Assessment of NTproBNP Concentration in Dogs - IDEXX ...
Assessment of NTproBNP Concentration in Dogs - IDEXX ...
Assessment of NTproBNP Concentration in Dogs - IDEXX ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
SMALL ANIMALS/EXOTICN-term<strong>in</strong>al pro-B-type natriuretic peptide is a cardiacbiomarker that is <strong>in</strong>creased <strong>in</strong> the blood <strong>of</strong> dogswith heart disease. 1,2 N-term<strong>in</strong>al pro-B-type natriureticpeptide is formed when its parent pro-hormone, pro-B-type natriuretic peptide, is cleaved <strong>in</strong>to 2 molecules,NT-proBNP and C-BNP. The pro-B-type natriuretic peptideis produced <strong>in</strong> response to an <strong>in</strong>crease <strong>in</strong> <strong>in</strong>tracardiachydrostatic pressure, <strong>in</strong>creased cardiac wall stress,angiotens<strong>in</strong> II, myocardial hypoxia, and heightenedsympathetic tone. 3 As such, both serum NT-proBNPand C-BNP concentrations represent potential diagnostictools to help diagnose congestive heart failure. 4,5 Inhumans, C-BNP 6–8 and NT-proBNP 9–11 assays possesshigh sensitivity and specificity <strong>in</strong> differentiat<strong>in</strong>g betweencardiac and pulmonary causes <strong>of</strong> respiratory distress.In circulation, C-BNP is rapidly degraded, 12 mak<strong>in</strong>glaboratory test<strong>in</strong>g difficult. Commercially availabletests <strong>in</strong> dogs and cats exclusively detect NT-proBNP,which is thought to possess a longer half-life.Results <strong>of</strong> a previous study 1 <strong>in</strong>dicate that dogs withrespiratory signs result<strong>in</strong>g from congestive heart failurehave significantly higher serum NT-proBNP concentrationsthan dogs with primary respiratory tract disease.The magnitude <strong>of</strong> difference between the 2 populationswas such that the serum NT-proBNP concentration provideda cl<strong>in</strong>ically useful test with an adequate sensitivityand specificity for differentiat<strong>in</strong>g between the 2 populations.However, all dogs did not undergo the sameset <strong>of</strong> diagnostic tests, and a substantial proportion <strong>of</strong>the study population lacked both evaluation <strong>of</strong> thoracicradiographs and an echocardiographic exam<strong>in</strong>ation.Thus, the usefulness <strong>of</strong> this peptide as an adjunct diagnostictest merits closer evaluation. We hypothesizedthat serum NT-proBNP concentration would be higher<strong>in</strong> dogs with congestive heart failure than <strong>in</strong> dogswith primary respiratory tract disease and that serumNT-proBNP concentration would help to differentiatebetween cardiac and noncardiac causes <strong>of</strong> respiratorysigns <strong>in</strong> dogs. The purpose <strong>of</strong> the multicenter studyreported here was to assess the cl<strong>in</strong>ical sensitivity andspecificity <strong>of</strong> a serum NT-proBNP assay to differentiatebetween cardiac versus noncardiac (ie, primary respiratorytract disease) causes <strong>of</strong> respiratory signs, and todeterm<strong>in</strong>e an optimal cut<strong>of</strong>f value that would facilitatethis assessment.Materials and MethodsAnimals—Study procedures were approved by the<strong>in</strong>stitutional animal use and care committees <strong>of</strong> eachqualify<strong>in</strong>g participat<strong>in</strong>g <strong>in</strong>stitution. Owner consent wasobta<strong>in</strong>ed for all dogs <strong>in</strong>cluded <strong>in</strong> the study. Fourteenveter<strong>in</strong>ary cardiology practices prospectively recruiteddogs between September 2006 and November 2007.<strong>Dogs</strong> were eligible for <strong>in</strong>clusion if the owner reported acompla<strong>in</strong>t <strong>of</strong> respiratory signs that were severe enoughto affect the dog’s quality <strong>of</strong> life. Qualify<strong>in</strong>g signs <strong>in</strong>cludedcough<strong>in</strong>g, stertor, stridor, excessive pant<strong>in</strong>g,<strong>in</strong>creased respiratory effort, tachypnea, or overt respiratorydistress. <strong>Dogs</strong> were excluded if respiratory signswere caused by obvious trauma (eg, vehicular trauma).<strong>Assessment</strong> <strong>of</strong> disease—All dogs underwentthoracic radiography and M-mode, 2-D, and Dopplerechocardiography. Vertebral heart size was measuredon the left or right lateral radiographic projection <strong>of</strong>the thorax by the attend<strong>in</strong>g cardiologist as previouslydescribed. 13,14 Additional diagnostic test<strong>in</strong>g to help determ<strong>in</strong>ethe underly<strong>in</strong>g cause <strong>of</strong> the respiratory signs(eg, fluoroscopy, tracheal wash, and bronchoscopy)was performed at the discretion <strong>of</strong> the attend<strong>in</strong>g cl<strong>in</strong>ician.The LVIDd, LVIDs, and LA:Ao were measured bymeans <strong>of</strong> standard echocardiographic techniques. 