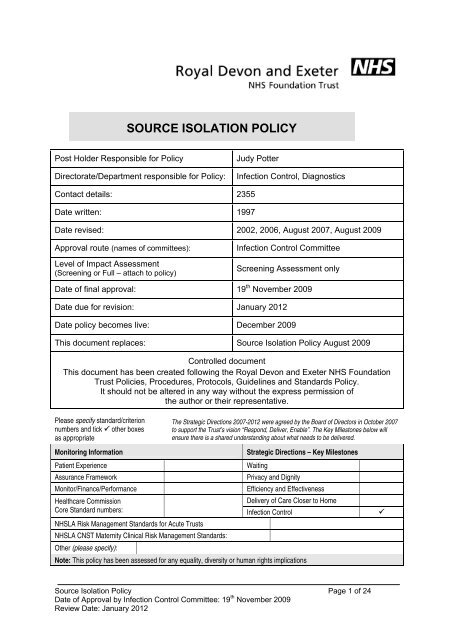
SOURCE ISOLATION POLICY - Royal Devon & Exeter Hospital
SOURCE ISOLATION POLICY - Royal Devon & Exeter Hospital
SOURCE ISOLATION POLICY - Royal Devon & Exeter Hospital
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CONTENTSPage1 Introduction 32 Routes of Transmission 33. Source Isolation Procedures 43.1 Communication 43.2 Accommodation 43.3 Hand Hygiene 53.4 Protective Clothing 53.5 Vulnerable Staff & Visitors 53.6 Equipment 63.7 Linen 63.8 Waste Disposal 63.9 Excreta 63.10 Sharps 63.11 Collection of Specimens 63.12 Management of Spillage 73.13 Crockery & Cutlery 73.14 Visits to other Departments 73.15 Transfer/Discharge of Patients 73.16 Visitors 73.17 Routine Cleaning 83.18 Last Offices 83.19 Terminal Cleaning 8 - 94. Tables of Communicable Diseases & Appropriate Precautions 10 - 205. Index of Specific Gastrointestinal Infections 21 - 23Appendix 1 -Management of the Contacts of Patients at R D & E<strong>Hospital</strong>s with probably Meningococcal Disease 24Source Isolation Policy Page 2 of 24Date of Approval by Infection Control Committee: 19 th November 2009Review Date: January 2012
1. IntroductionStandard precautions are the principal strategy for the prevention and control of nosocomialinfection. However, additional precautions are required for the care of patients who areknown or suspected to be infected (or colonised) with highly transmissible orepidemiologically important pathogens. Such precautions are known as source isolationprecautions.The infected/colonised patient, as the source of infection, is segregated from unaffectedpatients, usually in a single room but, on occasions, within a cohort of similarly affectedpatients. Physical segregation, combined with other precautions such as the use ofprotective clothing, is aimed at reducing the likelihood of infections spreading via theairborne, droplet or contact routes.The extent of isolation depends on:iiiThe infecting organism and the route of transmissionThe physical and mental abilities of the patient.These guidelines provide the information required to determine appropriate isolationprecautions based on the route of transmission. However, consideration must also be givento an individual patient’s mental or physical needs which often need to be balanced againstthe risk of transmission of infection. Care should be planned on an individual basis takinginto account the needs of the patient and susceptibility of other patients. The InfectionControl Team should be contacted for advice regarding individual patients.2. Routes of TransmissionKnowledge of the possible route of transmission is necessary to apply isolation precautionsappropriately and, in particular, to select appropriate protective clothing.a) Contact transmissionThis is the most important and frequent mode of transmission of nosocomialinfection. This may be direct contact such as touching, biting and kissing. It alsoincludes indirect contact via equipment (including sharp objects e.g. needles,blades), as well as the faecal oral route.b) Droplet transmission.Large droplets are generated from the source person primarily during coughing,sneezing, and talking, and during the performance of cough inducing proceduressuch as suctioning and bronchoscopy. Transmission occurs when dropletscontaining micro-organisms generated from the infected person are propelled ashort distance (approximately 1 metre) and deposited on the host's conjunctivae,nasal mucosa, or mouth.c) Airborne transmissionThis route of transmission can be divided into two types, droplet nuclei and dust.iDroplet nuclei.Small respiratory droplets rapidly evaporate into small-particle residues [5 µm orsmaller in size] known as droplet nuclei, that may contain micro-organisms. Dropletnuclei remain suspended in the air for long periods of time and may become inhaledby a susceptible host within the same room or over a longer distance from the sourcepatient.Source Isolation Policy Page 3 of 24Date of Approval by Infection Control Committee: 19 th November 2009Review Date: January 2012
iiDustSkin squames are shed from the skin surface at a rate of approximately 300 million aday and are the main component of dust. Some of the squames carry microorganisms.Small dust particles may remain airborne for several hours and can beinhaled or settle in wounds.3 Source Isolation Precautions3.1 Communicationa) Explain the rationale for isolation to the patient and, where possible, the duration ofisolation anticipated. Where available provide a patient information leaflet.b) Place the appropriate isolation card on the door of the room/bay and indicate theappropriate precautions.c) Record in the patient's notes that isolation has been commenced and the reasonwhy.d) Revise the nursing care plan accounting for infection control precautions to bemaintained by staff, patient and visitors.e) Inform the Infection Control Team that there is a patient in isolation.f) Check whether the patient has a ‘Notifiable Disease’ and if so complete NotificationCertificate. If a Notification Certificate Book is not held in your department, contactthe Infection Control Dept within their normal working hours.3.2 Accommodationa) Identify appropriate isolation facilities e.g. single room or cohort bay.