My life: in safe hands - Offender Health Research Network
My life: in safe hands - Offender Health Research Network
My life: in safe hands - Offender Health Research Network
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
AcknowledgementsWe would like to thank everyone who participated <strong>in</strong> this evaluation. We believe it has been considerablyenhanced by the contribution of 50 women service users who talked openly about their experience ofmedium secure services, their hopes and aspirations for the future and how they are supported to achievethem. In addition to women participants, over 60 other <strong>in</strong>dividuals <strong>in</strong>clud<strong>in</strong>g staff of medium secureservices, and other agencies as well as commissioners participated through questionnaires, <strong>in</strong>terviews anddiscussions as well as by provid<strong>in</strong>g documentation about policies and practices that affect this group ofexist<strong>in</strong>g and potential service users. We would like to thank them as they too talked openly with us aboutthe work they do. The Evaluation Advisory Group gave us <strong>in</strong>valuable encouragement and supportthroughout. The evaluation only came <strong>in</strong>to be<strong>in</strong>g as a result of work by Liz Mayne (Department of <strong>Health</strong>)who identified and supported secure services to enable many women with multiple needs take their livesback <strong>in</strong>to their own <strong>hands</strong>.F<strong>in</strong>ally, thanks are due to the Department of <strong>Health</strong> for demonstrat<strong>in</strong>g its cont<strong>in</strong>ued commitment todedicated secure services for women and for fund<strong>in</strong>g this evaluation.Georgie Parry‐CrookePenny StaffordJune 2009
ContentsPage no.Acronyms used <strong>in</strong> this reportSummaryi – vii1. Sett<strong>in</strong>g the scene: women’s medium secure services and the evaluation 11.1 Background to the evaluation 11.2 Background to women’s medium secure services 31.3 The chang<strong>in</strong>g landscape: recent policy, research and service development 41.4 The evaluation approach 91.5 The report structure 112. Mapp<strong>in</strong>g service provision across the country 152.1 The overall picture 162.2 Case study services 183. Women’s journeys through medium secure services: 253.1 Factors affect<strong>in</strong>g women’s routes to recovery 253.2 Philosophies and models of care: <strong>in</strong> theory and <strong>in</strong> practice 313.3 Implementation of policies to facilitate a route through 363.4 The importance of s<strong>in</strong>gle sex policy and provision 384. In whose <strong>hands</strong>: how are women <strong>safe</strong> and secure? 414.1 Def<strong>in</strong>itions of security 414.2 The experience of security: what did women say? 424.3 What did staff say about security? 435. Day‐to‐day realities: arrival <strong>in</strong>to and stay<strong>in</strong>g at a medium secure service 475.1 Early days: admission and arrival 475.2 Physical environments: what works for women and staff 505.3 Interventions, treatments and therapies 525.4 Service user <strong>in</strong>volvement 60
6. <strong>My</strong> <strong>life</strong> <strong>in</strong> my <strong>hands</strong>? Care Pathways, Care Plann<strong>in</strong>g and discharge 636.1 Care Pathways 646.2 Involv<strong>in</strong>g women <strong>in</strong> the process 656.3 The CPA meet<strong>in</strong>gs 686.5 CPA documents 696.5 Risk assessments 706.6 Mov<strong>in</strong>g on: the f<strong>in</strong>al steps 71Page no.7. Day‐to‐day for staff: work<strong>in</strong>g <strong>in</strong> a women’s medium secure service 757.1 Staff<strong>in</strong>g and staff<strong>in</strong>g structures 757.2 Recruitment and retention of staff 807.3 Tra<strong>in</strong><strong>in</strong>g and support 807.4 The role and purpose of supervision 838. Build<strong>in</strong>g on experience: <strong>in</strong> even <strong>safe</strong>r <strong>hands</strong>? 858.1 Good practice <strong>in</strong> women’s services 858.2 What needs to be addressed for the future? 888.3 Review<strong>in</strong>g the Service Specification 91Appendices1. Evaluation methods 952. Service Specification 1213. Provider Directory January 2009 125List of tables1. Current medium secure provision for women 162. Patient groups catered for 173. Rank order<strong>in</strong>g of key construct themes 274. Elements, i.e. people, <strong>in</strong>cluded <strong>in</strong> repertory grids 315. Policies <strong>in</strong> place 366. Interventions, treatments and therapies 537. Service user <strong>in</strong>volvement 608. Characteristics of women participants 959. Roles of professionals participat<strong>in</strong>g 952
Acronyms used <strong>in</strong> the report:BPDBMECAMHSCBTCFTCJSCNSCPACQCCSIPDBTHCALAMDTMHAMSUNICENOGNOMSNPSANSFOATSOTPCTPTSDPALSRMOSHATEMSS (W)WEMSSWISHWORPBorderl<strong>in</strong>e Personality OrderBlack and m<strong>in</strong>ority ethnicChild and Adult Mental <strong>Health</strong> ServicesCognitive Behaviour TherapyCommunity Forensic TeamsCrim<strong>in</strong>al Justice SystemCl<strong>in</strong>ical Nurse SpecialistCare Programme ApproachCare Quality CommissionCare Services Improvement PartnershipDialectical Behaviour Therapy<strong>Health</strong> Care AssistantLocal AuthorityMulti‐discipl<strong>in</strong>ary TeamMental <strong>Health</strong> ActMedium secure unitNational Institute of Cl<strong>in</strong>ical ExcellenceNational Oversight GroupNational <strong>Offender</strong> Management ServiceNational Patient Safety AgencyNational Service FrameworkOut of area treatment servicesOccupational TherapyPrimary Care TrustPost‐Traumatic Stress DisorderPatient Advisory Liaison ServiceResponsible Medical OfficerStrategic <strong>Health</strong> AuthorityTherapeutically Enhanced Medium Secure Services for WomenWomen’s Enhanced Medium Secure ServiceWomen <strong>in</strong> Secure HospitalsWomen’s Offend<strong>in</strong>g Reduction Programme
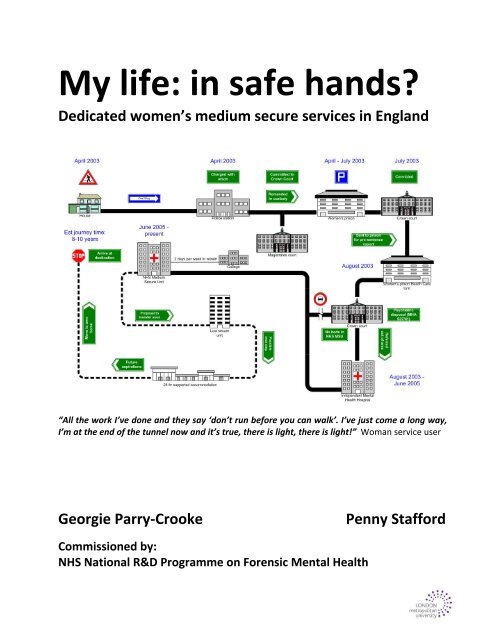
SummaryIntroductionIn 2000, there were 39 medium secure services <strong>in</strong> England. Of these, almost all were mixed provision with only 14NHS and 79 <strong>in</strong>dependent sector medium secure beds <strong>in</strong> dedicated women‐only services. By January 2009, there were27 dedicated women‐only medium secure services (n<strong>in</strong>e <strong>in</strong>dependent and 18 NHS) with a total of 51 wards andprovid<strong>in</strong>g 543 beds (261 <strong>in</strong> the <strong>in</strong>dependent sector and 282 with<strong>in</strong> NHS services). There was at least one service <strong>in</strong>each health region of the country; with six <strong>in</strong> the North‐West and only one <strong>in</strong> the South‐West. Of the 27 services, 19had a gender‐specific care pathway with either a women‐only rehabilitation or pre‐discharge ward, or a women‐onlylow secure or step‐down service. Four of the 27 services were women‐only sites with five on mixed sites but with noregular mixed activities. Seventeen were on sites where some activities were mixed.The overall aim of this study was to evaluate established, new and emerg<strong>in</strong>g dedicated women’s medium securemental health services that cater for women with complex needs. The evaluation <strong>in</strong>volved 50 women service usersand over 60 professionals <strong>in</strong> look<strong>in</strong>g at the way <strong>in</strong> which services have developed and their impact on women’s lives.Sections of the report are referred to <strong>in</strong> the text below.Sett<strong>in</strong>g the sceneThe quality and <strong>safe</strong>ty of secure mental healthprovision for women has been the subject of widerang<strong>in</strong>g discussion not<strong>in</strong>g that women <strong>in</strong> mixed‐sexservices have been disadvantaged by their m<strong>in</strong>oritystatus (1.2). They have also experienced the adverseeffects of gender and other <strong>in</strong>equalities on theirtreatment and care. Successive policies across theCrim<strong>in</strong>al Justice System and mental health haveargued the need to provide gender sensitive serviceswhich help to reduce women’s offend<strong>in</strong>g rates,respond to the specific needs of women and ensurewomen’s <strong>safe</strong>ty <strong>in</strong> s<strong>in</strong>gle‐sex provision. The morerecent development of medium secure services forwomen, supported by the Department of <strong>Health</strong> (1.3),was a response to the perceived vulnerability ofwomen which has resulted <strong>in</strong> a variety of researchstudies, policy developments and operational changes<strong>in</strong> service provision. Developments <strong>in</strong>cluded theclosure of all but one high secure service for women,the open<strong>in</strong>g of three Enhanced Medium SecureServices for Women, the sett<strong>in</strong>g up of four pilotresidential high support therapeutic services forwomen, the expansion of women‐only medium secureservices.Service provision <strong>in</strong> EnglandTwo separate mapp<strong>in</strong>g exercises for this evaluation (<strong>in</strong>2006 and 2009) showed there was considerablevariation across women’s medium secure services <strong>in</strong>terms of the type, size and range of provision. InJanuary 2009 there were 15 NHS Secure Services andeight <strong>in</strong>dependent hospitals provid<strong>in</strong>g medium securecare for women <strong>in</strong> s<strong>in</strong>gle sex wards (2.1). These werewomen‐only services or women‐only units with<strong>in</strong>mixed secure sett<strong>in</strong>gs provid<strong>in</strong>g a total of 386 bedsacross 38 wards.Independent sector services tended to provide ahigher number of beds for women. However, theyalso had more than the recommended number perward/unit.The case study services, selected on the basis oforganisational structure and location, illustrated someof the different ways <strong>in</strong> which the women’s mentalhealth policy agenda has been implemented (2.2).Women’s journeys through the serviceKey factors affect<strong>in</strong>g women’s routes to recovery(3.1) were determ<strong>in</strong>ed through the use of repertorygrid technique to elicit the elements (people <strong>in</strong>volved<strong>in</strong> enabl<strong>in</strong>g their care) and constructs (how womendiscrim<strong>in</strong>ated between their experiences of andrelationships with all the elements/people). Women’smost frequently referenced factors were:• Relationship with staff• Trust• Positive expectations• Empower<strong>in</strong>g approach• Reduc<strong>in</strong>g isolation• Good daily support• Relational security• Holistic approach• Meet<strong>in</strong>g emotional needs• Offer<strong>in</strong>g a range of <strong>in</strong>terventions
There was consensus among service users andprofessionals about the most important attributes of awomen’s medium secure service <strong>in</strong> relation torecovery.Philosophy, models and policies <strong>in</strong> practiceEssential to service provision was the development ofa coherent and thought‐through model or philosophyof care (3.2). The case study services had adopted avariety of approaches <strong>in</strong>clud<strong>in</strong>g Attachment Theory,Mentalisation, models of therapeutic communities,gender‐sensitive approaches, the Tidal Model andRAID (Re<strong>in</strong>force Appropriate, Implode Destructive).Where there was no clear model <strong>in</strong> place, staff andwomen described more tension, confusion and ahigher number of difficult <strong>in</strong>cidents. Staff <strong>in</strong> theseservices were also less likely to receive regular supportand supervision.Even with a clear model, services demonstrated thedifficulty at times of turn<strong>in</strong>g philosophy and policy <strong>in</strong>toevery day practice for a variety of reasons (3.3). Coreto this process was an understand<strong>in</strong>g that work<strong>in</strong>g <strong>in</strong>the service and reflect<strong>in</strong>g on theory needed to be<strong>in</strong>tegrated. Policy implementation was h<strong>in</strong>dered attimes by lack of staff; time; awareness and, <strong>in</strong> largermixed medium secure services, understand<strong>in</strong>g.S<strong>in</strong>gle sex policy and provisionAt the centre of the DH Women’s Mental <strong>Health</strong> Policywas the importance of offer<strong>in</strong>g women <strong>safe</strong> places towork towards their recovery <strong>in</strong>clud<strong>in</strong>g access towomen‐only services where appropriate which meettheir needs (3.4). There was agreement across womenand professionals about the importance of s<strong>in</strong>gle sexprovision although this varied across case study areas.Some women preferred s<strong>in</strong>gle sex wards but wantedthe opportunity to mix with men <strong>in</strong> off‐ward areas.Male staff were considered important <strong>in</strong> provid<strong>in</strong>gpositive role models although it was not always easyto f<strong>in</strong>d men who wanted to work with women.Women’s <strong>safe</strong>ty and securityWomen and professionals <strong>in</strong>volved <strong>in</strong> their care wereclear, regardless of term<strong>in</strong>ology, about the importanceof a number of key factors and <strong>in</strong> particular relationalsecurity which underp<strong>in</strong>ned what services shouldwork towards (4.1). For this study, relational securitywas def<strong>in</strong>ed as embody<strong>in</strong>g high staff‐to‐patient ratios,time spent <strong>in</strong> face‐to‐face contact, a balance between<strong>in</strong>trusiveness and openness and work<strong>in</strong>g towards highlevels of trust between patients and professionals.However, the <strong>in</strong>itial survey showed that policies aboutrelational security were only <strong>in</strong> place <strong>in</strong> half ofservices. In the case study areas, services describedways <strong>in</strong> which their practice aspired to or was alreadyconsistent with this def<strong>in</strong>ition even if they did not usethe same language to def<strong>in</strong>e what they experienced.However, there was considerable <strong>in</strong>consistency andeven where a policy was <strong>in</strong> place, staff weresometimes unclear about what this meant <strong>in</strong> practice.Women described what they valued about the service<strong>in</strong> terms consistent with the ideas underp<strong>in</strong>n<strong>in</strong>grelational security (4.2). This <strong>in</strong>cluded:• Be<strong>in</strong>g able to talk to staff• Be<strong>in</strong>g on a women‐only ward• Be<strong>in</strong>g able to address specific issues <strong>safe</strong>ly• Be<strong>in</strong>g able to just be with staff• Be<strong>in</strong>g able to form and susta<strong>in</strong> good peerrelationshipsSome women were frustrated by the level of physicalsecurity but <strong>in</strong> particular, <strong>in</strong>consistency of securitypolicy implementation was a cause of compla<strong>in</strong>t. Staffidentified factors which h<strong>in</strong>dered embedd<strong>in</strong>g relationsecurity <strong>in</strong>clud<strong>in</strong>g practical implications of low stafflevels, physical and procedural obscur<strong>in</strong>g relationalsecurity and where trust was difficult to achieveamong staff a well as women service users. Cont<strong>in</strong>uityand staff changes were also identified as potentialbarriers. Staff attitudes and the use of patroniz<strong>in</strong>glanguage sometimes <strong>in</strong>hibited relational security <strong>in</strong>practice (4.3).Day‐to‐day for womenWomen who participated <strong>in</strong> the evaluation rarelyreferred to an admissions policy (5.1) but describedthe process and their arrival. Mov<strong>in</strong>g to a mediumsecure sett<strong>in</strong>g was often seen as an improvement onwhere they moved from and a route to recovery. Keyto a smooth transition were speed, effectiveconsultation with women, provision of <strong>in</strong>formation,ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g contact pre‐admission, keep<strong>in</strong>g awoman’s outside connections and ensur<strong>in</strong>g cont<strong>in</strong>uityof staff through admission and arrival at the newservice. Professionals had to make decisions based on<strong>in</strong>dividual women’s needs but <strong>in</strong> the context of thebalance of women and levels of support available <strong>in</strong>the unit at the time.The physical environment (5.2) was important towomen and staff. While new build<strong>in</strong>gs were offputt<strong>in</strong>gto some <strong>in</strong>itially, most women appreciatedii
efforts made to make the unit look and feel homely.Some would have liked more say <strong>in</strong> design and décor.S<strong>in</strong>gle rooms with en‐suite bathrooms as well asaccess to communal areas <strong>in</strong>clud<strong>in</strong>g a gym, activityrooms, gardens and visit<strong>in</strong>g areas were all noted bywomen as contribut<strong>in</strong>g to their well‐be<strong>in</strong>g. For staff,design which <strong>in</strong>corporated zonal observation waswelcomed and the reduction <strong>in</strong>, what were seen to be<strong>in</strong>trusive, one‐to‐one observations helped to ensurestaff were available to provide escorts and be <strong>in</strong>volved<strong>in</strong> on and off‐ward activities.Services offered a range of <strong>in</strong>terventions, treatmentsand therapies (5.3). They were concerned thatwomen found ways of talk<strong>in</strong>g about their traumaticexperiences despite varied views about the type ofpsychological therapy to provide and when it shouldbe offered. In addition to psychological therapies,some offered specialist therapies from healthy liv<strong>in</strong>gto eat<strong>in</strong>g disorders. Formal, structured timetableswere mixed with <strong>in</strong>formal leisure activities and acrossservices respond<strong>in</strong>g to the <strong>in</strong>itial survey almost twothirds of women took part <strong>in</strong> community out<strong>in</strong>gs,shopp<strong>in</strong>g and social events.Women and staff recognized the value of ‘<strong>in</strong>formal’activities (5.3). Women wanted to do what was‘ord<strong>in</strong>ary’. Some staff and other professionals saw thisas hav<strong>in</strong>g a therapeutic potential <strong>in</strong> the same way thatmore formal <strong>in</strong>terventions were <strong>in</strong>tended to have.A dedicated Occupational Therapy (OT) service wasvalued where it was available. OTs worked withwomen to <strong>in</strong>crease their levels of <strong>in</strong>dependence andconfidence through education, tra<strong>in</strong><strong>in</strong>g and workopportunities. Mixed‐sex services aimed to providesome women‐only activities. Social Work was anotherimportant source of support to women who wantedcontact with their families. This was sometimes seenas a separate area of provision but one social workerwanted to see ward staff <strong>in</strong>volved <strong>in</strong> traditional socialwork issues as a means of support<strong>in</strong>g women andbuild<strong>in</strong>g team relationships.Access to sufficient and appropriate physicalhealthcare was not always provided (5.3). Womenservice users were particularly concerned that theirneeds were not be<strong>in</strong>g met <strong>in</strong> relation to see<strong>in</strong>g a GP orother doctors.Advocacy was provided <strong>in</strong> some but not all servicesand rarely was this gender‐specific. Few of the women<strong>in</strong>terviewed had sought out support from anadvocate. This may have been due to the underresourc<strong>in</strong>gof advocacy services and thus time‐limitsplaced on those offer<strong>in</strong>g to support women. However,advocates were <strong>in</strong>volved <strong>in</strong> support<strong>in</strong>g some women<strong>in</strong> a range of ways <strong>in</strong>clud<strong>in</strong>g practical problems and <strong>in</strong>issues relat<strong>in</strong>g to the unit or ward environmentA further aspect of day‐to‐day <strong>life</strong> for some womenwas their <strong>in</strong>volvement as service users <strong>in</strong> provisionand governance (5.4). The level and type ofopportunity ranged from unit/ward meet<strong>in</strong>gs,patients’ councils to representation on cl<strong>in</strong>icalgovernance groups and membership of a regionalservice user <strong>in</strong>volvement strategy group. Womenwere encouraged to be <strong>in</strong>volved but motivation to doso was a problem for some. Others were deterred byconcerns that change did not appear to result on thebasis of service user <strong>in</strong>volvement.Care pathways, plann<strong>in</strong>g and dischargeThe Care Programme Approach (CPA) provides theoverarch<strong>in</strong>g framework for the provision of mentalhealth services <strong>in</strong> England. Implicit is the <strong>in</strong>volvementof the person us<strong>in</strong>g the service and whereappropriate, their carer. The key to successful CarePlann<strong>in</strong>g and Care Pathways lay <strong>in</strong> the relationshipsbetween women service users, their care coord<strong>in</strong>atorand the team <strong>in</strong>volved <strong>in</strong> the care overall.Not all services <strong>in</strong>vited women to attend the whole ofthe CPA meet<strong>in</strong>g and some did not always want toattend (6.2). However, women did want to believethat they had made a significant contribution throughtheir own and others’ reports. Staff and womenservice users reported <strong>in</strong>consistencies of approach tocare plans and <strong>in</strong>put to CPAs which had resulted <strong>in</strong>some women challeng<strong>in</strong>g the content of report<strong>in</strong>g tocare teams and at review meet<strong>in</strong>gs (6.3). Women’s<strong>in</strong>volvement was patchy and ranged from one casestudy area where women said they had little or no<strong>in</strong>volvement <strong>in</strong> their Care Plans to one area wherewomen were <strong>in</strong>vited to provide a weekly report toward meet<strong>in</strong>gs about their care and progress. It wasnot clear that the impact of gender was be<strong>in</strong>gconsidered consistently <strong>in</strong> care plann<strong>in</strong>g, review orwith care coord<strong>in</strong>ators.Women service users and professionals agreed thatthere was a lack of suitable move‐on accommodation(6.6). Access to rehabilitation wards or low secureservices was severely limited. This had resulted <strong>in</strong> abottle‐neck situation until such time as appropriateiii
provision could be provided. In January 2009, only 12of 27 women’s medium secure services provided arehabilitation ward and just over half (14) had accessto their own low secure services. There was someevidence of <strong>in</strong>creased support provided by communityforensic teams to enable women to move <strong>in</strong>to thecommunity. Four pilot community therapeuticresidential services have been established for womenmany of whom will come from medium secureprovision.Day‐to‐day for staffWomen’s experience of medium secures services wasshaped by the staff and other professionals who theycame <strong>in</strong>to contact with. The composition of theworkforce, the provision of a multi‐discipl<strong>in</strong>ary teamand offer<strong>in</strong>g tra<strong>in</strong><strong>in</strong>g and support to staff wereessential <strong>in</strong> the delivery of services. Services wantedto work with dedicated, stable staff teams with anappropriate gender mix. However, given difficulties ofrecruitment and retention <strong>in</strong> areas, it was rare thatthis was achieved (7.1). Services looked for staff whowere motivated, committed and empowered <strong>in</strong> theirwork (7.2). In mixed‐sex services it was not alwayspossible to apply to work with women only. Thusthere was an element of uncerta<strong>in</strong>ty about therecruitment of appropriate staff. Services tried tobuild up a regular pool of agency staff <strong>in</strong> the <strong>in</strong>terestsof consistency on the unit.Although staff at all levels considered tra<strong>in</strong><strong>in</strong>g andsupervision key to effective delivery, there wereconsiderable gaps between policies and whathappened <strong>in</strong> practice result<strong>in</strong>g <strong>in</strong> many staff receiv<strong>in</strong>gno gender awareness tra<strong>in</strong><strong>in</strong>g (7.3). Reflectivepractice, supervision and access to counsell<strong>in</strong>g andsupport were recommended <strong>in</strong> the servicespecification. These were on offer and usuallyrequired <strong>in</strong> the case study services. However, due toshift patterns, the demand on qualified staff, limitedtime for ‘supervisees’ and sometimes lack ofconfidence among newly qualified/unqualified staff toseek support, supervision frequently took secondplace to service delivery (7.4).Build<strong>in</strong>g on experienceThe evaluation identified many ways <strong>in</strong> which serviceshad addressed the specific needs of women and<strong>in</strong>deed, some providers had been <strong>in</strong>vited to advisemen’s services on their philosophy of care andspecifically relational security. Good practice wasidentified <strong>in</strong> a variety of ways (8.1).Delivery of differential care to meet the specificneeds of women1. Philosophies of care for work<strong>in</strong>g with womenwere embedded with<strong>in</strong> the daily practice of mostcase study services based on gender sensitivepractice, promot<strong>in</strong>g a psycho‐social approachtak<strong>in</strong>g account of the context of women’s mentaldistress and acknowledg<strong>in</strong>g the impact of traumaand abuse on women’s mental health.2. Staff recruitment policies aimed to achieve a 7:3female to male gender ratio, with male staffprovid<strong>in</strong>g positive role models for women,although not all services had managed this yet.They also sought to appo<strong>in</strong>t ward staff with anactive <strong>in</strong>terest <strong>in</strong> and desire to work with women,and <strong>in</strong> most areas, the <strong>in</strong>duction and on‐go<strong>in</strong>g <strong>in</strong>servicetra<strong>in</strong><strong>in</strong>g <strong>in</strong>cluded women’s mental healthissues and gender specific practice.3. Dedicated psychologists for women’s serviceswere able to undertake formulation‐basedassessments and treatment plann<strong>in</strong>g<strong>in</strong>corporat<strong>in</strong>g psychological and socialperspectives acknowledg<strong>in</strong>g the importance ofthe woman’s story and <strong>life</strong> experiences andseek<strong>in</strong>g collaboration with the woman, with herviews and objectives be<strong>in</strong>g noted.4. Purpose‐built facilities as stand alone or attachedto ma<strong>in</strong> mixed‐units usually offered structuredprogrammes of therapeutic gender specificactivities as well as women be<strong>in</strong>g able to accessmixed‐sex sessions if available and appropriate.5. The Assessment and Care Plann<strong>in</strong>g Approaches<strong>in</strong> place suggested that some were formulationbasedencompass<strong>in</strong>g a biological, psychologicaland social perspective and acknowledged thewoman as an expert <strong>in</strong> her own “story” provid<strong>in</strong>ga basis for women to feel they were <strong>in</strong>volved <strong>in</strong>their care plann<strong>in</strong>g.Ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g women’s psychological and physical<strong>safe</strong>ty1. Relational security was well provided for <strong>in</strong> mostcase study areas with<strong>in</strong> regular professionalpractice by staff members on the wards and thestrong therapeutic relationships they built withthe women. Staff were provided withopportunities to develop reflective practice andwere supported to develop therapeuticrelationships with<strong>in</strong> appropriate professionalboundaries through regular group and <strong>in</strong>dividualsupervision.iv
2. Extra Care, Intensive Nurs<strong>in</strong>g Suites or HighSupport Areas on women’s wards allowedwomen who were acutely ill to be cared for awayfrom the ma<strong>in</strong> ward area. These areas were usedas a short term facility only. They providedwomen who were acutely distressed and at risk ofharm<strong>in</strong>g themselves or others with a <strong>safe</strong> butcomfortable environment without the need toisolate them completely, but where <strong>in</strong>tensivenurs<strong>in</strong>g <strong>in</strong>put and emotional support from staffwas available to them.3. Cl<strong>in</strong>ical nurse and other specialists wereemployed with<strong>in</strong> some women’s servicesprovid<strong>in</strong>g risk assessment, care plann<strong>in</strong>g,support and therapeutic and educational<strong>in</strong>terventions for women who, e.g. self <strong>in</strong>jure, aswell as advice and support to members of thecare team <strong>in</strong>volved <strong>in</strong> their care.4. The gender sensitive practice developed onwards supported staff to work towards deescalationus<strong>in</strong>g means other than control andrestra<strong>in</strong>t techniques for manag<strong>in</strong>g women’sbehaviour and it was reported that the use ofcontrol and restra<strong>in</strong>t techniques had become lessfrequent.5. The physical layout of the women’s wards wasmore likely to have been designed to allow zonalobservation with<strong>in</strong> the ma<strong>in</strong> day areas as analternative to <strong>in</strong>tensive one‐to‐one observations,which women often found <strong>in</strong>trusive.6. Team nurs<strong>in</strong>g approaches were developed acrossmost women’s wards so there was always amember of each woman’s team on duty who wasfamiliar with her care plan and <strong>in</strong>dividualformulation.Facilitat<strong>in</strong>g recovery for women, rehabilitation andresettlement1. Seamless care pathways Hav<strong>in</strong>g identified theneed for a gender‐specific route out of mediumsecure care for many of their women service users,some services have worked with regional teamsand commissioners to develop a seamless carepathway for women. Several wards worked with<strong>in</strong>ternal care pathways for women with markersfor progress. One service began the process preadmissionAnother described its access to aCommunity Forensic Team for women whorequired this support once discharged from the<strong>in</strong>patient service.2. The therapeutic treatment approaches on somewomen’s wards meant that women weresupported to develop knowledge and awareness oftheir own mental health needs. This was facilitatedby the women be<strong>in</strong>g given the opportunity toexplore their <strong>life</strong> stories and experiences <strong>in</strong> theirown time and with<strong>in</strong> the context of a trust<strong>in</strong>gtherapeutic relationship, to reach a sharedunderstand<strong>in</strong>g of how this impacted on theirmental well‐be<strong>in</strong>g.3. Women service user <strong>in</strong>volvement <strong>in</strong> serviceplann<strong>in</strong>g and development had enabled somewomen to take on responsibility for facilitat<strong>in</strong>guser group meet<strong>in</strong>gs and be<strong>in</strong>g representatives atexternal user networks and meet<strong>in</strong>gs.4. Social and vocational opportunities In one service,women had access to a voluntary organizationcommissioned to provide education and workrelatedtra<strong>in</strong><strong>in</strong>g and social opportunities <strong>in</strong>clud<strong>in</strong>g,for <strong>in</strong>stance, office work, desktop publish<strong>in</strong>g,participation <strong>in</strong> the runn<strong>in</strong>g of a social club/caféfor service users and advice about external tra<strong>in</strong><strong>in</strong>gand career opportunities. Women were alsocontribut<strong>in</strong>g to decision mak<strong>in</strong>g about ward andother activities <strong>in</strong> some areas.5. Provision of family/child visit<strong>in</strong>g suitesappropriate for children were seen as aconsiderable improvement on previous facilities.Structural and organisational factors1. Multi‐discipl<strong>in</strong>ary teams brought key staff andwomen service users together <strong>in</strong> decision‐mak<strong>in</strong>gprocesses. Staff across case study areasappreciated the value of this model of work<strong>in</strong>g.2. Streaml<strong>in</strong><strong>in</strong>g adm<strong>in</strong>istration wherever possiblefrom referral to discharge helped to ensure asmooth pathway <strong>in</strong>to and through a service. This<strong>in</strong>cluded new computerized systems for record<strong>in</strong>g<strong>in</strong>formation and complet<strong>in</strong>g CPA documentation.One service worked with staff on how they wrotereports to reduce judgmental language andimprove the overall balance of their report<strong>in</strong>g.3. Monitor<strong>in</strong>g activity was required <strong>in</strong> all servicesto provide data to commissioners and/or parentorganisations. Several had <strong>in</strong>troduced additionalways of captur<strong>in</strong>g service delivery, e.g. throughsatisfaction surveys <strong>in</strong> one case designed withwomen service users, staff tra<strong>in</strong><strong>in</strong>g needs analysisand take up of tra<strong>in</strong><strong>in</strong>g and support, as a means ofservice development. Two case study serviceswere develop<strong>in</strong>g research to determ<strong>in</strong>emean<strong>in</strong>gful ways of measur<strong>in</strong>g outcomes.Professionals and women service users also identifiedsignificant gaps and areas where there was room forv
development and improvement (8.2). On the basis ofthe case studies and review of documentation, wehave listed a range of areas which policy makers andservice providers may wish to consider for futuredevelopment.CONSIDERATIONS: ProcessesModels of care:• A written policy for relational security needs tounderp<strong>in</strong> service provision as an aid toconsistency of practice and essential to protectwomen at risk of suicide or self harm as well asaggressive behaviour.• Models of care (whether s<strong>in</strong>gle or based on arange of philosophical precepts) need to besupported by policy and operational practicedocumentation which articulate the approach andits use <strong>in</strong> the service for all staff.Referrals and admissions:• Women need to be able to access a bed <strong>in</strong> theirown geographical area unless they requirespecialized care outside the remit of NHSprovision, and it may be useful for levels ofreferrals and admissions and unmet demand forlocal women’s medium secure placements to beclosely monitored and reviewed.• Women were still not be<strong>in</strong>g appropriatelydiverted from the Crim<strong>in</strong>al Justice System, andthey were often remanded to prison even whenclear history of mental illness. There was little <strong>in</strong>reach <strong>in</strong>to women prisons, and delays <strong>in</strong> transfersto hospital sett<strong>in</strong>gs.• Admission processes need to reflect the womanservice user’s situation and balance this with thecomposition of the unit.• Time is needed for effective admissions <strong>in</strong>clud<strong>in</strong>gopportunities for women to visit the unit and bevisited by staff to <strong>in</strong>itiate the care plann<strong>in</strong>gprocess.Care plan development and implementation:• The development of <strong>in</strong>dividual care plans needs tobe consistent with<strong>in</strong> <strong>in</strong>dividual services. Tra<strong>in</strong><strong>in</strong>gfor staff on the care plan approach with clearerguidance would help to ensure greaterconsistency.• The implementation of <strong>in</strong>dividual care plans needsto be consistent to avoid patch<strong>in</strong>ess of provision,e.g. situations where rehabilitation for somewomen was compromised due to the lack ofavailability of staff.• There is a need for gender sensitive riskassessments and for histories of abuse be<strong>in</strong>gadequately taken <strong>in</strong>to account <strong>in</strong> thedevelopment of care plans.• The recent guidance on CPA recommends that <strong>in</strong>future service users are placed at the centre of theCPA process and are fully <strong>in</strong>volved <strong>in</strong> review<strong>in</strong>gtheir own care plans.Discharge plann<strong>in</strong>g:• Increased step down facilities need to cont<strong>in</strong>ue tobe developed as soon as possible to unblockexist<strong>in</strong>g bottle‐necks <strong>in</strong> some services.• It would also be helpful for discharge plann<strong>in</strong>g tobe commenced from day one of admission, withfor example, home area care coord<strong>in</strong>ators be<strong>in</strong>gasked to identify both possible future communityplacements for when a secure sett<strong>in</strong>g is no longerrequired by the woman, and for the responsibilityfor fund<strong>in</strong>g such future community placements tobe agreed and planned for <strong>in</strong> advance.• Home‐area care coord<strong>in</strong>ators and care teammembers could also be more actively <strong>in</strong>volved <strong>in</strong>the CPA process dur<strong>in</strong>g the women’s stay at theunit.Meet<strong>in</strong>g diverse needs:• Where a s<strong>in</strong>gle women’s ward forms part of theservice (as <strong>in</strong> two case study areas), considerationneeds to be given to the use of communal spaceand provid<strong>in</strong>g for women who may wish to be <strong>in</strong>quieter areas away from ma<strong>in</strong> ward areas.PracticalitiesEnvironment:• Due to the new Standards for MSUs there is nowa requirement for 5.2 metre perimeter fence forall medium secure units, <strong>in</strong>clud<strong>in</strong>g women’sservices even if this is not seen as appropriate.However, environmental security is still importantand should be emphasized due to the risk of selfharm.• Policies need to be implemented which addresshow to deal with environmental risk and itsreview.• Services not <strong>in</strong> purpose build units need toconsider how best to provide zonal rather thanone‐to‐one observations.• Wards need to have 10 and a maximum of 12beds.vi
Activities/OT:• Women’s services <strong>in</strong> mixed‐sex units withoutdedicated OTs may wish to consider facilitat<strong>in</strong>g an<strong>in</strong>crease <strong>in</strong> gender specific groups and activitiesand improve access to activities for women whoare not able to leave the ward or are not able to,or choose not to, attend mixed‐sex activities.Service user <strong>in</strong>volvement:• All services need to consider ways of encourag<strong>in</strong>gwomen to participate as part of their progress.They also need to ensure that feedback isprovided to avoid tokenism.Staff<strong>in</strong>g:• Services need to give consideration torecruitment and as far as possible recruit staffspecifically to the women’s service.• All services need to have job descriptions andperson specifications which reflect theirphilosophies and gender‐sensitive practice.Tra<strong>in</strong><strong>in</strong>g and supervision:• Increased resources <strong>in</strong>clud<strong>in</strong>g time are needed byall services to ensure that tra<strong>in</strong><strong>in</strong>g and supervisionare always available and attended. Take up needsto be monitored by unit/ward managers to furtherensure attendance.• In some areas staff were not receiv<strong>in</strong>gappropriate gender tra<strong>in</strong><strong>in</strong>g. Tra<strong>in</strong><strong>in</strong>g on genderissues as they affect women on the ward andimportantly <strong>in</strong> the community needs to be moreconsistently provided.• Additional models for support need to beencouraged <strong>in</strong>clud<strong>in</strong>g (as already happens <strong>in</strong>some services) peer‐support, mentor<strong>in</strong>g andshadow<strong>in</strong>g for new staff.Primary care:• Lack of access to primary health care services tomeet the physical health care, public health andscreen<strong>in</strong>g issues for women had been identified asa problem at some units.• Standards and Criteria for Women <strong>in</strong> MediumSecure Care from the Quality <strong>Network</strong> forForensic Mental <strong>Health</strong> Services requir<strong>in</strong>g womenmedium secure service to provide access to afemale GP and Practice Nurse, and to appropriatescreen<strong>in</strong>g and well‐women services.The f<strong>in</strong>d<strong>in</strong>gs from the evaluation suggest that thereare a number of ways <strong>in</strong> which the ServiceSpecification could now be updated to reflect thelearn<strong>in</strong>g from dedicated women’s medium secureservices s<strong>in</strong>ce the Implementation Guidance waspublished (8.3)Bartlett, A., & Hassell, Y. (2001). Do women needsecure services? Advances <strong>in</strong> Psychiatric Treatment, 7,302‐309.Forensic Directory (2009) St Andrew’s <strong>Health</strong>careCSIP (2008) Refocus<strong>in</strong>g the Care Programme ApproachTucker, S. & Ince, C. (2008) “Standards and Criteria forWomen <strong>in</strong> Medium Secure Care” Royal College ofPsychiatry: Quality <strong>Network</strong> for Forensic Services.vii
1: Sett<strong>in</strong>g the scene: women’s medium secure services and the evaluationWell, I suppose here it’s different from the high secure hospital I was <strong>in</strong>, you know? I can go out <strong>in</strong> thecommunity, on trips, I can go shopp<strong>in</strong>g. It’s really normal compared to where I was, very normal. Sowhen I came here it was a big change for me, I’d been locked up on big wards. I was there <strong>in</strong> 1989 and myfirst shopp<strong>in</strong>g trip, because I was mov<strong>in</strong>g on, was 2002 and that was the first time that I’d really seen theoutside world, you know? And that was just to shop a little bit and back but here you can, if you want,<strong>in</strong>stead of go<strong>in</strong>g shopp<strong>in</strong>g, you can go to the c<strong>in</strong>ema and you can go to b<strong>in</strong>go. They do community tripsfor a few of us who’ve got community leave, you know? I hadn’t seen those th<strong>in</strong>gs for years. I’d neversat <strong>in</strong> a bar and ate someth<strong>in</strong>g, it just didn’t feel normal to me, but now you just feel you are normal andyou are a human be<strong>in</strong>g, you know, you don’t feel like that at that k<strong>in</strong>d of hospital. I’m glad that peopleare mov<strong>in</strong>g off, especially females, because some don’t need to be <strong>in</strong> that k<strong>in</strong>d of place – I mean, I don’tneed to be, I didn’t need to be <strong>in</strong> there, you know? I’m glad … … gett<strong>in</strong>g out, to a better place. It was no<strong>life</strong> there really.Woman service userIn 2000, there were 39 medium secure services <strong>in</strong> England. Of these, almost all were mixed provisionwith only 14 NHS and 79 <strong>in</strong>dependent sector medium secure beds <strong>in</strong> dedicated women‐only services 1 .In January 2009, there were 27 dedicated women‐only medium secure services (n<strong>in</strong>e <strong>in</strong>dependent and 17NHS) with a total of 51 wards and provid<strong>in</strong>g 543 beds (261 <strong>in</strong> the <strong>in</strong>dependent sector and 282 with<strong>in</strong> NHSservices) 2 . There was at least one service <strong>in</strong> each health region of the country; with six <strong>in</strong> the North‐Westand only one <strong>in</strong> the South‐West. Of the 27 services, 12 had either a women‐only rehabilitation or predischargeward, of which seven provided a women‐only low secure or step‐down service. Five offered awomen‐only low secure service but no rehabilitation or pre‐discharge ward. Four of the 27 services werewomen‐only sites with five on mixed sites but no regular mixed activities. Seventeen were on sites wheresome activities were mixed.This evaluation <strong>in</strong>volved 50 women service users and over 60 professionals <strong>in</strong> look<strong>in</strong>g at the way <strong>in</strong> whichservices have developed and their impact on women’s lives.1.1 Background to the evaluationThe overall aim of this study was to evaluate established, new andemerg<strong>in</strong>g dedicated women’s medium secure mental health services thatcater for women with complex needs. It was funded by the NHS <strong>Research</strong>& Development for Forensic Mental <strong>Health</strong> and approved by the SouthEast Multi‐site <strong>Research</strong> Ethics Committee. The evaluation was supportedby an Advisory Group which <strong>in</strong>cluded women service users.The quality and <strong>safe</strong>ty of secure mental health provision for women hasbeen the focus of research and campaigns 3 , 4 , 5 , 6 and recent policy<strong>in</strong>itiatives 7 . There are consistent and <strong>in</strong>ter‐related themes <strong>in</strong> thisliterature. First, it is repeatedly noted that women with<strong>in</strong> mixed secure
services have been disadvantaged by their m<strong>in</strong>ority status and as aconsequence they have received services that have been primarilydeveloped with men <strong>in</strong> m<strong>in</strong>d, are often unfairly affected by <strong>in</strong>stitutionalresponses to the behaviours of men, and are at risk of furtherpsychological damage 8 , 9 , 10 .Second, evidence has accumulated about the adverse effects of genderand other <strong>in</strong>equalities on the treatment and care of women <strong>in</strong> secureprovision 11 , 12 , 13 , 14 . This <strong>in</strong>cludes the operation of double standards ofbehaviour, pernicious forms of misogyny 15 , 16 and limited access to workand tra<strong>in</strong><strong>in</strong>g 17 .Third, there is <strong>in</strong>creased awareness of the risk to women of harassmentand assault <strong>in</strong> mixed sex facilities 18 , 19 , 20 accompanied by the recognitionthat their therapeutic and <strong>safe</strong>ty needs are unlikely to be met <strong>in</strong> suchcontexts.One consequence of these concerns is that local high and medium secureunits frequently have been deemed unsuitable for ‘difficult’ women.Women‐only wards and units have been pioneered <strong>in</strong> a range of provision<strong>in</strong>clud<strong>in</strong>g dedicated medium secure services for women <strong>in</strong> the<strong>in</strong>dependent sector, and despite the costs and the implications of out ofarea placement this <strong>in</strong>volves it has become the emergent solution formany commissioners and providers 21 . There has also been a rapidexpansion of NHS women only medium secure units. The number of bedshas risen from just over 20 <strong>in</strong> 2000 to nearer 200 <strong>in</strong> 2006, an almost 10fold <strong>in</strong>crease. Nonetheless, Hassell and Bartlett 22 caution that thisdevelopment is likely to have a negative impact on the cont<strong>in</strong>uity of carefor <strong>in</strong>dividual women patients. Furthermore, as the annual costs of such aplacement are typically <strong>in</strong> excess of £125,000, this curtails thedevelopment of community based services that offer both diversion fromsecure service and opportunities for appropriate discharge.The recent development of ‘women’s services’ which is receiv<strong>in</strong>g policysupport from the Department of <strong>Health</strong> 23 , 24 has been largely a responseto the perceived vulnerability – and to a lesser degree the m<strong>in</strong>ority status– of women <strong>in</strong> low and medium secure services. Pilot<strong>in</strong>g and thenprovid<strong>in</strong>g – through Inequality Agenda Ltd – a national tra<strong>in</strong><strong>in</strong>gprogramme for staff work<strong>in</strong>g with women <strong>in</strong> secure services 25 hasprovided us with valuable <strong>in</strong>sights <strong>in</strong>to the demands and possibilities ofchange. It is encourag<strong>in</strong>g to f<strong>in</strong>d with<strong>in</strong> some services a real concern tomeet the mental health needs of women patients and not to ignore orreplicate the damage and deprivation of their earlier lives: we welcomedthis opportunity to evaluate these changes more systematically.Women’s m<strong>in</strong>ority statusis also suggested tocontribute to their be<strong>in</strong>gdeta<strong>in</strong>ed at levels ofsecurity that are muchhigher than they need(Bartlett, 2001).High security hospitalsalways had a degree ofservice segregation.However, <strong>in</strong> establish<strong>in</strong>gwomen‐only wards andunits the problems andneeds of women patients<strong>in</strong> the sector have beenbrought sharply <strong>in</strong>to focusfor many service providers.Historically, recruitmentand retention of staff werea particular problem withwomen’s wards be<strong>in</strong>gcharacterized as chaoticand violent. While this ledsome staff to concludethat ‘women together area nightmare’ and arebetter ‘managed’ onmixed wards, <strong>in</strong> others itawakened a serious<strong>in</strong>terest <strong>in</strong> the provision ofnew, women‐focusedforms of care.F<strong>in</strong>ally, support for the development of better mental health service forwomen from the Department of <strong>Health</strong> 26 , 27 has helped to prioritise thesedevelopments, which also have important relevance for the crim<strong>in</strong>al2
justice system. A recent study of women on remand 28 found that almost60% met criteria for be<strong>in</strong>g diagnosed with a mental disorder, with 11%be<strong>in</strong>g acutely psychotic; though this was be<strong>in</strong>g poorly detected bystandard prison health screen<strong>in</strong>g procedures on entry to prison. This andother evidence 29 , 30 validates current efforts to divert women from thecrim<strong>in</strong>al justice system 31 .1.2 Background to women’s medium secure servicesWomen represent a small m<strong>in</strong>ority (about 15%) of the patient populationwith<strong>in</strong> secure mental health sett<strong>in</strong>gs, and yet they have been much morelikely than men to be deta<strong>in</strong>ed as civil patients, especially <strong>in</strong> high securehospitals. Until recently almost all medium and low secure services havebeen provided <strong>in</strong> mixed‐sex wards which were typically very maledom<strong>in</strong>ated,with many women f<strong>in</strong>d<strong>in</strong>g it difficult to cope <strong>in</strong> theseenvironments. Consequently, <strong>in</strong> the past women have tended to spiral upthe system to high secure care. Dur<strong>in</strong>g 1999, an assessment of all womenpatients <strong>in</strong> high secure hospitals showed that the majority did not requiresuch a high level of security but would be more appropriately cared for <strong>in</strong>conditions of lesser security or community sett<strong>in</strong>gs. (In the case of womenpatients <strong>in</strong> Broadmoor hospital, only 18% were assessed as requir<strong>in</strong>g HighSecure care; Source: HSPSCB 31/12/1999). This position was clearly atodds with the standards set out <strong>in</strong> the new National Service Framework(NSF) for mental health published that year. Standard Five of the NSFstates that service users requir<strong>in</strong>g <strong>in</strong>patient care should be cared for “<strong>in</strong>the least restrictive environment consistent with the need to protect themand the public” 32 .In 2000, the NHS Plan 33 set a target to transfer at least 400 patients out ofhigh secure hospitals with women deemed as a priority group. This targetwas reiterated <strong>in</strong> the Department of <strong>Health</strong> priorities outl<strong>in</strong>ed <strong>in</strong>Improvement, expansion and reform the next three years priorities andplann<strong>in</strong>g framework 2003‐6, emphasis<strong>in</strong>g the need to ensure effective useof secure and forensic facilities. Subsequently the National Women’sMental <strong>Health</strong> (MH) Strategy of 2002 and the Implementation Guidance <strong>in</strong>2003 identified the need for <strong>in</strong>tegrated, dedicated women‐only securemental health services which provide gender‐specific services address<strong>in</strong>gthe specific mental health needs of women (e.g. histories of abuse, selfharm,and women as mothers). It <strong>in</strong>cludes a service specification andstandards for women’s secure services, pre‐empt<strong>in</strong>g the development of anational programme of reprovision of women’s secure services overseenand monitored by the National Oversight Group (NOG). The women’s MHstrategy consultation document highlighted the need for research todeterm<strong>in</strong>e whether there are advantages across a broad range ofoutcomes (<strong>in</strong>clud<strong>in</strong>g service user def<strong>in</strong>ed outcomes), <strong>in</strong> deliver<strong>in</strong>g mentalhealth care <strong>in</strong> women only environments. The implementation guidanceidentifies the need for an <strong>in</strong>dependent evaluation of dedicated women’sDur<strong>in</strong>g 1999, anassessment of all womenpatients <strong>in</strong> high securehospitals showed that themajority did not requiresuch a high level ofsecurity but would bemore appropriately caredfor <strong>in</strong> conditions of lessersecurity or communitysett<strong>in</strong>gs.The women’s MH strategyconsultation documenthighlighted the need forresearch to determ<strong>in</strong>ewhether there areadvantages across a broadrange of outcomes(<strong>in</strong>clud<strong>in</strong>g service userdef<strong>in</strong>ed outcomes), <strong>in</strong>deliver<strong>in</strong>g mental healthcare <strong>in</strong> women onlyenvironments.3
secure services as they represent new models of care. The <strong>in</strong>dependentevaluation will contribute to their cont<strong>in</strong>u<strong>in</strong>g development, enable shar<strong>in</strong>gof good practice, and provide measures of effectiveness of care with<strong>in</strong>these new and emerg<strong>in</strong>g service models for secure care for women.The evaluation will be of specific relevance to the Crim<strong>in</strong>al Justice System(CJS) priorities and <strong>in</strong> particular to the Jo<strong>in</strong>t DH and Prison ServiceStrategy 34 (2001) for develop<strong>in</strong>g mental health services <strong>in</strong> prisons. Thisidentifies performance <strong>in</strong>dicators, <strong>in</strong>clud<strong>in</strong>g the “quicker and moreeffective transfer arrangements for the most severely ill prisoners to NHSfacilities” and recommends <strong>in</strong>creased collaboration with NHS staff <strong>in</strong> themanagement of those who are seriously mentally ill. The Women’sOffend<strong>in</strong>g Reduction Programme (WORP) has a particular focus onmeet<strong>in</strong>g the needs of women with mental health problems. The WORPaction plan 35 <strong>in</strong>cludes action po<strong>in</strong>ts for improv<strong>in</strong>g availability of Mental<strong>Health</strong> Diversion Schemes, equipped specifically to deal with femaledefendants; equal access for women offenders to improved genderspecific mental health services <strong>in</strong>clud<strong>in</strong>g low and medium secure services;and <strong>in</strong> women’s prisons early assessment and identification of mentalhealth problems and need to transfer to NHS facilities at the earliest po<strong>in</strong>tof sentence.Women’s medium secure services form part of a national network ofsecure dedicated NHS services for women be<strong>in</strong>g developed as part of thereprovision of services to facilitate a programme of accelerated dischargeof patients from high secure care where women patients have beenidentified as a priority. The reprovision programme is underp<strong>in</strong>ned by thepr<strong>in</strong>ciples set out <strong>in</strong> Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women’s Mental <strong>Health</strong>:Implementation Guide and <strong>in</strong> particular, the service specification forwomen’s secure services described <strong>in</strong> section 7.2 (p.38‐44).1.3 The chang<strong>in</strong>g landscape:Recent policy, research and service developmentsS<strong>in</strong>ce this evaluation commenced <strong>in</strong> 2006, there have been a number ofimportant policy and service developments that have impacted on theprovision of medium secure mental health services for women. Asummary update on policy and service developments follows.1.3.1 Women <strong>in</strong> the Crim<strong>in</strong>al Justice SystemThere have been several key policy developments <strong>in</strong> relation to women <strong>in</strong>the Crim<strong>in</strong>al Justice System. In response to <strong>in</strong>creases <strong>in</strong> the female prisonpopulation the Home Office 36 launched its Women’s Offend<strong>in</strong>g ReductionProgramme <strong>in</strong> 2004, focus<strong>in</strong>g on improv<strong>in</strong>g community based services and<strong>in</strong>terventions that are tailored for women and support greater use ofcommunity rather than short term prison sentences. Despite this, <strong>in</strong> 2006the number of women <strong>in</strong> custody was still ris<strong>in</strong>g, with a 78% <strong>in</strong>crease <strong>in</strong>4
