Checklist for Letter of Medical Necessity - ControlYourPain.com
Checklist for Letter of Medical Necessity - ControlYourPain.com Checklist for Letter of Medical Necessity - ControlYourPain.com
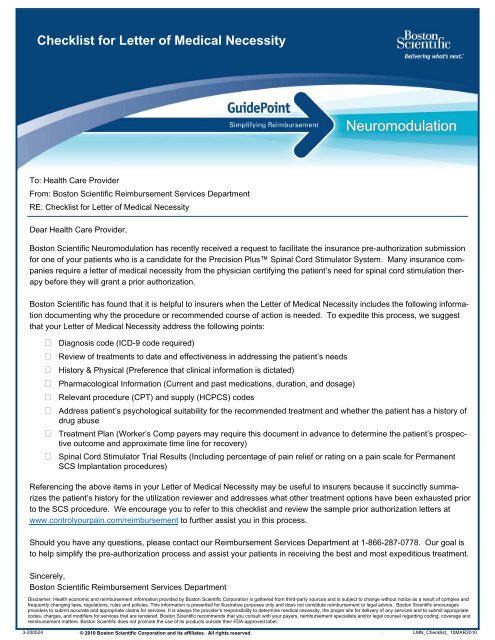
Checklist for Letter of Medical NecessityNeuromodulationTo: Health Care ProviderFrom: Boston Scientific Reimbursement Services DepartmentRE: Checklist for Letter of Medical NecessityDear Health Care Provider,Boston Scientific Neuromodulation has recently received a request to facilitate the insurance pre-authorization submissionfor one of your patients who is a candidate for the Precision Plus Spinal Cord Stimulator System. Many insurance companiesrequire a letter of medical necessity from the physician certifying the patient’s need for spinal cord stimulation therapybefore they will grant a prior authorization.Boston Scientific has found that it is helpful to insurers when the Letter of Medical Necessity includes the following informationdocumenting why the procedure or recommended course of action is needed. To expedite this process, we suggestthat your Letter of Medical Necessity address the following points: Diagnosis code (ICD-9 code required) Review of treatments to date and effectiveness in addressing the patient’s needs History & Physical (Preference that clinical information is dictated) Pharmacological Information (Current and past medications, duration, and dosage) Relevant procedure (CPT) and supply (HCPCS) codes Address patient’s psychological suitability for the recommended treatment and whether the patient has a history ofdrug abuse Treatment Plan (Worker’s Comp payers may require this document in advance to determine the patient’s prospectiveoutcome and approximate time line for recovery) Spinal Cord Stimulator Trial Results (Including percentage of pain relief or rating on a pain scale for PermanentSCS Implantation procedures)Referencing the above items in your Letter of Medical Necessity may be useful to insurers because it succinctly summarizesthe patient’s history for the utilization reviewer and addresses what other treatment options have been exhausted priorto the SCS procedure. We encourage you to refer to this checklist and review the sample prior authorization letters atwww.controlyourpain.com/reimbursement to further assist you in this process.Should you have any questions, please contact our Reimbursement Services Department at 1-866-287-0778. Our goal isto help simplify the pre-authorization process and assist your patients in receiving the best and most expeditious treatment.Sincerely,Boston Scientific Reimbursement Services DepartmentDisclaimer: Health economic and reimbursement information provided by Boston Scientific Corporation is gathered from third-party sources and is subject to change without notice as a result of complex andfrequently changing laws, regulations, rules and policies. This information is presented for illustrative purposes only and does not constitute reimbursement or legal advice. Boston Scientific encouragesproviders to submit accurate and appropriate claims for services. It is always the provider’s responsibility to determine medical necessity, the proper site for delivery of any services and to submit appropriatecodes, charges, and modifiers for services that are rendered. Boston Scientific recommends that you consult with your payers, reimbursement specialists and/or legal counsel regarding coding, coverage andreimbursement matters. Boston Scientific does not promote the use of its products outside their FDA-approved label.3-200524 © 2010 Boston Scientific Corporation and its affiliates. All rights reserved. . LMN_Checklist_ 10MAR2010
- Page 2 and 3: Pre-Authorization Reference GuideNe
- Page 4 and 5: Consent to Facilitate Pre-authoriza
- Page 6 and 7: Insurance Authorization FormComplet
- Page 8 and 9: **CONFIDENTIAL**Patient's Full Name
- Page 10 and 11: 2010 Physician Coding Scenarios for
- Page 12 and 13: 2010 Ambulatory Surgery Center Codi
- Page 14: 2010 Outpatient Coding Scenarios fo
<strong>Checklist</strong> <strong>for</strong> <strong>Letter</strong> <strong>of</strong> <strong>Medical</strong> <strong>Necessity</strong>NeuromodulationTo: Health Care ProviderFrom: Boston Scientific Reimbursement Services DepartmentRE: <strong>Checklist</strong> <strong>for</strong> <strong>Letter</strong> <strong>of</strong> <strong>Medical</strong> <strong>Necessity</strong>Dear Health Care Provider,Boston Scientific Neuromodulation has recently received a request to facilitate the insurance pre-authorization submission<strong>for</strong> one <strong>of</strong> your patients who is a candidate <strong>for</strong> the Precision Plus Spinal Cord Stimulator System. Many insurance <strong>com</strong>paniesrequire a letter <strong>of</strong> medical necessity from the physician certifying the patient’s need <strong>for</strong> spinal cord stimulation therapybe<strong>for</strong>e they will grant a prior authorization.Boston Scientific has found that it is helpful to insurers when the <strong>Letter</strong> <strong>of</strong> <strong>Medical</strong> <strong>Necessity</strong> includes the following in<strong>for</strong>mationdocumenting why the procedure or re<strong>com</strong>mended course <strong>of</strong> action is needed. To expedite this process, we suggestthat your <strong>Letter</strong> <strong>of</strong> <strong>Medical</strong> <strong>Necessity</strong> address the following points: Diagnosis code (ICD-9 code required) Review <strong>of</strong> treatments to date and effectiveness in addressing the patient’s needs History & Physical (Preference that clinical in<strong>for</strong>mation is dictated) Pharmacological In<strong>for</strong>mation (Current and past medications, duration, and dosage) Relevant procedure (CPT) and supply (HCPCS) codes Address patient’s psychological suitability <strong>for</strong> the re<strong>com</strong>mended treatment and whether the patient has a history <strong>of</strong>drug abuse Treatment Plan (Worker’s Comp payers may require this document in advance to determine the patient’s prospectiveout<strong>com</strong>e and approximate time line <strong>for</strong> recovery) Spinal Cord Stimulator Trial Results (Including percentage <strong>of</strong> pain relief or rating on a pain scale <strong>for</strong> PermanentSCS Implantation procedures)Referencing the above items in your <strong>Letter</strong> <strong>of</strong> <strong>Medical</strong> <strong>Necessity</strong> may be useful to insurers because it succinctly summarizesthe patient’s history <strong>for</strong> the utilization reviewer and addresses what other treatment options have been exhausted priorto the SCS procedure. We encourage you to refer to this checklist and review the sample prior authorization letters atwww.controlyourpain.<strong>com</strong>/reimbursement to further assist you in this process.Should you have any questions, please contact our Reimbursement Services Department at 1-866-287-0778. Our goal isto help simplify the pre-authorization process and assist your patients in receiving the best and most expeditious treatment.Sincerely,Boston Scientific Reimbursement Services DepartmentDisclaimer: Health economic and reimbursement in<strong>for</strong>mation provided by Boston Scientific Corporation is gathered from third-party sources and is subject to change without notice as a result <strong>of</strong> <strong>com</strong>plex andfrequently changing laws, regulations, rules and policies. This in<strong>for</strong>mation is presented <strong>for</strong> illustrative purposes only and does not constitute reimbursement or legal advice. Boston Scientific encouragesproviders to submit accurate and appropriate claims <strong>for</strong> services. It is always the provider’s responsibility to determine medical necessity, the proper site <strong>for</strong> delivery <strong>of</strong> any services and to submit appropriatecodes, charges, and modifiers <strong>for</strong> services that are rendered. Boston Scientific re<strong>com</strong>mends that you consult with your payers, reimbursement specialists and/or legal counsel regarding coding, coverage andreimbursement matters. Boston Scientific does not promote the use <strong>of</strong> its products outside their FDA-approved label.3-200524 © 2010 Boston Scientific Corporation and its affiliates. All rights reserved. . LMN_<strong>Checklist</strong>_ 10MAR2010
