Post death procedure - East Cheshire NHS Trust
Post death procedure - East Cheshire NHS Trust Post death procedure - East Cheshire NHS Trust
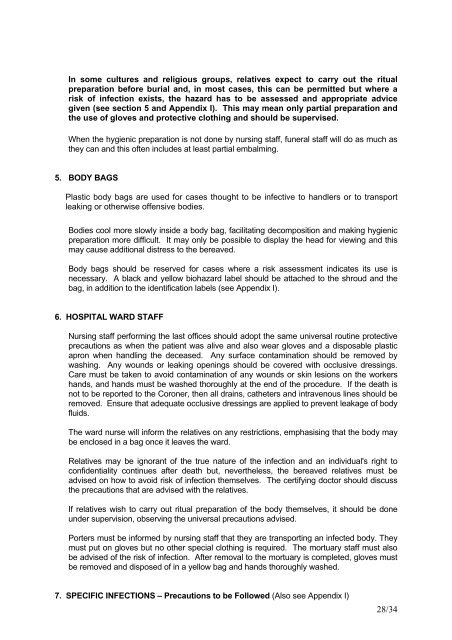
THE MORTUARY STAFF MUST BE INFORMED OF THE INFECTION RISKS ASSOCIATEDWITH THIS BODY.Please complete the following:Patients Name ........................................................................................………D.O.B. .....................................................................................................….Hospital Number .........................................................................................…Ward/Department ..........................................................................................Risk of Infection ..........................................................................................…REASON FOR USE OF BODY BAG (Please tick the relevant section)NOTE Ensure that attempts have been made to control blood loss prior toplacing body in the bag.DO NOT USE A SHEET INSIDE THIS BAG.ONCE IT IS SEALED IT OUGHT NOT BE RE-OPENED.1. Risk of infection – see Appendix I. 2. Uncontrollable loss of blood/body fluids. 3. No known medical history. 4. Unable to identify patient. Signature ....................................... Print Name ........................................Date .............................................................PLACE THIS FORM IN A SEALED ENVELOPE MARKED FOR THE ATTENTION OF THEMORTUARY TECHNICIAN AND GIVE TO PORTERS REMOVING THE BODY OR PLACEIN POCKET ON BODY BAG27/34
In some cultures and religious groups, relatives expect to carry out the ritualpreparation before burial and, in most cases, this can be permitted but where arisk of infection exists, the hazard has to be assessed and appropriate advicegiven (see section 5 and Appendix I). This may mean only partial preparation andthe use of gloves and protective clothing and should be supervised.When the hygienic preparation is not done by nursing staff, funeral staff will do as much asthey can and this often includes at least partial embalming.5. BODY BAGSPlastic body bags are used for cases thought to be infective to handlers or to transportleaking or otherwise offensive bodies.Bodies cool more slowly inside a body bag, facilitating decomposition and making hygienicpreparation more difficult. It may only be possible to display the head for viewing and thismay cause additional distress to the bereaved.Body bags should be reserved for cases where a risk assessment indicates its use isnecessary. A black and yellow biohazard label should be attached to the shroud and thebag, in addition to the identification labels (see Appendix I).6. HOSPITAL WARD STAFFNursing staff performing the last offices should adopt the same universal routine protectiveprecautions as when the patient was alive and also wear gloves and a disposable plasticapron when handling the deceased. Any surface contamination should be removed bywashing. Any wounds or leaking openings should be covered with occlusive dressings.Care must be taken to avoid contamination of any wounds or skin lesions on the workershands, and hands must be washed thoroughly at the end of the procedure. If the death isnot to be reported to the Coroner, then all drains, catheters and intravenous lines should beremoved. Ensure that adequate occlusive dressings are applied to prevent leakage of bodyfluids.The ward nurse will inform the relatives on any restrictions, emphasising that the body maybe enclosed in a bag once it leaves the ward.Relatives may be ignorant of the true nature of the infection and an individual's right toconfidentiality continues after death but, nevertheless, the bereaved relatives must beadvised on how to avoid risk of infection themselves. The certifying doctor should discussthe precautions that are advised with the relatives.If relatives wish to carry out ritual preparation of the body themselves, it should be doneunder supervision, observing the universal precautions advised.Porters must be informed by nursing staff that they are transporting an infected body. Theymust put on gloves but no other special clothing is required. The mortuary staff must alsobe advised of the risk of infection. After removal to the mortuary is completed, gloves mustbe removed and disposed of in a yellow bag and hands thoroughly washed.7. SPECIFIC INFECTIONS – Precautions to be Followed (Also see Appendix I)28/34