the number of women remanded <strong>in</strong>to custody over the previous ten years(a rise from 4221 to 7498) 37 . Statistics also showed that most women werestill be<strong>in</strong>g given immediate custodial offences for non‐violent offences,with two‐thirds of women sentenced dur<strong>in</strong>g 2006 given terms of sixmonths or less 38 . The Department of <strong>Health</strong>’s 39 “Women at Risk” reporton the mental health of women <strong>in</strong> contact with the crim<strong>in</strong>al justicesystem, published <strong>in</strong> 2006, recommended the development of better datacollection regard<strong>in</strong>g the needs of this vulnerable group of women to<strong>in</strong>form the plann<strong>in</strong>g and development of services to meet their needswhen transferr<strong>in</strong>g from or leav<strong>in</strong>g prison, as well as the development ofcourt diversion schemes and prison <strong>in</strong>‐reach services for women offenderswith mental health needs. Also <strong>in</strong> 2006, and follow<strong>in</strong>g the deaths of sixwomen at Styal prison, Baroness Jean Corston 40 was commissioned by theHome Office to undertake a review of Women with ParticularVulnerabilities <strong>in</strong> the Crim<strong>in</strong>al Justice System. Her report was published <strong>in</strong>March 2007 and the Government’s response 41 , <strong>in</strong> December 2007,accepted 40 of her 43 recommendations. The Government then producedits first National Service Framework for Female <strong>Offender</strong>s 42 <strong>in</strong> May 2008.However, one of Corston’s key recommendations, stat<strong>in</strong>g that “theGovernment should announce with<strong>in</strong> six months a clear strategy to replaceexist<strong>in</strong>g women’s prisons with geographically dispersed, small, multifunctionalcustodial centres with<strong>in</strong> 10 years”, was not fully taken on boarddespite widespread support for this proposal (a public op<strong>in</strong>ion pollcommissioned by Smart Justice 43 showed 86% of the public questionedsupported the proposal). Follow<strong>in</strong>g a pilot study an announcement wasmade that, whilst the Government accepted the pr<strong>in</strong>ciples upon whichCorston recommended the development of small custodial units forwomen, it had identified significant issues suggest<strong>in</strong>g standalone units ofthe size recommended (20 to 30 women) were neither feasible nordesirable. Implementation of the other recommendations is be<strong>in</strong>gregularly reported on, with a M<strong>in</strong>isterial statement <strong>in</strong> December 2008sett<strong>in</strong>g out progress <strong>in</strong>clud<strong>in</strong>g additional resources to divert vulnerablewomen from custody, development of a cross‐departmental Crim<strong>in</strong>alJustice Women’s Strategy Unit, the publication by NOMS of an <strong>Offender</strong>Management Guide to Work<strong>in</strong>g with Women 44 and Gender SpecificStandards for Women’s Prisons 45 . A review by Lord Bradley <strong>in</strong>to thediversion of offenders with mental health needs or learn<strong>in</strong>g disabilities toappropriate mental health sett<strong>in</strong>gs is due to report to the government <strong>in</strong>early 2009. Its recommendations are due to be taken forward <strong>in</strong> the<strong>Offender</strong> <strong>Health</strong> and Social Care Strategy, currently be<strong>in</strong>g developed bythe Department of <strong>Health</strong> to be published <strong>in</strong> the summer of 2009.Serious concerns regard<strong>in</strong>g the welfare of women prisoners and othervulnerable offenders (<strong>in</strong>clud<strong>in</strong>g those with mental health needs), and the<strong>in</strong>adequateness of the response to their plight, cont<strong>in</strong>ue to be raisedthrough various <strong>in</strong>dependent reports. A report by INQUEST 46 published <strong>in</strong>2008 exam<strong>in</strong>ed women’s deaths <strong>in</strong> custody between 1990 and 2007. It5
evealed a “shameful and deplorable” picture of preventable tragedy, withmany of the women dy<strong>in</strong>g be<strong>in</strong>g <strong>in</strong>appropriately placed <strong>in</strong> custody despiteclear evidence of their requir<strong>in</strong>g care <strong>in</strong> mental health sett<strong>in</strong>gs, and issuesraised from <strong>in</strong>vestigations <strong>in</strong>to deaths <strong>in</strong> 1990 still be<strong>in</strong>g just as prevalent17 years on. A report by the All‐Party Parliamentary Group on Prison<strong>Health</strong> on the Mental <strong>Health</strong> Problem <strong>in</strong> UK HM Prisons 47 described adysfunctional system and recommended a fundamental shift <strong>in</strong> th<strong>in</strong>k<strong>in</strong>g ateach stage of the <strong>in</strong>dividual’s pathway through mental health and crim<strong>in</strong>aljustice services. Dur<strong>in</strong>g 2008 two reports by the Sa<strong>in</strong>sbury Centre forMental <strong>Health</strong> 48 , 49 and one from Policy Exchange 50 all highlightedproblems with <strong>in</strong>adequate fund<strong>in</strong>g and resources for prison mental healthcare <strong>in</strong> England. These <strong>in</strong>cluded a lack of multidiscipl<strong>in</strong>ary expertise <strong>in</strong>prison In‐Reach teams, and an average of just 11% of the prisonhealthcare budget be<strong>in</strong>g spent on mental health care despite the muchhigher prevalence of mental disorder there than <strong>in</strong> the community where15% of health fund<strong>in</strong>g goes towards fund<strong>in</strong>g mental health services. Inaddition, some NHS regions spend significantly less than others, lead<strong>in</strong>g toa post‐code lottery of mental healthcare <strong>in</strong> prisons.1.3.2 Gender and Women’s Mental <strong>Health</strong>Follow<strong>in</strong>g the publication by the Department of <strong>Health</strong> (DH) of its nationalwomen’s mental health strategy 51 , NIMHE (National Institute for Mental<strong>Health</strong> <strong>in</strong> England) established its national programme on gender equalityand women’s mental health <strong>in</strong> order to support the ImplementationGuidance: Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women’s Mental <strong>Health</strong> 52 . Thisaimed to ensure the development of mental health systems able to deliverresponsive and gender sensitive services to meet the specific and diverseneeds of women. The work of the programme s<strong>in</strong>ce 2006 has focused onimprov<strong>in</strong>g women’s <strong>safe</strong>ty <strong>in</strong> <strong>in</strong>patient sett<strong>in</strong>gs as well as develop<strong>in</strong>gwomen only and gender sensitive day services 53 , improv<strong>in</strong>g choice andaccess to psychological therapies, and develop<strong>in</strong>g better per<strong>in</strong>atal mentalhealth services. Informed Gender Practice: Mental <strong>Health</strong> Acute Care thatworks for women 54 was published <strong>in</strong> July 2008 to encourage practitionerswork<strong>in</strong>g <strong>in</strong> acute mental health sett<strong>in</strong>gs to develop gender sensitivepractice with a focus on women’s physical and psychological <strong>safe</strong>ty. Inaddition, follow<strong>in</strong>g a two year pilot project, the Mental <strong>Health</strong> TrustCollaboration Project worked with 16 Mental <strong>Health</strong> Trusts across Englandto improve the care and support provided to service users who havesurvived sexual and other abuse, follow<strong>in</strong>g which a national policy waslaunched <strong>in</strong> June 2008 55 . This <strong>in</strong>cluded the provision of sexual abusetra<strong>in</strong><strong>in</strong>g to all Mental <strong>Health</strong> Trusts <strong>in</strong> England from November 2008 andthe publication of supportive practice guidance <strong>in</strong> April 2009. Deliver<strong>in</strong>gequality for women (<strong>in</strong>clud<strong>in</strong>g race equality for women from BMEcommunities) has also been a recent priority of the Gender and Women’sMental <strong>Health</strong> national programme. To help prepare mental healthproviders for the implementation of equality legislation, it producedguidel<strong>in</strong>es for Mental <strong>Health</strong> Trusts 56 about the implementation of thePublic Sector Gender Equality Duty which came <strong>in</strong>to force <strong>in</strong> April 2007.6
1.3.3 Safeguard<strong>in</strong>g patients, <strong>safe</strong>ty and s<strong>in</strong>gle‐sex provisionIn July 2006 the National Patient Safety Agency 57 released its secondPatient Safety Observatory Report stat<strong>in</strong>g that 122 ‘sexual <strong>safe</strong>ty’ <strong>in</strong>cidents<strong>in</strong> mental health <strong>in</strong>patient wards had been reported to them betweenNovember 2003 and September 2005. These <strong>in</strong>cluded 19 alleged rapes, 13cases of exposure, 18 cases of unwanted sexual advances and 26 cases of“<strong>in</strong>vasive touch<strong>in</strong>g”. Follow<strong>in</strong>g publication of the NPSA report, CommunityCare magaz<strong>in</strong>e used the Freedom of <strong>in</strong>formation Act to request<strong>in</strong>formation from Mental <strong>Health</strong> Trusts about sexual <strong>safe</strong>ty <strong>in</strong>cidents 58 .The 44 Trusts respond<strong>in</strong>g (out of the 70 approached) reported over 300<strong>in</strong>cidents dur<strong>in</strong>g the three years between 2003 and 2006, of which 224<strong>in</strong>volved assaults on patients by other patients. The follow<strong>in</strong>g year theGovernment published new guidance on “Safeguard<strong>in</strong>g Patients” 59 as itsresponse to the recommendations of the Shipman, Ayl<strong>in</strong>g, Neale andKerr/Haslam Inquiries, which covered boundary transgression issues <strong>in</strong>mental health services. This reviews the recommendations <strong>in</strong> theKerr/Haslam and Ayl<strong>in</strong>g <strong>in</strong>quiries about the failure of health organisationsto take seriously allegations of sexual assault on female patients.Dent 60 reported that sexual <strong>safe</strong>ty <strong>in</strong>cidents are treated as part of mentalhealth <strong>in</strong>patient <strong>life</strong> with disbelief built <strong>in</strong>to the system (as there is anattitude that patients cannot be believed because they are ill) and the lackof adequate tra<strong>in</strong><strong>in</strong>g and experienced staff exacerbate poor levels of<strong>safe</strong>ty on mixed <strong>in</strong>patient wards. In 2007, the Royal College ofPsychiatrists 61 produced guidel<strong>in</strong>es on sexual boundary issues <strong>in</strong>psychiatric sett<strong>in</strong>gs which <strong>in</strong>cluded particular issues for secure units andthe <strong>safe</strong>ty of women <strong>in</strong> these sett<strong>in</strong>gs, stat<strong>in</strong>g that their sexualvulnerability must be recognised and addressed by the multidiscipl<strong>in</strong>aryteam <strong>in</strong> <strong>in</strong>dividual care plans. The Mental <strong>Health</strong> Act Commission 62 <strong>in</strong>their Biennial Report for their report<strong>in</strong>g period 2005‐7 also raised seriousconcerns regard<strong>in</strong>g women’s sexual <strong>safe</strong>ty <strong>in</strong> <strong>in</strong>patient sett<strong>in</strong>gs andexpressed disappo<strong>in</strong>tment at the lack of progress <strong>in</strong> implement<strong>in</strong>g theGovernment’s policy on the provision of s<strong>in</strong>gle sex accommodation <strong>in</strong> allhospital wards.In the debate about the implementation by the Government of the LabourParty Manifesto pledge to eradicate mixed sex wards, the Shadow <strong>Health</strong>Secretary released figures from a Freedom of Information Survey <strong>in</strong>January 2009 63 which revealed that 2% of Mental <strong>Health</strong> Trusts were stillus<strong>in</strong>g “night<strong>in</strong>gale wards” (large, dormitory‐style rooms) to look after menand women; 8% still used curta<strong>in</strong>s and 11% used partitions rather thansolid walls to segregate patients <strong>in</strong> some areas; as many as 29% failed toprovide segregated wash<strong>in</strong>g facilities for patients <strong>in</strong> some areas; and 24%did not provide segregated toilet facilities on all wards. The 55 Mental<strong>Health</strong> Trusts respond<strong>in</strong>g to the survey had received 135 compla<strong>in</strong>ts frompatients about privacy and dignity issues <strong>in</strong> hospital dur<strong>in</strong>g the year toSeptember 2008. In response, the Government has announced its clearcommitment to eradicate all mixed‐sex hospital accommodation (<strong>in</strong> all7
cl<strong>in</strong>ical areas apart from Accident and Emergency), and is publish<strong>in</strong>gfurther guidance on its def<strong>in</strong>ition of s<strong>in</strong>gle sex accommodation as well assett<strong>in</strong>g up a £100m Privacy and Dignity Fund to help trust makeimprovements to hospital accommodation over the next six months. In2010/11 it will <strong>in</strong>troduce f<strong>in</strong>es for NHS Trusts not comply<strong>in</strong>g with therequirement to provide <strong>in</strong>patient care <strong>in</strong> s<strong>in</strong>gle sex accommodation 64 .1.3.4 NHS Commission<strong>in</strong>g arrangements and M<strong>in</strong>imum StandardsIn March 2006 the Government White Paper “Our <strong>Health</strong>, Our Care, OurSay” 65 outl<strong>in</strong>ed plans for major structural changes and a ‘changemanagement’ programme aimed at develop<strong>in</strong>g “World Class”commission<strong>in</strong>g <strong>in</strong> the NHS. Follow<strong>in</strong>g this, <strong>in</strong> July 2006 the number ofStrategic <strong>Health</strong> Authorities (SHAs) which are responsible for co‐ord<strong>in</strong>at<strong>in</strong>gand manag<strong>in</strong>g Primary Care Trusts was reduced from 28 to just 10 with theaim of strengthen<strong>in</strong>g commission<strong>in</strong>g capacity. The Department of <strong>Health</strong>at the same time published “<strong>Health</strong> Reform <strong>in</strong> England: update andCommission<strong>in</strong>g Framework” 66 which <strong>in</strong>troduced the regionalisation ofcommission<strong>in</strong>g of low and medium secure mental health services. FromApril 2007 these services have been commissioned on behalf of PrimaryCare Trusts by Specialised Commission<strong>in</strong>g Groups set up by the ten newlyformed Strategic <strong>Health</strong> Authorities, with PCT f<strong>in</strong>ancial allocations be<strong>in</strong>gtop‐sliced to fund this specialised commission<strong>in</strong>g. Other developmentsaffect<strong>in</strong>g the commission<strong>in</strong>g of secure mental health services <strong>in</strong>clude the<strong>in</strong>troduction of a new standard mental health contract <strong>in</strong> England whichwill place <strong>in</strong>dependent sector providers on a more level play<strong>in</strong>g field with<strong>in</strong>‐house NHS providers. These new contracts are due to be <strong>in</strong>troduced ona voluntary basis <strong>in</strong> April 2009 and compulsorily from April 2010. They willbe subject to regular reviews, with commissioners expected to review alist of quality <strong>in</strong>dicators as part of contract monitor<strong>in</strong>g. These quality<strong>in</strong>dicators, for medium secure units, are likely to overlap with NationalM<strong>in</strong>imum Standards 67 .Standards for Medium Secure Services that were developed by the RoyalCollege of Psychiatry Quality <strong>Network</strong> for Forensic Services have beenadopted by the Department of <strong>Health</strong> as National M<strong>in</strong>imum Standards foradult medium secure services <strong>in</strong> England with the Department publish<strong>in</strong>gBest practice Guidance based on these standards <strong>in</strong> July 2007. 68 TheRCPsych Quality <strong>Network</strong> has subsequently developed an additional set ofStandards and Criteria to specifically address the needs of Women <strong>in</strong>Medium Secure Care 69 . In 2009, only n<strong>in</strong>e women’s medium secureservices had become members of the Quality <strong>Network</strong> although jo<strong>in</strong><strong>in</strong>gwill become a requirement <strong>in</strong> the future. The add‐on standards forwomen’s services have yet to be adopted by the Department of <strong>Health</strong> asrequired quality standards for the Specialised Commission<strong>in</strong>g Groups to<strong>in</strong>corporate when develop<strong>in</strong>g their service specifications for women’ssecure services.8
1.3.5 Service developments for women requir<strong>in</strong>g medium secure careConcurrent with the evaluation process there has been a number of majorservice developments <strong>in</strong> secure mental health provision for women,<strong>in</strong>clud<strong>in</strong>g the closure of Broadmoor Hospital’s Women’s Service dur<strong>in</strong>g2007. This leaves just one National High Secure Service for women atRampton Hospital, based <strong>in</strong> a new purpose‐built facility which opened <strong>in</strong>December 2006 provid<strong>in</strong>g 50 beds across four wards <strong>in</strong>clud<strong>in</strong>g one forwomen with learn<strong>in</strong>g disabilities.Dur<strong>in</strong>g 2007 and 2008, three Women’s Enhanced Medium Secure Services(WEMSS) have been opened, one each <strong>in</strong> the North West, East Midlandsand London regions. Additionally, four High Support CommunityResidential projects are be<strong>in</strong>g developed to enable the rehabilitation andcommunity resettlement of women leav<strong>in</strong>g secure mental health services.Both of these new developments are pilot schemes funded by theDepartment of <strong>Health</strong> as part of the strategy for the Reprovision ofWomen’s Secure Services, and are aimed at improv<strong>in</strong>g care pathways forwomen <strong>in</strong> secure services. As well as these nationally commissioneddevelopments a significant number of additional medium secure beds <strong>in</strong>both the NHS and Independent sector were opened dur<strong>in</strong>g this period.This reorganisation of women’s secure services has seen the rapidexpansion of NHS women‐only units with many NHS Commissionersaim<strong>in</strong>g to return women placed <strong>in</strong> private out of area treatment service to<strong>in</strong>‐house NHS provision <strong>in</strong> their home area 70 , although private sectorprovision also cont<strong>in</strong>ues to expand with further <strong>in</strong>dependent sectorunits/beds open<strong>in</strong>g dur<strong>in</strong>g 2007‐08. In 2000, a survey of all mediumsecure units 71 found just 14 NHS medium secure beds for women <strong>in</strong> s<strong>in</strong>glesex wards and 79 medium secure beds <strong>in</strong> s<strong>in</strong>gle sex units <strong>in</strong> the<strong>in</strong>dependent sector. At that time most medium secure beds for womenwere provided with<strong>in</strong> mixed sex ward accommodation, and these provideda further 249 women’s beds, mak<strong>in</strong>g the total medium secure bedcapacity for women to 343. However, by January 2009 a follow‐uptelephone survey to all providers of medium secure care for women <strong>in</strong>s<strong>in</strong>gle gender units (see section 2) found the number of medium securebeds for women <strong>in</strong> s<strong>in</strong>gle sex sett<strong>in</strong>gs had <strong>in</strong>creased to 543 across bothsectors (NHS and Independent), with just a small number of women’s bedsstill provided <strong>in</strong> mixed sex wards, although these are now very much theexception rather than the rule.1.4 The evaluation approachWith<strong>in</strong> the context of the literature, policy and practice and <strong>in</strong> order toachieve its aim, the evaluation had six objectives as follows:• to exam<strong>in</strong>e the extent to which and how these services are deliver<strong>in</strong>gcare, support and treatment which meet the specific needs of women• to exam<strong>in</strong>e the extent to which and how these services are able to9
ma<strong>in</strong>ta<strong>in</strong> women’s <strong>safe</strong>ty and security <strong>in</strong> l<strong>in</strong>e with the servicespecification for dedicated secure services for women (detailed <strong>in</strong>Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women’s Mental <strong>Health</strong>: ImplementationGuidance)• to explore factors which help and h<strong>in</strong>der services <strong>in</strong> deliver<strong>in</strong>gappropriate care, support and treatment• to make recommendations for future service development• to enable women to participate <strong>in</strong> the process and express their viewsand needs• to enable other key stakeholders to contribute to the development ofwomen’s secure servicesThe evaluation did not set out to exam<strong>in</strong>e the extent to which women’smedium secure services were deliver<strong>in</strong>g differentiated care to meet thespecific and <strong>in</strong>dividual needs of women. This would have required a more<strong>in</strong>‐depth study of a small cohort of women service users. Further, it wasnot designed to exam<strong>in</strong>e the longer‐term outcomes of the servicesprovided to women. However, a follow‐up study of women who havemoved on from medium secure services would provide an <strong>in</strong>sight <strong>in</strong>to theimpact of differentiated care on women’s futures.Women‐only secure services <strong>in</strong>volved <strong>in</strong> the evaluation <strong>in</strong>cluded:• NHS self‐conta<strong>in</strong>ed women‐only units where either there are no malewards on site or women do not mix with male patients from otherwards.• NHS self‐conta<strong>in</strong>ed women‐only secure units where there is some levelof mix<strong>in</strong>g with male patients.• Independent sector and “not for profit” services.In addition to a survey of all women‐only medium secure services <strong>in</strong>England (NHS and Independent), six case study services were <strong>in</strong>vited tocontribute <strong>in</strong> more depth to the evaluation. From these the evaluationlearned about what helps or h<strong>in</strong>ders <strong>in</strong> develop<strong>in</strong>g services for women andabout how different contexts impact on provision.The case studies were based on a number of different stages <strong>in</strong>clud<strong>in</strong>g:1. Two stage qualitative study of women patients’ perceptions andviews: an <strong>in</strong>itial <strong>in</strong>terview used Repertory Grid <strong>in</strong>terview<strong>in</strong>gtechniques and women service users were <strong>in</strong>vited to talk about theirexperience of the service. The method provided an opportunity forwomen to determ<strong>in</strong>e the constructs and elements (roles of people andwhat they associate with them) which they considered important andcontributed to their perceptions and views. Some women took part <strong>in</strong>a follow up <strong>in</strong>terview.2. Rank order<strong>in</strong>g exercise: a content analysis of the <strong>in</strong>terviews withwomen was carried out to identify the most featured constructs and10
then women as well as other stakeholders were asked to rank them <strong>in</strong>order of importance. A comparison has helped us appreciate thedegree of shared understand<strong>in</strong>g of the aspects of the service thatwomen valued.3. Semi‐structured <strong>in</strong>terviews with other stakeholders: with cl<strong>in</strong>icians,support staff, advocates, service managers, multi‐discipl<strong>in</strong>ary teammembers and commissioners were conducted which explored theirexperience and views of deliver<strong>in</strong>g differentiated care and treatmentof women patients.4. Documentary review: a review of policies and protocols <strong>in</strong> order tounderstand the context.5. Documentary review and audit of CPA reviews: from this theevaluation explored women’s <strong>in</strong>volvement <strong>in</strong> care plann<strong>in</strong>g, gaug<strong>in</strong>gtheir progress towards discharge and recovery.In total, 50 women and 65 staff and other professionals participated <strong>in</strong><strong>in</strong>dividual discussions. Appendix 1 provides details of the evaluationapproach and methods and reflects on their use <strong>in</strong> this context.1.5 Report structureThis report is divided <strong>in</strong>to a further seven sections.• Section 2 provides a descriptive background and a map of serviceprovision across England as well as case study portraits.• Section 3 provides an overview of women’s journeys through mediumsecure services focus<strong>in</strong>g on what helps or h<strong>in</strong>ders them <strong>in</strong> gett<strong>in</strong>gwhere they hope to arrive; the philosophy and models of care <strong>in</strong> useand the implementation of policies that facilitate a route through.• Section 4 reflects on women’s day‐to‐day realities; their carepathways <strong>in</strong>, at and on from secure services with exploration of theearly days, admissions and arrival; and how <strong>life</strong> works on the wards.• Section 5 discusses mak<strong>in</strong>g it work for women patients and for staffwhilst ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g women’s <strong>safe</strong>ty.• Section 6 focuses on Care Pathways, Care Plann<strong>in</strong>g <strong>in</strong> theory and <strong>in</strong>practice as well as women’s discharge and mov<strong>in</strong>g on from mediumsecure services.• Section 7 is concerned with the work<strong>in</strong>g environment, ward staff andother professionals and the ways <strong>in</strong> which their experience has animpact on the service and the women with<strong>in</strong> it.• Section 8 looks to the future of gender sensitive, dedicated women’smedium secure services draw<strong>in</strong>g on what works well and areas forfuture development.Good practice <strong>in</strong> the case study areas was identified through the range ofdata collection methods and examples are <strong>in</strong>cluded throughout the report.It is important to note that all the services were at different stages – some11
well established, others new; some <strong>in</strong>volved <strong>in</strong> major expansions; someexperienc<strong>in</strong>g changes <strong>in</strong> leadership and management structures, and alldeliver<strong>in</strong>g a service with<strong>in</strong> a context of the effects of their <strong>in</strong>dependent,charitable and NHS status on funds and services.1 Bartlett, A., & Hassell, Y. (2001). Do women need secure services? Advances <strong>in</strong> Psychiatric Treatment, 7, 302‐309.2 Forensic Directory (2009) St Andrew’s <strong>Health</strong>care3 Allen, H. (1987). Justice Unbalanced; Gender, Psychiatry and Judicial Decisions. Milton Keynes: Open University Press4 Potier, M. (1993). Giv<strong>in</strong>g evidence: women's lives <strong>in</strong> Ashworth maximum security psychiatric hospital. Fem<strong>in</strong>ism andPsychology, 3(3), 335‐3475 Stafford, P. (1999). Def<strong>in</strong><strong>in</strong>g Gender Issues: Redef<strong>in</strong><strong>in</strong>g Women' Services. London: Women <strong>in</strong> Secure Hospitals (WISH)6 WISH. (1998). Break<strong>in</strong>g through the Barriers – Annual Report 1997‐1998. London: Women <strong>in</strong> Secure Hospitals (WISH)7 Department of <strong>Health</strong>. (2000). Provision of NHS Mental <strong>Health</strong> Services (Fourth Report of the Select Committee).London: The Stationery Office8 Barnes, M., Davis, A., Guru, S., Lewis, L., & Rogers, H. (2002). Women‐only and Women‐sensitive Mental <strong>Health</strong>Services: an Expert Paper. London: Department of <strong>Health</strong>9 L<strong>in</strong>dsay, D. G., Thomson, J. P. B., Mart<strong>in</strong>, S. H., & Johnstone, E. C. (2001). A survey of female patients <strong>in</strong> high securitypsychiatric care <strong>in</strong> Scotland. Crim<strong>in</strong>al Behaviour and Mental <strong>Health</strong>, 11, 86‐9310 Williams, J., Scott, S., & Bress<strong>in</strong>gton, C. (2004). Dangerous journeys: women's pathways through secure services. InN. Jeffcote & T. Watson (Eds.), Work<strong>in</strong>g Therapeutically with Women <strong>in</strong> Secure Sett<strong>in</strong>gs. London: Jessica K<strong>in</strong>gsley11 Aitken, G., & Noble, K. (2002). Violence and violation: women and secure sett<strong>in</strong>gs. Fem<strong>in</strong>ist Review, 68(Summer),68‐8812 McKeown, M., Anderson, J., Bennett, A., & Clayton, P. (2003). Gender politics and secure services for women:reflections on a study of staff understand<strong>in</strong>gs of challeng<strong>in</strong>g behaviour. Journal of Psychiatric and Mental <strong>Health</strong>Nurs<strong>in</strong>g, 15, 585‐59113 Warner, S., & Wilk<strong>in</strong>s, T. (2004). Between subjugation and survival: Women, borderl<strong>in</strong>e personality disorder andhigh security mental hospitals. Journal of Contemporary Psychotherapy, 34(3), 265 ‐ 27814 Williams, J., Scott, S., & Bress<strong>in</strong>gton, C. (2004). Dangerous journeys: women's pathways through secure services. InN. Jeffcote & T. Watson (Eds.), Work<strong>in</strong>g Therapeutically with Women <strong>in</strong> Secure Sett<strong>in</strong>gs. London: Jessica K<strong>in</strong>gsley15 Allen, H. (1987). Justice Unbalanced; Gender, Psychiatry and Judicial Decisions. Milton Keynes: Open UniversityPress16 Williams, J., Scott, S., & Bress<strong>in</strong>gton, C. (2004) op.cit.17 Hamlyn, B. (2000). Women prisoners: a survey of their work and tra<strong>in</strong><strong>in</strong>g experiences <strong>in</strong> custody and on release.London: Home Office <strong>Research</strong>, Development and Statistics Directorate18 Aitken, G., & Noble, K. (2002) op.cit.19 Department of <strong>Health</strong>: Women’s Mental <strong>Health</strong>: <strong>in</strong>to the ma<strong>in</strong>stream, DH 200220 Warner, S., & Wilk<strong>in</strong>s, T. (2004) op.cit.21 Bartlett, A., & Hassell, Y. (2001) op.cit.22 Bartlett, A., & Hassell, Y. (2001) ibid.23 Department of <strong>Health</strong> (2002) op.cit.24 Department of <strong>Health</strong> Implementation Guidance: Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women’s Mental <strong>Health</strong>, DH 200325 Scott, S., & Williams, J. (2004). Staff tra<strong>in</strong><strong>in</strong>g and support. In N. Jeffcote & T. Watson (Eds.), Work<strong>in</strong>g Therapeuticallywith Women <strong>in</strong> Secure Sett<strong>in</strong>gs. London: Jessica K<strong>in</strong>gsley.26 Department of <strong>Health</strong> (2002) op.cit.27 Department of <strong>Health</strong> Implementation Guidance (2003) op.cit.28 Parsons, S., Walker, L., & Grub<strong>in</strong>, D. (2001). Prevalence of mental disorder <strong>in</strong> female remand prisons. Journal ofForensic Psychiatry, 12(1), 194‐20229 O’Brien, M., Mortimer, L., S<strong>in</strong>gleton, N., & Meltzer, H. (2001). Psychiatric Morbidity among Women Prisoners <strong>in</strong>England and Wales. London: Office for National Statistics30 Scott, S., & Williams, J. (2004) op.cit.31 Home Office (2004) Women’s Offend<strong>in</strong>g Reduction Programme32 Department of <strong>Health</strong> (1999)12
33 Department of <strong>Health</strong>. (2000). Provision of NHS Mental <strong>Health</strong> Services (Fourth Report of the Select Committee).London: The Stationery Office34 Department of <strong>Health</strong> (2001) Jo<strong>in</strong>t DH and Prison Service Strategy London: The Stationery Office35 Home Office (2004) op.cit.36 Home Office (2004) op.cit.37 M<strong>in</strong>istry of Justice, Population <strong>in</strong> Custody, England and Wales, March 200838 M<strong>in</strong>istry of Justice (2007) Sentenc<strong>in</strong>g Statistics 2006, December 200739 DH/CSIP (2006) Women at Risk – The mental health of women <strong>in</strong> contact with the crim<strong>in</strong>al justice system. London ,Department of <strong>Health</strong>40 The Corston Report, Home Office, March 200741 Government Response to the Corston Report, Home Office, December 2007.42 M<strong>in</strong>istry of Justice/NOMS (2008) National Service Framework: Improv<strong>in</strong>g Services to Women <strong>Offender</strong>s, May 2008.43 Smart Justice (2007) ‘Public say: stop lock<strong>in</strong>g up so many women’44 NOMS (2008) <strong>Offender</strong> Management Guide to work<strong>in</strong>g with women, London, M<strong>in</strong>istry of Justice45 NOMS (2008) Gender Specific Standards for women’s prisons, London, M<strong>in</strong>istry of Justice46 INQUEST (2008) Dy<strong>in</strong>g on the Inside: Exam<strong>in</strong><strong>in</strong>g women’s deaths <strong>in</strong> prison, April 200847 All Party Parliamentary Group on Prison <strong>Health</strong>: (2006) The Mental <strong>Health</strong> Problem <strong>in</strong> UK HM Prisons48 SCMH (2008) Short‐Changed: spend<strong>in</strong>g on prison mental health care: London Sa<strong>in</strong>sbury Centre for Mental <strong>Health</strong>49 SCMH (2008) From the Inside: Experiences of Prison Mental <strong>Health</strong> Care; London: Sa<strong>in</strong>sbury Centre for Mental<strong>Health</strong>50 Brooker C et al (2008) Out of Sight, Out of M<strong>in</strong>d the state of mental healthcare <strong>in</strong> prison; Policy Exchange51 Department of <strong>Health</strong> (2002) op.cit.52 Department of <strong>Health</strong> Implementation Guidance (2003) op.cit.53 Department of <strong>Health</strong> (2006) Support<strong>in</strong>g Women Into the Ma<strong>in</strong>stream – Commission Women‐only Community DayServices DH54 Williams J & Paul J (2008) “Informed Gender Practice: Mental <strong>Health</strong> Acute Care that works for women.” NIMHE July55 NHS Confederation: Brief<strong>in</strong>g 162 Implement<strong>in</strong>g national policy on violence and abuse. NHS Confederation Mental<strong>Health</strong> <strong>Network</strong> <strong>in</strong> association with CSIP/DH, June 200856 CSIP (2007) “Deliver<strong>in</strong>g Gender Equality: “Rough Guide” to Gender Proof<strong>in</strong>g your service”: CSIP West MidlandDevelopment Centre, March 2007.57 National Patient Safety Agency (2006) With Safety <strong>in</strong> M<strong>in</strong>d. Patient Observatory Report No. 258 Community Care, 20 July p.6 and Mental <strong>Health</strong> Today September 2008 p.8.59 Department of <strong>Health</strong> (2007) Safeguard<strong>in</strong>g Patients: The Government Response to the recommendations of theShipman Inquiry’s fifth report and to the recommendations of the Ayl<strong>in</strong>g, Neale and Kerr/Haslam Inquiries. TSO April200760 Dent E. (2007) “Mental <strong>Health</strong>: The Safety Scandal” <strong>in</strong> the <strong>Health</strong> Service Journal, 8 November 2007 pp 22‐2461 Royal College of Psychiatrists College Report (CR145)(2007) Sexual boundary issues <strong>in</strong> psychiatric sett<strong>in</strong>gs, LondonJune 2007.62 MHAC (2008) Risk, Rights, Recovery Twelfth Biennial Report 2005‐2007, London, TSO63 Guardian.co.uk: 9th January 2009 “M<strong>in</strong>isters fail<strong>in</strong>g to abolish mixed‐sex wards, claim Tories”64 Guardian.co.uk : 28 th January 2009 “Hospitals with Mixed sex wards to face f<strong>in</strong>es – government measure aims tostop men and women be<strong>in</strong>g treated together <strong>in</strong> the NHS”.65 Department of <strong>Health</strong> (2006) “Our <strong>Health</strong>, Our Care, Our Say” DH66 Department of <strong>Health</strong> (2006) <strong>Health</strong> Reform <strong>in</strong> England: update and commission<strong>in</strong>g framework DH67 La<strong>in</strong>g & Buisson (2008) Market Report for Specialist Mental <strong>Health</strong> Services 2007‐08 edition68 Department of <strong>Health</strong> (2007) Best Practice Guidance: Specification for adult medium secure services, London , DH69 Tucker S & Ince C. (2008) “Standards and Criteria for Women <strong>in</strong> Medium Secure Care” Royal College of Psychiatry:Quality <strong>Network</strong> for Forensic Services.70 Dent E. (2006) “The Safer Sex” <strong>in</strong> The <strong>Health</strong> Service Journal. 6 th June 2006 p22‐2671 Hassell Y et al (2001) “The Chang<strong>in</strong>g climate for women patients <strong>in</strong> medium secure psychiatric units” PsychiatricBullet<strong>in</strong> (2001) 25: 340‐34213
2: Mapp<strong>in</strong>g service provision across EnglandI don’t want to spend the rest of my <strong>life</strong> <strong>in</strong> here or <strong>in</strong> hospital. I’ve only been <strong>in</strong> two and now I’m mov<strong>in</strong>gforward, you know, forward <strong>in</strong>stead of go<strong>in</strong>g backward. But it’s really normal compared to where I was.I’m glad that people can move off. I’m glad for gett<strong>in</strong>g to a better place.Woman service userWhat I get is a <strong>safe</strong> environment, I guess physically <strong>safe</strong>. I also feel quite happy emotionally that theyhaven’t tried to overdose me with medication. There have been times where I’ve been a bit down and I wasworried, oh God! They’re go<strong>in</strong>g to put me on more medication and – they haven’t! I’ve had quite a lot ofpsychology and the nurs<strong>in</strong>g staff I’ve used to talk to as well.Woman service userThis section of the report provides an overview of dedicated women’s medium secure services <strong>in</strong> Englandas well as detailed descriptions (based on a comb<strong>in</strong>ation of services’ own documentation and additional<strong>in</strong>formation collected for the evaluation) of the six case study services selected for the evaluation.Dur<strong>in</strong>g July 2006, our mapp<strong>in</strong>g exercise identified that <strong>in</strong> England there were 15 NHS Secure Services andeight <strong>in</strong>dependent hospitals provid<strong>in</strong>g medium secure care for women <strong>in</strong> s<strong>in</strong>gle sex wards. These werewomen‐only services or women‐only units with<strong>in</strong> mixed secure sett<strong>in</strong>gs provid<strong>in</strong>g a total of 386 beds across38 wards. This <strong>in</strong>formation was updated with a follow‐up survey of women’s medium secure careproviders. By January 2009, across England there were 18 NHS Trusts and n<strong>in</strong>e <strong>in</strong>dependent hospitalsprovid<strong>in</strong>g medium secure care for women <strong>in</strong> s<strong>in</strong>gle sex ward sett<strong>in</strong>gs with a total of 543 medium securebeds for women with 51 s<strong>in</strong>gle sex wards across the 27 hospital sites. There were 282 NHS; 41 <strong>in</strong>dependentnot‐for‐profit; and 220 <strong>in</strong>dependent beds. In addition to these 543 beds, there were still a small number ofmedium secure beds for women <strong>in</strong> mixed‐sex wards. Some were <strong>in</strong> medium secure services that only hadmixed sex ward facilities for women. Others were <strong>in</strong> mixed‐sex medium secure rehabilitation or predischargewards on sites where there was also s<strong>in</strong>gle sex admission or acute wards. However, these are not<strong>in</strong>cluded here <strong>in</strong> total bed numbers.The geographic spread shows the paucity of provision <strong>in</strong> some areas of the country. At the time of theevaluation, there was a m<strong>in</strong>imum of one NHS women’s medium secure ward or unit <strong>in</strong> each of the tenEnglish NHS Strategic <strong>Health</strong> Authority areas, with just one NHS service per SHA <strong>in</strong> the East Midlands, Eastof England, West Midlands, Yorkshire and Humber, South Central and the South West. However, therewere four NHS medium secure services for women <strong>in</strong> the North West, <strong>in</strong>clud<strong>in</strong>g a specialist learn<strong>in</strong>gdisability service, and as many as five NHS women’s services across the London SHA Region. There werefour <strong>in</strong>dependent organisations provid<strong>in</strong>g medium secure services for women <strong>in</strong> England, with one of thesebe<strong>in</strong>g a registered charity and not‐for‐profit company (St Andrew’s <strong>Health</strong>care Group). The other threewere private sector organisations, of which one (Partnerships <strong>in</strong> Care) dom<strong>in</strong>ates the market for<strong>in</strong>dependent secure service provision and was responsible for six of the n<strong>in</strong>e <strong>in</strong>dependent women’sservices.All medium secure services are governed by the NHS <strong>Health</strong>care Commission Standards although from 1 stApril 2009, a new organisation called the Care Quality Commission (CQC) became responsible for regulat<strong>in</strong>ghealth and social care <strong>in</strong> England. N<strong>in</strong>e services have jo<strong>in</strong>ed the Quality <strong>Network</strong> for Forensic Serviceswhich <strong>in</strong> 2008, and after consultation, published Standards and Criteria for Women <strong>in</strong> Medium SecureServices.15
2.1 The overall pictureIn September 2006 two questionnaires were sent to all providers ofwomen’s medium secure services ask<strong>in</strong>g for <strong>in</strong>formation about all theirwomen only sites and wards. The first concerned the service overall andwas targeted towards service managers or Cl<strong>in</strong>ical Leads for women’sservices. A second questionnaire (<strong>in</strong> some cases more than one) sought<strong>in</strong>formation about <strong>in</strong>dividual women’s wards. In response to this <strong>in</strong>itialsurvey, data was received from 14 of the 20 providers (one opened <strong>in</strong>2008), with 12 NHS Trusts and two of the four <strong>in</strong>dependent providerssupply<strong>in</strong>g <strong>in</strong>formation about their women’s services. In January 2009 andprior to completion of the evaluation, a follow‐up survey was undertakento update our data and mapp<strong>in</strong>g of services. Consequently further<strong>in</strong>formation was collected from all 27 women’s services provid<strong>in</strong>g mediumsecure care <strong>in</strong> s<strong>in</strong>gle sex accommodation, to ensure the most up‐to‐datedescription of provision across England.In 2009, of the 27 services, four described their provision as ‘self‐conta<strong>in</strong>edwomen only with no male wards on site’, six as services on sites wherethere are male wards but where women patients do not usually mix withmen patients; and 17 where there are also male wards on site andopportunities for women to attend some regular mixed‐sex activities.Twelve had only one women’s ward provid<strong>in</strong>g medium secure care. Tenservices had 2 women’s medium secure wards, and five services had threeor more wards offer<strong>in</strong>g medium secure care. Whilst 13 services hadwomen only rehabilitation or pre‐discharge or low dependency wardswith<strong>in</strong> their medium secure service the majority, 14 did not offer aseparate ward for women who no longer required acute care but stillrequir<strong>in</strong>g medium secure care. Three of the NHS services were pilot sitesfor the new Women’s Therapeutically Enhanced Medium Secure Service(WEMSS), and four services offered specialist medium secure care forwomen with learn<strong>in</strong>g disabilities (one NHS; three <strong>in</strong>dependent). As well asthe specialist learn<strong>in</strong>g disabilities services, four others said they acceptedwomen with some learn<strong>in</strong>g disabilities and usually only women with mildor moderate learn<strong>in</strong>g disabilities.Table 1: Current medium secure provision for womenSectorNo. ofsitesNo. ofwardsNo. ofbedsNHS Trusts16 providers18 31 282Independent4 providers9 20 261Totals 27 51 543Source: Forensic Directory 2008/Evaluation survey 2009One <strong>in</strong>dependent hospitalprovided a specialist unitwith five beds for deafwomen requir<strong>in</strong>g mediumsecure care. Whilst all theservices said they didaccept women with adiagnosis of emotionallyunstable personalitydisorder (<strong>in</strong>clud<strong>in</strong>gBorderl<strong>in</strong>e Personality andImpulsive Disorder*), twostipulated they wouldnormally only do so if thewoman also had adiagnosis of Mental Illnessalongside their BPDdiagnosis.* From hereon referred toas BPD given the widerrecognition of thisdiagnostic label especially16
2.1.1 On the wardsFrom the first survey (2006), we received <strong>in</strong>formation about 21 womenonlywards from the 14 respond<strong>in</strong>g services (one ward did not submit).This represented 208 beds <strong>in</strong> total. Ward sizes varied considerably fromfive to 16 beds. However, the smaller wards tended to be with<strong>in</strong> serviceswhich had more than one ward, for example, three five‐bed wards equal to15 beds overall.outside medical arenas.Most wards were full at the time of complet<strong>in</strong>g the questionnaire. Of the21, 16 had women wait<strong>in</strong>g for admission. A number of services noted thatthey rarely had vacancies and had made few of transfers or dischargesfrom the unit.The range of patient groups that these wards were able to cater for<strong>in</strong>cluded:Table 2: Patient groups catered for (n=21)Patient groupIndependentwards (n=6)NHSwards(n=15)Total(n=21)Women diagnosed with mental illness 6 13 19Women with Complex Needs 5 15 20Women with challeng<strong>in</strong>g behavior 5 12 17Women diagnosed with Borderl<strong>in</strong>e Personality 5 11 16DisorderWomen diagnosed with other Personality5 10 15DisorderWomen with learn<strong>in</strong>g disabilities 4 6* 10Other: Autistic Spectrum Disorder 0 4 4* Of these, three only took women with learn<strong>in</strong>g disabilitiesThere was little variation across the wards <strong>in</strong> terms of the patient groupsthey worked with. One provider had recently opened a service for deafwomen and others were dedicated services for women with learn<strong>in</strong>gdisabilities. Three‐quarters of services catered for women diagnosed witheither Borderl<strong>in</strong>e or Personality Disorder.In January 2009 the follow‐up survey of all 27 services provid<strong>in</strong>g mediumsecure care for women <strong>in</strong> s<strong>in</strong>gle sex wards, found that the 51 wards ranged<strong>in</strong> size from only four beds (<strong>in</strong> one WEMSS unit) to as many as 16 beds (<strong>in</strong>an <strong>in</strong>dependent hospital). The average number of beds per ward was 11overall, with an average of 13 beds for <strong>in</strong>dependent sector wards, but justn<strong>in</strong>e beds for NHS wards. (The service specification for Women’s SecureServices <strong>in</strong> the Implementation Guidance for the National Women’sMental <strong>Health</strong> Strategy 72 and the new Standards for Women’s MediumSecure Services 73 recommended a maximum of 12 beds per ward). Bedsper site also tended to be more <strong>in</strong> the <strong>in</strong>dependent sector, with an averageof 29 beds provid<strong>in</strong>g medium secure care for women per site, comparedwith an average of between 15 and 16 beds <strong>in</strong> NHS Trusts.17
2.2 Case study servicesThe follow<strong>in</strong>g descriptions were derived from <strong>in</strong>formation available <strong>in</strong> thepublic doma<strong>in</strong>, documentation sought for the evaluation and additionalmaterial provided through <strong>in</strong>terviews <strong>in</strong> some but not all cases.2.2.1 Case study 1: Newton Lodge NHSNewton Lodge (Yorkshire Centre for Forensic Psychiatry) is a 90‐bedmedium secure unit provided by the South West Yorkshire Mental <strong>Health</strong>NHS Trust and located <strong>in</strong> Wakefield on the Fieldhead Hospital site. It iscommissioned by the Yorkshire and Humber Specialist SecureCommission<strong>in</strong>g Team and caters for adult men and women from theYorkshire catchment area who require <strong>in</strong>patient medium secure mentalhealth services. It provides a service for women from the Humbersidecatchment area who have needs that cannot be appropriately met with<strong>in</strong>the mixed‐sex medium secure facility at the Humber Services <strong>in</strong> Hull. Thegeographical area covered by the unit is a mixture of rural and verysparsely populated areas such as the Yorkshire Moors and Dales, andurban districts <strong>in</strong>clud<strong>in</strong>g the city of Leeds and its surround<strong>in</strong>g conurbation.The Women’s Service, which opened <strong>in</strong> 2000, is based on Gaskell ward, as<strong>in</strong>gle‐sex acute admissions ward with 10 beds and an Extra Care Area.The medium secure rehabilitation or pre‐discharge ward (Priestley) ismixed‐sex with up to six (of 22) beds designated for women provid<strong>in</strong>g acare pathway for women on Gaskell ward who need to access a mediumsecure rehabilitation ward prior to mov<strong>in</strong>g on to low secure or communityfacilities <strong>in</strong> their home district. Women on Priestley are still able to accesssupport and therapeutic <strong>in</strong>put from the Gaskell ward team. The Women’sService also provides a prison <strong>in</strong>‐reach service to HMP New Hall, work<strong>in</strong>gwith women across the prison who are referred for mental health supportas well as those <strong>in</strong> the Prison <strong>Health</strong>care unit. Newton Lodge is alsocommissioned to provide gate‐keep<strong>in</strong>g assessments for men and women<strong>in</strong> community or prison sett<strong>in</strong>gs who are referred for medium secure carewith<strong>in</strong> the responsibility of the Primary Care Trusts across the YorkshireForensic Catchment Group.2.2.2 Case study 2: the Edenfield Centre NHSThe Edenfield Centre is a 118 bed medium secure unit provided by therecently formed Greater Manchester West Mental <strong>Health</strong> NHS FoundationTrust and first opened on the Prestwich Hospital site <strong>in</strong> 1986.Commissioned by the North West Specialist Commission<strong>in</strong>g Team, it catersfor adult men and women from the Greater Manchester area requir<strong>in</strong>g<strong>in</strong>patient medium secure mental health services. It also provides anoutpatient service via its community forensic mental health team. GreaterManchester, <strong>in</strong> the North West of England, is made up of ten metropolitanboroughs and has a large and ‘culturally diverse’ population exceed<strong>in</strong>g 2.5million. The Centre provides gate‐keep<strong>in</strong>g assessments for men andwomen <strong>in</strong> community or prison sett<strong>in</strong>gs who are referred for medium“We developed a forensicstrategy for women acrossYorkshire so the idea ofrecovery was veryfundamental to thatbecause we were look<strong>in</strong>gat hav<strong>in</strong>g a network ofservices across Yorkshirethat would enable womento move through theservices because we foundthat women weren’tgett<strong>in</strong>g stuck at highsecure, but the women wehad were gett<strong>in</strong>g stuck atmedium secure, and often<strong>in</strong> the <strong>in</strong>dependent sector,and the strategy wasabout creat<strong>in</strong>g thisnetwork and an ability tocreate a seamlesspathway for the women.”“I suppose the philosophyof care with women isabout help<strong>in</strong>g themrecover, its about be<strong>in</strong>gconscious of their pastexperiences and howimportant they were <strong>in</strong>th<strong>in</strong>gs be<strong>in</strong>g as they are at18
secure care with<strong>in</strong> the responsibility of the Primary Care Trusts acrossGreater Manchester.Women are a m<strong>in</strong>ority with<strong>in</strong> the <strong>in</strong>‐patient population, currentlyoccupy<strong>in</strong>g about a sixth of the beds. They were cared for on mixed sexwards but, as a response to local and national guidance, the unit openedits first women‐only ward with five beds <strong>in</strong> 1998. A further seven‐bedwomen’s ward opened <strong>in</strong> 2003 as a response to the closure of beds <strong>in</strong>high‐security hospitals with many patients assessed not to require thislevel of security and with the ‘Accelerated Discharge Programme’ aim<strong>in</strong>g toreturn women and men from high secure care to regional/medium secureservices <strong>in</strong> their area of orig<strong>in</strong>.Dur<strong>in</strong>g this process it became evident that many women required a higherlevel of procedural and relational security than was usually available with<strong>in</strong>medium secure sett<strong>in</strong>gs. As a result, a national programme was developedby the Department of <strong>Health</strong> to establish purpose built facilities offer<strong>in</strong>g‘Therapeutically Enhanced Medium Secure Services for Women’TEMSS(W), with the Edenfield Centre be<strong>in</strong>g selected as one of three pilotsites <strong>in</strong> England.The development of this service, which opened <strong>in</strong> July 2007, allowed forthe re‐provision of the exist<strong>in</strong>g 12 women’s beds plus an additional six‘enhanced’ beds <strong>in</strong> a new purpose built facility (i.e. 18 beds <strong>in</strong> total). The<strong>in</strong>patient women’s service therefore now comprises three wards provid<strong>in</strong>gfour ‘therapeutically‐enhanced’ beds; n<strong>in</strong>e beds for women who areacutely unwell <strong>in</strong>clud<strong>in</strong>g two beds for women with complex needs who arestepp<strong>in</strong>g‐down from but with the support of the TEMSS(W); and five bedsfor women whose mental health is currently more stable, provid<strong>in</strong>g a lessrestrictive environment than is available on the acute/admissions ward.the moment, <strong>in</strong> provid<strong>in</strong>gthem with a <strong>safe</strong>environment, <strong>in</strong> try<strong>in</strong>g toget a psychodynamicunderstand<strong>in</strong>g of what ishappen<strong>in</strong>g even if wedon’t use it <strong>in</strong> atherapeutic way with the<strong>in</strong>dividual women.”“One of the th<strong>in</strong>gs I wantto go back about andtry<strong>in</strong>g to th<strong>in</strong>k of positiveth<strong>in</strong>gs around recoveryhere is that we haveattempted to deconstructwhat the women’s needsare and not see them <strong>in</strong>terms of diagnosis but tosee what their cl<strong>in</strong>ical andrisk needs are.”2.2.3 Case study 3: Guild Lodge NHSGuild Lodge, a service provided by Lancashire Care NHS Foundation Trustwas opened <strong>in</strong> 1999 and is commissioned by the North West SpecialistCommission<strong>in</strong>g Team cater<strong>in</strong>g for adult men and women from Lancashireand South Cumbria requir<strong>in</strong>g <strong>in</strong>patient low or medium secure services. Italso provides step‐down accommodation <strong>in</strong> rehabilitation cottages justoutside the secure perimeter and a community forensic mental healthteam. Guild Lodge is commissioned to provide gate‐keep<strong>in</strong>g assessmentsfor men and women <strong>in</strong> community or prison sett<strong>in</strong>gs referred for low andmedium secure care that are the responsibility of the Primary Care Trustsacross Lancashire and South Cumbria.Women represent only about a fifth of the patient population on site andwere historically cared for <strong>in</strong> mixed sex wards. As the women’s service atGuild Lodge developed, a ward opened specifically for women from thedifferent mixed wards. Several years ago when the opportunity came toopen a second ward for women, a decision was made to split the two“We presented modelswith trauma, attachmentand recovery models andhad big discussions abouthow to <strong>in</strong>tegrate thoseand what would work best19
accord<strong>in</strong>g to the cl<strong>in</strong>ical needs of the patient group; with Elmbridgeestablished as an eight‐bedded ward for women with psychosis and/orcognitive needs and Marshaw as an eight‐bedded ward cater<strong>in</strong>g forwomen with relationship and attachment issues. Both wards arecommissioned to provide a service for women requir<strong>in</strong>g either low ormedium secure care. There is also a four‐bedded women’s step‐downfacility <strong>in</strong> the cottages outside the secure perimeter.2.2.4 Case study 4: Fromeside NHSFromeside, near Bristol, was a new 80‐bed medium secure unit and is thelargest development of its type <strong>in</strong> the UK, offer<strong>in</strong>g forensic services to alarge part of the South West <strong>in</strong>clud<strong>in</strong>g rural and urban conurbations ofBristol and Sw<strong>in</strong>don <strong>in</strong> particular. It has a 12 bed self‐conta<strong>in</strong>ed unit forwomen. The service, commissioned by the Avon and Wiltshire Mental<strong>Health</strong> Partnership NHS Trust and opened <strong>in</strong> December 2005, provides amedium secure environment for men and women between the ages of 18and 65. Patients are admitted from the courts hav<strong>in</strong>g been <strong>in</strong>volved withthe crim<strong>in</strong>al justice system, from high secure hospitals or from generalpsychiatric hospitals because they require care with<strong>in</strong> a medium secureenvironment. Some women have been admitted from prison <strong>in</strong>clud<strong>in</strong>gfrom Eastwood Park, a local women’s prison.Fromeside has eight wards of which seven care for men at different stages<strong>in</strong> their recovery and <strong>in</strong> 2005 it opened the new self‐conta<strong>in</strong>ed service forwomen. Fromeside provides a range of facilities <strong>in</strong>clud<strong>in</strong>g a café and theMalago Therapies Centre which <strong>in</strong>cludes workshops, a recreation hall, artspsychotherapy rooms <strong>in</strong>clud<strong>in</strong>g a music therapy workshop and a dramatherapy studio, and a therapies garden.on which ward area. Wehad more discussions onrecovery pr<strong>in</strong>ciples on oneward and trauma andattachment models onanother.”“We want to create an<strong>in</strong>tegrated system ofsecure <strong>in</strong>patient care forwomen. Women’s needsfor security arepredom<strong>in</strong>antly forrelational and proceduralsecurity and thereforemak<strong>in</strong>g the dist<strong>in</strong>ctionbetween exist<strong>in</strong>g (physical)medium and low securecare, particularly forlonger term care, isprobably unnecessary. Thisapproach is likely to createa sufficient critical mass ofpatients that will facilitatethe development of aneffective therapeuticservice [for women].”The women’s service was afforded the opportunity to take two years toplan the service before open<strong>in</strong>g. This allowed for the early appo<strong>in</strong>tment ofstaff, time to consult with women already <strong>in</strong> medium secure sett<strong>in</strong>gs, andto visit other services. The annually reviewed Service Specification statesthat the Women’s Service aims to:• Provide a gender sensitive <strong>in</strong>‐patient service for women who requiremedium security <strong>in</strong> the South West of England.• Provide a quaternary level referral and assessment service for womenfrom the South West.• Assist the forensic case managers <strong>in</strong> the management and plann<strong>in</strong>g ofcare pathways for women from the South West <strong>in</strong> medium and highsecure NHS facilities, out of area and <strong>in</strong>dependent sector placements.• Provide a liaison and advice service to the crim<strong>in</strong>al justice system, localtertiary forensic services and providers of WEMSS and High SecureServices.Teign Ward, as the women‐only service, has developed a policy for malestaff work<strong>in</strong>g on the ward and a philosophy and aims of care as part of its20
