Check GAD antibody positivity with the Diamyd anti-GAD RIA plate*
GAD in Metabolic - Diamyd Medical AB GAD in Metabolic - Diamyd Medical AB
GADGAD in GraphsGAD ELISPOT outperforms proliferationassays for detection of GADreactiveT cellsStimulation IndexIL-5 (pg/ml)121086420300250200150100500Control Type 2 Type 1*(n=23) (n=12) (n=31)Kotani et al (2002) Detection of GAD65 reactiveT cells in Type 1 diabetes by immunoglobulinfreeELISPOT assays. Diabetes Care 25:1390-1397• Cellular immune responses toß-cell autoantigens were studiedby proliferation and ELISPOT inPMBCs of Type 1, Type 2 diabetespatients and healthy controls• GAD65-specific proliferation wasdetected in 32% Type 1 patients,while IFN-γ ELISPOT GAD65-specificactivity was detected in 66% patientsImmunization with a GAD65/IL-4plasmid DNA vaccine prevents diabetesin NOD miceCMedium*untreatedHELGADGAD/IL-4GAD65 HSP60 CPHTisch et al. (2001) Antigen-specific mediatedsuppression of cell autoimmunity by plasmidDNA vaccination.J Immunol 166:2122-2132p=.003• Enhanced secretion of IL-5 anddecreased secretion of IFN-γ by Tcells from NOD mice immunized at12 wks old with pDNA encodingGAD65-IgFc and IL-4 and restimulatedwith GAD65.• Vaccination caused a shift in cytokineresponse to GAD65 stimulation*Human T Cells RecognizingGAD65 in Type 1a DiabetesODavid Hafler, Jack Sadie, David Breakstone and Sally Kentur laboratory has beeninterested in the functionof autoreactive T cells inhumans with autoimmunedisease and in particular,Multiple Sclerosis (MS) formany years. The T cell response is regulated in partthrough two signaling events. The first signal isthrough the T cell receptor by peptide processedfrom an antigen in the context MajorHistocompatibility Complex (MHC) proteins onan antigen-presenting cell (APC) and the second isthrough costimulation proteins, CD28 and CTLA-4by B7-1 and B7-2 proteins on APCs. We and othershad previously found that myelin basic protein(MBP) reactive T cells in patients with MS werecostimulation-independent (second signal) as comparedto T cells from normal individuals. This indicatesthat the autoreactive T cells behaved morelike T cells in a memory response and that the patienthas had T cells reactive to MBP for some time.This also suggests a method for differentiating patientT cell responses from those of controls andways of intervening in the autodestructive immuneresponse by the T cells.These data prompted us to examine this issuein Type 1 diabetes. Insulin-dependent Type 1a diabetesis an autoimmune disease mediated by Tlymphocytes recognizing pancreatic islet cell antigens.Glutamic acid decarboxylase 65 (GAD65)appears to be an important autoantigen in the disease.We found that in patients with new-onsetType 1a diabetes, GAD65-reactive T cells werestrikingly less dependent on CD28 and B7-1 costimulationto enter into cell cycle and proliferatethan were equivalent cells derived from healthycontrols. B7-2 appears to be the primary costimulatorymolecule engaging CD28 in T cell activationof GAD65-reactive T cells, and its engagementwith CTLA-4 appears to deliver a negativesignal. We hypothesize that these autoreactive Tcells have been activated in vivo and have differentiatedinto memory cells, suggesting a pathogenicrole in Type 1 diabetes. These findings stronglyindicate that the activation state of antigen-specificcells plays a role in the autoimmune processand selected costimulatory molecules may representthe target of future therapies.We are currently utilizing GAD65 for other studiesin Type 1a diabetes. These include studies examiningthe quantitation and phenotype of GAD65reactive T cells from controls and Type 1 diabeticswith a GAD peptide-loaded tetramer (HLADR*0401 loaded with GAD p555-567) and monitoringpotentially destructive GAD65 T cell autoreactiveresponses in long-term Type 1a diabetics receivingislet transplants. We are enthusiastic to continueto utilize GAD65 as a means of examining autoreactiveT cellresponses inhuman Type 1adiabetes.David Hafler, MD. is Professor of Neurology(Neuroscience) at