Pre-Authorization Reference GuideNeuromodulationImportant Resources:• Reimbursement Services Hours <strong>of</strong> Operation: 5:00 a.m. to 5:00 p.m., Pacific Time• Reimbursement Services Toll Free Number: 1-866-287-0778• Reimbursement Services Toll Free Fax Number: 1-877-835-2520 (Pre-authorization requests must be submitted tothis number)• Website: www.<strong>ControlYourPain</strong>.<strong>com</strong>/ReimbursementServices Provided:At the request <strong>of</strong> the Health Care Pr<strong>of</strong>essional (HCP), Boston Scientific facilitates the preparation and submission <strong>of</strong> requests<strong>for</strong> coverage determinations, prior authorization and pre-certifications including the following:• Provides in<strong>for</strong>mation on payor policies and procedures <strong>for</strong> obtaining prior authorization• Provides sample letters and in<strong>for</strong>mation on medical necessity and appeals <strong>of</strong> denied claims• Provides coordination and follow up services with payers relating to the pre-authorization process• Provides education on the pre-authorization processPre-Authorization Overview:This process involves obtaining advance notification from the health plan that medical necessity and other coverage criteriahave been met, as set <strong>for</strong>th by the health plan. Boston Scientific assists patients with the pre-authorization process uponreceipt <strong>of</strong> the below in<strong>for</strong>mation. (Note: all <strong>for</strong>ms referenced below can be found at www.<strong>ControlYourPain</strong>.<strong>com</strong>/Reimbursement)• Consent Form: Form must be <strong>com</strong>pleted by providers who request that Boston Scientific assist with the pre-authorizationprocess. By signing the <strong>for</strong>m, the provider gives Boston Scientific consent to facilitate the pre-authorization process on his orher behalf• Provider Intake Form: Provides relevant demographic in<strong>for</strong>mation <strong>for</strong> the physician, ambulatory surgery center (ASC), orhospital• Insurance Authorization Form: Provides general patient insurance in<strong>for</strong>mation (Note: providers may use this <strong>for</strong>m or theirown)• Clinical Documentation: Provides the insurer with a clinical history <strong>of</strong> treatment received prior to Precision Spinal CordStimulator (SCS) System re<strong>com</strong>mendation. Psychiatric evaluation, letter <strong>of</strong> medical necessity, and other applicable documentationmay need to be included <strong>for</strong> consideration• Other: Additional in<strong>for</strong>mation may be requested based on specific payer coverage criteria. For example, workers’ <strong>com</strong>pensationmay require a claim number and date <strong>of</strong> injury, and HMO cases may require a referral by the Primary Care PhysicianDisclaimer: Health economic and reimbursement in<strong>for</strong>mation provided by Boston Scientific Corporation is gathered from third-party sources and is subject to change without notice as a result <strong>of</strong> <strong>com</strong>plex andfrequently changing laws, regulations, rules and policies. This in<strong>for</strong>mation is presented <strong>for</strong> illustrative purposes only and does not constitute reimbursement or legal advice. Boston Scientific encouragesproviders to submit accurate and appropriate claims <strong>for</strong> services. It is always the provider’s responsibility to determine medical necessity, the proper site <strong>for</strong> delivery <strong>of</strong> any services and to submit appropriatecodes, charges, and modifiers <strong>for</strong> services that are rendered. Boston Scientific re<strong>com</strong>mends that you consult with your payers, reimbursement specialists and/or legal counsel regarding coding, coverage andreimbursement matters. Boston Scientific does not promote the use <strong>of</strong> its products outside their FDA-approved label.In<strong>for</strong>mation included herein is current as <strong>of</strong> January 14, 2010, but is subject to change without notice.3-200168 © 2010 Boston Scientific Corporation and its affiliates. All rights reserved. Page 1 <strong>of</strong> 2Pre-Auth_Reference Guide_10MAR2010
Frequently Asked QuestionsSCS Pre-AuthorizationNeuromodulationQ. How does Pre-authorization differ from Predetermination?A. Pre-authorization <strong>of</strong> benefits is the process that allows physicians and other healthcare providers to determine if thepatient is eligible <strong>for</strong> coverage <strong>for</strong> a proposed treatment or service. It is also the process <strong>of</strong> securing authorization from apayer <strong>for</strong> a specialist and/or referral <strong>for</strong> non-emergency healthcare service. Pre-authorization <strong>of</strong> benefits does notguarantee reimbursement.Predetermination <strong>of</strong> benefits is similar to pre-authorization in that it allows services and treatment to be reviewed <strong>for</strong>medical necessity. Benefit coverage is predetermined be<strong>for</strong>e services are rendered and any limitation under a plan canbe addressed be<strong>for</strong>e services are rendered. A predetermination is a courtesy, where a preauthorization is arequirement under a plan. Most predetermination requests can take 30 to 45 days, and a <strong>com</strong>plete history andphysical should be included.Q. Which payers require a pre-authorization <strong>for</strong> SCS procedures and therapies?A. A summary <strong>of</strong> typical pre-authorization requirements <strong>for</strong> different types <strong>of</strong> payers follows:♦ Medicare does not pre-authorize or guarantee benefits. However, the patient must meet the Medicare criteria<strong>for</strong> SCS coverage.♦ Medicaid requires pre-authorization <strong>for</strong> SCS procedures in many states. The pre-authorization process variesfrom state-to-state, so check with your local Medicaid <strong>of</strong>fice to determine the pre-authorization process <strong>for</strong> yourstate.♦ Commercial Payers typically re<strong>com</strong>mend predetermination <strong>for</strong> SCS procedures. Check with each payer toverify benefits, coverage policies, plan limitations, and/or exclusions.♦ Workers Compensation requires pre-authorization <strong>for</strong> SCS treatment plans.♦ Managed Care Payers:1. Health Maintenance Organizations (HMOs). HMO members <strong>of</strong>ten must receive their medical treatment fromphysicians and facilities within the HMO network. HMOs may require a referral authorization from the primarycare physician to the specialist. In addition to a referral authorization, the plan may require a separateauthorization <strong>for</strong> the services to be rendered.2. Preferred provider organizations (PPOs). These plans may not have pre-approval requirements <strong>for</strong>outpatient surgery. Members may also receive treatment from physicians and facilities outside the network, butdifferent benefits apply. The plan may allow benefits to be pre-determined prior to a procedure or service. Thecenter should schedule surgeries to allow <strong>for</strong> appropriate approval processing times. Predeterminations cantake 30 to 45 days <strong>for</strong> an out<strong>com</strong>e.Q. How long does the pre-authorization process take?A. This is dependant on the health plan and its pre-authorization requirements. Usually, the process can take anywherefrom five to 30 business days depending on how timely the health plan facilitates these requests.Disclaimer: Health economic and reimbursement in<strong>for</strong>mation provided by Boston Scientific Corporation is gathered from third-party sources and is subject to change without notice as a result <strong>of</strong> <strong>com</strong>plex andfrequently changing laws, regulations, rules and policies. This in<strong>for</strong>mation is presented <strong>for</strong> illustrative purposes only and does not constitute reimbursement or legal advice. Boston Scientific encouragesproviders to submit accurate and appropriate claims <strong>for</strong> services. It is always the provider’s responsibility to determine medical necessity, the proper site <strong>for</strong> delivery <strong>of</strong> any services and to submit appropriatecodes, charges, and modifiers <strong>for</strong> services that are rendered. Boston Scientific re<strong>com</strong>mends that you consult with your payers, reimbursement specialists and/or legal counsel regarding coding, coverage andreimbursement matters. Boston Scientific does not promote the use <strong>of</strong> its products outside their FDA-approved label.In<strong>for</strong>mation included herein is current as <strong>of</strong> January 14, 2010, but is subject to change without notice.3-200168 © 2010 Boston Scientific Corporation and its affiliates. All rights reserved. Page 2 <strong>of</strong> 2Pre-Auth_Reference Guide_10MAR2010
