DownloadThe Pharos Winter 2010 Edition - Alpha Omega Alpha
DownloadThe Pharos Winter 2010 Edition - Alpha Omega Alpha
DownloadThe Pharos Winter 2010 Edition - Alpha Omega Alpha
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
EditorialConsultations . . . going, going, gone?Edward D. Harris, Jr., MDDavid P. HillOnce upon a time, 1970 to be precise, I returned toDartmouth Medical School to join the junior facultyin Medicine. Its clinical arm was the Hitchcock Clinic. Mymotives in going north were several, but one was the superbgroup of clinicians in the Medicine section (Josh Burnett,the rheumatologist, in particular). Although it seems noweven more like a fairy tale, everyone at the Clinic was happy,it seemed. One reason was that everyone was salaried, andsalary was based on seniority. The senior pediatrician madea bit more salary than did the only cardiothoracic surgeon.Among other benefits of this payment structure was that freeinterchange of consultations was the norm, particularly the“curbstone” variety.Not long after my return to Hanover, a fee-for-servicecompensation structure with enhanced income for those whoperformed procedures swept through the Clinic quickly. Oneunintended outcome was the gradual suppression of curbsideconsultation. It did no good for the diabetologist to give awaymanagement skills about using the new drugs to the generalinternist. He would say, “Schedule that patient to see me nextweek.”Medicare, however, did save consultation for the cognitivespecialties* by establishing a different billing code that gavethe specialist an additional money for the added work involvedin seeing the patient, doing the needed testing, and makingthe appropriate recommendations to the referring physician.It must be added, however, that the non-cognitive specialists(they reject that phrase!) cared little about the pittance consultationfee. They often saw the patient without charge in returnfor the opportunity to perform a procedure that was indicated.A new balance point had been achieved.On November 25, the balance shifted again. A largelyoverlooked notice in the Federal Register from the Centerfor Medicare & Medicaid Services (CMS) reads, “beginningJanuary 1, <strong>2010</strong> [it will be policy] to budget neutrally eliminatethe use of all consultation codes (inpatient and office/outpatient)by increasing the work RVUs for new and establishedoffice visits.” 1p61769 It further states, “We support the view . . .that in most cases, there is no substantial difference in workbetween consultations and visits.” 1p61771Part of the logic for this change in CMS policy were datagathered by the Office of the Inspector General showingthat 47% of claims received by Medicare were billed as thewrong type or level of consultation, although more egregious* “Cognitive specialties” include those in pediatric and internalmedicine such as: infectious disease, allergy, endocrinology, nondialysisrelated nephrology, rheumatology, geriatrics, hematology andthe components of oncology not related to infusions, and parts ofother specialties such as non-operative dermatology.“mistakes,” e.g., claims not meeting the definition of consultation(19%) or lack of documentation (9%), were found as well.Keep in mind that by 2020 it is estimated that the costs ofhealth care in United States will have doubled, and that despitethe spending, the United States ranks (WHO data): An American woman is eleven times as likely to die in childbirthas a woman in Ireland.Will doing away with consultations for Medicare patients(private insurers will probably follow suit) disrupt the qualityof care that Americans expect and need? One physician bloggersays that cognitive specialists are faced with “the Hobson’schoice being (a) do your usual thorough and thoughtful evaluation,and lose money, or (b) streamline your process (e.g.,cutting allotted time from 60 mins./new patient to 30 mins.)or (c) having the patient who arrives for consultation fill outa detailed and organized history, followed by an interviewwith a nurse in your office, who edits the information into anelectronic format . . . at which point you come in, all charm,glance at the form, examine the patient as necessary, dictatea problem list and a high complexity plan, and schedule thepatient for a series of tests and follow-up visits.”In the next decade, cognitive specialists may graduallydisappear. Or perhaps the new paradigm will be online specialtyconsultations, such as the one offered by Partners, thecombine of Brigham and Women’s, Massachusetts General,and Dana Farber Cancer Center hospitals (econsults.partners.org). The rates are (additional cost for additional staining)Whatever direction is taken, the traditional concepts of consultationare gone.Very much needed, no matter what the outcome of ournation’s strategy for health care reform, is a strong and unifiedvoice of medicine. CMS has found that no matter whatchanges it suggests, the conflicting comments about themcancel each other out. Medicine needs a powerful group ofleaders with whom we can entrust our broad interests andwho must speak in unison for the greater good of our professionand our patients.Reference1. Centers for Medicare & Medicaid Services. Medicare Program;Payment Policies Under the Physician Fee Schedule and OtherRevisions to Part B for CY <strong>2010</strong>. Federal Register 2009 Nov 25; 74:61738–62188.The <strong>Pharos</strong>/<strong>Winter</strong> 2008 1
Issue On the coverSee page 18Page 18The effect of Gchat deprivation onmedical student productivityWhat did we do before there were hand-held devices?Steven Quinn24JosiahA patient makes an indelible impressionCrystal Bowe28Health PolicyWill health reform reduce costs?John A. Kastor, MD35Health reform requires confronting mythsThomas H. Lee, MD36POETRY1112Graft RejectionJ. Joseph Marr, MDMeditation on SurgicalMasksJenna Le27 CarotidWynne Morrison, MD32344349Winning Poems of the 2009Write a Poem for This PhotoContestWear Something RedCarol Abbott, MDThe Woman with EverythingAli ValdrighiA One Bag, One Leg LadyBhagirath Majmudar, MDUndauntedChristine D. Hudak, MDReflections on a PhotographNewton D. Scherl, MDThe GiftElyne N. KahnThe ChallengeDavid DeWittInformal EducationMelanie Buskirk52 SmokeAshley MannPage 24
Mario Lanza, his mother, Mrs. Cocozza, and KathrynGrayson. Credit: Photofest.4 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
Graft RejectionIwent to join the registryThere is out there a need for marrowIt seemed the right and proper thingYet I returned back home in sorrowYou cannot join our registryYou’re healthy, that’s quite true, she saidBut you are far too old right nowWe need a younger man insteadBut I’m quite strong from lifting weightsI also run around the trackWe’re sure that’s true but we don’t careNow go way and don’t come backI make it out of hamburgerTo keep the cost of goods quite lowIts lineage is very strongAt least I’m told that this is soOf quality we have no doubtShe said to me with rueful smileBut seventy is just too oldCare to sit down for a while?Rules are rules; that is quite trueOne must accept the things you sayBut I don’t think you understandI made this marrow yesterdayJ. Joseph Marr, MDDr. Marr (AΩA, Johns Hopkins University,1964) is a retired academic physician and amember of the editorial board of The <strong>Pharos</strong>.His address is: 14885 Irving Street, Broomfield,Colorado 80023. E-mail: marrj@mho.com.The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 1
Meditation onSurgical MasksErica AitkenBehind a surgical mask, no one can see you smile;hence, surgeons are compelled to seek out other waysof conveying the meanings that a smile conveys.All the alternatives are flawed: winking’s too mild;saying “haha” is too corny. A controlled trialinvestigating whether a sarcastic phraseachieves more good than harm is in its early days,and yet off-label use is already in style:attending surgeons often fling sardonic quipsat residents, med students, nurses, even the patient,using quips as a dubious form of compensationfor the fact that no one can see them quirk their lips.As long as masks remain opaque, flesh-cutting docswill likely never cease to make cutting remarks.Jenna LeMs. Le is a member of the Class of <strong>2010</strong> at Columbia University Collegeof Physicians & Surgeons. This poem won second prize in the 2009 <strong>Pharos</strong>Poetry Competition. The author’s address is: 630 W. 168th Street, P&S Box418, New York, New York 10032. E-mail: jnl2105@columbia.edu.12 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
Getting'drug'money'out'of'doctors’'officesPurushottam A. NagarkarThe author (AΩA, University of Texas Southwestern, 2009)is a member of the Class of <strong>2010</strong> at the University of TexasSouthwestern Medical Center at Dallas. This essay wonthird prize in the 2009 <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong> Helen H. GlaserStudent Essay Competition.Abrief survey of medical literature reveals that themarketing practices of pharmaceutical companieshave been under fire for decades. On medical schoolcampuses and in health care policy fora, it is a commonlyheardrefrain that “big pharma” spends as much on marketingas on R&D. In fact, a 2008 study published in PLoS Medicinecontended that pharmaceutical companies spend twice asmuch on marketing their drugs as they do on developing newones. 1 The FDA’s 1997 rule allowing pharmaceutical companiesto advertise prescription drugs directly to consumers isfrequently criticized as being wasteful, promoting unhealthybehavior, and—most damning—making the doctor- patientrelationship more difficult.In this environment, physicians find themselves underincreasing pressure to resist the overtures of pharmaceuticalrepresentatives, to spurn free pens and clipboards and rejectthe free lunches and “educational” dinners they have acceptedfor the past fifty years. Academic medical centers are rewritingthe guidelines that govern when and where pharmaceuticalrepresentatives can contact their faculty and staff, the types ofacceptable gifts and payments, and how CME course curriculaare created and funded. 2 All these efforts focus on doctors,attempting to change the way they interact with the drug industry,but ignore the powerful incentives driving the industryto continue targeting physicians with their marketing efforts.Effective solutions require a full understanding of thecauses and extent of the problem. Several features of the statusquo bear closer attention:1. The cost of prescription drugs2. The impact of pharmaceutical marketing on these costs3. The pharmaceutical industry’s marketing methods.The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 13
Getting drug money out of doctors’ officesChart 1. Distribution of U.S. Health Care Spending by Category.The primary source for Chart 1 is the Department of Health andHuman Services (DHHS) National Health Expenditure report, 3which provided data on insurance profits and overhead, governmentoverhead, as well as spending on public health, equipment,capital, and research. Salaries for doctors, other health careworkers, and all other workers associated with the health caresystem were obtained from the Department of Labor’s Bureauof Labor Statistics. 4 The National Health Expenditure reportestimates only outpatient prescription drug spending, so marketresearch reports 5 estimating total prescription drug spendingand the distribution by channel (outpatient, clinics, hospitals,etc.) were used to derive total spending on prescription drugs.Published profit margins for hospitals and clinics were usedto derive institutional profits. 6 Finally all remaining costs weregrouped into “Other Costs,” which primarily consists of hospitaland clinic operating costs (e.g., rent, utilities, legal costs, etc.).The cost of prescription drugsIn 2005, the United States spent $1.99 trillion on healthcare. The analysis of spending, labor, and industry data inChart 1 reveals where this money is spent.The impact of pharmaceutical industry marketingThirteen percent of total U.S. health care spending ($260billion) went to prescription drugs. In comparison, if U.S. percapita prescription drug spending decreased to the averagelevel of other G8 nations,* we would save $80 billion per year. 7Estimates by global market research companies show thatdrug marketing in Europe is about 12 percent of Europeanrevenue, while in the United States it is about 18 percent ($45billion). 8 This higher spending on marketing likely contributesto the $80 billion incremental cost by driving inefficient drugprescribing patterns. Thus there are two types of costs associatedwith pharmaceutical marketing—direct costs (the $45billion in marketing dollars being passed on as higher drugprices), and indirect costs (the portion of the $80 billion inincremental costs that is driven by inefficient or suboptimalprescribing patterns).* The G8 provides a good basis for comparison, since health outcomesare comparable to those in the United States. The $80 billionvalue is arrived at after correcting for purchasing parity. It accountsfor lower drug prices in countries that have less spending power. Thevalue would be higher without this correction.14 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
Chart 2. Marketing as a Percentage of Salesby Industry (2006)Industry data comprises representativecompanies: Grocers (Kroger, Albertson’s,Safeway), Automotive (GM, Ford, Chrysler,Honda, Toyota), Telecom (Spring, Verizon,AT&T), Retail (Macy’s, JC Penney, theLimited, GAP, Dillard’s, Nordstrom, BestBuy, Circuit City, Radio Shack, Target, andWalmart). 9Two questions about the direct costs need to be analyzed:1. Is the pharmaceutical industry unique in its reliance onmarketing?2. How is the money being spent—on doctors or on massmediaadvertising?The first question can be answered by comparing thepharmaceutical industry to the rest of the economy, shown inChart 2. The drug industry spends five times more on marketing(as a percentage of sales) than other retailers. As theindustry has become increasingly reliant on marketing, it haschanged the allocation of its marketing dollars. Between 1996and 2005, marketing grew from 14.2 percent to 18.2 percentof revenue—a compound annual growth rate (CAGR) of 2.8percent. The breakdown of this spending by category is shownin Chart 3.Spending on detailing—visits to doctors by sales representatives—decreasedfrom 5.4 percent of drug sales in 1997 to4.4 percent in 2005. The increase in spending was mostly ondrug samples (CAGR 3.7 percent). The data in Chart 3 countsdrug samples at their full retail price. Other estimates use thewholesale price of drug samples, physician surveys, and confidentialpharmaceutical industry data to arrive at a differentdistribution by category, shown in Chart 4.While there is some disagreement about whether drugChart 3. Marketing as a Percentage ofSales by CategoryThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 15
Getting drug money out of doctors’ officesChart 4. Marketing byChannel in 2004: TwoIndependent EstimatesEstimate 1 data from IMSHealth, a global health caremarket research company.Estimate 2 data from CAM,a global health care marketresearch company unaffiliatedwith IMS Health.samples or detailing accounts for the bulk of marketing costs,both are marketing activities primarily focused on physicians.Thus, the large majority of marketing budgets—the directcosts of marketing—are spent on physicians.The drivers of the indirect costs cannot be determinedfrom financial statements, simple market research, and industrytrends alone. However, many studies have looked at theeffect of detailing and drug samples on prescribing patterns.One study of obstetrician/gynecologists found that more thanninety percent of surveyed physicians thought that acceptingdrug samples was ethical. 10 More than sixty percent of thesedoctors admitted that they generally prescribed the brandsfor which they had samples, primarily because it was convenientand not for reasons of perceived clinical superiority.Another study found that doctors were three times less likelyto prescribe generic versions of drugs to uninsured patientsif they had access to drug samples. 11 Since the use of genericsis linked to lower costs, 12 these findings imply that, in theabsence of drug samples, prescribing patterns might shifttoward cheaper, clinically- equivalent generics. Thus it is likelythat some of the incremental $80 billion of drug costs in theUnited States compared to the rest of the G8 nations are dueto prescribing patterns.Marketing methods of the pharmaceutical industryAlthough detailing is a highly effective marketing technique,it is also labor- intensive and time- consuming. To compensatefor this, pharmaceutical companies have developedmethods to more efficiently target their detailing efforts.Retail pharmacies sell retail prescription records containingphysician identifiers to data- mining companies. The AMAmaintains and licenses a “masterfile” mapping these identifiersto detailed information about each physician. These two datasources allow pharmaceutical companies to know—in completedetail—the prescribing patterns of individual physicians.It lets them target their efforts effectively, but even moreimportantly, it lets them track the impact of their marketingdollars. For example, if a doctor starts prescribing a drug that asales representative has been pushing, the corporation knowsit is getting a good return on its investment. In this way, companiescan make intelligent decisions about allocating marketingdollars, choosing marketing strategies appropriate to eachphysician’s tendencies, spending more on the physicians whoprovide a return, and less on the ones who don’t.With these pieces of information in hand, the problem canbe summarized simply: Each year, pharmaceutical companiesspend $45 billion on marketing (with $40 billion spent directlyon doctors), tracking and targeting their efforts with doctorspecificprescription data, resulting in increased health carecosts of $80 billion per year.Striking down data miningMost current efforts at resolving this problem focus eitheron asking the industry to spend less on marketing or on settingguidelines for physician interaction with pharmaceutical representatives.But moral imperatives and ethical guidelines havenever proven effective at changing behavior. As long as there isa strong incentive to engage in unethical—but legal—activity, itwill continue. The better solution is to change the incentives andmake unethical behavior unrewarding. While it is probably notpossible to make pharmaceutical marketing unrewarding withoutmandating behavioral changes from physicians, the linchpinof the marketing machine is the ability to assess the return onmarketing dollars. Without access to physician- identifiable16 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
