Guidelines For Antimicrobial Therapy-2011 - Safdarjung Hospital
Guidelines For Antimicrobial Therapy-2011 - Safdarjung Hospital
Guidelines For Antimicrobial Therapy-2011 - Safdarjung Hospital
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
VARDHMAN MAHAVIR MEDIACL COLLEGE ANDSAFDARJUNG HOSPITALGUIDELINES FORANTIMICROBIAL THERAPY <strong>2011</strong>ANTIBIOTIC POLICY GROUP OF HOSPITAL INFECTION CONTROL COMMITTEE1
FOREWORDBacterial resistance to antibiotics is an evolutionary phenomenon. The more the bacteria arechallenged by antibiotics, the more the bacteria will evolve to beat them. Inappropriateprescribing practices in absence of monitored guidelines, extensive over the counter sales, selfmedication and use of antibiotic for trivial ailments and viral infections, poor adherence to afull course regimen, has compounded the problem. As the number of new antibiotics comingout of research is very limited global concern mount as new resistant strains emerge. As weare faced increasing challenge posed by drug resistance and ineffective antibiotics it hasbecome imperative to establish a policy to optimize and promote appropriate use.I appreciate the effort of <strong>Hospital</strong> infection control committee and various departments of SJHwho have worked on preparing this manual. This document is based on microbiological data ofthe hospital and formulated for use by doctors of this hospital. I hope this manual will helpin controlling irrational use and will guide the treating physician to choose most appropriate agentfor therapeutic and prophylactic use. With judicious use, we hope to ensure appropriate treatmentof our patients and to control development and dissemination of resistant bacteria within hospitaland community.DR N K MohantyAddl DG and Medical Superintendent2
MESSAGEIt gives me immense pleasure to present this handbook on <strong>Antimicrobial</strong> <strong>Therapy</strong> in Safdarjang<strong>Hospital</strong>, New Delhi and sincerely appreciate the efforts of Department of Microbiology informulating it under the able guidance of Dr N.K. Mohanty, Addl DG and Medical Superintendent,Safdarjang <strong>Hospital</strong>.The era of antibiotic started in 1930’s and seemed to conquer the infections. Subsequently withwidespread and indiscriminate use of antibiotics, microorganisms developed resistance to them,so much so, that now the antibiotic resistance has reached alarming proportion. Rational useof antibiotics is the order of the day. This antibiotic policy is certainly going to be of greathelp in containing the menace of antibiotic resistance and help in dealing with community aswell as hospital acquired infection effectively.(Dr Vinod Lal )Addl MS3
CONTRIBUTORSDr N. K. Mohanty (Add DG and MS)Dr Vinod Lal ( Addl MS)Dr M. Deb ( Microbiology)Dr B. Gupta (Medicine )Dr S, Prasad ( Medicine )Dr K.C Aggarwal (Paediatrics )Dr Mamta Sharma ( Neonatology)Dr VK Sharma ( Orthopaedics)Dr Gulshanjit Singh ( Surgery)Dr V.K. Tiwari (Burns and Plastic)Dr S. Salhan ( Obstetrics and Gynaecology)Dr A.K Rai (ENT)Dr C D Tripathi ( Pharmacology)Dr V. Ramesh ( Dermatology)Dr P.K Verma ( ICU)Dr Rajni Gaind ( Microbiology)Dr V.M Betigeri ( CTVS)Core GroupChairmanDr. M. Deb. (Microbiology)MembersDr. S. Prasad (Medicine)Dr. M. Sharma (Paediatrics)Dr. R. Gaind (Microbiology)4
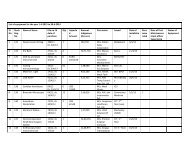
TABLE OF CONTENTSS.No Topics Page No.I. A Guid To Empirical Antibiotic <strong>Therapy</strong>. 6II. <strong>Antimicrobial</strong> Prescribina : Good Practice. 7III. Reserve Anti Microbials. 9IV. Hypersensitivity. 9V. Importance of Infection Control (IC) To Control <strong>Antimicrobial</strong> Resistance. 10VI. Initial Choice of <strong>Antimicrobial</strong> <strong>Therapy</strong> <strong>For</strong> Common Infections /Empirical <strong>Therapy</strong> <strong>For</strong> Common Infections.(a) GI And Intra – Abdominal Infections. 11(b) CNS Infections. 13(c) CVS Infections. 14(d) Skin And Soft Tissue Infections. 15(e) Bone And Joint Infections. 17(f) Respiratory Tract Infections. 18(g) GU Infections. 19(h) Parasitic Infections. 20(i) Acute Undifferentiated Febrile Illnesses. 21VII. Antibiotic Policy <strong>For</strong> Department of Paediatrics 22VIII. Antibiotic Policy <strong>For</strong> Department of Neonatology 24IX. Guielines <strong>For</strong> The Use of <strong>Antimicrobial</strong> Agents In NeutropenicPatients With Cancer 26X. Empirical Antibiotic Policy <strong>For</strong> ICU. 27XI. Antibiotic <strong>Therapy</strong> <strong>For</strong> Surgical Cases. 29XII. Empirical Antibiotic <strong>Therapy</strong> <strong>For</strong> Cardiac Surgery 30XIII. Empirical Antibiotic <strong>Therapy</strong> <strong>For</strong> Paediatri Surgery 30XIV. Empirical Antibiotic <strong>Therapy</strong> <strong>For</strong> Neurosorgery 31XV. Empirical Antibiotic <strong>Therapy</strong> <strong>For</strong> Orthopedics 31XVI. Antibiotic Policy <strong>For</strong> Obstetrics And Gynaecology 31XVII. Eye, Ear, Nose and Throat (ENT) And Oral Infections 33XVIII. Department of Burns And Plastic Surgery. 34XIX. Antifungal <strong>Therapy</strong>. 35XX. Alert Antibiotics : Guidlines <strong>For</strong> Optimising Use of Key <strong>Antimicrobial</strong>s. 36XXI. Treatment of Multi-Drug Resistant Bacterial Pathogens. 38XXII. Dosage Guide <strong>For</strong> Commonly Used <strong>Antimicrobial</strong> Agents. 40XXiii. Antibiotic Panels. 445
I. A GUIDE TO EMPIRICAL ANTIBIOTIC THERAPYInfections remain important threat to humans. Despite advances in medicine there isemergence of antimicrobial resistance both in community as well as in the hospital .Oneof the key factors contributing to antibiotic resistance is inappropriate use of antibiotics.These guidelines are developed by a multi-disciplinary working group to ensure balancedinput. It has considered the antimicrobial choice for specific conditions, and the existingpolicies for specific agents. The latest available evidence backed guidelines andrecommendations were followed with due modification to the antibiotic choices where it waswarranted by local antibiogram. The list of drugs includes commonly used antibiotics inthe OPD and in patients. These guidelines do not include antitubercular, antiviral andantiretroviral drugs. We believe that by following the guidelines it will be possible tomaintain a high standard of patient care, delivered in a consistent way across <strong>Safdarjung</strong><strong>Hospital</strong>. We recommend it to our colleagues.This manual will be revised as and when new recommendations come or with the changein the local antibiogram.This general guidance is not applicable to all patients. The choice of antimicrobial mayneed to be modified in the following situations :• Hypersensitivity to first choice antimicrobial (see guidance on hypersensitivity)• Recent antimicrobial therapy or preceding cultures indicating presence of resistantorganisms• In pregnant or lactating patients• In renal or hepatic failure (see data for individual antimicrobials)• Where significant drug interactions may occur.Though the manual only provides a general guideline in chosing the antibiotic, it incorporatesthe best in antimicrobial therapy and hence any deviation must be justified in documentationin the case records, as this will be followed by prescription. The compliance to generalprinciples (as mentioned in the section – GOOD PRACTICE) is especially subjected toclinical audit as deviation in these aspects with out a evidence backed and peer approvedreason will be considered as endangering the patient safety.We welcome suggestions from our colleagues/readers.Dr Monorama Deb Dr B. Gupta Dr Rajni GaindMember Secretary Member Infection Control OfficerInfection Control Team6
II.ANTIMICROBIAL PRESCRIBING: GOOD PRACTICE1. Send for the appropriate investigations in all infections as recommended. These arethe minimum required for diagnosis, prognosis and follow up of these infections.2. Microbiological samples must always be sent prior to initiating antimicrobial therapy.Rapid tests, such as Gram stain, can help determine therapeutic choices when empirictherapy is required.3. Differentiation between contamination, colonization and infection is important to preventoveruse of antibiotics4. Follow SJH policy If alternatives are chosen, document the reason in the case records.5. Choice of antibiotics: This depends on antibiotic susceptibility of the causativeorganism. There are some infections which can be treated by one of several drugs.The choice can be based on Toxicity, Efficacy, Rapidity of action, Pharmacokineticsand Cost. Use the most effective, least toxic and least expensive antibiotic forthe precise duration of time needed to cure or prevent infection. Beforeprescribing consider following :(a) Which organism is likely to cause the syndrome ?(b) What is the clinical diagnosis and what other steps should be taken to furtherdiagnostic precision?(c) Which antimicrobial agents are available and active against the presumed causeof the illness? Is their range of antimicrobial activity appropriate and whatinformation is available about the likelihood of drug resistance ?(d) Check for factors which will affect drug choice & dose, e.g., renal function,interactions, allergy, pregnancy and lactation.(e) Check that the appropriate dose is prescribed. If uncertain, contact InfectiousDiseases Physician or check in the formulary.(f) What is the duration of treatment ?(g) Is treatment working ?6. Clinical Diagnosis : The antibiotic treatment chosen must be based on someassumption regarding the nature of disease. The treating doctor may not havedifficulty in choosing the appropriate antibiotic to treat a disease caused by a singlemicroorganisms e.g scarlet fever, typhoid, anthrax, as microbiological diagnosis isimplicit in clinical diagnosis. However diseases such as pneumonia, meningitis andurinary tract infection can be caused by any number of different bacteria and doctormay be wrong if he has to guess which antimicrobial agent to use. In such instancesone should seek a bacteriological diagnosis.7. Empiric <strong>Therapy</strong> – If the causative agent is not known and where delay in initiatingtherapy would be life threatening or risk serious morbidity, antimicrobial therapy basedon a clinically defined infection is justified and the following points should be takeninto consideration :(a) Do not rush to treat ? If possible.(b) Collect the necessary specimens before commencing therapy.(c) Cover all possible microbial causes.(d) Try to attain synergy.(e) Consider possible interaction with other drugs.(f) Accuracy of diagnosis should be reviewed regularly and treatment altered/stoppedwhen microbiological results become available.(g) Use less costly drugs where possible.8. The need for antimicrobial therapy should be reviewed on a daily basis. <strong>For</strong> mostinfections 5 – 7 days of antimicrobial therapy is sufficient (simple UTI can beadequately treated with 3 days of antibiotic).7
