Overutilization of Antibiotics
Overutilization of Antibiotics
Overutilization of Antibiotics
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
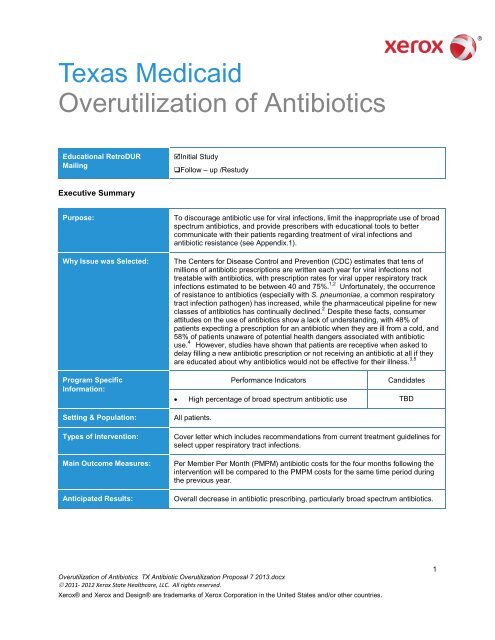
Texas Medicaid<strong>Overutilization</strong> <strong>of</strong> <strong>Antibiotics</strong>Educational RetroDURMailingInitial StudyFollow – up /RestudyExecutive SummaryPurpose:Why Issue was Selected:Program SpecificInformation:Setting & Population:Types <strong>of</strong> Intervention:Main Outcome Measures:Anticipated Results:To discourage antibiotic use for viral infections, limit the inappropriate use <strong>of</strong> broadspectrum antibiotics, and provide prescribers with educational tools to bettercommunicate with their patients regarding treatment <strong>of</strong> viral infections andantibiotic resistance (see Appendix.1).The Centers for Disease Control and Prevention (CDC) estimates that tens <strong>of</strong>millions <strong>of</strong> antibiotic prescriptions are written each year for viral infections nottreatable with antibiotics, with prescription rates for viral upper respiratory trackinfections estimated to be between 40 and 75%. 1,2 Unfortunately, the occurrence<strong>of</strong> resistance to antibiotics (especially with S. pneumoniae, a common respiratorytract infection pathogen) has increased, while the pharmaceutical pipeline for newclasses <strong>of</strong> antibiotics has continually declined. 2 Despite these facts, consumerattitudes on the use <strong>of</strong> antibiotics show a lack <strong>of</strong> understanding, with 48% <strong>of</strong>patients expecting a prescription for an antibiotic when they are ill from a cold, and58% <strong>of</strong> patients unaware <strong>of</strong> potential health dangers associated with antibioticuse. 4 However, studies have shown that patients are receptive when asked todelay filling a new antibiotic prescription or not receiving an antibiotic at all if theyare educated about why antibiotics would not be effective for their illness. 3,5Performance IndicatorsCandidates• High percentage <strong>of</strong> broad spectrum antibiotic use TBDAll patients.Cover letter which includes recommendations from current treatment guidelines forselect upper respiratory tract infections.Per Member Per Month (PMPM) antibiotic costs for the four months following theintervention will be compared to the PMPM costs for the same time period duringthe previous year.Overall decrease in antibiotic prescribing, particularly broad spectrum antibiotics.<strong>Overutilization</strong> <strong>of</strong> <strong>Antibiotics</strong> TX Antibiotic <strong>Overutilization</strong> Proposal 7 2013.docx© 2011- 2012 Xerox State Healthcare, LLC. All rights reserved.Xerox® and Xerox and Design® are trademarks <strong>of</strong> Xerox Corporation in the United States and/or other countries.1
Performance Indicator #1: High percentage <strong>of</strong> broad spectrum antibiotic useWhy has this indicator beenselected?The excessive use <strong>of</strong> antibiotics is related to the growing emergence <strong>of</strong> antibioticresistantbacteria. Provider education has been shown to be one component <strong>of</strong>decreasing the use <strong>of</strong> antibiotics in cases where they are not warranted.How will the patients beselected ?Candidates (denominator):Exception criteria(numerator):Patients receiving outpatient antibiotics in the past 365 days without a history <strong>of</strong>the following conditions in the past 2 years:• Asthma• Chronic obstructive pulmonary disease (COPD)• Chronic bronchitis• Heart failure• Renal failure• Diabetes mellitus• Immunocompromised patients (i.e., HIV+, cancer, history <strong>of</strong> organtransplantation)• TuberculosisPhysicians <strong>of</strong> candidates in the upper percentage <strong>of</strong> the plan for broad spectrumantibiotic use during the past 365 days. Infectious disease specialists areexcluded if specialist data is available.<strong>Overutilization</strong> <strong>of</strong> <strong>Antibiotics</strong> TX Antibiotic <strong>Overutilization</strong> Proposal 7 2013.docx© 2011- 2012 Xerox State Healthcare, LLC. All rights reserved.2
