The Peripheral Arterial Disease Guideline - Ochsner Academics
The Peripheral Arterial Disease Guideline - Ochsner Academics
The Peripheral Arterial Disease Guideline - Ochsner Academics
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
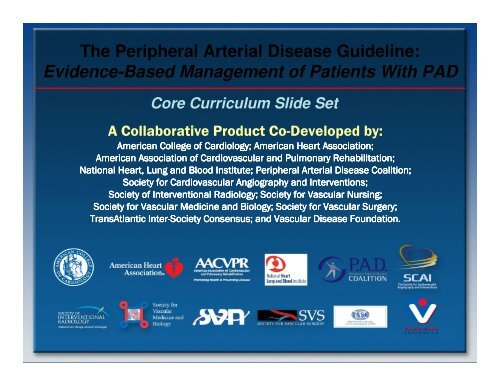
<strong>The</strong> <strong>Peripheral</strong> <strong>Arterial</strong> <strong>Disease</strong> <strong>Guideline</strong>:Evidence-Based Management of Patients With PADCore Curriculum Slide SetA Collaborative Product Co-Developed by:American College of Cardiology; American Heart Association;American Association of Cardiovascular and Pulmonary Rehabilitation;ion;National Heart, Lung and Blood Institute; <strong>Peripheral</strong> <strong>Arterial</strong> <strong>Disease</strong> Coalition;Society for Cardiovascular Angiography and Interventions;Society of Interventional Radiology; Society for Vascular Nursing;Society for Vascular Medicine and Biology; Society for Vascular Surgery;TransAtlantic Inter-Society Consensus; and Vascular <strong>Disease</strong> Foundation.
<strong>The</strong> <strong>Peripheral</strong> <strong>Arterial</strong> <strong>Disease</strong> Task to beAccomplished Is Encompassed in the Title:ACC/AHA <strong>Guideline</strong>s for the Management of PatientsWith <strong>Peripheral</strong> <strong>Arterial</strong> <strong>Disease</strong>:A Collaborative Report from theAmerican Association for Vascular Surgery/Society for Vascular Surgery,Society for Cardiovascular Angiography and Interventions,Society of Interventional Radiology,Society for Vascular Medicine and Biology, andthe ACC/AHA Task Force on Practice <strong>Guideline</strong>s.Also endorsed by the:American Association of Cardiovascular and Pulmonary Rehabilitation;National Heart, Lung, and Blood Institute;Society for Vascular Nursing;TransAtlantic Inter-Society Consensus; and<strong>The</strong> Vascular <strong>Disease</strong> Foundation.
Contributors<strong>The</strong> PAD <strong>Guideline</strong>s Implementation Task ForceSlide Set Co-EditorsMark A. Creager, MD, & Alan T. Hirsch, MDAlan T. Hirsch, Co-ChairVascular Medicine/CardiologyCarolyn Robinson, NP, Co-Chair,Vascular NursingThomas A. Biggs, MDFrank C. Brosius, III, MDMark A. Creager, MDJames B. Froehlich, MD, MPHWilliam R. Hiatt, MDKaren Lui, RN, MSTimothy Murphy, MDJeffrey W. Olin, DOHarvey M. Wiener, DO, Co-Chair,Interventional RadiologyJohn White, MD, Co-Chair,Vascular SurgeryArthur L. Riba, MDKerry J. Stewart, EdDDiane Treat-Jacobson, RN, PhDRose Marie Robertson, MDMark Sanz, MDPeter Sheehan, MDH. Eser Tolunay, PhDChristopher White, MD
Special Thanks to<strong>The</strong> PAD <strong>Guideline</strong>s Writing CommitteeMembersAlan T. Hirsch, MD, FACC, FAHA, ChairZiv J. Haskal, MD, FAHA, FSIR, Co-Chair,Norman R. Hertzer, MD, FACS, Co-ChairCurtis W. Bakal, MD, MPH, FAHAMark A. Creager, MD, FACC, FAHAJonathan L. Halperin, MD, FACC, FAHALoren F. Hiratzka, MD, FACC, FAHA, FACSWilliam R.C. Murphy, MD, FACC, FACSJules B. Puschett, MD, FAHAKenneth A. Rosenfield, MD, FACCDavid Sacks, MD, FACR, FSIRJames C. Stanley, MD, FACS, FACR, FSIRLloyd M. Taylor, Jr., MD, FACSChristopher J. White, MD, FACC, FAHA, FSCAIJohn White, MD, FACSRodney A. White, MD, FACSJeffrey W. Olin, DO, FACC
Applying Classification ofRecommendations and Level of EvidenceClass IClass IIaClass IIbClass IIIBenefit >>> RiskProcedure/ TreatmentSHOULD beperformed/administeredBenefit >> RiskAdditional studies withfocused objectivesneededIT IS REASONABLEto performprocedure/administertreatmentBenefit ≥ RiskAdditional studies withbroad objectivesneeded; Additionalregistry data would behelpfulProcedure/TreatmentMAY BE CONSIDEREDRisk ≥ BenefitNo additional studiesneededProcedure/Treatmentshould NOT beperformed/administeredSINCE IT IS NOTHELPFUL AND MAYBE HARMFULshouldis recommendedis indicatedis useful/effective/beneficialis reasonablecan be useful/effective/beneficialis probably recommendedor indicatedmay/might be consideredmay/might be reasonableusefulness/effectiveness isunknown /unclear/uncertainor not well establishedis not recommendedis not indicatedshould notis notuseful/effective/beneficialmay be harmful