9. All IV antibiotics may only be given for 48 – 72 hours without review and considerationof oral alternatives. New microbiological or other information (e.g. fever defervescencefor at least 24h, marked clinical improvement; low CRP) should at this stage oftenpermit a switch to oral antibiotic(s), or switch to an IV narrow spectrum alternative,or cessation of antibiotics (no infection present).10. Once culture reports are available, the physician should step down to the narrowestspectrum, most efficacious and most cost effective option. If there is no step downavailed, the reason shall be documented and is subjected to clinical audit.11. Some guiding principles for de-escalation / escalation:(a) If ESBL +ve: drug choice is monotherapy with carbepenems. Group I carbepenem.Piperacillin –Tazobactum & Cefoperazone –Sulbactum can be used if in vitrosensitive and for mild infections.(b) Vancomycin should be used only for confirmed MRSA infections and not MSSA.(c) In case of Pan drug resistant Pseudomonas /Acinetobacter sp combination therapyusing Colistin along with β lactams (using PK/PD principles) should be discussedwith microbiologist / physician.12. Treatment with antibiotic combinations: In order to avoid antagonism between drugsand undesirable side effects of several antibiotics it is advisable to use a single drugwherever possible. There are situations however, when the use of antibiotic combinationis desirable. The situations are:(a) A temporary expedient during the investigation of an obscure illness(b) To prevent the development of bacterial resistance in long term therapy e.gtreatment of tuberculosis.(c) To achieve synergistic effect, e.g. in treating infective endocarditis.(d) Mixed infection, when one drug is not effective against the pathogen.(e) To permit a reduction of the dose of potentially toxic drug.The choice of drug should be that they act synergistically. The following combinationsare synergistic1. Aminoglycoside and β–lactam antibiotic.2. β–lactam antibiotic and β–lactamase inhibitor.3. β–lactam antibiotic and cell wall inhibitor (Vancomycin)4. Sulphamethoxazole and Trimethoprim.13. Is Treatment working?: Where treatment is apparently failing, advice from an IDphysician should normally be sought rather than blindly changing to an alternativechoice of antimicrobial agent.<strong>Antimicrobial</strong> drug therapy cannot be considered in isolation and other aspects oftherapy must be taken into account in judging the effect of treatment. Even anappropriate antibiotic may be ineffective if pus is not drained, septic shock treatedand hypoxia and anemia corrected. There are several conditions in which chemotherapyalone cannot eliminate an infection. Obstructive lesions can cause infection to recur,unless they can be dealt with surgically. Also chemotherapy cannot obviate thenecessity for draining an abscess or removing sequestra or calculi. Failure oftreatment can also be due to a super-added infection, e.g. phlebitis, development ofresistance during therapy or poor tissue penetration.14. Laboratory control of the effects of treatment: Whether treatment has beensuccessful or not is best judged by clinical criteria, but it is useful to know whetherthe infecting organism has been eliminated. Repeated cultures are, therefore sometimesindicated.8
III.RESERVE ANTIMICROBIALSThese reserve antimicrobials will be made available following a recommendation from theMicrobiology Department as per culture report or if included in an antimicrobial policy fora clinical specialty that has been agreed with ID Physician. They are held in reserve tomaintain their effectiveness in treating certain difficult infections by reducing the spreadof microbial resistance and to encourage cost effective prescribing. Before a reserveantibiotic is issued to the ward, the pharmacist is instructed to ascertain the indication andif this falls outside the approved policy, to request that the prescriber consult the IDPhysician.The following criteria has been proposed to protect the Carbapenems and Linezolidfrom overuse –1. Severe sepsis as defined by more than one organ failure of new onset and/or elevatedserum lactate.2. Clinical failure of other classes of antibiotics over 48 hours in terms of worseninginflammatory markers, unresolving fever and new/worsening hemodynamic instability.3. Underlying severe immuno-suppression – Neutropeniea, immuno-suppressive therapy,or Diabetic Ketoacidosis (DKA).4. The organism is susceptible to only carbapenems / linezolid, as per culture report.The following criteria has been proposed for initiating Colistin –1. Pan-resistant organism as per culture report with evidence of invasive disease – fever/leucocytosis/elevated procalcitonin( PCT) or culture from a sterile site.2. Clinical failure of all other classes of antibiotics over 72 hours.The following criteria has been proposed for initiating Rifampicin –1. Empiric or proven TB as a part of ATT (4 drug regimen)2. As anti-bacterial only if prescribed as a combination regimen where the companion drugand Rifampicin, both are proven as susceptible as per culture report.RIFAMPICIN WILL NOT BE ISSUED ALONE AS AN ANTI-BACTERIAL.The following criteria has been proposed for initiating Aminoglycosides –I. Only as a part of initial empiric regimen of a combination therapy – shall step downto single drug after culture report.II. Other safer drug options have been ruled out in a culture reportIV.HYPERSENSITIVITYAll patients should be asked about drug allergies. This is the responsibility of the doctorwho writes the patient’s history. If a patient reports a drug allergy clarify whether this isan allergy or drug intolerance. In some cases there will be an overlap between drug allergyand drug intolerance.• Clinical features suggestive of drug allergy:One or more symptoms developed during or following drug administration includingdifficulty breathing, swelling, itching, rash, and anaphylaxis, swelling of the lips, lossof consciousness, seizures or congestion involving mucous membranes of eyes, noseand mouth.• Clinical features suggestive of drug intolerance:One or more symptoms developed during or following drug administration includinggastrointestinal symptoms e.g. nausea, vomiting, diarrhoea, abdominal pain and feelingfaint.9
If patients are unable to give an allergy history, the doctor should take reasonable stepsto contact someone who can provide a reliable allergy history. It is the prime responsibilityof the prescribing doctor to ensure that allergy history is documented in drug chart as• No known allergy (NKA).• History not available.V. IMPORTANCE OF INFECTION CONTROL (IC) TO CONTROL ANTIMICROBIALRESISTANCEThe use of antimicrobial agents inevitably leads to the emergence of resistant microorganisms.It also destroys the normal flora of the body and renders patients far more susceptible tocolonization with micro-organisms introduced from elsewhere in the hospital through the processof cross infection.• <strong>Hospital</strong>s may be considered as reservoirs and breeding grounds within the world ofantibiotic resistance.• Prevention of cross infection and good quality antimicrobial prescribing contribute to theprevention of antimicrobial resistance. Infection Control and Clinical Microbiology areinextricably linked.• There is no substitute of hand washing in preventing hospital acquired infection andthe spread of antibiotic resistant micro-organisms.• High standards of hospital cleanliness may be important in controlling the spread ofresistant organism in the environment. e.g. MRSA, Acinetobacter baumannii(Source : www.cdc.gov/getsmart)10
VI.INITIAL CHOICE OF ANTIMICROBIAL THERAPY FOR COMMON INFECTIONS/ EMPIRICALTHERAPY FOR COMMON INFECTIONSThese recommendations are for initial empiric treatment, based on likely microbial etiologyand antimicrobial susceptibility pattern observed in our setting.The antimicrobial agent with narrowest spectrum, least toxicity and cost should be chosenonce culture reports are available.(a)GI AND INTRA-ABDOMINAL INFECTIONSCondition Etiology(Likely pathogen)Antibiotics Comments1. Acute Viral None Rehydrationgastroenteritis Entertoxigenic andEntero-pathogenicE.coli2. Cholera V. cholerae Doxycycline 300 mg Prompt rehydrationp.o. x 1 doseessential3. Bacillary Shigella sp None needed fordysenterypreviously healthy patientwith mild symptoms.Ciprofloxacin 500 mgp.o.BID 3-5 d in:1. Patients with severesymptoms,2. Immunocompromisedpatients.4. Amoebic E. histolytica Metronidazole 400 mgdysenteryp.o. TID x 10 d5. Giardiasis Giardia lamblia Tinidazole 2 gm p.o. x1 dose ORMetronidazole 250mgTID x 5d6. Enteric fever S. enterica ser. Multi Drug Resistant MicrobiologicallyTyphi Ciprofloxacin 500 mg confirmed diagnosis :S. enterica ser. BD 5-7 d Obtain AST &Paratyphi A Ceftriaxone Ciprofloxacin MIC.2-3 g/d i.v 7-14 d •if MIC < 0.25 µg/ml,AzithromycinCiprofloxacin 750 mg1g/d (p.o.) x 5dBID p.o. x 14 daysNalidixic acid• If MIC > 0.25 µg/ml,Resistant ***treat as per AST report.Ceftriaxone 2-3 gm • Empiric therapy:i.v/d x14 dCo-trimoxazoleAzithromycin 1gm/d/p.o. if the prevalence ofCiproflox 400 mg MDR S.Typhi is veryi.v. 12 hrly x 14 days low (
ConditionEtiology(Likely pathogen)AntibioticsComments7. Cholangitis/Acute Enterobacteriaceae Ertapenem 1 gm i.v. OD • Duration: 7–10 dayscholecystitis * Anaerobes Alternatives : • Patients unresponsivePiperacillin + Tazobactam to antibiotics may4.5 gm i.v. 8 Hourly require surgery.OR 3.375gm i.v. 6 hourly8. Spontaneous Enterobacteriaceae Piperacillin + Tazobactam • Duration: 5 -7 daysbacterial (most often E. coli) 4.5 gm i.v. 8H ProphylaxisperitonitisOR 3.375gm i.v. 6hourly (only in patients withAlternatives :cirrhosis & ascites):Ertapenem 1 gm Co-trimoxazole 1 DSi.v. ODtablet OD×5-7 days orNorfloxacin 400 mg9. Secondary Enterobacteriaceae Ertapenem 1 gm i.v. OD • Surgery to eliminateperitonitis B. fragilis Alternatives : source of(bowel Enterococcus • Tigecycline 100 mg contamiamination,perforation)* initial dose, followed reduce bacterial load,by 50 mg i.v. (over and prevent recurrence30 to 60 minutes) • Duration: 5 - 7 days;Q12Hlonger if leukocytosis• Piperacillin+Tazobactam / left shift and fever4.5 gm i.v. 8 hourlly are slow to resolve orsource controlinadequate.10. Intra-abdominal As above As above Drainage of abscessabscessH. pylori PPI 2(i.e omeprazole Duration 14 daysassociated 20 mg BID) +disease. Pepticclarithromycin 500 mgulcer disease,P.O.BID + Amoxycilingastric MALT1000mg p.o.BID** lymphoma11. Amoebic liver E. histolytica Metronidaole 500mg i.v. Ultrasound guidedTID / 800mg PO TID drainage indicated inlarge abscesses, signsof imminent rupture andno respone to medicaltreatment* Ertapenem is suggested as initial empiric choice because of high prevalence of ESBL producingstrains among E.coli and Klebsiella sp. De-escalate therapy once antibiotic susceptibility isknown.** Mucosa asosciated lymphoid tissue12
(b)CNS INFECTIONSConditionEtiology(Likely pathogen)AntibioticsComments1. Acute Bacterial Strep pneumoniae CP 20L i.v. Q2H· Duration 10-14 daysmeningtis N. meningitidis • Penicillin intermediate Steroids Indication :(Community H. influenzae susceptible (MIC • Cloudy CSF·acquired) 0.12-1 µg/mL) • Bacteria in gram stainpneumococci. • WBC count >Ceftriaxone 2gm 1000/ml (CSF)i.v Q12 H.• Penicillin –resistant Dose Dexamthazone(MIC ≥ 2 µg/ml) 0.15 mg/kg × 4d.Pneumococci :1 st dose15 minCeftriaxone 2gm before 1 st dose ofi..Q12H + Vancomycin antibiotic.500mg i.v. Q6H2. Brain abscess Coagulase-negative • Ceftriaxone 2 gm i.v. Until resolved.Staphylococci, Q12H+MetronidazoleStaph. aureus, 500 mg i.v. Q8HAnaerobes3. Septic Staph aureus • Cloxacillin 2 gm i.v. Duration 3-4 weekscavernousQ4H + Gentamicinsinus1mg/kg i.v. Q8Hthrombosis4. Neurocy- Taenia solium • Albendazole 400 mg Individualize therapeuticsticercosis. p.o. Q12H, with decisions, based onDexamethasone 2mg the number location,p.o. Q8H x 10 days and viability of the• Antiepileptic therapy parasites within CNS.for seizures1.Single enhancinglesions –antiepileptics alone.2.>1- 100 enhancinglesions (cysticercoticencephalitis) –steroids alone;no antiparasiticdrug.13
(c)CVS INFECTIONSConditionEtiology(Likely pathogen)AntibioticsComments1. Infective Penicillin susceptible CP 120 – 180 L units/ 2-week regimen onlyendocarditis (MIC ≤ 0.1µgm/ml) day i.v. x 4 wks for un-complicated(native valve) Strep viridans OR cases of native valveCeftriaxone 2 gm i.v. IE due to highlyOD x 4 wkspenicillin susceptibleOR Strep viridans (MIC 0.5 µgm/ml. Gentamicin 1mg/kg i.v.Q8H x 4 - 6 weeks.“Culture negative”Ampicillin 2 gm i.v.Q4H +Gentamicin 1mg/kg i.v.Q8H x 4 6 weeks.2. Infective MSSA Cloxacillin 2 gm i.v. Cardiothoracicendocarditis Q4H + surgery consultation(prosthetic valve)Rifampicin 600 mg p.o.BIDGentamicin 1mg/kg i.v.Q8H x 2 wksMRSAVancomycin 15 mg/kgi.v. Q12H +Rifampicin 300 mg p.o.Q8H +Gentamicin 1mg/kg i.v.Q8H x 2 weeks14