‣ A side room with negative pressure ventilation may be required for airborneinfections - refer Section 4 for details.‣ It is particularly important to keep the door closed when the side room is used forisolating a patient with an airborne infection.‣ If a single room is indicated it is preferable that it has en-suite toilet and washingfacilities.b) Remove all inessential furniture and equipment.c) Ensure that appropriate equipment is available:Inside the roomHand cleansing facilitiesGloves & ApronsClinical waste bag holder/bin.Linen receptacle with water soluble bag.Sharps Bin (if safe to leave within room)ThermometerSphygmomanometer, Stethoscope (if required)Toileting and wash facilities (if no en suite bathroom).Outside the roomAppropriate protectiveclothingAlcohol hand rub.NB The mental health of the patient may dictate that it is unsafe to leave some ofthis equipment within the room. Always undertake a risk assessment.Source Isolation Policy Page 4 of 24Date of Approval by Infection Control Committee: 19 th November 2009Review Date: January 2012
3.3 Hand Hygienea) Within the roomHands must be cleansed prior to leaving the isolation room. Hand hygiene mustalso be performed between different patient care activities to prevent crosscontamination of different body sites. If the patient has diarrhoea soap and watershould be used for hand hygiene rather than alcohol rub.b) Immediately after leaving the roomCleanse hands..3.4 Protective ClothingIt is often unnecessary and inappropriate to require every person entering an isolation roomto wear protective clothing.If worn, protective clothing must be removed immediately prior to leaving the room and mustbe disposed of inside the room into a clinical waste bag (except when leaving the room todispose of used bedpans etc. when it is removed in the sluice after placing bedpan inmacerator/bedpan washer).The type of protective clothing required is dependent on the mode of transmission and thetype of contact. All that is usually required is disposable gloves and aprons.Guidance regarding the need for gloves and aprons is provided in the Index of Infections atSections 4 and has been divided into the following three categories:Limited to Standard Precautions (LSP)Direct contact and cleaning (DCC)All staff and visitors (ALL)If the infectious agent is transmitted inblood or other body fluids then protectiveclothing is only required when contactwith such material is anticipatedFor many conditions protective clothing isonly required for direct patient contactand activities such as bed making androom cleaning. In this situation protectiveclothing is not required for social contactby staff or visitors.For a small number of conditions it isappropriate for all persons entering theroom to wear protective clothing.Occasionally additional protective clothing, such as masks and gowns, is required. Wherethis is appropriate it has been identified in the Index of Infection (Section 4). However,please note that masks are rarely necessary and are of limited value in protecting againstinfection spread by the airborne respiratory route. It is more important that staff caring forpatients with airborne infections are immune.3.5 Vulnerable Staff & VisitorsSome may be more vulnerable than others to infection. In particular:‣ Pregnant women‣ Immunocompromised people (for any reason)‣ Staff with eczematous/psoriatic or similar skin lesions ( particularly relevant with MRSA)‣ Staff and visitors receiving antibiotics ( relevant to C.difficile infection)Source Isolation Policy Page 5 of 24Date of Approval by Infection Control Committee: 19 th November 2009Review Date: January 2012
