Conservative Management of Legg-Calve-Perthes Disease in ...
Conservative Management of Legg-Calve-Perthes Disease in ...
Conservative Management of Legg-Calve-Perthes Disease in ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
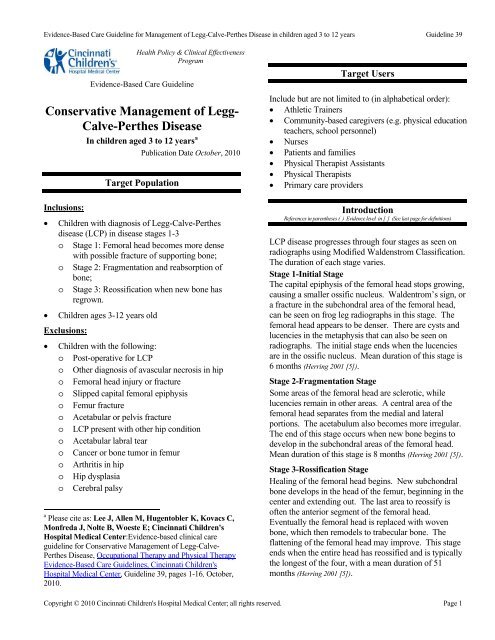
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39Health Policy & Cl<strong>in</strong>ical EffectivenessProgramEvidence-Based Care Guidel<strong>in</strong>e<strong>Conservative</strong> <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong>In children aged 3 to 12 years aInclusions:Publication Date October, 2010Target PopulationChildren with diagnosis <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong>disease (LCP) <strong>in</strong> disease stages 1-3o Stage 1: Femoral head becomes more densewith possible fracture <strong>of</strong> support<strong>in</strong>g bone;o Stage 2: Fragmentation and reabsorption <strong>of</strong>bone;o Stage 3: Reossification when new bone hasregrown.Children ages 3-12 years oldExclusions:Children with the follow<strong>in</strong>g:o Post-operative for LCPo Other diagnosis <strong>of</strong> avascular necrosis <strong>in</strong> hipo Femoral head <strong>in</strong>jury or fractureo Slipped capital femoral epiphysiso Femur fractureo Acetabular or pelvis fractureo LCP present with other hip conditiono Acetabular labral tearo Cancer or bone tumor <strong>in</strong> femuro Arthritis <strong>in</strong> hipo Hip dysplasiao Cerebral palsya Please cite as: Lee J, Allen M, Hugentobler K, Kovacs C,Monfreda J, Nolte B, Woeste E; C<strong>in</strong>c<strong>in</strong>nati Children'sHospital Medical Center:Evidence-based cl<strong>in</strong>ical careguidel<strong>in</strong>e for <strong>Conservative</strong> <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong>, Occupational Therapy and Physical TherapyEvidence-Based Care Guidel<strong>in</strong>es, C<strong>in</strong>c<strong>in</strong>nati Children'sHospital Medical Center, Guidel<strong>in</strong>e 39, pages 1-16, October,2010.Target UsersInclude but are not limited to (<strong>in</strong> alphabetical order): Athletic Tra<strong>in</strong>ers Community-based caregivers (e.g. physical educationteachers, school personnel) Nurses Patients and families Physical Therapist Assistants Physical Therapists Primary care providersIntroductionReferences <strong>in</strong> parentheses ( ) Evidence level <strong>in</strong> [ ] (See last page for def<strong>in</strong>itions)LCP disease progresses through four stages as seen onradiographs us<strong>in</strong>g Modified Waldenstrom Classification.The duration <strong>of</strong> each stage varies.Stage 1-Initial StageThe capital epiphysis <strong>of</strong> the femoral head stops grow<strong>in</strong>g,caus<strong>in</strong>g a smaller ossific nucleus. Waldentrom’s sign, ora fracture <strong>in</strong> the subchondral area <strong>of</strong> the femoral head,can be seen on frog leg radiographs <strong>in</strong> this stage. Thefemoral head appears to be denser. There are cysts andlucencies <strong>in</strong> the metaphysis that can also be seen onradiographs. The <strong>in</strong>itial stage ends when the lucenciesare <strong>in</strong> the ossific nucleus. Mean duration <strong>of</strong> this stage is6 months (Herr<strong>in</strong>g 2001 [5]).Stage 2-Fragmentation StageSome areas <strong>of</strong> the femoral head are sclerotic, whilelucencies rema<strong>in</strong> <strong>in</strong> other areas. A central area <strong>of</strong> thefemoral head separates from the medial and lateralportions. The acetabulum also becomes more irregular.The end <strong>of</strong> this stage occurs when new bone beg<strong>in</strong>s todevelop <strong>in</strong> the subchondral areas <strong>of</strong> the femoral head.Mean duration <strong>of</strong> this stage is 8 months (Herr<strong>in</strong>g 2001 [5]).Stage 3-Rossification StageHeal<strong>in</strong>g <strong>of</strong> the femoral head beg<strong>in</strong>s. New subchondralbone develops <strong>in</strong> the head <strong>of</strong> the femur, beg<strong>in</strong>n<strong>in</strong>g <strong>in</strong> thecenter and extend<strong>in</strong>g out. The last area to reossify is<strong>of</strong>ten the anterior segment <strong>of</strong> the femoral head.Eventually the femoral head is replaced with wovenbone, which then remodels to trabecular bone. Theflatten<strong>in</strong>g <strong>of</strong> the femoral head may improve. This stageends when the entire head has reossified and is typicallythe longest <strong>of</strong> the four, with a mean duration <strong>of</strong> 51months (Herr<strong>in</strong>g 2001 [5]).Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 1
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39Stage 4-Residual StageThere are no changes <strong>in</strong> the density <strong>of</strong> the bone, but theshape <strong>of</strong> the femoral head can change dur<strong>in</strong>g this phase.The f<strong>in</strong>al shape <strong>of</strong> the femoral head is developed onceskeletal growth is complete. The femoral head may varywidely <strong>in</strong> shape, from normal to flat, at the conclusion <strong>of</strong>this stage. The acetabulum can also change <strong>in</strong> shapedur<strong>in</strong>g this stage. Overgrowth <strong>of</strong> the greater trochantercan occur due to disruption <strong>of</strong> growth <strong>in</strong> the capitalphysis (Herr<strong>in</strong>g 2001 [5]).Several classification systems to describe the extent <strong>of</strong>the disease have been developed. The Catterall systemconsists <strong>of</strong> 4 groups classified based on the extent <strong>of</strong><strong>in</strong>volvement <strong>of</strong> the femoral head on radiographs (Wenger1991 [5a]). The Salter-Thompson system classifieschildren <strong>in</strong>to 2 groups based on the extent <strong>of</strong>subchondral fracture and amount <strong>of</strong> lateral marg<strong>in</strong> <strong>of</strong> thefemoral epiphysis (Wenger 1991 [5a]). Herr<strong>in</strong>g describesclassification based on the <strong>in</strong>volvement <strong>of</strong> the lateralpillar <strong>of</strong> the femoral head on radiographs (Herr<strong>in</strong>g 2004[4b]).The goal <strong>of</strong> treatment <strong>of</strong> children with LCP is to conta<strong>in</strong>the femoral head <strong>in</strong> the acetabulum to maximize aspherical shape <strong>of</strong> the femoral head for good jo<strong>in</strong>tcongruency (Leach 2006 [5], Wenger 1991 [5a]). However,there has been lack <strong>of</strong> agreement <strong>in</strong> treatment<strong>in</strong>terventions <strong>in</strong> children with LCP to achieve this goal(We<strong>in</strong>ste<strong>in</strong> 1997 [5a]). Treatment has ranged fromobservation only, perform<strong>in</strong>g range <strong>of</strong> motion (ROM)exercises, use <strong>of</strong> Petrie casts, use <strong>of</strong> braces, and surgical<strong>in</strong>tervention (Leach 2006 [5], Wenger 1991 [5a]). Evidence <strong>in</strong>the literature has been mixed regard<strong>in</strong>g the success <strong>of</strong>conservative treatment only or surgical <strong>in</strong>tervention(Brech 2006 [3b], Herr<strong>in</strong>g 2004 [3b], Canavese 2008 [4b]).Furthermore, there is limited evidence support<strong>in</strong>g atreatment pathway or methods <strong>in</strong> conservativemanagement <strong>of</strong> LCP.The objectives <strong>of</strong> this guidel<strong>in</strong>e are to: Guide and support consistency <strong>in</strong> delivery <strong>of</strong>physical therapy services for conservativemanagement <strong>of</strong> patients with LCP Promote and optimize range <strong>of</strong> motion, strength, andjo<strong>in</strong>t preservation to m<strong>in</strong>imize impairments andmaximize function Ma<strong>in</strong>ta<strong>in</strong> and improve patient and familysatisfactionEtiologyLCP affects children 3 to 12 years old and is mostcommon <strong>in</strong> children 5 to 7 years old (Leach 2006 [5],Wenger 1991 [5a]). Males are affected 3 to 5 times morethan females. There is bilateral hip <strong>in</strong>volvement <strong>in</strong> 10%to 20% <strong>of</strong> cases (Wenger 1991 [5a]). Children with LCPdisease typically present with a limp, which is acomb<strong>in</strong>ation <strong>of</strong> an antalgic and a Trendelenburg typegait pattern. Pa<strong>in</strong> is <strong>of</strong>ten present <strong>in</strong> the hip or referredto the thigh or knee (Tamai 2004 [5]) . Limp and pa<strong>in</strong> arecommonly made worse with strenuous activities (Tamai2004 [5]) . Range <strong>of</strong> motion <strong>of</strong> the hip is limited, with thegreatest limitations typically <strong>in</strong> hip abduction and<strong>in</strong>ternal rotation (Tamai 2004 [5], Wenger 1991 [5a]).The disease process <strong>in</strong>volves avascular necrosis <strong>of</strong> thefemoral head due to a loss <strong>of</strong> blood supply (Leach 2006[5]). As a result, growth is disturbed <strong>in</strong> the epiphysealand physeal plates, result<strong>in</strong>g <strong>in</strong> premature closure. Thiscan lead to a shortened femoral neck and trochantericovergrowth. There is an asymmetric repair processcaus<strong>in</strong>g deformity <strong>in</strong> the femoral head. The deformedfemoral head then leads to a deformed acetabulum,especially the lateral aspect (We<strong>in</strong>ste<strong>in</strong> 1997 [5a]). Theetiology <strong>of</strong> the disease is unclear, but one theory is thereis onset <strong>of</strong> the disease follow<strong>in</strong>g an episode <strong>of</strong> transientsynovitis <strong>of</strong> the hip (Leach 2006 [5], Wenger 1991 [5a]).Children who present with LCP are typically small fortheir age and have delayed bone age (Leach 2006 [5],We<strong>in</strong>ste<strong>in</strong> 1997 [5a], Wenger 1991 [5a]). Ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g thefemoral head <strong>in</strong> the acetabulum dur<strong>in</strong>g the repair processshould yield a more spherical femoral head and overall amore congruous jo<strong>in</strong>t (Wenger 1991 [5a]).PrognosisPrognosis <strong>of</strong> the disease has been determ<strong>in</strong>ed us<strong>in</strong>gseveral criteria, <strong>in</strong>clud<strong>in</strong>g age <strong>of</strong> onset <strong>of</strong> the disease(Leach 2006 [5], We<strong>in</strong>ste<strong>in</strong> 1997 [5a], Wenger 1991 [5a]), extent<strong>of</strong> <strong>in</strong>volvement <strong>of</strong> the femoral head (Leach 2006 [5], Wenger1991 [5a]) , amount <strong>of</strong> <strong>in</strong>congruity between the femoralhead and acetabulum (Leach 2006 [5]), and amount <strong>of</strong> hipjo<strong>in</strong>t deformity (We<strong>in</strong>ste<strong>in</strong> 1997 [5a]). Onset at a youngage, m<strong>in</strong>imal epiphyseal <strong>in</strong>volvement, and short duration<strong>of</strong> the disease are favorable prognostic factors. Onset atan older age, greater epiphyseal <strong>in</strong>volvement, lateralsubluxation <strong>of</strong> the femoral head, and longer duration <strong>of</strong>the disease make up some <strong>of</strong> the poor prognostic factors(Tamai 2004 [5]).Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 2
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39Guidel<strong>in</strong>e RecommendationsAssessment and Differential DiagnosisCl<strong>in</strong>ical Assessment1. It is recommended that a thorough history andexam<strong>in</strong>ation be completed to establish a differentialdiagnosis and <strong>in</strong>dividualized plan <strong>of</strong> care (APTA 2001[5]).2. It is recommended that the follow<strong>in</strong>g are assessed atthe <strong>in</strong>itial evaluation, on a monthly basis or sooner ifthe patient demonstrates a change <strong>in</strong> status, and atdischarge (Local Consensus [5]): Pa<strong>in</strong> and symptoms Lower extremity (LE) passive range <strong>of</strong> motion(PROM) and active range <strong>of</strong> motion (AROM) Lower extremity strength Gait Balance Outcome measuresPa<strong>in</strong> and symptoms3. It is recommended that pa<strong>in</strong> is assessed us<strong>in</strong>g theOucher pa<strong>in</strong> scale (Beyer 2005 [4a]) or NumericalRat<strong>in</strong>g Scale (NRS) (Williamson 2005 [1b], von Baeyer2009 [4b]).Lower extremity PROM and AROM4. It is recommended that a fluid filled goniometer beused to measure ROM (Rao 2001 [4b]). Hip motionsto assess <strong>in</strong>clude hip flexion, abduction, extension,<strong>in</strong>ternal rotation, external rotation.Note 1: Use <strong>of</strong> a l<strong>in</strong>ear goniometer is alsoacceptable based on availability <strong>in</strong> the cl<strong>in</strong>ic (Rao2001 [4b], Clapper 1988 [4b], Local Consensus [5]).Note 2: Children with LCP who have bettercover<strong>in</strong>g <strong>of</strong> the femoral head <strong>in</strong> the acetabulumand a more normalized acetabular shape willhave greater hip abduction range <strong>of</strong> motion(Grzegorzewski 2006 [4b]).5. It is recommended that knee and ankle range <strong>of</strong>motion be assessed at the <strong>in</strong>itial evaluation andthereafter if they are significantly limited.Lower extremity strength6. It is recommended that quantitative muscle test<strong>in</strong>g isperformed us<strong>in</strong>g a hand held dynamometer due to itshigh <strong>in</strong>tra- and <strong>in</strong>ter-rater reliability (Gajdosik 2005[4b], Escolar 2001 [4b]). Muscle groups to assess<strong>in</strong>clude hip flexors, hip abductors, hip extensors, hip<strong>in</strong>ternal rotators, hip external rotators, kneeextensors, knee flexors, and any other muscle groupthat is significantly limitedGait7. It is recommended that gait be qualitatively assessedfor common LCP deviations. Commonly observedgait characteristics seen <strong>in</strong> children with LCP<strong>in</strong>clude, but are not limited to: <strong>in</strong>creased hip adduction on stance leg (Westh<strong>of</strong>f2006 [4b]), trunk lean outside the normal range (Westh<strong>of</strong>f 2006[4b]), trendelenburg (Westh<strong>of</strong>f 2006 [4b]) (hip drop onunaffected limb while <strong>in</strong> sw<strong>in</strong>g), compensated trendelenburg/reversetrendelenburg/Duchenne (Westh<strong>of</strong>f 2006 [4b])(trunk lean to the affected side while <strong>in</strong> stanceon the affected limb), toe <strong>in</strong> or toe out (Yoo 2008 [4b]).Note 1: Based on limited accessibility andfeasibility, the gold standard for gait analysis <strong>of</strong>3-D gait k<strong>in</strong>ematics and k<strong>in</strong>etics (Toro 2003 [1b]) isnot recommended to be used <strong>in</strong> the cl<strong>in</strong>ic (LocalConsensus [5]).Note 2: There is <strong>in</strong>sufficient evidence and lack <strong>of</strong>reliability and validity (Toro 2003 [1b]) to supportuse <strong>of</strong> observational gait assessment tools withthis population (Local Consensus [5]).Balance8. It is recommended that balance be assessed based onweight bear<strong>in</strong>g status. The desired outcome is thatthe patient ma<strong>in</strong>ta<strong>in</strong> balance for age appropriatetimes for safe ambulation and stair negotiation (LocalConsensus [5]).Note: In patients 7 years or older, balance is tobe assessed us<strong>in</strong>g the Pediatric Balance Scale(Franjo<strong>in</strong>e 2003 [4b]). If the patient is younger than7 years old, the test is unavailable, time does notpermit its use, or the patient is unable to followcommands, balance is assessed us<strong>in</strong>g s<strong>in</strong>gle legstance on the <strong>in</strong>volved side compared to theun<strong>in</strong>volved side (Local Consensus [5]).Outcome measure scores9. It is recommended that the age appropriate PediatricQuality <strong>of</strong> Life Inventory Version 4.0 (PedsQL)(Varni 2001 [4a])Physical Function<strong>in</strong>g section isadm<strong>in</strong>istered at the <strong>in</strong>itial evaluation, on a monthlybasis for reassessment <strong>of</strong> patient’s reportedfunctional status, and at discharge (Local Consensus[5]).Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 3
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39Note 1: The Parent Report for Toddlers isadm<strong>in</strong>istered for children 2 to 4 years old (Varni2007a [4a]).Note 2: The Young Child Self Report isadm<strong>in</strong>istered for children 5 to 7 years old (Varni2007a [4a]).Note 3: The Child Self Report is adm<strong>in</strong>isteredfor children 8 to12 years old (Varni 2007a [4a]).Note 4: For patients who are 5 to 12 years oldand unable to conceptually understand thequestionnaire tool, it is acceptable for the parentto complete the parent proxy form for the youngchild (age 5 to 7 years old) or child (age 8 to 12years old (Varni 2007b [4a]).Classification <strong>of</strong> Phases <strong>of</strong> Rehabilitation10. It is recommended that the Classification Instrument<strong>in</strong> <strong>Perthes</strong> (CLIPer) be used to place the patient <strong>in</strong>toa rehabilitation classification phase uponexam<strong>in</strong>ation (Local Consensus [5]) (See Appendix 1 for<strong>in</strong>structions and score sheet).Note 1: <strong>Conservative</strong> physical therapy treatmentwill be guided us<strong>in</strong>g the rehabilitationclassification phases (Local Consensus [5]).11. It is recommended that the patient be re-exam<strong>in</strong>edus<strong>in</strong>g the CLIPer on a monthly basis to determ<strong>in</strong>ethe appropriate progression through therehabilitation classification stages (Local Consensus[5]).Note 1: The patient is to be re-exam<strong>in</strong>ed soonerif there is a change <strong>in</strong> status (Local Consensus [5]).Note 2: Pa<strong>in</strong>, ROM, strength, gait, and balancewill be monitored at each treatment visit todeterm<strong>in</strong>e need for reassessment andreclassification us<strong>in</strong>g the CLIPer (Local Consensus[5]). (See Appendix 1 for <strong>in</strong>structions and scoresheet).12. It is recommended the patient is referred back to theorthopedic surgeon if the patient’s status worsensover two consecutive PT sessions (Local Consensus[5]).