Consent to Facilitate Pre-authorization Form toBoston Scientific Reimbursement Services Department25155 Rye Canyon LoopValencia, CA 91355Fax <strong>com</strong>pleted Form to 1-877-835-2520Consent to facilitate pre-authorization <strong>for</strong> the purpose <strong>of</strong> insurance pre-authorization to be conducted byBoston Scientific Neuromodulation <strong>for</strong> the Precision Plus Spinal Cord Stimulator SystemI, _________________________________________________ (printed physician’s name), authorize Boston ScientificNeuromodulation to facilitate insurance pre-authorization assistance on my behalf <strong>for</strong> the Spinal Cord Stimulation(SCS)Trial and/or Permanent procedure <strong>for</strong> my patient(s). I give Boston Scientific the authorization to act on my behalf <strong>for</strong> thepurposes <strong>of</strong> obtaining, submitting, and receiving all in<strong>for</strong>mation <strong>for</strong> my patient (s) as it relates to the benefits inquiry andthe pre-authorization process <strong>for</strong> the SCS procedure.Boston Scientific assists with the pre-authorization process by relaying in<strong>for</strong>mation provided from the healthcare providerto the patient’s health plan and does not make any representation or guarantee <strong>of</strong> coding, coverage, and paymentas the final coverage decision <strong>for</strong> the SCS procedure is determined by the health plan based on actual claims <strong>for</strong> servicesrendered and in accordance with applicable contracts. Boston Scientific handles patient in<strong>for</strong>mation, and is permittedto use and disclose patient in<strong>for</strong>mation, as set <strong>for</strong>th in its Business Associate Agreement sent to you.I understand that this <strong>for</strong>m must be signed by me be<strong>for</strong>e Boston Scientific can proceed with the pre-authorization assistance<strong>for</strong> my patient (s). I also understand that this authorization will remain active, unless revoked by me.__________________________________________________Physician’s Signature_______/_______/_______DatePhysician’s NPI#:_________________________________Physician’s TIN#:_________________________________Practice Street Address 1:________________________________________________________________Practice Street Address 2:________________________________________________________________City:_______________________________ State:_______ Zip Code:_________________FAX <strong>com</strong>pleted <strong>for</strong>m to the Boston Scientific Reimbursement Services Department at1-877-835-2520.Please retain a copy <strong>for</strong> your records.All questions regarding this <strong>for</strong>m should be directed to the Boston Scientific Reimbursement Services Department at1-866-287-0778.Disclaimer: Reimbursement in<strong>for</strong>mation provided by Boston Scientific Corporation is gathered from third-party sources and is presented <strong>for</strong> illustrative purposes only. This in<strong>for</strong>mation doesnot constitute reimbursement or legal advice. Boston Scientific Corporation makes no representation or warranty regarding this in<strong>for</strong>mation or its <strong>com</strong>pleteness, accuracy, timeliness, or applicabilitywith a particular patient. Boston Scientific Corporation specifically disclaims liability or responsibility <strong>for</strong> the results or consequences <strong>of</strong> any actions taken in reliance on in<strong>for</strong>mation inthis document. Laws, regulations and payer policies concerning reimbursement are <strong>com</strong>plex and change frequently. Providers are responsible <strong>for</strong> making appropriate decisions relating tocoding and reimbursement submissions and <strong>for</strong> submitting accurate and appropriate claims <strong>for</strong> services. Accordingly, providers should consult with payers, reimbursement specialistand/or their legal counsel regarding coding, coverage and reimbursement matters.In<strong>for</strong>mation included herein is current as <strong>of</strong> March 10, 2010, but is subject to change without notice.3-200511Page 1 <strong>of</strong> 1Boston Scientific Consent to facilitate pre-authorization Form
Provider Intake FormComplete and Fax <strong>for</strong>m to 1-877-835-2520 orEmail to: BSN.IntakeUnit@bsci.<strong>com</strong>NeuromodulationPhysician In<strong>for</strong>mationAdditional Facility In<strong>for</strong>mation (if applicable) Additional Facility In<strong>for</strong>mation (if applicable) Additional Facility In<strong>for</strong>mationPhysician: (if applicable) Additional Facility In<strong>for</strong>mation Practice (if Name: applicable) Additional Facility In<strong>for</strong>mation (if applicable)Address: Additional Facility In<strong>for</strong>mation (if applicable) Additional Facility In<strong>for</strong>mation (if applicable) Additional FacilityIn<strong>for</strong>mation (if applicable) Additional Facility In<strong>for</strong>mation (if applicable) Additional Facility In<strong>for</strong>mation (if applicable)City: Additional Facility In<strong>for</strong>mation State: (if applicable) Zip: Additional Phone: Facility In<strong>for</strong>mation (if applicable) Fax: Additional FacilityIn<strong>for</strong>mation Contact(s): (if applicable) Additional Facility In<strong>for</strong>mation (if applicable) Additional Facility In<strong>for</strong>mation (if applicable)Email:TIN: Billing NPI: Doctor NPI: BCBS:Medicaid: UPIN: ACS: Other:Trial in Office: Yes No Please Provide Facility In<strong>for</strong>mation BelowFacility In<strong>for</strong>mationTrial Perm In-Patient Hospital Outpatient Hospital Ambulatory Surgical CenterFacility:Address:City: State: Zip: Phone: Fax:Contact(s):Email:TIN: Billing NPI: BCBS: Other:Additional Facility In<strong>for</strong>mation (if applicable)Trial Perm In-Patient Hospital Outpatient Hospital Ambulatory Surgical CenterFacility:Address:City: State: Zip: Phone: Fax:Contact(s):Email:TIN: Billing NPI: BCBS: Other:CommentsFor Boston Scientific Internal Use Only—SCS Sales Representative In<strong>for</strong>mation:Name: Phone: Territory: RBM Name:Disclaimer: Boston Scientific Neuromodulation will work to obtain authorization on behalf <strong>of</strong> the physician and the facility, upon request.The above in<strong>for</strong>mation must be <strong>com</strong>pleted in its entirety to facilitate appropriate processing. In<strong>for</strong>mation missing from this Form maycause delays in the pre-authorization process. Boston Scientific does not guarantee authorization or payment <strong>for</strong> services. The patientor patient’s guardian remains liable <strong>for</strong> payment <strong>of</strong> services or goods received except as otherwise provided by law.3-200526BSC Provider Intake Form10MAR010
