Controlled Drugs Policy Clinical Policy CL060 - NHS County Durham
Controlled Drugs Policy Clinical Policy CL060 - NHS County Durham
Controlled Drugs Policy Clinical Policy CL060 - NHS County Durham
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
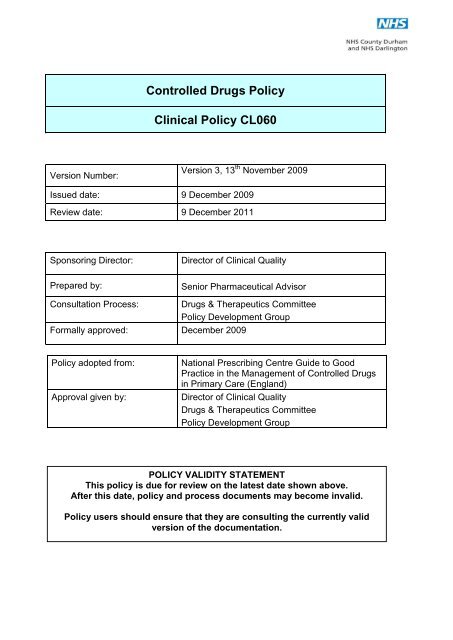
Version Number:<br />
<strong>Controlled</strong> <strong>Drugs</strong> <strong>Policy</strong><br />
<strong>Clinical</strong> <strong>Policy</strong> <strong>CL060</strong><br />
Version 3, 13 th November 2009<br />
Issued date: 9 December 2009<br />
Review date: 9 December 2011<br />
Sponsoring Director: Director of <strong>Clinical</strong> Quality<br />
Prepared by: Senior Pharmaceutical Advisor<br />
Consultation Process: <strong>Drugs</strong> & Therapeutics Committee<br />
<strong>Policy</strong> Development Group<br />
Formally approved: December 2009<br />
<strong>Policy</strong> adopted from: National Prescribing Centre Guide to Good<br />
Practice in the Management of <strong>Controlled</strong> <strong>Drugs</strong><br />
in Primary Care (England)<br />
Approval given by: Director of <strong>Clinical</strong> Quality<br />
<strong>Drugs</strong> & Therapeutics Committee<br />
<strong>Policy</strong> Development Group<br />
POLICY VALIDITY STATEMENT<br />
This policy is due for review on the latest date shown above.<br />
After this date, policy and process documents may become invalid.<br />
<strong>Policy</strong> users should ensure that they are consulting the currently valid<br />
version of the documentation.
Document Information<br />
Document Title: <strong>Controlled</strong> <strong>Drugs</strong> <strong>Policy</strong><br />
Initial Issue: Version 1: 13 March 2008<br />
Document history<br />
Version Date Significant Changes<br />
2 30 June 2009 <strong>Policy</strong> has been significantly re-drafted<br />
3 13 Nov 2009 Contact names, SOPs and Audits updated<br />
Equality impact assessments:<br />
Date Issues<br />
18 August 2009<br />
There are no specific equality and diversity issues which arise within this policy<br />
document.
<strong>Controlled</strong> <strong>Drugs</strong> <strong>Policy</strong><br />
Contents<br />
Section Title Page<br />
1<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
8<br />
9<br />
INTRODUCTION<br />
DEFINITIONS<br />
POLICY DETAIL<br />
DUTIES AND RESPONSIBILITIES<br />
IMPLEMENTATION<br />
TRAINING<br />
DOCUMENTATION<br />
MONITORING, REVIEW AND ARCHIVING<br />
IMPACT ASSESSMENTS<br />
Appendices to the <strong>Policy</strong><br />
1<br />
2<br />
3<br />
4<br />
5<br />
Relevant acts of parliament and regulations<br />
Accountable officer<br />
Monitoring and auditing the management and use of controlled<br />
drugs<br />
Possession of controlled drugs<br />
Purchasing and supply of controlled drugs<br />
6<br />
7<br />
7<br />
8<br />
9<br />
9<br />
9<br />
10<br />
11<br />
14<br />
18<br />
20<br />
24<br />
25<br />
2
6<br />
7<br />
8<br />
9<br />
10<br />
11<br />
12<br />
13<br />
14<br />
15<br />
16<br />
17<br />
18<br />
19<br />
20<br />
21<br />
22<br />
Preparation and administration of controlled drugs<br />
Prescribing of controlled drugs<br />
Prescribing in instalments<br />
Private prescriptions<br />
Prescriptions for prisoners and other agency agreements for <strong>NHS</strong><br />
services<br />
Storage of controlled drugs<br />
Dispensing of controlled drugs<br />
Recording of controlled drugs<br />
Transportation of controlled drugs<br />
Administration of controlled drugs<br />
Nurses working in the community<br />
Palliative care<br />
Self-medication<br />
Patients travelling overseas<br />
Destruction of controlled drugs 56<br />
Standard Operating Procedures 59<br />
Patient information<br />
28<br />
30<br />
35<br />
37<br />
39<br />
40<br />
43<br />
47<br />
50<br />
51<br />
52<br />
53<br />
54<br />
55<br />
60<br />
3
A<br />
B<br />
C<br />
D<br />
E<br />
F<br />
G<br />
H<br />
I<br />
J<br />
K<br />
L<br />
M<br />
N<br />
Appendices of Procedures<br />
List of <strong>Controlled</strong> <strong>Drugs</strong> and Their Schedules 61<br />
Summary of legal requirements of the possession and supply of<br />
<strong>Controlled</strong> <strong>Drugs</strong>.<br />
Relevant Contact Details regarding <strong>Controlled</strong> <strong>Drugs</strong><br />
Information Sharing Code in respect of the operation of the <strong>County</strong><br />
<strong>Durham</strong> and Darlington Local Intelligence Network for <strong>Controlled</strong><br />
<strong>Drugs</strong> governance<br />
<strong>Controlled</strong> <strong>Drugs</strong> Practice Declaration and Self Assessment Audit<br />
for GP Practices 2009/10<br />
<strong>Controlled</strong> Drug Personal Declaration and Self Assessment Audit<br />
for GP‘s 2009/10<br />
<strong>Controlled</strong> <strong>Drugs</strong> Practice Declaration and Self Assessment Audit<br />
for Dental Practices 2009/10<br />
<strong>Controlled</strong> Drug Personal Declaration and Self Assessment Audit<br />
for Dentist‘s 2009/10<br />
<strong>Controlled</strong> Drug : Practice Audit by PCT Pharmacist<br />
<strong>Controlled</strong> Drug : Personal Audit by PCT Pharmacist<br />
<strong>Controlled</strong> Drug : OOH/UCC/Dispensing Doctor Audit<br />
<strong>Controlled</strong> Drug : Community Hospital Audit<br />
<strong>Controlled</strong> Drug : Prison Audit<br />
Useful External Contacts<br />
62<br />
64<br />
66<br />
82<br />
92<br />
103<br />
113<br />
124<br />
133<br />
140<br />
148<br />
155<br />
172<br />
4
O<br />
P<br />
Q<br />
R<br />
S<br />
T<br />
Table of <strong>Controlled</strong> <strong>Drugs</strong> and Indications allowed to be prescribed<br />
by Nurse Independent Prescriber‘s<br />
Methods of Destruction of <strong>Controlled</strong> <strong>Drugs</strong><br />
Standard Operating Procedure for witnessing destruction of<br />
<strong>Controlled</strong> drugs by a delegated PCT Pharmacist<br />
<strong>Controlled</strong> Drug Destruction Record Form<br />
Summary of <strong>Controlled</strong> Drug guidance for GP‘s<br />
Guidance on Standard Operating Procedures<br />
176<br />
177<br />
180<br />
189<br />
190<br />
194<br />
5
1. Introduction<br />
<strong>Controlled</strong> <strong>Drugs</strong> <strong>Policy</strong><br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong> and <strong>NHS</strong> Darlington aspires to the highest standards of<br />
corporate behaviour and clinical competence, to ensure that safe, fair and equitable<br />
procedures are applied to all organisational transactions, including relationships<br />
with patients their carers, public, staff, stakeholders and the use of public resources.<br />
In order to provide clear and consistent guidance, <strong>NHS</strong> <strong>County</strong> <strong>Durham</strong> and <strong>NHS</strong><br />
Darlington will develop documents to fulfil all statutory, organisational and best<br />
practice requirements and support the principles of equal opportunity for all.<br />
This document gives guidance on the requirements of The Misuse of <strong>Drugs</strong> Act<br />
1971, the Misuse of <strong>Drugs</strong> Safe Custody Regulations 1973, and the<br />
recommendations resulting from the Fourth Report of the Shipman Inquiry and<br />
associated amendments to the Misuse of <strong>Drugs</strong> Regulations 2001.<br />
The Misuse of <strong>Drugs</strong> Act and Misuse of <strong>Drugs</strong> Regulations govern the<br />
circumstances under which controlled drugs (CDs) may be manufactured,<br />
possessed, supplied, imported and exported. Full details of the relevant legislation<br />
are in Appendix 1.<br />
1.1 Status<br />
This policy is a <strong>Clinical</strong> policy.<br />
1.2 Purpose and scope<br />
This document aims to<br />
� Develop good practice in the management of controlled drugs in primary care in line<br />
with current legislation.<br />
� Identify robust systems for obtaining, storing, supplying, recording, monitoring and<br />
safe disposal of CDs, whilst at the same time ensuring appropriate and convenient<br />
access for those patients that require them.<br />
This policy is applicable to Health Care Providers within Co <strong>Durham</strong> and Darlington<br />
PCT‘s, including independent contractors and directly managed services and staff<br />
where controlled drugs are handled, prescribed or used, including: -<br />
GP and Dental Practices<br />
Pharmacies<br />
Midwifery Services<br />
Out of Hours/ Urgent Care/Walk in Centre Services<br />
Patients own homes<br />
Care Homes<br />
Community Hospitals<br />
6
Community Nursing Services<br />
Community Palliative Care Services<br />
Substance Misuse Services<br />
Hospices<br />
Prison Services<br />
2. Definitions<br />
There are no specific definitions applicable to this policy<br />
3. General <strong>Policy</strong> Statement<br />
Co <strong>Durham</strong> and Darlington PCT‘s have an obligation to comply with legislation<br />
outlined in Appendix 1 and with the Health Care Commission Standards for Better<br />
Health: Core Standard : C4 D in that organisations keep patients, staff and visitors<br />
safe by having systems to ensure that medicines are handled safely.<br />
Each practice (GP, Dental etc), pharmacies, services and PCT directly managed<br />
services and staff, are required to have clear practice standard operating<br />
procedures (SOP‘s) covering issues relating to the prescribing, receipt, storage,<br />
supply, recording, monitoring, administration and disposal of controlled drugs.<br />
These SOPs should provide a full audit trail to track the movement of CDs in<br />
primary care from acquisition to administration.<br />
As designated bodies Co <strong>Durham</strong> and Darlington PCT‘s have a duty under the<br />
Health Act 2006 to : -<br />
Appoint an Accountable Officer and describe the duties and responsibilities of<br />
the officer to improve the safe management of CDs. The regulations specify who<br />
may be appointed as an Accountable Officer.<br />
Share intelligence on CD issues with other local and national agencies.<br />
Have the power of entry and inspection for the police and other nominated<br />
people to enter premises to inspect stocks and records of CDs.<br />
Specific procedures applicable to this policy are shown in Appendices 3-22<br />
The Care Quality Commission is responsible for overseeing the Regulation of the<br />
management of CDs by the PCT.<br />
7
4. Duties and Responsibilities<br />
Trust board:<br />
The Trust Board has overall responsibility within each Trust for setting the strategic<br />
context in which organisational process documents are developed, and for<br />
establishing a scheme of governance for the formal review and approval of such<br />
documents.<br />
Chief Executive<br />
The Chief Executive has overall responsibility for the strategic direction and<br />
operational management, including ensuring that Trust process documents comply<br />
with all legal, statutory and good practice guidance requirements.<br />
Director of <strong>Clinical</strong> Quality<br />
The director of clinical quality is the sponsoring director for this document and is<br />
responsible for ensuring that:<br />
The document is drafted, approved and disseminated in accordance with the<br />
<strong>Policy</strong> for the Development and Approval of Policies.<br />
The necessary training or education needs and methods required to<br />
implement this policy are identified and resourced or built into the delivery<br />
planning process.<br />
Mechanisms are in place for the regular evaluation of the implementation<br />
and effectiveness of this policy.<br />
<strong>Controlled</strong> <strong>Drugs</strong> Accountable Officer<br />
The duties of the Accountable Officer are shown in Appendix 2<br />
All staff<br />
All staff, including temporary and agency staff, are responsible for:<br />
Compliance with relevant process documents. Failure to comply may<br />
result in disciplinary action being taken.<br />
Co-operating with the development and implementation of policies and<br />
procedures and as part of their normal duties and responsibilities.<br />
Identifying the need for a change in policy or procedure as a result of<br />
becoming aware of changes in practice, changes to statutory requirements,<br />
revised professional or clinical standards and local/national directives, and<br />
advising their line manager accordingly.<br />
Identifying training needs in respect of policies and procedures and bringing<br />
them to the attention of their line manager.<br />
Attending training / awareness sessions when provided.<br />
8
5. Implementation<br />
This policy will be available to all Staff, in particular the staff listed in Section 1.2 of<br />
the policy for the circumstances described there.<br />
All directors and managers are responsible for ensuring that relevant staff within<br />
their own directorates and departments have read and understood this document<br />
and are competent to carry out their duties in accordance with the procedures<br />
described.<br />
It may be necessary to develop specific implementation plans.<br />
6. Training Implications<br />
The sponsoring director will ensure that the necessary training or education needs<br />
and methods required implementing the policy or procedure(s) are identified and<br />
resourced or built into the delivery planning process. This may include identification<br />
of external training providers or development of an internal training process.<br />
It has been determined that there are no specific training requirements associated<br />
with this policy/procedure.<br />
7. Documentation<br />
7.1 Other related policy documents.<br />
Safe and Secure Handling of Medicines (2008)<br />
7.2 Legislation and statutory requirements<br />
Misuse of <strong>Drugs</strong> Act 1971<br />
Misuse of Drug Regulations 2001 (2001 Regulations)<br />
Misuse of <strong>Drugs</strong> (Safe Custody) Regulations 1973<br />
Misuse of <strong>Drugs</strong> (Supply to Addicts) Regulations 1997<br />
Medicines Act 1968<br />
Health Act 2006<br />
Dangerous <strong>Drugs</strong>, England, Scotland: The <strong>Controlled</strong> <strong>Drugs</strong><br />
(Supervision of Management and Use) Regulations Health Act 2006<br />
7.3 Best practice recommendations<br />
National Prescribing Centre Guide to Good Practice in the Management of<br />
<strong>Controlled</strong> <strong>Drugs</strong> in Primary Care (England) 2 nd Edition February 2007<br />
9
7.4 References<br />
The major references consulted in preparing this document are described above.<br />
8. Monitoring, Review and Archiving<br />
Monitoring<br />
The director of clinical quality as sponsor director, will agree with the policy<br />
manager a method for monitoring the dissemination and implementation of this<br />
policy. Monitoring information will be recorded in the policy database.<br />
Review<br />
The sponsoring director will ensure that each policy document is reviewed in<br />
accordance with the timescale specified at the time of approval. No policy or<br />
procedure will remain operational for a period exceeding three years without<br />
a review taking place.<br />
Staff who become aware of changes in practice, changes to statutory requirements,<br />
revised professional or clinical standards and local/national directives that affect, or<br />
could potentially affect policy documents, should advise the sponsoring director as<br />
soon as possible, via line management arrangements. The sponsoring director will<br />
then consider the need to review the policy or procedure outside of the agreed<br />
timescale for revision.<br />
If the review results in changes to the document, then the initiator should inform the<br />
policy manager who will renew the approval and re-issue under the next ―version‖<br />
number. If, however, the review confirms that no changes are required, the title<br />
page should be renewed indicating the date of the review and date for the next<br />
review and the title page only should be re-issued.<br />
For ease of reference for reviewers or approval bodies, changes should be noted<br />
on the ―Document history‖ table on page 2 of this document.<br />
NB: If the review consists of a change to an appendix or procedure document,<br />
approval may be given by the sponsor director and a revised document may be<br />
issued. Review to the main body of the policy must always follow the original<br />
approval process.<br />
Archiving<br />
The <strong>Policy</strong> Manager will ensure that archived copies of superseded policy<br />
documents are retained in accordance with Records Management: <strong>NHS</strong> Code of<br />
Practice 2006.<br />
10
9 Audit / Impact Assessment Statements<br />
EQUALITY IMPACT ASSESSMENT FORM<br />
Please refer to the corporate checklist for further information.<br />
Name of function/strategy/policy/service: <strong>Controlled</strong> <strong>Drugs</strong> <strong>Policy</strong><br />
Date of Review: 18 August 2009<br />
a) Please provide a brief description of the function/strategy/policy/service:<br />
This document gives guidance on the requirements of The Misuse of <strong>Drugs</strong> Act<br />
1971, the Misuse of <strong>Drugs</strong> Safe Custody Regulations 1973, and the<br />
recommendations resulting from the Fourth Report of the Shipman Inquiry and<br />
associated amendments to the Misuse of <strong>Drugs</strong> Regulations 2001.<br />
The Misuse of <strong>Drugs</strong> Act and Misuse of <strong>Drugs</strong> Regulations govern the<br />
circumstances under which controlled drugs (CDs) may be manufactured,<br />
possessed, supplied, imported and exported.<br />
b) What Type of positive and negative equality & diversity implications are you<br />
aware of that arise from your function/strategy/policy/service?<br />
There are no specific equality and diversity issues which arise within this policy document.<br />
c) In line with our statutory duty under equality legislation do your<br />
functions/strategies/policies/services make reference to equality wherever relevant?<br />
In line with the Race Equality Duty to<br />
eliminate discrimination, harassment,<br />
promoting equality of opportunity and good<br />
relations between people of different racial<br />
groups<br />
In line with the Disability Equality Duty to<br />
promote positive attitudes towards<br />
disabled persons and encourage<br />
participation by disabled people<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong> aspires to the highest<br />
standards of corporate behaviour and clinical<br />
competence, to ensure that safe, fair and<br />
equitable procedures are applied to all<br />
organisational transactions, including relationships<br />
with patients their carers, public, staff,<br />
stakeholders and the use of public resources. In<br />
order to provide clear and consistent guidance,<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong> will develop documents to<br />
fulfil all statutory, organisational and best practice<br />
requirements and support the principles of equal<br />
opportunity for all.<br />
Applied equally to all employees<br />
11
In line with the Gender Equality Duty to<br />
eliminate unlawful discrimination and<br />
harassment & promote equality of<br />
opportunity between men and women<br />
Other relevant equality legislation/best<br />
practice?<br />
Applied equally to all employees<br />
d) What relevant groups have a legitimate interest in the<br />
function/strategy/policy/service?<br />
Does it impact differently on particular minority groups?<br />
If Yes – Which Groups are affected, and how are they affected?<br />
Group Impact<br />
All Trust<br />
employees<br />
This policy is appropriate and applicable to those staff identified in Section<br />
1.2.<br />
e) Please outline below any work you have carried out to assess, monitor, address and review<br />
the equality implications of your function/strategy/policy/service and identify additional work<br />
that needs to be carried out to meet requirements of our statutory duties.<br />
Area of Work<br />
Consultation<br />
Monitoring & Target<br />
Setting<br />
Access to<br />
Information/Services<br />
Marketing &<br />
promotion<br />
Work already<br />
carried out /<br />
Measures in Place<br />
<strong>Drugs</strong> &<br />
Therapeutics<br />
Committee<br />
Work Required Timescales<br />
Management Group<br />
to approve<br />
Review June 2011<br />
Available to staff via<br />
the Intranet and hard<br />
copy of policy.<br />
Signpost access to<br />
services and support.<br />
All staff informed of<br />
approval and<br />
publication of the<br />
policy.<br />
June 2011<br />
Following approval<br />
Following approval<br />
12
Training/Briefing<br />
staff<br />
Employment Issues<br />
Review and<br />
Evaluation<br />
N/A<br />
Review June 2011<br />
June 2011<br />
WHERE APPROPRIATE, ACTIONS AND TARGETS DESCRIBED HERE SHOULD BE<br />
EVIDENT IN SERVICE AREA PLANS<br />
13
RELEVANT ACTS OF PARLIAMENT AND REGULATIONS<br />
1.1 Misuse of <strong>Drugs</strong> Act 1971<br />
Appendix 1<br />
The Act establishes a series of criminal offences for the unauthorised use, possession,<br />
supply, importation and unlawful production of drugs considered ‗dangerous or<br />
otherwise harmful‘, with potential for diversion and misuse.<br />
<strong>Drugs</strong> controlled under this act are divided into 3 classes – A, B & C in order to<br />
determine the penalties for offences committed under the act. The class of drug<br />
reflects its relative harm when misused. The maximum penalties for offences of<br />
possession and supply of the main CDs within each class are outlined in the table<br />
below.<br />
Drug Class Penalties for Penalties for<br />
Class A<br />
possession supply<br />
Diamorphine (heroin), Cocaine (Crack), Up to seven years Up to life<br />
MDA (Ecstasy, lysergic acid diethylamide imprisonment or an imprisonment or an<br />
(LSD), methamphetamine, cocaine, more unlimited fine or unlimited fine or<br />
potent opioid analgesics e.g. methadone both<br />
both<br />
Class B<br />
Up to five years Up to 14 years<br />
Amphetamine, barbiturates, Cannabis *, less imprisonment or an imprisonment or an<br />
potent opioids e.g. codeine<br />
unlimited fine or unlimited fine or<br />
both<br />
both<br />
Class C<br />
Up to two years Up to 14 years<br />
Benzodiazepines (and zolpidem), ketamine, imprisonment or an imprisonment or an<br />
anabolic steroids and gamma-<br />
unlimited fine or unlimited fine or<br />
hydroxybutyrate (GBH)<br />
both<br />
both<br />
NB: Any class B drug in an injectable form is treated as Class A.<br />
* The Advisory Council on the Misuse of <strong>Drugs</strong> reviews and advises Ministers in<br />
the United Kingdom on measures that deal with social problems caused by drug<br />
misuse. Therefore the above summary may change, for up to date and detailed<br />
information contact The Home Office.<br />
1.2 Misuse of Drug Regulations 2001 (2001 Regulations)<br />
These regulations<br />
Authorise and govern certain activities which would otherwise be illegal under<br />
the Misuse of <strong>Drugs</strong> Act.<br />
Identify those Health Care Professionals who may legitimately posses and<br />
supply CDs.<br />
Establish a regime of control around prescribing, administration, safe custody,<br />
dispensing, record keeping and destruction or disposal.<br />
The 2001 regulations divide CDs into 5 schedules, which dictate the degree to<br />
which a CDs use is regulated, which in turn depends upon the therapeutic<br />
benefit versus harm when misused.<br />
Schedule 1 CDs are subject to the highest level of control whereas Schedule 5<br />
CDs are subject to a much lower level of control.<br />
Regulations are subject to amendments: full details are available from the Home<br />
Office and the Office of Public Sector information website. www.opsi.gov.uk
1.2.1 Schedule 1 (CD Licence)<br />
These drugs have no recognised medicinal use, although Sativex® (a cannabis based<br />
product) can be supplied on a named patient basis under Home Office Licence.<br />
Examples: cannabis, coca leaf, mescaline, ecstasy, hallucinogens (e.g. LSD) and raw<br />
opium.<br />
Only certain people licensed by the Home Office may possess Sch 1 drugs for<br />
research or other special purposes Practitioners and pharmacists may not lawfully<br />
possess Sch 1 drugs except under licence from the home office.<br />
1.2.3 Schedule 2 (CD)<br />
Includes more than 100 drugs such as the opiates, the major stimulants, secobarbital<br />
and amphetamine.<br />
Sch 2 CDs (except quinalbarbitone) are subject to safe custody requirements (under<br />
the Misuse of <strong>Drugs</strong> Safe Custody Regulations 1973).They must be stored in a locked<br />
receptacle, such as an appropriate CD cabinet or approved safe, which can be opened<br />
by the person in lawful possession of the CD or a person authorised by them.<br />
Quinalbarbitone is exempt from safe custody requirements but is it considered good<br />
practice to store with other CDs.<br />
A licence is required to import and export drugs in Sch 2. They may be manufactured<br />
or compounded by a licence holder, a practitioner, a pharmacist or a person lawfully<br />
conducting a retail pharmacy business acting in their capacity as such.<br />
A pharmacist may only supply Sch 2 CDs to a patient only on the authority of a<br />
prescription in the required form issued by an appropriate prescriber.<br />
A pharmacist may only supply Sch 2 CDs for the purpose of stock in primary care on<br />
the authority of a requisition in the required form issued by an appropriate person.<br />
SCH2 CDs may be administered to a patient by a doctor or dentist or by any person<br />
acting in accordance with the directions of an appropriately qualified prescriber.<br />
Nurse independent prescriber‘s are permitted to prescribe, administer or direct anyone<br />
to administer some CDS for specific conditions and routes of administration. Full<br />
details are given at www.doh.gov.uk/nonmedicalprescribing<br />
A CD register must be kept for Sch 2 CDs and this must comply with the requirements<br />
of the 2001 regulations.<br />
The destruction of Sch 2 CDs stock must only take place in the presence of an<br />
appropriately authorised person. Patient returns do not currently have to be witnessed<br />
but good practice would deem that another person should witness their destruction.<br />
1.2.4 Schedule 3 (CD No Register)<br />
Sch 3 includes a small number of minor stimulant drugs and others which are less<br />
likely to be misused than Sch 2.<br />
The majority of Sch 3 drugs are exempt from safe custody requirements. Exceptions<br />
are: Flunitrazepam, Temazepam, Buprenorphine, Diethylpropion, which must be<br />
stored in a locked receptacle, such as an appropriate CD cabinet or approved safe,<br />
which can be opened by the person in lawful possession of the CD or a person<br />
authorised by them.<br />
A pharmacist may only supply Sch 3 CDs for the purpose of stock in primary care on<br />
the authority of a requisition in the required form issued by an appropriate person.<br />
Page 15 of 196
Certain prescription requirements apply.<br />
There is no legal requirement to record transactions of Sch 3 CDs in a CD register<br />
The requirements for destruction do not apply unless the CDs are manufactured by the<br />
individual.<br />
Sch 3 drugs are subject to full import and export control.<br />
1.2.5 Schedule 4 (CD Benzodiazepines and CD Anabolic steroids)<br />
Sch 4 is split into 2 parts<br />
Part 1 (CD Benzodiazepines) contains most of the benzodiazepines, plus eight<br />
other substances including zolpidem, fencamfamin and mesocarb.<br />
Part 2 (CD Anabolic steroids) contains most of the anabolic and androgenic<br />
steroids such as testosterone, together with clenbuterol and growth hormones.<br />
There is no restriction on the possession of a Sch 4 Part 2 (CD Anabolic<br />
steroids) drug when it is in the form of a medicinal product.<br />
Possession of a drug from Sch 4 Part 1 (CD Benzodiazepines) is an offence without<br />
the authority of a prescription in the required form. Possession, by practitioners and<br />
pharmacists acting in their professional capacities, is authorised.<br />
<strong>Drugs</strong> in Part 1 (CD Benzodiazepines) are subject to full import and export control and<br />
a Home Office licence is also required for importation and exportation of Part 2<br />
Anabolic Steroids unless the substance is in the form of a medicinal product and is for<br />
personal use/ administration.<br />
All substances from Sch 4 are exempt from safe custody requirements with destruction<br />
only applying to importers, exporters and manufacturers.<br />
Prescription-writing requirements set out in the 2001 Regulations for these CDs do not<br />
apply, except those requirements laid down in the Medicines Act 1968.<br />
CD registers do not need to be kept for Sch 4 drugs, although records should be kept if<br />
such CDs are compounded.<br />
1.2.6 Schedule 5 (CD Invoice)<br />
Schedule 5 contains preparations of certain CDs e.g. codeine, pholcodine, morphine,<br />
which are exempt from full control when present in medicinal products of low strength,<br />
as their risk of misuse is reduced.<br />
There is no restriction on the import, export, possession, administration or destruction<br />
of these preparations and safe custody Regulations do not apply.<br />
The Misuse of <strong>Drugs</strong> Regulations have been amended so that preparations containing<br />
more than 0.1% cocaine are no longer exempt from prohibitions on import, export and<br />
possession.<br />
A practitioner or pharmacist acting in his capacity as such, or a person holding an<br />
appropriate licence, may manufacture or compound any CD in schedule 5.<br />
Appendix A contains a list of the most commonly used controlled drugs and their<br />
Schedules.<br />
Appendix B contains a summary of the legal requirements, possession and supply.<br />
Page 16 of 196
1.3 Misuse of <strong>Drugs</strong> (Safe Custody) Regulations 1973<br />
These regulations impose controls on the storage of CDs. The degree of control<br />
depends on the premises where the drugs are stored.<br />
All Schedule 2 and some Schedule 3 CDs should be stored securely in accordance<br />
with the safe custody regulations. These regulations state that such CDs must be<br />
stored in a cabinet or safe, locked with a key. It should be made from metal, with<br />
suitable hinges and fixed to a wall or floor with rag bolts that are not accessible from<br />
outside the cabinet.<br />
1.4 Misuse of <strong>Drugs</strong> (Supply to Addicts) Regulations 1997<br />
These regulations prohibit doctors from prescribing, administering or supplying<br />
diamorphine, cocaine or dipipanone for the treatment of addiction or suspected<br />
addiction except under a Home Office Licence. A licence is not required with such<br />
drugs for the treatment of organic disease or injury.<br />
1.5 Medicines Act 1968<br />
This Act sets out the requirements for a valid prescription. It also allows Midwives to<br />
possess and administer diamorphine, morphine, pethidine or pentazocine.<br />
A number of Health Care Professionals are permitted to supply or administer<br />
medicines in accordance with a patient group direction under medicines act legislation.<br />
Some of these professional groups, but not all, are permitted to supply or administer<br />
CDs in accordance with a PGD under Misuse of <strong>Drugs</strong> legislation.<br />
1.6 Health Act 2006<br />
See section 2.2<br />
1.7 Dangerous <strong>Drugs</strong>, England, Scotland: The <strong>Controlled</strong> <strong>Drugs</strong><br />
(Supervision of Management and Use) Regulations 2006 Health Act 2006<br />
These regulations set out the requirements for certain <strong>NHS</strong> bodies and independent<br />
health care bodies to appoint an Accountable Officer and describe the duties and<br />
responsibilities of Accountable Officers to improve the safe management and use of<br />
CDs.<br />
The regulation requires specific bodies to co-operate with each other, including with<br />
regard to sharing of information, about concerns about the use and management of<br />
CDs, and set out arrangements relating to powers of entry and inspection.<br />
Page 17 of 196
ACCOUNTABLE OFFICER<br />
Page 18 of 196<br />
Appendix 2<br />
2.1 Appointment of Accountable Officer<br />
As designated bodies, Co <strong>Durham</strong> <strong>NHS</strong> and Darlington <strong>NHS</strong> have a duty to appoint an<br />
Accountable Officer. The Health Act 2006 specifies who may be appointed as an<br />
Accountable Officer.<br />
The Accountable Officer cannot be a person who routinely supplies, administers or<br />
disposes <strong>Controlled</strong> <strong>Drugs</strong> as part of their duties.<br />
The PCT must notify the Head of Operations at the Care Quality Commission of the<br />
nomination or appointment of their Accountable Officer, and also the removal or<br />
change of an Accountable Officer.<br />
These notifications can be made via the Accountable Officer notification form available<br />
via the Care Quality Commission Website.<br />
www.cqc.org.uk/guidanceforprofessionals/healthcare/allhealthcarestaff/managingrisk/c<br />
ontrolleddrugs/accountabl/accountableofficernotificationform.cfm<br />
The Care Quality Commission is required to publish a list of Accountable Officers in<br />
England and an up to date list is available via their website.<br />
Contact details for Co <strong>Durham</strong> <strong>NHS</strong> and Darlington <strong>NHS</strong> Accountable Officer see<br />
Appendix C<br />
2.2 Roles and Responsibilities of the Accountable Officer<br />
The Accountable Officer is responsible for ensuring the safe and effective use and<br />
management of controlled drugs within Co <strong>Durham</strong> and Darlington PCT.<br />
The Accountable Officer must have regard to best practice in relation to the<br />
management of controlled drugs;-<br />
Secure the safe management and use of CDs in particular<br />
Establish and ensure appropriate arrangements to comply with Misuse of <strong>Drugs</strong><br />
Legislation.<br />
Ensure adequate and up to date Standard Operating Procedures are in place in<br />
relation to the management of CDs.<br />
Ensure adequate destruction and disposal arrangements for CDs<br />
Ensure monitoring and auditing of the management and use of CDs<br />
Ensure relevant individuals receive appropriate training<br />
Maintain a record of concerns regarding relevant individuals<br />
Assess and investigate concerns<br />
To take appropriate action if there are well founded concerns<br />
To establish arrangements for sharing information<br />
The PCT Accountable Officer has the authority to inspect CD registers, premises and<br />
general drug control procedures in practices and nominate certain designated PCT<br />
personnel to facilitate this or perform inspection on their behalf.<br />
The PCT Accountable Officer is responsible for arranging periodic inspections of<br />
premises which are used in connection with controlled drugs and are not subject to
inspection by the Care Quality Commission or the Royal Pharmaceutical Society<br />
Inspectors (RPSGB). Advanced notification of the inspection does not have to be<br />
provided.<br />
2.3 Local Intelligence Network<br />
Local Agencies required by legislation to share information include: Health Care<br />
organisations, the police, social services and relevant inspectorates, Care Quality<br />
Commission and RPSGB.<br />
Responsibility for establishing the Local Intelligence Network lies with the PCT<br />
Accountable Officer. The network will enable agencies that have cause for concern<br />
about the activities of any Healthcare professional to share them as soon as possible<br />
with other local agencies who may be affected or who may have complimentary<br />
information.<br />
Full details can be found in the Information Sharing Code for <strong>Durham</strong> and Darlington<br />
Local Intelligence Network. Appendix D<br />
Page 19 of 196
Page 20 of 196<br />
Appendix 3<br />
MONITORING AND AUDITING THE MANAGEMENT AND USE OF CONTROLLED<br />
DRUGS<br />
3.1 <strong>Controlled</strong> drugs declaration statement and self assessment<br />
All organisations providing clinical services are required to complete a declaration (at<br />
least every two years) on whether or not their organisation keeps stocks of CDs.<br />
Those that do hold stocks of CDs will be required to complete a self assessment of<br />
their management of CDs.<br />
The self assessment will inform other monitoring and inspection activities.<br />
A declaration and self assessment questionnaire will be sent by the PCT Medicines<br />
Management Team to GPs on Co <strong>Durham</strong> and Darlington performers list, registered<br />
dentists on Co <strong>Durham</strong> and Darlington performers lists and PCT /CHS services.<br />
Appendix E, F, G, H for details of the forms.<br />
The forms should be returned to Co <strong>Durham</strong> and Darlington PCT Medicines<br />
Management Team.<br />
Co <strong>Durham</strong> and Darlington PCTs will be required to complete the Health Care<br />
Commission Annual Health Check Core Standards Assessment.<br />
3.2 Routine Inspections<br />
Inspection remains a useful tool to check physical arrangements for the storage,<br />
record keeping and management of CDs, to support individual and organisational<br />
development and to identify and investigate concerns.<br />
The Health Act has created power of entry and inspection for the police and other<br />
nominated people to enter premises to inspect stocks and records of CDs. See table<br />
below<br />
The PCT Accountable Officer is responsible for authorising PCT personnel, as a<br />
nominated person, to carry out these duties on his behalf, completing the PCT Audit<br />
Tool. See Appendix I, J, K, L and M.<br />
This delegation excludes premises subject to inspection by the Care Quality<br />
Commission or the Royal Pharmaceutical Society Inspectors (RPharmSGB).<br />
The PCT inspecting body is the Care Quality Commission, however, routine<br />
inspections of PCT /CHS services will also be performed by authorised PCT staff in<br />
order to support development and identify concerns.<br />
3.3 Inspection Responsibilities<br />
Area Inspecting Body<br />
GP Practices<br />
PCTs. Inspection will be announced and<br />
<strong>NHS</strong> dentists<br />
may be combined with other visits.<br />
Community Pharmacies The Royal Pharmaceutical Society<br />
PCTs Care Quality Commission
PCT Prisons<br />
PCT Community Hospitals<br />
PCT Services/clinics etc.<br />
PCT<br />
PCT<br />
PCT<br />
<strong>NHS</strong> Trusts Care Quality Commission<br />
Independent Healthcare sector<br />
including GPs in private practice<br />
Care Quality Commission<br />
Care Homes Care Quality Commission<br />
3.3.1 Standards for Inspection<br />
A small number of routine inspections of a random sample (about 10%) must be<br />
performed on an annual basis. The Head of Medicines Management or the<br />
Accountable Officer for the PCT will determine the number and frequency of routine<br />
monitoring visits.<br />
Routine inspections will be performed by designated PCT pharmacists. Pharmacists<br />
who perform monitoring must not do so in practices or services where they work or are<br />
registered as a patient.<br />
To ensure consistency common guidelines will be followed: -<br />
<strong>Controlled</strong> drugs: Monitoring and inspection guidelines - Core activities for CD<br />
monitoring and inspection work - Primary care : Department of Health - Publications<br />
Inspections will comply with the ten principles of inspection set out in the government‘s<br />
policy on Inspection of Public Services.<br />
http://archive.cabinetoffice.gov.uk/opsr/documents/pdf/policy.pdf<br />
Those involved in monitoring and inspection are required to complete the mandatory<br />
PCT training and the National Prescribing Centre competency framework.<br />
http://www.npc.co.uk/pdf/CDI_Competency_Framework.pdf<br />
Notification will be given prior to a routine inspection. Unannounced inspections may<br />
only be carried out under specific directions from the Accountable Officer.<br />
3.4 Monitoring <strong>Controlled</strong> Drug Prescribing and Requisitions<br />
The PCT Medicines Management team will monitor <strong>NHS</strong> and private prescribing and<br />
requisitions of Schedule2 and 3 controlled drugs via ePACT data on a quarterly basis.<br />
These reports will inform other monitoring and inspection activities to determine<br />
whether any further action is needed. Currently there is no facility to monitor <strong>NHS</strong><br />
dentist prescribing by this method.<br />
ePACT data is available for a rolling 60-month historical period only therefore local<br />
historical data will be archived and stored securely and via designated spread sheets,<br />
as this information may be required as evidence by other bodies.<br />
The PCT Pharmaceutical Advisers will use the reports generated to:<br />
Identify GP practices, private practice, non medical prescriber‘s and services,<br />
with a higher than average cost or frequency of CD prescribing/requisitions<br />
compared with the PCT average.<br />
Prescribing/ordering of excessive quantities.<br />
Prescribing for drug addicts<br />
Identify where prescriptions/ requisitions were dispensed or supplied from.<br />
Page 21 of 196
This will enable monitoring of prescribing and ordering patterns to determine<br />
specific medicines and quantities prescribed.<br />
These techniques do not detect inappropriate, fraudulent or criminal behaviour or<br />
identify individual patients; it identifies prescriber‘s/services with unusual<br />
prescribing/requisition patterns for these drugs.<br />
When unusual and/or excessive prescribing or ordering is identified from these reports<br />
the PCT Pharmaceutical Advisers may contact the prescriber or service lead. The<br />
prescriber or service lead may use this information to identify patients receiving<br />
unusual or excessive quantities and take action or identify a legitimate reason or raise<br />
concerns. Where a legitimate reason is identified the advisers should be informed so<br />
this can be logged onto the database.<br />
If anomalies or abnormal prescribing patterns are picked up and no legitimate reason<br />
is identified, the PCT Pharmaceutical Advisers will seek guidance and expert help via<br />
the <strong>Clinical</strong> Governance Leads and the Accountable Officer will be notified.<br />
If concerns are raised about controlled drugs, by any Healthcare Professional, from the<br />
ePACT data, these should be reported. There are a number of mechanisms for this –<br />
See Reporting concerns section 13.6<br />
3.5 Information Sharing<br />
In sharing information the PCT will have regard to the Data Protection Act 1998 and<br />
the codes of practice on confidentiality, in particular the Caldecott principles.<br />
The Local Intelligence Network code of conduct on information sharing will be followed.<br />
Wherever possible, information will be anonymous. In exceptional circumstances the<br />
PCT may determine that it is in the public interest to share patient/ practitioner<br />
identifiable information or that they are required to do so by statute. The patients/<br />
practitioners consent should be sought or they should be notified of the disclosure<br />
unless such action would prejudice an investigation.<br />
3.6 Reporting Concerns<br />
In addition to concerns arising from routine monitoring and inspection, concerns may<br />
be raised by individuals.<br />
The Public Interest Disclosure Act 1998 protects employees who are worried about<br />
wrongdoing in their place of work and want to raise concerns,<br />
The Act applies to all <strong>NHS</strong> employees and includes all self-employed <strong>NHS</strong><br />
Professionals (i.e. doctors, dentists, opticians, optometrists, and pharmacists).<br />
For the purpose of the Act, the employer of a self employed <strong>NHS</strong> Professional is<br />
deemed to be the relevant PCT or Strategic Health Authority.<br />
Other relevant policies are the<br />
PCT Whistleblower <strong>Policy</strong><br />
PCT Incidents Reporting <strong>Policy</strong><br />
Concerns may be raised by following the above policies or reporting direct to any of<br />
the relevant personnel or regulatory authorities listed in Appendix C and N.<br />
Page 22 of 196
3.7 <strong>Controlled</strong> Drug Review<br />
Information from declaration and self assessment, routine monitoring and other<br />
sources will be reviewed to decide whether any further action is needed<br />
The review will assess the organisation/practitioners clinical standards in the<br />
prescribing, supply, administration, storage, record keeping and disposal of CDs and<br />
assure compliance with the Misuse of <strong>Drugs</strong> Act 2001 and associated Regulations,<br />
medicines legislation and any relevant professional codes of practice.<br />
Page 23 of 196
POSSESSION OF CONTROLLED DRUGS<br />
Page 24 of 196<br />
Appendix 4<br />
Unlawful possession of any CD in Schedule 2 to 4 (part1) is a criminal offence.<br />
Persons who can legally possess CDs include:-<br />
Medical Practitioners (this includes doctors and dentists)<br />
Pharmacists or a person lawfully conducting a retail pharmacy business<br />
Supplementary Prescriber‘s where CDs form part of a clinical management plan<br />
Nurse Independent prescriber‘s, but restricted to specific CDs for specific<br />
indications<br />
Any person administering under the directions of a doctor or dentist<br />
Midwives acting in their capacity as such (restrictions apply)<br />
Paramedics acting in their capacity as such (restrictions apply)<br />
Health Professionals supplying or administering CDs under a PGD (restrictions<br />
apply)<br />
Persons in charge of a hospital or care home with nursing<br />
Someone who is transferring, with permission, a CD to another person who is<br />
lawfully allowed to have it in their possession. This permission may be granted<br />
by the person authorised to possess and should be in writing<br />
Someone who has legally been prescribed a CD<br />
Someone who has found a CD and is immediately taking it to a person who may<br />
lawfully possess it. E.g. a pharmacist for a medicinal product, a police officer for<br />
illicit drugs<br />
Someone who has removed a CD from someone else to stop them offending<br />
and is immediately taking it to a person who may lawfully possess it.<br />
Other categories (not applicable to primary care) are allowed, for full details refer to the<br />
Misuse of <strong>Drugs</strong> Act.