<strong>Management</strong> RecommendationsPhysical Therapy Interventions13. It is the recommendation that the patient diagnosedwith LCP and is a candidate for conservativemanagement receive supervised physical therapy<strong>in</strong>tervention (Local Consensus [5]). (See Appendix 2 foralgorithm).Note: Physical therapy <strong>in</strong>terventions have beenshown to improve ROM and strength <strong>in</strong> thispatient population (Brech 2006 [3b]). Individualswho participate <strong>in</strong> supervised cl<strong>in</strong>ic visitsdemonstrate greater improvement <strong>in</strong> musclestrength, functional mobility, gait speed, andquality <strong>of</strong> exercise performance than those whoreceive a home exercise program alone or no<strong>in</strong>struction at all (Friedrich 1996 [2b]). Individualswho receive regular positive feedback from aphysical therapist are more likely to be compliantwith a supplemental home exercise program(Sluijs 1993 [4b]).14. It is recommended that supervised physical therapyis supplemented with a customized written homeexercise program (Friedrich 1996 [2b]) <strong>in</strong> all phases <strong>of</strong>rehabilitation15. It is recommended that the physical therapist engage<strong>in</strong> ongo<strong>in</strong>g communication with the patient, family,and referr<strong>in</strong>g physician regard<strong>in</strong>g the diseaseprocess and plan <strong>of</strong> care (Local Consensus [5]).16. It is recommended that the patient beg<strong>in</strong> physicaltherapy upon diagnosis <strong>of</strong> LCP (Local Consensus [5]).17. It is recommended that advancement through thephases <strong>of</strong> rehabilitation follow a goal based ratherthan a time based progression.Note: Treatment is to focus on conta<strong>in</strong>ment <strong>of</strong>the femoral head <strong>in</strong> the acetabulum throughouteach phase <strong>of</strong> the disease (Leach 2006 [5]).Phases <strong>of</strong> RehabilitationSevere Involvement Phase (CLIPer score 14 to 24)18. It is recommended that goals <strong>of</strong> this phase <strong>in</strong>clude(Local Consensus [5]): Reduce pa<strong>in</strong> to less than 7/10 Increase ROM to 50% or greater <strong>of</strong> theun<strong>in</strong>volved side Increase strength to 50% or greater <strong>of</strong> theun<strong>in</strong>volved side Patient to be <strong>in</strong>dependent with the appropriateassistive device and weight bear<strong>in</strong>g precautionsImprove balance to 50% or greater <strong>of</strong> themaximum Pediatric Balance Scale score ors<strong>in</strong>gle limb stance <strong>of</strong> the un<strong>in</strong>volved side.19. It is recommended that supervised Physical Therapyservices are provided weekly (Bailes 2008 [5a]) at afrequency <strong>of</strong> 2 times per week (Local Consensus [5]).Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 4
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 3920. It is recommended that treatment <strong>in</strong>terventions <strong>of</strong>the Severe Involvement Phase <strong>in</strong>clude: Pa<strong>in</strong>o Hot pack for pa<strong>in</strong> management withstretch<strong>in</strong>g (Nadler 2004 [1b])o Cryotherapy (Nadler 2004 [1b])o Medications as prescribed by the referr<strong>in</strong>gphysician for pa<strong>in</strong> (Local Consensus [5]).ROM (See Appendix 3 for exerciseprescription)o Static stretch for LE musculature (Moseley2005 [2A], Bandy 1998 [2a], Davis 2005 [2b]) withor without use <strong>of</strong> a hot pack based onpatient preference and comfort.o Dynamic ROM(Bandy 1998 [2a])and activeassistive range <strong>of</strong> motion (AAROM) maybe appropriate if the patient is muscleguard<strong>in</strong>g due to pa<strong>in</strong> and unable to achieveend range motion with static stretch (LocalConsensus [5]).o Perform AROM and AAROM follow<strong>in</strong>gpassive stretch<strong>in</strong>g to ma<strong>in</strong>ta<strong>in</strong> newly ga<strong>in</strong>edROM (Dep<strong>in</strong>o 2000 [2b]).oPerform stretch<strong>in</strong>g <strong>in</strong> a position that issuitable for the <strong>in</strong>dividual and <strong>in</strong>clude hipIR, hip ER, hip abduction, hip extension,and any other lower extremity motion thatis significantly limited (Local Consensus [5]).Strength (See Appendix 4 for exerciseprescription)o Beg<strong>in</strong> with isometric exercise and progressto isotonic exercises <strong>in</strong> a gravity lessenedposition with further progression to isotonicexercises aga<strong>in</strong>st gravity. It is appropriateto <strong>in</strong>clude concentric and eccentriccontractions (Brech 2006 [3b]).o Beg<strong>in</strong> with 2 sets <strong>of</strong> 10 to 15 repetitions <strong>of</strong>each exercise (Rhea 2002 [2b], Faigenbaum 1996[4b]), with progression to 3 sets <strong>of</strong> eachexercise to be used (Rhea 2002 [2b]).Note: If the patient is unable to perform 2sets <strong>of</strong> 10 repetitions <strong>of</strong> an exercise, thedifficulty <strong>of</strong> the exercise is to be decreasedeither through weight or type <strong>of</strong> exercise(Local Consensus [5]).o Focus on strengthen<strong>in</strong>g <strong>of</strong> hip abductors,hip flexors, hip external rotators, hip<strong>in</strong>ternal rotators, hip extensors, or any otherlower extremity muscle group that displaysoooosignificant strength deficits (Westh<strong>of</strong>f 2006[4b], Bolgla 2005 [4b]). Special attention is tobe given to the gluteus medius <strong>in</strong> order tom<strong>in</strong>imize <strong>in</strong>traarticular pa<strong>in</strong> (Plasschaert 2006[4b]) and for pelvic control dur<strong>in</strong>g s<strong>in</strong>gle legactivities and ambulation (Westh<strong>of</strong>f 2006 [4b],Bolgla 2005 [4b]).Performance <strong>of</strong> weight bear<strong>in</strong>g vs. nonweightbear<strong>in</strong>g exercises is based on theweight bear<strong>in</strong>g status as determ<strong>in</strong>ed by thephysician, patient’s tolerance to weightbear<strong>in</strong>g positions, and safety (Local Consensus[5]).Weight bear<strong>in</strong>g activities can be performedwhen the patient can apply weight on the<strong>in</strong>volved extremity (Bolgla 2005 [4b]) andsafely perform the exercise <strong>in</strong> a stand<strong>in</strong>gposition.Closed cha<strong>in</strong> double limb exercises withlight resistance (less than full body weight)(e.g. Total Gym ®) may be performed(Bolgla 2005 [4b]).It is not recommended to perform s<strong>in</strong>glelimb closed cha<strong>in</strong> exercises on the <strong>in</strong>volvedside (Local Consensus [5]) due to <strong>in</strong>creased<strong>in</strong>tra-articular pressure <strong>in</strong> the hip jo<strong>in</strong>t(Levangie 1992 [5]).Balanceo Activities that <strong>in</strong>clude double limb stanceand a narrowed base <strong>of</strong> support on stablesurfaces may be performed if weightbear<strong>in</strong>g status and symptoms allow (LocalConsensus [5]).o It is not recommended to perform s<strong>in</strong>glelimb activities (Local Consensus [5])due to<strong>in</strong>creased <strong>in</strong>tra-articular pressure <strong>in</strong> the hipjo<strong>in</strong>t (Levangie 1992 [5]) .Gaito Follow the referr<strong>in</strong>g physician’s guidel<strong>in</strong>esfor weight bear<strong>in</strong>g status (Local Consensus [5]).o Beg<strong>in</strong> gait tra<strong>in</strong><strong>in</strong>g with the appropriateassistive device given weight bear<strong>in</strong>g statusas determ<strong>in</strong>ed by the referr<strong>in</strong>g physician orbased on the patient’s tolerance to fullweight bear<strong>in</strong>g due to pa<strong>in</strong> or safety (LocalConsensus [5]).Moderate Involvement Phase (CLIPer score 6 to 13)21. It is recommended that goals <strong>of</strong> this phase <strong>in</strong>clude:Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 5