(d)SKIN AND SOFT TISSUE INFECTIONSConditionEtiology(Likely pathogen) Antibiotics Comments1. Cellulitis Strep. pyogenes, Cefazolin 1 gm i.v.Staph aureus Q8H × 7-10 days(until clinical cure)Alternatives :1.Cloxacillin 500 - 1000mg p.o. Q6H × 7-10days2.Cephalexin 500 mgp.o. Q6H × 7- 10 days2. Furunculosis Staph. aureus 1.Cloxacillin 500 - 1000mg p.o. Q6H × 7-10days2.Cephalexin 500 mgp.o. Q6H × 7- 10 days3. Diabetic foot– Staph. aureus 1.Cloxacillin 500 - 1000mild (localized mg p.o. Q6H × 7-10cellulitis, nodayssystemic2.Cefazolin 1 gm i.v. Q8Hsymptoms)/Cephalexin 500 mgp.o. Q6H × 7-10 days4. Diabetic foot– Polymicrobial – Cefazolin 1 gm i.v. Surgical consultationmoderate to (Staph aureus Q8H + for drainage orsevere (limb Strep. pyogenes, Gentamicin 5 mg/kg i.v. debridementthreatening - aerobic gram- Q24Hsevere cellulitis negative bacilli, OR Ciprofloxacin 400 mg/gangrene / anaerobes) i.v Q12H +MetronidazoleSIRS)500 mg i.v. Q8HAlternate regimens :1.Tigecycline 100 mginitial dose, followed by50 mg i.v. (over 30 to60 minutes) Q12H2.Ertapenem 1 gm i.v.OD3.Piperacillin-Tazobactam4.5 gm i.v. Q8H5. Necrotizing Strep. pyogenes CP 20 L Units i.v. Q4H Surgical debridement.fasciitis+ Clindamycin 600 mgi.v. Q6H6. Tinea Malassezia furfur Topical treatment :versicolor1.Ketoconazole 2% creamlocally BD × 2 weeks2.Selenium Sulfide 2.5%lotion locally (apply;leave for 10 minutes& wash off) × 7 daysSystemic treatment:1.Fluconazole 400 mgp.o. × 1 dose2.Itraconazole 400 mgp.o. OD × 3 – 7 days15
7. Tinea corporis / T. rubrum Topical treatment :cruris / pedis1.ClotrimazoleBD × 6 weeks2.MiconazoleBD × 6 weeks3.TerbinafineBD × 2-3 weeksSystemic treatment :1.Terbinafine 250 mgp.o. OD × 2 weeks.2.Fluconazole 150 mg p.o.once-a-week × 4 weeks(T corporis) and× 8 weeks (T pedis)8. Tinea capitis T. tonsurans Terbinafine 250 mg p.o.M. canis OD × 4 – 8 Weeks.9. Onychomycosis T. rubrum Finger nails :1.Terbinafine 250 mg p.o.OD × 6 weeks.2.Itraconazole 200 mg p.o.BID × 1 week/monthx 2 months.3.Fluconazole 150 – 300mg p.o. once-a-week× 3 – 6 months.Toe nails :1.Terbinafine 250 mg p.o.OD x 12 weeks.2.Itraconazole 200 mg p.o.BID × 1 week/month ×3 – 4 months3.Fluconazole 150 – 300mg p.o. once-a-week ×6 – 12 months.10. Mycetoma :Actinomycotic Aerobic • Streptomycin 15 mg/kg/ Duration: Until clinicalmycetoma actinomycetes day i.m. + CotrimoxazolecureDS 1 tab p.o. BID • Aminoglycosides aregiven in cycles of 3ORweeks each × 2 or• Amikacin 15 mg/kg/day more, as needed, withwith Co-trimoxazole DS1 interval of 2 weekstab p.o. BIDbetween cyclesEumycotic Eumycetes Itraconazole 200 mg • Surgical debridementmycetomaas needed11. Scabies Sarcoptes scabei Topical treatment :• Permethrin 5% cream(apply to entire skinbelow neck & leavefor 8 hours)Systemic treatment:·• Ivermectin 200 mgm/kgp.o. × 1 dose16
12. Surgical site M. abscessus • Surgical debridement,infections caused M. fortuitumwith removal of allby rapidly M. chelonei foreign bodiesgrowing (atypical) • Antibiotics :mycobacteriaClarithromycin 500 mgp.o. BID + Ciprofloxacin500 mg p.o. BID +Amikacin 500 mg i.v.OD × 3 months13. Bites (cat, dog, Pasteruella multocida Amoxicillin-Clavulanatehuman, rat) Capnocytophaga 625 mg p.o. TIDEikenellaStrep viridansSpirillum minusStreptobacillusmoniliformis(e)BONE & JOINT INFECTIONSConditionEtiology(Likely pathogen) Antibiotics Comments1. Acute osteo- Staph. aureus Cloxacillin 1 gm i.v. Q4H <strong>For</strong> optimal treatment,myelitis – OR Cefazolin 1 gm i.v. microorganism(s)(Haematogenous)Q8H + Gentamicin 80 mg should be identifiedNormalHost i.v. Q12H OR Amikacin by blood culture or500mg i.v. Q12H aspiration or bonebiopsy.Duration: 6 weeks Canswitch to oral therapyonce clinicalimprovement occurs.2. Osteomyelitis: Polymicrobial No empiric therapy unless • Surgical debridementContiguous focus acutely ill Severe condition will enhance cure rate(Decubitus ulcer/Cloxacillin 1 gm i.v. Q4H • Definitive treatmentdiabetic foot) OR Cefazolin 1 gm i.v. guided by bone biopsyQ8H + Gentamicin 80 mg / deep curettings (NOTi.v. Q12H ORsuperficial swabs)Amikacin 500mg i.v. Q12H culture & susceptibilitystudiesDuration: minimum 6weeks after surgicaldebridement3. Chronic No empiric therapy Definitive treatmentosteomyelitisguided by bone biopsy,culture & susceptibilitystudies.4. Septic arthritis Staph. aureus Cloxacillin 1 gm i.v. Q4H Obtain synovial fluidAlternative:cultures.Cefazolin 1 gm i.v. Q8H Orthopedic consultationDuration: 14 – 28 days (for surgical drainage)17
5. Prosthetic joint Coagulase - negative No empiric therapy unless Obtain culture ofinfections Staphylococci, acutely ill In severely ill periprosthetic tissue /Staph. aureus, patients (awaiting results synovial fluid. AvoidStreptococci, of diagnostic studies): culturing superficialGram negative bacilli Vancomycin 15 mg/kg i.v. wound / sinus tractsQ12H + Gentamicin 1 mg/kg i.v. Q8H + Rifampicin300 mg p.o. Q8H(f)RESPIRATORY TRACT INFECTIONSConditionEtiology(Likely pathogen) Antibiotics Comments1. Acute pharyngitis Strep.pyogenes Benzathine penicillin The large majority of(Strep. Grp A) 12 L units i.m. x 1dose adults with acuteViral Alternatives:· pharyngitis have a self-• Penicillin V 500 mg limited illness, for whichp.o. Q8H x 10 d supportive care• Amoxicillin 500 mg (analgesics, antipyreticsQ8H p.o. x 10 d ,saline gargles) only isPenicillin allergic neededpatients :• Antibiotic treatment• Erythromycin 500 mg benefits only thosep.o. Q6H x 10 d patients with GABHSinfection• Limit antibioticprescriptions topatients who are mostlikely to have GABHSinfection - fever,tonsillar exudates, nocough, & tenderanterior cervicallymphadenopathy• Throat swab culturesrecommended forroutine evaluation ofpharyngitis2. Acute epiglotitis H influenzae Ceftriaxone 1 gm i.v OD Airway management3. Ludwig’s angina Polymicrobial x 7-10 d ClindamycinVincent’s angina (oral anaerobes) 600mg i.v. Q8HAlternative : Amoxicillin Airway managementClavulanate 1000 mg • Surgical drainagep.o. BID × 7-10 d4. Acute bronchitis Viral None required5. Acute bacterial Strep. pneumoniae Amoxicillin 500 mg p.o.rhinosinusitis. H. influenzae TID x 10-14 d.(Antibiotics if M. catarrhalissymptoms for7– 10 days,facial pain,purulent nasaldischarge)18
6. Acute bacterial Strep. pneumoniae Amoxicillin 500 mg p.o.exacerbation of H. influenzae TID x 7dCOPD (increased M. catarrhalis Alternatives :dyspnea, in• Doxycycline 100 mg-creased sputump.o. BD × 7 dvolume, and• Azithromycin 500 mgincreased sputum p.o. OD × 3 d ·purulence).7. Communityacquiredpneumonia*CURB-65 Strep pneumoniae Amoxycillin 500 mg p.o.score = 1Q8H x 7 dCURB-65 Strep pneumoniae CP 20 L units i.v. Q4Hscore = 2x 7-10 dCURB-65 Strep pneumoniae Ceftriaxone 1 gm i.v.score = 3 Legionella spp. Q12H + AzithromycinEnterobacteriaceae 500 mg i.v./ p.o. ODAlternative: Levofloxacin750 mg i.v. (to bechanged to p.o.)OD x 7-10d8. Ventilator Gram-negatives: See VAP at page no.associated E. coli, Klebsiella, 28-29pneumonia Enterobacter,Pseudomonasaeruginosa9. Pneumocystis P. jiroveci Co-trimoxazolepneumoniaDose: Trimethoprim(PCP) in AIDS15 mg/kg/d x 21d*CURB-65 scoring system: 6 point score (range 0-5). Gives one point each for:C Confusion (abbreviated mental test score < 8 or new disorientation in person, place,or time)U Urea > 7 mmol/l (55 mg/dL)R Respiratory rate > 30/minB Low Blood pressure (SBP < 90 mm Hg or DBP < 60 mm Hg)Age > 65 yearsSevere pneumonia = CURB-65 score of > 3(g)GU INFECTIONSConditionEtiology(Likely pathogen) Antibiotics CommentsAcute uncomplicated E. colicystitis in women –dysuria andfrequency in healthy,adult, non-pregnantwomen with normalurinary tractCiprofloxacin 500 mgp.o. BID x 3 dAlternative : Nitrofurantoin100 mg p.o. BID x 7 d19
Pyelonephritis– uncomplicated E. coli Amikacin 15mg/kg i.v. Duration :(no underlying GU Q24H Mild to moderate casesdisease)Severely ill (MODS, septic – 7days; Severe casesshock): Ertapenem 1 gm – 14 days; hospitalizei.v. Q24H; de-escalate as patientper AST reportsComplicated UTI E. coli, Proteus, Carbapenem (Imipenem Duration: 10 - 14 days.(underlying GU Pseudomonas /Meropenem) de-escalatedisease) aeruginosa, as perv AST reports.Acinetobacter spp.Foley catheter Gram-negative bacilli As per AST reports Urine sample for cultureassociated UTI A. Treat only when obtained through a newpatient has systemic catheter (after removingsymptoms (fever, SIRS) the indwelling catheter)When this is notpossible, obtain samplethrough catheter port,(and not the drainagebag).(h)PARASITIC INFECTIONSConditionEtiology(Likely pathogen) Antibiotics Comments1. Malaria P. vivax <strong>For</strong> blood stage:Chloroquine phosphate.Day 1: 1,000 mg p.o.(600 mg base) (4 tablets)Day 2: 1,000 mg p.o.(600 mg base) (4 tablets)Day 3: 500 mg p.o.(300 mg base) (2 tablets).<strong>For</strong> radical cure:Chloroquine plusPrimaquine phosphate.15mg p.o. OD x 14 d.In G6PD deficiency (mild)primaquine 0.75 mg/kgonce a week x 6 weeks.Not in severe G6PDdeficiencyP. falciparum Artemether 20 mg +Lumefantrine 120 mg(co-formulated tablets)4 tablets BID x 3 d20
2. Severe malaria P. falciparum Preferred: Artesunate Patients with one or2.4 mg/kg i.v. given as a more of the followingbolus at 0, 12, and 24 h, clinical criteria are& then daily + Doxycycline considered to have100 mg p.o.Q12H ‘severe malaria’ andAlternative: Quinine should be treated withdihydrochloride (in 5% i.v. antimalarialsdextrose) 20 mg/kg i.v. • Comaover 4 hours, followed by • Severe anemia10 mg/kg i.v. Q8H, with • Renal failureDoxycycline or• ARDSClindamycin.• ShockSwitch to p.o. therapy as • DICsoon as possible to • Acidosiscomplete 7day• Hemoglobinuria• Jaundice,• Parasitemia >5%*Consider exchangetransfusion for personswith parasitemia >10%3. Visceral L. donovani 1.Amphotericin B 0.5leishmaniasismg/kg/day i.v. OD x(kala azar) 30 d.2.Amphotericin B 1.0mg/kg/day i.v. onalternate days x 15doses.3.Miltefosine 2.5 mg/kg/day (bodyweight>25 kg 50 mgBD; body weight
Scrub typhus Orientia Doxycycline 100 mg p.o.tsutsugamushi BID x 7 daySpotted feverDoxycycline 100 mg p.o.BID x 5-7 daysDengue fever Dengue virus No antiviral effective. Prompt and meticulousChikungunya Chikungunya virus fluid replacement forDSS.Acute undifferen- • Orientia Doxycycline 100 mg p.o. These patients presenttiated fever with tsutsugamushi BID + Ertapenem 1 gm with fever for 5 – 15severe sepsis • Gram-negative i.v. Q24H days with no evident(community bacteria Tailor antibiotic regimen focus of infection andacquired) • Leptospira once diagnosis confirmed features of severe• S.Typhi malaria should be ruled sepsis (multi-organout.dysfunction and/orshock);Melioidosis • Burkholderia Initial intensive therapy : 4 - 8 weeks of intensivepseudomallei Ceftazidime 2 gm i.v. therapy for patients whoQ8H x 14 daysare critically ill, haveEradication therapy : extensive pulmonaryCotrimoxazoledisease, deep seatedDS 2 tab p.o. BID + collections or organDoxycyclineabscesses,100 mg p.o. BID x 3 osteomyelitis, septicmonthsarthritis or neurologicmelioidosis.VII.ANTIBIOTIC POLICY FOR DEPARTMENT OF PEDIATRICSSPECIFIC CONDITIONS1. PYGOENIC MENINIGITIS✓<strong>For</strong> below 2 monthsAntibiotic Each dose Frequency Route Duration< 7 days age > 7 days ageInj. Ampicillin and 100mg/kg/dose 12 hrly 8 hrly IV 3 weeksInj. Gentamicin 5mg/kg/dose 24 hrly 24 hrly IVORInj. Cefotaxime and 50mg/kg/dose 12 hrly 8 hrly IV 3 weeksInj. Gentamicin 5mg/kg/dose 24 hrly 24 hrly IV✓<strong>For</strong> 2 months and above - Inj Ceftriaxone(100mg/kg/d-2 divided dosage)<strong>For</strong> Neisseria – 7 days<strong>For</strong> H. influenza -10 days<strong>For</strong> S. pneumoniae -14 daysIf cultures & sensitivity report does not reveal any organism – for 10 days.However in strong clinical suspicion for staphylococcus infection in the form of skinpustules, Otitis Media , arthritis or flowing external wounds – Inj. Vancomycin is addedin the above regimen for minimum period of 2 weeks. In case ceftriaxone is not available,Inj cefotaxime (200mg/kg/d, 3-4 divided doses) is given for the same duration .22
