Assessment of Balance and Gait in the Older Adult at ... - UCSF Fresno
Assessment of Balance and Gait in the Older Adult at ... - UCSF Fresno
Assessment of Balance and Gait in the Older Adult at ... - UCSF Fresno
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
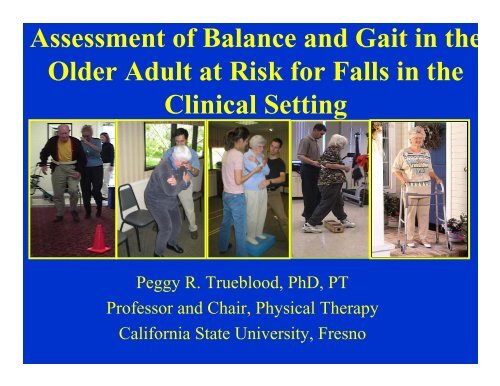
<strong>Assessment</strong> <strong>of</strong> <strong>Balance</strong> <strong>and</strong> <strong>Gait</strong> <strong>in</strong> <strong>the</strong><strong>Older</strong> <strong>Adult</strong> <strong>at</strong> Risk for Falls <strong>in</strong> <strong>the</strong>Cl<strong>in</strong>ical Sett<strong>in</strong>gPeggy R. Trueblood, PhD, PTPr<strong>of</strong>essor <strong>and</strong> Chair, Physical TherapyCalifornia St<strong>at</strong>e University, <strong>Fresno</strong>
Objectives• Describe key fall risk factors <strong>in</strong> <strong>the</strong> older adultacross various sett<strong>in</strong>gs.• Identify <strong>the</strong> effect <strong>of</strong> ag<strong>in</strong>g on balance <strong>and</strong> gait• Identify <strong>the</strong> multiple systems th<strong>at</strong> contribute to <strong>the</strong>normal postural control system as a framework toidentify impairments.
•Use evidence-based tools to assess fall risk<strong>in</strong> <strong>the</strong> area <strong>of</strong> gait <strong>and</strong> balance; cognition;depression; home <strong>and</strong> environmentalbarriers <strong>and</strong> fear <strong>of</strong> fall<strong>in</strong>g with <strong>at</strong>tention tocultural vari<strong>at</strong>ions <strong>and</strong> type <strong>of</strong> sett<strong>in</strong>g.• Assess for <strong>and</strong> underst<strong>and</strong> <strong>the</strong> variedassistive devices/technology <strong>and</strong> protectivewear available.
Just <strong>the</strong> Facts• California currently has <strong>the</strong> largestolder adult popul<strong>at</strong>ion <strong>of</strong> any st<strong>at</strong>e <strong>in</strong><strong>the</strong> USA.• <strong>Older</strong> adults are <strong>the</strong> fastest grow<strong>in</strong>gsegment <strong>of</strong> <strong>the</strong> popul<strong>at</strong>ion (20% <strong>of</strong>popul<strong>at</strong>ion by 2020)• Although <strong>the</strong> 60+ age group represents10% <strong>of</strong> <strong>the</strong> popul<strong>at</strong>ion, <strong>the</strong>y accountfor over 40% <strong>of</strong> <strong>the</strong> hospitaliz<strong>at</strong>ionsdue to <strong>in</strong>juries.