operational policy. The service has a strong commitment to reflectivepractice through the process of daily multi‐discipl<strong>in</strong>ary team handovers,weekly meet<strong>in</strong>gs which offer opportunities for reflective practice andthrough supervision. There are monthly psychoanalytic case presentationsfor staff to discuss how they manage their own feel<strong>in</strong>gs. There are fourteam leaders. There are no locked doors with<strong>in</strong> the ward and service user<strong>in</strong>volvement is considered key to the effectiveness of the service. This<strong>in</strong>cludes employment of a service user <strong>in</strong>volvement worker; a closework<strong>in</strong>g relationship with WISH and MIND advocates; appo<strong>in</strong>tmentof service user representatives; weekly community meet<strong>in</strong>gs and women’sfeedback <strong>in</strong>to CPA meet<strong>in</strong>gs. There is a monthly service user steer<strong>in</strong>g groupand facilities management meet<strong>in</strong>g. Community Meet<strong>in</strong>gs on Teign Wardalso form an important aspect of how ‘bus<strong>in</strong>ess’ gets done. The service hasbenefited from hav<strong>in</strong>g time to work with women and build the staff team<strong>in</strong> a way that will lead to susta<strong>in</strong>able approaches and services. Teign Wardhas been acknowledged as develop<strong>in</strong>g <strong>in</strong>itiatives of broader use <strong>in</strong> mediumsecure services and regularly advises plann<strong>in</strong>g <strong>in</strong> the men’s service atFromeside.2.2.5 Case study 5: the Dene, Partnerships <strong>in</strong> Care, IndependentThe Dene, Partnerships <strong>in</strong> Care, is one of five medium secure services theyprovide for women. However, the Dene is the only PiC medium secureservice that caters exclusively for women and it recently extended itsprovision <strong>in</strong> 2008 from 50 beds for women with mental illness to 80 to<strong>in</strong>clude a Learn<strong>in</strong>g Disability service and enhancement to a specialistTrauma and Complex PTSD service. Ward size has <strong>in</strong>creased from 12/13 to16 which has had more recent staff<strong>in</strong>g implications. The service aims for a70/30 ratio but are achiev<strong>in</strong>g approximately 50+ women to 40+ men <strong>in</strong>their ward staff. Psychologists, OTs and social workers have usually beenwomen.The Dene takes women from all over UK, Channel Islands and the Isle ofMan. There are limited secure services for women <strong>in</strong> Wales and Scotlandand these women tend to be referred to the Dene.The Dene aims to <strong>in</strong>volve women <strong>in</strong> 25 hours of activities per week and hasa range of facilities for them to use <strong>in</strong>clud<strong>in</strong>g a sports hall, tennis court,gymnasium and communal recreation areas. Creative activities areavailable with<strong>in</strong> a purpose built art room and workshop, and women haveuse of two practice kitchens. The service also employs a nutritionist and adietician to work with women <strong>in</strong> relation to weight and fitness. There is alibrary which enables women to participate <strong>in</strong> a basic skills programmewith the education team. The psycho‐educational programme coverstrauma, flashbacks, self‐harm, and anger management.PiC has a number of specialist forums <strong>in</strong>clud<strong>in</strong>g one for people withLearn<strong>in</strong>g Disabilities, a Women’s Liaison Group, and a Personality Disordergroup. These forums provide an essential part of service development and“Across the male service,all the teams work acrossseven wards and thatmakes it really hard to allbe s<strong>in</strong>g<strong>in</strong>g from the samehymn sheet, really hard.It’s a privilege to have adedicated team.”“We’ve reorganised theCl<strong>in</strong>ical Governancesystem try<strong>in</strong>g to make surefront‐l<strong>in</strong>e staff understandwhat this is and mak<strong>in</strong>gsure everyone felt<strong>in</strong>volved. Th<strong>in</strong>gs fittogether better now. The<strong>in</strong>dependent sector’sadvantage if that they canredirect its focus to areasof perceived need.”“Our whole ethos isaround women who comehere who have had verymajor problems, verycomplicated lives and a21
staff from the Dene are active representatives. The Dene has implementeda care pathways for women policy, developed by PiC.PiC recently opened a nearby women‐only low secure step down facility,Pelham Woods, with 21 beds. This has positively impacted onopportunities for women from the Dene although the number of beds islimited by comparison to the 80 bed medium secure service.2.2.6 Case study 6: St. Andrew’s Hospital, IndependentSt. Andrew’s is a large <strong>in</strong>dependent hospital located <strong>in</strong> Northampton (andalso a registered charity) with a total of 512 beds cover<strong>in</strong>g medium andlow secure services, as well as open and bra<strong>in</strong> <strong>in</strong>jury services for adults<strong>in</strong>clud<strong>in</strong>g elderly people and adolescents. Until summer 2007, there were25 beds <strong>in</strong> two medium secure wards for women with 14 beds <strong>in</strong> GeneralPsychiatry and 11 beds for women with Learn<strong>in</strong>g Disabilities compared to55 beds for men. Women from both wards then moved to the newpurpose built unit for women’s secure services, Smyth House. The servicehas expanded its total numbers from 25 to 41 and is comprised of threeunits each with access to separate secure outside courtyards.whole set of difficulties.Most have been throughall sorts of treatment orbeen told they areuntreatable or had verynegative experiences. Wesay across the board ‘weare go<strong>in</strong>g to take threemonths and we are justgo<strong>in</strong>g to learn everyth<strong>in</strong>gwe can about who you areand where you come from.We are go<strong>in</strong>g to look at itwith our eyes rather thaneveryone else’s and at theend we will say what ourview is’. We have an ethosthat is all about recoveryfrom the very beg<strong>in</strong>n<strong>in</strong>g.”The Stowe Unit (Mental <strong>Health</strong>) is the most supervised environment andaccommodates service users considered to be at immediate risk of selfharm<strong>in</strong>gand/or physically aggressive behaviours. It has 13 bedrooms, anextra care suite and a seclusion room each of which has en‐suite facilities.The Seacole Unit (Mental <strong>Health</strong>) accommodates service users regarded aspresent<strong>in</strong>g lower risk of self‐harm<strong>in</strong>g and/or physically aggressivebehaviours. It has 15 bedrooms, and a seclusion room each of which hasen suite facilities and lockable storage. The Sitwell Unit (Learn<strong>in</strong>g Disability)will accommodate women who <strong>in</strong>itially require medium security due totheir severe challeng<strong>in</strong>g behaviour and then cont<strong>in</strong>ue to care for thosewho have progressed <strong>in</strong> their treatment and rehabilitation to discharge.The Unit has 13 bedrooms, an extra care suite and a seclusion room.The Women’s Service philosophy of treatment is theoretically based oncontemporary social learn<strong>in</strong>g theory, and <strong>in</strong> practice is based on therecognition of the importance of multi‐discipl<strong>in</strong>ary assessment andtreatment. Social learn<strong>in</strong>g theory emphasises the need to comb<strong>in</strong>e medicaland social treatments <strong>in</strong> a complementary manner, to mitigate the effectsof any illness, and to help promote more adaptive attitudes, skills andbehaviour. The long term aim of treatment is recovery, rehabilitation andaccommodation <strong>in</strong> an appropriate environment, with the least restrictions.2.3 Commission<strong>in</strong>g proceduresAs described <strong>in</strong> 1.3.4, fund<strong>in</strong>g for secure services has undergonerestructur<strong>in</strong>g and services are now commissioned on behalf of PrimaryCare Trusts by Specialised Commission<strong>in</strong>g Groups set up by the ten newly22
formed Strategic <strong>Health</strong> Authorities. The relationship between NHSservices and the Specialised Commission<strong>in</strong>g Groups was relativelystraightforward and often geographically determ<strong>in</strong>ed, i.e. fund<strong>in</strong>g wouldbe provided for women who were from the area. For <strong>in</strong>dependentservices, different types of agreement had to be negotiated. In one casestudy area, the regional commission<strong>in</strong>g team agreed a service levelagreement for the mixed‐sex hospital as a whole. They purchased a blockrather than <strong>in</strong>dividual beds <strong>in</strong>clud<strong>in</strong>g some <strong>in</strong> the women’s service. Theadvantage of this was that it ensured the referral and admissionsprocesses were not adversely affected by difficulties over fund<strong>in</strong>g.A different model operated <strong>in</strong> another case study service where spotpurchas<strong>in</strong>gwas the norm. This and other <strong>in</strong>dependent services were oftenunder commercial pressures to admit women but <strong>in</strong> the knowledge thatthe process of admission was sometimes too rushed and <strong>in</strong>volvedconsiderable ‘paperwork’. They were sometimes unclear about fund<strong>in</strong>gsources which <strong>in</strong>terfered with effect<strong>in</strong>g a smooth referral process.However, a perceived advantage of this model was that services couldrespond with more flexibility to areas of need and provide services towomen where there were gaps <strong>in</strong> other provision.• There was considerable variation across women’s medium secure services <strong>in</strong> terms of provision.• Independent sector services tended to provide a higher number of beds for women. However, theyalso had more than the recommended number per ward/unit.• The case study services, selected on the basis of organisational structure and location, illustrate someof the different ways <strong>in</strong> which the women’s mental health policy agenda has been implemented.72 DOH (2003) op.cit.73 Tucker, S. & Ince, C. (2008) op.cit23
3. Women’s journeys through medium secure services:F<strong>in</strong>d<strong>in</strong>g synergies between philosophies, policies and practiceGood staff will have time for you and talk about your problems and they will listen, be proactive and theywill help you if you are struggl<strong>in</strong>g and perhaps if they are not aware that you are struggl<strong>in</strong>g, they will helpyou as well. They take an <strong>in</strong>terest <strong>in</strong> your care and try and do th<strong>in</strong>gs if you say, like if I say I want to do theOT groups then I would have liked someone to have helped me with that rather than me hav<strong>in</strong>g to goknock<strong>in</strong>g on doors and say<strong>in</strong>g I want to do this. So somebody to help and get your programme the wayyou want it.Woman service userIn an ideal world, women’s medium secure services would operate with a synergy between philosophies ofcare, operational policies and practice based on an <strong>in</strong>‐depth understand<strong>in</strong>g of women’s, carers’ and staffviews of what the service should look like to support women’s recovery. Based on the f<strong>in</strong>d<strong>in</strong>gs from theevaluation, this synergy was exactly what services were try<strong>in</strong>g to achieve. At the same time, they werework<strong>in</strong>g with<strong>in</strong> the conf<strong>in</strong>es of limited resources, different and sometimes compet<strong>in</strong>g views of what wasneeded and what works; and a normative attitude which reflected the gender divide that is pervasive <strong>in</strong>society more broadly. All of these had an impact on how services developed, were successful <strong>in</strong> theirendeavors and how they were perceived by external audiences. This section exam<strong>in</strong>es first what women,and the staff who work with them, believed was essential to creat<strong>in</strong>g an environment that enabled womento benefit from the service and journey through it, which for some would lead to leav<strong>in</strong>g the securesystem. It then moves to describe the philosophies of care <strong>in</strong> place with<strong>in</strong> the case study areas and theextent to which they reflected what women believed was important <strong>in</strong> their care. F<strong>in</strong>ally, it describes thepolicies <strong>in</strong> use and their implementation, assess<strong>in</strong>g how far and <strong>in</strong> what ways they underp<strong>in</strong> the services’ability to achieve their aims and objectives.3.1 Factors affect<strong>in</strong>g women’s routes to recoveryWomen who participated <strong>in</strong> the evaluation were <strong>in</strong>vited to take part <strong>in</strong> anexercise which asked them to identify a set of elements, i.e. people (whichcould <strong>in</strong>clude themselves) <strong>in</strong>volved <strong>in</strong> or enabl<strong>in</strong>g their care. A series ofTriads (sets of three elements) were presented to elicit bi‐polar personalconstructs, i.e. how the women discrim<strong>in</strong>ated between their experiencesof, and relationships with, different elements and women were also askedto rank all the elements (people) aga<strong>in</strong>st all the constructs. Bothqualitative and quantitative analysis of grid data were carried out to arriveat the most frequently referenced factors and women’s commentary onhow they viewed the contribution of people and factors to their recovery.Some women commented that they found this an <strong>in</strong>terest<strong>in</strong>g and usefulexercise where they reflected <strong>in</strong> new ways on their situation and the carethey received. Interest<strong>in</strong>gly, the analysis did not identify particulardifferences between case study sites or between women with differentcharacteristics.25
So, what was most important to women?• Relationship with staff:Women wanted a care team to display human attributes, e.g. sense ofhumour, ability to understand them as <strong>in</strong>dividuals, show empathy, andto share commonalities.• Trust:Women said that only if they believed staff really cared about them,and were not ‘just do<strong>in</strong>g a job’, could they trust them. They needed toknow that staff really listened and could validate their feel<strong>in</strong>gs ratherthan judge or trivialise them.• Positive expectations:Women wanted staff to believe they will get better (recover) andreassure, encourage and provide positive feedback on their progress.• Empower<strong>in</strong>g approach:Women looked to others to help them understand their own illness orbehaviour and take responsibility for manag<strong>in</strong>g this themselves.• Reduc<strong>in</strong>g isolation:Women wanted to ma<strong>in</strong>ta<strong>in</strong> connections with <strong>life</strong> outside the unit andbe enabled to keep contact with family.• Good daily support:Women identified a need for cont<strong>in</strong>uous access to emotional, socialand practical support as well as regular activities to keep themoccupied or take their m<strong>in</strong>d off th<strong>in</strong>gs so that they could cope with <strong>life</strong>on the ward.• Relational Security:Women described the importance of services promot<strong>in</strong>g anatmosphere of trust, strong leadership and consistency of teamapproach with good therapeutic relationships, <strong>in</strong>clud<strong>in</strong>g with malestaff as positive role models.• Holistic Approach:Women sought people who offered understand<strong>in</strong>g of and response tothe social context of their illness or behaviour, e.g. abuse and socioeconomicfactors.• Emotional needs:Women believed <strong>in</strong> the importance of services which ensured thatthey were not just manag<strong>in</strong>g needs but facilitat<strong>in</strong>g the process ofchange.• Range of Interventions:Women wanted robust and structured programmes of appropriatetherapeutic and social activities.While the language sometimes differed, there was consensus amongwomen and staff about the most important attributes of a women’smedium secure service. Women who took part <strong>in</strong> a second <strong>in</strong>terview andall staff and others provid<strong>in</strong>g the service were asked to rank order tenstatements from the women’s perspective. The results of the rankorder<strong>in</strong>g exercise are shown below <strong>in</strong> table 3. There was a high degree of26
correlation between the women’s and professionals’ rank orders(Spearman r 0.85 p
• understand<strong>in</strong>g women as <strong>in</strong>dividuals rather than just see<strong>in</strong>g them assomeone with a particular diagnosis or <strong>in</strong>dex offence• be<strong>in</strong>g available when women needed someone to talk to who listensand validates their feel<strong>in</strong>gs and• work<strong>in</strong>g towards recoveryIn addition, both women service users and staff identified a variety offactors which impacted on women’s potential for recovery <strong>in</strong>clud<strong>in</strong>g thefollow<strong>in</strong>g;• Multi‐discipl<strong>in</strong>ary and ward teams needed to hold values <strong>in</strong> keep<strong>in</strong>gwith gender‐sensitive service philosophies and positive attitudestowards work<strong>in</strong>g with women creat<strong>in</strong>g a culture that is supportive towomen and validates their emotions. A small number of staff and <strong>in</strong>particular among those based at mixed‐provision sites and who had nochoice about which wards they worked on, said they were <strong>in</strong>itiallysceptical about the concept of gender‐sensitive models and s<strong>in</strong>gle‐sexsecure services. However, <strong>in</strong> all the case study areas, most staffdescribed their understand<strong>in</strong>g of the models <strong>in</strong> place and theircommitment to the provision of dedicated women’s secure services.Recruitment was noted as key <strong>in</strong> ensur<strong>in</strong>g that prospective teammembers signed up to exist<strong>in</strong>g philosophies and demonstrated that,even <strong>in</strong> the absence of experience, they held a positive attitudetowards work<strong>in</strong>g with women.• Staff needed to listen to women <strong>in</strong> the context of one‐to‐onetherapeutic relationships and understand their needs with<strong>in</strong> a holistic<strong>life</strong> context. All services used a ‘named’ or ‘primary’ nurse structurewhereby women had ongo<strong>in</strong>g access to a qualified nurse anddeveloped a relationship with someone who knew about their <strong>life</strong>.Usually a second qualified staff member was assigned to each womanwho was the back‐up when the first named was unavailable. Levels ofchoice women were given varied. However, some noted that,although they did not choose who to have, they were able to refer toteam leaders and/or the ward manager if they felt the relationshipwas productive or positive for them. For staff, this was an importantaspect of how they worked with women. Some were frustrated by lackof time to give <strong>in</strong>dividual attention due to their other duties. Otherswere concerned that the nature or content of these relationships wasnot always clear and that they did not always have access toappropriate supervision to enable them to explore their concernsfurther.• Therapeutic relationships needed to facilitate a process of <strong>in</strong>ternalchange and not create on‐go<strong>in</strong>g dependency on mental healthprofessionals. While women and staff valued the provision of highlevels of emotional support, they recognized that this alone would notvery much on us to allowthem to explore emotionswhich have typically beenburied or repressed and hasled to drug use, selfharm<strong>in</strong>g, fire sett<strong>in</strong>g and allof these k<strong>in</strong>d of th<strong>in</strong>gs andthe only th<strong>in</strong>g that is doneby us is to allow them toexperience that as be<strong>in</strong>gconta<strong>in</strong>able so they areallowed to express theseth<strong>in</strong>gs that they feel.”“It’s about recognis<strong>in</strong>g thewomen’s emotional needsand respond<strong>in</strong>g to them butalso enabl<strong>in</strong>g them tounderstand and managethemselves rather thanmeet<strong>in</strong>g some of thewomen’s needs withouthelp<strong>in</strong>g them to recover. It’sabout a process of <strong>in</strong>ternalchange.”“We developed a forensicstrategy for women acrossthe region so the idea ofrecovery was veryfundamental to thatbecause we were look<strong>in</strong>g athav<strong>in</strong>g a network of servicesacross Yorkshire that wouldenable women to movethrough the servicesbecause we found thatwomen weren’t gett<strong>in</strong>gstuck at high secure, but thewomen we had were gett<strong>in</strong>gstuck at medium secure, andoften <strong>in</strong> the <strong>in</strong>dependentsector, and the strategy wasabout creat<strong>in</strong>g this networkand an ability to create aseamless pathway for thewomen.”“They’ll sit with me for hourssometimes, when you’re28
enable women to take <strong>in</strong>creas<strong>in</strong>g responsibility for their mental healthand engage <strong>in</strong> a process of change lead<strong>in</strong>g, it was hoped, to recovery.In addition to team nurs<strong>in</strong>g, some services had <strong>in</strong>troduced groupswhich focused on self‐reflection, awareness rais<strong>in</strong>g and develop<strong>in</strong>gstrategies for self‐management of needs as part of the weeklyprogramme of events. The latter <strong>in</strong>cluded learn<strong>in</strong>g to recognise signsof relapse and develop<strong>in</strong>g appropriate cop<strong>in</strong>g mechanisms. Oneservice had developed an Associate Practitioner role where a memberof staff provided cl<strong>in</strong>ical <strong>in</strong>terventions to women focused on theirunderstand<strong>in</strong>g and self‐management of mental health issues. These<strong>in</strong>cluded self‐<strong>in</strong>jury, hear<strong>in</strong>g voices, self‐esteem and anxietymanagement, with<strong>in</strong> the context of a gradually establishedtherapeutic relationship while work<strong>in</strong>g <strong>in</strong> a support role <strong>in</strong> thewomen’s service.• “Seamless” pathways for women were also identified as important fortheir recovery. For one service, there was only limited access togender‐specific routes out, with some women transferred to a mixedsex rehabilitation ward <strong>in</strong> the same service. Not all PCT areas <strong>in</strong> thisregion had women or men‐only low secure services. This women’sservice, <strong>in</strong>clud<strong>in</strong>g some of the women service users, had worked withtheir Specialist Commission<strong>in</strong>g Team to successfully bid to theDepartment of <strong>Health</strong> for fund<strong>in</strong>g for a High Support ResidentialService for women transferr<strong>in</strong>g out of secure mental health facilities. Itopened <strong>in</strong> early 2009 and, it is hoped, provides a gender‐specific carepathway for women to return to a community sett<strong>in</strong>g either directly orvia rehabilitation or low secure sett<strong>in</strong>gs as appropriate for the<strong>in</strong>dividual.upset, staff will sit and talkyou through it.”Woman service user“<strong>My</strong> CNS has given me a lotof help, seen me through thewhole th<strong>in</strong>g, like self harm –no matter what you arego<strong>in</strong>g through whatever thepa<strong>in</strong> – it’s like she is go<strong>in</strong>gthrough it with you –doesn’t say it’s right orwrong.”Woman service user• Structured ‘therapeutic’ days as well as <strong>in</strong>formal activities wereessential to women whilst conf<strong>in</strong>ed to the wards. Women describedthe monotony of weekends and the importance of be<strong>in</strong>g busy. All thecase study services provided some weekday formal and <strong>in</strong>formalactivities and several offered a full programme to women. Formalactivities ranged from <strong>in</strong>dividual psychology, OT and education togroup work focus<strong>in</strong>g on varied issues. Some services had <strong>in</strong>volvedwomen <strong>in</strong> consideration of what should be on offer. Less formally,services offered hairdress<strong>in</strong>g, opportunities to cook for themselvesand others and occasional social events <strong>in</strong>clud<strong>in</strong>g themed take‐awaymeals. Some staff commented that even the <strong>in</strong>formal activities had atherapeutic potential as they <strong>in</strong>creased self‐esteem and confidence aswell as prepar<strong>in</strong>g women for mov<strong>in</strong>g on from medium secure.• Markers of progress were important as means of reflect<strong>in</strong>g back towomen what had changed dur<strong>in</strong>g their time at the medium secureservice. In addition to the required monitor<strong>in</strong>g of a woman’s progressthrough ongo<strong>in</strong>g discussions with women, with the MDT and throughthe CPA process, some services had <strong>in</strong>troduced <strong>in</strong>novative methods29
which could both motivate women and, depend<strong>in</strong>g on their progress,provide tangible ways of measur<strong>in</strong>g change. One case study servicehad developed a ‘status’ system and an <strong>in</strong>centive programme. Thestatus system enabled women to earn privileges and lose them too.The highest level was four <strong>in</strong> one ward which <strong>in</strong>cluded hold<strong>in</strong>g a roomkey, unsupervised activity, e.g. use of the computer or gym andswimm<strong>in</strong>g pool. Level four meant consideration for a move to adifferent ward and rehab. The level women were placed on reflectedthe progress they were mak<strong>in</strong>g <strong>in</strong> relation to self harm or aggressivebehaviour. Its purpose was to keep women <strong>safe</strong> and enable them toreduce risk to themselves or others. The <strong>in</strong>centive programme paidwomen to attend essential sessions daily over a 12 week period up toa maximum of £1.50 per day.Due to the <strong>in</strong>dividuality of each woman's repertory grid <strong>in</strong>terview, withboth the elements and personal constructs be<strong>in</strong>g freely elicited, it was notpossible to undertake an electronic analysis of aggregated grid data.However, a manual review of how the women rated each construct wasundertaken by look<strong>in</strong>g at the mean scores <strong>in</strong> each grid. From this it wasestablished what women rated most positively, <strong>in</strong> terms of what helps toensure their <strong>safe</strong>ty and their progress toward recovery with the top threethemes be<strong>in</strong>g:1) Relational Security2) Communicat<strong>in</strong>g positive expectations3) Good daily supportIn terms of who the women identified as elements <strong>in</strong> their grid <strong>in</strong>terviews,i.e. who were the <strong>in</strong>dividuals that they felt had an important impact ontheir care and <strong>safe</strong>ty, a member of the nurs<strong>in</strong>g team on the ward wasidentified at least once by all the women <strong>in</strong>terviewed, with theResponsible Cl<strong>in</strong>ician (was RMO) or psychiatrist be<strong>in</strong>g identified as anelement <strong>in</strong> nearly all of the grid <strong>in</strong>terviews. Table 4 gives details of therole/relationship of the <strong>in</strong>dividuals <strong>in</strong>cluded as elements <strong>in</strong> each of the grid<strong>in</strong>terviews.A review of how well each of the elements was rated aga<strong>in</strong>st theconstructs <strong>in</strong> the women’s grid showed that the Primary Nurses were mosthighly rated of the professionals <strong>in</strong>volved <strong>in</strong> their care, whilst “otherpatients” were rated as hav<strong>in</strong>g the most negative impact, with manywomen comment<strong>in</strong>g on the detrimental effect of disruptive behavioursfrom other patients on their ward. It was notable that nearly threequarters of women service users <strong>in</strong>cluded a family member or friend fromoutside the unit. Ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g contact was a key factor to enable somewomen return to their home area.30
Table 4: Elements, i.e. people, <strong>in</strong>cluded <strong>in</strong> Repertory GridsElementNo. of times <strong>in</strong>cluded at %least once <strong>in</strong> gridAny nurse or ward staff 42 100Psychiatrist/Responsible Cl<strong>in</strong>ician 35 83<strong>My</strong>self (Prompted) 31 74Family or friends 30 71Primary/named nurse 24 57Psychologist 19 45Social worker 18 43Occupational therapist 18 43Other patients on ward 18 43Ward managers 12 29Others 12 29It is <strong>in</strong>terest<strong>in</strong>g to note that women, albeit frequently prompted, saw thatthey were also important <strong>in</strong> how they could benefit or not from theservice they received.3.2 Philosophies and models of care: <strong>in</strong> theory and <strong>in</strong> practiceThe survey of all services revealed that, while there may not have beenspecific policies <strong>in</strong> place, most had a philosophy of care which supportedtheir work with women. Some noted that this <strong>in</strong>cluded frameworks formeet<strong>in</strong>g the diversity of need supported by strong ward boundaries andcrucially, effective user <strong>in</strong>volvement processes. In all but one of the casestudy areas the concept of relational security (discussed further <strong>in</strong> section4 of the report) underp<strong>in</strong>ned service philosophies.There were some shared aspects to the philosophies of care adopted bythe case study services and there were as many areas of difference. Herewe briefly describe these philosophies <strong>in</strong> each case study area beforeturn<strong>in</strong>g to the reasons which underp<strong>in</strong> their use, how far and <strong>in</strong> what waysthey enable services to function and, <strong>in</strong>terest<strong>in</strong>gly, why they differ fromone service to another.“The model of care for theenhanced beds is veryclearly def<strong>in</strong>ed but it’s tooearly days to say whether itis an effective model,though I am quite sure it willbe and will maybe need alittle bit of tweak<strong>in</strong>g, but itclearly meets the needs ofthe women. It is based onattachment theory andmentalisation and has aclear evidence base.”In one service, a philosophy of care based on gender sensitive andpsychodynamic approaches with an ethos of empowerment,<strong>in</strong>dependence and recovery, has been <strong>in</strong> place for some years.Recently dur<strong>in</strong>g the sett<strong>in</strong>g up of a new TEMSS(W) service, a moredetailed evidence‐based ‘model of care’ has been developed based onAttachment Theory <strong>in</strong>tegrated with Mentalisation (as developed byBateman and Fonagy 74 ) and draw<strong>in</strong>g on Alanen’s 75 Integrated Needs‐Adapted approaches for women with psychosis. Although <strong>in</strong>itiallydeveloped for a new women’s “enhanced” service, the model had31
started to <strong>in</strong>form practice throughout the women’s service. It aimedto create a therapeutic culture <strong>in</strong>formed by awareness of the impactof early trauma with a formulation‐based holistic approach (i.e.attempt<strong>in</strong>g to understand the women’s emotional, behavioral,<strong>in</strong>terpersonal or mental health difficulties from a biological,psychological and social perspective). The approach relies heavily onrelational work between the staff team and the women. Through afocus on Mentalisation‐based treatments, the staff team aimed tohelp women to understand and manage their own mental healthdifficulties that <strong>in</strong>volved work<strong>in</strong>g with women <strong>in</strong> a process of enquirywhich acknowledged that women themselves were the experts ontheir own story and nurtur<strong>in</strong>g their capacity for change.“She is really good, sheadvises you, it’s like she gets<strong>in</strong>to your <strong>life</strong> and reads yourm<strong>in</strong>d and everyth<strong>in</strong>g shesays to me is correct. Shemakes me look at mymistakes, my illness anddifferent th<strong>in</strong>gs like that <strong>in</strong> adifferent perspective that Ididn’t see before”.Woman service userAttachment Theory provided the basis of a model of care for a secondservice albeit formulated as part of a different approach. Althoughbased with<strong>in</strong> a mixed secure service, the women’s service developedits own model of care and related policies some of which were laterexplored <strong>in</strong> relation to the men’s service. This service offered supportwith<strong>in</strong> a high dependency unit and a rehabilitation unit, both of whichneeded to be able to make use of the model of care. Here it focusedon attachment be<strong>in</strong>g understood as part of a model of recovery.F<strong>in</strong>d<strong>in</strong>g ways for women to feel <strong>safe</strong> and take positive risks was animportant part of how staff worked with women with<strong>in</strong> very clearboundaries. The service recognised that women needed to be able todevelop and ma<strong>in</strong>ta<strong>in</strong> relationships before they move forward torecovery. The model was seen as a helpful framework to refer back toand tra<strong>in</strong><strong>in</strong>g was provided for all staff. A series of study sessions totalk about the model of care as well as facilitated reflective practicehave supported staff <strong>in</strong> develop<strong>in</strong>g their understand<strong>in</strong>g andimplementation of Attachment Theory <strong>in</strong> situ. The Recovery Model isan approach that focuses on a woman’s potential for recovery and isseen as a personal journey. Its function is to “… [enable] people withmental health problems to ma<strong>in</strong>ta<strong>in</strong> or rebuild valuable and satisfy<strong>in</strong>glives with<strong>in</strong> and beyond the limits imposed by their difficulties” 76 . Thewomen’s service has a dedicated OT who works with women ondevelop<strong>in</strong>g their skills and confidence. The OT department <strong>in</strong> thismixed secure service worked with Kielhofner’s Model of HumanOccupation 77 . This model is based on three elements of volition,habituation and performance capacity and was seen to be very helpful<strong>in</strong> a secure service for holistic OT assessments and develop<strong>in</strong>gappropriate occupation.“Kielhofner looks atenvironments where someenvironments can ‘afford’people, <strong>in</strong> his language, or‘repress’ people <strong>in</strong> theiroccupational performanceand that’s really important<strong>in</strong> a secure unit.”“That’s really <strong>in</strong>terest<strong>in</strong>g aswe haven’t asked thewomen, we’ve asked thestaff what do you th<strong>in</strong>k ofthe model of care. They sayit’s different here and givepractical examples but Ith<strong>in</strong>k it’s about hav<strong>in</strong>g atherapeutic milieu.”One service worked with<strong>in</strong> a philosophy of collaboration. This was atan operational level and focused on women’s <strong>in</strong>volvement <strong>in</strong> their“There are models and theyare implemented todifferent degrees <strong>in</strong> differentparts of the service. There’s32
care. Collaboration with<strong>in</strong> the staff team where <strong>in</strong>dividuals were ableto work <strong>in</strong> a self‐reflective manner was seen to have a positive impacton how staff then worked with women. The service had undergoneconsiderable change at senior staff levels and through expansion ofthe service. With major developments, the service had <strong>in</strong>troduced amore streaml<strong>in</strong>ed structure and a commitment to staff tra<strong>in</strong><strong>in</strong>g <strong>in</strong> DBTto underp<strong>in</strong> its philosophy. As a women‐only service, albeit part of alarger organisation, there has been some flexibility <strong>in</strong> determ<strong>in</strong><strong>in</strong>g thephilosophical direction for the future. The unit provides a range ofspecialist services and has found that through mak<strong>in</strong>g appropriateassessments and placement with<strong>in</strong> a specialist ward, staff were betterable to understand and work with women’s needs <strong>in</strong> relation to, forexample, a form of mental illness or learn<strong>in</strong>g disability. This hadhelped move away from descriptions of behavior to explor<strong>in</strong>g thefactors which underp<strong>in</strong>ned it <strong>in</strong> a therapeutic environment. Atherapeutic community model had been adopted with recognitionthat events affected the whole service and thus needed to bediscussed across the community <strong>in</strong>clusive of women and staff.also an understand<strong>in</strong>g of theimpact of developmentaltrauma and there be<strong>in</strong>g aprocess for people need<strong>in</strong>gto understand their owndifficulties and hav<strong>in</strong>gtherapeutic approaches towork through them.”In another service, the team reported that a model of care whichprovided a gender sensitive approach had been developed andadopted across the women’s service although there were someoperational differences at ward level reflect<strong>in</strong>g the differ<strong>in</strong>g cl<strong>in</strong>icalneeds of the patient groups. As a start<strong>in</strong>g po<strong>in</strong>t, the service hadadopted the Commission<strong>in</strong>g Team’s Standards of Care for Women’sSecure Services, with some members of the team hav<strong>in</strong>g been<strong>in</strong>volved <strong>in</strong> the development of these regional standards. They hadalso looked at WISH (Women In Secure Hospitals) Standards andRecommendations for key attributes for a gender sensitive service,and <strong>in</strong>corporated as many of these that they could <strong>in</strong>to their model.An away day, <strong>in</strong>volv<strong>in</strong>g Commissioners, MDT members, ward staff andwomen service users, was organised to contribute to thedevelopment of their model of care. They looked at Trauma,Attachment and Recovery models and discussed how to <strong>in</strong>tegratethem <strong>in</strong>to how they work with women, and what would work best oneach ward area; with recovery pr<strong>in</strong>ciples be<strong>in</strong>g particularly importantfor some women and trauma and attachment models be<strong>in</strong>gparticularly pert<strong>in</strong>ent to meet<strong>in</strong>g the needs of others. Efforts hadbeen made not to replicate the traditional division betweenPersonality Disorder/Mental Illness wards that had been set up <strong>in</strong>other services, but <strong>in</strong>stead to focus on women’s recovery. Ratherthan see<strong>in</strong>g them <strong>in</strong> terms of diagnosis, they attempted todeconstruct what women’s cl<strong>in</strong>ical and risk needs were with<strong>in</strong> a moreholistic context, and then to <strong>in</strong>corporate gender <strong>in</strong>fluences with<strong>in</strong>their <strong>in</strong>dividual case formulations.“We presented modelsabout trauma, attachmentand recovery and had bigdiscussions about how to<strong>in</strong>tegrate those and whatwould work best on whichward area.”33
For one women’s service, there were no separate operational policiesor a written model of care but they operated on the basis of Unit orTrust‐wide policies. The philosophy of care on the women’s ward wasgender sensitive and holistic tak<strong>in</strong>g account of women’s backgroundsand <strong>life</strong> experiences. Various models and approaches had beenreviewed by the team and <strong>in</strong>fluenced their <strong>in</strong>dividual practice with thewomen, <strong>in</strong>clud<strong>in</strong>g psycho‐social approaches and the Tidal Model(http://www.tidal‐model.com), which emphasizes the importance ofthe recovery process start<strong>in</strong>g from day one or when the patient is attheir lowest ebb and is centered around them reclaim<strong>in</strong>g their ownstory as a way of ga<strong>in</strong><strong>in</strong>g understand<strong>in</strong>g of the causes of their mentaldistress and tak<strong>in</strong>g back control of their lives. But, whilst there is noapproved “model of care” document for the ward its philosophy ofcare is led and driven by the cl<strong>in</strong>ical leads who aimed to embed it <strong>in</strong>the culture of the Women’s Service and the way <strong>in</strong> which the teamthought and responded to women’s needs on a day to day basis. Itencouraged a ‘positive’ attitude toward work<strong>in</strong>g with women <strong>in</strong> asecure sett<strong>in</strong>g. The ethos was based on try<strong>in</strong>g to provide a “human”response to women’s emotional distress and putt<strong>in</strong>g the women’sneeds as paramount rather than try<strong>in</strong>g to fit the women <strong>in</strong>to aparticular set of procedures or ways of work<strong>in</strong>g.“With<strong>in</strong> this gender specificservice we have no specificmodel but what we havedone is use the pr<strong>in</strong>ciples ofpsycho‐social <strong>in</strong>terventions<strong>in</strong> agreement with thenational standards and thegender policy and assupported by NICE. Theoutcome has beentremendous! If you come<strong>in</strong>to our ward, theatmosphere is constantlynormalised, <strong>in</strong>cident levelshave gone down and youf<strong>in</strong>d there is more opennessand <strong>in</strong>teraction and the rightattitude <strong>in</strong> care. It hasultimately led to reduction<strong>in</strong> use of the Extra CareArea.”In the sixth case study area, contemporary social learn<strong>in</strong>g theoryprovided an overall framework and was argued to emphasise theimportance of comb<strong>in</strong><strong>in</strong>g ‘medical and social treatments <strong>in</strong> acomplementary manner, to mitigate the effects of any illness, and tohelp promote more adaptive attitudes, skills and behaviour’. As atreatment approach RAID (Re<strong>in</strong>force Appropriate, ImplodeDestructive) was adopted across the entire medium secure service.RAID is based on a philosophy of how to view and work with extremebehaviour argued to enable staff to <strong>in</strong>tervene positively andeffectively to m<strong>in</strong>imise its occurrence. It is not a s<strong>in</strong>gle approach butbased <strong>in</strong> many <strong>in</strong>clud<strong>in</strong>g behavioural theory. There is one tra<strong>in</strong><strong>in</strong>gprovider <strong>in</strong> the UK (http://www.apt.ac/raid.html). Staff were alltra<strong>in</strong>ed to encourage positive behaviour, to record ‘green’ behaviours,acknowledg<strong>in</strong>g a woman’s progress as well as ‘red’ or negativebehaviour. In addition and although this service made use ofstandardised care plann<strong>in</strong>g and documentation, for example, it wasalso clear about work<strong>in</strong>g with<strong>in</strong> a gender specific model of care. Thus,the RAID approach also took <strong>in</strong>to account women’s backgrounds,types of exploitation and subsequent vulnerability, child care issuesand exploration of women’s roles as daughters, mothers, partners andhow these roles impact on their quality of <strong>life</strong>. Staff were risk awareand work<strong>in</strong>g to make sure women received appropriate levels of“We are try<strong>in</strong>g to givepositive feedback but also tomake clear what is notacceptable behaviour. Forexample, if a woman putsher feet on the table,challenge this <strong>in</strong> a gentleway and not just shout ‘getyour feet off the table!’.Suggest to her this isn’t thedone th<strong>in</strong>g and give her anopportunity to respondappropriately without itbecom<strong>in</strong>g an issue.”34
monitor<strong>in</strong>g and support. Good relationships were seen as one meansof mak<strong>in</strong>g sure staff were aware if someth<strong>in</strong>g was wrong and thusrecognise that someth<strong>in</strong>g needed to be done.The philosophies described above were usually articulated by those <strong>in</strong>senior cl<strong>in</strong>ical positions with<strong>in</strong> the case study areas: consultantpsychiatrists, heads of psychology and senior nurs<strong>in</strong>g staff <strong>in</strong>clud<strong>in</strong>g wardmanagers. In one area, however, and on the basis of an audit, the serviceidentified that staff were keen to work with a model but needed tra<strong>in</strong><strong>in</strong>gto help them understand the complexity of theory and its use <strong>in</strong> practice.In a number of areas, it was not always clear what had led to adopt<strong>in</strong>g aparticular approach although contributory factors were said to <strong>in</strong>clude:• Senior staff with experience of a specific model would often <strong>in</strong>fluenceservice development and thus the choice of model• Time provided for new service development to explore differentapproaches and their potential use• Evidence‐base for an approach used successfully with women withcomplex needs• Exist<strong>in</strong>g services review<strong>in</strong>g philosophy and policy <strong>in</strong> the context ofbidd<strong>in</strong>g for new services, e.g. the WEMSS• Exist<strong>in</strong>g organizational approaches that the service was required toadopt, e.g. where it was part of a large structure that already had amodel of care <strong>in</strong> place.In some cases, staff referred to develop<strong>in</strong>g the model through theirpractice. In one area, work<strong>in</strong>g with attachment theory become importantonce women had arrived <strong>in</strong>to the new service. It was clear that work<strong>in</strong>gtowards recovery was essential but that women needed to be able towork on relationship build<strong>in</strong>g <strong>in</strong> order to work on recovery.Dur<strong>in</strong>g the course of the evaluation, many staff and most women<strong>in</strong>terviewed found it difficult to articulate that a specific model orphilosophy of care had been adopted <strong>in</strong> their service. However, theyfrequently referred to tak<strong>in</strong>g a positive attitude and the importance ofshared values, shared approaches and shared goals but these were notnecessarily connected to a theoretical approach.In one case study service, concern was expressed by some professionalsthat if staff responded to women’s emotional distress by simply tell<strong>in</strong>gthem to th<strong>in</strong>k positively this could be extremely <strong>in</strong>validat<strong>in</strong>g. Here it wasalso reported that on occasion there was a reluctance by some workers toproperly acknowledge that a woman’s emotional distress had led todangerous behaviours <strong>in</strong> the past yet it was essential that this connectionwas understood and addressed as part of the woman’s recovery process.“We’ve had lots of newlyqualified staff nurses andthey’ve really embraced theconcept of work<strong>in</strong>g with<strong>in</strong> aframework.”“Before, we would gostraight to the recoverymodel but we had to startall over aga<strong>in</strong> and th<strong>in</strong>kabout attachment, aboutwhy women behave <strong>in</strong> suchways and how that can bel<strong>in</strong>ked to how they developrelationships and enabl<strong>in</strong>gwomen to trust us, workwith us and feel <strong>safe</strong> <strong>in</strong> theenvironment.”“We have various modelsdepend<strong>in</strong>g on the ward theyare on. The ma<strong>in</strong> th<strong>in</strong>g isvalidat<strong>in</strong>g their difficulties,their issues and work<strong>in</strong>g onhow we can make their livesbetter or chang<strong>in</strong>g theirbehaviour so they canfunction better on their ownor outside or <strong>in</strong> a less secureenvironment.”35
The term<strong>in</strong>ology differed but what emerged as important <strong>in</strong> all serviceswas ensur<strong>in</strong>g that senior members of staff had or were plann<strong>in</strong>g to put <strong>in</strong>place a clear framework that allowed staff and women to operateeffectively. The framework provided an overview of the direction of theservice with<strong>in</strong> which operational policies could be developed andimplemented. A coherent and thought‐through model or philosophy ofcare was essential and where this was not the case, staff and womendescribed more tension, confusion and a higher number of difficult<strong>in</strong>cidents. Staff were also less likely to receive regular support andsupervision.3.3 Implementation of policies to facilitate a route throughIn the <strong>in</strong>itial survey and f<strong>in</strong>al follow‐up of services, we asked about therange of policies <strong>in</strong> place. Dedicated women’s services were often leftjuggl<strong>in</strong>g demands <strong>in</strong> terms of the range and content of policies to put <strong>in</strong>place. On the one hand, there was agreement that policies needed toreflect the purpose and philosophy of the service as laid out <strong>in</strong>Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women’s Mental <strong>Health</strong> ImplementationGuidance. On the other hand, some services were constra<strong>in</strong>ed by therequirements of their ‘parent’ organization.In some case study areas, the Women’s Service had developed a full policyfor its new service which covered all aspects of practice. The follow<strong>in</strong>gtable illustrates the range of policies and the extent to which they are <strong>in</strong>place with<strong>in</strong> <strong>in</strong>dividual services. Those which have developed or beenredesigned recently were more likely to have all of these either as<strong>in</strong>dividual or as part of an overarch<strong>in</strong>g service operational policy.Table 5: Policies <strong>in</strong> place 2006 (n=13, 1=not known)Policy In place Not <strong>in</strong> placeManagement of12 1aggression/distressChild visit<strong>in</strong>g 12 1Management of self10 3harmEqualities and diversity 10 3Sexuality andrelationshipsAnti‐bully<strong>in</strong>g orharassmentImplementation ofRelational Security9 48 56 7The follow<strong>in</strong>g is an exampleof a service policy whichnotes its ‘ethos is committedto examples of goodpractice emanat<strong>in</strong>g fromresearch <strong>in</strong>to theexperiences and needs ofwomen service users <strong>in</strong>secure sett<strong>in</strong>gs. These placeparticular emphasis on theneed to provide physicalenvironments, activities andprofessional services <strong>in</strong> amanner that is gendersensitiveand the need totake particular account ofthe fact that many womenservice users will have hadpast experiences <strong>in</strong>volv<strong>in</strong>gabuse or other trauma. Ofparticular consideration are:• National ServiceFramework for Mental<strong>Health</strong> 1999• The standards of carefor women (MDTWork<strong>in</strong>g Group forWomen Service Users <strong>in</strong>Forensic Psychiatry,1999, 2002)• Philosophy of care(WISH 1999)• Equality and DiversityPolicy• Women’s Mental<strong>Health</strong>: Into thema<strong>in</strong>stream (DOH,36
Few additional policies were identified apart form one service which had a‘male staff work<strong>in</strong>g with women’ policy. However, some services notedthat they were <strong>in</strong> the process of develop<strong>in</strong>g gender specific policies <strong>in</strong>particular.At the outset of the evaluation, less than half of services respond<strong>in</strong>g to thesurvey had a policy on Relational Security although one noted thatrelational security was ‘understood and reflected <strong>in</strong> the ward’s staff<strong>in</strong>gprofile’. Where there was a policy <strong>in</strong> place, two services commented onthe importance of this to the way <strong>in</strong> which they were able to work withwomen. Where services were women only (or on sites with men but nomix<strong>in</strong>g between them), the development of women‐specific policies wasconsidered most relevant. Interest<strong>in</strong>gly, one service said all its policieswere under review as none were gender‐specific. This seemed to be acommon situation and few services said they had all seven of theidentified policies <strong>in</strong> place. Policies which are likely to be at the heart ofwomen’s secure services tended to be least likely to be <strong>in</strong> place – sexualityand relationships as well as relational security. Those without frequentlynoted that these policies were <strong>in</strong> draft or <strong>in</strong> discussion with<strong>in</strong> their service.2001)• Ma<strong>in</strong>stream<strong>in</strong>g Genderand Women’s Mental<strong>Health</strong> (DOH, 2003)• Women at Risk 2006• Support<strong>in</strong>g Women <strong>in</strong>tothe Ma<strong>in</strong>stream 2006• Tackl<strong>in</strong>g the <strong>Health</strong>Effects of DomesticViolence and Abuse2006• ‘Secure Futures.’S<strong>in</strong>ce then, and over a period of two years, most women’s medium secureservices now have these and other relevant policies. Indeed, there hasbeen considerable change over time which has been <strong>in</strong>fluenced by anumber of key factors:• the implementation process of Ma<strong>in</strong>stream<strong>in</strong>g Gender which hasrequired considerable time to turn the guidance <strong>in</strong>to reality• the publication of Best Practice Guidance: Specification for AdultMedium Secure Services (DH 2007)• the publication of Implementation Criteria for RecommendedSpecification: Adult Medium Secure Units (Quality <strong>Network</strong> forForensic Mental <strong>Health</strong> 2008)Whilst not all services are members of the Forensic Quality <strong>Network</strong>, thepublication of standards which emphasise relational security has had animpact. In addition, the Implementation Criteria conta<strong>in</strong>s a substantialsection on women’s services.Providers had different views of what policies best represented the effortsof their women’s secure service. Ensur<strong>in</strong>g local development of policies forwomen’s services based on consultation with women themselves hadbeen very useful.The questionnaires suggested that there are clear reasons for the extentto which services have appropriate policies <strong>in</strong> place. Services described thefactors which enabled implementation as well as those that h<strong>in</strong>dered it.Three key factors which helped were frequently identified across theservices <strong>in</strong>clud<strong>in</strong>g the importance of strong leadership, ensur<strong>in</strong>g staff37
awareness of policies and the <strong>in</strong>volvement of staff <strong>in</strong> local policydevelopment. Implementation was further supported by hav<strong>in</strong>g thefollow<strong>in</strong>g <strong>in</strong> place:• Experienced staff teams• Consistency of approach (by multi‐discipl<strong>in</strong>ary and nurs<strong>in</strong>g teams)• Regular review of policies and procedures• Resources for implementationFactors which h<strong>in</strong>dered implementation were most usually where theabove were not <strong>in</strong> place. However, services noted other issues whichacted as barriers <strong>in</strong> their sett<strong>in</strong>gs. These <strong>in</strong>cluded:• Lack of appropriate staff; use of bank/agency staff and high levels ofnew and <strong>in</strong>experienced staff• Lack of time for staff to read and absorb policies• Individual staff who lack awareness of the issues <strong>in</strong> relation towomen’s mental health• Lack of understand<strong>in</strong>g <strong>in</strong> large mixed MSUsWomen <strong>in</strong>terviewed also suggested that even if they did not want thedetail of policies, they experienced their impact and sometimes saw themas ‘the rules’. They too wanted consistency and consultation. In one casestudy area, women described how policies changed depend<strong>in</strong>g on whichstaff were on duty. An example they gave was about smok<strong>in</strong>g and gardenaccess once their build<strong>in</strong>g became no‐smok<strong>in</strong>g, some staff allowedcont<strong>in</strong>uous access and others who did not despite agreements at thecommunity meet<strong>in</strong>g and a service policy.Concerns raised by services were consistent and it was clearly a resourc<strong>in</strong>gas well as staff retention issue for many. This was also raised <strong>in</strong> relation totra<strong>in</strong><strong>in</strong>g (see section 7) where levels of gender specific tra<strong>in</strong><strong>in</strong>g appearedlow often as result of staff turnover.3.4 The importance of s<strong>in</strong>gle sex policy and provisionLocated at the centre of the DH Women’s Mental <strong>Health</strong> policy was theimportance of offer<strong>in</strong>g women <strong>safe</strong> places to work towards their recovery.This required that women, for whom it was appropriate, had access todedicated women‐only services that would meet their needs. Theevaluation f<strong>in</strong>d<strong>in</strong>gs suggested that there was broad agreement about theimportance of s<strong>in</strong>gle sex policy and provision but the form this tookdiffered as did women’s and staff attitudes towards them. However, itwas not always clear that the concept of differentiated care wasunderstood as more than s<strong>in</strong>gle sex provision.In one case study area, it was reported that when s<strong>in</strong>gle sex provision was“They are not <strong>in</strong> a separateservice! They live on samegender wards and that ishow we perceive it. Isuppose my philosophy isthat we don’t have awomen’s service and amen’s service we have aforensic service for men andwomen and we havepathways for men and forwomen and we certa<strong>in</strong>ly <strong>in</strong>our service try to have staffwork<strong>in</strong>g solely with men orsolely with women because Ith<strong>in</strong>k there are more th<strong>in</strong>gsthat are common than thereare differences.”“Be<strong>in</strong>g on a women onlyward is very much different,it is more settled and it’smore pleasant, it really ismore pleasant. The girls geton really well we all helpeach other <strong>in</strong> various waysfrom do<strong>in</strong>g each other’slaundry to mak<strong>in</strong>g brews foreach other.”Woman service user“You need <strong>in</strong>teraction withmen. Some people havefears of be<strong>in</strong>g around menanyway and the way ofgett<strong>in</strong>g over those fears is tohave male workers, be<strong>in</strong>gable to ga<strong>in</strong> trust <strong>in</strong> malesupporter.”Woman service user“In some ways I don’t wantunescorted ground leave butI know some womenwouldn’t m<strong>in</strong>d. I don’t38