Applying Classification ofRecommendations and Level of EvidenceClass IClass IIaClass IIbClass IIIBenefit >>> RiskProcedure/Treatment SHOULDbe performed/administeredBenefit >> RiskAdditional studies withfocused objectivesneededIT IS REASONABLE toperformprocedure/administertreatmentBenefit ≥ RiskAdditional studies withbroad objectives needed;Additional registry datawould be helpfulProcedure/TreatmentMAY BE CONSIDEREDRisk ≥ BenefitNo additional studiesneededProcedure/Treatmentshould NOT beperformed/administeredSINCE IT IS NOTHELPFUL AND MAYBE HARMFULLevel A Multiple (3-5) population risk strata evaluatedGeneral consistency of direction and magnitude of effectLevel BLevel CLimited (2-3) population risk strata evaluatedVery limited (1-2) population risk strata evaluated
Why a PAD <strong>Guideline</strong>?• To enhance the quality of patient care• Increasing recognition of the importance of atherosclerotic lowerextremity PAD:– High prevalence– High cardiovascular risk– Poor quality of life• Improved ability to detect and treat renal artery disease• Improved ability to detect and treat abdominal aortic aneurysm• <strong>The</strong> evidence base has become increasingly robust, so that adata-driven care guideline is now possible
PAD <strong>Guideline</strong>:<strong>The</strong> Target Audiences Are Diverse• Primary care clinicians– Family practice– Internal medicine– PA, NP, nurse clinicians• Cardiovascular/vascular medicine,vascular surgical, & interventionalradiology trainees• Vascular specialistsThis is not intended to be a procedural guideline;it is intended to provide a guide to optimal lifelong PAD care.
PADEpidemiology
Prevalence of PADNHANES 1Aged >40 yearsSan Diego 2Mean age 66 yearsNHANES 1Aged 70 yearsRotterdam 3Aged >55 yearsDiehm 4Aged 65 yearsPARTNERS 54.3%11.7%14.5%Aged >70 years, or 50–69 years with a history diabetes or smoking19.1%19.8%In a primary carepopulation defined byage and common riskfactors, the prevalence ofPAD was approximatelyone in three patients29%0% 5% 10% 15% 20% 25% 30% 35%NHANES=National Health and Nutrition Examination Study;PARTNERS=PAD Awareness, Risk, and Treatment: New Resources for Survival [program].1. Selvin E, Erlinger TP. Circulation. 2004;110:738-743.2. Criqui MH, et al. Circulation. 1985;71:510-515.3. Diehm C, et al. Atherosclerosis. 2004;172:95-105.4. Meijer WT, et al. Arterioscler Thromb Vasc Biol. 1998;18:185-192.5. Hirsch AT, et al. JAMA. 2001;286:1317-1324.
Prevalence of PAD Increases With AgeRotterdam Study (ABI
Gender Differences in thePrevalence of PADPrevalence (%)181614121086WomenMen6880 Consecutive Patients (61% Female)in 344 Primary Care Offices42085Age (years)Adapted from Diehm C. Atherosclerosis. 2004;172:95-105 with permission from Elsevier.
Ethnicity and PAD:<strong>The</strong> San Diego Population StudyFraction of Population With PAD (%)109876543210NHW Black Hispanic AsianNHW = Non-hispanic white.Reprinted with permission from Criqui, et al. Circulation. 2005:112:2703-07.
Diabetes Increases the Risk of PADPrevalence of PAD (%)25201510512.519.9*22.4*0Normal GlucoseToleranceImpaired GlucoseToleranceDiabetesImpaired glucose tolerance was defined as oral glucose tolerance test value ≥140 mg/dL but
CRP as Predictor of Incident PAD0.20.17hs-CRP (mg/dL)0.10.10.130.0NoneIntermittentClaudication<strong>Peripheral</strong> ArterySurgeryCRP = C-reactive protein; hs-CRP = high-sensitivity C-reactive proteinRidker, et al. Circulation.1998;97:425-28.
Risk Factors for PADReduced IncreasedSmokingDiabetesHypertensionHypercholesterolemiaHyperhomocysteinemiaC-Reactive ProteinRelative Risk01 2 3 4 5 6Hirsch AT, et al. J Am Coll Cardiol. 2006;47:e1-e192.
PARTNERS: Prevalence of PADand Other CVD in Primary Care Practices29% of Patients in a Target Population Were Diagnosed WithPAD Using An Office-Based ABI29%44%56%Patients diagnosed with PADPAD onlyPAD and CVDABI=ankle-brachial index; CVD=cardiovascular disease. Hirsch, AT et al. JAMA. 2001;286:1317-24.