References1. CDC. Get Smart: Know when antibiotics work. Available at: http://www.cdc.gov/getsmart/index.html. Accessedon June 13, 2013.2. Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. CochraneDatabase <strong>of</strong> Systematic Reviews 2005, Issue 4. Art. No.: CD003539. DOI:101002/14561858. CD003539.pub2.3. Rybak MJ. Resistance to antimicrobial agents: an update. Pharmacotherapy 2004;24(12):203S-215S.4. Vaden JE, Marcus R, Hadler JL, et al. Consumer attitudes and use <strong>of</strong> antibiotics. Emerg Inf Dis Sept2003;9(9):1128-35.5. Pontes MC, Pontes NM. Debiasing effects <strong>of</strong> education about appropriate antibiotic use on consumers’preferences for physicians. Health Care Manage Rev Jan-Mar 2005;30(1):9-16.6. Snow V, Mottur-Pilson C, Gonzales R, et al. Principles <strong>of</strong> appropriate antibiotic use for treatment <strong>of</strong> nonspecificupper respiratory tract infections in adults. Ann Intern Med 2001;134:487-489.7. Wong DM, Blumberg DA, Lowe LG. Guidelines for the use <strong>of</strong> antibiotics in acute URTI. Am Fam Physician2006:74:956-69.8. CDC. Treatment guidelines for upper respiratory tract infections. Availableat: http://www.cdc.gov/getsmart/campaign-materials/treatment-guidelines.html Accessed on June 13, 2013.9. Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis inchildren and adults. Clin Infect Dis 2012;54(8):e72-e112. Available at:http://cid.oxfordjournals.org/content/early/2012/03/20/cid.cir1043.full. Accessed on June 13, 2013.10. Wald ER, Applegate KE, Bordley C, et al. Clinical practice guideline for the diagnosis and management <strong>of</strong> acutebacterial sinusitis in children aged 1 to 18 years. Pediatrics 2013;108(3):798-808. Availableat: http://pediatrics.aappublications.org/content/early/2013/06/19/peds.2013-1071. Accessed on June 25, 2013.11. Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management <strong>of</strong> groupA streptococcal pharyngitis: A 2012 update by the Infectious Disease Society <strong>of</strong> America. Clin Infect Dis2012;55(10):e86-e102. Available at: http://cid.oxfordjournals.org/content/early/2012/09/06/cid.cis629.fullAccessed on June 20, 2013.12. Snow V, Mottur-Pilson C, et al. Principles <strong>of</strong> appropriate antibiotic use for treatment <strong>of</strong> acute bronchitis. AnnIntern Med 2001;134:518-2.13. Braman SS. Chronic cough due to acute bronchitis. ACCP evidenced-based clinical practiceguidelines. Chest 2006;129;95S-103S.14. CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis <strong>of</strong>pertussis. MMWR 2005;54 (No. RR-14);1-16.15. Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management <strong>of</strong> acute otitismedia. Pediatrics 2013;131(3):e964-e999. Available at:http://pediatrics.aappublications.org/content/131/3/e964.full.pdf+html Accessed on June 25, 2013.<strong>Overutilization</strong> <strong>of</strong> <strong>Antibiotics</strong> TX Antibiotic <strong>Overutilization</strong> Proposal 7 2013.docx© 2011- 2012 Xerox State Healthcare, LLC. All rights reserved.3
AppendixesRecommendations to consider before prescribing antibiotics for your patients• Usually viral in origin with symptoms lasting 10-14 days, rarely associated withcomplications, and antibiotics <strong>of</strong>fer no benefit.Upper Respiratory• <strong>Antibiotics</strong> do not shorten the duration <strong>of</strong> illness or prevent complications.Tract Infections (URTI)(in general) 6-8 • Purulent nasal/throat secretions alone do not predict bacterial infection or benefit fromantibiotics.• Consider influenza and pneumococcal vaccines in high-risk patients.• Most ambulatory care cases are caused by uncomplicated viral URTIs.Acute BacterialRhinosinusitis 9,10(ABRS)Adult• Patients that may benefit from antibiotics include: persistent symptoms lasting > 7-10days without improvement; severe symptoms (i.e., high fever, purulent nasal dischargeor facial pain) lasting for at least 3-4 days at the beginning <strong>of</strong> an illness; OR onset <strong>of</strong> newfever, headache, or increase <strong>of</strong> worsening nasal discharge following a typical URTI thatwere initially improving.