first <strong>in</strong>troduced at the unit, it was on the basis of promot<strong>in</strong>g women’s<strong>safe</strong>ty and awareness of their vulnerability with<strong>in</strong> mixed‐sex wards.However, over the years and as the women’s service developed, it becameclearer to the cl<strong>in</strong>ical team that women’s needs were different and, as am<strong>in</strong>ority group with<strong>in</strong> forensic services, their needs could not bespecifically targeted when they were cared for alongside men. Whilsts<strong>in</strong>gle sex provision was still seen as a pre‐requisite for women’s <strong>safe</strong>ty, itwas also recognized as essential <strong>in</strong> order to provide appropriate genderspecific care.At another service, all the women <strong>in</strong>terviewed said they preferred be<strong>in</strong>gon a women‐only ward, stat<strong>in</strong>g it felt <strong>safe</strong>r. Two of the women though saidthat whilst they liked be<strong>in</strong>g on a women only ward, they did like to havethe opportunity to mix with men <strong>in</strong> off‐ward areas and dur<strong>in</strong>g someactivities. Two women spoke about previously be<strong>in</strong>g cared for on mixedsexwards. One reported she had felt threatened by the presence of malepatients and their behaviour on the ward, say<strong>in</strong>g she would not feel <strong>safe</strong> ifmale patients had access to sleep<strong>in</strong>g or liv<strong>in</strong>g areas on her current ward.The other also said she had felt <strong>in</strong>timidated when on a mixed sex ward.Women’s attitudes were sometimes determ<strong>in</strong>ed by their own experiencesof abuse and relationship to men <strong>in</strong> other circumstances. However, morebroadly, many women said they were not concerned by limited contact,e.g. through service‐user groups, but they would not seek out to gobeyond an occasional hello <strong>in</strong> a corridor to men from the men’s service. Inone service, return<strong>in</strong>g from community leave was identified as a potentialproblem as women had to walk through the grounds to get to their unit.They were issued with mobile phones to call the unit for an escortalthough they had not been allowed phones hitherto.In mixed‐sex services which <strong>in</strong>cluded a women‐only unit, staff identified anumber of issues which, <strong>in</strong> their view, made it more difficult to deliver aneffective service. These <strong>in</strong>cluded:• Lack of critical mass: two case study areas provided one ward each of12 women <strong>in</strong> large mixed units. This had led to be<strong>in</strong>g forced to takewomen with a range of needs and diagnoses who might not be treatedtogether if placed <strong>in</strong> a larger women‐only unit.• Service scepticism: whilst chang<strong>in</strong>g with time, services with a higherproportion of men tended not to recognize that some women, giventheir histories of abuse, needed to be provided for <strong>in</strong> women‐onlyservices which took a gendered approach to the provision of care.• Disproportionate resource allocation: <strong>in</strong> addition to hold<strong>in</strong>g differentattitudes which could be very blam<strong>in</strong>g of women, men’s units <strong>in</strong> mixedservices were reported as hav<strong>in</strong>g access to fewer resources which hadled to criticisms of dedicated services for womenparticularly want to behang<strong>in</strong>g around the groundswith dodgy men, you know.”Woman service user“Some disagree with myformulation but I reallywonder if there isn’t afem<strong>in</strong>ist backlash of ‘what’sso special about women?’and there’s a huge amountof envy to do with all thatwomen get. I like the factthat women have exposureto males and there isn’t thisth<strong>in</strong>g that they can’ttolerate a male and I th<strong>in</strong>kwe can risk manage butthere’s a total bl<strong>in</strong>d spotabout the type of male theyhave exposure to is allpeople that you or Iwouldn’t like to meet on adark night, thank you verymuch!”“I th<strong>in</strong>k we can provide a<strong>safe</strong> environment and I don’tth<strong>in</strong>k you can do that on amixed ward because thewomen are vulnerable, theyare <strong>in</strong> a m<strong>in</strong>ority. You cantarget sexual abuse issueswithout the woman hav<strong>in</strong>gto leave the room ratherthan be sat <strong>in</strong> a room withsomeone who has been anabuser. So it’s not just aboutkeep<strong>in</strong>g women <strong>safe</strong> it’s alsoabout be<strong>in</strong>g able to targettheir specific needs and thefact that their needs aredifferent from men.”At the same time, there was recognition that women’s services had the39
advantage of dedicated and highly visible staff teams that women sawfrequently <strong>in</strong> the sitt<strong>in</strong>g room and other areas of the unit, as one person<strong>in</strong>terviewed said:“I was talk<strong>in</strong>g to an OT about th<strong>in</strong>gs for women. We’ve tried to talk about hav<strong>in</strong>ga male‐specific service agenda start<strong>in</strong>g to <strong>in</strong>troduce the idea that that there arespecific areas to th<strong>in</strong>k about. (In the women’s service) we’ve got a record ofbirthdays and anniversaries. The OT was say<strong>in</strong>g the male service was different, forexample, they don’t even know which of the men are fathers.”While services were <strong>in</strong> agreement that women‐only was more appropriatewith male staff to provide positive role models, it was not always easy tof<strong>in</strong>d male nurses who wanted to work with women. Most services hadagreements that male staff did not go to women’s bedrooms or onto acorridor where there are bedrooms; they did not give <strong>in</strong>jections orsanitary products and <strong>in</strong> some cases, did not do night‐time observations.Some men were concerned that women might accuse them of forms ofsexual abuse. Interest<strong>in</strong>gly <strong>in</strong> this study, few of the male staff <strong>in</strong>terviewedhad wanted to work <strong>in</strong> a dedicated women’s service. Their choices weremore usually <strong>in</strong>formed by location and position. (See also section 7 onwork<strong>in</strong>g <strong>in</strong> a women’s service.)• Women and professionals <strong>in</strong>volved <strong>in</strong> their care were clear, regardless of term<strong>in</strong>ology, about theimportance of key factors and <strong>in</strong> particular relational security which underp<strong>in</strong>ned what services shouldwork towards. However, the survey showed that policies about relational security were only <strong>in</strong> place <strong>in</strong>half of services.• Essential to service provision was the development of a coherent and thought‐through model orphilosophy of care. Where this was not the case, staff and women described more tension, confusionand a higher number of difficult <strong>in</strong>cidents. Staff were also less likely to receive regular support andsupervision.• The case study services demonstrated the difficulty at times of turn<strong>in</strong>g philosophy and policy <strong>in</strong>to everyday practice for a variety of reasons. However, core to this process was an understand<strong>in</strong>g that work<strong>in</strong>g<strong>in</strong> the service and be<strong>in</strong>g able to reflect on theory needed to be <strong>in</strong>tegrated.• Some women’s services were constra<strong>in</strong>ed by their location as a relatively small part of mixed provision.• Policy implementation was h<strong>in</strong>dered by lack of staff; time; awareness and, <strong>in</strong> larger mixed mediumsecure services, understand<strong>in</strong>g.74 Bateman,A. & Fonagy,P. (2004) Psychotherapy for Borderl<strong>in</strong>e Personality Disorder: mentalisation‐based treatment OxfordUniversity Press75 Alanen, Y.O. (1997) Schizophrenia: Its Orig<strong>in</strong>s and Need‐Adapted Treatment Karnac Books76 Repper,J. and Perk<strong>in</strong>s,R. (2003) Social Inclusion and Recovery: A model for mental health practice Elsevier Ltd77 Kielhofner,G. et al (2008) Model of Human Occupation: Theory an Application Lipp<strong>in</strong>cott Williams and Wilk<strong>in</strong>s40
4. In whose <strong>hands</strong>: how are women <strong>safe</strong> and secure?The consultants hold our lives <strong>in</strong> their <strong>hands</strong> so whatever they say goes – the top dog. They make thedecision about whether we’re ready for discharge. I tell m<strong>in</strong>e everyth<strong>in</strong>g about past, present, future.Woman service userAt my last (mixed) hospital, they didn’t protect me from sex offenders and I got sexually abused. They said Iwas psychotic and <strong>in</strong>jected me. Here the doctor said I was hypersensitive emotionally and shouldn’t havebeen treated that way. The doctors here are a solid block for me. They nurture me and make me feelconfident to walk on my own and to explore myself. They give me wisdom about my illness and help mebecome sturdy with expla<strong>in</strong><strong>in</strong>g the way I am. They really care which is very unusual.Woman service userThe philosophies of care and policies described <strong>in</strong> section 3 were underp<strong>in</strong>ned by consideration of how toma<strong>in</strong>ta<strong>in</strong> women’s <strong>safe</strong>ty. This has been def<strong>in</strong>ed as physical, procedural and relational, each of which <strong>in</strong>practice carries def<strong>in</strong>itions dependent on levels of understand<strong>in</strong>g and diversity of context. The evaluationexam<strong>in</strong>ed the range of <strong>in</strong>terpretations of <strong>safe</strong>ty and security from the perspectives of women service usersthrough to commissioners of services <strong>in</strong> order to make sense of whose <strong>safe</strong>ty and what security were be<strong>in</strong>greferred to. This section explores more specifically how far and <strong>in</strong> what ways the essential concept ofrelational security and practice has been adopted by women’s secure services.4.1 Def<strong>in</strong>itions of securityThose <strong>in</strong>volved <strong>in</strong> the provision of services for women were asked abouttheir understand<strong>in</strong>g of the concept of relational security and the ways <strong>in</strong>which they believed the concept was or was not core to service delivery.Women patients were also asked if this was mean<strong>in</strong>gful to them and ifso, how did they see its role <strong>in</strong> service provision. Standard def<strong>in</strong>itions ofsecurity <strong>in</strong> use covered the follow<strong>in</strong>g:Physical securityPhysical security referred to the design and ma<strong>in</strong>tenance of build<strong>in</strong>gs,fitt<strong>in</strong>gs and the site of the unit <strong>in</strong>clud<strong>in</strong>g, for example, the height of theperimeter fence, gate entry and key management of the service. The 49standards for medium secure services were applied across s<strong>in</strong>gle andmixed‐sex services.Procedural securityProcedural security referred to the policies developed and proceduresimplemented to ensure the smooth‐runn<strong>in</strong>g of the service rang<strong>in</strong>g fromthe use of seclusion, observation procedures through to the control ofmail and use of telephones for example.“People <strong>in</strong>itially th<strong>in</strong>k it’sjust about quantity of staffand it is partly aboutquantity of staff but I th<strong>in</strong>kcrucially it’s about quality ofstaff and the quality of therelationships that they canhave with patients. It’sabout us<strong>in</strong>g thoserelationships as a way ofmanag<strong>in</strong>g and ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>gbehaviours and that iswithout hav<strong>in</strong>g to resort toother strategies orstructures or observations orwhatever, so for me it’sreally about the quality andthe k<strong>in</strong>d of skills the personhas <strong>in</strong> terms of theunderstand<strong>in</strong>g they have.The women’s service verymuch focuses on reflectivepractice th<strong>in</strong>k<strong>in</strong>g aboutwhat we do.”41
Relational securityRelational security lies at the heart of the National Women’s Mental<strong>Health</strong> (MH) Strategy (DH 2002) and the Implementation Guidance (DH2003) for gender‐specific services address<strong>in</strong>g the specific mental healthneeds of women (e.g. with histories of abuse and/or self‐harm).Relational security has been embedded <strong>in</strong> the standards for all mediumsecure services. In the context of women’s services. It encapsulates theimportance of high staff‐to‐patient ratios, the amount of time spent <strong>in</strong>face‐to‐face contact with women and a balance between <strong>in</strong>trusivenessand openness; work<strong>in</strong>g towards high levels of trust between patientsand professionals. ‘Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women’s Mental <strong>Health</strong>’states that structures for the provision of secure <strong>in</strong>patient servicesrequire a range of provision:“<strong>My</strong> role as a nurse is toma<strong>in</strong>ta<strong>in</strong> the security of thepatient, to develop trust<strong>in</strong>gand work<strong>in</strong>g relationshipswith them, help them formgood friendships, goodrelations with staff andensure that the patient cantrust the staff.”“to create an <strong>in</strong>tegrated system of secure <strong>in</strong>patient care for women.Women’s needs for security are predom<strong>in</strong>antly for relational andprocedural security and therefore mak<strong>in</strong>g the dist<strong>in</strong>ction betweenexist<strong>in</strong>g (physical) medium and low secure care, is probablyunnecessary.”There was some variation across the case study areas, staff groups andamong women themselves. For example, <strong>in</strong> one area, all staff<strong>in</strong>terviewed provided a def<strong>in</strong>ition of relational security even though theyidentified some concerns about how it happened <strong>in</strong> practice. In anotherarea, staff <strong>in</strong>terviewed had no clear ideas about relational security.However, some here described their practice <strong>in</strong> ways consistent with theconcept.4.2 The experience of security: what did women say?It was rare that any of the women we met used the language associatedwith security as described above. However, many did describe factorswhich broadly fit with<strong>in</strong> the concept of relational security and believedthat this ‘different’ way of work<strong>in</strong>g had helped them to stay <strong>safe</strong><strong>in</strong>clud<strong>in</strong>g:• be<strong>in</strong>g able to talk to staff who they knew well and trusted. Onewoman spoke about the atmosphere on her unit, and the fact it wasaccept<strong>in</strong>g of all women whether well or very unwell – the staff“accept you as you are”.• be<strong>in</strong>g on a women‐only ward had been very important to many <strong>in</strong>keep<strong>in</strong>g them <strong>safe</strong>, although as one women noted, s<strong>in</strong>ce she hasbeen more settled and transferred to the mixed‐sex pre‐dischargeward, be<strong>in</strong>g on a mixed ward has worked well for her.• be<strong>in</strong>g able to address specific issues <strong>in</strong> a <strong>safe</strong> way. One woman whohas a history of self harm<strong>in</strong>g said she had completed a course withthe Cl<strong>in</strong>ical Nurse Specialist for self harm and it had benefited her,“I feel <strong>safe</strong>, I used to selfharm a lot and sometimes Ididn’t feel <strong>safe</strong> but I haven’tself harmed s<strong>in</strong>ce aboutSeptember/October lastyear…..I used to use icecubes and elastic bands,they taught me how to usethe ice cubes and elasticbands <strong>in</strong>stead of burn<strong>in</strong>gmyself or cutt<strong>in</strong>g and thatreally worked for me. Justbe<strong>in</strong>g able to turn to thestaff you know if you get theurge they will talk it throughwith you, you don’t feel asthough you are on yourown, just until that phasehas f<strong>in</strong>ished.”Woman service user42
particularly the focus on relapse prevention. After complet<strong>in</strong>g thecourse she had had a review with the psychologist who hadsummarized the most important po<strong>in</strong>ts for her <strong>in</strong>to one leaflet,which she felt would help to her keep herself <strong>safe</strong> <strong>in</strong> the future.• be<strong>in</strong>g able to just be with staff was important to some women whoappreciated that higher staff ratios meant there were opportunitiesfor staff to be on the unit. One woman described the importance ofstaff who could sit with her, observ<strong>in</strong>g her <strong>in</strong> a more relaxed way andthat she felt able to talk or not while reassured by their presence.• be<strong>in</strong>g able to form and susta<strong>in</strong> good peer relationships with otherwomen played a significant part <strong>in</strong> how <strong>safe</strong> they felt. One womandescribed how her friends ‘shopped’ her, tell<strong>in</strong>g staff that she was atrisk by vomit<strong>in</strong>g her medication. Staff encouraged her peers to<strong>in</strong>tervene <strong>in</strong> the first <strong>in</strong>stance while they provided back‐up whichproved not to be necessary. She said she appreciated that her friendshad ‘cared’.Most of the women who were <strong>in</strong>terviewed said they felt the level ofprocedures and restrictions <strong>in</strong> place was appropriate, recogniz<strong>in</strong>g theywere there to keep them <strong>safe</strong>, and they said these had been expla<strong>in</strong>edadequately. Women held this view about levels of physical security aswell and said they understood the need for this even though it wasoverly restrictive <strong>in</strong> some <strong>in</strong>stances and confus<strong>in</strong>g <strong>in</strong> others.“<strong>My</strong> belief is that there aremany women who have hadyears and years and years of<strong>in</strong>dividual psychology andyou know what? They havenot processed any of itbecause they have neverbeen <strong>safe</strong> and I don’t believethat when people feelun<strong>safe</strong> they are able to work<strong>in</strong> –depth at all. What we tryand achieve is <strong>safe</strong>ty firstwith an emphasis early on <strong>in</strong>the psycho‐social treatmentprogramme on build<strong>in</strong>gskills be that aroundmanag<strong>in</strong>g anxiety or deal<strong>in</strong>gwith feel<strong>in</strong>gs or<strong>in</strong>terpersonal relationships.”One woman felt however there were too many restrictions and rules,and that they were just told what they could or could not do without anyexplanation as to why. An example of this was where women weresometimes told they could only go outside to smoke at certa<strong>in</strong> times andsometimes there were no restrictions to when they went.There were <strong>in</strong>stances <strong>in</strong> which women described experiences where theyhad not felt sufficiently <strong>safe</strong> <strong>in</strong> the service <strong>in</strong>clud<strong>in</strong>g:• a very few women who talked about bully<strong>in</strong>g and how it was dealtwith• new women arriv<strong>in</strong>g at the ward or unit• high staff turnover result<strong>in</strong>g <strong>in</strong> women feel<strong>in</strong>g less able to f<strong>in</strong>dsomeone they knew and trusted to talk to.4.3 What did staff say about security?Key staff <strong>in</strong> senior positions were more likely to provide a def<strong>in</strong>ition oftypes of security and their place with<strong>in</strong> their sett<strong>in</strong>g. In one case studyarea, the term relational security had not been adopted but the conceptsand practices had been as part of their philosophy of care. Staff<strong>in</strong>terviewed said they were not familiar with the term but outl<strong>in</strong>ed amodel and practice premised on understand<strong>in</strong>g that women needed to“There is some very positivepractice but I th<strong>in</strong>k staff arenot always consistent andthis doesn’t promoterelational security whenstaff don’t all ma<strong>in</strong>ta<strong>in</strong> the43
feel <strong>safe</strong> <strong>in</strong> the service and <strong>in</strong> relationships <strong>in</strong> order to work on their ownrecovery.Case example:Operational polices for the women’s wards <strong>in</strong> one case study area<strong>in</strong>cluded the implementation of relational security and stressed itsimportance with<strong>in</strong> the women’s service <strong>in</strong> achiev<strong>in</strong>g <strong>safe</strong>ty throughestablish<strong>in</strong>g “good rapport and an effective therapeutic alliance betweenpatient and staff”. Written policies also emphasized the importance ofstaff hav<strong>in</strong>g thorough knowledge of their service user’s <strong>in</strong>dividual case,enabl<strong>in</strong>g them to detect and act on changes <strong>in</strong> mental state promptly,and policies recognized the importance of staff awareness of their ownresponses to service user distress or anger, aim<strong>in</strong>g to establish a cultureof reflective practice.There was also unit‐wide guidance available on relational security whichemphasized the importance of ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g professional boundarieswhilst also develop<strong>in</strong>g close work<strong>in</strong>g relationships with service users andprovid<strong>in</strong>g empathy.The model of care be<strong>in</strong>g developed with<strong>in</strong> the women’s service based onAttachment Theory provided awareness of issues like re‐enactment oftrauma, the importance of <strong>in</strong>terpersonal relationships, and the effects ofdysfunctional attachment that may be experienced by women withhistories of abuse.Interviews with staff from the various discipl<strong>in</strong>es <strong>in</strong>dicated that therewas good awareness of the particular importance of relational securitywhen work<strong>in</strong>g with<strong>in</strong> the women’s service, with all staff be<strong>in</strong>g able togive descriptions of what the term relational security meant to them.The ma<strong>in</strong> problem identified by some staff, <strong>in</strong> terms of theimplementation of relational security on the women’s wards, was that of<strong>in</strong>consistency <strong>in</strong> the way some staff applied procedures and <strong>in</strong>dividualcare plans.One member of the multi‐discipl<strong>in</strong>ary team emphasized the importanceof understand<strong>in</strong>g the offence and to not deny that the women theservice works with have often committed very serious offences. He feltthat sometimes women’s violent actions were only expla<strong>in</strong>ed (andperhaps excused) by the context of them surviv<strong>in</strong>g abuse, although itwas also the case that many of the men service users at the unit werealso survivors of childhood abuse although this was not used to try andexpla<strong>in</strong> or excuse their violent offences <strong>in</strong> the same way.The women service users who met the evaluation team all reported theygenerally felt <strong>safe</strong> on the unit. One woman reported that although shefelt <strong>safe</strong>r on a women‐only ward, she found disruptive behavior by someof the other women and the consequent staff <strong>in</strong>terventions (i.e. use ofrestra<strong>in</strong>t) upsett<strong>in</strong>g. Another woman reported she had been attacked byanother patient on a couple of occasions although the ward staff haddealt with those <strong>in</strong>cidents promptly and appropriately. One woman saidsame rules or work to thesame policies andprocedures.”“It’s easy to have a go atnurses – we’ve got somebrilliant ones. On thewomen’s service it’s reallyimportant that they’repeople who do have skills <strong>in</strong>relationship build<strong>in</strong>g andhave a degree of<strong>in</strong>telligence. When it’s notthere it’s stark. Patientspo<strong>in</strong>t it out and say ‘I don’twant that person on shift,don’t ask me to go and tellsomeone what my problemsare when they’re notsomeone I can trust andthey don’t listen to me’.That’s the biggest issue forme.”“I th<strong>in</strong>k relational security ishighly important becauseaga<strong>in</strong> look<strong>in</strong>g at thehistories of the women thatwe tend to have here youare go<strong>in</strong>g to have problems<strong>in</strong> terms of <strong>in</strong>terpersonalrelat<strong>in</strong>g, a lot of reenact<strong>in</strong>gand a lot of early childhoodabuse and I supposedysfunctional attachmentsand I th<strong>in</strong>k its importantthat staff are tra<strong>in</strong>ed <strong>in</strong>recognis<strong>in</strong>g those and arealso supported and havesupervision around that.”“Numbers of staff is anissue and patients willalways say they want morestaff. Nurses will always saythey want more staff. <strong>My</strong>experience is it’s the<strong>in</strong>verted U curve where youget to a certa<strong>in</strong> staff topatient ratio and then staffregardless of discipl<strong>in</strong>e start44
she felt that when the ward was short staffed it did not feel quite so<strong>safe</strong>.One of the women who used to self harm frequently when she first came<strong>in</strong>to the unit expla<strong>in</strong>ed how support from her care team and help withdevelop<strong>in</strong>g appropriate cop<strong>in</strong>g strategies had enabled her to stop anyself harm<strong>in</strong>g for over six months now and that due to this help she nowfelt <strong>safe</strong>r.congregat<strong>in</strong>g and talk<strong>in</strong>g tothemselves. There are timeswhen they need morepeople but I would rathersee more OTs and technical<strong>in</strong>structors who can takepeople out and doactivities.”Key features which enabled relational security to be embedded <strong>in</strong> serviceprovision <strong>in</strong>cluded:• High levels of staff retention• Provision of regular support and supervision for staff on the wards• Provision of unit‐wide guidance which emphasised the importance ofma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g professional boundaries while develop<strong>in</strong>g close work<strong>in</strong>grelationships with women• Involv<strong>in</strong>g ward staff <strong>in</strong> cl<strong>in</strong>ical <strong>in</strong>terventions• Zonal observations which allowed staff to spend time with womenand pick up early signs of risk behaviours or changes <strong>in</strong> a woman’smental state• Provision of risk assessment and care plann<strong>in</strong>g which supportedwomen to develop <strong>safe</strong> and appropriate relationships• Ensur<strong>in</strong>g local level discussions <strong>in</strong> teams• Support for the development of positive peer relationships amongwomenHowever, there were factors which were seen to h<strong>in</strong>der the process:• The concept and language of relational security was not alwaysmean<strong>in</strong>gful.• There were some concerns about the practical implications ofrelational security which <strong>in</strong>cluded low staff<strong>in</strong>g levels and fewopportunities for support<strong>in</strong>g staff <strong>in</strong> how they worked with women.• Physical and procedural security were seen to obscure theimportance of relational security, for example, where some questionthe need for perimeter fences at all, others were frustrated at hav<strong>in</strong>gto comply with generic standards of physical security deemedunnecessary <strong>in</strong> women’s provision. In one service, a new build<strong>in</strong>corporated a child visit<strong>in</strong>g suite with separate entry for familiesand children. However, they have been required to address this byclos<strong>in</strong>g this entrance.• Trust lies at the centre of this approach but was perceived as be<strong>in</strong>gcomplex to create and requir<strong>in</strong>g understand<strong>in</strong>g and will<strong>in</strong>gness onthe part of staff as well as women service users• Cont<strong>in</strong>uity across the service was important but some womensuggested that staff had favourites and thus treated womendifferently.“I th<strong>in</strong>k aga<strong>in</strong> there is somevery positive practice, but Ith<strong>in</strong>k staff are not alwaysconsistent, and this doesn’tpromote relational security,when not all staff ma<strong>in</strong>ta<strong>in</strong>the same rules and work tothe same policies andprocedures, but I th<strong>in</strong>k thereare some very goodtherapeutic relationshipsbetween <strong>in</strong>dividualmembers of staff andwomen they work with butthe <strong>in</strong>consistency is a bigproblem.”“The patients are veryimportant as well assometimes they are the bestpeople to judge whenanother person is not well.You can just tell becausesometimes it’s like look<strong>in</strong>g <strong>in</strong>the mirror, you can see youremotions <strong>in</strong> them.”Woman service user“They are not major th<strong>in</strong>gsbut to be signed off asmedium secure now youhave to be like male mediumsecurity. Into thema<strong>in</strong>stream wanted thatnot to be the case, to bedifferent for women. Soth<strong>in</strong>gs that aren’t caus<strong>in</strong>gproblems at all <strong>in</strong> terms ofwomen are go<strong>in</strong>g to have alot of money thrown at themto alter them.”45
• Individual approaches and attitudes had <strong>in</strong> a small number ofsituations prevented staff from fully implement<strong>in</strong>g the relationalsecurity model. Some professionals were perceived as ‘old‐school’and reliant on treatment by medication. Others were seen as stillf<strong>in</strong>d<strong>in</strong>g it difficult to move away from view<strong>in</strong>g women as attentionseek<strong>in</strong>g, for example, to understand<strong>in</strong>g a woman’s <strong>life</strong> experienceand therefore context for her behaviour.• The use of patroniz<strong>in</strong>g or <strong>in</strong>fantalis<strong>in</strong>g language concerned somewomen and the professionals work<strong>in</strong>g with them. This <strong>in</strong>cludedreferr<strong>in</strong>g to women service users as ‘the girls’ on wards where mostwomen were over 30. In services where there was ongo<strong>in</strong>g tra<strong>in</strong><strong>in</strong>gand CPD related to gender issues, language was rarely identified asan issue.• Changes <strong>in</strong> staff and high levels of turnover prevented thedevelopment of mean<strong>in</strong>gful relationships <strong>in</strong> some <strong>in</strong>stances.“I don't like the newlyqualified ones very much ‐ Idon't talk to them, they'rethe same age as my son,and I'm not go<strong>in</strong>g to go tohim with my problems, soI'm not go<strong>in</strong>g to go to some24 year old, and pour myheart out. I f<strong>in</strong>d thempatronis<strong>in</strong>g as well,sometimes ‐ you know ‐ likeit's curfew time, girls andbleurgh, don't call me a girland don't tell me it's curfewtime. I did have a spat witha couple of them ‐ one wascall<strong>in</strong>g me sweetie, andanother one was call<strong>in</strong>g melovey. And I said can youstop the staff from call<strong>in</strong>gme that, because I f<strong>in</strong>d itpatronis<strong>in</strong>g and I don't likeit. So they've stopped it.”Woman service user• The concept and practice of relational security were not universal. In some cases, services had adoptedthe philosophy but not the term<strong>in</strong>ology. In others, a policy was <strong>in</strong> place but some staff were unclearabout what this meant <strong>in</strong> practice.• Women described what they valued about the service <strong>in</strong> terms consistent with the ideas underp<strong>in</strong>n<strong>in</strong>grelational security.• Some were frustrated by the level of physical security but <strong>in</strong> particular, <strong>in</strong>consistency of security policyimplementation was a cause of compla<strong>in</strong>t.46
5. Day‐to‐day realities: arrival <strong>in</strong>to and stay<strong>in</strong>g at medium secure servicesI th<strong>in</strong>k other women patients are very important because sometimes they are the best people to judgewhen another is not well. There have been <strong>in</strong>stances on the ward where the patients have observed andbeen say<strong>in</strong>g ‘that person’s go<strong>in</strong>g to self‐harm’; you can just tell because sometimes it’s like look<strong>in</strong>g <strong>in</strong> themirror and you can see your emotions <strong>in</strong> them. You try and expla<strong>in</strong> to the nurs<strong>in</strong>g staff and they’re like,‘well, we don’t have any signs’ so that makes it difficult for you. Sometimes I th<strong>in</strong>k it helps people that wenotice someth<strong>in</strong>g and can go and talk to them as we seem to pick th<strong>in</strong>gs up easier. That’s where thepatients come <strong>in</strong>.Woman service userThe day‐to‐day <strong>life</strong> of women patients <strong>in</strong> medium secure services and their as well as staff perceptions ofroutes to recovery were shaped by a variety of factors. These <strong>in</strong>cluded the <strong>in</strong>terior as well as exteriorphysical environment; the rules and regulations <strong>in</strong> operation at the time; the range of activities on offer orobligatory and, importantly the overall ambience of the unit. Each impacted differently either because ofdifferences <strong>in</strong> service ethos, structure and space or because of the ways <strong>in</strong> which <strong>in</strong>dividual womenresponded to them <strong>in</strong> the context of their own situation. This section exam<strong>in</strong>es these different responsesand identifies areas of apparent shared effective practice for a dedicated women’s service.5.1 Early days: admissions and arrivalWomen’s services operated a range of admission procedures from aneight‐hour turn around be<strong>in</strong>g promoted by an <strong>in</strong>dependent provider toprocesses which could take many months to conclude. One servicedescribed their weekly admissions and transfer panel where discussionwas based on a structured pre‐admission assessment process templatewith <strong>in</strong>clusion and exclusion criteria and consideration of whether thewoman could fit <strong>in</strong>to the service as it stands. Services noted the need toachieve a balance which did not keep women wait<strong>in</strong>g too long yet gavethem time to adjust to a possible move. With the growth <strong>in</strong> the numberof women com<strong>in</strong>g via the Crim<strong>in</strong>al Justice system, time was not alwaysavailable but ideally should have been provided. Further constra<strong>in</strong>ts onthe ideal policy resulted from the necessary but sometimes convolutedarrival at agreement of how a placement would be paid for.The women who participated <strong>in</strong> the evaluation rarely talked aboutformal admissions policies. However, they frequently described theexperience of admission and then arrival at the medium secure service.For many, mov<strong>in</strong>g to medium secure represented an improvement <strong>in</strong>their circumstances, a sign of hope that they were on ‘the way out’ andan opportunity to live with<strong>in</strong> a more congenial and often more attractiveenvironment.Some women were <strong>in</strong>strumental <strong>in</strong> the choice of service and most“I was at Broadmoor forseven years and didn’t reallyneed to be there but therewas nowhere <strong>in</strong> my area Icould go. Then this placewas built and they said I wasa good candidate. I thoughtit was really nice and when Icompared it withBroadmoor, it was just likeheaven here!”Woman service user“It was a slow process. I keptcom<strong>in</strong>g down (to visit),meet<strong>in</strong>g the girls, com<strong>in</strong>g tothe community meet<strong>in</strong>g andthen I f<strong>in</strong>ally moved. So thattook three months which isgood <strong>in</strong> a way as then itwasn’t a big jump. Go<strong>in</strong>gback, com<strong>in</strong>g down to seethe girls and they’re ever sonice. That took a weight off47
wanted to be placed close to family, friends or where they came from.Others specifically wanted to be away from a location where they wereknown. Not all were so fortunate <strong>in</strong> terms of choice and althoughservices for women were work<strong>in</strong>g to provide appropriate placements,constra<strong>in</strong>ts of fund<strong>in</strong>g and local availability determ<strong>in</strong>ed and <strong>in</strong>deedlimited choice. The Dene <strong>in</strong> West Sussex offered services to women fromany area and frequently had women from Scotland and Wales as well asother less well‐served areas of the UK.A small number of women expressed concern about their admission. Thiswas more likely to be <strong>in</strong> relation to appropriateness of the placementrather than the process. Staff also noted that for some women mov<strong>in</strong>gfrom prison or a high secure hospital and arrival at a medium secureservice could trigger mixed feel<strong>in</strong>gs.Some women missed the stricter regimes of high secure sett<strong>in</strong>gs andothers were concerned that by mov<strong>in</strong>g from prison to a secure mentalhealth service, they were wrongly identified as hav<strong>in</strong>g mental illness andworse, had no idea of how long they would stay. A pre‐def<strong>in</strong>ed prisonsentence was preferable. For one woman, however, the moverepresented a positive change and she noted ‘how clean it all was, howcomfortable and how gentle everyone was’ on arrival.Standard admission criteria for women’s dedicated medium secureservices usually <strong>in</strong>cluded the follow<strong>in</strong>g:• adult women of work<strong>in</strong>g age (18‐65 years) from specified geographicareas who will benefit from admission to a women’s secure serviceand be able to <strong>in</strong>tegrate <strong>safe</strong>ly <strong>in</strong>to the environment and the patientpopulation• deta<strong>in</strong>ed under the Mental <strong>Health</strong> Act 1983 (MHA) or Crim<strong>in</strong>alProcedure Act 1991 (CPA) with a primary diagnosis of mental illness• the service will recognise the complex psychopathology with<strong>in</strong> thelegal category of psychopathic disorder as def<strong>in</strong>ed under the MHA• assessment may be offered for women with borderl<strong>in</strong>e learn<strong>in</strong>gdisability• women with severe mental impairment are excluded as are womenwith major acquired or organic bra<strong>in</strong> damage.Assessment policies which supported decision‐mak<strong>in</strong>g were importantand <strong>in</strong> particular where <strong>in</strong>itial assessments exam<strong>in</strong>ed the way <strong>in</strong> which awoman could benefit from environments where relational as well asprocedural and physical security were adhered to.my shoulders, that the girlswere go<strong>in</strong>g to be all rightbecause you worry aboutth<strong>in</strong>gs like that”.Woman service user“They wanted me to becloser to my family, so theymoved me. I didn’t really getasked, they just did it. It waspresumed to be the best forme and as I wasn’t that well,would I really have beenable to say anyth<strong>in</strong>g not tomove? Where I was did sayto me that if I didn’t want togo, I could have stayed therebut the ball was roll<strong>in</strong>g.”Woman service user“I th<strong>in</strong>k it works fairly well. Ifwomen are hav<strong>in</strong>gdifficulties with otherplacements, it’s importantthat they’re not left <strong>in</strong> asituation where they’re notgett<strong>in</strong>g the service theyneed for a long time. Thepre‐admission assessment isresponsive to patients’needs and if there is a needfor psychological or OTassessment they will go outtoo <strong>in</strong> advance. We’ve beenable to give the patient lotsof <strong>in</strong>formation and they’vefelt relatively well‐<strong>in</strong>formedwhen they come.”“We’ve had women fromBroadmoor where we’vebeen lots of times to developcare plans so that a womanis very clear about what sheneeds to achieve to stepdownand visits herewhereby they’ve already gotsometh<strong>in</strong>g to do, the OTknows what they’re<strong>in</strong>terested <strong>in</strong>. We also go tothe CPA before they get hereso care plans can be made48
Case example:In terms of referrals from prison, although the cl<strong>in</strong>ical team was able torespond by arrang<strong>in</strong>g an assessment visit with<strong>in</strong> an appropriate time frame,usually the recommended two‐week period, due to <strong>in</strong>sufficient beds to meetthe demand for medium secure for women from the area, women were ofteneither wait<strong>in</strong>g with<strong>in</strong> the prison sett<strong>in</strong>g for a prolonged period for a bed tobecome available or referred to the commission<strong>in</strong>g team to f<strong>in</strong>d a bed <strong>in</strong> theprivate sector. One cl<strong>in</strong>ician who regularly assessed women <strong>in</strong> prisonreported that, because he was aware that due to the long wait<strong>in</strong>g times forfemale beds at the unit, if he felt the woman needed to transfer from prisonto a more therapeutic sett<strong>in</strong>g rather than wait the ‘arbitrary’ three monthperiod for a bed to become available at the service, know<strong>in</strong>g that it washighly unlikely to happen, he took a more proactive approach and referredthe woman through to the <strong>in</strong>dependent sector without delay.Although on occasion women were referred directly from the courts, due tothe small number of beds <strong>in</strong> the women’s service, and with several womenusually on the wait<strong>in</strong>g list, it was rare that the service admitted a womandirectly from court. However, if she was assessed as urgently requir<strong>in</strong>g amedium secure mental health sett<strong>in</strong>g, the case was referred to theSpecialised Secure Commission<strong>in</strong>g Team to f<strong>in</strong>d an appropriate placement <strong>in</strong>the <strong>in</strong>dependent sector, which usually required her be<strong>in</strong>g placed out of area.For women who received a Restricted Hospital Order and who requiredsupervision from the community forensic team once they were eventuallydischarged <strong>in</strong>to the community, the aim will normally be to br<strong>in</strong>g them backto the unit as soon as a bed becomes available. This was because thecl<strong>in</strong>icians who acted as Responsible Medical Officer for the women <strong>in</strong> thecommunity believed it was necessary for them to have worked with a woman<strong>in</strong> the <strong>in</strong>‐patient sett<strong>in</strong>g before tak<strong>in</strong>g on responsibility for them <strong>in</strong> thecommunity. However, this led to delays <strong>in</strong> women be<strong>in</strong>g able to move alongthe care pathway at the appropriate time, for once women were placed <strong>in</strong>the <strong>in</strong>dependent sector and they already had access to a medium secure bedthey may not have been given the same priority when a bed becomesavailable at the unit as a woman who was <strong>in</strong> a prison or community sett<strong>in</strong>g.This lead to blockages <strong>in</strong> the care pathway with out‐of‐area womensometimes hav<strong>in</strong>g to wait lengthy periods of time to be returned to an NHSbed <strong>in</strong> their home area.In the case study areas, staff <strong>in</strong>volved <strong>in</strong> the admissions process andwomen identified a number of factors which helped the admissionsprocess work well <strong>in</strong>clud<strong>in</strong>g:• Speed of pre‐admission assessments• Consultation with the woman concerned about her needs• Provision of <strong>in</strong>formation to the woman about the new service• Keep<strong>in</strong>g the woman <strong>in</strong> touch with the new service, e.g. send<strong>in</strong>gpictures and arrang<strong>in</strong>g ongo<strong>in</strong>g visits while wait<strong>in</strong>g for a space• Ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g the woman’s outside connections, e.g. with children,so it’s a gradual lett<strong>in</strong>g goand gradual <strong>in</strong>troduction tous – unless it’s anemergency when we’ll br<strong>in</strong>ga woman <strong>in</strong> very quickly.”“We’re a bit different to amen’s service! When com<strong>in</strong>gfrom prison, rather thancom<strong>in</strong>g via the vehicle airlock which is standard forthe men’s service, what weprefer is that women justwalk through the front doorif at all possible, not <strong>in</strong>handcuffs, not <strong>in</strong> shacklesbecause that’s just add<strong>in</strong>gmore trauma.”“In some parts of thecountry an assessment takesplace, we supply the reportsand it goes to the Fund<strong>in</strong>gPanel and then they are notsure, then there may begate‐keep<strong>in</strong>g by the localMSU and this could takeseveral months. Sometimesthe patient’s cl<strong>in</strong>ical needsseem to take a m<strong>in</strong>orposition <strong>in</strong> terms of therank<strong>in</strong>g of priorities.”“This is perhaps worse <strong>in</strong> thesense that there areobviously <strong>in</strong>sufficient bedsand we don’t have thecapacity to admit thenumber of women referredand that leads to thewomen spend<strong>in</strong>g longerperiods of time <strong>in</strong> prisonwhen they are deemed torequire treatment <strong>in</strong>hospital. There are noguidel<strong>in</strong>es <strong>in</strong> place as to howlong a person can wait or49
prior to the move and on arrival at the new service• Cont<strong>in</strong>uity of staff, e.g. ensur<strong>in</strong>g the woman’s primary nurseattended the discharge meet<strong>in</strong>g from the previous placement and<strong>in</strong>vit<strong>in</strong>g previous placement staff to attend first CPA meet<strong>in</strong>g at thenew service.A number of changes were identified as potential for improvement:• Enhanced communication between commissioners and referrers toensure agreement prior to movement which was seen to beespecially important where referrals take place very quickly• Reduc<strong>in</strong>g the patch<strong>in</strong>ess of referral processes• Reduc<strong>in</strong>g commercial pressures on some <strong>in</strong>dependent sectorproviders for rapid admissions before there has been sufficientopportunity to meet with the woman concerned and staff <strong>in</strong>volved <strong>in</strong>her care.From the women’s perspective, central to ensur<strong>in</strong>g smooth admissionand arrival for women were:• Visits to the service and from staff to the <strong>in</strong>dividual woman <strong>in</strong>anticipation of transfer• Clarity about what was happen<strong>in</strong>g and why <strong>in</strong> relation to transfers,expla<strong>in</strong><strong>in</strong>g the need for appropriate provision and thus how decisionsare made• Sufficient time to ensure appropriateness of the admission for thewoman concerned and <strong>in</strong> relation to the mix of women <strong>in</strong> the unit• Provision of a policy or at a m<strong>in</strong>imum, service expectations on arrival• Time to absorb change on arrival before hav<strong>in</strong>g to deal with officialpaperwork.ought to wait or noguidel<strong>in</strong>es about when it isappropriate to refer urgentlyto the private sector. That isleft to an <strong>in</strong>dividual’s cl<strong>in</strong>icaldiscretion when to do that. Itake the approach that if Iknow there’s no po<strong>in</strong>t <strong>in</strong>wait<strong>in</strong>g an arbitrary threemonths, and there is noprospect of a bed then I takea more proactive approachand refer sooner rather thanlater, I won’t delay at all andI would refer to the<strong>in</strong>dependent sector.”“We had a case where noone knew who was fund<strong>in</strong>gthe current placement of awoman even though shewas <strong>in</strong> hospital. It tookseveral weeks to clarify whowas fund<strong>in</strong>g her and shewas a restricted patient. Sothe M<strong>in</strong>istry of Justice hadto get agreement to atransfer and it took four orfive months dur<strong>in</strong>g whichtime the patient absconded– aga<strong>in</strong>!”For professionals mak<strong>in</strong>g decisions about referrals and admissions, animportant factor was the balance of women already part of the unit.Consideration had to be given to how settled the unit was, possibledisruption that might be created by a new service user and the staff<strong>in</strong>gand support <strong>in</strong> place to give sufficient support to someone com<strong>in</strong>g <strong>in</strong>.5.2 Physical environments: what works for women and staff?For women and the staff work<strong>in</strong>g with them, the physical environment ofa women’s service was a key factor <strong>in</strong> how well the service was able tofunction. Four of the case study services were housed <strong>in</strong> relatively newbuild<strong>in</strong>gs. Two opened dur<strong>in</strong>g the course of the evaluation and <strong>in</strong> onecase, women and staff here were asked to make comparisons betweenthe old and new build<strong>in</strong>gs.50
Women identified the importance of design and layout of the unit andhow it felt to be there. For example, one woman on arriv<strong>in</strong>g from anolder style hospital to a new‐build unit observed that it still smelt like ahospital and for her worse was the fear that it would be a less settledenvironment where women were far less well than she was used to.Immediate responses were <strong>in</strong>fluenced by previous experience. Somewomen found their most recent placement <strong>in</strong>to new‐build units too‘sterile’. Many, however, experienced a more homely approach with<strong>in</strong>clean and modern build<strong>in</strong>gs. They said this was very important to them.They liked hav<strong>in</strong>g their own rooms (often with en‐suite bathrooms) andaccess to communal areas sometimes <strong>in</strong>clud<strong>in</strong>g a women’s gym, activityrooms, gardens and visit<strong>in</strong>g areas for families and children.“I th<strong>in</strong>k lett<strong>in</strong>g patients layaround all day and sleep<strong>in</strong>g<strong>in</strong> the day room could bechanged. It’s not nice if youare sitt<strong>in</strong>g <strong>in</strong> the room andall you can hear is snor<strong>in</strong>g.”Woman service userWomen’s <strong>in</strong>put <strong>in</strong>to design varied across services. However, with newbuild units they were less likely to have had any <strong>in</strong>put <strong>in</strong>to thearchitecture or basic decor. These units were all required to meet anumber of physical security standards as well as ensure that they couldprovide a <strong>safe</strong>, ligature‐ proof environment. Although women were ableto <strong>in</strong>dividualise their rooms with posters for example, some said theywould have liked a more active role <strong>in</strong> at least the decoration of the<strong>in</strong>terior shared spaces.Women at one unit were clear that the shared space was just too small.The day room acted as sitt<strong>in</strong>g room, d<strong>in</strong><strong>in</strong>g room, television room andgarden access. This service had a number of other rooms for activities,meet<strong>in</strong>gs and one‐to‐one one sessions but the ma<strong>in</strong> area was limited <strong>in</strong>the number of people that could be accommodated at any one time.One new‐build service was designed with open‐plan day areas to threesides of the office/observation area. Other rooms led from the open planarea which was large enough to have several seat<strong>in</strong>g areas and aseparate d<strong>in</strong><strong>in</strong>g room.A further important consideration was how to ensure that designenabled women to be ‘at home’ whilst staff were able to observe theactivity with<strong>in</strong> common areas as well as mix with women on the unit <strong>in</strong> arelatively relaxed way. Zonal observation of shared areas was thus thepreferred option for services over <strong>in</strong>tensive one‐to‐one observationswhich some women found <strong>in</strong>trusive. In addition, many women notedthat one‐to‐one observations impacted on the unit more generallywhere activities, e.g. escorts for access, on/off ward activities, had to belimited due to the unavailability of staff.One service was able to partition off areas for the provision of a higherlevel of support, others had dedicated and usually separate areas.Key physical environmental considerations for women and staff <strong>in</strong>cludedthe provision of:51
• Private rooms with en‐suite bathrooms• Lockable space <strong>in</strong> their rooms• Zonal observation areas• Women‐only areas, e.g. bedroom corridors• Permanent and not timed garden access• Sufficient space <strong>in</strong> day rooms for all women to use• High support/<strong>in</strong>tensive nurs<strong>in</strong>g areas for women when acutely illOutdoor space <strong>in</strong> the form of gardens and/or access to hospital groundswas very important to many women at the units. At all the case studyunits, garden space was considered essential and was provided.However, <strong>in</strong> all cases the use of outdoor space raised some issues forwomen and staff alike <strong>in</strong>clud<strong>in</strong>g the follow<strong>in</strong>g:• Women said they preferred garden doors to be open at least all dayrather than timed exits. In one service, they were concerned thatdifferent staff operated different rules for giv<strong>in</strong>g access.• Staff <strong>in</strong> one service observed that regulations would require them to<strong>in</strong>stall immovable (and to them unattractive, difficult to use)furniture <strong>in</strong> their garden. Provid<strong>in</strong>g shelter from the ra<strong>in</strong> was anotherissue.• Where feasible and agreed, some women had leave to go outunescorted <strong>in</strong> hospital groups or further afield.Of considerable concern <strong>in</strong> at least three case study areas was theimpact of the standards for medium secure services. These imposedgeneric requirements, e.g. the height of perimeter fenc<strong>in</strong>g regardless ofappropriateness <strong>in</strong> a woman’s service. In 2008, one women’s mediumsecure service was forced to become low secure as a result of <strong>in</strong>spection.“You get <strong>in</strong>spected. Thisdoesn’t fit withempowerment because we’llbe replac<strong>in</strong>g the gardenfurniture. We’ve just beentold to do this, well, wewon’t say that but youknow, it doesn’t promoteempowerment does it?”“(The standards for mediumsecure services) place far toomuch emphasis on physicalsecurity but that’s the worldwe live <strong>in</strong>. The person who<strong>in</strong>spects us is male and he’svery staunch <strong>in</strong> his views.”5.3 Interventions, treatments and therapies5.3.1 The rangeWomen’s services agreed that it was essential to provide women withaccess to a range of activities and therapies. There was a high level ofcommitment <strong>in</strong> most services to f<strong>in</strong>d<strong>in</strong>g ways of meet<strong>in</strong>g women’spsychological needs as well offer<strong>in</strong>g opportunities to be <strong>in</strong>volved <strong>in</strong> otherways which were <strong>in</strong>tended to facilitate recovery.Services participat<strong>in</strong>g <strong>in</strong> the orig<strong>in</strong>al survey were asked about the<strong>in</strong>terventions, treatments and therapies available to women. Table 6shows the total number of wards provid<strong>in</strong>g the different treatments. Itwas <strong>in</strong>terest<strong>in</strong>g to note that despite most provid<strong>in</strong>g <strong>in</strong>dividual therapyand creative therapies, these were not be<strong>in</strong>g used by all women. In oneyear, only eight wards had more than 60% of women who attended<strong>in</strong>dividual therapy. They were less likely to have attended well‐womensessions and complementary therapies featured <strong>in</strong> only two cases.“I had psychology for sixyears at the other place socom<strong>in</strong>g here it’s the sameth<strong>in</strong>g but it’s more work<strong>in</strong>gto the future <strong>in</strong>stead ofbackwards. There it was allbackwards, the past. This isforward now, the future. It’sweird because I alwaysthought therapy talkedabout the bad th<strong>in</strong>gs butnow we’re talk<strong>in</strong>g about thegood th<strong>in</strong>gs and whatmoves me on.”Woman service user52
Table 6: Interventions, treatments and therapies 2006 (n=21 wards)Interventions/treatmentsand therapiesIndependentwards (n=6)NHS wards(n=15)Total(n=21)Individual psychological6 15 21therapyCreative therapies 6 12 18Well‐women sessions &5 10 15screen<strong>in</strong>gGroup therapy 5 7 12Dialectical Behaviour1 3 4Therapy (DBT)Individual therapy based on 2 5 7DBTHarm‐m<strong>in</strong>imisation/reduction approach to self<strong>in</strong>jury4 10 14Whilst not all wards provided all the <strong>in</strong>terventions we specified, 18 wardsprovided <strong>in</strong>formation about additional types of specialist therapy thatthey offered to women. These <strong>in</strong>cluded:• Psychotherapy for eat<strong>in</strong>g disorders/issues• Smok<strong>in</strong>g cessation• Fire sett<strong>in</strong>g• Substance misuse• Mental health awareness• Offend<strong>in</strong>g behaviour• <strong>Health</strong>y liv<strong>in</strong>g• Cognitive problem solv<strong>in</strong>g group• Relationship groupThis represented a wide range of different provision. Some wards saidthat they had <strong>in</strong>troduced new developments very recently and werepilot<strong>in</strong>g their usefulness, e.g. a cognitive problem solv<strong>in</strong>g group.Wards were offer<strong>in</strong>g a wide range of activities to patients. Whilstvocational tra<strong>in</strong><strong>in</strong>g was <strong>in</strong>frequently offered, on‐site education sessionsand creative arts were provided and taken up by women. Highest levelsof up‐take were <strong>in</strong> relation to sports and exercise (16 wards said over60% of women took part), community <strong>in</strong>clusion, e.g. leisure activities andshopp<strong>in</strong>g (14 wards said over 60%) and social events (15 wards said over60%).In the case study areas, services said that they provided structuredtimetables of <strong>in</strong>dividual and group activities. These were weekday onlyand some women said they would like more to be offered at weekendswhich became bor<strong>in</strong>g. In one service, women were asked to complete an53