PURCHASING AND SUPPLY OF CONTROLLED DRUGS<br />
Page 25 of 196<br />
Appendix 5<br />
A requisition is required for purchase of Schedule 2 and 3 controlled drugs.<br />
The requisition must contain the following information<br />
Name and address and profession or occupation of the recipient<br />
Purpose for which drug supplied<br />
Name form and strength of the drug and quantity to be supplied<br />
Date on which supplied<br />
Faxed or other electronically transmitted requisitions are not currently permitted.<br />
Invoices should be retained for a minimum of two years. It is good practice to keep<br />
records for longer as any investigations take longer than 2 years.<br />
5.1 Supply from community pharmacy (FP10CDF forms)<br />
<strong>Controlled</strong> drugs ordered from a community pharmacy should be made using the<br />
dedicated CD Requisition Form (FP10CDF).<br />
FP10CDF forms are available from the service which supplies other controlled<br />
stationary e.g. prescription forms.<br />
PCT shared services office which supplies other controlled stationery (i.e.FP10).<br />
Contact: -<br />
The Office Services Manager<br />
John Snow House<br />
Telephone 0191 3011300<br />
Independent Hospitals, Out of Hours, Community Hospitals etc will be provided with an<br />
organisation code and/or a practice code for the purpose of ordering controlled drugs<br />
from a community pharmacy. Please contact the PCT Medicines Management Team<br />
for more details.<br />
FP10CD forms are controlled stationery, with unique numbers, and should be stored<br />
securely with access limited to authorised personnel. The minimum number of forms<br />
should be held (i.e. 1 form per GP at any one time).To order controlled drugs all fields<br />
of the form Part B to D should be completed. The person ordering the CDs should sign<br />
the requisition by hand, all other parts of the form may be printed or completed by<br />
another designated person.<br />
If a messenger is sent to collect the CD they must carry a bearer‘s note, signed and<br />
dated by the prescriber, stating that they are authorised to collect the CD. The<br />
pharmacy may retain the bearers note for a minimum of 2 years.<br />
Dispensing Doctors should not supply controlled drugs ordered on a requisition as they<br />
are not permitted to carry out a wholesale function unless they have a wholesalers<br />
licence.<br />
Pharmacies who supply the CD must record their name and address on the forms and<br />
submit these to the Prescription Pricing Division (PPD) of the <strong>NHS</strong> Business Services<br />
Authority (BSA).<br />
5.2 Supply of controlled drugs from a wholesaler or <strong>NHS</strong> Hospital Trust<br />
Supply of controlled drugs from a wholesaler or <strong>NHS</strong> Trust should be made via a<br />
written requisition, containing all the details as per the FP10CDF.<br />
Pharmacists and doctors may order controlled drugs, for their dispensary,<br />
electronically from wholesalers; however, doctors must provide a written requisition on
eceipt of the controlled drugs. Pharmacists do not need to issue a signed order when<br />
purchasing from a pharmaceutical wholesaler, however, this does not apply to support<br />
pharmacist prescriber function.<br />
5.3 GP Practices<br />
Previous recommendations were that the practice holds a central stock under the care<br />
of a designated person for distribution to individual GP for their bags.<br />
The introduction of designated controlled drug requisition forms in 2008 and the<br />
subsequent monitoring of these now make this recommendation obsolete.<br />
GP practices who wish to continue to hold a central stock of CDs should ensure a full<br />
auditable trail is available from ordering to administration and overseen by a<br />
designated member of staff.<br />
The FP10CDF requisition to replenish bags or stock should be completed by the<br />
doctor who requires the stock for their bag.<br />
There is a distinction between supplies of CDs prescribed for individual patients on a<br />
prescription and those obtained by practitioners for stock or bags for home visits etc.<br />
Medicines prescribed for an individual patient must be supplied to, and used by, that<br />
patient only.<br />
Practitioners must NOT use patient specific CD prescriptions to replace or top up their<br />
bags for home visits, etc, or practice stock, even if the stock was used for that patient<br />
initially. This could be considered as a potential offence under the Theft Act 1968 and<br />
might be seen as a means of obtaining CDs by deception.<br />
GPs can claim the cost of injectable controlled drugs, purchased by the practice, which<br />
have been administered to patients. To do this the GP should generate an FP10 and<br />
submit this to the Prescription Pricing Division (PPD) of the <strong>NHS</strong> Business Services<br />
Authority (BSA) at the end of the month along with other personally administered<br />
claims on form FP34D or FP34PD for dispensing doctors. For more information<br />
contact the PPD on 0845 6101171.<br />
5.4 Urgent Supplies (GPs)<br />
A practitioner who requires a Sch 2 or 3 CD urgently and who is unable to supply a<br />
signed requisition (FP10CDF) can request the drugs to be supplied in an emergency.<br />
The practitioner may be supplied with the CD provided he/she gives an undertaking to<br />
supply the completed requisition (FP10CDF) within 24 hours. Failure to do this is a<br />
criminal offence on the part of the practitioner.<br />
5.5 ACQUISITION OF CONTROLLED DRUGS BY OTHER HEALTHCARE<br />
PROFESSIONALS<br />
In addition to the legal requirements and good practice described previously, the<br />
following applies when other healthcare professionals acquire CDs.<br />
5.5.1 Midwives<br />
Community Midwives should obtain controlled drugs for stock in accordance with their<br />
employing authority policies and procedures. For more details on the regulations and<br />
midwives refer to the National Prescribing Centre Guidance : - NPC - Home Page<br />
Alternatively, a prescription can be written by a doctor e.g. a GP if that patient is under<br />
their care. The patient obtains the prescribed CD from a pharmacy and keeps it in their<br />
home until it is required for administration by the midwife.<br />
Page 26 of 196
5.5.2 Paramedics<br />
Ambulance paramedics can supply and / or administer under PGD all drugs listed in<br />
schedule 4 and 5. Under separate exemptions and a group authority, <strong>NHS</strong> ambulance<br />
paramedics serving at any approved ambulance station are able to administer<br />
diazepam and/or morphine sulphate injection (to a max of 20mg) for immediate<br />
necessary treatment of sick or injured persons.<br />
Out of Hours, Urgent Care, Walk in Centres etc. are not approved ambulance stations<br />
therefore registered paramedics who are required to administer diazepam or<br />
midazolam in the course of their duties must do so under an approved Patient Group<br />
Direction (PGD). Currently administration of schedule 2 controlled drugs (i.e. morphine,<br />
diamorphine) are not allowed via PGD for use in trauma.<br />
5.5.3 Hospices, community hospitals and independent hospitals<br />
Where a hospice, community hospital or private hospital does not employ a<br />
pharmacist, the person or acting person in charge may obtain CDs via a requisition<br />
signed by a doctor or dentist employed or engaged there.<br />
If supplies are obtained from a community pharmacy the FP10CDF requisition form<br />
must be used. A designated organisation code and/or practice code will be issued by<br />
the PCT and PPD for the specific purpose of ordering controlled drugs from community<br />
pharmacies via FP10CDF requisitions.<br />
If supplies are requested via a wholesaler or the pharmacy department of an <strong>NHS</strong><br />
Trust with whom a service level agreement (SLA) is in place a written requisition form<br />
should be used which complies with the regulations set out above. (FP10CDF forms<br />
do not apply).<br />
5.5.4 Out of Hours premises<br />
At out of hour‘s premises, as long as the ordering, supply or dispensing of CDs is<br />
undertaken by a doctor or pharmacist, CD stock can be ordered as in section15.5.3<br />
above.<br />
Acquisition may be undertaken by anyone else i.e. office manager of the Out of Hours<br />
Provider – under these circumstances a Home Office licence is required.<br />
Page 27 of 196
PREPARATION AND ADMINISTRATION OF CONTROLLED DRUGS<br />
6.1 Legal Framework<br />
Any person may legally administer a schedule 5 CD to any other person<br />
Page 28 of 196<br />
Appendix 6<br />
Administration of CDs via PGD applies to the specified healthcare professional in the<br />
PGD, this cannot be delegated to another person.<br />
Doctors and dentists and any person acting in accordance with the directions of a<br />
doctor or dentist may administer Sch 2, 3 or 4 CD from stock.<br />
Nurse independent prescriber‘s or any person acting in accordance with their<br />
directions can administer a limited range of controlled drugs. See Appendix O<br />
Some professional groups, not all, are permitted to supply or administer controlled<br />
drugs in accordance with a PGD.<br />
A carer/relative, can, with consent, administer a CD that has been individually<br />
prescribed for a third party. As CDs are included within the legal category of<br />
prescription only medicines (POM), home carers who are competent to administer<br />
medicines should also be competent to administer CDs.<br />
Midwives may possess those CDs which they may also lawfully administer (i.e.<br />
diamorphine, morphine, pethidine and pentazocine)<br />
Ambulance paramedics see section 15 above<br />
6.2 Good Practice<br />
Except in exceptional circumstances, the person prescribing the CD should not also<br />
personally undertake all of the following tasks: preparation, dispensing, transportation<br />
and administration of the CD.<br />
A record of each administration should be kept in the relevant patient clinical notes.<br />
This record should specify the date, time, strength, presentation and form of<br />
administration, dose administered as well as the name and occupation of the person<br />
administering it.<br />
There should be policies and procedures that define safe medicine practice for the<br />
preparation and administration of injections including CDs that comply with the<br />
National Patient Safety Alerts: Promoting safer use of injectable medicines. Further<br />
details can also be found in the PCT Safe and Secure Handling of Medicines <strong>Policy</strong><br />
and the PCT Syringe driver policy.<br />
6.3 Naloxone<br />
Naloxone injection, an antidote to opiate-induced respiratory depression, should be<br />
available in all clinical locations where diamorphine and morphine injections are stored<br />
and administered, including GPs bags; as per the National Patient Safety Agency<br />
alerts <strong>NHS</strong> to risks with high dose morphine and diamorphine injections<br />
6.4 Extemporaneous preparation of methadone<br />
If a licensed product is available, methadone mixture should only be prepared<br />
extemporaneously if the quantity of methadone dispensed on a regular basis is large<br />
enough to preclude storage of sufficient quantities of the licensed product.<br />
SOPs must be in place for the extemporaneous preparation of methadone
It is essential that robust standards and systems are in place to ensure the quality of<br />
the prepared methadone so that patient care is not compromised.<br />
Full guidance can be found at http://www.rpsgb.org/pdfs/coepsgssmeds.pdf<br />
Page 29 of 196
7.1 Medical practitioners<br />
PRESCRIBING OF CONTROLLED DRUGS<br />
Page 30 of 196<br />
Appendix 7<br />
Doctors and dentists may prescribe all CDs in Schedules 2 to 5 for organic disease.<br />
Doctors are only able to prescribe diamorphine, dipipanone and cocaine to substance<br />
misusers for the treatment of addiction if they hold a licence issued by the Home Office. All<br />
doctors may prescribe such drugs for patients, including substance misusers, for the relief<br />
of pain due to organic disease or injury without a specific licence.<br />
(Note: supplementary prescriber‘s working within agreed patient specific management plans<br />
who prescribe for substance misusers for the treatment of addiction are not currently able to<br />
apply for a licence from the Home Office: currently licences are restricted to doctors; this<br />
may be subject to change in the future).<br />
7.2 Non-medical prescriber‟s<br />
7.2.1 Community practitioner nurse prescriber‟s<br />
Community practitioner nurse prescriber‘s may only prescribe those products and<br />
medicines specified in the Nurses Prescriber‘s‘ Formulary for community practitioners. No<br />
CDs are included in this formulary.<br />
7.2.2 Nurse independent prescriber‟s<br />
Nurse independent prescriber‘s are permitted to prescribe, administer, or direct anyone to<br />
administer certain CDs solely for specific medical conditions.<br />
7.2.3 Pharmacist independent prescriber‟s<br />
Pharmacist independent prescriber‘s cannot currently prescribe CDs, although community<br />
pharmacists can advise on and sell Schedule 5 CDs from a pharmacy.<br />
7.2.4 Supplementary prescriber‟s<br />
Registered nurses, pharmacists and Registered midwives, chiropodist / podiatrist, physio-<br />
therapist, radiographer and optometrist supplementary prescriber‘s may now prescribe any<br />
CD as long as it is within the <strong>Clinical</strong> Management Plan specific to that patient and agreed<br />
between the independent prescriber (doctor or dentist), supplementary prescriber and the<br />
patient.<br />
7.2.5 Midwives<br />
Midwives may also train as nurse independent prescriber‘s. Midwives who are not trained<br />
as nurse independent prescriber‘s may administer CDs under Exemption Orders under<br />
medicines regulations.<br />
7.3 Patient Group Directions<br />
The supply and administration of the following CDs is currently allowed under PGDs:<br />
Diamorphine, but only for the treatment of cardiac pain by nurses working in<br />
coronary care units or hospital accident and emergency departments.<br />
Midazolam. (This is the only Sch 3 CD allowed under a PGD)<br />
All drugs listed in Schedule 4 of the Regulations except:<br />
The anabolic steroids in part 2 of that Schedule<br />
Injectable formulations for the purpose of treating a person who is addicted to a<br />
drug
All drugs listed in Schedule 5 of the Regulations.<br />
The amended Regulations allow nurses, midwives, pharmacists, optometrists, chiropodists,<br />
radiographers, orthoptists, physiotherapists, ambulance paramedics, occupational<br />
therapists, orthotists and prosthetists to supply or administer CDs in Schedule 4 and 5.<br />
7.4 Exemptions<br />
Midwives, who are not trained as nurse independent prescriber‘s may administer some<br />
specific named CDs under Exemption Orders under medicines legislation.<br />
7.5 PRESCRIPTION REQUIREMENTS<br />
7.5.1 Schedule 2 and 3 controlled drugs (except temazepam)<br />
A prescription for Schedule 2 and 3 CDs (with the exception of temazepam and<br />
preparations containing it) must:<br />
Contain the following details, written so as to be indelible, e.g. written by hand,<br />
typed or computer-generated:<br />
The patient‘s full name, address and, where appropriate, age<br />
The name and form of the drug, even if only one form exists<br />
The strength of the preparation, where appropriate<br />
The dose to be taken (Take as directed or as required are not acceptable)<br />
The total quantity of the preparation, or the number of dose units, to be<br />
supplied in both words and figure<br />
Be signed by the prescriber with their usual signature (this must be handwritten)<br />
and dated by them (the date does not have to be handwritten)<br />
The address of the prescriber must be stated on the prescription and must be within<br />
the UK. (NB: the UK does NOT include the Channel Islands or the Isle of Man)<br />
Dentists: prescriptions issued by a dentist must contain the words ‗for dental<br />
treatment only‘.<br />
7.5.2 Temazepam and Schedule 4 and 5 controlled drugs<br />
Prescriptions for temazepam and for Schedule 4 and 5 CDs are exempt from the specific<br />
prescription requirements, however, they must still comply with the general prescription<br />
requirements.<br />
7.5.3 Quantity supplied on prescription<br />
The quantity of drug prescribed on each prescription should be appropriate for the clinical<br />
need of the patient. Careful consideration should be given to the quantities prescribed, both<br />
to anticipate requirements, e.g. over a weekend, and to reduce the amount of excess CDs<br />
stored in the patient‘s home.<br />
Although not a legal requirement, there is a strong recommendation that prescriptions for<br />
Schedule 1, 2, 3 and 4 CDs are limited to a quantity necessary for up to 30 days clinical<br />
need.<br />
7.5.4 Prescribing more than 30 days supply<br />
In exceptional circumstances where the prescriber believes a supply of more than 30 days<br />
medication is clinically indicated and would not pose an unacceptable threat to patient<br />
safety the prescriber:<br />
Should make a note of the reasons for this in the patient‘s notes<br />
Be ready to justify his / her decision if required<br />
Page 31 of 196
7.5.5 Repeat prescribing<br />
Current legislation does not allow Schedule 2 and 3 CDs to be prescribed as repeat<br />
prescriptions (i.e. to be part of the repeat prescribing system within a practice, or part of a<br />
repeat dispensing system).<br />
7.5.6 <strong>NHS</strong> repeat dispensing scheme<br />
Schedule 4 and 5 CDs may be ordered on prescriptions issued under the repeat dispensing<br />
scheme. For Schedule 4 CDs, the first prescription must be dispensed within 28 days.<br />
Currently Schedule 2 and 3 CDs are not permitted on prescriptions issues under repeat<br />
dispensing schemes.<br />
7.5.7 Dispensing more than 30 days supply<br />
It is not illegal for a pharmacist to dispense a prescription for more than 30 days<br />
supply, but they must satisfy themselves as to the clinical appropriateness of the<br />
prescription before doing so<br />
A pharmacist does not need to contact the prescriber each time they receive a prescription<br />
requesting a supply in excess of 30 days of a Schedule 2-4CD. There may be<br />
circumstances where there is a genuine need to prescribe more than 30 days supply and<br />
pharmacists should exercise their professional judgement and assess both the prescription<br />
and the situation to check the suitability for the patient. Where there is concern that the<br />
prescription is not appropriate the prescriber should be contacted.<br />
7.5.8 Good practice (general)<br />
All prescriptions for Schedule 2 and 3 CDs should include the patients <strong>NHS</strong> number where<br />
possible so that the usage of CDs by individual patients can be audited.<br />
The professional registration number and the profession of the person who signs the<br />
prescription should be added to the CD prescriptions they write, to assist with any future<br />
audit. The prescriber‘s full name, address, telephone number and the PCT in which they are<br />
working should also be included on the prescription. This information is generally preprinted<br />
on the prescription.<br />
Dosages and frequencies for all CDs should normally be presented in full by the prescriber,<br />
to aid administration by nurses and carers. (i.e. Take one tablet up to four times a day when<br />
required for pain relief). Particular care should be taken to ensure clarity of dosage<br />
instructions where systems such as syringe drivers are being used.<br />
Any space on the prescription form that has not been written on must be blanked off,<br />
e.g. by drawing a line through it to reduce the opportunity for fraud.<br />
CDs have the potential to be diverted to the illicit market. For this reason, when a patient<br />
presents a CD prescription for an acute condition, more than two/three weeks after the<br />
prescription was issued, it would be prudent to check with the patient and/or prescriber that<br />
the supply of the CD is still warranted before dispensing the item.<br />
Computer systems should be used, wherever feasible, as an additional method to record<br />
and audit the prescribing of CDs. If a prescriber makes a domiciliary visit, and a CD is<br />
administered or a handwritten prescription for a CD is issued, it is good practice to make a<br />
note of this on the patient‘s computer record as soon as possible after the event. The doctor<br />
should also record the administration of a CD to a patient<br />
Page 32 of 196
7.5.9 Validity of prescriptions<br />
The validity period of <strong>NHS</strong> and private prescriptions for Schedule 1, 2, 3 and 4 CDs has<br />
been restricted to 28 days. This means that the prescription should not be dispensed if<br />
more than 28 days have elapsed since it was signed and dated by the prescriber, or if the<br />
prescription has a later start date, not more than 28 days from this date.<br />
In the case of a prescription containing a Schedule 2 or 3 CD, which directs that specified<br />
instalments of the total amount may be supplied at stated intervals, the first instalment must<br />
be supplied no later than 28 days after the ‗appropriate date‘.<br />
See the following website for further details The Misuse of <strong>Drugs</strong> (Amendment No. 2)<br />
Regulations 2006<br />
7.5.10 Technical errors on a prescription<br />
Pharmacists are able to supply Schedule 2 and 3 CDs except temazepam (which is exempt<br />
from CD prescription requirements), against some prescriptions that have a minor technical<br />
error but where the prescriber‘s intention is clear.<br />
The only errors that pharmacists may amend are:<br />
Minor typographical errors or spelling mistakes<br />
Where the total quantity of the preparation of the CD or the number of dosage units<br />
as the case may be is specified in either words or figures but not both (i.e. they may<br />
add the words or the figures to the CD prescription if they have been omitted).<br />
As a safeguard to these changes the pharmacist must satisfy two pre-conditions before<br />
amending the prescription and supplying the CD:<br />
He must be satisfied on reasonable grounds, having exercised due diligence that the<br />
prescription is genuine and that he is supplying the drug in accordance with the<br />
intention of the prescriber<br />
Any correction must be marked so as to be attributable to the pharmacist to ensure it<br />
is readily identifiable, for the purpose of the audit.<br />
Additional guidance is available at www.rpsgb.org.uk<br />
7.5.12 Prescribing to self and family<br />
Other than in emergencies, no prescriber should prescribe any drug for themselves<br />
or anyone with whom they have a close personal or emotional relationship.<br />
There may be some cases, such as in an emergency situation in which prescribing for<br />
family, friends or self is immediately necessary to:<br />
Save life<br />
Avoid significant deterioration in the patients health<br />
Alleviate uncontrollable pain<br />
And that no other person with the legal right to prescribe is available to assess the patient‘s<br />
clinical condition and to delay prescribing would put the patient‘s health at risk, or cause<br />
unacceptable pain.<br />
The British Medical Association (BMA) and the General Medical Council (GMC) advise<br />
doctors against prescribing for themselves, family, friends and colleagues. There is a risk<br />
that doctors who self-treat may ignore or deny serious health problems. There is also a risk<br />
that self-prescribing could lead to drug abuse or addiction.<br />
Page 33 of 196
The RPSGB and Nursing and Midwifery Council (NMC) also advise against self prescribing,<br />
and prescribing for friends, family and colleagues. See NMC ‗Standards of Proficiency to<br />
prescribe‘ www.nmc-uk.org and RPSGB ‗Code of Ethics‘ www.rpsgb.org.uk<br />
7.5.13 Security of Prescription pads<br />
There are regulations covering security measures to prevent users unlawfully obtaining<br />
supplies of drugs and syringes; prescription pads; and headed notepaper from<br />
premises.<br />
<strong>NHS</strong> Security Management Service; Security of Prescription Forms Guidance 2008<br />
and the PCT Guidance on security of prescriptions pads must be followed.<br />
Do not leave blank prescription pads lying around unattended.<br />
Blank prescription pads should never be pre-signed<br />
Pads should always be locked away at night in case of unlawful entry<br />
Prescriber‘s must never use blank or out of date prescription pads as spare notepads<br />
Prescription forms for Schedule 2 & 3 CDs should not routinely be sent to the patient‘s<br />
pharmacy via the postal system, but should be collected by a healthcare professional,<br />
a member of their staff, the patient or their representative.<br />
Prescriptions for the treatment of drug addiction may be sent to pharmacies when it is<br />
not practical for the pharmacists to collect prescriptions from the premises i.e. due to<br />
distance and it is not always desirable for the patient to be handed the prescription.<br />
It is good practice to keep a record of controlled drug prescription forms awaiting<br />
collection in the practice (including prescriptions for drug addiction). Also for the<br />
person collecting the prescription to date and sign for receipt of the prescription form.<br />
Care must be taken to ensure other prescriptions for the patient are also collected at<br />
the same time.<br />
Page 34 of 196
PRESCRIBING IN INSTALMENTS<br />
Page 35 of 196<br />
Appendix 8<br />
Some CDs can be dispensed to substance misusers in instalments providing they are<br />
prescribed using specific <strong>NHS</strong> prescription forms. FP10 (MDA)<br />
A prescriber writing a private prescription can also ask for the prescription to be dispensed<br />
in instalments.<br />
8.1 FP10 (MDA)<br />
The form FP10 (MDA) is used to prescribe in instalments Schedule 2 CDs, buprenorphine<br />
(Schedule 3) or diazepam (Schedule 4) for drug addiction. This form must not be used for<br />
any other purpose. E.g. when the total quantity needs to be dispensed at one time – in this<br />
case the normal FP10 form must be used.<br />
Hospital or clinical-based prescriber‘s use a variation of this form – FP10 (MDA) SS that is<br />
overprinted with the words ‗HOSPITAL PRESCRIBER‘. The SS forms are intended to be<br />
used for computer-generated prescriptions although they can be handwritten as well.<br />
8.1.2 Details to be specified<br />
If a CD prescription is to be dispensed in instalments, e.g. daily, then the prescription must<br />
specify the following details:<br />
1. The number of instalments<br />
2. The intervals to be observed between instalments; if necessary, instructions for<br />
supplies at weekends or bank holidays should be included<br />
3. The total quantity of CD that will provide treatment for a period not exceeding<br />
14 days.<br />
4. The quantity to be supplied in each instalment<br />
Points 1, 2 and 3 are required by the <strong>NHS</strong> (General Medical Services Contract) Regulations<br />
2004. Points 2 and 4 are required under the Misuse of <strong>Drugs</strong> Regulations 2001, Regulation<br />
15.<br />
8.2 Collection of instalments<br />
The prescription must be dispensed on the date on which it is due. If the client does not<br />
collect an instalment when it is due that supply is no longer valid. The client cannot collect<br />
that supply the following day.<br />
If a prescriber has ordered several days‘ instalments to be collected on one day and the<br />
client does not come in on the specified day, then he loses the complete instalment; he<br />
cannot have the remainder of the instalment. Pharmacists should endorse the prescription<br />
‗NOT DISPENSED‘ for that instalment and, if possible, notify the prescriber.<br />
However, guidance from the Home Office has indicated that the use of specific wording will<br />
enable those supplying CDs to issue the remainder of an instalment prescription when the<br />
person has failed to collect the instalment on the specified day. The wording below can be<br />
used if a prescription does not contain such wording the Regulations only permit the supply<br />
to be made in accordance with the prescriber‘s instalment direction. Further guidance can<br />
be found at:-<br />
www.pharmj.com/Editorial/20050430/society/ethics.hmtl.<br />
‗Supervised consumption of daily dose specified days; the remainder of supply<br />
to take home. If an instalment prescription covers more than one day and is not<br />
collected on the specified day, the total amount prescribed less the amount<br />
prescribed for the days used may be supplied‘
‗Unsupervised consumption; instalment prescriptions covering more than one day<br />
should be collected on the specified day; if this collection is missed the remainder of<br />
the instalment (i.e. the instalment less the amount prescribed for the days missed)<br />
may be supplied.‘<br />
8.3 <strong>NHS</strong> forms issued to substance misusers<br />
Issued by / in Type of form Region What is allowed<br />
GPs<br />
Hospital or clinic<br />
based prescriber‘s<br />
Nurse independent<br />
prescriber‘s<br />
Supplementary prescriber‘s<br />
FP10(MDA) or<br />
FP10(MDA) SS<br />
FP10(MDA) SS<br />
FP10(MDA) or<br />
FP10(MDA) SS<br />
FP10(MDA) SS<br />
FP10(MDA) SP<br />
England<br />
England<br />
England<br />
England<br />
Schedule 2 CDs, buprenorphine,<br />
diazepam, plus single supplies of<br />
water for injection as necessary<br />
Schedule 2 CDs, buprenorphine,<br />
diazepam, plus single supplies of<br />
any other medication allowed on<br />
FP10<br />
Diazepam for treatment of initial<br />
or acute withdrawal symptoms<br />
caused by the withdrawal of<br />
alcohol from persons habituated<br />
to it.<br />
Schedule 2 CDs, provided this is<br />
agreed by a doctor in the patient‘s<br />
<strong>Clinical</strong> Management Plan.<br />
8.4 Good Practice<br />
On FP10 (MDA) prescriptions, it is good practice for the duration of the instalments to be<br />
set out on the prescription, e.g. dispense daily for five days starting on x date.<br />
The client should collect the CD in person. If he or she is unable to collect prescriptions<br />
personally, the client may arrange for a representative to collect it. The representative<br />
should bring a suitable note on each occasion to ensure they have authority to collect.<br />
The requirements to see identification on collection only apply to the first dispensing of an<br />
instalment prescription.<br />
8.5 Prescribing controlled drugs for addiction<br />
Only doctors are able to prescribe diamorphine, dipipanone or cocaine to substance<br />
misusers for treatment of addiction, but only if they hold a licence, issued by the Home<br />
Office. Prescriber‘s can prescribe such drugs for patients, including substance misusers, for<br />
relief of pain due to organic disease or injury, without a specific licence.<br />
Page 36 of 196
PRIVATE PRESCRIBING<br />
Page 37 of 196<br />
Appendix 9<br />
Besides reviewing the current legal framework, this document helps to establish good<br />
practice for the management of CDs. Although this is presented in the form of guidance for<br />
the <strong>NHS</strong>, this is equally applicable to professionals providing health care in non-<strong>NHS</strong><br />
settings. The law relating to prescribing applies to all <strong>NHS</strong> and non-<strong>NHS</strong> settings and good<br />
governance is equally applicable to Non <strong>NHS</strong> organisations.<br />
The term ‗private prescriber‘ is used to describe the situation when a private prescription is<br />
written, either by <strong>NHS</strong> or non-<strong>NHS</strong> practitioners, in either <strong>NHS</strong> or non-<strong>NHS</strong> settings.<br />
9.1 Legal framework<br />
When writing private prescriptions, prescriber‘s must comply with all legal requirements,<br />
including appropriate record keeping, when ordering, prescribing, dispensing, administering<br />
and destroying CDs.<br />
Registerable private doctors and independent clinics, as defined under section 2 of the<br />
Care Standards Act 2000, are required to be registered with the Healthcare Commission, as<br />
laid out in the Health and Social Care (Community Health and Standards) Act (2003) and<br />
Private and Voluntary Health Care (England) Regulations 2001. *There is a need to<br />
demonstrate safe systems of handling and prescribing CDs in meeting the National<br />
Minimum Standards for Independent Healthcare<br />
www.dh.gov.uk/assetRoot/04/07/83/67/04078367.pdf<br />
Normally, private prescriptions can allow a prescriber to request that the prescription is<br />
repeatable ** for a specified number of times. However, this is not permitted for Schedule 2<br />
and 3 CDs. It is possible to prescribe Schedule 4 and 5 CDs on a repeat basis, both<br />
privately and under <strong>NHS</strong> repeat dispensing arrangements.<br />
* It is an offence under the Care Standards Act 2000 section 11 to carry on or manage a<br />
registerable service without first being registered to do so. Failure to apply for registration<br />
could render the practitioner liable to prosecution and could lead to the refusal of the<br />
application to register.<br />
** The repeat method is where a private prescription is written for a specified quantity of<br />
drugs and the prescriber endorses the prescription with the number of times the prescription<br />
should be repeated. The pharmacist is then able to make the specified number of<br />
dispensing transactions from that prescription.<br />
9.2 Standardised private prescription form<br />
All private prescriptions for human use of Schedule 1, 2 and 3 CDs (including temazepam)<br />
that are presented for dispensing in the community (not the hospital) must be written on a<br />
standard prescription form which must include the private prescriber‘s unique (six digit)<br />
identification number issued specifically for the private prescribing activity.<br />
There are two types of forms available:<br />
Personalised FP10 (PDC) NC – These contain the prescriber‘s details already printed.<br />
Non personalised forms FP10 (PCD) SS – These allow private prescriber‘s to print private<br />
CD prescriptions, including their private prescriber details, using their practice computer<br />
systems.
Private prescriber‘s should obtain stocks of private prescription forms via their designated<br />
PCT.<br />
9.3 Private prescriber identification number<br />
Prescriber‘s who issue private prescriptions for Schedule 2 and 3 CDs that will be<br />
dispensed by community pharmacists must have a unique prescriber identification number.<br />
Any prescriber requiring a private prescriber identification number should apply via local<br />
PCT. A number will be then issued by the PPD of the <strong>NHS</strong> Business Services Authority. It<br />
will be different from the prescriber‘s <strong>NHS</strong> prescriber code if they have one. A prescriber<br />
who practices in the <strong>NHS</strong> and privately will, therefore have two identifier numbers (one <strong>NHS</strong><br />
and one private).<br />
Prescriber‘s working in private practice in a hospital should inform patients that private<br />
prescriptions not written on the standard form can only be dispensed in a hospital<br />
pharmacy.<br />
9.4 Submission of prescription<br />
The original or a copy of each prescription for a Schedule 1, 2 or 3 CD should be submitted<br />
after dispensing (community pharmacists or dispensing doctors) to the relevant National<br />
Health Service Agency (<strong>NHS</strong> Business Services Authority for England) along with a CD<br />
submission form (FP34PCD). Until the Miscellaneous Provisions Regulations are amended<br />
a copy needs to be submitted.<br />
9.5 Good practice<br />
The National <strong>Clinical</strong> Assessment Service (NCAS) and the <strong>NHS</strong> <strong>Clinical</strong> Governance<br />
Support Team have suggested the following good practice for private prescriber‘s:<br />
Private prescriber‘s should produce their own guidance for use in their services with respect<br />
to:<br />
Treatment, prescribing and review policies<br />
<strong>Clinical</strong> governance systems<br />
Training and continuing professional development (CPD)<br />
This guidance should be rooted in any relevant national good practice guidance,<br />
Including ‗Drug misuse and dependence: guidelines on clinical management‘<br />
published by DH.<br />
Private prescriber‘s should, in most circumstances and with the patient‘s agreement,<br />
contact the patient‘s private or <strong>NHS</strong> GP before initiating treatment and during the course of<br />
treatment.<br />
Private prescriber‘s should, in most circumstances, liaise as appropriate with other health<br />
care professionals involved in the care of the patient. This should include the pharmacist/<br />
dispensing doctor.<br />
Private prescriber‘s should indicate on the prescription when prescribing for a non-UK<br />
resident. Several of the points here are included in Regulation under the Health and Social<br />
Care (Community Health and Standards) Act (2003), and private and Voluntary Health Care<br />
(England) Regulations 2001.<br />
Page 38 of 196
Page 39 of 196<br />
Appendix 10<br />
Prescriptions for prisoners and other agency agreements for <strong>NHS</strong> services<br />
In England, the <strong>NHS</strong> provides prescriptions for prisoners and some other patients under<br />
SLA‘s with other organisations. Traditionally, this has been treated for administrative<br />
convenience in the same way as private work in order to prevent submission to and<br />
reimbursement by the relevant <strong>NHS</strong> agency. However, the new standardised private<br />
prescription forms should not be used for such patients as this is classed as <strong>NHS</strong> activity.