15,16Detection <strong>of</strong> tricuspid regurgitation by use <strong>of</strong> echocardiographywas recorded. Pulmonary hypertension wasarbitrarily def<strong>in</strong>ed as a velocity <strong>of</strong> tricuspid regurgitation> 3.25 m/s (pressure gradient > 42.3 mm Hg). Inthe absence <strong>of</strong> tricuspid regurgitation, a presumptiveechocardiographic diagnosis <strong>of</strong> pulmonary hypertensionwas made <strong>in</strong> dogs with a comb<strong>in</strong>ation <strong>of</strong> severeright ventricular hypertrophy or dilation, flattened<strong>in</strong>terventricular septum, and an enlarged ma<strong>in</strong> pulmonaryartery, <strong>in</strong> the absence <strong>of</strong> <strong>in</strong>creased right ventricularto pulmonary artery outflow velocity.A standardized patient datasheet was used to recordpatient signalment, cl<strong>in</strong>ical signs, and diagnosticf<strong>in</strong>d<strong>in</strong>gs. On the basis <strong>of</strong> this workup, and withoutknowledge <strong>of</strong> the NT-proBNP assay results, a boardcertifiedveter<strong>in</strong>ary cardiologist assigned the dog to 1<strong>of</strong> 4 groups as follows: group 1 <strong>in</strong>cluded dogs with congestiveheart failure (f<strong>in</strong>d<strong>in</strong>gs <strong>of</strong> severe cardiac disease,perihilar or caudodorsal pulmonary <strong>in</strong>terstitial pattern,cardiomegaly, enlarged pulmonary ve<strong>in</strong>s, pleural effusion,and ascites) and without primary respiratory tractdisease; group 2 <strong>in</strong>cluded dogs with primary respiratorytract disease (parenchymal lung disease [f<strong>in</strong>d<strong>in</strong>gs<strong>of</strong> cranioventral or lobar alveolar pattern, lung lobe torsion,and bullae] or upper airway disease [f<strong>in</strong>d<strong>in</strong>gs <strong>of</strong>laryngeal paralysis, brachycephalic syndrome, collaps<strong>in</strong>gtrachea, and moderate or severe bronchiolar pulmonarypattern]) and without underly<strong>in</strong>g cardiac disease(no heart murmur and no evidence <strong>of</strong> cl<strong>in</strong>ically relevantleft-sided cardiac disease on echocardiography); group3 <strong>in</strong>cluded dogs with primary respiratory tract disease(as described for group 2 dogs) that also had heart diseasethat was not congestive heart failure (detection <strong>of</strong>heart murmur or cardiac disease on echocardiographywithout evidence <strong>of</strong> congestive heart failure on thoracicradiography, physical exam<strong>in</strong>ation, or other diagnostictests); and group 4 <strong>in</strong>cluded dogs for which the etiology<strong>of</strong> respiratory signs could not be reliably ascribedto either respiratory tract disease or congestive heartfailure.Measurement <strong>of</strong> serum NT-proBNP concentration—Venousblood samples were collected at the time<strong>of</strong> admission. Blood was drawn <strong>in</strong>to pla<strong>in</strong> evacuatedglass tubes that did not conta<strong>in</strong> any additives. Sampleswere centrifuged with<strong>in</strong> 60 m<strong>in</strong>utes after collection,and serum was stored at –20°C prior to batched overnightshipment for analysis. Samples were shipped withcold packs and pack<strong>in</strong>g materials provided by the assaymanufacturer. Serum NT-proBNP concentration wasdeterm<strong>in</strong>ed with a commercially available can<strong>in</strong>e-specificNT-proBNP assay a as previously described. 2Statistical analysis—Data were summarized asmedian (IQR [ie, 25th to 75th percentile]) or mean ±1320 Scientific Reports JAVMA, Vol 235, No. 11, December 1, 2009
SD. Multiple group comparisons <strong>of</strong> radiographic, echocardiographic,and NT-proBNP data were performed viaKruskal-Wallis analysis and the Dunn multiple comparisontests. The Spearman method was used to test forcorrelations between serum NT-proBNP concentrationand body weight, age, and radiographic and echocardiographicheart size. Multivariate l<strong>in</strong>ear regression wasperformed to identify whether these variables were associatedwith serum NT-proBNP concentration; cut<strong>of</strong>fP values for entry <strong>in</strong>to and removal from the multivariatemodel were < 0.05 and > 0.10, respectively. Receiver-operat<strong>in</strong>gcharacteristic curves were constructed todeterm<strong>in</strong>e the sensitivity, specificity, positive and negativepredictive values, accuracy (def<strong>in</strong>ed as the sum <strong>of</strong>the concordant results divided by the sum <strong>of</strong> all results<strong>in</strong> a 2 X 2 table), and AUC ROC<strong>of</strong> NT-proBNP results,compared with the cardiologist’s diagnosis. All analyseswere performed with standard s<strong>of</strong>tware. b,c Values <strong>of</strong> P
