CMS' Data Collection Tool FAQ - Nursing Home Help
CMS' Data Collection Tool FAQ - Nursing Home Help
CMS' Data Collection Tool FAQ - Nursing Home Help
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
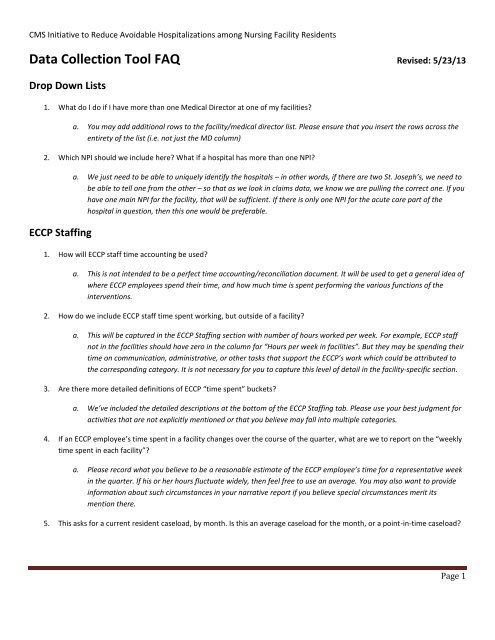
CMS Initiative to Reduce Avoidable Hospitalizations among <strong>Nursing</strong> Facility Residents<strong>Data</strong> <strong>Collection</strong> <strong>Tool</strong> <strong>FAQ</strong> Revised: 5/23/13Drop Down Lists1. What do I do if I have more than one Medical Director at one of my facilities?a. You may add additional rows to the facility/medical director list. Please ensure that you insert the rows across theentirety of the list (i.e. not just the MD column)2. Which NPI should we include here? What if a hospital has more than one NPI?ECCP Staffinga. We just need to be able to uniquely identify the hospitals – in other words, if there are two St. Joseph’s, we need tobe able to tell one from the other – so that as we look in claims data, we know we are pulling the correct one. If youhave one main NPI for the facility, that will be sufficient. If there is only one NPI for the acute care part of thehospital in question, then this one would be preferable.1. How will ECCP staff time accounting be used?a. This is not intended to be a perfect time accounting/reconciliation document. It will be used to get a general idea ofwhere ECCP employees spend their time, and how much time is spent performing the various functions of theinterventions.2. How do we include ECCP staff time spent working, but outside of a facility?a. This will be captured in the ECCP Staffing section with number of hours worked per week. For example, ECCP staffnot in the facilities should have zero in the column for “Hours per week in facilities”. But they may be spending theirtime on communication, administrative, or other tasks that support the ECCP’s work which could be attributed tothe corresponding category. It is not necessary for you to capture this level of detail in the facility-specific section.3. Are there more detailed definitions of ECCP “time spent” buckets?a. We’ve included the detailed descriptions at the bottom of the ECCP Staffing tab. Please use your best judgment foractivities that are not explicitly mentioned or that you believe may fall into multiple categories.4. If an ECCP employee’s time spent in a facility changes over the course of the quarter, what are we to report on the “weeklytime spent in each facility”?a. Please record what you believe to be a reasonable estimate of the ECCP employee’s time for a representative weekin the quarter. If his or her hours fluctuate widely, then feel free to use an average. You may also want to provideinformation about such circumstances in your narrative report if you believe special circumstances merit itsmention there.5. This asks for a current resident caseload, by month. Is this an average caseload for the month, or a point-in-time caseload?Page 1
CMS Initiative to Reduce Avoidable Hospitalizations among <strong>Nursing</strong> Facility ResidentsFacility Turnovera. The intent here is to collect an approximation of the average caseload for the month. This way if a person wascarrying a caseload of 80 residents during the month, and there were several discharges by the end of the month,the average would be a better reflection of the level of activity for the month.1. Do we include RNs in administrative roles?Resident Rostera. Yes, please include all roles (e.g., RNs who perform direct care AND those who fulfill clinical or administrative roles).1. How is “change in condition” defined?a. The purpose of capturing changes in condition is to provide evidence of the impact of ECCP interventions, such asthe early identification and/or treatment of resident changes in condition. As a guideline, these would be eventsthat elicit the consultation of the attending physician, a nurse practitioner, or a registered nurse such as a directorof nursing. While this guideline should enable the capturing of an appropriate type of change in condition, ECCPsare not limited to this guideline and can enter other changes in condition that were identified and addressedwithout the need for a consultation by one of the aforementioned individuals.2. Do I have to collect information on all changes in condition?a. Yes. This data collection tool is intended to capture up to four changes in condition per resident per quarter. If morethan four changes in condition need to be documented, you may