2. LOWER RESPIRATORY TRACT INFECTION –as per F-IMNCI recommendations, pneumoniais categorized in to 3 types – very severe pneumonia, severe pneumonia and pneumonia.(a) <strong>For</strong> very severe Pneumonia: - Inj Ampicillin and gentamycin for less than 2 monthsand inj . Ampicillin for more than 2 months is recommended. In case of non responsein 2 days, inj 3 rd generation cephalosporin’s (3GC) or Inj chloramphenicol can be used.(b) <strong>For</strong> severe pneumonia –Inj Ampicillin (If this is not available Inj chloramphenicol) for7-10 days. In case of non response in 2 days the patient is searched for pus collectionlike empyema, or at any other site. In case it is excluded 3GC is recommended fora period of 3-4 weeks.(c) <strong>For</strong> pneumonia – oral amoxicillin for a period of 5 to 10 days is recommended. Incase of non availability oral Co-trimoxazole or macrolides can be used.(d) <strong>For</strong> post measles bronchopneumonia – Inj ampicillin + cloxacillin + gentamicin for2 to 3 weeks is recommended .3. UPPER RESPIRATORY TRACT INFECTIONS – As these are mostly viral in originantibiotics are hardly needed barring following situations.(a) Follicular tonsillitis (Gr. A Streptococcus ) Inj benzathine penicillin in single doseor oral amoxicillin or erythromycin for 10 days is recommended .(b) Faucial diphtheria –Inj procaine penicillin for 10 days in recommended.(c) URI with AOM –oral amoxicillin or Co-trimoxazole for 7 to 10 days in recommended.(d) Acute Sinusitis with URI : Oral amoxicillin for 7-10 daus is recommended.(e) Acute epiglottis – these patients are admitted and Inj ampicillin + chloramphenicolare given4. DYSENTERY–(a) <strong>For</strong> indoor cases- Inj ceftriaxone(100mg/kg) for 5-7 d.(b) <strong>For</strong> OPD cases—oral ciprofloxacin for 3 days is recommended . In case on nonresponse in 2 days oral cefixime or ofloxacin are to be used .5. CHOLERA–single dose oral doxycycline (50mg for less than 3 year and 100 mg for thoseabove.6. ENTERIC FEVER(a) <strong>For</strong> OPD cases- oral ciprofloxacin for 10-14days.(b) <strong>For</strong> indoor cases –Inj ciprofloxacin is started . In case of non response in7 days time,it is changed to ceftriaxone or as per culture & sensitivity report.7. UTI(a) Uncomplicated (without any urinary tract obstruction) and more than 2 months oldcases oral cotrimoxazole (5 days for lower UTI and 7-10 days for upper UTI ) is given.(b) <strong>For</strong> less than 2 months – most of these patients are admitted and Inj amp +gentamicin are given for 10 -14 days.(c) <strong>For</strong> immunocompromized hosts : Inj piperacillin-tazobactum for the coverage ofpseudomonas is given along with Inj ampicillin + gentamicin .8. MALARIAAs per National Malaria Control Program Delhi comes under low risk zone oralchloroquine is given for OPD cases and for indoor cases Inj quinine is which is changedin to oral quinine as the patient recovers to complete the course of 10 days .9. MASTOIDITIS AND OTHER ACUTE EAR INFECTIONThese cases are referred to ENT after starting oral amoxicillin10. CSOMUsually antibiotic is not started until there is exacerbation and these are referredENT23to
11. SEVERE ACUTE MALNUTRITIONFirst line antibiotics started is Inj ampicillin + gentamicin till culture and sensitivity reportis available.12. MENINGOCOCCEMIA3 RD generation cephalosporin(3GC) for 7 days is given.13. RHEUMATIC HEART DISEASE-Prophylactically Inj. Benzyl penicillin -12 L IU is given and in case of allergy to penicillin,oral erythromycin 250 mg twice daily for 3 days is given.14. STAPHYLOCOCCAL INFECTION<strong>For</strong> mild localized infection oral amoxyclav (or erythromycin ) along with local treatmentis given.<strong>For</strong> invasive infection (Pneumonia or meningitis) Initially Inj. ampicillin +gentamicin +cloxacillinis started . In case of non response in 2 days time Inj. vancomycin is added. Inj linezolidis started when either vancomycin resistant staphylococcus or vancomycin resistantenterococci is found in culture & sensitivity report.15. SOME RARE CONDITIONS(a) BRAIN ABCESS–Inj vancomycin +ceftriaxone +metronidazole for 3to 4 week is givenas the broad coverage of aneaerobes and staph infection along with local drainageof pus.(b) PERITONITIS–Inj amp+choloramphenicol for 7 to 10 days is recommended for primaryperitonitis.(c) OSTEOMYLITS–<strong>For</strong> more than 2 months cases inj amp+ +cloxa +genta is given for4-6 weeks along with surgical treatment . <strong>For</strong> less than 2 months cases inj ceftrixone( or cefotaxim)+ gentamycin +cloxacllin are given .(d) TETANUS–Inj crystalline penicillin (2lac IU /kg/ d / Q12h ) is given . Alternativeantibiotic is erythromycin.(e) TUBERCULER MENINGITIS–as per RNTCP guidelines.(f) PERTUSSIS–Macrolide (erythromycin for 10 days or azithromycin for 5 days) is thefirst choice. Other antibiotic are amoxicillin and cotrimoxazole.(g) HEPATIC COMA–Inj ceftriaxone +cloxacillin for 7 to 10 day along with bowel washwith ampicillin are done.(h) ACUTE ENDOCARDITIS–Inj Crystaline penicillin plus gentamicin for 3-4 weeks isgiven which is tailored depending upon culture & sensitivity report.VIII. ANTIBIOTIC POLICY FOR DEPARTMENT OF NEONATOLOGY• <strong>For</strong> early onset sepsis:1. Use injection Ampicillin and Gentamicin as 1 st line2. If extensive skin pustules or abscess, give Cloxacillin instead of ampicillin3. If no improvement in 48-72 hours, change to second line of antibiotics i.e. Injcefotaxime and amikacin.• <strong>For</strong> Meningitis and Late onset sepsis1. Use inj. Cefotaxime and amikacin asfirst line2. If evidence of staphylococca infection in form of skin pustules, give vancomycininstead of cefotaxime. Use ceftazidime, if pseudomonas infection is suspected.3. If no improvement in 48-72 hours, change to second line antibiotics i.e. inj. Vancomycin( if not given 1 st line) or Inj. Ciprofloxacin.24
4. Use Inj. Meropenam or Inj. Cefperazone- sulbactum or Inj. Piperacillin -Tazobactum ,Linezolid as thirds line antibiotic if culture sensitivity report shows multidrug resistanceor after consultation with the microbiologist.• <strong>For</strong> congenital Syphilis: Use penicillin (crystalline/Procaine)ANTIBIOTIC THERAPY OF NEONATAL SEPSIS1. Septicemia or pneumoniaAntibiotic Each dose Frequency Route Duration< 7 days age > 7 days ageInj. Ampicillin 50mg/kg/dose 12 hrly 8 hrly IV 7-10 daysORInj. Cloxacillin 50mg/kg/dose 12 hrly 8 hrly IV 7-10 daysANDInj. Gentamicin 5mg/kg/dose 24 hrly 24 hrly IV 7-10 daysORInj. Amikacin 15mg/kg/dose 24 hrly 24 hrly IV 7-10 days2. MeningitisAntibiotic Each dose Frequency Route Duration< 7 days age > 7 days ageInj. Ampicillin 100mg/kg/dose 12 hrly 8 hrly IV 3 weeksANDInj. Gentamicin 2.5mg/kg/dose 12 hrly 8 hrly IV 3 weeksORInj. Cefotaxime 50mg/kg/dose 12 hrly 8 hrly IV 3 weeksANDInj. Gentamicin 2.5mg/kg/dose 12 hrly 8 hrly IV 3 weeks• <strong>For</strong> Asymptomatic babies :1. In asymptomatic babies, presence of foul smelling liquor or two or more risk factorswarrants the initiation of antibiotic therapy2. A sepsis screen should be done in such infants3. If the sepsis screen is negative and infant remains asymptomatic at 48 -72 hours,the antibiotics may be discontinued.4. Risk factors for early onset sepsis are :(a) Maternal fever (Temperature > 37.9 o C ) before delivery or during labor(b) Membranes ruptured more than 24 hours before delivery.(c) More than three vaginal examinations during labor.(d) Low birth weight (
• If gram stain shows Chlamydia , use sulphacetamide (10%) eye drops .3. <strong>For</strong> oral thrush• Local application of 1% Clotrimazole / 0.25% gentian violetIX. GUIDELINES FOR THE USE OF ANTIMICROBIAL AGENTS IN NEUTROPENIC PATIENTSWITH CANCER.Principles :• Empirical antibiotic therapy should be administered promptly to all neutropenic patients atthe onset of fever.• Antibiotics chosen should• Provide adequate coverage of Pseudomonas aeruginosa• Be based on local antimicrobial susceptibility patterns of frequently identified bacterialpathogens,1. Definition(a) Fever: a single oral Temperature of 38.3 o C(101 0 F) or temperature of > 38.0 o C (100.4 0F) for > 1hour(b) Neutropenia : Neutrophil count < 500 cells/mm 3 or a count < 1000 cells /mm 3 witha predicted decrease to < 500 cells/mm 3 .2. Initial evaluation(a) Determine whether the patient is at high risk for complications – haematologicalmalignancy, bone marrow transplantation, Absolute neutrophil count (ANC)< 100 cells/cmm 3 , clinically unstable patient, clinically evident focus of infection, significant comorbidities.(b) Determine whether Vancomycin therapy is needed –evidence of i.v. catheterinfection, presence of severe mucositis, known to be colonized / infected with MRSA,clinically unstable patient ( Hypotension).3. Initial antibiotic therapy(a) Oral route :for low risk adult only, use ciprofloxacin + amoxicillin –clavulanate(b) Monotherapy when Vancomycin not indicated : cefepime 2 gm i.v. BD or Ceftazidime2 gm i.v. Q8H(c) Two drugs without Vancomycin : Amikacin (15mg/ kg i.v. Q24H) + piperacillin +Tazobactum ( 4.3 gm i.v. Q8h) or Cefepime ( 2 gm i.v. BD )or Ceftazidime (2 gmi.v. Q8H).(d) Vancomycin plus 1 or 2 antibiotics, if criteria for use of Vancomycin is met: As above+ Vancomycin ( 15 mg /Kg i.v. Q12h).4. Modification of therapy during the first week of treatment with duration of treatment<strong>Therapy</strong>A. Patient becomes afebrile in 3 days ·• Etiologic agent identified – adjust therapyto most appropriate drugs.• No etiologic agent identified :✓ Patient at low risk initially, and on oralantibiotics with no subsequentcomplications – continue use of the samedrugs✓ Patient at low risk initially and therapywith i.v.drugs begun with no subsequentcomplications – change to oralciprofloxacin + amoxicillin – clavulanateafter 48 hours .✓ Patient at high risk initially with nosubsequent complication – continue useof same i.v.drugsDuration1. Patient afebrile by day 3·• ANC ≥ 500cells /mm 3 for 2 consecutivedays, no definite site of infection, andno positive cultures – stop antibiotictherapy when the patient is afebrile for≥ 48 h.• ANC < 500 cells /mm 3✓ Patient initially at low risk , and nosubsequent complications –stop therapywhen patient is afebrile for 5-7 days✓ Patient initially at risk and no subsequentcomplications – continue same antibiotics26
B. Persistent fever throughout the first3 days :✓ Reassess therapy on day 3✓ If no clinical worsening , continue useof the same antibiotics.✓ Stop Vancomycin ( if part of initialregimen) if cultures negative✓ If there progressive disease, changeantibiotics ( Imipenem 0.5gm i.v.Q6H /Meropenem 1gmi.v.Q8H).✓ If patient febrile after 72-96 hours,consider adding Amphotericin B, withand without a change in antibioticregimen.✓ Additional indications for Amphotericin B/Voriconazole : Pleural rub, pulmonaryinfiltrates suggestive of invasiveaspergillosis, paranasal sinusitis.2. Persistent fever on day 3.• ANC ≥ 500cells /mm 3 – stop antibiotics4-5 days after ANC ≥ 500cells /mm 3 .·• ANC < 500 cells /mm 3 - reassess andcontinue antibiotics for 2 more weeks;reassess and consider stopping therapyif no disease site foundX. EMPIRICAL ANTIBIOTIC POLICY FOR ICUPATIENT RISK STRATIFICATIONPATIENT TYPE 1 (CAI) PATIENT TYPE 2(HAI) PATIENT TYPE 3(NI)Community Acquired <strong>Hospital</strong> Associated NosocomialInfection Infection InfectionNo contact with health Contact with health care Long hospitalization and/ orcare system system (e.g. Recent hospital invasive procedures within lastNo prior antibiotic treatment admission, nursing home, 90 daysNo procedures done dialysis without invasive Recent & multiple antibioticPatient young with few co procedure within last 90 days therapies- with in last 90 daysmorbid conditions Recent antibiotic therapy- Major invasive procedures donewith in last 90 daysStructural lung disease, AdvancedMinimum procedures done AIDS, Neutropenia other severePatient old with multiple co immunodeficiencymorbidities27