prescription data, pharmaceutical companies would be unableto efficiently target their marketing efforts.This approach is already being pursued by several states.New Hampshire, Vermont, and Maine have passed laws thatprevent the transmission or use of prescriber- identifiableprescription data, effectively short- circuiting the pharmaceuticalmarketing mechanism. The New Hampshire law waschallenged by two data- mining companies, and was initiallystruck down by a federal district court judge as a violation ofthe First Amendment. However, in November 2008 a threejudgepanel of the moderate First Circuit federal appeals courtreversed the district court decision and upheld the law, arguingthat it only regulates conduct and therefore is not a FirstAmendment violation. 13 This bodes well for the Vermont andMaine laws. The advantage of this approach is that it onlychanges the incentives: new guidelines don’t have to be writtenand doctors don’t have to be persuaded that their clinicaldecision- making is affected by marketing pitches. Withoutdata to track the effectiveness of their marketing dollars, pharmaceuticalcompanies might voluntarily reduce their spendingon detailing. This would weaken the pharmaceutical/physicianrelationship, resulting in a reduction of the overall spendingon drugs through greater use of clinically equivalent generics.More importantly, regulating the use of prescription informationis justifiable within a framework of individual privacyprotection. Apart from state licensing boards, the FDA, andthe DEA, no other entity needs access to physician- specificprescription data. This approach does not create complicatedand unenforceable ethical guidelines for physicians, and doesnot require public corporations to behave in a way out ofkeeping with their fiduciary duties.Can there be health care reform withoutpharmaceutical company regulation?The long-term effects of such laws are unpredictable. Willpharmaceutical companies find other ways to track the returnon their marketing dollars? Will they start spending more ondirect-to- consumer advertising? Will doctor/patient interactionssuffer as a result? Will companies spend even more ondetailing because they cannot efficiently allocate their currentbudgets? Will doctors who have come to rely on detailers toprovide them with information on new drugs find themselvesbehind the curve? These claims will no doubt be made by industryspokesmen. In the next few years it will be necessary tolook at prescription and market research data from states thathave successfully implemented these laws. If these data showthat the direct and indirect costs of marketing have indeedbeen reduced as a result of prescription privacy laws, it maybe time for other states to follow suit.References1. Gagnon M-A, Lexchin J. The cost of pushing pills: A newestimate of pharmaceutical promotion expenditures in the UnitedBy and about Purushottam NagarkarI am planning on pursuing a career inPlastic and Reconstructive Surgery. I have alongstanding interest in health care policy,with a special emphasis on its economic aspects.I earned my BS in Electrical Engineeringfrom Rice University in Houston, and worked as a managementconsultant with the Boston Consulting Group.States. PLoS Med 2008; 5: e12. Coleman DL, Kazdin AE, Miller LA, et al. Guidelines for interactionsbetween clinical faculty and the pharmaceutical industry:One medical school’s approach. Acad Med 2006; 81: 154–603. U.S. Department of Health and Human Services, NationalHealth Expenditure Data. http://www.cms.hhs.gov/NationalHealthExpendData/downloads/tables.pdf.4. U.S. Department of Labor Bureau of Labor Statistics. ftp.bls.gov/pub/special.requests/ep/ind-occ.matrix/occ_pdf/occ_29-1060.pdf5. IMS Health, News Releases (2005). 2004 Year-End U.S.Prescription and Sales Information and Commentary. http://www.imshealth.com/portal/site/imshealth/menuitem.0103f29c72c419cd88f611019418c22a/?vgnextoid=41a67900b55a5110VgnVCM10000071812ca2RCRD&vgnextfmt=default.6. American Hospital Association. Trendwatch Chartbook2007: Trends Affecting Hospitals and Health Systems. www.aha.org/aha/research-and-trends/chartbook/2007chartbook.html.7. OECD Health Division. OECD Health Data 2007. Version:October 2007. Paris (France): Organisation for Economic Co-operationand Development; 2007.8. Donohue JM, Cevasco M, Rosenthal MB. A decade of directto-consumeradvertising of prescription drugs. N Engl J Med 2007;367: 673–81.9. U.S. Securities and Exchange Commission form 10-K filings.http://edgar.sec.gov/. See note to Chart 1 for companies researched.10. Morgan MA, Dana J, Loewenstein G, Zinberg S, SchulkinJ. Interactions of doctors with the pharmaceutical industry. J MedEthics 2006; 32: 559–63.11. Miller DP, Mansfield RJ, Woods, JB, et al. The impact of drugsamples on prescribing to the uninsured. South Med J 2008; 101;888–93.12. Haas JS, Phillips KA, Gerstenberger EP, Seger AC. Potentialsavings from substituting generic drugs for brand-name drugs:Medical expenditure panel survey, 1997–2000. Ann Intern Med2005; 142: 891–97.13. IMS Health Inc. and Verispan, LLC v. Ayotte. 07-1945 (1stCir. 2008). www.ca1.uscourts.gov/pdf.opinions/07-1945P-01A.pdf.The author’s address is:2610 Allen Street #1202Dallas, Texas 75204E-mail: nagarkar@alumni.rice.eduThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 17
The ethicsofcosmeticenhancementAnna Raphael, MD18 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>Illustration by Laura Aitken
The author is a resident in Internal Medicine at MontefioreMedical Center in the Bronx. This essay won first prize inthe 2009 <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong> Helen H. Glaser StudentEssay Competition.The burgeoning use of cosmetic procedures and thepotential ethical implications of this trend have beenon my mind since I came face to face with these issuesas a medical student rotating through the dermatology andsurgery departments. I had already seen shows like ExtremeMakeover and knew that going under the knife wasn’t for me.However, now that I was going to be a physician, I not onlyhad to consider what I would do for myself, but what I coulddo and would do for others. The struggle to define the boundarybetween treatment and enhancement is not unique to thefields of plastic surgery and dermatology. Many specialties,from psychiatry to medicine, raise the possibility of makingus “better than well,” 1pxv offering drugs for social anxiety orerectile dysfunction, for example. Still, plastic surgery anddermatology remain the two fields with the most potential forenhancing the healthy rather than simply treating the ill.Over the past few decades, cosmetic plastic surgery anddermatology procedures have been democratized for the publicand adopted with great enthusiasm by physicians. In 2007,board- certified physicians performed 11.8 million cosmeticprocedures in the United States. 2 The top four surgical procedures—breastaugmentation, liposuction, nose reshaping, andeyelid surgery—accounted for 1,175,500 of these procedures, 2up from 443,728 of the top four surgical procedures combinedin 1997. 3 Annual expenditures have increased from an estimated$1 to $2 billion in 1996 to $12.4 billion in 2007. 2,31975—The)FTC)permits)physicians)to)advertise.))The)flood)gates)open.This enormous growth in cosmetic procedures results fromchanges in the law, technology, attitudes, and finances. In thepast, cosmetic surgery was a well- guarded secret of mostlywealthy and upper- middle-class clients. At the same time,physicians were prohibited from advertising their services. InThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 19
The ethics of cosmetic enhancement1975, the Federal Trade Commission lifted its ban on physicianadvertising, and physicians began promoting cosmeticservices. 4 The introduction of less invasive procedures such asBotox injections and injectable wrinkle fillers fueled much ofthe more recent growth, and nonsurgical cosmetic proceduresaccounted for eighty-five percent of total cosmetic proceduresin 2007. 2,5 Botox injection is by far the most common, with4.6 million treatments given by board-certified physiciansin 2007, an increase of 488 percent from 2000. 2 The visualnature of cosmetic procedures made them well-suited to exposureon television and in women’s magazines. Not surprisingly,the American public became more aware and accepting ofcosmetic procedures. 5,6 Finally, health care reform in the 1990sthat reduced reimbursement for reconstructive and medicalprocedures prompted many physicians to start offeringcosmetic procedures or expand existing cosmetic practices. 6Physicians partnered with financial agencies so that morepeople could secure cosmetic surgeries with credit or monthlyinstallments. Today, more than two-thirds of American cosmeticsurgery patients earn less than $50,000 per year. 7While cosmetic procedures have boomed in number, therehas been a simultaneous shortage of reconstructive plasticsurgery and medical dermatology services. Evidence for thisrelative workforce shortage is not as clear-cut as the evidenceof the increase in cosmetic procedures, but it is still highlycompelling. It is suggested anecdotally within the specialtiesand by surveys of residency faculty, physician practice mix,and patient wait times for noncosmetic appointments. Astudy using physician data from the American Medical GroupAssociation and Medical Economics magazine showed thatbetween 1992 and 2002 cosmetic procedures as a percentageof plastic surgery practice increased from twenty-sevenpercent to fifty-eight percent, and the average number ofcosmetic procedures per surgeon annually increased fromfifty-two in 1994 to 105 in 2002. 8 In a recent survey of burncenters, thirty-eight percent anticipated needing to recruit anew burn surgeon in the next five years and eighty-nine percentexpected it would be difficult to do so. 9Botox%first,%then%maybe%look%at%skin%cancerIn dermatology, the reported amount of cosmetic workis also significant. According to a 2007 American Academyof Dermatology (AAD) practice survey, fifty-four percent ofdermatologists reported that cosmetic procedures made upabout ten percent of their practice. 10 Regardless of whethermedia exposure and the popularity of cosmetic proceduresmake the proportion of cosmetic work done by dermatologistsseem higher than what it actually is, surveys of patientsshow problems with access and patient dissatisfaction. Surveysreported in 2006 and 2007 showed that patients were morelikely to get a timely appointment with a dermatologist whenthey requested Botox injections than when they reporteda changing mole, with an average wait time of six to eightdays for the former and twenty-six to thirty-eight days forthe latter. 11,12 Doctors themselves note that specialists in pediatricplastic surgery and dermatology are harder to find. 13Pediatric dermatology and plastic surgery practices are lesslucrative than those treating adults, which get higher insurancereimbursements and often incorporate out-of-pocketcosmetic procedures into their practices. One dermatologyresident professed an interest in pediatric dermatology to me,but acknowledged that pursuing it would decrease her futureincome by $100,000 per year.Beyond the practical dilemmas that a relative workforceshortage creates for the medical profession and patients inneed of noncosmetic services, we need to consider the ethicsof the burgeoning availability and use of cosmetic procedures.Key to the ethics of cosmetic and reconstructive proceduresare these questions: normal? functional impairment mean? plastic surgery and dermatology take on cosmetic procedures?The%cosmetic/noncosmetic%boundary—how%to%define%functional%impairment?The line dividing cosmetic andnoncosmetic procedures is often difficultto define. However, when public resources are used tofinance procedures along this continuum, as in certain countrieswith national health insurance, a distinction must bemade. People generally agree that reconstructive surgery fordisfigurement due to burns, trauma, surgery (e.g., mastectomyfor breast cancer), or congenital abnormality should be coveredby government-financed health care. On the other hand,surgery to correct unattractive appearances due to age or heredityis more difficult to justify when public funds are used.In the 1980s, the Netherlands established objective appearancecriteria for cosmetic procedures to be covered bynational health insurance. These included women havingbreasts whose nipples were at or below the level of their elbows,women with greater than four dress sizes differencebetween their upper and lower bodies, and people who looked20 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
at least ten years older than their chronological ages. 14The seemingly arbitrary nature of these criteria leadsus to wonder how they were decided. At the same time,such standards illustrate that large variations to “normal”appearance must be present before intervention canbe considered. No other national insurance program Iexamined provided coverage for the type of cosmeticprocedures once subsidized in the Netherlands.The philosopher John Rawls spoke of the virtue ofequal opportunity for individuals, which would require eliminatingsocial disadvantages caused by racism, sexism, or lowersocioeconomic status. 15 Norman Daniels interprets equal opportunityas it relates to health care as the ability of individualsto remain as close to “normal functioning” as possible andthereby enjoy their “fair share of the range of opportunitiesreasonable people would choose in a given society.” 15 Theeconomic and social advantages of being tall and good-lookingare well-known. Tall men and attractive men and women havehigher incomes and are more likely to find desirable mates(i.e., similarly tall, attractive and/or wealthy) than their shortand unattractive counterparts. Thus, even if shortness andunattractiveness are part of the range of human variation, onecould argue that such people are functionally impaired in theirability to reach the highest strata of society.It is no surprise that women comprise the vast majorityof patients undergoing cosmetic procedures, making up approximatelyninety percent of cosmetic patients in 2000 and2007. 2,14 The pressure on women to conform to stereotypicalWestern notions of beauty results in Asian woman havingeyelid reconstruction surgery and Jewish or Iranian womengrowing up with the expectation of getting a “nose job.” Whena mother takes her teenage daughter to the mother’s plasticsurgeon, a new kind of family resemblance is perpetuated. 14The American Society of Plastic Surgeons (ASPS) distinguishesbetween cosmetic and reconstructive surgery on itsweb site in an extensive section for “Patients & Consumers.”This distinction hinges on the term “normal”—cosmeticsurgery is performed on normal structures, while reconstructivesurgery is performed on abnormal structures to“improve function” or “approximate a normal appearance.” 16Rhinoplasties and eyelid surgeries, typically cosmetic procedures,could be considered reconstructive if they improvedobstructed breathing or vision. The ASPS does not make anyethical or moral distinctions between cosmetic and reconstructivesurgery on its web site, nor in its 2006 code of ethics.Its explanation that cosmetic surgery is not usually covered byhealth insurance “because it is elective” 16 seems incomplete,however. Many reconstructive surgeries, such as reconstructionfollowing mastectomy or the autotransplantation of a toefor an amputated thumb could also be considered “elective”because they do not improve patient survival, and patients stillhave to choose to have them done. It would be more appropriateto say that cosmetic procedures are not usually coveredBy and about Anna RaphaelPrimarily raised in upstate New York,I graduated from Wellesley College witha degree in biological chemistry andworked as a medical writer before enteringthe University of Pittsburgh Schoolof Medicine, where I edited the literaryand arts magazine Murmurs. My interests include theintersections of sociology and literature with medicine.In June 2009 I began my internship in internal medicinein New York City.by insurance because they are performed on normal, insteadof abnormal structures. Noncosmetic procedures still betterserve what we traditionally view as the goals of medicine.Providing)big)breasts—is)this)the)“healing)good”?The goals of medicine, like the morality of medicine, havebeen described in various ways. Daniels takes a Rawlsian approachto propose that the goals of medicine are to keep allindividuals as close to normal functioning as possible, to create“normal competitors” for the world’s opportunities, evenif not equal ones. 15p316 But with limited health care resources,physicians are not obligated to do everything possible tonormalize people’s functions, let alone enhance them. 15 Wecannot create a world of “normal competitors” because evenassuming an ideal situation in which everyone has the abilityto pay for health care (i.e., universal health insurance), geographicdisparities in the numbers of health care providers andthe availability of technologies will still exist. Moreover, careitself is imperfect. This nevertheless leaves the door open forpeople to privately purchase cosmetic procedures.In the Aristotelian essentialist position of EdmundPellegrino, the goal or “end” of clinical medicine is a healinggood intimately bound up in the physician-patient relationship.17 This internal good is distinct from external goods suchas physician fees for consultation or treatment. The good iscomprised of a “medical good” (technical skills or knowledge);the patient’s perception of good; the “good for humans ashumans,” rooted in common principles of autonomy, beneficence,nonmalfeasance, and justice; and the spiritual good thatThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 21