STORAGE OF CONTROLLED DRUGS<br />
Page 40 of 196<br />
Appendix 11<br />
This section covers the legal and good practice issues for the storage of CDs. It does not<br />
cover any clinical or drug stability issues, which should be addressed separately.<br />
All Schedule 2 (except quinalbarbitone) and Schedule 3 CDs (except Buprenorphine,<br />
Diethylpropion, Flunitrazepam and Temazepam) are subject to safe custody requirements<br />
and must be kept in a locked receptacle, which is so constructed and maintained to prevent<br />
unauthorised access to drugs.<br />
In residential and healthcare settings it is recommended that the specifications of cabinets<br />
and safes set out in Schedule 2 of the Safe Custody Regulations should be regarded as a<br />
minimum standard for the storage of CDs.<br />
11.1 <strong>Controlled</strong> drug cabinets/safes<br />
Requirements and/or recommendations are that:<br />
The receptacle should consist of a locked safe/cabinet preferably of steel, with<br />
suitable hinges, fixed to a wall or the floor with rag bolts (these bolts should not be<br />
accessible from outside the cabinet)<br />
Ideally the safe/cabinet should be within a cupboard or in such a position as to avoid<br />
easy detection by intruders.<br />
Nothing should be displayed outside to indicate that CDs are kept within the<br />
container.<br />
The room containing the safe/cabinet should be lockable and tidy to avoid drugs<br />
being misplaced.<br />
This room should not normally be accessible to patients, nor should the keys<br />
required for access. However, if patients do have to enter the area where CDs are<br />
stored, it is good practice that they should be continuously supervised until such time<br />
as they leave the area.<br />
The walls of the room should be constructed to a suitable thickness using suitable<br />
materials.<br />
The locked receptacle must only be opened by the person in lawful possession of the<br />
CDs or a person authorised by him/her.<br />
Stock should be kept to a minimum and the cabinet should not contain anything other than<br />
the drugs, or the drugs and register. (The register does not have to be kept locked with the<br />
drugs).<br />
The CD register should be stored safely outside the CD container but near to it but not<br />
easily visible or accessible.<br />
Items such as money should not be stored in the CD cabinet.<br />
Tamper evident manufacturer seals must be left in tact on receipt of the CD and only<br />
opened at time of administration/supply.<br />
All services/practices must have SOP in place for management of CD stock held on the<br />
premises.<br />
One designated person within the premises should take overall responsibility for the<br />
management of controlled drugs including keys/codes. The number of sets of keys to the<br />
container, and who holds them, or who has access to the codes for digital key pads, must
e known at all times by the designated person. The keys should always be kept separate<br />
from the container and should never be accessible to unauthorised persons. The container<br />
should only be opened by the designated person, or by the person authorised by them, e.g.<br />
a locum. The designated person remains ultimately accountable for the management of the<br />
CDs.<br />
Other drugs that are liable to misuse can be locked in the container if this is deemed<br />
appropriate by the relevant health care professional.<br />
<strong>Drugs</strong> in Schedules 4 and 5 can also be a target for substance misusers. Dispensary areas<br />
are required to be secure enough to prevent unauthorised access, but additional<br />
precautions, such as keeping these items out of sight of patients, may be advisable.<br />
All CDs should be stored out of sight and reach of children<br />
11.2 <strong>Controlled</strong> drugs in a „doctor‟s bag‟<br />
A‘ doctor‘s bag‘ is a locked bag, box or case for home visits, etc. which should be kept<br />
locked at all times, except when in immediate use. The person in lawful possession of this<br />
bag, or an individual authorised by them, must always retain the keys.<br />
Legal precedent holds that such a bag is regarded, once locked, as a suitable receptacle for<br />
storing CDs, but a locked car is not. Bags containing CDs should not be left in a vehicle<br />
overnight, or in a vehicle left unattended for long periods of time.<br />
For a bag for home visits, etc. a digital combination lock on a case is often the most<br />
practical and convenient solution and avoids problems with keys.<br />
The stock levels held in this bag should be kept to a minimum and informed by previous<br />
requirements.<br />
Normally, only one strength of each CD should be kept in a bag for home visits, etc. in order<br />
to minimise the risk of confusion, error and inappropriate administration.<br />
Oral preparations of CDs would not routinely be considered essential items to be carried in<br />
such a bag.<br />
The doctor, or a delegated member of staff, should undertake a monthly stock check of CDs<br />
held within each bag for home visits and a record made that this has been done. This<br />
process also provides a good opportunity to check for any out-of-date (or ‗soon to expire‘)<br />
stock. This needs to be included in an SOP.<br />
When a bag for home visits, etc. containing CDs is in the practice, it should be stored in a<br />
safe place away from patient areas in a locked room. This location should be determined by<br />
carrying out a risk assessment.<br />
A separate CD register should be kept for the CD stock held within the bag and a running<br />
balance maintained.<br />
Restocking of a bag for home visits, etc. from FP10CDF or practice stock should be<br />
witnessed by another member of the practice staff, as should the appropriate entries into<br />
the CD register.<br />
Where a prescription is written by a doctor following administration of a CD to a patient, the<br />
doctor should endorse the form with the words ‗administered‘ and then date it. This process<br />
Page 41 of 196
aims to avoid unauthorised individuals attempting to reuse such prescriptions to obtain CDs<br />
illegally<br />
When a drug from the doctor‘s bag is administered to a patient, an entry must be made in<br />
the CD register for that bag. Personal administration should also be recorded in the<br />
patient‘s notes/computer record.<br />
Each professional should also assess the risks and benefits in relation to where they store<br />
CDs and registers in relation to each other. A balance has to be achieved between having<br />
the CD register readily available to make an entry at the time of administration, and the<br />
possibility of the bag and the register both being stolen, with the consequent loss of both<br />
the CDs and the audit trail.<br />
If CDs kept in a bag for home visits, etc. expire, they should be returned to the central<br />
practice stock for future destruction in the presence of an authorised individual. If the<br />
practice does not hold central stock, then the CDs need to be destroyed directly from the<br />
bag, witnessed by an authorised individual and appropriate records made in the CD<br />
register.<br />
A small number of GPs continue to provide their own personal service in the out-of-hours<br />
period, and would therefore use their own bag in the same way as they do during normal<br />
hours. However, the majority of GPs delegate responsibility to an organised provider of outof-hours<br />
services e.g. a GP Co-operative or a deputising service.<br />
In terms of good practice when managing CDs out-of-hours, reference should be made to<br />
the following DH guidance ‗Securing proper access to medicines in the out-of-hours period‘<br />
www.out-of-hours.info/downloads/short_medicines_guidance.pdf and the accompanying<br />
practical guide:<br />
www.out-of-hours.info/downloads/medicines_supply_guidance_a_practical_guide.pdf.<br />
Page 42 of 196
DISPENSING OF CONTROLLED DRUGS<br />
Page 43 of 196<br />
Appendix 12<br />
12.1. General<br />
In this context, the term ‗dispense‘ means to assemble and to supply a medicine<br />
(please note ‗dispense‘ is not defined in legislation).<br />
A second person should check the quantity/volume and strength of a CD being<br />
dispensed, although this may not be practiced in all situations.<br />
All CDs should normally be dispensed in child-resistant containers, or with childresistant<br />
closures.<br />
As with all dispensed medicinal products (except unlicensed medicines), it is a legal<br />
requirement to provide a manufacturer‘s patient information leaflet.<br />
Details of supplies of Schedule 2 CDs must be entered into the CD register as soon as<br />
possible and at the latest the next day following the day of supply.<br />
The date entered in the CD register should be the date of supply (i.e. the date on<br />
which the CD is handed to the patient/carer/representative) and not the date when it is<br />
assembled.<br />
The pharmacist/dispensing doctor must endorse prescriptions for Schedule 2 and 3<br />
CDs with the date of supply to the patient.<br />
Advice to patients, their representatives or carers should include safe and secure<br />
storage at home, especially out of sight and reach of children, and safe disposal by<br />
returning any unused CDs to a pharmacy.<br />
If a prescription for a CD is handed in for dispensing, but is not due to be collected until<br />
a future date or time, the prescription can be assembled in advance. However, details<br />
should not be entered in the CD register until after the CD has been supplied to the<br />
patient/carer/representative.<br />
Patients, or other people collecting Schedule 2 and 3 drugs on their behalf, should sign<br />
for them. This applies to both <strong>NHS</strong> and private prescriptions; there is space on the<br />
back of the form for this purpose. See below for details on proof of identity for<br />
Schedule 2 CDs.<br />
12.2 Dispensing against instalment prescriptions FP10 (MDA)<br />
For instalment prescriptions of Schedule 2 CDs, each supply must be entered, on the<br />
day of supply, into the relevant section of the CD register. This task must not be left<br />
until the end of the prescription period or carried out in advance.<br />
Instalments must only be supplied on the day that they are due, as specified on the<br />
prescription.<br />
Medical Services Contract) Regulations 2004 specify only a sufficient quantity of<br />
drugs as will provide treatment for not more than 14 days can be prescribed on <strong>NHS</strong><br />
instalment prescriptions.
Prescriptions are valid for 28 days. The 28 day period starts on the applicable date<br />
entered on the prescription form. This date will be the date of signing or a start date<br />
specified by the prescriber on the form. The first instalment must be dispensed within<br />
the 28-day limit, with the remainder instalments dispensed in accordance with<br />
instructions.<br />
Where appropriate, shared care arrangements for the prescribing and dispensing of<br />
CDs for substance misusers, should be developed<br />
If an instalment prescription for a CD is presented, then it should be stamped with the<br />
pharmacy/dispensing practice address at the time of the first dispensing. This is to<br />
prevent the possibility of future misdirection of the prescription.<br />
In practice, methadone prescriptions are often made up in advance, to ensure<br />
substance misusers can be dealt with in a proactive and timely manner when they<br />
present for their medicine. The pre-assembled methadone must be stored in a cabinet<br />
which meets the legal requirements, or be under the direct personal supervision of the<br />
pharmacist/doctor.<br />
If the patient does not collect the instalment, it can be returned to stock, provided it is<br />
labelled appropriately as stock, e.g. with batch number and expiry date. Where CDs<br />
are assembled in advance for instalment dispensing and not collected, the patient<br />
medication record should be amended and the prescription annotated to reflect the fact<br />
that the supply was not collected.<br />
Guidance on instalments prescribing and pharmacy closures can be found at<br />
www.rpsgb.org.uk/pdfs/LEBapprovwordinginstalprescs.pdf<br />
Pharmacists dispensing CDs to substance misusers should liaise with the prescriber<br />
regarding collection/non-collection of the CDs by these clients<br />
Patients receiving methadone, diazepam and buprenorphine may require supervision<br />
of consumption by a pharmacist. This should ideally be carried out in a quiet area of<br />
the pharmacy. This area should not normally be the dispensary, or involve taking the<br />
patient through the dispensary.<br />
Particular care should be exercised when a third party collects a CD for a patient being<br />
treated for addiction. RPSGB guidance states that third party collection of CDs for addicts<br />
should only occur in exceptional circumstances. A letter of authority from the patient should<br />
be obtained on every occasion that the representative collects the prescription and this<br />
letter should be retained in the pharmacy. If a patient regularly sends a third party to collect<br />
a supply, it may be necessary for the pharmacist to notify either the clinic where the<br />
substance misuser is being treated, or the prescriber.<br />
12.3 „Owing‟ prescriptions for controlled drugs<br />
If the pharmacist/dispensing doctor are unable to supply the total quantity of the drug<br />
requested, the entry made in the CD register must only be for the quantity of the drug<br />
actually supplied. A further entry must be made when the balance is supplied. If the patient<br />
no longer requires the balance of the prescription, the prescription should be endorsed with<br />
the amount dispensed. It is good practice to record the reason why the remainder was not<br />
dispensed, e.g. the patient has died.<br />
Page 44 of 196
Dispensed items or Owings for Schedule 2, 3 or 4 CDs cannot be supplied more than 28<br />
days after the appropriate date on the prescription.<br />
Where the prescriber has written on the prescription that it must be supplied on a specific<br />
date, as in the case for instalment prescriptions, those instructions must be complied with.<br />
Where a prescription requires a specific quantity of CDs to be dispensed on a specific date,<br />
the dispenser may not dispense a part of this quantity and then rest at a later date, as this<br />
would deviate from the prescriber‘s instructions. The stock initially held in the dispensary,<br />
plus the balance remaining, can be dispensed to the patient, as long as it is done during the<br />
same calendar day.<br />
12.4 Emergency supplies to patients<br />
Under no circumstances may an emergency supply of a schedule 2 or 3 CD be made to a<br />
patient. The only exception to this rule is phenobarbital for the treatment of epilepsy. An<br />
emergency supply of Schedule 4 or 5 CDs may be made as long as the other conditions for<br />
the supply of a POM medicine are satisfied, taking into consideration the abuse potential of<br />
these drugs.<br />
12.5 Dispensing doctors<br />
It is lawful for a dispensing doctor to delegate the act of dispensing medicines for their<br />
patients to employed staff.<br />
Practice and partners carry vicarious liability for errors made, or for the breach of the law. A<br />
dispenser or other dispensing doctor employee would not normally be expected to dispense<br />
a Schedule 2 or 3 CD without first checking the dispensed items with a doctor. The<br />
Dispensing Doctor‘s Association‘s Guidelines for dispensing doctors state that ‗the doctor<br />
should check all prescriptions for CDs‘.<br />
Updated guidance on managing the use of CDs is available from the Dispensing Doctor‘s<br />
Association www.dispensingdoctor.org/.<br />
12.6 Proof of Identity; Prescriptions for Schedule 2 controlled drugs<br />
Patients or their representatives may require evidence of identity when collecting Schedule<br />
2 CDs.<br />
Persons asked to supply Schedule 2 CDs on prescription must seek to establish whether<br />
the person collecting the drug is the patient, the patient‘s representative or a health care<br />
professional acting in his professional capacity on behalf of the patient.<br />
Where the person is the patient or the patient‘s representative, e.g. a friend, neighbour, etc.,<br />
the dispenser<br />
May request evidence of that person‘s identity, and<br />
May refuse to supply the drug if he is not satisfied as to the identity of that person<br />
Where the person collecting the prescription is a health care professional acting in his<br />
professional capacity on behalf of the patient, the dispenser:<br />
Must obtain the person‘s name and address<br />
Must, unless he is acquainted with that person, request evidence of that person‘s<br />
identity; but<br />
May supply the drug even if he is not satisfied as to the identity of that person.<br />
Page 45 of 196
Any strengthening of controls has been balanced with ensuring that patients have access to<br />
medicines they need and have been prescribed for them. The new requirement placed on<br />
the dispenser therefore allows them:<br />
Discretion not to ask patients or patient representatives for proof of identity if for<br />
example they have concerns that to do so may compromise patient confidentiality or<br />
deter patients from having their medicine dispensed.<br />
It is a requirement to record the following information in the CD register for Schedule 2 CDs<br />
supplied on prescription:<br />
Whether the person who collected the drug was the patient, the patient‘s<br />
representative or a health care professional acting on behalf of the patient.<br />
If the person who collected the drug was a health care professional acting on behalf<br />
of the patient, that person‘s name and address.<br />
If the person collected the drug was the patient or their representative, whether<br />
evidence of identity was requested (as a matter of good practice a note as to why the<br />
dispenser did not ask may be included but this is not mandatory).<br />
And whether evidence of identity was provided by the person collecting the drug.<br />
RPSGB have issued professional guidance ‗Changes in the management of CDs affecting<br />
pharmacists (England, Scotland and Wales)‘ for their members on what forms of<br />
identification may be considered suitable and advice on circumstances where discretion<br />
should be exercised. This guidance is available from the following website:<br />
www.rpsgb.org.uk/pdfs/cdmanagechguid.pdf<br />
It is good practice to record information to support the proof of identity requirements<br />
outlined.<br />
As a matter of good practice, the form of identification for health care professionals should<br />
be their professional registration number.<br />
Page 46 of 196
RECORDING OF CONTROLLED DRUGS<br />
Page 47 of 196<br />
Appendix 13<br />
This section applies to all CD registers, whether held by a doctor, a pharmacist or other<br />
health care professional (personally or as part of the activities of an organisation).<br />
Records for Schedule 2 CDs must be kept in a CD register. This is not a legal requirement<br />
for Schedule 3, 4 or 5 CDs.<br />
All health care professionals who hold personal CD stock must keep their own CD register,<br />
and they are personally responsible for keeping this accurate and up-to-date.<br />
13.1 <strong>Controlled</strong> Drug Registers<br />
Currently the register must:<br />
Be bound (not loose-leaved) or a computerised system which is in accordance with best<br />
practice guidance<br />
Contain class sections for each individual drug<br />
Have the name of the drug specified at the top of each page<br />
Have the entries in chronological order and made on the day of the transaction or<br />
the next day<br />
Have the entries made in ink or otherwise so as to be indelible or in a computerised<br />
form in which every such entry is attributable and capable of being audited and is in<br />
accordance with the best practice guidance endorsed by the Secretary of State<br />
under Section 2 of the <strong>NHS</strong> Act 1977.<br />
Not have cancellations, obliterations or alterations: corrections must be made by a<br />
signed and dated entry in the margin or at the bottom of the page.<br />
Be kept at the premises to which it relates and be available for inspection at any<br />
time. A separate register must be kept for each set of premises (for example, not just<br />
the main surgery)<br />
Be kept for a minimum of two years after the date of the last entry, once completed<br />
Not be used for any other purpose<br />
13.2 Computerised controlled drug registers<br />
If the CD register is held in computerised form it must be attributable and capable of being<br />
audited the following should be put in place:<br />
Safeguards should be incorporated in the software to ensure the author of each entry<br />
is identifiable<br />
Entries cannot be altered at a later date<br />
A log of all data entered is kept and can be recalled for audit purposes<br />
Full details see www.opsi.gov.uk/si/si2005/20052864.htm<br />
13.4 Record keeping requirements<br />
For CDs received into stock the following details must be recorded in the CD register:<br />
The date on which the CD was received<br />
The name and address of the supplier, e.g. wholesaler, pharmacy<br />
The quantity received<br />
The name, form and strength of the CD<br />
For CDs supplied to patients (via prescriptions), or to practitioners (via requisitions),<br />
or personally administered the following details must be recorded in the CD register<br />
The date on which the supply/ administration was made
The name and address of the patient or practitioner receiving the CD<br />
Particulars of the authority of person who prescribed or ordered or administered the<br />
CD<br />
The quantity supplied/administered<br />
The name, form and strength in which the CD was supplied/administered<br />
The 2001 Regulations were amended in July 2006 to make clear that the record keeping<br />
requirements of the CD Regulations are a minimum and do not prevent any person required<br />
to keep a CD register from including additional related information.<br />
It is good practice to record the batch number and expiry date of the CD, time of<br />
administration and maintain a running balance.<br />
13.5 Prescriber and dispenser details<br />
CD registers are allowed but not required to include:<br />
The prescriber identification number (six digit private prescriber code or the <strong>NHS</strong><br />
prescriber code) and or professional registration number of the prescriber where<br />
known<br />
The name and professional registration number of the pharmacist or dispensing<br />
doctor<br />
As the dispensing of a prescription can involve several pharmacists, it should be the<br />
pharmacist who makes the supply of CDs to a patient or his/her representative whose name<br />
and professional number are entered in the CD register.<br />
13.6 Maintaining a running balance of stock<br />
Pharmacists and other health care professionals who supply CDs should maintain a running<br />
balance of stock in their CD registers as a matter of good practice. The aim of maintaining<br />
running balances in CD registers is to ensure irregularities are identified as quickly as<br />
possible.<br />
The running balance of drug remaining should be calculated and recorded after each<br />
transaction and balances should be checked with the physical amount of stock at regular<br />
intervals. Guidance on this can be found on the RPSGB website<br />
www.rpsgb.org.uk/pdfs/cdrunningbalanceguid.pdf<br />
Accountability for maintaining the running balance of CD stock and dealing with any<br />
discrepancies lies with the health care professional in charge and not with the person to<br />
whom they may delegate day-to-day responsibility under defined SOPs.<br />
13.7 Physical reconciliation with stock levels<br />
The running balance recorded in the CD register should be checked with the physical<br />
amounts of stock at regular intervals, at least once a month is recommended for infrequent<br />
users (i.e. GP practices) or weekly where there is a high usage or turnover of staff (i.e.<br />
OOH)<br />
Wherever possible, two members of staff should check all stock received or removed, and<br />
both individuals should initial the entry in the CD registers, or a record made that the stock<br />
balance has been checked.<br />
It is good practice for a health care professional/registered manager or registered provider,<br />
when first taking over accountability for premises that hold CD stock, and where they will be<br />
in regular attendance, to ensure the CD stock levels are correct. This primarily applies to:-<br />
Page 48 of 196
GP practices holding CD stock in the surgery<br />
Pharmacies<br />
Dispensing doctor practices<br />
Care homes, community hospitals and hospices<br />
Independent health care establishments, hospitals and community hospitals without<br />
a pharmacy.<br />
Where changeover of responsibility occurs very frequently, e.g. when multiple locums are<br />
required within community pharmacies, out-of-hours providers or GP practices, it would be<br />
impractical to carry out stock checks at every changeover. SOPs for the reconciliation of<br />
physical stock with balances should define how often this task takes place; as a minimum it<br />
should take place weekly. If usage of CDs is high, e.g. in drug and alcohol units, palliative<br />
care establishments, etc., then stock checks should be carried out more frequently and by<br />
different, suitably trained members of staff. The day-to-day responsibility for this task can be<br />
delegated under SOPs, to another appropriate, suitably trained, member of staff who is<br />
routinely present at the premises.<br />
The accountability for maintaining the correct balance of CD stock lies with the professional<br />
in charge and not with the person to whom they may delegate the day-today responsibility.<br />
13.8 Preservation of records<br />
Registers, requisitions and orders for CDs must be preserved for two years. It is<br />
recommended that records are preserved for longer as this may be required as evidence if<br />
an untoward incident occurs and investigations may take longer than 2 years<br />
13.9 Dealing with discrepancies<br />
SOPs should clearly define the action to be taken if a discrepancy arises. Once resolved,<br />
a note should be made in the CD register correcting the discrepancy in the balance. It is<br />
also advisable to keep appropriate records of the action taken when discrepancies arise.<br />
If the source of the discrepancy cannot be identified during the stock check, then a<br />
nominated member of the relevant organisation should be informed and a formal internal<br />
investigation undertaken. This process may include discussion with the relevant<br />
professional body, or other inspectors. If this still does not resolve the issue satisfactorily<br />
then the police should be informed. The Accountable Officer should be informed of any<br />
concerns in relation to the management and use of CDs.<br />
Page 49 of 196
TRANSPORTATION OF CONTROLLED DRUGS<br />
Page 50 of 196<br />
Appendix 14<br />
All health care professionals in legal possession of a CD have a professional duty of care to<br />
take all reasonable steps to maintain safe custody of that CD at all times.<br />
Nurses, midwives, doctors, pharmacists, pharmacy staff and other health care<br />
professionals, plus formal carers and patients‘ representatives, are legally allowed to<br />
transport CDs to a patient, provided the CDs have been prescribed, by an appropriate<br />
prescriber, for the patient.<br />
Any nominated individual is also allowed to return CDs from the patient to the pharmacy, or<br />
the practice for destruction.<br />
The person authorised to possess may grant permission, and it should be in writing.<br />
Community pharmacies and GP practices must not accept waste medicines, including CDs,<br />
from care homes providing nursing care.<br />
Health care professionals involved in the delivery of patient care should not routinely<br />
transport a patient‘s own CDs to and from the patient‘s home. Where this is essential, part<br />
of an organised service, or where pharmacies operate collection and delivery schemes to<br />
the household and other needy patients, it is good practice to keep the CDs out of view<br />
during transit.<br />
CDs should not generally be transported via mail, taxi services or equivalent. However, in<br />
exceptional circumstances, where urgent clinical need dictates, dispensed CDs can be sent<br />
to a patient, or stock CDs to premises, via such routes. Where the mail route is used, the<br />
CD should always be sent as a special delivery item to ensure the pathway is auditable.<br />
If transport of CDs or CD prescriptions via mail, taxi services or equivalent has to be used<br />
an SOP should be developed which reflects a risk management assessment.
ADMINISTRATION OF CONTROLLED DRUGS<br />
Page 51 of 196<br />
Appendix 15<br />
A record of administration should be made in the patient‘s records which detail dose, form<br />
and route, site of injection, expiry date, time of administration and if records require this the<br />
batch number and expiry date.<br />
If the patient has nursing records for administration of medicines, (i.e. palliative care,<br />
residential care homes and hospices) these should be completed by the person<br />
administering the medicine, (this also applies to the patient, carer, visiting doctor etc) so a<br />
full record is made to avoid accidental overdose.<br />
Also, if the patients nursing records have a running balance of the patients own controlled<br />
drugs this should be maintained by all visiting healthcare professionals.
NURSES WORKING IN THE COMMUNITY<br />
Page 52 of 196<br />
Appendix 16<br />
16.1 Transportation<br />
Nurses should not routinely transport CDs. This should only be undertaken in<br />
circumstances where there is no other reasonable mechanism available. CDs should be<br />
kept out of sight during transportation.<br />
16.2 Administration<br />
Nurse may administer CDs to a patient in their care, as long as they are acting in<br />
accordance with the directions of a doctor or dentist or in accordance with an approved<br />
Patient Group Direction.<br />
Nurse independent prescriber‘s, or nurses acting under the directions of a nurse<br />
independent prescriber, can administer the CDs listed in the table in Appendix O but solely<br />
for the medical conditions specified.<br />
Midwives may administer diamorphine, morphine, pentazocine and pethidine to their<br />
patients, acting on their own professional judgement.<br />
Any CD that is administered by a nurse must be recorded in the nurse‘s and patient‘s notes,<br />
stating the medicine and dose administered, the date of administration, the method of<br />
administration and the person who administered it.<br />
For CDs stored in a patient‘s home, the nurse should keep a running balance. Any<br />
discrepancy must be investigated and reported to the nurse manager, the Head of<br />
Medicines Management and an incident form completed.<br />
16.3 Administration on a verbal instruction<br />
The NMC has published ‗Guidelines for the administration of medicines‘, which includes<br />
guidance on CDs, and is available at:<br />
www.nmc-uk.org/aFrameDisplay.aspx?DocumentID=610<br />
16.4 Disposal of controlled drugs<br />
Prescribed drugs including CDs are the property of the patient and remain so even after<br />
death. However, it is illegal to possess CDs that have not been prescribed for you. In the<br />
first instance the patient/patient‘s relatives should be advised that all CDs no longer<br />
required should be returned to a pharmacy for safe destruction.<br />
It should not normally be the responsibility of the community nurses to become involved in<br />
the disposal of unwanted CDs. However, there may be occasions when it is appropriate for<br />
nursing staff to become involved in recovery/disposal of CDs.<br />
A possible staged approach would be:<br />
If return by relatives/next of kin is not practical or possible then the following action<br />
could be taken<br />
Nurse with another member of the nursing team acting as a witness disposes of CD<br />
in an appropriate and safe manner. This should be within an agreed local SOP and<br />
should include appropriate record keeping in patient‘s notes. See Appendix P and Q<br />
for details on safe disposal of controlled drugs.<br />
Or<br />
Nurse could take CDs to local community pharmacy who would be asked to<br />
countersign patient nursing record.<br />
Appendix 17
PALLIATIVE CARE<br />
17.1 Good Practice<br />
It is good practice to only prescribe quantities of CDs that are needed by the patient for<br />
effective symptom control. This can include CDs for regular dosage, plus a quick-acting CD<br />
at an appropriate dose for breakthrough pain. The good practice principles for managing<br />
CDs described earlier in these guidelines apply equally to the palliative care situation.<br />
Where prescriber‘s are prescribing high doses CDs for palliative care, it is recommended<br />
that the specialist palliative care team are contacted for advice and support, wherever<br />
feasible. Any actions resulting from such a contact should be recorded in the patient‘s<br />
notes.<br />
If a prescriber is prescribing high doses of CDs for a patient, particularly where prolonged<br />
use is expected, then it is recommended that this is reported to the Medicines Management<br />
team at the PCT to aid the interpretation of routine ePACT data.<br />
Palliative care patients may obtain CD prescriptions from more than one source, e.g. GPs,<br />
hospices, hospitals, out-of-hours services and specialist palliative care teams. In such<br />
circumstances, one professional in the locality, could take on a co-ordinating role to avoid<br />
over-supply and to help maintain patient and public safety.<br />
Additional sources of information:<br />
Cancer Care Alliance www.cancernorth.nhs.uk or www.cancercarealliance.nhs.uk<br />
Liverpool Care Pathway www.lep-mariecurie.org.uk<br />
<strong>NHS</strong> End of Life Programme www.endoflifecare.nhs.uk<br />
National Council for Palliative Care www.ncpc.org.uk<br />
PCT Syringe Driver <strong>Policy</strong> http://intranet/PCTServices/2041.htm<br />
17.2 Out-of-hours palliative care<br />
There are sometimes problems encountered with the availability of medicines for palliative<br />
care patients in the community during the out-of-hours period. To maintain effective<br />
symptom control in patients choosing to be treated at home, or in other care environments,<br />
it is important that health care professionals ensure sufficient quantities of appropriate<br />
palliative care drugs, including CDs, are available to anticipate deterioration in the patient‘s<br />
condition. The potential needs of deteriorating conditions need to be balanced with the<br />
safety risk of increased quantities of CDs left in the domiciliary/care setting.<br />
For specific recommendations about the manner in which a patient-centred, high quality<br />
palliative care service can be provided out-of-hours, please refer to ‗Securing proper access<br />
to medicines in the out-of-hours period‘<br />
www.out-of-hours.info/downloads/short_medicines_guidance.pdf<br />
and the accompanying practical guide<br />
www.out-of-hours.info/downloads/medicines_supply_guidance_a_practical_guide.pdf.<br />
And the<br />
PCT Syringe Driver <strong>Policy</strong> – http://intranet/PCTServices/2041.htm<br />
Page 53 of 196
SELF-MEDICATION<br />
Page 54 of 196<br />
Appendix 18<br />
If patients are self-medicating, whether in a hospice or hospital, their CDs should be kept in<br />
a locked metal receptacle immediately adjacent to their bed, or in their bedside locker. The<br />
receptacle should not be readily portable. In order to prevent unauthorised access, each<br />
receptacle should have an individual key, with a master key kept by the person in charge<br />
(on duty).<br />
Where a patient is being treated in their own home, professional advice and supporting<br />
information should be provided in a timely way, by the most appropriate professional, to<br />
ensure safety and efficacy is maintained.
PATIENTS TRAVELLING OVERSEAS<br />
Page 55 of 196<br />
Appendix 19<br />
Travellers carrying prescribed drugs controlled under Schedules 1, 2, 3 and 4 Part I to The<br />
Misuse of <strong>Drugs</strong> Regulations 2001 may require a personal licence.<br />
Persons travelling for over three months either abroad or to the United Kingdom<br />
will need to have a personal licence.<br />
If a person is staying outside their resident country for a period exceeding 3 months<br />
they are advised to register with a doctor in the country they are visiting for the<br />
purpose of receiving further prescriptions.<br />
Persons travelling for three months or fewer will not need a personal export/import<br />
licence.<br />
Applications should be made at least 10 days prior to travel.<br />
Licences are normally issued with an expiry date of one week after the expected return to<br />
the UK.<br />
A personal licence has no legal standing outside the UK and is intended to allow travellers<br />
to pass through the UK customs unhindered.<br />
Other countries may have their own import regulations for controlled drugs.<br />
Travellers should check this with the UK-based representative(s) of the<br />
country/countries to which they are travelling.<br />
Further details and Personal licence application forms can be downloaded from Personal<br />
licences | Home Office - Tackling <strong>Drugs</strong> Changing Lives<br />
It is good practice for CDs to be carried in original packaging in hand luggage with a letter<br />
from the prescribing doctor confirming the carriers name, destination, drug details and<br />
amount.
DESTRUCTION OF CONTROLLED DRUGS<br />
20.1 Stock controlled drugs (including doctor‟s bags)<br />
Stock refers to CDs that have not been issued/dispensed to a patient.<br />
Page 56 of 196<br />
Appendix 20<br />
When Schedule 2 CDs plus temazepam, flunitrazepam, buprenorphine and diethylpropion<br />
pass their expiry date, they should be stored in the CD cabinet/safe or doctors bag (if no<br />
central stock held in practice) until destruction. They should be segregated and clearly<br />
marked as ‗date-expired‘ stock to prevent them being issued in error to patients.<br />
20.1.1 Authorised witnesses<br />
Destruction of obsolete, expired and unwanted Schedule 2 CD stock must be witnessed by<br />
an authorised person.<br />
The following classes of people are currently authorised by the Secretary of State for Health<br />
and the Home Secretary to witness the destruction of CDs: -<br />
Chief dental officer of the DH or a senior dental officer to whom authority has been<br />
delegated<br />
Supervisors of midwives appointed by the Local Supervising Authority<br />
Senior officers in an <strong>NHS</strong> Trust who report directly to the Trust Chief Executive and<br />
who have responsibility for health and safety, security or risk management matters in<br />
the Trust<br />
Chief Executives of <strong>NHS</strong> Trusts<br />
A PCT chief pharmacist or pharmaceutical/prescribing adviser who reports directly to<br />
the chief executive or to a director of the PCT<br />
A registered medical practitioner who has been appointed to the PCT Professional<br />
Executive Committee or equivalent<br />
The PCT board executive member with responsibility for clinical governance or risk<br />
management<br />
Medical director of a PCT<br />
Inspectors of the RPSGB<br />
Police constables<br />
Holders of specific roles within the independent health care sector, for example,<br />
registered managers of independent hospitals.<br />
Public limited companies operating retail pharmacies nominated persons for their<br />
own stock of CDs<br />
Persons in charge or acting person in charge of private hospitals providing palliative<br />
care or hospices wholly or mainly maintained by a public authority out of public funds<br />
or by a charity or by voluntary subscription.<br />
Persons or class of persons authorised by the Accountable Officer<br />
For <strong>County</strong> <strong>Durham</strong> and Darlington PCTs Authorised persons see Appendix Q.<br />
Stock CDs from GP practices, dentists, vets, midwives, community hospitals, Out of<br />
Hours/Urgent Care centres or nursing homes should not be sent to a pharmacy for<br />
destruction. Practices should contact an authorised witness.<br />
An authorised person cannot witness the destruction of CDs that have been supplied to<br />
them or by them – there must be an appropriate separation of roles and responsibilities.