Presumptive treatment is based on above risk stratification.PATIENT TYPE 1 (CAI) PATIENT TYPE 2(HAI) PATIENT TYPE 3 (NI)Community acquired <strong>Hospital</strong> Associated Nosocomialinfection Infection infection1. Blood stream infections : possible pathogens Acinetobacter sp , Pseudomonas sp, E.coli , Klebsiella sp, , Staphylococcus aureus , Enterococcus sp, and Coagulase NegativeStaphylococcus (CONS).Ceftriaxone OR Ceftriaxone OR Imipenem OR Meropenem*Amoxicillin –Clavulanate OR Cefperazone –sulbactum OR +Cefperazone -sulbactum Ertapenem Vancomycin or Teicoplanin± Vanconycin /Teicoplanin *If prior exposure-Carbapenems±Amikacin use Colistin2. Complicated intraabdominal infections in ICU : possible pathogens Pseudomonas sp,E. coli , Klebsiella sp, Enterococcus sp.Ceftriaxone/ Cefotaxime Piperacillin + Tazobactum OR Meropenem OR Imipenem+ Metronidazole Cefperazone + Sulbactum OR + Vancomycin OR TeicoplaninErtapenem± Amikacin+ Vancomycin/ Teicoplanin3. Respiratory Tract Infections In ICU and VAP : possible pathogens Acinetobacter sp,Pseudomonas sp, E. coli , Klebsiella sp, , Enterobacter sp and Staphylococcus aureus.Ceftriaxone OR Piperacillin + Tazobactum OR Imipenem OR Meropenem +Co-amoxiclav, + Macrolide Cefopeazone + Sulbactum OR Newer Fluroquinolones +If Beta lactum allergy Ertapenem Linezolid or VancomycinLevofloxacin/moxifloxacin Add One of the following If prior exposure toOR Clindamyin+azetronam as per diagnosis Carbapene-use Colistin√ Aspiration after recentabdominal surgery -Clindamycin√ Renal failure, MRSA-Vancomycin/Teicoplanin√ Patients on high dose ofsteroids-Clarithromycin/Levofloxacin(Cover Legionella)4. Urinary Tract Infections in ICU: Possible pathogens Escherichia coli, Klebsiella spp.,Pseudomonas spp, Enterococcus sppNitrofurantoin OR Piperacillin + Tazobactum OR No exposure to CarbapenemCefuroxime OR Cefperazone + Sulbactum OR Imipenem OR MeropenemErtapenem OR Ertapenem Prior exposure to carbapenemFluroquinolonesColistin–until culture reportNOTE :1. Send samples for culture before starting antimicrobial therapy.2. Escalate/ descalate the antibiotic dose/ change as per the culture sensitivity report.3. Preferably choose narrowest spectrum antibiotic to which the isolated pathogen issusceptible28
4. Patients transferred from OT to the ICU. The surgical antibiotic policy should becontinued in ICU unless there is evidence and a change or withdrawl of antibiotic isrequired.Suspect VAP:1. If patient has(i) new or progressive radiographic infiltrate,(ii) new onset of fever,(iii) purulent sputum,(iv) leukocytosis,(v) decline in oxygenation.2. A clinical pulmonary infection score (CPIS) >6 highly suggestive of VAPObtain sample (ET aspirate or BAL) for quantitative culture before starting antibiotics asgiven above.After 48 to 72 hours, de-escalate antibiotics as per AST reports (if clinical improvement)Stop antibiotics after 7 to 8 days(From : Neiderman MS. Clin Infect Dis. 2006; 42 Suppl 2:S72-81)Central Venous Catheter (CVC) related blood stream infections (BSI)• Two sets of blood samples for culture (at least 1 drawn percutaneously) should be obtainedfrom all patients with suspected CVC related BSI• A positive culture result for a blood sample drawn through a CVC requires clinicalinterpretation (presence or absence of features of SIRS, MODS, hypotension), but anegative result excludes CVC-related bloodstream infection.• CVC should be removed and cultured if the patient has erythema or purulence overlyingthe catheter exit site, or clinical signs of severe sepsis (signs and symptoms of MODSand/or hypotension) Culture of catheter tips should be done only when catheter-relatedbloodstream infection is suspectedInterpretation of culture results:Scenario DiagnosisBlood culture negative; catheter tip negative Look for another sourceBlood culture positive; catheter tip negative CVC related BSI (if no other source evident)Blood culture positive; catheter tip positive CVC related BSIBlood culture negative; catheter tip positive Colonization. Consider CVC related BSI ifaccompanied by features of SIRS, and noother source evident(From: <strong>Guidelines</strong> for the management of intravascular catheter related infections. Clin Infect Dis.2001; 32:1249-72)XI.ANTIBIOTIC THERAPY FOR SURGICAL CASESI. Empirical antibiotic therapy for surgical cases1. Clean cases: Only one dose recommended at the time of induction. Repeat seconddose if surgery lasts for more than 4 hours.• Cefuroxime plus Metronidazole - for anaerobic cover if required. Add Gentamicin,if gram negative cover is required.29
2. Clean cases where contamination is suspected.The following surgical situations are recognized:(a) Road traffic accidents (RTA)(b) Biliary and GI surgery(c) Genitourinary systemRecommendation :(a) Road traffic accident : assess the extent and site of injuryCefuroxime or Amoxicillin – Clavulanic acid(With or without Metronidazole)(b) Biliary and GI surgeryCefuroxime or Cefperazone – sulbactum(With or without Metronidazole)(c) Genitourinary systemOfloxacin plus gentamicin3. Contaminated septicaemic casesEvidence of sepsis is likely to be present before surgery. If already on definitivetherapy this can be continued pre-operatively. However in case of no antibiotics arebeing used, empirical therapy with Beta-lactam – Beta-lactamase inhibitor combinationwith or without metronidazole to be considered. <strong>Therapy</strong> may vary with type and siteof infection.(a) Soft tissue infection – cover Staph. aureus(b) GI inections – cover E.coli and anaerobes(c) GU infections - E.coli and Pseudmonas spAll efforts should be made to establish bacterial infection from pus, body fluids.4. Surgical cases involving surgical implantsChoice IClindamycin + OfloxacinChoice 2Teicoplanin / Vancomycin + OfloxacinTwo doses recommendedDose 1 - at the time of induction of anesthesia,Dose 2 - 4 hours after surgery (except Teicoplanin / Vancomycin)XII.EMPIRICAL ANTIBIOTIC THERAPY FOR CARDIAC SURGERYInjection Ceftriaxone 2gm IV twice daily / Injection Co-Amoxyclav1.2 gm IV 8 hourly ×72 hours.(Change protocol every 6-9 months based on clinical and microbiological reports)XIII. EMPIRICAL ANTIBIOTIC THERAPY FOR PAEDIATRIC SURGERY1. Day Care Surgery(a) Clean cases (hernia, circumcision, orchidopexy): Single dose of Inj. Cefuroximebefore the induction.2. Clean contaminated cases :Major: Abdomial, thorcic, surgery, bowel resection, hydronephrosis, tracheooesophagealfistula repair: cefuroxime , cefotaxime + gentamicin30
3. Contaminated cases , appendicitis/peritonitis :(a) Cefotaxime + Amikacin with or without Metronidazole(b) Clindamycin + Amikacin4. Special cases(a) MRSA/MRSE: Vancomycin/ Teicoplanain(b) Prophylaxis for UTI : Co-Trimoxazole (Septran)/CephalexinXIV. EMPIRICAL ANTIBIOTIC THERAPY FOR NEUROSURGERYNote: No antibiotics for clean cases other than chemoprophylaxis.Routine use: Cefuroxime + Gentamicin1. Fracture Skull with CSF leak: same as above. Look for evidence of infection and useevidence based defnitive therapy.2. Neurosurgery lasting less than 4-6 hours: Single dose of Cefuroxime before induction.3. Neurosurgery lasting more than 4-6 hours (2 doses): Cefuroxime + Amikacin. Firstdose at induction and 2 nd dose after 8 hours.4. Community acquired bacterial meningitis in immunocompetent cases: Ceftriaxone.5. Elderly group and immunocompromised patients with bacterial meningitis: Cefotaxime/Ceftriaxone with or without Vancomycin.6. Shunt associated infections: Cefuroxime (in case of strong clinical evidence MRSA:Vancomycin / Teicoplanin).7. Complicated meningitis: 3 rd Generation cephalosporins (Ceftriaxone) + Amikacin with orwithout Vancomycin.8. Brain abscess: Piperacillin /Piperacillin - Tazobactum with or without Metronidazole.XV. EMPIRICAL ANTIBIOTIC THERAPY FOR ORTHOPEDICS1. Clean non infected cases with minor implants (K wires) / no implants✓ Inj. Cefazolin 1gm i.v.Q8H OR Cefuroxime 1.5gm i.v. Q12H + Gentamicin 80mg i.v.Q12H OR Amikacin 500mg i.v. Q12H for 3 days2. Surgeries with major implants (T.H.R / T.K.R)✓ Inj. Cefazolin 1gm i.v.Q8H OR Cefuroxime 1.5gm i.v. Q12H + Inj Gentamicin 80mgi.v. Q12H OR Inj Amikacin 500mg i.v. Q12H for 5 days✓ In selected cases ( High risk/ immune-compromised patients )- Inj Gentamicin 80mg i.v.Q12H OR Inj Amikacin 500mg i.v. Q12H + Teicoplanin 10mg/Kg i.v. Q12H OR Vancomycin15 mg /Kg i.v. Q12H for 5 days3. Open Injuries /Fractures✓ Inj. Cefazolin 1gm i.v.Q8H OR Cefuroxime 1.5gm i.v. Q12H + Gentamicin 80mg i.v.Q12H OR Amikacin 500mg i.v. Q12H + Inj metronidazole 500 mg i.v. Q8H✓ Gas gangrene : Penicillin G 10 lac units i.v.Q4H + Clindamycin 600 mg i.v. Q8H +Gentamicin 80mg i.v. Q12H OR Amikacin 500mg i.v. Q12HXVI. ANTIIBIOTIIC POLICY FOR OBSTETRICS AND GYNAECOLOGY1. EMPIRICAL ANTIBIOTIC THERAPY FOR OBSTETRICS AND GYNAECOLOGYConditionCommonAlternate antibioticsorganismsAntibiotic of choiceand commentsClean surgical wound Mainly skin Cefazolin 1 g i.v. x Administer only afterElective LSCS without bacteria 1 dose clamping of the cordlabor, PROM31
Clean episiotomy andNo antibioticsminor tearClean contaminated Inj Ampicillin 500mg 6 1 st dose being givensurgical wound – LSCShourly + Inj Gentmicin 1.5 0-60 minutes prior toin labour or with PROM,mg/Kg every 8 hourly+Inj skin incision.Vaginal and Total Metronidazole 500mg 8Abdominal hysterectomyhourly for 24-48 hours(VH and TAH),radicalsurgery for malignancyPerinatal Group B Group B Ampicillin 1g.i.v q 6h; in Group b Streptococci (GBS)Streptococcal infection Streptococci labour, or after membranes UTI during pregnancyrupture (which ever is should be treated and theseearlier) until delivery. women should get GBSprophylaxis in labour orafter membrane rupture.Routine screening for GBSby vaginal culture is notrecommended.Valvular heart disease Streptococci Ampicillin 2 g i.v. +Gentamicin 1.5 mg/Kgi.v. stat. Follow upwith Ampicillin 1.0 g i.v.after 6 hoursManual removal of Vagianl and Ampicillin 1 g p.o stat andPlacenta OR 3 rd or 4 th perineal flora Inj Metronidazole 500mg i.vdegree perineal tearsstat and repeat 6H laterSeptic abortion Polymicrobial Inj Ceftriaxone 2g i.v BD+ Modify as per culture reportPelvic abscessInj Amikacin 500 mg i.vPeritonitisBD with Inj Metronidazole500 mg i.v 8H for 5-7daysElective minor A single dose of cap 1 st dose given 0-60 minprocedures ( MTP, MTP Amoxiciilin/Ampicillin/ prior to skin incisionwith ligation, D & C ,Co-Amoxclav OR Injendometrial aspiration)Ceftriaxone 2g i.v.BD+InjAmikacin 500mg i.v.BDfor 5-7 days with InjMetronidazole 500 mg i.v.8H for 24-48 hours.Local wound infection Mainly skin, No systemic infectionanaerobic ✓ No systemic antibioticsbacteria and ✓ Only local wound carevaginal flora with antiseptics andantibacterial agentsWith systemic signs Modify as per culture✓ Inj Ceftriaxone -2gm IV report.BD for 48 hour followedby Ceftriaxone 1gm IV Remove sutures and drainBD for 5-7 days plus pus if requiredInj Amikacin 500mg IVBD for 5 days with orwithout Metronidazole32
Asymptomatic bacteriuria E.coli Tab Nitrofurantoin 100mg To be started after collectingin pregnancy 6H for 3 days urine for culture sensitivityCystitisPost operativeTab Co-Amoxyclav 625mg Consult ID Physicianrespiratory tract infection8H x 10dORTab LevofloxacinPost operative fever Multiple Intermittent fever Consult ID Physicianwith no localizing signs etiology ✓ Course of chloroquine Identify and treat cause-malaria, Continous fever ,toxicenteric fever, ✓ Inj Ceftriaxone -2gm IVUTI, BD for 48 hour followed Collect appropriate samplesby Ceftriaxone 1gm IV before starting therapy.BD for 5-7 days plusInj Amikacin 500mg IVBD for 5 days with orwithout Metronidazole.If no response 48 hrs✓ Inj Clindamycin +Gentamicin till culturereport available2. Management of OPD Patients(a) PID1 st : line: Tab Cefixime 400mg Plus Tab Doxycycline 100mg BD × 14 days Plus TabMetronidazole 400mg BD × 14 days2 nd line: Tab Ofloxacin 200mg BD × 14 days Plus Tab Metronidazole 400mg BD ×14 daysNote : Partner treatment: Tab Cefixime 400mg stat. Plus Tab Azithromycin 1 gmstat(b) Vaginal infection ( Vaginitis )Tab Fluconazole 150mg stat Plus Tab Tinidazole 2 gm stat.During 1 st trimester of pregnancy: Miconazole/Clotrimazole and Tinidazole vaginalsuppository.During 2 nd trimester of pregnancy: Tab Metronidazole 400mg BD × 7 days(c) CandidiasisTab Fluconazole 150mg stat OR Clotrimazole vaginal pessary 100 mg HS ×7 daysOR Clotrimazole vaginal pessary 200 mg HS ×3 days OR Miconazole vaginal pessary100 mg HS ×7 days OR Miconazole vaginal pessary 200 mg HS ×3 daysRecurrent candidiasisTab Fluconazole 150 mg on day 1, 4, and 7 then weekly × 6 monthsItraconazole 2 BD TabXVII. EYE, EAR, NOSE AND THROAT (ENT) AND ORAL INFECTIONS1. Purulent Conjunctivitis: Chloramphenicol 0.5% eye drops or 1% eye ointment every4-6 hours, continuing for 3 days after symptoms have resolved.2. Orbital Cellulitis Commonest causative organism: Haemophilus influenzae, Staph.aureus.Cefotaxime IV 1 - 2g TDS Plus Metronidazole IV 500mg TDS Plus Flucloxacillin IV 1g QDS33