The ethics of cosmetic enhancementrespects the patient as a divine or spiritual being and is thehighest good that must be served. 17 Cosmetic procedures fitthese different “goods” to varying degrees. They certainly involvetechnical competence and knowledge. Something seeminglyas simple as a Botox injection is done in a systematicway, taking into account facial muscle and nerve anatomy andtitrating to a proper dose of the toxin over time. Many patientsand surgeons testify to how a cosmetic procedure radicallychanged a patient’s life for the better. The availability of cosmeticprocedures is consistent with the principle of patientautonomy; favorable results can count as beneficence. One canargue, however, that such procedures violate the principle ofnonmalfeasance, since healthy patients with normal anatomythus experience the risks and complications associated withcosmetic procedures. Cosmetic surgeons and dermatologistspoint out that complication rates are low and risks versuspotential benefits must be weighed by each patient. At firstit seems difficult to see how cosmetic procedures serve aspiritual good, but if we consider one’s spirituality to includeself-esteem and outlook, it can surely be positively affected bycosmetic procedures.Franklin Miller and Howard Brody take the position thatthe goals and the morality of medicine “are not timeless andunchanging; of necessity they evolve along with human historyand culture.” 18p585 The goals of medicine developed bythe Hastings Center that Miller and Brody cite are examplesof this evolution, as they allow that physicians may pursuea “peaceful death” for patients, something that would havebeen unthinkable before the concepts and principles of patientautonomy, withdrawal of life-sustaining measures, and,to a lesser extent, physician-assisted suicide, became moreaccepted by mainstream medicine. 3 According to Miller andBrody, the problems treated by cosmetic procedures simplydo not qualify as maladies. 3 While they may cause suffering,physicians are not obligated to “relieve any and all pain andsuffering.” 3p354 Only certain physicians, such as psychiatrists,might find themselves compelled to relieve the suffering associatedwith the failures and disappointments of everydaylife, and even they must establish boundaries. Patients withborderline personality disorder, for example, may be told thatthey can call as late as 6 PM to speak with their psychiatrists;after that time, they must leave a message.Treating)the)pain)of)“insufficiency)of)physical)appearance”Related to the goals of medicine is the morality of medicine.Depending on whether we value autonomy or a broadly-definedpatient spirituality more than the principle of nonmalfeasance,cosmetic surgery may or may not be acceptableaccording to the essentialist position of Pellegrino. RobertVeatch takes an entirely externalist position, arguing that medicinehas no common internal core values and that all medicalvalues come from external, culturally-specific sources. 19According to this view, the practice of a nonmedically indicatedprocedure such as castration by physicians would beacceptable because a particular society values the outcome,in this case the preservation of a high-pitched, beautiful singingvoice. 19 Cosmetic surgery would be entirely permissibleaccording to this view because our society values the results.Miller and Brody take a position in between the internalist/essentialist and the externalist positions. They hold that boththe goals and morality of medicine are influenced by internalprofessional virtues related to the commonality of healing, aswell as by external cultural factors. This position may be theclosest to reality. Miller and Brody have stringent criteria forwhat defines a “malady” and for the types of communicationsthat physicians can have with patients. 3 They argue that the“defects” cosmetic patients choose to change must be clearlyvisible. A defect that, to others, may appear perfectly normalmay cause the person with the defect intense dissatisfactionor unhappiness. Like other types of pain, pain associated withone’s physical appearance may be at once undeniable to thesufferer but unverifiable to others. 20Though Miller and Brody would not consider healthypatients with normal (if undesired) features as having maladies,perhaps the increasing prevalence and acceptability ofcosmetic procedures is changing the commonly understooddefinition of “malady,” along with the definition of “normal”itself. This appears to be more prevalent in certain affluentcommunities. According to Alex Kuczynski, a New York Citystyle reporter, people in certain parts of the country expectwomen’s breasts to be augmented. 7 Most breast implants areround instead of the more naturally shaped teardrop. 7 The unnaturalupper fullness that round implants create is valued, asis the way that augmented breasts remain erect when womenare lying down. Surgical “vaginal rejuvenation”—removingexcess skin to tighten sagging labia—while still uncommon, isone of the fastest-growing areas of cosmetic surgery. 7 Equallyworrisome are the hymenoplasties performed on women whohave had premarital sex but who for cultural reasons need toappear to be virgins. In all these cases, different norms areimposed on women and perpetuated through cosmetic procedures—painful,expensive, and not without risk.We may have to accept the evolving concept of “normal”using Miller and Brody’s evolutionary position on medicine,22 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
at least in specific groups of society. Nevertheless, they pointout other ethical issues in the field of enhancement: cosmeticprocedure advertisements often misrepresent benefits in proportionto risks to play on the public’s insecurities, violationsof the morality of medicine, as well as the ASPS’s own code ofethics in the case of misrepresentative advertising. 3 Cosmeticsurgeons claim to enhance self-confidence, although they generallydo not work with a team of mental health professionals,as would those serving sex reassignment surgery patients. 3No#conclusion#with#which#all#doctors#could#agreeFew would argue that cosmetic procedures should notbe permitted. The relative shortage of medical dermatologyand reconstructive plastic surgery services is a related ethicalproblem that our profession will have to address. Perhaps thecreation of dedicated medical and reconstructive tracks withinresidency programs should emphasize improved noncosmeticpatient care, thus retaining more physicians in such practices.The public also bears responsibility for creating the currentenvironment. In trying to become prettier, thinner, youngerlooking,or more virginal, the public recasts the collective definitionof “normal” in ways that discriminate against women,the elderly, minorities who don’t conform to mainstream idealsof beauty, and the poor who, despite being able to splurgeon a procedure or two using credit cards, can never attain themaintained chic of the rich achieved through regular cosmeticprocedures.As physicians we have the ability to choose what servicesto provide our patients. Discouraging sexism and other formsof discrimination, providing timely access to noncosmeticservices, and adhering to a morality of medicine that valuesrestoration to normal more than manipulation of the normalare to me the most compelling reasons for physicians to limittheir cosmetic practices.References1. Kramer PD. Listening to Prozac. New York: Viking; 1993.2. American Society of Plastic Surgeons. Plastic Surgery ProceduralStatistics Press Kit. 2008 Plastic Surgery Procedural Statistics.www.plasticsurgery.org/Media/Statistics.html.3. Miller FG, Brody H, Chung KC. Cosmetic surgery and theinternal morality of medicine. Camb Q Healthc Ethics 2000; 9:353–64.4. Rothman SM, Rothman DJ. The Pursuit of Perfection: ThePromise and Perils of Medical Enhancement. New York: PantheonBooks; 2003.5. Liu TS, Miller TA. Economic analysis of the future growthof cosmetic surgery procedures. Plast Reconstruc Surg 2008; 121:404e—12e.6. American Society of Plastic Surgeons. The History of PlasticSurgery, ASPS and PSEF. www.plasticsurgery.org/About_ASPS/History_of_Plastic_Surgery.html.7. Kuczynski A. Beauty Junkies: Inside Our $15 Billion Obsessionwith Cosmetic Surgery. New York: Doubleday; 2006.8. Krieger LM, Lee GK. The economics of plastic surgery practices:Trends in income, procedure mix, and volume. Plast ReconstrSurg 2004; 114: 192–99.9. Faucher LD. Are we headed for a shortage of burn surgeons?J Burn Care Rehabil 2004; 25: 464–47.10. Burton A. Too busy with Botox or just not enough dermatologists?Lancet Oncol 2008; 825–26.11. Resneck JS, Lipton S, Pletcher MJ. Short wait times for patientsseeking cosmetic botulinum toxin appointments with dermatologists.J Am Acad Dermatol 2007; 57: 985–89.12. Tsang MW, Resneck JS Jr. Even patients with changing molesface long dermatology appointment wait-times: A study of simulatedpatient calls to dermatologists. J Am Acad Dermatol 2006;55: 54–58.13. Hester EJ, McNealy KM, Kelloff JN, et al. Demand outstripssupply of US pediatric dermatologists: Results from a national survey.J Am Acad Dermatol 2004; 50: 431–34.14. Blum VL. Flesh Wounds: The Culture of Cosmetic Surgery.Berkeley (CA): University of California Press; 2003.15. Daniels N. Normal functioning and the treatment-enhancementdistinction. Camb Q Healthc Ethics 2000; 9: 309–22.16. American Society of Plastic Surgeons. Plastic Surgery FAQ:What is the difference between cosmetic and reconstructive surgery?http://www.plasticsurgery.org/Patients_and_Consumers/Plastic_Surgery_FAQs/What_is_the_difference_between_cosmetic_and_reconstructive_surgery.html.17. Pellegrino ED. The internal morality of clinical medicine:A paradigm for the ethics of the helping and healing professions. JMed Philos 2001; 26: 559–79.18. Miller FG, Brody H. The internal morality of medicine: Anevolutionary perspective. J Med Philos 2001; 26: 581–99.19. Veatch RM. The impossibility of a morality internal to medicine.J Med Philos 2001; 26: 621–42.20. Scarry E. The Body in Pain: The Making and Unmaking ofthe World. New York: Oxford University Press; 1985.The author’s e-mail address is araphael@medalum.pitt.edu.The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 23
The effect of Gchat deprivation onmedical student productivitySteven QuinnThe author is a member of the Class of 2012 at theFeinberg School of Medicine at Northwestern University.This essay won an honorable mention in the 2009 <strong>Alpha</strong><strong>Omega</strong> <strong>Alpha</strong> Helen H. Glaser Student Essay competition.My experiment started on Friday, January 30, at exactly12:00 AM according to the friend I was talkingto over instant message as he counted downfrom the official time.gov web site. Back when I was five, Ifirst discovered the wonders of the natural world. I wish Icould say that it was an ant that I stared at in awe that led meto science, but I really can’t remember. Still, I love science.So this is a science experiment, and I must follow the rules ofan experiment: change a single independent variable and observeits effects on any number of dependent variables. Whatdid I change that fateful midnight? We’ll get to that. First, Ineed to bring you up to speed.Med school. Two-thirds of the way done with my first24 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
Illustrations by Jim M’Guinnessyear. I’m still in that tender phase where the term “ischioanalfossa” can put a smile on my face. I’m still caught betweenthe professional sterility of a hospital and the preciousfreedom of a student. But recently my grades have been declining.And Friday, January 30, is the two-week mark beforeour fourth and most difficult test. Friday, January 30, is thatdreaded time when everyone starts studying and, unfortunately,some people stop showering.But I find that the farther I get in my medical training, themore I try to escape it. I’m drawn to projects that couldn’tpossibly be farther from my future. I’ve taken on a timeconsumingrole as producer for our yearly sketch comedyshow. I’ve spent countless hours designing our class hoodieand t-shirt. But creative outlets aren’t the only reasons formy academic nadir. I’ve grown lazy. I’ve started watching TVand lost the will to turn it off. I’ve maintained only enoughenergy to change the channel to something less repulsivethan silence and study. I do my assignments while chattingon-line, occasionally peeking behind my laptop lid just intime to see a building explode on my HDTV.I take pride in being on-line nearly 24/7. I read RSS feedsabout the latest phones and hottest gadgets instead of reviewinglectures. I use my BlackBerry religiously, whethershowing visitors around the top of the Hancock Tower orsitting on the toilet bowl by my lonesome self. I’ve fallen victimto the ease with which I can read and respond to e-mails,texts, instant messages, and even Facebook notifications.I’m shackled to my computer, to my phone, and to theInternet. And so my experiment was designed to changethat. No, I’m not giving up my computer, my phone, or theInternet. That would just be too cruel. One independentvariable at a time, remember? All I’m doing is giving upGmail’s built-in chat for the two weeks before the exam. Yes,it’s an experiment designed to see how much instant messagingaffects my academic performance, but more importantlyit’s a test of my own determination and willpower.And so at 12:00 AM on Friday, January 30, I turned offchat in Gmail.The protocol? Perhaps I should have thought it throughbefore starting. Well, I did know that I didn’t want anybodyto know about it while it was still underway. That would havespoiled the fun. So I didn’t reveal the parameters of this experimentto anyone except the friend who counted down thetime for me.I started this experiment with the intent to quit Gchatand only Gchat, so I could still text, e-mail, and call people.But I faced a few troubling ethical dilemmas with that basicexperimental premise. I found myself e-mailing back andThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 25
The effect of Gchat deprivation on medical student productivityBy and about Steven QuinnI love living in Chicago despiteits cold winters and hot summers.When not busy rocking anatomyprac ticals, I am creatively involvedwith both the school’s literarymagazine and yearly comedy show. I plan tocontinue working on graphic design—throughwriting, photography, and filmmak ing—in myfree time until I graduate in 2012.forth with friends every five seconds. It was instant e-mailinginstead of instant messaging; could I proceed or would thatbe missing the point? I found myself trying to plan a studysession with my roommate and a friend that my roommatewas talking to on-line; could I ask him to tell her what/when/where and just use him as a proxy for my technological Lentor would I not be giving up enough?I managed to survive the moral quandaries by choosing togo conservative. I stayed as far awayfrom anything that might be construedas a breach of con duct by allthe naysayers out there. I never usedanybody else’s Gchat and I neverused anybody as a Gchat liaison. Ididn’t want the baby (read: results)to be thrown out with the bathwater(read: technicalities).And what resulted from turningoff Gchat? Besides infuriating thetwo girls I was holding active conversationswith (hey, I’m a sticklerfor anal-retentive, obsessivecompulsiveprecision), I’ve foundtime to read over lecture material,complete assignments early, and goto sleep before midnight.I will admit that the first few dayswere tough. I found myself loadingup Gmail and keeping it in the backgroundlike I used to—available andwaiting for anybody to start up aconversation. Whenever I sat downto work, I took out my laptop to getonline, only to find a distinct lack ofthings to do since Gchat was turnedoff. The addiction was slowly fading.I no longer left my browser openonce I was done reading my e-mailand feeds; I closed the window. I nolonger reached for my laptop when I started to study; I tookout my syllabus.But it is not enough. While I’m ten to twenty lecturesahead of where I would normally be at this time, I’m stillten to twenty lectures behind the best in our class. While Isleep an hour more each night, it’s still an hour less than theamount needed to wake up refreshed. Giving up Gchat canonly get me so far, because the problem lies deeper than that.There’s something preventing me from diving head-first intomy future. It’s not a question of being in the right field, becauseI adore medicine. But despite my interest, this malaisepersists. I must identify and deal with whatever is holdingme back before I can reach maximal productivity.I avoid doing work despite the fact that I love everything Ido. Gchat isn’t the problem, it’s just a distraction. And sincegiving it up, I’ve found other distractions. I peruse Facebooklike it’s CNN during election sea son, madly posting on people’swalls and commenting on their photos. I start (and finish)more crosswords. I even sit and stare at nothing at all.And while it certainly has some obvious benefits, gettingrid of an entire avenue of communication also has its downsides.I found myself one day in the following situation:26 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
Noon. My friends are in the library and I am in my apartment.Earlier we mentioned eating lunch, but no specifics.We need to organize a get-together, but their phones don’tget service in the library, so they can’t call or text me. Onthe other hand, my BlackBerry isn’t sending or receiving anye-mails due to a server outage, so they can’t e-mail me andI can’t e-mail them. And all this time I’m staring at the littleGchat icon on my phone, scrolling back and forth over ithoping I might accidentally click on it, void the integrity ofthe experiment, and be freed from the misery that is technologicalabstinence. Instead I just send them an e-mail frommy laptop convincing them to leave their comfortable seatsin the library and give me a call. We finally meet up and eatout somewhere an hour later. An hour. Wasted. Fie, lack ofGchat, fie!I turned in my fourth test on Friday, February 13, at exactly12:00 PM, two weeks and twelve hours after I startedthe experiment. But I didn’t get back on-line until a fewhours after that. (So much for that anal-retentive, obsessivecompulsiveprecision that got me yelled at.) I didn’t get backon-line because I didn’t really want to. I no longer felt theurge to. It was a foreign, freeing feeling after so many yearsof being te thered to it. But of course technology is the futureand I am right at the vanguard embracing it. I just don’t wantto embrace it so hard it sucks the life out of me.Was it worth it? Absolutely. When the experiment started,I couldn’t wait to feel the rush of being on-line again. Theknowledge that I would get my drug back kept me alive duringmy self-imposed withdrawal. Before that, I didn’t thinkI’d be able to give it up completely. Forever. But maybe that’spossible now. Would I do it again? If I did, I would allow myselfone caveat. I would let myself go on Gchat on my phone.As inconve nient as it is to type out even short e-mails on atiny keyboard with my knuckles knocking into each other, itwould be nearly impossible for me to try to maintain multipleGchat conversations all feigning interest in other people’sdays. Thus, Gchat on my phone would serve purely as a toolto set up real-life meetings—and an effective one at that.What did I learn? By chatting with people less, I talk topeople more. I listen to people more. Gchat is a prison ofsuperficial connectivity that prevents us from true interactions.And those interactions are something I need to holdon to because they’re the only things keeping me afloat untilI regain the wonder with which I once viewed the world, untilI find medicine’s proverbial ant. I need to take advantageof the time I’m given in this tender phase of my life, becauseonce it passes, the ischio-anal fossa will become just anotherbody part instead of the butt of a clever joke.CarotidWhile lying in the angle of your armI drink in an awareness of your pulse,A beacon like a message to the starsOf a life’s center even as my own.My lips move from your face to find the softCavern of your neck, where they pause, partingTo feel the rushing stream of nourishmentPass bounding underneath the curious touch.Not so long past the purpose of our lungsWas as a bellows for our too hot hearts.No wonder then that a catch in my breathIs coupled with my body’s surge of warmth.In stupor sweet our hands lie intertwined;I cannot tell which fingers yours, which mine.Wynne Morrison, MDDr. Morrison is an assistant professor in Anesthesiologyand Critical Care at the University of Pennsylvania Schoolof Medicine and the Children’s Hospital of Philadelphia. Heraddress is: 34th Street & Civic Center Drive, Philadelphia,Pennsylvania 19104. E-mail: morrisonw@email.chop.edu.The author’s address is:333 E. Ontario Street, Apartment #2113BChicago, Illinois 60611E-mail: s-quinn@northwestern.eduThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 27
