The Cone Beam specialists - Henry Schein Halas
The Cone Beam specialists - Henry Schein Halas
The Cone Beam specialists - Henry Schein Halas
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Introducing<br />
Body Logic<br />
<strong>The</strong> <strong>Cone</strong> <strong>Beam</strong> Specialists<br />
logic<br />
body<br />
<strong>Henry</strong> <strong>Schein</strong> <strong>Halas</strong> and <strong>Henry</strong> <strong>Schein</strong> Shalfoon are delighted to<br />
introduce Body Logic to its Australia/New Zealand customers.<br />
Read inside to discover how four of the world’s leading cone beam<br />
brands – iCat, Gendex, Morita, Planmeca – will come together under one<br />
umbrella, so that customers will experience unmatched sales expertise<br />
Case RepoR t<br />
and after-sales support from the most experienced and skilled specialist<br />
cone beam team in Australasia.<br />
Extractions Avoided by i-CAT ®<br />
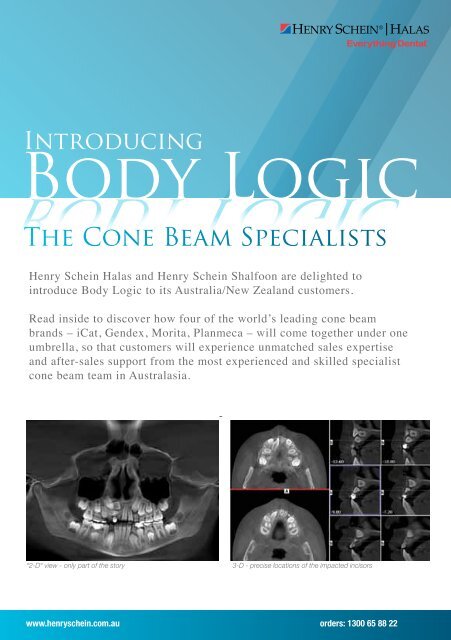
“2-D“ view - only part of the story 3-D - precise locations of the impacted incisors<br />
This 8-year-old male was referred to my office by an oral surgeon. <strong>The</strong> surgeon was tasked with the removal<br />
of both the right lateral and central incisors following a previous orthodontic exam. <strong>The</strong> oral surgeon felt that<br />
through another orthodontic diagnosis and treatment plan utilizing an i-CAT<br />
www.henryschein.com.au orders: 1300 65 88 22<br />
® CBCT scan, both incisors could<br />
be saved. After taking the scan, I realized that the lateral incisor was oriented with the facial surface oriented<br />
buccally. <strong>The</strong> central incisor’s facial surface, on the other hand, was facing the midline of the palate. Both
ody logic<br />
Introducing Body Logic<br />
Body Logic was introduced to the Australian dental<br />
market in 1999 and since that time has established<br />
itself as the leading supplier of <strong>Cone</strong> <strong>Beam</strong> Imaging<br />
systems in Australasia. <strong>The</strong>y have successfully<br />
established the iCAT as Australasia’s #1 choice for<br />
cone beam CT, with a large network of machines<br />
installed across both countries, in general dentistry,<br />
dental specialities and Radiology.<br />
This success has been built on a commitment to<br />
providing equipment of the highest imaging ® quality<br />
and reliability, as well as dedication to providing high<br />
quality continuing education seminars and hands-on<br />
courses to the dental community. <strong>The</strong>se courses<br />
have utilized outstanding international speakers<br />
such as Prof Bill Scarfe and Dr Steve Olmos, and<br />
continually receive outstanding, positive feedback<br />
from attending practitioners.<br />
E REPORT i-CAT<br />
Lisa McAsey<br />
brought a copy of a standard two-dimensional panoramic radiograph from the previous consultation, which<br />
Lisa’s philosophy is simple: honesty, ethical integrity industry is testament to her ability to accept and<br />
demonstrated an un-erupted lower right first bicuspid. <strong>The</strong> 2-D panoramic image showed that the tooth was failing<br />
and prompt service. She measures her success by promote change and to lead the dental industry<br />
to her erupt; relationships however, with it was her difficult clients to and determine by exceeding exactly what in was innovation. preventing Her the relationships eruption, vital with information her clients necessary are<br />
before their expectations the proper diagnosis & satisfaction and treatment with quality plan services could be developed. invaluable An and i-CAT she endeavours to promote their<br />
and products.<br />
success at all times.<br />
Lisa’s approach is one that respects all aspects of Lisa is a problem solver, a lateral thinker and a<br />
the business process. She understands the absolute pioneer in the dental industry with a wonderful<br />
need for consistency in support and supply so that reputation, born of unyielding loyalty. Her family life is<br />
her clients can have the confidence to run their central to her beliefs and the motivation to fulfill her<br />
businesses as they choose. Her longevity in the potential and help others to achieve theirs.<br />
® 3-D cone beam scan clearly revealed<br />
the development of a supernumerary tooth with a full crown, inhibiting the eruption of the impacted bicuspid.<br />
With multiple views, sections, and renderings at my disposal, I had the good fortune of sharing my findings with the<br />
parents and the patient. <strong>The</strong> vividness of the views on my monitor during the consultation clearly left a favorable<br />
impression on both the parents and the patient.<br />
...Case continued on next page<br />
2<br />
Impacted bicuspid superimposed in 2-D<br />
We are now able to introduce Body Logic to a wider<br />
market, to leverage this expertise and commitment to<br />
a wider cone beam audience – which includes existing<br />
users of Gendex, Morita and Planmeca cone beam<br />
equipment, and, of course, to all prospective purchasers<br />
and anyone interested in finding our more about the<br />
benefits of <strong>Cone</strong> <strong>Beam</strong> Imaging for their patients and<br />
treatment planning.<br />
Existing iCat users will of course continue to receive the<br />
excellent after-sales support they are accustomed to<br />
and we will also be able to integrate and streamline the<br />
support that <strong>Henry</strong> <strong>Schein</strong> cone beam customers have<br />
received vi their own DI Support line. By creating a larger<br />
team of people who are specialized and totally dedicated<br />
to <strong>Cone</strong> <strong>Beam</strong> Imaging, we are indeed recognizing the<br />
importance of this area to dentistry, and ensuring that all<br />
our customers and prospective customers receive advice<br />
and support which is unparalleled.<br />
Unusual Impaction Revealed by i-CAT ®<br />
Supernumerary tooth with a full crown<br />
This following case involves a young teenage patient who presented to my office for a second opinion. This is a nice<br />
illustration General of Manager<br />
how even simple dental findings with the i-CAT ® can convert consultations into starts. <strong>The</strong> parents
Brett Butcher<br />
Sales and Marketing Manager<br />
Brett Butcher has held the position of Sales and<br />
Marketing Manager since 2005 and, in that time, he<br />
has guided the company to a position of market leader<br />
in the highly competitive field of 3D Dental Imaging.<br />
As well as exceptional sales and insightful marketing<br />
skills, Brett recognises his obligation and responsibility<br />
to our Health Care Professional clients and is<br />
committed to understanding their needs and supplying<br />
Laszlo Varkovi<br />
Sales Specialist<br />
Laszlo has developed an impressive career firstly with<br />
<strong>Halas</strong> Dental, then since 2005 with <strong>Henry</strong> <strong>Schein</strong> <strong>Halas</strong>.<br />
His experience was gained initially as a territory<br />
manager for consumables, and then in recent years<br />
as an equipment sales specialist. As a result of this<br />
grounding, he has developed a strong understanding<br />
of how dental practices tick, and a keen sense of<br />
what dentists require from their industry suppliers and<br />
representatives.<br />
Craig Cannons<br />
Technical & Training Manager<br />
Craig became part of our team in October 2007, having<br />
spent more than 20 years in the dental industry. His<br />
vast experience in product management and training<br />
and his technical prowess made him the perfect<br />
candidate to take on the role which we consider to be<br />
a priority, that of ensuring that all clients receive the<br />
highest level of support with limited downtime.<br />
With close to 60 machines under his care this is an<br />
extremely demanding role and one he performs to<br />
the highest standard. This level of support has helped<br />
