Nursing protocol for use of patient controlled analgesia - the Royal ...
Nursing protocol for use of patient controlled analgesia - the Royal ...
Nursing protocol for use of patient controlled analgesia - the Royal ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
PAIN SERVICE - ADULTS<strong>Nursing</strong> Protocol <strong>for</strong> <strong>use</strong> <strong>of</strong> Patient Controlled Analgesia (PCA):1. Explanation should be given to <strong>patient</strong>s by anaes<strong>the</strong>tist and/or nursing staff. "PainAfter Surgery" (RCHT023) <strong>patient</strong> in<strong>for</strong>mation sheet to be given to <strong>patient</strong>s preoperatively.2. A PCA care plan must be implemented.3. PCA must be prescribed on <strong>the</strong> prescription chart with full instructions asnecessary, <strong>of</strong> lockout time and mg per bolus. Disposable PCA has a set lockout <strong>of</strong>6 minutes (see page 2).4. Check current pump <strong>protocol</strong> matches <strong>the</strong> <strong>patient</strong> prescription.5. Be<strong>for</strong>e setting up a PCA machine ensure service record up to date. If out <strong>of</strong> servicean alternative pump must be <strong>use</strong>d.6. Patients should have a pain score <strong>of</strong> mild pain or less be<strong>for</strong>e leaving recovery.7. Prior to <strong>the</strong> <strong>patient</strong> leaving recovery <strong>the</strong> asset number <strong>of</strong> PCA should be recordedon <strong>the</strong> recovery sheet and pain service pink database <strong>for</strong>m.8. Syringes may be changed by a registered nurse who is competent in <strong>the</strong>administration <strong>of</strong> IV drugs and undergone suitable training in <strong>the</strong> management <strong>of</strong>PCA. Attained written and practical competence. Maintaining competence byregular <strong>use</strong> <strong>of</strong> skill and attending 3 yearly medical device training and clinicalupdates. Ano<strong>the</strong>r registered nurse/midwife/learner must act as checker. Pleaserefer to <strong>the</strong> Role <strong>of</strong> <strong>the</strong> Checker Policy.9. An aseptic non-touch technique must be <strong>use</strong>d. Please refer to <strong>the</strong> Role <strong>of</strong> <strong>the</strong>Checker Policy.10. Ensure clamp on administration set is released prior to commencing <strong>the</strong> infusion, toprevent accidental bolus.11. Be<strong>for</strong>e attaching <strong>the</strong> designated administration set, <strong>the</strong> syringe must be purged /primed by <strong>the</strong> pump.12. Ensure only designated syringes are <strong>use</strong>d ie BD Plastipak 50mL luerlock.13. PCA should be administered via a specifically designed PCA giving set or aseparate IV cannula - a Y connector should not be <strong>use</strong>d. PCA can be run via acentral line (see page 2 <strong>for</strong> Disposable PCA).Document Author Page(s) Version Last Review Reviewed By Next Review DuePain Service Adults - Pain 1 <strong>of</strong> 4 06 July 2012 Pain July 2015PCAServicesServices
14. If additional fluids are to be inf<strong>use</strong>d, with <strong>the</strong> exception <strong>of</strong> clear IV fluids, <strong>the</strong>y mustbe run via a separate giving set in addition to PCA, i.e., blood, blood products,insulin or heparin. If a disposable PCA is in <strong>use</strong>, always <strong>use</strong> additional cannula <strong>for</strong>all fluids.15. PCA infusion pumps should be positioned no higher than cannula site to preventsiphoning <strong>of</strong> contents due to <strong>the</strong> effect <strong>of</strong> gravity.16. Prescribed night sedation may be given to <strong>patient</strong>s with PCA but no o<strong>the</strong>r narcoticor sedation should be given unless prescribed by <strong>the</strong> anaes<strong>the</strong>tist.17. No intramuscular opioids should be given <strong>for</strong> <strong>the</strong> duration <strong>of</strong> <strong>the</strong> PCA infusionsunless sanctioned/prescribed by <strong>the</strong> anaes<strong>the</strong>tist. A warning label should beattached to <strong>the</strong> prescription chart advising <strong>of</strong> this.18. Naloxone should be prescribed prior to <strong>patient</strong> leaving recovery or on setting upPCA. incase <strong>of</strong> respiratory depression.19. Delays in renewing syringes should be avoided to achieve continuous <strong>analgesia</strong>.20. PCA giving sets should be changed every 48-72 hours or according to hospitalpolicy.21. PCA should normally be continued until it is appropriate to start administering oral<strong>analgesia</strong>.22. Please ensure alternative <strong>analgesia</strong> has been prescribed be<strong>for</strong>e discontinuingPCA.23. Any opiate left in <strong>the</strong> syringe must be discarded into a denaturing kit. This shouldbe witnessed by two nurses and documented in <strong>the</strong> ward's wastage book.24. Keys <strong>for</strong> PCA machines should be kept toge<strong>the</strong>r with <strong>the</strong> <strong>controlled</strong> drug keys by<strong>the</strong> nurse in charge.25. On discontinuation, <strong>the</strong> pump should be cleaned and labeled according to hospitalpolicy and returned to <strong>the</strong>atres or pump library <strong>for</strong> storage.26. If equipment is faulty it must be returned to Medical Physics after being cleanedand labeled according to hospital policy.Clinical Observations:Monitoring should be documented on <strong>the</strong> MEWS Chart and AnalgesicAssessment Chart.1. Postoperative observations should be recorded every 15 minutes <strong>for</strong> 1 hour and<strong>the</strong>n every 30 minutes <strong>for</strong> <strong>the</strong> next 2 hours.Document Author Page(s) Version Last Review Reviewed By Next Review DuePain Service Adults - Pain 2 <strong>of</strong> 4 06 July 2012 Pain July 2015PCAServicesServices
2. Respiratory rate, sedation and pain scores must be recorded hourly until 24 hourspostop and <strong>the</strong>n every 2 hours until <strong>the</strong> PCA is ceased. The frequency <strong>of</strong> o<strong>the</strong>robservations may be reduced after 12 hours unless o<strong>the</strong>rwise clinically indicated.3. If a fur<strong>the</strong>r loading dose is administered by an anaes<strong>the</strong>tist or specialist pain nurse<strong>the</strong>n observations should be recorded every 15 minutes <strong>for</strong> one hour to ensure<strong>patient</strong>'s condition is stable.4. IV cannula site should be observed frequently <strong>for</strong> signs <strong>of</strong> inflammation re cannulacare plan.5. Disposable PCAFor <strong>use</strong> in designated areas onlyClinical observations remain <strong>the</strong> sameDisposable PCA set up by <strong>the</strong> anes<strong>the</strong>tist or pain servicesAdditional cannula required <strong>for</strong> fluidsLock out time <strong>for</strong> disposable PCA is 6 minutesProblems:1. Respiratory DepressionMorphine can ca<strong>use</strong> sedation and respiratory depression. This is usually gradualin onset and detectable as a slow respiratory rate in a very sedated <strong>patient</strong>. Thesedation score must be regularly measured on every <strong>patient</strong> with PCA. If <strong>the</strong>respiratory rate is less than 8 and/or sedation score 3, remove handset/stopinfusion. Give oxygen 4 litres and in<strong>for</strong>m medical staff. Consider giving naloxone.If respiratory rate 8 and sedation score
Pruritis is occasionally a side effect <strong>of</strong> morphine and can be treated with ei<strong>the</strong>r anantihistamine eg, Piriton or by a low dose <strong>of</strong> Naloxone. Please seek medical advicein this instance.5. Inadequate AnalgesiaFollow RCHT guidelines. Ensure <strong>the</strong> equipment is functioning correctly and that<strong>the</strong> line is not occluded. Check that <strong>the</strong> <strong>patient</strong> understands how to <strong>use</strong> <strong>the</strong> PCA.Call pain team or anaes<strong>the</strong>tist – an additional bolus dose may be required oranalgesics o<strong>the</strong>r than opioids.Any problems should be documented in <strong>the</strong> appropriate <strong>patient</strong> records.ReferencesArfean. Z. Owen. H. (1995) Current Anaes<strong>the</strong>sia and Critical Care, 6, pp 76-80.Gell Walker V, Tye T (2000) Patient Controlled Analgesia <strong>Nursing</strong> Times Vol 96 No 25 pp38-39MacIntyre. P. Ready. L. (1996) Acute Pain Management: A Practical Guide.MacIntyre P (2001) Safety and Efficacy <strong>of</strong> PCA British Journal <strong>of</strong> Anaes<strong>the</strong>sia 87(1) pp 36-46MacIntyre P, Ready L (2001) Acute Pain Management: A Practical Guide WB Saunders,London<strong>Royal</strong> Marsden Manual <strong>of</strong> Clinical <strong>Nursing</strong> Procedures. 