<strong>in</strong>dividual timetable weekly mak<strong>in</strong>g choices about what they wouldattend the follow<strong>in</strong>g week. These activities are discussed <strong>in</strong> more detailbelow.5.3.2 Psychological therapiesAll of the case study areas provided psychological therapy for <strong>in</strong>dividualsand <strong>in</strong> groups but arranged and delivered <strong>in</strong> a variety of ways. Thephilosophy of care which underp<strong>in</strong>ned the service provided the basis forthe range and content of provision. For example, <strong>in</strong> one area, womenwere encouraged to jo<strong>in</strong> a group for ‘deal<strong>in</strong>g with feel<strong>in</strong>gs’ before theybegan to consider <strong>in</strong>dividual therapy. This was <strong>in</strong> recognition of women’sexperience and the need to develop strategies before mov<strong>in</strong>g on to <strong>in</strong>depthexploration of their past and actions. Any group or <strong>in</strong>dividual workwas expected to be supported by staff on the ward although this was notalways the case.Case example:There was widespread awareness among nurs<strong>in</strong>g staff of the importance ofrespond<strong>in</strong>g appropriately to the emotional needs of women service users.One nurse manager spoke of the “sponge‐like” quality of women to absorbhigh levels of support and attention from staff, and warned that problemsarise if this support is not available. Nurs<strong>in</strong>g support on the wards wasorganized with each woman hav<strong>in</strong>g an allocated team of ward staff, with atleast one member of her team always be<strong>in</strong>g on duty at any time. Womenwere encouraged to approach a member of their own team if they needemotional support or to talk for example about issues relat<strong>in</strong>g to their <strong>in</strong>dexoffence, past experiences of abuse or for support around self <strong>in</strong>jury.Someone familiar with their needs and care plan should always be on hand.Each woman also had an allocated primary nurse who provided regular oneto‐onesessions which usually <strong>in</strong>cluded specific work to help her understandand manage her own mental health needs, for example help<strong>in</strong>g to recognizeearly signs of relapse or to develop alternative cop<strong>in</strong>g strategies to self‐<strong>in</strong>jury.Women would normally have face to face contact with their psychiatrist(RMO) on at least a weekly basis, either with<strong>in</strong> the weekly ward round or on aone‐to‐one basis. A Senior House Officer (SHO) was also available to providemedical <strong>in</strong>put as required, <strong>in</strong>clud<strong>in</strong>g physical health issues, on a day to daybasis. Most of the women who met the evaluation team spoke positivelyabout their relationship with their psychiatrist. A number of women reportedthey believed medication played a key role <strong>in</strong> the management of theirmental health needs, with some feel<strong>in</strong>g it was one of the most importantaspects of their treatment at the unit.The psychology department provided a comprehensive assessment and<strong>in</strong>dividual formulation of each woman’s needs dur<strong>in</strong>g the post‐admissionperiod and one‐to‐one psychology therapy sessions are offered whenappropriate, often with a focus on <strong>in</strong>dex offence work. The formulationbasedassessments undertaken by the psychologists were shared across theMDT so they could <strong>in</strong>form the work of the nurs<strong>in</strong>g and OT teams and supportappropriate engagement with the women on the wards.“<strong>My</strong> primary nurse wasreally good, he listened tome, listened to what I had tosay, and he also seemedconcerned about what washappen<strong>in</strong>g to me. I couldalso have a bit of a laughwith him… he helped me tounderstand about my illness,how to deal with it better.”Woman service user“Sometimes ward staffbelieve that psychologyunsettles women, whenwomen access psychology towork on difficult issues, theywill come back onto theward very unsettled as theirsession has brought upissues that have upset them,but this is part of theprocess, but the women willthen pick up on the idea thatthe ward staff believe thatperhaps psychology isn’t anygood for them, and that54
Some members of ward staff found it difficult to know how best to supportwomen return<strong>in</strong>g from psychology sessions when they had been work<strong>in</strong>g ondistress<strong>in</strong>g issues. Where it worked, it worked well. However, it was felt thatsometimes ward staff underm<strong>in</strong>ed the work of the psychologist, bysupport<strong>in</strong>g or mak<strong>in</strong>g suggestions that the women are better off notattend<strong>in</strong>g such sessions.One woman <strong>in</strong>terviewed reported that she had recently decided todiscont<strong>in</strong>ue her psychotherapy, say<strong>in</strong>g that one of her care team on the wardfelt it was not help<strong>in</strong>g her to keep go<strong>in</strong>g back over the past. However, whenasked about the role of her therapy <strong>in</strong> her recovery, it was clear the womanbelieved she would not have made the progress she had done if it had notbeen for the work with the psychotherapist.In addition to meet<strong>in</strong>g with a consultant psychiatrist and the ResponsibleMedical Officer (RMO and from 2009, Responsible Cl<strong>in</strong>ician), as part ofthe MDT, women were be<strong>in</strong>g seen by psychologists, psychotherapistsand meet<strong>in</strong>g with nurs<strong>in</strong>g staff who had received tra<strong>in</strong><strong>in</strong>g <strong>in</strong>psychological therapies <strong>in</strong>clud<strong>in</strong>g DBT. What appeared to be importantwas f<strong>in</strong>d<strong>in</strong>g ways for women to talk about traumatic experiences <strong>in</strong> theirpast and how they related to why they had been placed <strong>in</strong> a secureservice, <strong>in</strong> ways that supported them. Formal activities provided oneopportunity for expression.Case example:In this area, cl<strong>in</strong>ical psychologists were <strong>in</strong>volved <strong>in</strong> women’s care from themoment they arrived. Initially, this would be through carry<strong>in</strong>g outassessments to identify women’s cl<strong>in</strong>ical and ‘forensic’ needs with a focus onrisk assessment. Hav<strong>in</strong>g this at the outset enabled the service to monitor awoman’s progress through her care pathway and what had or had not beenprovided as part of this. At this stage, there was little <strong>in</strong>dividual work butwomen were encouraged to take part <strong>in</strong> groups and focus on understand<strong>in</strong>gtheir own problems and develop<strong>in</strong>g skills. With a DBT approach on one ward,groups were designed to enable women to build skills <strong>in</strong> tolerat<strong>in</strong>g distress,social skills, emotional regulation and problem solv<strong>in</strong>g.underm<strong>in</strong>es the process, andwill agree with the wardstaff and th<strong>in</strong>k well I won’tbother with this anymore,rather than the ward staffsupport<strong>in</strong>g the therapeuticprocess.”“I’m do<strong>in</strong>g CBT. It’s quitegood – we’ve been talk<strong>in</strong>gabout OCD behaviours andit’s good because no‐one’sever really sat down with meand said ‘What do you do?Why do you do this? A lot ofthe time, because it soundssilly what I do, I’membarrassed to tell peoplebut this time I’m tell<strong>in</strong>g hereveryth<strong>in</strong>g.”Woman service user“We have a very therapeuticprogramme for women todevelop social skills or beable to learn problemsolv<strong>in</strong>gskills. I th<strong>in</strong>keveryth<strong>in</strong>g has an impact ontheir mental health so it’sabout look<strong>in</strong>g at the broaderpicture rather than just, say,medication forschizophrenia.”The service provides a CBT programme of groups as well as other group work,e.g. liv<strong>in</strong>g well with schizophrenia, <strong>in</strong>tended to support women <strong>in</strong> develop<strong>in</strong>gtheir own skills. The service was concerned about attendance but overrid<strong>in</strong>gthis was whether women had ga<strong>in</strong>ed someth<strong>in</strong>g from the experience.Attendance at groups was l<strong>in</strong>ked to an <strong>in</strong>centive programme where womenwere ‘rewarded’ for tak<strong>in</strong>g part <strong>in</strong> the activities identified <strong>in</strong> their care plan.Participation was voluntary.The provision of group work was encouraged but reflected that access to<strong>in</strong>dividual therapy may take a considerable period of time to organize due todemand across the service as a whole.55
This service had a dedicated therapy suite away from the wards. For somethis was a disadvantage act<strong>in</strong>g to discourage women when their riskassessment meant they could not leave the ward. For others, it was an<strong>in</strong>centive.Women <strong>in</strong> medium secure services said that:• They were able to exercise some choice about the type and timecommitment to psychological therapies. Some women had comefrom services where they had been <strong>in</strong> therapy for years. They thenfound they could attend groups and undertake other activities as analternative.• They appreciated learn<strong>in</strong>g to take a more positive outlook and somesaw that therapy was a way of mov<strong>in</strong>g forward.• They could become confused by different staff views about the valueof therapy and more cont<strong>in</strong>uity would have been helpful.What was <strong>in</strong>terest<strong>in</strong>g was where the l<strong>in</strong>e was drawn <strong>in</strong> relation to whatwas or was not perceived as psychological therapy. Informal discussionsabout a variety of issues were viewed as be<strong>in</strong>g just as important towomen as the formal provision of therapy.In one area, the staff team believed that an appropriate range oftherapeutic <strong>in</strong>terventions and occupational therapy <strong>in</strong>clud<strong>in</strong>g creativetherapies and leisure activities, were made available to women serviceusers. Named nurses played an important part <strong>in</strong> <strong>in</strong>dividual women’scare. There were also Associate Practitioners based on the ward whowere unqualified support workers and l<strong>in</strong>ked <strong>in</strong> very closely withpsychology or OT staff. These had protected time to undertake specificpieces of therapeutic work with women <strong>in</strong>clud<strong>in</strong>g, for example, CBTwork, self esteem and self perception, anxiety management, relapseprevention, women’s offend<strong>in</strong>g and risk management, e.g. fire‐sett<strong>in</strong>g.As Associate Practitioners were ward‐based, they were on the wardenough to be able to gradually build relationships with the women,especially with those who found it more difficult to engage with apsychologist where contact was more formal as they came to providetherapy sessions and then left.5.3.3 Occupational therapy: beyond the stereotypeOccupational therapy (OT) has changed over the years and the casestudies here demonstrated the ways <strong>in</strong> which this has happened <strong>in</strong>women’s medium secure services. While occupational therapists wereprimarily focused on work<strong>in</strong>g with women to develop skills that wouldfacilitate their recovery and enable them to manage <strong>in</strong> lower‐secure orcommunity sett<strong>in</strong>gs, not all services were able to give the role andfunction of OT the centrality it required. Resources affected some while“We don’t sit around andmake baskets! We produceda magaz<strong>in</strong>e and weproduced a leaflet aboutself‐harm and PTSD to beleft <strong>in</strong> doctors’ surgeries andcasualty departments sothat they’ll have a betterunderstand<strong>in</strong>g of us.”Woman service user56
other services were perceived as be<strong>in</strong>g less open to the idea of genderfocusedOT. Where it worked well, OT was an <strong>in</strong>tegrated function with<strong>in</strong>the women’s service feed<strong>in</strong>g <strong>in</strong>to women’s psychological recovery anddevelopment of skillsHowever, not all services were able to allocate an OT to women’sprovision. In one case study area, whilst there was a dedicatedpsychologist for the women’s service there was only a “l<strong>in</strong>ked”occupational therapist. However, the appo<strong>in</strong>tment of a dedicated OT forthe women’s service would have enhanced the development of genderspecific groups and activities for the women at this unit. In turn, somestaff argued this would improve access to activities for women who werenot able to leave the ward or not able to, or chose not to, access mixedsexactivities.In another area, many of the therapeutic and activity groups were notgender specific, as often there were not enough women to support theprovision of women‐only groups. Efforts were be<strong>in</strong>g made to providesome choices for women‐only activities and creative therapies, and theOT service had allocated a women‐only afternoon each week whichprovided social contact time for women. This OT department also ran asupport group for women who self‐<strong>in</strong>jure, and the service as a whole hadbeen develop<strong>in</strong>g practice guidel<strong>in</strong>es to support <strong>safe</strong>r self‐<strong>in</strong>jury as well aseducation and tra<strong>in</strong><strong>in</strong>g resources for staff and service users.“Women can express an<strong>in</strong>terest <strong>in</strong> OT and we sayhas anyone got ideas andwe’re open. But the keysessions are essentials.Some f<strong>in</strong>d it quite hard whenthey come. ‘You do get up <strong>in</strong>the morn<strong>in</strong>g, you do comeand have breakfast andactually you can’t go to yourbedroom’ unless on a higherstatus. Once they get usedto that, it’s quite healthy tohave a rout<strong>in</strong>e aga<strong>in</strong>because it’s also about howsociety out there works.”Opportunities for women to <strong>in</strong>crease their levels of <strong>in</strong>dependence andbecome <strong>in</strong>volved <strong>in</strong> education, tra<strong>in</strong><strong>in</strong>g and paid or unpaid work werepromoted <strong>in</strong> all the case study areas. We <strong>in</strong>terviewed women who:• Worked with<strong>in</strong> the secure service, e.g. <strong>in</strong> the café• Attended a range of classes with<strong>in</strong> the service <strong>in</strong>clud<strong>in</strong>g literacy,numeracy, IT and GCSE subjects• Attended local colleges• Undertook Open University degreesThere was some debate about how far a ‘teacher’ would be fullyparticipant <strong>in</strong> discussions about <strong>in</strong>dividual women and their Care Plans.Some services employed a dedicated teacher while others contractedlocal agencies. However, neither model appeared to put education nearto the centre of a woman’s plan and <strong>in</strong> one case, this had led to stafffeel<strong>in</strong>g that education was treated as a ‘poor relative’ despite itsapparent successes and therapeutic potential.5.3.4 Social work support: essential l<strong>in</strong>ks outside the serviceSocial workers had very specific and for some, pivotal roles with<strong>in</strong>women’s services. A pr<strong>in</strong>cipal area of work was to help women ma<strong>in</strong>ta<strong>in</strong>contact with families and their children where appropriate and feasible.“That’s someth<strong>in</strong>g I wouldstand up and shout about!I’ve seen young ladies thathave never taken examsbefore, have sat them forthe first time and passed.Not long ago we had onewho passed an exam andsaid ‘I never thought I coulddo this and now I’ve got acertificate!’.”“We had one woman whohad been labelleddangerous. We had to haveseveral nurses, the children,the father and their socialworker so the number of57
From pre‐admissions and arrival through to mov<strong>in</strong>g on, social workersprovided women with support:• Rega<strong>in</strong><strong>in</strong>g and susta<strong>in</strong><strong>in</strong>g family contact where appropriate• Supervision of child visits• Family home visits• Contribut<strong>in</strong>g to CPA and Tribunal reports• Liais<strong>in</strong>g with external agencies, e.g. CPNs and Social ServicesSocial workers experienced a very high demand on their time. They saidthey needed to be clear and boundaried about what they could offer towomen as well as staff <strong>in</strong> the service. One social worker argued that itwas important to <strong>in</strong>volve ward staff <strong>in</strong> traditionally ‘social work’ issues,e.g. family visits, as a means of support<strong>in</strong>g women as well as build<strong>in</strong>gteam relationships.Social workers, <strong>in</strong> addition to other professionals, frequently had officespace some distance removed from the ward which reduced theirvisibility and the access that women had to them. One suggested hold<strong>in</strong>ga regular ‘surgery’ where women could f<strong>in</strong>d a social worker on the unitand see them almost immediately.adults <strong>in</strong> the room wasabsurd! We worked welltogether, social servicesbacked out and wemanaged, with the mentalhealth assessment and herreal diagnosis, to rehab herout. Now she’s liv<strong>in</strong>g withher partner and children.That’s where social work fits<strong>in</strong>to medium secure withwomen.”“<strong>My</strong> ideal scenario would bethat there are some facilitieswhere I could be moreaccessible, where I wouldhave some space where Icould see people, could eatand socialise with them.”5.3.6 Advocacy and <strong>in</strong>volv<strong>in</strong>g women <strong>in</strong> their careOf the 14 returned questionnaires <strong>in</strong> the 2006 survey, n<strong>in</strong>e services saidthey had made advocacy available to women and one noted access tolocal Patient Advisory Liaison Service. Services were much less likely tooffer a gender specific advocacy. At that time, WISH was mak<strong>in</strong>g regularvisits to three services which <strong>in</strong>creased to six by 2009. In addition, anduntil 2009, WISH provided a service to four PiC women’s services.Interest<strong>in</strong>gly, few of the women <strong>in</strong>terviewed had sought out the supportof an advocate even though they often knew that an advocacy servicewas available. The lack of use may have been attributable to reports thatadvocates were spread very th<strong>in</strong>, services were under resourced andthus unable to provide an <strong>in</strong>‐depth service to all women. At the sametime, one advocate said that women service users were sometimes sobusy, with activities and meet<strong>in</strong>gs with other staff, it was hard to makeappo<strong>in</strong>tments with them.Advocates were <strong>in</strong>volved <strong>in</strong> issues <strong>in</strong>clud<strong>in</strong>g:• support<strong>in</strong>g women after arrival• support<strong>in</strong>g women <strong>in</strong> develop<strong>in</strong>g confidence• provid<strong>in</strong>g practical <strong>in</strong>formation• sort<strong>in</strong>g practical problems, e.g. benefits issues• support<strong>in</strong>g women <strong>in</strong> relation to their families• ward environments and compla<strong>in</strong>ts about these58
• personal issues affect<strong>in</strong>g women and their care plansOne of the key difficulties they experienced was the time limitation. Forexample, contracts services held with WISH were sometimes for as littleas one day per month. Part‐time roles also meant advocates could not beavailable to attend CPA meet<strong>in</strong>gs or support women at meet<strong>in</strong>gs withsolicitors.Advocacy services also raised concerns about the perceived lack ofacknowledgement of the need for gender‐specific advocacy; that <strong>in</strong>some circumstances how women are listened to, respected and notjudged was, <strong>in</strong> itself, is a factor <strong>in</strong> their treatment, care and recovery; andthat advocates had been seen <strong>in</strong> some circumstances as <strong>in</strong>terfer<strong>in</strong>g <strong>in</strong>situations where staff saw themselves as the professionals and thusbelieved they knew best.5.3.7 Physical health careMost case study areas described a range of health promotion and illnessprevention activities <strong>in</strong>clud<strong>in</strong>g discussion groups with women andsometimes annual health screen<strong>in</strong>g. What worked less well was women’saccess to physical health care professionals as and when they neededthem. Women described the variety of situations where they wanted tosee doctors and preferably a female GP. Only one case study serviceoffered this and along with one other, ensured access to a femalepractice nurse to see women <strong>in</strong> the unit. Women could usually requestto see a doctor and sometimes staff would call one to the unit. Howwomen accessed health care <strong>in</strong>cluded:• On unit appo<strong>in</strong>tments with a GP and/or practice nurse• On site appo<strong>in</strong>tments• Well‐woman service• Leave to see GPs and/or dentists outside the site• Admission to Accident and Emergency departmentsProvision varied widely across the case study areas. A few womendescribed feel<strong>in</strong>g that their physical health needs were not takenseriously enough. In one case, a woman described be<strong>in</strong>g denied access toa GP despite subsequently be<strong>in</strong>g diagnosed as very unwell.An important consideration for staff was the relationship between selfharm,self‐harm policies <strong>in</strong> the service and the way <strong>in</strong> which physicalhealth care services could therefore be used. Restricted access was seento have resulted from ward staff sometimes see<strong>in</strong>g a woman’s requestfor medical care <strong>in</strong> relation to her self‐harm as seek<strong>in</strong>g to be looked after<strong>in</strong> a hospital environment. It was not clear if this approach was perceivedas happen<strong>in</strong>g <strong>in</strong> relation to other medical issues.“We’ve got a female GP andpractice nurse as a sharedresource but we feel weactually need our own fulltimephysical healthcarenurse. Although a lot of thenurses are dual‐qualified wewant somebody who’s notcounted <strong>in</strong> with thenumbers, who is go<strong>in</strong>g topick up on healthcareneeds.”“(The doctor) only comesonce a week and everyth<strong>in</strong>gis screened by the nursesbefore you get to see him. Ifyou have a problem, youhave to wait a week which isnot good enough. And wedon’t have access to afemale GP. When the PCTwas brought <strong>in</strong> and serviceusers had their say, we werereassured that they wouldget a female doctor andthey had female nurses. Onewoman had to have an<strong>in</strong>ternal recently and when itcame to the crunch, she hadto see a male doctor. Forsomeone who’s had issueswith men, it could be quitetraumatic”Woman service user59
Physical health was also supported by health promotion sessions and theprovision of activities. Case study services were concerned about thecomb<strong>in</strong>ation of some medications and poor diets and provided access togyms, cycl<strong>in</strong>g and <strong>in</strong> some services, a swimm<strong>in</strong>g pool, classes andnutritional advice. Women at one service compla<strong>in</strong>ed about the qualityof food they were given and as a result, they often chose to buysandwiches, crisps and other ‘fast’ foods from the café. Some women atthis service and where able to do so, elected to cook for themselves, oneof whom would also cook for others once a week. In another service,concern was shown by women and staff about women’s health. It wasnoted that approximately two thirds of women service users had a bodymass <strong>in</strong>dex (BMI) of 30 or above and were classified as obese and manywomen were considered to be at risk of coronary heart disease.5.3.5 Social <strong>life</strong> for women: community and be<strong>in</strong>g ‘ord<strong>in</strong>ary’It was artificial to draw a l<strong>in</strong>e between social and other activities as bothwomen service users and staff described the vital role of a social <strong>life</strong> <strong>in</strong>women’s recovery and for some, progress towards discharge. Socialactivities varied depend<strong>in</strong>g on the unit and the level of security requiredfor each woman.However, women frequently talked about the importance of hav<strong>in</strong>gopportunities to do what women anywhere might do <strong>in</strong>clud<strong>in</strong>g hav<strong>in</strong>g amassage or a manicure. Some services provided this on site although itwas patchy and for example, <strong>in</strong> one service where a local charity hadcome twice a month, they then ceased to provide the service. Othersaccessed hairdressers and massage off their ward but still on site. Theyhad to be eligible for leave to make use of these.A second and vital aspect of social <strong>life</strong> for most women who wereentitled to community leave was to be able to go to a café, a meal outand the c<strong>in</strong>ema. If the leave was unescorted, there were no problems.However, for women who required escorted community leave, staffwere not always available and thus leave would be cancelled. Womenwere often disappo<strong>in</strong>ted.A physical health care issue as well as a social one, some women on oneward reported that they had opportunities to <strong>in</strong>crease/ma<strong>in</strong>ta<strong>in</strong> their<strong>in</strong>dependence through self‐cater<strong>in</strong>g, purchas<strong>in</strong>g and prepar<strong>in</strong>g their ownmeals, and could access cookery sessions via the OT department ifrequired.“For some it’s extraord<strong>in</strong>aryand what may be ord<strong>in</strong>aryfor me may not be ord<strong>in</strong>aryfor somebody else likehandl<strong>in</strong>g money, order<strong>in</strong>gfood or pay<strong>in</strong>g forsometh<strong>in</strong>g.”“For people’s birthdays we’dhave a buffet. We’d get £10per week and choose whatwe wanted to do like b<strong>in</strong>goor get a DVD but theystopped do<strong>in</strong>g it. I th<strong>in</strong>k it’sbecause people weren’tbother<strong>in</strong>g to go to thecommittee.”Woman service user5.4 Service user <strong>in</strong>volvement: level and typeWomen’s <strong>in</strong>volvement <strong>in</strong> their care was an essential component of howservices delivered a dedicated service. The follow<strong>in</strong>g table shows therange of opportunities and how many services provided women with60
access to different ways of be<strong>in</strong>g <strong>in</strong>volved.Table 7: Service user <strong>in</strong>volvementRange of <strong>in</strong>volvement Independent(n=2*)NHS(n=11)Total(n=14)Patients’ council/user groups: 2 8 10ward basedPatients’ council/user groups: 2 8 10across siteParticipation <strong>in</strong> Cl<strong>in</strong>ical1 2 3Governance* no response from one service to this range of questionsThe first survey of dedicated women’s services revealed that they werelikely to have ward and site based user groups where women fed <strong>in</strong>tobroader discussions of service provision. The most usual model was for aweekly meet<strong>in</strong>g the purpose of which ranged from deal<strong>in</strong>g with practicalconcerns, e.g. repairs, to policies and at times concerns about<strong>in</strong>terpersonal issues on the ward. Some services employed service user<strong>in</strong>volvement workers to facilitate women’s participation.Beh<strong>in</strong>d these activities lay the belief that for women to be empoweredand active <strong>in</strong> their recovery, local <strong>in</strong>volvement was one means by whichthis could be achieved. For some, there was an <strong>in</strong>herent contradictionbetween the concept of empowerment and be<strong>in</strong>g <strong>in</strong> an environmentpremised on control. Others recognized that they could be empoweredthrough the mechanisms created to give them ways of contribut<strong>in</strong>g totheir own care and the quality of provision they receive.As a prelim<strong>in</strong>ary stage <strong>in</strong> the evaluation, we were <strong>in</strong>vited to attendservice user groups to discuss the project with women and receive theirfeedback on the proposed approach. These meet<strong>in</strong>gs suggested thatthere were different levels of <strong>in</strong>terest <strong>in</strong> service user <strong>in</strong>volvement andthe groups had varied levels of energy and motivation.At one service, the user group was run by the women themselvesmeet<strong>in</strong>g weekly on their ward. A number of these women were also partof a regional service user <strong>in</strong>volvement strategy group for forensicservices and participated <strong>in</strong> regional <strong>in</strong>volvement conferences as well ashav<strong>in</strong>g participated <strong>in</strong> a Women’s Involvement project which <strong>in</strong>formedthe [successful] tender for a High Support Residential Service. Therewere also opportunities to contribute to Trust‐based <strong>in</strong>volvementprojects with two of the women (who met with the evaluation team)attend<strong>in</strong>g regular user group meet<strong>in</strong>gs on the ma<strong>in</strong> hospital site.Another of the case study areas had a structure which <strong>in</strong>cluded unit orward weekly meet<strong>in</strong>gs which members of the MDT tried to attend. Inaddition, other staff, <strong>in</strong>clud<strong>in</strong>g the Facilities Manager, were <strong>in</strong>vited <strong>in</strong>order to address practical issues, e.g. the quality of meals, directly with“I don’t th<strong>in</strong>k this experiencehas empowered me. It’sprobably done the oppositeand taken away all of mycontrol. I have chosen tomake myself empowered. Icould have just sat there andsaid ‘oh, everybody tells mewhat to do’ but I have got<strong>in</strong>volved as I have alwaysbeen quite a motivatedperson.”Woman service user“It gets us together todiscuss any issues on theward, people sleep<strong>in</strong>g <strong>in</strong> theday room, the quality of <strong>life</strong>.A lot of the time I don’t th<strong>in</strong>kit has any impact at all.”Woman service user“There’s a patient rep whogoes to the Cl<strong>in</strong>ical Team61
the women. A representative from these meet<strong>in</strong>gs attended thewomen’s service user group facilitated by a member of staff. From thisgroup, there were representatives on a hospital‐wide group.Did women feel that service user <strong>in</strong>volvement was more than tokenisticand provided an effective means of <strong>in</strong>teract<strong>in</strong>g with the service? In onearea, <strong>in</strong> addition to ward and service meet<strong>in</strong>gs, satisfaction surveys wereused to elicit women’s views. Women had contributed to the design ofthe survey and suggested that this was a useful mechanism for userfeedback.They had been kept <strong>in</strong>formed about the f<strong>in</strong>d<strong>in</strong>gs and onewoman believed that the service had acted on the basis of these. Fromthe <strong>in</strong>terviews we carried out, these views ranged from th<strong>in</strong>k<strong>in</strong>g thatthey were listened to and the groups worked reasonably well to concernthat user‐<strong>in</strong>volvement did not always result <strong>in</strong> action.Women were encouraged to become actively <strong>in</strong>volved but some werenot motivated to do so. Sometimes this was attributed to not be<strong>in</strong>g wellenough. Sometimes, women were perceived as just not car<strong>in</strong>g about thebroader aspects of service provision. In one area, a programme of socialevents ceased as the result of women not attend<strong>in</strong>g a sub‐groupmeet<strong>in</strong>g. This was reactivated as a result of discussion <strong>in</strong> the communitymeet<strong>in</strong>g.meet<strong>in</strong>g. I don’t th<strong>in</strong>k theywork well. It’s an example ofthe dynamic <strong>in</strong> a secure unitplus the more mundaneth<strong>in</strong>g that wheels turnslowly <strong>in</strong> organisations. Ifyou don’t get a ‘yes’immediately, there’s a groupthat f<strong>in</strong>d it hard to toleratewait<strong>in</strong>g.”“I th<strong>in</strong>k that th<strong>in</strong>gs arelistened to but they are notalways followed through.Unless you take th<strong>in</strong>gs to amanager or one of the wardreps, you don’t really have avoice.”Woman service userIssues:• The physical environment was important to women and staff. Whilst new build<strong>in</strong>gs were off‐putt<strong>in</strong>gto some <strong>in</strong>itially, most women appreciated efforts made to make the unit look and feel homely.Some would have liked more say <strong>in</strong> design and décor.• Most services were concerned that women found ways of talk<strong>in</strong>g about their traumatic experiencesdespite contradictory views about the type of psychological therapy to provide and when it shouldbe offered.• Women and staff recognized the value of ‘<strong>in</strong>formal’ activities. Women wanted to do what was‘ord<strong>in</strong>ary’. Some staff and other professionals saw this as hav<strong>in</strong>g a therapeutic potential <strong>in</strong> the sameway that more formal <strong>in</strong>terventions were <strong>in</strong>tended to have.• Access to sufficient and appropriate physical healthcare was not always provided and women serviceusers were particularly concerned that their needs were not be<strong>in</strong>g met <strong>in</strong> relation to see<strong>in</strong>g a GP orother doctors.62
6. <strong>My</strong> <strong>life</strong>: <strong>in</strong> my <strong>hands</strong>? Care Pathways, Care Plann<strong>in</strong>g and dischargeI’ve got to th<strong>in</strong>k that <strong>in</strong> the long run they only want what’s best for me but I need people on my teamwho I can trust. I do trust the staff, don’t get me wrong, but there’s some I wouldn’t talk to because oftheir attitude. The people on my team, I get on well with. I’d been th<strong>in</strong>k<strong>in</strong>g to change my carecoord<strong>in</strong>ator because I wasn’t happy with the care I was gett<strong>in</strong>g. It was brought up <strong>in</strong> the ward round thatI didn’t get on with my care coord<strong>in</strong>ator so it happened and I got someone I wanted.Woman service user‘An <strong>in</strong>tegrated care pathway (ICP)• is a multidiscipl<strong>in</strong>ary outl<strong>in</strong>e of anticipated care, placed <strong>in</strong> an appropriate timeframe, to help a patientwith a specific condition or set of symptoms move progressively through a cl<strong>in</strong>ical experience topositive outcomes• ICPs are important because they help to reduce unnecessary variations <strong>in</strong> patient care and outcomes.• They support the development of care partnerships and empower patients and their carers and• ICPs can also be used as a tool to <strong>in</strong>corporate local and national guidel<strong>in</strong>es <strong>in</strong>to everyday practice,manage cl<strong>in</strong>ical risk and meet the requirements of cl<strong>in</strong>ical governance.’ 78The Care Programme Approach (CPA) def<strong>in</strong>es the overarch<strong>in</strong>g framework for the provision of mentalhealth, <strong>in</strong>clud<strong>in</strong>g secure, services. Most recently reviewed <strong>in</strong> 2008, the CPA has four ma<strong>in</strong> elements asdef<strong>in</strong>ed <strong>in</strong> ‘Build<strong>in</strong>g Bridges: A guide to arrangements for <strong>in</strong>ter–agency work<strong>in</strong>g for the care andprotection of severely mentally ill people’ 79 which states that there are four dist<strong>in</strong>ct aspects to the CPA:Assessment:A Care Plan:A Key Worker:Regular Review:systematic arrangements for assess<strong>in</strong>g the health and social needs of peopleaccepted by the specialist mental health services;the formation of a Care Plan which addresses the identified health and socialcare needs;the appo<strong>in</strong>tment of a Care Coord<strong>in</strong>ator to keep <strong>in</strong> close touch with the patientand monitor care; andregular review, and if need be, agreed changes to the Care Plan.These four pr<strong>in</strong>ciples of assessment, Care Plan, Care Coord<strong>in</strong>ation and review are the cornerstones of theCare Programme Approach. Implicit <strong>in</strong> all of them is <strong>in</strong>volvement of the person us<strong>in</strong>g the service, and,where appropriate, their carer.Ma<strong>in</strong>stream<strong>in</strong>g Gender <strong>in</strong> Women’s Mental <strong>Health</strong> 80 states that:• assessment should <strong>in</strong>form a formal Care Plann<strong>in</strong>g process under CPA;• it should be multi‐discipl<strong>in</strong>ary, holistic and comprehensive <strong>in</strong>clud<strong>in</strong>g violence and abuse, self‐harm,substance misuse, eat<strong>in</strong>g disorders, sexuality and gender sensitive assessment of risk;• it will need to take place <strong>in</strong> a variety of sett<strong>in</strong>gs <strong>in</strong>clud<strong>in</strong>g the community, family and residentialhomes, and distant secure placements <strong>in</strong>clud<strong>in</strong>g prisons, high secure hospitals and the <strong>in</strong>dependentsector; and• l<strong>in</strong>ks with local court/police diversion and liaison services should be explicitly agreed.63
This section of the report exam<strong>in</strong>es Care Pathways and Care Plann<strong>in</strong>g as experienced by women and staff.Some of the case study services reported considerable improvement <strong>in</strong> the last few years mov<strong>in</strong>g from,for example, treatment and care plans that were not sufficiently needs‐led to new CPA documentationand needs‐based care plans.The evaluation showed that while <strong>in</strong> theory women’s services had similar policies, <strong>in</strong> practice theirimplementation varied considerably. Indeed, with<strong>in</strong> a s<strong>in</strong>gle service, practice was sometimes dependenton the RMO/RCO <strong>in</strong>volved <strong>in</strong> a woman’s care rather than as agreed across the service. Systematic use ofdocumentation processes and computerised record keep<strong>in</strong>g played a significant part <strong>in</strong> ensur<strong>in</strong>g morerigorous and transparent procedures. Nevertheless, realistically the key factor <strong>in</strong> successful Care Plann<strong>in</strong>glay <strong>in</strong> the relationships between a woman and her care coord<strong>in</strong>ator and team.6.1 Care PathwaysIn section 3.1, we described how women and service providers wantedto work towards a ‘seamless’ pathway through and hopefully out ofsecure sett<strong>in</strong>gs. The Care Pathway ideally acts as a road map for the<strong>in</strong>dividual. However, as the follow<strong>in</strong>g three examples illustrate (not theirreal names), <strong>in</strong> reality the Pathway was neither seamless nor withoutsome twists and turns en route. What is strik<strong>in</strong>g for these women is thatit was the move to their current sett<strong>in</strong>g that activated the process.Alice’s Care Pathway:Now 24, Alice was just twenty when she committed her <strong>in</strong>dex offence. Shehad a history of physical and sexual abuse dur<strong>in</strong>g her childhood and at thetime of the offence she was us<strong>in</strong>g illicit drugs and dr<strong>in</strong>k<strong>in</strong>g heavily, and allthis had impacted severely on her mental health. She was <strong>in</strong>itiallyremanded to prison where she spent about six months wait<strong>in</strong>g for her trialto come up at the Crown Court. Whilst on remand she received no help forher drug and alcohol problem and her mental health deteriorated yetfurther, lead<strong>in</strong>g to her be<strong>in</strong>g transferred from prison to an <strong>in</strong>dependentmedium secure hospital for assessment under the Mental <strong>Health</strong> Act.When her case came up <strong>in</strong> court she was given a restricted hospital order(Mental <strong>Health</strong> Act S.37/41) and returned to the same <strong>in</strong>dependentmedium secure unit as, at the time, there were no beds available <strong>in</strong> theNHS medium secure women’s service <strong>in</strong> her area. She spent about twoyears <strong>in</strong> this <strong>in</strong>dependent hospital, dur<strong>in</strong>g which time Alice felt there waslittle or no proper support available to help her get well or overcome hersubstance misuse problems. She feels it was not until about three and ahalf years after she committed her offence, when she was transferred tothe unit where she is now (an NHS medium secure women’s service), thatshe was able to access the help she required to get her <strong>life</strong> back on track.After spend<strong>in</strong>g about a year on the unit, with the help of the psychologistand nurse therapists specialis<strong>in</strong>g <strong>in</strong> help<strong>in</strong>g women who are surviv<strong>in</strong>gchildhood trauma and abuse (<strong>in</strong>clud<strong>in</strong>g child sexual abuse) and with drugand/or alcohol problems, she is now ready to transfer to a low secureservice nearer to her home area. She is look<strong>in</strong>g forward to mov<strong>in</strong>g <strong>in</strong> twoweeks time.64
Barbara’s Care Pathway:Barbara is <strong>in</strong> her early forties and has been diagnosed with schizophrenias<strong>in</strong>ce she was <strong>in</strong> her mid‐twenties. Follow<strong>in</strong>g her <strong>in</strong>dex offence, despitehav<strong>in</strong>g a long history of mental Illness and previous formal admissions tohospital, she was remanded <strong>in</strong>to prison custody for ten months before hercase went to trial. Dur<strong>in</strong>g this period on remand she received little <strong>in</strong> the wayof care or treatment for her mental illness. When her case was eventuallyheard <strong>in</strong> the Crown Court she was given a restricted hospital order (MHAS.37/41) but, due to no beds be<strong>in</strong>g available <strong>in</strong> the local NHS Medium SecureUnit (MSU), she was sent out of area to an <strong>in</strong>dependent medium securehospital for three months whilst wait<strong>in</strong>g for an NHS medium secure bed tobecome available. Once admitted to the NHS secure unit she started to seea psychologist regularly to explore issues to do with her offence, and alsolearned a lot about her illness and how to manage it better and preventrelapse dur<strong>in</strong>g one to one sessions with her named nurse. After about eightmonths on the admissions/acute ward she was transferred to a rehabilitationward where she has been mak<strong>in</strong>g good progress for the past three months.Her consultant has recently written to the M<strong>in</strong>istry of Justice Mental <strong>Health</strong>Unit to request leave for her to attend a course at the local college one dayper week. She is hop<strong>in</strong>g that it won’t be too long now before she moves to ahostel or supported accommodation <strong>in</strong> the community.Carol<strong>in</strong>e’s Care Pathway:Carol<strong>in</strong>e has learn<strong>in</strong>g disabilities and spent most of her childhood years <strong>in</strong>care. She is now <strong>in</strong> her early thirties but has been <strong>in</strong> hospital s<strong>in</strong>ce she was ateenager. After her <strong>in</strong>dex offence she was <strong>in</strong>itially remanded to prison, butwas given a Hospital Order (MHA S.37/41) by the Crown Court and sent to ahigh security hospital where she spent n<strong>in</strong>e years. About seven years agoshe was transferred from high security care to a learn<strong>in</strong>g disability mediumsecure ward <strong>in</strong> an <strong>in</strong>dependent hospital. In this service, as well as medication,which is what Carol<strong>in</strong>e believes helps her most, she has also been see<strong>in</strong>g apsychologist who has supported her to develop cop<strong>in</strong>g strategies around herself‐<strong>in</strong>jury. She also attends an anger management group run by thepsychology department. She is look<strong>in</strong>g forward to be<strong>in</strong>g transferred to thelow secure service at the same hospital with<strong>in</strong> the next few months, and fromthere it is planned she moves back to her home area to a new purpose‐builtunit which will provide cont<strong>in</strong>u<strong>in</strong>g care for women with learn<strong>in</strong>g disabilities.6.2 Involv<strong>in</strong>g women <strong>in</strong> the processMost services respond<strong>in</strong>g to the survey said that all women attendedCPA review meet<strong>in</strong>gs. However, <strong>in</strong> over half of these the <strong>in</strong>vitation wasextended to only part of this discussion. Staff said they tried toencourage women to be <strong>in</strong>volved <strong>in</strong> the process as a whole which<strong>in</strong>cluded:“They don’t attend themeet<strong>in</strong>gs but they areallowed to come at the end.What happens at themoment is all theprofessionals sit and read65
• Ensur<strong>in</strong>g all women have a named nurse• Involv<strong>in</strong>g women <strong>in</strong> plann<strong>in</strong>g for the CPA meet<strong>in</strong>g• Us<strong>in</strong>g self‐assessment forms and/or contributions to written reports• Offer<strong>in</strong>g opportunities for advocates, friends and family to attendthe CPA meet<strong>in</strong>g with the women concerned.In addition, some services described specific <strong>in</strong>itiatives to promote<strong>in</strong>volvement. Examples of these <strong>in</strong>cluded women be<strong>in</strong>g part ofdevelop<strong>in</strong>g a pro‐forma to be used for their feedback to the CPAmeet<strong>in</strong>g; active service user groups; and <strong>in</strong> one case, call<strong>in</strong>g the plan a‘recovery plan’ with women able to direct the content. Most servicessaid they encouraged women to submit their own reports to the CPAmeet<strong>in</strong>g.In the case study areas, Care Plann<strong>in</strong>g tended to use an <strong>in</strong>dividual caseformulation approach <strong>in</strong>formed by gender and other diversity issues.Multi‐discipl<strong>in</strong>ary teams made conscious efforts not to be diagnosis‐led<strong>in</strong> the way they responded to women’s needs look<strong>in</strong>g beyond a narrowmedical with<strong>in</strong> the context of a wider social model, thus avoid<strong>in</strong>greplication of traditional divisions between mental illness and personalitydisorder. The Plans either conta<strong>in</strong>ed all areas to be covered or separatePlans were prepared for different aspects of a woman’s situation, e.g.one for plann<strong>in</strong>g home visits and another for eat<strong>in</strong>g disorders.the reports and havediscussions and then thewomen are <strong>in</strong>vited so theyaren’t really <strong>in</strong>volved to mym<strong>in</strong>d. I try and work asmuch as I can by shar<strong>in</strong>g myunderstand<strong>in</strong>g with thewomen and putt<strong>in</strong>gtogether a picture of why Ith<strong>in</strong>k th<strong>in</strong>gs have gonewrong for them with them. Idon’t th<strong>in</strong>k that this is doneenough and I th<strong>in</strong>k it’s a realfailure that we don’t <strong>in</strong>cludethe women from the veryoutset. There is noownership of their recovery,there’s no <strong>in</strong>volvement <strong>in</strong>this is what I need to do, or Iunderstand what I need todo or I completely agreewith what I need to do, theyhave it imposed on them.”Case example:At this service, full CPA reviews were scheduled on a three‐monthly basiswith the women <strong>in</strong>vited to attend, although sometimes they were onlyasked to come <strong>in</strong> at the end of the meet<strong>in</strong>g, once the reports had beendiscussed and decisions made. One women said “[I am] not <strong>in</strong>volved <strong>in</strong> thediscussion, but called <strong>in</strong> at the end to be told what was decided”. Therewere <strong>in</strong>tegrated CPA reports with separate sections completed by differentmembers of the multi‐discipl<strong>in</strong>ary team, e.g. medical, nurs<strong>in</strong>g, OT,psychology, social work, and also a form completed by the women giv<strong>in</strong>gtheir views on their current mental health, their treatment and their goalsfor the next three months and a year ahead. The primary nurs<strong>in</strong>g reportalso <strong>in</strong>cluded a section about service user views and/or requests. TheOccupational Therapy reports were based on an <strong>in</strong>terview with the serviceuser, review<strong>in</strong>g their Care Plan and their goals. However, women told usthey did not always get the opportunity to see the <strong>in</strong>tegrated reports priorto their review meet<strong>in</strong>g which had impacted negatively on their ability to beproperly <strong>in</strong>volved <strong>in</strong> any discussions or <strong>in</strong>deed challenge any of the contentof the reports, which they felt did not always reflect their perspective. Onewoman said she did not attend reviews although she was <strong>in</strong>vited, as she feltthere would be no po<strong>in</strong>t. As a sentenced prisoner on a Restricted Order,any major decisions about her future were made outside of the CPAprocess with the M<strong>in</strong>istry of Justice hav<strong>in</strong>g to give approval for access andtransfers.“The women aren’t as<strong>in</strong>volved as they could be ‐<strong>in</strong> terms of decisions thatare made by the Cl<strong>in</strong>icalTeam just tend to be with<strong>in</strong>the medical model, it doesk<strong>in</strong>d of impact a lot and stillrema<strong>in</strong>s with us despiteattempts to make it moremixed and psychological.”“Care Plann<strong>in</strong>g with thewomen I would say we aregett<strong>in</strong>g there. We probablydo more on the women’sservice than we do on themale service. I would saythat is partly because the66
In between the three‐monthly reviews, the Cl<strong>in</strong>ical Team met on a weeklybasis to review each woman’s Care Plan and progress. These meet<strong>in</strong>gs werefor care team members only with women not attend<strong>in</strong>g or <strong>in</strong>vited to takepart. However, the women were aware of when their Cl<strong>in</strong>ical Team wasmeet<strong>in</strong>g and were encouraged to put any requests, for example for changesto supervision levels, access or visits, to the meet<strong>in</strong>g via their primarynurse, who gave them feedback about any discussions or decisions maderegard<strong>in</strong>g their Care Plan.A number of staff echoed a service user’s view that more could be done to<strong>in</strong>volve the women from the outset <strong>in</strong> the CPA review process so theirviews and experiences could better <strong>in</strong>form decisions about their Care Plan.Some staff also felt decisions made with<strong>in</strong> the CPA process needed to be<strong>in</strong>formed by a more holistic perspective <strong>in</strong>clud<strong>in</strong>g social and psychologicalformulations of women’s needs which take <strong>in</strong>to account the woman’s <strong>life</strong>experiences rather than so much emphasis be<strong>in</strong>g placed on medicaldiagnoses <strong>in</strong> determ<strong>in</strong><strong>in</strong>g appropriate goals and treatment plans.There was evidence that the CPA process did take <strong>in</strong>to account women’spast experiences of abuse, with appropriate treatment <strong>in</strong>terventions madeavailable and generally staff appeared to have good awareness of how suchexperiences might impact on a woman’s mental health and herrelationships and attachments to others <strong>in</strong>clud<strong>in</strong>g members of her careteam. However, a m<strong>in</strong>ority of staff felt there was not enough awareness ofhow vulnerable women impacted on each other on the ward. They believedwomen could often be re‐traumatized by the distress or aggressivebehaviours of other “frightened or frighten<strong>in</strong>g” women on the ward, andthat Care Plans should take better account of what staff <strong>in</strong>terventions arerequired to support peer relationships and <strong>in</strong>teraction on the ward.Case example:One of the case study areas brought together <strong>in</strong> one document its policiesas they perta<strong>in</strong>ed to the whole women’s service. With<strong>in</strong> this, the section onCare Plann<strong>in</strong>g provided a detailed and clear description of how the processshould take place (<strong>in</strong>clud<strong>in</strong>g approach, associated activities and examples ofcontent) and how it related to the CPA and risk assessments for <strong>in</strong>dividualwomen.All women were allocated a care coord<strong>in</strong>ator on arrival at the unit as well asa named associate nurse and two further named staff (often <strong>Health</strong> CareAssistants (HCAs)) to ensure that <strong>in</strong> the absence of the care coord<strong>in</strong>ator,there was always someone to turn to who had a specific <strong>in</strong>terest <strong>in</strong> them.Representatives from external agencies as appropriate would be agreed atthis po<strong>in</strong>t. An <strong>in</strong>itial Care Plan was drawn up focus<strong>in</strong>g on areas from mentalhealth needs to budget<strong>in</strong>g and day‐to‐day self care. The Care Plan was seento be an all encompass<strong>in</strong>g document which noted the different andimportant aspects of the woman’s experience at the unit. Staff said thatCare Plans took <strong>in</strong>to account women’s often difficult histories <strong>in</strong> order tohelp determ<strong>in</strong>e the types of activities and <strong>in</strong>terventions which would beagreed. For example, a woman who had been sexually abused by a malewomen expect/demand itand you couldn’t get awaywith not do<strong>in</strong>g it which Ith<strong>in</strong>k is great that they setthose standards for us tofollow and also because werecognise that we need that.We need their <strong>in</strong>volvementand co‐operation.”“I th<strong>in</strong>k we are quite good atthe CPA framework andorganisation andconsistency and mak<strong>in</strong>g surethat we don’t miss outattention to differentaspects of care andtreatment and that there isgood communication. A lotof that is due to our goodcomputer system, but yes Ith<strong>in</strong>k it’s quite good really.We have a fullmultidiscipl<strong>in</strong>ary team withsome very skilledprofessionals and I th<strong>in</strong>k it isan open culture heregenerally speak<strong>in</strong>g and Idon’t th<strong>in</strong>k there is a fear ofpeople speak<strong>in</strong>g up orvoic<strong>in</strong>g concerns.”“Sometimes people canmisconstrue what you say.You can say someth<strong>in</strong>g andthree different people hearthree different th<strong>in</strong>gs andthen it gets written <strong>in</strong> yournotes and it’s not correct orit’s not what you <strong>in</strong>tended itto be. I feel it’s the youngerless‐experienced staff thattake it the wrong way andthey’ll happily start writ<strong>in</strong>gloads of stuff that’s not trueor is <strong>in</strong>correct.”Woman service user67
therapist <strong>in</strong> another service was allocated a male therapist at the newservice. The Care Plann<strong>in</strong>g process helped to identify the issue and toensure that this woman was reallocated to a female therapist.Care programme update meet<strong>in</strong>gs took place either weekly or at leastevery two weeks and staff said women had an opportunity to <strong>in</strong>put there.After an <strong>in</strong>itial CPA meet<strong>in</strong>g at three months, subsequent meet<strong>in</strong>gs wereheld on a six‐monthly basis. A patient self‐report provided an opportunityfor women to reflect on their progress and aspirations and they were ableto read staff reports <strong>in</strong> advance of the CPA meet<strong>in</strong>gs. Women wereencouraged to attend the whole meet<strong>in</strong>g and to br<strong>in</strong>g advocates (whereavailable as they did not always have time), family or friends.Women <strong>in</strong>terviewed at this service had a clear sense of the Care Plann<strong>in</strong>gprocess and the role of the care coord<strong>in</strong>ator. However, they held differentviews about how well the process worked for them. For example, onewoman described <strong>in</strong> detail all the people <strong>in</strong>volved <strong>in</strong> her team, their rolesand how, when she felt changes were needed, she was able to articulatethis successfully. Conversely, a second woman expressed concern thatmembers of her team recorded <strong>in</strong>formation about her <strong>in</strong> ways that wereeither open to <strong>in</strong>terpretation or would be mislead<strong>in</strong>g to others <strong>in</strong>volved <strong>in</strong>the CPA and Care Plann<strong>in</strong>g. She knew she could read the documents, notesand reports but this would only be after vett<strong>in</strong>g by staff thus mak<strong>in</strong>g it, <strong>in</strong>her view, a po<strong>in</strong>tless exercise. This woman attended the CPA meet<strong>in</strong>g andrema<strong>in</strong>ed concerned that, thanks to the reports, misunderstand<strong>in</strong>gpersisted yet she did not want to have to keep expla<strong>in</strong><strong>in</strong>g herself.“Women are very <strong>in</strong>volved <strong>in</strong>their care plans. Some don’tagree if they feel th<strong>in</strong>gs aretoo prescriptive but we canwork round that andchange. Often it’s aboutchang<strong>in</strong>g the term<strong>in</strong>ology, ‘Idon’t like the way you’vewritten that, I’m neveraggressive. Just because Ishout …’ and it’s okay. So it’sth<strong>in</strong>k<strong>in</strong>g about how we uselanguage and just be<strong>in</strong>g abit more flexible.”Many of the women here wanted more frequent contact with their RMO aspart of their Care Plann<strong>in</strong>g and review.Another of the case study areas had <strong>in</strong>troduced a system wherebywomen provided written feedback to weekly ward rounds and a keyconcern for women from several case study services was that theprocess of staff record<strong>in</strong>g of observations and reflections <strong>in</strong> their formaldocumentation was open to <strong>in</strong>terpretation. Not all the women whoraised this had looked at the reports themselves. However, dur<strong>in</strong>g CPAmeet<strong>in</strong>gs, some had challenged the content of these reports. Aware ofthese concerns, one service had worked with staff on their report<strong>in</strong>g andwrit<strong>in</strong>g skills to ensure a non‐judgmental and accurate approach whenadd<strong>in</strong>g to case notes, Care Plans and thus reports for the CPA.Views varied across the staff/multi‐discipl<strong>in</strong>ary teams about the currentlevel of <strong>in</strong>volvement of women and <strong>in</strong>deed the extent to which such<strong>in</strong>volvement should be encouraged. In one service, women said theyeither had no Care Plan or if they did, had not been <strong>in</strong>volved <strong>in</strong> itsdevelopment. There was a high level of <strong>in</strong>consistency here that somewomen attributed to <strong>in</strong>dividual staff and whether or not they did thePlan.68
