GUIDELINES INFORMED CONSENT
guidelines for informed consent - The Dentists Insurance Company
guidelines for informed consent - The Dentists Insurance Company
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
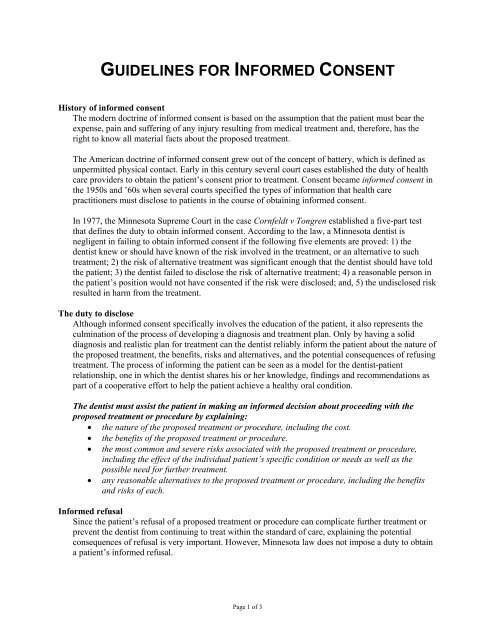
<strong>GUIDELINES</strong> FOR <strong>INFORMED</strong> <strong>CONSENT</strong>History of informed consentThe modern doctrine of informed consent is based on the assumption that the patient must bear theexpense, pain and suffering of any injury resulting from medical treatment and, therefore, has theright to know all material facts about the proposed treatment.The American doctrine of informed consent grew out of the concept of battery, which is defined asunpermitted physical contact. Early in this century several court cases established the duty of healthcare providers to obtain the patient’s consent prior to treatment. Consent became informed consent inthe 1950s and ’60s when several courts specified the types of information that health carepractitioners must disclose to patients in the course of obtaining informed consent.In 1977, the Minnesota Supreme Court in the case Cornfeldt v Tongren established a five-part testthat defines the duty to obtain informed consent. According to the law, a Minnesota dentist isnegligent in failing to obtain informed consent if the following five elements are proved: 1) thedentist knew or should have known of the risk involved in the treatment, or an alternative to suchtreatment; 2) the risk of alternative treatment was significant enough that the dentist should have toldthe patient; 3) the dentist failed to disclose the risk of alternative treatment; 4) a reasonable person inthe patient’s position would not have consented if the risk were disclosed; and, 5) the undisclosed riskresulted in harm from the treatment.The duty to discloseAlthough informed consent specifically involves the education of the patient, it also represents theculmination of the process of developing a diagnosis and treatment plan. Only by having a soliddiagnosis and realistic plan for treatment can the dentist reliably inform the patient about the nature ofthe proposed treatment, the benefits, risks and alternatives, and the potential consequences of refusingtreatment. The process of informing the patient can be seen as a model for the dentist-patientrelationship, one in which the dentist shares his or her knowledge, findings and recommendations aspart of a cooperative effort to help the patient achieve a healthy oral condition.The dentist must assist the patient in making an informed decision about proceeding with theproposed treatment or procedure by explaining:• the nature of the proposed treatment or procedure, including the cost.• the benefits of the proposed treatment or procedure.• the most common and severe risks associated with the proposed treatment or procedure,including the effect of the individual patient’s specific condition or needs as well as thepossible need for further treatment.• any reasonable alternatives to the proposed treatment or procedure, including the benefitsand risks of each.Informed refusalSince the patient’s refusal of a proposed treatment or procedure can complicate further treatment orprevent the dentist from continuing to treat within the standard of care, explaining the potentialconsequences of refusal is very important. However, Minnesota law does not impose a duty to obtaina patient’s informed refusal.Page 1 of 3
Depending on the circumstances, dentists should beware of continuing to treat where the patient’srefusal jeopardizes the possibility for a successful outcome, in which case terminating care may be theonly reasonable option. In any case, a patient’s refusal should be thoroughly documented in thepatient’s chart.Exceptions to disclosureMinnesota law provides several exceptions to the dentist’s duty to obtain informed consent. Adentist is justified in withholding material information from a patient if the disclosure of theinformation could:• complicate or hinder the treatment.• cause such emotional distress as to preclude a rational decision by the patient.• cause psychological harm to the patient.Additionally, the nondisclosure of the information must be consistent with accepted dental practice.The patient’s informed consent is not required in emergency situations where the patient is incapableof consenting. However, there are very few dental emergencies (as distinguished from medicalemergencies in the dental office) that prevent a discussion with the patient before treatment proceeds.Other exceptions to the dentist’s duty to obtain informed consent include situations where the patientis already aware of the risks or where the patient specifically requests not to be informed. Theseexceptions should be used rarely, if at all.The informed consent discussionThe dentist should obtain the patient’s informed consent through a face-to-face discussion thatallows the patient sufficient time