- Page 1: ADULTPOST DEATH PROCEDURES(Version
- Page 4 and 5: Roman Catholic ChaplainsFather Pete
- Page 7 and 8: handling policy.) Remove all put on
- Page 9 and 10: SECTION FOUR - PROCEDURES FOR MANAG
- Page 11 and 12: PLEASE NOTE: It is the doctor’s d
- Page 13 and 14: BAHAI1 Bahai relatives may wish to
- Page 15 and 16: 1 The relatives of a Jainist patien
- Page 17 and 18: 1 There are no special requirements
- Page 19 and 20: 3 Orthodox Parses require a priest
- Page 21 and 22: 09.00 hours. The doctor involved sh
- Page 23 and 24: SECTION SEVEN - MORTUARY DEPARTMENT
- Page 25 and 26: SECTION EIGHT - INFECTION PREVENTIO
- Page 27: Body BagsA risk assessment must be
- Page 31 and 32: Bahkshi S.S. (1994)Infectious Disea
- Page 33 and 34: APPENDIX I Cont …..InfectionNotif
- Page 35 and 36: ACTION TO BE TAKEN WHERE A DEATH OC
- Page 37 and 38: NoPart 3 - ASSESSMENT OF IMPACTRACE
- Page 39: OTHER - Additional groups that may
In some cultures and religious groups, relatives expect to carry out the ritualpreparation before burial and, in most cases, this can be permitted but where arisk of infection exists, the hazard has to be assessed and appropriate advicegiven (see section 5 and Appendix I). This may mean only partial preparation andthe use of gloves and protective clothing and should be supervised.When the hygienic preparation is not done by nursing staff, funeral staff will do as much asthey can and this often includes at least partial embalming.5. BODY BAGSPlastic body bags are used for cases thought to be infective to handlers or to transportleaking or otherwise offensive bodies.Bodies cool more slowly inside a body bag, facilitating decomposition and making hygienicpreparation more difficult. It may only be possible to display the head for viewing and thismay cause additional distress to the bereaved.Body bags should be reserved for cases where a risk assessment indicates its use isnecessary. A black and yellow biohazard label should be attached to the shroud and thebag, in addition to the identification labels (see Appendix I).6. HOSPITAL WARD STAFFNursing staff performing the last offices should adopt the same universal routine protectiveprecautions as when the patient was alive and also wear gloves and a disposable plasticapron when handling the deceased. Any surface contamination should be removed bywashing. Any wounds or leaking openings should be covered with occlusive dressings.Care must be taken to avoid contamination of any wounds or skin lesions on the workershands, and hands must be washed thoroughly at the end of the <strong>procedure</strong>. If the <strong>death</strong> isnot to be reported to the Coroner, then all drains, catheters and intravenous lines should beremoved. Ensure that adequate occlusive dressings are applied to prevent leakage of bodyfluids.The ward nurse will inform the relatives on any restrictions, emphasising that the body maybe enclosed in a bag once it leaves the ward.Relatives may be ignorant of the true nature of the infection and an individual's right toconfidentiality continues after <strong>death</strong> but, nevertheless, the bereaved relatives must beadvised on how to avoid risk of infection themselves. The certifying doctor should discussthe precautions that are advised with the relatives.If relatives wish to carry out ritual preparation of the body themselves, it should be doneunder supervision, observing the universal precautions advised.Porters must be informed by nursing staff that they are transporting an infected body. Theymust put on gloves but no other special clothing is required. The mortuary staff must alsobe advised of the risk of infection. After removal to the mortuary is completed, gloves mustbe removed and disposed of in a yellow bag and hands thoroughly washed.7. SPECIFIC INFECTIONS – Precautions to be Followed (Also see Appendix I)28/34