<strong>Balance</strong> Disorders <strong>and</strong> Fallsare serious problems fac<strong>in</strong>g<strong>the</strong> older adult• 1 <strong>in</strong> 3 persons > 65 years <strong>of</strong> age will fall (1 <strong>in</strong> 2persons > 80 years <strong>of</strong> age)• Higher <strong>in</strong>cidence <strong>in</strong> <strong>in</strong>stitutions vs communitydwell<strong>in</strong>g(50% <strong>of</strong> residents <strong>of</strong> LTC facilitiesexperience falls)• 60% among those with history <strong>of</strong> falls
Falls present a serious health risk eventhose th<strong>at</strong> do not cause <strong>in</strong>juryPsychological TraumaFear <strong>of</strong> Fall<strong>in</strong>gLoss <strong>of</strong> Self-ConfidenceInactivityFunctional Decl<strong>in</strong>eDecreased Quality <strong>of</strong> Life
Can Measure Fear <strong>of</strong> Fall<strong>in</strong>g throughSt<strong>and</strong>ardized Self-Report Tests– ABC (Activities-specific <strong>Balance</strong>Confidence Scale) (Powell <strong>and</strong> Myers,1995)– BES (<strong>Balance</strong> Efficacy Scale) (Rose DJ,2003, 2010)– FES (Falls Efficacy Scale) (T<strong>in</strong>etti et al1990)
Causes <strong>of</strong> Falls are Multi-factorialINTRINSICPeripheralSensory LossSlowed CentralProcess<strong>in</strong>gMuscleWeaknessCognitiveImpairment<strong>Balance</strong> <strong>and</strong> <strong>Gait</strong>ImpairmentsEnvironmentalHazardsChange <strong>in</strong>Medic<strong>at</strong>ionsSocialSett<strong>in</strong>gExternaldem<strong>and</strong>s (busyenvironments)EXTRINSIC
Most Common Risk FactorsRisk FactorSig/TotalMeanRR-ORRangeMuscle weakness 10/11 4.4 1.5 – 10.3History <strong>of</strong> Falls 12/13 3.0 1.7 – 7.0<strong>Gait</strong> deficit 10/12 2.9 1.3 – 5.6<strong>Balance</strong> deficit 8/11 2.9 1.3 –5.6Assistive Device Use 8/8 2.6 1.2 – 4.6Visual deficit 6/12 2.5 1.6 – 3.5Arthritis 3/7 2.4 1.9 – 2.9Impaired ADL 8/9 2.3 1.5 – 3.1Depression 3/6 2.2 1.7 – 2.5Cognitive Deficit 4/11 1.8 1.0 – 2.3Age > 80 yrs 5/8 1.7 1.1 – 2.5American Geri<strong>at</strong>ric Society Guidel<strong>in</strong>esAGS Guidel<strong>in</strong>es, 2001
Risk Factor C<strong>at</strong>egoriesINTRINSIC (<strong>in</strong>ternal) (55%)–Medical conditions–<strong>Gait</strong> <strong>and</strong> <strong>Balance</strong> deficits–Damage to Sensory Systems–Musculoskeletal Problems(weakness)–Cognitive impairments
• EXTRINSIC (Environmental)HAZARDS (45%)–Visual <strong>and</strong> Surfaceconditions–Social sett<strong>in</strong>g–Medic<strong>at</strong>ions–Activity level–External dem<strong>and</strong>s(Busy Environments)
Most falls (85%) occur <strong>in</strong> <strong>the</strong>home dur<strong>in</strong>g normal activities <strong>of</strong>daily liv<strong>in</strong>g
Multiple Risk Factors <strong>and</strong> Fall Risk• Percentage <strong>of</strong> recurrent falls <strong>in</strong>creasesfrom 10-69% as # risk factors <strong>in</strong>creasesfrom 1-4(Nevitt et al, 1989)• Risk <strong>of</strong> fall<strong>in</strong>g ranged from 12% (no riskfactor) to 100% ( 3 risk factors): Hipweakness, unstable balance, gre<strong>at</strong>er than 4meds(Robb<strong>in</strong>s et al, 1989)
The gre<strong>at</strong>er <strong>the</strong> number<strong>of</strong> risk factors present,<strong>the</strong> gre<strong>at</strong>er <strong>the</strong>likelihood<strong>of</strong> falls
The Four C’sFall Prevention must be:• Consistent• Cross Discipl<strong>in</strong>es• Coord<strong>in</strong><strong>at</strong>ed• Culture
Cl<strong>in</strong>ical Algorithm•System<strong>at</strong>ic process <strong>of</strong>decision-mak<strong>in</strong>g•Guides <strong>in</strong>tervention•Management <strong>of</strong> olderpersons <strong>in</strong> cl<strong>in</strong>icalsett<strong>in</strong>g or emergencyroom•Person presents witha recurrent fall or hasdifficultywalk<strong>in</strong>g/balance