3. Corneal Ulcer : Oflox/ Ciproflox/Moxiflox Plus Amikacin/Gentamicin Plus Natamicin eyedrops4. Endopthalmitis: Local antibiotics as corneal ulcer plus systemic antibiotics5. Otitis Media: AcuteAmoxicillin PO 500mg TDS for 5 days OR Erythromycin PO 250-500mg QDS for 5 days6. Otitis Media: Chronic : Co-amoxiclav PO 625mg TDS for 7 days OR Doxycycline 200mgstat, then 100mg OD Plus Metronidazole PO 500mg TDS (Treat for 7 days)7. Otitis externa: Gentisone HC Ear Drops, Instil 3 drops 3-4 times daily and at night ORSofradex Ear Drops, Instil 3 drops, 3-4 times daily OR Otomize Spray, 1 metered sprayTDS for 10 daysFlucloxacillin PO 500mg QDS for 5days8. Malignant Otitis Externa:Commonest causative organism: Pseudomons sp.Ceftazidime IV 1-2g TDS OR Ciprofloxacin PO 750mg BD (or IV 400mg BD if oral routeis contraindicated)6. Sore Throat:Most cases are of viral aetiology. If, however, the onset is dramatic with high temperature,bacteriological investigations are indicated. Take swab exudates of pus from the inflamedarea.7. Streptococcal Tonsilitis:Penicillin V PO 500mg QDS for 10 days, OR Erythromycin PO 250-500mg QDS for 10days, ORClarithromycin PO 500mg BD if intolerant of erythromycin8. Epiglottitis: Cefotaxime IV 1g TDS9. Oral candidiasis:Nystatin mouth Suspension 1ml QDS for 7-14 days. Swill round the mouth for 1 min thenswallow.OR Amphotericin B Lozenges qds OR <strong>For</strong> resistant cases: - Fluconazole PO 50 mg ODfor 7-14 days10. Angular Cheilitis:Miconazole oral gel, 5ml QDS for at least 2 weeks or until all clinical signs and symptomshave resolved.XVIII. DEPARTMENT OF BURNS AND PLASTIC SURGERYANTIBIOTIC POLICY FOR BURNS PATIENTI. Prophylactic antibioticsProphylactic antibiotic in burns are indicated in all admitted patients.• Patient without Tetanus immunizationInj Crystalline PenicillinInj Gentamicin•· Patient coming to hospital after 48 hours and without any culture reportInj Amoxicillin + Clavulanic acidInj Gentamicin34
II.Empirical <strong>Therapy</strong>• 1 st Line antibiotics - for patients who develop fever or any sign/symptom ofinfection without microbiological proof of infection.Inj Ceftazidime or Inj Ciprofloxacin + Inj Amikacin• 2 nd line 3 therapy or Curative therapy – Given on basis of pus culture andsensitivity report. <strong>For</strong> Gram negative: Inj Cefoperazone + Sulbactum OR Piperacillin + TazobactumPlus Netilmicin In Gram negative resistant to above: Ertapenem OR Meropenem OR Imipenem.(Ertapenem is not used for Pseudomonas)• 3 rd line therapy : <strong>For</strong> multidrug resistant organism <strong>For</strong> Gram Negative : Injection Colistin, Inj. TigecyclineTigecycline used as monotherapy for soft tissue infections and combinationtherapy for blood stream infections. <strong>For</strong> Gram positive (MRSA): Inj Vancomycin OR Inj Clindamycin OR Inj Teicoplanin.III. Indication for antifungal agentsPatient with extensive burn not responding to 3 rd line therapy• Empirical therapy : azoles Inj Fluconazole• After culture report: Non albicans candida - Caspofungin.Amphotericin B is toxic to all burn patient as renal system compromised, henceCaspofungin is used.ANTIBIOTIC POLICY FOR PLASTIC SURGERYAntibiotic used in peri-operative periodInj Amoxy-Clav or Inj Ceftriaxone Or Inj CefotaximePlusInj Amikacin or Inj GentamicinAfter 4-5 days switch to oral antibiotics, which include Tab Amoxy + Clavulanic acid OrTab Cefuroxime Or Tab CiprofloxacinXIX. ANTIFUNGAL THERAPYFungal therapy is usually started based on positive cultures or systemic evidenceof fungal infection. It is advised to take paired cultures if fungal infection issuspected. Evidence includes persistent sepsis / SIRS despite broad spectrum antibiotic(exclude sepsis, abscess, drug fever, DVT etc). Treat according to identification andsensitivity of Candida isolate.Fluconazole IV/oral 400mg OD if fluconazole naïve or sensitiveOr2 nd line Caspofungin IV (for Candida krusei and C. glabrata as inherently resistant toFluconazole.) Caspofungin dose: 70mg on Day 1 (loading), 50mg OD (80kg) thereafter.Moderate to severe hepatic dysfunction: reduce the subsequent daily dose to 35mg OD.Check for drug interactions.Or3 rd line – Ambisome / Liposomal Amphotericin B IV 3mg/kg OD. (As Caspofungin isinherently inactive against Zygomycetes, Cryptococcus, Fusarium and Trichosporon Spp)To be decided by Microbiologist / Intensivists based On Patient’s Hepatic / RenalFunctions/ Severity of Infection / Drug Interactions e.g. Rifampicin, Carbamazepine,Phenytoin, Efavirenz, Nevirapine, Cyclosporin, Dexamethasone, Tacrolimus etc.35
XX.ALERT ANTIBIOTICS: GUIDELINES FOR OPTIMISING USE OF KEY ANTIMICROBIALSTo Prevent and Control the Emergence and Spread of <strong>Antimicrobial</strong>-Resistant Microorganismsin <strong>Hospital</strong>s” one major strategic goal is to “define guidelines for use ofkey antibiotics”, injectables (“Alert” antibiotics) targeted in these guidelines areCiprofloxacin, Ceftazidime, Cefotaxime, Ceftriaxone, Vancomycin (or Teicoplanin),Imipenem, Levofloxacin, Meropenem, Moxifloxacin, Tazocin, Linezolid (oral/IV),Voriconazole, Caspofungin, Valganciclovir, Ertapenem and Newer Preparations ofAmphotericin.Collectively, these are among the drugs most frequently prescribed irrationally which islargely responsible for the current escalation of antibiotic costs. They also account fora significant proportion of serious antibiotic toxicity including Clostridium difficile diarrhoeaand CNS toxicity/seizures as well as the emergence of major antimicrobial resistance.Safer, cheaper and equally effective alternatives are often available which allow suchagents to be kept in reserve for occasions when there are clear cut microbiologicalindications. It is critical, therefore, that these Alert antibiotics be prescribed only on therecommendation of senior medical staff or after discussion with the on-call Microbiologistor ID physician.ALERT ANTIBIOTICS AND THEIR INDICATIONS1. CIPROFLOXACIN, INTRAVENOUSOral ciprofloxacin is well absorbed and this is therefore the preferred route of administration.Intravenous therapy is only indicated in the following situations:• When the patient is unable to swallow or the oral route is otherwise compromised·• In serious sepsis (e.g. nosocomial pneumonia in ITU) when the recommended doseis 400mg 8 hourly.Indications for Ciprofloxacin in the Antibiotic Policy, either alone or in combination,are as follows:• second line therapy in exacerbation of chronic bronchitis• pyelonephritis• acute inflammatory infective diarrhoeas• serious infected diabetic ulcers, infected burn wounds with coliforms or Pseudomonasinfection present• treatment of documented or presumed gram-ve bacilli resistant to penicillins orcephalosporins or when the patient is allergic (history of anaphylactic reaction orrash) to these agents• selected haematology patients requiring prophylaxis• severe acute pelvic inflammatory diseaseNote: Fluoroquinolones are the only oral agents with activity against Pseudomonasaeruginosa2. CEFTAZIDIMELimited use only. Main indication is documented or suspected Pseudomonas aeruginosainfection. Other indications currently listed in the Antibiotic Policy are as follows:• Second line agent in neutropenic patients with septicaemia or pneumonia• Empiric therapy of CAPD associated peritonitis (not children), 1g IV stat then 125mg/litre in each bag• Empiric therapy of post operative, post traumatic or shunt associated meningitis• Empiric therapy of infective exacerbation of cystic fibrosis3. PIPERACILLIN + TAZOBACTUMCurrently listed in the antibiotic Policy for the following:• Pneumonia or septicaemia in neutropenic patients (+ Gentamicin)• As a single agent (or in combination with Gentamicin) for treatment of sepsis whichhas not responded to first line treatment or if it is not appropriate for gentamicin tobe added to first-line therapy.36
4. CEFTRIAXONEIV Ceftriaxone is currently listed in the Antibiotic Policy for the following:• Epiglottitis,• Brain abscess,• Bacterial meningitis,• Pyelonephritis in children,• Empiric therapy of septicaemia in children,• In ascites for treatment of sub-acute bacterial peritonitis,• Skin and soft tissue infections managed via out-patients or the home IV antibioticprogramme,• Acute septic monoarthritis if penicillin allergic,• Spontaneous bacterial peritonitis.5. APPROPRIATE USE OF CARBEPENEMS• Very high rates ( 60-75%) of resistance to 3 rd and 4 th generation cephalosporins {dueto extended spectrum beta-lactamases (ESBL) production} observed in E. coli andKlebsiella species at <strong>Safdarjung</strong> Hospaital.• This pattern of resistance although seen primarily among nosocomially acquiredinfections, is also seen isolates of E coli and Klebsiella species isolated fromcommunity acquired infections.• These strains of bacteria are frequently resistant to other major classes of antibiotics(fluoroquinolones, β-lactam + β-lactamase inhibitor (BL + BLI) combinations andaminoglycosides)• Carbapenems (Imipenem, Meropenem and Ertapenem), â-lactam antibiotics withexceptionally broad spectrum of activity, are the only class of antimicrobials whichremain effective against ESBL-producing isolates of E coli and Klebsiella species• Imipenem is susceptible to degradation by the enzyme dehydropeptidase-1 (DHP-1)located in renal tubules and requires coadministration with a DHP-1 inhibitor cilastatin.Meropenem and Ertapenem are administered without a DHP-1 inhibitor.Indications for carbapenem use:1. Infections [e.g., bacteremia, pyelonephritis, intra-abdominal infections (peritonitis, cholangitis,abscesses), nosocomial pneumonia etc.] confirmed (by appropriate culture and susceptibilitystudies) to be caused by Gram-negative bacteria (E coli, Klebsiella spp., Enterobacter spp.,Pseudomonas aeruginosa, other non-fermenting Gram-negative bacilli) resistant to otherclasses of antimicrobials and susceptible only to carbapenems in-vitro2. Initial empiric treatment for severe, life-threatening infections (associated with multi-organdysfunction, septic shock) caused by Gram-negative bacteria.• Febrile neutropenia• Ventilator associated / nosocomial pneumonia• Pyelonephritis / complicated urinary tract infections• Complicated intra-abdominal infectionsOnce the culture and susceptibility reports are available, choose the most appropriateantibiotic based on spectrum of activity, toxicity and cost (‘de-escalation’).Indications for Ertapenem use: Ertapenem has excellent in-vitro and in-vivo activityagainst ESBL producing Enterobacteriaceae, but lacks activity against Pseudomonasaeruginosa, and is therefore not considered appropriate for the treatment of conditionslike febrile neutropenia and serious nosocomial infections. Ertapenem does not selectCarbapenem-resistant Pseudomonas aeruginosa (at least in the short-term). Its use shouldbe restricted to severe Gram-negative or polymicrobial community acquired infectionsconfirmed to be caused by susceptible bacterial pathogens. Hence, this drug may berecommended as the initial choice for ESBL producing strains of E coli and Klebsiella.37
