
0.9%<br />
(0.5-1.6)<br />
Blood sugar check<br />
(n=6865) 2<br />
1.1%<br />
(0.8-1.6)<br />
16.7%<br />
(14.5-19.3)<br />
66.0%<br />
(63.3-68.7)<br />
12.4%<br />
(10.9-13.9)<br />
2.3%<br />
(1.7-3.0)<br />
1.5%<br />
(1.1-2.2)<br />
Blood cholesterol check<br />
(n=5805) 3<br />
1.3%<br />
(0.9-1.8)<br />
17.5%<br />
(14.8-20.5)<br />
62.6%<br />
(59.6-65.5)<br />
14.3%<br />
(12.5-16.3)<br />
2.7%<br />
(2.1-3.4)<br />
1.7%<br />
(1.2-2.5)<br />
Flu vaccination (65<br />
years old and over)<br />
(n=928)<br />
14.4%<br />
(10.9-18.7)<br />
15.2%<br />
(11.7-19.5)<br />
67.6%<br />
(61.1-73.5)<br />
2.0%<br />
(1.0-3.7)<br />
0.6%<br />
(0.2-2.4)<br />
0.2%<br />
(0.0-1.1)<br />
Cervical smear test<br />
(only women) (n=4007)<br />
4<br />
1.9%<br />
(1.2-2.8)<br />
8.5%<br />
(7.1-10.3)<br />
58.2%<br />
(54.9-61.5)<br />
23.3%<br />
(20.8-26.0)<br />
5.9%<br />
(4.6-7.6)<br />
2.2%<br />
(1.6-2.9)<br />
Mammogram (only women) (n=3650) 5<br />
30-49 years (n=1919)<br />
1.4%<br />
(0.7-2.8)<br />
14.4%<br />
(12.0-17.1)<br />
43.1%<br />
(38.9-47.4)<br />
29.7%<br />
(26.5-33.3)<br />
6.6%<br />
(5.0-8.7)<br />
4.8%<br />
(3.5-6.5)<br />
50 years or more<br />
(n=1731)<br />
2.8%<br />
(1.7-4.5)<br />
8.2%<br />
(6.2-10.6)<br />
41.7%<br />
(38.3-45.2)<br />
40.6%<br />
(37.1-44.2)<br />
4.5%<br />
(3.2-6.1)<br />
2.3%<br />
(1.5-3.6)<br />
1 Excluding patients diagnosed with high blood pressure<br />
2 Excluding patients diagnosed with high blood glucose<br />
3 Excluding patients diagnosed with high blood cholesterol<br />
4 Excluding women diagnosed with cervical cancer<br />
5 Excluding women diagnosed with breast cancer<br />
Take home messages<br />
<br />
<br />
<br />
<br />
<br />
A high proportion of patients attending primary care with unhealthy lifestyles<br />
(especially risky drinkers) do not perceive the need to change their habits.<br />
Half the patients reported not having had any discussion on healthy lifestyles with their GPs.<br />
Patients overestimate their need to be screened for cardiovascular risk factors and for cancer.<br />
Further studies are needed to investigate the reasons behind these perceptions so that suitable strategies<br />
may be devised to tackle them.<br />
Health professionals should be conversant with the recommended testing intervals for cardiovascular risk<br />
factors and for screening for cancer in order to better educate patients in the judicious use of such tests.<br />
71