The First Step: Identify<strong>in</strong>g <strong>and</strong>Assess<strong>in</strong>g Risk• Intensity <strong>of</strong> <strong>in</strong>itial assessment varies by targetpopul<strong>at</strong>iont (AGS Guidel<strong>in</strong>es, 2001)• High risk groups require more comprehensive<strong>and</strong> detailed assessments:• Circumstances <strong>of</strong> fall• Identific<strong>at</strong>ion <strong>of</strong> risk factors for falls• Medical co-morbidity• Functional st<strong>at</strong>us• Environmental risk assessment
Risk Factors Vary by Sett<strong>in</strong>gsCommunity Sett<strong>in</strong>gsPrevious fall caus<strong>in</strong>g fractureCaucasianImpaired cognitive functionImpaired balancePsychotropic drug useHospital Sett<strong>in</strong>gsAcute illnessExtended bed restDecreased mobilityDeliriumAcute illnessUnfamiliar surround<strong>in</strong>gsPsychotropic medic<strong>at</strong>ionsNurs<strong>in</strong>g Home Sett<strong>in</strong>gsLower body weaknessPoor vision & hear<strong>in</strong>gDisorient<strong>at</strong>ionNumber <strong>of</strong> fallsImpaired balanceDizz<strong>in</strong>essLow body massBe<strong>in</strong>g femaleUse <strong>of</strong> mechanicalrestra<strong>in</strong>ts
Community Sett<strong>in</strong>gs• Medic<strong>at</strong>ions*(antihypertensives, anti-diabeticagents <strong>and</strong> sed<strong>at</strong>ives most <strong>of</strong>tencited)• Physical Disabilities• Poor Vision• Cognitive Impairment• Healthy older adults mayoverestim<strong>at</strong>e physical abilities<strong>and</strong> fall due to risk-tak<strong>in</strong>gbehaviors•Lee et al (2006) noted medical illnesses more important than medic<strong>at</strong>ions as risk factors <strong>of</strong> falls<strong>in</strong> older community dwellers).
Falls Significantly ImpactAcute Care Hospitals• Among older adults, falls are <strong>the</strong> lead<strong>in</strong>g cause <strong>of</strong><strong>in</strong>jury de<strong>at</strong>hs <strong>and</strong> <strong>the</strong> most common cause <strong>of</strong>hospital admissions due to <strong>in</strong>jury.• In <strong>Fresno</strong> county 75% <strong>of</strong> hospitalizedun<strong>in</strong>tentional <strong>in</strong>juries were due to falls <strong>in</strong> peopleover 60 years <strong>of</strong> age•Every 18 seconds an older adult is<strong>in</strong> <strong>the</strong> emergency room because <strong>of</strong>a fall
Injury Rel<strong>at</strong>ed Hospitaliz<strong>at</strong>ions by Age <strong>in</strong><strong>Fresno</strong> County 2006Age Groups
Acute Care Risk <strong>Assessment</strong>sHendrich Fall Risk <strong>Assessment</strong>Risk Factor Scale ScoreHistory <strong>of</strong> YES 7FallsNO 0Incont<strong>in</strong>ence YES 3NO 0Confusion YES 3Disorient<strong>at</strong>ion NO 0Depression YES 4NO 0Dizz<strong>in</strong>ess YES 3Vertigo NO 0Poor Mobility YES 2Weakness NO 0Poor YES 3Judgment NO 0Morse Fall Risk <strong>Assessment</strong>Risk Factor Scale ScoreHistory <strong>of</strong> YES 25FallsNO 0Secondary YES 15DiagnosisNO 0Ambul<strong>at</strong>ory Furniture 30Aid Cane/Walker 15None 0IV/Hepar<strong>in</strong> YES 20Lock NO 0<strong>Gait</strong>/ Impaired 20Transfers Weak 10Normal 0Mental Impaired 15St<strong>at</strong>us Normal 0
Acute Care Risk <strong>Assessment</strong>sHendrich <strong>Assessment</strong>Morse <strong>Assessment</strong>• Only two c<strong>at</strong>egories:high <strong>and</strong> low risk(most put <strong>in</strong>to highrisk)• Can use <strong>in</strong> LTC• Interventions based onspecific areas <strong>of</strong> risk• Less research asMorse• High Risk > 45• Moder<strong>at</strong>e Risk 25-44• Low Risk 0-24 driven• Interventionsst<strong>and</strong>ardized by level<strong>of</strong> risk• Not designed for longtermcare sett<strong>in</strong>g