forge Body Logic’s exceptional reputation for customer<br />
service and support.<br />
) Orders: 1300 65 88 22 8 www.henryschein.com.au<br />
products which will aid and support his clients and their<br />
patients.<br />
Brett also has a high degree of technical knowledge<br />
which puts him in the unique position of being able to<br />
offer support, clear communication and knowledgeable<br />
assistance. This, combined with his personal drive and<br />
commitment, places him in a class of his own.<br />
His success has been built around partnering with<br />
customers to help them achieve their ideal and unique<br />
surgery set-up, and guiding them through what can<br />
often be a difficult and drawn out process.<br />
He has a keen interest in dental imaging, and is now<br />
delighted to be joining the Body Logic team, to be able<br />
to continue to offer customers high levels of support in<br />
the specialized area of cone beam imaging.<br />
Craig also conducts all onsite customer training for new<br />
users and owners and, again, his attention to detail and<br />
his development of our comprehensive training ensures<br />
all users are competent and proficient in the operation<br />
of their iCAT, making the transition to 3D a smooth and<br />
successful one.<br />
Craig’s adept ability to resolve problems in a timely<br />
manner and delegate where needed ensures this<br />
department is cornerstone for Body Logic’s success<br />
in the 3D market.<br />
3
ody logic<br />
4<br />
Experience | Training | Education | Maintenance | Support | Expertise<br />
Australia’s #1<br />
Choice for<br />
<strong>Cone</strong> <strong>Beam</strong> CT
Experience the new<br />
GXCB-500<br />
the latest in cone beam 3-D<br />
imaging technology.<br />
• Standard Scan Mode - 8 cm by 8 cm<br />
• Extended Diameter Scan (EDS) Mode<br />
- 14 cm by 8 cm<br />
• Captures vital anatomical structures<br />
• Also easily switches to 2-D panoramic<br />
projections with the same sensor<br />
• Exceptional scan and reconstruction time<br />
) Orders: 1300 65 88 22 8 www.henryschein.com.au<br />
5
ody logic<br />
CASE REPORT i-CAT<br />
CASE REPORT i-CAT<br />
6<br />
Extractions Avoided by i-CAT ®<br />
Extractions Avoided by i-CAT ®<br />
“2-D“ view - only part of the story<br />
“2-D“ view - only part of the story<br />
®<br />
®<br />
3-D - precise locations of the impacted incisors<br />
3-D - precise locations of the impacted incisors<br />
This 8-year-old male was referred to my office by an oral surgeon. <strong>The</strong> surgeon<br />
was tasked with the removal of both the right lateral and central incisors following a<br />
This 8-year-old male was referred to my office by an oral surgeon. <strong>The</strong> surgeon was tasked with the removal of both<br />
the right lateral and central incisors following a previous orthodontic exam. <strong>The</strong> oral surgeon felt that through another<br />
orthodontic diagnosis and treatment plan utilizing an i-CAT ® This 8-year-old male was referred to my office by an oral surgeon. <strong>The</strong> surgeon was tasked with the removal of both<br />
the right lateral and central incisors following a previous orthodontic CBCT scan, exam. both <strong>The</strong> incisors oral surgeon could be felt saved. that through After taking another the<br />
scan, orthodontic I realized diagnosis that the and lateral treatment incisor plan was utilizing oriented an with i-CAT the facial surface oriented buccally. <strong>The</strong> central incisor’s facial<br />
surface, on the other hand, was facing the midline of the palate. Both incisors were horizontally stacked with the<br />
central positioned above the lateral incisor.<br />
Determination of the orientations of the incisors is not possible with just a panoramic-type image, as illustrated by the<br />
reconstructed pan from the scan data (image on the left). However, the axial images from the CBCT scan demonstrate<br />
the orientation of both teeth. <strong>The</strong> cross-sectional views further demonstrate the horizontal “stacking” of both teeth<br />
(image on the right).<br />
A Phase I treatment plan was devised that included rapid maxillary expansion followed by upper fixed appliances. After<br />
expansion, along with leveling and aligning the arch, guided eruption techniques will be employed to bring both incisors<br />
into the arch form during Phase I treatment.<br />
...Case continued on next page<br />
® previous orthodontic exam. <strong>The</strong> oral surgeon felt that through another orthodontic<br />
diagnosis and treatment plan utilizing an i-CAT<br />
CBCT scan, both incisors could be saved. After taking the<br />
scan, I realized that the lateral incisor was oriented with the facial surface oriented buccally. <strong>The</strong> central incisor’s facial<br />
surface, on the other hand, was facing the midline of the palate. Both incisors were horizontally stacked with the<br />
central positioned above the lateral incisor.<br />
Determination of the orientations of the incisors is not possible with just a panoramic-type image, as illustrated by the<br />
reconstructed pan from the scan data (image on the left). However, the axial images from the CBCT scan demonstrate<br />
the orientation of both teeth. <strong>The</strong> cross-sectional views further demonstrate the horizontal “stacking” of both teeth<br />
(image on the right).<br />
A Phase I treatment plan was devised that included rapid maxillary expansion followed by upper fixed appliances. After<br />
expansion, along with leveling and aligning the arch, guided eruption techniques will be employed to bring both incisors<br />
into the arch form during Phase I treatment.<br />
...Case continued on next page<br />
® CBCT scan, both incisors could be<br />
saved. After taking the scan, I realized that the lateral incisor was oriented with the<br />
facial surface oriented buccally. <strong>The</strong> central incisor’s facial surface, on the other<br />
hand, was facing the midline of the palate. Both incisors were horizontally stacked<br />
with the central positioned above the lateral incisor.Determination of the orientations<br />
of the incisors is not possible with just a panoramic-type image, as illustrated by the<br />
reconstructed pan from the scan data (image on the left). However, the axial images<br />
from the CBCT scan demonstrate the orientation of both teeth. <strong>The</strong> cross-sectional<br />
views further demonstrate the horizontal “stacking” of both teeth (image on the right).<br />
A Phase I treatment plan was devised that included rapid maxillary expansion followed<br />
by upper fixed appliances. After expansion, along with leveling and aligning the arch,<br />
guided eruption techniques will be employed to bring both incisors into the arch form<br />
during Phase I treatment.<br />
Bradford N. Edgren, DDS, MS<br />
Bradford N. Edgren, DDS, MS<br />
Dr. Bradford Edgren earned both his Doctorate of Dental Surgery, as Valedictorian, and<br />
Dr. Bradford Edgren earned both his Doctorate of Dental Surgery, as Valedictorian, and<br />
his Master of Science in Orthodontics from University of Iowa, College of Dentistry. He is<br />
his Master of Science in Orthodontics from University of Iowa, College of Dentistry. He is<br />
a Diplomate of the American Board of Orthodontics and an affiliate member of the SW<br />
a Diplomate of the American Board of Orthodontics and an affiliate member of the SW<br />
Angle Society. Dr. Edgren has presented to numerous groups on the value of CBCT and<br />
Angle Society. Dr. Edgren has presented to numerous groups on the value of CBCT and<br />
cephalometrics. His articles have been published in both the AJODO and American Journal<br />
cephalometrics. His articles have been published in both the AJODO and American Journal<br />
of Dentistry. Dr. Edgren currently has an active private practice in Greeley, CO.<br />
of Dentistry. Dr. Edgren currently has an active private practice in Greeley, CO.
