Kovey Oral Hematinics in Pediatrics.pdf - Helen DeVos Children's ...
Kovey Oral Hematinics in Pediatrics.pdf - Helen DeVos Children's ...
Kovey Oral Hematinics in Pediatrics.pdf - Helen DeVos Children's ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Oral</strong> <strong>Hemat<strong>in</strong>ics</strong> <strong>in</strong><strong>Pediatrics</strong>Karen <strong>Kovey</strong>, Pharm.D., BCPS<strong>Helen</strong> <strong>DeVos</strong> Children’s HospitalPediatric Blood ManagementConference 2010 - GVSU
Objectives• Overview of iron absorption, metabolism,distribution and storage• Review physiologic impact of <strong>in</strong>flammation• Discuss different forms of available oralproducts• Identify expected outcomes with ironreplacement• Optimize oral hemat<strong>in</strong>ic therapy with adjunctivemedications
Introduction• Average adult European/American dietprovides 10-20mg iron/day• Approximately 10% of dietary iron isabsorbed/day (1-2mg/day) and• Approximately 1-2mg of iron is lost/day• Females at <strong>in</strong>creased risk of iron deficiency• Requirement for erythropoiesis 20-30mg/day
Iron Absorption• Primary site: duodenum1. Reduction of iron to ferrous state(Fe 2+ ) -<strong>in</strong>organic iron2. Apical uptake by DMT13. Intracellular storage by Ferrit<strong>in</strong>4. Basolateral release byFerroport<strong>in</strong>5. Reuptake by Ferrit<strong>in</strong> <strong>in</strong> bloodand delivery to RBC precursors
Alteration of Iron Absorption• Competition with other divalent cations (copper,magnesium, z<strong>in</strong>c, calcium)• pH alteration: proton pump <strong>in</strong>hibitors, antacids, H2blockers, neonates• B<strong>in</strong>ders: co-adm<strong>in</strong>istration with tetracycl<strong>in</strong>es, phenoliccompounds, phytates• Impaired Iron Uptake: H. pylori, gastric atrophy• Iron storage status, presence of hypoxia, rate oferythropoiesis• Expression of hepcid<strong>in</strong>
Iron Distribution &Cycl<strong>in</strong>g• Iron is transferr<strong>in</strong> bound <strong>in</strong>plasma• Delivered to bone marrow,muscle and liver where it isstored• Iron is released fromtransferr<strong>in</strong> via pHalternation <strong>in</strong>side theendosome
Iron Distribution & Cycl<strong>in</strong>g
Impact of Chronic Inflammation onIron HomeostasisInt-γ, TNF-α, Interleuk<strong>in</strong>s (IL)-1, 6, & 101. Decreased RBC half life2. Impaired erythropoiet<strong>in</strong> (EPO) production3. Impaired responsiveness of erythroid cellsto EPO4. Inhibition of proliferation anddifferentiation of erythroid cells5. Increased iron storage
Impact of Acute Inflammation onIron HomeostasisInterleuk<strong>in</strong>s 6 and 8 (major) and TNF-α andIL-1 (m<strong>in</strong>or)1. Perioperative or traumatic blood loss2. Blunted erythropoiesis due to decreased ironbioavailability (hepcid<strong>in</strong>)
Impact of Inflammation on IronHomeostasis
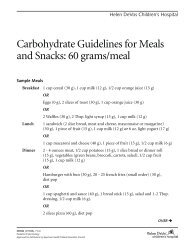
Enteral Iron Products
Enteral Iron Dos<strong>in</strong>g• Dos<strong>in</strong>g for anemia:• Premature Neonates: 2-4mg elemental Fe/kg/day• Infants and Children:• Severe anemia: 4-6mg elemental Fe/kg/day• Mild/Moderate anemia: 3mg elemental Fe/kg/day• Anemia Prophylaxis: 1-2 mg elemental Fe/kg/day• Adults:• Anemia: 2-3mg elemental Fe/kg/day• Anemia Prophylaxis: 60mg elemental Fe/day
Enteral Iron ProductsInorganic IronSaltsFerrous sulfateFerrous gluconateFerrous fumarateOrganic IronHeme Iron PolypeptidePolysaccharide Iron ComplexChelated Iron ProductsFerrous bis glyc<strong>in</strong>ateFerrochel & Sumalate ironElemental IronSaltsCarbonyl Iron
Immediate Release (IR) Preparations1. Ferrous sulfate 300mg or 325mg2. Ferrous gluconate 27mg (Fergon®)3. Ferrous Bis-Glyc<strong>in</strong>ate 27mg (Gentle Iron®)4. Carbonyl Iron 45mg or 50mg (Feosol®, PerfectIron®)5. Polysaccharide Iron Complex (PIC) 22mg + HemeIron Polypeptide as Proferr<strong>in</strong> (HIP) 6mg mixtures(Bifera®)6. Heme Iron Polypeptide 12mg (Proferr<strong>in</strong>® ES)