Brigham and Women’sHospital and Harvard Medical School inBoston, MA., and the head of the MolecularImmunology Laboratory. Hafler’s main clinicaland research interests are in human autoimmunediseases: Multiple Sclerosis, Type 1diabetes and rheumatoid arthritis. His goalsare to understand the nature of self-recognitionby T cells, to understand how that immuneresponse leads to autoimmune disease andhow one can alter this response to developnovel therapiesSally Kent, Ph.D., is an Instructor in Neurologyand Associate Immunologist at Brigham andWomen’s Hospital and Harvard MedicalSchool in Boston, MA. Kent has specialized inNKT cell function in Type 1a diabetics by examiningperipheral blood and pancreatic draininglymph nodes. In Type 1a diabetes, Kenthas focused on GAD65 T cell reactivity as ameasure of autoreactivity and memory T cellresponses in controls and patients and inpatients undergoing islet cell transplantation.page 28 dmccad june 2003
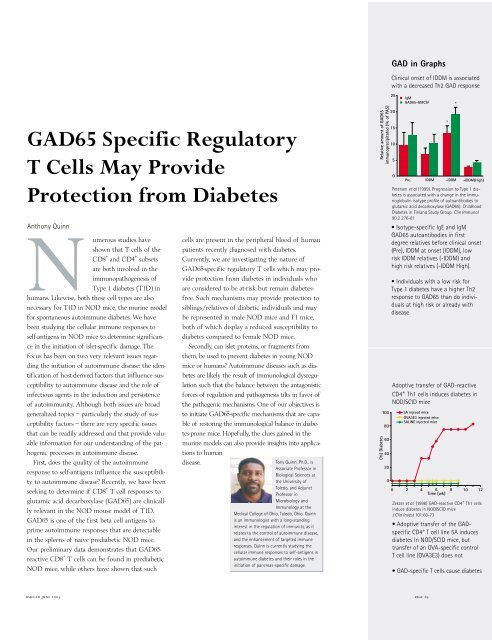
GAD in GraphsGAD65 Specific RegulatoryT Cells May ProvideProtection from DiabetesNAnthony Quinnumerous studies haveshown that T cells of theCD8 + and CD4 + subsetsare both involved in theimmunopathogenesis ofType 1 diabetes (T1D) inhumans. Likewise, both these cell types are alsonecessary for T1D in NOD mice, the murine modelfor spontaneous autoimmune diabetes. We havebeen studying the cellular immune responses toself-antigens in NOD mice to determine significancein the initiation of islet-specific damage. Thefocus has been on two very relevant issues regardingthe initiation of autoimmune disease: the identificationof host-derived factors that influence susceptibilityto autoimmune disease and the role ofinfectious agents in the induction and persistenceof autoimmunity. Although both issues are broadgeneralized topics – particularly the study of susceptibilityfactors – there are very specific issuesthat can be readily addressed and that provide valuableinformation for our understanding of the pathogenicprocesses in autoimmune disease.First, does the quality of the autoimmuneresponse to self-antigens influence the susceptibilityto autoimmune disease? Recently, we have beenseeking to determine if CD8 + T cell responses toglutamic acid decarboxylase (GAD65) are clinicalllyrelevant in the NOD mouse model of T1D.GAD65 is one of the first beta cell antigens toprime autoimmune responses that are detectablein the spleens of naive prediabetic NOD mice.Our preliminary data demonstrates that GAD65-reactive CD8 + T cells can be found in prediabeticNOD mice, while others have shown that suchcells are present in the peripheral blood of humanpatients recently diagnosed with diabetes.Currently, we are investigating the nature ofGAD65-specific regulatory T cells which may provideprotection from diabetes in individuals whoare considered to be at-risk but remain diabetesfree.Such mechanisms may provide protection tosiblings/relatives of diabetic individuals and maybe represented in male NOD mice and F1 mice,both of which display a reduced susceptibility todiabetes compared to female NOD mice.Secondly, can islet proteins, or fragments fromthem, be used to prevent diabetes in young NODmice or humans? Autoimmune diseases such as diabetesare likely the result of immunological dysregulationsuch that the balance between the antagonisticforces of regulation and pathogenesis tilts in favor ofthe pathogenic mechanisms. One of our objectives isto initiate GAD65-specific mechanisms that are capableof restoring the immunological balance in diabetes-pronemice. Hopefully, the clues gained in themurine models can also provide insights into applicationsto humandisease.Tony Quinn, Ph.D., isAssociate Professor inBiological Sciences atthe University ofToledo, and AdjunctProfessor inMicrobiology andImmunology at theMedical College of Ohio, Toledo, Ohio. Quinnis an immunologist with a long-standinginterest in the regulation of immunity, as itrelates to the control of autoimmune disease,and the enhancement of targeted immuneresponses. Quinn