Must seek advice prior to caring for patients in isolation.3.6 EquipmentDisposable equipment should be used whenever possible. Non disposable equipment mustbe decontaminated in accordance with the Decontamination Policy when removed from theroom. Wherever possible equipment should be allocated for sole use of the patient anddecontaminated when no longer required.3.7 LinenAll laundry from isolation rooms must be managed as fouled/infected laundry and thereforebe placed in water soluble bags within the room and then into an outer linen sack.3.8 Waste DisposalAll waste must be disposed of into clinical waste bags inside the room. Double bagging isnot necessary. The bag should be placed immediately at the designated collection point.3.9 ExcretaExcreta can be disposed of directly into the toilet adjoining the room. If no en-suite facilities,cover commode/bed pan and take directly to the sluice. Pans and urinals must be heatdisinfected in washer/disinfector or, if disposable, be placed directly into the macerator.Gloves and aprons should then be removed and discarded in clinical waste bin and handswashed.3.10 SharpsA sharps bin should be kept inside the room for sharps disposal, unless this will be a hazardto the patient.3.11 Collection of SpecimensSpecimens should be obtained within the room. Care must be taken to avoid contaminatingthe outside of the specimen container. All clinical specimens should be regarded aspotentially infectious and handled as such. However, since it is National Health and SafetyPolicy, specimens from patients likely to have the following organisms have to be treated as‘high risk ‘and identified on the accompanying form, with a label to indicate this.INFECTION SUSPECTED ORGANISM SPECIMENHEPATITISBlood Borne Viruses Blood and body fluidsHepatitis B&CHIV / AIDSHIV I+IIBlood and body fluidsHTLV I+IITBMycobacteriumSpecimens from site oftuberculosis (MTB)infectionEg: sputum, urineTYPHOIDSalmonella typhiFaeces & Blood CulturesSalmonella paratyphiBrucella abortus/melitensisBlood CulturesBone MarrowBRUCELLOSIS("UNDULANT FEVER")PLAGUE Yersinia pestis Specimens from discharginglesionsSputumSource Isolation Policy Page 6 of 24Date of Approval by Infection Control Committee: 19 th November 2009Review Date: January 2012
ANTHRAXBacillus anthracisYELLOW FEVER Arboviruses BloodON NO ACCOUNT SHOULD ANY SPECIMENS BE TAKEN FROM PATIENTS WITHSUSPECTED VIRAL HAEMORRHAGIC FEVER (eg: LASSA/EBOLA, etc., A POTENTIALLYLETHAL CROSS-INFECTION HAZARD) WITHOUT CONTACTING A MEDICALMICROBIOLOGIST FIRST.3.12 Management of SpillageRefer to Decontamination Policy.3.13 Crockery and CutleryCrockery and cutlery is adequately decontaminated by dishwasher. Return items to kitchenpromptly.3.14 Visits to other DepartmentsWherever possible, the department should be notified in advance so that arrangements maybe made to prevent possible spread of infection i.e. patients with infections spread by theairborne route should be seen at the end of a list/session. Ward staff should advise of anynecessary precautions. The Infection Control Nurse can also be contacted for advice. Afterthe investigation/treatment is completed, surfaces with which the patient has had contactshould be cleaned with hot water and detergent or detergent wipes.Portering staff and other staff accompanying the patient do not need to wear protectiveclothing but must clean their hands thoroughly after having direct contact with the patient.Wheelchairs/trolleys used to transport patients to other departments must be cleaned withhot water and detergent or detergent wipes.3.15 Transfer/Discharge of PatientsPatients can be transferred from one ward to another ward or unit, if clinical need dictates.The receiving area must be informed in advance of the nature of the infection to ensure thatthe appropriate facilities are available and the required precautions are applied. Movementfor non clinical reasons, e.g. outlying medical patients who are in isolation rooms to surgicalwards to increase bed availability in medicine, should be avoided.On discharge ensure that receiving hospital/nursing home or community services areinformed of any necessary precautions. If transport by ambulance is required, theAmbulance Service must be informed of any necessary precautions.3.16 VisitorsVisitors must report to the nurses’ station prior to entering the room. It may be necessary toask about immunisation status prior to visiting. In some circumstances visiting may berestricted. If visiting is allowed it is usually unnecessary for visitors to wear protectiveclothing but they should be advised to wash/clean their hands when leaving the room.Visitors may need to be shown how to do this. Visitors should be advised not to visit otherpatients but if this is necessary they should do so before visiting the patient in isolation.They should be advised not to eat or drink whilst in the isolation room. Visiting by youngchildren should be discouraged. If visitors insist on bringing young children they must beinformed of any risks.Source Isolation Policy Page 7 of 24Date of Approval by Infection Control Committee: 19 th November 2009Review Date: January 2012