Why 3-D, Why i-CAT ®<br />
i-CAT<br />
®<br />
i-CAT<br />
i-CAT<br />
<strong>The</strong> CBCT scanner scanner will will also also help help me follow me follow the eruption the eruption path of path of<br />
the maxillary right <strong>The</strong> right CBCT canine. scanner Guided Guided will eruption also eruption help techniques me techniques follow may the be eruption may be path of<br />
necessary with the this maxillary this tooth tooth in right the in canine. future the future as Guided treatment as eruption treatment progresses. techniques progresses. may be<br />
Currently, the<br />
the necessary lateral<br />
lateral<br />
incisor<br />
incisor with is this bonded<br />
is tooth bonded<br />
and in the being<br />
and future guided<br />
being as treatment into<br />
guided into progresses.<br />
occlusion. <strong>The</strong> Currently, central incisor the lateral is still incisor horizontally is bonded impacted, and being awaiting guided into<br />
occlusion. <strong>The</strong> central incisor is still horizontally impacted, awaiting<br />
future exposure occlusion. and bonding. <strong>The</strong> central <strong>The</strong> right incisor canine is still is erupting horizontally buccally impacted, awaiting<br />
future exposure and bonding. <strong>The</strong> right canine is erupting buccally<br />
to the lateral incisor. future exposure and bonding. <strong>The</strong> right canine is erupting buccally<br />
to the lateral to incisor. the lateral incisor.<br />
In the past, when addressing impacted teeth, the orthodontist has had to rely upon periapical,<br />
panoramic, and occlusal radiographs to determine the location of impacted teeth. Panoramic<br />
radiographs are suitable for a comprehensive and overall view of the jaws and teeth.<br />
However, panoramic radiographs possess inherent magnification and distortion errors that<br />
result in inconsistent information. Distortion errors with panoramic radiographs can vary from<br />
one part of the film to the next. All the anatomical elements that lie between the x-ray tube<br />
and the film are superimposed upon one another. Moreover, because of the nature of the<br />
focal trough of the panoramic radiograph, important anatomical features, undiagnosed<br />
pathologies, and/or teeth may lie outside the radiographic image. I have multiple cases where<br />
impacted teeth were missed on a standard 2-D image only to be diagnosed when a CBCT<br />
scan was made. One doesn’t realize how large the distortion errors are in standard 2-D<br />
panoramics until after looking at CBCT scans.<br />
CBCT completely eliminates the superimposition of images or structures outside the area<br />
of interest. Data from a single CBCT scan can be viewed as images in the axial, coronal, and<br />
sagittal planes. This is referred to as multiplanar reformatted imaging. CBCT scans can also<br />
provide cross-sectional images that are extremely useful in cases with impacted teeth. CBCT<br />
images do not possess magnification errors – true anatomic measurements are realizable.<br />
<strong>The</strong>se true anatomic measurements improve surgical predictably as well as reduce surgical<br />
time. Since I have always taken pans plus lateral and frontal cephalograms on all my patients,<br />
the i-CAT ® Why 3-D, Why i-CAT<br />
machine with the EFOV makes it extremely easy to get these images all at once.<br />
I am now able to perform my 3-dimensional cephalometric analyses with a 3-dimensional<br />
machine. I also treat a number of patients with Temporomandibular Disorders. This machine<br />
is great for TMJ imaging. In the past I would take a submental vertex radiograph, calculate the<br />
angulations of the condyles for corrected tomographs, and then finally take the images of the<br />
condyles. This would take a considerable amount of time. Now, with a single scan, I can view<br />
images of the condyles within a matter of minutes.<br />
®<br />
In the past, when addressing impacted teeth, the orthodontist has had to rely upon periapical,<br />
panoramic, and occlusal radiographs to determine the location of impacted teeth. Panoramic<br />
radiographs are suitable for a comprehensive and overall view of the jaws and teeth.<br />
However, panoramic radiographs possess inherent magnification and distortion errors that<br />
result in inconsistent information. Distortion errors with panoramic radiographs can vary from<br />
one part of the film to the next. All the anatomical elements that lie between the x-ray tube<br />
and the film are superimposed upon one another. Moreover, because of the nature of the<br />
focal trough of the panoramic radiograph, important anatomical features, undiagnosed<br />
pathologies, and/or teeth may lie outside the radiographic image. I have multiple cases where<br />
impacted teeth were missed on a standard 2-D image only to be diagnosed when a CBCT<br />
scan was made. One doesn’t realize how large the distortion errors are in standard 2-D<br />
panoramics until after looking at CBCT scans.<br />
CBCT completely eliminates the superimposition of images or structures outside the area<br />
of interest. Data from a single CBCT scan can be viewed as images in the axial, coronal, and<br />
sagittal planes. This is referred to as multiplanar reformatted imaging. CBCT scans can also<br />
provide cross-sectional images that are extremely useful in cases with impacted teeth. CBCT<br />
images do not possess magnification errors – true anatomic measurements are realizable.<br />
<strong>The</strong>se true anatomic measurements improve surgical predictably as well as reduce surgical<br />
time. Since I have always taken pans plus lateral and frontal cephalograms on all my patients,<br />
the i-CAT<br />
Imaging Sciences International<br />
1910 North Penn Road<br />
Hatfield, PA 19440<br />
(800) 205-3570<br />
® Why 3-D, Why i-CAT<br />
machine with the EFOV makes it extremely easy to get these images all at once.<br />
I am now able to perform my 3-dimensional cephalometric analyses with a 3-dimensional<br />
machine. I also treat a number of patients with Temporomandibular Disorders. This machine<br />
is great for TMJ imaging. In the past I would take a submental vertex radiograph, calculate the<br />
angulations of the condyles for corrected tomographs, and then finally take the images of the<br />
condyles. This would take a considerable amount of time. Now, with a single scan, I can view<br />
images of the condyles within a matter of minutes.<br />
®<br />
In the past, when addressing impacted teeth, the orthodontist has had to rely upon periapical,<br />
panoramic, and occlusal radiographs to determine the location of impacted teeth. Panoramic<br />
radiographs are suitable for a comprehensive and overall view of the jaws and teeth.<br />
However, panoramic radiographs possess inherent magnification and distortion errors that<br />
result in inconsistent information. Distortion errors with panoramic radiographs can vary from<br />