Nurs<strong>in</strong>g Home Residents morevulnerable due to..• Increased frailty• More co-morbidities• Cognitive deficits• Inactivity• Medical Side Effects• Caregiver/p<strong>at</strong>ient r<strong>at</strong>ios are poor• Lack <strong>of</strong> skilled pr<strong>of</strong>essionals(Special Report, Office <strong>of</strong> Prov<strong>in</strong>cial Health Officer, 2004)
Pros <strong>and</strong> Cons <strong>of</strong> Assistive DevicesAdvantages• Provide biomechanicstabiliz<strong>at</strong>ion via<strong>in</strong>creas<strong>in</strong>g BOS• Aids <strong>in</strong> recovery <strong>of</strong>equilibrium when<strong>in</strong>stability occurs• Provides tactilesom<strong>at</strong>osensory<strong>in</strong>form<strong>at</strong>ion from <strong>the</strong>h<strong>and</strong> which contributesto postural stability viasp<strong>at</strong>ial orient<strong>at</strong>ionDisadvantages• Increases <strong>at</strong>tentional <strong>and</strong>neuromotor dem<strong>and</strong>s• Potential destabiliz<strong>in</strong>geffect (eg when moves oradvances device)• Interfere with limbmovement dur<strong>in</strong>g balancerecovery• UE jo<strong>in</strong>t forces may behigh• Metabolic <strong>and</strong> physiologicdem<strong>and</strong> may be high
Outp<strong>at</strong>ient Risk <strong>Assessment</strong>s• Initial Screen<strong>in</strong>g:–TUG–T<strong>in</strong>etti <strong>Gait</strong> <strong>and</strong> <strong>Balance</strong> Scale• If <strong>at</strong> risk refer to physical oroccup<strong>at</strong>ional <strong>the</strong>rapy for more <strong>in</strong>-depthbalance assessment
Measure <strong>of</strong> Fall RiskTimed Up <strong>and</strong> Go (TUG)>13.5 secs high risk for fallsTime ittakes tost<strong>and</strong>up, walk10 feet (3meters)<strong>and</strong>return to<strong>the</strong> chair<strong>and</strong> sitdown.for falls
T<strong>in</strong>etti <strong>Balance</strong> <strong>and</strong> <strong>Gait</strong>(T<strong>in</strong>etti, 1986)• Uses a 3 po<strong>in</strong>t scale; Separ<strong>at</strong>e balance <strong>and</strong>gait portion• Reliable (.85 <strong>in</strong>ter-r<strong>at</strong>er)• Scores less than 12/16 on balance portion <strong>at</strong>risk for falls; Less than 8/12 on gait portionsignificant• Scores less than 22/28 risk for fall<strong>in</strong>g• Primarily used for screen<strong>in</strong>g
O<strong>the</strong>r Performance Based <strong>Balance</strong> Tests– Berg <strong>Balance</strong> (Berg et al 1992)• Functional balance measure - 14 items - uses 5po<strong>in</strong>t scale (more sensitive than T<strong>in</strong>etti)• Reliable <strong>and</strong> valid (.97-.98 <strong>in</strong>ter <strong>and</strong> <strong>in</strong>tra-r<strong>at</strong>er)• < 46/56 risk for fall<strong>in</strong>g• Scores <strong>of</strong> 36 <strong>and</strong> less <strong>in</strong>dic<strong>at</strong>e a 100%risk <strong>of</strong> fall<strong>in</strong>g (Shumway-Cook, 1997)• Correl<strong>at</strong>ed to T<strong>in</strong>etti (.91); TUG (.76)
– Dynamic <strong>Gait</strong> Index (AnneShumway-Cook 1995)• Most appropri<strong>at</strong>e test to assess fall risk <strong>in</strong>p<strong>at</strong>ients with vestibular dysfunction(Whitney et al, 2000)• Scores <strong>of</strong> 19 or less predictive <strong>of</strong>falls <strong>in</strong> elderly• Tests 8 facets <strong>of</strong> gait (with orwithout assistive device)
Cl<strong>in</strong>ical Approach to Falls• NOT WHAT DISEASE caused <strong>the</strong> problem?(Based on one disease/diagnosis model)• BUT WHAT COMBINATION <strong>of</strong>Physiologic changes, impairments <strong>and</strong>diseases are contribut<strong>in</strong>g?• AND WHICH ONES can be modified?(Multifactorial impairment <strong>and</strong> <strong>in</strong>terventionmodel)