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39 Reduce pa<strong>in</strong> to less than 4/10 Increase ROM to greater than 75% <strong>of</strong> theun<strong>in</strong>volved side Increase strength to greater than 75% <strong>of</strong> theun<strong>in</strong>volved side Progress from use <strong>of</strong> an assistive device ifapproved by physician and without adverseeffects Independence with a step to pattern on stairswithout UE support Improved efficiency <strong>in</strong> walk<strong>in</strong>g Improved balance to greater than 75% <strong>of</strong> themaximum Pediatric Balance Scale score ors<strong>in</strong>gle limb stance <strong>of</strong> the un<strong>in</strong>volved side(Local Consensus [5])22. It is recommended that supervised Physical Therapyservices are provided on a weekly basis (Bailes 2008[5a]) at a frequency <strong>of</strong> 1 to 2x/week (Local Consensus[5]).23. It is recommended that treatment <strong>in</strong>terventions <strong>of</strong>the Moderate Involvement Phase <strong>in</strong>clude: Pa<strong>in</strong>o Hot pack for pa<strong>in</strong> management withstretch<strong>in</strong>g (Nadler 2004 [1b])o Cryotherapy (Nadler 2004 [1b])o Medications as prescribed by the referr<strong>in</strong>gphysician for pa<strong>in</strong> (Local Consensus [5]).ROM (See Appendix 3 for exerciseprescription)o Static stretch for LE musculature (Moseley2005 [2A], Bandy 1998 [2a], Davis 2005 [2b]) withor without use <strong>of</strong> a hot pack based onpatient preference and comforto Dynamic ROM (Bandy 1998 [2a])andAAROM may be appropriate if the patientis muscle guard<strong>in</strong>g due to pa<strong>in</strong> and unableto achieve end range motion with staticstretch (Local Consensus [5]).o Perform AROM and AAROM follow<strong>in</strong>gpassive stretch<strong>in</strong>g to ma<strong>in</strong>ta<strong>in</strong> newly ga<strong>in</strong>edROM (Dep<strong>in</strong>o 2000 [2b]).oPerform stretch<strong>in</strong>g <strong>in</strong> a position that issuitable for the <strong>in</strong>dividual and <strong>in</strong>clude hipIR, hip ER, hip abduction, hip extension,and any other lower extremity motion thatis significantly limited (Local Consensus [5]).Strengthen<strong>in</strong>g (See Appendix 4 for exerciseprescription.)o Perform isotonic exercises <strong>in</strong> gravitylessened and aga<strong>in</strong>st gravity positions, and<strong>in</strong>clude concentric and eccentriccontractions (Brech 2006 [3b]).o Weight bear<strong>in</strong>g and non-weight bear<strong>in</strong>gactivities can be used <strong>in</strong> comb<strong>in</strong>ation basedon the patient’s ability (Jacobs 2008 [4b]) andgoals <strong>of</strong> the treatment session.o Upper extremity supported functionaldynamic s<strong>in</strong>gle limb activities (e.g. step ups,side steps) may be performed (LocalConsensus [5]).o Double limb closed cha<strong>in</strong> exercises may beused with light resistance (e.g. m<strong>in</strong>i-squats,wall-sits) if the weight bear<strong>in</strong>g status allows(Local Consensus [5]).Balanceo Activities that <strong>in</strong>clude double limb stancewith narrowed base <strong>of</strong> support on unstablesurfaces may be performed as weightbear<strong>in</strong>g status and patient comfort allow(Local Consensus [5]).o Limit prolonged s<strong>in</strong>gle limb activities (LocalConsensus [5]) due to excessive jo<strong>in</strong>tcompressive forces (Levangie 1992 [5]).Gaito Cont<strong>in</strong>ue to follow the referr<strong>in</strong>g physician’sguidel<strong>in</strong>es for weight bear<strong>in</strong>g status (LocalConsensus [5]).o Progress to gait tra<strong>in</strong><strong>in</strong>g without use <strong>of</strong> anassistive device as appropriate, focus<strong>in</strong>g onm<strong>in</strong>imiz<strong>in</strong>g deficits and improv<strong>in</strong>gefficiency <strong>of</strong> walk<strong>in</strong>g (Local Consensus [5]).o Stair negotiation and other functionalmobility (Local Consensus [5]).Mild Involvement Phase (CLIPer score 0 to 5)24. It is recommended that goals <strong>of</strong> this phase <strong>in</strong>clude: Reduce pa<strong>in</strong> to 1/10 or less Increase range <strong>of</strong> motion to 90% or greater <strong>of</strong>the un<strong>in</strong>volved side Increase strength to 90% or greater <strong>of</strong> theun<strong>in</strong>volved side Improve balance to 90% or greater <strong>of</strong> themaximum Pediatric Balance Scale score ors<strong>in</strong>gle limb stance <strong>of</strong> the un<strong>in</strong>volved side Ambulation with a non-pa<strong>in</strong>ful limp withnormal efficiencyCopyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 6
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39o Negotiation <strong>of</strong> stairs utiliz<strong>in</strong>g a reciprocalpattern(Local Consensus [5])25. It is recommended that supervised physical therapyservices are provided on a periodic or bimonthlybasis (Bailes 2008 [5a]) at a frequency <strong>of</strong> 1 to 2x/month(Local Consensus [5]).26. It is recommended that treatment <strong>in</strong>terventions <strong>of</strong>the Mild Involvement Phase <strong>in</strong>clude: Pa<strong>in</strong>o Hot pack for pa<strong>in</strong> management withstretch<strong>in</strong>g (Nadler 2004 [1b])o Cryotherapy (Nadler 2004 [1b])o Medications as prescribed by the referr<strong>in</strong>gphysician for pa<strong>in</strong> (Local Consensus [5])ROM (See Appendix 3 for exerciseprescription.)o Static stretch for LE musculature (Moseley2005 [2A], Bandy 1998 [2a], Davis 2005 [2b]) withor without use <strong>of</strong> a hot pack based onpatient preference and comfort (Nadler 2004[1b])o Dynamic ROM (Bandy 1998 [2a])andAAROM may be used if the patient ismuscle guard<strong>in</strong>g due to pa<strong>in</strong> and is unableto achieve end range <strong>of</strong> motion with staticstretch (Local Consensus [5]).o Perform AROM and AAROM follow<strong>in</strong>gpassive stretch<strong>in</strong>g to ma<strong>in</strong>ta<strong>in</strong> newly ga<strong>in</strong>edROM (Dep<strong>in</strong>o 2000 [2b]).oPerform stretch<strong>in</strong>g <strong>in</strong> a position that issuitable for the <strong>in</strong>dividual and <strong>in</strong>clude hipIR, hip ER, hip abduction, hip extension,and any other lower extremity motion thatis significantly limited (Local Consensus [5]).Strengthen<strong>in</strong>g (See Appendix 4 for exerciseprescription)o Isotonic exercises <strong>in</strong> gravity lessened andaga<strong>in</strong>st gravity positions may be used and<strong>in</strong>clude concentric and eccentriccontractions (Brech 2006 [3b])o Functional dynamic s<strong>in</strong>gle limb activitieswith UE support as needed for patientsafety (e.g. step ups, sidesteps) may beperformed (Local Consensus [5])o Closed k<strong>in</strong>etic cha<strong>in</strong> s<strong>in</strong>gle limb exerciseswith light resistance (leg press) may beperformed (Bolgla 2005 [4b]).Balanceo Double limb stance with narrowed base <strong>of</strong>support on unstable surfaces withperturbations may be performed as weightbear<strong>in</strong>g status and patient comfort allow(Local Consensus [5]).o Limit prolonged s<strong>in</strong>gle limb activities (LocalConsensus [5]) due to excessive jo<strong>in</strong>tcompressive forces (Levangie 1992 [5]).Gaito Cont<strong>in</strong>ue to follow the referr<strong>in</strong>g physician’sguidel<strong>in</strong>es for weight bear<strong>in</strong>g statuso Progress to gait tra<strong>in</strong><strong>in</strong>g without the use <strong>of</strong>an assistive device as appropriate, focus<strong>in</strong>gon m<strong>in</strong>imiz<strong>in</strong>g deficits and improv<strong>in</strong>g theefficiency <strong>of</strong> walk<strong>in</strong>g.o Stair negotiation and other functionalmobility.o Progress to walk<strong>in</strong>g on uneven surfaceswith an emphasis on safety.(Local Consensus [5])Discharge Criteria27. It is recommended that children may be dischargedfrom physical therapy at the time <strong>of</strong> surgical<strong>in</strong>tervention or when four <strong>of</strong> the five follow<strong>in</strong>gcriteria have been met: Pa<strong>in</strong> rat<strong>in</strong>g 0 to 1/10 Range <strong>of</strong> motion 90 to 100% <strong>of</strong> the un<strong>in</strong>volvedside Strength 90 to 100% <strong>of</strong> the un<strong>in</strong>volved side Balance 90 to 100% <strong>of</strong> the maximum score onthe Pediatric Balance Scale or ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>gbalance with SLS 90 to 100% <strong>of</strong> the un<strong>in</strong>volvedside Gait presents with a non-pa<strong>in</strong>ful limp and uses areciprocal pattern on the stairs.(Local Consensus [5])28. It is recommended that follow<strong>in</strong>g discharge fromsupervised physical therapy, the patient cont<strong>in</strong>ue ahome exercise program to ma<strong>in</strong>ta<strong>in</strong> improvements<strong>in</strong> strength, balance, locomotor function, and pa<strong>in</strong>management (Local Consensus [5]) until it has beendeterm<strong>in</strong>ed by the physician that the disease processis complete (Local Consensus [5]).29. It is recommended that physical therapy services areprovided as needed on a consultative basis (Bailes2008 [5a]) to manage flare up <strong>of</strong> symptoms or otherconcerns (Local Consensus [5]).Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 7