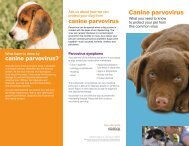
SMALL ANIMALS/EXOTICFigure 1—Box and whisker plot <strong>of</strong> serum NT-proBNP concentration<strong>in</strong> dogs <strong>in</strong> which the etiology <strong>of</strong> respiratory signs is congestiveheart failure (group 1; n = 62), primary respiratory tract disease(group 2; 21), and respiratory tract disease with concurrentheart disease (group 3; 27). For each plot, the box representsthe IQR, the horizontal l<strong>in</strong>e <strong>in</strong> the middle <strong>of</strong> the box representsthe median, and the whiskers denote the range extend<strong>in</strong>g to 1.5times the IQR from the upper and lower quartiles. Outlier valuesbetween 1.5 to 3.0 times the IQR are denoted as squares. *Significantly(P < 0.005) different from value for group 1 dogs.Tricuspid regurgitation was detected <strong>in</strong> 34 (34/62[55%]), 5 (5/21 [24%]), and 18 (18/27 [67%]) group1, 2, and 3 dogs, respectively. A diagnosis <strong>of</strong> pulmonaryhypertension was made for 16 (16/62 [26%]) group 1dogs (mean ± SD tricuspid regurgitation velocity, 3.78± 0.49 m/s; n = 16), 7 (7/21 [33%]) group 2 dogs (4.69± 0.89 m/s; 5), and 5 (5/27 [19%]) group 3 dogs (4.27 ±0.60 m/s; 5). Median (IQR) serum NT-proBNP concentration<strong>in</strong> group 2 dogs with pulmonary hypertensionwas significantly (P = 0.002) higher than <strong>in</strong> group 2dogs without pulmonary hypertension (1,028 pmol/L[559 to 1,829 pmol/L] vs 309 pmol/L [196 to 461 pmol/L], respectively). In contrast, median (IQR) serum <strong>NTproBNP</strong>concentration <strong>in</strong> group 1 dogs with pulmonaryhypertension was not significantly (P = 0.41) higherthan <strong>in</strong> group 1 dogs without pulmonary hypertension(2,078 pmol/L [1,484 to 3,071 pmol/L] vs 2,541 pmol/L [1,539 to 3,141 pmol/L], respectively). Also, median(IQR) serum NT-proBNP concentration <strong>in</strong> group 3 dogswith pulmonary hypertension was not significantly (P =0.81) higher than <strong>in</strong> group 3 dogs without pulmonaryhypertension (478 pmol/L [348 to 1,616 pmol/L] vs504 pmol/L [301 to 1,107 pmol/L], respectively).Univariate regression analysis revealed that serumNT-proBNP concentration was significantly but poorlycorrelated to body weight (r = 0.21; P = 0.029), VHS(r = 0.55; P < 0.001), LVIDs <strong>in</strong>dexed to body weight(r = 0.27; P = 0.021), and LA:Ao (r = 0.61; P < 0.001).Multiple regression analysis revealed that only LA:Ao(β coefficient = 757.9; P < 0.001) and VHS (β coefficient= 218.3; P = 0.043) were correlated with serumNT-proBNP concentration.Figure 2—The ROC curve display<strong>in</strong>g the sensitivity and specificity <strong>of</strong> serumNT-proBNP concentration to dist<strong>in</strong>guish between cardiac and noncardiac(ie, primary respiratory tract disease) as the cause <strong>of</strong> respiratorysigns <strong>in</strong> 110 dogs (solid l<strong>in</strong>e). The 95% CIs are displayed as the dashedl<strong>in</strong>es. The diagonal dotted l<strong>in</strong>e represents the l<strong>in</strong>e <strong>of</strong> no discrim<strong>in</strong>ation.Various potential diagnostic cut<strong>of</strong>f values (pmol/L) are <strong>in</strong>dicated along thecurve. AUC ROC= 0.905.Receiver-operat<strong>in</strong>g characteristic curve analysis—SerumNT-proBNP concentrations > 1,158 pmol/L differentiated group 1 dogs from group 2 and 3 dogswith a sensitivity <strong>of</strong> 85.5%, specificity <strong>of</strong> 81.3%, positivepredictive value <strong>of</strong> 85.5%, negative predictive value<strong>of</strong> 81.3%, and accuracy <strong>of</strong> 83.6%. The AUC ROCwas90.5% (95% CI, 83.4% to 95.2%; Figure 2). Additionalcut<strong>of</strong>f values for serum NT-proBNP that yielded either asensitivity > 90% or a specificity > 90% were identified(NT-proBNP > 963 pmol/L [sensitivity, 90.3%; specificity,73.5%]; NT-proBNP > 1,829 pmol/L [sensitivity,64.5%; specificity, 91.7%]). The AUC ROCwas 93.0%(95% CI, 85.2% to 97.4%) when differentiat<strong>in</strong>g betweengroup 1 dogs and group 2 dogs and was 88.5% (95% CI,79.9% to 94.3%) when differentiat<strong>in</strong>g between group 1dogs and group 3 dogs.DiscussionOur results <strong>in</strong>dicate that serum NT-proBNP concentration<strong>in</strong> dogs with respiratory signs helps to differentiatebetween congestive heart failure and primaryrespiratory tract disease as an underly<strong>in</strong>g cause. Ourresults are consistent with those <strong>of</strong> other studies 1,17–19,dthat have evaluated circulat<strong>in</strong>g C-BNP and NT-proBNPconcentrations <strong>in</strong> dogs with respiratory tract disease.DeFrancesco et al 17 reported that plasma C-BNP concentrationhad a sensitivity <strong>of</strong> 90% and a specificity <strong>of</strong>78% <strong>in</strong> differentiat<strong>in</strong>g between 101 dogs with congestiveheart