Interest<strong>in</strong>gly, while some staff argued that women should have an<strong>in</strong>creased level of <strong>in</strong>put to the CPA process, most women themselvessaid they were happy with their level of <strong>in</strong>volvement <strong>in</strong> the CPA processand all appeared to have an awareness of how the CPA review processworked and who acted as their Care Coord<strong>in</strong>ator. The women alsoreported they felt their views were taken <strong>in</strong>to account and that, whereappropriate, their needs relat<strong>in</strong>g to issues such as past abuse, self‐harmand family contact were taken <strong>in</strong>to account with<strong>in</strong> their Care Plans.6.3 The CPA Meet<strong>in</strong>gsThe CPA meet<strong>in</strong>gs usually drew together the professionals <strong>in</strong>volved <strong>in</strong>the delivery of care for an <strong>in</strong>dividual woman. These <strong>in</strong>cluded <strong>in</strong>‐servicestaff, sometimes service commissioners, external agencies, e.g. from awomen’s local area, and representation from the M<strong>in</strong>istry of Justicewhere appropriate. The purpose of the meet<strong>in</strong>gs was to review progressand plan for a woman’s future based on their and the woman’s ownreports.Women’s experience of and attitudes to the CPA meet<strong>in</strong>gs varied acrossand sometimes with<strong>in</strong> services. The <strong>in</strong>terviews with women suggestedthat some were more motivated to believe that the CPA meet<strong>in</strong>g couldaddress their concerns and enable their progress.The practice of attendance also varied and a small number of womensaid very clearly that they did not want to be there throughout. Theypreferred the discussion to take place amongst professionals who wouldthen relay their decisions and women could comment on them. Otherswanted the choice of how they participated and the flexibility to attendthe whole meet<strong>in</strong>g one time but not another. Staff, even <strong>in</strong> the sameservice, had different views on this too.Whilst some professionals felt women were adequately <strong>in</strong>volved, manyargued that decisions were made without the proper <strong>in</strong>volvement of thewoman concerned. They reported that often women would only be<strong>in</strong>vited <strong>in</strong>to their CPA review after the professionals had alreadydiscussed their case and made decisions, <strong>in</strong> order to be told about whathad already been decided. Some staff felt it would be preferable forwomen to be <strong>in</strong>vited <strong>in</strong>to CPA reviews at the start of their meet<strong>in</strong>g sothey could put their views and requests for any changes to the Care Planand then leave. The multi‐discipl<strong>in</strong>ary team could then have a frankdiscussion, without the women be<strong>in</strong>g present, but at least it would be<strong>in</strong>formed by the women’s views. The women could be then told aboutthe decisions made after the meet<strong>in</strong>g.Women sometimes had access to an advocate from WISH or M<strong>in</strong>d, forexample, to support them dur<strong>in</strong>g their CPA review meet<strong>in</strong>g. In one case“They said I was gett<strong>in</strong>g abit high but I was try<strong>in</strong>g toput my po<strong>in</strong>t across. Youneed time to expla<strong>in</strong> but it’sa rushed approach asthey’re wait<strong>in</strong>g for the nextperson.”Woman service user“I th<strong>in</strong>k <strong>in</strong> the ma<strong>in</strong>, we do<strong>in</strong>volve <strong>in</strong>dividual women. Ith<strong>in</strong>k it is simply impossibleto do it <strong>in</strong> the same way thatyou could <strong>in</strong> a non‐secureservice, I don’t th<strong>in</strong>k that isan ideal that one shouldeven strive for personally.Women are welcome andencouraged to attend butfrom my own experience Iam not comfortable withtalk<strong>in</strong>g about the women’scare and treatmentcompletely frankly with theMD team whilst the womanis there listen<strong>in</strong>g to it, or allof it.”“The one th<strong>in</strong>g I have beendisappo<strong>in</strong>ted with is thatwomen do not attend thewhole of the meet<strong>in</strong>g, theyare <strong>in</strong>vited <strong>in</strong> only half waythrough and towards theend almost just to hear thef<strong>in</strong>al summ<strong>in</strong>g up wheredecisions are expla<strong>in</strong>edrather than a consensusbe<strong>in</strong>g arrived at.”69
study area, the advocate had started to help women prepare a writtensheet for their meet<strong>in</strong>g list<strong>in</strong>g the issues they wanted to discuss and anyrequests they wished to make. Three of the women <strong>in</strong>terviewed abouttheir experiences of and <strong>in</strong>volvement <strong>in</strong> the CPA process were supportedby a WISH advocate to prepare for and dur<strong>in</strong>g review meet<strong>in</strong>gs, withthese women all say<strong>in</strong>g this support was helpful and important to them.Of the two women not access<strong>in</strong>g advocacy support one felt she did notneed any support to put her own views forward and the other wassupported by a family member. Advocates themselves noted that theycould not always attend each woman’s CPA meet<strong>in</strong>g given their limitedresources.6.4 CPA documentsAs part of the evaluation, we reviewed CPA documents for 20 womenacross four case study services. Albeit a very small number, the reportsrevealed the follow<strong>in</strong>g;• In all four sites, <strong>in</strong>tegrated CPA report<strong>in</strong>g had been implemented,with different members of MDT enter<strong>in</strong>g their reports directly on toone form on the system.• There was no clear evidence that the impact of gender was be<strong>in</strong>gconsidered <strong>in</strong> the case formulation as documented <strong>in</strong> the report. Thiswas found <strong>in</strong> less than a quarter of cases, although there was someevidence <strong>in</strong> a further seven and no evidence <strong>in</strong> nearly half (n<strong>in</strong>e).• In just six cases were women's experiences of abuse addressed <strong>in</strong> theCare Plan, but while specific therapeutic <strong>in</strong>terventions were plannedfor the women, scant reference was made to how their experiencesmay impact on <strong>in</strong>terpersonal relationships and trust <strong>in</strong> the unit(<strong>in</strong>clud<strong>in</strong>g with staff) and how this should be supported. Thepotential for further victimisation or retraumatisation was rarelyaddressed. There was some evidence that Care Plann<strong>in</strong>g took this<strong>in</strong>to account but not across all services and for all women where thishad been identified as an issue.• Record<strong>in</strong>g user views <strong>in</strong> the actual report varied across case studyareas. In one, this was always carried out but across three areas, thiswas the case <strong>in</strong> just five of 11 reports.“I haven’t had anyone sit medown and write a care plans<strong>in</strong>ce I’ve been on this wardand I have been here twomonths. <strong>My</strong> understand<strong>in</strong>gis that they are supposed tosit down with you and drawit up. I don’t like my primarynurse who dilly‐dalliesaround. I’ve asked him todraw me up a care plan buthe doesn’t.”Woman service userClearly there was considerable variation across the case study areas andsometimes with<strong>in</strong> one service. This lack of consistency was reflected bywomen some of whom said that they did not know who their CareCoord<strong>in</strong>ator was nor did they feel they had been sufficiently consultedabout the content of their Care Plann<strong>in</strong>g.6.5 Risk assessment70
Risk assessments provided an essential underp<strong>in</strong>n<strong>in</strong>g to women’s <strong>safe</strong>tyand to the <strong>safe</strong>ty of staff. L<strong>in</strong>ked to the CPA, we asked if women were<strong>in</strong>volved <strong>in</strong> their risk assessment process. One service said they were notand only one said that it depended on their capability at the time.Women were also much less likely to be asked to sign the completed riskassessment documents. Services were also unlikely to have any genderspecific risk assessment procedures. Of the five respond<strong>in</strong>g to the surveythat did, one said this was with specific reference to unescorted groundleave and the risks of mix<strong>in</strong>g with male patients.A few women were concerned that, through lack of consultation, theirbehaviour was misrepresented <strong>in</strong> case files and risk assessments.Only two services had a forensic community team for women whichlooked at risk <strong>in</strong> the context of mov<strong>in</strong>g on from secure services. In onecase, this was the cl<strong>in</strong>ical team which carried a community caseload. Inthe other, the team was composed of psychiatry, psychology, nurs<strong>in</strong>gand social work plus a support worker. They said they worked with arange of services <strong>in</strong>clud<strong>in</strong>g courts, prisons, adult mental health units,CAMHS units and learn<strong>in</strong>g disability services.Six services (four NHS and two <strong>in</strong>dependent) offered a risk assessedcommunity <strong>in</strong>clusion programme to women. These were described as:• Individual programmes of access to the community• Programmes completed by MDT• Assessment of risk when go<strong>in</strong>g to day services, social services andother agencies• Women’s mental health development group is <strong>in</strong>volved• Programme of community leave, work experience and opportunitiesSome services took a risk assessment and management approachsensitive to work<strong>in</strong>g with women who were survivors of violence orabuse. In one case study area, staff described if a women escalated orbecame distressed there was a will<strong>in</strong>gness to step back and not to go <strong>in</strong>and put <strong>hands</strong> on but to recognize the re‐enactment of trauma. It wasfelt that sometimes this women’s service was criticized by the widerservice due to a lack of understand<strong>in</strong>g of this aspect of the model, andstaff work<strong>in</strong>g <strong>in</strong> other parts of the site sometimes thought they just letthe women get away with too much rather than see<strong>in</strong>g it as a clear partof a model of care and implement<strong>in</strong>g more appropriate ways to managerisks <strong>in</strong> that situation.6.6 Mov<strong>in</strong>g on: the f<strong>in</strong>al stepsThis evaluation has highlighted ways <strong>in</strong> which the expansion of dedicatedmedium secure provision for women has significantly improved thesituation of many and <strong>in</strong>creased women’s chances of lead<strong>in</strong>g lives which71
allowed them to make more of, if not fulfill, their potential. The <strong>in</strong>crease<strong>in</strong> bed spaces has resulted <strong>in</strong> mov<strong>in</strong>g most women from high securesett<strong>in</strong>gs and provided an alternative to custodial sentences for some. Atthe same time, putt<strong>in</strong>g <strong>in</strong>to practice the philosophy which underp<strong>in</strong>spolicies for women has identified a significant issue <strong>in</strong> terms ofthroughput and achiev<strong>in</strong>g an agreed care pathway. Many services hadlittle access to either low secure or community‐based <strong>in</strong>dependent liv<strong>in</strong>goptions which were appropriate for this group of women. While somewomen cont<strong>in</strong>ued to need medium secure care, many others did not.Where do they go next?Here we describe what was available as well as exam<strong>in</strong>e the barriers tomove‐on which prevented some women from tak<strong>in</strong>g that f<strong>in</strong>al step to<strong>in</strong>dependence.The first survey for this evaluation revealed that that services rarely hadvacancies and noted low numbers of transfers or discharges. Overalldur<strong>in</strong>g a one year period and across all wards, 49 of 188 women weretransferred or discharged as follows:Discharged to community sett<strong>in</strong>g 10Transferred to lower secure 20Transferred to another MSU 16Transferred back to prison 2Of 21 wards, n<strong>in</strong>e made no transfers or discharges of which three wardsfor women with learn<strong>in</strong>g disabilities said that patient movement wasalmost nil. Average lengths of stay varied considerably from four monthsto several years although, as noted by one service, this ranged from sixmonths to 12 years on one ward. Length of stay did not appear to berelated to discharge.Women service users and professionals agreed that a major barrier towomen’s recovery and discharge was the lack of appropriate move‐onservices. In January 2009, only 12 of the 27 services provided arehabilitation ward and just over half (14) had access to low secureservices. The open<strong>in</strong>g of four pilot community therapeutic residentialservices for women with complex needs adds a further range ofprovision.One of the case study areas had established a step‐down facility forwomen leav<strong>in</strong>g medium secure care and the community forensic team tosupport women mov<strong>in</strong>g <strong>in</strong>to the community who require ongo<strong>in</strong>gsupervision from a specialist forensic service. There was also evidence ofthe team work<strong>in</strong>g with wider community services to help <strong>in</strong>crease theirunderstand<strong>in</strong>g of gender sensitive provision so they are better able tosupport women leav<strong>in</strong>g the service.“All the work I’ve done andthey say ‘don’t run beforeyou can walk’ and ‘how longis a piece of str<strong>in</strong>g’. I’ve justcome a long way, I’m at theend of the tunnel now andit’s true though, there islight, there is light!”Woman service user“I talk to the psychiatristabout my overnight leavesand how it went. She said Ishould get a conditionaldischarge. I’m hop<strong>in</strong>g theHome Office will come to myCPA. They were meant tocome but they didn’t turn upso hopefully they’ll comethis time. (Where go<strong>in</strong>g to)the staff stay at the house,they’re very supportive aswell and nice, really nice.”Woman service user“I th<strong>in</strong>k sometimes wait<strong>in</strong>gfor th<strong>in</strong>gs can be the mostfrustrat<strong>in</strong>g th<strong>in</strong>g, they canbe very slow to do th<strong>in</strong>gs orget anywhere… like fromprison I had to go over to an<strong>in</strong>dependent hospitalbecause I was wait<strong>in</strong>g for abed here….[now I am] readyto go on to supported liv<strong>in</strong>gaccommodation but it’sgo<strong>in</strong>g to take months andmonths……Yeah they will sayyou are ready for this butyou have got to wait monthsand months.”Woman service user“No, I don’t th<strong>in</strong>k it workswell, but I don’t th<strong>in</strong>k itworks well anywhere72
Case example:Internally there was a care pathway for women at this unit, with womenadmitted to one ward be<strong>in</strong>g referred to a second (often described as a “predischarge”ward) once their mental health was more settled, and women <strong>in</strong>the “Enhanced” service could be referred on to a ward which had two bedsspecifically designated as “step‐down” places for the TEMSS service.However, as well as blockages <strong>in</strong> the Care Pathway <strong>in</strong> terms of womenaccess<strong>in</strong>g a bed at this service at the time it was required, many of theprofessional stakeholders reported concerns about delays <strong>in</strong> discharge forwomen patients. These were due to a shortage of appropriate placements oflesser security or <strong>in</strong> the community, or, <strong>in</strong> the case of women requir<strong>in</strong>gcommunity placements, the current fund<strong>in</strong>g arrangements meant there wasa dis<strong>in</strong>centive for placements to be arranged as fund<strong>in</strong>g responsibilities movefrom the NHS to Local Authorities. Although there may often be delays <strong>in</strong>f<strong>in</strong>d<strong>in</strong>g appropriate placements, once a community placement was secured,women benefited from the support of the Community Forensic Team whoprovided supervision and support for women who were discharged <strong>in</strong>to thecommunity and back‐up and advice to their community‐based serviceproviders across the locality.because of the fund<strong>in</strong>garrangements, because thepeople who are go<strong>in</strong>g tofund them when they areout are not the same peoplewho fund them when theyare <strong>in</strong> so there is actually af<strong>in</strong>ancial <strong>in</strong>centive to delay,procrast<strong>in</strong>ate as much asthey can because that is acost sav<strong>in</strong>g.”It was reported that whilst there was, <strong>in</strong> pr<strong>in</strong>ciple, an agreement that fund<strong>in</strong>gwould be available for the provision of a step‐down facility for women on thehospital site but outside of the secure perimeter, as had recently beenprovided for the men patients, no date was known for when this would bebuilt/opened. Of the six women <strong>in</strong>patients <strong>in</strong>terviewed four were wait<strong>in</strong>g forappropriate move‐on placements to be identified or for a bed to becomeavailable.Services with a s<strong>in</strong>gle ward frequently experienced greater frustration atthe absence of move on accommodation. Women at different stages <strong>in</strong>their recovery meant that those ready to step down were required tolive with women who were much less well at the time. Staff <strong>in</strong> oneservice described how the lack of low secure or other step‐downaccommodation meant women had to be well enough to go straight <strong>in</strong>tothe community. In order to effect successful move‐on, they hadnegotiated with commissioners for women to have trial periods thusrequir<strong>in</strong>g payment for two beds dur<strong>in</strong>g this time. The rationale was toensure women received sufficient support from the women’s service andshould the move not be successful, they had somewhere to return to.At the time of the evaluation, it was unclear what impact the nationalmove to the use of <strong>in</strong>dividual budgets <strong>in</strong> relation to discharge plann<strong>in</strong>gand routes back <strong>in</strong>to the community would have for this group ofwomen.73
• While women service users did not always want to attend the whole CPA meet<strong>in</strong>g, they did want tobelieve that they had made a significant contribution through their own and others’ reports.• Staff and women service users reported <strong>in</strong>consistencies of approach to care plans and <strong>in</strong>put to CPAswhich had resulted <strong>in</strong> some women challeng<strong>in</strong>g the content of report<strong>in</strong>g to care teams and at reviewmeet<strong>in</strong>gs.• It was not clear that the impact of gender was be<strong>in</strong>g considered consistently <strong>in</strong> care plann<strong>in</strong>g, reviewor with care coord<strong>in</strong>ators.• Women service users and professionals agreed that there was a lack of suitable move‐onaccommodation. Access to rehabilitation wards or low secure services was limited. This had resulted<strong>in</strong> a bottle‐neck situation until such time as appropriate provision could be provided.• Further research will be helpful <strong>in</strong> understand<strong>in</strong>g the impact of <strong>in</strong>dividual budgets and theircontribution to mov<strong>in</strong>g the needs of this group of women <strong>in</strong>to ma<strong>in</strong>stream provision.78 Middleton, S. Barnett, J. & Reeves, D. (2007) What is an <strong>in</strong>tegrated care pathway? Bandolier Evidence BasedMedic<strong>in</strong>e Vol.3, No.379 Department of <strong>Health</strong> (1995) Components of CPA London HMSO80 Department of <strong>Health</strong> (2003) op.cit.74
7. Day‐to‐day for staff: work<strong>in</strong>g <strong>in</strong> a women’s medium secure serviceIt’s not helpful if we’ve got a member of staff who arrives for a 12 hour shift and when they’re one hour<strong>in</strong>to it says ‘only another 11 hours to go!’. That’s not helpful but I suppose they have personal issues aswell. We need more stability of staff, more permanents because we’ve lost a lot of staff and we’re back <strong>in</strong>a position where we’ve got a lot of agency staff. It unsettles us, makes us feel un<strong>safe</strong>. There’s lessopportunity to talk to anybody if you need to and sometimes it unsettles the ward to an extent where therecan be quite a bit of self harm happen<strong>in</strong>g. Other than that, I would say it was perfect here!Woman service userWomen’s experience of medium secure services was shaped by the unit staff and other professionals whothey came <strong>in</strong>to contact with. Considerable thought had been given to establish<strong>in</strong>g organisational structureswhich supported an efficient and effective service whilst ensur<strong>in</strong>g that the philosophy of care as well as thepromotion of relational security were part of the reality of women’s experience. Women service users<strong>in</strong>terviewed for the evaluation described how important it was that the professionals, <strong>in</strong>clud<strong>in</strong>g qualifiedand unqualified staff, they worked with understood what <strong>life</strong> was like from their perspective. Severalwomen said they felt staff treated them <strong>in</strong> ways they found unsympathetic and attributed this to the factthat, whatever happened, staff left at the end of their shift or work<strong>in</strong>g day but they have to stay on. Amongthe professionals and staff groups participat<strong>in</strong>g here, many described their commitment to dedicatedwomen’s services and their desire to contribute to develop<strong>in</strong>g and ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g good practice which wouldled to women achiev<strong>in</strong>g their aspirations and full recovery for some. These same <strong>in</strong>dividuals also describedthe barriers they faced <strong>in</strong> achiev<strong>in</strong>g organizational and personal aims which <strong>in</strong> turn impacted on thewomen.Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women's Mental <strong>Health</strong> 81 states <strong>in</strong> the specification that services must payattention to the composition of the workforce; the provision of multi‐discipl<strong>in</strong>ary management; tra<strong>in</strong><strong>in</strong>gand support for staff and for research to be carried out. This section exam<strong>in</strong>es the ‘work<strong>in</strong>g’ environments,factors which enabled staff to deliver effective services, and improvements needed to ensure thatprovision meets its contractual agreements.7.1 Staff<strong>in</strong>g and staff<strong>in</strong>g structuresIn addition to sett<strong>in</strong>g up a “multi‐discipl<strong>in</strong>ary/multi‐agency managementteam to help create gender sensitive organisational culture, policies andpractice”, the specification expected services to develop a range of specificcharacteristics. The evaluation f<strong>in</strong>d<strong>in</strong>gs suggested that it was prov<strong>in</strong>gdifficult for many services to meet all of these particular expectations.1. Multi‐discipl<strong>in</strong>ary/multi‐agency management teams:The role of the management team extended to all aspects of awoman’s care and care pathway. In the case study areas, this wasrecognized as central to how well the women’s service functioned. Theteams were usually multidiscipl<strong>in</strong>ary (MDTs) and <strong>in</strong>ternal to theservice with representatives of external agencies feed<strong>in</strong>g <strong>in</strong>to the CPA75
process. MDTs met on a regular and frequent basis with RMOs see<strong>in</strong>gwomen weekly or fortnightly. Some staff <strong>in</strong>volved <strong>in</strong> the MDT wereunable to attend all meet<strong>in</strong>gs due to other commitments. This couldimpact on communication about <strong>in</strong>dividual women and the service asa whole.Women service users were usually aware that there was a teammanagement approach to the provision of care and who the relevantmembers of the team were. However, frequently they mentioned the‘distance’ between themselves and senior members of the team<strong>in</strong>clud<strong>in</strong>g the consultant psychiatrists. Some women and staff alsodescribed how, despite its best <strong>in</strong>tentions, a team approach did notchange the reality of secure services where ultimately the womenthemselves did not have the power to effect change.“This is the reality. You haveno choice about whetheryou are locked up or not,that’s not your decision, it’ssociety’s decision via thecourts or Mental <strong>Health</strong> Actwhich makes empowermenta challenge. Everyone wouldregard empowerment as animportant th<strong>in</strong>g. Howreadily you can empowersomeone who is ultimatelypowerless is challeng<strong>in</strong>g.”Case example:In one service, the MDT and staff group had changed some of their work<strong>in</strong>gpractices as a result of experience <strong>in</strong> their early days. There was recognitionthat it was difficult to ensure effective communication from the MDT to thestaff group as a whole. One way of ameliorat<strong>in</strong>g this was to have senior andqualified nurses attend<strong>in</strong>g the weekly ward rounds. They also <strong>in</strong>troducedwritten summary feedback sheets for each woman from the ward roundwhich all staff had access to.Like many other women’s services, the physical layout of this unit wasdesigned to provide greater communication between staff and womenservice users. The office space was completely visible to the women on thema<strong>in</strong> ward which meant that they could observe, although not hear, whatwas happen<strong>in</strong>g. Some staff described be<strong>in</strong>g conscious of how they <strong>in</strong>teracted<strong>in</strong> that space and that it was an opportunity to model how people relate <strong>in</strong>the professional group.Members of the MDT said they visited the ward frequently and aimed toma<strong>in</strong>ta<strong>in</strong> high visibility. However, a disadvantage for them was that their ownoffice space was some distance away and on the floor above, thus potentiallyre<strong>in</strong>forc<strong>in</strong>g a strict hierarchy to the women and nurs<strong>in</strong>g staff. It meant thatmembers of the MDT had to make a conscious effort to go to the ward.2. A dedicated, appropriately skilled staff group with capacity for crosscover and the development of specialist skills:Operational policies for the case study areas showed that they allsought to put <strong>in</strong> place the team envisaged for women’s services.However, <strong>in</strong> mixed services, the practice for recruit<strong>in</strong>g and/ordeploy<strong>in</strong>g staff with<strong>in</strong> the service as a while varied. In one area,nurs<strong>in</strong>g staff were allocated through a central system and this mighthave <strong>in</strong>cluded allocation to the women’s service. In another, nurs<strong>in</strong>gstaff from with<strong>in</strong> or outside could apply for posts with<strong>in</strong> the women’s“I th<strong>in</strong>k people <strong>in</strong>itially th<strong>in</strong>kit’s just about quantity ofstaff and it is partly aboutquantity of staff but I th<strong>in</strong>kcrucially it’s about quality ofstaff and the quality of therelationships that they canhave with patients. It’sabout us<strong>in</strong>g those76
service as a separate employment opportunity. MDT positions wereusually advertised for the women’s service <strong>in</strong> question rather thandraw<strong>in</strong>g on a hospital pool of professionals.In one area, they developed an Associate Practitioner role thatprovided various cl<strong>in</strong>ical <strong>in</strong>terventions to women and focused onsupport<strong>in</strong>g their understand<strong>in</strong>g and self‐management of mental healthissues, <strong>in</strong>clud<strong>in</strong>g a self‐<strong>in</strong>jury support group; hear<strong>in</strong>g voices; selfesteem; and anxiety management, with<strong>in</strong> the context of a therapeuticrelationship built gradually whilst work<strong>in</strong>g <strong>in</strong> a support role on thewomen’s wards.Capacity was an issue <strong>in</strong> two of the case study areas.relationships as a way ofmanag<strong>in</strong>g and ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>gbehaviours and that iswithout hav<strong>in</strong>g to resort toother strategies orstructures or observations orwhatever, so for me it’sreally about the quality andthe k<strong>in</strong>d of skills the personhas <strong>in</strong> terms of theunderstand<strong>in</strong>g they have.The women’s service verymuch focuses on reflectivepractice th<strong>in</strong>k<strong>in</strong>g aboutwhat we do.”Case example:The usual staff<strong>in</strong>g complement was six staff dur<strong>in</strong>g the day, of whom twowere qualified. In the past, it had been three qualified staff on each shift, butthis was reduced due to the Cost Improvement Programme. Some staffbelieved this had a negative impact on the level of service provided to thewomen. Whilst it was felt by both staff and women alike that hav<strong>in</strong>g six staffmembers on duty was adequate for the most part, it was reported that it wasnot unusual for staff to be called away to work elsewhere due to staffsickness or shortages on other wards <strong>in</strong> this mixed unit. It was also said to bethe case that it was often male staff members that were asked to cover onother wards, thus impact<strong>in</strong>g on the gender balance of the women’s serviceteam. The gender mix was generally aimed to be at a 3:7 ratio male tofemale, and it was recognized that it is valuable for some women to haveaccess to good male role models among the staff team.At night time four staff were on duty, two of whom would be qualified and atleast two will be female as this was seen to be important to protect women’sprivacy and dignity dur<strong>in</strong>g the night‐time shift.Whilst overall staff<strong>in</strong>g levels on this ward did not appear to be a concern, oneof the women who had transferred to a second ward <strong>in</strong> the same service feltthe number of staff was too low. There were usually just four staff on dutydur<strong>in</strong>g the day for up to 22 service users, a “massive” drop from the staff<strong>in</strong>put available to the women whilst they were on the previous ward. Sheexpla<strong>in</strong>ed the situation had been made worse recently because an elderlymale patient who needed a high level of care due to his physical frailtygenerally monopolized two members of the staff. If someone then neededescorted leave that left just one staff member to respond to the needs of theother 20 service users on the ward. She felt this sometimes compromisedboth <strong>safe</strong>ty and the quality of care available on the ward.Situations where there were regular staff shortages impacted on theday to day care provided. In one service, a ward with a rehabilitativefocus meant that most of the women required a significant amount of“In terms of relationalsecurity, numbers of staffare an issue and patientswill say they always wantmore staff. Nurses willalways say they want morestaff. <strong>My</strong> experience is it’sthe <strong>in</strong>verted U curve whereyou get to a certa<strong>in</strong> numberand all staff regardless ofdiscipl<strong>in</strong>e startcongregat<strong>in</strong>g. I would rathersee more OTs and TechnicalInstructors that can takepeople out to do activities.“We did go through a phasewith lots of patients on oneto one observations. It’simportant that members ofstaff who are there, arethere regularly and knowthe patients pretty wellrather than huge numbersof bank or agency staff. Butit may be too tight and somewho want ground leave maynot be able to take it andyou can’t achieve targets <strong>in</strong>terms of patient activities.”77
leave off the ward to help facilitate their rehabilitation and thedemand for escorts was high. Here there was a new ward with noaccess to outside space without leav<strong>in</strong>g the ward area, so whenescorts were unavailable, go<strong>in</strong>g out for walks or fresh air wasrestricted. Whilst typically there were two or three members of staffon duty when there were only two, leave opportunities for womenrequir<strong>in</strong>g escorts were effectively prevented (this was because onequalified nurse must rema<strong>in</strong> on the ward to hold the medication keysand another to hold the security keys). As a result, hav<strong>in</strong>g the womencooped up on the ward for most of the day led to frustrations be<strong>in</strong>gexpressed verbally and had a knock on effect on all the women.3. A stable staff group which will help consistency <strong>in</strong> practice and thedevelopment of therapeutic relationships:Women service users and the professionals <strong>in</strong>volved <strong>in</strong> their care gavea clear message that a stable staff group was essential for them all forthe follow<strong>in</strong>g reasons:• Frequent staff changes were unsettl<strong>in</strong>g for women• Non‐permanent staff were sometimes perceived as <strong>in</strong>vest<strong>in</strong>g less<strong>in</strong> the service as they would not be stay<strong>in</strong>g• The development of relational security was more realistic with astable staff group• Opportunities for staff development were improved where thestaff group was permanent and <strong>in</strong>dividuals stayed for some time <strong>in</strong>post.One service said that although encourag<strong>in</strong>g men to work <strong>in</strong> the unithad been difficult, nurs<strong>in</strong>g staff usually stayed for about two years.This was contrasted <strong>in</strong> other services where nurs<strong>in</strong>g groups werereliant on agency staff and there was a much higher turnover. Theethos of the service and the provision of support were key factorsaffect<strong>in</strong>g recruitment and retention. (See also 7.3 below.)“I th<strong>in</strong>k aga<strong>in</strong> there is somevery positive practice, but Ith<strong>in</strong>k staff are not alwaysconsistent, and this doesn’tpromote relational security,when not all staff ma<strong>in</strong>ta<strong>in</strong>the same rules and work tothe same policies andprocedures, but I th<strong>in</strong>k thereare some very goodtherapeutic relationshipsbetween <strong>in</strong>dividualmembers of staff andwomen they work with butthe <strong>in</strong>consistency is a bigproblem.”Case example:In this service, there was no dedicated staff team specifically for thewomen’s service, although nurses and support worker staff were allocated tospecific wards and whilst there was some <strong>in</strong>ternal movement for short noticesickness, the ward teams were fairly stable and established. Other membersof the multi‐discipl<strong>in</strong>ary team, such as OT staff, worked across men andwomen’s wards (although there was an OT who worked across the threewomen’s areas and the women’s service has a fairly stable <strong>in</strong>put from thedepartment). There were Consultant Psychiatrists (RMOs) allocated to thewomen’s service but they also worked on the men’s wards. RMOs workedacross both medium and low secure services so they could follow serviceusers as they moved from medium to low secure care.78
The majority of the ward staff were female, although the team said therewere some very good male staff members work<strong>in</strong>g <strong>in</strong> the women’s servicethat positively chose to work with women and who provided good male rolemodels for the women.Whilst, on the whole, the ward teams were fairly stable, due to uncerta<strong>in</strong>tyabout the future of one of the women’s wards they have lost some of theirjunior staff nurses and there were vacancies on the ward. The senior nurs<strong>in</strong>gteam and support workers though were fairly established and providedcont<strong>in</strong>uity <strong>in</strong> relationships with the women.4. An appropriate gender mix of staff:All the case study services agreed with the guidance and were work<strong>in</strong>gtowards achiev<strong>in</strong>g a 7:3 female to male gender ratio across the wardsand multi‐discipl<strong>in</strong>ary teams, as well as a broad skill and knowledgemix. However, this had been with vary<strong>in</strong>g success:• One service which achieved this ratio had also until recently onlyemployed men <strong>in</strong> ward manager roles• Two services said that until very recently, ward managers werealways men and <strong>in</strong> one area, many of the staff were male• Professionals <strong>in</strong> a range of roles (social workers, psychologists,OTs) were more likely to be women• One service still had nurs<strong>in</strong>g groups with a higher proportion ofmen and attributed this to the reluctance of female staff towork<strong>in</strong>g with women as they would feel more vulnerable.“We’ve had lots of newlyqualified staff and they’vereally embraced the conceptof work<strong>in</strong>g with<strong>in</strong> aframework rather than justdo<strong>in</strong>g what you have to do.”“At first I wanted tocont<strong>in</strong>ue on the acute wardsso I was a bit apprehensivebut when I was work<strong>in</strong>g onhere, I got really passionateabout it.”Case example:The staff recruitment and retention policies across this women’s serviceaimed to recruit a dedicated team to work with the women, with nurs<strong>in</strong>g jobdescriptions specific to the women’s service reflect<strong>in</strong>g its philosophy of care.A gender ratio of 7:3 female to male was aimed for and a broad skill mix. Theservice favoured staff who actively chose to work with women. Individualswere needed who could create a non‐judgmental therapeutic environment,work appropriately with women by provid<strong>in</strong>g active listen<strong>in</strong>g, empathy,warmth and compassion.The acute admissions and treatment ward typically had five staff on dutydur<strong>in</strong>g the day <strong>in</strong>clud<strong>in</strong>g at least two qualified nurses, although the numbervaried accord<strong>in</strong>g to what was happen<strong>in</strong>g on the ward, for <strong>in</strong>stance if a womanis be<strong>in</strong>g cared for <strong>in</strong> the <strong>in</strong>tensive nurs<strong>in</strong>g suite or <strong>in</strong> seclusion, additionalstaff were available. It was reported by staff that generally the 7:3 genderratio was achieved and they felt that many of the women had very goodrelationships with male staff. The presence of male staff was seen to add adifferent k<strong>in</strong>d of dynamic and have a positive “defus<strong>in</strong>g” effect with<strong>in</strong> theemotionally highly‐charged ward environment. As an acute ward, womentended to spend more time there so the demand for escorts was not usuallyhigh. As the ward layout was designed to facilitate zonal observation, theneed for one‐to‐one nurs<strong>in</strong>g was reduced. Feedback <strong>in</strong>dicated staff<strong>in</strong>g levels“One of the biggestchallenges we face is gett<strong>in</strong>gmale staff to work here. Wehave a policy about malestaff work<strong>in</strong>g with womenso they don’t give Depo<strong>in</strong>jections, sanitary products,they don’t do observationsat night. We thought hatwould be good andprotective but some malestaff say they don’t want tobecome deskilled, they’d feelthey’re not help<strong>in</strong>g orthey’re worried that womenwill accuse them of sexualacts.”79
on the ward were generally adequate with resources be<strong>in</strong>g appropriatelyallocated, although it was felt it was <strong>in</strong>evitable that there will always beexceptional days when, due to untoward <strong>in</strong>cidents on the ward and/or a highdemand for escorts for court appearances for example, staff resources weretemporarily overstretched.7.2 Recruitment and retention of staffThe recruitment of appropriate ward staff was considered to be veryimportant <strong>in</strong> all the case study services. Where team structures weredependent on smaller numbers of qualified staff, e.g. two qualified staffper ward per shift, and high numbers of health care assistants and supportworkers, considerable thought needed to be given to who would be mostsuitable. The HCAs and support staff were an essential resource towomen’s services and were usually the staff to spend most time withwomen <strong>in</strong> the units.Services said they were usually look<strong>in</strong>g for ward staff who:• were motivated to work with women• were sensitive to issues which affect women and women’sexperiences• have the capacity to work with the model of care <strong>in</strong> operationIn mixed‐sex provision, staff and service managers agreed that new staffshould be recruited specifically to work with<strong>in</strong> the women’s service. In oneservice, they were able to do so and these posts had their own jobdescriptions which reflected the philosophy of care. In another area, theperson specification stated that the service wished to appo<strong>in</strong>t staff whohad an active <strong>in</strong>terest <strong>in</strong> and desire to work with women service users, andthe <strong>in</strong>duction and on‐go<strong>in</strong>g <strong>in</strong>‐service tra<strong>in</strong><strong>in</strong>g <strong>in</strong>cluded women’s mentalhealth issues and gender specific practice. However, this was not alwaysthe case and one provider was mov<strong>in</strong>g towards a centralised employmentprocess which would not necessarily address the needs of the women’sservice. A concern here was that applicants would choose to work <strong>in</strong> themen’s service.“You’re look<strong>in</strong>g at people’sattitudes more thanknowledge because youwouldn’t for an HCA forexample have anexpectation of someonewho’s been work<strong>in</strong>g <strong>in</strong> afactory would have a lot ofknowledge of psychiatrichospitals or gender specificservices. You’re look<strong>in</strong>g for apositive attitude.”“Men’s is seen as an easieroption. Evidence shows thatwomen burn out quickerthan men.”Agency or bank staff provided a back up source of staff and services triedto ensure a regular pool of people to choose from to ensure some level ofcont<strong>in</strong>uity.The retention of staff was of equal importance and services identified anumber of <strong>in</strong>itiatives to encourage staff to stay <strong>in</strong>clud<strong>in</strong>g:• Committed and positive teamwork:Ensur<strong>in</strong>g the <strong>in</strong>volvement of staff <strong>in</strong> meet<strong>in</strong>gs and discussions was asimportant <strong>in</strong> some services as <strong>in</strong>volv<strong>in</strong>g women themselves. However,80
this was not always apparent and some support staff did not feelsufficiently <strong>in</strong>cluded.• Provision of tra<strong>in</strong><strong>in</strong>g, support and supervision:One case study service had employed three Cl<strong>in</strong>ical Development staffeach with different specialist skills to support ward managers andprovide practice development <strong>in</strong> relation to cl<strong>in</strong>ical skills andknowledge. They also offered bursaries which offered unqualified staffthe opportunity to tra<strong>in</strong> as mental health nurses. These staffcommitted to return to work for the service post‐tra<strong>in</strong><strong>in</strong>g.• Staff who are empowered <strong>in</strong> their work:Dedicated teams who worked <strong>in</strong> a reflective way were seen to bebetter able to reta<strong>in</strong> staff. One service provided a group analystmonthly to meet with staff, <strong>in</strong> service counsell<strong>in</strong>g and access for HCAsto the women’s service psychologist as opportunities for staff toaddress distress and ga<strong>in</strong> <strong>in</strong> confidence.7.3 Tra<strong>in</strong><strong>in</strong>g, support and supervisionThe importance of tra<strong>in</strong><strong>in</strong>g <strong>in</strong>clud<strong>in</strong>g gender awareness as well theprovision of formal supervision and other support were considered bystaff at all levels to be key to the effective delivery of services to women.However, the reality was that <strong>in</strong> addition to many examples of goodpractice, services experienced ongo<strong>in</strong>g barriers which <strong>in</strong> particularprevented qualified and unqualified staff from access<strong>in</strong>g formal and<strong>in</strong>formal support.Case example:This service provided a wide range of tra<strong>in</strong><strong>in</strong>g and support specifically for thenurs<strong>in</strong>g teams whose staff worked most closely with women. In addition to aservice‐wide <strong>in</strong>duction, staff at the women’s service attended tra<strong>in</strong><strong>in</strong>gspecific to the women’s service. Inequality Agenda provided genderawarenesstra<strong>in</strong><strong>in</strong>g at the outset of the service. However, it was difficult tooffer this on an ongo<strong>in</strong>g basis. The women’s service tra<strong>in</strong><strong>in</strong>g was still gendersensitive, usually focused on the model of care. S<strong>in</strong>ce the service opened,when staff attended tra<strong>in</strong><strong>in</strong>g was dependent on when they started and theperiods dur<strong>in</strong>g which the tra<strong>in</strong><strong>in</strong>g was offered. Some staff noted that this wasparticularly useful to clarify the model of care and queries about work<strong>in</strong>gwith women <strong>in</strong> a dedicated service.The service offered two‐weekly tra<strong>in</strong><strong>in</strong>g sessions provided by a colleaguefrom a specific discipl<strong>in</strong>e with<strong>in</strong> the team. These sessions have covered:• The model of care• Work<strong>in</strong>g with women with children• Prison cultures• CBTManagerial supervision was required for all ward staff <strong>in</strong> this service. Team81
leaders supervised qualified staff who, once experienced, <strong>in</strong> turn might havebeen a mentor to HCAs. Cl<strong>in</strong>ical supervision was provided approximatelymonthly on an <strong>in</strong>dividual basis to discuss specific issues as well a group withan external psychologist for all staff.Staff were also encouraged to make use of <strong>in</strong>formal support from colleagues,<strong>in</strong> handovers as a peer group and specifically through access to the servicepsychologist.Effective support was helped by committed senior members of the MDTwho ensured that tra<strong>in</strong><strong>in</strong>g and supervision were available and rigorouslyused. However, other factors often h<strong>in</strong>dered take up <strong>in</strong>clud<strong>in</strong>g situationswhere there was no protected time for attend<strong>in</strong>g tra<strong>in</strong><strong>in</strong>g or supervisionwhich led to sometimes rely<strong>in</strong>g on the good will of ward staff to come <strong>in</strong>early or stay on after f<strong>in</strong>ish<strong>in</strong>g their shift. Other factors <strong>in</strong>cluded:• Lack of understand<strong>in</strong>g about what was or should have been availableand know<strong>in</strong>g how to access this• Demands on senior ward staff prevent<strong>in</strong>g them from provid<strong>in</strong>g regularsupervision or mentor<strong>in</strong>g• Staff shortages on shifts• Lack of resources for specialist tra<strong>in</strong><strong>in</strong>g, e.g. gender awarenessNevertheless, there was no question about the value derived fromdifferent <strong>in</strong>puts and that they directly impacted on women’s care.“We’re go<strong>in</strong>g to havedifficulties this year becauseour tra<strong>in</strong><strong>in</strong>g budget is fairlytight. Also because ourstaff<strong>in</strong>g levels are not overgenerous,releas<strong>in</strong>g frontl<strong>in</strong>estaff is always adifficulty but we’re try<strong>in</strong>g tomake sure all font l<strong>in</strong>e staffhave some tra<strong>in</strong><strong>in</strong>g. We’vebeen putt<strong>in</strong>g on CPDprogrammes but it has notbeen as systematic as itshould have been.”7.3.1 Tra<strong>in</strong><strong>in</strong>gThe specification states that ‘the service will need to be able to providetra<strong>in</strong><strong>in</strong>g to other organisations and professionals as well as appropriatetra<strong>in</strong><strong>in</strong>g for its own staff group’. One case study area had a long lead‐<strong>in</strong>development period prior to the open<strong>in</strong>g of the service. Induction tra<strong>in</strong><strong>in</strong>g<strong>in</strong>clud<strong>in</strong>g gender awareness was provided to the first cohort of staffrecruited before any women were admitted to the unit. This wasrecognized as a luxury. However, the benefits were perceived asconsiderable <strong>in</strong>clud<strong>in</strong>g:• Time to focus on the service and the team• Opportunity to develop and embed a model of care• Team build<strong>in</strong>g• Intensive delivery of gender awareness tra<strong>in</strong><strong>in</strong>g for all staffThe reality was that where women’s wards were redeveloped fromexist<strong>in</strong>g services, e.g. <strong>in</strong> a mixed sett<strong>in</strong>g, it was not possible to have an‘empty’ unit and thus the time for a dedicated <strong>in</strong>duction.Staff were all expected to attend general service <strong>in</strong>ductions which would<strong>in</strong>clude tra<strong>in</strong><strong>in</strong>g about health and <strong>safe</strong>ty, policies and practices and“I th<strong>in</strong>k sometimes somestaff get lost <strong>in</strong> the theory ofit. So at handovers, ifsometh<strong>in</strong>g’s happened, youtry and th<strong>in</strong>k about that andtry and work it out. We alsohave more formal structures<strong>in</strong> place, reflective practiceonce a week, a groupanalyst who comes once amonth and we’re look<strong>in</strong>g tomake these much moreattachment focused. But thebiggest challenge is the drip,drip, drip, day to day.”82
work<strong>in</strong>g with<strong>in</strong> a secure sett<strong>in</strong>g. Differentiated care and its relevance wasnot necessarily part of specific tra<strong>in</strong><strong>in</strong>g nor part of the women’s service<strong>in</strong>duction. Of the 14 survey responses, one <strong>in</strong>dependent sector service hadno staff who had received tra<strong>in</strong><strong>in</strong>g specifically to help them work withwomen with mental health needs. However, across the other services, theproportion of staff who had received gender awareness tra<strong>in</strong><strong>in</strong>g rangedfrom 10 to 100%. Some services noted their concern that tra<strong>in</strong><strong>in</strong>g hadbeen <strong>in</strong>sufficient, and that staff turnover, or dissatisfaction with tra<strong>in</strong><strong>in</strong>greceived <strong>in</strong> one case, had impacted on the proportion of those tra<strong>in</strong>ed.Medium secure services for women provided gender awareness tra<strong>in</strong><strong>in</strong>g <strong>in</strong>some form or other for new staff. This ranged from gender as part of amore general service (and <strong>in</strong> the <strong>in</strong>dependent sector, corporate) <strong>in</strong>ductionto specific gender tra<strong>in</strong><strong>in</strong>g provided by, for example, Inequality Agenda.Where gender awareness tra<strong>in</strong><strong>in</strong>g was provided, it was usually as:• Three one‐day courses for support workers, nurses, OTs and OTsupport, adm<strong>in</strong>istration, cater<strong>in</strong>g and ma<strong>in</strong>tenance staff• One and three day courses for nurs<strong>in</strong>g assistants, nurses, medicalstaff, psychologists and social workersServices also provided tra<strong>in</strong><strong>in</strong>g <strong>in</strong> their specific model of care, otherpsychological approaches and group skills facilitation.7.4 The role and provision of supervisionThe service specification recommends that staff support ‘should be<strong>in</strong>tegral to the organisation of services and <strong>in</strong>clude supervision, space forreflective practice and access to work‐related confidential counsell<strong>in</strong>g andcrisis support’.All women’s medium secure services provided some tra<strong>in</strong><strong>in</strong>g even if notalways gender focused. The case study services described <strong>in</strong> detail theirprovision and some of the factors which helped or h<strong>in</strong>dered <strong>in</strong> its take up.In addition, l<strong>in</strong>e management structures have been implemented to<strong>in</strong>clude the provision of formal supervision for all staff. Most wards had as<strong>in</strong>gle manager supported by team leaders/senior staff who <strong>in</strong> turnmanaged less experienced and unqualified staff.On paper, there were clear guidel<strong>in</strong>es about the provision of supervision.Qualified staff were usually expected to have monthly <strong>in</strong>dividual cl<strong>in</strong>icalsupervision and with other staff, attend monthly group practice sessions.One service had developed a support mechanism for new staff as asupplement to formal managerial or cl<strong>in</strong>ical supervision which <strong>in</strong>cludedallocation of a qualified staff mentor and an experienced HCA to shadowon the ward. However, <strong>in</strong> practice the reality <strong>in</strong> some services washaphazard and some ward staff reported rarely hav<strong>in</strong>g supervision due toother priorities on the ward.“It’s really up to us to be abit proactive <strong>in</strong> organis<strong>in</strong>gthe meet<strong>in</strong>gs for supervisionbecause they can getforgotten about.”“It can be very, verysupportive as long as you letit be and with regard tocont<strong>in</strong>u<strong>in</strong>g professionaldevelopment, aga<strong>in</strong> it’sdown to the <strong>in</strong>dividual toput yourself forward. I th<strong>in</strong>kthe ones who are moreproactive probably f<strong>in</strong>d theyget more out of it.”83
Unqualified support staff and HCAs were the most likely not to receive thesupervision they had been told was forthcom<strong>in</strong>g. In at least three of thecase study areas, those <strong>in</strong>terviewed described how, despite spend<strong>in</strong>g agreat deal of time with women service users, they found it difficult toobta<strong>in</strong> and sometimes to ask for the support they needed.Key concerns for services <strong>in</strong>cluded:• Increas<strong>in</strong>g demands on qualified staff who were be<strong>in</strong>g pulled <strong>in</strong> toomany directions and unable to give sufficient time to others• Limited time available for ‘supervisees’ due to the demands of theward and need to balance staff requirements with facilitation ofwomen’s activities, e.g. escorted leave• Recognition of the importance and value of support• Lack of confidence among newly qualified/unqualified staff to seek outand ask for supportA further important consideration identified <strong>in</strong> one case study area washow to support ancillary staff, for example, housekeepers and otherdomestic employees to whom women service users might choose todisclose sensitive <strong>in</strong>formation. They noted:“To be honest, and I amgo<strong>in</strong>g to be honest, I haveonly ever had onemanagerial supervision and Ihave been here 4 years – Ihave had one lot ofsupervision and that waswith my old ward managerand I haven’t had any [oneto‐one]cl<strong>in</strong>ical supervision.”“I am manag<strong>in</strong>g six supportworkers and two seniornurses. For their cl<strong>in</strong>icalsupervision, people werechas<strong>in</strong>g me and I just keptsay<strong>in</strong>g ‘I’m too full’. Whatdo I get? A flat battery!”“We did a brief research project about the fact that particularly women oftenchose unqualified members of staff to disclose [abuse] to or to talk to and it maynot even be the support workers, it may be the domestics or the housekeepers andI th<strong>in</strong>k this has had to be someth<strong>in</strong>g we have had to become very sensitive to and Ith<strong>in</strong>k sometimes it is about not want<strong>in</strong>g a professional response and want<strong>in</strong>g ahuman response so aga<strong>in</strong> that’s someth<strong>in</strong>g we have also tried to th<strong>in</strong>k about,what are their needs, what do you do if you are the housekeeper and you areclean<strong>in</strong>g on the ward and somebody comes and talks to you. What do you do withthat <strong>in</strong>formation, where do you take it, do you feel you have the skills to respondto it. We have started to th<strong>in</strong>k about this <strong>in</strong> a wider format really.”We identified very few areas where tra<strong>in</strong><strong>in</strong>g was offered to thesemembers of staff.• Professionals across all areas valued a multi‐discipl<strong>in</strong>ary and multi‐agency structure even though thelatter was harder to achieve.• Services wanted to work with dedicated, stable staff teams with an appropriate gender mix. However,given difficulties of recruitment and retention it was rare that this was achieved.• There were considerable gaps between tra<strong>in</strong><strong>in</strong>g and supervision policies <strong>in</strong> services and what happened<strong>in</strong> practice result<strong>in</strong>g <strong>in</strong> many staff receiv<strong>in</strong>g no gender awareness tra<strong>in</strong><strong>in</strong>g. Supervision frequently tooksecond place amongst a range of compet<strong>in</strong>g demands on senior ward staff.81 Department of <strong>Health</strong> (2004) Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women’s Mental <strong>Health</strong> DH84