Susta<strong>in</strong>ed or Extended Release (SRor ER) Preparations1. SlowFe® (ferrous sulfate 45mg elementaliron)2. Ferro-Sequels® (Ferrous fumarate 50mg)
Liquid Preparations1. Ferrous sulfate elixir 220mg/5mL (44mgelemental iron/5mL)2. Ferrous sulfate drops 75mg/0.6mL (15mgelemental iron/0.6mL)3. Fer-In-Sol® (ferrous sulfate drops) 75mg/1mL(15mg elemental iron/1mL)4. Poly-Vi-Sol w/Iron Infant Drops – conta<strong>in</strong>10mg elemental iron per 1mL
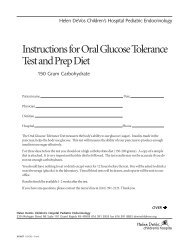
Prescription Only Iron Supplements
Niferex-150®Iron (elemental iron)• Sumalate®* iron . . . . .. . . . . . . . . . . . . . . . . . . . . . 50 mg• Polysaccharide iron . . . . . . . . . . . . . . . . . . . . . . . 100 mg• Succ<strong>in</strong>ic acid . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . 50 mg• Vitam<strong>in</strong> C• Ester-C ® supplement ... . . . . . . . . . . . . . . . . . . . . 50 mgSumalate®* = ferrous asparto glyc<strong>in</strong>ate
Niferex-150 Forte®Iron (elemental iron)• Sumalate® iron . . ... . . . . .. . . . ... . . . . . . . 50 mg• Polysaccharide iron . . . . …. .. ... . . . . . . . 100 mg• Succ<strong>in</strong>ic acid . . . . . . . . . . .. .. .. . ... .. . . . . . 50 mg• Vitam<strong>in</strong> C• Ester-C ® supplement . . ... . . … . . .. . . . . . 60 mg• Folic acid, USP . . . . . . . . . . .. . . . .. .. . . . . . . 1 mg• Vitam<strong>in</strong> B12 (cyanocobalam<strong>in</strong>) . . . .. . . . . 25 mcg
Repliva® 21/7Iron (elemental iron)• Ferrochel®………………………………….……………..70 mg• Ferrous fumarate…………………………….....………...81 mg• Succ<strong>in</strong>ic acid………………………………………………150 mg• Vitam<strong>in</strong> C (ascorbic acid)………………………………..140 mg• Vitam<strong>in</strong> C as Ester-C ®• Ascorbic acid (as calcium ascorbate)………………..…60 mg• Threonic acid (as calcium threonate)………………….0.8 mg• Folic acid, USP……………………………………………....1 mg• Vitam<strong>in</strong> B 12 (cyanocobalam<strong>in</strong>)…………………. …….10 mcg• Days 21-28:Succ<strong>in</strong>ic acid (purple pill)………………….150 mgFerrochel® = iron bis glyc<strong>in</strong>ate chelate
Evaluat<strong>in</strong>g Efficacy of IronReplacement Therapy
Van Wyck DB, et al. Venofer Cl<strong>in</strong>ical Trials Group2005.Non-dialysis dependent adults with CKD given IV ironsucrose 1000mg <strong>in</strong> divided doses over 14 days vsFerrous sulfate 325mg TID x 14 days• IV iron group had 44.3% of patients achieve an <strong>in</strong>crease<strong>in</strong> Hgb ≥ 1 vs. 28% <strong>in</strong> the PO iron group• Mean Hgb was significantly higher <strong>in</strong> the IV vs. POgroup• Percent of patients report<strong>in</strong>g ADE’s same though 4cases of anaphylaxis <strong>in</strong> IV group
Agarwal R, et al. Am J Nephrol 2006.Non-dialysis dependent adults with CKD given sodiumferric gluconate 250mg IV x 4 doses over 22 days vs.oral ferrous sulfate 325mg TID x 42 days.• Use of ESA excluded• Increase <strong>in</strong> Hgb was significant with IV iron but not PO ironthough end po<strong>in</strong>ts for both were similar (mean 11.3 g/dL forIV vs. 10.9 g/dL)• IV iron <strong>in</strong>creased ferrit<strong>in</strong> and TSAT significantly vs. PO• IV iron had higher quality of life scores than PO
Bencaiova G, et al. Eur J Ob Gyn 2009.Pregnant women given iron sucrose 200mg IV x 3doses over 17 weeks vs oral ferrous sulfate 80mgdaily• No significant different between Hgb response between IVand PO group (80% vs. 75% with f<strong>in</strong>al Hgb ≥ 11g/dL• Goal ferrit<strong>in</strong> of ≥ 50 mcg/L reached by 49% of women <strong>in</strong> theIV group vs 14% <strong>in</strong> the PO group• 60% of the PO group experienced ADE’s vs. 30.8% <strong>in</strong> the IVgroup• Authors felt non-standard dose of PO iron may havecontributed to outcomes