failure and 78 dogs with respiratory tract disease.Prosek et al 18 reported that plasma C-BNP concentrationhad a sensitivity <strong>of</strong> 86.4% and a specificity<strong>of</strong> 80.8% <strong>in</strong> differentiat<strong>in</strong>g between 22 dogs with congestiveheart failure and 26 dogs with respiratory tractdisease. Wess et al d reported that a plasma NT-proBNPconcentration > 520 pmol/L had a sensitivity <strong>of</strong> 94.7%and a specificity <strong>of</strong> 96.2% <strong>in</strong> differentiat<strong>in</strong>g between 19dogs with cardiac disease and 57 dogs with respiratorytract disease. In a study <strong>of</strong> 46 dogs, F<strong>in</strong>e et al 19 reportedthat a serum or plasma NT-proBNP concentration> 1,400 pmol/L detected 92% <strong>of</strong> dogs with heart fail-1322 Scientific Reports JAVMA, Vol 235, No. 11, December 1, 2009
ure. Boswood et al 1 reported that a plasma NT-proBNPconcentration > 210 pmol/L had a sensitivity <strong>of</strong> 85.5%and a specificity <strong>of</strong> 82.4% <strong>in</strong> differentiat<strong>in</strong>g betweendogs with cardiac disease and those with respiratorytract disease. Thus, our results are <strong>in</strong> general agreementwith those <strong>of</strong> other studies. Our study was unique <strong>in</strong>its large multicentered design and the requirement thatall dogs undergo both thoracic radiography and echocardiographyas part <strong>of</strong> their diagnostic workup. In ourstudy as well as <strong>in</strong> others <strong>in</strong> humans 20–22 and dogs, 2,23serum NT-proBNP concentration was correlated withechocardiographic and radiographic measures <strong>of</strong> cardiacenlargement.Our results as well as those <strong>of</strong> F<strong>in</strong>e et al 19 <strong>in</strong>dicatea higher diagnostic cut<strong>of</strong>f value for serum NT-proBNPconcentration than those <strong>of</strong> studies by Boswood et al 1and Wess et al d ; the reason for the discrepancy is unclear.Results <strong>of</strong> previous studies have revealed ranges <strong>of</strong>circulat<strong>in</strong>g NT-proBNP concentrations <strong>in</strong> both healthydogs 2,24 and dogs with heart disease or respiratory tractdisease 2,24,25 that are higher than those <strong>in</strong>itially reportedby Boswood et al. 1 It is <strong>in</strong>terest<strong>in</strong>g to note that the lowercirculat<strong>in</strong>g NT-proBNP concentrations were reportedfrom studies 1,d <strong>in</strong> Europe, and differences <strong>in</strong> the studypopulation or sample handl<strong>in</strong>g may be responsible forthe variation <strong>in</strong> values. In humans, NT-proBNP, whilerelatively stable, compared with C-BNP, degrades ifsamples are left at room temperature, 26 and careful attentionto sample collection, handl<strong>in</strong>g, and shipp<strong>in</strong>g isrequired. To the authors’ knowledge, the <strong>in</strong> vitro stability<strong>of</strong> can<strong>in</strong>e NT-proBNP has not been reported; however,our experience with shipp<strong>in</strong>g protocols <strong>in</strong>dicatesthat NT-proBNP degrades dur<strong>in</strong>g overnight shipp<strong>in</strong>g ifnot ma<strong>in</strong>ta<strong>in</strong>ed at 4°C. Future studies are needed to furtherevaluate different handl<strong>in</strong>g and shipp<strong>in</strong>g protocolsbefore wide-rang<strong>in</strong>g cl<strong>in</strong>ical recommendations regard<strong>in</strong>gNT-proBNP assay results can be made.The cl<strong>in</strong>ical usefulness <strong>of</strong> diagnostic assays can becompared among various studies 27 by exam<strong>in</strong><strong>in</strong>g results<strong>of</strong> ROC curve analysis. Inspection <strong>of</strong> the ROC curve <strong>in</strong>dicatesassay sensitivity and specificity at any given cut<strong>of</strong>fvalue. The AUC ROCreflects the discrim<strong>in</strong>atory ability<strong>of</strong> the test with 50% <strong>in</strong>dicat<strong>in</strong>g no ability and 100%<strong>in</strong>dicat<strong>in</strong>g perfect ability to discrim<strong>in</strong>ate between conditions.To be cl<strong>in</strong>ically useful, diagnostic tests shouldpossess an AUC ROC<strong>of</strong> at least 75% to 85%. 