7th EditionIVAC.PCAM Syringe Pump (Cardinal Health) Directions <strong>for</strong> Use.Role <strong>of</strong> <strong>the</strong> Checker Policy RCHT Document LibraryAseptic Non Touch Technique Policy RCHT Document Library Aug 2010Document Author Page(s) Version Last Review Reviewed By Next Review DuePain Service Adults - Pain 4 <strong>of</strong> 4 06 July 2012 Pain July 2015PCAServicesServices
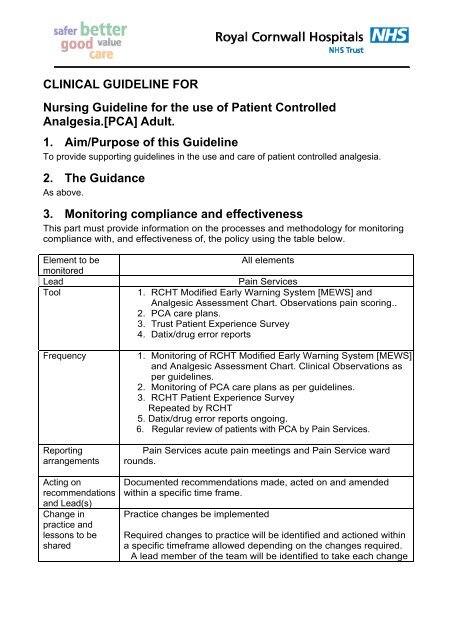
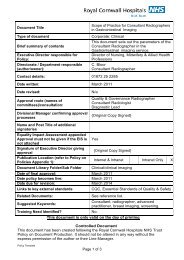
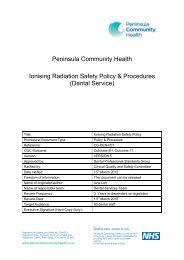
Appendix 1. Governance In<strong>for</strong>mationDocument Title<strong>Nursing</strong> guideline <strong>for</strong> <strong>the</strong> <strong>use</strong> <strong>of</strong> PatientControlled Analgesia [PCA] Adult.Date Issued/Approved: 27 July 2012Date Valid From: 27 July 2012Date <strong>for</strong> Review: 1 st July 2015Directorate / Department responsible(author/owner):Pain ServicesContact details: 01872 252792/ 2839Brief summary <strong>of</strong> contentsPain Services.<strong>Nursing</strong> guideline <strong>for</strong> <strong>the</strong> <strong>use</strong> <strong>of</strong> PatientControlled Analgesia [PCA] Adult.Suggested Keywords:Target AudienceExecutive Director responsible <strong>for</strong>Policy:RCHT PCT CFTMedical DirectorDate revised: 23/07/2012This document replaces (exact title <strong>of</strong>previous version):Approval route (names <strong>of</strong>committees)/consultation:Divisional Manager confirmingapproval processes<strong>Nursing</strong> Protocol <strong>for</strong> <strong>the</strong> <strong>use</strong> <strong>of</strong> PatientControlled Analgesia.Pain services RCHTLearning and Development RCHTDr Paul Upton Medical DirectorGovernance RCHTDuncan BlissName and Post Title <strong>of</strong> additionalsignatoriesSignature <strong>of</strong> Executive Director givingapprovalPublication Location (refer to Policyon Policies – Approvals andRatification):Document Library Folder/Sub FolderLinks to key external standardsRelated Documents:Not required.Internet & Intranet Intranet OnlyDocument library and Pain Sub FolderGovernance Team can adviseRole <strong>of</strong> <strong>the</strong> checkerIntravenous Drug Administering
Training Need Identified?Registered Nurse competent inadministering intravenous medication.PCA training pack completed.Practical assessment completed.Medical devices PCA pump trainingattended/completed.Regular or 3 yearly updates.Version Control TableDateVersion11/04/2012 0511/04/2012 0523/07/2012 06Summary <strong>of</strong> ChangesNow on current hospital template andheadings.Page 2. NO 17Naloxone to be prescribed prior to <strong>patient</strong>leaving recovery or on setting up PCA.Added page 1 No2 A PCA care plan must beimplemented.Amended Page 2 Clinical Observations:Monitoring should be documented on <strong>the</strong> MEWSChart and Analgesic Assessment Chart.Changes Made by(Name and Job Title)Sharon DunstanSenior Pain SpecialistNurse.Sharon DunstanSenior Pain SpecialistNurse.Sharon DunstanSenior Pain SpecialistNurse.All or part <strong>of</strong> this document can be released under <strong>the</strong> Freedom <strong>of</strong> In<strong>for</strong>mationAct 2000This document is to be retained <strong>for</strong> 10 years from <strong>the</strong> date <strong>of</strong> expiry.This document is only valid on <strong>the</strong> day <strong>of</strong> printingControlled DocumentThis document has been created following <strong>the</strong> <strong>Royal</strong> Cornwall Hospitals NHS TrustPolicy on Document Production. It should not be altered in any way without <strong>the</strong>express permission <strong>of</strong> <strong>the</strong> author or <strong>the</strong>ir Line Manager.