From Horak (2006)
Biomechanical Constra<strong>in</strong>ts• Size <strong>and</strong> Quality <strong>of</strong> <strong>the</strong> Base <strong>of</strong> Support
Biomechanical Constra<strong>in</strong>ts• Limits <strong>of</strong> Stability: The fur<strong>the</strong>st distance <strong>in</strong> anydirection a person can lean away from midl<strong>in</strong>e(vertical) without alter<strong>in</strong>g <strong>the</strong> BOS (by stepp<strong>in</strong>g,reach<strong>in</strong>g or fall<strong>in</strong>g)
Factors affect<strong>in</strong>g Center <strong>of</strong> Gravity <strong>and</strong>Limits <strong>of</strong> StabilityMechanical (actual):• COG position & control• Base <strong>of</strong> Support• Biomechanics– Range <strong>of</strong> Motion– StrengthInternal (perception)• Accur<strong>at</strong>e <strong>in</strong>terpret<strong>at</strong>ion• Experience (anxiety/fear)• Pa<strong>in</strong>
Cl<strong>in</strong>ical Test: Functional Reach Test• Reliable (.89 test –retest)• Scores less than 6-7<strong>in</strong>ches <strong>in</strong>dic<strong>at</strong>elimited functionalbalance (Healthynormal adults can reach10 <strong>in</strong>ches or more)Duncan et al, 1990)
Assess<strong>in</strong>g Lower Extremity Strength• 30 Second ChairSt<strong>and</strong>– # <strong>of</strong> times personst<strong>and</strong>s <strong>in</strong> 30seconds– http://www.exrx.net/Calcul<strong>at</strong>ors/SeniorChair t<strong>and</strong>.htmlSenior Fitness Test (Rikli & Jones, 2001)
Adaptive Movement Str<strong>at</strong>egiesSelection is context specificAnkle Str<strong>at</strong>egy:• Slow Adjustments• COG Near Center• Broad Support BaseHip Str<strong>at</strong>egy• Rapid Adjustments• COG Near Perimeter• Narrow Support BaseSuspension & Step• COG exceed<strong>in</strong>g LOS
Anticip<strong>at</strong>ory Postural Set• Muscle activ<strong>at</strong>ionprior to an expectedCOG disturbance• Prepar<strong>at</strong>ory <strong>in</strong> n<strong>at</strong>ure• Designed tocounteract apredicted COG shift• Tested dur<strong>in</strong>g T<strong>in</strong>etti<strong>Balance</strong>
CENTRAL MOTORIMPAIRMENTS• Str<strong>at</strong>egy selection problems• Increased reaction times• Increased movement times• Selection <strong>of</strong> str<strong>at</strong>egies tocounteract falls not optimal• Anticip<strong>at</strong>ory posturaladjustments slowed
Sensory Str<strong>at</strong>egiesVisualSystemVestibularSystemSom<strong>at</strong>o-Sens<strong>at</strong>ionLight<strong>in</strong>g;movement <strong>of</strong> self orenvironmentGravity;L<strong>in</strong>ear & AngularHead <strong>and</strong> EyeMovementSurface changes &irregularities; BOSchanges
SOMATOSENSORY SYSTEMInform<strong>at</strong>ion from sk<strong>in</strong>,jo<strong>in</strong>ts, <strong>and</strong> muscles sentto <strong>the</strong> bra<strong>in</strong> to provide<strong>in</strong>form<strong>at</strong>ion about jo<strong>in</strong>t<strong>and</strong> body positionnecessary for balancecontrol
Impairments <strong>in</strong> Som<strong>at</strong>osens<strong>at</strong>ion• Nerves th<strong>at</strong> carry sensory<strong>in</strong>form<strong>at</strong>ion to bra<strong>in</strong> deterior<strong>at</strong>ewith age• Decreased proprioception• Increased threshold tovibr<strong>at</strong>ory sens<strong>at</strong>ion
VISUAL SYSTEMVision plays twomajor roles:1) objectidentific<strong>at</strong>ion(central vision)2) motion sense(peripheralvision)