27 Our studyyielded an AUC ROC<strong>of</strong> 90.5%, which is comparable toresults from 3 <strong>of</strong> the largest studies 9,10,28 <strong>in</strong> humans.Maisel et al 28 reported that plasma or whole bloodC-BNP concentration had a 90% sensitivity, a 76% specificity,and an AUC ROC<strong>of</strong> 91% for predict<strong>in</strong>g the presenceor absence <strong>of</strong> congestive heart failure <strong>in</strong> a cohort<strong>of</strong> 1,586 patients with shortness <strong>of</strong> breath. Januzzi et al 9reported that a circulat<strong>in</strong>g NT-proBNP concentration >900 pg/mL had an 87% sensitivity, an 86% specificity,and an AUC ROC<strong>of</strong> 94% for predict<strong>in</strong>g acute congestiveheart failure <strong>in</strong> 600 patients with dyspnea, while Moeet al 10 reported that, compared with traditional evaluationwithout the use <strong>of</strong> biomarker assays, use <strong>of</strong> aNT-proBNP assay <strong>in</strong>creased the AUC ROCfrom 83% to90% for predict<strong>in</strong>g acute heart failure <strong>in</strong> 500 patientspresent<strong>in</strong>g to the emergency room with dyspnea. Inhumans, natriuretic peptide test<strong>in</strong>g is currently recommendedas one <strong>of</strong> the first cl<strong>in</strong>ical steps <strong>in</strong> evaluat<strong>in</strong>gpatients suspected <strong>of</strong> hav<strong>in</strong>g heart failure. 29 Use <strong>of</strong> <strong>NTproBNP</strong>assay <strong>in</strong> these patients is strongly associatedwith shortened hospital stay, lower rate <strong>of</strong> rehospitalization,and reduced f<strong>in</strong>ancial cost. 8,10In our study as well as <strong>in</strong> others, 9,11,28,30 the diagnosticgold standard was the cl<strong>in</strong>ical evaluation by a boardcertifiedcardiologist <strong>of</strong> a uniform set <strong>of</strong> diagnostic tests,<strong>in</strong>clud<strong>in</strong>g physical exam<strong>in</strong>ation, thoracic radiography,and echocardiography. Our study <strong>in</strong>cluded a diagnosticcategory for <strong>in</strong>stances where a def<strong>in</strong>itive cl<strong>in</strong>ical diagnosiscould not be confidently made (group 4), andit is unlikely that large numbers <strong>of</strong> misdiagnoses weremade <strong>in</strong> groups 1 through 3. Despite this protocol, differentiation<strong>of</strong> cardiac versus respiratory tract disease <strong>in</strong>dogs can be challeng<strong>in</strong>g, and it is possible that misdiagnoseswere made <strong>in</strong> our study, especially <strong>in</strong> dogs withconcurrent heart and respiratory tract disease. If so,this may have affected the sensitivity and specificity thatwere determ<strong>in</strong>ed for the NT-proBNP assay. One potentiallimitation <strong>of</strong> our study <strong>in</strong>volves the use <strong>of</strong> secondaryand tertiary referral centers from which patients wererecruited. This may <strong>in</strong>troduce bias <strong>in</strong>to the study’s patientpopulation; however, workup by cardiology specialistsperform<strong>in</strong>g echocardiography was an <strong>in</strong>tegralpart <strong>of</strong> the study and necessitated use <strong>of</strong> this particularpatient population.A diagnostic assay has potential cl<strong>in</strong>ical value if thecurrent means <strong>of</strong> diagnosis possesses accuracy lowerthan that afforded by the assay. In our study, the accuracy<strong>of</strong> NT-proBNP assay was 83.6%. In humans, the accuracy<strong>of</strong> correctly diagnos<strong>in</strong>g congestive heart failureby emergency room physicians is surpris<strong>in</strong>gly low, rang<strong>in</strong>gfrom 60% to 75%, and missed diagnoses contributeto the <strong>in</strong>-hospital mortality rate. 27,31 In one <strong>of</strong> the largeststudies, 7 <strong>in</strong>volv<strong>in</strong>g 1,538 patients admitted to the emergencyroom with congestive heart failure, accuracy <strong>of</strong>diagnosis by the primary physician was only 74%. Thisaccuracy <strong>in</strong>creased to 81.5% if circulat<strong>in</strong>g NT-proBNPconcentrations were used <strong>in</strong> conjunction with the primaryphysician’s assessment. To our knowledge, the accuracy<strong>of</strong> diagnos<strong>in</strong>g congestive heart failure <strong>in</strong> dogs byveter<strong>in</strong>arians <strong>in</strong> private practice has not been reported.This variable should be explored aga<strong>in</strong>st NT-proBNP–assisted workup <strong>in</strong> future studies.The cl<strong>in</strong>ical performance <strong>of</strong> a diagnostic test is acompet<strong>in</strong>g balance between sensitivity and specificity.Ga<strong>in</strong>s <strong>in</strong> sensitivity are made at the expense <strong>of</strong> specificityand vice versa. The ROC curve analysis allows identification<strong>of</strong> various cut<strong>of</strong>f values, which maximize eitherparameter. In our study, lower<strong>in</strong>g the cut<strong>of</strong>f value to 963pmol/L <strong>in</strong>creased sensitivity to > 90%, while <strong>in</strong>creas<strong>in</strong>gthe cut<strong>of</strong>f value to 1,829 pmol/L <strong>in</strong>creased specificity to> 90%. In previous studies <strong>in</strong> dogs 2 and humans, 27,27,32an <strong>in</strong>termediate gray zone, <strong>in</strong> which assay results areless reliable, has been proposed. In a population <strong>of</strong> dogswith mitral valve disease and dilated cardiomyopathy, 2a serum NT-proBNP concentration > 1,725 pmol/L or