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 3930. It is recommended that the post-operative guidel<strong>in</strong>efor LCP be followed when a patient is dischargedfrom conservative management physical therapydue to surgical <strong>in</strong>tervention. (Local Consensus [5]).Future Research Agenda1. In children ages 3 to 12 years old with <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> disease, what is the reliability and validity <strong>of</strong>the Classification Instrument <strong>in</strong> <strong>Perthes</strong> (CLIPer)?2. In children ages 3 to 12 years old with <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> disease, what are the effects <strong>of</strong> weightbear<strong>in</strong>g on symptoms, jo<strong>in</strong>t preservation, andfunction?Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 8
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39Appendix 1Classification Instrument <strong>in</strong> <strong>Perthes</strong> (CLIPer)Doma<strong>in</strong>s <strong>of</strong> Assessment DescriptionScorePa<strong>in</strong> with ADLs7 to10/10 44 to 6/10 20 to 3/10 0Hip ROMLess than 50% <strong>of</strong> un<strong>in</strong>volved side for the majority <strong>of</strong> directions 650 to 75% <strong>of</strong> un<strong>in</strong>volved side for the majority <strong>of</strong> directions 376 to 100% <strong>of</strong> un<strong>in</strong>volved side for the majority <strong>of</strong> directions 0Hip StrengthLess than 50% <strong>of</strong> un<strong>in</strong>volved side for the majority <strong>of</strong> muscle groups 650 to 75% <strong>of</strong> un<strong>in</strong>volved side for the majority <strong>of</strong> muscle groups 376 to 100% <strong>of</strong> un<strong>in</strong>volved side for the majority <strong>of</strong> muscle groups 0BalancePediatric balance score less than 50% <strong>of</strong> best score (best score=56) OR SLSwith eyes open less than 50% <strong>of</strong> time on un<strong>in</strong>volved sidePediatric balance score 50 to 75% <strong>of</strong> best score (best score=56) OR SLSwith EO <strong>of</strong> un<strong>in</strong>volved side 50 to 75% length <strong>of</strong> timePediatric balance score 76 to 100% <strong>of</strong> best score (best score=56) OR SLSwith EO 76 to 100% <strong>of</strong> un<strong>in</strong>volved side420GaitNWB and uses an assistive device and without AD, displays excessive gaitdeficits with decreased efficiencyNo assistive device and displays excessive deficits without a decrease <strong>in</strong>efficiencyUses step to pattern on stairsNon-pa<strong>in</strong>ful limpAble to perform reciprocal pattern on stairs420Rehabilitation Classification PhaseScore total 14 to 24: Severe InvolvementScore total 6 to 13: Moderate InvolvementScore total 0 to 5: Mild InvolvementTOTAL:Instructions for useUpon exam<strong>in</strong>ation, assess pa<strong>in</strong> with ADL’s, hip range <strong>of</strong> motion, hip strength, balance, and gait. Assign a correlat<strong>in</strong>gscore for each doma<strong>in</strong> <strong>of</strong> assessment based on exam<strong>in</strong>ation results and total the sum. Place the patient <strong>in</strong> a rehabilitationclassification phase based on the total score to guide physical therapy treatment.Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 9
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39Appendix 2Start: Patient has beendiagnosed with <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong>Is classification score14 to 24?NoYesFollow severe <strong>in</strong>volvement phasetreatmentIs classification score6 to 13?NoYesFollow moderate <strong>in</strong>volvement phasetreatmentIs classification score0 to 5?YesNoDoes patient meetdischarge criteria?YesDiscont<strong>in</strong>ue PT.Cont<strong>in</strong>ue with HEP.Follow consultativemodel as needed.Follow mild <strong>in</strong>volvement phasetreatmentPt to have immediatesurgical procedure?NoYesDiscont<strong>in</strong>ue preoperativePT.Guidel<strong>in</strong>ediscont<strong>in</strong>ued.Reassess monthly or sooner if patient demonstrates a change <strong>in</strong> status: Pa<strong>in</strong>, ROM, Strength, Balance, and GaitHas classification scorechanged?YesDoes condition worsenover 2 consecutive PTsessions?YesRefer back toOrthopaedicsurgeon.NoNoCont<strong>in</strong>ue PT undercurrent rehabilitationphasePlace patient <strong>in</strong> newclassification phasebased on new scorefor cont<strong>in</strong>uedtreatmentCopyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 10
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39Appendix 3ROM Exercise PrescriptionIntervention Parameters Intensity Notes Muscle GroupsStatic Stretch 2 m<strong>in</strong>utes <strong>of</strong> stretch<strong>in</strong>gper day, per musclegroup (Santonja Med<strong>in</strong>a 2007[2b], Cipriani 2003 [4b]).Gentle static hold DynamicStretch30 second hold time,do<strong>in</strong>g 4 repetitions permuscle group (Bandy 1994[2a], Reid 2004 [2b], Dep<strong>in</strong>o2000 [2b]).If not tolerated, may do10 to 30 second hold timewith repetitions adjustedto meet 2 m<strong>in</strong>uterequirement (e.g. ifhold<strong>in</strong>g 15 seconds,would do 8 stretches)(Cipriani 2003 [4b], Roberts1999 [4b]).5 second hold, done with24 repetitions permuscle group per day tomeet 2 m<strong>in</strong>ute stretch<strong>in</strong>gtime required (Bandy 1998[2a], Santonja Med<strong>in</strong>a 2007[2b], Cipriani 2003 [4b]).Should be with<strong>in</strong> patientpa<strong>in</strong> tolerance andwithout muscle guard<strong>in</strong>gso as to prevent tissuedamage and <strong>in</strong>flammatoryresponse (Bandy 1994 [2a],Santonja Med<strong>in</strong>a 2007 [2b],Davis 2005 [2b]).Self selected <strong>in</strong>tensity bypatient as long as notcaus<strong>in</strong>g pa<strong>in</strong>This is the preferredmethod <strong>of</strong> stretch<strong>in</strong>g toga<strong>in</strong> flexibility and/orROM (Moseley 2005 [2A],Bandy 1994 [2a], Davis 2005[2b]).stretch<strong>in</strong>g be done afterwarm up, but prior toactive exercises toma<strong>in</strong>ta<strong>in</strong> newly ga<strong>in</strong>edROM (Dep<strong>in</strong>o 2000 [2b]).Dynamic stretch is donewith patient activation <strong>of</strong>antagonistic muscle group(Bandy 1998 [2a]).This is done if patientdoes not tolerate staticstretchAny limited motions ortight muscles <strong>in</strong> the lowerextremities should beaddressed, but withparticular emphasis on thefollow<strong>in</strong>g: hip adductors hip <strong>in</strong>ternal rotators hip external rotators hip flexors(Local Consensus [5])Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 11
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39Appendix 4Strengthen<strong>in</strong>g Exercise PrescriptionIntervention Parameters Intensity Notes Muscle GroupsIsometricStrengthen<strong>in</strong>g 10 second hold with 10repetitions per muscle Performed atapproximately 75% Performed with hip <strong>in</strong>neutral position,Any lower extremitymuscle that demonstratesgroup, for a total <strong>of</strong> 100 maximal contraction o 0 degrees hip weakness should beseconds (Local Consensus (Local Consensus [5])flexion/extension, addressed, however,[5]).o 0 degrees hipspecial attention should be Can adjust hold time to 5abduction/adductiongiven to the follow<strong>in</strong>g:seconds, would thenand hip abductorsadjust to 20 repetitions too 0 degrees hip(especially gluteusmeet 100 secondexternal/<strong>in</strong>ternal medius)requirementrotation hip <strong>in</strong>ternal rotators(Local Consensus [5]) hip external rotatorsIsotonic High repetitions (10 to Low resistance hip flexorsStrengthen<strong>in</strong>g 15 reps) and 2 to 3 sets(Campos 2002 [2b],Faigenbaum 1999 [2b]).Perform both concentricand eccentric contractions(Brech 2006 [3b])Rest 1 to 3 m<strong>in</strong>utesbetween sets (Campos 2002[2b], Jacobs 2008 [4b], Bolgla2005 [4b])(depend<strong>in</strong>g onstrength and endurance)Rest can <strong>in</strong>clude exercise<strong>of</strong> a different musclegroup or cessation <strong>of</strong>activityIf patient is unable toperform 2 sets <strong>of</strong> 10repetitions with properform, exercise <strong>in</strong>tensityshould be decreased eitherthrough weight or type <strong>of</strong>exercisehip extensors(Plasschaert 2006 [4b],Westh<strong>of</strong>f 2006 [4b], Bolgla2005 [4b])Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 12