3.17 Routine CleaningIsolation rooms must be cleaned at least as frequently as other patient areas using standardcleaning procedures. Cloths must be disposable. Mop heads must be removed and shouldbe laundered after use or disposable mop heads discarded.3.18 Last OfficesFollowing death, the body may remain an infection risk to personnel and therefore isolationprecautions must be maintained whilst Last Offices are performed.Last Offices are performed in accordance with local Trust procedures.All bodies should be sealed in a leak proof cadaver bag.3.19 Terminal CleaningTerminal cleaning of the environment and furniture can be arranged via thehousekeeping/domestic supervisor. However, when housekeeping services are not availableit is the responsibility of the nursing staff to ensure the room is cleaned before reuse. Thecleaning procedure below should be followed:Procedure• Clean thoroughly, and remove, patient equipment before terminal cleaning of theenvironment commences.• Dispose of any contaminated disposable patient care items as clinical waste.• Strip the bed linen and bag appropriately.• Dispose of debris/rubbish into a clinical waste bag.• Remove any dignity curtains for laundering.• Arrange for removal of radiator covers (if appropriate)• Clean the environment thoroughly using NaDCC sanitiser solution 1000ppm e.g.Chlor-clean or Actichlor plus.. Steam cleaners may be used for difficult to cleanequipment.‣ Start with high cleaning - curtain rails, overhead light and bedside TV orphone equipment, high shelves/ledges.‣ Clean all other surfaces, including the inside of the bedside locker. Wallwashing is not required but remove visible splash marks.‣ Clean bed frame and mattress.‣ Clean handwashing sink and any en-suite facilities - include cistern and doorhandles, light pulls etc.Source Isolation Policy Page 8 of 24Date of Approval by Infection Control Committee: 19 th November 2009Review Date: January 2012
‣ Clean patient equipment that could not be removed from the room.‣ Mop vinyl flooring. Place mophead in laundry bag and return for launderingor, if disposable mop head used, discard as clinical waste. If room is carpetedthis must be vacuumed and then steam cleaned using a steamcleaner/extractor.‣ Dispose of cloths, gloves and aprons into a clinical waste bag. Removewaste bag from room. WASH HANDS• .Replace radiator covers• Hang clean curtainsSource Isolation Policy Page 9 of 24Date of Approval by Infection Control Committee: 19 th November 2009Review Date: January 2012
4 Tables of Communicable Diseases and Appropriate PrecautionsDisease or OrganismAnthraxCutaneousPulmonaryMode of transmissionfrom person to personIn the health care settingContact with lesionsPerson to person spreadunknown.* See commentsSingleroomYesYesGloves Apron Other PPE VisitorRestrictionsALLALLALLALLSeecomments -Bronchiolitis Droplet Yes DCC DCC - Exclude preschoolchildrenBrucellosisNo person to personNo LSP LSPChickenpox(Varicella zoster)Creutzfeldt JakobDisease (CJD) andrelated disordersspreadAirborne via respiratorysecretions and vesicle fluidContact with vesicleexudateContact via instrumentsused for invasiveproceduresYes DCC DCC - Exclude nonimmuneDurationofisolationDuration ofdiseaseClinicalRecovery1 weekafter onsetor untillesions aredryNo LSP LSP - - Duration ofhospitalstayCommentsNOTIFIABLE DISEASEInfection Control Team must beinformed if anthrax issuspected.*In the event of a deliberaterelease of anthrax spores thepatient, his/her belongings and theenvironment may becontaminated. Refer to HPAguidelines www.hpa.org.ukNon immune staff must beexcluded.Negative pressure isolation roompreferredAlso refer Varicella Zosterinformation on ComexSpecial precautions required forinvasive proceduresAlso refer CJD guidanceKey to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne - via droplet nucleii or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentSource Isolation Policy Page 10 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Disease or OrganismCroupCryptococcusneoformansCytomegalovirusDengue FeverDiarrhoea (suspectedinfective) See Section5 for individual causesDiphtheriaRespiratoryMode of transmissionfrom person to personIn the health care settingDropletContact via contaminatedhands.No person to personspreadContact with saliva, blood,urineContact via contaminatedsharpsContact via faecal oralrouteDropletSingleroomGloves Apron OtherPPEVisitorRestrictionsYes DCC DCC - Exclude preschoolchildrenNo LSP LSPNo LSP LSP -DurationofisolationClinicalrecoveryNo LSP LSP ClinicalrecoveryYes DCC DCC Variable VariableseeSection 4.1YesALLALLExcludenon immuneCutaneousDirect contact with skinlesionsEncephalitisContact via faecal oral(suspected infective) routeEnterovirusContact via faecal oral Yes for DCC DCC(Echo and Coxsackie) routeinfants onlyEpiglottitis Droplet Yes DCC DCC Exclude preschoolUntilswabs arerepeatedlynegativeCommentsAlways consider othercommunicable diseases whentravelling from abroad. Isolate ins/r until diagnosis is confirmed.Refer Section 5 of this policyNOTIFIABLE DISEASE.Yes DCC DCCInform infection control onsuspicion.Yes LSP LSP NOTIFIABLE DISEASE48hoursafterstartingappropriateantibiotictherapyImmunisation