one part of the film to the next. All the anatomical elements that lie between the x-ray tube<br />
and the film are superimposed upon one another. Moreover, because of the nature of the<br />
focal trough of the panoramic radiograph, important anatomical features, undiagnosed<br />
pathologies, and/or teeth may lie outside the radiographic image. I have multiple cases where<br />
impacted teeth were missed on a standard 2-D image only to be diagnosed when a CBCT<br />
scan was made. One doesn’t realize how large the distortion errors are in standard 2-D<br />
panoramics until after looking at CBCT scans.<br />
CBCT completely eliminates the superimposition of images or structures outside the area<br />
of interest. Data from a single CBCT scan can be viewed as images in the axial, coronal, and<br />
sagittal planes. This is referred to as multiplanar reformatted imaging. CBCT scans can also<br />
provide cross-sectional images that are extremely useful in cases with impacted teeth. CBCT<br />
images do not possess magnification errors – true anatomic measurements are realizable.<br />
<strong>The</strong>se true anatomic measurements improve surgical predictably as well as reduce surgical<br />
time. Since I have always taken pans plus lateral and frontal cephalograms on all my patients,<br />
the i-CAT<br />
Imaging Sciences International<br />
1910 North Penn Road<br />
Hatfield, PA 19440<br />
(800) 205-3570<br />
® Why 3-D, Why i-CAT<br />
machine with the EFOV makes it extremely easy to get these images all at once.<br />
I am now able to perform my 3-dimensional cephalometric analyses with a 3-dimensional<br />
machine. I also treat a number of patients with Temporomandibular Disorders. This machine<br />
is great for TMJ imaging. In the past I would take a submental vertex radiograph, calculate the<br />
angulations of the condyles for corrected tomographs, and then finally take the images of the<br />
condyles. This would take a considerable amount of time. Now, with a single scan, I can view<br />
images of the condyles within a matter of minutes.<br />
®<br />
In the past, when addressing impacted teeth, the orthodontist has had to rely upon periapical,<br />
panoramic, and occlusal radiographs to determine the location of impacted teeth. Panoramic<br />
radiographs are suitable for a comprehensive and overall view of the jaws and teeth. However,<br />
panoramic radiographs possess inherent magnification and distortion errors that result in<br />
inconsistent information. Distortion errors with panoramic radiographs can vary from one part<br />
of the film to the next. All the anatomical elements that lie between the x-ray tube and the film<br />
are superimposed upon one another. Moreover, because of the nature of the focal trough of<br />
the panoramic radiograph, important anatomical features, undiagnosed pathologies, and/<br />
or teeth may lie outside the radiographic image. I have multiple cases where impacted teeth<br />
were missed on a standard 2-D image only to be diagnosed when a CBCT scan was made.<br />
One doesn’t realize how large the distortion errors are in standard 2-D panoramics until<br />
after looking at CBCT scans.CBCT completely eliminates the superimposition of images<br />
or structures outside the area of interest. Data from a single CBCT scan can be viewed as<br />
images in the axial, coronal, and sagittal planes. This is referred to as multiplanar reformatted<br />
imaging. CBCT scans can also provide cross-sectional images that are extremely useful<br />
in cases with impacted teeth. CBCT images do not possess magnification errors – true<br />
anatomic measurements are realizable. <strong>The</strong>se true anatomic measurements improve surgical<br />
predictably as well as reduce surgical time. Since I have always taken pans plus lateral<br />
and frontal cephalograms on all my patients, the i-CAT ® machine with the EFOV makes it<br />
extremely easy to get these images all at once. I am now able to perform my 3-dimensional<br />
cephalometric analyses with a 3-dimensional machine. I also treat a number of patients with<br />
Temporomandibular Disorders. This machine is great for TMJ imaging. In the past I would<br />
take a submental vertex radiograph, calculate the angulations of the condyles for corrected<br />
tomographs, and then finally take the images of the condyles. This would take a considerable<br />
amount of time. Now, with a single scan, I can view images of the condyles within a matter<br />
of minutes.<br />
g Sciences International<br />
1910 North Penn Road<br />
Hatfield, PA 19440<br />
(800) 205-3570<br />
) Orders: 1300 65 88 22 8 www.henryschein.com.au<br />
®<br />
®<br />
CASE REPORT<br />
CASE REPORT<br />
CASE REPORT<br />
www.i-CAT.com<br />
www.i-CAT.com<br />
7
ody logic<br />
All volume sizes<br />
leading the way...<br />
Planmeca ProMax 3D<br />
Planmeca ProMax 3D is an intelligent and multipurpose<br />
X-ray unit series designed to obtain complete<br />
information on patient anatomy in the minutest detail.<br />
<strong>The</strong> units provide digital panoramic, cephalometric, 3D<br />
CBVT imaging, and 3D photo, as well as advanced<br />
imaging software tools to comply with every possible<br />
need in dental radiology.<br />
Planmeca ProMax 3Ds<br />
is ideal for imaging of small details Ø50 x 80 mm<br />
Planmeca ProMax 3D<br />
Covers the whole dentition area Ø80 x 80 mm<br />
Planmeca ProMax 3D Mid<br />
offers the widest selection volumes<br />
sizes Ø160 x 160 mm<br />
8<br />
Planmeca ProMax 3D Max<br />
enables imaging of the whole maxillofacial<br />
region Ø230 x 260 mm<br />
ProMax 3D ProFace<br />
produces 3D face photo in addition to traditional<br />
maxillofacial radiography.<br />
Full MAC<br />
Support
Morita 3De<br />
Veraviewepocs 3DE offers digital 3D, Panoramic & cephalometric<br />
(optional) imaging options with no cassette change required. This<br />
model features built-in sensors for all image types designed to save<br />
time and for ease of use. With 40x40 & 40x80mm 3D fields of view,<br />
3De is suitable for over 90% of all clinical cases.<br />
Features<br />
Veraviewepocs 3D<br />
• 3D, True panoramic (not reconstructed), pedo, TMJ,<br />
maxillary sinus images,<br />
bite wing & cephalometric capabilities<br />
• Easy positioning for 3D images – simply click the region<br />
of interest on the panoramic view<br />
• High resolution, contrast rich 3D images of both hard<br />
and soft tissue with minimal artifacts – and no distortion<br />
• Low dose and is only 1.8 times that of a Panoramic X-ray<br />
with film exposure.<br />
Also available...<br />
3DE with Ceph<br />
FOV 40 x 40 & 40 x 80<br />
3D Type A<br />
FOV 80 x 80<br />
3D Type B<br />
with Ceph FOV 80 x 80<br />
3D Accuitomo 80<br />
FOV 40 x 40, 60 x 60 & 80 x 80<br />
3D Accuitomo 170<br />
FOV 40 x 40, 60 x 60, 80 x 80,<br />
100 x 50, 100 x 100, 140 x 50,<br />
140 x 100, 170 x 50 & 170 x 120mm<br />
Thinking ahead. Focused on life.<br />
) Orders: 1300 65 88 22 8 www.henryschein.com.au<br />