Appendix 2.Initial Equality Impact Assessment Screening FormName <strong>of</strong> service, strategy, policy or project (hereafter referred to as policy) to beassessed: <strong>Nursing</strong> guideline <strong>for</strong> <strong>the</strong> <strong>use</strong> <strong>of</strong> Patient Controlled Analgesia [PCA]Adult.Directorate and service area:Is this a new or existing Procedure?Pain ServicesName <strong>of</strong> individual completingassessment: Sharon DunstanExistingTelephone:01872 2527921. Policy Aim* To provide a guide to appropriate and safe administration in<strong>the</strong> <strong>use</strong> <strong>of</strong> PCA <strong>analgesia</strong>.2. Policy Objectives* Available to nursing staff and medical staff.3. Policy – intendedOutcomes*4. How will youmeasure <strong>the</strong> outcome?5. Who is intended tobenefit from <strong>the</strong> Policy?6a. Is consultationrequired with <strong>the</strong>work<strong>for</strong>ce, equalitygroups, local interestgroups etc. around thispolicy?b. If yes, have <strong>the</strong>segroups been consulted?c. Please list any groupswho have been consultedabout this procedure.To standardise practice resulting in safe administration <strong>of</strong>PCA <strong>analgesia</strong> and reduce errors.Regular visits to <strong>patient</strong>s with PCA <strong>analgesia</strong> ensuringguidelines are followed. Regular audit.Reduced datix reports received.Patient satisfaction regards to pain control.Patients, medical and nursing staff.NoN/APreviously practice development and infection control.*Please see Glossary7. The ImpactPlease complete <strong>the</strong> following table using ticks. You should refer to <strong>the</strong> EA guidance notes<strong>for</strong> areas <strong>of</strong> possible impact and also <strong>the</strong> Glossary if needed. Where you think that <strong>the</strong> policy could have a positive impact on any <strong>of</strong> <strong>the</strong> equalitygroup(s) like promoting equality and equal opportunities or improving relationswithin equality groups, tick <strong>the</strong> ‘Positive impact’ box. Where you think that <strong>the</strong> policy could have a negative impact on any <strong>of</strong> <strong>the</strong> equalitygroup(s) i.e. it could disadvantage <strong>the</strong>m, tick <strong>the</strong> ‘Negative impact’ box.
Where you think that <strong>the</strong> policy has no impact on any <strong>of</strong> <strong>the</strong> equality group(s) listedbelow i.e. it has no effect currently on equality groups, tick <strong>the</strong> ‘No impact’ box.Equality Positive Negative No Reasons <strong>for</strong> decisionGroup Impact Impact ImpactAge √ Child health has its own guidelinesrelating to care <strong>of</strong> PCA <strong>analgesia</strong>.Disability√Religion orbeliefGenderTransgenderPregnancy/MaternityRaceSexualOrientationMarriage / CivilPartnership√√√√√√√You will need to continue to a full Equality Impact Assessment if <strong>the</strong> following havebeen highlighted: A negative impact and No consultation (this excludes any policies which have been identified as notrequiring consultation).8. If <strong>the</strong>re is no evidence that <strong>the</strong> policypromotes equality, equal opportunitiesor improved relations - could it beadapted so that it does? How?Full statement <strong>of</strong> commitment to policy <strong>of</strong>equal opportunities is included in <strong>the</strong> policyPlease sign and date this <strong>for</strong>m.Keep one copy and send a copy to Matron, Equality, Diversity and Human Rights,c/o <strong>Royal</strong> Cornwall Hospitals NHS Trust, Human Resources Department, ChyveanHo<strong>use</strong>, Penventinnie Lane, Truro, Cornwall, TR1 3LJA summary <strong>of</strong> <strong>the</strong> results will be published on <strong>the</strong> Trust’s web site.Signed ______Sharon Dunstan__________________________________Date _____23/07/2012____________________________________