Indication of Meropenem and ImipenemBut both Meropenem and Imipenem regarded as third line agents and are reserved for:• serious infections due to multiple resistant strains (e.g. ESBL)• empiric use in the seriously ill patient in either ITU or Haematology• the treatment of infective exacerbations in Cystic fibrosis (CF)• severe acute necrotising pancreatitis• Outside these clinical settings it should only be used after consultation with aMicrobiologist or ID physician.Unlike Imipenem , Meropenem has not been associated with CNS toxicity. Also, it isadministered by convenient IV bolus injection. Clinicians must be aware that mechanismof resistance to Meropenem and Imipenem are different and hence in-vitro test for onecarbapenem cannot be used to interpret the other.DoseImipenem* : 500 mg i.v. Q6HMeropenem : 1 gm i.v.Q8HErtapenem : 1gm i.v. /i.m.Q 24H*Note Anti-infective Sub-committee recommends use at a more frequent dosinginterval. They believe that optimum plasma concentrations are more reliablymaintained with 6-hourly dosing.6. LINEZOLID (IV AND ORAL FORMS)Linezolid should only be prescribed after consulting an ID specialist ormicrobiologist and a mandatory order form completed.• Restricted indications including infections due to proven glycopeptide-insensitiveStaphylococcus aureus or Vancomycin-resistant enterococcus (currently uncommon).• To enable IV/oral switch from IV Vancomycin (used for MRSA or MRSE) to oralLinezolid (when patient discharge is possible and continuation treatment using combinationrifampicin /trimethoprim is inappropriate.• May be an option in surgical site infections (e.g. large bowel surgery, vascular surgery,etc).• Poor IV access and a glycopeptide is indicated.• Use in out-patient home parenteral antibiotic therapy for skin and soft tissue infectionsas an alternative to IV Teicoplanin.• Rare cases of proven hypersensitivity/allergy to the glycopeptides.7. VANCOMYCINVancomycin is the drug of choice for in-patient treatment of the following infections.• Serious (e.g. bacteraemia, osteomyelitis) coagulase negative staphylococcal andMRSA infections and penicillin resistant enterococcal infections• Empiric therapy in febrile neutropenic patients not responding to first line therapy• Continuous ambulatory peritoneal dialysis (CAPD) associated peritonitis• Prosthetic valve endocarditis8. TEICOPLANINTeicoplanin is a suitable alternative to Vancomycin only for:• patients receiving out-patient/home parenteral therapy with glycopeptides• inability to tolerate Vancomycin• oncology/haematology patients• Rare cases of Vancomycin resistant and teicoplanin sensitive strains.XXI. TREATMENT OF MUTI-DRUG RESISTANT BACTERIAL PATHOGENS :1. Methicillin- resistant S. aureus (MRSA)(a) These organisms are considered resistant to all penicillins, Cephalosporins and Macrolides.(b) Though MRSA strains may be reported as susceptible to Fluoroquinolones,Aminogycogides, Chloramphenicol and Doxycycline in-vitro, these drugs are NOT tobe used alone or as initial treatment for serious MRSA infections.38
(c)(d)(e)(f)Similarly Rifampicin is not to be used as monotherapy for MRSA infectionsThe drug of Choice for treatment of infections due to MRSA is the glycopeptidesi.e Vancomycin and Teicoplanin.Linezolid can be used to treat skin and soft tissue infections caused by MRSA.Mupirocin local application (intranasally bid x 5 days ) for eradicating nasal carriage.2. Extended spectrum â-lactamases (ESBL) producing Klebsiella sp and E.coli.(a) ESBLs are plasmid mediated â- lactamases that confer resistance to broad spectrumβ- lactum antibiotics including third and fourth generation Cepahlosporins, Azetronam,and extended spectrum penicillins. These plasmids often encode mutations whichconfere resistance to other broad spectrum agents including Aminoglycosides , Cotrimoxazoleand Fluoroquinolones, resulting in organism resistant to most broadspectrum antibiotics.(b) A major problem with ESBLs is their capacity to cause therapeutic failure withCephalosporins and Azetronam when host organism appears to be susceptible to theseagents in laboratory tests. Hence CLSI recommends that laboratories should reportESBL producing isolates as resistant to all penicillins, Cephalosporins ( includingCefepime and Cefpirome), and azetronam irrespective of the in-vitro test results.(c) The emergence of ESBL producing enterobacteriaceae is realted to indiscriminate useof third generation cephalosporins.(d) The carbapenems ( Ertapenem, Meropenem and Imipenem ) are currently consideredthe drug of choice for serious infections caused by these pathogens . Piperacillin–tazobactam and Cefperazone sulactum may be considered options in mild infectionsand when ESBL producers are demonstrably susceptible in –vitro.(e) Recommended measures to control spread of ESBL producing organism :(i) Improved lab detection and reporting of ESBL(ii) Enhanced infection surveillance and control in ICUs(iii) Prevent spread by barrier precautions : Gowns and gloves(iv) Hand Washing(v) Restricted use of 3 rd generation Cephalosporins3. Carbapenem resistant Klebsiella sp and E.coli.✓✓✓✓✓(a) Mechanism of resistance :Combinations of ESBL or AmpC and porin loss: Porin loss is often unstable and mayimpose a fitness cost, meaning that these strains rarely spread. Ertapenem is particularlyaffected.Acquired carbapenemases(b) TreatmentMost carbapenemase producers are extremely drug resistant : being resistant to â-lactamantibiotics, aminogycosides, and â-lactam –âlactam inhibitor combinations..Polymyxins, Tigecycline & Fosfomycin are the agents with most frequent in vitroactivity, but all have limitations. Dosage will vary with the patient and infection site, butshould be on the principle of ‘highest safe’ rather than ‘minimum potentially effective;durations should be as standard for the infection type.Colistin - Case reports of successful use in a range of infections due to Carbapenemaseproducers .Tigecycline : Active in vitro vs. most carbapenem-resistant E. coli. Licensed for skin andsoft tissue and complicated intraabdominal infections. Case reports of success in variousinfections with carbapenemase producers. Low blood concentrations; off-label use shouldbe cautious for blood stream infections, unsuitable in urinary infections as only 22%excreted in urine. Excess deaths in some trials, esp. ventilator pneumonia (not a licensedindication).Others : a few isolates are susceptible to other antibiotics including e.g. Chloramphenicol,Ciprofloxacin and Cotrimoxazole. Most producers, however, are resistant to these drugs39
XXII. DOSAGE GUIDE FOR COMMONLY USED ANTIMICROBIAL AGENTSANTIBIOTIC ADVERSE REACTION ROUTE PAEDIATRIC DOSE ADULT DOSEAmikacin Nephrotoxicity, Intravenous 15-22.5 mg/Kg/day 15mg/Kg/day qOtotoxicity in 2-3 doses 8-12 hours, maxdoses 1.5mg/KgAmoxycillin Fever, rash, diarrhoea, Oral 20-50 mg/Kg/day, 250-500 mg qabdominal cramps, 3-4 doses 8 hourlyAST ALT elevation.Amoxycillin- Rash, diarrhoea, Oral 40 mg/Kg/day 375 mg 8 hourlyabdominal camps, AST ( amoxicillin) in 2 625-1000 mg 12clavunate ALT elevation doses hourly(co-amox-90mg/Kg/day ifyclav) penicillin resistant S.pneumonia suspectedin otitis mediaIntravenous 100 mg/Kg/dayAmpicillin Hypersensitivity Intravenous 100-400 mg/kg/day 500 mg-1 gm q 6reaction, nausea, or in 4 doses( IV) hourlydiarrhoea, exfoliative oraldermatitis, seizures,precipitates infectiousmononucleosis rash,interstitial nephritis.Azithromycin Leukopenia, transient Oral 10 mg/Kg/day 500mg dailyelevation of liveronce dailyenzymes, renal toxicity.Enteric fever 20 mg/Kg/day once dailyAzetronam Rash, Diarrhoea Intravenous 90-120 mg/Kg/day 1-2 g q 8 hourly ,vomiting, AST, ALT q 6-8 hrly Max dose 8 gmelevation In cystic fibrosis in 24 hoursmax dose 200mg/Kg/dayBenzathine Hypersensitivity, and Intramuscular 1,200,000 units 1.2-2.4 million unitspenicillin Jarisch Herxheimer ( > 30 Kg) /dosereaction, haemolyticanemia, seizures600,000 unitswith high doses in( < 30 kg)renal failureCefadroxil Rash eosinophilia Oral 30 mg/Kg/day in 500mg bid or 1 g2 doses bidCefazolin Leukopenia, eosinophilia, Intravenous 100 mg/Kg/day 3-4 0.5-2 gm q 6-8rash, transient elevation divided doses hourlyof liver enzymes,renal toxicity.40
ANTIBIOTIC ADVERSE REACTION ROUTE PAEDIATRIC DOSE ADULT DOSECefepime Same as third generation Intravenous 1-4 gm/day 2-3cephalosporins. adjustdosesdose in renal failureCefixime Diarrhoea, leukopenia, Oral 15 mg/kg/day in 400 mg/day in 1-2renal toxicity, 2 divided doses divided dosestransient elevation of20 mg/kg/day inliver enzymes.2 divided dosesfor enteric fever.Cefotaxime Arrythmia, transient Intravenous 100 mg/kg/day 1-2 gm 6-8 hourlyelevation of liverin 3-4 dividedenzymes, renaldoses 200 mg/kgtoxicity./day in 4 divideddoses for meningitisCeftazidime Hypersensitivity reaction, Intravenous 75-100 mg/kg/day 1-2 g q 8 -12 hourlydizziness, rash, diarrhoea, in 3 divided doses (IV)colitis, exfoliative Intramuscular 100 mg/kg/daydermatitis, in meningitis (IV)thrombocytopeniaCeftriaxone Gall bladder sludging, Intravenous 50-100 mg/kg/day 1-2 gm q 12-24transient elevation of in 2 divided doses hourlyliver enzymes, renal Meningitis 100toxicity mg/kg/day in 2divided dosesCefuroxime Leukopenia, eosinophilia, Intravenous 75-100 mg/kg/day in 750mg -1.5g qallergic reaction, 3 divided doses 8hourlytransient elevation ofliver enzymes, renaltoxicityCefuroxime Leukopenia, eosinophilia, Oral 20-30 mg/kg/day in 250- 500 mg bidaxetil allergic reaction, transient 2 divided doseselevation of liverenzymes, renal toxicityCephalexin Transient neutropenia, Oral 30-40 mg/kg/day in 250-500 mg q 8AST and ALT 3 divided doses hourlyelevation, arthralgia,rash, eosinophilia.Chloram- Bone marrow Oral 75-100 mg/kg/day in 50 mg/kg/day in 4phenicol suppression, aplastic 4 divided doses divided dosesanaemia , grey baby Intravenous Avoid in infantssyndrome, hemolysis inless than 3 monthsG6PD deficiencyCiprofloxacin Nausea, vomiting, Oral 20-30 mg/kg/day in 250-750 mg q 12abdominal discomfort, 2 divided doses hourlyarthralgia, photosensitivity Intravenoustransient elevationof liver enzymes,41
ANTIBIOTIC ADVERSE REACTION ROUTE PAEDIATRIC DOSE ADULT DOSEClarithro- Transient elevation of Intravenous 15 mg/kg/day in 2 250-500 mg bidmycin liver enzymes, divided dosesrenal toxicity, nausea, Oralabdominal crampsClindamycin Diarrhoea, nausea, Oral 40-60 mg/kg/day in 150-300 mg q 6-8pseudomembranous 3-4 divided doses hourly(oral,iv)colitis, skin rash, Intravenous Severe infectionsErythema multiforme, 300-600 mg 8raised ALT AST,hourly IVthrombocytopenia,leucopeniaCloxacillin Dose related Oral 50-100 mg/kg/day 250-500 mg/kg/dayneutropenia, elevated Intravenous in 3-4 divided in 3-4AST, ALT, Cholecystitis, doses. divided dosesinterstitiaL nephritis. 100-200 mg/Kg/day 1-2 gram q 6 hourly.divided q 6 hourlyCo- Megaloblastic anaemia, Oral 5-10 mg/kg/day in 160 mgtrimoxazole disturbance, rash, 2 divided doses ( Trimethoprim) biderythema multiforme(5-0 mg trimethoprim).major/minor 20 mg/kg/day in 4divided doses inpneumocystisjiroveci pneumoniaErtapenem Diarrhoea, nausea, Intravenous 3-12 years : 15 13 years and abovevomiting, headache, Intramuscular mg/Kg twice daily. 1 gm IVhallucination, seizures, (not to exceed infusion/IM oncearrhythmia, 1gm/day) daily in 3-5 mlpseudomembranousof lidocaincolitis, dose reduction inCI ifrenal failurehypersensitivity tolidocaine/β lactamErythro Arrhythmia Jaundice Oral 40 mg/kg/day in 250- 500mg qmycin 4 divided doses 6hourlyFurazolidine Avoid alcohol, Oral 100 mg 3-4 100mg 3-4 timestyramine containing times a day a dayfood, MAO inhibitors, 5mg/Kg in 3-4Nausea headache,divided doses (notdizziness, fall in BP,below one year)urticaria, safety inpregnancy unknown.Gentamicin Nephrotoxicity Intravenous 5-7.5 mg/kg/day in 1.3-6 mg/kg/day inototoxicity and optic Intramuscular 2-3 divided doses 3 dividedneuritisdosesImipenem- Nausea vomiting Intravenous 75-100 mg/kg/day 2-4/day in 4cilastin seizures in 3-4 divided divided dosesLevofloxacin Nausea, diarrhoea, rash Oral Intravenous 500mg once daily42