9
high tech | DENTISTRY<br />
body logic<br />
high tech | DENTISTRY<br />
Obstructive sleep sleep<br />
apnea-hyponea apnea-hypopnea syndrome: syndrome:<br />
Obstructive Clinical sleep<br />
Clinical applications<br />
applications<br />
of cone beam<br />
of<br />
apnea-hypopnea CT<br />
cone beam CTsyndrome:<br />
Clinical applications of cone beam CT<br />
By Allison K. Lohse, BS<br />
William C. Scarfe, BDS, FRACDS, MS, Dipl. ABOMR<br />
Fidaa Shaib, MD, DABSM, CBSM and<br />
By Allison Allan G. K. Farman, Lohse, BS BDS, PhD, DSc, MBA, Dipl. ABOMR, Dipl. JBOMR<br />
William C. Scarfe, BDS, FRACDS, MS, Dipl. ABOMR<br />
Fidaa Shaib, MD, DABSM, CBSM and<br />
Allan G. Farman, BDS, PhD, DSc, MBA, Dipl. ABOMR, Dipl. JBOMR<br />
S<br />
S<br />
leep-Disordered Breathing (SDB) is a group cular diseases including high blood pressure, depres-<br />
of disorders characterized by disturbances in sion, irritability, learning and memory difficulties,<br />
the normal respiratory pattern during sleep. weight gain, impotence and headaches. In addition,<br />
Those are related to increased upper airway resistance<br />
and include snoring; upper airway resistance<br />
syndrome; and obstructive sleep apnea-hypopnea<br />
syndrome (OSAHS). OSAHS is the most common<br />
disorder and characterized by snoring, repetitive<br />
total or partial collapse of the pharyngeal airway<br />
during sleep terminated by oxygen desaturation or<br />
EEG arousal before ventilation resumes. Airway<br />
obstruction is manifested by a reduction in airflow,<br />
termed hypopnea, or a complete cessation of airflow,<br />
termed apnea, despite ongoing inspiratory<br />
effort. Hypopnea is defined in adults as a 10-second<br />
event where despite continued breathing, ventilation<br />
during sleep is reduced by at least 50% from<br />
baseline. Apnea is total cessation of airflow for at<br />
least 10 seconds. Apnea can be obstructive or due<br />
to failure in control centrally.<br />
<strong>The</strong> early effects of repeated disrupted sleep are<br />
waking somnolence, impaired mental function,<br />
delayed reaction time and difficulty maintaining<br />
concentration. Long term effects of recurrent sleep<br />
arousal in association with intermittent hypoxia and<br />
hypercapnia have been associated with cardiovas-<br />
there is evolving evidence that SDB may contribute to<br />
insulin resistance and other components of the metabolic<br />
syndrome. Population-based studies suggest<br />
that OSAHS is a relatively common disorder. In those<br />
aged 30 to 60 years, 24% of men and 9% of women<br />
are reported to have abnormal AHI indices.<br />
104 10 Australasian Dental Practice September/October 2009<br />
1 <strong>The</strong><br />
prevalence of symptomatic OSAHS is conservatively<br />
estimated to be 1% to 2% in middle-aged men and<br />
approximately 0.5% to 1%, in middle-aged women. 2<br />
“CBCT has<br />
particular<br />
application in<br />
the diagnosis<br />
and assessment<br />
of therapy in<br />
OSAHS patients<br />
and has the<br />
potential<br />
to eliminate<br />
the need for<br />
additional<br />
static<br />
imaging...”<br />
leep-Disordered Breathing (SDB) is a group<br />
of disorders characterized by disturbances in<br />
the normal respiratory pattern during sleep.<br />
Those are related to increased upper airway resistance<br />
and include snoring; upper airway resistance<br />
syndrome; and obstructive sleep apnea-hypopnea<br />
syndrome (OSAHS). OSAHS is the most common<br />
disorder and characterized by snoring, repetitive<br />
total or partial collapse of the pharyngeal airway<br />
during sleep terminated by oxygen desaturation or<br />
EEG arousal before ventilation resumes. Airway<br />
obstruction is manifested by a reduction in airflow,<br />
termed hypopnea, or a complete cessation of airflow,<br />
termed apnea, despite ongoing inspiratory<br />
effort. Hypopnea is defined in adults as a 10-second<br />
event where despite continued breathing, ventilation<br />
during sleep is reduced by at least 50% from<br />
baseline. Apnea is total cessation of airflow for at<br />
least 10 seconds. Apnea can be obstructive or due<br />
to failure in control centrally.<br />
<strong>The</strong> early effects of repeated disrupted sleep are<br />
waking somnolence, impaired mental function,<br />
delayed reaction time and difficulty maintaining<br />
cular diseases including high blood pressure, depression,<br />
irritability, learning and memory difficulties,<br />
weight gain, impotence and headaches. In addition,<br />
there is evolving evidence that SDB may contribute to<br />
insulin resistance and other components of the metabolic<br />
syndrome. Population-based studies suggest<br />
that OSAHS is a relatively common disorder. In those<br />
aged 30 to 60 years, 24% of men and 9% of women<br />
are Sleep reported apnea to have is not abnormal always easily AHI indices. diagnosed as<br />
symptoms might not be evident, either to the<br />
patient or others. Factors contributing to the presence<br />
and severity of SDB are multifactorial and<br />
include reduced airway anatomy, nasal blockage,<br />
the presence and distribution of body fat and<br />
muscle tone. Being even moderately overweight is<br />
the most common risk factor, especially a body<br />
mass index or BMI (weight in kilograms divided by<br />
height in meters squared) greater than 28. Other<br />
risk factors include collar size of snoring patients<br />
(greater than 17 inches for men, 15 inches for<br />
women), physical nasal obstruction, underactive<br />
thyroid and excessive fat around the neck area.<br />
concentration. Long term effects of recurrent sleep<br />
arousal in association with intermittent hypoxia and<br />
hypercapnia have been associated with cardiovas-<br />
1 <strong>The</strong><br />
prevalence of symptomatic OSAHS is conservatively<br />
estimated to be 1% to 2% in middle-aged men and<br />
approximately 0.5% to 1%, in middle-aged women. 2<br />
“CBCT has<br />
particular<br />
application in<br />
the diagnosis<br />
and assessment<br />
of therapy in<br />
OSAHS patients<br />
and has the<br />
potential<br />
to eliminate<br />
the need for<br />
additional<br />
static<br />
imaging...”<br />
Sleep apnea is not always easily diagnosed as<br />
symptoms might not be evident, either to the<br />
patient or others. Factors contributing to the presence<br />
and severity of SDB are multifactorial and<br />
include reduced airway anatomy, nasal blockage,<br />
the presence and distribution of body fat and<br />
muscle tone. Being even moderately overweight is<br />
the most common risk factor, especially a body<br />
mass index or BMI (weight in kilograms divided by<br />
height in meters squared) greater than 28. Other<br />
risk factors include collar size of snoring patients<br />
(greater than 17 inches for men, 15 inches for<br />
women), physical nasal obstruction, underactive<br />
thyroid and excessive fat around the neck area.