Anyone directly involved with a GP practice, or who is authorised to supply CDs from the<br />
GP practice, e.g. a PCT clinical governance lead working in their own practice, or practice<br />
based pharmacists, must not be asked to witness the destruction of CDs in that GP<br />
practice, even if they are included within the authorised groups.<br />
Home Office <strong>Drugs</strong> Licensing is responsible for the processing of applications for<br />
authorisation to witness the destruction of CDs under Regulation 27(1) of the Misuse of<br />
<strong>Drugs</strong> Regulations 2001. These authorisations cover the holders of specified jobs and<br />
locations within the private sector, e.g. regional managers of major retail pharmacy chains.<br />
For further information, contact the Home Office <strong>Drugs</strong> Licensing on 0207 035 0483 or<br />
email Licensing enquiry. aadu@homeoffice.gsi.gov.uk.<br />
Accountable Officers should not be designated as authorised people to witness destruction<br />
as one of the criteria for Accountable Officers is their independence from day-to-day<br />
management of CDs.<br />
20.1.2 Recording<br />
When a CD is destroyed, details of the drug must be entered into the CD register. This<br />
should include: the name of the drug; form; strength and quantity; the date it was destroyed;<br />
and the signature of the authorised person who witnessed the destruction and the<br />
professional destroying it (i.e. two signatures)<br />
20.2 „Patient-returned‟ controlled drugs<br />
‗Patient-returned‘ CDs are those that have been prescribed for, and dispensed to, a named<br />
patient and then returned unused or part-used for destruction.<br />
<strong>Controlled</strong> <strong>Drugs</strong> (Supervision of Management and Use) Regulations 2006 require SOPs to<br />
be in place for maintaining a record of Schedule 2 drugs that have been returned by the<br />
patients.<br />
It is good practice for pharmacists and doctors to keep a separate book to record all CDs<br />
returned by patients. Although it is not a legal requirement to witness destruction of ‗patientreturned‘<br />
CDs by an authorised witness, good practice would recommend that they are<br />
witnessed by another member of staff and the signature of both the person witnessing and<br />
the person destroying should be entered in a separate book set aside for this purpose<br />
Medicines returned from patient stocks should NOT be re-issued or used to treat other<br />
patients.<br />
For pharmacists, the RPSGB Code of Ethics prevents pharmacists reusing patient returns.<br />
A breach of this requirement could form the basis of disciplinary action.<br />
Community pharmacies can accept CDs returned by patients from their own homes and<br />
from care homes (personal care) for safe destruction and onward disposal even if they did<br />
not originally dispense them.<br />
Pharmacists are not able to accept waste medicines, including CDs, from care homes<br />
(nursing), unless the pharmacy holds a waste management licence. It should be noted<br />
that the definition of ―care services‖ may exclude certain <strong>NHS</strong> premises.<br />
Under the Waste Management Regulations, a pharmacy does not require a Waste<br />
Management Licence to store its own unwanted expired stock, pending disposal. There is<br />
also an exemption in the Waste Management Licence Regulations for the secure storage at<br />
a pharmacy, pending disposal, of waste medicines, which have been returned to the<br />
Page 57 of 196
pharmacy from households or by individuals. This includes waste medicines from a<br />
patient‘s own home or a care home providing residential care, but NOT from a care home<br />
providing nursing care (this is classed as industrial waste).<br />
20.3 Methods of destruction<br />
CDs can be placed into waste containers only after the CD has been rendered irretrievable<br />
(i.e. by denaturing). See Appendix P and Q.<br />
The RPSGB issues guidance on the methods of destruction/denaturing that meet the<br />
requirements of the Misuse of <strong>Drugs</strong> Regulations 2001 and the health and safety needs of<br />
people undertaking the role.<br />
20.4 Environment Agency Regulations and permissions on waste<br />
The destruction and disposal of CDs are also subject to Waste Management Licensing<br />
Regulations 1994. Having considered the risks posed by destruction of CDs in a pharmacy,<br />
the Environment Agency (EA). Which covers England and Wales, has decided that it does<br />
not believe it is in the public interest to expect pharmacies to obtain a waste management<br />
licence for denaturing CDs and this is seen by the EA as a ‗low risk‘ activity. The EA<br />
emphasises, however, that it may amend or revoke its position at any time and will continue<br />
enforcement in all circumstances where activity has or is likely to cause pollution or harm to<br />
health.<br />
For further information on Waste Management Regulation visit the following website:<br />
www.environmentagency.gov.uk.<br />
Guidance on The Hazardous Waste Regulations 2005 can be found on the RPSGB<br />
website:<br />
www.rpsgb.org/pdfs/hazwastehospphguid.pdf. Since the guidance was published, the EA<br />
has agreed that pharmacists may de-blister and otherwise treat waste CDs in a pharmacy<br />
without the need to obtain a licence. Further information on this may be found on the EA<br />
website: www.environment-agency.gov.uk<br />
Page 58 of 196
STANDARD OPERATING PROCEDURES<br />
Page 59 of 196<br />
Appendix 21<br />
Standards for Better Health Core Standard 4d requires each service and practice to have<br />
clear practice policy covering issues relating to the prescribing, ordering, receipt, storage,<br />
monitoring and disposal of controlled drugs. This policy should ensure that there is a full<br />
audit trail for the movement of controlled drugs in primary care form acquisition to<br />
administration and disposal.<br />
Standard operating procedures must be developed which describes the responsibilities and<br />
procedures to provide clarity and consistency for all staff handling controlled drugs within<br />
agreed working practices and current legislation.<br />
Each service should have a designated person responsible for the management of<br />
controlled drugs on the premises.<br />
Each Nursing team should have procedures in place to ensure the safe handling of<br />
controlled drugs in the domiciliary and educational setting.<br />
Baseline information which should be contained in an SOP can be found in Appendix T.
Page 60 of 196<br />
Appendix 22<br />
PATIENT INFORMATION<br />
<strong>NHS</strong> Direct<br />
The <strong>NHS</strong> direct website has developed a Common Health Question about CDs specifically<br />
to inform the public and is available from What is a controlled drug (medicine)? - Health<br />
Questions - <strong>NHS</strong> Direct<br />
Medicines Guides for patients<br />
Medicines guides provide a source of information for members of the public who are looking<br />
for information about individual medicines. Guides for CDs that have been published can be<br />
found at Medicine Guides - Welcome
Appendix A – List of <strong>Controlled</strong> <strong>Drugs</strong> and their Schedules<br />
This list is not exhaustive: it covers the most common drugs encountered in general<br />
practice. Practice computer system may be able to help for specific examples not listed<br />
below. Brand names are not listed except where no generic name exists, or is not<br />
commonly used.<br />
Schedule 1 CDs are drugs with virtually no medical uses, such as cannabis and<br />
hallucinogens. Possession and supply of these drugs is limited to persons granted a special<br />
licence by the Home Office except for Sativex spray. It is not a requirement for a prescribing<br />
doctor or dispensing pharmacist to contact the Home Office in relation to obtaining a licence<br />
to prescribe or supply Sativex spray. The Home Office has also lifted the record-keeping<br />
requirements and, therefore, pharmacists do not need to record Sativex in their CD<br />
registers.<br />
<strong>Controlled</strong> drug<br />
Schedule<br />
<strong>Controlled</strong> drug<br />
Schedule<br />
Amobarbital (Sodium<br />
Amytal<br />
3 Fentanyl 2<br />
Anabolic Steroids 4 (part 2) Flunitrazepam 3<br />
Benzodiazepines<br />
Hydromorphone 2<br />
(Except temazepam,<br />
midazolam,<br />
flunitrazepam)<br />
4 (part 1)<br />
Buprenorphine 3 Kaolin & Morphine<br />
Mixture & tablets<br />
5<br />
Chlordiazepoxide 4 (part 1) Meprobamate 3<br />
Cocaine 2 Methadone 2<br />
Co-codamol 5 Midazolam 3<br />
Codeine<br />
2<br />
Morphine * 2<br />
Oral codeine max<br />
strength
Appendix B Summary of Legal Requirements of the Possession and Supply of CDs<br />
Prescription requirements<br />
Handwriting requirements<br />
Requisitions necessary<br />
Records to be kept in CD register<br />
Emergency supplies allowed<br />
Safe Custody<br />
Date of supply to marked on<br />
prescription<br />
Address of prescriber to be within<br />
the UK<br />
Stock destruction to be witnessed<br />
Validity of prescription<br />
Invoices to be kept for 2 years<br />
Import / export licence required<br />
Yes<br />
No<br />
Yes<br />
Yes<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
28 days<br />
No<br />
Yes<br />
Schedule 2: CD<br />
Secobarbital<br />
Yes<br />
No<br />
Yes<br />
Yes<br />
No<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
28 days<br />
No<br />
Yes<br />
Yes<br />
No<br />
Yes<br />
No<br />
No<br />
No<br />
Yes<br />
Yes<br />
No<br />
28 days<br />
Yes<br />
Yes<br />
Phenobarbital<br />
Yes<br />
No<br />
Yes<br />
No<br />
Yes<br />
No<br />
Yes<br />
Yes<br />
No<br />
28 days<br />
Yes<br />
Yes<br />
Schedule 3: CD No Reg<br />
Temazepam<br />
No<br />
No<br />
Yes<br />
No<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
No<br />
28 days<br />
Yes<br />
Yes<br />
Diethylpropion<br />
Flunitrazepam<br />
(Rohypnol)<br />
Yes<br />
No<br />
Yes<br />
No<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
No<br />
28 days<br />
Yes<br />
Yes<br />
Buprenorphine<br />
(Subutex)<br />
Yes<br />
No<br />
Yes<br />
No<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
No<br />
28 days<br />
Yes<br />
Yes<br />
Schedule 4:<br />
CD Benz and<br />
CD Anab<br />
No<br />
No<br />
No<br />
No<br />
Yes<br />
No<br />
No<br />
No<br />
No<br />
28 days<br />
Yes<br />
Yes<br />
Schedule 5:<br />
CD Inv<br />
No<br />
No<br />
No<br />
No<br />
Yes<br />
No<br />
No<br />
No<br />
No<br />
6 months<br />
Yes<br />
Yes
Appendix C<br />
Relevant Contact Details Re: <strong>Controlled</strong> <strong>Drugs</strong><br />
Contact Title Email Telephone<br />
Dr. Hilton Accountable hilton.dixon@nhs.net<br />
0191 3011300<br />
Dixon Officer for<br />
<strong>County</strong> <strong>Durham</strong><br />
and Darlington<br />
PCTs<br />
Kate<br />
Huddart<br />
Vicki<br />
Vardy<br />
Alison<br />
Hopkins<br />
Paul<br />
Errington<br />
Senior<br />
Pharmaceutical<br />
Adviser for<br />
<strong>County</strong> <strong>Durham</strong><br />
and Darlington<br />
PCTs<br />
<strong>Controlled</strong> Drug<br />
Accountable<br />
Officer Support<br />
and Data<br />
Manager for<br />
<strong>County</strong> <strong>Durham</strong><br />
and Darlington<br />
PCTs<br />
RPSGB<br />
Professional<br />
Standards<br />
Inspector<br />
<strong>Controlled</strong> Drug<br />
and Chemical<br />
Liaison Officer<br />
Kate.huddart@nhs.net 01388 825687<br />
Vicki.vardy@nhs.net 01388 825680<br />
Alison.hopkins@rpsgb.org<br />
020 75722557<br />
Paul.errington@durham.pnn.police.uk 0191 3752626
Appendix D<br />
Information Sharing Code in respect of the operation of the <strong>County</strong> <strong>Durham</strong> and<br />
Darlington Local Intelligence Network for controlled drugs governance<br />
Disclaimer<br />
The contents should not be used as expert opinion, legal or otherwise.<br />
Professional advice should be sought where appropriate. Any liability arising<br />
from action taken in relation to the contents of the Protocol is excluded.<br />
Version 3 November 2009<br />
Page 64 of 196
Information Sharing Code in respect of the operation of the <strong>County</strong> <strong>Durham</strong> and<br />
Darlington Local Intelligence Network for controlled drugs governance<br />
Contents<br />
Section 1 – Background and scope of the Code<br />
Section 2 – Purposes for sharing information<br />
Section 3 – Information to be shared<br />
Section 4 – Arrangements for sharing information<br />
Section 5 – Access and security<br />
Section 6 – Dissemination, monitoring and review<br />
Section 7 – Advice and guidance<br />
Appendices<br />
Appendix 1 – Data Protection and Caldicott principles<br />
Appendix 2 –<strong>County</strong> <strong>Durham</strong> and Darlington Local Intelligence Network<br />
Appendix 3 – Specialist advice and guidance<br />
Page 65 of 196
Section 1<br />
Background and scope of the Code<br />
1.1 Background<br />
Legislation, guidance and Government policy all emphasise the importance of<br />
confidentiality and the protection of personal information. Strong emphasis is also<br />
placed on the need to share information in order to provide effective, integrated<br />
services.<br />
The Heath Act 2006 includes a legal duty of collaboration for local agencies to share<br />
information, within certain constraints, about the use of controlled drugs in the health<br />
and social care sectors. The active duty of collaboration should be manifested through<br />
the operation of a Local Intelligence Network (LIN) through which information can be<br />
shared, analysed and acted upon.<br />
Within the Department of Health Safer Management of controlled drugs: (1) guidance<br />
on strengthened governance arrangements published in January 2007 it states:-<br />
Care should also be taken with sharing information about identifiable health and social<br />
care professional and where possible, they should be made aware of concerns raised<br />
about them. Intelligence networks may wish to agree a code on information-sharing<br />
and nominate a person to be responsible for ensuring the code is followed.<br />
This Information Sharing Code (ISC) has been drawn up by the LIN to assist the<br />
appropriate sharing of information, some of which may be personal information, about<br />
the use of controlled drugs.<br />
The code is intended to reinforce current working practices, give guidance to staff and<br />
be a training resource for new members of staff. It defines the information which will be<br />
transferred between the organisations listed and arrangements for assisting<br />
compliance with relevant legislation and guidance including the Data Protection Act,<br />
1998.<br />
1.2 Framework for confidentiality and information sharing<br />
Four key documents provide the main national framework for information sharing:<br />
Data Protection Act 1998 – This Act provides the main legislative framework for<br />
confidentiality and information sharing issues. The Act stipulates eight principles<br />
(see Appendix 1) that must be followed when personal information is ―processed‖<br />
by organisations. (“Processing” refers to any work done with personal information<br />
including obtaining, recording, viewing, listing, disclosing and destroying.) The Act<br />
stipulates the conditions under which information may be shared i.e. the legal<br />
justifications.<br />
Human Rights Act 1998 – This Act incorporates Article 8 of the European<br />
Convention of Human Rights which provides that everyone has the right to respect<br />
for their private and family life, home and correspondence.<br />
Caldicott Guidance – The Caldicott Committee produced their report on the<br />
―Review of Patient Identifiable Information‖ in December 1997. Caldicott guidance<br />
applies to all <strong>NHS</strong> organisations and local authority Social Services Departments.<br />
Guidance is based on six key principles (see Appendix 1). Organisations are<br />
required to appoint Caldicott Guardians to oversee the confidentiality / information<br />
sharing process.<br />
Page 66 of 196
The <strong>NHS</strong> Confidentiality Code of Practice – The Code of Practice was issued in<br />
July 2003 and applies to all <strong>NHS</strong> organisations. It is a guide to required practice on<br />
confidentiality, security and disclosure of personal information.<br />
The health and social care agencies in <strong>County</strong> <strong>Durham</strong> and Darlington have developed<br />
this Information Sharing Agreement to formalise good practice guidelines for sharing<br />
information with regard to controlled drugs.<br />
1.3 Members of LIN that will work within the code<br />
� <strong>County</strong> <strong>Durham</strong> Primary Care Trust<br />
� Darlington Primary Care Trust<br />
� <strong>County</strong> <strong>Durham</strong> and Darlington Foundation Trust<br />
� Tees, Esk and Wear Valley <strong>NHS</strong> Trust<br />
� Woodlands Hospital, Darlington<br />
� St Cuthbert‘s Hospice<br />
� St Theresa‘s Hospice<br />
� Willowburn Hospice<br />
� The Inspectorate of the Royal Pharmaceutical Society of Great Britain (RPSGB)<br />
� Care Quality Commission<br />
� <strong>Durham</strong> Constabulary<br />
� <strong>County</strong> <strong>Durham</strong> Social Services.<br />
� Darlington Social Services<br />
� North East <strong>NHS</strong> (Strategic Health Authority)<br />
� North East Ambulance Service (NEAS)<br />
� <strong>NHS</strong> Counter Fraud and Security Management<br />
� <strong>Durham</strong> DAAT<br />
� Darlington DAAT<br />
� Prison Cluster representation<br />
As the Local Intelligence Network matures it may be necessary to include any other<br />
responsible body (as defined within the CD regulations) located in <strong>County</strong> <strong>Durham</strong> and<br />
Darlington with a legal obligation to appoint an Accountable Officer and associated<br />
duty to collaborate on issues relating to controlled drugs.<br />
1.4 Approval of the Code<br />
The local intelligence network member‘s representative of the list in Para 1.3 will be<br />
asked to approve the final draft of the code at a LIN meeting, in particular to:<br />
Facilitate the sharing of information on the basis detailed in the code;<br />
Support staff and new members of the local intelligence network in the<br />
implementation of the code through the provision of training, advice and guidance;<br />
Provide relevant information to facilitate monitoring and review.<br />
Page 67 of 196
Section 2<br />
Purposes for sharing information<br />
The purpose of this code is to provide a framework for the sharing of data,<br />
information and knowledge relating to the use, handling, prescribing or<br />
management of controlled drugs (CD) in order to achieve the following:<br />
Section 3<br />
Review or analysis of trends in CD use<br />
Interpretation of CD data in relation to local influences<br />
Identification of persons or groups of people who are managing, using,<br />
prescribing or handling CDs inappropriately or illegally<br />
Identifying “best practice” in the management of CDs (with the exception<br />
of best clinical practice)<br />
Identifying poor systems of control for the management of CDs<br />
Raising concerns relating to any of the above.<br />
Information to be shared<br />
The <strong>Controlled</strong> <strong>Drugs</strong> (Supervision of Management and Use) Regulations 2006 state<br />
that there is an active duty to share any information that<br />
―[An organisation that is party to this agreement] may disclose to any other<br />
[organisation that is party to this agreement] any information in its possession or<br />
control which it reasonably considers it should share with that body for the purposes<br />
of—<br />
(a) identifying cases in which action may need to be taken in respect of matters arising<br />
in relation to the management or use of controlled drugs by a relevant person;<br />
(b) the consideration of issues relating to the taking of action in respect of such<br />
matters;<br />
(c) the taking of action in respect of such matters.‖<br />
Such information may include but is not restricted to data extracted from:<br />
Prescribing reports (e-PACT) for GPs, Dentists, Nurse prescribers and private<br />
prescribers of CDs<br />
Records of ordering , receipt and dispensing of CD‘s<br />
Records of administration of CDs within hospitals and hospices<br />
Records of the destruction of CDs in any setting<br />
e-PACT reports generated that detail the dispensing of controlled drugs by<br />
pharmacies<br />
Records of the supply of ward CD stationary<br />
Records of supply of FP10PCD prescriptions to private prescribers<br />
Records of supply of CDs from wholesalers<br />
Records of issues to wards and departments from the JAC system or similar<br />
stock management system in hospitals<br />
Routine stock checks of CDs held in wards and departments in hospitals and<br />
hospices<br />
Records of Drug Testing and Treatment Orders<br />
Records of arrests for drug related crime<br />
Information discerned from any of the above that will provide:<br />
Page 68 of 196
Patterns or trends in the prescribing, ordering, receipt, dispensing,<br />
administration or destruction of controlled drugs on an individual practitioner,<br />
collection of practitioners or population basis.<br />
Details of anomalies within the prescribing, ordering, receipt, dispensing,<br />
administration or destruction of controlled drugs on an individual practitioner,<br />
collection of practitioners or population basis.<br />
Details of CDs, the whereabouts of which cannot be ascertained.<br />
Identification of areas or activities for which record keeping is not adequate<br />
Patterns or trends in activities relating to the enforcement of controlled drugs<br />
legislation.<br />
Information or knowledge regarding causes for concern relating to CD use or<br />
management, actual or suspected, derived from:<br />
A complaint or the analysis of complaints<br />
An incident report or the analysis of incident reports<br />
The conduction or results of an investigation into an incident or complaint<br />
―Whistle-blowing‖ or other report of a concern relating to professional conduct or<br />
performance.<br />
Confiscation of controlled drugs that have been possessed illegally.<br />
The report or investigation of an alleged or actual criminal act relating to<br />
controlled drugs<br />
A report resulting from an inspection carried out by the RPSGB, CSCI, HCC or<br />
PCT.<br />
Communications from <strong>NHS</strong> Counter Fraud & Security Management Services<br />
(<strong>NHS</strong> CF&SMS).<br />
Where a concern has been raised information may be shared that includes any of the<br />
above in addition to or contained within the following:<br />
―Occurrence Reports‖ (as defined in the 2006 regulations)<br />
Reports of a concern where evidence or information has been collated.<br />
The agenda, minutes and reports of a LIN incident panel.<br />
Letters of referral to regulatory, indemnifying or representative bodies.<br />
Referrals to the police or <strong>NHS</strong> CF&SMS<br />
Minutes of meetings of the LIN<br />
Personal information may include:<br />
The person‘s name, and or any aliases they live under<br />
The person‘s address(s)<br />
The person‘s occupation<br />
The person‘s age and date of birth.<br />
The person‘s sex<br />
Information about the person‘s social circumstances (which may include<br />
references to ethnicity)<br />
Information about the person‘s health or healthcare<br />
Information relating to the person‘s alleged or proven, past or present criminal<br />
offences<br />
The person‘s movements, habits, conduct or practises.<br />
Page 69 of 196
Section 4<br />
Arrangements for sharing information<br />
4.1 Provision of information<br />
Information which is not personally identifiable information will be shared in any<br />
of the following formats:<br />
Face to face & telephone conversation<br />
Post<br />
Fax<br />
e-mail<br />
Where information identifies an organisation or practice (or similar collective)<br />
information will be shared in the following ways:<br />
Face to face & telephone conversation<br />
Post using recorded/special delivery<br />
Secure fax (or secure faxing method)<br />
e-mail using a password protected file<br />
Where information identifies an individual or could be used to identify an<br />
individual the following methods will be used:<br />
Face to face & telephone conversation conducted in privacy<br />
Post using recorded delivery<br />
Safe Haven Fax or secure faxing method<br />
4.2 Consent from service users<br />
4.2.1 Sharing with Consent<br />
If an organisation wishes to disclose information under this code that contains person<br />
identifiable information but this information is not required for the purposes of<br />
identifying cases in which action may need to be taken, the organisation must remove<br />
the person identifiable information. If this is not possible or the organisation considers it<br />
necessary to disclose person identifiable information, the organisation must, where<br />
practicable, obtain the consent of the patient to whom the information relates. In such<br />
cases only the minimum amount of person identifiable information will be disclosed.<br />
4.2.2 Other Justifications for Sharing<br />
Where it is not appropriate to use consent as the basis for sharing information, the<br />
following justifications may be applicable:<br />
Information shared for medical purposes between health professionals<br />
Information can be shared if it is for medical purposes and is shared between<br />
health professionals. The terms ―medical purposes‖ and ―health professionals‖<br />
are defined in the Data Protection Act.<br />
Serious harm<br />
It may be justified to share information where there is evidence that serious<br />
harm would be caused to the service user, (or another person) if this was not<br />
Page 70 of 196
done. This may arise for example in relation to child, adult or public protection<br />
issues.<br />
Vital interests<br />
Information may be shared where this is in the ―vital interests‖ of the service<br />
user or another person. This refers to life or death circumstances.<br />
Prevention or detection of crime<br />
Personal information may be provided to the Police where this is necessary for<br />
the prevention or detection of crime. This is a power not an obligation. A<br />
judgement needs to be made in each case as to whether it is appropriate to<br />
release information taking into account the following criteria. Advice should be<br />
sought if there is uncertainty about interpreting these criteria. Information should<br />
only be disclosed where:<br />
- without disclosure the task of preventing or detecting crime would be<br />
prejudiced;<br />
- information shared is limited to what is strictly relevant to a specific<br />
investigation;<br />
- there are satisfactory undertakings that the information will not be used for<br />
any other purpose than the specific investigation.<br />
It may also be appropriate to disclose information under Section 29 of the Data<br />
Protection Act in response to investigations by the <strong>NHS</strong> Counter Fraud and<br />
Security Management Service (CF&SMS). Service Users should not be<br />
informed about information disclosed unless the appropriate officer of the<br />
CF&SMS concurs.<br />
Court Order<br />
Information must be shared where the service is instructed to do so by a Court<br />
(including a Coroner‘s Court.)<br />
Wherever possible and appropriate service users should be informed if their<br />
information is to be shared without consent.<br />
4.2.3 Confidentiality<br />
The right to confidentiality is extended to all persons including clinicians, unless an<br />
organisation considers that disclosure is necessary for:<br />
(a) identifying cases in which action may need to be taken in respect of matters arising<br />
in relation to the management or use of controlled drugs by a relevant person;<br />
(b) the consideration of issues relating to the taking of action in respect of such<br />
matters;<br />
(c) the taking of action in respect of such matters<br />
The sharing of information relating to the management of controlled drugs is facilitated<br />
by the operation of the Local Intelligence Network. The framework under which the LIN<br />
operates is provided in Appendix 2<br />
Page 71 of 196
Section 5<br />
Access and security<br />
5.1 Need to know<br />
All the members of the LIN may be privy to information as detailed in section 3.<br />
Sharing of the information detailed in section 3 that has been made available to the<br />
LIN within a recipient organisation will be restricted to those persons who need the<br />
information to carry out their duties in relation to the investigation of a concern. In such<br />
circumstances the organization will be bound by its own information governance or<br />
confidentiality policy as well as the Data Protection Act 1998.<br />
5.2 Secure storage and transfer of personal information<br />
Steps should be taken by all members of LIN to ensure that personal information is<br />
held and transmitted securely. Organisations should ensure that their staff have<br />
access to their policies on Confidentiality and Information Security and <strong>NHS</strong> staff have<br />
access to the <strong>NHS</strong> Confidentiality Code of Practice. (See Appendix 3 for details).<br />
Guidance on security issues is given in the Procedures Section B of the Information<br />
Sharing Protocol.<br />
5.3 Retention of records<br />
Files relating to an individual‘s controlled drugs management will remain active for the<br />
duration of time practitioners continue to practice within the <strong>County</strong> <strong>Durham</strong> and<br />
Darlington LIN area. The files will be archived once practitioners cease to practice in<br />
the <strong>County</strong> <strong>Durham</strong> and Darlington LIN area and retained for a period of 25 years to<br />
provide evidence if required in any future litigation which may be brought.<br />
Each organisation that is party to this agreement has responsibility for retaining<br />
information that relates to practitioners within their scope of responsibility.<br />
Files of information that arise from an investigation of a LIN incident panel will be<br />
retained by the PCT Accountable Officer or his/her deputy until such time as the<br />
concern is resolved. Once resolution is achieved the files will be transferred to the<br />
most appropriate organisation to be kept with the practitioner‘s individual file.<br />
CD files relating to individual practitioners may be passed on to other Accountable<br />
Officers at their request should a practitioner move from the area covered by the LIN<br />
into another LIN area.<br />
The Accountable Officer of each organisation or for organisations without an<br />
Accountable Officer the LIN member will act as the data controller for shared data<br />
originating in their respective organisation.<br />
Section 6<br />
Dissemination, monitoring and review of the Code<br />
LIN Members will make copies of the code and the protocol available to all<br />
relevant staff and on request to service users. Partners will ensure that<br />
appropriate training is provided to all relevant staff.<br />
LIN Members should ensure they are familiar with the requirements of The<br />
<strong>Controlled</strong> <strong>Drugs</strong> (Supervision of Management and Use) Regulations 2006 and<br />
with their internal policies relating to the implementation of these regulations.<br />
Page 72 of 196
Section 7<br />
LIN Members should investigate any breaches of the code and ensure that<br />
problems are addressed as promptly as possible within their partner<br />
organisations.<br />
The code will be reviewed every twelve months. Changes to the code will not be<br />
considered during this period unless they are required urgently.<br />
As part of the review process all LIN members will be asked about use of the<br />
code, any proposals they may have for addressing specific problems and any<br />
amendments they feel are necessary.<br />
Advice and guidance<br />
Sources of advice about confidentiality and information sharing issues are included in<br />
Appendix 3 of the agreement.<br />
Details of relevant additional guidance are given in Appendix 3.<br />
Page 73 of 196
Appendix 1 of Information sharing Code - Key principles<br />
The eight principles of the Data Protection Act:<br />
1.Fair and lawful: Personal data shall be processed fairly and lawfully and, in<br />
particular, shall not be processed unless certain conditions are met, also the<br />
processing must adhere to the fair processing code.<br />
2. Use for specified purposes: Personal data shall be obtained only for one or more<br />
specified purposes, and shall not be further processed in any manner incompatible<br />
with that purpose or purposes.<br />
3. Adequate, relevant and not excessive: Personal data shall be adequate, relevant<br />
and not excessive in relation to the purpose.<br />
4. Accurate and up to date: Personal data shall be accurate and, where necessary,<br />
kept up to date.<br />
5. Don‟t keep longer than necessary: Personal data processed for any purpose or<br />
purposes shall not be kept longer than is necessary for that purpose or those<br />
purposes.<br />
6. Rights given under the act: Personal data shall be processed in accordance with<br />
the rights of the data subject under this act‖.<br />
7. Security: Appropriate and organisational measures shall be taken against<br />
unauthorised or unlawful processing of personal data and against accidental loss or<br />
destruction of, or damage to, personal data.<br />
8. Disclosure outside Europe: Personal data shall not be transferred to a country<br />
outside the European Economic area, without adequate protection.<br />
The six Caldicott Principles:<br />
1. Define Purposes: Every proposed use or transfer of patient-identifiable information<br />
within or from an organisation should be clearly defined and scrutinised, with<br />
continuing uses regularly reviewed, by an appropriate guardian.<br />
2. Use anonymised information if possible: Patient-identifiable information items<br />
should not be included unless it is essential for the specified purpose. The need for<br />
patients to be identified should be considered at each stage of satisfying the purpose.<br />
3. Use the minimum information necessary: The minimum amount of identifiable<br />
information should be transferred or made accessible that is necessary for a given<br />
function to be carried out.<br />
4. Access to personal information on a need to know basis: Only those individuals<br />
who need access to patient-identifiable information should have access to it, and they<br />
should only have access to the information items that<br />
they need to see. This may mean introducing access controls or splitting information<br />
flows where one information flow is used for several purposes.<br />
5. Staff must be aware of their responsibilities: Action should be taken to ensure<br />
that those handling patient-identifiable information – both clinical and non-clinical staff<br />
– are made fully aware of their responsibilities and obligations to respect patient<br />
confidentiality.<br />
6. Use only when lawful: Every use of patient-identifiable information must be lawful.<br />
Page 74 of 196
Appendix 2 of Information Sharing Code<br />
Framework for a <strong>Controlled</strong> <strong>Drugs</strong> Local Intelligence<br />
Network.<br />
Introduction<br />
The Heath Act 2006 includes a legal duty of collaboration for local agencies to share<br />
information, within certain constraints, about the use of controlled drugs in the health<br />
and social care sectors. The duty of collaboration should be manifested through the<br />
operation of a local intelligence network through which information can be shared,<br />
analysed and acted upon.<br />
Remit<br />
The remit of the group is twofold:<br />
1. To comply with the duty of collaboration as defined by the Health Act 2006 (and<br />
related regulations) with regard to identifying and resolving issues of<br />
a. poor management of controlled drugs<br />
b. poor clinical/professional handling or use of controlled drugs.<br />
2. To act as a forum for the dissemination of best practice in the 2006 (and related<br />
regulations) with regard to identifying and resolving management of controlled<br />
drugs.<br />
Area of operation<br />
The local intelligence network covers the people living or working in the geographical<br />
area of <strong>County</strong> <strong>Durham</strong> and Darlington<br />
Membership of the network<br />
The Accountable Officers of healthcare organisations within the defined boundaries. (A<br />
named and fully informed deputy of the accountable officer may be nominated in place<br />
of the organisations Accountable Officer)<br />
Named representatives from the organisations below:<br />
� Care Quality Commission (CQC)<br />
� The inspectorate of the Royal Pharmaceutical Society of Great Britain (RPSGB)<br />
� The Healthcare Commission<br />
� The Police<br />
� Local Authority provided Social Services Department<br />
� North East <strong>NHS</strong> (Strategic Health Authority)<br />
A non-executive director who will offer lay representation.<br />
In addition the network should include input from the following where such expertise is<br />
not already found in the group:<br />
� Chief pharmacists<br />
� Medical directors<br />
� Nursing directors,<br />
� Social care providers and<br />
� <strong>Clinical</strong> governance leads of the healthcare organisations<br />
� Representatives of local wholesale dealers<br />
The network will be chaired by the PCT Accountable Officer who will have the<br />
additional responsibility of liaising with representatives of neighbouring local<br />
intelligence networks.<br />
Page 75 of 196
It remains the duty of each organisation to ensure full clinical engagement in the<br />
management of controlled drugs within its area of responsibility.<br />
Meeting Arrangements<br />
Regular communication will be necessary to share information of non-specific trends<br />
(for example an increase or decrease in the number of patients receiving palliative<br />
care) and to advise the network of any issues relating the quality or effectiveness of<br />
the information that is available for monitoring purposes. This will predominantly be<br />
done using teleconferencing or e-mail.<br />
Initially the members of the network will meet formally four times a year.<br />
On occasions where concerns are raised ad-hoc meetings are to be called, by the<br />
responsible Accountable Officer, that includes only those members of the network on<br />
whom the concern will impact. It will remain the duty of the responsible accountable<br />
officer to escalate the concern to the full network if they consider this to be necessary<br />
and co-ordinate the necessary meetings.<br />
Contact Management<br />
For use when causes of concern require rapid sharing of information to safeguard the<br />
public, the network maintains a list of emergency contacts for each organisation which<br />
can be used when the member of the group (or the relevant accountable officer) is not<br />
contactable (e.g. during annual leave). Wherever possible an out-of-hours contact will<br />
also be maintained.<br />
The PCT Accountable Officer is responsible for maintaining this list and testing its<br />
operation.<br />
Information sharing<br />
An information sharing agreement will be developed and subsequently adopted by<br />
each responsible organisation that will enable collaboration as outlined below.<br />
Each organisation should decide what information is shared routinely and the<br />
frequency in which this information is produced or updated based upon the validity and<br />
reliability of the data.<br />
Only information that is useful to partner organisations should be shared. Such<br />
information may be useful by means of providing context to the interpretation of other<br />
data, complimenting other data, direct addition to other data or increasing the pool of<br />
collective knowledge.<br />
Data may include:<br />
� Complaints<br />
� Incident reports<br />
� Whistle blowing<br />
� Reports from visits or inspections<br />
� Self declarations from CD holders<br />
And where there is good validity and reliability:<br />
� Concerns raised during performance review<br />
� Analysis of prescribing trends<br />
� Analysis of dispensing trends<br />
And in the future<br />
� Wholesaler/supply chain reports<br />
� Records of administration<br />
Page 76 of 196
Other information or knowledge may include:<br />
� Interpretation of data<br />
� Changes to clinical practice<br />
� Police activity<br />
� Reasonable suspicion, conjecture, speculation and predictions.<br />
The network recognises that in the course of implementing better management of<br />
controlled drugs areas of practice which do not comply with the letter of the law will be<br />
uncovered. Where an undertaking is made by the professional concerned to remedy<br />
the problems and such problems are considered not to be due to an unsafe disregard<br />
for the law or to malicious intent, such discrepancies do not automatically require<br />
raising as a concern to the network.<br />
The body of data to be routinely collated will be developed over time as systems are<br />
devised that allow the production of a consistent data set. A centralised secure<br />
repository of information will be established once a technological solution can be<br />
found. It will remain the responsibility of the producing organisation to securely store<br />
and archive the information it produces.<br />
During the course of responding to a concern each organisation will make available<br />
data or information in an open and timely manner on the request of a member of the<br />
network.<br />
In the process for raising a concern to the local intelligence network each organisation<br />
continues to be responsible for monitoring use of controlled drugs by its staff, patients<br />
and clients. The tools that the organisations use should be operated in such a manner<br />
that the threshold that any anomaly has to cross before an enquiry is made is very low.<br />
This low threshold will trigger enquiries that in the most part will be explained by the<br />
normal variation in practice. Any anomalies that are not sufficiently accounted for, or<br />
leave room for doubt will be highlighted to the local intelligence network. When an<br />
anomaly is first highlighted to the local intelligence network it should be anonymous<br />
unless the cause for concern is proven and serious. Anonymous reports will be<br />
compared for patterns or similarities and only if a pattern or similarity is observed will<br />
identifying details be exchanged.<br />
Confidentiality rules should be maintained at all times and this is the responsibility of<br />
the organisational lead. When sharing this becomes essential to take an investigation<br />
further then all other parties are bound by the same rules.<br />
Where concerns have been dealt with without the need to involve the whole network<br />
the responsible accountable officer should circulate a report of the concern and its<br />
subsequent resolution to inform the whole network.<br />
Administrative Support<br />
The PCT hosts administrative support that:<br />
� Co-ordinates the meetings and activities of the network,<br />
� Acts as a librarian for shared data and information and<br />
� Collates and analyses data and information in response to a concern being<br />
raised and elevated to include the whole network.<br />
All other administrative support remains the responsibility of the organisations within<br />
the network.<br />
Page 77 of 196
Appendix 3<br />
Additional guidance and key contacts<br />
Guidance<br />
The <strong>Controlled</strong> <strong>Drugs</strong> (Supervision of Management and Use) Regulations 2006:<br />
www.opsi.gov.uk/si/si2006/20063148.htm<br />
The Data Protection Act 1998 can be accessed via the Information<br />
Commissioner‘s website at www.informationcommissioner.gov.uk<br />
The <strong>NHS</strong> Confidentiality Code of Practice is available at<br />