Pieracci FM, et al. Surgical Infections2009.Adult SICU patients given ferrous sulfate 325mg TID +500mg Ascorbic Acid TID + Folic Acid 1mg daily + B121mg daily vs Placebo until discharge (≥ 5 days)• Excluded: chronic <strong>in</strong>flammatory disease, ESRD and unableto receive blood transfusions• Physician discretion was allowed regard<strong>in</strong>g <strong>in</strong>itiation oferythropoiet<strong>in</strong> therapy• Average treatment course: 19 days• No difference <strong>in</strong> f<strong>in</strong>al Hct, serum iron level, ferrit<strong>in</strong> level, eZPPconcentration and rate of <strong>in</strong>fection.• Treatment group required significantly less RBC transfusionsand less erythropoiet<strong>in</strong>
McClung JP, et al. Am J Cl<strong>in</strong> Nutr 2009.Female US Army soldiers given 8 weeks of 100 mgferrous sulfate PO daily vs placebo.• Serum ferrit<strong>in</strong> levels rose 87% <strong>in</strong> the treatment group vs. 66%<strong>in</strong> the placebo group.• Serum Hgb levels rose <strong>in</strong> the treatment vs. placebo groupthough were not significantly different between groups at theend of the study• Vigor and 2-mile run time improved <strong>in</strong> treatment group
<strong>Kovey</strong> KL, Kaaya BM, Baard J and Hassan N.2009.High dose oral iron (≥6 mg elem. Fe/kg/day) foriron deficiency anemia <strong>in</strong> children 2-8 yearsold <strong>in</strong> Namibia, Africa• Case series of 5 children treated with 6-10mg elementalFe/kg/day (ferrous fumerate or ferrous gluconate) + Vitam<strong>in</strong>C 200-400mg/day + Folic acid 5mg/day• Average <strong>in</strong>crease <strong>in</strong> Hgb of 4.2 g/dL at day 7-14 (average 9.8days). This was a average <strong>in</strong>crease of 100% over basel<strong>in</strong>e.• No reported side effects and no child had to stop treatment.
Hb Level<strong>Kovey</strong> KL, Kaaya BM, Baard J andHassan N. 2009.High Dose Iron Replacement Therapy <strong>in</strong> ChildrenCase 1: 6mg/kg x 7d; 10mg/kg/dCase 3: 10mg/kg/dCase5: 10mg/kg/dCase 7: 8mg/kg/dCase 2: 8mg/kg/dCase 4: 6mg/kg/dCase 6: 10mg/kg/d121086425.885.284.793.17.935.864.953.412.63.875.823.828.167.869.649.29.427.019.4411.100 2 4 6 8 10 12 14 16 18Days of Therapy
Adjuvants for Erythropoiesis• Folic Acid: absorbed <strong>in</strong> small <strong>in</strong>test<strong>in</strong>e, for nucleic acidsynthesis• Dos<strong>in</strong>g: Age10 years: 1-3mg daily• Cyanocobalam<strong>in</strong> (Vitam<strong>in</strong> B12): requires <strong>in</strong>tr<strong>in</strong>sic factorfrom stomach for absorption <strong>in</strong> the term<strong>in</strong>al ileum, fornucleic acid synthesis• Dos<strong>in</strong>g: Weight < 10kg: 100mcg IM monthlyWeight > 10kg: 200mcg IM monthly• Vitam<strong>in</strong> E: 25-50 IU orally daily, required for neonatalenteral iron supplementation to protect aga<strong>in</strong>st iron<strong>in</strong>ducedlipid oxidation
Adjuvants for Erythropoiesis• Ascorbic Acid (Vitam<strong>in</strong> C)• Prevents formation of <strong>in</strong>soluble iron complexes• Reduces iron to ferrrous state (Fe 2+ ) forabsorption• Dos<strong>in</strong>g Recommendation:• Children < 10kg: 250mg/day divided and given withiron• Children > 10kg: 500mg/day divided and given withiron
Summary
References1. Munoz M et al. World J Gastroenterol 2009;15:4617-26.2. Taketomo CK, et al. Pediatric Dosage Handbook 16 th ed. Lexi-Comp,Hudson, OH; 2009-20103. Product Information: Repliva 21/7 Tablets, Ther-Rx Corp. St. Louis, MO;03/10.4. McClung JP, et al. Am J Cl<strong>in</strong> Nutr 2009;90:124-31.5. Pieracci FM, et al. Surgical Infections 2009;10:9-19.6. Agarwal R, et al. Am J Nephrol 2006;26:445-54.7. Van Wyck DB, et al. Kidney International 2005;68:2646-56.8. Andrews NC. Disorders of iron metabolism. N Engl J Med1999;341(26):1986-95.9. Weiss G, et al. N Engl J Med 2005;325(10):1011-23.10. Ganz T. Blood 2003;102:783-88.