ZosiahLaura AitkenCrystal BoweThe author is a member of the Class of <strong>2010</strong> at the BrodySchool of Medicine at East Carolina University. This essaywon an honorable mention award in the 2009 <strong>Alpha</strong> <strong>Omega</strong><strong>Alpha</strong> Helen H. Glaser Student Essay competition.January 3, after finishing her first day of class in thesecond semester of her second year of medical school,was the day a twenty-eight-year-old African Americanwoman began a mother’s nightmare journey. After a morningof pathology and pharmacology lectures, she hurried over toher OB/GYN for her scheduled prenatal appointment. Shethought it was just a routine prenatal visit until her clearlyworried obstetrician concluded his examination. At twentysixweeks gestation, she was eight centimeters dilated and,the physician said, about to deliver her third son prematurely.She visibly paled and likely would have shrieked if she hadn’tseen one of her fourth-year colleagues looking on. Her physiciancalmly noted all of this and kindly pulled the drape,blocking the student’s view. As if that drape were a solid wall,she allowed herself to burst into tears at the thought of anotherpremature labor, of repeating a nightmare she thoughtshe had left behind.Thirty minutes after her diagnosis, she was in the OR beingprepped for surgery. Her son was soon delivered, tiny butso beautiful, though only two pounds twelve ounces. Thenbegan the NICU routine that was to consume their familyonce again.Surprisingly, her first words after awakening from sedationwere singularly focused on her son and his currentstatus. She asked about her son’s vital signs, his oxygen saturation,and how he was being ventilated. The nurse lookedperplexed, until her husband explained (almost apologetically),“She’s a medical student.” The nurse nodded in apparentunderstanding and told them to relax. She said she wouldcheck for the answers to those questions, left the room, andnever returned.The next few days were frantic for everyone. The patientseemed to disobey every physician order to stay in bed andrest. Instead, she went to the NICU as often and for as longas she could physically stand the pain. Fearing it would makeher sleepy, she refused medication until the pain made itimpossible to walk from her room to the NICU. She annoyednurses, students, residents, and fellows with her incessantquestions and hovering vigilance over their every move. Shequickly came to define the term “terrible patient.”On Sunday, the neonatologist told her that the teamwanted to meet with her and her husband. Already feelingthreatened and anxious, she had no illusions about what a28 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
meeting on a Sunday morning with the entire teammeant. To her nonphysician husband she simply said:“They don’t need you to meet with them for goodnews. Good news comes routinely.”With that they rushed to the NICU and were escortedto a bare conference room filled by a large tablesurrounded by somber but familiar faces. The neonatologiststarted to talk. “We didn’t expect this, but there has been aturn for the worse.” There was a glimmer of sadness in hiseyes and a hesitance in his voice, but his experience allowedhim to continue. He kept talking, but the parents were nolonger with him. She, especially, was watching the residents,who were looking down, away, anywhere but in the eyes ofher and her husband. Their forced solemnity and discomforttold her all she needed to know.While they had been gazing around, the NICU fellowhad pulled up a CT scan on the screen. The neonatologistshook his head. “In twenty-six years, I’ve never seen a bleedthis severe. An intraparenchymal hemorrhage this severe. . .” He kept talking, but her eyes were fixed on the screen.The whole left hemisphere seemed to glow like a light. Theneonatologist kept talking, explaining the process of a bleedof this severity. He then explained how the blood wouldhemolyze, and how this type of bleeding carried an almostcertainty of death.Her husband grabbed her hand. “What is he saying?” Theneonatologist tried to explain, but still he stared at her.“He’s saying that our son is going to die.”She could feel the relief from everyone in the room thatsomeone had finally said it. The residents looked up asthough it was now permissible to engage the parents, asthough looking at them before that moment would have betrayeda truth for which no one wanted to be responsible.The neonatologist walked them out of the room soonafter, explaining that he would allow them time to think overwhat was said, and make any decisions with which they werecomfortable.The parents requested a DNR status for their son thatafternoon, and Josiah, as they had christened him, died thenext day. As they walked out of the pod where Josiah haddrawn his last breath only minutes earlier, one of her classmates(a third-year) took her hand, silent, but comfortingnonetheless. She and her husband walked out of the NICU,and tried to return to their life.The next year, as a third-year student, she returned to theNICU on her first rotation of her pediatrics clerkship. Sheseemed the typical medical student. She asked questions, acceptedpatient assignments, and read about their conditions.When asked what she wanted to do in her medical career (orif she even knew yet), she always responded, “Pediatrics andthen, hopefully, neonatology.”There were moments when she lost her composure, becameless than a medical student and perhaps more a futureBy and about Crystal BoweI am an MD/MPH student at the Brody Schoolof Medicine in Greenville, North Carolina.When I’m not studying, I enjoy playing chesswith my husband, reading Harry Potter with my son, orsimply spending time with my friends. I am excited aboutthe opportunities and challenges that lie ahead of me in mymedical career!physician, but it is these moments that haunt her. She boiledwith fury when hearing a resident say that the parents mustnot care for the child because they weren’t present every dayin the unit. She choked back tears while witnessing otherparents receive the terrible news their child wouldn’t survive.Other moments were different. There were times whenshe would stand over her patients’ isolettes and talk to them,when she lingered over a Ballard exam just to watch a babybreathe. She found it easy to sit with the mothers of the sickestbabies, to listen to their thoughts, concerns, worries, andfears. She would sit and listen, often without speaking, neveruncomfortable with the tears, the long silent pauses, or thequiet desperation in the parent’s voice.She still wants a career in pediatrics, and especiallyneonatology. Even serving in the same NICU where Josiahdied, it was clear to her and others that she enjoyed thosedays more than any other of her clerkships. She was neverbothered by the long hours, never tired of poring throughrecords, examining infants, researching differentials. Shestayed up late at night reading a neonatology primer for residentsas if it were a bestselling novel.It has been said that physicians are terrible patients, butwhat about the patient that becomes a physician? Is it betterfor the physician to have the separation that comes withnever having been the patient that he or she now proposes totreat? And what should be a physician’s passion, her drivingforce? Should it be the general goal to do no harm and heal ifpossible? Might there be fear that this patient-student’s goalis no longer that noble aim, but a personal vendetta againstdeath?She does see a bit of her son in each of the babies shetreats, and wants fervently to ensure their hospital coursehas the happy ending denied her own. But is that right? Is ita good reason to enter a field, to choose a life-long profession?In the end, this patient thought it was, and hopefullyshe was right.The author’s address is:600 Moye BoulevardGreenville, North Carolina 27834E-mail: ccorncason@gmail.comThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 29
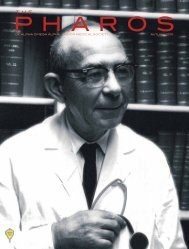
2009 <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong>/Association of American MedicalColleges Robert J. Glaser Distinguished Teacher AwardsEach year since 1988, <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong>, in cooperation with theAssociation of American Medical Colleges, presents four faculty members inAmerican medical schools with the AΩA Distinguished Teacher Award. In 1997,AΩA named the award to honor its retiring executive secretary Robert J. Glaser,MD. Nominations for the award are submitted to the AAMC each spring by thedeans of medical schools.Nominations were reviewed by a committee chosen by AΩA and theAAMC. This year’s committee members were: Peter G. Anderson, DMV, PhD;Paul Aravich, PhD; Carmine D. Clemente, MD, PhD, MS; Linda S. Costanzo,PhD; Arthur Dalley, PhD; Helen C. Davies, PhD; Daniel W. Foster, MD; StevenL. Galetta, MD; David E. Golan, MD, PhD; Charles H. Griffith, MD, MSPH, MS;Robert M. Klein, PhD; David W. Nierenberg, MD; John Nolte, PhD; Louis N.Pangaro, MD; Richard M. Schwarzstein, MD; Robert T. Watson, MD; Jeffrey G.Wiese, MD.Winners of the award receive $10,000, their schools receive $2,500, andactive AΩA chapters at those schools receive $1,000. Schools nominatingcandidates for the award receive a plaque with the name of the nominee.Brief summaries of the accomplishments in medical education of the 2009award recipients follow.Edward D. Harris, Jr., MD, Executive SecretaryClockwise from top left: Ronald A. Arky, MD; David A.Asch, MD, MBA; Eugene C. Corbett, Jr., MD; Erika A.Goldstein, MD, MPH.Ronald A. Arky, MDCharles S. Davidson DistinguishedProfessor of Medicine and Dean ofCurriculum, Harvard Medical SchoolAs the Charles S. DavidsonDistinguished Professor of Medicine atHarvard Medical School, Ronald Arky(AΩA, Cornell Medical College, 1955)has discovered both his passion and hisstrengths. Arriving at Harvard in 1963after receiving his MD from CornellMedical College, Dr. Arky has focusednot only on his expertise in endocrinologyand internal medicine, but on thefuture of how medical students shouldand can learn their craft and be readyfor the new imperatives of practice.Harvard students have honored himmultiple times. One citation was forhis “vital campus presence, unendingadvocacy of students and commitmentto clinical education.” His platformfor innovation has been Chair of theDepartment of Medicine at the MountAuburn Hospital in Cambridge, servingfrom 1971 to 1993. He was instrumentalin creating the HMS New Pathway thathelped integrate for students the basic,behavioral, social, and clinical sciences,giving them a sense of a longitudinalunderstanding of a medical career.His concepts are being implementedat many academic medical centersin the United States and Canada. AsMaster of the F. W. Peabody Society,one of four at HMS, Dr. Arky has hadthe opportunity to advise and mentorhundreds of students, all of whom aregrateful to him for his care and personalattention.David A. Asch, MD, MBARobert D. Eilers Professor ofMedicine and Health CareManagement and Economics,University of Pennsylvania School ofMedicine and the Wharton SchoolDr. Asch (AΩA, Cornell University,1984), a member of the faculty of theUniversity of Pennsylvania for nineteenyears, has been a major contributor toinnovative educational programs thatconnect the School of Medicine with30 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
the wider university community. In1993, in partnership with faculty fromthe Wharton School, he developed atraining program that enables thosewith doctoral training in economics,psychology, sociology, and relatedfields to spend two years working in theSchool of Medicine. Using the resourcesof the Philadelphia VA Hospital, hecreated an externally funded ambulatorycare training program for students,residents, nurse practitioners, and MBAstudents. Students from the Schoolof Engineering and Applied Sciencescan, with a partnership that Dr. Aschhelped develop, learn special expertisein medical informatics. As director ofthe RWJ Foundation Health and SocietyScholars Program he has enabled intellectualleaders to catalyze the creationof a new field aimed at understandingthe social determinants of health. Morerecently he created a Master of Sciencein Health Policy Research that trainsmedical students in a joint MD/MSHPprogram in health policy research.Many of his trainees have won nationalprizes (including several awarded atthe White House) and career developmentawards. One student commented,“I want Dr. Asch to teach all of myclasses.”Eugene C. Corbett, Jr., MDAnne L. and Bernard B. BrodieProfessor of Medicine, Professorof Nursing, University of VirginiaSchool of MedicineDr. Corbett (AΩA, University ofVirginia, 2001) earned his MD at theUniversity of Chicago, and took histraining in Internal Medicine at theBayview Medical Center at JohnsHopkins University. After eleven yearsin rural community practice, duringwhich he provided opportunities formedical students and residents to learnambulatory medicine, he joined thefaculty at UVa. His dean reports thathe has received “almost every educationaward that can be given in theSchools of Medicine and Nursing atthe University,” including the covetedRobley Dunglison Award for the topclinical teacher by the Class of 2003.Clinical skills education has been amajor focus of his interests, leadingto his current role as chair of theAAMC Task Force on the ClinicalSkills Education of Medical Students,from which three monographs havealready been published. In recognition,the Clerkship Directors in InternalMedicine awarded Dr. Corbett theLouis N. Pangaro Educational ProgramDevelopment Award. He has definitelyjoined Ken Ludmerer in presentingthe coming of the second revolution inAmerican Education, emphasizing thatcareful examination of the patient is notpassé.Erika A. Goldstein, MD, MPHProfessor of Internal Medicine,University of Washington School ofMedicineDr. Goldstein (AΩA, Universityof Rochester, 1981) came to theUniversity of Washington as a residentin Internal Medicine. Following herchief residency she was recruited tothe faculty and now is a Professor ofMedicine. Along the way she earnedher Master of Public Health and a MAin Anthropology. Her strength and lovein medicine is teaching, but her deanlabels her a “ ‘triple threat’ visionary,organizer, and role model” in medicaleducation, and a different kind of triplethreat—teacher, mentor, and friend—for students, residents, and faculty.Not surprisingly, she was recognizedas the Distinguished Clinical TeacherAward recipient at UW in 2000, 2001,2002, and 2003, and in 2003 receiveda designation as “Teacher Superior inPerpetuity,” one of fourteen facultyever to have received this honor. Herpublications relevant to medical educationinclude chapters and papersfocusing on continuous professionalimprovement, and she has designedinstitutional approaches that can beimplemented by all academic medicalcenters. She has promoted fundamentalclinical skills using the competencybasedapproach. One student referredto this “uncommonly decent humanbeing” by the comment, “There is areason she is the only faculty memberwe call by her first name. She is morethan a faculty . . . she is our friend.”Distinguished teacher nomineesThomas Andreoli, MD, University of Arkansasfor Medical Sciences College of MedicineM. J. Barchman, MD, The Brody School ofMedicine at East Carolina UniversityCharles L. Bardes, MD, Weill Cornell MedicalCollege of Cornell UniversityCraig W. Clarkson, PhD, Tulane UniversitySchool of MedicineLarry Rex Cochard, PhD, NorthwesternUniversity, The Feinberg School of MedicineTomer Davidov, MD, University of Medicineand Dentistry of New Jersey, Robert WoodJohnson Medical SchoolStephen E. DiCarlo, PhD, Wayne StateUniversity School of MedicineRenee Z. Dintzis, PhD, Johns HopkinsUniversity School of MedicineStephen W. Downing, PhD, University ofMinnesota Medical SchoolStephen Evans, MD, Georgetown UniversitySchool of MedicineJoseph C. Fantone III, MD, University ofMichigan Medical SchoolPaul Gillespie FitzGerald, PhD, University ofCalifornia, Davis, School of MedicineRichard A. Hoppmann, MD, University ofSouth Carolina School of MedicineLinda Y. Johnson, PhD, University of TexasHealth Science Center at San AntonioJames P. Keating, MD, Washington Universityin St. Louis School of MedicineMichael W. King, PhD, Indiana UniversitySchool of MedicineGary L. Kolesari, MD, PhD, Medical College ofWisconsinSalvatore Mangione, MD, Jefferson MedicalCollege of Thomas Jefferson UniversitySusan Masters, PhD, University of California,San Francisco, School of MedicineGary C. McCord, MD, Texas A&M HealthScience Center College of MedicineDennis H. Novack, MD, Drexel UniversityCollege of MedicineDavid A. Rogers, MD, Southern IllinoisUniversity School of MedicineCharles B. Rush, MD, Vanderbilt UniversitySchool of MedicinePaul F. Shanley, MD, State University of NewYork Upstate Medical University College ofMedicineBarbara Sheline, MD, MPH, Duke UniversitySchool of MedicineGerald H. Sterling, PhD, Temple UniversitySchool of MedicineLinda C. Stone, MD, Ohio State UniversityCollege of MedicineMarc Tischler, PhD, University of ArizonaCollege of MedicineNagaswami Vasan, PhD, DVM, MS, UMDNJ—New Jersey Medical SchoolBruce Wallace, PhD, University of ColoradoDenver School of MedicineMichael I. Zucker, MD, David Geffen School ofMedicine at UCLAThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 31
Wear Something Red“Wear something red—”His last hotmail had said,“So I will know it’s you.I’ve booked a room for two,I’m sure it’s safe—but just the same,I made it in another name.And just in case my train is late,(It gets in at half past eight),You should just sit and wait.”I never did believe in fate,A “likely” story I can easily create,And so I lied about my weight—About my age as well—I have to say,(He’ll never know my true birthday).A few more pounds I need to lose,But proper foods are hard to choose.This suit—it does look somewhat tight,But all the same it looks all right.I like to show a flash of thigh,But just enough to catch his eye!Of course a lot depends on how I sit,How much to open that inviting slit.I’m glad it shows my cleavage too,Although for him it may be nothing new.I like my hat (not recently designed).It took a lengthy search to find,Dear Mother’s hatbox—for ages out ofmind.Her skilful milliner—long dead!I’m sure she would have said,“Wear something mod instead.”Too late now! He said he wanted red.Speaking of time: did I misread?I’m almost certain he agreed,To keep in touch at any rate,(“I’ll call you if I’m running late.”)But … why would I expect a call?(Sigh) I don’t have a “cell” at all!Now it’s almost half past ten.I’ve learnt my lesson once again,Where is this “Renaissance Man” of mine?(“Likes music, food and wine—Seeks lady friend to share fine thingsof life—and any thrills life brings.”)Too bad! I should have known then,I’ve been a pawn for men again.Carl Abbott, MDDr. Abbott was elected to AΩA at Dalhousie Universityin 1975. His address is: 5845 Inglewood Drive, Halifax, NS,Canada B3H 1B2. E-mail: cabbott@dal.ca.Winning%Poems%%of%the2009%Write%a%Poem%%%for%This%Photo%ContestThese poems are the winners of the 2009 Write a Poem for This Photo Contest.Congraulations to contest winners Carl Abbott, Christine Hudak, BhagirathMajmudar, Newton Scherl, and Ali Valdrighi.! ! !The Woman with EverythingThere she sat in another lobbyChecking into a fancy hotelBut from the downcast turn of her red lipsIt may as well have been a cheap motelSuites plucked straight from HollywoodfilmsLittered with thousand dollar winePrivate jets at her disposalEverything was perfectly divineYet our privileged heroineFelt a million miles from grandEven with so much fineryAt the drop of a handShe couldn’t help rememberAll the times beforeThe empty lonely nightsAs another marriage hit the floorHer family torn to shredsChildren in stony, silent tearsNo one left to ease the burdenOf the long stretched out yearsThe woman with everythingSat alone with all her bagsWondering why if she had everythingShe felt like all she had were rags.Ms. Valdrighi’s e-mail address is: alivaldrighi@netscape.net.Ali ValdrighiA One Bag, One Leg LadyReady for a solitary journeyAll longings and belongingscompressed in a single bagfilled with dying sighs and tamed tears.Stretched out handle held byinvisible, resolute handsready to carry the cargo.A discovering head covered with a hatuncovering a thousand loose threadsfinally untangled, free of knots.A window showing a blind futureand a past swarming with emotionsthat came to a standstilllike a spinning top.Guts, glia, gonads joiningin harmony with her heart.Life—a tragedy to one who feelsand a comedy to one who thinks.Her feet fatigued from draggingwill now take steady stepson a leg that lags no moreto reach an unknown address.May the winds blow on her back!Bhagirath Majmudar, MDDr. Majmudar was elected to AΩA at EmoryUniversity in 1979. His address is: PathologyDepartment, Grady Health System, 80 Jesse Hill Jr.Drive S.E., Atlanta, Georgia 30303. E-mail: bmajmud@emory.edu.32 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