Insurance Authorization FormComplete and Fax <strong>for</strong>m to 1-877-835-2520 orEmail to: BSN.IntakeUnit@bsci.<strong>com</strong>ConfidentialIf Form received in error, please contact Boston Scientific at 1-866-287-0778NeuromodulationI - Implant Center In<strong>for</strong>mationPractice Name:Site <strong>of</strong> Service:Implant Surgeon: Contact Number: Surgery Date:II - Patient In<strong>for</strong>mationPatient Name:Address:Parent Name:City: State: Zip Code:Home Phone #: DOB: Sex:III - Employer In<strong>for</strong>mation (Required <strong>for</strong> Workers Compensation)Employer Name: Employer Address 1:Employer Address 1: Work Phone:( )IV - Workers’ CompensationInsurance Company: Adjuster: Phone:Claim #:Date <strong>of</strong> Injury:V - Primary Health Plan In<strong>for</strong>mation (Please attach front and back copy <strong>of</strong> health insurance card)Check Health Plan Type: HMO PPO EPO POS Medicare Worker Comp. Medicaid OtherPrimary Health plan Name:Address: City: State: Zip:Plan Phone #: Member Name: DOB: ID#:ID#: Group Plan #: Relationship to Patient:VI - Secondary Health Plan In<strong>for</strong>mation (Please attach front and back copy <strong>of</strong> health insurance card)Secondary Health plan Name: Phone #:Address: City: State: Zip:Secondary Member's Name: ID #: Group #:VII - Primary Care Physician In<strong>for</strong>mation (Required <strong>for</strong> HMO members)Primary Care Physician Name:Phone:Address: City: State: Zip:VIII - AuthorizationI authorize Boston Scientific (BSC) Neuromodulation’s Reimbursement Services Department to release pertinent in<strong>for</strong>mation about my medical condition <strong>for</strong> the purpose <strong>of</strong>securing health insurance benefits in<strong>for</strong>mation as it relates to the insurance pre-authorization process <strong>for</strong> the Trial and/or Permanent Spinal Cord Stimulation procedure. I alsoauthorize BSC Neuromodulation’s Reimbursement Services Department to act as my representative and on my behalf to secure all authorization necessary from my healthplan regarding my spinal cord stimulator procedure. I understand that I may revoke this authorization at any time by giving my physician or BSC Neuromodulation a statementto withhold my personal and medical in<strong>for</strong>mation from that time <strong>for</strong>ward.Patient’s Name:_____________________________________________Patient or Legal Guardian’s Signature: __________________________Relationship to patient: _____________________________________________________________________ Date: ____________________________Disclaimer: Boston Scientific Neuromodulation will endeavor to obtain authorization from your insurance <strong>com</strong>pany to reimburse your healthcare provider <strong>for</strong> services or itemscovered by an authorization. However there is no guarantee that your healthcare provider will receive authorization or payment from your insurance <strong>com</strong>pany. You remain liable<strong>for</strong> payment <strong>of</strong> services or items received except as otherwise provided by law.3-200525 BSC Insurance Authorization Form_10MAR010
Statement <strong>of</strong> <strong>Medical</strong> <strong>Necessity</strong> Instructional <strong>Letter</strong>NeuromodulationDear Valued Boston Scientific Customer,Fax <strong>com</strong>pleted <strong>for</strong>m to 1-877-835-2520We are pleased to <strong>of</strong>fer you an additional tool, our Statement <strong>of</strong> <strong>Medical</strong> <strong>Necessity</strong> Form (“Form”), to assist in the preauthorizationprocess <strong>for</strong> the Precision Plus Spinal Cord Stimulator System <strong>for</strong> your patients.The Form provides you with an easy, check box <strong>for</strong>mat. You may choose to use this Form in place <strong>of</strong>, or in addition to, aletter <strong>of</strong> medical necessity. It is important to note that medical necessity requirements may vary by insurance carrier.Properly <strong>com</strong>pleting the <strong>for</strong>m does not necessarily guarantee reimbursement by the pertinent payer. Boston Scientific ismaking no representation or warranty regarding coverage, and although we are assisting with the prior authorizationprocess, the ultimate responsibility <strong>for</strong> obtaining reimbursement rests with the provider or physician.Instructions <strong>for</strong> <strong>com</strong>pleting the <strong>Medical</strong> <strong>Necessity</strong> Form1. Enter the patient’s full name, the physician name, name <strong>of</strong> surgery site, physician state, NPI and TIN# in thecorresponding sections2. Check the applicable Site <strong>of</strong> Surgery3. Check the applicable SCS Procedure Type4. Check the diagnosis code, as determined by the physician5. Under the Physician’s Order Section, select the procedure (s) and enter the corresponding number <strong>of</strong> units6. Read the Physician Certification Section. The physician must sign and date the Form7. Fax <strong>com</strong>pleted <strong>for</strong>m, and all other requested clinical in<strong>for</strong>mation, to the Boston Scientific ReimbursementServices Department at 1-877-835-2520Should you have any questions, please call our Reimbursement Services Department at 1-866-287-0778. We areavailable to assist you Monday through Friday from 5:00am to 5:00pm, Pacific Time.We hope that our Statement <strong>of</strong> <strong>Medical</strong> <strong>Necessity</strong> Form will be useful to you and we look <strong>for</strong>ward to continuing to serveyou and your patients.Sincerely,Tonya WaltersReimbursement Services ManagerBoston Scientific NeuromodulationDisclaimer: Health economic and reimbursement in<strong>for</strong>mation provided by Boston Scientific Corporation is gathered from third-party sources and is subject to change without notice as a result <strong>of</strong> <strong>com</strong>plex and frequently changing laws, regulations, rulesand policies. This in<strong>for</strong>mation is presented <strong>for</strong> illustrative purposes only and does not constitute reimbursement or legal advice. Boston Scientific encourages providers to submit accurate and appropriate claims <strong>for</strong> services. It is always the provider’sresponsibility to determine medical necessity, the proper site <strong>for</strong> delivery <strong>of</strong> any services and to submit appropriate codes, charges, and modifiers <strong>for</strong> services that are rendered. Boston Scientific re<strong>com</strong>mends that you consult with your payers, reimbursementspecialists and/or legal counsel regarding coding, coverage and reimbursement matters. Boston Scientific does not promote the use <strong>of</strong> its products outside their FDA-approved label.3-200608© 2010 Boston Scientific Corporation and its affiliates. All rights reserved. . BSC_CMN INSTRUCTIONS Version 2_24JUN2010
**CONFIDENTIAL**Patient's Full Name:Physician Name:Fax <strong>com</strong>pleted <strong>for</strong>m and supporting clinical documentation to 1-877-835-2520Statement <strong>of</strong> <strong>Medical</strong> <strong>Necessity</strong>Patient's DOB:Name <strong>of</strong> Surgery Site:**CONFIDENTIAL**State: NPI #: TIN #:Site <strong>of</strong> Surgery: Physician Office ASC Outpatient Hospital Inpatient HospitalSCS Procedure Type: SCS Trial SCS Permanent Implant SCS Trial & Permanent ImplantDiagnosis Codes: Check the primary code that appliesThis <strong>for</strong>m contains a list <strong>of</strong> diagnosis, CPT and ICD-9-CM, codes <strong>com</strong>monly applicable to patients <strong>for</strong> whom spinal cord stimulation is prescribed.However, it is NOT a <strong>com</strong>plete list <strong>of</strong> potentially applicable codes. If another code is applicable to your patient, please check the "Other" box or<strong>com</strong>plete the "Notes" section and fill in the appropriate code.337.2 Reflex sympathetic dystrophy 337.29 Reflex sympathetic dyst., spec. 338.2 Chronic pain337.22 Reflex sympath. dyst., lower limb 338.22 Chronic post-thoracotomy pain 338.28 Other chronic postoperative338.21 Chronic pain due to trauma 353.6 Phantom limb pain (syndrome) 354.4 Causalgia <strong>of</strong> upper limb338.4 Chronic pain syndrome 354.9 Mononeuritis, upper limb, unspec. 