ANTIBIOTIC ADVERSE REACTION ROUTE PAEDIATRIC DOSE ADULT DOSELinezolid Peripheral and optic Oral 10mg/kg/dose 6-8 400-600 mg q 12neuropathy, Intravenous hourly (oral,IV) hourlythrombocytopenia,hypertension,myelosuppression,colitis.Meropenem Hypotension, transient Intravenous 60 mg/kg/day in 3-4 1.5-3 gm/day in 3elevation of Intramuscular divided doses divided dosesliver enzymes, renal (IV) 6 gm /day inmodification in divided doses in meningitisrenal failuremeningitisMetronidazole Nausea, metallic taste, Intravenous 7.5 mg/kg/day /dose 500-700 q 8hourlydisulfuran like Oral 3-times/dayreaction with alcohol,30-50 mg/kg/day inperipheral neuropathy3 divided dosesfor liver abscessNalidixic Hepatotoxicity, myalgia, Oral 55mg/kg/day in 3 1 gm 4 times/dayacid leukopenia, vertigo, divided dosesrash, dizziness,pseudotumor cerebri,seizure, avoid inG6PD deficiencyNitrofuran- Discoloration of urine, Oral 8 mg/kg/day in 2 50-100 mg q 6toin vertigo,rash, divided doses hourly. ( 5-7methemoglobinemia,mg/kg/day incholestatic jaundice,4 divided doses)hepatocellular damagemax dose 400mg.and neuropathy. Avoidat term and labourNorfloxacin Same as quinolones Oral 20-30 mg/kg/day in 200-400 mg twice2 divided doses dailyOfloxacin Leukopenia , transient Oral 20 mg/kg/day in 200-400 qelevation of liver enzymes, 2 divided doses 12 hourlyrenal toxicity. May intravenousprecipitatepsychosis/seizures,photosensitivity.Penicillin G Hypersensitivity Oral 50,000 units/kg/reaction like anaphylaxisdose 6 hourlyrare.nonfatal reactions(oral)are like serum sickness,rash contact Intravenous 200,000-400,000 2-24 million units /dermatitis seen in 1 units /Kg/day in 4 day in dividedin 1000 adults. Jarisch divided doses (IV) doses q 4-6 hoursHerxheimer reaction,(IV)haemolytic anaemiawith high dosesPenicillin V Rash, haemolytic anaemia, Oral 20-50 mg/kg/day 250-500 mg everyinterstitial nephritis, in 4 divided doses 6-8 hourly.seizure with high doses.43
ANTIBIOTIC ADVERSE REACTION ROUTE PAEDIATRIC DOSE ADULT DOSEPiperacillin – Leukopenia, transient Intravenous 200-400 mg/kg/day 4.5 gm q 8hourlyTazobactum elevation of liver in 3-4 dividedenzymes, renal toxicity.dosesTeicoplanin Hypersensitivity Intravenous 10 mg/kg/day / 400mg once dailyreactions, rash, less dose every (6-30 mg/kg/day)nephrotoxic as Intramuscular 12 hours for 3compared todoses theVancomycin.10 mg/kg/dayonce dailyTigecycline Nausea vomiting , Intravenous Above 18 years 100mg followed byallergic reactions,50 mg everyphotosensitivity,12 hourly infusionpseudo tumourover 30-60 minutes.cerebri,pancreatitis.No dose adjustmentto renal failureVancomycin Red man syndrome, Intravenous 40-60 mg/kg/day in 0.5 gm q 6hourly oroto-toxicity, 3-4 divided doses 1 gm q 12 hourlynephrotoxicity.Note: This list of drugs includes commonly used antibiotics /antimicrobials agents in theOPD / admitted patients. This does not include antitubercular, antifungal and antiviral agents.Doses for neonates and infants less than 3 months are mentioned separately in neonataldrug policy.XXIII. ANTIBIOTIC PANELSThe results of in-vitro antibiotic susceptibility testing guide clinician in appropriate selectionof initial empiric regimens and, drugs used for individual patients in specific situations.The selection of an antibiotic panel for susceptibility testing is based on commonlyobserved susceptibility patterns and revised periodically. This panel is meant to promoterational antibiotic use.44
Antibiotic Panels <strong>2011</strong>1. Blood cultureORGANISMANTIBIOTICFIST LINE SECOND LINETHIRD LINESalmonella Typhi Ampicillin,Salmonella Paratyphi A ChloramphenicolCotrimoxazole,CiprofloxacinCeftriazone,CefiximeNalidixic acid *Gram- negative Ampicillin, Amikacin, Piperacillin ** Imipenem, Meropenembacteria (E. coli, Ciprofloxacin Cefepime, Beta lactam+ ColistinKlebsiella spp Proteus, Gentamicin, Beta lactamase inhibitorCitrobacter spp etc) CefotaximeCeftazidime,AugmentinEnterococci Penicillin, Vancomycin, Linezolid,Ampicillin, High Teicoplanin Chloramphenicol,level Gentamicin,Erythromycin.CiprofloxacinTetracyclineRifampicin***(V.R.E.)Pneumococci Penicillin Vancomycin Teicoplanin, Imipenem, MeropenemChloramphenicol, Co –trimoxazoleCefotaxime, ErythromycinOfloxacinClindamycin,Staphylococci Penicillin, Vancomycin, Teicoplanin Linezolid(Coagulase Positive/ Cefoxitin**** Netilmycin, Amikacin ChloramphenicolNegative) Gentamycin, Ciprofloxacin Rifampicin*** (VISA)Erythromycin (MRSA/MRSE)ClindamycinStreptococci spp Penicillin,CefotaximeHaemophilus spp. Ampicillin,ChloramphenicolCefurioxime,CefotaximeNOTE* Nalidixic acid resistant Salmonella but sensitive to Ciprofloxacin must be treated withcare as there could be treatment failure due to therapy with Ciprofloxacin, thusalternative drugs may be used.* * Piperacillin given in neonates.*** Rifampicin is an antitubercular drug and should be reserved for treatment failure casesonly. Should not be used as monotherapy.**** Cefoxitin is used currently instead of Oxacillin / Methicillin to detect methicillin resistance45
2. Cerebrospinal / Sterile FluidORGANISMANTIBIOTICFIRST LINE SECOND LINE THIRD LINEGram- negative bacteria Chloramphenicol. Amikacin, Piperacillin * Meropenem(E. coli, Klebsiella spp Ampicillin Gentamicin, Beta lactam + Beta ColistinProteus, Citrobacter spp Cefotaxime Ceftazidime, lactamase inhibitor,etc)CefepimeEnterococci Penicillin, Ampicillin Vancomycin ChloramphenicolHigh level Gentamicin Teicoplanin LinezolidPneumococci Penicillin, Vancomycin, MeropenemChloramphenicol, Teicoplanin,CefotaximeStaphylococci Penicillin, Cefoxitin Vancomycin, Teicoplanin -(Coagulase Positive/ Gentamicin, Amikacin. CiprofloxacinNegative) Chloramphenicol (MRSA/MRSE)Streptococci Spp Penicillin, Cefotaxime, - -ChloramphenicolHaemophilus app. Ampicillin, Amoxicillin+ClavulanateChloramphenicolCefuroxime sodium,CefotaximeMeningococci Penicillin Cefotaxime, - -ChloramphenicolNOTE* Piperacillin given in NeonatesOral antibiotics must not be used for Central nervous system (CNS) infectionsThe following antibiotics are contraindicated in CNS infectionsMacrolidesTetracyclineFluroquinolone – Ciprofloxacin etcClindamycinFirst and second generation Cephalosporins except Cefuroxime sodium3. ENDOTRACHEAL / SUCTION TIP SECRETIONSORGANISMANTIBIOTICFIRST LINE SECOND LINE THIRD LINEGram- negative bacteria Ciprofloxacin, Amikacin, Cefepime, Colistin. Tigecycline(E. coli, Klebsiella spp Ampicillin Gentamicin, Beta lactam + BetaProteus, Citrobacter Cefotaxime lactamase inhibitorspp.etc) Ceftazidime, Imipenem, MeropenemPiperacillinEnterococci Penicillin, Ampicillin, Vancomycin LinezolidHigh level Gentamicin Teicoplanin,Staphylococci Penicillin, Cefoxitin Vancomycin, Linezolid(Coagulase Gentamicin, Teicoplanin AmikacinPositive / Negative) Chloramphenicol (MRSA/MRSE)46
4. RESPIRATORY SAMPLE - SPUTUMORGANISMANTIBIOTICFIRST LINE SECOND LINE THIRD LINEGram -negative bacteria Ampicillin Cefuroxime Amikacin Cefepime Imipenem,(E. coli, Klebsiella sp Gentamicin, Ciprofloxacin Meropenem,Proteus, Citrobacter spp Cotrimoxazole Cefotaxime, Colistin,etc) Tetracycline Ceftazidime Beta TigecyclineAmoxycillin + Clav Lactam +Betalactamase inhibitorPseudomonas / Non- Ciprofloxacin, Betalactam + colistinfermenters Gentamicin Amikacin, BetalactamaseCeftazidime, Cefepime Inhibitor, Imipenem,PiperacillinMeropenemEnterococci Penicillin, Ampicillin, Vancomycin Tetracycline,High level Gentamicin Teicoplanin ChloramphenicolErythromycin,Linezolid (V.R.E.)CiprofloxacinPneumococci Penicillin, Cefotaxime, Vancomycin,Chloramphenicol, Ofloxacin TeicoplaninCotrimoxazole,ErythromycinClindamycin,Staphylococci Penicillin, Cefoxitin Vancomycin, Linezolid(Coagulase Positivie/ Gentamicin, Teicoplanin Netilmicin,Negative) Erythromycin AmikacinTetracycline,CiprofloxacinClindamycin(MRSA/MRSE)Streptococci spp Penicillin, CephadroxylErythromycin,TetracyclineHaemophilus spp Ampicillin, Ciprofloxacin -Cefuroxime,CefotaximeAmoxacillin + ClavTetracycline,Erythromycin47
5. PUS /GENITAL SAMPLESORGANISMANTIBIOTICFIRST LINE SECOND LINETHIRD LINEGram-negative Bacteria Ampicillin, Amikacin, Ceftazidime Tigecycline,(E. coli, Klebsiella spp Gentamicin, Cefepime, β ColistinProteus, Citrobacter spp Cefotaximelactam + β lactamaseetc) Tetracycline, inhibitor Ciprofloxacin,Chloramphenicol Oflo acinPseudomonas / Non Amikacin, Betalactam + Beta -fermenters Ciprofloxacin, Lactamase Inhibitor,Ceftazidime Cefepime, Imipenem, MeropenemGentamicinEnterococci Penicillin, Ampicillin, Vancomycin LinezolidHigh level Gentamicin TeicoplaninChloramphenicol,Erythromycin,TetracyclinePneumococci Penicillin, Cefotaxime -Erythromycin,Tetracycline OfloxacinStaphylococci (Coag Penicillin, Oxacillin Vancomycin, Linezolid (VISA)Positive/Negative) Gentamicin, TeicoplaninErythromycinNetilmycin, AmikacinChloramphenicol OfloxacinTetracycline,(MRSA/MRSE)ClindamycinCiprofloxacinStreptococci Spp Penicillin, - -Cephadroxyl,Erythromycin,CotrimoxazoleTetracycline48
6. URINE CULTUREORGANISMANTIBIOTICFIRST LINE SECOND LINETHIRD LINEGram-negative bacteria Ampicillin, Amikacin, Cefotaxime Imipenem,(E. coli, Klebsiella spp, Norfloxacin Ceftazidime, Beta MeropenemProteus, Citrobacter spp Cefuroxime Lactam+ Beta Cefepimeetc.) Cortrimoxazole, lactamaseNalidixic acidinhibitor,Netilmicin,Nitrofurantoin, OfloxacinCiprofloxacinGentamicin,Pseudomanas / Non Ciprofloxacin, Betalactam + -fermenters Ceftazidime Beta lactamasePiperacillin Amikacin, Inhibitor,GentamicinImipenem,MeropenenmEnterococci Penicillin, Ampicillin, Vancomycin LinezolidHigh level Gentamicin Teicoplanin,Ciprofloxacin,NitrofuratoinStaphylococci (Coagulase Oxacillin Gentamicin, Vancomycin, LinezolidPositive / Negative) Norfloxacin Teicoplanin Netilmicin,CotrimoxazoleCiprofloxacin,NitrofurantoinOfloxacin(MRSA/MRSE)NOTEBeta lactam + beta lactamase Inhibitor – Cefperazone + sulbactum, Piperacillin + TazobactumVRE Vancomycin resistant EnterococciMRSA, MRSE Methicillin Resistant Staphylococcus aureus and Methicillin resistant StapylococcusEpidermidis. Also referred to as ORSA or ORSE for Oxacillin resistant Staphylococcusaureus or epidermidisVISA Vancomycin Intermediate sensitivet Stapylococcus aureus. Also referred to asGISA - Glycopeptide Intermediate sensitive Staphylococcus aureus<strong>For</strong> isolates from Urology, ICU Burns and Haematology perform Ist, second and third linedrugs on first day when necessaryReferences1. Performance Standards for <strong>Antimicrobial</strong> Susceptibility testing internationalSupplement,Jan2010. CLSI, USA.2. Antibiotic Policy Group of <strong>Hospital</strong> infection Control Committee, Christian MedicalCollegeandhospital,vellore, TamilNadu-632004.49
GLOSSARY – COMMONLY USED ANTIMICROBIAL AGENTS<strong>Antimicrobial</strong> Class <strong>Antimicrobial</strong> Subclass Agents and their Generic namesI. Beta lactams Penicillins Penicillin(a) Penicillins Amino penicillin Amoxicillin, AmpicillinUreidopenicillin Piperacillin, Azlocillin, MezlocillinCarboxypenicillin Carbenicillin, TicarcillinPenicillinase stable Cloxacillin, Dicloxacillin, Methicillin,penicillin Amidinopenicillin Oxacillin, NafcillinMecillinam(b) Beta lactam+Beta Amoxicillin + Clavlactamase inhibitorAmpicillin + SulbactamCefperazone+ SulbactamTicarcillin + Clavulanic acidPiperacillin+ Tazobactam(c) Cephems Cephalosporin I Cefazolin, Cephalothin, Cephapirin,(parenteral)cephradineCephalosporin II Cefamandole, Cefonicid, CefuroximesodiumCephalosporin III Cefoperazone, Cefotaxime, Ceftazidime,Ceftizoxime, CeftriaxoneCephalosporin IV CefepimeCephamycinCefmetazole, Cefotetan, Cefoxitin(d) Cephems (Oral) Cephalosporin Cefaclor, Cefadroxyl, Cefdinir, Cefprozil,Ceftibuten, Cephelexin Cefditoren,Cefetamet, Cefixime, Cefpodoxime,Cefuroxime (axetil ) CephradineCarbacephemLoracabacef(e) Monobactams(f) CarbapenemsII. AminocyclitolsIII. AminoglycosidesIV. AnsamycinsAztreonamImipenem, Meropenem, ErtapenemSpectinomycin, TrospectinomycinAmikacin Gentamicin, Kanamycin,Netilmicin, Streptomycin, Tobramycin.RifampicinV. Quinolones Quinolone Cinoxacin, Nalidixic acidFluoro quinolones Ciprofloxacin, Clinafloxacin, Enoxacin,Flerofloxacin, Gatifloxacin Gemifloxacin,Levofloxacin, Lomefloxacin,moxifloxacin, Norfloxacin, Sparfloxacin,Ofloxacin.VI. Folate pathwayinhibitorsVII. FosfomycinVIII. KetolidesIX. LincosamidesSulfonamides, Trimethoprim,Trimethoprim sulfamethoxazoleFosfomycinTelithromycinClindamycin50
X. Lipopeptides DaptomycinXI. MacrolidesErythromycin, Azithromycin,Clarithromycin,XII. NitrofuransNitrofurantoinXIII. NitroimidazolesMetronidazoleXIV. OxazolidinonesLinezolidXV. Glycopeptides Glycopeptides VancomycinLipoglycopeptides TeicoplaninXVI. PhenicolsChloramphenicolXVII. StreptograminsQuinupristin DalfopristinXVIII. TetracyclinesDoxycycline, Minocycline, Tetracycline.51