Undaunted“Vamp,” they whispered,Not softly enough, as sheStrode from the soirée.“Kept woman,” others hissed,Citing her wardrobe,Jewels and seductive currency.Look below the hat andAbove the décolletageAnd see the truth.Somber resolve.Courage to embark onThe next journey.Determination to leaveLuxurious, meaningless trappings,For the wealth of today.Christine D. Hudak, MDDr. Hudak was elected to AΩA in 1991 at the Ohio State UniversityCollege of Medicine. Her address is: 444 North Main Street, Akron, OH44309. E-mail: hudakch@summa-health.org.Reflections on a PhotographThis woman in redAppears very well fedA stylish hat sits upon her headI approached her with fear and dreadShe turned to me and then she said“I’m on my way to again be wedMy late husband is now officially deadI am heading to my new love, NedI hope he will be as gentle in bedThis bag I carry appears weighted with leadIt contains the ashes of my deceased FredI’m looking for somewhere they can be spread”We glanced, we parted, no tears were shedI hope she is happy—this woman in redNewton D. Scherl, MDDr. Scherl was elected to AΩA in 1954 at the MarquetteMedical School, now the Medical College of Wisconsin. Hisaddress is: 363 Castle Drive, Englewood Cliffs, New Jersey,07632. E-mail: nscherl@nj.rr.com.The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 33
The GiftOn that first day of classwe were like the young childat the county fairholding a plump plastic sackto her face peering inat the goldfishturning cramped circlesin awe of the responsibility before us.We were timidfearful we would stumbledrop this gift to the groundand lose the chanceto learn your secrets.But we proceededencouraged by lessonsheld captivebeneath your skin.We grew more comfortablesometimes so engrossedas to forget that these structureswere once alivewere once partsof a whole that danced and spokeand laughed and weptand made choiceslike the choice that brought you to us.And by the time your outer sheetshad been entirely stripped awayand your secrets exposedit was clearthat our responsibility was notto preserve this giftbut to preserve your hopethat you would make physiciansfrom youthful studentsand through uswith usheal.Elyne N. KahnMr. Kahn is a member of the Class of 2011 at Vanderbilt University School ofMedicine. This poem was an entry in the 2009 <strong>Pharos</strong> Poetry Competition. Mr.Kahn’s address is: 1606 18th Avenue South, #25, Nashville, Tennessee 37212. E-mail:elyne.kahn@gmail.com.34 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
The editors invite original articles and lettersto the editor for the Health Policy section,length 1500 words or fewer for articles,250 words or fewer for letters.Please send your essays toinfo@alphaomegaalpha.org or to our regularmailing address: 525 Middlefield Road, Suite130, Menlo Park, CA 94025. All essays aresubject to review by the editorial board ofThe <strong>Pharos</strong>.Health PolicyWill health reform reduce costs?John A. Kastor, MDThe author (AΩA, New York University 1981) is editor ofthe Health Policy section of The <strong>Pharos</strong> and professor ofMedicine at the University of Maryland, Baltimore.As part of his health care reform program, PresidentObama has pledged to reduce what health care costs.How realistic is this goal? Let’s look at two of the elementsthat directly affect how doctors practice medicine.Preventive careIt is a convention that preventive care reduces medicalcosts. If such risk factors as hypertension, hypercholesterolemia,smoking, and obesity are better controlled by regularambulatory visits, and patients are regularly screened forcancer, the use of expensive hospital admissions should bereduced. Universal coverage with medical insurance for everycitizen should remove the monetary factor that prevents manypatients from receiving the preventive care they need. But willpreventive care for all really save money?Let’s take just one example from my specialty of cardiology.Compare the cost of prescribing a statin for everyonewith elevated LDL cholesterol with the savings producedby not having to hospitalize those who would havedeveloped myocardial infarction were they not takinga statin. The problem here is that providinguniversal preventive care includes many morepeople than it directly helps. Someday, wemay know better who really needs to have the LDL cholesterolreduced and treat only them. Not yet, however. Obviously,there is great benefit to those whose illnesses are prevented orpostponed, but have we saved money by applying preventivecare in these cases?Salaried versus fee-for-service practiceIn July 2009, the president visited the Cleveland Clinic andcame away praising the way it delivers medical care while costingless than other large hospitals.David Brown, the medical reporter at the Washington Postand a physician, wrote, “The average spending on a Medicarepatient with severe chronic disease during the last two yearsof life was $35,455 at the Cleveland Clinic, which was thecheapest. Massachusetts General Hospital came in at $47,880,Johns Hopkins at $60,653, and UCLA Medical Center led thelist at $72,793.” 1The Cleveland Clinic controls costs in several ways. Onerelates to the way the doctors practice. All are members ofan integrated multispecialty group practice and are salaried. 2Theoretically, salaried doctors are less likely to overuse testsor consultations since their incomes are not directly dependenton fee-for-service compensation. If this is true, thenoverall health care costs would decrease or not grow so fastif more doctors worked in such salaried group practices.Although some doctors work in the type of salaried practicepraised by President Obama , we can reasonably assume thatThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>35
most are paid by fee-for-service. According to the AmericanMedical Association’s (AMA) Physician Masterfile, 3 141,188of the 801,746 direct patient care physicians in the UnitedStates (18 percent) are in solo or two member practices and311,713 (39 percent) are in group practices of three or more.*Data on how they are paid, by salary or fee-for-service, are notincluded in the AMA survey. 3How many doctors now practicing privately would voluntarilybecome salaried employees of not-for-profit groups andgive up the higher incomes that can accompany efficient privatepractices? Specific incentives might help, but what formwould they take, and how much would they cost? Forcing doctorsinto such groups, of course, is politically untenable—notthe “American way.” Furthermore, forming such groups anddeveloping the systems to assure their financial efficiency will* Many of the other physicians in the AMA Physician Masterfile areemployees of city, state, or federal governments and medical schools,and many, if not most, are probably salaried. 190,549 (24 percent) arereportedly working in hospitals, some presumably as radiologists,pathologists, hospitalists, and emergency physicians.take time and capital. The Cleveland Clinic’s group practice isas old as the Clinic itself, which was founded in 1921. 4 Many ofits efficiencies depend upon refinements made to the systemover decades.References1. Brown D. Obama visits clinic known for quality care, controllingcosts. Washington Post 2009 Jul 23: .2. Kastor JA. Chapter 2. Cleveland Clinic: The clinical factory.In: Kastor JA. Specialty Care in the Era of Managed Care: ClevelandClinic versus University Hospital of Cleveland. Baltimore (MD): TheJohns Hopkins University Press; 2005: 16–23.3. Weaver T (Chicago, IL). E-mail communication 2009 Aug 25.4. Clough JD (Cleveland, OH). E-mail communication 2009 Aug 11.The author’s address is:University of Maryland Medical System110 South Paca StreetRoom 2N-139Baltimore, Maryland 21201E-mail: jkastor@medicine.umaryland.eduHealth reform requires confronting mythsThomas H. Lee, MDThe author (AΩA, Cornell University Medical College 1979)is Network President of Partners Healthcare System andProfessor of Medicine at Harvard Medical SchoolProgress in health reform just might be underway, becausethe pain of the status quo is beginning to exceedthe fear of the unknown for virtually all major stakeholders.But real movement will require that these stakeholders—includingproviders—confront some of the myths thatprop up the status quo. Here are five widely-held but flawedbeliefs 1 worth taking on:1. Choice equals qualityAmerican patients treasure the freedom to go to any doctorthey choose, but they cannot judge the quality of providersfrom available data, so they rely upon the recommendationsof doctors, family, and friends. They suspect that government,health plans, or provider organizations might restrict theirfreedom of choice for financial reasons—and these suspicionshave some merit.The irony is that patients’ freedom of choice inevitablyleads to the fragmentation of care—and worsens efficiency,safety, and quality. Patients end up with physicians in multiplehospitals and practices, and no communication among them.Their care would be better if they valued coordination amongtheir physicians more than their freedom to go anywhere.They do not realize that average physicians who work closelytogether might help them more than brilliant physicians whodo not.2. Higher quality will reduce costsThere are some issues for which better quality really doesreduce costs, like smoking cessation and heart failure diseasemanagement programs. But the harsh reality is that betterquality usually means higher costs, not lower.Nevertheless, many politicians and provider leaders suggestthat our cost challenges can be addressed throughprevention of disease. But prevention requires medicationsand patient education, both of which are costly. And, sooneror later, everyone does become sick and expire—generating36 The <strong>Pharos</strong>/<strong>Winter</strong> 2008
considerable costs in the process.An analysis from the American Diabetes Association,American Heart Association, and American Cancer Societyexamined this issue using data on a national sample. 2 Theyconcluded that the only preventive activity likely to be costsavingover thirty years is smoking cessation. Other preventiveinterventions such as control of blood pressure, diabetes, andcholesterol would substantially increase overall health carecosts.Secondary prevention programs that are focused on patientswith a high risk for hospital admissions, such as patientswith known heart disease, might actually save enoughthrough avoided hospitalizations to offset their expense. Butwhen preventive programs are focused on lower-risk patients,they do not save money. Some preventive programs actuallyrequire more to “buy” a year of life than liver transplantationprograms. 33. Market forces can control costsFor every health care provider pinning hopes on betterquality, there is at least one health care purchaser who believesthat market forces can drive out waste and raise quality. Thesemarket forces would be unleashed by exposing patients to thetrue costs of care and providing data on the costs of care fromvarious providers.Unfortunately, patients do not enjoy exposure to costs,especially when they are sick. Few people have signed up forhealth insurance products designed to turn them into consumers.Furthermore, the data intended to help patients makechoices are just not that helpful and are used by only smallnumbers of patients.An additional limitation for market forces is that about halfof costs are expended for five percent of patients. These patientsare too sick and have conditions too complex to behavelike consumers. In fact, if they shopped around and got theircare at multiple places, their overall treatment would likelydeteriorate.4. A single-payer system would address all our problemsFor every political conservative who hopes that marketforces can solve health care’s woes, someone on the ideologicalleft believes in a single government-run health care system.They cite countries where single-payer systems provideuniversal access, and where health data are better than in theUnited States.A single-payer system could address the issue of accessto care, but it would not necessarily address the quality andsafety problems generated by a fragmented delivery system.Real progress in these areas will require payment systemsthat reward providers who can organize themselves aroundperformance goals.5. Physicians’ autonomy is the most important guaranteeof qualityThe most uncomfortable myth represents a challengeto physicians who oppose any threat to their individual autonomy.These colleagues argue that medicine is a mix of artand science, and they look with scorn on “cookbook medicine.”They worry that guidelines and disease managementprograms might control costs at the expense of their patients’outcomes. They want to be free to do what is best for their patients,and to make their own judgment about what that mightbe. They do not want to be forced to work in teams, and theydo not want to be told what to do.Many of the physicians who feel this way are, in fact, wonderfulpeople and terrific doctors. But concern over risingcosts has helped expose the tremendous unexplainable variationin care patterns among physicians —raising the questionof whether they can all be practicing the very best medicine.Efforts to reduce variation inevitably erode individual physicianautonomy.Furthermore, medical progress has made the right thing todo in many situations much more clear—thereby making possibleincreased roles for non-physicians. Nurses, pharmacists,and even the patients themselves can be active participants inhealth care delivery, if physicians will let them be membersof the team. Physicians can be the leaders of those teams, butthey have to keep in mind that team leaders are also teammembers. That means following the same protocols, using thesame terminology, updating “teammates” on what is happening.And being part of a team inevitably means giving up someautonomy—that is, if you want your team to win.There are still countless opportunities when the right thingto do is unknown, and physician autonomy will always be animportant value in medicine. But individual physician autonomyis not the highest value in medicine, and there are timeswhen it should be placed subservient to other values—mostnotably what is best for patients.References1. Lee TH, Mongan JJ. Chaos and Organization in Health Care.Cambridge (MA): MIT Press; 2009: 233–39.2. Kahn R, Robertson RM, Smith R, Eddy D. The impact of preventionon reducing the burden of cardiovascular disease. Circulation2008; 118: 576–85.3. Cohen JT, Neumann PJ, Weinstein MC. Does preventive caresave money? Health economics and the presidential candidates. NEngl J Med 2008; 358: 661–63.The author’s address is:Partners HealthCare SystemPrudential Tower, 11th Floor800 Boylston StreetBoston, Massachusetts 02199E-mail: thlee@partners.orgThe <strong>Pharos</strong>/<strong>Winter</strong> 2008 37
The physician at the moviesPeter E. Dans, MDThe Curious Case of Benjamin ButtonStarring Brad Pitt, Cate Blanchett, Taraji P. Henson, and JuliaOrmond.Directed by David Fincher. Rated PG-13. Running time 165minutes.When I say that this film’s main asset is that it is watchable,I don’t mean to damn it with faint praise. Beingwatchable is no small distinction given the current crop ofHollywood offerings. It’s less shallow than most and has anintriguing premise. Other assets are the acting of Brad Pitt,whose voice and image are in almost every scene; the supportingcast, especially Taraji P. Henson; and the art direction,makeup, and visual effects for which it won Oscars. Italso is more literate than most films produced today, possiblybecause it’s very loosely based on a short story by F. ScottFitzgerald (more about that later). The discontinuities betweenscenes and its limited action are compensated for bythe voiceover narration. The story begins in an ICU on theday Hurricane Katrina is about to hit New Orleans. Benjamin’saged wife Daisy (Cate Blanchett), whose pain is being regulatedwith a morphine drip, is dying of cancer. She tells herdaughter Caroline (Julia Ormond) to read Benjamin’s diary,which recounts his life. In the process, Caroline will learn thatBenjamin is her father.It’s 1918 and a New Orleans clockmaker who lost his son inWorld War I completes construction of a clock for the trainstation where he last saw his son alive as he went off to war.Unveiled on the day World War I ends, the clock has beenmade to run backwards in the clockmaker’s hope that all thosekilled in the war would return home alive. That same day ina local hospital, a progeria-like baby boy is born to a womanwho dies after the delivery. The embarrassed father scoops upthe child and is carried along by the crowd to the train stationwhere he witnesses the clock run back in time. He then runsout and deposits the child with $18 on the step of a home forthe elderly run by a kind and energetic black woman namedQueenie (Taraji P. Henson). She decides to rear the child asher own, saying that he may be ugly but he’s “still a child ofGod.” She names the “child,” actually an old man who can’twalk unassisted, Benjamin. He is, as Queenie says, like “somecreatures who aren’t meant to survive.” The saving grace isthat he’s like everyone else in this nursing home, where theresidents are seen going through their daily routine. An exmilitaryman raises the flag daily. An ex-opera singer singsWagner. A man repeats his story about having been struck bylightning seven times and each time the scene plays out in hismind and onscreen. Supper is at 5:30.Queenie’s helpmate Tizzy (Mahershalalhashbaz Ali) is anequally good man who had been a dresser for John WilkesBooth and recites Shakespeare. This prompts Benjamin toarticulate a catch phrase like the line in Forrest Gump about“Life being like a box of chocolates, you never know whatyou’ll get” (except of course if you buy a Whitman’s Sampler).In this case, it’s, “You never know what’s coming for you.” On aSaturday night they go to church, where a faith healer attemptsBrad Pitt as Benjamin Button in The Curious Case of Benjamin Button. Photo credit Warner Bros. Pictures and Paramount Pictures38 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