• Standard dose amoxicillin/clavulanate or either doxycycline or respiratory quinolone(lev<strong>of</strong>loxacin, moxifloxacin), if penicillin-allergic, are reasonable first-line agents inpatients with uncomplicated ABRS. Macrolides and trimethoprim/sulfamethoxazole areno longer recommended for empiric therapy based on high rates <strong>of</strong> resistance.• High dose amoxicillin/clavulanate (2 g orally twice daily) is recommended in certainpatients*Children• ABRS is likely when patients with a URTI present with: persistent illness (i.e., nasaldischarge <strong>of</strong> any quality and/or daytime cough) > 10 days without improvement;worsening or new onset <strong>of</strong> symptoms after initial improvement; OR severe symptomonset > 3 consecutive days (i.e., fever >102.2°F and purulent nasal discharge).• <strong>Antibiotics</strong> should be prescribed in patients with severe onset and worsening courseABRS, while antibiotics OR a 3-day additional observation can be <strong>of</strong>fered to children withpersistent illness.• Amoxicillin with or without clavulanate is recommended as first-line therapy. If penicillinallergic,cefdinir, cefuroxime, cepodoxime, a combination <strong>of</strong> clindamycin (or linezolid)and cefixime, or lev<strong>of</strong>loxacin can be used.• High dose amoxicillin clavulanate (90 mg/kg/d twice daily) is recommended in certainpatients** Patients from regions with high endemic rates <strong>of</strong> invasive penicillin non-susceptible S.pneumoniae, severe infection, attend daycare, aged < 2 or >65 years, have recenthospitalization or antibiotic exposure, or are immunocompromised.• <strong>Antibiotics</strong> should be given only to patients with Group A beta-hemolyticstreptococcal (GABHS) pharyngitis; only 5-15% <strong>of</strong> adult acute pharyngitis casesand 20-30% <strong>of</strong> pediatric cases are caused by GABHS.• Rapid antigen diagnostic testing and/or culture should be performed because <strong>of</strong>tenAcute Pharyngitis 11 clinical features alone do not reliably discriminate between GABHS and viral pharyngitis.Acute Bronchitis 8,12-14(Acute Cough Illness)• Penicillin or amoxicillin is preferred treatment. If penicillin-allergic, a first-generationcephalosporin (if not anaphylactically sensitive), clindamycin, clarithromycin, orazithromycin are recommended.• Analgesics, antipyretics, and supportive care should be <strong>of</strong>fered.• Most acute bronchitis cases (> 90%) are caused by viruses; antibiotics are notrecommended regardless <strong>of</strong> the duration <strong>of</strong> the cough.• If cough lasts > 3 weeks or the patient has fever, tachypnea, tachycardia, or evidence <strong>of</strong>consolidation on chest exam, consider chest radiography.• <strong>Antibiotics</strong> are indicated for suspected or confirmed pertussis; first line agents are<strong>Overutilization</strong> <strong>of</strong> <strong>Antibiotics</strong> TX Antibiotic <strong>Overutilization</strong> Proposal 7 2013.docx© 2011- 2012 Xerox State Healthcare, LLC. All rights reserved.4
macrolides or trimethoprim/sulfamethoxazole.Acute Otitis Media 15(AOM)• <strong>Antibiotics</strong> should be prescribed for AOM in children > 6 months with severesigns and symptoms (i.e., moderate to severe otalgia for at least 48hrs ortemperature >102.2°F) and for bilateral AOM in children < 24 months withoutsevere signs and symptoms.• Observation with close follow-up may be appropriate for patients with non-severe signsand symptoms and are 6 to 23 months with unilateral AOM or are > 24 months withunilateral or bilateral AOM.• High dose amoxicillin (80-90 mg/kg/day) is the first-line agent. High dose amoxicillin/clavulanate should be used if the patient received amoxicillin within the last 30 days, hasconcurrent conjunctivitis, or if coverage for a β-lactamase positive organism is needed.• If penicillin-allergic, cefdinir, cefpodoxime, cefuroxime or a macrolide may be used.• <strong>Antibiotics</strong> are not indicated for otitis media with effusion in the absence <strong>of</strong> clinicalsymptoms.• Prophylactic antibiotics should not be prescribed to reduce the risk <strong>of</strong> AOM in childrenwith recurrent AOM.<strong>Overutilization</strong> <strong>of</strong> <strong>Antibiotics</strong> TX Antibiotic <strong>Overutilization</strong> Proposal 7 2013.docx© 2011- 2012 Xerox State Healthcare, LLC. All rights reserved.5