SMALL ANIMALS/EXOTICuse subjective diagnostic term<strong>in</strong>ology, such as unlikely,possible, and very likely, to convey assay results. 28,29,33Results that fall <strong>in</strong>to the possible category automaticallytrigger additional diagnostic <strong>in</strong>vestigation to <strong>in</strong>crease(or decrease) the confidence <strong>of</strong> diagnosis. Thesealgorithms underscore the diagnostic limitations <strong>of</strong> natriureticpeptide assay <strong>in</strong> both humans and dogs, andNT-proBNP assay results should complement and notreplace the medical history, physical exam<strong>in</strong>ation, andconventional diagnostic test<strong>in</strong>g.In our study, most <strong>of</strong> the patient population comprisedgeriatric small-breed dogs, and as such, manydogs had concurrent cardiac and respiratory tractdisease or pulmonary hypertension. Results <strong>of</strong> previousstudies 2,24 <strong>in</strong>dicate that, although circulat<strong>in</strong>gNT-proBNP concentration is generally low <strong>in</strong> dogs withasymptomatic heart disease, it can be markedly high<strong>in</strong> <strong>in</strong>dividual dogs. These high concentrations woulddecrease the discrim<strong>in</strong>atory ability <strong>of</strong> NT-proBNP <strong>in</strong>dogs with concurrent cardiac and respiratory tract disease.Indeed, <strong>in</strong> our study, the discrim<strong>in</strong>atory power <strong>of</strong>NT-proBNP was lower <strong>in</strong> dist<strong>in</strong>guish<strong>in</strong>g between group1 and 3 dogs versus between group 1 and 2 dogs. Ourresults <strong>in</strong>dicate that serum NT-proBNP concentration ishigh <strong>in</strong> dogs with respiratory tract disease and pulmonaryhypertension. In humans, NT-proBNP is producedby the right ventricle <strong>in</strong> response to myocyte stress, 34,35and although the high plasma NT-proBNP concentrationsare generally lower than for diseases that primarilyaffect the left ventricle, 36 serum NT-proBNP concentrationis correlated with severity <strong>of</strong> right ventriculardysfunction and pressure overload. 33–36 In our study,dogs with primary respiratory tract disease and pulmonaryhypertension had a 3-fold <strong>in</strong>crease <strong>in</strong> the medianserum NT-proBNP concentration, compared withdogs with respiratory tract disease without pulmonaryhypertension. This phenomenon may contribute to alikelihood <strong>of</strong> false-positive result for congestive heartfailure (ie, the diagnosis <strong>of</strong> congestive heart failure <strong>in</strong>dogs with primary respiratory tract disease as the cause<strong>of</strong> respiratory signs). This concept <strong>of</strong> false-positive resultfor congestive heart failure on the basis <strong>of</strong> NT-proB-NP assay results <strong>in</strong> patients with respiratory and cardiacdisease is <strong>in</strong>trigu<strong>in</strong>g. On one hand, the production <strong>of</strong>NT-proBNP <strong>in</strong> response to pulmonary hypertensionconfounds the determ<strong>in</strong>ation <strong>of</strong> the cause <strong>of</strong> respiratorysigns. On the other hand, assay results <strong>in</strong> thispopulation should not be summarily discounted, as <strong>NTproBNP</strong>is strongly correlated to mortality and morbidityrates. In human patients with pulmonary hypertension,a serum NT-proBNP concentration > 1,400 pmol/L hada sensitivity <strong>of</strong> 100% for predict<strong>in</strong>g the 3-year mortalityrate and, <strong>in</strong> this respect, was superior to other parameters,such as exercise test results, pulmonary vascularresistance, functional cl<strong>in</strong>ical class, and cardiac <strong>in</strong>dex. 37Thus, NT-proBNP assay results may have importantprognostic value <strong>in</strong> dyspneic patients despite their potentialto confound diagnosis <strong>of</strong> etiology.In conclusion, serum NT-proBNP concentration<strong>in</strong> dogs with respiratory signs <strong>in</strong> the present studyhelped to differentiate between congestive heart failureand primary respiratory tract disease as the underly<strong>in</strong>gcause. The presence <strong>of</strong> concurrent cardiac and respiratorytract disease or pulmonary hypertension couldconfound diagnosis. The NT-proBNP assay should beused <strong>in</strong> conjunction with medical history, physical exam<strong>in</strong>ationf<strong>in</strong>d<strong>in</strong>gs, and other diagnostic test resultsto help achieve a diagnosis for the cause <strong>of</strong> respiratorysigns <strong>in</strong> dogs.a. Can<strong>in</strong>e CardioCare NT-proBNP, Veter<strong>in</strong>ary Diagnostics Institute,Irv<strong>in</strong>e, Calif.b. GraphPad Prism, version 4.0, Graph Pad S<strong>of</strong>tware Inc, San