to heal Benjamin by casting him down and telling him to walkunassisted with only his two canes, which he does for the firsttime. Then the preacher dies. The significance of this escapedme except that, as Benjamin notes, death is a common visitoras “people came and people left” the home.There is a confusing set of scenes where a so-called bushmanfrom Africa appears at the home. I found it hard tounderstand his words and switched on the English subtitles,which were quite useful. The bushman reflects on the factthat “when you’re different like us, you’re going to be alone alot,” but then he goes on to say that many folks (tall, skinny,fat) who are not so different are alone, too. A pianist comes tothe home and Benjamin becomes very attached to her as sheteaches him how to play, saying, “It is not how you play buthow you feel about playing.”Meanwhile Benjamin is growing younger. He goes to aparty where he sees a little girl of eight, presumably his ownage, (although he looks like he’s in his 70s) and “loves her fromthe first.” He is given a job by a tugboat captain who wanted tobe an artist, but his father refused to send him to art school,insisting that he continue in the family tugboat business. Sohis artistry is the tattoos on his body. He initiates Benjaminto the screenwriter’s perception of rites of passage into adulthoodby taking him to a bar to get drunk, and to a brothel toconsort with prostitutes, which he enjoys. There he encountershis real father, a rich man who drives up to the brothel inhis limousine. Dad, who runs Button’s Buttons, a prosperousenterprise that his grandfather started during the Civil War,recognizes him but does not let on.As Benjamin gets younger, Queenie feels sorry for him becausehe’ll get to see the people he loves die, and that he does,including his pianist friend. In 1936, Benjamin joins the tugboatcaptain to salvage and repair ships ferrying supplies onthe Murmansk run in the North Atlantic. Before he leaves, hepromises Queenie to say his prayers every night and to writeto her and Daisy. By now Daisy is eighteen and a member ofthe American Ballet Company in New York. After months inMurmansk, he writes Daisy to say that he has found a womanto love and begins an affair with the wife of the British Consul,whose rules for the affair are: (1) Never look at me during theday, (2) We must part before sunrise, and (3) Never say “I loveyou.” At this point in the reading, Caroline asks Daisy if shewants her to continue the story and Daisy says yes because atleast he found someone to keep him warm. (How civilized!)Much of the next few scenes are of the romance, until the affairends abruptly on the evening of December 7, 1941, whenhis paramour doesn’t come down for their nightly rendezvous.The tug is commissioned by the U.S. Navy, and after enteringthe war zone, is sunk. The captain dies, but not before helaments how his body art (his only pride and joy) has beendevastated and utters a line that will recur when Benjamin’sfather dies: “You can be as mad as a mad dog at the way thingswent. You can swear and curse the fates, but when it comes toTaraji P. Henson as Queenie in The Curious Case of BenjaminButton. Photo credit Warner Bros. Pictures and Paramount Picturesthe end, you have to let go.”After the war, Benjamin meets Daisy in New Orleans butwhen he refuses to have sex with her during her brief stay, sheis angry and returns to New York. Benjamin’s dying father reconnectswith him and leaves him the Button factory and considerablewealth, which Benjamin uses to help Queenie andher home. He then goes to New York to see Daisy perform inthe ballet scene in Carousel, hoping to sweep off her feet, butshe snubs him. Later, on a world tour in Paris, Daisy sustains adevastating accident that Benjamin describes like the cascadeof events leading to medical catastrophes, 1 as he cataloguesthe timing of a series of seemingly unrelated circumstancesinvolving a number of disparate people that led to Daisybeing run down and having her leg crushed. As he notes,“Sometimes we are on a collision course and we just don’tknow it, whether by accident or design, and there is nothingwe can do about it.” He flies to Paris, but Daisy sends him awaybecause she doesn’t want him to see her as she is. Finally, theyget together and there are a number of scenes of them havingsex. Daisy opens a dance studio and after they have a “normal”child, she worries that she is getting older while he is gettingThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 39
The physician at the moviesyounger, and that he will tire of her. He denies this and tellsher, “You can’t be perfect forever.” (I didn’t know anyone everis perfect.) However, he decides after a few years that he can’tbe a doting father because he’s growing younger and doesn’twant Daisy to have the burden of another child. He cashes inhis possessions, leaves the money to Daisy and the child, andgoes off to an ashram in India, which again makes no sense.He finally comes back to see the child. Although Daisy is happilymarried, she can’t resist one more bout of sex with BradPitt (oops, excuse me, Benjamin Button) who then completeshis life journey and the story ends as Katrina hits.The Fitzgerald story is much different. 2 Set in Baltimoreinstead of New Orleans, it has a more medically interestingopening as the father runs to the Maryland Private Hospital forLadies and Gentlemen where he is treated rudely by a DoctorKeene who is on his way home and is worried about howthe baby he just delivered will affect his reputation. Button,who had dreams of a strapping boy whom he would sendto Yale, runs into the hospital where the nurses are terrifiedwhen he tells them his name. Finally, he is led to the “cryingroom” where he sees “wrapped in a voluminous blanket, andpartially crammed into one of the cribs (with his legs hangingover the side), an old man apparently seventy years of age. Hissparse hair was almost white, and from his chin dripped a longsmoke-colored beard, which waved absurdly back and forth,fanned by the breeze coming in at the window.” 2 Althoughthe mother survives, we don’t hear more of her. The father,who is devastated and wondering what Baltimore society willsay about his son, goes off to get him a suit to take him home.They age together in different directions.At eighteen, Benjamin passes the entrance exam to Yale butis thrown out when the registrar sees that he looks fifty yearsold. When the Yalies hound him to the station for his returnhome, he vows to take it out on Yale by going to Harvard. Heworks for his father and the company prospers. When he looksfifty (actual age about twenty) he sees an eighteen-year-oldwith whom he falls in love. She marries him against her parents’wishes and to the opprobrium of society. She tolerates hisdesire to stay at home rather than go out dancing. They have ason, Roscoe, and get along well until she gets to be thirty-five,about his age, and he becomes attracted to younger women.He wants to go out, but his wife does not and they drift apart.The Spanish-American War allows him to leave home and hegains a brevet general’s rank after charging up San Juan Hillwith Teddy Roosevelt. On his return, he and Roscoe, whograduates from Harvard, get along well and Benjamin turnsthe business over to him. During the next ten years, the nowtwenty-something father becomes young and frisky and hisson, now part of Baltimore society is embarrassed. Roscoeagrees to send Benjamin off to Harvard where he joins thefootball team in his first year scoring “seven touchdownsand fourteen field goals” to crush Yale. He becomes a legendbut as he goes through his four years, his skills decay. Aftergraduation, he goes home and pleads with Roscoe, who isunhappy with him, to send him to St. Midas, a prep schoolfor Yale, but he is refused. When America enters World WarI, he receives a letter re-commissioning him as a general buthe is summarily kicked out of Camp Mosby in South Carolina,because he is now a callow youth. He ultimately ages down tobabyhood and his nanny cares for him until he departs thisworld.As you can see, this story is thin gruel for a feature-lengthmotion picture even though it makes more sense than what wesee on the screen. The changes in the story are legion, includingthe setting in pre-Katrina New Orleans, the clockmaker,Armistice Day, the size of the baby in the hospital, the motherdying, the father abandoning the baby, the black couple, thenursing home, the tugboat captain, the house of prostitution,the profanity, Murmansk and the affair, World War IIscenes, Daisy being a ballet dancer and her world tour withthe American Ballet, the daughter, his going to India and thereturn to the home, and finally their last sex scene togetherand all the sex scenes for that matter. This does not count thelarge number of goofs and anachronisms in the film, detailedon the Internet Movie Database (IMDB) website (imdb.com).One wonders if F. Scott Fitzgerald is turning over in his graveat the major surgery on his story or just happy that his estateis getting some residuals.References1. Mold JW, Stein HF. The cascade effect in the clinical care ofpatients. N Engl J Med 1986; 314: 512–14.2. Fitzgerald FS. The Curious Case of Benjamin Button andOther Jazz Age Stories. Penguin Books: New York; 2008.Taking ChanceStarring Kevin Bacon.Directed by Ross Katz. Running time 77 minutes.Based on the true story of a dead Marine’s voyage homefrom Iraq to Wyoming, this beautifully-rendered andremarkably apolitical film is both somber and important. Itopens with a black screen as we hear the voices of Marines onpatrol in Ramadi. A suspicious vehicle is spotted approachingthe convoy at a high speed. All of a sudden there’s an explosion,followed by the firing of machine guns, mortars, andgrenade-launchers. Chance Phelps, a Pfc. (promoted posthumouslyto Lance Corporal), is riding shotgun, his favorite position.He had insisted on going on the patrol, even though hewas not scheduled to do so. Refusing to take cover, he drawsthe enemy fire to himself by rapidly firing his machine gun,thereby protecting the rest of the convoy. While being evacuated,he sustains a head wound and dies. The film follows the40 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
transport of his body to Ramstein Air ForceBase in Germany and on to Dover Air ForceBase in Delaware, where the loving caretaken by the workers in the mortuary and allthe support services is quietly evinced.What makes this journey different fromthose that have occurred over 3,500 timesis the nature of the person who volunteersto transport the body. An officer is not usuallyassigned to escort an enlisted man, butLieutenant Colonel Michael R. Strobl (KevinBacon), in reviewing the casualty reports,notes that Chance enlisted in Strobl’s hometownof Clifton, Colorado, and so volunteersto take Chance home. The trip is importantto Strobl, who had fought in OperationDesert Storm and now is on his second officeduty assignment tour, which he soughtbecause he wanted to stay with his wife andchildren. He feels guilty for not being in Iraqfighting alongside his fellow Marines.The screenplay was based on Strobl’s actionreport. Usually, such reports are fairlystraightforward bare-bones accounts of thetrip and issues that occurred. The reportsare designed to help others do things better:making sure that maps of the destinationand cell phone chargers are available, forexample. However, probably because of whatthe trip meant for him, Strobl was alert toeverything that transpired and was taken byhow he and the casket containing Chance’sbody were treated along the way. The resultwas a twenty-page report that was subsequentlyauthorized to be circulated to thefamily as well as his comrades in arms andlater appeared on the Internet, where it cameto the filmmakers’ attention.The film shows the amazing stylized ritualof the journey as the Marine and hisescort are treated with dignity, honor, andrespect at all points, starting at the mortuary where techniciansclean Chance’s body, fit him for a new uniform, eventhough the casket will be closed because of the severe injuries,and clean his few effects: a Saint Christopher’s medal hisGrandma gave him, which he was wearing that Good Fridayin 2004 when he was killed; his dog tags; and his watch, stillon Iraq time. As the casket is about to be loaded into thehearse for transport to the airport, a technician says, “It wasmy privilege to care for him.” Strobl is accorded respect bythe airlines agents, including a flight attendant who giveshim a small crucifix. Later, he gives it to Chance’s mother,for whom he feels it was intended. She places it on the casketKevin Bacon in Taking Chance. Photo credit James Bridges/HBO.before it is lowered into the ground. Also beautifully shownis the reverence of the baggage handlers in loading the casketin Philadelphia and unloading it in Minneapolis, where Stroblmeets another Marine escorting a body and learns that theescort is the Marine’s brother, whose family is meeting themat the airport.Strobl elects to stay with the body in an airport hangar duringthe layover rather than go to a hotel. The respect by airportpersonnel and passengers continues in Billings, Montana,and then by passing motorists on the long drive to Dubois,Wyoming, where the family had moved. There are some movingscenes as Strobl meets with Chance’s divorced parents,The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 41
The physician at the moviesKevin Bacon as Lt. Col. Michael Strobl and Noah Fleiss as Army Sergent in Taking Chance. Photo credit James Bridges/HBO.his stepfather, and sister, as well as the veterans at the VFWHall. One very close friend blames himself for Chance’s deathand wonders what he could have done differently. The answer,which is difficult to accept, is nothing, but it mirrors the guiltfelt by Strobl. In an exchange with a VFW member, Stroblcastigates himself saying, “I was trained to fight. I’m not overthere. I’m not a Marine.” The man brings him up short saying;“You brought Chance home. You were his witness.” The DVDhas some excellent special features involving fellow Marines,some of whom give up their leaves to be with the Phelps familyon Memorial Day. The mother feels like she gained sons andthe feeling is mutual.Chance is described as always getting into trouble; hismother said that being his mom was a challenge. Everyoneagreed that he was the type of kid whose ever-present smilewould defuse a situation or help him escape punishment aftersome wrongdoing. He reveled in doing things that nobodyelse wanted to do. Chance was a good athlete and was beingscouted in high school by major league teams becauseof his ninety-four-mile-an-hour fastball. His father was disappointedwhen he passed up that opportunity and appliedto the Marines after 9/11, but Chance said that was what healways wanted to be. Being underage at seventeen, his parentshad to approve his enlistment. Despite his mother’s beingagainst it, she went along and said that she did not regretdoing so. He thrived in boot camp, as he continued to be afun-loving guy who touched many of his platoon members’lives. As his platoon leader said, “He died a hero. More importantly,he lived a hero. It may sound ironic but if the worldhad more people like Chance Phelps, there wouldn’t be a needfor a Marine Corps.” A Marine training camp mess hall isdedicated to him, which his sister said was fitting because heloved food. As for the film, Chance’s father, a Vietnam veteranwho placed his medals on the casket, said it best; it’s good forAmericans to know Chance’s story “no matter whether you’reantiwar or pro-war.”Addendum: A posting on the film’s IMDB website notesthat two of the most dramatic scenes were not in Strobl’sreport: he slept in a hotel as is usual and not the hangar, andthere was no mention of a Marine escorting his dead brother.These may have been Hollywood inventions; even had theybeen deleted, it would not have lessened the thrust and impactof the film.Dr. Dans (AΩA, Columbia University College of Physicians andSurgeons, 1960) is a member of The <strong>Pharos</strong>’s editorial board andhas been its film critic since 1990. His address is:11 Hickory Hill RoadCockeysville, Maryland 21030E-mail: pdans@comcast.net42 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
TheChallengeBeep!A ten dollar clock whinesAs ambient light shinesExhausted eyes, weary brainIn the moment, break the chainWhiz!An aging projector chidesAs one studies Netter’s guidesSore bum, a cephalic veinIn the moment, break the chainPop!A cadaver’s joint criesAs a classmate grows wiseFormaldehyde, lab coat stainIn the moment, break the chainSizzle!An enticing TV-dinner singsAs eyes glaze over meaningless thingsCalming bike rides, little strainIn the moment, break the chainSigh!A worn medical student groansAs mind stretches on carpal bonesWandering thoughts, barely saneIn the moment, break the chainCreak!A tempting bed selfishly protestsAs sleep comes without care ofsuccessDistracting dreams, efforts drainIn the moment, break the chainDavid DeWittMr. DeWitt is a member of the Class of 2012 atthe Sanford School of Medicine at the Universityof South Dakota. This poem won honorable mentionin the 2009 <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong> <strong>Pharos</strong> PoetryCompetition. Mr. DeWitt’s e-mail address is: dave.dewitt@gmail.com.Illustration by Jim M’GuinnessThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 43
Reviews and reflectionsDavid A. Bennahum, MD, and Jack Coulehan, MD, Book Review EditorsThe Picture of Health: A Viewfrom the PrairieEssays by Richard P. Holm, MD, andphotographs by Judith R. Peterson, MDSouth Dakota Agricultural HeritageMuseum Press, Brookings, SouthDakota, 2008Reviewed by John A. Trotter, PhDThe major themes of this collectionof essays by Richard Holm andphotographs by Judith Peterson includethe importance of humility in dealingwith the world and the people in it, deeplistening to understand the world andthe people in it, and taking the time toreally hear what is being communicatedby the world and the people in it.These precepts apply to doctors intheir treatment of patients, to parents intheir relationships with their children,and to people in any kind of relationships.They might also be said to applyto photographers who seek to producepictures that convey their authenticresponses to the visual world.The three essays at theend of the book, whichwere written as editorialsfor the Journal ofthe South DakotaMedical Association during Dr. Holm’stenure as president of that organization(2001–2002), are the most completestatements of these themes and, unlikethe essays that accompany individualphotographs, were written primarily fora physician audience. They are intendedas cautionary tales and give the reader apretty clear picture of Dr. Holm’s characterand beliefs.In “Hobbit Lesson” the message isthat power corrupts: “and today, ourprofession in particular can bring outthe worst in people.” Using the writingsof Tolkien as his point of reference,Holm urges doctors not to wear thering of power, but rather to understandthat “it is a privilege to have a job thatprovides the opportunity to be of suchservice to people,” “Let us all, each andevery one of us, never forget the darkand evil lure of the ‘ring’ of power . . .and may the humility of the Hobbit bealways at our side to protect us.”In “Who Makes the Best Doctor?”the author argues that the metricscommonly used to measure physicianperformance are seriously flawed.Outcomes measured in terms of adherenceto protocols, cost of care, andpatient satisfaction, are, he argues, bothinternally inconsistent and (intentionallyor unintentionally) exclude the mostimportant components of physicianperformance: “I submit that the mostimportant characteristics of an idealdoctor are immeasurable! What aboutthe mysterious internal thing that drivesa doctor to continuously learn throughouta lifetime? How about the intuitivetalent of an older doctor and thewisdom that comes from experience?How can you calculate levels of honesty,patience, and compassion?” He drawslessons from two studies of diagnosticperformance. These studies indicatedthat the most accurate determinationsof the presence or absence of “nodules”in artificial breast models were madeby those who took the longest time tomake the examinations, and in internalmedicine cases, “80 percent of the correctdiagnoses came from the ‘history’(listening to the patient’s story), 15 percentfrom the exam, and 5 percent fromtesting.” Dr. Holm feels that “somewherein this analysis of time and listening isa very key component of that elusiveobjective we are searching for calledquality.”In “The Elephant Stake” Dr. Holmasks, “Why is it that we have this overwhelmingand paralyzing fear of sufferingand death in this country?” Hisanswer: “I believe one reason is thatmodern medicine has given all of usa false sense of security.” He argues aswell that parental protection of childrenfrom any experience of death has contributedto the impossible belief thatmedicine can prolong life indefinitelyand prevent any and all forms of suffering.He asks physicians to becomeexperts on death and dying in orderto “untether” from the fear of death.“Drop[ping] the fear of death [will allowus to] revel in the bright beautiful daywe have before us.”The brief essays that constitute themain section of the book were originallywritten as editorials to be readon a weekly program on South DakotaPublic Television. The series, which wasentitled On Call, featured one or morephysician experts each week, who presentedon a medical topic, followed byDr. Holm’s commentary. It is importantto understand this because, if the essaysseem incomplete in themselves, that isbecause they are missing the materialon which they were intended to providecommentary. It also helps to realize thatthe editorials were intended for oralpresentation. These mini- essays are full44 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