and prophylaxis ofclose contacts may be necessaryKey to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne - via droplet nucleii or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentSource Isolation Policy Page 11 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Disease or OrganismGas GangreneMode of transmissionfrom person to personIn the health care settingNo person to personspreadSingleroomGloves Apron OtherPPEGlandular fever Contact via saliva (kissing) No LSP LSPGonococcal InfectionGenito-urinary tractOphthalmianeonatorumHepatitisUndiagnosedContact with exudate frommucous membranes of theGTContact via unwashedhandsContact with blood, faecesand other body fluids(percutaneous expsure)VisitorRestrictionsDurationofisolationCommentsNo LSP LSP Infection is usually endogenousYes,childrenonlyYesLSPDCCLSPDCC24 hours ofantibiotictherapyNOTIFIABLE DISEASEYes LSP LSP NOTIFIABLE DISEASEHepatitis A Contact (faecal-oral) Yes LSP LSP LSP 7 daysafter onsetof jaundiceHepatitis B, C & δHerpes simplex TypeI and IIContact with blood andbody fluids (usuallypercutaneous exposure viaused sharps)Contact with lesions andvia shared towels etc.DropletNotusually*Notusually*NOTIFIABLE DISEASELSP LSP LSP NOTIFIABLE DISEASE (if acute)*Single room required ifbleeding uncontrollably or haslarge open wounds orreceiving haemodialysis.LSP LSP All lesionsscabbed* Single room may be required ifpatient has extensive lesionsAlso refer Herpes Simplexinformation on Comex.Herpes zosterRefer ShinglesKey to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne - via droplet nucleii or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentSource Isolation Policy Page 12 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Disease or OrganismMode of transmissionfrom person to personIn health care settingSingleroomGloves Apron OtherPPEVisitorRestrictionsDurationofisolationCommentsHumanImmunodeficiencyVirusDirect or indirect contactwith blood and body fluids(usually percutaneousexposure via used sharps)No LSP LSP LSPPatients with AIDS may haveinfectious conditions that requireisolationImpetigoRefer streptococcalinfectionInfestationsHuman FleasCat/dog fleasLice (Body)Lice (Head)Contact with patient andbedding and clothingN/AContact with patients,clothing, bedding, towelsetcContact (head to head)and via shared combs,head wear, pillowsYesALL ALL GownsDCCNoYes ALL ALL GownsDCCYes DCC DCCRecommendlimiting visitorsto those whohave alreadyhad contactuntil treatedRecommendlimiting visitorsto those whohave alreadyhad contactuntil treatedAdvise visitorsto avoid headto headcontactUntilpatient,beddingandclothingaretreated.Untilpatientbeddingandclothingare treatedUntiltreatedLice (pubic) Contact (usually sexual) No LSP LSP UntiltreatedHuman fleas are extremelyuncommon.Treat animals and environmentBody lice live in the seams ofclothing.As this is usually STD considerreferral to GUM clinic forscreeningKey to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne - via droplet nucleii or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentSource Isolation Policy Page 13 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Disease or OrganismMode of transmissionfrom person to personIn the health care settingSingleroomGloves Apron OtherPPEVisitorRestrictionsDurationofisolationCommentsInfestationscontinuedScabiesContact with skin(prolonged skin contactusually required)YesDCCDCCNoneUntiltreatedItching may continue for severaldays/weeksClose contacts will need treatmentCrusted/atypicalscabiesContact with skin,bedding, clothing etcYesDCCGownDCCRecommendlimiting visitorsto those whohave alreadyhad contactuntil treatedAs advisedby the ICTRefer to dermatologistContacts will need treatment.Also refer Scabies guidanceWormsContact via faecal oralrouteNo LSP LSP UntiltreatedInfluenza, Seasonal Droplets Yes LSP LSP Advise elderlyvisitors to beimmunisedLegionnaires’No person to personDiseasespreadLeptospirosis(Weil’s Disease)LiceRefer InfestationsListeriosisContact with blood andurineMother to baby in uteroand during delivery3 daysafter onsetFamily contacts or equivalent mayneed treatmentAlert ICT if more than one case onsame wardNo LSP LSP N/A Microbiologist MUST be contactedto arrange for rapid diagnosticmethods to be set up.NOTIFIABLE DISEASENo LSP LSP N/A NOTIFIABLE DISEASEYesin neonatalunit onlyLSP LSP ClinicalrecoveryMicrobiologists should beinformed as potentially foodborneContact (faecal oral)although very rareKey to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne - via droplet nucleii or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentSource Isolation Policy Page 14 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Disease or OrganismMalariaMode of transmissionfrom person to personIn the health care settingContact via percutaneousexposureSingleroomGloves