copy and paste these columns to allow foradditional changes in condition. Again, collecting this data is critical to provide evidence of the impact ofinterventions.3. What constitutes a medication review that we should track?a. The purpose of this data element is to record whenever ECCP staff trigger or are involved in a review of a resident’smedications. The intent is to assess the impact the ECCPs have on prescribed medications.4. Do medication reviews only refer to antipsychotics?a. No. Any medication review that occurs should be captured. If you believe that there are additional characteristicsabout the review that should be documented, then feel free to include this in the comments column.5. How is “advance directive” defined?a. This is the legal documentation that specifies a beneficiary’s or their authorized representative’s choices for thetype of care to be administered upon certain events. They include Do Not Resuscitate, Do Not Hospitalize, etc.6. What if the advance directives in place are not covered via the drop down list?a. For the current version of the tool, please include the combination of ADs that most closely approximates what iscurrently signed. In the next iteration of the tool, we anticipate the functionality of being able to select multiple ADdocuments in any combination. If you find that the available options are not representative enough, then pleaseinclude any pertinent information in your narrative report.Page 2
CMS Initiative to Reduce Avoidable Hospitalizations among <strong>Nursing</strong> Facility Residents7. What is included in a resident’s preferences for care?a. Preferences of care are typically resident preferences regarding daily life. These include items such as wake/sleeptime, food, bathing, and etc. preferences. These do not include advance directive documents.8. For “Does POC include documentation of resident/family preferences for care?” If there is documentation on preferencesfor care, but it is not in the plan of care (but somewhere else in the patient file) what should be indicated here?a. This element is capturing if a resident’s preferences are documented is a standardized location. If preferences existselsewhere and not in the plan of care, then please answer this as “no”.9. For “NF permanent discharge reason”: What should be captured here for a resident who is transferred to a hospital andthen “loses their bed” at the facility?a. For now, you can leave the discharge reason blank, use the “outcome of transfer” column in the hospitalizationtracking tab to indicate the most appropriate outcome (admitted--status uncertain, for example), and include acomment to indicate the resident is being discharged from the NF but is still in the hospital. Once the residentleaves the hospital, one of the current options should suffice. Note that, according to the eligibility definitions, aresident who is discharged and out of the NF for more than 30 days comes back in with a new admission date.10. What is meant by Routine-Care NP/PA?a. This would typically be an NP/PA that is employed by an attending physician or by the facility and visits the residentroutinely (e.g., every 60 days) regardless of the ECCP’s interventions. This would not be an NP/PA employed by anECCP.Hospitalization Tracking1. What’s the source of the hospitalization symptoms for transfer?a. Source for symptoms is the INTERACT program manual.2. What’s the source of the hospitalization diagnosis for transfer?a. Source for diagnosis is the INTERACT program manual.3. For the columns “Primary/Secondary nursing facility reasons for transfer: DIAGNOSIS”: often a diagnosis cannot be made inthe NF, which is why a resident is being transferred to the hospital. In that case, what should be captured here?a. Please select the most likely diagnosis which resulted in the transfer. If no diagnosis can be ascertained, select“other”. Final diagnoses will be reported in the ‘hospital discharge diagnosis’ column if available, and in claimsdata. These columns are intended to capture, as reasonably as possible, the reasons for the transfer at the time ofthe transfer.4. When a resident returns to the NF from a hospital transfer, what constitutes “adequate” information?a. This was intentionally left as a more subjective field. The intent is to capture the in-taking NF staff’s assessment ofthe level of communication during a transfer back into a facility. For different transfers, the level of communicationneeded could vary widely. Please use your best judgment.Page 3