Diego,Calif.c. MedCalc, version 9.5.1.0, MedCalc S<strong>of</strong>tware, Mariakerke, Belgium.d. Wess G, Timper N, Hirschberger J. The utility <strong>of</strong> NT-proBNPto differentiate cardiac and non-cardiac causes <strong>of</strong> cough<strong>in</strong>g ordyspnea <strong>in</strong> dogs (abstr). J Vet Intern Med 2007;21:608.References1. Boswood A, Dukes-McEwan J, Loureiro J, et al. The diagnosticaccuracy <strong>of</strong> different natriuretic peptides <strong>in</strong> the <strong>in</strong>vestigation <strong>of</strong>can<strong>in</strong>e cardiac disease. J Small Anim Pract 2008;49:26–32.2. Oyama MA, Fox PR, Rush JE, et al. Cl<strong>in</strong>ical utility <strong>of</strong> serum N-term<strong>in</strong>al pro-B-type natriuretic peptide concentration for identify<strong>in</strong>gcardiac disease <strong>in</strong> dogs and assess<strong>in</strong>g disease severity.J Am Vet Med Assoc 2008;232:1496–1503.3. de Bold AJ, Ma KK, Zhang Y, et al. The physiological and pathophysiologicalmodulation <strong>of</strong> the endocr<strong>in</strong>e function <strong>of</strong> the heart.Can J Physiol Pharmacol 2001;79:705–714.4. Braunwald E. Biomarkers <strong>in</strong> heart failure. N Engl J Med2008;358:2148–2159.5. Maisel A, Mueller C, Adams K Jr, et al. State <strong>of</strong> the art: us<strong>in</strong>gnatriuretic peptide levels <strong>in</strong> cl<strong>in</strong>ical practice. Eur J Heart Fail2008;10:824–839.6. Maisel AS. The diagnosis <strong>of</strong> acute congestive heart failure: role<strong>of</strong> BNP measurements. Heart Fail Rev 2003;8:327–334.7. McCullough PA, Nowak RM, McCord J, et al. B-type natriureticpeptide and cl<strong>in</strong>ical judgment <strong>in</strong> emergency diagnosis <strong>of</strong> heartfailure: analysis from Breath<strong>in</strong>g Not Properly (BNP) Mult<strong>in</strong>ationalStudy. Circulation 2002;106:416–422.8. Mueller C, Scholer A, Laule-Kilian K, et al. Use <strong>of</strong> B-type natriureticpeptide <strong>in</strong> the evaluation and management <strong>of</strong> acute dyspnea.N Engl J Med 2004;350:647–654.9. Januzzi JL Jr, Camargo CA, Anwarudd<strong>in</strong> S, et al. The N-term<strong>in</strong>alPro-BNP <strong>in</strong>vestigation <strong>of</strong> dyspnea <strong>in</strong> the emergency department(PRIDE) study. Am J Cardiol 2005;95:948–954.10. Moe GW, Howlett J, Januzzi JL, et al. N-term<strong>in</strong>al pro-B-type natriureticpeptide test<strong>in</strong>g improves the management <strong>of</strong> patientswith suspected acute heart failure: primary results <strong>of</strong> the Canadianprospective randomized multicenter IMPROVE-CHFstudy. Circulation 2007;115:3103–3110.11. Alibay Y, Beauchet A, El Mahmoud R, et al. Plasma N-term<strong>in</strong>al probra<strong>in</strong>natriuretic peptide and bra<strong>in</strong> natriuretic peptide <strong>in</strong> assessment<strong>of</strong> acute dyspnea. Biomed Pharmacother 2005;59:20–24.12. Pemberton CJ, Johnson ML, Yandle TG, et al. Deconvolutionanalysis <strong>of</strong> cardiac natriuretic peptides dur<strong>in</strong>g acute volumeoverload. Hypertension 2000;36:355–359.13. Buchanan JW, Bücheler J. Vertebral scale system to measure can<strong>in</strong>eheart size <strong>in</strong> radiographs. J Am Vet Med Assoc 1995;206:194–199.14. Hansson K, Haggstrom J, Kvart C, et al. Interobserver variability<strong>of</strong> vertebral heart size measurements <strong>in</strong> dogs with normal andenlarged hearts. Vet Radiol Ultrasound 2005;46:122–130.15. Hansson K, Haggstrom J, Kvart C, et al. Left atrial to aortic root<strong>in</strong>dices us<strong>in</strong>g two-dimensional and M-mode echocardiography<strong>in</strong> cavalier K<strong>in</strong>g Charles spaniels with and without left atrialenlargement. Vet Radiol Ultrasound 2002;43:568–575.16. Sahn DJ, DeMaria A, Kisslo J, et al. Recommendations regard<strong>in</strong>gquantitation <strong>in</strong> M-mode echocardiography: results <strong>of</strong> a survey<strong>of</strong> echocardiographic measurements. Circulation 1978;58:1072–1083.17. DeFrancesco TC, Rush JE, Rozanski EA, et al. Prospective cl<strong>in</strong>icalevaluation <strong>of</strong> an ELISA B-type natriuretic peptide assay <strong>in</strong>1324 Scientific Reports JAVMA, Vol 235, No. 11, December 1, 2009