Diagnosis of OSAHS is made through a sleep study that is generally<br />
performed at a sleep laboratory. Various physiologic<br />
functions related to sleep are recorded using a polysomnogram, a<br />
compilation of tests including an electroencephalogram, electrooculogram,<br />
nasal pressure and flow, abdominal and chest<br />
excursions, electromyogram and pulse oximetry. <strong>The</strong> severity of<br />
the OSAHS is indexed using the Apnea/Hypopnea Index (AHI)<br />
calculated by adding the total number of apneas and hypopneas and<br />
dividing by the number of hours of observed sleep. Another metric<br />
is the Respiratory Disturbance Index (RDI) which also includes<br />
other respiratory disturbances such as respiratory event related<br />
arousals. Severity of OSAHS is generally defined using AHI or<br />
RDI. An AHI or RDI of 5-15 is considered mild; 16-25 moderate<br />
and; greater than 26 severe. A second study is usually performed<br />
while using a continuous positive airway pressure (CPAP) ventilation<br />
machine as therapy to prevent obstructive events)(Figure 1).<br />
<strong>The</strong>rapies of OSAHS are primarily directed at pneumatically<br />
splinting the airway open or secondarily adjusting the airway in<br />
making it less apt to collapse. CPAP is the primary and most<br />
effective therapy initially offered for treatment of OSAHS. 3 It is<br />
usually provided in association with behavioral changes such as<br />
avoiding alcohol, smoking and medicines that cause sleepiness;<br />
and altered sleep posture or nutritional and dietary counseling to<br />
reduce weight. Unfortunately, CPAP is a cumbersome modality<br />
and hence approximately 25-50% of patients with OSAHS will<br />
either refuse the offer of CPAP therapy, or will not tolerate it. 4<br />
Secondary therapy for patients suffering from OSAHS who<br />
cannot tolerate CPAP is directed towards physically widening the<br />
pharyngeal airway. This can be performed reversibly by the use of<br />
removable oral appliances (OA) or permanently by surgery. OAs are<br />
categorized by the method used to improve the patency of the<br />
airway space. <strong>The</strong> most common OA appliances are mandibular<br />
advancement devices (MAD), which protrude the mandible anteriorly<br />
to pull the muscles of the oropharynx forward, and tongue<br />
retaining devices (TRD) that aim at holding the tongue in a protrusive<br />
position. <strong>The</strong>se devices can be “titrated” to best fit the patient<br />
for comfort and efficiency (Figure 2). However, OA appliances are<br />
therapeutic only if selected appropriately for the specific site(s) of<br />
upper airway obstruction, which varies between individuals. 5,6<br />
For patients with severe AHI and co-morbidities (e.g. significant<br />
bradycardia, severe hypercarbia, cor pulmonale and extreme hypersomnolence)<br />
on whom CPAP is not a viable option, surgery is<br />
usually the most appropriate alternative. Surgery options include<br />
upper airway soft tissue correction to enlarge the pharyngeal space<br />
and prevent airway collapse (e.g. removal of tonsils or adenoids,<br />
radiofrequency ablation of the tongue or soft palate (somnoplasty),<br />
uvulopalatopharyngoplasty and laser-assisted uvulopalatopharyngoplasty,<br />
and reduction in tongue size or movement of the mandible<br />
anteriorly (e.g. genioglossal advancement with hypoid myotomy,<br />
bimaxillary advancement, or maxillomandibular advancement).<br />
Procedures to improve upper airway patency are successful in certain<br />
subsets of patients, but some do not achieve desired relief. 7<br />
If secondary treatments are necessary, the site of the oropharyngeal<br />
obstruction must be identified such that appropriate therapy<br />
can be applied. Numerous supplemental tests can be performed to<br />
determine the site of reduction in airway caliber including<br />
fiberoptic nasopharyngoscopy with the Müller maneuver, sleep<br />
endoscopy, fluoroscopy, rhinomanometry and diagnostic imaging<br />
studies. <strong>The</strong> specific role of diagnostic imaging is to evaluate the<br />
high tech | DENTISTRY<br />
Figure 1. Example of CPAP device with patient wearing full face<br />
mask in sleep laboratory facility.<br />
Figure 2. Example of Herbst MAD device allowing titratable<br />
mandibular advancement using a bilateral piston system comprised<br />
of rods and sleeves from the anterior (a) and posterior (b) views.<br />
Figure 3. Patient seated in CBCT machine (iCAT Platinum edition,<br />
Imaging Sciences International). For OSAHS patients scan<br />
technique is modified such that the chin support is removed and<br />
the patient is allowed to adopt habitual head position.<br />
) 11<br />
Orders: 1300 65 88 22 8 www.henryschein.com.au<br />
September/October 2009 Australasian Dental Practice 105
high tech | DENTISTRY<br />
body logic<br />
morphology of the upper airway, determine<br />
the site and degree of pharyngeal<br />
obstruction, identify potential causative<br />
conditions (Table 1) and anatomic characteristics<br />
that may be predictive of<br />
therapeutic efficacy. Lateral cephalometric<br />
radiography (LCR) has been long<br />
been used in clinical practice. Numerous<br />
authors have reported a variety of craniofacial<br />
anatomical abnormalities associated<br />
with OSAHS on LCR including reduced<br />
retroglossal airway linear dimensions, a<br />
long, bulky soft palate, an inferiorly<br />
placed hyoid bone and mandibular<br />
deficiency. 8-13 Computed tomography and<br />
magnetic resonance imaging have been<br />
used in the research environment to provide<br />
three-dimensional metrics of the naso-,<br />
oro- and hypo-pharyngeal regions such as<br />
minimal cross-sectional area, minimal<br />
antero-posterior/lateral dimensions and<br />
airway volumes. <strong>The</strong> results from these<br />
studies indicate that the upper airway is significantly<br />
narrowed among patients with<br />
OSA compared to controls, but that the site<br />
of narrowing varies among OSA patients.<br />
<strong>Cone</strong> beam computed tomography<br />
(CBCT) scanners have been available for<br />
craniofacial imaging since 2001 in the<br />
United States (Figure 3). <strong>The</strong> CBCT has a<br />
cone- or pyramidal shaped beam originating<br />
from a low-energy fixed anode tube that is<br />
projected through the subject to an attached<br />
single solid-state or amorphous silicon 2D<br />
panel detector that rotates with the beam. In<br />
a single, rapid (5-20 sec) rotation, precise,<br />
accurate high resolution volumetric data is<br />
acquired. Reconstruction and subsequent<br />
viewing of the digital data is accomplished<br />
on a personal computer. Standard viewing<br />
layouts include the display of coronal,<br />
sagittal and axial data sets concurrently. A<br />
main advantage of using CBCT to image the<br />
oropharynx is the low dosage of radiation<br />
relative to conventional spiral computed<br />
tomography. Ludlow, et al reported largefield<br />
of view CBCT effective dose (E 2007)<br />
varied from 68 to 1,073µSv with most<br />
in the 100-200µSv range as compared to<br />
multi detector CT (range; 534-860µSv). 14<br />
Although soft tissue is not clearly delineated<br />
from other soft tissue on CBCT, it clearly<br />
shows high contrast between bone, teeth,<br />
empty space and soft tissue in general. It is<br />
ideal to show the patency of the airway<br />
related to the position of the hard tissue structures<br />
of the skull. <strong>The</strong> spatial resolution is also<br />
much greater than conventional CT, with a<br />