of homey advice. For example:“Check your own blood pressure regularlyand do what is necessary to keepit under control.”“Eat 40 percent less, live 40 percentlonger.”“We must end the cycle of domesticviolence. It has to do with giving awaycontrol of another person and takingcontrol of oneself.”“With help and the right medicineyou can say, ‘Out, out, damn obsession.’ ”“Those in medicine have ancientand modern promises to keep, and youshould expect no less.”“All of us can help bring to an endthis compulsion. We need to hold twohands out to those who abuse or mayabuse, say ‘never more,’ and may thehealing power of forgiveness (the mosteffective medicine) fill our veins, sweepthrough our bodies, and find its way toour hearts.”The editorials cover a range of topicsand some include interesting historicalfacts. For instance, when Stalin,Churchill, and FDR were dividing uppostwar Europe at the Yalta conference,Churchill was weakened by alcohol, andFDR had a blood pressure of 240/130.Holm asks us to imagine “how the historyof the world would be different hadwe understood then what we know nowabout how to control blood pressure.”Another editorial notes how Pasteur“almost by accident” first observed immunityinduced by vaccination.Each essay includes an accompanyingcolor photograph by Judith Peterson.A striking aspect of this collection ofphotographs is the absence of people.The closest one comes to images ofpeople are the feet clothed by stripedsocks that enter from the bottom of onepicture, a brownish-red footprint, and amotion-blurred photograph of peoplemoving. The absence of people fromthe photographs in a book about humanhealth entitled The Picture of Healthposes an interesting question: how dophotographs that have no people inthem serve to illuminate essays on humanhealth?Despite the absence of people, most(if not all) of the photographs evokeor illustrate the subject of the essaysthat they accompany. For example, thepicture of a rusted chain that accompaniesthe essay on abuse and domesticviolence, the “KEEP RIGHT” signpainted on the street that accompaniesthe “Primer on Medical Ethics,” and theunder-sink drain pipe that accompaniesthe essay on constipation and laxatives.Some of the photographs are cute, likethe one of beaded toy rats that accompaniesthe essay on “Coronary HeartDisease and the Rat.” Some are intendedto convey mystery or meaning throughout-of- focus or motion-blurred imagesaccompanying the essays on psychosis,spirituality in medicine, dreaming, andsports medicine.Most of the photographs did notseem particularly innovative, or exploreunusual dimensions of the subject ofthe essay. There was at least one notableexception, however. The photograph ofthe American Flag blowing in the windthat accompanies the essay on posttraumaticstress disorder is a compellingimage that greatly expands the meaningof the essay. The oversaturated colorsof the almost posterized image are jarring,as is the sense of the flag in chaoticmotion. The composition refuses to bequiet, as the eye is taken back and forthfrom the deep empty space on the rightto the noisy flag on the left. This photographseems to me to be a fully- realizedauthentic response to a troubling aspectof the world we live in.Overall I found this to be a friendlyand encouraging book, although notespecially provocative or deep.Dr. Trotter is Professor of Cell Biology andPhysiology Emeritus and Deputy ExecutiveVice President for Health Sciences at theUniversity of New Mexico Health SciencesCenter. His address is:Health Sciences and Services Building,Suite 3021 University of New MexicoMSC09 5300Albuquerque, New Mexico 87131-0001Christians in the Movies: ACentury of Saints and SinnersPeter E. Dans (Foreword by JosephBottoms)Rowman & Littlefield Publishers, Inc.,Lanham, Maryland, 2009, 348 pagesReviewed by Maria A. Basile, MDBefore medical school, maybe evenbefore college, did you have a friendwho you liked to go to the movies with?Was he (or she) funny, smart, opinionated,fair and insightful, with interestsand tastes close enough to your ownto pick movies you’d both enjoy, butdifferent enough that the conversationafter the movie became the most interestingpart of all? Well, I’ve found yourfriend. His name is Peter E. Dans, andafter reading his book, Christians inthe Movies: A Century of Saints andSinners, I feel like I’ve been to the movieswith him a hundred times.Dr. Dans, a board-certified internist,is associate professor of Medicineat Johns Hopkins School of Medicine.He has shared his love of the cinemaarts on these pages, writing the column“The Physician at the Movies,” for The<strong>Pharos</strong> for more than ten years, andauthoring a similar volume of reviewsentitled, Doctors at the Movies: Boil theWater and Just Say Aah. In that work,released in 2000, Dans explores the waythat movies throughout history haveperpetuated myths and clichés regardingdoctors, and have reflected society’sperceptions of doctors and doctoring,its changing attitudes toward science,and the evolution of issues that still surroundus, unite us, and divide us.The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 45
Reviews and reflectionsIn Christians in the Movies, Dansexamines with the same careful sensibilitythe changing attitudes towardChristians, in many cases Catholics, asreflected in the movies. A true moviebuff, he compiles his impressions ofover 200 films, arranged by decades,from the silent era to the present. Heintroduces each decade with historicalcontext that sheds light on his reviewsof the films that follow.The reviews are peppered with interestingbackstories, adding well researchedand often compelling detailssurrounding the people, production,and themes of these films. It is here thatDans showcases his depth of knowledgeof the American filmmaking industry,his embrace of the social contexts thatshape and drive it, and his inability (likemost doctors I know) to resist a greatstory. Whether he is contrasting “TheReal Scopes Trial vs. Inherit the Wind,”revealing the deep-seated roots of atraumatic Catholic education that led todirector Luis Buñuel’s cinematic attackson the Catholic Church, or tracing “TheTransformation of Nuns from Beautifuland Serene to Weird and Nasty,” Dans’sbackstories are filled with intelligentand informed commentary, languagethat proves generous and fair, and agenuine sense of curiosity that helpsthe reader understand why he wroteChristians in the Movies. The backstoriesare the highlight of this book.In chapter one, “PortrayingChristians in Film,” Dans outlines thetrajectory and purpose of his work,describing the social and political influencethat organized religions andreligious organizations have had on theAmerican movie industry. He introducesthe Motion Picture ProductionCode, adopted in 1930, and the NationalLegion of Decency, established originallyby the American Catholic bishopsand later including many Protestant andJewish clergy. He explores the differingtreatment of Christian groups in societyas reflected in films over the years, culminatingin The Passion of the Christ,produced by Mel Gibson in 2004, whichDans argues served as a Rorschach Testfor American society. Dans ends chapterone with the question, “Why ShouldChristians Care About Their Portrayalin Film?” This is his first call to thereader, in whom he hopes by the end ofthis work to ignite a vision of personaland societal responsibility for the returnof balance in the movies we watch, andin the things we do. “The restoration ofa better movie culture,” he argues, “likethe return of civility and good mannersin everyday life, is our responsibilityboth individually and collectively.”The arrangement of Dans’s reviewschronologically by decade proves a logicaland palatable system for presentingthis encyclopedic work, setting it up asreadable, yet also easily referenced. Hischapter introductions follow the arc ofhis thesis, that the portrayal of Christiansin early films is favorable and reverential,but becomes much less favorable as thetwentieth century winds to a close.Dans’s collection of reviews providesextensive support for his theme. Eachanalysis is bite-sized, just a few paragraphs,including enough plot and detailto identify the film, and enough commentaryto assist the reader in understandingat a glance how the film fitsinto the context that Dans has laid out.Before long, the reader becomes accustomedto Dans’s style of commentaryand trusts him as a reliable reviewer. Heis clear as to what he likes about movies,and proves a sharp critic of work thatfalls short of an informed audience’sexpectations. Reading reviews of moviesI had seen helped me understand myoriginal reactions to the films as I comparedthem to his reactions and framedthem within the questions he has carefullyraised. Really—it was like that conversationat the diner after watching amovie with your friend.Dans makes no claims of being agreat authority on religion or film. Hetries hard not to criticize any givenfilm’s (in)consistencies with biblicaltexts or traditional religious teachings.His casual style of analysis is neverthreatening or pedantic. He discloseshis Catholic upbringing and reminds usof this context in often lighthearted andhumorous ways throughout the book.Make no mistake, however—neither hislove of movies, nor his foundation ofbelief shield him from being offended ascertain movies during the decades fromthe eighties through the present growat first critical and then clearly anti-Catholic (Agnes of God, 1985; Priest,1988); and finally adopt a more dangerousstance, sheer indifference, renderinglost faith as less a tragedy thanan irrelevant annoyance (Dogma, 1999;Chocolat, 2000).Christians in the Movies: A Centuryof Saints and Sinners was a pleasureto read. It should appeal to cinephilesof any faith, and may prove an importantanalysis of how the treatment ofChristians in the movies reflects society’schallenge, as once-revered institutionsmay be vilified, undervalued, anddiscarded. With our leisure time anddisposable funds so limited, and theshift of viewing habits from a night atthe movies with friends to DVD familynights at home, the movie industry isfacing a crisis of its own. This may bea critical time to pick up Dans’s clarioncall to participate in restoring the balance.His backstories can show us why;the chapter introductions explain how.Should this be important to physicians?Only if we sense our own professionalidentity being vilified, undervalued,then discarded, like the church. Onlyif we believe there is balance to be restoredto society’s perception of ourroles, once revered, now increasinglyignored. Only if we still care.Dr. Basile is Clinical Assistant Professorof Surgery and Preventive Medicine at theCenter for Medical Humanities, CompassionateCare, and Bioethics of the StonyBrook University School of Medicine. Heraddress is:HSC Level 3, Room 080Stony Brook University School of MedicineStony Brook, New York 11790E-mail: maria.basile@stonybrook.edu46 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
Letters to the editorSelling Teaching HospitalsThe recent informative review ofJohn A. Kastor’s book, Selling TeachingHospitals and Practice Plans: GeorgeWashington and Georgetown, by PascalJames Imperato, MD, MPH&TM(Summer 2009, pp. 47–48), states thatAppendix A lists six universities whosehospitals are owned by for-profit companies.The University of SouthernCalifornia no longer belongs on thatlist since in 2009 USC UniversityHospital and Norris Cancer Hospitalwere purchased by the University fromTenet.L. Julian Haywood, MD(AΩA, Howard University, 1981)Los Angeles, CaliforniaMedical hand-me-downsAs I was dressing for the beach theother day my wife asked: “How canyou wear those old bathing trunks?They’re full of tears, are shredding, andthe elastic has worn out.” I respondedshortly, “They’ve been my bathingtrunks for many years. I like them andam comfortable in them. So I’m wearingthem.”As we bobbed up and down inthe water, though, I started to thinkmedically (as is sometimes my wont).Specifically I was thinking of a womanI had given an expert opinion on onlythat morning. It was the case of fortyfive-year-oldLetitia, who was applyingfor long-term disability on the basis ofrheumatoid arthritis. The administrativelaw judge, faced with voluminousmedical records, a tearful claimant,and an aggressive attorney (whostood to gain some twenty percentof any awards in favor ofthe claimant) called on meto help him interpretthe records so that hecould evaluate theclaim.I startedwith Day One, some seven years previously.Letitia had had a mild respiratoryinfection, low-grade fever andgeneralized achiness, especially in theneck and shoulders. When it persistedfor a week she saw her primary carephysician who did the usual laboratorytests including a sed rate which was30—the only abnormality. He madethe quite proper diagnosis of probablecommon influenza and, rememberinghis medical school days, and in honorof the mild elevation of ESR, wrote“R.O. rheumatoid arthritis.”Letitia recovered promptly fromthat episode but in the course of thenext two years had brief episodes ofbody aching and each time that ominous“Rule out R.A.” was written. Ayear after that, having moved to a newcommunity and acquiring a differentphysician, she was found on routine examinationto be at risk for osteoporosisand was started on medication. Hergeneral doctor referred her for evaluationto an orthopedist who reviewedher record and referred to her in hisnotes as “with a history suspicious forrheumatoid arthritis.” The next doctordown the line, the gynecologist whoremoved her uterine fibroids, referredto her as a “43-year old woman withrheumatoid arthritis.” During thisentire time her sed rates, CRPs, latexfixations, ANAs, and x-rays of jointshad been entirely within normal limits.However, every time Letitia had anache or a pain she would tell all: “Youknow, it’s because I have rheumatoidarthritis.”When she fell on hard times at ageforty-five she felt even more achy andbecame convinced that she was forevera crippled victim of rheumatoidarthritis, a disease for which there wasnot, and never had been, any evidence.Letitia was the victim of a “hand-medown”diagnosis—words which havebeen carried forth through a medicalrecord without being specificallyrendered invalid.We have all seen countless examplesof this sort of perpetuation of diagnosiswhen it has once been proposed. Theestablishment of “check-mark” sheetsof medical history and findings makeit even easier to perpetuate this mistake.It’s far easier to check the “yes”box when asked if there is a history ofarthritis and to include the code forrheumatoid arthritis for patients likeLetitia that will ensure that this quiteimproper diagnosis follows her andwill be included to the end of her days.Perhaps worse, Letitia may “google”“rheumatoid arthritis” and discovera whole new set of symptoms whichshe may come to believe she has, anda “worst-case” scenario which she cancome to believe is responsible for hernot having a job.How can this be prevented?Especially in the modern era of punchboardcharts. There must be a columnfor “diagnosis established with a reasonabledegree of medical certainty,”not just those which have been entertained.This will require the physicianwho makes the check-marks to actuallythink (remember that?) about whetherthe evidence really establishes reasonablemedical certainty. Letitia shouldhave been told years ago that she surelydoes not have rheumatoid arthritis; shewould then probably not have developed“google symptoms.”As with everything in medicine,however, we should not throw out thebaby with the bath water. I remembercoming as a visiting professor to a largemunicipal hospital and being presentedwith a middle-aged male patient whohad been in the teaching hospital forover a year but remained a diagnosticpuzzle. His voluminous recordsincluded lengthy notes from successivegenerations of medical students,interns, residents, attendings, andconsultants (who included all classes ofinternists, neurologists, dermatologists,The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 47
OF ALPHA OMEGA ALPHA HONOR MEDICAL SOCIETY Summer 2009Lettersvascular and other surgeons, andnurse-practitioners). I, too, was puzzledby this man who was obviouslychronically ill, had a non-characteristicrash, non-specific cardiac findings,rather severe neuropathy which wasnon-diabetic, and depression. I lookedover the lengthy record and found agreat many diagnoses having beenproposed and many carried forwardas “hand-me-downs.” I then went backto the very first record, written bya fourth-year student and obviouslygiven short shrift, who made the diagnosisof “Hansen’s Disease.” No one,unfortunately, had carried this downand thus this unfortunate man withleprosy had remained undiagnosed.Charles M. Plotz, MD, MedScD(AΩA, SUNY Downstate, 1968)Emeritus Professor of MedicineBrooklyn, New YorkI get nervous when I receive a largePriority Mail envelope. That is, until Irecall that a subpoena must be deliveredin person. When I opened the bigenvelope yesterday and saw the coverof The <strong>Pharos</strong>, my immediate reactionwas, “No, it’s not possible.”Well, of course, it was not only possible,it was true. I have always admiredthe publication for its brilliant editingand for its oustanding artwork. For thislongtime bar poet, whose oeuvre isusually submitted in blue ballpint penon a stack of cocktail napkins, to be therecipient of such elegance—well, it’soverwhelming. No, truly. The feelingis quite like that I experienced the daythat I was told I had been elected toAΩA. These are honors quite considerable.And more than a little moving.Robert L. Chesanow, MD(AΩA, Washington University in St.Louis, 1975)Cheshire, ConnecticutAccelerating humanevolution??I will agree that human behavior hasevolved—at times for the better and attimes for the worse. However, I do notthink that humans or human naturehave evolved at all. To me evolutionwould refer to changes in the geneticcode that would alter the human whohad it. I do not beliefve that we humanshave evolved to suit our current societyand economy. I sometimes think thatwe have cancelled survival of the fittestand promoted survival of the less fit.Do I think the use of chemicals to enhancebrain funciton is a good thing?No, I do not. Show me the data.Treatment of malfunction of brainchemicals is a different matter. Alterationof those chemicals in cases of bipolardisease, depression, obsessive-compulsivedisorder, or maybe schizophrenia certainlyare needed. By definition no morethan fifty percent can be above average.Granted it would be desirable to havemore people better educated and moreable to use their abilities to the maximum.It is my view that we have too many relyingon drugs rather than using commonsense and good judgment.Donald W. Bales, MD(AΩA, University of Tennessee, 1946)Kingsport, TennesseeI read with interest the editorialby Dr. Harris in the recent issue ofThe <strong>Pharos</strong> (Summer 2009, p. 1) assertingthat human evolution is beingaccelerated by both modern medicalinterventions and cognition-enhancingdrugs. Perhaps my knowledge is incomplete,but I fail to see how eithercould produce the genetic change and/or selection required for real evolution.Longevity, as produced by dialysis (orany other late-life intervention), has noconnection to the genetic variation thatwould lead to a naturally longer life.Likewise, unless drug therapy producesgamete-changing effects (rather thanmere stimulation of neurotransmitters),it is also difficult to link these effects toevolutionary change.Unfortunately, while any interventionafter the reproductive agehas passed is genetically ineffective,medicine has facilitated the survivalof many unfortunate individuals withotherwise fatal defects to an age wherereproduction is possible. Rather thandwell on the sad thoughts that furtherdiscussion of this would unavoidablyproduce, let us agree that the editorialtopic is a difficult one.Now, I would agree that recentmedical advances give the appearanceof evolution; however, the fundamentalsubstance of humanity has languished,deprived of the pressures of selection.Unless (and it may be soon) we canpick and choose genetic material beforebirth, no real evolutionary change ispossible (save perhaps slow regression).So, although the overall message of theeditorial was thought-provoking, theattempt to link the grand themes ofevolution, time, and medical trainingwas less than successful.James Berry MD(AΩA, University of Texas at Houston,1983)Nashville, TennesseeThe right to sueTo Dr. Manganiello’s three prerequisitesto health care reform (Summer2009, p. 43), I would add a fourth: Areform of our country’s medical malpracticelitigation system.The current system promulgates thenotion that someone must be to blame48 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