the diagnosis <strong>of</strong> congestive heart failure <strong>in</strong> dogs present<strong>in</strong>g withcough or dyspnea. J Vet Intern Med 2007;21:243–250.18. Prosek R, Sisson DD, Oyama MA, et al. Dist<strong>in</strong>guish<strong>in</strong>g cardiacand noncardiac dyspnea <strong>in</strong> 48 dogs us<strong>in</strong>g plasma atrial natriureticfactor, B-type natriuretic factor, endothel<strong>in</strong>, and cardiactropon<strong>in</strong>-I. J Vet Intern Med 2007;21:238–242.19. F<strong>in</strong>e DM, Declue AE, Re<strong>in</strong>ero CR. Evaluation <strong>of</strong> circulat<strong>in</strong>gam<strong>in</strong>o term<strong>in</strong>al-pro-B-type natriuretic peptide concentration<strong>in</strong> dogs with respiratory distress attributable to congestiveheart failure or primary pulmonary disease. J Am Vet Med Assoc2008;232:1674–1679.20. Karabulut A, Kaplan A, Aslan C, et al. The association betweenNT-proBNP levels, functional capacity and stage <strong>in</strong> patientswith heart failure. Acta Cardiol 2005;60:631–638.21. Mueller T, Gegenhuber A, Poelz W, et al. Biochemical diagnosis<strong>of</strong> impaired left ventricular ejection fraction–comparison<strong>of</strong> the diagnostic accuracy <strong>of</strong> bra<strong>in</strong> natriuretic peptide (BNP)and am<strong>in</strong>o term<strong>in</strong>al proBNP (NT-proBNP). Cl<strong>in</strong> Chem Lab Med2004;42:159–163.22. Silver MA, Maisel A, Yancy CW, et al. BNP Consensus Panel2004: a cl<strong>in</strong>ical approach for the diagnostic, prognostic, screen<strong>in</strong>g,treatment monitor<strong>in</strong>g, and therapeutic roles <strong>of</strong> natriureticpeptides <strong>in</strong> cardiovascular diseases. Congest Heart Fail2004;10:1–30.23. MacDonald KA, Kittleson MD, Munro C, et al. Bra<strong>in</strong> natriureticpeptide concentration <strong>in</strong> dogs with heart disease and congestiveheart failure. J Vet Intern Med 2003;17:172–177.24. Tarnow I, Olsen LH, Kvart C, et al. Predictive value <strong>of</strong> natriureticpeptides <strong>in</strong> dogs with mitral valve disease. Vet J 2008;180:195–201.25. Hori Y, Tsubaki M, Katou A, et al. Evaluation <strong>of</strong> NT-pro BNPand CT-ANP as markers <strong>of</strong> concentric hypertrophy <strong>in</strong> dogswith a model <strong>of</strong> compensated aortic stenosis. J Vet Intern Med2008;22:1118–1123.26. Michaud K, Augsburger M, Donze N, et al. Evaluation <strong>of</strong> postmortemmeasurement <strong>of</strong> NT-proBNP as a marker for cardiacfunction. Int J Legal Med 2008;122:415–420.27. Ray P, Delerme S, Jourda<strong>in</strong> P, et al. Differential diagnosis <strong>of</strong> acutedyspnea: the value <strong>of</strong> B natriuretic peptides <strong>in</strong> the emergencydepartment. QJM 2008;101:831–843.28. Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement<strong>of</strong> B-type natriuretic peptide <strong>in</strong> the emergency diagnosis <strong>of</strong>heart failure. N Engl J Med 2002;347:161–167.29. Swedberg K, Cleland J, Dargie H, et al. Guidel<strong>in</strong>es for the diagnosisand treatment <strong>of</strong> chronic heart failure: executive summary(update 2005): The Task Force for the Diagnosis and Treatment<strong>of</strong> Chronic Heart Failure <strong>of</strong> the European Society <strong>of</strong> Cardiology.Eur Heart J 2005;26:1115–1140.30. Berdague P, Caff<strong>in</strong> PY, Barazer I, et al. Use <strong>of</strong> N-term<strong>in</strong>al prohormonebra<strong>in</strong> natriuretic peptide assay for etiologic diagnosis <strong>of</strong>acute dyspnea <strong>in</strong> elderly patients. Am Heart J 2006;151:690–698.31. Ray P, Birolleau S, Lefort Y, et al. Acute respiratory failure <strong>in</strong> theelderly: etiology, emergency diagnosis and prognosis. Crit Care2006;10:R82.32. van Kimmenade RR, P<strong>in</strong>to YM, Bayes-Genis A, et al. Usefulness<strong>of</strong> <strong>in</strong>termediate am<strong>in</strong>o-term<strong>in</strong>al pro-bra<strong>in</strong> natriuretic peptideconcentrations for diagnosis and prognosis <strong>of</strong> acute heart failure.Am J Cardiol 2006;98:386–390.33. Mueller C, Breidthardt T, Laule-Kilian K, et al. The <strong>in</strong>tegration<strong>of</strong> BNP and NT-proBNP <strong>in</strong>to cl<strong>in</strong>ical medic<strong>in</strong>e. Swiss Med Wkly2007;137:4–12.34. Goetze JP, Videbaek R, Boesgaard S, et al. Pro-bra<strong>in</strong> natriureticpeptide as marker <strong>of</strong> cardiovascular or pulmonary causes <strong>of</strong>dyspnea <strong>in</strong> patients with term<strong>in</strong>al parenchymal lung disease.J Heart Lung Transplant 2004;23:80–87.35. Pruszczyk P. N-term<strong>in</strong>al pro-bra<strong>in</strong> natriuretic peptide as an <strong>in</strong>dicator<strong>of</strong> right ventricular dysfunction. J Card Fail 2005;11:S65–S69.36. Pruszczyk P, Kostrubiec M, Bochowicz A, et al. N-term<strong>in</strong>al probra<strong>in</strong>natriuretic peptide <strong>in</strong> patients with acute pulmonary embolism.Eur Respir J 2003;22:649–653.37. Fijalkowska A, Kurzyna M, Torbicki A, et al. Serum N-term<strong>in</strong>albra<strong>in</strong> natriuretic peptide as a prognostic parameter <strong>in</strong> patientswith pulmonary hypertension. Chest 2006;129:1313–1321.SMALL ANIMALS/EXOTICJAVMA, Vol 235, No. 11, December 1, 2009 Scientific Reports 1325