www.dh.gov.uk/ipu/confiden<br />
Caldicott requirements are available at www.dh.gov.uk<br />
Specialist advice: contact details<br />
In relation to controlled drugs governance and management:<br />
Kate Huddart<br />
Senior Pharmaceutical Adviser<br />
Medicines Management (Commissioning)<br />
<strong>County</strong> <strong>Durham</strong> and Darlington Primary Care Trusts<br />
Merrington House<br />
Merrington Lane Industrial Estate<br />
Spennymoor<br />
<strong>County</strong> <strong>Durham</strong><br />
DL16 7UT<br />
Tel: 01388 82 5687<br />
Email: kate.huddart@nhs.net<br />
In relation to information sharing and the Data Protection Act<br />
Kevin Garrigan<br />
Information Governance Manager<br />
Tel: 0191 301 3820<br />
Email: kevin.garrigan@nhs.net<br />
Page 78 of 196
Appendix E<br />
<strong>Controlled</strong> <strong>Drugs</strong> Practice Declaration & Self Assessment audit for<br />
GP Practices 2009/2010<br />
Please complete the form below:<br />
Name of organisation/Practice<br />
Address of organisation/Practice<br />
Telephone Number<br />
Name of person completing form (Please<br />
print name)<br />
PPA Practice Code i.e. A12345<br />
Please indicate which applies to you: (please tick box)<br />
GP Nurse Practice Manager Other<br />
Please complete the relevant parts of the questionnaire below. This questionnaire relates to activities,<br />
since October 2008 and relates to schedule 2 and 3 <strong>Controlled</strong> <strong>Drugs</strong> (CDs) including Midazolam &<br />
Temazepam, as they are subject to a higher level of control.<br />
Area of activity Yes/No If answer is YES<br />
Question 1 Does the practice write/print<br />
prescriptions for CDs?<br />
Question 2 Does the practice supply or<br />
dispense CDs?<br />
Question 3 (i) a. Are CDs stocked either on the<br />
premises or off site? E.g. in<br />
doctor‘s bag/Emergency box.<br />
(ii)<br />
Question 4 Do you destroy or dispose of CDs<br />
(patient returns/stock) in the<br />
practice?<br />
Page 79 of 196<br />
Please complete<br />
TABLE A and<br />
SECTION 1<br />
Please complete<br />
TABLE A and<br />
SECTION 2<br />
Please complete<br />
TABLE A and<br />
SECTION 3<br />
Please complete<br />
TABLE A and<br />
SECTION 4
<strong>Controlled</strong> <strong>Drugs</strong> Practice Declaration Statement for GP Practices 2009/2010<br />
In ALL cases please delete as applicable and sign the declaration below:<br />
a) I declare to the best of my knowledge and belief that the organisation/practice does not handle,<br />
use or manage Schedule 2 or 3 CDs on any premises from which I provide clinical services.<br />
OR<br />
b) I declare that to the best of my knowledge and belief that I do/do not comply (please delete as<br />
appropriate) with the provisions of the Misuse of <strong>Drugs</strong> Act 1971 and the associated Regulations in its<br />
handling, use, prescribing and management of schedule 2 and 3 CDs.<br />
Signature*<br />
Name and registration number<br />
Date of Signing<br />
* This form must be signed by appropriately authorised personnel, who have responsibility for the management<br />
and use of CDs within the organisation/Practice.<br />
Please note that you must notify us of any material changes to the answers to questions 1 to 4 within 14<br />
days of change.<br />
Please return your completed <strong>Controlled</strong> Drug Declaration to:<br />
Vicki Vardy<br />
<strong>Controlled</strong> Drug Accountable Support & Data Manager<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong><br />
Merrington House<br />
Merrington Lane Ind estate<br />
Spennymoor<br />
CO. <strong>Durham</strong><br />
DL16 7UT<br />
Telephone number; 01388 285680<br />
Vicki.vardy@nhs.net<br />
Page 80 of 196
TABLE A: General Information; Please complete in ALL cases<br />
Does the practice have written standard<br />
operating procedures or written policies<br />
covering the handling and management<br />
of CDs, appropriate to the activities<br />
carried out at the premises?<br />
Does the practice have in place a local<br />
procedure for dealing with a significant<br />
event* involving CDs?<br />
Does the practice have appropriate<br />
procedures for the initial and continuing<br />
training or development of all staff<br />
involved in the prescribing, handling,<br />
supply and administration of CDs?<br />
Are there any specific restrictions (iii) that<br />
have been applied that would affect the<br />
handling/prescribing/supply/administration<br />
of CDs by any of the healthcare<br />
professionals involved with your practice?<br />
Yes/No Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 81 of 196
Section one:<br />
Prescribing of CDs<br />
Have there been any patient or carer<br />
complaints* involving the prescribing of<br />
CDs by your practice?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about unusual,<br />
excessive or inappropriate prescribing of<br />
CDs by your practice?<br />
Have there been any significant events (iv) **<br />
involving the prescribing of CDs within<br />
your practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
* This includes complaints about failing to prescribe appropriate doses and/or appropriate medicines<br />
** Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 82 of 196
Section Two:<br />
Supply/Dispensing of CDs<br />
Does the practice supply/dispense CDs<br />
as part of substance misuse treatment?<br />
If so, are the drugs checked against the<br />
prescription by a GP when<br />
supplying/dispensing?<br />
Does the practice supply/dispense CDs<br />
against private prescriptions:<br />
a) For or from substance misuse<br />
services?<br />
b) Elsewhere?<br />
Does the practice supply CDs against (v) a<br />
signed order:<br />
a) To doctors?<br />
b) To others (not including patients)?<br />
From where does your practice obtain (vi)<br />
stocks of CDs?<br />
Does your practice provide advice (vii) to<br />
patients on the safekeeping and disposal<br />
of unwanted CDs within your practice?<br />
Are patient returned medicines ever (viii) reused<br />
in the practice?<br />
Are patient information leaflets supplied (ix)<br />
to all patients supplied/dispensed CDs by<br />
the practice?<br />
Have there been any patient or carer<br />
complaints involving the<br />
supply/dispensing of CDs in your<br />
practice?<br />
(x)<br />
Have there been any concerns expressed (xi)<br />
by colleagues, police, drugs misuse<br />
service or others about CDs<br />
supply/dispensed from the organisation<br />
/practice?<br />
Have there been any significant events* (xii)<br />
involving the supply/dispensing of CDs<br />
from your practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 83 of 196
Section Three:<br />
3.1) Security and safe custody of CDs on premises<br />
Does the practice store CDs in:<br />
a) A central store? (e.g. A single<br />
cupboard that holds all CD stocks for the<br />
practice)<br />
b) Doctors bags?<br />
c) Other places (please details)?<br />
Are all CDs (including patient returned<br />
CDs or unwanted/obsolete CDs) are kept<br />
locked in a cupboard that complies with<br />
BS2881 (a metal cupboard with an<br />
internal locking system)?<br />
Is access to CDs controlled within (xiii) your<br />
practice?<br />
e.g. Keys held only by appropriate staff<br />
If yes, then who?<br />
Do you utilise the CD storage facilities (xiv)<br />
for storage of anything other than CDs?<br />
If so, please state<br />
How often does date checking of (xv) CD<br />
stock take place in your practice?<br />
Give details of date checking procedures<br />
How often does date checking of (xvi) CD<br />
stock in Doctors bags take place?<br />
(where applicable)<br />
Please give details of date checking<br />
procedures<br />
Are all stock CDs kept in the original (xvii)<br />
manufacturers pack within the practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 84 of 196
If a dispensing practice,are dispensed<br />
patients medicines appropriately labelled<br />
in the practice?<br />
Are different strengths of the same<br />
medicine segregated in any way?<br />
Do you have out of date or obsolete<br />
stock CDs currently stored in the<br />
practice?<br />
Are out of date/obsolete/patient returned (xviii)<br />
CDs segregated from other in date CDs<br />
in the practice?<br />
If Yes, where?<br />
Are patient returned medicines (xix) ever<br />
reused in the practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
3.2) Security and Safe custody of CDs in transport<br />
Do you transport or are you responsible<br />
for the transport of CDs (this includes<br />
sending CDs using third party carriers<br />
such as delivery drivers and postal<br />
system) to other sites?<br />
If NO, please move on to section 3.3<br />
What procedure do you have in place for<br />
the transport of CDs in the practice?<br />
Are CDs routinely kept under lock and<br />
key during transport?<br />
If No, then please provide details.<br />
What records are maintained of CDs in<br />
transport?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 85 of 196
3.3) Security and Safe custody of CD registers<br />
Yes/No or Details<br />
N/A<br />
Do you keep an up to date CD register in<br />
the practice?<br />
Do you keep running balances of stock<br />
CDs held?<br />
If yes:<br />
a) Do you audit your running totals?<br />
(state how often and date of last<br />
audit)<br />
b) Are the running totals audited by<br />
an independent 3 rd party (i.e. PCT<br />
staff)? (state how often and date of<br />
last audit)<br />
Have you identified any discrepancies<br />
between running totals and actual CD<br />
balances, since October 2008 in the<br />
practice?<br />
If yes:<br />
a) What was the explanation for the<br />
discrepancy?<br />
b) What action was taken?<br />
Do you maintain records of all receipts<br />
and supplies of CDs within your practice?<br />
If yes, for how long do you keep records?<br />
Have there been any patient or carer<br />
complaints involving the storage,<br />
transport or record keeping of CDs in the<br />
practice?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about the storage,<br />
transport or record keeping of CDs in the<br />
practice?<br />
Have there been any significant events*<br />
involving the storage, transport or<br />
recording keeping of CDs?<br />
Page 86 of 196
Section Four:<br />
Destruction and Disposal of CDs<br />
Patients Returned CDs<br />
What records do you keep of CDs<br />
returned to you by patients for disposal<br />
within the practice? (Where applicable)<br />
Do you routinely destroy patients old or<br />
obsolete CDs in the practice?<br />
What arrangements do you have in place<br />
to dispose of patients old or obsolete CDs<br />
in the practice?<br />
Is the destruction of patients old or<br />
obsolete CDs witnessed in the practice?<br />
If yes, by whom?<br />
Do you keep records of the destruction of<br />
patients old or obsolete CDs in the<br />
practice?<br />
Stock CDs (if applicable)<br />
How often do you aim to destroy out of<br />
date or obsolete stock CDs in the<br />
practice?<br />
Do you have any out of date or obsolete<br />
stock CDs currently awaiting destruction?<br />
Who usually witnesses your stock CDs<br />
destruction?<br />
When was the last witnessed CD stock<br />
destroyed?<br />
Are records of stock destruction kept in<br />
the CD register within the practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 87 of 196
Have there been any patient or carer<br />
complaints involving the destruction or<br />
disposal of CDs in the practice?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about the destruction<br />
or disposal of CDs in the practice?<br />
Have there been any significant events*<br />
involving the destruction or disposal of<br />
CDs in the practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Please return your completed self assessment audit to:<br />
Vicki Vardy<br />
<strong>Controlled</strong> Drug Accountable Support & Data Manager<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong><br />
Merrington House<br />
Merrington Lane Ind estate<br />
Spennymoor<br />
CO. <strong>Durham</strong><br />
DL16 7UT<br />
Telephone Number; 01388 825680<br />
Vicki.vardy@nhs.net<br />
Page 88 of 196
Appendix F<br />
<strong>Controlled</strong> <strong>Drugs</strong> Personal Declaration & Self Assessment audit for<br />
individual GPs 2009/2010<br />
Please complete the form below:<br />
Name of Clinician<br />
Address of main workplace<br />
Telephone Number<br />
Name (Please print name)<br />
GMC Number<br />
Please indicate which applies to you: (please tick box)<br />
Partner GP Salaried GP Locum GP Other<br />
Please complete the relevant parts of the questionnaire below. This questionnaire relates to activities<br />
since October 2008 and relates to schedule 2 and 3 <strong>Controlled</strong> <strong>Drugs</strong> (CDs) including Midazolam &<br />
Temazepam, as they are subject to a higher level of control.<br />
Question 1<br />
Question 2<br />
Question 3<br />
Area of activity Yes/No If the answer is YES<br />
Do you prescribe CDs? Please complete TABLE A<br />
and SECTION 1<br />
Do you supply CDs? Please complete TABLE A<br />
and SECTION 2<br />
Do you administer CDs (or<br />
supervise or assist patients own<br />
administration)?<br />
Question 4 (xx) a. Do you keep a stock of CDs?<br />
(xxi) e.g. In doctor‘s bag.<br />
(xxii) b. Do you keep patients CDs?<br />
Question 5 Do you destroy or dispose of CDs<br />
(patient returns/stock)?<br />
Please complete TABLE A<br />
and SECTION 3<br />
Please complete TABLE A<br />
and SECTION 4<br />
Please complete TABLE A<br />
and SECTION 5<br />
Page 89 of 196
<strong>Controlled</strong> <strong>Drugs</strong> Personal Declaration Statement for individual GPs<br />
2009/2010<br />
In ALL cases please delete as applicable and sign the declaration below:<br />
c) I declare to the best of my knowledge and belief that I do not handle, use or manage<br />
Schedule 2 or 3 CDs.<br />
OR<br />
d) I declare that to the best of my knowledge and belief that I do/do not comply (please delete as<br />
appropriate) with the provisions of the Misuse of <strong>Drugs</strong> Act 1971 and the associated Regulations in its<br />
handling, use, prescribing and management of schedule 2 and 3 CDs.<br />
Signature*<br />
Name and registration number<br />
Date of Signing<br />
Please note that you must notify us of any material changes to the answers to questions 1 to 5 within 14<br />
days of change.<br />
Please return your completed declaration to:<br />
Vicki Vardy<br />
<strong>Controlled</strong> Drug Accountable Support & Data Manager<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong><br />
Merrington House<br />
Merrington Lane Ind estate<br />
Spennymoor<br />
CO. <strong>Durham</strong><br />
DL16 7UT<br />
Telephone Number; 01388 825680<br />
Vicki.vardy@nhs.net<br />
Page 90 of 196
TABLE A: General Information; Please complete in ALL cases<br />
Do you have written standard operating<br />
procedures or written policies covering<br />
the handling and management of CDs,<br />
appropriate to the activities carried out at<br />
the premises?<br />
Do you have in place a procedure for<br />
dealing with a significant event* involving<br />
CDs?<br />
Do you have appropriate arrangements in<br />
place, for ongoing personal<br />
development/training<br />
CDs?<br />
with regards to<br />
Are there any specific restrictions (xxiii) that<br />
have been applied that would affect the<br />
handling/prescribing/supply/administration<br />
of CDs by yourself?<br />
Yes/No Details<br />
* Significant event include any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 91 of 196
Section one:<br />
Prescribing of CDs<br />
Have there been any patient or carer<br />
complaints* involving the prescribing of<br />
CDs by you?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about unusual,<br />
excessive or inappropriate prescribing of<br />
CDs by you?<br />
Have there been any significant events (xxiv) **<br />
involving the prescribing of CDs by you?<br />
Yes/No or<br />
N/A<br />
Details<br />
* This includes complaints about failing to prescribe appropriate doses and/or appropriate medicines<br />
** Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 92 of 196
Section Two:<br />
Supply of CDs<br />
Do you supply CDs as part of substance<br />
misuse treatment?<br />
If so, are the drugs checked against your<br />
prescription by someone other than<br />
yourself, when being supplied?<br />
Do you supply CDs to patients against<br />
private prescriptions written by:<br />
c) Other doctors?<br />
d) Yourself?<br />
Do you supply CDs against a signed (xxv)<br />
order:<br />
c) Other doctors?<br />
d) To others (not including patients)?<br />
e) Yourself?<br />
From where do you obtain your stocks (xxvi) of<br />
CDs?<br />
Do you provide advice to patients on (xxvii) the<br />
safekeeping and disposal of unwanted<br />
CDs?<br />
Are patient returned medicines ever (xxviii) reused<br />
by you?<br />
Are patient information leaflets supplied (xxix)<br />
to all patients receiving CDs directly from<br />
you?<br />
Have there been any patient or carer (xxx)<br />
complaints involving the supply of CDs by<br />
you?<br />
Have there been any concerns expressed (xxxi)<br />
by colleagues, police, drugs misuse<br />
service or others about the supply of CDs<br />
by you?<br />
Have there been any significant events* (xxxii)<br />
involving the supply of CDs by you?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 93 of 196
Section Three:<br />
Administration of CDs (This excludes supervision of CDs consumed by addicts)<br />
The CDs used for administration are:<br />
a) Stock CDs?<br />
b) Patients own CDs?<br />
c) Both a) and b)<br />
Do you maintain records of<br />
administration:<br />
If Yes, where? (Register, MAR charts etc)<br />
Is administration of CDs witnessed?<br />
If not, what risk management policies are<br />
in place to cover administration?<br />
Have there been any patient or carer (xxxiii)<br />
complaints involving the administration of<br />
CDs by you?<br />
Have there been any concerns expressed (xxxiv)<br />
by colleagues, police, drugs misuse<br />
service or others about the administration<br />
of CDs by you?<br />
Have there been any significant events* (xxxv)<br />
involving the administration of CDs by<br />
you?<br />
Yes/No or<br />
N/A<br />
Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 94 of 196
Section Four:<br />
4.1) Security and safe custody of CDs on premises<br />
Do you store CDs in:<br />
d) A central store (e.g. a single cupboard<br />
that holds all CD stocks for your use)?<br />
e) Doctors bags?<br />
f) Other places (please details)?<br />
Are all CDs (including patient returned<br />
CDs or unwanted/obsolete CDs) are kept<br />
locked in a cupboard that complies with<br />
BS2881 (a metal cupboard with an<br />
internal locking system)?<br />
Is access to CDs controlled? (xxxvi)<br />
E.g. keys held by appropriate staff?<br />
If yes, then how?<br />
Do you utilise the CD storage facilities (xxxvii)<br />
for storage of anything other than CDs?<br />
If so, please state<br />
How often does date checking of (xxxviii) CD<br />
stock take place?<br />
Give details of date checking procedures<br />
How often does date checking of (xxxix) CD<br />
stock in Doctors bags take place?<br />
(where applicable)<br />
Please give details of date checking<br />
procedures<br />
Are all stock CDs kept in the original (xl)<br />
manufacturers pack?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 95 of 196
Are dispensed patients medicines<br />
appropriately labelled by you?<br />
Are different strengths of the same<br />
medicine segregated in any way?<br />
Do you have out of date or obsolete<br />
stock CDs currently stored?<br />
Are out of date/obsolete/patient returned (xli)<br />
CDs segregated from other in date CDs?<br />
Are patient returned medicines (xlii) ever<br />
reused by you?<br />
Yes/No or<br />
N/A<br />
Details<br />
4.2) Security and Safe custody of CDs in transport<br />
Do you transport or are you responsible<br />
for the transport of CDs (this includes<br />
sending CDs using third party carriers<br />
such as delivery drivers and postal<br />
system)?<br />
If NO, please move on to section 4.3<br />
What procedure do you have in place for<br />
the transport of CDs?<br />
Are CDs routinely kept under lock and<br />
key during transport?<br />
If No, then please provide details.<br />
What records are maintained of CDs in<br />
transport?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 96 of 196
4.3) Security and Safe custody of CD registers<br />
Yes/No or Details<br />
N/A<br />
Do you keep an up to date CD register by<br />
yourself?<br />
Do you keep running balances of stock<br />
CDs held?<br />
If yes:<br />
c) Do you audit your running totals?<br />
(state how often and date of last<br />
audit)<br />
d) Are the running totals audited by<br />
an independent 3 rd party (i.e. PCT<br />
staff)? (state how often and date of<br />
last audit)<br />
Have you identified any discrepancies<br />
between running totals and actual CDs<br />
held in the last 12 months?<br />
If yes:<br />
a) What was the explanation for the<br />
discrepancy?<br />
b) What action was taken?<br />
Do you maintain records of all receipts<br />
and supplies of CDs?<br />
If yes, for how long do you keep records?<br />
Have there been any patient or carer<br />
complaints involving the storage,<br />
transport or record keeping of CDs by<br />
you?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about the storage,<br />
transport or record keeping of CDs by<br />
you?<br />
Have there been any significant events*<br />
involving the storage, transport or<br />
recording keeping of CDs by you?<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 97 of 196
Section Five:<br />
Destruction and Dispose of CDs<br />
Patient returned CDs<br />
What records do you keep of CDs<br />
returned to you by patients for disposal<br />
(where applicable)?<br />
Do you routinely destroy patients old or<br />
obsolete CDs?<br />
What arrangements do you have in place<br />
to dispose of patients old or obsolete<br />
CDs?<br />
Is the destruction of patients old or<br />
obsolete CDs witnessed?<br />
If yes, by whom?<br />
Do you keep records of the destruction of<br />
patients old or obsolete CDs?<br />
Stock CDs (if applicable)<br />
How often do you aim to destroy out of<br />
date or obsolete stock CDs?<br />
Do you have any out of date or obsolete<br />
stock CDs currently awaiting destruction?<br />
Who usually witnesses your stock CDs<br />
destruction?<br />
When was the last witnessed CD stock<br />
destroyed?<br />
Are records of stock destruction kept in<br />
the CD register by you?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 98 of 196
Have there been any patient or carer<br />
complaints involving the destruction or<br />
disposal of CDs by you?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about the destruction<br />
or disposal of CDs by you?<br />
Have there been any significant events*<br />
involving the destruction or disposal of<br />
CDs by you?<br />
Yes/No or<br />
N/A<br />
Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Please return your completed CD Declaration & self assessment audit to:<br />
Vicki Vardy<br />
<strong>Controlled</strong> Drug Accountable support & Data Manager<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong><br />
Merrington House<br />
Merrington Lane Ind estate<br />
Spennymoor<br />
CO. <strong>Durham</strong><br />
DL16 7UT<br />
Telephone Number; 01388 825680<br />
Vicki.vardy@nhs.net<br />
Page 99 of 196
Appendix G<br />
<strong>Controlled</strong> <strong>Drugs</strong> Practice Declaration & Self Assessment for Dental<br />
Practices 2009/2010<br />
Please complete the form below:<br />
Name of organisation/Practice<br />
Address of organisation/Practice<br />
Telephone Number<br />
Name of person completing form (Please<br />
print name)<br />
Please indicate which applies to you: (please tick box)<br />
Dentist Nurse Practice Manager Other<br />
Please complete the relevant parts of the questionnaire below. This questionnaire relates to activities<br />
since October 2008 and relates to schedule 2 and 3 <strong>Controlled</strong> <strong>Drugs</strong> (CDs) including Midazolam &<br />
Temazepam, as they are subject to a higher level of control.<br />
Area of activity Yes/No If the answer is YES<br />
Question 1 Does the practice write/print<br />
prescriptions for CDs?<br />
Question 2 Does the practice supply or<br />
dispense CDs?<br />
Question 3 (xliii) a. Are CDs stocked either on the<br />
premises or off site? E.g. in<br />
dentist‘s bag/emergency box.<br />
(xliv)<br />
Question 4 Do you destroy or dispose of CDs<br />
(patient returns/stock) in the<br />
practice?<br />
Page 100 of 196<br />
Please complete TABLE<br />
A and SECTION 1<br />
Please complete TABLE<br />
A and SECTION 2<br />
Please complete TABLE<br />
A and SECTION 3<br />
Please complete TABLE<br />
A and SECTION 4
<strong>Controlled</strong> <strong>Drugs</strong> Practice Declaration Statement for Dental Practice 2009/2010<br />
In ALL cases please delete as applicable and sign the declaration below:<br />
e) I declare to the best of my knowledge and belief that the organisation/practice does not handle,<br />
use or manage Schedule 2 or 3 CDs on any premises from which I provide clinical services.<br />
OR<br />
f) I declare that to the best of my knowledge and belief that I do/do not comply (please delete as<br />
appropriate) with the provisions of the Misuse of <strong>Drugs</strong> Act 1971 and the associated Regulations in its<br />
handling, use, prescribing and management of schedule 2 and 3 CDs.<br />
Signature*<br />
Name and registration number<br />
Date of Signing<br />
* This form must be signed by appropriately authorised personnel, who have responsibility for the management<br />
and use of CDs within the organisation/practice.<br />
Please note that you must notify us of any material changes to the answers to questions 1-4 within 14<br />
days of change.<br />
Please return your completed <strong>Controlled</strong> Drug Declaration to:<br />
Vicki Vardy<br />
<strong>Controlled</strong> Drug Accountable Support & Data Manager<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong><br />
Merrington House<br />
Merrington Lane Ind estate<br />
Spennymoor<br />
CO. <strong>Durham</strong><br />
DL16 7UT<br />
Telephone number; 01388 285680<br />
Vicki.vardy@nhs.net<br />
Page 101 of 196
TABLE A: General Information; Please complete in ALL cases<br />
Does the practice have written standard<br />
operating procedures or written policies<br />
covering the handling and management<br />
of CDs, appropriate to the activities<br />
carried out at the premises?<br />
Does the practice have in place a local<br />
procedure for dealing with a significant<br />
event* involving CDs?<br />
Does the practice have appropriate<br />
procedures for the initial and continuing<br />
training or development of all staff<br />
involved in the prescribing, handling,<br />
supply and administration of CDs?<br />
Are there any specific restrictions (xlv) that<br />
have been applied that would affect the<br />
handling/prescribing/supply/administration<br />
of CDs by any of the healthcare<br />
professionals involved in your practice?<br />
Yes/No Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 102 of 196
Section one:<br />
Prescribing of CDs<br />
Have there been any patient or carer<br />
complaints* involving the prescribing of<br />
CDs by your practice?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about unusual,<br />
excessive or inappropriate prescribing of<br />
CDs by your practice?<br />
Have there been any significant events (xlvi) **<br />
involving the prescribing of CDs within<br />
your practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
* This includes complaints about failing to prescribe appropriate doses and/or appropriate medicines<br />
** Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 103 of 196
Section Two:<br />
Supply/Dispensing of CDs<br />
Are drugs checked against your<br />
prescription by someone other than<br />
yourself, when being supplied?<br />
Does the practice supply/dispense CDs<br />
against private prescriptions:<br />
e) For or from substance misuse<br />
services?<br />
f) Elsewhere?<br />
Does the practice supply CDs against (xlvii) a<br />
signed order:<br />
f) To doctors?<br />
g) To others (not including patients)?<br />
From where does your practice obtain (xlviii)<br />
stocks of CDs?<br />
Does your practice provide advice (xlix) to<br />
patients on the safekeeping and disposal<br />
of unwanted CDs within your practice?<br />
Are patient returned medicines ever (l) reused<br />
in the practice?<br />
Are patient information leaflets supplied (li)<br />
to all patients supplied/dispensed CDs by<br />
the practice?<br />
Have there been any patient or carer<br />
complaints involving the<br />
supply/dispensing of CDs in your<br />
practice?<br />
(lii)<br />
Have there been any concerns expressed (liii)<br />
by colleagues, police, drugs misuse<br />
service or others about CDs<br />
supply/dispensed from the<br />
organisation/practice?<br />
Have there been any significant events* (liv)<br />
involving the supply/dispensing of CDs<br />
from your practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 104 of 196
Section Three:<br />
3.1) Security and safe custody of CDs on premises<br />
Does the practice store CDs in:<br />
g) A central store?(e.g. a single<br />
cupboard that holds all CD stocks for the<br />
practice)<br />
h) Dentist bags?<br />
i) Other places (please details)?<br />
Are all CDs (including patient returned<br />
CDs or unwanted/obsolete CDs) are kept<br />
locked in a cupboard that complies with<br />
BS2881 (a metal cupboard with an<br />
internal locking system)?<br />
Is access to CDs controlled within (lv) your<br />
practice?<br />
E.g. keys held only by appropriate staff<br />
If yes, then how?<br />
Do you utilise the CD storage facilities (lvi)<br />
for storage of anything other than CDs?<br />
If so, please state<br />
How often does date checking of (lvii) CD<br />
stock take place in your practice?<br />
Give details of date checking procedures<br />
How often does date checking of (lviii) CD<br />
stock in medical bags take place?<br />
(where applicable)<br />
Please give details of date checking<br />
procedures<br />
Are all stock CDs kept in the original (lix)<br />
manufacturers pack within the practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 105 of 196
Are dispensed patients medicines<br />
appropriately labelled in the practice?<br />
Are different strengths of the same<br />
medicine segregated in any way?<br />
Do you have out of date or obsolete<br />
stock CDs currently stored in the<br />
practice?<br />
Are out of date/obsolete/patient returned (lx)<br />
CDs segregated from other in date CDs<br />
in the practice?<br />
Are patient returned medicines (lxi) ever<br />
reused in the practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
3.2) Security and Safe custody of CDs in transport<br />
Do you transport or are you responsible<br />
for the transport of CDs (this includes<br />
sending CDs using third party carriers<br />
such as delivery drivers and postal<br />
system)?<br />
If NO, please move on to section 3.3<br />
What procedure do you have in place for<br />
the transport of CDs in the practice?<br />
Are CDs routinely kept under lock and<br />
key during transport?<br />
If No, then please provide details.<br />
What records are maintained of CDs in<br />
transport?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 106 of 196
3.3) Security and Safe custody of CD registers<br />
Yes/No or Details<br />
N/A<br />
Do you keep an up to date CD register in<br />
the practice?<br />
Do you keep running balances of stock<br />
CDs held?<br />
If yes:<br />
e) Do you audit your running totals?<br />
(state how often and date of last<br />
audit)<br />
f) Are the running totals audited by<br />
an independent 3 rd party (i.e. PCT<br />
staff)? (state how often and date of<br />
last audit)<br />
Have you identified any discrepancies<br />
between running totals and actual CD<br />
balance since October 2008 in the<br />
practice?<br />
If yes:<br />
a) What was the explanation for the<br />
discrepancy?<br />
b) What action was taken?<br />
Do you maintain records of all receipts<br />
and supplies of CDs within your practice?<br />
If yes, for how long do you keep records?<br />
Have there been any patient or carer<br />
complaints involving the storage,<br />
transport or record keeping of CDs in the<br />
practice?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about the storage,<br />
transport or record keeping of CDs in the<br />
practice?<br />
Have there been any significant events*<br />
involving the storage, transport or<br />
recording keeping of CDs?<br />
Page 107 of 196
Section Four:<br />
Destruction and Dispose of CDs<br />
Patient returned CDs<br />
What records do you keep of CDs<br />
returned to you by patients for disposal<br />
within the practice? (Where applicable)<br />
Do you routinely destroy patients old or<br />
obsolete CDs in the practice?<br />
What arrangements do you have in place<br />
to dispose of patients old or obsolete CDs<br />
in the practice?<br />
Is the destruction of patients old or<br />
obsolete CDs witnessed in the practice?<br />
If yes, by whom?<br />
Do you keep records of the destruction of<br />
patients old or obsolete CDs in the<br />
practice?<br />
Stock CDs (if applicable)<br />
How often do you aim to destroy out of<br />
date or obsolete stock CDs in the<br />
practice?<br />
Do you have any out of date or obsolete<br />
stock CDs currently awaiting destruction?<br />
Who usually witnesses your stock CDs<br />
destruction?<br />
When was the last witnessed CD stock<br />
destroyed?<br />
Are records of stock destruction kept in<br />
the CD register within the practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 108 of 196
Have there been any patient or carer<br />
complaints involving the destruction or<br />
disposal of CDs in the practice?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about the destruction<br />
or disposal of CDs in the practice?<br />
Have there been any significant events*<br />
involving the destruction or disposal of<br />
CDs in the practice?<br />
Yes/No or<br />
N/A<br />
Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Please return your completed CD Declaration & self assessment audit to:<br />
Vicki Vardy<br />
<strong>Controlled</strong> Drug Accountable Support & Data Manager<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong><br />
Merrington House<br />
Merrington Lane Ind estate<br />
Spennymoor<br />
CO. <strong>Durham</strong><br />
DL16 7UT<br />
Telephone Number; 01388 825680<br />
Vicki.vardy@nhs.net<br />
Page 109 of 196
Appendix H<br />
<strong>Controlled</strong> <strong>Drugs</strong> Personal Declaration & Self-Assessment Audit for<br />
Dentists 2009/2010<br />
Please complete the form below:<br />
Name of Clinician<br />
Address of main workplace<br />
Telephone Number<br />
Name (Please print name)<br />
GDC Number<br />
Please indicate which applies to you: (please tick box)<br />
Dentist Other<br />
Please complete the relevant parts of the questionnaire below. This questionnaire relates to activities<br />
since October 2008 and relates to schedule 2 and 3 <strong>Controlled</strong> <strong>Drugs</strong> (CDs) including Midazolam &<br />
Temazepam, as they are subject to a higher level of control.<br />
Area of activity Yes/No If the answer<br />
is YES<br />
Question 1 Do you prescribe CDs? Please complete<br />
TABLE A and<br />
Question 2 Do you supply CDs?<br />
SECTION 1<br />
Please complete<br />
TABLE A and<br />
SECTION 2<br />
Question 3 Do you administer CDs (or supervise or<br />
Please complete<br />
assist patients own administration)?<br />
TABLE A and<br />
SECTION 3<br />
Question 4 (lxii) a. Do you keep a stock of CDs? E.g. in<br />
Please complete<br />
dentist‘s bag/Emergency box.<br />
TABLE A and<br />
(lxiii) b. Do you keep patients CDs?<br />
SECTION 4<br />
Question 5 Do you destroy or dispose of CDs (patient<br />
Please complete<br />
returns/stock)?<br />
TABLE A and<br />
SECTION 5<br />
Page 110 of 196
<strong>Controlled</strong> <strong>Drugs</strong> Personal Declaration Statement for Dentist‟s<br />
2009/2010<br />
In ALL cases please delete as applicable and sign the declaration below:<br />
g) I declare to the best of my knowledge and belief that I do not handle, use or manage<br />
Schedule 2 or 3 CDs.<br />
OR<br />
h) I declare that to the best of my knowledge and belief that I do/do not comply (please delete as<br />
appropriate) with the provisions of the Misuse of <strong>Drugs</strong> Act 1971 and the associated Regulations in its<br />
handling, use, prescribing and management of schedule 2 and 3 CDs.<br />
Signature*<br />
Name and registration number<br />
Date of Signing<br />
Please note that you must notify us of any material changes to the answers to questions 1-5 within 14<br />
days of change.<br />
Please return your completed declaration to:<br />
Vicki Vardy<br />
<strong>Controlled</strong> Drug Accountable Support & Data Manager<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong><br />
Merrington House<br />
Merrington Lane Ind estate<br />
Spennymoor<br />
CO. <strong>Durham</strong><br />
DL16 7UT<br />
Telephone Number; 01388 825680<br />
Vicki.vardy@nhs.net<br />
Page 111 of 196
TABLE A: General Information; Please complete in ALL cases<br />
Do you have written standard operating<br />
procedures or written policies covering<br />
the handling and management of CDs,<br />
appropriate to the activities carried out at<br />
the premises?<br />
Do you have in place a procedure for<br />
dealing with a significant event* involving<br />
CDs?<br />
Do you have appropriate arrangements in<br />
place for ongoing personal<br />
development/training with regards CDs?<br />
Are there any specific restrictions (lxiv) that<br />
have been applied that would affect the<br />
handling/prescribing/supply/administration<br />
of CDs by yourself?<br />
Yes/No Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 112 of 196
Section one:<br />
Prescribing of CDs<br />
Have there been any patient or carer<br />
complaints* involving the prescribing of<br />
CDs by you?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about unusual,<br />
excessive or inappropriate prescribing of<br />
CDs by you?<br />
Have there been any significant events (lxv) **<br />
involving the prescribing of CDs by you?<br />
Yes/No or<br />
N/A<br />
Details<br />
* This includes complaints about failing to prescribe appropriate doses and/or appropriate medicines<br />
** Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 113 of 196
Section Two:<br />
Supply of CDs<br />
Are drugs checked against your<br />
prescription by someone other than<br />
yourself, when being supplied?<br />
Do you supply CDs to patients against<br />
private prescriptions written by:<br />
g) Other dentist‘s?<br />
h) Yourself?<br />
Do you supply CDs against a signed (lxvi)<br />
order:<br />
h) Other dentist‘s?<br />
i) To others (not including patients)?<br />
j) Yourself<br />
From where do you obtain your stocks (lxvii) of<br />
CDs?<br />
Do you provide advice to patients on (lxviii) the<br />
safekeeping and disposal of unwanted<br />
CDs?<br />
Are patient returned medicines ever (lxix) reused<br />
by you?<br />
Are patient information leaflets supplied (lxx)<br />
to all patients receiving CDs directly from<br />
you?<br />
Have there been any patient or carer (lxxi)<br />
complaints involving the supply of CDs by<br />
you?<br />
Have there been any concerns expressed (lxxii)<br />
by colleagues, police, drugs misuse<br />
service or others about the supply of CDs<br />
by you?<br />
Have there been any significant events* (lxxiii)<br />
involving the supply of CDs by you?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 114 of 196
Section Three:<br />
Administration of CDs (This excludes supervision of CDs consumed by addicts)<br />
Are the CDs used for administration:<br />
d) Stock CDs?<br />
e) Patients own CDs?<br />
f) Both a) and b)<br />
Do you maintain records of<br />
administration:<br />
If Yes, where? (Register, MAR charts etc)<br />
Is administration of CDs witnessed?<br />
If not, what risk management policies are<br />
in place to cover administration?<br />
Have there been any patient or carer (lxxiv)<br />
complaints involving the administration of<br />
CDs by you?<br />
Have there been any concerns expressed (lxxv)<br />
by colleagues, police, drugs misuse<br />
service or others about the administration<br />
of CDs by you?<br />
Have there been any significant events* (lxxvi)<br />
involving the administration of CDs by<br />
you?<br />
Yes/No or<br />
N/A<br />
Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 115 of 196
Section Four:<br />
3.1) Security and safe custody of CDs on premises<br />
Do you store CDs in:<br />
j) A central store?(e.g. a single<br />
cupboard that holds all CDs)<br />
k) Dentist‘s bags?<br />
l) Other places (please details)?<br />
Are all CDs (including patient returned<br />
CDs or unwanted/obsolete CDs) are kept<br />
locked in a cupboard that complies with<br />
BS2881 (a metal cupboard with an<br />
internal locking system)?<br />
Is access to CDs controlled? (lxxvii)<br />
E.g. Keys held only by appropriate staff<br />
If yes, then how?<br />
Do you utilise the CD storage facilities (lxxviii)<br />
for storage of anything other than CDs?<br />
If so, please state<br />
How often does date checking of (lxxix) CD<br />
stock take place?<br />
Give details of date checking procedures<br />
How often does date checking of (lxxx) CD<br />
stock in medical bags take place?<br />
(where applicable)<br />
Please give details of date checking<br />
procedures<br />
Are all stock CDs kept in the original (lxxxi)<br />
manufacturers pack?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 116 of 196
Are dispensed patients medicines<br />
appropriately labelled by you?<br />
Are different strengths of the same<br />
medicine segregated in any way?<br />
Do you have out of date or obsolete<br />
stock CDs currently stored?<br />
Are out of date/obsolete/patient returned (lxxxii)<br />
CDs segregated from other in date CDs?<br />
Are patient returned medicines (lxxxiii) ever<br />
reused?<br />
Yes/No or<br />
N/A<br />
Details<br />
3.2) Security and Safe custody of CDs in transport<br />
Do you transport or are you responsible<br />
for the transport of CDs (this includes<br />
sending CDs using third party carriers<br />
such as delivery drivers and postal<br />
system)?<br />
If NO, please move on to section 3.3<br />
What procedure do you have in place for<br />
the transport of CDs?<br />
Are CDs routinely kept under lock and<br />
key during transport?<br />
If No, then please provide details.<br />
What records are maintained of CDs in<br />
transport?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 117 of 196
3.3) Security and Safe custody of CD registers<br />
Do you keep an up to date CD register?<br />
Do you keep running balances of stock<br />
CDs held?<br />
If yes:<br />
g) Do you audit your running totals?<br />
(state how often and date of last<br />
audit)<br />
h) Are the running totals audited by<br />
an independent 3 rd party (i.e. PCT<br />
staff)? (state how often and date of<br />
last audit)<br />
Have you identified any discrepancies<br />
between running totals and actual CD<br />
balances since October 2008?<br />
If yes:<br />
a) What was the explanation for the<br />
discrepancy?<br />
b) What action was taken?<br />
Do you maintain records of all receipts<br />
and supplies of CDs?<br />
If yes, for how long do you keep records?<br />
Have there been any patient or carer<br />
complaints involving the storage,<br />
transport or record keeping of CDs by<br />
you?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about the storage,<br />
transport or record keeping of CDs by<br />
you?<br />
Have there been any significant events*<br />
involving the storage, transport or<br />
recording keeping of CDs by you?<br />
Yes/No or<br />
N/A<br />
Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Page 118 of 196
Section Five:<br />
Destruction and Dispose of CDs<br />