is currently studying thecellular immune responses to self-antigens inautoimmune diabetes and their roles in theinitiation of pancreas-specific damage.Relative amount of GAD65immunoprecipitated (% of PAS)(%) Diabetes10080604020Clinical onset of IDDM is associatedwith a decreased Th2 GAD response2520151050IgMGAD65-GMCSFPre. IDDM -IDDM -IDDM(High)Petersen et al (1999). Progression to Type 1 diabetesis associated with a change in the immunoglobulinisotype profile of autoantibodies toglutamic acid decarboxylase (GAD65). ChildhoodDiabetes in Finland Study Group. Clin Immunol90:2 276-81• Isotype-specific IgE and IgMGAD65 autoantibodies in firstdegree relatives before clinical onset(Pre), IDDM at onset (IDDM), lowrisk IDDM relatives (-IDDM) andhigh risk relatives (-IDDM High).• Individuals with a low risk forType 1 diabetes have a higher Th2response to GAD65 than do individualsat high risk or already withdiseaseAdoptive transfer of GAD-reactiveCD4 + Th1 cells induces diabetes inNOD/SCID mice5A injeced miceOVA3E3 injected miceSALINE injected mice00 2 4 6 8 10 12Time (wk)Zekzer et al. (1998) GAD-reactive CD4 + Th1 cellsinduce diabetes in NOD/SCID miceJ Clin Invest 101:68-73• Adoptive transfer of the GADspecificCD4 + T cell line 5A inducesdiabetes In NOD/SCID mice, buttransfer of an OVA-specific controlT cell line (OVA3E3) does not• GAD-specific T cells cause diabetes**dmccad june 2003page 29
- Page 4 and 5: forewordResearch Scientists through
- Page 6 and 7: The Story ofGADRobert Dinsmoor1975R
- Page 8 and 9: Åke Lernmark, MD, Ph.D., and his c
- Page 10 and 11: theory, the immune system mistakenl
- Page 12 and 13: GAD Back to the Future…Åke Lernm
- Page 14 and 15: 100GAD in GraphsGAD65 DNA vaccinati
- Page 16 and 17: In Nature, Anything that CanHappen
- Page 18 and 19: References1. Baekkeskov, S., et al,
- Page 20 and 21: GAD in GraphsIncidence of diabetes
- Page 22 and 23: References1. Quinn A, et al,MHC cla
- Page 24 and 25: References1. Tisch, R., et al,Induc
- Page 26 and 27: Vaccination with GAD PlasmidSuppres
- Page 30 and 31: GAD in GraphsA1004 wks of age% Inci
- Page 32 and 33: Mark Atkinson, Ph.D.,is an American
- Page 34 and 35: GAD in GraphsIL-4 (pg/ml)2501007550
- Page 36 and 37: References1. Kobayashi T, et al,Isl
- Page 38 and 39: References1. A.Falorni, et al,Radio
- Page 40 and 41: References1. Chattopadhyay, S., et
- Page 42 and 43: Diamyd’s Commercial Development o
- Page 44: T cell GAD65For use of GAD in immun
<strong>GAD</strong> in Graphs<strong>GAD</strong>65 Specific RegulatoryT Cells May ProvideProtection from DiabetesNAnthony Quinnumerous studies haveshown that T cells of <strong>the</strong>CD8 + and CD4 + subsetsare both involved in <strong>the</strong>immunopathogenesis ofType 1 diabetes (T1D) inhumans. Likewise, both <strong>the</strong>se cell types are alsonecessary for T1D in NOD mice, <strong>the</strong> murine modelfor spontaneous autoimmune diabetes. We havebeen studying <strong>the</strong> cellular immune responses toself-<strong>anti</strong>gens in NOD mice to determine significancein <strong>the</strong> initiation of islet-specific damage. Thefocus has been on two very relevant issues regarding<strong>the</strong> initiation of autoimmune disease: <strong>the</strong> identificationof host-derived factors that influence susceptibilityto autoimmune disease and <strong>the</strong> role ofinfectious agents in <strong>the</strong> induction and persistenceof autoimmunity. Although both issues are broadgeneralized topics – particularly <strong>the</strong> study of susceptibilityfactors – <strong>the</strong>re are very specific issuesthat can be readily addressed and that provide valuableinformation for our understanding of <strong>the</strong> pathogenicprocesses in autoimmune disease.First, does <strong>the</strong> quality of <strong>the</strong> autoimmuneresponse to self-<strong>anti</strong>gens influence <strong>the</strong> susceptibilityto autoimmune disease? Recently, we have beenseeking to determine if CD8 + T cell responses toglutamic acid decarboxylase (<strong>GAD</strong>65) are clinicalllyrelevant in <strong>the</strong> NOD mouse model of T1D.