8. Build<strong>in</strong>g on experience: <strong>in</strong> even <strong>safe</strong>r <strong>hands</strong>I feel a lot is a lot of work from yourself, I mean its trial and error with your medication – I have hadchanges and side effects but it’s changed and I have a say <strong>in</strong> that, not too big a say but I can speak andthere is the option to talk about it. I also feel that there is a strong work<strong>in</strong>g force here, that you can go toanyone of the staff who you trust and who you know will advise you well, who will listen and understandand who will help you. I have a great team, I can’t want for a better team who works with me. So I th<strong>in</strong>k ittakes a lot from yourself, I th<strong>in</strong>k you have got to meet your medication half way and I th<strong>in</strong>k that’simportant to ma<strong>in</strong>ta<strong>in</strong> a strong mental well be<strong>in</strong>g.Woman service userIn 2000, the report Good Girls: surviv<strong>in</strong>g the secure system 82 said ‘(women’s) stories revealed a sharedbelief that the dream of discharge could best be achieved by toe<strong>in</strong>g the l<strong>in</strong>e rather than fully address<strong>in</strong>g thecauses of their distress’. This evaluation has presented evidence which suggests that not only has thenumber of dedicated women’s medium secure services grown to better accommodate women withcomplex needs, many of these demonstrated that they were turn<strong>in</strong>g the corner and enabl<strong>in</strong>g women, withtheir help, to take back their dream <strong>in</strong>to their own <strong>hands</strong>.This section first identifies a number of key areas of good practice and what services themselves believedworked well <strong>in</strong> their context. It then considers the implications of the f<strong>in</strong>d<strong>in</strong>gs and what rema<strong>in</strong>s to beaddressed by policy makers, service providers and staff, service users and researchers <strong>in</strong> the field. Thirdand f<strong>in</strong>ally, it reviews the current service specification which formed the framework for the development ofdedicated women’s secure services.8.1 Good practice <strong>in</strong> women’s servicesThe evaluation f<strong>in</strong>d<strong>in</strong>gs have demonstrated the variety of ways <strong>in</strong> which the service specification forwomen’s secure services has been or is be<strong>in</strong>g implemented. The six case study areas had all developeddifferent approaches to philosophies of care. We could not f<strong>in</strong>d evidence from discussions with women andprofessionals or across changes <strong>in</strong> women’s situations, that the philosophy of care was necessarily theprimary factor to determ<strong>in</strong>e how women perceived the impact of the service on their recovery.More importantly, factors <strong>in</strong>clud<strong>in</strong>g the follow<strong>in</strong>g appeared to provide the keys to successfulimplementation of the specification:• A strong, transparent and embedded framework for staff and women service users underp<strong>in</strong>ned by theconcept of relational security and a clear understand<strong>in</strong>g of the importance of boundaries• An effective multi‐discipl<strong>in</strong>ary team which communicates across all staff groups and with womenservice users• Gender‐sensitive tra<strong>in</strong><strong>in</strong>g and supervision for all <strong>in</strong>clud<strong>in</strong>g ancillary workers i.e., that it is required forthe entire staff group• Gender‐specific care pathways that enable women to move through and out of medium secureservices• Planned programmes of activities <strong>in</strong>clud<strong>in</strong>g some fun.85
In order to understand what works well and what may be deemed good practice <strong>in</strong> women’s mediumsecure provision, we asked services <strong>in</strong> the orig<strong>in</strong>al survey to identify what they felt most proud about. Wereceived an <strong>in</strong>terest<strong>in</strong>g array of responses from the team to the women patients. Key to many serviceswere the follow<strong>in</strong>g:• Patient <strong>in</strong>volvement and <strong>in</strong> particular through user groups• The care women received which empowered them• The strength of relational security• Gender specific approaches implemented with<strong>in</strong> a women‐only service• Committed staff teams and multi‐discipl<strong>in</strong>ary work<strong>in</strong>g• Provision of therapy and other means of meet<strong>in</strong>g women’s needs• Specific and specialist areas of development, for example, for women with disabilities8.1.1 Delivery of differential care to meet the specific needs of women1. Philosophies of care for work<strong>in</strong>g with women were embedded with<strong>in</strong> the daily practice of staff teams<strong>in</strong> most case study services based on gender sensitive practice, promot<strong>in</strong>g a psycho‐social approachtak<strong>in</strong>g account of the context of women’s mental distress and acknowledg<strong>in</strong>g the impact of traumaand abuse on women’s mental health.2. Staff recruitment policies aimed to achieve a 7:3 female to male gender ratio, with male staffprovid<strong>in</strong>g positive role models for women, although not all services had managed this yet. They alsosought to appo<strong>in</strong>t ward staff with an active <strong>in</strong>terest <strong>in</strong> and desire to work with women, and <strong>in</strong> mostareas, the <strong>in</strong>duction and on‐go<strong>in</strong>g <strong>in</strong>‐service tra<strong>in</strong><strong>in</strong>g <strong>in</strong>cludes women’s mental health issues andgender specific practice.3. Dedicated psychologists for women’s services were able to undertake formulation‐basedassessments and treatment plann<strong>in</strong>g <strong>in</strong>corporat<strong>in</strong>g psychological and social perspectives whichacknowledged the importance of the woman’s story and <strong>life</strong> experiences and while seek<strong>in</strong>gcollaboration with the woman, with her views and objectives be<strong>in</strong>g sought.4. Purpose‐built facilities as stand alone or attached to the ma<strong>in</strong> mixed‐units usually offered structuredprogrammes of therapeutic gender specific activities as well as women be<strong>in</strong>g able to access mixed‐sexactivity sessions when available and appropriate.5. The Assessment and Care Plann<strong>in</strong>g Approaches <strong>in</strong> place suggested that some were formulation‐basedencompass<strong>in</strong>g a biological, psychological and social perspective and acknowledged the woman as anexpert <strong>in</strong> her own “story” provid<strong>in</strong>g a basis for women to feel they were <strong>in</strong>volved <strong>in</strong> their careplann<strong>in</strong>g.8.1.2 Ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g women’s psychological and physical <strong>safe</strong>ty1. Relational security was well provided for <strong>in</strong> most case study areas with<strong>in</strong> regular professional practiceby staff members on the wards and the strong therapeutic relationships they built with the women. Inthe ma<strong>in</strong>, ward staff were provided with some opportunities to develop reflective practice and were86
supported to develop therapeutic relationships with<strong>in</strong> appropriate professional boundaries throughregular group and <strong>in</strong>dividual supervision.2. Extra Care, Intensive Nurs<strong>in</strong>g Suites or High Support Areas on women’s wards allowed women whowere acutely ill to be cared for away from the ma<strong>in</strong> ward area. These areas were used as a short termfacility only. They provided women who were acutely distressed and at risk of harm<strong>in</strong>g themselves orothers with a <strong>safe</strong> but comfortable environment without the need to isolate them completely, butwhere <strong>in</strong>tensive nurs<strong>in</strong>g <strong>in</strong>put and emotional support from staff was available to them.3. Cl<strong>in</strong>ical nurse and other specialists were employed with<strong>in</strong> some women’s services provid<strong>in</strong>g riskassessment, care plann<strong>in</strong>g, support and therapeutic and educational <strong>in</strong>terventions for women who,e.g. self <strong>in</strong>jure, as well as advice and support to members of the care team <strong>in</strong>volved <strong>in</strong> their care.4. The gender sensitive practice developed on wards supported staff to work towards de‐escalationus<strong>in</strong>g means other than control and restra<strong>in</strong>t techniques for manag<strong>in</strong>g women’s behaviour and it wasreported that the use of control and restra<strong>in</strong>t techniques had become less frequent.5. The physical layout of the women’s wards were more likely to have been designed to allow zonalobservation with<strong>in</strong> the ma<strong>in</strong> day areas as an alternative to <strong>in</strong>tensive one‐to‐one observations, whichwomen often found <strong>in</strong>trusive.6. Team nurs<strong>in</strong>g approaches were developed across most women’s wards so there was always amember of each woman’s team on duty who was familiar with her care plan and <strong>in</strong>dividualformulation.8.1.3 Facilitat<strong>in</strong>g recovery for women, rehabilitation and resettlement1. Seamless care pathways Hav<strong>in</strong>g identified the need for a gender‐specific route out of medium securecare for many of their women service users, some services have worked with regional teams andcommissioners to develop a seamless care pathway for women. Several wards worked with <strong>in</strong>ternalcare pathways for women with markers for progress. One service began the process pre‐admissionAnother described its access to a Community Forensic Team for women who required this supportonce discharged from the <strong>in</strong>patient service.2. The therapeutic treatment approaches on some women’s wards meant that women were supportedto develop knowledge and awareness of their own mental health needs. This was facilitated by thewomen be<strong>in</strong>g given the opportunity to explore their <strong>life</strong> stories and experiences <strong>in</strong> their own time andwith<strong>in</strong> the context of a trust<strong>in</strong>g therapeutic relationship, to reach a shared understand<strong>in</strong>g of how thisimpacted on their mental well‐be<strong>in</strong>g.3. Women service user <strong>in</strong>volvement <strong>in</strong> service plann<strong>in</strong>g and development had enabled some women totake on responsibility for facilitat<strong>in</strong>g user group meet<strong>in</strong>gs and be<strong>in</strong>g representatives at external usernetworks and meet<strong>in</strong>gs.4. Social and vocational opportunities In one service, women had access to a voluntary organizationcommissioned to provide education and work‐related tra<strong>in</strong><strong>in</strong>g and social opportunities <strong>in</strong>clud<strong>in</strong>g, for<strong>in</strong>stance, office work, desktop publish<strong>in</strong>g, participation <strong>in</strong> the runn<strong>in</strong>g of a social club/café for service87
users and advice about external tra<strong>in</strong><strong>in</strong>g and career opportunities. Women were also contribut<strong>in</strong>g todecision mak<strong>in</strong>g about ward and other activities <strong>in</strong> some areas.5. Provision of family/child visit<strong>in</strong>g suites appropriate for children were seen as a considerableimprovement on previous facilities.8.1.4 Structural and organisational factors1. Multi‐discipl<strong>in</strong>ary teams brought key staff and women service users together <strong>in</strong> decision‐mak<strong>in</strong>gprocesses. Staff across case study areas appreciated the value of this model of work<strong>in</strong>g.2. Streaml<strong>in</strong><strong>in</strong>g adm<strong>in</strong>istration wherever possible from referral to discharge helped to ensure a smoothpathway <strong>in</strong>to and through a service. This <strong>in</strong>cluded new computerized systems for record<strong>in</strong>g <strong>in</strong>formationand complet<strong>in</strong>g CPA documentation. One service worked with staff on how they wrote reports toreduce judgmental language and improve the overall balance of their report<strong>in</strong>g.3. Monitor<strong>in</strong>g activity was required <strong>in</strong> all services to provide data to commissioners and/or parentorganisations. Several had <strong>in</strong>troduced additional ways of captur<strong>in</strong>g service delivery, e.g. throughsatisfaction surveys <strong>in</strong> one case designed with women service users, staff tra<strong>in</strong><strong>in</strong>g needs analysis andtake up of tra<strong>in</strong><strong>in</strong>g and support, as a means of service development. Two case study services weredevelop<strong>in</strong>g research to determ<strong>in</strong>e mean<strong>in</strong>gful ways of measur<strong>in</strong>g outcomes.8.2 What needs to be addressed for the future?The Equal Opportunities Commission 83 said ‘Most women still have very different <strong>life</strong> experiences frommost men … because women’s lives are different from men’s they need different th<strong>in</strong>gs from public services.Meet<strong>in</strong>g their needs often means chang<strong>in</strong>g the content of services and how they are delivered’.The evaluation identified many ways <strong>in</strong> which services had addressed the specific needs of women and<strong>in</strong>deed, found that some providers had been <strong>in</strong>vited to advise men’s services on their philosophy of careand specifically relational security. However, professionals and women service users identified significantgaps and areas where there was room for development and improvement. Services participat<strong>in</strong>g <strong>in</strong> thesurvey were <strong>in</strong>vited to comment on areas for change. These tended to reflect some of their previouslyraised concerns about factors which h<strong>in</strong>dered policy implementation and focused on the follow<strong>in</strong>g:• Ensur<strong>in</strong>g staff are permanent• Facilitat<strong>in</strong>g an attitude change among generic staff and management• Ensur<strong>in</strong>g that the environment meets the physical and relational security needs of women• Increas<strong>in</strong>g tra<strong>in</strong><strong>in</strong>g and ensur<strong>in</strong>g that gender awareness tra<strong>in</strong><strong>in</strong>g was provided for all staffOn the basis of the case studies and review of documentation, we have listed a range of areas which policymakers and service providers may wish to consider for future development. These are addressed below.88
8.2.1 ProcessesModels of care:• A written policy for relational security needs to underp<strong>in</strong> service provision as an aid to consistency ofpractice and essential to protect women at risk of suicide or self harm as well as aggressive behaviour.• Models of care (whether s<strong>in</strong>gle or based on a range of philosophical precepts) need to be supported bypolicy and operational practice documentation which articulate the approach and its use <strong>in</strong> the servicefor all staff. Some services have versions for women service users outl<strong>in</strong><strong>in</strong>g how they work <strong>in</strong> the unit.These documents additionally provide a basis for service review and help ensure a consistent approachacross the ward and multi‐discipl<strong>in</strong>ary teams.Referrals and admissions:• In general, women need to be able to access a bed <strong>in</strong> their own geographical area unless, as <strong>in</strong> somecases, a women has specialist needs, e.g. learn<strong>in</strong>g disabilities, autistic spectrum disorder and her needscannot be met locally. In addition, if the circumstances of the women's offence means she needs tomove away from her home area then it maybe preferable for her to be referred to OATS.• However, women should be able to access treatment <strong>in</strong> their own area. In the <strong>in</strong>terviews for this study,family members featured highly with over 70% of women <strong>in</strong>clud<strong>in</strong>g a family member or friend fromoutside the unit as important. In their personal constructs, support to ma<strong>in</strong>ta<strong>in</strong> contact with familymembers was a key factor for women service users. At the same time, for women plann<strong>in</strong>g to returnto their home location after be<strong>in</strong>g sent out of area, lack of contact with their home team anddifficulties <strong>in</strong> decid<strong>in</strong>g appropriate care pathways was likely to disadvantage them over women able toaccess a medium secure bed <strong>in</strong> their own locality.• It also may be useful for levels of referrals and admissions and unmet demand for local women’smedium secure placements to be closely monitored and reviewed, to ensure women are not penalizedby rout<strong>in</strong>ely be<strong>in</strong>g referred to out of area private sector providers, often at some considerable distancefrom their families, social networks and home area care teams.• Women were still not be<strong>in</strong>g appropriately diverted from the Crim<strong>in</strong>al Justice System, and they wereoften remanded to prison even when there was a clear history of mental illness. There was little <strong>in</strong>reach<strong>in</strong>to women’s prisons, and often delays <strong>in</strong> transfers to hospital sett<strong>in</strong>gs. This area of referralprocesses needs strengthen<strong>in</strong>g <strong>in</strong> light of the Corston Report and the forthcom<strong>in</strong>g Bradley review.• Admission processes need to reflect the woman service user’s situation and balance this with thecomposition of the unit.• Time is needed for effective admissions <strong>in</strong>clud<strong>in</strong>g opportunities for women to visit the unit and bevisited by staff to <strong>in</strong>itiate the care plann<strong>in</strong>g process.Care plan development and implementation:• The development of <strong>in</strong>dividual care plans needs to be consistent with<strong>in</strong> <strong>in</strong>dividual services. Tra<strong>in</strong><strong>in</strong>g forstaff on the care plan approach with clearer guidance would help to ensure greater consistency andthis guidance could be developed further through on‐go<strong>in</strong>g reflective practice groups active <strong>in</strong> casestudy areas.• The implementation of <strong>in</strong>dividual care plans needs to be consistent to avoid patch<strong>in</strong>ess of provision,e.g. situations where rehabilitation for some women was compromised due to the lack of availability ofstaff.• There is a need for gender sensitive risk assessments and for histories of abuse be<strong>in</strong>g adequately taken<strong>in</strong>to account <strong>in</strong> the development of care plans.89
• The recent guidance on CPA 84 recommends that <strong>in</strong> future service users are placed at the centre of theCPA process and are fully <strong>in</strong>volved <strong>in</strong> review<strong>in</strong>g their own care plans and, for those who are able, theyshould be encouraged to take a lead role <strong>in</strong> review meet<strong>in</strong>gs <strong>in</strong>clud<strong>in</strong>g, for example, send<strong>in</strong>g out<strong>in</strong>vitations to the meet<strong>in</strong>g jo<strong>in</strong>tly with their Care Coord<strong>in</strong>ator and chair<strong>in</strong>g meet<strong>in</strong>gs.Discharge plann<strong>in</strong>g:• It is hoped that where little exists, <strong>in</strong>creased step down facilities cont<strong>in</strong>ue to be developed as soon aspossible to unblock exist<strong>in</strong>g bottle‐necks <strong>in</strong> some services.• It would also be helpful for discharge plann<strong>in</strong>g to start from day one of admission, with for example,home area care coord<strong>in</strong>ators be<strong>in</strong>g asked to identify both possible future community placements forwhen a secure sett<strong>in</strong>g is no longer required by the woman, and for the responsibility for fund<strong>in</strong>g suchfuture community placements to be agreed and planned for <strong>in</strong> advance.• Home‐area care coord<strong>in</strong>ators and care team members could also be more actively <strong>in</strong>volved <strong>in</strong> the CPAprocess dur<strong>in</strong>g the women’s stay at the unit.Meet<strong>in</strong>g diverse needs:• Where a s<strong>in</strong>gle women’s ward forms part of the medium secure service (as <strong>in</strong> two case study areas),consideration needs to be given to the use of communal space and provid<strong>in</strong>g for women who may wishto be <strong>in</strong> quieter areas away from ma<strong>in</strong> ward areas.8.2.2 PracticalitiesEnvironment:• Due to the new Standards for MSUs there is now a requirement for a 5.2 metre perimeter fence for allmedium secure units, <strong>in</strong>clud<strong>in</strong>g women’s services even if this is not seen as appropriate. However,environmental security is still important and should be emphasised especially due to the risk of selfharm.• Policies need to be implemented which address how to deal with environmental risk and its review.• Services not <strong>in</strong> purpose‐built units need to consider how best to provide zonal rather than one‐to‐oneobservations.• Wards need to keep at best to 10 and a maximum of 12 beds.Activities/OT:• Women’s services <strong>in</strong> mixed‐sex units without dedicated OTs may wish to consider facilitat<strong>in</strong>g this to<strong>in</strong>crease gender specific groups and activities for women and improve access to activities for womenwho are not able to leave the ward or are not able to, or choose not to, access mixed‐sex activities.Service user <strong>in</strong>volvement:• Women service users described the ways <strong>in</strong> which they contributed to service development. Someservices had worked with users to develop satisfaction surveys, newsletters and events’ committees.All services need to consider ways of encourag<strong>in</strong>g women to participate as part of their progress. Theyalso need to ensure that feedback is provided to avoid tokenism.Staff<strong>in</strong>g:• Services need to give consideration to recruitment and as far as possible recruit staff specifically to thewomen’s service.90
• All services need to have job descriptions and person specifications which reflect their philosophies andgender‐sensitive practice.Tra<strong>in</strong><strong>in</strong>g and supervision:• Increased resources <strong>in</strong>clud<strong>in</strong>g time are needed by all services to ensure that tra<strong>in</strong><strong>in</strong>g and supervision arealways available and attended. Take up needs to be monitored by unit/ward managers to furtherensure attendance.• In some areas staff were not receiv<strong>in</strong>g appropriate gender tra<strong>in</strong><strong>in</strong>g. Tra<strong>in</strong><strong>in</strong>g on gender issues as theyaffect women on the ward and importantly <strong>in</strong> the community needs to be more consistently provided.• Additional models for support need to be encouraged <strong>in</strong>clud<strong>in</strong>g (as already happens <strong>in</strong> some services)peer‐support, mentor<strong>in</strong>g and shadow<strong>in</strong>g for new staff.Primary care:• Lack of access to primary health care services to meet the physical health care, public health andscreen<strong>in</strong>g issues for women had been identified as a problem at some units.• Standards and Criteria for Women <strong>in</strong> Medium Secure Care from the Quality <strong>Network</strong> for ForensicMental <strong>Health</strong> Services 85 requir<strong>in</strong>g women’s medium secure services to provide access to a female GPand Practice Nurse, and to appropriate screen<strong>in</strong>g and well‐women services.8.2.3 Monitor<strong>in</strong>g, evaluation and researchThere are a number of potential future studies that would contribute to the development of women’smedium secure services.Monitor<strong>in</strong>g and evaluation:• Ongo<strong>in</strong>g monitor<strong>in</strong>g, the development of outcome <strong>in</strong>dicators of women’s recovery and serviceevaluation will ensure that services review their process from aspiration through to successfulimplementation and delivery of services accord<strong>in</strong>g to the specification.• The development of ongo<strong>in</strong>g peer‐review and report<strong>in</strong>g would contribute to determ<strong>in</strong><strong>in</strong>g how far andwhat ways services are achiev<strong>in</strong>g <strong>in</strong> relation to appropriate benchmark<strong>in</strong>g.<strong>Research</strong>:• Based on the qualitative learn<strong>in</strong>g from this evaluation, a further study to determ<strong>in</strong>e and quantitativelymeasure degrees of women’s progress across and with<strong>in</strong> services aga<strong>in</strong>st previously determ<strong>in</strong>ed<strong>in</strong>dicators (see above).• <strong>Research</strong> will be needed to explore the impact of <strong>in</strong>dividual budgets and their contribution towardsmov<strong>in</strong>g the needs of women <strong>in</strong> medium secure services <strong>in</strong>to ma<strong>in</strong>stream provision.8.3 Review<strong>in</strong>g the Service SpecificationThe f<strong>in</strong>d<strong>in</strong>gs from the evaluation suggest that there are a number of ways <strong>in</strong> which the Service Specificationcould now be updated to reflect the learn<strong>in</strong>g from dedicated women’s medium secure services s<strong>in</strong>ce the91
Implementation Guidance was published. Here we have not addressed every part of the specification butidentify a number of specific areas which would benefit from review.• Environmental security provided by the built environment, wherever possible, rather than perimeterfences and specifically address ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g an environment that reduces as far as possible the capacity forserious self‐harm:Due to the new Standards for MSUs, there is now a requirement for a 5.2 metre perimeter fence for allmedium secure units, <strong>in</strong>clud<strong>in</strong>g women’s services. However, environmental security is still important andshould be emphasized especially due to the risk of self harm.• Access is also required to non‐specialist, non‐secure services <strong>in</strong>clud<strong>in</strong>g acute <strong>in</strong>patient and communitysett<strong>in</strong>gs (e.g. assertive outreach teams, high support community residential placements) that will acceptwomen with challeng<strong>in</strong>g/offend<strong>in</strong>g/self‐harm<strong>in</strong>g behaviours.Care pathways for women were still problematic with few gender specific services available outside secureservices, and services that accept patients be<strong>in</strong>g transferred/discharged from secure services were oftenmale dom<strong>in</strong>ated. The Specification should <strong>in</strong>clude clearly identified gender specific care pathways for thosewomen requir<strong>in</strong>g women only sett<strong>in</strong>gs.• Forensic community teams: These should be multi‐discipl<strong>in</strong>ary and <strong>in</strong>clude <strong>in</strong>put from the follow<strong>in</strong>gdiscipl<strong>in</strong>es: psychiatry, psychology, psychotherapy, social work, occupational therapy and nurs<strong>in</strong>g. Sessional<strong>in</strong>put from other services/discipl<strong>in</strong>es such as substance misuse and eat<strong>in</strong>g disorders may be required. Itmay be appropriate to arrange secondments from learn<strong>in</strong>g disabilities/ rehabilitation/probation services to<strong>in</strong>crease the range of experience, the likelihood of recruitment and the capacity for <strong>in</strong>ter‐agency liaison.There was an issue for women <strong>in</strong> out of area treatment services (OATS) who require ongo<strong>in</strong>g support ofCommunity Forensic teams especially restricted patients who are likely to get conditional dischargesupervised by Community Forensic Teams (CFTs), as they may be disadvantaged if local teams andresponsible cl<strong>in</strong>icians not <strong>in</strong>volved <strong>in</strong> their current treatment/care plann<strong>in</strong>g.• Outreach – consultation, liaison and crisis <strong>in</strong>terventionSupport to: crim<strong>in</strong>al justice system: probation service (<strong>in</strong>clud<strong>in</strong>g bail and probation hostels), courts andprisons; (Women still not be<strong>in</strong>g appropriately diverted from CJS, and usually remanded to prison evenwhen clear history of mental illness, also <strong>in</strong>adequate <strong>in</strong> reach <strong>in</strong>to women prisons, and delays <strong>in</strong> transfersto hospital sett<strong>in</strong>gs.This area needs strengthen<strong>in</strong>g <strong>in</strong> light of the Corston Report and forthcom<strong>in</strong>g Bradley review.• Private sector/out‐of‐area placements.Currently women <strong>in</strong> out of area placements are not always regularly visited by local area team and carecoord<strong>in</strong>ators. There is a need for the specification to make clear that women placed out of area need a carecoord<strong>in</strong>atorto be regularly <strong>in</strong>volved <strong>in</strong> their CPA care plann<strong>in</strong>g and to identify future care pathway optionsat time of referral to out of area hospital, as well as agree<strong>in</strong>g fund<strong>in</strong>g with PCTs/LAs once women ready tomove on.• Assessment and care plann<strong>in</strong>g:Assessment should <strong>in</strong>form a formal care plann<strong>in</strong>g process under CPA.The importance of <strong>in</strong>volv<strong>in</strong>g women <strong>in</strong> CPAs should be <strong>in</strong>cluded <strong>in</strong> the specification <strong>in</strong> l<strong>in</strong>e with newguidance from CSIP on refocus<strong>in</strong>g CPA. ‘Assessments should <strong>in</strong>clude rout<strong>in</strong>e exploration of histories ofabuse, and care plans should take such experiences <strong>in</strong>to account to ensure provision of appropriate92
therapeutic <strong>in</strong>terventions, <strong>in</strong>form<strong>in</strong>g relational approaches and to protect survivors of abuse from risk of reenactmentof abuse and re‐traumatisation’ (as already referenced CSIP 2008 Refocus<strong>in</strong>g CPA).• Treatment and cont<strong>in</strong>u<strong>in</strong>g careTeams should provide a therapeutic and non‐<strong>in</strong>stitutionalised ethos which consistently <strong>in</strong>corporates a highlevel of relational security <strong>in</strong> all areas of the unit, e.g. ward activity areas and psychological therapysett<strong>in</strong>gs.A written policy would ensure consistency of practice.• Community follow‐up of all women discharged from secure care <strong>in</strong>clud<strong>in</strong>g those who do not requiresecure placement, but whose behaviours are too unusual/severe to be conta<strong>in</strong>ed by local general mentalhealth teams, and those with established forensic/offend<strong>in</strong>g problems and mental illness/personalitydisorder.At the present time Community Forensic Teams are often only funded to work with conditionally dischargedpatients, and are not available <strong>in</strong> all areas.• Operational policies and proceduresPolicies and procedures should <strong>in</strong>clude the follow<strong>in</strong>g:Clarity regard<strong>in</strong>g the operational management of an environment with a high level of relational security.A written policy will aid consistency of practice <strong>in</strong> this area and essential to protect women at risk of suicideself harm as well as aggressive behaviour.• Staff supportThis should be <strong>in</strong>tegral to the organisation of services and <strong>in</strong>clude supervision, space for reflective practiceand access to work‐related confidential counsell<strong>in</strong>g and crisis support.The case studies showed often limited resources available to implement supervision policies. Thespecification needs strengthen<strong>in</strong>g to ensure adequate resources are made available for staff supervisionand support <strong>in</strong> women’s services.82 Parry‐Crooke, G. Oliver, C. & Newton, J. (2000) Good Girls: surviv<strong>in</strong>g the secure system WISH/University of NorthLondon83 EOC (2004) Improv<strong>in</strong>g service delivery for disadvantaged adults Equal Opportunities Commission84 CSIP (2008) Refocus<strong>in</strong>g the Care Programme Approach85 Tucker, S. & Ince, C. (2008) op.cit.93
Appendix 1: Evaluation methodology1. Overview of the evaluation:The evaluation was designed to ensure maximum participation from all key stakeholder groupsthrough the study of both the development and delivery of secure services for women as well as theimpact they have on women’s current and future lives. The design <strong>in</strong>corporated a multi‐methodapproach mak<strong>in</strong>g use of both quantitative and qualitative data collection methods to enable betterunderstand<strong>in</strong>g of the breadth of issues across services as well as offer<strong>in</strong>g <strong>in</strong>‐depth and detailedexploration with<strong>in</strong> a number of case study sites. Women patients were <strong>in</strong>volved <strong>in</strong> determ<strong>in</strong><strong>in</strong>g thef<strong>in</strong>al design through participation <strong>in</strong> prelim<strong>in</strong>ary discussions as well as the use of repertory gridanalysis which identified key issues as they perceived them. The design offered a number of ways totriangulate data as well as to further <strong>in</strong>crease <strong>in</strong>ternal validity through evaluator‐triangulation. Keycomponents were the collection of <strong>in</strong>formation from all secure services for women about policiesand practices <strong>in</strong> place; <strong>in</strong>terviews with women patients and other stakeholders; and consider<strong>in</strong>g the‘future’ for women <strong>in</strong> relation to recovery and rehabilitation. The methods of data collection andtreatment allowed for analysis with<strong>in</strong> and across data sets.2. Evaluation design:In plann<strong>in</strong>g the design of this evaluation, we wanted to ensure women service users were <strong>in</strong>volvedfrom the outset and played a role <strong>in</strong> def<strong>in</strong><strong>in</strong>g “what works for them” <strong>in</strong> terms of service delivery. Theevaluation was concerned with both process (the development and delivery of services) andoutcomes (the difference these services make to women patients’ progress and recovery). The studyset out to use a multi‐method approach <strong>in</strong>clud<strong>in</strong>g:1. Postal pro‐forma cohort survey to all women‐only medium secure services2. Establishment of unit/evaluation team Liaison Groups (<strong>in</strong>clud<strong>in</strong>g representation from women)3. Two stage qualitative study of women patients’ perceptions and views us<strong>in</strong>g Repertory GridInterview<strong>in</strong>g Techniques4. Semi‐structured <strong>in</strong>terview survey of other stakeholders5. Rank order<strong>in</strong>g exercise to measure consensus between women patients’ perceptions of “whatworks for them” and those of service providers6. Documentary review of policies and protocols7. Documentary review and audit of CPA reviews of women patients to exam<strong>in</strong>e evidence of their<strong>in</strong>volvement and gauge their progress towards discharge and recoveryWhile the evaluation adopted a case study approach enabl<strong>in</strong>g detailed data collection about theselected services, multi‐methods allowed greater access to the breadth of <strong>in</strong>formation and learn<strong>in</strong>gavailable (across all sites). The evaluation was approved by the South East Multi‐site <strong>Research</strong> EthicsCommittee <strong>in</strong> 2006. The methods are described and reviewed below.3. Evaluation participantsThe evaluation aimed to reflect the holistic ethos which underp<strong>in</strong>ned the reprovision of secureservices for women by <strong>in</strong>volv<strong>in</strong>g the full range of stakeholders <strong>in</strong> contribut<strong>in</strong>g to the study. The proformasurvey was sent to managers of all services and we received completed questionnaires from14 of (the then total number of) 20 providers (70%). At the end of the evaluation, we followed up allservices with a telephone survey <strong>in</strong>clud<strong>in</strong>g seven new ones and received a 100% response.We sought access and permission to conduct <strong>in</strong>‐depth case studies with six units. The f<strong>in</strong>al selectionwas based on the <strong>in</strong>formation provided through the postal pro‐forma survey of all units <strong>in</strong> Englandand guidance from the Evaluation Advisory Group, tak<strong>in</strong>g the follow<strong>in</strong>g criteria <strong>in</strong>to consideration:94
• regional spread of units• legal status of patients, i.e. civil patients via mental health system, or admitted viacourts/prison• ethnic group of women patients• age of women patients• unit cater<strong>in</strong>g for women with learn<strong>in</strong>g disabilitiesKey stakeholder groups who participated <strong>in</strong> the case studies <strong>in</strong>cluded:Women patients: we <strong>in</strong>volved 50 women <strong>in</strong> the evaluation represent<strong>in</strong>g 34% of women provided forby the case study services at the time and 13% of women patients across all women’s mediumsecure services <strong>in</strong> England. Characteristics of women participants are described below.Table 8: Characteristics of women service users participat<strong>in</strong>g (n=50)CharacteristicNumberAge ranges: Under 25 825‐34 1435‐44 1145‐54 655+ 1Not known 10Ethnicity: White BR 31Black BR 3Asian 30ther 3Not known 10Length of stay: under 6 months 96 months to 1 yr 101 – 2 years 132 – 5 years 35 – 10 years 5Not known 10Staff of secure services: Between eight and ten staff and other professionals were <strong>in</strong>vited toparticipate from each site and we met with a total of 65 <strong>in</strong>dividuals. In some cases, we were able tomeet as many people as were <strong>in</strong>terested or could f<strong>in</strong>d time with up to 15 <strong>in</strong> one area. In others,logistics and cancellations made it more difficult to achieve more than eight people.Table 9: Roles of professionals participat<strong>in</strong>gRoleNumberMedical directors; Cl<strong>in</strong>ical Lead/service manager; RMOs 14Psychologists 8Occupational Therapists; Teachers 6Social workers 3Ward/unit managers 8Qualified nurs<strong>in</strong>g staff 10HCAs/support workers 6Advocates; service user <strong>in</strong>volvement staff 4Commissioners 3Total 6295
Two Modern Matrons and a Community Team Manager participated <strong>in</strong> a group discussion. We wereparticularly keen to <strong>in</strong>volve staff work<strong>in</strong>g most closely on a day‐to‐day basis with women and overhalf of those <strong>in</strong>terviewed were nurses, support staff and OTs.4. Data Collection and stakeholder <strong>in</strong>volvement4.1 Postal pro‐forma survey of all women‐only secure services:This survey was conducted across all women’s secure services <strong>in</strong> England to ascerta<strong>in</strong> <strong>in</strong>formation onservices’ facilities. The purpose of the survey was to ensure that the evaluation maximised thepotential understand<strong>in</strong>g about current service use and practices across the range and diversity ofsecure services for women. Detailed case study material was analysed with<strong>in</strong> this wider context. Thesurvey covered a variety of topics <strong>in</strong>clud<strong>in</strong>g:• <strong>in</strong>formation about admission and discharge rates, case mix, legal status of patients, age, ethnicgroup, average length of stay• range, frequency/<strong>in</strong>tensity and take‐up of treatment and activities provided• provision and nature of gender awareness tra<strong>in</strong><strong>in</strong>g for staff• arrangements for women patients’ <strong>in</strong>volvement <strong>in</strong> <strong>in</strong>dividual care plann<strong>in</strong>g as well as• service plann<strong>in</strong>g and development• availability of <strong>in</strong>dependent advocacy, <strong>in</strong>clud<strong>in</strong>g the <strong>in</strong>volvement of WISHThe pro‐forma also requested <strong>in</strong>formation about the range and content of policies <strong>in</strong> place, forexample, for the management of self‐harm, sexuality/relationships, and manag<strong>in</strong>g aggression. Thepostal survey further served to canvass services about their <strong>in</strong>terest <strong>in</strong> and ability to participate asone of a number of case studies for the evaluation. In particular, it asked about arrangements foruser <strong>in</strong>volvement at the service and other relevant <strong>in</strong>formation required for selection of the servicefor the ma<strong>in</strong> study, e.g. length of time established, admission criteria, legal status and care‐path ofpatients, women’s ethnic group, age and mental health classification.On reflection:The pro‐forma served an important purpose <strong>in</strong> alert<strong>in</strong>g services to the evaluation. However, <strong>in</strong> orderto achieve a reasonable return, we began by identify<strong>in</strong>g an appropriate staff member by telephonebut still had to give considerable time follow<strong>in</strong>g up where the questionnaire was with<strong>in</strong> a service. Insome cases and despite repeated calls and emails, we did not receive a response. A telephonesurvey might have been more successful <strong>in</strong> elicit<strong>in</strong>g the data and <strong>in</strong>creas<strong>in</strong>g response.4.2 Secure Service Liaison Groups:We had hoped to establish a group for each unit to be <strong>in</strong>cluded <strong>in</strong> the ma<strong>in</strong> study with service userrepresentation, as well as members of multi‐discipl<strong>in</strong>ary teams, and service managers. The purposeof these groups was to contribute to the development of data collection <strong>in</strong>struments and evaluationprocedures to ensure they are sensitive to environmental and cultural factors and provide an‘access’ po<strong>in</strong>t and opportunities for <strong>in</strong>formation through‐flow from the evaluation team to staff andwomen patients throughout the <strong>life</strong> of the study.Where service user groups were operat<strong>in</strong>g, we were <strong>in</strong>vited to discuss the evaluation with groupmembers (or their representatives) as well as address any queries women raised.On reflection:The reality of the liaison groups was such that we worked with service/unit managers and groupdiscussions tended to be ad hoc. What proved essential was to have a l<strong>in</strong>k person <strong>in</strong> each area who96
could facilitate our access to both women service users and those work<strong>in</strong>g with them. Attend<strong>in</strong>gservice user groups slowed the process of data collect<strong>in</strong>g. However, they offered an opportunity tomeet with women <strong>in</strong>formally, discuss the evaluation with them and meant that on return<strong>in</strong>g toconduct <strong>in</strong>terviews, many were familiar with who we were. We provided written as well as verbal<strong>in</strong>formation at this and other po<strong>in</strong>ts <strong>in</strong> the process as agreed with the MREC and service providers. Inone case study area, women compla<strong>in</strong>ed about the paper overload.4.3 Elicit<strong>in</strong>g the perceptions/views of women patients:This aspect of the evaluation focused on what women found helpful <strong>in</strong> keep<strong>in</strong>g them <strong>safe</strong> andsupport<strong>in</strong>g their recovery. Women patients were <strong>in</strong>vited to participate <strong>in</strong> prelim<strong>in</strong>ary and follow‐up<strong>in</strong>‐depth <strong>in</strong>terviews. The purpose of these <strong>in</strong>terviews was to learn about secure services from theperspective of women patients. Where a service was new or recently established, this approachprovided useful learn<strong>in</strong>g as part of process evaluation.In the first <strong>in</strong>stance, we used repertory grid <strong>in</strong>terviews to elicit the views of women patients, atechnique developed by psychologist George Kelly 86 <strong>in</strong> the 1950s, as a means of study<strong>in</strong>g an<strong>in</strong>dividual’s personal ‘constructs’ or perceptions and how they discrim<strong>in</strong>ated between different‘elements’ <strong>in</strong> their environment enabl<strong>in</strong>g them to anticipate events and make sense of theirexperiences. The most recent edition of the Handbook of Repertory Grid Techniques 87 firstpublished <strong>in</strong> 1977, gives many examples of the different contexts <strong>in</strong> which the technique is nowsuccessfully used both <strong>in</strong> cl<strong>in</strong>ical and research fields and, for example, describes its value as a tool forexplor<strong>in</strong>g the personal constructs and evaluatory processes of people with learn<strong>in</strong>g disabilities, andgives examples of its use with<strong>in</strong> forensic sett<strong>in</strong>gs.Dur<strong>in</strong>g the repertory grid <strong>in</strong>terviews both the elements, i.e. those people that the woman viewed asimportant to her care at the unit, and the constructs, i.e. how the woman discrim<strong>in</strong>ates betweendifferent elements, were elicited from the women. Personal constructs were elicited by present<strong>in</strong>gtriads of elements, usually people (chosen by a random method) and ask<strong>in</strong>g the woman to expla<strong>in</strong>how two of these elements were similar, but different from the third.The selection of women patients for <strong>in</strong>terview <strong>in</strong>cluded some consultation with the MDT to ensurevulnerability and security issues are considered. In the ma<strong>in</strong>, we <strong>in</strong>cluded mostly women patientswho had already had their first CPA review s<strong>in</strong>ce admission to the unit so they had sufficientexperience of the service be<strong>in</strong>g evaluated. However, we also issued an open <strong>in</strong>vitation, ask<strong>in</strong>gwomen to <strong>in</strong>dicate whether they had had a CPA review as it was helpful to <strong>in</strong>clude some patientswho were new to the service and from whom we learned a great deal from <strong>in</strong>itial and follow up<strong>in</strong>terviews.On reflection:The repertory grid <strong>in</strong>terviews offered a different way of <strong>in</strong>volv<strong>in</strong>g women <strong>in</strong> shap<strong>in</strong>g the evaluationas well as f<strong>in</strong>d<strong>in</strong>g out about their experience of services. Direct question<strong>in</strong>g would not have providedthe same <strong>in</strong>sights and some women commented that the technique had given them different waysof look<strong>in</strong>g at how they perceived people who were important <strong>in</strong> help<strong>in</strong>g or h<strong>in</strong>der<strong>in</strong>g their recoveryand f<strong>in</strong>d<strong>in</strong>g connections between them. The <strong>in</strong>terviews <strong>in</strong>volved a ‘card game’ with coloured cardsthat were shuffled and represented <strong>in</strong> different triads to women. A small number of women foundthe process difficult and could not complete the whole process. However, most were engaged andwith breaks, some women spent up to an hour and a half <strong>in</strong> discussion.4.4 Semi‐structured <strong>in</strong>terviews with other stakeholders:We believed that the <strong>in</strong>volvement of other stakeholders was of vital importance to the evaluation <strong>in</strong>order to generate as full a picture as possible of how secure services for women function.97
Participants <strong>in</strong> this aspect of the evaluation <strong>in</strong>cluded cl<strong>in</strong>icians, support staff, advocates, servicemanagers, multi‐discipl<strong>in</strong>ary team members and service commissioners. These <strong>in</strong>terviews focusedon their views and experience of provid<strong>in</strong>g differentiated care and treatment to women patients (i.e.a gender specific/sensitive service) <strong>in</strong>clud<strong>in</strong>g provision of <strong>in</strong>terventions to address the specific needsof women patients l<strong>in</strong>ked to their experience of gender and other <strong>in</strong>equalities (e.g. self‐harm, sexualabuse histories, racism).The <strong>in</strong>terviews <strong>in</strong>cluded questions about the <strong>in</strong>volvement of women <strong>in</strong> their assessment and careplann<strong>in</strong>g, gender awareness tra<strong>in</strong><strong>in</strong>g undertaken and the unit’s approach to relational security andhow they view this is work<strong>in</strong>g. A core set of topics relevant to all stakeholders were developed withadditional topics specific to the range of <strong>in</strong>dividuals/areas represented with<strong>in</strong> the sample.On reflection:These <strong>in</strong>terviews provided an essential source of data which contributed to the evaluation ofservices. Women’s experiences and view alone would not have sufficed as the organisational andagency issues were central to women’s potential recovery. They also provided an opportunity toreflect women service users’ views back to professionals as described <strong>in</strong> 4.5 below.4.5 Measur<strong>in</strong>g consensus between service users and other stakeholders:In order to identify where there was consensus of views and perceptions, a content analysis wascarried out of the personal constructs elicited from the repertory grid <strong>in</strong>terviews with womenpatients. Their personal constructs were grouped to identify the key themes expressed by women.The 12 most featured construct types formed a list of the service attributes perceived to be mostimportant to women patients. Women patients (at a follow‐up <strong>in</strong>terview), staff and otherstakeholders <strong>in</strong>volved <strong>in</strong> the semi‐structured <strong>in</strong>terviews, were asked to rank these from 1 to 10 <strong>in</strong>order of importance to them. Staff ranked the 10 constructs accord<strong>in</strong>g to what they believed to bemost important for women patients. A comparison of the rank order<strong>in</strong>g was used to illustrate thedegree of shared understand<strong>in</strong>g of aspects of the service that women value or f<strong>in</strong>d helpful.4.6 Documentary review of policies, protocols and guidel<strong>in</strong>es/facilities audit:A checklist and audit document were <strong>in</strong>tended for use to review relevant policies and procedures ateach unit, e.g. relational security, as well as an audit checklist of the physical environment and thefacilities at each unit. Case study services provided policy and procedure documents. However, <strong>in</strong>the event, we did not conduct a systematic audit of facilities and the environment.On reflection:This aspect of the evaluation was not as successful as we had envisaged and may have been overambitious.While the case study services made us welcome and provided a high level of assistance <strong>in</strong>facilitat<strong>in</strong>g access, an environmental audit was yet one more request. The <strong>in</strong>terviews with womenand professionals asked about the physical environment and the feedback was <strong>in</strong>structive.4.7 Review<strong>in</strong>g progress of women patients and discharge plann<strong>in</strong>g:In addition to seek<strong>in</strong>g women’s own views and <strong>in</strong> order to more fully understand their <strong>in</strong>volvement<strong>in</strong> the care process, their progress was addressed by seek<strong>in</strong>g the consent of those woman alreadyparticipat<strong>in</strong>g <strong>in</strong> the study for the evaluation team to access to their CPA review and DischargePlann<strong>in</strong>g documentation dur<strong>in</strong>g the study period. A checklist and audit tool were designed<strong>in</strong>corporat<strong>in</strong>g the CPA monitor<strong>in</strong>g and audit checklist and the SCMH/MHAC CPA audit document 88 ,along with appropriate gender specific requirements and measures of user <strong>in</strong>volvement. This<strong>in</strong>cluded the key recommendations for action on <strong>in</strong>dividual assessment and care plann<strong>in</strong>g made <strong>in</strong>section 5.1 of Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women’s Mental <strong>Health</strong> Implementation Guidance. Theanalysis of CPA review documentation was undertaken on site dur<strong>in</strong>g the f<strong>in</strong>al visit.98
On reflection:This aspect of the evaluation required seek<strong>in</strong>g women’s consent for a f<strong>in</strong>al time, the consent of theMDT and then f<strong>in</strong>d<strong>in</strong>g opportunities to access paper and/or on l<strong>in</strong>e files. Whilst <strong>in</strong>terest<strong>in</strong>g as anexercise, what it revealed was someth<strong>in</strong>g about the women but more about the way <strong>in</strong> which casenotes were kept and CPA reviews carried out. The data was not sufficiently robust to drawconclusions <strong>in</strong> this context.5. Recruitment and access to <strong>in</strong>formationThere were a number of issues that needed to be addressed when develop<strong>in</strong>g appropriate routes<strong>in</strong>to the evaluation for participants. It was vital that both women, staff/members of multidiscipl<strong>in</strong>aryteams and other stakeholders were clear about how the evaluation was to be conductedand what it was hoped would emerge from it. The follow<strong>in</strong>g ‘ground rules’ were employed <strong>in</strong> theplann<strong>in</strong>g and delivery of the evaluation.• Recognition that women patients <strong>in</strong> secure services are not a homogeneous group, althoughthey may share some common experiences and mental health needs. The evaluation may notprovide women from all services <strong>in</strong> England with the opportunity to provide the detail of theirexperiences, however a broad cross section of women will be able to participate.• Awareness that many of the women patients have long‐term mental health disabilities and arevulnerable. Their <strong>in</strong>terests and welfare need to be <strong>safe</strong>guarded throughout the process.• Recognition and respect for the responsibilities of cl<strong>in</strong>ical and other staff <strong>in</strong> relation towomen’s <strong>safe</strong>ty and welfare.• Provision of a written statement for women patients, staff and others outl<strong>in</strong><strong>in</strong>g the purpose andconduct of the evaluation <strong>in</strong>clud<strong>in</strong>g the issues to be addressed, <strong>in</strong>formation about the proposedstrategy and with proposals for feed<strong>in</strong>g back the f<strong>in</strong>d<strong>in</strong>gs. It will also be important to ensure thatwomen fully understand that while their views will be listened to, there is no guarantee thatthey will be implemented.• Provision of written <strong>in</strong>formed consent demonstrat<strong>in</strong>g that women and staff understand thenature and purpose of their participation <strong>in</strong> the evaluation.• An explicit understand<strong>in</strong>g of the confidentiality guidel<strong>in</strong>es that will regulate the evaluation, e.g.that women can express their views where staff are not present; that the f<strong>in</strong>d<strong>in</strong>gs will beconfidential to the evaluators, that they will be provided to the National Oversight Group andothers <strong>in</strong> an aggregated and anonymised form and that while quotation may be used to illustratestakeholders views, no <strong>in</strong>dividual will be identifiable from any report.• Provision of an environment where all parties feel <strong>safe</strong> and comfortable, where women canchoose to withdraw at any time and that evaluators are able to offer appropriate responses andsupport to women who raise queries and concerns or become distressed.In addition to these ‘ground rules’, it was important to demonstrate good practice <strong>in</strong> the follow<strong>in</strong>gways:• by ensur<strong>in</strong>g that women patients and staff/multi‐discipl<strong>in</strong>ary team members and otherstakeholders see that this exercise can be conducted <strong>in</strong> an accessible way, where jargon isavoided and language or literacy do not act as barriers to participation• by us<strong>in</strong>g methods which are flexible and reflexive allow<strong>in</strong>g for full exploration of issues andconcerns raised• by be<strong>in</strong>g open to receiv<strong>in</strong>g <strong>in</strong>formation and views of women patients <strong>in</strong> particular through anywritten or verbal forms other than those proposed here.99
6. Data analysisThe analysis of data collected for the evaluation reflected the multi‐method approach describedhere.Various specialist software programmes are now available for the analysis of the repertory grid data,many of which are available freely as shareware (e.g. INGRID, FLEXIGRID, WEBGRID, GRIDSTAT).Richard Bell 89 also provides detailed guidance and <strong>in</strong>structions for undertak<strong>in</strong>g both s<strong>in</strong>gle andmultiple grid analysis us<strong>in</strong>g a range of features and facilities available <strong>in</strong> SPSS such as cluster analysis.While we reviewed the various programme options available, we decided to use the sharewareprogramme GRIDSTAT as it provided the most straightforward solution to data preparation and<strong>in</strong>put and gave us a range of pre‐programmed analysis options that met our requirements <strong>in</strong>clud<strong>in</strong>ganalysis of variance (ANOVA) and cluster analysis. A content analysis of the personal construct datawas undertaken by the research team, to compile a list of the 10 most frequent constructtypes/themes given by women patients for use <strong>in</strong> the rank order<strong>in</strong>g exercise, to measure the degreeof shared understand<strong>in</strong>g between staff and women patients about ” what works” for the women.The qualitative data generated from <strong>in</strong>‐depth <strong>in</strong>terviews with staff and other stakeholders as well asfrom the follow up <strong>in</strong>terviews with women patients was stored as anonymised Word files andanalysed us<strong>in</strong>g Framework 90 . Framework offers a means of conduct<strong>in</strong>g with<strong>in</strong> and across caseanalysis. Through a process of identify<strong>in</strong>g common themes and chart<strong>in</strong>g data with<strong>in</strong> these themes, arobust and comprehensive analysis is provided.86 Kelly G. (1955) The Psychology of Personal Constructs, New York, W.W. Norton87 Fransella F. (2004) Handbook of Repertory Grid Technique Wiley88 Sa<strong>in</strong>sbury Centre for Mental <strong>Health</strong> (2005) Brief<strong>in</strong>g 29 “The Care Programme Approach – Back on Track”London, SCMH89 Bell R. (1997) “Us<strong>in</strong>g SPSS to Analyse Repertory Grid Data” Melbourne, University of Melbourne90 Ritchie,J & Lewis J (2004) Qualitative <strong>Research</strong> Practice Sage100