Patient returned CDs<br />
What records do you keep of CDs<br />
returned to you by patients for disposal<br />
(where applicable)?<br />
Do you routinely destroy patients old or<br />
obsolete CDs?<br />
What arrangements do you have in place<br />
to dispose of patients old or obsolete<br />
CDs?<br />
Is the destruction of patients old or<br />
obsolete CDs witnessed?<br />
If yes, by whom?<br />
Do you keep records of the destruction of<br />
patients old or obsolete CDs?<br />
Stock CDs (if applicable)<br />
How often do you aim to destroy out of<br />
date or obsolete stock CDs?<br />
Do you have any out of date or obsolete<br />
stock CDs currently awaiting destruction?<br />
Who usually witnesses your stock CDs<br />
destruction?<br />
When was the last witnessed CD stock<br />
destroyed?<br />
Are records of stock destruction kept in<br />
the CD register?<br />
Yes/No or<br />
N/A<br />
Details<br />
Page 119 of 196
Have there been any patient or carer<br />
complaints involving the destruction or<br />
disposal of CDs by you?<br />
Have there been any concerns expressed<br />
by colleagues, police, drugs misuse<br />
services or others about the destruction<br />
or disposal of CDs by you?<br />
Have there been any significant events*<br />
involving the destruction or disposal of<br />
CDs by you?<br />
Yes/No or<br />
N/A<br />
Details<br />
* Significant event includes any action or omission resulting in patient(s) being harmed or any action or<br />
omission that nearly happened but did not (near miss)<br />
Please return your completed CD Declaration & self assessment audit to:<br />
Vicki Vardy<br />
<strong>Controlled</strong> Drug Accountable support & Data Manager<br />
<strong>NHS</strong> <strong>County</strong> <strong>Durham</strong><br />
Merrington House<br />
Merrington Lane Ind estate<br />
Spennymoor<br />
CO. <strong>Durham</strong><br />
DL16 7UT<br />
Telephone Number; 01388 825680<br />
Vicki.vardy@nhs.net<br />
Page 120 of 196
Appendix I<br />
Practice Name<br />
Practice Address<br />
<strong>Controlled</strong> <strong>Drugs</strong>: Practice Audit by PCT Pharmacist<br />
Practice Representative (Print<br />
Name)<br />
Practice Representative<br />
(Signature)<br />
PCT Pharmacist (Print Name)<br />
PCT Pharmacist (Signature)<br />
Date of Visit<br />
Personnel Prescribing CDs<br />
1.<br />
2.<br />
3.<br />
4.<br />
5.<br />
6.<br />
Personnel with access to CD<br />
receptacle<br />
1.<br />
2.<br />
3.<br />
4.<br />
Overall responsibility for CDs rests<br />
with:<br />
7.<br />
8.<br />
9.<br />
10.<br />
11.<br />
12.<br />
5.<br />
6.<br />
7.<br />
8.<br />
Page 121 of 196
Section 1: Obtaining <strong>Controlled</strong> <strong>Drugs</strong><br />
Main Supplier of CDs:<br />
Orders authorised by:<br />
Person authorised to receive<br />
CDs at premises:<br />
Is there a written standard operating procedure in place for<br />
ordering CDs?<br />
Is a record of orders kept for a minimum of 2 years?<br />
Are CD orders authorised?<br />
Is there a written standard operating procedure in place for<br />
the receipt of CDs?<br />
Is there a written standard operating procedure in place for<br />
the receipt of CDs delivered via transport systems?<br />
Is the level of stock held to a minimum and reviewed<br />
annually?<br />
YES NO<br />
Page 122 of 196
Section 2: Supply of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you supply CDs to addicts?<br />
Do you supply CDs against private<br />
prescriptions:<br />
(a) From addiction services?<br />
(b) Elsewhere?<br />
Do you supply CDs:<br />
(a) To doctors?<br />
(b) To others (excluding patients)<br />
Do you provide advice to patients on the<br />
safekeeping and disposal of unwanted CDs?<br />
Are patient information leaflets supplied to all<br />
patients receiving CDs?<br />
Are patient returned medicines ever reused?<br />
Have there been any patient or carer<br />
complaints involving the supply of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the supply of CDs from the<br />
organisation?<br />
Have there been any significant events<br />
involving the supply of CDs relating to the<br />
organisation?<br />
Yes No Details<br />
Page 123 of 196
Section 3: Administration of <strong>Controlled</strong> <strong>Drugs</strong><br />
Are CDs which are administered:<br />
(a) Stock CDs?<br />
(b) Patient‘s own CDs?<br />
Do you maintain records of administration?<br />
(If yes, where? E.g. Register, MAR chart etc.)<br />
Is the administration of CDs witnessed?<br />
If administration is not witnessed, do you have<br />
risk management policies in place?<br />
Have there been any patient or carer<br />
complaints involving the administration of<br />
CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the administration of CDs from<br />
the organisation?<br />
Have there been any significant events<br />
involving the administration of CDs relating to<br />
the organisation?<br />
Yes No Details<br />
Yes No Details<br />
Page 124 of 196
Section 4a: Storage of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you have any current Chief Constable<br />
exemption certificates in operation for your<br />
CD storage facilities?<br />
Are Schedule 2 CDs stored in a locked,<br />
secure, non-portable receptacle?<br />
Is the receptacle permanently affixed to an<br />
internal wall?<br />
Is the receptacle used only for CDs?<br />
Are all stock CDs kept in their original<br />
containers?<br />
Are different strengths of the same medicines<br />
segregated?<br />
Are there any patient‘s own medicines stored<br />
in the CD receptacle?<br />
Are out of date/returned medicines/out of date<br />
stock segregated?<br />
Are patient returned medicines ever reused?<br />
Is there a written standard operating<br />
procedure which details routine date checking<br />
of stock CDs?<br />
How often does routine date checking take<br />
place?<br />
Is the room containing the CD receptacle<br />
lockable?<br />
Is the room containing the CD receptacle kept<br />
locked?<br />
Does the room containing the CD receptacle<br />
have limited access?<br />
Is there a named person detailed in a written<br />
standard operating procedure, with<br />
responsibility for the CD receptacle and a list<br />
of the current key holder(s)?<br />
Is there a clear daily audit trail for key holders<br />
(i.e. keys signed in and out, and not stored in<br />
a drawer)?<br />
Do you store naloxone in the practice?<br />
Yes No Details<br />
Page 125 of 196
Section 4b: Security and safe custody of <strong>Controlled</strong> <strong>Drugs</strong> in transport<br />
Do you transport or are you responsible for<br />
the transport of CDs (this includes sending<br />
CDs using third party carriers)?<br />
Do you have written standard operating<br />
procedures in place for the transport of CDs?<br />
Are CDs kept in a locked receptacle during<br />
transport?<br />
Are records maintained of CDs in transport?<br />
Section 4c: Register of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you maintain a controlled drug register?<br />
Are the controlled drugs kept at more than<br />
one surgery site?<br />
Is there a separate register for each area<br />
where the CDs are stored?<br />
Is the CD register stored safely, near to, but<br />
outside the CD receptacle?<br />
Are all records, registers and invoices kept for<br />
a minimum of 2 years?<br />
Have there been any patient or carer<br />
complaints involving the storage, transport or<br />
record keeping of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the storage, transport or<br />
record keeping of CDs?<br />
Have there been any significant events<br />
involving the storage, transport or record<br />
keeping of CDs?<br />
Yes No Details<br />
Yes No Details<br />
Page 126 of 196
Section 4c: Paper based CD registers<br />
The following table may be used to identify which procedures are being followed and the number of<br />
registers in current use. Tick the box to indicate whether the criteria are being followed in the practice.<br />
Criterion Register Comments<br />
1. Format of register<br />
1.1 Bound book<br />
1.2 Separate section per drug<br />
1.3 Separate section per presentation with<br />
name and strength at top of each page<br />
2. Entries<br />
2.1 In ink<br />
2.2 Chronological order<br />
2.3 Entries within 24 hours<br />
3. Errors and corrections<br />
3.1 As margin/foot notes<br />
3.2 Corrections dated<br />
3.3 Corrections initialled<br />
4. Record of receipt<br />
4.1 Date of receipt<br />
4.2 Name and address of supplier<br />
4.3 Amount obtained<br />
4.4 Form and strength obtained<br />
4.5 Running balance<br />
4.6 Signature<br />
4.7 Process for discrepancies<br />
5. Record of supply<br />
5.1 Date of supply<br />
5.2 Name and address of person supplied<br />
5.3 Authority to supply<br />
5.4 Amount supplied<br />
5.5 Form and strength supplied<br />
5.6 Running balance<br />
5.7 Signature<br />
Criterion Register Comments<br />
5.8 Collected by<br />
6. Record of administration<br />
6.1 Date of administration<br />
6.2 Name and address of person<br />
administered to (where appropriate)<br />
6.3 Name and authority of person<br />
administering<br />
6.4 Amount administered<br />
6.5 Form administered<br />
6.6 Time of administration<br />
6.7 Running balance<br />
6.8 Signature and witness where appropriate<br />
6.9 Procedure if pack contents incorrect<br />
7. Stock check<br />
7.1 Evidence of appropriate stock check e.g.<br />
monthly<br />
7.2 Stock checked and correct<br />
7.3 Different people carrying out stock check<br />
Page 127 of 196
Section 5: Destruction of <strong>Controlled</strong> <strong>Drugs</strong><br />
Are CDs destroyed using recommended<br />
methods?<br />
Are there any CDs awaiting destruction in the<br />
CD receptacle?<br />
Is date expired CD stock clearly labelled?<br />
Is date expired CD stock clearly segregated?<br />
Have there been any patient or carer<br />
complaints involving the destruction of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the destruction of CDs?<br />
Have there been any significant events<br />
involving the destruction of CDs?<br />
Destruction of stock controlled drugs<br />
Is there a written standard operating<br />
procedure for the destruction of controlled<br />
drugs?<br />
Is destruction of stock CDs witnessed by an<br />
authorised person?<br />
Is the authorised person NOT directly involved<br />
with CD supply in the practice?<br />
Is the name, form, strength and quantity of the<br />
drug destroyed, entered into the CD register?<br />
Is the date of destruction entered into the<br />
register?<br />
Is the signature of the witness entered into the<br />
register?<br />
Is there a written standard operating<br />
procedure for the destruction of expired stock<br />
from doctor‘s bags?<br />
Destruction of patient returned controlled<br />
drugs<br />
Are records made of patient returned CDs in a<br />
separate book (not the CD register)?<br />
Does this book record:<br />
The date received?<br />
Name and address of the patient prescribed<br />
CD?<br />
Pharmacy/practice where originally<br />
dispensed?<br />
Name, quantity, form of CD?<br />
Role of person returning CD?<br />
Name and signature of staff receiving CD?<br />
Name and signature of staff destroying CD<br />
and date?<br />
Destruction of patient returned controlled<br />
drugs<br />
Does this book record:<br />
Name and signature of witness to destruction<br />
and date?<br />
Yes No Details<br />
Yes No Details<br />
Page 128 of 196
Are patient returned CDs destroyed as soon<br />
as possible?<br />
Is the patient returns process audited?<br />
Page 129 of 196
Section 6: General<br />
Do all staff know who to contact at the<br />
Primary Care Organisation regarding<br />
concerns about other colleagues in relation to<br />
CDs?<br />
Comments<br />
Yes No Details<br />
It is good practice to keep all audit records for 7 years<br />
Revision Date: August 2010<br />
Page 130 of 196
Appendix J<br />
GP Name<br />
GP Address<br />
GP Signature<br />
<strong>Controlled</strong> <strong>Drugs</strong>: Personal Audit by PCT Pharmacist<br />
PCT Pharmacist (Print Name)<br />
PCT Pharmacist (Signature)<br />
Date of Visit<br />
Section 1: Obtaining <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you obtain controlled drugs from your local pharmacist?<br />
Do you obtain controlled drugs by signed requisition?<br />
Do you use practice headed paper for your signed<br />
requisition?<br />
Do you obtain controlled drugs using an FP10<br />
Do you obtain controlled drugs from patients who have died?<br />
Is there a written standard operating procedure in place for<br />
ordering CDs?<br />
Is a record of orders kept for a minimum of 2 years?<br />
Is there a written standard operating procedure in place for<br />
the receipt of CDs?<br />
Is there a written standard operating procedure in place for<br />
the receipt of CDs delivered via transport systems?<br />
Is the level of stock in your bag held to a minimum and<br />
reviewed annually?<br />
Section 2: Supply of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you supply CDs to addicts?<br />
Do you supply CDs against private<br />
prescriptions:<br />
(c) From addiction services?<br />
(d) Elsewhere?<br />
Do you supply CDs:<br />
(c) To doctors?<br />
(d) To others (excluding patients)<br />
Do you provide advice to patients on the<br />
YES NO<br />
Yes No Details<br />
Page 131 of 196
safekeeping and disposal of unwanted CDs?<br />
Are patient information leaflets supplied to all<br />
patients receiving CDs?<br />
Are patient returned medicines ever reused?<br />
Have there been any patient or carer<br />
complaints relating to you involving the supply<br />
of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others relating to you about the supply of<br />
CDs from the organisation?<br />
Have there been any significant events<br />
involving the supply of CDs relating to you?<br />
Section 3: Administration of <strong>Controlled</strong> <strong>Drugs</strong><br />
Are CDs which are administered:<br />
(c) Stock CDs?<br />
(d) Patient‘s own CDs?<br />
Do you maintain records of administration?<br />
(If yes, where? E.g. Register, MAR chart etc.)<br />
Is the administration of CDs witnessed?<br />
If administration is not witnessed, do you have<br />
risk management policies in place?<br />
Have there been any patient or carer<br />
complaints involving the administration of CDs<br />
by you?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the administration of CDs by<br />
you?<br />
Have there been any significant events<br />
involving the administration of CDs relating to<br />
you?<br />
Section 4a: Storage of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you store controlled drugs in a locked<br />
doctors‘ bag?<br />
Do you store controlled drugs in your car?<br />
If you store controlled drugs in your car are<br />
they stored in a locked container?<br />
If you store controlled drugs in your car, is the<br />
car locked?<br />
If you store controlled drugs in your car, are<br />
they stored in a locked boot?<br />
When would you store controlled drugs in<br />
your car?<br />
Yes No Details<br />
Yes No Details<br />
Page 132 of 196
Would controlled drugs be left overnight in<br />
your car?<br />
Are out of date/returned medicines/out of date<br />
stock segregated?<br />
Are patient returned medicines ever reused?<br />
Is there a written standard operating<br />
procedure which details routine date checking<br />
of stock CDs?<br />
How often does routine date checking take<br />
place?<br />
Where is your bag, containing controlled<br />
drugs stored out of hours?<br />
Is the room containing the CDs kept locked?<br />
Does the room containing the CDs have<br />
limited access?<br />
Do you carry naloxone in your bag?<br />
Do you store naloxone in your practice?<br />
Section 4b: Security and safe custody of <strong>Controlled</strong> <strong>Drugs</strong> in transport<br />
Do you transport or are you responsible for<br />
the transport of CDs (this includes sending<br />
CDs using third party carriers)?<br />
Do you have written standard operating<br />
procedures in place for the transport of CDs?<br />
Are CDs kept in a locked receptacle during<br />
transport?<br />
Are records maintained of CDs in transport?<br />
Section 4c: Register of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you maintain a controlled drug register?<br />
Is the CD register kept with the controlled<br />
drugs?<br />
Are all records, registers and invoices kept for<br />
a minimum of 2 years?<br />
Have there been any patient or carer<br />
complaints involving the storage, transport or<br />
record keeping of CDs regarding you?<br />
Have there been any concerns regarding you<br />
expressed by colleagues, police, substance<br />
Yes No Details<br />
Yes No Details<br />
Page 133 of 196
misuse services or others about the storage,<br />
transport or record keeping of CDs?<br />
Have there been any significant events<br />
regarding you involving the storage, transport<br />
or record keeping of CDs?<br />
Section 4c: Paper based CD registers<br />
The following table may be used to identify which procedures are being followed and<br />
the number of registers in current use. Tick the box to indicate whether the criteria are<br />
being followed in the practice.<br />
Criterion Register Comments<br />
1. Format of register<br />
1.1 Bound book<br />
1.2 Separate section per drug<br />
1.3 Separate section per presentation with<br />
name and strength at top of each page<br />
2. Entries<br />
2.1 In ink<br />
2.2 Chronological order<br />
2.3 Entries within 24 hours<br />
3. Errors and corrections<br />
3.1 As margin/foot notes<br />
3.2 Corrections dated<br />
3.3 Corrections initialled<br />
4. Record of receipt<br />
4.1 Date of receipt<br />
4.2 Name and address of supplier<br />
4.3 Amount obtained<br />
4.4 Form and strength obtained<br />
4.5 Running balance<br />
4.6 Signature<br />
4.7 Process for discrepancies<br />
Criterion Register Comments<br />
5. Record of supply<br />
5.1 Date of supply<br />
5.2 Name and address of person supplied<br />
5.3 Authority to supply<br />
5.4 Amount supplied<br />
5.5 Form and strength supplied<br />
5.6 Running balance<br />
5.7 Signature<br />
5.8 Collected by<br />
6. Record of administration<br />
6.1 Date of administration<br />
6.2 Name and address of person<br />
administered to (where appropriate)<br />
6.3 Name and authority of person<br />
administering<br />
6.4 Amount administered<br />
6.5 Form administered<br />
Page 134 of 196
6.6 Time of administration<br />
6.7 Running balance<br />
6.8 Signature and witness where appropriate<br />
6.9 Procedure if pack contents incorrect<br />
7. Stock check<br />
7.1 Evidence of appropriate stock check e.g.<br />
monthly<br />
7.2 Stock checked and correct<br />
Section 5: Destruction of <strong>Controlled</strong> <strong>Drugs</strong><br />
Are CDs destroyed using recommended<br />
methods?<br />
Are there any CDs awaiting destruction in the<br />
GP bag<br />
Is date expired CD stock clearly labelled?<br />
Is date expired CD stock clearly segregated?<br />
Have there been any patient or carer<br />
complaints involving the destruction of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the destruction of CDs?<br />
Have there been any significant events<br />
involving the destruction of CDs?<br />
Destruction of stock controlled drugs<br />
Is the out of date stock from your emergency<br />
bag destroyed by a GP?<br />
Is destruction of stock CDs witnessed by an<br />
authorised person?<br />
Is the authorised person NOT directly involved<br />
with CD supply in the practice?<br />
Is the name, form, strength and quantity of the<br />
drug destroyed, entered into the CD register?<br />
Is the date of destruction entered into the<br />
register?<br />
Is the signature of the witness entered into the<br />
register?<br />
Is there a written standard operating<br />
procedure for the destruction of expired stock<br />
from doctor‘s bags?<br />
Destruction of patient returned controlled<br />
drugs<br />
What do you do when Sch 2 controlled drugs<br />
that are no longer required by your patient for<br />
use in their home e.g. terminal care? Are the<br />
Yes No Details<br />
Yes No Details<br />
Page 135 of 196
drugs:<br />
Returned by you to a community<br />
pharmacy?<br />
Returned by others to a community<br />
pharmacy?<br />
Added to your own emergency bag<br />
stock?<br />
Destroyed by you?<br />
Destroyed by a District Nurse?<br />
Destroyed by patient‘s relatives?<br />
Destroyed by an authorised person?<br />
Are records made of patient returned CDs in a<br />
separate book (not the CD register)?<br />
Does this book record:<br />
The date received?<br />
Name and address of the patient prescribed<br />
CD?<br />
Pharmacy/practice where originally<br />
dispensed?<br />
Name, quantity, form of CD?<br />
Role of person returning CD?<br />
Name and signature of staff receiving CD?<br />
Name and signature of staff destroying CD<br />
and date?<br />
Name and signature of witness to destruction<br />
and date?<br />
Are patient returned CDs destroyed as soon<br />
as possible?<br />
Is the patient returns process audited?<br />
Section 6: General<br />
Do all staff know who to contact at the<br />
Primary Care Organisation regarding<br />
concerns about other colleagues in relation to<br />
CDs?<br />
Comments<br />
Yes No Details<br />
It is good practice to keep all audit records for 7 years<br />
Revision Date: August 2010<br />
Page 136 of 196
Appendix K<br />
OOH/UCC/Practice Name<br />
<strong>Controlled</strong> <strong>Drugs</strong>: OOH/UCC/Dispensing Doctors Audit<br />
OOH/UCC/Practice Address<br />
OOH/UCC/Practice<br />
Representative (Print Name)<br />
OOH/UCC/Practice<br />
Representative (Signature)<br />
PCT Pharmacist (Print Name)<br />
PCT Pharmacist (Signature)<br />
Date of Visit<br />
Personnel Prescribing CDs<br />
1.<br />
2.<br />
3.<br />
4.<br />
5.<br />
6.<br />
Personnel with access to CD<br />
receptacle<br />
1.<br />
2.<br />
3.<br />
4.<br />
Overall responsibility for CDs rests<br />
with:<br />
7.<br />
8.<br />
9.<br />
10.<br />
11.<br />
12.<br />
5.<br />
6.<br />
7.<br />
8.<br />
Page 137 of 196
Section 1: Obtaining <strong>Controlled</strong> <strong>Drugs</strong><br />
Main Supplier of CDs:<br />
Orders authorised by:<br />
Person authorised to receive<br />
CDs at premises:<br />
Is there a written standard operating procedure in place for<br />
ordering CDs?<br />
Is a record of orders kept for a minimum of 2 years?<br />
Are CD orders authorised?<br />
Is there a written standard operating procedure in place for<br />
the receipt of CDs?<br />
Is there a written standard operating procedure in place for<br />
the receipt of CDs delivered via transport systems?<br />
Is the level of stock held to a minimum and reviewed<br />
annually?<br />
Section 2: Supply of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you supply CDs to addicts?<br />
Do you supply CDs against private<br />
prescriptions:<br />
(e) From addiction services?<br />
(f) Elsewhere?<br />
Do you supply CDs:<br />
(e) To doctors?<br />
(f) To others (excluding patients)<br />
Are the drugs checked against the<br />
prescription by a GP when dispensing<br />
schedule 2 and 3 controlled drugs?<br />
Do you provide advice to patients on the<br />
safekeeping and disposal of unwanted CDs?<br />
Are patient information leaflets supplied to all<br />
patients receiving CDs?<br />
Are patient returned medicines ever reused?<br />
Have there been any patient or carer<br />
complaints involving the supply of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the supply of CDs from the<br />
organisation?<br />
Have there been any significant events<br />
involving the supply of CDs relating to the<br />
organisation?<br />
YES NO<br />
Yes No Details<br />
Page 138 of 196
Section 3: Administration of <strong>Controlled</strong> <strong>Drugs</strong><br />
Are CDs which are administered:<br />
(e) Stock CDs?<br />
(f) Patient‘s own CDs?<br />
Do you maintain records of administration?<br />
(If yes, where? E.g. Register, MAR chart etc.)<br />
Is the administration of CDs witnessed?<br />
If administration is not witnessed, do you have<br />
risk management policies in place?<br />
Have there been any patient or carer<br />
complaints involving the administration of<br />
CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the administration of CDs from<br />
the organisation?<br />
Have there been any significant events<br />
involving the administration of CDs relating to<br />
the organisation?<br />
Section 4a: Storage of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you have any current Chief Constable<br />
exemption certificates in operation for your<br />
CD storage facilities?<br />
Are Schedule 2 CDs stored in a locked,<br />
secure, non-portable receptacle?<br />
Are Schedule 3 CDs stored in a locked,<br />
secure, non-portable receptacle?<br />
Is the receptacle permanently affixed to an<br />
internal wall?<br />
Is the receptacle used only for CDs? (i.e. is<br />
there a separate CD cupboard?)<br />
Are all stock CDs kept in their original<br />
containers?<br />
Are different strengths of the same medicines<br />
segregated?<br />
Are there any patient‘s own medicines stored<br />
in the CD receptacle?<br />
Are out of date/returned medicines/out of date<br />
stock segregated?<br />
How are out of date/returned medicines/out of<br />
date stock segregated?<br />
Are patient returned medicines ever reused?<br />
Is there a written standard operating<br />
Yes No Details<br />
Yes No Details<br />
Yes No Details<br />
Page 139 of 196
procedure which details routine date checking<br />
of stock CDs?<br />
How often does routine date checking take<br />
place?<br />
Is the room containing the CD receptacle<br />
lockable?<br />
Is the room containing the CD receptacle kept<br />
locked?<br />
Does the room containing the CD receptacle<br />
have limited access?<br />
Is there a named person detailed in a written<br />
standard operating procedure, with<br />
responsibility for the CD receptacle and a list<br />
of the current key holder(s)?<br />
Is there a clear daily audit trail for key holders<br />
(i.e. keys signed in and out, and not stored in<br />
a drawer)?<br />
Do you store naloxone in the practice?<br />
Section 4b: Security and safe custody of <strong>Controlled</strong> <strong>Drugs</strong> in transport<br />
Do you transport or are you responsible for<br />
the transport of CDs (this includes sending<br />
CDs using third party carriers)?<br />
Do you have written standard operating<br />
procedures in place for the transport of CDs?<br />
Are CDs kept in a locked receptacle during<br />
transport?<br />
Are records maintained of CDs in transport?<br />
Section 4c: Register of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you maintain a controlled drug register?<br />
Are the controlled drugs kept at more than<br />
one surgery site?<br />
Is there a separate register for each area<br />
where the CDs are stored?<br />
Is the CD register stored safely, near to, but<br />
outside the CD receptacle?<br />
Are all records, registers and invoices kept for<br />
a minimum of 2 years?<br />
Have there been any patient or carer<br />
complaints involving the storage, transport or<br />
record keeping of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
Yes No Details<br />
Yes No Details<br />
Page 140 of 196
or others about the storage, transport or<br />
record keeping of CDs?<br />
Have there been any significant events<br />
involving the storage, transport or record<br />
keeping of CDs?<br />
Section 4c: Paper based CD registers<br />
The following table may be used to identify which procedures are being followed and<br />
the number of registers in current use. Tick the box to indicate whether the criteria are<br />
being followed in the practice.<br />
Criterion Register Comments<br />
1. Format of register<br />
1.1 Bound book<br />
1.2 Separate section per drug<br />
1.3 Separate section per presentation with<br />
name and strength at top of each page<br />
2. Entries<br />
2.1 In ink<br />
2.2 Chronological order<br />
2.3 Entries within 24 hours<br />
2.4 Are entries dated, timed and signed by<br />
two practitioners<br />
3. Errors and corrections<br />
3.1 As margin/foot notes<br />
3.2 Corrections dated<br />
3.3 Corrections initialled<br />
4. Record of receipt<br />
4.1 Date of receipt<br />
4.2 Name and address of supplier<br />
4.3 Amount obtained<br />
4.4 Form and strength obtained<br />
4.5 Running balance<br />
4.6 Signature<br />
4.7 Process for discrepancies<br />
5. Record of supply<br />
5.1 Date of supply<br />
5.2 Name and address of person supplied<br />
5.3 Authority to supply<br />
5.4 Amount supplied<br />
5.5 Form and strength supplied<br />
5.6 Running balance<br />
5.7 Signature<br />
Criterion Register Comments<br />
5.8 Collected by<br />
6. Record of administration<br />
6.1 Date of administration<br />
6.2 Name and address of person<br />
administered to (where appropriate)<br />
6.3 Name and authority of person<br />
administering<br />
6.4 Amount administered<br />
Page 141 of 196
6.5 Form administered<br />
6.6 Time of administration<br />
6.7 Running balance<br />
6.8 Signature and witness where appropriate<br />
6.9 Procedure if pack contents incorrect<br />
7. Stock check<br />
7.1 Evidence of appropriate stock check e.g.<br />
monthly<br />
7.2 Stock checked and correct<br />
7.3 Different people carrying out stock check<br />
Section 5: Destruction of <strong>Controlled</strong> <strong>Drugs</strong><br />
Are CDs destroyed using recommended<br />
methods?<br />
Are there any CDs awaiting destruction in the<br />
CD receptacle?<br />
Is date expired CD stock clearly labelled?<br />
Is date expired CD stock clearly segregated?<br />
Have there been any patient or carer<br />
complaints involving the destruction of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the destruction of CDs?<br />
Have there been any significant events<br />
involving the destruction of CDs?<br />
Destruction of stock controlled drugs<br />
Is there a written standard operating<br />
procedure for the destruction of controlled<br />
drugs?<br />
Is destruction of stock CDs witnessed by an<br />
authorised person?<br />
Is the authorised person NOT directly involved<br />
with CD supply in the practice?<br />
Is the name, form, strength and quantity of the<br />
drug destroyed, entered into the CD register?<br />
Is the date of destruction entered into the<br />
register?<br />
Is the signature of the witness entered into the<br />
register?<br />
Is there a written standard operating<br />
procedure for the destruction of expired stock<br />
from doctor‘s bags?<br />
Destruction of patient returned controlled<br />
drugs<br />
Are records made of patient returned CDs in a<br />
separate book (not the CD register)?<br />
Does this book record:<br />
The date received?<br />
Name and address of the patient prescribed<br />
CD?<br />
Destruction of patient returned controlled<br />
Yes No Details<br />
Page 142 of 196
drugs<br />
Does this book record:<br />
Pharmacy/practice where originally<br />
dispensed?<br />
Name, quantity, form of CD?<br />
Role of person returning CD?<br />
Name and signature of staff receiving CD?<br />
Name and signature of staff destroying CD<br />
and date?<br />
Name and signature of witness to destruction<br />
and date?<br />
Are patient returned CDs destroyed as soon<br />
as possible?<br />
What methods are used to destroy patient<br />
returned controlled drugs? (Dispensing<br />
Doctors)<br />
Is the patient returns process audited?<br />
Section 6: General<br />
Do all staff know who to contact at the<br />
Primary Care Organisation regarding<br />
concerns about other colleagues in relation to<br />
CDs?<br />
Can the nurse/ECP/dispenser in charge<br />
explain protocol/policy if a vial/tablet is:<br />
Broken<br />
Unaccounted for<br />
Out of date<br />
No longer required by the patient after<br />
dispensing<br />
Yes No Details<br />
Page 143 of 196
Comments<br />
It is good practice to keep all audit records for 7 years<br />
Revision Date: August 2010<br />
Page 144 of 196
Appendix L<br />
Community Hospital Name<br />
Community Hospital Address<br />
Community Hospital<br />
Representative (Print Name)<br />
Community Hospital<br />
Representative (Signature)<br />
PCT Pharmacist (Print Name)<br />
PCT Pharmacist (Signature)<br />
Date of Visit<br />
Personnel Prescribing CDs<br />
Personnel with access to CD<br />
receptacle<br />
<strong>Controlled</strong> <strong>Drugs</strong>: Community Hospital Audit<br />
Page 145 of 196
Overall responsibility for CDs rests<br />
with:<br />
Section 1: Obtaining <strong>Controlled</strong> <strong>Drugs</strong><br />
Main Supplier of CDs:<br />
Orders authorised by:<br />
Person(s) authorised to receive<br />
CDs at premises:<br />
Is there a written standard operating procedure in place for<br />
ordering CDs?<br />
Is a record of orders kept for a minimum of 2 years?<br />
Are CD orders authorised?<br />
Is there a written standard operating procedure in place for<br />
the receipt of CDs?<br />
Is there a written standard operating procedure in place for<br />
the receipt of CDs delivered via transport systems?<br />
Is the level of stock held to a minimum and reviewed<br />
annually?<br />
Section 2: Supply of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you provide advice to patients on the<br />
safekeeping and disposal of unwanted CDs?<br />
Are patient information leaflets supplied to all<br />
patients receiving CDs?<br />
Are patient returned medicines ever reused?<br />
Have there been any patient or carer<br />
complaints involving the supply of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the supply of CDs from the<br />
organisation?<br />
Have there been any significant events<br />
involving the supply of CDs relating to the<br />
organisation?<br />
Section 3: Administration of <strong>Controlled</strong> <strong>Drugs</strong><br />
Are CDs which are administered:<br />
(g) Stock CDs?<br />
(h) Patient‘s own CDs?<br />
Do you maintain records of administration?<br />
(If yes, where? E.g. Register, drug cardex<br />
YES NO<br />
Yes No Details<br />
Yes No Details<br />
Page 146 of 196
etc.)<br />
Is the administration of CDs witnessed?<br />
If administration is not witnessed, do you have<br />
risk management policies in place?<br />
Have there been any patient or carer<br />
complaints involving the administration of<br />
CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the administration of CDs from<br />
the organisation?<br />
Have there been any significant events<br />
involving the administration of CDs relating to<br />
the organisation?<br />
Section 4a: Storage of <strong>Controlled</strong> <strong>Drugs</strong><br />
Are Schedule 2 CDs stored in a locked,<br />
secure, non-portable receptacle?<br />
Is the receptacle permanently affixed to an<br />
internal wall?<br />
Is the receptacle used only for CDs?<br />
Are all stock CDs kept in their original<br />
containers?<br />
Are different strengths of the same medicines<br />
segregated?<br />
Are there any patient‘s own medicines stored<br />
in the CD receptacle?<br />
Are out of date/returned medicines/out of date<br />
stock segregated?<br />
Are patient returned medicines ever reused?<br />
Is there a written standard operating<br />
procedure which details routine date checking<br />
of stock CDs?<br />
How often does routine date checking take<br />
place?<br />
Is the room containing the CD receptacle<br />
lockable?<br />
Is the room containing the CD receptacle kept<br />
locked?<br />
Does the room containing the CD receptacle<br />
have limited access?<br />
Is there a named person detailed in a written<br />
standard operating procedure, with<br />
Yes No Details<br />
Page 147 of 196
esponsibility for the CD receptacle and a list<br />
of the current key holder(s)?<br />
Is there a clear daily audit trail for key holders<br />
(i.e. keys signed in and out, and not stored in<br />
a drawer)?<br />
Do you store naloxone in the department?<br />
Section 4b: Security and safe custody of <strong>Controlled</strong> <strong>Drugs</strong> in transport<br />
Do you have written standard operating<br />
procedures in place for the transport of CDs?<br />
Are CDs kept in a locked receptacle during<br />
transport?<br />
Are records maintained of CDs in transport?<br />
Section 4c: Register of <strong>Controlled</strong> <strong>Drugs</strong><br />
Do you maintain a controlled drug register?<br />
Is the CD register stored safely, near to, but<br />
outside the CD receptacle?<br />
Are all records, registers and invoices kept for<br />
a minimum of 2 years?<br />
Have there been any patient or carer<br />
complaints involving the storage, transport or<br />
record keeping of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the storage, transport or<br />
record keeping of CDs?<br />
Have there been any significant events<br />
involving the storage, transport or record<br />
keeping of CDs?<br />
Section 4c: Paper based CD registers<br />
Yes No Details<br />
Yes No Details<br />
Yes No Details<br />
The following table may be used to identify which procedures are being followed and<br />
the number of registers in current use. Tick the box to indicate whether the criteria are<br />
being followed in the practice.<br />
Criterion Register Comments<br />
1. Format of register<br />
1.1 Bound book<br />
1.2 Separate section per drug<br />
1.3 Separate section per presentation with<br />
name and strength at top of each page<br />
2. Entries<br />
2.1 In ink<br />
Page 148 of 196
2.2 Chronological order<br />
2.3 Entries within 24 hours<br />
3. Errors and corrections<br />
3.1 As margin/foot notes<br />
3.2 Corrections dated<br />
3.3 Corrections initialled<br />
4. Record of receipt<br />
4.1 Date of receipt<br />
4.2 Name and address of supplier<br />
4.3 Amount obtained<br />
4.4 Form and strength obtained<br />
4.5 Running balance<br />
4.6 Signature<br />
4.7 Process for discrepancies<br />
5. Record of supply (discharge/return of<br />
patient‟s own drugs)<br />
5.1 Date of supply<br />
5.2 Name and address of person supplied<br />
5.3 Authority to supply<br />
5.4 Amount supplied<br />
5.5 Form and strength supplied<br />
5.6 Running balance<br />
5.7 Signature<br />
5.8 Collected by<br />
6. Record of administration<br />
6.1 Date of administration<br />
6.2 Name of person administered to (where<br />
appropriate)<br />
6.3 Name and authority of person<br />
administering<br />
6.4 Amount administered<br />
6.5 Form administered<br />
6.6 Time of administration<br />
6.7 Running balance<br />
6.8 Signature and witness where appropriate<br />
6.9 Procedure if pack contents incorrect<br />
7. Stock check<br />
7.1 Evidence of appropriate stock check e.g.<br />
monthly<br />
7.2 Stock checked and correct<br />
7.3 Different people carrying out stock check<br />
Section 5: Destruction of <strong>Controlled</strong> <strong>Drugs</strong><br />
Are CDs destroyed using recommended<br />
methods?<br />
Are there any CDs awaiting destruction in the<br />
CD receptacle?<br />
Is date expired CD stock clearly labelled?<br />
Is date expired CD stock clearly segregated?<br />
Yes No Details<br />
Page 149 of 196
Have there been any patient or carer<br />
complaints involving the destruction of CDs?<br />
Have there been any concerns expressed by<br />
colleagues, police, substance misuse services<br />
or others about the destruction of CDs?<br />
Have there been any significant events<br />
involving the destruction of CDs?<br />
Destruction of stock controlled drugs<br />
Is there a written standard operating<br />
procedure for the destruction of controlled<br />
drugs?<br />
Is destruction of stock CDs witnessed by an<br />
authorised person?<br />
Is the authorised person NOT directly involved<br />
with CD supply in the practice?<br />
Is the name, form, strength and quantity of the<br />
drug destroyed, entered into the CD register?<br />
Is the date of destruction entered into the<br />
register?<br />
Is the signature of the witness entered into the<br />
register?<br />
Destruction of patient returned controlled<br />
drugs<br />
Are records made of patient‘s own CDs in a<br />
separate book (not the stock CD register)?<br />
Does this book record:<br />
The date received?<br />
Name and address of the patient prescribed<br />
CD?<br />
Pharmacy where originally dispensed?<br />
Name, quantity, form of CD?<br />
Role of person returning CD?<br />
Name and signature of staff receiving CD?<br />
Name and signature of staff destroying CD<br />
and date?<br />
Name and signature of witness to destruction<br />
and date?<br />
Are patient‘s own CDs destroyed as soon as<br />
possible?<br />
Is the patient‘s own returns process audited?<br />
Page 150 of 196
Section 6: General<br />
Do all staff know who to contact at the<br />
Primary Care Organisation regarding<br />
concerns about other colleagues in relation to<br />
CDs?<br />
Comments<br />
Yes No Details<br />
It is good practice to keep all audit records for 7 years<br />
Revision Date: August 2010<br />
Page 151 of 196
Appendix M <strong>Controlled</strong> <strong>Drugs</strong>: Prison Audit<br />
Medicines Handling Audit for use in IDTS Implementation and CD Management<br />
Criterion 1 There are clear lines of accountability<br />
throughout the organisation…<br />
1.1 Job description of lead Pharmacist /pharmacy<br />
technician describes clear managerial and<br />
professional accountability to the PCT and/or<br />
Healthcare Manager<br />
1.2 Terms of reference of responsible committee(s)<br />
include medicines management and<br />
involvement of a Pharmacist in advising on IDTS<br />
e.g. DTC; IDTS steering & implementation<br />
groups<br />
1.3 An Organisational chart shows the relevant links<br />
to medicines management in IDTS ( clinical and<br />
medicines supply)<br />
1.4 A strategy exists for ensuring the safe & secure<br />
handling of medicines and this includes CDs<br />
1.5 There is an index of medicines policies relating<br />
to CDs and these are accessible and up to date<br />
& available in healthcare and pharmacy dept<br />
Criterion 2 Suitable controls are in place that ensure the<br />
principles of the NPC primary Care CD<br />
Guidance and Duthie report are met<br />
Wings, clinics & wards<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
Planning for<br />
Delivery (1)<br />
Planning for<br />
Delivery (1)<br />
Planning for<br />
Delivery (1)<br />
Planning for<br />
Delivery (1)<br />
IDTS Delivery<br />
(22-<br />
Pharmacy)<br />
Comments Relating to Interpretation for<br />
CDs in Prisons
2.1 Designated staff check items received against<br />
requisition/delivery note<br />
2.2 Goods are signed for at wing level by<br />
designated staff<br />
2.3 Designated staff return requisition/delivery note<br />
to confirm delivery<br />
Pharmacy/Healthcare Centre (HCC)<br />
2.4 There is a schedule for rolling stock checks that<br />
is adhered to and SOPs must reflect the checks<br />
and frequency of checks<br />
2.5 Ad hoc orders are in writing and meet the legal<br />
requirements<br />
IDTS Delivery<br />
(22 -<br />
Pharmacy)<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
Page 153 of 196<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
Where administration/supply occurs on a<br />
designated wing or area/clinic room: official<br />
CD Requisition book is needed (carbonated<br />
and sequentially numbered)<br />
Usually the top (white) copy of the requisition<br />
book mentioned in 2.2<br />
CD Stocks checked regularly in Healthcare on<br />
wings/areas/clinic rooms. An overall prison<br />
stock reconciliation check by designated staff<br />
(e.g.by pharmacist on clinical visit) will be<br />
required at least once a month. This monthly<br />
check to be recorded in a different colour ink<br />
for ease of reconciliation/audit (e.g. green/red<br />
pen). In an on-site pharmacy dept, a rolling<br />
stock check of pharmacy stocks should be<br />
performed at least weekly.<br />
If discrepancies arise, or if volume of use<br />
necessitates, more frequent checks would be<br />
needed.Records of checks must be kept for<br />
as long as legislation dictates. (see section<br />
2.9 - soon to be 11 years, as for registers)<br />
For wings/wards/treatment rooms, requisition<br />
books as in 2.2 are required.