355.71 Causalgia <strong>of</strong> lower limb354.5 Mononeuritis multiplex 722.82 Postlaminectomy synd., thoracic 722.83 Postlaminectomy syndrome, lumbar355.8 Mononeuritis <strong>of</strong> lower limb, unspec. 724.02 Spinal stenosis, lumbar region 724.2 Lumbago723.4 Brachial neuritis or radiculitis NOS 724.4 Thoracic, lumbosac., neur., radicu. 729.2 Neuralgia, neuritis, and radicu.,724.3 Sciatica 953.1 Dorsal nerve root injury Other-Indicate ICD-9 Code:729.5 Pain in limb 953.2 Lumbar nerve root injury337.20 Reflex sympathetic dyst., unspec. 337.21 Reflex sympath.dyst., upper limbPhysician's Order: Check box (es) <strong>for</strong> services & supplies rendered________________________________SCS Trial Procedure CodesCPT Code Description Units63650 Implant neuroelectrodes95972 Analyze neurostim., 1st hour95973 Analyze neurostim., add. 30 minC1778L8680Lead, neurostimulatorImplt. Neurostim. electr.For Inpatient Hospital Use OnlyCPT Code Description Units03.93 Imp/rep/spine stim lead86.98 Ins/rep 2 pul gen, rechrgNotes Section:SCS Permanent Implant Procedure CodesCPT Code Description Units63650 Implant neuroelectrodes63655 Implant neuroelectrodes63685 Insrt/redo spine n generator95972 Analyze neurostim., 1st hour95973 Analyze neurostim, add. 30 min.C1778 Lead, neurostimulatorC1787 Patient progr, neurostim.C1820 Generator neuro rechg bat syC1883 Adapt/ext, pacing / neuro lead (Splitter)L8680 Implt neurostim electr.L8687 Implt nrostm pls gen dua recL8699 Prosthetic implant NOS / (Splitter)PHYSICIAN CERTIFICATION SECTION:By signing below, I certify that (1) I am the physician identified in the first section <strong>of</strong> this document, (2) I have <strong>com</strong>pleted this document in itsentirety (or reviewed it carefully after it was <strong>com</strong>pleted by an employee under my direction), (3) all the in<strong>for</strong>mation provided by me or mystaff, including the patient diagnosis, CPT codes selected, and medical documentation supporting SCS: a) confirms this patient's suitability <strong>for</strong>SCS based on Medicare's National Conditions <strong>of</strong> Coverage <strong>for</strong> SCS and b) is true, accurate, and <strong>com</strong>plete to the best <strong>of</strong> my knowledge.Physician Signature:3-200607Clinical documentation attached (i.e., treatment history and psychological evaluation )Date:_____/_____/_____Patient's insurance in<strong>for</strong>mation attachedBSC_CMN_Version 2.0 24JUN2010
2010 Physician Coding and PaymentQuick Reference <strong>for</strong> Spinal Cord StimulationNeuromodulationImportant: While we have provided a summary <strong>of</strong> the "final" physician reimbursement rates, please be aware that Congressionallegislation will be required to override an additional Sustainable Growth Rate (SGR) reduction <strong>of</strong> 21.2%. We have not included thisadditional reduction in the rates we present here and have instead used the temporary 2010 conversion factor. 1Reimbursement Coding and Medicare Payment Guide: This in<strong>for</strong>mation pertains to the Centers <strong>for</strong> Medicare and MedicaidServices’ (CMS) 2010 coding and national payment rates <strong>for</strong> the pr<strong>of</strong>essional <strong>com</strong>ponent <strong>of</strong> spinal cord stimulator (SCS) procedures and the<strong>com</strong>mon coding scenario <strong>for</strong> those procedures per<strong>for</strong>med in the <strong>of</strong>fice setting.CPT 2 / HCPCS 3CodeDescriptionGlobal SurgeryPeriodMedicare NationalAverage Payment 4,563650 Percutaneous implantation <strong>of</strong> neurostimulator electrode array; epidural (each) 10 $ 39463655Laminectomy <strong>for</strong> implantation <strong>of</strong> neurostimulator electrodes, plate/ paddle(s),epidural6,7 Removal <strong>of</strong> spinal neurostimulator electrode percutaneous array(s), including63661fluoroscopy, when per<strong>for</strong>med6 Removal <strong>of</strong> spinal neurostimulator electrode plate/paddle(s) placed via63662laminotomy or laminectomy, including fluoroscopy, when per<strong>for</strong>med6,7 Revision including replacement, when per<strong>for</strong>med, <strong>of</strong> spinal neurostimulator63663electrode percutaneous array(s), including fluoroscopy, when per<strong>for</strong>medRevision including replacement, when per<strong>for</strong>med, <strong>of</strong> spinal neurostimulator63664 6 electrode plate/paddle(s) placed via laminotomy or laminectomy, includingfluoroscopy, when per<strong>for</strong>med63685636889597295973L8680 8L9900Insertion or replacement <strong>of</strong> spinal neurostimulator pulse generator or receiver,direct or inductive couplingRevision or removal <strong>of</strong> implanted spinal neurostimulator pulse generator orreceiverElectronic analysis <strong>of</strong> implanted neurostimulator pulse generator system;<strong>com</strong>plex spinal cord, with intraoperative or subsequent programming, first hourElectronic analysis <strong>of</strong> implanted neurostimulator pulse generator system;<strong>com</strong>plex spinal cord, with intraoperative or subsequent programming, eachadditional 30 minutes after first hourImplantable neurostimulator electrode, eachOrthotic and prosthetic supply, accessory, and/or service <strong>com</strong>ponent <strong>of</strong> anotherHCPCS "L" code90 $ 80310$ 535 (Non-Facility)$ 299 (Facility)90 $ 68710$ 792 (Non-Facility)$ 462 (Facility)90 $ 71510 $ 37310XXXZZZNANA$ 337$ 102 (Non-Facility)$ 76 (Facility)$ 57 (Non-Facility)$ 46 (Facility)$ 377 (Floor)$ 502 (Ceiling)Part BContracted Price1Department <strong>of</strong> Health and Human Services. Centers <strong>for</strong> Medicare and Medicaid Services. MLN Matters® Number: MM6796. http://www.cms.hhs.gov/MLNMattersArticles/downloads/MM6796.pdf . NationalAverage Medicare physician payment rates calculated using a 2010 conversion factor <strong>of</strong> $36.0846. Rates subject to change and do not reflect a Sustainable Growth Rate reduction.Expiration date <strong>for</strong> MD rates: 1MAR2010 Subject to Change.2CPT Copyright 2009 American <strong>Medical</strong> Association (AMA). All rights reserved. CPT ® is a registered trademark <strong>of</strong> the American <strong>Medical</strong> Association. Applicable FARS/DFARS Restrictions Apply toGovernment Use. Fee schedules, relative value units, conversion factors and/or related <strong>com</strong>ponents are not assigned by the AMA, are not part <strong>of</strong> CPT, and the AMA is not re<strong>com</strong>mending their use. The AMAdoes not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability <strong>for</strong> data contained or not contained herein.3In the physician <strong>of</strong>fice setting, the Medicare Part B Contractor has jurisdiction <strong>for</strong> this implantable prosthetic device. (CMS Transmittal 803, CR 4363, March 24, 2006)4 2010 Medicare base reimbursement amounts are shown without geographic adjustment.5Medicare payment range reflects the “floor” and “ceiling” rates established <strong>for</strong> these codes. Refer to: http://www.cms.hhs.gov/DMEPOSFeeSched/LSDMEPOSFEE/ <strong>for</strong> appropriate payment by state.6AMA created four new CPT codes specific to removal and revision <strong>of</strong> both the percutaneous and laminectomy leads. The new 2010 CPT codes (63661-63664) are more specific; replacing CPT 63660.7Do not report 63661 or 63663 when removing or replacing a temporary percutaneously placed array <strong>for</strong> an external generator (AMA_CPT 2010 coding book; pg 311).8On December 18, 2009, CMS issued a 2010 HCPCS Correction clarifying that the long code descriptor <strong>for</strong> L8680 will remain unchanged from the CY 2009 descriptor(see www.cms.hhs.gov/HCPCSReleaseCodeSets/ANHCPCS/list.asp).See back page <strong>for</strong> important in<strong>for</strong>mation about the uses and limitations <strong>of</strong> this document.