Apron OtherPPEVisitorRestrictionsDurationofisolationCommentsNo LSP LSP NOTIFIABLE DISEASEAlways consider the possibility ofother tropical infections which maybe infectious. Therefore untildiagnosis confirmed a single roomis advisable.Measles Airborne Yes DCC DCC Exclude non -immuneMeningitis4 daysafter rashappearsNOTIFIABLE DISEASE.Also refer Measles information onComex.UndiagnosedBacterial? Droplet transmission? Indirect contact (faecaloral)Yes DCC DCC SurgicalmasksVariabledependingon causeNOTIFIABLE DISEASEMasks for airway managementand close prolonged contactMeningococcal(Neisseriameningitidis)Other bacterialcausese.g.pneumococcal,haemophilusinfluenzaeViralDroplet Yes DCC DCC As above 48 hours ofappropriateantibioticsNo person to persontransmissionContact (faecal oral)+/- DropletNo LSP LSPYes DCC DCC ClinicalrecoveryNOTIFIABLE DISEASEAntibiotic prophylaxis may berequired for household andmouth kissing contacts. CCDCor Health Protection Nurse willadvise. Refer Appendix 1.NOTIFIABLE DISEASECommonly caused by enterovirusKey to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne - via droplet nucleii or skin scales – remain suspended in the air for long periodsPPE – Personal Protective EquipmentSource Isolation Policy Page 15 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Disease or OrganismMode of transmissionfrom person to personIn the health care settingSingleroomGloves Apron OtherPPEVisitorRestrictionsDurationofisolationCommentsMeningococcal Septicaemia – See Meningococcal MeningitisMulti-Resistant GramNegative OrganismsMumpsMycoplasmapneumoniaParvo virus (human)(Slapped Cheek)PlagueBubonicPneumonicPolioDepends on site ofcolonisation. Contact viaunwashed hands mostsignificant route oftransmission.DropletContact with urine/salivaPossibly(Seekadvice)Source Isolation PolicyApproved by Infection Control Committee: 19 th November 2009Review Date: January 2012DCC DCC On theadvice oftheInfectionControlTeamYes DCC DCC Surgicalmask forclosecontact/airwaymanagementExclude nonimmune9 days afteronsetDroplet No LSP LSP 10 daysafter onsetDropletContact with pus frombuboesAirborneContact via faecal oralrouteDropletYesYesYesLSP LSP ExcludepregnantwomenALLALLALLALLMask,GownALLExclude unlessalreadyexposedYes LSP LSP Exclude nonimmuneUsuallyonce rashappearsbut seecomments.Duration ofdisease7 days fromonset ofsymptomsFor ESBL and AMP C producingbacteria refer to ESBL/AMP Cguidance.NOTIFIABLE DISEASEPatients are usually no longerinfectious by the time the diagnosisis confirmed.Patients in aplastic crisis may beinfectious for 1 week after onset.Exclude pregnant members of staff.NOTIFIABLE DISEASEContact Infection Control Teamimmediately on suspicion.Person to person transmission israre but the patient should betransferred to high securityinfectious disease unit.NOTIFIABLE DISEASEKey to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne – via droplet uclei or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentPage 16 of 24
Disease or OrganismMode of transmissionfrom person to personIn the health care settingSingleroomGloves Apron Other PPE VisitorRestrictionsDurationofisolationCommentsPsittacosisPerson to person spreadvery rareNo LSP LSP N/APyrexia of UnknownOrigin with recenttravel abroadQ-feverRabiesRingworm (extensive)As cause is unknown allmodes of transmissionmust be consideredNo person to personspreadContact via percutaneousexposure to salivaDroplets of saliva toconjunctiva/mucosa.Contact with skin scales,nail and hair andvia associated equipmente.g.hair clippers, shaversYes ALL ALL Limited topreviouscontacts andclose familyNo LSP LSPYes ALL ALL Masks andeyeprotectionif coughingLimitedVariable –clinicalrecovery ifcause notconfirmedClinicalrecoveryMalaria, typhoid and Hepatitis Aare the commonest causes ofPUO in returned travellers BUTalways consider possibility ofViral Haemmorhagic Fever.Also refer VHF guidance.NOTIFIABLE DISEASEContact Microbiologist andInfection Control Team ifsuspected.Person to person transmission isonly a theoretical risk but becauseof the implications of acquisitionstrict adherence to isolationprecautions must be observed.No DCC DCC Variable Own bath shower facilitiesdesirable.Rubella Droplet Yes DCC DCC Exclude nonimmune4 daysafter onsetof rash.NOTIFIABLE DISEASEALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne – via droplet nuclei or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentSource Isolation Policy Page 17 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Disease or OrganismMode of transmissionfrom person to personIn the health care settingSingleroomGloves Apron OtherPPEVisitorRestrictionsDurationofisolationCommentsSmallpoxContact with vesiclesAirborne via respiratorydroplet nucleiiYes ALL ALL Masks,gownsand eyeprotectionALLExcludeunless alreadyexposedUntilinformedby