2.6 Copies of orders are kept for 2 years at least see 2.9 below<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
Page 154 of 196<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
2.7 Job descriptions identify responsible staff Legally the doctor is responsible for CD<br />
ordering in Healthcare. The Head of<br />
Healthcare (principal healthcare professional)<br />
should be the designated person responsible<br />
for the possession/handling of CDs in the<br />
prison. The Principal Pharmacist is<br />
responsible for the possession/handling of<br />
CDs in the Pharmacy. Job Descriptions<br />
should include delegated responsibilities of<br />
other prison and healthcare staff relating to<br />
medicines, including CDs.<br />
2.8 Duties of purchasing and receipt are separated Where ever practical, duties should be<br />
separated. All receipts of stock must be<br />
witnessed and checked against the order<br />
2.9 Records are held for periods of time identified by<br />
the CD Regulations e.g. CD Register, CD<br />
Prescriptions and Requisitions/Orders<br />
/requisition and signed as such.<br />
Currently all Registers, requisitions and<br />
orders (and invoices) for controlled drugs<br />
must be preserved for 2 years. The 2001<br />
Regulations have been amended to allow the<br />
information in these records to be preserved<br />
in the original paper form or in computerised<br />
form (as long as secure). Once<br />
computerised recording is in common use,<br />
The Government intends that secure<br />
computerised copies be kept for 11 years.
2.10 An audit trail exists for the ordering, receipt and<br />
supply of medicines<br />
Criterion 3 Medicines are stored and handled in a safe<br />
and secure manner<br />
HCC, wings, clinics & wards<br />
3.1 Medicines are locked away immediately on<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
Page 155 of 196<br />
Essential for CDs as every tablet or ml of<br />
liquid must be accounted for and there must<br />
be a robust audit trail in place.<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
receipt<br />
IDTS Delivery<br />
(22-Pharmacy)<br />
3.2 CD Medicine storage cabinets meet standards<br />
Facilities see the Silver level of the 'Sold Secure'<br />
of the Misuse of <strong>Drugs</strong> Regulations<br />
Required (7 & standard SS304 (domestic safes).Currently<br />
8)<br />
exceed the Misuse of Drug regulations but<br />
advised by the Home Office as being more<br />
effective and appropriate for prisons.<br />
Stationery is kept secure: Facilities Must be kept secure and only available to<br />
Required (7 & designated authorised persons. Their security<br />
8) & IDTS must be dealt with in the relevant Standard<br />
Delivery (22 - Operating Procedures<br />
Pharmacy)<br />
3.3 CD requisition books and Registers<br />
3.4 Prescription pads & charts<br />
3.5 Order Pads<br />
Transport of medicines:
3.6 There is a Standard Operating Procedure for the<br />
secure transport of CDs into and within the<br />
prison<br />
3.7 Ward/wing/clinic area CD's are sealed in a<br />
designated bag/box before delivery to them<br />
Page 156 of 196<br />
Facilities<br />
Required (7&8)<br />
IDTS Delivery<br />
(22 -<br />
Pharmacy)<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
3.8 All stock medicines are sent in sealable<br />
container<br />
Security: Facilities<br />
Required (7&8)<br />
This should be considered in the prison Risk<br />
Management procedure. The messenger<br />
transporting drugs must be aware of the<br />
security issues and the audit trail in 2.9.<br />
Authorised signatory must ensure they sign to<br />
confirm exactly what is received i.e. quantity<br />
and strength of drug. (Gate staff are NOT<br />
authorised signatories). There must be a<br />
robust audit trail from receipt of CD at the<br />
Gate to Healthcare/Pharmacy.<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
Must be considered in prison's CD policy,<br />
including all places in the prison where the<br />
CDs are stored and administered.<br />
Recommended that benzodiazepines are<br />
stored and managed as for all other CDs<br />
3.9 Pharmacy/HCC is secure Gated room; walls floors and ceilings solid.<br />
3.10 Access to Pharmacy/HCC areas is restricted<br />
3.11 Entrances to Pharmacy/HCC have secure solid<br />
doors & security locks<br />
Other:<br />
Adhere to Prison security guidelines
3.12 Lists of CDs that are stocked are available,<br />
maintained and updated regularly for healthcare,<br />
all areas, wings, clinics & wards<br />
3.13 Medicines etc for emergency use are available<br />
in a suitable presentation and regularly checked<br />
for expiry dates and stock levels maintained<br />
3.14 Policies and procedures in place that describe<br />
the actions to be taken with CDs if prison<br />
security is breached or if discrepancies in CD<br />
stock levels are identified<br />
Page 157 of 196<br />
IDTS Delivery<br />
(22-<br />
Pharmacy)<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
IDTS Delivery<br />
(22- Pharmacy<br />
and 24)<br />
IDTS Delivery (<br />
22- Pharmacy)<br />
Facilities<br />
Required (7&8)<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
Naloxone must be available for use in opiate<br />
toxicity (in Emergency Bags?). Consider<br />
availability where opiates are administered<br />
AND where toxicity likely to be identified (on<br />
wings?). Staff training and administration<br />
procedures must also be completed.<br />
This relates to when either<br />
Healthcare/Pharmacy security is breached or<br />
when there is "loss of control" in the prison or<br />
a prison area. Risks to the security of CDs<br />
must be considered in such cases.<br />
Discrepancies and security breaches should<br />
be recorded as critical incidents and a<br />
procedure for reporting these incidents should<br />
be in place. This would include the escalation<br />
of the incident to high risk/ investigation<br />
should more than one incident occur in a<br />
given area over a specified time period,<br />
especially if the same practitioner is involved.
Criterion 4 Prescription, supply and administration<br />
conform to the requirements of relevant<br />
legislation. Prescription, supply and<br />
administration of medicines is undertaken<br />
only by appropriately qualified staff.<br />
Page 158 of 196<br />
IDTS Delivery<br />
(22 -<br />
Pharmacy)<br />
Facilities<br />
Required (<br />
7&8)<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
4.1 All prescriptions are written by a doctor IDTS Delivery<br />
(21)<br />
4.2 All issues of CDs, including benzodiazepines,<br />
are administered by supervised consumption<br />
underpinned by an SOP<br />
4.3 Administration charts are always available to<br />
record all transactions with prisoners including<br />
issues of 'canteen list' medicines<br />
IDTS Delivery<br />
(21 and 22 -<br />
Pharmacy)<br />
Recommend that all Methadone is<br />
administered via automated pumps (manual<br />
or computerised depending on frequency)<br />
NOT by measuring out doses in conical<br />
measures unless methadone is used<br />
infrequently. Pharmacists should advise about<br />
use, maintenance and calibration of these.<br />
SOPs must specify these details.<br />
Administration of CDs requires 2 staff, one of<br />
whom should be a Healthcare Professional<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
Nurse and pharmacist prescribers can<br />
prescribe CDs for substance misuse via<br />
Supplementary Prescribing ONLY<br />
currently.<br />
For IDTS programme<br />
If CDs are administered using a computerised<br />
record, then any written Drug Administration<br />
charts and patient medical notes should<br />
clearly state that the patient is receiving<br />
treatment for substance misuse and what they<br />
are prescribed. This allows for any clinical<br />
review (e.g. for a pharmacist checking the<br />
appropriateness of another prescribed/OTC<br />
medicine or another prescriber) to take into<br />
account this therapy.
4.4 All prescriptions are clinically checked by a<br />
pharmacist<br />
4.5 All relevant policies are in place and up to date<br />
(including PGDs)<br />
4.6 Proof of registration of all pharmacists &<br />
Pharmacy Technicians is checked annually<br />
4.7 Pharmacy services are in place to monitor and<br />
review prescription writing against locally agreed<br />
standards e.g. administration charts handwritten<br />
by Docs/nurse prescribers are clear and<br />
legible<br />
4.8 Prisoners have access to advice and<br />
counselling re their medicines from a<br />
pharmacist/technician or if not available, other<br />
member of the HC staff<br />
4.9 Prisoners are supplied with written information<br />
leaflets ideally each time a medicine is<br />
dispensed (in accordance with EU regulations)<br />
Page 159 of 196<br />
The prescriber is responsible until the<br />
pharmacist check is made<br />
see 4.12 below<br />
Workforce (14) Pharmacy technicians should be registered if<br />
they are managing the supply/administration<br />
of CDs.<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
IDTS Delivery<br />
(22 -<br />
Pharmacy)<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
Prescription writing for CDs must comply with<br />
the Misuse of <strong>Drugs</strong> Regulations.(latest<br />
guidance Jul 06) i.e. quantity must still be in<br />
words & figures etc but Dr does not now need<br />
to handwrite whole prescription<br />
CARAT staff should be able to signpost<br />
prisoners for medicines advice, so this advice<br />
can be part of the advice and counselling<br />
available to prisoners receiving treatment for<br />
substance misuse (including treatment for<br />
benzodiazepines, alcohol as well as opiate<br />
misuse).<br />
Because the CDs will be administered under<br />
supervision (NIP) Healthcare/ pharmacy<br />
should make any patient information leaflets<br />
available during initial stabilisation as well as<br />
later during treatment
4.10 There is a procedure for correctly identifying<br />
prisoners when administering medication<br />
4.11 Prisoners are observed taking/using their NIP<br />
medicines by HC staff<br />
4.12 Supply and administration of drugs is covered<br />
by a Patient Group Direction where appropriate<br />
4.13 Any CDs issued to prisoners directly from stock<br />
are issued under the directions of a doctor and<br />
recorded<br />
Criterion 5 The prescribing, supply, administration, safe<br />
custody and destruction of controlled<br />
medicines complies with the appropriate<br />
legislation.<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
Page 160 of 196<br />
Some IT systems will provide for iris or<br />
fingerprint recognition. In the absence of<br />
these, there must be a clearly stated means<br />
of confirming prisoner ID as part of the SOPs<br />
for administration of methadone.<br />
This should be the case for all CDs used in<br />
Substance Misuse, including benzodiazepines<br />
and SOPs should specify this. Prison<br />
procedures and protocols should mirror those<br />
in primary care/ community pharmacy.<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
Not applicable for CDs for Substance<br />
Misuse as these cannot be supplied under<br />
PGDs. Naloxone is able to be administered,<br />
exempt from the Medicines Act, in an<br />
emergency however.<br />
As all doses will be administered under<br />
supervision (NIP), the CDs should be<br />
administered from stock supplies. There must<br />
be set protocols for administration by<br />
supervised consumption.
5.1 All relevant policies are in place and up to date<br />
5.2 Prescriptions for CDs comply with Legislation<br />
5.3 Pharmacy CD registers are stored for 2 years Likely to be eleven years when regulations<br />
amended<br />
5.4 CD requisitions and registers are completed<br />
correctly<br />
5.5 CD levels checked by the auditor are correct<br />
5.6 CD checks are up to date<br />
5.7 Only authorised personnel order, supply,<br />
possess, prescribe & administer CDs<br />
5.8 The destruction and disposal of CDs complies<br />
with legislation<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
Page 161 of 196<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
Legally only the doctor or pharmacist can<br />
order CDs and so must countersign any<br />
Requisitions but the Head of Healthcare<br />
(healthcare professional) should have<br />
designated overall authority and<br />
accountability for the management of CDs<br />
within the prison. Responsibilities in this<br />
section should be delegated to appropriate<br />
named staff only.<br />
Advice from the PCTs Accountable Officer<br />
should be sought. It is important that there is<br />
an efficient mechanism for arranging for CD<br />
destruction to prevent excess stocks being<br />
stored.
Criterion 6 All medicines no longer required are<br />
destroyed or otherwise disposed of in<br />
accordance with safety, legal and<br />
environmental requirements<br />
6.1 The Pharmacy/HCC procedure is in place and<br />
up to date<br />
6.2 The prison's policy for the management of<br />
pharmaceutical waste is in line with that of the<br />
PCT<br />
6.3 An audit trail exists that can be used to follow<br />
the handling of pharmaceutical waste<br />
Criterion 7 The organisation reports adverse incidents<br />
involving medicinal products and devices to<br />
the relevant agency, and appropriately<br />
manages any subsequent required action.<br />
7.1 Procedure is in place and up to date and<br />
pharmacy/HCC responsibilities are documented<br />
7.2 Staff are aware of incident/ADR/defective<br />
product recall procedures<br />
7.3 There is evidence that recalls are effectively<br />
implemented<br />
Page 162 of 196<br />
IDTS Delivery<br />
(22 -<br />
Pharmacy)<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
IDTS Delivery<br />
(22 -<br />
Pharmacy)<br />
Note the destruction of CDs stock must be<br />
witnessed by an authorised person (check<br />
with Accountable Officer at PCT) and<br />
rendered irretrievable. An SOP is needed.<br />
See 5.8 above<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
Incidents involving CDs are a high priority for<br />
identifying, reporting, investigating and<br />
actioning any follow-up. There should be an<br />
SOP specifying a clear cascade of<br />
alerts/recalls to relevant staff.
7.4 Errors are reported through a risk management<br />
framework<br />
7.5 Medication incidents are investigated and<br />
reported locally<br />
7.6 All NPSA alerts and safety notices are<br />
implemented<br />
Criterion 8 Supervision of pharmaceutical dispensing<br />
processes is undertaken in accordance with<br />
relevant legislation and current professional<br />
standards.<br />
8.1 Procedures are in place and up to date IDTS Delivery<br />
(22-Pharmacy)<br />
Yes No IDTS Toolkit<br />
Reference<br />
8.2 Staff rotas are in place to ensure adequate<br />
cover<br />
Page 163 of 196<br />
Section<br />
Workforce<br />
(15,18)<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
There will always need to be 2 people ( one of<br />
which must be a registered nurse or<br />
registered pharmacy technician or doctor or<br />
pharmacist, plus another competent person)<br />
involved in administering CDs to patients<br />
8.3 Checking technicians are externally accredited Registered Pharmacy Technicians should<br />
complete the ACT course, especially if there<br />
8.4 All prescriptions are clinically checked by a<br />
pharmacist<br />
IDTS Delivery<br />
(22-Pharmacy)<br />
is not an on-site pharmacist.<br />
This should be incorporated into the supply<br />
process, as for patients receiving other<br />
medication, to ensure quality of care. Initial<br />
supplies may not have been checked by a<br />
pharmacist if they have not dispensed the CD.<br />
In this case responsibility rests with the<br />
prescriber until the clinical check has been
8.5 Medication-related errors are recorded and<br />
reviewed<br />
8.6 Policies and procedures are in place if<br />
extemporaneous preparations are needed<br />
8.7 Extemps are only prepared where no equivalent<br />
licensed product is available<br />
Criterion 9 The risk management process contained<br />
within the Risk Management standard is<br />
applied to the safe and secure handling of<br />
medicines.<br />
19.1 All identified risks are documented, assessed<br />
and prioritised<br />
19.2 Action plans are developed and implemented<br />
9.3 The PCT Board or equivalent is informed and<br />
updated on significant risks<br />
Page 164 of 196<br />
Planning for<br />
Delivery (5)<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
made by the pharmacist.<br />
See section 7<br />
Prison Pharmacies should not be<br />
reconstituting Methadone Mixture from the<br />
powder and diluents or using the concentrate.<br />
All supplies should be made using the 1mg/ml<br />
Methadone Mixture that is commercially<br />
available.<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
The IDTS implementation group within the<br />
establishment (in partnership with the D&T /<br />
Medicines Committee) should identify any<br />
risks associated with the medicines storage<br />
and handling of CDs. These should be<br />
included in the PCT/Prison Risk Register.
9.4 Staff are aware of systems in place to minimise<br />
risk e.g. protocols for dispensing and supply of<br />
medicines<br />
Criterion 10 All healthcare staff involved with medicines<br />
undertakes continuing professional<br />
development to ensure that there are safe<br />
and secure handling processes in place.<br />
Page 165 of 196<br />
Workforce (14,<br />
15,16, 17 &<br />
19)<br />
All staff involved in medicines storage and<br />
handling of CDs should have read and signed<br />
the relevant SOPs<br />
Pharmacy Pharmacists: All pharmacists involved in IDTS<br />
should have completed the CPPE course<br />
'Substance Use & Misuse' and the viva day to<br />
attain the RCGP Part 1 certificate in<br />
Substance Misuse. Pharmacy Technicians<br />
should all be registered and have completed<br />
the CPPE course 'Substance Use and<br />
Misuse- fundamentals and practicalities for<br />
the pharmacy technician‘ (modules 1-3) and<br />
the viva day to attain the RCGP Part 1<br />
certificate in Substance Misuse. Pharmacists<br />
involved in clinical services should have<br />
10.1 Training and development plans are in place<br />
10.2 All pharmacy staff maintain CPD records<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
completed RCGP part 2 training.<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
10.3 Staff are aware of local policies<br />
Other healthcare staff / Prison Officers Medicines Management training required by<br />
these groups should be identified, prioritised<br />
and needs met prior to approval of statement<br />
of readiness. This includes training for staff<br />
not directly involved in medicines handling
10.4 Training and development plans are in place<br />
10.5 Healthcare staff maintain CPD records<br />
10.6 Staff are aware of local policies<br />
Criterion 11 The organisation, through the Lead<br />
Pharmacist/Technician, has access to up-todate<br />
legislation and guidance relating to the<br />
safe and secure handling of medicines.<br />
11.1 Can demonstrate access to relevant information<br />
and means of update<br />
11.2 Can demonstrate mechanism for cascading<br />
information to appropriate prison staff<br />
Criterion 12 Adequate resources support the safe and<br />
secure handling of medicines.<br />
12.1 A development plan that includes <strong>Controlled</strong><br />
<strong>Drugs</strong> is in place & there is a planned review<br />
process<br />
Page 166 of 196<br />
Facilities<br />
Required (7&<br />
8)<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
Planning for<br />
Delivery (1 &<br />
6) Workforce<br />
(14,15 20)<br />
and storage.<br />
The registered pharmacy practitioner and<br />
Head of Healthcare will be responsible for<br />
ensuring that developments/requirements in<br />
the management of CDs are identified and<br />
cascaded to other staff as necessary.<br />
Comments Relating to Interpretation for<br />
CDs in Prisons
12.2 The pharmacy service & medicines<br />
administration is safely resourced in terms of<br />
staffing, equipment and facilities<br />
12.3 If resources are not adequate, key areas where<br />
funding is required are identified in the<br />
development plan<br />
Criterion 13 The system in place is monitored and<br />
reviewed by management and the Board in<br />
order to make improvements to the system<br />
13.1 Internal audits reports are seen by the Board<br />
13.2 Minutes of relevant meetings are seen by the<br />
Board<br />
13.3 The PCT Accountable Officer for <strong>Controlled</strong><br />
<strong>Drugs</strong> is also included in IDTS implementation,<br />
as appropriate, and has access to<br />
documentation in 13.1. & 13.2 above<br />
Yes No IDTS Toolkit<br />
Reference<br />
Section<br />
Page 167 of 196<br />
It is essential that, as well as the medical and<br />
nursing workforce needs identified by IDTS<br />
implementation, the growth needed in<br />
pharmacy staff (Pharmacy technicians,<br />
Pharmacy Assistants and Pharmacist clinical<br />
input) is included in the IDTS workforce<br />
requirements.<br />
Comments Relating to Interpretation for<br />
CDs in Prisons<br />
N.B. CD Regulations & The Health Act require<br />
appointment of an Accountable Officer to<br />
ensure there are robust arrangements for safe<br />
& effective handling of CDs. The PCT<br />
Accountable Officer will have jurisdiction over<br />
prisons in their area.
Criterion 14 The PCT Board seeks independent<br />
assurance that an appropriate and effective<br />
system is in place.<br />
14.1 External audit reports reviewed<br />
Page 168 of 196<br />
Commissioning<br />
(11)<br />
Future external audits are likely to include the<br />
management of CDs. A duty of Collaboration<br />
is placed on responsible bodies (Healthcare<br />
organisations, police forces, Healthcare<br />
Commission, Prison Inspectorate etc) under<br />
the Health Act 2006 to share information on<br />
CDs.
Appendix N<br />
USEFUL EXTERNAL CONTACTS<br />
British Medical Association<br />
BMA House Tel: 0207 387 4499<br />
Tavistock Square Fax: 0207 383 6400<br />
London Website: www.bma.org.uk<br />
WC1H 9JP<br />
Care Quality Commission<br />
Citygate Tel: 03000 616 161<br />
Gallowgate<br />
Newcastle upon Tyne Website: www.cqc.org.uk<br />
NE1 4PA<br />
Community practitioners‘ and Health Visitors Association<br />
33-37 Moreland Street Tel: 0207 505 3000<br />
London<br />
EC1V 8HA Website: www.amicustheunion.org/cphva/<br />
Council for Healthcare Regulatory Excellence<br />
1 st Floor, Kierran Cross Tel: 0207 389 8030<br />
11 Strand Fax: 0207 389 8040<br />
London Website: www.chre.org.uk<br />
WC2N 5HR<br />
Department of Health<br />
Richmond House Tel: 0207 210 4850<br />
79 Whitehall Website: www.dh.gov.uk<br />
London<br />
SW1A 2NS<br />
Dispensing Doctors‘ Association<br />
Low Hagg Farm Tel: 01751 430835<br />
Starfitts Lane Fax: 01751 430836<br />
Kirbymoorside Website: www.dispensing doctor.org<br />
North Yorkshire<br />
YO62 7JF<br />
Environment Agency<br />
Millbank Tower Tel: 08708 506 506<br />
25 th Floor Website: www.environment-agency.gov.uk<br />
21/24 Millbank<br />
London<br />
SW1P 4XL
General Medical Council<br />
Regent‘s Place Tel: 0845 357 3456<br />
350 Euston Road Website: www.gmc-uk.org<br />
London<br />
NW1 3JN<br />
Home Office <strong>Drugs</strong> Licensing Branch<br />
2 Marsham Street Tel: 0207 035 0483<br />
London Website: www.homeoffice.gov.uk<br />
SW1P 4DF<br />
Home Office <strong>Drugs</strong> Legislation and Enforcement Unit<br />
2 Marsham Street Tel: 0207 035 0464<br />
London Website: www.homeoffice.gov.uk<br />
SW1P 4DF<br />
Medicines and Healthcare products Regulatory Agency<br />
Market Towers Tel: 0207 084 2000<br />
1 Nine Elms lane Fax: 0207 084 2353<br />
London Website: www.mhra .gov.uk<br />
SW8 5NQ<br />
National <strong>Clinical</strong> Assessment Service (part of the National Patient Safety Agency)<br />
Market Towers Tel: 0207 062 1620<br />
1 Nine Elms Lane Fax: 0207 084 3851<br />
London Website: www.ncas.npsa.nhs.uk<br />
SW8 5NQ<br />
National Patient Safety Agency<br />
4-8 Maple Street Tel: 0207 927 9500<br />
London Website: www.npsa.nhs.uk<br />
W1T 5HD<br />
National Pharmacy Association<br />
Mallinson House Tel: 01727 832161<br />
38-42 St Peter‘s Street Fax: 01727 840858<br />
St Albans Website: www.npa.co.uk<br />
Hertfordshire<br />
AL1 3NP<br />
National Prescribing Centre<br />
The Infirmary Tel: 0151 794 8134<br />
70 Pembroke Place Fax: 0151 794 8139<br />
Liverpool Website: www.npc.co.uk (Internet)<br />
L69 3GF www.npc.nhs.uk (<strong>NHS</strong>Net)<br />
National Treatment Agency<br />
8 th Floor Tel: 020 7261 8801<br />
Hercules House Fax: 020 7261 8883<br />
Hercules Road Website: www.nta.nhs.uk<br />
London<br />
SE1 7DU<br />
Page 170 of 196
<strong>NHS</strong> <strong>Clinical</strong> Governance Support Team<br />
1 st Floor Tel: 0116 295 2000<br />
St. Johns House Fax: 0116 295 2001<br />
30 East Street Website: www.egsupport.nhs.uk<br />
Leicester<br />
LE1 6NB<br />
<strong>NHS</strong> Direct<br />
Headquarters Tel: 0207 599 4200<br />
207 Old Street Fax: 0207 599 4299<br />
London Website: www.nhsdirect.nhs.uk<br />
EC1V 9PS<br />
Nursing and Midwifery Council<br />
23 Portland Place Tel: 020 7637 7181<br />
London Fax: 020 7436 2924<br />
W1B 1PZ Website: www.nmc-uk.org<br />
Pharmaceutical Services Negotiating Committee<br />
59 Buckingham Street Tel: 01296 432 823<br />
Aylesbury Fax: 01296 438 427<br />
Buckinghamshire Website: www.psnc.org.uk<br />
HP20 2PJ<br />
Prescription Pricing Divisions of the <strong>NHS</strong> Business Services Authority<br />
Bridge House Tel: 0191 232 5371<br />
152 Pilgrim Street Fax: 0191 232 2480<br />
Newcastle-upon-Tyne Website: www.ppa.org.uk<br />
NE1 6SN<br />
Prescribing Support Unit<br />
The Health and Social Care Information Centre Tel: 0113 254 7041<br />
1 Trevelyan Square Fax: 0113 254 7097<br />
Boar lane Website: www.psu.nhs.uk<br />
Leeds<br />
LS1 6AE<br />
Royal College of General Practitioners<br />
RCGP Substance Misuse Unit Tel: 0845 4564041 Ext. 217<br />
14 Princess Gate Fax: 0207 225 3047<br />
Hyde Park Website: www.regp.org.uk/substance<br />
London<br />
SW7 1PU<br />
Royal College of Nursing<br />
Head Office Tel: 0207 409 3333<br />
20 Cavendish Square Website: www.ren.org.uk<br />
London<br />
W1G 0RN<br />
Royal Pharmaceutical Society of Great Britain<br />
1 Lambeth High Street Tel: 0207 735 9141<br />
London Fax: 0207 735 7629<br />
SE1 7JN Website: www.rpsgb.org.uk<br />
Page 171 of 196
UK Home Care Association<br />
42b Banstead Road Tel: 0208 288 1551<br />
Carshalton Beeches Fax: 0208 288 1550<br />
Surrey Website: www.ukhca.co.uk<br />
SM5 3NW<br />
Page 172 of 196
Drug<br />
Appendix O<br />
Table of <strong>Controlled</strong> drugs and indications allowed to be prescribed by Nurse<br />
Independent Prescriber‟s<br />
Schedule*<br />
Indication<br />
Page 173 of 196<br />
Route of administration<br />
Buprenorphine 3 Transdermal use in palliative care Transdermal<br />
Chlordiazepoxide<br />
Hydrochloride<br />
4<br />
Treatment of initial or acute<br />
withdrawal symptoms caused by<br />
the withdrawal of alcohol from<br />
persons habituated to it<br />
Codeine phosphate 5 N/A Oral<br />
Co-phenotrope 5 N/A<br />
Use in palliative care, pain relief<br />
Oral<br />
Diamorphine<br />
2 in respect of suspected myocardial Oral or parenteral<br />
Hydrochloride<br />
infarction of for relief of acute or<br />
severe pain of trauma, including<br />
in either case post-operative pain<br />
relief<br />
Use in palliative care, treatment<br />
of initial or acute withdrawal<br />
Diazepam<br />
4 symptoms caused by the withdrawal<br />
of alcohol from persons<br />
habituated to it, tonic-clonic<br />
seizures<br />
Oral, parenteral or rectal<br />
Dihydrocodeine tartrate 5 N/A Oral<br />
Fentanyl 2 Transdermal use in palliative care Transdermal<br />
Lorazepam 4 Use in palliative care, tonic-clonic<br />
seizures<br />
Oral or parenteral<br />
Midazolam 3 Use in palliative care, tonic-clonic<br />
seizures<br />
Use in palliative care, pain relief in<br />
respect of suspected myocardial<br />
Parenteral or buccal<br />
Morphine hydrochloride 2 infarction or for relief of acute or<br />
severe pain after trauma, including<br />
in either case post-operative pain<br />
relief<br />
Use in palliative care, pain relief<br />
Rectal<br />
Morphine sulphate 2 in respect of suspected myocardial<br />
infarction or for relief of acute or<br />
severe pain after trauma, including<br />
in either case post-operative pain<br />
relief<br />
Oral, parenteral or rectal<br />
Oral or parenteral<br />
Oxycodone<br />
2 Use in palliative care<br />
administration in<br />
Hydrochloride<br />
palliative care<br />
*Schedule 1-5 of the Misuse of <strong>Drugs</strong> Regulations 2001<br />
For the purposes of nurse independent prescribing, palliative care means the care of patients with advanced progressive<br />
illness.<br />
Oral
Appendix P<br />
Methods of Destruction of <strong>Controlled</strong> <strong>Drugs</strong><br />
All medicines should be disposed of in a safe and appropriate manner. Medicines<br />
should be disposed of in relevant waste containers which are then sent for incineration<br />
and should not be disposed of in the sewerage system.<br />
All CDs in Schedule 2, 3 and 4 (part I) can be placed into waste containers only after<br />
the controlled drug has been rendered irretrievable (i.e. by denaturing).<br />
Wherever practicable, CD denaturing kits should be used in order to denature CDs.<br />
Where this is not possible or practical other methods of denaturing may be used. In the<br />
past, various methods have been used to denature controlled drugs, including grinding<br />
together with other waste medicines, and / or dissolving in soapy water or adsorbing<br />
onto cat litter.<br />
Having considered the risks posed by destruction of CDs in a pharmacy, the<br />
Environment Agency (EA), which covers England and Wales, has decided that it does<br />
not believe it is in the public interest to expect pharmacies to obtain a waste<br />
management license for denaturing CDs and this is seen by the EA as a ‗low risk‘<br />
activity. The EA emphasises, however, that it may amend or revoke its position at any<br />
time and will continue enforcement in all circumstances where activity has or is likely to<br />
cause pollution or harm to health. So, pharmacists must ensure that the activities they<br />
undertake to denature CDs protect the environment and workers and others within the<br />
pharmacy. These guidelines may transfer to other Healthcare settings e.g. Community<br />
Nursing.<br />
Solid dose formulations<br />
Tablets and capsules can be removed from their outer packaging, removed from blister<br />
packaging and placed in a CD denaturing kit. If a person is removing tablets / capsules<br />
from blister packs they should wear gloves.<br />
CD denaturing kits can be obtained from some PCTs, waste contractors, <strong>NHS</strong><br />
Supplies and the National Pharmacy Association.<br />
Best practice would be to grind* or crush* the solid dose formulation before adding to<br />
the CD denaturing kit to ensure that whole tablets or capsules are not readily<br />
recoverable.<br />
An alternative method of denaturing is to crush or grind the solid dose formulation and<br />
place it into a small amount of hot, soapy water stirring sufficiently to ensure the drug<br />
has been dissolved or dispersed. The resulting mixture may then be added to an<br />
appropriate waste disposal bin supplied by the waste contractor.<br />
*If grinding or crushing of tablets or capsules takes place, steps must be taken to<br />
ensure that particles of CD dust are not released into the air or that this is minimised.<br />
The use of a small amount of water whilst grinding or crushing may assist. It may also<br />
be necessary for the person involved in the grinding or crushing to wear a suitable face<br />
mask for protection, suitable gloves and ensure that the area is well ventilated.<br />
Liquid dose formulations<br />
A CD liquid can be poured from its container and added to the normal CD denaturing<br />
kit where it will mix with the other waste materials, thus rendering it irretrievable.<br />
Page 174 of 196
An alternative method of disposing of a large quantity of a liquid controlled drug is by<br />
adding and adsorbing it into an appropriate amount of cat litter, or similar product.<br />
However, this activity would need to take account of health and safety regulations so<br />
that the person destroying the CDs and the environment are safeguarded from harm<br />
and pollution. The cat litter or similar product should be disposed of for incineration via<br />
the usual waste disposal methods for medicines.<br />
Parenteral formulations<br />
Liquid ampoules should be opened and as much of the content as possible emptied<br />
into the CD denaturing kit or disposed of in the same manner as disposing of liquids<br />
outlined above.<br />
The ampoule should be disposed off in the sharps bin. The sharps bin should be<br />
labelled ―contains mixed pharmaceutical waste and sharps – for incineration‖.<br />
Ampoules containing the CD in a powder form can be opened, water added to dissolve<br />
the powder and the resultant mixture poured into the CD denaturing kit or the bin that<br />
is used for disposal of liquid medicines. The ampoule can then be disposed of in the<br />
sharps bin. The sharps bin should be labelled ―contains mixed pharmaceutical waste<br />
and sharps – for incineration‖. These are the ideal methods of denaturing ampoules.<br />
Suitable gloves should be worn by the person breaking open glass ampoules as a<br />
safety measure and to minimise the risk of injury from sharps.<br />
An alternative but less preferable, disposal method is where the ampoules are crushed<br />
with a pestle inside an empty plastic container. Once broken, a small quantity of hot<br />
soapy water (for powder ampoules) or cat litter (for liquid ampoules) is added. If these<br />
methods are used, care should be taken to ensure that the glass does not harm the<br />
person destroying the CD. The resulting liquid mixture should then be disposed of in a<br />
CD denaturing kit or in the bin that is used for disposal of liquid medicines.<br />
Fentanyl and buprenorphine patches<br />
The active ingredient in the patches can be rendered irretrievable by removing the<br />
backing and folding the patch over on itself and then placing it in a waste disposal bin<br />
or preferably a CD denaturing kit. Gloves must be worn by the person destroying the<br />
CD.<br />
Aerosol formulations<br />
Aerosol formulations should be expelled into water (to prevent droplets of drug<br />
entering the air). As a further precaution, it would be advisable for a facemask to be<br />
worn by staff undertaking the activity and to ensure that the area where the destruction<br />
takes place is well ventilated. The resulting solution can then be disposed of in<br />
accordance with the above guidance on destruction of liquid formulations.<br />
<strong>Controlled</strong> Drug Denaturing Kit<br />
Shake container to loosen granules.<br />
Fill container with one filling. (I.e. even if only one tablet/ampoule to destroy &<br />
complete the process below)<br />
Add the controlled drug as above to half the capacity of the jar.<br />
Fill to capacity with water.<br />
Replace lid securely.<br />
Shake thoroughly to disperse.<br />
Page 175 of 196
Contents congeal in 3 - 5 minute<br />
Dispose of the denaturing kit in the designated medicines waste bins<br />
immediately do not keep for further use.<br />
Dispose of denaturing container by secure incineration service.<br />
<strong>Controlled</strong> drug denaturing kits should not be used for the destruction of non CD<br />
medicines.<br />
Page 176 of 196
Appendix Q<br />
Standard Operating Procedure for witnessing the destruction of <strong>Controlled</strong><br />
<strong>Drugs</strong> by a delegated PCT Pharmacist.<br />
Version: 2<br />
Date produced: 16/9/07, Updated November 2009<br />
Revision Date: November 2012<br />
Produced By: Kate Huddart (Senior Pharmaceutical Adviser)<br />
Purpose: To ensure a standardised approach to controlled drug destruction by<br />
delegated PCT Pharmacists across <strong>County</strong> <strong>Durham</strong> and Darlington.<br />
1. Authorisation.<br />
1.1 PCT staff that destroys controlled drugs must have delegated authority from the<br />
Accountable Officer in writing. Currently delegated authority rests with the 7<br />
pharmacists employed within the Medical Directorate:-<br />
Kate Huddart<br />
Sharron Kebbell<br />
Linda Neely<br />
Joan Sutherland<br />
Ian Morris<br />
Hazel Betteney<br />
Stephen Purdy<br />
1.2 The above named delegated PCT Pharmacists are directly accountable to the<br />
Accountable Officer for controlled drugs destruction.<br />
2. Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in a G.P Practice / Dispensing Doctors<br />
2.1 Delegated PCT Pharmacist should take their own CD Destruction Log and a<br />
CD Denaturing kit with them to the practice.<br />
2.2 Delegated PCT Pharmacist inspects CD cupboard to ensure that it is of the<br />
correct standard and mounted in a secure way.<br />
Page 177 of 196
2.3 Delegated PCT Pharmacist, along with Practice Witness (G.P, Practice<br />