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39Members <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong>Team 2010Division <strong>of</strong> Occupational Therapy and Physical TherapyGuidel<strong>in</strong>e Development TeamJulie A. Lee, PT, DPT, Team Leader, Division <strong>of</strong> OccupationalTherapy and Physical TherapyMichael D. Allen, PT, OCS, Division <strong>of</strong> Occupational Therapy andPhysical TherapyKathleen Hugentobler, PT, DPT, Division <strong>of</strong> Occupational Therapyand Physical TherapyChristopher Kovacs, PT, DPT, CSCS, Division <strong>of</strong> OccupationalTherapy and Physical TherapyJessica K<strong>in</strong>g Monfreda PT, DPT, Division <strong>of</strong> Occupational Therapyand Physical TherapyBarbara Nolte, PT, Division <strong>of</strong> Occupational Therapy and PhysicalTherapyElizabeth Woeste, MPT, Division <strong>of</strong> Occupational Therapy andPhysical TherapySenior Cl<strong>in</strong>ical DirectorRebecca D. Reder OTD, OTR/L, Division <strong>of</strong> Occupational Therapyand Physical TherapyDivision <strong>of</strong> Health Policy & Cl<strong>in</strong>ical Effectiveness SupportEloise Clark, MPH, FacilitatorDanette Stanko, MA, MPH, EpidemiologistEdward Donovan, MD, Medical Director, Cl<strong>in</strong>ical EffectivenessUma Kotagal, MBBS, MSc, VP, Division DirectorAll Team Members and Cl<strong>in</strong>ical Effectiveness support staff listedabove have signed a conflict <strong>of</strong> <strong>in</strong>terest declaration and none werefound.Ad hoc AdvisorsMichelle Kiger, OTR/L, Division <strong>of</strong> Occupational Therapy andPhysical TherapyMary Gilene, MBA, Division <strong>of</strong> Occupational Therapy and PhysicalTherapyBarbarie Hill MLS, Pratt LibraryKaren Vonderhaar, MS, RN, MethodologistDevelopment ProcessThe process by which this guidel<strong>in</strong>e was developed is documented <strong>in</strong>the Guidel<strong>in</strong>e Development Process Manual; a Team B<strong>in</strong>derma<strong>in</strong>ta<strong>in</strong>s m<strong>in</strong>utes and other relevant development materials. Therecommendations conta<strong>in</strong>ed <strong>in</strong> this guidel<strong>in</strong>e were formulated by an<strong>in</strong>terdiscipl<strong>in</strong>ary work<strong>in</strong>g group which performed systematic searchand critical appraisal <strong>of</strong> the literature, us<strong>in</strong>g the Table <strong>of</strong> EvidenceLevels described follow<strong>in</strong>g the references, and exam<strong>in</strong>ed current localcl<strong>in</strong>ical practices.To select evidence for critical appraisal by the group for thisguidel<strong>in</strong>e, the Medl<strong>in</strong>e, EmBase and the Cochrane databases weresearched for dates <strong>of</strong> January 1970 to April 2009 to generate anunref<strong>in</strong>ed, “comb<strong>in</strong>ed evidence” database us<strong>in</strong>g a search strategyfocused on answer<strong>in</strong>g cl<strong>in</strong>ical questions relevant to <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> and employ<strong>in</strong>g a comb<strong>in</strong>ation <strong>of</strong> Boolean search<strong>in</strong>gon human-<strong>in</strong>dexed thesaurus terms (MeSH head<strong>in</strong>gs us<strong>in</strong>g an OVIDMedl<strong>in</strong>e <strong>in</strong>terface) and “natural language” search<strong>in</strong>g on search<strong>in</strong>g onhuman-<strong>in</strong>dexedthesaurus terms (MeSH head<strong>in</strong>gs us<strong>in</strong>g an OVID Medl<strong>in</strong>e <strong>in</strong>terface)and “natural language” search<strong>in</strong>g on words <strong>in</strong> the title, abstract, and<strong>in</strong>dex<strong>in</strong>g terms. The citations were reduced by: elim<strong>in</strong>at<strong>in</strong>gduplicates, review articles, non-English articles, and adult articles.The result<strong>in</strong>g abstracts were reviewed by a methodologist to elim<strong>in</strong>atelow quality and irrelevant citations. Dur<strong>in</strong>g the course <strong>of</strong> theguidel<strong>in</strong>e development, additional cl<strong>in</strong>ical questions were generatedand subjected to the search process, and some relevant review articleswere identified.Tools to assist <strong>in</strong> the effective dissem<strong>in</strong>ation and implementation <strong>of</strong>the guidel<strong>in</strong>e may be available onl<strong>in</strong>e athttp://www.c<strong>in</strong>c<strong>in</strong>natichildrens.org/svc/alpha/h/health-policy/evbased/default.htm. Experience with the implementation <strong>of</strong> earlierpublications <strong>of</strong> this guidel<strong>in</strong>e has provided learn<strong>in</strong>gs which have been<strong>in</strong>corporated <strong>in</strong>to this revision.Once the guidel<strong>in</strong>e has been <strong>in</strong> place for three years, the developmentteam reconvenes to explore the cont<strong>in</strong>ued validity <strong>of</strong> the guidel<strong>in</strong>e.This phase can be <strong>in</strong>itiated at any po<strong>in</strong>t that evidence <strong>in</strong>dicates acritical change is needed.Recommendations have been formulated by a consensus processdirected by best evidence, patient and family preference and cl<strong>in</strong>icalexpertise. Dur<strong>in</strong>g formulation <strong>of</strong> these recommendations, the teammembers have rema<strong>in</strong>ed cognizant <strong>of</strong> controversies anddisagreements over the management <strong>of</strong> these patients. They havetried to resolve controversial issues by consensus where possible and,when not possible, to <strong>of</strong>fer optional approaches to care <strong>in</strong> the form <strong>of</strong><strong>in</strong>formation that <strong>in</strong>cludes best support<strong>in</strong>g evidence <strong>of</strong> efficacy foralternative choices.The guidel<strong>in</strong>e has been reviewed and approved by cl<strong>in</strong>ical experts not<strong>in</strong>volved <strong>in</strong> the development process, distributed to seniormanagement, and other parties as appropriate to their <strong>in</strong>tendedpurposes.The guidel<strong>in</strong>e was developed without external fund<strong>in</strong>g. All TeamMembers and Cl<strong>in</strong>ical Effectiveness support staff listed have declaredwhether they have any conflict <strong>of</strong> <strong>in</strong>terest and none were identified.Copies <strong>of</strong> this Evidence-based Care Guidel<strong>in</strong>e (EBCG) and its anyavailable implementation tools are available onl<strong>in</strong>e and may bedistributed by any organization for the global purpose <strong>of</strong> improv<strong>in</strong>gchild health outcomes. Website address:http://www.c<strong>in</strong>c<strong>in</strong>natichildrens.org/svc/alpha/h/healthpolicy/ev-based/default.htmExamples <strong>of</strong> approved uses <strong>of</strong> theEBCG <strong>in</strong>clude the follow<strong>in</strong>g:• copies may be provided to anyone <strong>in</strong>volved <strong>in</strong> the organization’sprocess for develop<strong>in</strong>g and implement<strong>in</strong>g evidence based careguidel<strong>in</strong>es;• hyperl<strong>in</strong>ks to the CCHMC website may be placed on theorganization’s website;• the EBCG may be adopted or adapted for use with<strong>in</strong> theorganization, provided that CCHMC receives appropriateattribution on all written or electronic documents; and• copies may be provided to patients and the cl<strong>in</strong>icians who managetheir care.Notification <strong>of</strong> CCHMC at HPCEInfo@cchmc.org for any EBCG,or its companion documents, adopted, adapted, implemented orhyperl<strong>in</strong>ked by the organization is appreciated.Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 13
Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39NOTE: These recommendations result from review <strong>of</strong> literatureand practices current at the time <strong>of</strong> their formulations. Thisguidel<strong>in</strong>e does not preclude us<strong>in</strong>g care modalities provenefficacious <strong>in</strong> studies published subsequent to the current revision<strong>of</strong> this document. This document is not <strong>in</strong>tended to imposestandards <strong>of</strong> care prevent<strong>in</strong>g selective variances from therecommendations to meet the specific and unique requirements<strong>of</strong> <strong>in</strong>dividual patients. Adherence to this guidel<strong>in</strong>e is voluntary.The cl<strong>in</strong>ician <strong>in</strong> light <strong>of</strong> the <strong>in</strong>dividual circumstances presented bythe patient must make the ultimate judgment regard<strong>in</strong>g thepriority <strong>of</strong> any specific procedure.For more <strong>in</strong>formation about this guidel<strong>in</strong>e, its support<strong>in</strong>g evidencesand the guidel<strong>in</strong>e development process, contact the Health Policy &Cl<strong>in</strong>ical Effectiveness <strong>of</strong>fice at: 513-636-2501 orHPCEInfo@cchmc.org ..Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 14
......Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 39ReferencesNote: When us<strong>in</strong>g the electronic version <strong>of</strong> this document, <strong>in</strong>dicates a hyperl<strong>in</strong>k to the PubMed abstract. A hyperl<strong>in</strong>k follow<strong>in</strong>gthis symbol goes to the article PDF when the user is with<strong>in</strong> theCCHMC network.1. APTA: Who Are Physical Therapists, and What Do They Do?In Guide To Physical Therapy Practice. Edited by Association,A. P. T., Alexandria, VA, APTA, 2001, [5] .2. Bailes, A. F.; Reder, R.; and Burch, C.: Development <strong>of</strong>guidel<strong>in</strong>es for determ<strong>in</strong><strong>in</strong>g frequency <strong>of</strong> therapy services <strong>in</strong> apediatric medical sett<strong>in</strong>g. Pediatr Phys Ther, 20(2): 194-8, 2008,[5a] .3. Bandy, W. D.; Irion, J. M.; Bandy, W. D.; and Irion, J. M.:The effect <strong>of</strong> time on static stretch on the flexibility <strong>of</strong> thehamstr<strong>in</strong>g muscles.[see comment]. Physical Therapy, 74(9):845-50; discussion 850-2, 1994, [2a] .4. Bandy, W. D.; Irion, J. M.; and Briggler, M.: The effect <strong>of</strong>static stretch and dynamic range <strong>of</strong> motion tra<strong>in</strong><strong>in</strong>g on theflexibility <strong>of</strong> the hamstr<strong>in</strong>g muscles. J Orthop Sports Phys Ther,27(4): 295-300, 1998, [2a] .5. Beyer, J. E.; Turner, S. B.; Jones, L.; Young, L.; Onikul, R.;and Bohaty, B.: The alternate forms reliability <strong>of</strong> the Oucherpa<strong>in</strong> scale. Pa<strong>in</strong> Manag Nurs, 6(1): 10-7, 2005, [4a] .6. Bolgla, L. A., and Uhl, T. L.: Electromyographic analysis <strong>of</strong>hip rehabilitation exercises <strong>in</strong> a group <strong>of</strong> healthy subjects. JOrthop Sports Phys Ther, 35(8): 487-94, 2005, [4b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16187509.7. Brech, G. C.; Guarnieiro, R.; Brech, G. C.; and Guarnieiro,R.: Evaluation <strong>of</strong> physiotherapy <strong>in</strong> the treatment <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> disease. Cl<strong>in</strong>ics (Sao Paulo, Brazil), 61(6): 521-8, 2006,[3b] .8. Campos, G. E. et al.: Muscular adaptations <strong>in</strong> response to threedifferent resistance-tra<strong>in</strong><strong>in</strong>g regimens: specificity <strong>of</strong> repetitionmaximum tra<strong>in</strong><strong>in</strong>g zones. Eur J Appl Physiol, 88(1-2): 50-60,2002, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=124362709. Canavese, F., and Dimeglio, A.: <strong>Perthes</strong>' disease: prognosis <strong>in</strong>children under six years <strong>of</strong> age. Journal <strong>of</strong> Bone & Jo<strong>in</strong>t Surgery- British Volume, 90(7): 940-5, 2008, [4b] .10. Cipriani, D.; Abel, B.; and Pirrwitz, D.: A comparison <strong>of</strong> twostretch<strong>in</strong>g protocols on hip range <strong>of</strong> motion: implications fortotal daily stretch duration. Journal Of Strength AndCondition<strong>in</strong>g Research / National Strength & Condition<strong>in</strong>gAssociation, 17(2): 274-278, 2003, [4b] http://search.ebscohost.com/log<strong>in</strong>.aspx?direct=true&db=cmedm&AN=12741862&log<strong>in</strong>page=Log<strong>in</strong>.asp&site=ehost-live&scope=site11. Clapper, M. P., and Wolf, S. L.: Comparison <strong>of</strong> the reliability<strong>of</strong> the Orthoranger and the standard goniometer for assess<strong>in</strong>gactive lower extremity range <strong>of</strong> motion. Phys Ther, 68(2): 214-8,1988, [4b] .12. Davis, D. S.; Ashby, P. E.; McCale, K. L.; McQua<strong>in</strong>, J. A.;and W<strong>in</strong>e, J. M.: The effectiveness <strong>of</strong> 3 stretch<strong>in</strong>g techniqueson hamstr<strong>in</strong>g flexibility us<strong>in</strong>g consistent stretch<strong>in</strong>g parameters. JStrength Cond Res, 19(1): 27-32, 2005, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=1570504113. Dep<strong>in</strong>o, G. M.; Webright, W. G.; and Arnold, B. L.: Duration<strong>of</strong> Ma<strong>in</strong>ta<strong>in</strong>ed Hamstr<strong>in</strong>g Flexibility After Cessation <strong>of</strong> an AcuteStatic Stretch<strong>in</strong>g Protocol. J Athl Tra<strong>in</strong>, 35(1): 56-59, 2000, [2b].14. Escolar, D. M.; Henricson, E. K.; Mayhew, J.; Florence, J.;Leshner, R.; Patel, K. M.; and Clemens, P. R.: Cl<strong>in</strong>icalevaluator reliability for quantitative and manual muscle test<strong>in</strong>gmeasures <strong>of</strong> strength <strong>in</strong> children. Muscle Nerve, 24(6): 787-93,2001, [4b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=1136026215. Faigenbaum, A. D.; Westcott, W. L.; Loud, R. L.; and Long,C.: The effects <strong>of</strong> different resistance tra<strong>in</strong><strong>in</strong>g protocols onmuscular strength and endurance development <strong>in</strong> children.Pediatrics, 104(1): e5, 1999, [2b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=1039029116. Faigenbaum, A. D.; Westcott, W. L.; Micheli, L. J.;Outerbridge, A. R.; Long, C. J.; LaRosa-Loud, R.; andZaichkowsky, L. D.: The Effects <strong>of</strong> Strength Tra<strong>in</strong><strong>in</strong>g andDetra<strong>in</strong><strong>in</strong>g on Children. Journal <strong>of</strong> Strength & Condition<strong>in</strong>gResearch, 10(2): 109-114, 1996, [4b] .17. Franjo<strong>in</strong>e, M. R.; Gunther, J. S.; and Taylor, M. J.: Pediatricbalance scale: a modified version <strong>of</strong> the berg balance scale forthe school-age child with mild to moderate motor impairment.Pediatr Phys Ther, 15(2): 114-28, 2003, [4b] .18. Friedrich, M.; Cermak, T.; and Maderbacher, P.: The effect<strong>of</strong> brochure use versus therapist teach<strong>in</strong>g on patients perform<strong>in</strong>gtherapeutic exercise and on changes <strong>in</strong> impairment status. PhysTher, 76(10): 1082-8, 1996, [2b] .19. Gajdosik, C. G.: Ability <strong>of</strong> very young children to producereliable isometric force measurements. Pediatr Phys Ther, 17(4):251-7, 2005, [4b] .20. Grzegorzewski, A. et al.: The role <strong>of</strong> the acetabulum <strong>in</strong> <strong>Perthes</strong>disease. Journal <strong>of</strong> Pediatric Orthopedics, 26(3): 316-21, 2006,[4b] .21. Herr<strong>in</strong>g, J. A.: <strong>Legg</strong>-<strong>Calve</strong>s-<strong>Perthes</strong> <strong>Disease</strong>. In Tachdjian'sPediatric Orthopaedics, pp. 675. Edited by Herr<strong>in</strong>g, J. A.,Elsevier Health Sciences, 2001, [5] .22. Herr<strong>in</strong>g, J. A.; Kim, H. T.; and Browne, R.: <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> disease. Part I: Classification <strong>of</strong> radiographs with use <strong>of</strong>the modified lateral pillar and Stulberg classifications. Journal <strong>of</strong>Bone & Jo<strong>in</strong>t Surgery - American Volume, 86-A(10): 2103-20,2004, [4b] .23. Herr<strong>in</strong>g, J. A.; Kim, H. T.; Browne, R.; Herr<strong>in</strong>g, J. A.; Kim,H. T.; and Browne, R.: <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> disease. Part II:Prospective multicenter study <strong>of</strong> the effect <strong>of</strong> treatment onoutcome.[see comment]. Journal <strong>of</strong> Bone & Jo<strong>in</strong>t Surgery -American Volume, 86-A(10): 2121-34, 2004, [3b] .24. Jacobs, C. A.; Lewis, M.; Bolgla, L. A.; Christensen, C. P.;Nitz, A. J.; and Uhl, T. L.: Electromyographic Analysis <strong>of</strong> HipAbductor Exercises Performed by a Sample <strong>of</strong> Total HipArthroplasty Patients. J Arthroplasty, 2008, [4b] .25. Leach, J.: Orthopedic Conditions. In Physical Therapy forChildren, pp. 498-499. Edited by Campbell, S.; Palisano, R.; andVander L<strong>in</strong>den, D., Saunders, 2006, [5] .26. Levangie, P., and Nork<strong>in</strong>, C.: The Hip Complex. In Jo<strong>in</strong>tstructure and function: a comprehensive analysis pp. 326.Edited by Levangie, P., and Nork<strong>in</strong>, C., Philadelpha FA DavisPhiladelpha, 1992, [5] .27. Local Consensus: dur<strong>in</strong>g the guidel<strong>in</strong>e development timeframe.ed., [5].28. Moseley, A. M.; Herbert, R. D.; Night<strong>in</strong>gale, E. J.; Taylor, D.A.; Evans, T. M.; Robertson, G. J.; Gupta, S. K.; and Penn,J.: Passive stretch<strong>in</strong>g does not enhance outcomes <strong>in</strong> patientswith plantarflexion contracture after cast immobilization forankle fracture: a randomized controlled trial. Arch Phys MedRehabil, 86(6): 1118-26, 2005, [2A] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=1595404929. Nadler, S. F.; We<strong>in</strong>gand, K.; and Kruse, R. J.: Thephysiologic basis and cl<strong>in</strong>ical applications <strong>of</strong> cryotherapy andthermotherapy for the pa<strong>in</strong> practitioner. Pa<strong>in</strong> Physician, 7(3):395-9, 2004, [1b] .30. Plasschaert, V. F. et al.: Hip abductor function <strong>in</strong> adults treatedfor <strong>Perthes</strong> disease. Journal <strong>of</strong> Pediatric Orthopaedics, Part B,15(3): 183-9, 2006, [4b] .Copyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 15