to make an informed decision. The discussion should beappropriate to the patient’s level of understanding.Ideally, the informed consent discussion should take place at least several days before treatment, suchas when the dentist presents the treatment plan. Since the dentist is legally obligated to discloseinformation in a manner the patient can understand, the discussion should involve lay terminology,not scientific jargon. For the same reason, consider providing translated informed consent materialsand, if necessary, an interpreter for non-English-speaking patients who may require it. The dentistmust decide what to tell the patient about a procedure based on whether the patient has undergone thesame or similar procedure previously. The use of educational materials is recommended.Because the dentist bears the ultimate responsibility for informing the patient, the informed consentdiscussion cannot be delegated to staff. Although staff can assist by presenting the patient withprinted or audiovisual materials, the dentist should personally solicit and address the patient’squestions and concerns.Informed consent for minor patientsFor minor patients, obtain the informed consent of the parent, custodial parent or legal guardian.Where parents live separately, the patient’s personal information form should indicate which parent isthe custodial parent. Where separated parents share custody, the patient’s record should containletters from each providing consent and authorization to treat. Asking for a parent’s or custodialparent’s blanket consent for emergency treatment in advance of an emergency is one useful way toavoid confusion and delays should the patient require emergency care when a parent or legal guardianis not present. However, this blanket consent should only be relied upon after every reasonableattempt to contact a parent or legal guardian has been made.Page 2 of 3
Documenting informed consentThe patient’s treatment record should document the informed consent discussion and the patient’sdecision.The Board of Dentistry under Section 3100.9600 Recordkeeping, Subpaprgraph 9, requires atminimum, that the patient record document the fact that the dentist discussed with the patient risks,benefits and alternatives of treatment options, and whether the patient consented to or refused theproposed treatment or procedure. Where the proposed treatment or procedure is extensive, invasive orrisky, a written informed consent form is recommended for facilitating and documenting thediscussion. (i.e., extensive: full mouth restoration; invasive: root canal; risky: third molar extractions.)Content of informed consent formsForms for many procedures are available through professional liability insurers, commercial vendorsand dental specialty organizations. Many dentists customize purchased forms or develop their ownforms. Whether purchased or developed by the dentist for his or her own use, adequate forms shouldaddress the nature of the proposed treatment, benefits, risks and alternatives, and the commonconsequences of not performing treatment, as well as enable the dentist to include informationspecific to the case at hand. The form should be signed by the patient and the dentist or a witness. Thepatient should receive a copy of the form and the original should be kept in the patient’s chart.Summary• Obtaining informed consent involves providing the patient with information about the natureof the proposed treatment, the benefits and alternatives of the proposed treatment, the risks oftreatment, as well as any other information specific to the patient’s unique condition. Patientswho refuse treatment must be informed of the potential consequences of their decision.• Informed consent is a process, not a form. It involves a face-to-face discussion between thedentist and patient, conducted with sufficient time to address all of the patient’s questions andconcerns. The task of obtaining a patient’s informed consent cannot be delegated to staff.• The informed consent discussion should be documented in the patient record, although thelaw does not specify the means. Informed consent forms can be useful for helping the patientretain information, as well as for guiding and documenting the informed consent discussion.• The informed consent discussion, even if properly conducted and documented, does notabsolutely insulate the dentist from an allegation of negligence or lack of informed consent.However, being able to supply documentation of the discussion often dissuades patients frompursuing a complaint. In all cases, thorough documentation greatly increases the dentist’schance of successfully defending against such allegations.For more informationFor more information about informed consent call 800.733.0634 or fax your request to 916.498.6175.Guidelines MNPage 3 of 3








![치아 미백(표백)[TOOTH WHITENING (BLEACHING)]에 대한 정보 동의서](https://img.yumpu.com/52851055/1/190x245/-tooth-whitening-bleaching-.jpg?quality=85)