Manager or Practice Nurse) ensures keys are stored in a secure way.<br />
2.4 Delegated PCT Pharmacist makes an entry in the practice CD register giving<br />
the following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Drug, Formulation and Strength<br />
Batch Number and date of expiry<br />
Quantity to be destroyed<br />
Signature of the delegated PCT Pharmacist<br />
RPSGB number of the delegated Pharmacist<br />
e.g. 18/9/07 Morphine Sulphate 10mg (Sevredol) 24 tablets BN 213AB Expired<br />
20/06/07. Destroyed by PCT Pharmacist K E Huddart MRPharm Reg No 91749<br />
2.5 Practice Witness also signs the entry in the CD register.<br />
2.6 Prior to destruction check that any remaining in date stock balances with the<br />
running balance of stock.<br />
2.7 Amend running balance of stock<br />
2.8 Delegated PCT Pharmacist then makes an entry in their own CD Destruction<br />
Log Book giving the following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Drug, Formulation and Strength<br />
Quantity destroyed<br />
Signature of Pharmacist<br />
Printed name of Pharmacist<br />
2.9 Practice Witness also signs and prints their name against the entry in the<br />
delegated PCT Pharmacist‘s CD Destruction Log Book.<br />
2.10 The delegated PCT Pharmacist then carries out the destruction of the CD in the<br />
presence of the Practice Witness.<br />
2.11 The controlled drug must be destroyed as outlined in the RPSGB guidance for<br />
pharmacists on the Safe Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in England, Scotland and<br />
Wales.<br />
2.12 The process from 2.4 to 2.11 is repeated for each different strength and<br />
presentation of controlled drug that is out of date.<br />
2.13 The used CD Denaturing kit is then placed in the yellow medicines waste bin.<br />
2.14 The delegated PCT Pharmacist conducts a spot check on 2 other CD‘s running<br />
balances of stock. The delegated pharmacist makes an entry within the practice CD<br />
register on the relevant page of the stock check, noting any discrepancies or<br />
amendments to the running total<br />
E.g. 18/09/07 Stock check of Morphine Sulphate 10mg (Sevredol) tablets by PCT<br />
Pharmacist. K E Huddart MRPharm Reg. No. 91749. Stock check correct.<br />
Page 178 of 196
2.15 The delegated PCT Pharmacist conducts a CD Practice Audit (Appendix I within<br />
CD <strong>Policy</strong>) or a G.P. Dispensing Practice Audit (Appendix K within CD <strong>Policy</strong>), if the<br />
practice has not had a previous audit conducted during that financial year.<br />
2.16 If a previous CD Practice Audit has been completed then the delegated PCT<br />
Pharmacist must complete a CD Destruction Form (Appendix R within CD <strong>Policy</strong>)<br />
and forward this form to the Prescribing Support Technician as a record of the visit.<br />
2.17 Any discrepancies or any other concerns must be notified to the Head of<br />
Medicines Management and the PCT‘s Accountable Officer immediately.<br />
3 Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in GP individual stocks<br />
3.1 Delegated PCT Pharmacist should take their own CD Destruction Log and a<br />
CD Denaturing kit with them to the practice.<br />
3.2 Delegated PCT Pharmacist inspects CDs are stored in a secure way by the<br />
G.P.<br />
3.3 Delegated PCT Pharmacist makes an entry in the G.P. CD register giving the<br />
following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Drug, Formulation and Strength<br />
Batch Number and date of expiry<br />
Quantity to be destroyed<br />
Signature of the delegated PCT Pharmacist<br />
RPSGB number of the delegated Pharmacist<br />
3.4 GP must also sign the entry in his/her CD register.<br />
3.5 Prior to destruction check that any remaining in date stock balances with the<br />
running balance of stock.<br />
3.6 Amend running balance of stock<br />
3.7 Delegated PCT Pharmacist then makes an entry in their own CD Destruction<br />
Log Book giving the following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Drug, Formulation and Strength<br />
Quantity destroyed<br />
Signature of Pharmacist<br />
Printed name of Pharmacist<br />
3.8 GP must sign and print their name against the entry in the delegated PCT<br />
Pharmacist‘s CD Destruction Log Book.<br />
3.9 The delegated PCT Pharmacist then carries out the destruction of the CD in the<br />
presence of the GP.<br />
Page 179 of 196
3.10 The controlled drug must be destroyed as outlined in the RPSGB guidance for<br />
pharmacists on the Safe Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in England, Scotland and<br />
Wales.<br />
3.11 The process from 3.3 to 3.10 is repeated for each different strength and<br />
presentation of controlled drug that is out of date.<br />
3.12 The used CD Denaturing kit is then placed in the yellow Medicines Waste bin.<br />
3.13 The delegated PCT Pharmacist conducts a spot check on 2 other CD‘s running<br />
balances of stock. The delegated pharmacist makes an entry within the practice CD<br />
register on the relevant page of the stock check, noting any discrepancies or<br />
amendments to the running total<br />
E.g. 18/09/07 Stock check of Morphine Sulphate 10mg (Sevredol) tablets by PCT<br />
Pharmacist. K E Huddart MRPharm Reg. No. 91749. Stock check correct.<br />
3.14 The delegated PCT Pharmacist conducts a GP CD audit if the GP has not had<br />
a previous CD audit in that financial year.<br />
3.15 If a previous GP CD Audit has been completed then the delegated PCT<br />
Pharmacist must complete a CD Destruction Form (Appendix R within CD <strong>Policy</strong>) and<br />
forward this form to the Prescribing Support Technician as a record of the visit.<br />
3.16 Any discrepancies or any other concerns must be notified to the Head of<br />
Medicines Management and the PCT‘s Accountable Officer immediately.<br />
4 Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in a Community Pharmacy<br />
4.1 Delegated PCT Pharmacist should take their own CD Destruction Log and a CD<br />
Denaturing kit with them to the practice.<br />
4.2 Delegated PCT Pharmacist inspects CD cupboard to ensure that it is of the<br />
correct standard and mounted in a secure way<br />
4.3 Delegated PCT Pharmacist, along with community pharmacist ensures keys are<br />
stored in a secure way.<br />
4.4 Delegated PCT Pharmacist to ensure that any patient returned controlled drugs<br />
are separated and inform the community pharmacist that they need to be destroyed by<br />
the community pharmacist as soon as possible in line with RPSGB guidance for<br />
pharmacists on the safe destruction of <strong>Controlled</strong> drugs in England, Scotland and<br />
Wales.<br />
4.5 Delegated PCT Pharmacist to ensure that all out of date stock is clearly marked<br />
‗out of date‘ on packaging and has been segregated from other stock. The RPSGB<br />
inspector currently recommends out of date stock is placed in a clear bag,<br />
appropriately labelled, stating ‗out of date stock‘ and also the quantity enclosed within.<br />
4.6 Delegated PCT Pharmacist makes an entry in the community pharmacy CD<br />
register giving the following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Page 180 of 196
Drug, Formulation and Strength<br />
Batch Number and date of expiry<br />
Quantity to be destroyed<br />
Signature of the delegated PCT Pharmacist<br />
RPSGB number of the delegated Pharmacist<br />
E.g. 18/9/07 Morphine Sulphate 10mg (Sevredol) 24 tablets BN213AB Expired<br />
20/06/07. Destroyed by PCT Pharmacist K E Huddart MRPharm Reg No 91749<br />
4.7 The community pharmacist must also sign and add their RPSGB number to the<br />
entry in the CD register.<br />
4.8 Prior to destruction the delegated PCT pharmacist must check that any<br />
remaining in date stock balances with running balance of stock. Please Note that out of<br />
date CDs should be included in the running balance until they are destroyed.<br />
4.9 Delegated PCT Pharmacist then makes an entry in their own CD<br />
Destruction Log Book giving the following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Drug, Formulation and Strength<br />
Quantity destroyed<br />
Signature of Pharmacist<br />
Printed name of Pharmacist<br />
4.10 Community Pharmacist also signs and prints their name against the entry in the<br />
delegated PCT Pharmacist‘s CD Destruction Log Book.<br />
4.11 The delegated PCT Pharmacist then carries out the destruction of the CD in the<br />
presence of the community pharmacist.<br />
4.12 The controlled drug must be destroyed as outlined in the RPSGB guidance for<br />
pharmacists on the Safe Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in England, Scotland and<br />
Wales.<br />
4.13 The process from 4.6 to 4.12 is repeated for each different strength and<br />
presentation of controlled drug that is out of date.<br />
4.14 The used CD Denaturing kit should then be placed in the yellow Medicines<br />
Waste bin within the department.<br />
4.15 The delegated PCT Pharmacist conducts a spot check on 2 other CD‘s running<br />
balances of stock. The delegated pharmacist makes an entry within the practice CD<br />
register on the relevant page of the stock check, noting any discrepancies or<br />
amendments to the running total<br />
E.g. 18/09/07 Stock check of Morphine Sulphate 10mg (Sevredol) tablets by PCT<br />
Pharmacist. K E Huddart MRPharm Reg. No. 91749. Stock check correct.<br />
4.16 The delegated PCT Pharmacist completes a CD destruction form for community<br />
pharmacy (Appendix R within CD <strong>Policy</strong>) and forwards this to the Prescribing Support<br />
Technician as a record of the visit.<br />
4.17 Any discrepancies or any other concerns must be notified to the Head of<br />
Medicines Management and the PCT‘s Accountable Officer immediately.<br />
Page 181 of 196
4.18 The Head of Medicines Management will discuss any discrepancy or other<br />
concern with the relevant parties e.g. RPSGB Inspector.<br />
5 Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in the OOH‟s Centres<br />
5.1 All stock within UCC/OOH CD cupboard expiring within the week is highlighted<br />
to the UCC/OOH manager when a spot check is carried out.<br />
5.2 If the stock has not been used within that month, the UCC/OOH manager then<br />
contacts the delegated PCT Pharmacist and organises a date for destruction.<br />
5.3 Delegated PCT Pharmacist should take their own CD Destruction Log and a CD<br />
Denaturing kit with them to the practice.<br />
5.4 Delegated PCT Pharmacist inspects CD cupboard to ensure that it is of the<br />
correct standard and mounted in a secure way.<br />
5.5 Delegated PCT Pharmacist, along with ECP/<strong>Clinical</strong> Lead ensures keys are<br />
stored in a secure way.<br />
5.6 Delegated PCT Pharmacist makes an entry in the UCC/OOH Centre CD<br />
register giving the following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Drug, Formulation and Strength<br />
Batch Number and date of expiry<br />
Quantity to be destroyed<br />
Signature of the delegated PCT Pharmacist<br />
RPSGB number of the delegated Pharmacist<br />
E.g. 18/9/07 Morphine Sulphate 10mg (Sevredol) 24 tablets BN 213AB Expired<br />
20/06/07. Destroyed by PCT Pharmacist K E Huddart MRPharm Reg No 91749<br />
5.7 Emergency Care Practitioner/ <strong>Clinical</strong> Lead must also sign the entry in the CD<br />
register.<br />
5.8 Prior to destruction check that any remaining in date stock balances with the<br />
running balance of stock.<br />
5.9 Amend running balance of stock.<br />
5.10 Delegated PCT Pharmacist then makes an entry in their own CD Destruction<br />
Log Book giving the following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Drug, Formulation and Strength<br />
Quantity destroyed<br />
Signature of Pharmacist<br />
Printed name of Pharmacist<br />
5.11 ECP/<strong>Clinical</strong> Lead also signs and prints their name against the entry in the<br />
delegated PCT Pharmacist‘s CD Destruction Log Book.<br />
Page 182 of 196
5.12 The UCC/OOH Centre stock control book should be amended accordingly by<br />
the ECP /<strong>Clinical</strong> Lead witnessing the destruction and initialled by the delegated PCT<br />
Pharmacist.<br />
5.13 The delegated PCT Pharmacist then carries out the destruction of the CD in the<br />
presence of the ECP or <strong>Clinical</strong> Lead.<br />
5.14 The controlled drug must be destroyed as outlined in the RPSGB guidance for<br />
pharmacists on the Safe Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in England, Scotland and<br />
Wales.<br />
5.15 The process from 5.6 to 5.14 is repeated for each different strength and<br />
presentation of controlled drug that is out of date.<br />
5.16 The used CD Denaturing kit is then placed in the yellow medicines waste bin at<br />
the UCC. Please Note: If the UCC/OOH centre does not have a medicines waste bin<br />
for out of date medicines then take the used CD Denaturing kit to the nearest available<br />
GP practice or community pharmacy and place in their yellow medicines waste bin.<br />
5.17 The delegated PCT Pharmacist conducts a spot check on 2 other CD‘s running<br />
balances of stock. The delegated pharmacist makes an entry within the practice CD<br />
register on the relevant page of the stock check, noting any discrepancies or<br />
amendments to the running total<br />
E.g. 18/09/07 Stock check of Morphine Sulphate 10mg (Sevredol) tablets by PCT<br />
Pharmacist. K E Huddart MRPharm Reg. No. 91749. Stock check correct.<br />
5.18 The delegated PCT Pharmacist should conduct an UCC/OOH centre CD audit<br />
(Appendix K within CD <strong>Policy</strong>) if the UCC/OOH centre has not had a previous audit<br />
conducted in that financial year.<br />
5.19 If a previous CD UCC/OOH centre audit has been completed then the<br />
delegated PCT Pharmacist must complete a CD destruction form (Appendix R within<br />
CD <strong>Policy</strong>) and forward it to the Prescribing Support Technician as a record of the visit.<br />
5.20 Any discrepancies or any other concerns must be notified to the Head of<br />
Medicines Management and the PCT‘s Accountable Officer immediately.<br />
5.21<br />
6 Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in Prisons.<br />
6.1 Delegated PCT Pharmacist should take their own CD Destruction Log and a CD<br />
Denaturing kit with them to the prison.<br />
6.2 Delegated PCT Pharmacist inspects CD cupboard to ensure that it is of the<br />
correct standard and mounted in a secure way.<br />
6.3 Delegated PCT Pharmacist, along with Prison Pharmacist ensures keys are<br />
stored in a secure way.<br />
6.4 Delegated PCT Pharmacist to ensure that any patient returned controlled drugs<br />
are separated and inform the prison pharmacist that they need to be destroyed by the<br />
community pharmacist as soon as possible in line with RPSGB guidance for<br />
Page 183 of 196
pharmacists on the safe destruction of <strong>Controlled</strong> drugs in England, Scotland and<br />
Wales.<br />
6.5 Delegated PCT Pharmacist to ensure that all out of date stock is clearly marked<br />
‗out of date‘ on packaging and has been segregated from other stock. The RPSGB<br />
inspector currently recommends out of date stock is placed in a clear bag,<br />
appropriately labelled, stating ‗out of date stock‘ and also the quantity enclosed within.<br />
6.6 Delegated PCT Pharmacist makes an entry in the prison pharmacy CD register<br />
giving the following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Drug, Formulation and Strength<br />
Batch Number and date of expiry<br />
Quantity to be destroyed<br />
Signature of the delegated PCT Pharmacist<br />
RPSGB number of the delegated Pharmacist<br />
E.g. 18/9/07 Morphine Sulphate 10mg (Sevredol) 24 tablets BN 213AB Expired<br />
20/06/07. Destroyed by PCT Pharmacist K E Huddart MRPharm Reg No 91749<br />
6.7 The prison pharmacist must also sign and add their RPSGB number to the entry<br />
in the CD register.<br />
6.8 Prior to destruction the delegated PCT pharmacist must check that any<br />
remaining in date stock balances with running balance of stock. Please Note that out of<br />
date CDs should be included in the running balance until they are destroyed.<br />
6.9 Delegated PCT Pharmacist then makes an entry in their own CD Destruction Log<br />
Book giving the following details of the <strong>Controlled</strong> Drug destruction:-<br />
Date<br />
Drug, Formulation and Strength<br />
Quantity destroyed<br />
Signature of Pharmacist<br />
Printed name of Pharmacist<br />
6.10 Prison Pharmacist also signs and prints their name against the entry in the<br />
delegated PCT Pharmacist‘s CD Destruction Log Book.<br />
6.11 The delegated PCT Pharmacist then carries out the destruction of the CD in the<br />
presence of the Prison Pharmacist.<br />
6.12 The controlled drug must be destroyed as outlined in the RPSGB guidance for<br />
pharmacists on the Safe Destruction of <strong>Controlled</strong> <strong>Drugs</strong> in England, Scotland and<br />
Wales.<br />
6.13 The process from 6.6 to 6.12 is repeated for each different strength and<br />
presentation of controlled drug that is out of date.<br />
6.14 The used CD Denaturing kit should then be placed in the yellow medicines<br />
waste bin within the department.<br />
6.15 The delegated PCT Pharmacist conducts a spot check on 2 other CD‘s running<br />
balances of stock. The delegated pharmacist makes an entry within the prison<br />
Page 184 of 196
pharmacy CD register on the relevant page of the stock check, noting any<br />
discrepancies or amendments to the running total<br />
E.g. 18/09/07 Stock check of Morphine Sulphate 10mg (Sevredol) tablets by PCT<br />
Pharmacist. K E Huddart MRPharm Reg. No. 91749. Stock check correct.<br />
6.16 The delegated PCT Pharmacist should conduct a CD Prison Audit (Appendix M<br />
within CD policy), if the prison has not had a previous audit conducted in that financial<br />
year.<br />
6.17 If a previous CD Prison Pharmacy Audit has been completed then the delegated<br />
PCT Pharmacist must complete a CD Destruction Form (Appendix R within CD <strong>Policy</strong>)<br />
and forward this form to the Prescribing Support Technician as a record of the visit.<br />
6.18 Any discrepancies or any other concerns must be notified to the Head of<br />
Medicines Management and the PCT‘s Accountable Officer immediately.<br />
6.19 The Head of Medicines Management will discuss any discrepancy or other<br />
concern with the relevant parties e.g. RPSGB Inspector.<br />
Page 185 of 196
Appendix R <strong>Controlled</strong> Drug Destruction Record<br />
Location (please circle) Name and Address of location<br />
General Practice<br />
Community Pharmacy<br />
Community Hospital<br />
Other – please give detail<br />
Details of <strong>Controlled</strong> drugs destroyed<br />
Drug name /strength / formulation Quantity Reason for destruction<br />
Comments/advice given<br />
Authorised witness<br />
(name and designation)<br />
Second witness<br />
(name and designation)<br />
Date<br />
Page 186 of 196
Appendix S – SUMMARY OF CONTROLLED DRUGS GUIDANCE FOR GPs<br />
1.0 INTRODUCTION<br />
1.1 Medicines Legislation governs the purchase, prescribing, storage, record<br />
keeping, monitoring and destruction of <strong>Controlled</strong> <strong>Drugs</strong>.<br />
1.2 The PCT Accountable Officer and the Police have the right of entry into<br />
premises for the purpose of <strong>Controlled</strong> <strong>Drugs</strong> Monitoring and Inspection. This<br />
authority can be delegated to suitably trained personnel such as the PCT<br />
Commissioning Pharmaceutical Advisers.<br />
1.3 Refer to the PCT <strong>Controlled</strong> Drug <strong>Policy</strong> for more detailed guidance and be<br />
aware that legislation around CDs is subject to change.<br />
2.0 GOVERNANCE, INSPECTION AND MONITORING<br />
2.1 All practices and GPs are required to complete an annual declaration stating<br />
whether or not they keep a stock of CDs.<br />
2.2 Practices and GPs holding stock will be required to complete a self assessment<br />
of their management of CDs<br />
2.3 PCT will arrange for a small number of routine inspections from a random<br />
sample of GPs, annually.<br />
2.4 <strong>Controlled</strong> drug prescribing and purchases are monitored by the PCT via ePACT<br />
and GPs may periodically be requested to review their prescribing.<br />
3.0 STANDARD OPERATING PROCEDURES (SOPs) Appendix T of CD <strong>Policy</strong><br />
3.1 These should ensure there is a full audit trail for movement of CDs from<br />
acquisition to administration and disposal and record keeping.<br />
3.2 SOPs should also include how to deal with discrepancies in CD stock and<br />
register; how and to whom staff can raise any concerns relating to CDs.<br />
4.0 PURCHASING CONTROLLED DRUGS<br />
4.1 A requisition form FP10CDF should be completed to purchase Schedule 2 & 3<br />
CDs<br />
4.2 FP10CDF forms are available from the service that provides prescription forms.<br />
4.3 FP10CDF forms are controlled stationary and should be stored securely with<br />
restricted access.<br />
4.4 GPs must not use FP10 prescriptions to top up their personal or practice stock<br />
CDs.<br />
4.5 A system should be put in place for completing the FP10CDF forms as these are<br />
monitored to individual GPs via ePACT.<br />
4.6 The pharmacy will record the name of the person collecting the CDs in their<br />
registers.<br />
4.7 If a member of staff is sent to collect the CD they must carry a bearer‘s note,<br />
signed and dated by the prescriber, stating they are authorised to carry the CD;<br />
the pharmacy may retain the note.<br />
5.0 STORAGE IN THE PRACTICE<br />
5.1 CDs requiring safe custody must be stored in a designated locked CD cabinet or<br />
safe.<br />
5.2 The cabinet should be metal and fixed to the wall or floor with rag bolts and<br />
within a lockable room with restricted access.<br />
5.3 Ideally no other items should be stored in the CD cupboard/ safe; if this isn‘t<br />
possible the CDs should be segregated from other items stored in the<br />
cabinet/safe.<br />
5.4 A designated person should be responsible for the safe custody of the keys and<br />
records of who has access to keys or security code numbers. It is recommended<br />
Page 187 of 196
that key codes are changed regularly to maintain security.<br />
5.5 A designated person should be responsible for accepting stock into the practice,<br />
transfer of stock to individual GPs and maintaining the stock CD register.<br />
6.0 STORAGE IN GP HOME VISIT BAGS<br />
6.1 Bags should be lockable and kept locked at all times except when in use.<br />
6.2 <strong>Controlled</strong> drugs should not be left unattended in a car for prolonged periods of<br />
time.<br />
6.3 When on annual leave the Dr should consider handing over their controlled<br />
drugs to the practice for safekeeping.<br />
6.4 <strong>Controlled</strong> drug stock should be kept to a minimum and only one strength kept to<br />
reduce the likelihood of an error.<br />
6.5 Each ‗bag‘ must have its own designated CD register, which should ideally be<br />
kept separate from the bag, in case the bag is lost or stolen.<br />
6.6 Each GP is personally responsible for making entries into their bag register.<br />
6.7 Supplies into a doctor‘s bag should be witnessed; this is considered essential if<br />
top up is made from the practice central store.<br />
6.8 SHARED BAGS: A full audit of the date and time of bags being handed to and<br />
from each person should be made in a hard bound book. The stock balance and<br />
CD register should be checked at each handover. The bag should be locked in a<br />
cupboard with restricted access when not in use. A record should be made of<br />
who has access to the bag and who is responsible for handing over and<br />
receiving the bag.<br />
7.0 STOCK CHECKS<br />
Designated person(s) should be responsible for checking the CD stock and<br />
expiry dates on at least a monthly basis and a record made that this has been<br />
done.<br />
8.0 CONTROLLED DRUG REGISTERS<br />
8.1 The registers must be bound or computerised.<br />
8.2 Entries in hard copy must be made in ink and in chronological order;<br />
computerised records must be fully attributable and auditable.<br />
8.3 A separate page is required for each controlled drug and presentation and<br />
strength.<br />
8.4 A running balance should be maintained.<br />
8.5 All receipts and issues should be made within 24 hours of transaction<br />
8.6 There should be no gaps between each line in the register<br />
8.7 If an error is made then do not obliterate. Bracket entry in a manner that details<br />
can still be seen, mark ‗error‘ and next to or in margin write the correct details<br />
8.8 <strong>Drugs</strong> received; All register entries must show: -<br />
Date received<br />
Name and address of person or firm from whom they are received<br />
Name and signature of person making the CD entry.<br />
The amount received<br />
Form and strength in which supplied<br />
Running balance<br />
8.9 <strong>Drugs</strong> administered/ supplied<br />
Date and time administration/ supply made<br />
Name and address of person for whom it was administered/supplied.<br />
Name and authority of person who supplied/administered the item.<br />
Amount administered/supplied<br />
Running balance.<br />
Page 188 of 196
Reimbursement should be made via a personally administered claim via FP10<br />
for the practice.<br />
9.0 OUT OF DATE STOCK or STOCK NO LONGER REQUIRED<br />
9.1 The PCT Commissioning Medicines Management Team should be contacted to<br />
make arrangements for disposal of stock CDs as this can only be performed by<br />
an authorised person.<br />
9.2 If the practice hold a central stock out of date CDs can be returned to the central<br />
store; a record of this should be made in the CD registers.<br />
9.3 If the practice does not hold central stock the destruction should take place<br />
directly from the doctor‘s bag.<br />
9.4 Out of date stock should be clearly marked and segregated from in date stock.<br />
10.0 PATIENTS OWN CONTROLLED DRUGS<br />
10.1 Medicines dispensed for one patient must not be used to treat another patient.<br />
10.2 Patients should be encouraged to return their unwanted CDs to a pharmacy for<br />
destruction.<br />
10.3 Nursing and practice staff should not accept patients controlled drugs for<br />
destruction except in exceptional circumstances.<br />
10.4 If handed to a GP they cannot in theory be passed on to a pharmacy for<br />
destruction.<br />
10.5 The CDs should be recorded in a book specifically kept for this purpose.<br />
10.6 Strict environment legislation covers the handling of all waste in the UK;<br />
medicines should never be disposed of in household waste, sinks or flushing<br />
down toilets.<br />
10.7 CDs should be denatured before destruction. ‗DOOP‘ kits specifically designed<br />
for this purpose are available from the waste company or the PCT; the DOOP kit<br />
should be disposed of in the pharmaceutical waste bins.<br />
10.7 Destruction should be witnessed.<br />
10.8 ONLY in exceptional circumstances, district/community nursing staff can<br />
destroy, with consent, patients controlled drugs and a record must be made and<br />
witnessed if possible.<br />
10.9 If a GP administers a patients own CDs during a home visit a record of this must<br />
be made on the patient held nursing records or administration chart if available<br />
and the practice computerised medical records. This should include drug, dose,<br />
form, date and time of administration and if applicable running balance.<br />
11.0 PRESCRIPTIONS<br />
11.1 It is a criminal offence for a pharmacist to dispense a controlled drug against a<br />
prescription which does not fully comply with legislation.<br />
11.2 Prescriptions for CDs should be limited to 30 days supply.<br />
11.3 Instalment prescriptions for drug addiction must be limited to a maximum of 14<br />
days supply.<br />
11.3 If more than 30 days supply is considered clinically appropriate a note should be<br />
made in the patient‘s records stating the reason why.<br />
11.4 Prescriptions for CDs are valid for 28 days; a later start date can be added; for<br />
instalment prescriptions, the first instalment must be made within 28 days of the<br />
start date.<br />
11.5 A Home Office licence is required to prescribe diamorphine, dipipanone and<br />
cocaine to substance misusers; GPs can prescribe these drugs for the relief of<br />
pain due to organic disease or injury without a licence.<br />
11.6 Other than in emergencies practitioners should not prescribe for themselves or<br />
anyone they have a close personal relationship with including friends, family and<br />
colleagues.<br />
Page 189 of 196
12.0 PRIVATE PRESCRIPTIONS<br />
12.1 A unique private prescriber code is required for a practitioner wishing to issue<br />
private prescriptions.<br />
12.2 Requests for a private prescriber code should be made to the PCT.<br />
12.3 Private prescriptions must be written on designated private prescription forms<br />
FP10 (PDC) NC.<br />
12.4 FP10(PDC) NC private prescriptions are available from the PCT.<br />
13.0 PATIENTS TRAVELLING OVERSEAS<br />
13.1 Persons travelling for over three months either abroad or to the UK will need a<br />
personal export/import licence.<br />
13.2 If travelling for 3 months or less a Home Office licence is not required.<br />
13.3 A personal licence has no authority outside the UK; it allows unhindered<br />
passage through UK customs.<br />
13.4 Personal licence application forms can be downloaded from the Home Office<br />
web site.<br />
13.5 Applications should be made at least 10 days prior to travel.<br />
13.6 Licences are normally issued with an expiry date of one week after the expected<br />
return to the UK.<br />
13.7 It is good practice for CDs to be carried in their original container in hand<br />
luggage with a letter from the prescribing doctor confirming the carriers name,<br />
destination, drug details and amount.<br />
13.8 If a person is staying outside their resident country for a period exceeding 3<br />
months they should be advised to register with a doctor in the country they are<br />
visiting for the purpose of receiving further prescriptions.<br />
13.9 Other countries have their own import regulations for controlled drugs; travellers<br />
should check this with UK based representative of country they are travelling to.<br />
Issued by PCT Commissioning Medicines Management Team September 2008. Valid until 2010 or<br />
sooner if newlegislation. To be read in conjunction with full PCT <strong>Controlled</strong> Drug <strong>Policy</strong>.<br />
Page 190 of 196
APPENDIX T – GUIDANCE ON STANDARD OPERATING POLICY<br />
This is intended as a guide for areas to consider when completing an SOP. Not all<br />
areas but most will apply to each setting and more details may need to be added; refer<br />
to full policy.<br />
Designated person with overall<br />
responsibility for controlled drugs<br />
List of personnel allowed to prescribe<br />
controlled drugs<br />
List of personnel allowed to<br />
supply/administer controlled drugs via<br />
PGD<br />
List of personnel allowed access to<br />
controlled drug cabinet/safe/Drs bag<br />
Prescriptions for controlled drugs<br />
generated by (hand/computer/both)<br />
A maximum of 30 days supply will be<br />
prescribed.<br />
Who is allowed to generate<br />
prescriptions for CDs via computer<br />
Prescription for controlled drugs<br />
awaiting doctor‘s signature are placed<br />
separately – where.<br />
Details of where records are made for<br />
CD prescriptions awaiting collection<br />
Where are CD prescriptions awaiting<br />
collection stored?<br />
Details of where records are made of<br />
person collecting the CD prescription<br />
Procedure for missing CD<br />
prescriptions<br />
Name and Address of where CDs are<br />
ordered from<br />
Persons authorised to order<br />
controlled drugs<br />
Requisition forms used<br />
Requisition forms are stored securely,<br />
where<br />
How is the requisition form sent to the<br />
supplier<br />
How are the CDs transferred from<br />
supplier to the premises and by whom<br />
The level of stock required is<br />
If more than 30 days supply of a CD<br />
is required on a prescription the<br />
prescribing doctor will make a note in<br />
the patient‘s clinical records.<br />
Page 191 of 196
eviewed annually by<br />
Who is authorised to receive<br />
controlled drugs onto the premises<br />
Where are the CDs placed when they<br />
arrive at premises<br />
The CDs received into the premises<br />
are recorded in the controlled drug<br />
register immediately on receipt by?<br />
A running balance is maintained and<br />
the stock checked on receipt.<br />
The record of order and invoices<br />
stored for 7 years, where?<br />
Supply<br />
Statement if CDs are supplied or not<br />
Who is allowed to supply CDs<br />
Including supply from central store to<br />
doctors bags<br />
What is the procedure for supplying<br />
CDs<br />
Administration<br />
Are patients own CDs administered<br />
Are stock CDs administered to<br />
patients<br />
Records of administration include<br />
patients name, address, Drug, dose,<br />
route and time of administration.<br />
This record is made where<br />
CD register<br />
Patients clinical records<br />
If patient has medicines chart/nursing<br />
record or similar a record is also<br />
made there.<br />
The administration of CDs is<br />
witnessed by.<br />
If administration is not witnessed<br />
state circumstances where this is<br />
allowed.<br />
Storage<br />
Where are controlled drugs stored<br />
List all places including each<br />
individual doctors bag<br />
Is a Home Office Licence required<br />
Are there keys? What is procedure for<br />
access and storing keys?<br />
Who is allowed access to keys/ codes<br />
and how is this regulated?<br />
Doctors/Home visit bag (lockable<br />
how?)<br />
Points to consider<br />
Page 192 of 196
Where is the bag stored<br />
Whilst in practice<br />
When on a home visit<br />
When car unattended<br />
Overnight<br />
When on holiday<br />
Transport<br />
Who is allowed to transport CDs<br />
Under what circumstances<br />
What records are made<br />
Stock Checks<br />
List of CDs allowed to be stocked in<br />
each area<br />
The stock balance is checked by<br />
This check is performed (state<br />
intervals)<br />
A record of the check is made (in the<br />
CD register/on computer)<br />
Destruction - Stock<br />
Out of date/obsolete and CDs no<br />
longer required are segregated by<br />
placing in a bag (preferably clear<br />
plastic) clearly labelled out of date<br />
stock not for use.<br />
Where CDs awaiting destruction are<br />
stored)<br />
Out of date CDs should remain in<br />
running balance in register until time<br />
of destruction.<br />
Contact authorised person list names<br />
and contact email/phone number.<br />
Who is responsible for overseeing<br />
this<br />
Destruction Patients Own<br />
Patients own medicines are not<br />
reused for the treatment of any other<br />
patient<br />
Do you advise Patients to return CDs<br />
to community pharmacy for<br />
destruction<br />
Under what circumstances do you<br />
receive or are responsible for<br />
destruction of patients own CDs<br />
CD denaturing kits must be used<br />
Enter details of how this is done<br />
Where to obtain kits and where to<br />
dispose of<br />
Records must be kept, how is this<br />
done and where<br />
Page 193 of 196
Patients Own CDs - residential<br />
Is the patient self medicating<br />
Is there a policy/procedure for<br />
patients who self medicate?<br />
All above may apply & help complete<br />
SOP<br />
Record Keeping, including CD<br />
registers<br />
Where will records be stored<br />
Should be kept for minimum of 7<br />
years or longer if other <strong>NHS</strong> record<br />
keeping policies apply<br />
Dealing with discrepancies and<br />
concerns<br />
How are discrepancies in the running<br />
balance dealt with<br />
If stock/patients own CDs are missing<br />
who should this be reported to<br />
Give details of incident reporting<br />
system<br />
Give details of who else staff may<br />
contact if they have concerns<br />
How will staff reporting concerns be<br />
protected<br />
How would you deal with member of<br />
staff about whom concerns have<br />
been raised? May refer to other<br />
policies about fitness to practice,<br />
regulatory authority and codes of<br />
conduct etc<br />
National Patient Safety Alerts<br />
Different strengths of injectable<br />
opiates should be stored separately.<br />
High dose injectable opiates i.e.<br />
diamorphine 30mg and over should<br />
be clearly marked and stored<br />
separately from lower strengths. How<br />
is this achieved in organisation?<br />
Naloxone should be kept in each<br />
clinical area including Drs bags where<br />
injectable opiates are stored/<br />
administered.<br />
How is this done in the organisation?<br />
There should be clear SOPs for<br />
administration of injections including<br />
how to prepare an injection i.e.<br />
reconstitute<br />
Page 194 of 196
Staff should be made aware of any SOPs applicable in the organisation and a record<br />
made that they have read and understood them including the consequences of not<br />
complying with the SOP.<br />
SOPs should be reviewed on a regular basis to ensure they are practical and reflect<br />
current practice and legislation. If training or competency is required in order to<br />
implement an SOP a record should be made of when, how, what and to whom this was<br />
completed.<br />
Page 195 of 196