...Evidence-Based Care Guidel<strong>in</strong>e for <strong>Management</strong> <strong>of</strong> <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> <strong>Disease</strong> <strong>in</strong> children aged 3 to 12 years Guidel<strong>in</strong>e 3931. Rao, K. N., and Joseph, B.: Value <strong>of</strong> measurement <strong>of</strong> hipmovements <strong>in</strong> childhood hip disorders. Journal <strong>of</strong> PediatricOrthopedics, 21(4): 495-501, 2001, [4b] .32. Reid, D. A., and McNair, P. J.: Passive force, angle, andstiffness changes after stretch<strong>in</strong>g <strong>of</strong> hamstr<strong>in</strong>g muscles. Med SciSports Exerc, 36(11): 1944-8, 2004, [2b] .33. Rhea, M. R.; Alvar, B. A.; Ball, S. D.; and Burkett, L. N.:Three sets <strong>of</strong> weight tra<strong>in</strong><strong>in</strong>g superior to 1 set with equal<strong>in</strong>tensity for elicit<strong>in</strong>g strength. Journal <strong>of</strong> Strength &Condition<strong>in</strong>g Research, 16(4): 525-9, 2002, [2b] .34. Roberts, J. M., and Wilson, K.: Effect <strong>of</strong> stretch<strong>in</strong>g durationon active and passive range <strong>of</strong> motion <strong>in</strong> the lower extremity. BrJ Sports Med, 33(4): 259-63, 1999, [4b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=1045048135. Santonja Med<strong>in</strong>a, F. M.; Sa<strong>in</strong>z De Baranda Andujar, P.;Rodriguez Garcia, P. L.; Lopez M<strong>in</strong>arro, P. A.; andCanteras Jordana, M.: Effects <strong>of</strong> frequency <strong>of</strong> static stretch<strong>in</strong>gon straight-leg raise <strong>in</strong> elementary school children. Journal <strong>of</strong>Sports Medic<strong>in</strong>e & Physical Fitness, 47(3): 304-8, 2007, [2b].36. Sluijs, E. M.; Kok, G. J.; and van der Zee, J.: Correlates <strong>of</strong>exercise compliance <strong>in</strong> physical therapy. Phys Ther, 73(11):771-82; discussion 783-6, 1993, [4b] .37. Tamai, J.; Bulent, E.; and Dormans, J.: Hip Disorders. InPediatric Orthopaedics and Sports Medic<strong>in</strong>e: The Requisites <strong>in</strong>Pediatrics Series. Requisite Series, Mosby (An affiliate <strong>of</strong>Elsevier), pp. 191-195. Edited by Bell, L., St. Louis, Mosby,2004, [5] .38. Toro, B.; Nester, C. J.; and Farren, P. C.: A review <strong>of</strong>observational gait assessment <strong>in</strong> cl<strong>in</strong>ical practice. PhysiotherapyTheory and Practice, 19: 137-149, 2003, [1b] .39. Varni, J. W.; Limbers, C. A.; and Burw<strong>in</strong>kle, T. M.: Howyoung can children reliably and validly self-report their healthrelatedquality <strong>of</strong> life?: an analysis <strong>of</strong> 8,591 children across agesubgroups with the PedsQL 4.0 Generic Core Scales. HealthQual Life Outcomes, 5: 1, 2007a, [4a] .40. Varni, J. W.; Limbers, C. A.; and Burw<strong>in</strong>kle, T. M.: Parentproxy-report <strong>of</strong> their children's health-related quality <strong>of</strong> life: ananalysis <strong>of</strong> 13,878 parents' reliability and validity across agesubgroups us<strong>in</strong>g the PedsQL 4.0 Generic Core Scales. HealthQual Life Outcomes, 5: 2, 2007b, [4a] .41. Varni, J. W.; Seid, M.; and Kurt<strong>in</strong>, P. S.: PedsQL 4.0:reliability and validity <strong>of</strong> the Pediatric Quality <strong>of</strong> Life Inventoryversion 4.0 generic core scales <strong>in</strong> healthy and patientpopulations. Med Care, 39(8): 800-12, 2001, [4a] .42. von Baeyer, C. L.; Spagrud, L. J.; McCormick, J. C.; Choo,E.; Neville, K.; and Connelly, M. A.: Three new datasetssupport<strong>in</strong>g use <strong>of</strong> the Numerical Rat<strong>in</strong>g Scale (NRS-11) forchildren's self-reports <strong>of</strong> pa<strong>in</strong> <strong>in</strong>tensity. Pa<strong>in</strong>, 143(3): 223-7,2009, [4b] .43. We<strong>in</strong>ste<strong>in</strong>, S. L.: Natural history and treatment outcomes <strong>of</strong>childhood hip disorders. Cl<strong>in</strong> Orthop Relat Res, (344): 227-42,1997, [5a] .44. Wenger, D. R.; Ward, W. T.; and Herr<strong>in</strong>g, J. A.: <strong>Legg</strong>-<strong>Calve</strong>-<strong>Perthes</strong> disease. Journal <strong>of</strong> Bone & Jo<strong>in</strong>t Surgery -American Volume, 73(5): 778-88, 1991, [5a] .45. Westh<strong>of</strong>f, B.; Petermann, A.; Hirsch, M. A.; Willers, R.; andKrauspe, R.: Computerized gait analysis <strong>in</strong> <strong>Legg</strong> <strong>Calve</strong> <strong>Perthes</strong>disease--analysis <strong>of</strong> the frontal plane. Gait Posture, 24(2): 196-202, 2006, [4b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=1622603146. Williamson, A., and Hoggart, B.: Pa<strong>in</strong>: a review <strong>of</strong> threecommonly used pa<strong>in</strong> rat<strong>in</strong>g scales. J Cl<strong>in</strong> Nurs, 14(7): 798-804,2005, [1b] .47. Yoo, W. J.; Choi, I. H.; Cho, T. J.; Chung, C. Y.; Park, M.S.; and Lee, D. Y.: Out-toe<strong>in</strong>g and <strong>in</strong>-toe<strong>in</strong>g <strong>in</strong> patients with<strong>Perthes</strong> disease: role <strong>of</strong> the femoral hump. J Pediatr Orthop,28(7): 717-22, 2008, [4b] http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18812896Note: Full tables <strong>of</strong> evidence grad<strong>in</strong>g system available <strong>in</strong> separatedocument: Table <strong>of</strong> Evidence Levels <strong>of</strong> Individual Studies by Doma<strong>in</strong>,Study Design, & Quality (abbreviated table below) Grad<strong>in</strong>g a Body <strong>of</strong> Evidence to Answer a Cl<strong>in</strong>ical Question Judg<strong>in</strong>g the Strength <strong>of</strong> a Recommendation (abbreviated tablebelow)Table <strong>of</strong> Evidence Levels (see note above)Quality level Def<strong>in</strong>ition1a† or 1b†Systematic review, meta-analysis, or metasynthesis<strong>of</strong> multiple studies2a or 2b Best study design for doma<strong>in</strong>3a or 3b Fair study design for doma<strong>in</strong>4a or 4b Weak study design for doma<strong>in</strong>Other: General review, expert op<strong>in</strong>ion, case5report, consensus report, or guidel<strong>in</strong>e†a = good quality study; b = lesser quality studyTable <strong>of</strong> Recommendation Strength (see note above)StrengthDef<strong>in</strong>ition“Stronglyrecommended”“Recommended”No recommendationmadeThere is consensus that benefits clearlyoutweigh risks and burdens(or visa-versa for negativerecommendations).There is consensus that benefits are closelybalanced with risks and burdens.There is lack <strong>of</strong> consensus to directdevelopment <strong>of</strong> a recommendation.Dimensions: In determ<strong>in</strong><strong>in</strong>g the strength <strong>of</strong> a recommendation, thedevelopment group makes a considered judgment <strong>in</strong> a consensusprocess that <strong>in</strong>corporates critically appraised evidence, cl<strong>in</strong>icalexperience, and other dimensions as listed below.1. Grade <strong>of</strong> the Body <strong>of</strong> Evidence (see note above)2. Safety / Harm3. Health benefit to patient (direct benefit)4. Burden to patient <strong>of</strong> adherence to recommendation (cost, hassle,discomfort, pa<strong>in</strong>, motivation, ability to adhere, time)5. Cost-effectiveness to healthcare system (balance <strong>of</strong> cost /sav<strong>in</strong>gs <strong>of</strong> resources, staff time, and supplies based on publishedstudies or onsite analysis)6. Directness (the extent to which the body <strong>of</strong> evidence directlyanswers the cl<strong>in</strong>ical question [population/problem, <strong>in</strong>tervention,comparison, outcome])7. Impact on morbidity/mortality or quality <strong>of</strong> lifeCopyright © 2010 C<strong>in</strong>c<strong>in</strong>nati Children's Hospital Medical Center; all rights reserved. Page 16