for every adverse outcome, and encouragesdisproportionately huge plaintiffawards. The resulting enormous cost ofprofessional liability insurance for hospitalsand clinicians must get passedon, at least in part, to the consumer.Health care expenses are also driven upby the performance of countless unnecessarytests, so as to avoid the unlikelybut not impossible chance of missing asignificant diagnosis in a patient withan unremarkable presentation, followedby a medically unsophisticated jurybeing persuaded that the test “should”have been done. In still other instances,a sympathetic jury may simply wish tomake it possible for the plaintiff to receivefunds from the institution, practitioner,or insurance company with thedeepest pockets.It is discouraging, though perhapsnot surprising, that with all the discussionof health care reform in the media,the subject of runaway malpracticelitigation and its effect on health carecosts gets glossed over or not mentionedat all. Measures such as placingcaps on awards for damages and painand suffering (which some states havealready done), and the use of impartialexpert physician panels to review caseson their true medical merit could bringdown the cost of health care significantly,making it more affordable forgovernment programs, insurance companies,and private individuals.Before the government tries to figureout how to pay for coverage, let itbe part of the solution by lowering thecost of that coverage—not by decliningpayment for services rendered, but bymaking it less financially burdensomefor physicians and hospitals to practicemedicine. Until this issue is widelydiscussed and ultimately addressed,I fear that attempts at reform will beunsuccessful, and our country’s reputationfor inefficiency in its health caresystem will persist.Jeffrey S. Menkes, MD(AΩA, Yale University School ofMedicine, 1972)Manchester, ConnecticutInformal EducationShe sat alone within her roomBedside roses full in bloomA listless look, a foreign stareLips reciting familiar prayerThe room was bare, clean and whiteAnything but a healing sightWe were strangers in her worldIntimate secrets soon unfurledIn we marched, one by oneHer quiet sanctuary came undoneStudents stood along the wallDetailed health at prompt recallWe looked at her just like a textA detailed case, she’s quite complexHer heart was failing, slow but sureHer trust in us to find a cureHer quiet way, it drew me nearWhat I’d say was yet unclearAs I knelt beside her chairI felt, I knew, her calm despairI peeled away my stethoscopeFeeling ways to help her copeI placed it softly in her earsShe knew not what she would hearThe drum I placed upon her chestAnd in one breath I did confessThe sound she heard, it was her ownHer heart was sick, the beat postponedShe looked down into my eyesHer lips apart, content surpriseA simple tear, a quiet smileMy little gesture well worthwhileMelanie BuskirkMs. Buskirk is a member of the Class of 2011 at Mayo MedicalSchool. This poem won honorable mention in the 2009 <strong>Pharos</strong>Poetry Competition. The author’s address is: 207 5th Avenue SW#408, Rochester, Minnesota 55902. E-mail: buskirk.melanie@mayo.edu.The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 49
alphaomegaalpha.orgThe new <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong> web siteWe invite you to visit our freshly redesigned web site,featuring our new logo. The web site now includes the abilityto search for members by last name, submit programapplications on-line, and much more. We hope you’ll giveit a test drive!Winner of the 2009 <strong>Pharos</strong> Editor’sPrizeThe 2009 <strong>Pharos</strong> Editor’s prize has beenawarded to Terrell Nabseth Stevenson ofthe University of California, San Francisco,Class of 2011, for her essay, “The powerof language in medicine—Case study:Mongolism” (<strong>Winter</strong> 2009, pp. 4–9).Ms. Stevenson tell us: I received myBA from Stanford University in History,with an emphasis on modern Europeanhistory. One of my final research projects, which inspiredmy article in The <strong>Pharos</strong>, was entitled “The Language ofDown Syndrome: The Weight of Language on People withTrisomy 21 from 1866 to the Present.” During the first twoyears of medical school, the amount of science to be learnedwas overwhelming, so I continued to turn to reading andwriting as my creative outlets. I am grateful to discover thatmy interests in history have a valued place in the field ofmedicine, and I look forward to future projects in the historyof medicine.Announcing the <strong>2010</strong> <strong>Pharos</strong> Editor’s PrizeFor the thirteenth year, <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong> is pleasedto offer up to four prizes of $1000, $750, $500, and $250 tothe author(s) of original nonfiction manuscripts publishedin The <strong>Pharos</strong>. Authors need not be members of ΑΩΑ, butmust be forty-five years old or younger as of Decemberof the calendar year in which the paper is submitted. Tobe competitive for a prize, the paper submitted must bein the standard format of The <strong>Pharos</strong> (see Instructions for<strong>Pharos</strong> Authors immediately following), and not publishedpreviously in any form. Content should be in the areas emphasizedby The <strong>Pharos</strong>—medical history and biography,ethics, professional issues, and personal essays. Essays submittedto the ΑΩΑ Helen H. Glaser Student Essay competitionare not eligible for this prize, nor are previous winnersof the Editor’s Prize eligible to compete. All manuscriptsare subject to review of <strong>Pharos</strong> editorial board members.Judging will be on the basis of style and composition, originality,scholarship, and interest and relevance to medicine.50 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
National and chapter newsDr. Francis Neelon joins the <strong>Pharos</strong>editorial boardWe are pleased to announce the appointmentof Francis A. Neelon, MD, tothe editorial board of The <strong>Pharos</strong>.Forty years elapsed between Dr.Neelon’s arrival as an intern at DukeUniversity in 1962, his appointment tothe faculty in Endocrinology and GeneralInternal Medicine, and his retirement in2002. Since retiring from Duke, he has served as medicaldirector of the Rice Diet Program in Durham. He has along interest in how the humanities (particularly literature)enhance life in the practice of medicine. He is a foundingmember of the Osler Literary Roundtable, which has metweekly at Duke for twenty-two years to read and discusspoetry and short fiction. He is a past president of theAmerican Osler Society, and for ten years he served as editorof the North Carolina Medical Journal. Dr. Neelon hasthis to say about his appointment to The <strong>Pharos</strong>:I graduated from medical school having absorbed thepervasive (albeit unvocalized) advice that the goal of “real”medicine is to unravel the secrets of the body well enoughto devise treatments that will forestall or undo the ravagesof disease. Over the course of years since, and in thesteady company of patients, I have come to value the olderwisdom—that the real task of medicine is to find ways tobe helpful to people who are in trouble. Nowadays we areinundated by appeals to let “evidence-based medicine”(largely evidence-based treatment) guide what is best toprescribe for patients with this or that kind of disease. Ihave no problem with guidance in what-to-do; my pitfallis how to get patients to do-what-they-should. Few of thepapers in the medical journals I read help me sort out thedilemmas of doctoring, I suppose because those problemsdo not lend themselves to the abstraction that would permittheir assembly into a scientific paper. That means I rely onthe stories, the poems, the musings, the historical or personalessays that do, sometimes, clarify things. Because The<strong>Pharos</strong> is a bastion of this kind of writing, I have for yearsanticipated its quarterly arrival, even when my copies werehand-me-downs from Harold Godwin. I am delighted nowto be asked to serve on the editorial board; I look forwardto my official association with The <strong>Pharos</strong>.CorrectionThe Autumn issue incorrectly identified the visiting professorat the University of Kansas in 2008/2009. The actualvisiting professor of Dr. Allan R. Fleming of the Universityof Kansas Medical Center.Instructions for <strong>Pharos</strong> authorsWe welcome material that addresses scholarly and nontechnicaltopics in medicine and public health such as history,biography, health services research, ethics, education,and social issues. Poetry is welcome, as well as photograph/poetry combinations. Photography and art may also besubmitted. Scholarly fiction is accepted. All submissionsare subject to editorial board review. Contributors neednot be members of <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong>. Papers by medicalstudents and residents are particularly welcome.Submissions must meet the following criteria:1. Submissions may not have been published elsewhereor be under review by another journal.2. Essays should have a maximum of 15 pages (approximately5000 words), and be submitted in 12-pointtype, double-spaced, with one-inch margins. They shouldbe accompanied by a covering letter and a title page withthe word count (or page count), return address, and e-mailaddress. Papers exceeding the page count noted will bereturned to the author. References should not exceed 20unique items (see below).3. Poems or photograph/poetry combinations should bein 12-point type, with one-inch margins, with the author’sname, address, and e-mail address on the first page.4. Send your submissions to Edward D. Harris, Jr. M.D.,Editor of The <strong>Pharos</strong>, 525 Middlefield Road, Suite 130,Menlo Park, California 94025. You may also e-mail them to:postmaster@alphaomegaalpha.org.5. After peer review, comments on the manuscript willbe sent to the author along with an editorial decision. Everyattempt is made to complete preliminary reviews withinsix weeks.6. The editors of The <strong>Pharos</strong> will edit all manuscriptsthat are accepted for publication for style, usage, relevance,felicity, and grace of expression, and may provide appropriateillustrative material. Authors should not purchaseillustrative material because the editors cannot guaranteethat it will be used.7. In accordance with revised copyright laws, each contributorwill need to sign an Author’s Agreement, whichwill be sent with the edited galleys. Information on copyrightownership and re- publication of articles is detailed inthe Author’s Agreement.Reference informationAuthors are responsible for the accuracy of citationsand quotations in their papers. Once a manuscript hasbeen accepted for publication, therefore, the author willbe required to provide photocopies of all direct quotationsfrom the primary source material, indicating page numbers.(Please mark the quoted material on the photocopies withhighlighter.) In addition, the editors will require photocopiesof all references: the title page and copyright pages of allbooks cited, the first and last pages of book chapters cited,and the first and last pages of journal articles cited, as wellas the Table of Contents of the particular issue of the journalin which the cited article appeared. The foregoing itemsThe <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong> 51
National and chapter newswill be used to verify the accuracy of the quotations in thetext and the references cited, and to correct any errors oromissions. The photocopies will not be returned.References should be double-spaced, numbered consecutivelyin the text, and cited at the end in the followingstandard form:JournalZilm DH, Sellers EM, MacLeod SM, Degani N.Propranolol effect on tremor in alcoholic withdrawal. AnnIntern Med 1975; 83: 234–36.BookHarris ED Jr. Rheumatoid Arthritis. Philadelphia: WBSaunders; 1997.Book ChapterPelligrini CA. Postoperative Complications. In: Way LW,editor. Current Surgical Diagnosis and Treatment, Ninth<strong>Edition</strong>. Norwalk (CT): Appleton & Lange; 1991: pp 25–41.Each reference should be listed in the bibliography onlyonce, with multiple uses of a single reference citing thesame bibliography reference number. Examples are availableat our web site: www.alphaomegaalpha.org.Citation of web sites as references is discouraged unlessa site is the single source of the information in questionor has official or academic credentials. Examples of suchsites are official government web pages such as that of theNational Institutes of Health. Encyclopedia sites such asbritannica.com are not primary references.Leaders in American MedicineIn 1967, as a result of a generous gift from Drs. DavidE. and Beatrice C. Seegal, <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong> initiated aprogram of one-hour videotapes featuring interviews withdistinguished American physicians and medical scientists.The collection has been donated to the NationalLibrary of Medicine, which will maintain it for permanentuse by scholars visiting the library. Videotapes continueto be available for loan from AΩA. A listing of availabletapes can be found on our web site: www.alphaomegaalpha.org,or by contacting Ms. Debbie Lancasterat d.lancaster@alphaomegaalpha.org or (650) 329-0291.Please also contact Ms. Lancaster to borrow tapes. Thosewishing to purchase copies may do so by contacting Ms.Nancy Dosch, manager, Historical Audiovisuals, Historyof Medicine, Building 38, Room 1E-21, 8600 RockvillePike, Bethesda, Maryland 20891. Telephone (301) 402-8818, e-mail nancy_dosch@nlm.nih.gov.SmokeIthought of you the first time I feltlike a medical student—standingat the light board before an x-ray, discussingthe bones in the hand, pointing tothat picture and knowing I would bea doctor now. You smile at me as I attemptto identify every structure my handdrifts over, cradle my head just so on yourchest to hear your heart, trace the musclesin your shoulders when water beads there,diamondlike, transient. They saywe are not just the sum of the parts and Ido not know if you mean more to me now thatI have named each part for you, memorizedeach ponderous and gleaming organ, allthe waxy tendons and tissues like goldleaf, the helix of veins weaving upeach arm. Every structure has become yours,no matter whose name, no matterwhose body on the table. Your pacemakertattoos its message on the EKG, youroxygen decrescendoes on the green monitorbeside me and your unknown pain twistsin my flank alongside yours. Everyone’sagony is yours, and mine as well, andwhen you die, it will be me who killsyou, who lets you die, your face a softsapphire in my small hands, yourwide eyes that flicker and fade outbefore me. I know what will happen andI still have that x-ray to bring youback each time, the ghostly outline thatoutlives us both, the white haze not bone butsmoke, a scorch marked deep into the skin—a sign of damage, of something burning, butalso of life remaining, of something living onto burn.Ashley MannMs. Mann is a member of the Class of 2011 at the University ofMissouri—Kansas City School of Medicine. This poem won first prizein the 2009 <strong>Pharos</strong> Poetry Competition. Ms. Mann’s e-mail address is:aah9pd@umkc.edu.52 The <strong>Pharos</strong>/<strong>Winter</strong> <strong>2010</strong>
Web SitePhotographyContestPurposeTo encourage photography that illustrates AΩA’smotto: “Be Worthy to Serve the Suffering.”PrizesTwelve winning photographs will be selected tobe displayed for one month each on AΩA’s web site:alphaomegaalpha.org. A short description of the photographand its context will be displayed with the photograph.No cash prizes will be awarded.EligibilityOnly amateur photographers. Anyone may participate,except for professional photographers and thoseaffiliated with the AΩA national office operations, includingcontractors, staff, and members of the Board ofDirectors and <strong>Pharos</strong> Editorial Board members.DatesPhotographs must be submitted by e-mail no laterthan February 15, <strong>2010</strong>.Requirements for the photos1. Photos must not have been published elsewhere,and must the work of one person.2. All entries must be submitted by e-mail.3. Only one entry per person is allowed.4. Files must be submitted in JPEG format, and mustbe at least 500 KB in size, and no larger than2 MB.5. Files must be uncropped and generally unedited(except for brightness, contrast, and color balance).Conversion of color photos to black andwhite is allowed.6. Photographs must be in landscape orientationand must be able to be cropped to fit thedimensions of the photograph on AΩA’s homepage.7. Each photograph must be accompanied by thephotographer’s name, address, telephone number,e-mail address, and a description of thephoto of less than 100 words.8. Photographs must adhere to HIPAA regulations.9. The photographer of a winning photographmust sign a release allowing <strong>Alpha</strong> <strong>Omega</strong><strong>Alpha</strong> the sole right to display the photographfor a period of one year. Copyright remainswith the photographer.10. Send entries to info@alphaomegaalpha.org.All e-mails must have the subject: AOA WebSite Photography Contest.More informationContact Managing Editor Debbie Lancaster at(650) 329-0291 or info@alphaomegaalpha.org.
Handsome)and)elegant,on)of)AOA<strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong> necktie or bowtieFashioned from fine silk by Vineyards Vinesof Martha’s Vineyard, Massachusetts.Necktie, $45.00Bowtie (freestyle), $38.00To order, send a check to<strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong>525 Middlefield Road, Suite 130Menlo Park, California 94025Or order online atwww.asphaomegaalpha.org/store(Price includes shipping and handling)