2010 Physician Coding Scenarios <strong>for</strong> Spinal Cord StimulationImportant: The following are coding scenarios <strong>for</strong> <strong>com</strong>monly per<strong>for</strong>med Spinal Cord Stimulator (SCS) procedures. Payer policies will varyand should be verified prior to treatment <strong>for</strong> limitations on diagnosis, coding or site <strong>of</strong> service requirements. The coding options listed withinthis guide are <strong>com</strong>monly used codes and are not intended to be an all-inclusive list. We re<strong>com</strong>mend consulting your relevant manuals <strong>for</strong>appropriate coding options.Trial: Single or Dual Lead in Facility (POS: 22, 24)Code Modifier Units Comments63650 163650 51 1 1 If dual lead procedure95972 1 Use if per<strong>for</strong>med95973 Units determined by programming timeTrial: Single or Dual Lead in Physician Office (POS: 11)Code Modifier Units Comments63650 163650 51 1 If dual lead procedure95972 1 Use if per<strong>for</strong>med95973 Units determined by programming timeL8680 8 / 16 Use 16 units <strong>for</strong> dual lead procedureL9900 1 Patient trial kitImplant: IPG and Percutaneous Lead(s) (POS: 22, 24)Code Modifier Units Comments63650 58 2 1 Use if staged63650 58, 51 1 Use if staged; if dual lead procedure63685 58 1 Use if staged95972 1 Use if per<strong>for</strong>med95973 Units determined by programming timeImplant: IPG and Laminectomy Lead (POS: 22, 24)Code Modifier Units Comments63655 58 1 Use if staged63685 58 1 Use if staged95972 1 Use if per<strong>for</strong>med95973 Units determined by programming timePain Management Reimbursement HotlinePhone: (866) 287-0778 Monday – Friday5:00 a.m. to 5:00 p.m. Pacific TimeFax: (877) 835-2520www.controlyourpain.<strong>com</strong>/reimbursementBoston Scientific CorporationNeuromodulation25155 Rye Canyon LoopValencia, CA 91355www.bostonscientific.<strong>com</strong>1 Modifier 51: Indicates multiple procedures. (Please verify with payer.)2Modifier 58: Indicates that it is a staged or related service by same physician during the post-operative period (use within global period).Health economic and reimbursement in<strong>for</strong>mation provided by Boston Scientific Corporation is gathered from third-party sources and is subject to change without notice as a result <strong>of</strong> <strong>com</strong>plex and frequentlychanging laws, regulations, rules and policies. This in<strong>for</strong>mation is presented <strong>for</strong> illustrative purposes only and does not constitute reimbursement or legal advice. Boston Scientific encourages providers tosubmit accurate and appropriate claims <strong>for</strong> services. It is always the provider’s responsibility to determine medical necessity, the proper site <strong>for</strong> delivery <strong>of</strong> any services and to submit appropriate codes,charges, and modifiers <strong>for</strong> services that are rendered. Boston Scientific re<strong>com</strong>mends that you consult with your payers, reimbursement specialists and/or legal counsel regarding coding, coverage andreimbursement matters. Boston Scientific does not promote the use <strong>of</strong> its products outside their FDA-approved label.In<strong>for</strong>mation included herein is current as <strong>of</strong> May 05, 2010, but is subject to change without notice.3-200545© 2010 Boston Scientific Corporation and its affiliates. All rights reserved.Outpatient_2010_QRG_06.07.2010
2010 Ambulatory Surgery Center Coding and PaymentQuick Reference <strong>for</strong> Spinal Cord StimulationNeuromodulationReimbursement Coding and Medicare Payment Guide: This in<strong>for</strong>mation pertains to the Centers <strong>for</strong> Medicare and MedicaidServices’ (CMS) 2010 coding and national payment rates <strong>for</strong> spinal cord stimulator (SCS) procedures per<strong>for</strong>med in theAmbulatory Surgery Center (ASC). Medicare reimbursement <strong>for</strong> the ASC is bundled into the Ambulatory PaymentClassification (APC) where payment covers both the procedural and device <strong>com</strong>ponents.CPT Code 1PaymentDescriptionPercutaneous implantation <strong>of</strong> neurostimulator electrode array;63650epidural (each)Laminectomy <strong>for</strong> implantation <strong>of</strong> neurostimulator electrodes, plate/63655paddle(s), epidural6 Removal <strong>of</strong> spinal neurostimulator electrode percutaneous array(s),63661including fluoroscopy, when per<strong>for</strong>medRemoval <strong>of</strong> spinal neurostimulator electrode plate/paddle(s) placed63662 6 via laminotomy or laminectomy, including fluoroscopy, whenper<strong>for</strong>medRevision including replacement, when per<strong>for</strong>med, <strong>of</strong> spinal63663 6 neurostimulator electrode percutaneous array(s), includingfluoroscopy, when per<strong>for</strong>medRevision including replacement, when per<strong>for</strong>med, <strong>of</strong> spinal63664 6 neurostimulator electrode plate/paddle(s) placed via laminotomy orlaminectomy, including fluoroscopy, when per<strong>for</strong>medInsertion or replacement <strong>of</strong> spinal neurostimulator pulse generator or63685receiver, direct or inductive coupling63688Revision or removal <strong>of</strong> implanted spinal neurostimulator pulsegenerator or receiverAPC 2StatusIndicatorMedicare NationalAverage Payment 30040 H8 4 $ 3,4960061 J8 5 $ 4,9700687 A2 7 $ 7870039 8 H8 $ 12,8770688 A2 $ 941Pain Management Reimbursement HotlinePhone: (866) 287-0778 Monday – Friday5:00 a.m. to 5:00 p.m. Pacific TimeFax: (877) 835-2520www.controlyourpain.<strong>com</strong>/reimbursementBoston Scientific CorporationNeuromodulation25155 Rye Canyon LoopValencia, CA 91355www.bostonscientific.<strong>com</strong>1CPT Copyright 2009 American <strong>Medical</strong> Association. All rights reserved. CPT ® is a registered trademark <strong>of</strong> the American <strong>Medical</strong> Association. Applicable ARS/DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related <strong>com</strong>ponents are not assigned by the AMA,are not part <strong>of</strong> CPT, and the AMA is not re<strong>com</strong>mending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMAassumes no liability <strong>for</strong> data contained or not contained herein.2CMS 42 CFR Parts 410, 416, and 419 [CMS–1414–FC]. Available online at http://edocket.access.gpo.gov/2009/pdf/E9-26499.pdf3Medicare reimbursement amounts are shown without geographic adjustment <strong>for</strong> wage.4Device-intensive procedure on ASC list in CY 2007; paid at adjusted rate, not subject to multiple reduction rule.5Device-intensive procedure added to ASC list in CY 2008 or later paid at adjusted; not subject to multiple reduction rule.6AMA created four new CPT codes specific to removal and revision <strong>of</strong> both the percutaneous and laminectomy leads. The new 2010 CPT codes (63661-63664) aremore specific; replacing CPT 63660.7Surgical procedure on ASC list in CY 2007; payment based on OPPS relative weight, subject to multiple reduction rule.8APC 0039 includes CPT codes 61885 (single-array cranial neurostimulators), 64590 (peripheral nerve stimulator), and 63685 as a result <strong>of</strong> 2010 Final OPPS/ASCRule. APC 0222 has been discontinued as a result <strong>of</strong> the consolidation <strong>of</strong> 63685 into APC 0039.See back page <strong>for</strong> important in<strong>for</strong>mation about the uses and limitations <strong>of</strong> this document.