Impairments <strong>in</strong> Visual System• Reduced visual acuity• Ability to accommod<strong>at</strong>e• Inability to adapt to <strong>the</strong> dark• Contrast sensitivity• Depth perception disorders (can be caused byc<strong>at</strong>aracts <strong>in</strong> one eye)• Glaucoma (difficulty with peripheral vision)• C<strong>at</strong>aracts (cloud <strong>the</strong> lens)• Macular Degener<strong>at</strong>ion (near <strong>and</strong> distant visionprimarily affected)
Common Impairments <strong>in</strong>Peripheral Visual SystemNormalGlaucomaVisionMacularC<strong>at</strong>aractDegener<strong>at</strong>ion
VESTIBULAR SYSTEMReceptors conta<strong>in</strong><strong>in</strong>g hair cells with<strong>in</strong> <strong>the</strong> “<strong>in</strong>nerear” sends <strong>in</strong>form<strong>at</strong>ion to <strong>the</strong> bra<strong>in</strong> about <strong>the</strong>position <strong>of</strong> <strong>the</strong> head <strong>in</strong> space <strong>and</strong> sudden changes<strong>in</strong> <strong>the</strong> direction <strong>of</strong> movement <strong>of</strong> <strong>the</strong> head; alsoplays role <strong>in</strong> stabiliz<strong>in</strong>g our gaze dur<strong>in</strong>gmovement
Two major roles:
Impairments <strong>in</strong> PeripheralVestibular System• Deficiencies– Loss <strong>of</strong> hair cells– Reduction <strong>in</strong> VOR ga<strong>in</strong>
Need to be able to choose accur<strong>at</strong>e sensorysystem <strong>in</strong> any given task for normal balance.
Abnormal Sensory Organiz<strong>at</strong>ion• Dysfunction - person who is unableto use a sense• People who select <strong>in</strong>accur<strong>at</strong>e sense– elderly who are “visually dependent”– p<strong>at</strong>ients with post traum<strong>at</strong>ic dizz<strong>in</strong>ess<strong>of</strong>ten select vision as a reference <strong>and</strong>become unstable <strong>in</strong> an environment
– Assess<strong>in</strong>g Sensory Systems• Romberg Test (feet toge<strong>the</strong>r, EO, 20 seccompared to feet toge<strong>the</strong>r, EC, 20 sec);orig<strong>in</strong>ally used to test for posteriorcolumn disorders (Thyssen 1982)• T<strong>and</strong>em (Sharpened) Romberg to<strong>in</strong>crease challenge• Cl<strong>in</strong>ical Test for Sensory Interaction on<strong>Balance</strong> (CTSIB)– Condition 1 = EO, firm surface– Condition 2 = EC, firm surface– Condition 3 = EO, foam surface– Condition 4 = EC, foam surfaceModified Cl<strong>in</strong>icalTest for SensoryInteraction on<strong>Balance</strong> (mCTSIB)(Horak & Shumway1986)
Orient<strong>at</strong>ion <strong>in</strong> SpaceDeterm<strong>in</strong><strong>at</strong>ion <strong>of</strong>Body PositionCompare, Select& Comb<strong>in</strong>e Senses+VisualSystemVestibularSystemSom<strong>at</strong>o-Sens<strong>at</strong>ion• Process <strong>in</strong>puts from <strong>the</strong> periphery• Weight <strong>in</strong>puts based upon relevance (Sensory Weight<strong>in</strong>g)• Select appropri<strong>at</strong>e sensory <strong>in</strong>put based upon•Availability•Accuracy•Value to <strong>the</strong> task <strong>at</strong> h<strong>and</strong>
Control <strong>of</strong> DynamicsFunctional walk<strong>in</strong>g is a smooth progression <strong>of</strong> <strong>the</strong> COG asweight is shifted from one limb to <strong>the</strong> o<strong>the</strong>r, m<strong>in</strong>imiz<strong>in</strong>g <strong>the</strong>associ<strong>at</strong>ed energy dem<strong>and</strong>s
Resources Required forNormal <strong>Gait</strong>• Free passive jo<strong>in</strong>t mobility• Appropri<strong>at</strong>e tim<strong>in</strong>g <strong>of</strong> muscles• Appropri<strong>at</strong>e <strong>in</strong>tensity <strong>of</strong> muscleaction• Normal sensory <strong>in</strong>put(proprioceptive, vestibular, visual)• Appropri<strong>at</strong>e <strong>at</strong>tention <strong>and</strong> motiv<strong>at</strong>ion• Adapt<strong>at</strong>ion (change surfaces; avoidobstacles; alter speed)