theInfectionControlTeamNOTIFIABLE DISEASECONTACT MICROBIOLOGISTAND INFECTION CONTROLIMMEDIATELY ON SUSPICIONImplement Major Incident PlanShinglesContact with exudateAirborne via vesicle fluid(in disseminated shingles)Yes DCC DCC Exclude if nonimmune tochickenpox1 weekafter onsetor untillesions aredryExclude staff non-immune tochicken poxAlso refer Varicella Virus(VZ),chickenpox and shinglesinformation on Comex.Streptococcal (GroupA) InfectionIncluding sore throatscarlet fever, impetigo,erysipelas, woundInfection, toxic shocksyndrome, puerperalfever.Contact with lesionsDropletsYes DCC DCC Recommendexcludingchildren andany visitor witha wound.48 hrs fromcommencingappropriateantibioticsScarlet Fever – NOTIFIABLEDISEASEStaff with sore throats should seekadvice from Occupational HealthStreptococcal GroupB (Neonatal)Contact via faeces, skinsitesNo LSP LSP N/AKey to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne - via droplet nucleii or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentSource Isolation Policy Page 18 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Disease or OrganismMode of transmissionfrom person to personIn the health care settingSingleroomGloves Apron Other PPE VisitorRestrictionsDurationofisolationCommentsSyphyllisEarly congenitalPrimary SecondaryLatent & LateTetanusContact with lesions,secretions, bloodNo person to personspreadNo person to personspreadNo LSP LSP 24 hrs ofeffectivetherapyNo LSP LSPN/ANo LSP LSP N/A NOTIFIABLE DISEASEToxoplasmosisNo person to personspreadNo LSP LSP N/ATuberculosisPulmonary (open) iesputum smear positiveAirborne via resp dropletnucleiYes LSP LSP HEPAmasks forcoughinducingproceduresLimit tohousehold/family contactsUsually 2weekstreatmentNOTIFIABLE DISEASEAlso Refer TB guidanceNegative pressure ventilationpreferable.MDRTB must be nursed innegative pressure isolation.Pulmonary (closed) No spread No LSP LSP N/AExtrapulmonary No spread No LSP LSP N/A(excluding openabscess and otherdrainage lesions)Key to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne - via droplet nucleii or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentSource Isolation Policy Page 19 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Disease or OrganismMode of transmissionfrom person to personIn the health care settingSingleroomGloves Apron OtherPPEVisitorRestrictionsDurationofisolationCommentsTyphoid &ParatyphoidIndirect contact -faecal/urine/oral spreadYes, withen-suitefacilitiesDCC DCC Advisevisitors not toeat or drink inthe isolationroomVariableNOTIFIABLE DISEASEEnsure blood cultures and stoolsare labelled with risk of infectionstickersTyphusIndirect contact viainoculation injuryNo Yes LSP LSP Until anyinfestion istreatedNOTIFIABLE DISEASEEnsure patient is free ofinfestation.VancomycinResistantEnterococcus (VRE)Varicella Zoster ReferChicken pox orShinglesViral HaemorrhagicFever (eg Lassa,Ebola, Marburg)Whooping CoughYellow FeverContact withcolonised/infected sitesContact - percutaneousexposure to blood andbody fluids?Droplet - pharyngealsecretionsAirborne - respiratorysecretionsContact - percutaneousexposureYes DCC DCC - - UntilinformedbyInfectionControlYes ALL ALL MasksVisorsALLImmediatefamily/partnerExcludechildren.Yes DCC DCC Exclude nonimmuneAs advisedbyInfectionControlTeam5 daysafterantibioticsstartedYes LSP LSP 5 daysafter onsetAlso Refer VRE/GRE GuidanceNOTIFIABLE DISEASECONTACT INFECTIONCONTROL IMMEDIATELY ONSUSPICIONAlso refer VHF guidanceNOTIFIABLE DISEASENOTIFIABLE DISEASEKey to table Modes of transmissionALL = Applies to all persons entering the room Contact – direct (touching, kissing, biting) or indirect via equipment/fomites (includes percutaneousDCC = Required for direct contact or cleaning exposure via used sharps)LSP = Limited to standard precautions Droplet - large respiratory droplets propelled a short distance onlyN/A = Not applicable Airborne - via droplet nucleii or skin scales – remain suspended in the air for long periodsPPE = Personal Protective EquipmentSource Isolation Policy Page 20 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
5. Index of Specific Gastrointestinal InfectionsOrganism Risk Group Source Person toPersonSpreadIncubationPeriodPeriod ofExcretionSpecific Therapy Single Room DurationofIsolationNotesAdenovirusPre schoolchildrenHuman ++ ? 2-5 days No Yes Durationof diseaseAmoebic DysenteryForeignTravellersHuman + ?May beprolongedVariable Metronidazole Yes Durationof diseaseNOTIFIABLEDISEASEAstrovirusPre schoolchildrenHuman ++ ? 