7. Topic guides and research toolsSizes of boxes for comments and font sizes have been reduced for reproduction reasons.7.1 Pro‐forma survey to dedicated women’s medium secure servicesEvaluation of Women’s Secure Services:Questionnaire for Providers of medium secure services with women‐only wardsBackground:The National Programme on Forensic Mental <strong>Health</strong> R&D has commissioned this evaluation on behalf of theDepartment of <strong>Health</strong>’s National Oversight Group which oversees the secure mental health sector.Reorganisation of secure mental health services is underway nationally <strong>in</strong> l<strong>in</strong>e with the NHS Plan 1 . This<strong>in</strong>cludes a programme of accelerated discharge of patients from high secure hospitals with women deemed apriority. As part of the reprovision of services, a national network of secure dedicated NHS services for womenis be<strong>in</strong>g established, with currently just under 200 beds nation‐wide. Other mental health services for womenbe<strong>in</strong>g developed <strong>in</strong>clude women‐only self‐conta<strong>in</strong>ed <strong>in</strong>patient wards, crisis houses, and high supportcommunity residential services.Ma<strong>in</strong>stream<strong>in</strong>g Gender and Women’s Mental <strong>Health</strong>: Implementation Guidance 2 <strong>in</strong>cludes a specification fordedicated secure services for women, identify<strong>in</strong>g the need for a gender sensitive approach. It alsorecommends an evaluation of these new dedicated secure services to assess whether they are deliver<strong>in</strong>g care,support and treatment that meet the specific needs of women, as well as ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g women’s <strong>safe</strong>ty andsecurity.The evaluation has been designed to determ<strong>in</strong>e the extent to which the new women’s secure services are:• Deliver<strong>in</strong>g differentiated care, support and treatment to meet the specific needs of women;• Ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g women’s psychological and physical <strong>safe</strong>ty;• Facilitat<strong>in</strong>g the recovery process for women patients, <strong>in</strong>clud<strong>in</strong>g their rehabilitation and positiveresettlement <strong>in</strong> the community with an appropriate level of support.Women‐only secure services to be evaluated <strong>in</strong>clude:• NHS self‐conta<strong>in</strong>ed women‐only units where either there are no male wards on site or women do not mixwith male patients from other wards.• NHS self‐conta<strong>in</strong>ed women‐only secure units where there is some level of mix<strong>in</strong>g with male patients, forexample dur<strong>in</strong>g off‐ward activities and/or at the rehabilitation stage.• Independent sector and “not for profit” services (these are ma<strong>in</strong>ly stand alone services).Survey of all women‐only medium secure services <strong>in</strong> England (NHS and Independent)As the first stage of the evaluation, this questionnaire has been sent to all providers of medium secure care <strong>in</strong>women‐only wards/sett<strong>in</strong>gs.Complet<strong>in</strong>g this questionnaire:Part A: To be completed by Manager or Cl<strong>in</strong>ical Lead for women’s servicesPart B: To be completed for each women‐only ward by person responsible e.g. Ward ManagerReferences:1. Department of <strong>Health</strong> (2000) The NHS Plan, London, DH2. Department of <strong>Health</strong> (2003) Ma<strong>in</strong>stream<strong>in</strong>g Gender & Women’s Mental <strong>Health</strong>: Implementation Guidance,London, DH101
QUESTIONNAIRE A: ABOUT THE SERVICEYou have been asked to complete this questionnaire because of your overall knowledge about secureprovision to women. You are probably the Manager or Cl<strong>in</strong>ical Lead for women’s services.Please contact us if you have any queries:Georgie Parry‐Crooke: Tel: 020 7133 5092 Email: g.parry‐crooke@londonmet.ac.ukPenny Stafford: Tel: 01904 421460 Email: penny@walkerhill.co.ukA1. General Information about Service Provider:Hospital/Unit Name:Name of NHS Trust:OrOrganisation Nameif Independent provider:Name and position ofPerson complet<strong>in</strong>g thisQuestionnaire:Please provide yourContact telephoneNumber and emailA2. Are you a provider of Women’s Secure Services?Please confirm that you provide a secure mental health service that is either only for women patients, or thathas at least one women‐only ward that can meet the security needs of women patients assessed as requir<strong>in</strong>gmedium secure care.YesNo (In this case this survey does not apply, and we do not need you to answer anyfurther questions, but please return this questionnaire <strong>in</strong> the enclosed pre‐paid envelopeso we can amend our records).A3. If yes: Is your women’s secure service:A self‐conta<strong>in</strong>ed women‐only secure unit with no male wards on site.Self‐conta<strong>in</strong>ed women‐only unit/ward(s) on a site where there are male wards butwhere women patients do not mix at all with men patients from other wards on siteSelf‐conta<strong>in</strong>ed women‐only unit/ward(s) on a site where there are male wards andwhere there is some level of mix<strong>in</strong>g between women and men patients, for exampledur<strong>in</strong>g off‐ward activities and/or at the rehabilitation stage.A4. Policies and procedures for women’s secure unit/ward(s)(i)Which of the follow<strong>in</strong>g policies are <strong>in</strong> place with<strong>in</strong> your women’s secure service(s)102
Management of self harmManagement of aggressionSexuality and relationshipsAnti‐Bully<strong>in</strong>g or harassmentImplementation of Relational SecurityChild visit<strong>in</strong>gEqualities and diversityAny other policies you would like us to know about?[Please attach a copy of your policies if possible](ii)Which policy/policies best represents the efforts of your women’s secure service? Why?(iii)What do you th<strong>in</strong>k most helps the implementation of policies with<strong>in</strong> your women’s secure service?(iv)What do you th<strong>in</strong>k most h<strong>in</strong>ders the implementation of policies with<strong>in</strong> your women’s secure service?A5. Service User Involvement and Advocacy:(i)How does your service encourage or enable women patients to be <strong>in</strong>volved the formal CPA (CarePlann<strong>in</strong>g Approach) process?(ii)What proportion of CPA review meet<strong>in</strong>gs are attended by women patients?Please give or estimate %(iii)Are women patients generally <strong>in</strong>vited to attend the whole CPA review meet<strong>in</strong>g, orjust part of the meet<strong>in</strong>g?Yes patients are generally <strong>in</strong>vited to attend their full CPA review meet<strong>in</strong>g103
Patients are generally only <strong>in</strong>vited to attend part of their CPA review meet<strong>in</strong>gPatients are generally not <strong>in</strong>vited to attend their CPA review meet<strong>in</strong>gs.(iv)Are women patients encouraged to submit their own written report for their CPA review?YesNo(v)Are women patients <strong>in</strong>volved <strong>in</strong> their risk assessment process?Yes, women patients are generally <strong>in</strong>volved <strong>in</strong> their own risk assessmentNo, women patients are not usually <strong>in</strong>volved <strong>in</strong> their own risk assessment(vi)Are women patients <strong>in</strong>vited to sign their completed risk assessment documents?YesNo(vii)Have you <strong>in</strong>troduced any gender specific risk assessment procedures for your women’s secureservice?YesNo(viii)Are <strong>in</strong>dependent advocates available to support women with their CPA reviews?YesNo(ix)Is <strong>in</strong>dependent gender specific advocacy available to your women patients?YesNo, but there is an <strong>in</strong>dependent advocacy service available for our patientsNo, there is currently no <strong>in</strong>dependent advocacy service available for our patients(x)Are patients’ councils, self‐advocacy or user groups established for patients?Yes, ward‐based group(s) establishedYes, across site group(s) establishedNo, there are currently no user or self‐advocacy groups at this hospital104
(xi)Do women patients participate <strong>in</strong> Cl<strong>in</strong>ical Governance at your hospital?YesNo(xii)Are arrangements <strong>in</strong> place for WISH (Women In Secure Hospitals) to make regular visits to yourwomen’s secure ward(s)?YesNoA6. Jo<strong>in</strong>t Work<strong>in</strong>g and External L<strong>in</strong>ks(i)Do you provide a forensic community team for women?YesNo (skip to question (iii))If Yes: Which discipl<strong>in</strong>es are represented on the team (e.g. psychiatry, psychology, etc)(ii) Is there regular liaison between the forensic community team and follow<strong>in</strong>g local CJS and health services?(Please tick all that apply)CourtsCourt and/or police diversion schemesPrisonsProbation serviceAdult mental health unitsCAMHS unitsLearn<strong>in</strong>g disability services(iii)Is there a risk assessed community <strong>in</strong>clusion programme available to your women patients <strong>in</strong> mediumsecure care?YesNoIf Yes: Please give details105
A7. Provision of Gender Awareness and/or Gender specific tra<strong>in</strong><strong>in</strong>g for staff:What percentage of the current staff group has received tra<strong>in</strong><strong>in</strong>g to specifically help them work well withwomen with mental health needs?Please give or estimate %Please tell us about the tra<strong>in</strong><strong>in</strong>g provided (e.g. date length of courses, topics covered, etc) and who attended(e.g. healthcare staff, MDT members etc), who was the tra<strong>in</strong><strong>in</strong>g provider, etc?A8. Number of women‐only secure wards?How many women‐only wards offer<strong>in</strong>g medium secure care are there at your unit/hospital?Write In NumberA9. Th<strong>in</strong>k<strong>in</strong>g of the service you currently offer to women requir<strong>in</strong>g medium secure care:What do you feel most proud of?What would you most like to change?A10. Participation <strong>in</strong> Case Studies for National Evaluation ProgrammeWe will be carry<strong>in</strong>g out detailed case studies over the next 18 months of at least six women‐only mediumsecure services as part of this national evaluation commissioned by the NHS National R&D Programme forForensic Mental <strong>Health</strong>. These will <strong>in</strong>volve researchers mak<strong>in</strong>g a number of visits to service sites, to <strong>in</strong>terviewmembers of multi‐discipl<strong>in</strong>ary teams, ward staff and women patients, to review policies and procedures, andwith patients’ consent, to review CPA documentation. (Full <strong>Research</strong> Ethics Committee Approval has beenobta<strong>in</strong>ed for this study.)Would your service like to be considered for <strong>in</strong>clusion <strong>in</strong> the case study phase of this evaluation programme?YesNot sure (please provide further <strong>in</strong>formation )NoTHANK YOU VERY MUCH FOR YOUR GENEROUS TIME AND EFFORT COMPLETING THIS QUESTIONNAIRE106
NOW PLEASE COMPLETE (OR ARRANGE FOR THE RELEVANT WARD MANAGER OR OTHER PERSON TOCOMPLETE) A PART B QUESTIONNAIRE FOR EACH OF THESE WOMEN’S WARDSPLEASE RETURN:Part A QuestionnairePart B Questionnaire (completed for each ward)Copies of relevant policies and other materialsTO:Hospital / Secure Unit Name:QUESTIONNAIRE B: ABOUT YOUR WARDYou have been asked to complete this questionnaire because of your knowledge about a ward provid<strong>in</strong>gsecure care to women on this site. You probably manage this wardPlease contact us if you have any queries:Georgie Parry‐Crooke: Tel: 020 7133 5092 Email: g.parry‐crooke@londonmet.ac.ukPenny Stafford: Tel: 01904 421460 Email: penny@walkerhill.co.ukB1. Ward Details(i)Ward name:(ii)Number of beds:(iii)Number of beds currently occupied:(iv)If there is a wait<strong>in</strong>g list how many women are wait<strong>in</strong>g for a bed:(v)Date Established:(If not known please write <strong>in</strong> approximately how long the ward has beenoperat<strong>in</strong>g as a women‐only secure service)(vi)What patient group does your ward cater for? (Please tick all that apply)Women diagnosed with mental illnessWomen diagnosed with Personality DisorderWomen with learn<strong>in</strong>g disabilitiesWomen with Complex Needs (e.g. more than one diagnosis)107
Women with challeng<strong>in</strong>g behaviourWomen diagnosed with Borderl<strong>in</strong>e Personality DisorderOther (write <strong>in</strong>) _____________________________________(vii)Does the ward have the follow<strong>in</strong>g?Seclusion roomQuiet/low stimulus area/roomWomen‐only secure outside spaceCrisis suite(s) i.e. bedroom, Day and bathroom area that are separate, or can be separated offChild/family visit<strong>in</strong>g areaWard lay‐out suitable for zonal observationWard environment designed to m<strong>in</strong>imise the capacity for serious self harm(viii)What percentage of ward staff time was spent keep<strong>in</strong>g women “under observation” <strong>in</strong> the lastmonth?Please give or estimate %B2. DETAILS OF ADMISSIONS OVER PAST 12 MONTHS(i)Over the past 12 months (or s<strong>in</strong>ce open<strong>in</strong>g if ward established for less than a year) how many patientshave been admitted to this ward (<strong>in</strong>clud<strong>in</strong>g transfers from other units/wards)Write <strong>in</strong> number:(ii)Please give a breakdown of admissions over past 12 months by legal status:Number on a Civil Order under Mental <strong>Health</strong> Act (i.e. Section, 2 or 3):Number on Court Order (i.e. section 35,36,37,38 ‐ <strong>in</strong>clud<strong>in</strong>g those withRestriction orders):Number of Prison Transfers (i.e. section 47, 48 ‐ <strong>in</strong>clud<strong>in</strong>g those withRestriction orders):108
(iii)Did you admit any women be<strong>in</strong>g transferred from a high security hospital dur<strong>in</strong>g the past 12 months?If Yes: Write <strong>in</strong> number:(iv)How many of the patients you admitted to the ward dur<strong>in</strong>g the past 12 months were subject torestriction orders (i.e. s41 or s49) under the Mental <strong>Health</strong> Act?Write <strong>in</strong> number:(v)Please give a breakdown of admissions to your ward dur<strong>in</strong>g the past 12 months by age group: (Write<strong>in</strong> number)20 or under:21 up to 25 years:26 up to 45 years:46 up to 60 years:61 and over:(vi)Please give a breakdown of admissions to your ward dur<strong>in</strong>g the past 12 months by ethnic group:(Write <strong>in</strong> number)White:Black (African/Caribbean):Black Asian:Mixed Ethnic group:Ch<strong>in</strong>eseOther ethnic group:(vii)How many patients have been discharged or transferred out from your ward dur<strong>in</strong>g past 12 months?Number discharged to community sett<strong>in</strong>g:Number transferred to lower secure sett<strong>in</strong>g:Number transferred to another mediumsecure sett<strong>in</strong>g:Number transferred back to prison:Number transferred to high securityhospital:109
(viii)Of the patients discharged or transferred from your ward <strong>in</strong> the past 12 months what was the averagelength of stay?Write <strong>in</strong> number of months:B3. Treatment and activities provided:(i)Please tick any of the follow<strong>in</strong>g <strong>in</strong>terventions, treatments and therapies that are available to yourpatients, and write <strong>in</strong> the percentage (estimate or actual) of women admitted to your ward who haveused them <strong>in</strong> the last year?Individual psychological therapyGroup therapyCreative therapies (e.g. art, drama)Complementary therapies (e.g. Massage, nutritional)Well‐women sessions & screen<strong>in</strong>g(ii)Is a programme of Dialectical Behaviour Therapy available to your patients?Yes.Yes.(Group)(Individual)No.(iii)Do you provide any other specialist therapy or group work for women, for example for those whoexperience eat<strong>in</strong>g distress, substance misuse, self <strong>in</strong>jury, or therapy to address patterns of offend<strong>in</strong>g(e.g. fire‐sett<strong>in</strong>g)Yes.No.If Yes: Please give details(iv)Has your ward <strong>in</strong>troduced a harm‐m<strong>in</strong>imisation or harm‐reduction approach to manag<strong>in</strong>g self‐<strong>in</strong>jury?Yes.No.110
(v)Which of the follow<strong>in</strong>g activities are available to your patients, and approximately what proportion ofwomen admitted to your ward have used them <strong>in</strong> the past year?Write <strong>in</strong> percentage (estimate or actual) of patients who used:Education sessions provided on‐siteEducation Courses off‐site (e.g. at local college)Vocational tra<strong>in</strong><strong>in</strong>g on‐siteVocational tra<strong>in</strong><strong>in</strong>g off‐siteWork placementsParent<strong>in</strong>g skills groups/tra<strong>in</strong><strong>in</strong>g<strong>Health</strong> promotion course/groupsCreative arts (e.g. pottery, artwork, crafts)Sports and exercise (e.g. basketball, gym, etc)Social events (e.g. quiz nights, etc)Community <strong>in</strong>clusion (e.g. leisure facilities, shops, etc)THANK YOU FOR YOUR TIME AND EFFORT COMPLETING THIS QUESTIONNAIREPlease return it to your service manager or whoever asked you to help by complet<strong>in</strong>g the form7.2 First <strong>in</strong>terview with women service usersEvaluation of Women’s Medium Secure Services: Repertory Grid Technique• Purpose of the evaluation: to learn about women and staff’s experiences and views of the secure service.To feed <strong>in</strong>to develop<strong>in</strong>g services <strong>in</strong> the future.• Who we are: not from the secure services but completely <strong>in</strong>dependent. All have spent a lot of time talk<strong>in</strong>gwith other women patients <strong>in</strong> secure sett<strong>in</strong>gs as part of research and evaluations.• Discussion is <strong>in</strong>formal: it will take between an hour and an hour and a half and is confidential.• Use of tape recorder/note‐tak<strong>in</strong>g: Audio‐tape, how we use it, keep it – go through confidentialitystatement.• What happens to the <strong>in</strong>formation: it will be compiled <strong>in</strong>to reports which feed <strong>in</strong>to mak<strong>in</strong>grecommendations for the future.• Consent forms: for this <strong>in</strong>terview and expla<strong>in</strong> others for subsequent participation.Repertory Grid technique will be used to freely elicit elements and personal constructs from women patientsto enable them to describe and evaluate their experiences of the secure unit where they are deta<strong>in</strong>ed, <strong>in</strong> theirown words, and us<strong>in</strong>g their own value systems to report what is important to them. The <strong>in</strong>terview will take111
the follow<strong>in</strong>g form, and the topics and issues covered will be decided entirely by the <strong>in</strong>terviewee based onwhat they believe is important to their <strong>safe</strong>ty and recovery.Elicit<strong>in</strong>g Elements:Each woman will firstly be asked to list everyth<strong>in</strong>g and everybody at the secure unit that they feel impacts <strong>in</strong>an important way on their care/treatment, <strong>safe</strong>ty and recovery:<strong>Research</strong>er: We would like to know about all the people and/or th<strong>in</strong>gs here that you th<strong>in</strong>k are important toyour <strong>safe</strong>ty and recovery at the unit. Can you name at least six people at the unit or th<strong>in</strong>gs (e.g. an activity, aroom, a rule, or anyth<strong>in</strong>g else) about the unit, that you feel are important to help<strong>in</strong>g you get well and mak<strong>in</strong>gyou feel <strong>safe</strong>?Prompts: Any others? Is that all?Once the researcher is satisfied the women has listed all the elements (people or th<strong>in</strong>gs) that she feels areimportant to her care and <strong>safe</strong>ty at the unit, the <strong>in</strong>terviewee will be offered a short break (Offered hotdr<strong>in</strong>k/toilet/etc). Dur<strong>in</strong>g this break the researcher will write out the names of elements on to cards andorganise them <strong>in</strong>to triads (groups of three) us<strong>in</strong>g a random method, to then be presented back to <strong>in</strong>terviewee<strong>in</strong> order to elicit personal constructs.Elicit<strong>in</strong>g Personal Constructs:The number of triads presented to the <strong>in</strong>terviewee will depend on the number of elements elicited from them.If only the m<strong>in</strong>imum number of elements were elicited (six) then n<strong>in</strong>e triads will be presented to her, and up toa maximum of twenty triads will be used to elicit their personal constructs.<strong>Research</strong>er: [The first triad (3 cards with name of an element on each) will be shown to <strong>in</strong>terviewee andread out: The <strong>Research</strong>er then asks:]In what way are two of these similar but different from the third?Prompts: Can you expla<strong>in</strong> a bit more what you mean by ..………….? Is there any other way those two are similarbut different from the third? Are another two of them similar <strong>in</strong> some other way but different from the third?This will then be repeated for each triad.7.3 Second <strong>in</strong>terview with women service usersEvaluation of Women’s Medium Secure Services: Topic Guide• Purpose of the evaluation: to learn about women and staff’s experiences and views of the secure service.To feed <strong>in</strong>to develop<strong>in</strong>g services <strong>in</strong> the future.• Who we are: not from the secure services but completely <strong>in</strong>dependent. All have spent a lot of time talk<strong>in</strong>gwith other women patients <strong>in</strong> secure sett<strong>in</strong>gs as part of research and evaluations.• Discussion is <strong>in</strong>formal: it will take between an hour and an hour and a half and is confidential.• Use of tape recorder/note‐tak<strong>in</strong>g: Audio‐tape, how we use it, keep it – go through confidentialitystatement.• What happens to the <strong>in</strong>formation: it will be compiled <strong>in</strong>to reports that feed <strong>in</strong>to mak<strong>in</strong>g recommendationsfor the future.• Consent forms: for this <strong>in</strong>terview and expla<strong>in</strong> others for subsequent participation.112
Early days • how did you get to the unit• arrival and admission• first impressions• layout and access• own rooms/décor/choices/<strong>in</strong>volvement <strong>in</strong> choice• improvements to environment• location of the unit/close to relatives and friends• relevance/difference this makes to them• environment/security/appropriate areas• <strong>in</strong>volvement <strong>in</strong> process/whoServices provided/needed: • range/level of care/treatment/support serviceschoice of care/treatment/other services• access to/ use/ views of creative/ complimentarytherapies• access to community and opportunities to doactivities outside the unit• physical health careExperiences/practicalities of service provision/dailyliv<strong>in</strong>g:Start with ask<strong>in</strong>g women to complete a weeklytimetable of activities. Follow up from list if notmentioned.• education/tra<strong>in</strong><strong>in</strong>g- choice if what do- views of tra<strong>in</strong><strong>in</strong>g/ providers• psychotherapy/counsell<strong>in</strong>g- choice if what do- views of tra<strong>in</strong><strong>in</strong>g/ providers• medical and drug treatment- choice of hav<strong>in</strong>g/not hav<strong>in</strong>gdrugs/other treatment- <strong>in</strong>formation provided abouttreatment- how raise concerns/with whom• social activities- choice of what do- views of activities• user <strong>in</strong>volvement- local arrangements- personal <strong>in</strong>volvement/ howhappened/ what do- usefulness of user groups/needfor/improvementsSafety <strong>in</strong> the environment: - risks and dangers- physical and emotional <strong>safe</strong>ty- provided via policy/practice/ patient<strong>in</strong>volvementRules/regulations and policies: • know what they are/how f<strong>in</strong>d out• who decides what can/can’t do• appropriate/<strong>in</strong>appropriate attitudes or behaviour• how dealt with• new policy/rules needed/what/whyFormal staff<strong>in</strong>g arrangements: • levels and roles• relationships with staff/what want/need• non‐cl<strong>in</strong>ical staff/role/relevance• ancillary staff• health care workers113
CPA and women’s <strong>in</strong>volvement:(Complete Section A of CPA audit form)• when and how takes place/with whom• know<strong>in</strong>g the care coord<strong>in</strong>ator• level of <strong>in</strong>volvement• review process/level and range of <strong>in</strong>put• role of different professionals/mean<strong>in</strong>g of multidiscipl<strong>in</strong>aryteam• keep<strong>in</strong>g a copy/know<strong>in</strong>g what’s <strong>in</strong> the care planOther relationships: • relationships with family/friends• how system supports them or not• other women <strong>in</strong> the unit• contact with men (<strong>in</strong> mixed services)External agencies: • statutory/non‐statutory (advocacy/support)• relationships/what want/need• access<strong>in</strong>g college/education• volunteer<strong>in</strong>g• us<strong>in</strong>g advocacy outside the unitHow women can have control over own lives: • becom<strong>in</strong>g empowered/what means/howhappens• control over own lives/participation <strong>in</strong> plann<strong>in</strong>g• how this can be createdDischarge (if relevant): • concept of rehabilitation• contact with outreach/community services• resettlement/where/how• support given/requiredChange and improvement: • what important to keep/how/why• what needs to be changed/how/whyAt the end of the <strong>in</strong>terview, ask the <strong>in</strong>terviewee to rank order our list of ten service attributes <strong>in</strong> the order thatshe believes are most important to ensur<strong>in</strong>g good care to women patients <strong>in</strong> secure units.7.4 CPA audit form for use <strong>in</strong> second <strong>in</strong>terviews with womenEVALUATION WOMEN’S SECURE SERVICES: SECOND INTERVIEW WITH WOMEN CPA AUDIT FORMInterview Reference no:SECTION A: (Ask service user dur<strong>in</strong>g their <strong>in</strong>terview with<strong>in</strong> section of topic guide on Care Plann<strong>in</strong>g/CPA)SERVICE USER INTERVEWWARD NAME:UNIT/HOSPITAL NAME:1) Do you know what the Care Programme Approach is?(It is also known as CPA)Yes / No(If NO give brief explanation of CPA and importance)2) Do you know who your care co‐ord<strong>in</strong>ator is? Yes / No114
115If Yes who is it: _____________________________________ (name/role)3) Who else is <strong>in</strong>volved your CPA process? (list roles)4) Do all the professionals <strong>in</strong>volved work together as a team? Yes / NoAny Comments:5) Do you usually attend your CPA review meet<strong>in</strong>gs?Always / sometimes / neverAttend whole meet<strong>in</strong>g / attend part of meet<strong>in</strong>gAny comments:6) If attends review meet<strong>in</strong>gs: Do you feel able to take part <strong>in</strong> the discussions at your review meet<strong>in</strong>gsand put forward your views and requests?Yes / To some extent / No / don’t know or not sure7) Do you have someone to support you at review meet<strong>in</strong>gs?Don’t need / advocate / named nurse / someone else / No8) Do you get to read the CPA reports before your review meet<strong>in</strong>g?Yes / sometimes / No / DK9) Are you asked to put you own views <strong>in</strong> a report?Yes with<strong>in</strong> a professional’s report / In own separate report / No10) Were you asked to sign a copy of your Care Plan? Yes / No / DK11) Were you given a copy of your CPA care plan to keep? Yes / No / DK12) Are you happy with the amount of <strong>in</strong>volvement you have <strong>in</strong> draw<strong>in</strong>g up your written care plan?Yes / Yes to some extent / No / DKAny comments:13) Are you happy that your written care plan takes account of your own views of your strengths andweaknesses?Yes / Yes to some extent / No / DKAny comments:14) Are you happy that your written care plan takes account of and provides for any needs you may haveas a result of any past experiences of be<strong>in</strong>g a victim of violence and/or abuse?Yes / yes to some extent / no / not applicable / DK15) Are you happy that your written care plan takes account of and provides for any needs you may haverelat<strong>in</strong>g to self‐<strong>in</strong>jury or risk of self harm?Yes / yes to some extent / no / not applicable / DK
16) Are you happy that your written care plan takes account of and provides for any needs you mayhave for contact and <strong>in</strong>volvement with family members (<strong>in</strong>clud<strong>in</strong>g children) or friends from outside theunit?Yes / yes to some extent / no / not applicable / DKSECTION B: (Interviewer review/audit of CPA reports/care plan)INTERVIEWER AUDIT OF CPA DOCUMENTS:1) Was the Care Co‐ord<strong>in</strong>ator Identified <strong>in</strong> CPA Care Plan? Yes / No2) Who had contributed written reports to CPA review? (list by role)3) Were service user views recorded <strong>in</strong> CPA reports/care plan? Yes / No4) Was the name of person responsible for implement<strong>in</strong>g each action <strong>in</strong> the CPA care plan? Yes / No5) Were any needs identified for which no help was available? Yes / NoIf Yes: Give details:6) Was there any evidence that the impact of gender had been <strong>in</strong>cluded <strong>in</strong> the case formulation and careplann<strong>in</strong>g? Yes / to some extent / NoComments:7) Has future care pathway and appropriate lower secure/step down facilities been identified orsearched for? Yes / No8) Has S.117 discharge plann<strong>in</strong>g commenced? Yes / No9) Needs associated with: Was this identified asneed <strong>in</strong> the care plan?Does care plan say how these needs are tobe met?Relationships with family & friends Yes / no Yes / NoRelationship with own children / or Yes / No / NAYes / No / NAloss of childrenRelationships on ward/unit Yes / No Yes / NoIndex offence/behaviour Yes / No Yes / NoWork and education Yes / No Yes / NoCultural (<strong>in</strong>clud<strong>in</strong>g ethnicity) Yes / No Yes / NoPhysical health Yes / No Yes / NoWell Women /sexual health issues Yes / No Yes / NoEmotional Yes / No Yes / NoSelf <strong>in</strong>jury Yes / No Yes / NoRisk of suicide Yes / No Yes / NoSubstance misuse Yes / No Yes / NoExperiences of violence/abuse Yes / NoYes / No(<strong>in</strong>c. impact on trust andrelationships with professionals) Yes / NoYes / No(Inc. potential for re‐victimisationand or retraumatisation)Yes / NoYes / NoSexuality Yes / No Yes / NoAdvocacy Yes / No Yes / NoOther (gender sensitive/specific) Yes / No Yes / No116
7.5 Stakeholder topic guideEvaluation of Women’s Medium Secure Services: ‘Stakeholder’ Topic Guide• Purpose of the evaluation: to learn about women and staff’s experiences and views of medium secureservices. To feed <strong>in</strong>to develop<strong>in</strong>g services <strong>in</strong> the future. Funded by Forensic R&D, DoH but work<strong>in</strong>g withNHS and <strong>in</strong>dependent sector services.• Who we are: not from the secure services or DoH but completely <strong>in</strong>dependent (LondonMet base). All havespent a lot of time talk<strong>in</strong>g with women patients, staff and others with an <strong>in</strong>terest as part of research andevaluations.• Discussion is <strong>in</strong>formal: it will take between an hour and an hour and a half and is confidential.• Use of voice recorder/note‐tak<strong>in</strong>g: Audio‐record<strong>in</strong>g, how we use it, keep it – go through confidentialitystatement.• What happens to the <strong>in</strong>formation: it will be compiled <strong>in</strong>to reports which feed <strong>in</strong>to mak<strong>in</strong>grecommendations for the future and Consent forms: for this <strong>in</strong>terview.• Service attributes ‐ what YOU consider most important for women’s recovery- reasons/if and how provided for- 10 most featured construct types/service attributes perceivedto be most important to women patients and rated here• Eligibility criteria ‐ do women <strong>in</strong> need have access to service- effectiveness of referral/assessment process- appropriateness related to patient mix, security- <strong>in</strong>‐reach to women prisoners who need transfer- how pathways are identified before admission/do theywork/get women who should be there• Models of care ‐ which models <strong>in</strong>fluence what happens/% <strong>in</strong>fluence- % staff on ward with confidence to listen to women talkabout their past lives/sexual abuse- what is differentiated care/if and why important• Service delivery ‐ identify<strong>in</strong>g women’s needs‐ range/level of care/treatment/support services‐ surviv<strong>in</strong>g child sexual abuse or other abuse/violence‐ women who self‐<strong>in</strong>jure‐ women with specific <strong>in</strong>dex offences (eg fire‐sett<strong>in</strong>g)and offence related rehabilitation‐ gender appropriate risk assessment‐ choice of care/treatment/other services‐ access to/use/views of psychological therapies‐ access to/use/views of creative/complimentary therapies‐ experiences/practicalities of service provision/daily liv<strong>in</strong>g‐ physical health care• Service specification ‐ local meet<strong>in</strong>g the requirements of national spec- methods of review and monitor<strong>in</strong>g services- exist<strong>in</strong>g policies: how f<strong>in</strong>d out about/how used <strong>in</strong> practice- women‐only sett<strong>in</strong>gs: advantages/disadvantages for womenand/or staff• Gender Equality duty ‐ impact of legislation on provision as yet/if any- nature or staff commitment- how communicated to women117
• Service standards ‐ local/regional/national‐ existence/knowledge of- need for/purpose served- measurement of standards met/unmet/significance• Staff<strong>in</strong>g arrangements ‐ levels and roles- effects of women on 1‐1 obs on general staff activities, e.g.escorts for access, on/off ward activities- use of de‐escalation/no and tra<strong>in</strong>ed to ma<strong>in</strong>ta<strong>in</strong> stability- do levels and roles allow for allow for good/adequate<strong>in</strong>teraction with women <strong>in</strong> ward sett<strong>in</strong>gs?- tra<strong>in</strong><strong>in</strong>g/support provided to staff- supervision on women’sneeds/gender/ethnicity- own relationships with other staff/what want/need- non‐cl<strong>in</strong>ical staff/role/relevance- ancillary staff/health care workers• Care plann<strong>in</strong>g process: ‐ when and how takes place- level of <strong>in</strong>volvement of staff/team members- review process/level and range of <strong>in</strong>put- role of professionals/mean<strong>in</strong>g of multi‐discipl<strong>in</strong>ary team- their experience of <strong>in</strong>volvement <strong>in</strong> care plann<strong>in</strong>g• CPA tak<strong>in</strong>g account ‐ of women’s experiences of violence/abuse/CSA- ensur<strong>in</strong>g care, <strong>safe</strong>ty, recovery and- prevention of re‐traumatisation/victimisation with<strong>in</strong> service• Liaison and collaboration ‐ jo<strong>in</strong>t work<strong>in</strong>g with community and CJS agencies‐ support<strong>in</strong>g opportunities to <strong>in</strong>teract with community‐ levels of <strong>in</strong>tegration‐ External agencies statutory/non‐statutory (advocacy/support)- relationships/what want/need• Safety <strong>in</strong> the environment ‐ risks and dangers/how assessed/how addressed- physical and emotional <strong>safe</strong>ty/howperceived/assessed/addressed- provided via policy/practice/patient <strong>in</strong>volvement• Relational security ‐ def<strong>in</strong>ition/mean<strong>in</strong>g <strong>in</strong> this context- efforts to ensure high levels of relational security for women- what helps/h<strong>in</strong>ders implementation of relational security• Built environment: ‐ layout and access/<strong>safe</strong>ty/ease of work<strong>in</strong>g- rooms/décor/choices/<strong>in</strong>volvement <strong>in</strong> choice- improvements to environment• Levels of autonomy and control ‐ importance for women or not/how achieved• Discharge (if relevant): ‐ concept of rehabilitation/what means/how practiced- contact with outreach/community services- resettlement/where/how- support given/required• Frustrations ‐ factors make difficult to meet women’s mh needs‐ how staff cope with these frustrations118
• Change and improvement: ‐ what important to keep/how/why‐ what needs to be changed/how/why7.6 Mapp<strong>in</strong>g service provision January 2009TEMPLATE FOR WOMEN’S MS SERVICES MAPPING/DIRECTORYService Name:Address:Tel no: Email: Contact Name:IF NHS Trust name: Commission<strong>in</strong>g team: Locality served:IF INDEPENDENTProviderOrganisation:Any block NHScontracts?Ma<strong>in</strong> Catchment area(s)served:Women only site:□(Please tick)Women‐only ward(s) on mixed‐sex site (withno mixed‐sex activities) □No: ofHow many beds <strong>in</strong> each women’s MS ward:women’s MSwardsDoes the service have a women‐only rehabilitation or pre‐charge ward?Does the service also have a women‐only low secure or step‐down facilityDoes the service accept women who’s ma<strong>in</strong> present<strong>in</strong>g diagnosis isBorderl<strong>in</strong>e Personality Disorder?Does the service accept women with learn<strong>in</strong>g disabilities?Women‐only ward(s) onmixed‐sex site(with some mixed‐sexactivities) □Yes / NoYes / NoYes / NoYes / NoOther questions to ask/update on phone:1) [If not women only site](a) Is there a dedicated Multi‐discipl<strong>in</strong>ary team for the women’s service?(b) Is there a dedicated ward team(s) for the women’s ward(s)?Yes / NoYes / No2) Can we check aga<strong>in</strong> which of these policies you currently have <strong>in</strong> place?Management of self‐harmManagement of aggression/distressSexuality and RelationshipsAnti‐bully<strong>in</strong>g or harassmentImplementation of Relational securityChild Visit<strong>in</strong>gEquality and diversity119
Are these policiesTrust‐wide / Unit‐wide / specific to the women’s service3) Do you have a written/agreed model or philosophy of care document for your women’s service?Yes / No(If yes would you be able to email/post us a copy??)4) FOR NHS Services:‐ Are you commissioned to provide a Gate‐keep<strong>in</strong>g Role for women requir<strong>in</strong>gSecure services <strong>in</strong> your locality/region?Yes /NoIF YES – Approximately what percentage of women requir<strong>in</strong>g medium secure care are placed <strong>in</strong>Independent/Out of Area Services ?5) Do you provide an <strong>in</strong>‐reach service for women <strong>in</strong> prison?Yes / No6) What percentage of your staff work<strong>in</strong>g <strong>in</strong> women’s service have undertaken Gender awarenessand/or gender specific tra<strong>in</strong><strong>in</strong>g?7) AND What percentage of your staff work<strong>in</strong>g <strong>in</strong> women’s service have undertaken Gender awarenessand/or gender specific tra<strong>in</strong><strong>in</strong>g <strong>in</strong> the past 12 months?120
Appendix 2:Service SpecificationMa<strong>in</strong>stream<strong>in</strong>g gender and women's mental health: implementation guidance (2004)Service specification for <strong>in</strong>tegrated, dedicated secure services for womenClient group: services (<strong>in</strong>clud<strong>in</strong>g serviceWomen with complex mental health careneeds. Women <strong>in</strong> this group often:• have more than one diagnosis <strong>in</strong>clud<strong>in</strong>gmental illness, substance misuse, learn<strong>in</strong>gdisabilities,• eat<strong>in</strong>g disorders and personality disorder,particularly borderl<strong>in</strong>e personalitydisorder;• have a history of significant and susta<strong>in</strong>edviolence and abuse and significantexperience of separation• and loss, <strong>in</strong>clud<strong>in</strong>g that of their children;• experience <strong>in</strong>tense feel<strong>in</strong>gs ofpowerlessness and vulnerability withdifficulties <strong>in</strong> form<strong>in</strong>g• trust<strong>in</strong>g relationships;• present with self‐harm, offend<strong>in</strong>gbehaviours, pervasive anger, depression,mood <strong>in</strong>stability,• dissociation and/or anxiety;• are managed <strong>in</strong> conditions of physicalsecurity greater than their needs.Structures:• short assessment and longer‐termplacements;• a range of <strong>in</strong>patient sett<strong>in</strong>gs that cancater for the range of needs <strong>in</strong>clud<strong>in</strong>g<strong>in</strong>tensive care, challeng<strong>in</strong>g behaviour,remand assessment, rehabilitation; forwomen with a diagnosis of personalitydisorder, women with learn<strong>in</strong>g andassociated disabilities; women with<strong>in</strong> theprison service who require a securemental health sett<strong>in</strong>g given their highlevels of psychiatric morbidity;• services for the small number of women,currently <strong>in</strong> high secure care, who havecommitted severe offences or who havevery challeng<strong>in</strong>g behaviours who couldnot be catered for with<strong>in</strong> exist<strong>in</strong>g• medium secure care, but who do notneed Category ‘B’ high secure care;• multi‐discipl<strong>in</strong>ary, multi‐agency teams tosupport <strong>in</strong>patient services.Services ideally need to be large enoughto support at least two multi‐discipl<strong>in</strong>aryteams to enable mutual learn<strong>in</strong>g andsupport, and to provide specialist coverfor times of additional need/holidays, etc.Physical design:• environmental security provided by thebuilt environment, wherever possible,rather than perimeter fences andspecifically address ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g anenvironment that reduces as far aspossible the capacity for serious selfharm;• ward lay‐out <strong>in</strong> which zonal observation isa realistic alternative to high levels of oneto one, or more, nurs<strong>in</strong>g;• crisis suite(s) i.e. bedroom, day andbathroom area(s) that are separate, orcan be separated off;• child/family visit<strong>in</strong>g areas;• women‐only secure outside space;• wards with no more than 12 beds;• quiet/low stimulus area(s).Access is also required to non‐specialist, nonsecureservices <strong>in</strong>clud<strong>in</strong>g acute <strong>in</strong>patient andcommunity sett<strong>in</strong>gs (e.g. assertive outreachteams, high support community residentialplacements) that will accept women withchalleng<strong>in</strong>g/offend<strong>in</strong>g/self‐harm<strong>in</strong>gbehaviours.Physical health care:Inpatient services should have dedicatedprimary health care <strong>in</strong>put <strong>in</strong>clud<strong>in</strong>g wellwomansessions, dentistry and generalpractice and suitable arrangements for theprovision of specialist, secondary physicalhealth care when required. <strong>Health</strong> promotionservices should also be provided.121
Forensic community teams:These should be multi‐discipl<strong>in</strong>ary and <strong>in</strong>clude<strong>in</strong>put from the follow<strong>in</strong>g discipl<strong>in</strong>es:psychiatry, psychology, psychotherapy, socialwork, occupational therapy and nurs<strong>in</strong>g.Sessional <strong>in</strong>put from other services/discipl<strong>in</strong>essuch as substance misuse and eat<strong>in</strong>g disordersmay be required. It may be appropriate toarrange secondments from learn<strong>in</strong>gdisabilities/ rehabilitation/probation servicesto <strong>in</strong>crease the range of experience, thelikelihood of recruitment and the capacity for<strong>in</strong>ter‐agency liaison.Outreach – consultation, liaison and crisis<strong>in</strong>terventionSupport to:• crim<strong>in</strong>al justice system: probation service(<strong>in</strong>clud<strong>in</strong>g bail and probation hostels),courts and prisons;• local adult and child and adolescentmental health and learn<strong>in</strong>g disabilitiesservices, giv<strong>in</strong>g advice on how womenmay be cared for without admission tosecure beds;• private sector/out‐of‐area placements.Assessment and care plann<strong>in</strong>g:• assessment should <strong>in</strong>form a formal careplann<strong>in</strong>g process under CPA;• should be multi‐discipl<strong>in</strong>ary, holistic andcomprehensive <strong>in</strong>clud<strong>in</strong>g violence andabuse, self‐harm, substance misuse,eat<strong>in</strong>g disorders, sexuality and gendersensitive assessment of risk.• will need to take place <strong>in</strong> a variety ofsett<strong>in</strong>gs <strong>in</strong>clud<strong>in</strong>g the community, familyand residential homes, and distant secureplacements <strong>in</strong>clud<strong>in</strong>g prisons, high securehospitals and the <strong>in</strong>dependent sector;• l<strong>in</strong>ks with local court/police diversion andliaison services should be explicitlyagreed.Treatment and cont<strong>in</strong>u<strong>in</strong>g careTeams should provide the follow<strong>in</strong>g:Therapeutic and non‐<strong>in</strong>stitutionalised ethoswhich consistently <strong>in</strong>corporates the follow<strong>in</strong>g<strong>in</strong> all areas of the unit e.g. ward, activityareas, psychological therapy sett<strong>in</strong>gs:• a high level of relational security;• a positive expectation of hope andrecovery;• recognition of the strengths, abilities andcompetencies of women patients;• development of ‘non‐punitive’ strategiesfor the management and reduction ofthreatened andactual aggression towardsstaff and patients;• ensure that, <strong>in</strong> all aspects of cl<strong>in</strong>icalpractice, situations are not created thatmay be perceived or experienced asabusive by women patients (or staff ).A range of outpatient and <strong>in</strong>patient<strong>in</strong>terventions <strong>in</strong>clud<strong>in</strong>g:• a range of <strong>in</strong>tegrated psychologicaltherapies that are psycho‐dynamically<strong>in</strong>formed e.g. family, systemic,cognitive/behavioural approaches <strong>in</strong>group and <strong>in</strong>dividual sett<strong>in</strong>gs to helpwomen address e.g. their self‐harm,substance misuse, eat<strong>in</strong>g disorders;patterns of offend<strong>in</strong>g (particularly firesett<strong>in</strong>g)– the therapeutic process shouldbe fully <strong>in</strong>formed by an understand<strong>in</strong>gthat these presentations are <strong>in</strong>ter‐l<strong>in</strong>kedsymptoms of primary distress located <strong>in</strong>the lives and experiences of women,notably childhood sexual abuse;• creative therapies;• complementary therapies;• medication: to be ma<strong>in</strong>ta<strong>in</strong>ed at thelowest level possible for satisfactorytherapeutic benefit without unduesuppression of feel<strong>in</strong>gs/emotions and/orundue weight ga<strong>in</strong>.An <strong>in</strong>tegrated ‘daily liv<strong>in</strong>g’ programme<strong>in</strong>clud<strong>in</strong>g:• education (<strong>in</strong>clud<strong>in</strong>g basicnumeracy/literacy), creative arts, sportsand opportunities for exercise,occupational activities, health promotion,development of cop<strong>in</strong>g, social andparent<strong>in</strong>g skills, social/leisureopportunities.Activities should be tailored to an <strong>in</strong>dividual’sability and level of confidence to enable122
women to learn new skills and <strong>in</strong>crease theirself esteem through concrete achievement.Note To m<strong>in</strong>imise women’s sense of isolationand enhance their movement towards<strong>in</strong>dependence, services should facilitate their<strong>in</strong>volvement/contact with all relevantcommunity sett<strong>in</strong>gs and activities.Community follow‐up of all womendischarged from secure care <strong>in</strong>clud<strong>in</strong>g thosewho do not require secure placement, butwhose behaviours are too unusual/severe tobe conta<strong>in</strong>ed by local general mental healthteams, and those with establishedforensic/offend<strong>in</strong>g problems and mentalillness/personality disorder.Service standards, evaluation and monitor<strong>in</strong>gproceduresThese need to be developed <strong>in</strong> closeconsultation with women patients <strong>in</strong> all newservice models of care.Operational policies and proceduresPolicies and procedures should <strong>in</strong>clude thefollow<strong>in</strong>g:• Clarity regard<strong>in</strong>g the operationalmanagement of an environment with ahigh level of relational security.Note: This relates to the nature and quality oftherapeutic relationships developed andsusta<strong>in</strong>ed between patients and staff,primarily nurs<strong>in</strong>g staff, with<strong>in</strong> the context of<strong>safe</strong>, conta<strong>in</strong>ed and fully expla<strong>in</strong>edboundaries. It is dependent upon high staff:patient ratios; the appropriate level, attitudeand quality of staff engagement with patients;appropriate staff tra<strong>in</strong><strong>in</strong>g andactivities/<strong>in</strong>terventions provided by the staffgroup. Relational security needs to be<strong>in</strong>formed by an understand<strong>in</strong>g of the impactof surviv<strong>in</strong>g severe violence and abuse onwomen’s profound sense of powerlessnessand vulnerability. A positive experience of‘here and now’ relationships is crucial to therecovery process, those that address the ways<strong>in</strong> which women have been silenced andbeg<strong>in</strong>s to give them a ‘voice’.• Mixed‐sex activities, if and when, cl<strong>in</strong>icallyappropriate.Note: Women‐only activities should be thenorm with the potential for mixed‐sexactivities conf<strong>in</strong>ed to the recovery/rehabilitative process. Any mixed‐sex activityshould be organised with around equalnumbers of women and men. Decisions onappropriateness should be made on an<strong>in</strong>dividual basis: the <strong>in</strong>clusion of womenpatients should be dictated by a woman’sability to make <strong>safe</strong> and <strong>in</strong>formed decisionsabout her welfare; the <strong>in</strong>clusion of menpatients should be based on a risk assessmentto ensure that they have the ability to engage<strong>in</strong> mixed‐sex activity <strong>in</strong> a <strong>safe</strong> and appropriatemanner.• Observation policies sensitive to women’sneed for privacy and least restrictive caresuch as zonal observation, high level ofstaff : patient engagement (see relationalsecurity above) and additional supportplans.• Self‐harm<strong>in</strong>g behaviour <strong>in</strong>clud<strong>in</strong>gagreements with local emergency careproviders (see Section 8.5).WorkforceDevelopment of:• a dedicated, appropriately skilled staffgroup with capacity for cross cover andthe development of specialist skills;• a stable staff group which will helpconsistency <strong>in</strong> practice and thedevelopment of therapeutic relationships;• an appropriate gender mix of staff(exist<strong>in</strong>g women‐only services often use am<strong>in</strong>imum of 70% female nurs<strong>in</strong>g staffwith access to women staff at all times).Staff should be recruited who have made anactive and appropriate choice to work withwomen patients, are committed to work<strong>in</strong>gholistically and have an understand<strong>in</strong>g of keygender issues relevant to women <strong>in</strong> securecare. The <strong>in</strong>troduction of sharedposts/secondments/reciprocal placementsacross secure and general mental healthservices would provide a means of extend<strong>in</strong>g123
staff skills, promot<strong>in</strong>g a greater mutualunderstand<strong>in</strong>g and knowledge and reduc<strong>in</strong>gthe risk of staff ‘burnout’.Tra<strong>in</strong><strong>in</strong>gThe service will need to be able to providetra<strong>in</strong><strong>in</strong>g to other organisations andprofessionals as well as appropriate tra<strong>in</strong><strong>in</strong>gfor its own staff group.Staff supportThis should be <strong>in</strong>tegral to the organisation ofservices and <strong>in</strong>clude supervision, space forreflective practice and access to work‐relatedconfidential counsell<strong>in</strong>g and crisis support.ManagementMulti‐discipl<strong>in</strong>ary/multi‐agency managementteams to help create gender sensitiveorganisational culture, policies and practice.<strong>Research</strong>Sufficient fund<strong>in</strong>g should be available toensure that services are established with aculture of research and audit. Formal l<strong>in</strong>ks toan academic base should be made.124
Appendix 3: Provider directory: January 2009East MidlandsNHSArnold LodgeCordelia Close, Leicester LE5 0LETel: 0116 225 610Provider: Nott<strong>in</strong>ghamshire <strong>Health</strong> NHS TrustNo of medium secure beds for women: 20Rehabilitation ward:NoLow secure/step down:NoNotes: Includes WEMSS pilotIndependentCalverton HillRamsdale Park, Calverton Road, Arnold NG5 8PTTel: 0115 966 150Provider: Partnerships In CareNo of medium secure beds for women: 32Rehabilitation ward:YesLow secure/step down:YesSt Andrews <strong>Health</strong>careBill<strong>in</strong>g Road, Northampton NN1 5DGTel: 01604 616000Provider: St Andrews <strong>Health</strong>care GroupNo of medium secure beds for women: 41Rehabilitation ward:YesLow secure/step down:YesNotes: Includes a Specialist Learn<strong>in</strong>g Disability unitEast of EnglandNHSRunwell Hospital, Runwell Chase, Wickford SS11 7XXTel: 01268 366040Provider: South Essex PartnershipUniversity NHS FoundationNo of medium secure beds for women: 10Rehabilitation ward:NoLow secure/step down:NoIndependentKneesworth HouseBass<strong>in</strong>gbourne‐cum‐Kneesworth, Old North Road,Royston SG8 5JPTel: 01763 255700Provider: Partnerships In CareNo of medium secure beds for women: 11Rehabilitation ward:YesLow secure/step down:YesSt John's HouseLion Road, Palgrave, Diss IP22 1BATel: 01379 643334Provider: Partnerships In CareNo of medium secure beds for women: 16Rehabilitation ward:NoLow secure/step down:YesNotes: This is a specialist learn<strong>in</strong>g disability serviceLondonNHSBracton CentreBracton Lane, Leyton Cross Road, Dartford DA2 7AFTel: 01322 297634Provider: Oxleas NHS Foundation TrustNo of medium secure beds for women: 9Rehabilitation ward:YesLow secure/step down:NoJohn Howard Centre12 Kenworthy Road, London E9 5TDTel: 0208 510 229Provider: East London and City UniversityNHS TrustNo of medium secure beds for women: 14Rehabilitation ward:NoLow secure/step down:YesNorth London ForensicC/o St Bernards Hospital, Uxbridge Road, SouthallUB1 3EUTel: 0208 354 8354Provider: Barnet, Enfield & Har<strong>in</strong>gay Mental<strong>Health</strong> NHS TrustNo of medium secure beds for women: 10Rehabilitation ward:YesLow secure/step down:NoNotes: Temporarily relocated due to fireShaftesbury Cl<strong>in</strong>icSpr<strong>in</strong>gfield Hospital, 61 Glenburnie Road, LondonSW17 7DJTel: 0208 6825899Provider: South West London and St GeorgesNHS FoundationNo of medium secure beds for women: 10Rehabilitation ward:NoLow secure/step down:No125
The Orchard UnitSt Bernards Hospital, Uxbridge Road, Southall UB1 3EUTel: 0208 3548354Provider: West London Mental <strong>Health</strong> NHS TrustNo of medium secure beds for women: 50Rehabilitation ward:NoLow secure/step down:YesNotes: Includes WEMSS pilotNorth EastNHSHutton CentreSt Lukes Hospital, Marton Road, Middlesborough TS4 3AFTel: 01642 283300Provider: Tees, Esk & Wear Valleys NHSFoundation TrustNo of medium secure beds for women: 14Rehabilitation ward:NoLow secure/step down:NoNorth WestNHSEdenfield CentrePrestwich Hospital, Bury New Road, Prestwich M25 3BLTel: 0161 7723159Provider: Greater Manchester West Mental NHSFoundation TrustNo of medium secure beds for women: 18Rehabilitation ward:YesLow secure/step down:NoNotes: Includes WEMSS pilotGuild LodgeGuild Park, Whitt<strong>in</strong>gham Lane, Goosnargh PR3 2AZTel: 01772 406600Provider: Lancashire Care NHS Foundation TrustNo of medium secure beds for women: 16Rehabilitation ward:YesLow secure/step down:YesScott Cl<strong>in</strong>icRa<strong>in</strong>hill Road, St Helens WA9 5BDTel: 0151 4306300Provider: Mersey Care NHS TrustNo of medium secure beds for women: 8Rehabilitation ward:NoLow secure/step down:NoWoodviewCalderstones, Mitton Road, Whalley, Clitheroe BB7 9PETel: 01254 822121Provider: Calderstones NHS TrustNo of medium secure beds for women: 6Rehabilitation ward:YesLow secure/step down:YesNotes: Specialist Learn<strong>in</strong>g Disability ServiceIndependentAlpha Hospital BuryBuller Street, Bury BL8 2BSTel: 0161 7627200Provider: Alpha HospitalsNo of medium secure beds for women: 23Rehabilitation ward:YesLow secure/step down:YesNotes: Includes specialist secure service for deafwomenArbury CourtTownfield Lane, W<strong>in</strong>wick, Warr<strong>in</strong>gton WA2 8TRTel: 01925 400600Provider: Partnerships In CareNo of medium secure beds for women: 22Rehabilitation ward:YesLow secure/step down:YesSouth CentralNHSThames HouseLittlemore Mental <strong>Health</strong> Centre, Sandford Road,Littlemore, Oxford OX4 4XNTel: 0845 2191027Provider: Oxfordshire & Buck<strong>in</strong>ghamshireMental <strong>Health</strong> NHSNo of medium secure beds for women: 24Rehabilitation ward:NoLow secure/step down:NoIndependentChadwick LodgeChadwick Drive, Eaglestone, Milton Keynes MK6 5LSTel: 01908 608600Provider: The Priory GroupNo of medium secure beds for women: 20Rehabilitation ward:NoLow secure/step down:YesSouth EastNHSAmber LodgeAshen Hill Unit, The Drive, Hell<strong>in</strong>gly BN7 4ERTel: 01323 440022Provider: Sussex Partnership NHSFoundation TrustNo of medium secure beds for women: 6Rehabilitation ward:NoLow secure/step down:Yes126
Trevor Gibbens UnitWest MidlandsHermitage Lane, Maidestone ME16 9QQNHSTel: 01622 723100 Ardenleigh UnitProvider: Kent and Medway NHS and Social Care 385 K<strong>in</strong>gsbury Road, Birm<strong>in</strong>gham B24 9SAPartnershipTel: 0121 6784400No of medium secure beds for women: 15 Provider: Birm<strong>in</strong>gham and Solihull MentalRehabilitation ward:Yes<strong>Health</strong> NHSLow secure/step down: No No of medium secure beds for women: 30Rehabilitation ward:YesIndependent Low secure/step down: NoThe DeneGatehouse Lane, Goodards Green, Hassocks BN6 9LETel: 01444 231000 Yorkshire and HumberProvider: Partnerships In Care NHSNo of medium secure beds for women: 80 Newton LodgeRehabilitation ward: No Ouchthorpe Lane, Wakefield WF1 3SPLow secure/step down: Yes Tel: 01924 327352Notes: Includes a new learn<strong>in</strong>g disability unit Provider: South West Yorkshire NHS Mental<strong>Health</strong> TrustSouth West No of medium secure beds for women: 10NHS Rehabilitation ward: NoFromeside Low secure/step down: NoBlackberry Hill, Stapleton, Bristol BS16 1EGTel: 0117 9583678 IndependentProvider: Avon and Wiltshire mental <strong>Health</strong> Stockton HallNHS TrustThe Village, Stockton On the Forest, York YO32 9UNNo of medium secure beds for women: 12 Tel: 01904 400500Rehabilitation ward: No Provider: Partnerships In CareLow secure/step down: No Total no of medium secure beds for women: 16Rehabilitation ward:NoLow secure/step down:No127