Normal Ag<strong>in</strong>g• Should notaffect range <strong>of</strong>motion• Should notaffect tim<strong>in</strong>g <strong>of</strong>muscle activity• Can producemuscle weakness• Can affect visual,proprioceptive,<strong>and</strong> vestibularsystems• Decl<strong>in</strong>e <strong>in</strong> dualtasks• Decrease <strong>in</strong>adapt<strong>at</strong>ion <strong>of</strong> gait
Detectable gait abnormalities arepresent <strong>in</strong>…..20-40% <strong>of</strong> adults age 65 <strong>and</strong>over <strong>and</strong> 50% <strong>of</strong> adults age 85<strong>and</strong> over
Muscle WeaknessHip extensorsKnee extensorsPlantarflexorsDorsiflexors
THEORETICAL EXPLANATIONS?• Multisystem degrad<strong>at</strong>ion <strong>and</strong> p<strong>at</strong>hology• Preferential Shift <strong>in</strong> Str<strong>at</strong>egy Used– Trad<strong>in</strong>g speed for accuracy• Altered <strong>in</strong>form<strong>at</strong>ion-process<strong>in</strong>g– Overall slow<strong>in</strong>g <strong>in</strong> plann<strong>in</strong>g <strong>and</strong> execution– Change <strong>in</strong> way movement problem issolved
Cognitive Process<strong>in</strong>g• <strong>Older</strong> adults with cognitive problems have 2 X higherrisk <strong>of</strong> falls than cognitively normal older adults.• Postural control is impaired by a secondarycognitive task• Falls can result from <strong>in</strong>sufficient cognitiveprocess<strong>in</strong>g to control posture while occupiedwith a secondary cognitive task• Ag<strong>in</strong>g leads to a decl<strong>in</strong>e <strong>in</strong> <strong>at</strong>tention <strong>and</strong> canlead to <strong>in</strong>creased dual task cost
Impact <strong>of</strong> Ag<strong>in</strong>g on Cognitive SkillsFrom: Hedden T, Gabrieli JDE: Insights <strong>in</strong>to <strong>the</strong> age<strong>in</strong>g m<strong>in</strong>d: a view fromcognitive neuroscience. N<strong>at</strong> Rev Neurosci 2004, 5(2):87-96.
Cognitive Tests•M<strong>in</strong>i Mental Exam (
TUGc <strong>and</strong> TUGm• Now have modified TUG to add asecondary task• TUG cognitive (TUGc)= count<strong>in</strong>gbackwards from a number between 80-100(> 15 seconds <strong>in</strong>creased risk for falls)• TUG manual (TUGm) = carry<strong>in</strong>g a glass <strong>of</strong>w<strong>at</strong>er (> 14.5 seconds or more than 4.5seconds difference between regular TUG<strong>and</strong> TUGm <strong>in</strong>creased risk for falls)
Extr<strong>in</strong>sic Risk Factors• Home Fall Hazards• Public Fall Hazards
Home Safety Checklists• Self- report• Quick Screen<strong>in</strong>g <strong>of</strong> safety hazards• Most also <strong>in</strong>clude recommend<strong>at</strong>ions• Few have demonstr<strong>at</strong>ed reliability/validitystudies• Focus on hazards ra<strong>the</strong>r than <strong>the</strong> use <strong>of</strong> <strong>the</strong>environment• Resources: Center for Disease Control(CDC) <strong>and</strong> Rebuild<strong>in</strong>g Toge<strong>the</strong>r
O<strong>the</strong>r Extr<strong>in</strong>sic Risk Factors• Social Situ<strong>at</strong>ion– Liv<strong>in</strong>g alone– Socially isol<strong>at</strong>ed• Activity Level– Active versussedentary– Prior experience
The Good News?Many, if not all, risk factors can bereduced or elim<strong>in</strong><strong>at</strong>ed us<strong>in</strong>g evidencebased<strong>in</strong>tervention str<strong>at</strong>egies.





![Assistive Mobility Devices For Prevention Of Falls[1] - UCSF Fresno](https://img.yumpu.com/48127846/1/190x245/assistive-mobility-devices-for-prevention-of-falls1-ucsf-fresno.jpg?quality=85)