2-7 days No Yes Durationof diseaseBacillus cereus All ages Food esp.Chinesetakeaway- 1-6 hours N/A No No N/A NOTIFIABLEDISEASE asfoodpoisoningCalicivirus All ages Human ++ 24-48 hours 2-3 days No Yes Durationof diseaseCampylobacter All ages FoodRaw milkWater+ 2-7 days Variable PossiblyErythromycin orCiprofloxacinIf possibleDurationof diseaseNOTIFIABLEDISEASE asfoodpoisoningClostridiumbotulinumAll ages Food - 12-36 hours N/A Specific Anti-toxin No N/A NOTIFIABLEDISEASE asfoodpoisoningClostridium difficile Post antibiotic Human.Contaminatedenvironment++ Variable VariableOralMetronidazoleYes48 hoursafterresolutionofsymptomswith returnto normalbowelactionInformInfectionControlNursesAlso referC.difficileguidanceSource Isolation Policy Page 21 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Organisms Risk Group Source Person toPersonSpreadIncubationPeriodPeriod ofExcretionSpecificTherapySingleRoomDuration ofIsolationNotesClostridiumperfringensAll agesFood esp. cookedmeats- 10-18 hours N/A No No N/A NOTIFIABLEDISEASE asfoodpoisoningCryptosporidium Mainly children HumanWaterAnimal contactE. Coli 0157 All ages Contact with cattleContaminated food.+ 2-14 days 1-3 weeks No Yes Duration ofdisease++ Variable If severe Yes 48 hours afterresolution ofsymptomsNOTIFIABLEDISEASE asfoodpoisoningNOTIFIABLEDISEASE asfoodpoisoningEnteropathogenicE.coliChildren under3 yearsHuman ++ 12-72 hours Variable Not usually Yes Duration ofdiseaseNOTIFIABLEDISEASE asfoodpoisoningGiardia lamblia All ages HumanWater++ 1-4 weeks Variable MetronidazoleIfpossibleDuration ofdiseaseNOTIFIABLEDISEASE asfoodpoisoningNorovirus All ages Human +++ 24-48 hours Variable No Yes Min 48 hoursresolution ofsymptomsNOTIFIABLEDISEASE asfoodpoisoningAlso refer viralgastroenteritisguidanceRotavirusMainly preschool childrenHuman ++ 1-4 days 2-5 days No Yes Min 48 hoursresolution ofsymptomsSource Isolation Policy Page 22 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
Organisms Risk Group Source Person toPersonSpreadIncubationPeriodPeriod ofExcretionSpecificTherapySingleRoomDuration ofIsolationNotesSalmonella sp.(nontyphi)All ages Food Human cases + 12-72 hours Variable Severecases onlyYesDuration ofdiseaseNOTIFIABLEDISEASE asfoodpoisoningSalmonella typhi ¶typhiAll ages esp.after foreigntravelHuman Food ++ 1-3 weeks Variable Yes Yes Period ofhospitalisationNOTIFIABLEDISEASEShigella spYoung childrenFollowingforeign travelHuman ++ 1-7 days Variable If severe Yes Period ofhospitalisationNOTIFIABLEDISEASE asfoodpoisoningStaph aureus All ages Food esp. cookedmeats- 2-6 hours N/A No No N/A NOTIFIABLEDISEASE asfoodpoisoningVibrio cholerae Travel abroad HumanWaterFood+ 1-5 days Variable YesTetracyclineYesPeriod ofhospitalisationNOTIFIABLEDISEASEYersinia sp Mainly children Food + 3-7 days Variable If severe Yes Duration ofdiseaseNOTIFIABLEDISEASE asfoodpoisoningSource Isolation Policy Page 23 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012
MANAGEMENT OF THE CONTACTS OF PATIENTS AT RD&E HOSPITAL WITHPROBABLE MENINGOCOCCAL DISEASEThe object of this flowchart is to identify contacts at risk of meningococcalinfection, and to prescribe them appropriate antimicrobial prophylaxis within12 hoursAPPENDIX 1Patient with probable meningococcal disease in the <strong>Royal</strong> <strong>Devon</strong> and <strong>Exeter</strong><strong>Hospital</strong>Action by medical/nursing member of team, at the earliest opportunityTelephone the Health Protection Unit (HPU) 01803 861833 and ask for the Doctor/Nurse on duty for PublicHealth. Out of normal working hours ask RD+E switchboard for the <strong>Devon</strong> & Cornwall Health Protection UnitContact Rota 1 st on.1) Have the patient’s details to hand2) If possible have a relative / partner / friend accompanying the patient availableAction by duty HPU DoctorHPU doctor will draw up lists of contacts, either by visiting or talking on ‘phone to hospitalstaff or persons who have accompanied the patient to hospital. An assessment is made ofwhich contacts need prophylaxis, this includes hospital and ambulance staff as well asfamily / community contactsCopy list of staff contacts to <strong>Exeter</strong> Occupational Health Service (EXOHS)Close/ family contacts needingprophylaxis- present in hospitalStaff contacts needing prophylaxis- <strong>Hospital</strong> staff- Others e.g. ambulanceAll other contacts needingprophylaxis- not present in hospitalEmergency Deptartment (ED) at RD&E informed by phone (01392 402310) orfax (01392 402313) of list of contacts needing prophylaxis.Action by GP/DDOCDuty GP/DDOC phoned andfaxed to prescribeappropriate antibioticAction by ED doctorED doctor to prescribe and dispense from stock ciprofloxacin orrifampicin or ceftriaxone as appropriate to contacts. Drug stock andpatient leaflets held in ED pharmacy cupboard.Copy of prescription to go to EXOHS and HPUAction by EXOHSKeep records of1) all staff contacts2) all staff antibiotic prescriptionsAction by HPU doctorMake a record of1) all contacts2) all antibiotic prescriptionsSource Isolation Policy Page 24 of 24Approved by Infection Control Committee: 19 th November 2009Review Date: January 2012