voxel resolution between 0.076 and 0.4 mm.<br />
Figure 4. Reorientation of volumetric data to adjust patient head position during scan<br />
to anthropomorphic standard reference planes. Lateral (a) and frontal (b) volume rendering<br />
show that the patient was originally scanned with the head raised and tilted towards<br />
the right. Comparable lateral (c) and frontal (d) volumetric rendering with<br />
adjusted data to position Frankfort horizontal (FH) parallel to floor and mid-sagittal<br />
plane perpendicular to FH.<br />
Table 1. Anatomic Abnormalities associated with OSAHS<br />
Region Structure Condition<br />
Nasal Cavity Turbinate Hypertrophy, polyps, mucosal<br />
thickening, hyper-secretion<br />
Septae Deviated<br />
Maxillofacial/Skeletal Mandible Relative hypoplasia, deficiency, cross-bite,<br />
mandibular tori<br />
Maxilla Relative hypoplasia, deficiency, cross-bite<br />
Hyoid Caudal displacement relative of the cervical<br />
spine and mandible<br />
Upper Airway Soft palate Excessive length, low lying position<br />
Tongue Macroglossia, short length, loss of<br />
muscle tone<br />
Nasopharynx Hypertrophic adenoids, fatty lumen<br />
Oropharynx Hypertrophic tonsils, lumen thickening,<br />
fat pad accumulation<br />
Hypopharynx Lumen thickening<br />
Larynx Abnormal vocal cord anatomy, paralysis<br />
of vocal cords<br />
106 12 Australasian Dental Practice September/October 2009
high tech | DENTISTRY<br />
CBCT has particular application in the diagnosis<br />
and assessment of therapy in OSAHS<br />
patients and has the potential to eliminate the<br />
need for additional static imaging. <strong>The</strong> resulting<br />
volume of digital data can be manipulated to<br />
allow the clinician three-dimensional images that<br />
can be re-oriented in all three axes to correspond<br />
to anthropometric reference planes (Figure 4) and<br />
can be selectively contrasted, emphasized<br />
or reduced to visualize certain anatomical structures<br />
such as the craniofacial skeleton or airway<br />
(Figure 5). Data can exported as a DICOM (Digital<br />
Imaging and Communications in Medicine)<br />
format data set and imported into proprietary<br />
orthodontic image and analysis programs (e.g.<br />
InVivoDental by Anatomage or Dolphin 3D)<br />
which have specific modules capable of demonstrating<br />
and recording the airway and its<br />
surrounding structures. <strong>The</strong>se programs offer<br />
practitioners opportunities to interact with the<br />
data and allow visualization of both untreated<br />
obstruction tendencies and potentially of changes<br />
in the airway by treatment modality. In this way,<br />
it may help identify those subsets of patients who<br />
may or may not benefit from a choice of treatment<br />
modalities. CBCT has been applied to<br />
describe significant differences in total airway<br />
volume and the antero-posterior dimension of the<br />
oropharyngeal airway between OSA and gendermatched<br />
controls, differences in airway shape<br />
between OSA (concave or elliptical) and non-<br />
OSA (concave, round, or square). 15,16 Recent<br />
research in the authors’ clinic applied CBCT<br />
imaging to patients with and without OSA to<br />
determine a quantifiable relationship between<br />
airway patency and mandibular advancement<br />
using OA. 17 It was determined that custom<br />
titrated MAD devices repositioned the mandible<br />
on average horizontally 4mm and vertically 8mm<br />
and resulted in an average oropharyngeal volume<br />
increase of ~2800mm 3 . It was possible to predict<br />
the airway volume gained, the amount of crosssectional<br />
area gained at the narrowest cross<br />
section; the cross-sectional area gained at C2; and<br />
the lateral linear dimension gained at this level<br />
from the distance the mandible is advanced.<br />
In collaboration with colleagues of the University<br />
of Louisville Multidisciplinary Sleep<br />
Team, a specific CBCT imaging protocol has<br />
been developed that has proven particularly<br />
useful in the assessment of soft and hard tissue<br />
contributors to mechanical obstruction in<br />
patients with OSAHS. This involves:<br />
a. Sequential axial and coronal images (1mm<br />
thickness/3mm interval). <strong>The</strong>se conventional<br />
orthogonal images enable visualization of<br />
potential nasal obstructions (Figure 6) and<br />
anatomic anomalies, palatal and mandibular<br />
structures and provide an overview of the max-<br />
Figure 5. 3D volumetric image of the right side of an OSA patient demonstrating<br />
airway only (a) and with maxillofacial skeleton overlay (b). This is performed by<br />
selective segmentation procedures (Images created using Dolphin 3D V.11).<br />
Figure 6. Reference sagittal orthogonal image at 0.4mm (a) of pediatric OSAHS<br />
patient demonstrating of coronal scans at progressively posterior locations. Note<br />
the generalized mucosal thickening of the turbinates of the right nasal fossa and<br />
marked reduction and partial occlusion in nasal cavity space.<br />
Figure 7. Reference sagittal CBCT image (a) and corresponding 0.4 mm axial cross sectional<br />
images of the upper (b) and lower retro-palatal (c), and retroglossal (d) airway.<br />
) 13<br />
Orders: 1300 65 88 22 8 www.henryschein.com.au<br />
108 Australasian Dental Practice September/October 2009
high tech | DENTISTRY<br />
body logic<br />
imum and minimal (Figure 7) caliber of<br />
the airway space. Because of the relatively<br />
poor contrast resolution of CBCT<br />
imaging, potential specific soft tissue factors<br />
(e.g. muscular hypertrophy, redundant<br />
fat pads) are unable to be visualized.<br />
b. Ray-sum and maximum intensity projection<br />
simulated panoramic, lateral<br />
cephalometric, postero-anterio and submentovertex<br />
images. Specific volumetric<br />
rendering of the CBCT data can be<br />
performed to produce conventional craniofacial<br />
skull images. <strong>The</strong>se projections<br />
demonstrate global deficiencies of the maxillofacial<br />
skeleton in all three orthogonal<br />
planes that may contribute to the obstruction<br />
(e.g. retrognathia, maxillary cross-bite,<br />
mandibular asymmetry, palatal soft tissue)<br />
and allow visualization and measurement of<br />
parameters that have been reported to be<br />
associated with OSAHS (Figure 8).<br />
c. Regionally corrected temporomandibular<br />
joint images. Visualization of the TMJ<br />
articulation provides information of the<br />
relative stability of morphology of this<br />
determinant of mandibular position.<br />
Active degenerative joint disease either<br />
osteoarthritic, autoimmune or idiopathic<br />
in nature can reduce mandibular ramal<br />
length resulting in an anterior open bite<br />
and produce substantial inferior and posterior<br />
positional changes in the location of<br />
the associated soft tissue (Figure 9).<br />
d. Three dimensional analysis of upper<br />
airway anatomy. Concomitant segmentation<br />
of hard tissue maxillofacial skeleton,<br />
airway space and facial soft tissue surfaces<br />
from 3D CBCT data provides dynamic<br />
visualization of the interrelationship of<br />
these structures on airway obstruction.<br />
This facilitates identification and classification<br />
of the level of the obstruction (Table<br />
2) and quantitative analysis of linear, area<br />
and volumetric parameters (Figures 10 and<br />
11). Images also provide superior visualization<br />
of airway shape and caliber as well<br />
as soft tissue elements such as the<br />
epiglottis and soft palate. 18<br />