<strong>GAD</strong>65 is one of <strong>the</strong> first beta cell <strong>anti</strong>gens toprime autoimmune responses that are detectablein <strong>the</strong> spleens of naive prediabetic NOD mice.Our preliminary data demonstrates that <strong>GAD</strong>65-reactive CD8 + T cells can be found in prediabeticNOD mice, while o<strong>the</strong>rs have shown that suchcells are present in <strong>the</strong> peripheral blood of humanpatients recently diagnosed <strong>with</strong> diabetes.Currently, we are investigating <strong>the</strong> nature of<strong>GAD</strong>65-specific regulatory T cells which may provideprotection from diabetes in individuals whoare considered to be at-risk but remain diabetesfree.Such mechanisms may provide protection tosiblings/relatives of diabetic individuals and maybe represented in male NOD mice and F1 mice,both of which display a reduced susceptibility todiabetes compared to female NOD mice.Secondly, can islet proteins, or fragments from<strong>the</strong>m, be used to prevent diabetes in young NODmice or humans? Autoimmune diseases such as diabetesare likely <strong>the</strong> result of immunological dysregulationsuch that <strong>the</strong> balance between <strong>the</strong> antagonisticforces of regulation and pathogenesis tilts in favor of<strong>the</strong> pathogenic mechanisms. One of our objectives isto initiate <strong>GAD</strong>65-specific mechanisms that are capableof restoring <strong>the</strong> immunological balance in diabetes-pronemice. Hopefully, <strong>the</strong> clues gained in <strong>the</strong>murine models can also provide insights into applicationsto humandisease.Tony Quinn, Ph.D., isAssociate Professor inBiological Sciences at<strong>the</strong> University ofToledo, and AdjunctProfessor inMicrobiology andImmunology at <strong>the</strong>Medical College of Ohio, Toledo, Ohio. Quinnis an immunologist <strong>with</strong> a long-standinginterest in <strong>the</strong> regulation of immunity, as itrelates to <strong>the</strong> control of autoimmune disease,and <strong>the</strong> enhancement of targeted immuneresponses. Quinn is currently studying <strong>the</strong>cellular immune responses to self-<strong>anti</strong>gens inautoimmune diabetes and <strong>the</strong>ir roles in <strong>the</strong>initiation of pancreas-specific damage.Relative amount of <strong>GAD</strong>65immunoprecipitated (% of PAS)(%) Diabetes10080604020Clinical onset of IDDM is associated<strong>with</strong> a decreased Th2 <strong>GAD</strong> response2520151050IgM<strong>GAD</strong>65-GMCSFPre. IDDM -IDDM -IDDM(High)Petersen et al (1999). Progression to Type 1 diabetesis associated <strong>with</strong> a change in <strong>the</strong> immunoglobulinisotype profile of auto<strong>anti</strong>bodies toglutamic acid decarboxylase (<strong>GAD</strong>65). ChildhoodDiabetes in Finland Study Group. Clin Immunol90:2 276-81• Isotype-specific IgE and IgM<strong>GAD</strong>65 auto<strong>anti</strong>bodies in firstdegree relatives before clinical onset(Pre), IDDM at onset (IDDM), lowrisk IDDM relatives (-IDDM) andhigh risk relatives (-IDDM High).• Individuals <strong>with</strong> a low risk forType 1 diabetes have a higher Th2response to <strong>GAD</strong>65 than do individualsat high risk or already <strong>with</strong>diseaseAdoptive transfer of <strong>GAD</strong>-reactiveCD4 + Th1 cells induces diabetes inNOD/SCID mice5A injeced miceOVA3E3 injected miceSALINE injected mice00 2 4 6 8 10 12Time (wk)Zekzer et al. (1998) <strong>GAD</strong>-reactive CD4 + Th1 cellsinduce diabetes in NOD/SCID miceJ Clin Invest 101:68-73• Adoptive transfer of <strong>the</strong> <strong>GAD</strong>specificCD4 + T cell line 5A inducesdiabetes In NOD/SCID mice, buttransfer of an OVA-specific controlT cell line (OVA3E3) does not• <strong>GAD</strong>-specific T cells cause diabetes**dmccad june 2003page 29