Individuals “At Risk” for Lower Extremity PADBased on the epidemiologic evidence base,an “at risk” population for PAD can be objectively defined by:• Age less than 50 years with diabetes, and one additionalrisk factor (e.g., smoking, dyslipidemia, hypertension, orhyperhomocysteinemia)• Age 50 to 69 years and history of smoking or diabetes• Age 70 years and older• Leg symptoms with exertion (suggestive of claudication) orischemic rest pain• Abnormal lower extremity pulse examination• Known atherosclerotic coronary, carotid, or renal arterydisease
PADPrognosis
<strong>The</strong> Natural History of PAD• Individuals with PAD are at increased risk forcardiovascular ischemic events due to concomitant CAD(fatal and non-fatal MI) and cerebrovascular disease(fatal and non-fatal stroke).• Cardiovascular events are more frequent than ischemiclimb events in any lower extremity PAD cohort,regardless of the clinical presentation.
Natural History of AtheroscleroticLower Extremity PADPAD Population (50 years and older)Initial clinical presentationAsymptomatic PAD20%-50%Atypical leg pain40%-50%Claudication10%-35%Critical limb ischemia1%-2%ProgressivefunctionalimpairmentAlive w/ 2 limbs50%1-year outcomesAmputation25%CV mortality25%5-year outcomes(to next slide)Reprinted with permission from Hirsch AT, et al. Circulation. 2006;113:e463-654.
Natural History of AtheroscleroticLower Extremity PADFor each of these PAD clinical syndromesAsymptomatic PAD20%-50%Claudication10%-35%Atypical leg pain40%-50%Limb morbidity5-year outcomesCV morbidity & mortalityStable claudication70%-80%Worseningclaudication10%-20%Critical limb ischemia1%-2%Nonfatal CV event(MI or stroke) 20%Mortality15%-30%Amputation(see CLI data)CV causes75%Non-CV causes25%CLI=critical limb ischemia; CV=cardiovascular; MI=myocardial infarctionReprinted with permission from Hirsch AT, et al. Circulation. 2006;113:e463-654.
Contemporary PADRates of Myocardial Infarction and Death3649 subjects (average age 64 years) followed up for 7.2 yearsPercentageHooi JD, et al. J Clin Epid. 2004;57:294–300.
Long-Term Survival in Patients With PAD100Survival (%)755025Normal subjectsAsymptomatic PADSymptomatic PADSevere symptomatic PAD0 2 4 6 8 10 12YearCriqui MH et al. N Engl J Med. 1992;326:381-386. Copyright © 1992 Massachusetts Medical Society. All rights reserved.
Relative Risk of Death in PatientsWith PAD10Relative Risk (95% CI)86423.1(1.9–4.9)5.9(3.0–6.6)6.6(2.9–14.9)0All Causes CVD CHDCause of DeathCI=confidence interval; CHD=coronary heart disease; CVD=cardiovascular disease.Criqui MH, et al. N Engl J Med. 1992;326:381-386.
10-Year Natural History in Patients WithIntermittent Claudication10080Patients (%)604020SurvivalMIInterventionAmputation00 1 2 3 4 5 6 7 8 9 10Time (years)Ouriel K. Lancet. 2001;358;1257-1264.
Association Between ABI andAll-Cause Mortality*Total Mortality (%)8070605040302010Risk increases atABI values below1.0 and above 1.3N=574801.40(n=156)(n=141)(n=186)(n=310)(n=709)(n=1750)(n=1578)(n=696)(n=156)(n=66)Baseline ABIAge range=mid- to late-50s; ABI=ankle-brachial index; *Median duration of follow-up was 11.1 (0.1–12) years.Adapted from O’Hare AM et al. Circulation. 2006;113:388-393.
Cardiovascular Risk Increases WithDecreases in Ankle-Brachial IndexFramingham “High Risk” = 20% at 10 yearsEvery patient with PAD is at “very high risk”CHD Event Outcomesper Year (%)432101.4%>1.1 1.1–1.01 1.0–0.91 0.9–0.71
Baseline Physical Activity and Mortality inPersons With PAD10P = 0.02P-trend = 0.003Adjusted Hazards Ratio(95% Confidence Intervals)8642P = 0.07P = 0.6101st Quartile 2nd Quartile 3rd Quartile 4th QuartilePhysical Activity QuartileReprinted with permission fromGarg P K, et al. Circulation. 2006;114:242-248.
Mortality According to ABI and Diabetes:Strong Heart Study80n=4393Incidence of Deathper 1000 Patient Years70605040302010NondiabeticIFGDiabetic01.4Ankle-Brachial IndexABI=ankle-brachial index; IFG=impaired fasting glucose.Reprinted with permission from Resnick, H. E. et al. Circulation. 2004;109:733-739.
Critical Limb Ischemia (CLI)Fate of Patients With CLI After Initial TreatmentSummary of 6-month outcomes from 19 studiesAlive withamputation35%Dead20%Alive withoutamputation45%Critical limbischemia is definedas ischemic restpain, nonhealingwounds, organgrene.Dormandy JA, Rutherford RB. J Vasc Surg. 2000;31:S1-S296.