e. Comparison of pre- and post-therapy<br />
effects. Volumetric superimposition of CBCT<br />
datasets can be performed to produce<br />
colour-contrasted blended views of the<br />
mechanical and resultant airway changes<br />
as a result of specific therapies (Figure 12).<br />
In addition to the imaging protocol presented<br />
above, it is possible to generate<br />
video frame of reference “fly through”<br />
reconstructions (e.g. Osiris imaging Software.<br />
V3.1, University Hospital of<br />
Figure 8. Ray sum simulated lateral cephalometric images demonstrating tracing of<br />
soft (a) and hard tissue (b) measurements using specific orthodontic analysis software<br />
(Images created using Dolphin 3D V.11).<br />
Figure 9. Temporomandibular image protocol demonstrating ray sum reformatted<br />
panoramic (b), 5mm thick sagittal (a and b) and sequential 1mm cross-sectional right<br />
(d) and left (e) images. Note the marked osteoarthritic degenerative joint disease of the<br />
right TMJ articulation in this OSAHS patient contributing to reduction in mandibular<br />
ramal length and asymmetry of the mandible.<br />
Table 2. Classification of Velohypopharyneal Airway Obstruction 18<br />
Type Sub-Type Description<br />
I Retropalatal or velopharyngeal<br />
II Combined retropalatal and hypopharyngeal/retroglossal (base of tongue)<br />
IIa Predominantly retropalatal<br />
IIb Predominantly retroglossal<br />
III Isolated retroglossal or hypopharyngeal (base of tongue)<br />
14<br />
110 Australasian Dental Practice September/October 2009
high tech | DENTISTRY<br />
Geneva, Switzerland and OnDemand3D,<br />
CyberMed Inc., Seoul, Korea). While<br />
images produced by this technique demonstrate<br />
the static airway, this non-invasive<br />
approach serves as a potential method to<br />
create virtual fiberoptic nasopharyngoscopy<br />
visualizations (Figure 13).<br />
OSAHS is an important public health<br />
concern because of under diagnosis and<br />
associated cardiovascular consequences.<br />
As upper airway constriction is an important<br />
contributing factor, CBCT technology<br />
provides a rapid low dose 3D imaging<br />
modality capable of providing simultaneous<br />
hard and soft tissue images<br />
facilitating visualization of upper airway<br />
characteristics. This, together with clinical<br />
information, may provide a valuable<br />
assessment tool of patients with OSAHS<br />
and assist in treatment modality choice<br />
based on predictable outcomes.<br />
References<br />
1. Lee-Chiong T, Sateia M, Carskadon M. Snoring and<br />
sleep disordered breathing. Philadelphia: Sleep Medicine.<br />
2002; 349-355.<br />
2. Young T, Palta M, Dempsey J, Skatrud J, Weber S,<br />
Badr S. <strong>The</strong> occurrence of sleep-disordered breathing<br />
among middle-aged adults. N Engl J Med. 1993;<br />
328:1230-1235.<br />
3. Giles TL, Lasserson TJ, Smith BJ, White J, Wright<br />
J, Cates CJ. Continuous positive airways pressure for<br />
obstructive sleep apnoea in adults. Cochrane Database<br />
Syst Rev; 2006 Jan 25; (1):CD001106.<br />
4. Zozula R, Rosen R. Compliance with continuous<br />
positive airway pressure therapy: Assessing and<br />
improving treatment outcomes (review). Curr Opin<br />
Pulm Med. 2001; 7:391-398.<br />
5. Shepard JW Jr, Gefter WB, Guilleminault C, et al.<br />
Evaluation of the upper airway in patients with<br />
obstructive sleep apnea. Sleep. 1991; 14:361–371.<br />
6. Launois SH, Feroah TR, Campbell WN, Issa FG,<br />
Morrison D, Whitelaw WA, Isono S, Remmers JE. Site<br />
of pharyngeal narrowing predicts outcome of surgery<br />
for obstructive sleep apnea. Am Rev Respir Dis.1993;<br />
147:182–189.<br />
7. Veasey SM, Guilleminault C, Strohl K, Sanders M,<br />
Ballard R, Magalang U, et al: Medical <strong>The</strong>rapy for<br />
Obstructive Sleep Apnea: A review by the Medical<br />
<strong>The</strong>rapy for Obstructive Sleep Apnea Task Force of<br />
the Standards of Practice Committee of the American<br />
Academy of Sleep Medicine. Sleep & Breathing.<br />
2006; 29:1036-1044.<br />
8. Riley R, Guilleminault C, Herran J, Powell N. Cephalometric<br />
analyses and flow volume loops in obstructive<br />
sleep apnoea patients. Sleep. 1983; 6:303–311.<br />
9. Rivlin J, Hoffstein V, Kalbfleisch J, McNicholas W,<br />
Zamel N, Bryan AC. Upper airway morphology in<br />
patients with idiopathic obstructive sleep apnea. Am<br />
Rev Respir Dis. 1984; 129:355–360.<br />
10. Hochban W, Brandenburg U. Morphology of the<br />
viscerocranium in obstructive sleep apnoea syndrome<br />
± cephalometric evaluation of 400 patients. J Craniomaxillofac<br />
Surg. 1994; 22:205-213.<br />
11. Cistulli PA. Craniofacial abnormalities in obstructive<br />
sleep apnoea: implications for treatment.<br />
Respirology. 1996; 3:167-174.<br />
Figure 10. Lateral oblique 3D images of the segmented airway of an OSAHS patient<br />
after application of software algorithm to identify the volume of specific portions of the<br />
oro-pharyngeal airway. Retroglossal (a) and retropalatal (b) volumes are identified by<br />
a solid - the level of the minimum cross-sectional airway within the segment is identified<br />
as a radial disc (Images created using Dolphin 3D V.11).<br />
Figure 11. Lateral 3D images of the segmented airway of another OSAHS patient after<br />
demonstrating the specific volumes of retroglossal (a) and retropalatal (b) airway<br />
space. <strong>The</strong> software algorithm identifies and displays the axial images at which the<br />
minimum cross-sectional area is present (c and d) and allows for measurement of antero-posterior<br />
and transverse dimensions (Images created using Dolphin 3D V.11).<br />
12. Tangugsorn V, Skatvedt O, Krogstad O, Lyberg T.<br />
Obstructive sleep apnoea: a cephalometric study. Part<br />
I. Cervico-craniofacial skeletal morphology. Eur J<br />
Orthodontics. 1995; 17: 45-56.<br />
13. Tangugsorn V, Skatvedt O, Krogstad O, Lyberg T.<br />
Obstructive sleep apnoea: a cephalometric study. Part<br />
II. Uvulo-glossopharyngeal morphology. Eur J Orthodontics.<br />
1995; 17: 57-67.<br />
14. Ludlow JB, Ivanovic M. Comparative dosimetry of<br />
dental CBCT devices and 64-slice CT for oral and<br />
maxillofacial radiology. Oral Surg Oral Med Oral<br />
Pathol Oral Radiol Endod. 2008; 106:106-14.<br />
15. Ogawa T, Encisco R, Memon A, Mah J, Clark G.<br />
Evaluation of 3D airway imaging of obstructive sleep<br />
apnea with cone-beam computed tomography. Stud<br />
Health Technol Inform. 2005; 111:365-368.<br />
16. Ogawa T, Enciso R, Shintaku W, Clark G, et al:<br />
Evaluation of cross-section airway configuration of<br />
obstructive sleep apnea. Oral Surg Oral Med Oral<br />
Pathol Oral Radiol Endod. 2007; 103:102-108.<br />
17. Haskell JA, McCrillis J, Haskell BS, Scheetz JP,<br />
Scarfe WC, Farman AG. Effects of Mandibular<br />
Advancement Device (MAD) on Airway Dimensions<br />
Assessed With <strong>Cone</strong>-<strong>Beam</strong> Computed Tomography.<br />
Semin Orthod. 2009; 15:132-158.<br />
18. Fujita S: Pharyngeal surgery for management of<br />
snoring and obstructive sleep apnea, in Fairbanks DN,<br />
Fujita S, Ikematsu T, et al (eds). Snoring and Obstructive<br />
Sleep Apnea. New York, NY: Raven Press, 1987.<br />
p. 101-128.<br />
) 15<br />
Orders: 1300 65 88 22 8 www.henryschein.com.au<br />
112 Australasian Dental Practice September/October 2009
ody logic<br />
16<br />
CB-500<br />
Powered by I-CAT<br />
Veraviewepocs 3D<br />
<strong>The</strong> <strong>Cone</strong> <strong>Beam</strong> <strong>specialists</strong><br />
ProMax 3D<br />
Largest range – world’s leading brands<br />
HSH 0368