2010 Ambulatory Surgery Center Coding Scenarios <strong>for</strong> Spinal Cord Stimulation (Place <strong>of</strong> Service 24)Important: The following are coding scenarios <strong>for</strong> <strong>com</strong>monly per<strong>for</strong>med Spinal Cord Stimulator (SCS) procedures. Payerpolicies will vary and should be verified prior to treatment <strong>for</strong> limitations on diagnosis, coding or site <strong>of</strong> service requirements.The coding options listed within this guide are <strong>com</strong>monly used codes and are not intended to be an all-inclusive list. Were<strong>com</strong>mend consulting your relevant manuals <strong>for</strong> appropriate coding options.Trial Procedure: Single or Dual Percutaneous LeadCode Modifier Units Comments63650 163650 1 If dual lead procedureImplant Procedure: Single or Dual Percutaneous Lead & IPGCode Modifier Units Comments63685 58 1 1 Use if staged63650 58 163650 58 1 If dual lead procedureImplant Procedure: Laminectomy Lead & IPGCode Modifier Units Comments63685 58 1 Use if staged63655 58 1 Use if laminectomy lead placementCPT and Related HCPCS Association <strong>for</strong> Non-Medicare Payers 2CPT HCPCS Descriptor63663, 6366463650, 63655L8680 3Implantable neurostimulator electrode, each63685 L8687 Implantable neurostimulator pulse generator, dual array, rechargeable, includes extensionNANAL8681L8689Patient programmer (external) <strong>for</strong> use with implantable programmable neurostimulator pulsegenerator, replacement onlyExternal recharging system <strong>for</strong> battery (internal) <strong>for</strong> use with implantable neurostimulator,replacement onlyNA L8699 Prosthetic implant, not otherwise specifiedNA L9900 Orthotic and prosthetic supply, accessory, and/or service <strong>com</strong>ponent <strong>of</strong> another HCPCS “L” codeDeviceCode 4Revenuecode 278Description<strong>Medical</strong>/ surgical supplies - other implants1Modifier 58: Indicates that it is a staged or related service by same physician during the post-operative period (use within global period).2Please verify with local payers <strong>for</strong> specific device coding requirements.3On December 18, 2009, CMS issued a 2010 HCPCS Correction clarifying that the long code descriptor <strong>for</strong> L8680 will remain unchanged from the CY 2009descriptor (see www.cms.hhs.gov/HCPCSReleaseCodeSets/ANHCPCS/list.asp).4Medicare Claims Processing Manual, Chapter 4. CMS, Baltimore, MDHealth economic and reimbursement in<strong>for</strong>mation provided by Boston Scientific Corporation is gathered from third-party sources and is subject to change without notice as a result <strong>of</strong> <strong>com</strong>plex and frequentlychanging laws, regulations, rules and policies. This in<strong>for</strong>mation is presented <strong>for</strong> illustrative purposes only and does not constitute reimbursement or legal advice. Boston Scientific encourages providers tosubmit accurate and appropriate claims <strong>for</strong> services. It is always the provider’s responsibility to determine medical necessity, the proper site <strong>for</strong> delivery <strong>of</strong> any services and to submit appropriate codes,charges, and modifiers <strong>for</strong> services that are rendered. Boston Scientific re<strong>com</strong>mends that you consult with your payers, reimbursement specialists and/or legal counsel regarding coding, coverage andreimbursement matters. Boston Scientific does not promote the use <strong>of</strong> its products outside their FDA-approved label.In<strong>for</strong>mation included herein is current as <strong>of</strong> May 5, 2010, but is subject to change without notice.3-200547© 2010 Boston Scientific Corporation and its affiliates. All rights reserved.Outpatient_2010_QRG_06.07..2010
2010 Outpatient Hospital Coding and PaymentQuick Reference <strong>for</strong> Spinal Cord StimulationNeuromodulationReimbursement Coding and Medicare Payment Guide: This in<strong>for</strong>mation pertains to the Centers <strong>for</strong> Medicare and MedicaidServices’ (CMS) 2010 coding and national payment rates <strong>for</strong> spinal cord stimulator (SCS) procedures in the outpatient hospital. In thehospital outpatient prospective payment system (OPPS), Medicare bundles the reimbursement <strong>for</strong> the procedural and device <strong>com</strong>ponentsinto an ambulatory payment classification (APC).CPT Code 1PaymentDescriptionPercutaneous implantation <strong>of</strong> neurostimulator electrode array; epidural63650(each)Laminectomy <strong>for</strong> implantation <strong>of</strong> neurostimulator electrodes, plate/63655paddle(s), epidural5 Removal <strong>of</strong> spinal neurostimulator electrode percutaneous array(s),63661including fluoroscopy, when per<strong>for</strong>med5 Removal <strong>of</strong> spinal neurostimulator electrode plate/paddle(s) placed via63662laminotomy or laminectomy, including fluoroscopy, when per<strong>for</strong>medRevision including replacement, when per<strong>for</strong>med, <strong>of</strong> spinal63663 5 neurostimulator electrode percutaneous array(s), including fluoroscopy,when per<strong>for</strong>medRevision including replacement, when per<strong>for</strong>med, <strong>of</strong> spinal63664 5 neurostimulator electrode plate/paddle(s) placed via laminotomy orlaminectomy, including fluoroscopy, when per<strong>for</strong>medInsertion or replacement <strong>of</strong> spinal neurostimulator pulse generator or63685receiver, direct or inductive coupling636889597295973APC 2StatusIndicatorMedicare NationalAverage Payment 3When Billing Medicare: The following C-codes are required <strong>for</strong> billing Medicare outpatient procedures with the applicable CPT codes, butare not separately payable by Medicare.C-Code 8 Description CPT CodeC1778C1787C1820Revision or removal <strong>of</strong> implanted spinal neurostimulator pulse generatoror receiverElectronic analysis <strong>of</strong> implanted neurostimulator pulse generator system;<strong>com</strong>plex spinal cord, with intraoperative or subsequentprogramming, first hourElectronic analysis <strong>of</strong> implanted neurostimulator pulse generator system;<strong>com</strong>plex spinal cord, with intraoperative or subsequent programming,each additional 30 minutes after first hourLead, neurostimulators (implantable)Patient programmer (external) <strong>for</strong> use with implantable programmable neurostimulatorpulse generatorGenerator, neurostimulator (implantable) and external recharging system <strong>for</strong> battery (internal) <strong>for</strong> usewith implantable neurostimulator0040 S 4 $ 4,4290061 S $ 5,8320687 T 6 $ 1,3240039 7 S $ 13,8920688 T $ 1,9320692 S $ 1080692 S $ 10863663, 6366463650, 63655C1883 Adapter/extension, pacing lead or neurostimulators lead (implantables) 6365063685636851CPT Copyright 2009 American <strong>Medical</strong> Association. All rights reserved. CPT ® is a registered trademark <strong>of</strong> the American <strong>Medical</strong> Association. Applicable FARS/DFARS Restrictions Apply to Government Use.Fee schedules, relative value units, conversion factors and/or related <strong>com</strong>ponents are not assigned by the AMA, are not part <strong>of</strong> CPT, and the AMA is not re<strong>com</strong>mending their use. The AMA does not directly orindirectly practice medicine or dispense medical services. The AMA assumes no liability <strong>for</strong> data contained or not contained herein.2CMS 42 CFR Parts 410, 416, and 419 [CMS–1414–FC]. Available online at http://edocket.access.gpo.gov/2009/pdf/E9-26499.pdf32010 Medicare base reimbursement amounts are shown without geographic adjustment.4Significant procedure, not subject to multiple reduction rule.5AMA created four new CPT codes specific to removal and revision <strong>of</strong> both the percutaneous and laminectomy leads. The new 2010 CPT codes (63661-63664) are more specific; replacing CPT 636606Significant procedure, multiple surgical reduction applies.7APC 0039 includes CPT codes 61885 (single-array cranial neurostimulators), 64590 (peripheral nerve stimulator), and 63685 as a result <strong>of</strong> 2010 Final OPPS/ASC Rule. APC 0222 has been discontinued as aresult <strong>of</strong> the consolidation <strong>of</strong> 63685 into APC 0039.8CMS 42 CFR Parts 410, 416, and 419 [CMS–1404–FC; CMS–3887–F; CMS–3835–F–1]. Available online at http://edocket.access.gpo.gov/2008/pdf/E8-26212.pdfReimbursement Hotline: (866) 287-0778www.controlyourpain.<strong>com</strong>/reimbursementSee back page <strong>for</strong> important in<strong>for</strong>mation about the uses and limitations <strong>of</strong> this document.
2010 Outpatient Coding Scenarios <strong>for</strong> Spinal Cord Stimulation (Place <strong>of</strong> Service 22)Important: The following are coding scenarios <strong>for</strong> <strong>com</strong>monly per<strong>for</strong>med Spinal Cord Stimulator (SCS) procedures. Payer policies will vary andshould be verified prior to treatment <strong>for</strong> limitations on diagnosis, coding or site <strong>of</strong> service requirements. The coding options listed within thisguide are <strong>com</strong>monly used codes and are not intended to be an all-inclusive list. We re<strong>com</strong>mend consulting your relevant manuals <strong>for</strong>appropriate coding options.Trial Procedure: Single or Dual Percutaneous LeadCode Modifier Units Comments63650 163650 1 If dual lead procedure95972 1 Use if per<strong>for</strong>med95973 Units determined by programming timeC1778 1 Use two units if dual lead procedureC1883Lead extension, if used (2 if dual leads)Implant Procedure: Single or Dual Percutaneous Lead & IPGCode Modifier Units Comments63685 58 1 1 Use if staged63650 58 163650 58 1 If dual lead procedure95972 1 Use if per<strong>for</strong>med95973 Units determined by programming timeC1820 1C1778 1 Use two units if dual lead procedureC1883Implant Procedure: Laminectomy Lead & IPGCode Modifier Units Comments63685 58 1 Use if stagedLead extension, if used (2 if dual leads)63655 58 1 Use if laminectomy lead placement95972 1 Use if per<strong>for</strong>med95973 Units determined by programming timeC1820 1C1778 1C1883CPT and Related HCPCS Association <strong>for</strong> Non-Medicare Payers 2CPT63663, 6366463650, 63655HCPCS DescriptorL8680 3Implantable neurostimulator electrode, eachLead extension, if usedNote: Where revenue center coding is to be utilized, Revenue code 278: <strong>Medical</strong>/ surgical supplies - other implants applies to implantableSCS systems (including generator and leads).63685 L8687 Implantable neurostimulator pulse generator, dual array, rechargeable, includes extensionNAL8681Patient programmer (external) <strong>for</strong> use with implantable programmable neurostimulator pulse generator,replacement onlyNA L8689 External recharging system <strong>for</strong> battery (internal) <strong>for</strong> use with implantable neurostimulator, replacement onlyNA L8699 Prosthetic implant, not otherwise specifiedNA L9900 Orthotic and prosthetic supply, accessory, and/or service <strong>com</strong>ponent <strong>of</strong> another HCPCS “L” code1Modifier 58: Indicates that it is a staged or related service by same physician during the post-operative period (use within global period).2Please verify with local payers <strong>for</strong> specific device coding requirements.3On December 18, 2009, CMS issued a 2010 HCPCS Correction clarifying that the long code descriptor <strong>for</strong> L8680 will remain unchanged from the CY 2009 descriptor(see www.cms.hhs.gov/HCPCSReleaseCodeSets/ANHCPCS/list.asp ).Health economic and reimbursement in<strong>for</strong>mation provided by Boston Scientific Corporation is gathered from third-party sources and is subject to change without notice as a result <strong>of</strong> <strong>com</strong>plex and frequently changing laws,regulations, rules and policies. This in<strong>for</strong>mation is presented <strong>for</strong> illustrative purposes only and does not constitute reimbursement or legal advice. Boston Scientific encourages providers to submit accurate and appropriate claims<strong>for</strong> services. It is always the provider’s responsibility to determine medical necessity, the proper site <strong>for</strong> delivery <strong>of</strong> any services and to submit appropriate codes, charges, and modifiers <strong>for</strong> services that are rendered. BostonScientific re<strong>com</strong>mends that you consult with your payers, reimbursement specialists and/or legal counsel regarding coding, coverage and reimbursement matters. Boston Scientific does not promote the use <strong>of</strong> its products outsidetheir FDA-approved label.In<strong>for</strong>mation included herein is current as <strong>of</strong> May 05, 2010, but is subject to change without notice.3-200546© 2010 Boston Scientific Corporation and its affiliates. All rights reserved.Outpatient_2010_QRG_06.07.2010