How to manage type 2 diabetes in medical and surgical patients in ...
How to manage type 2 diabetes in medical and surgical patients in ...
How to manage type 2 diabetes in medical and surgical patients in ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
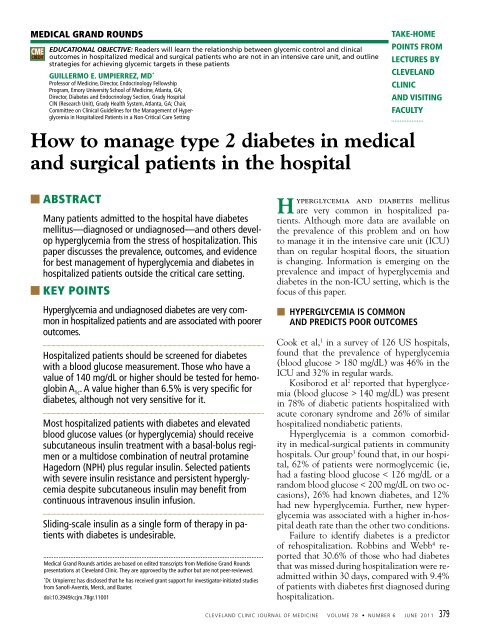
TYPE 2 DIABETES IN THE HOSPITALTABLE 1Categories of <strong>diabetes</strong>TEST NORMAL PREDIABETES DIABETESHemoglob<strong>in</strong> A 1c< 5.7% 5.7%–6.4% ≥ 6.5%Fast<strong>in</strong>g plasma glucose < 100 mg/dL 100–125 mg/dL ≥ 126 mg/dL2-Hour plasma glucose a < 140 mg/dL 140–199 mg/dL ≥ 200 mg/dL baPerformed dur<strong>in</strong>g an oral glucose <strong>to</strong>lerance testbOr r<strong>and</strong>om plasma glucose ≥ 200 mg/dL plus symp<strong>to</strong>msINFORMATION FROM AMERICAN DIABETES ASSOCIATION. DIAGNOSIS AND CLASSIFICATION OF DIABETES MELLITUS.DIABETES CARE 2010; 33(SUPPL 1):S62–S69.Hemoglob<strong>in</strong> A 1cis not very goodby itself as ascreen<strong>in</strong>g test,but is veryspecific as afollow-up test■■WHAT DIAGNOSTIC CRITERIASHOULD WE USE?Blood glucose greater than 140 mg/dLA consensus statement from the AmericanAssociation of Cl<strong>in</strong>ical Endocr<strong>in</strong>ologists(ACE) <strong>and</strong> the American Diabetes Association(ADA) 5 def<strong>in</strong>es <strong>in</strong>-hospital hyperglycemiaas a blood glucose level greater than 140mg/dL on admission or <strong>in</strong> the hospital. If theblood glucose is higher than this, the questionarises as <strong>to</strong> whether the patient has preexist<strong>in</strong>g<strong>diabetes</strong> or has stress hyperglycemia.Hemoglob<strong>in</strong> A 1cof 6.5% or higherIn view of the uncerta<strong>in</strong>ty as <strong>to</strong> whether a patientwith an elevated blood glucose level haspreexist<strong>in</strong>g <strong>diabetes</strong> or stress hyperglycemia,upcom<strong>in</strong>g guidel<strong>in</strong>es will recommend measur<strong>in</strong>gthe hemoglob<strong>in</strong> A 1clevel if the blood glucoselevel is higher than 140 mg/dL.A patient with an elevated blood glucoselevel (>140 mg/dL) whose hemoglob<strong>in</strong> A 1clevel is 6.5% or higher can be identified ashav<strong>in</strong>g <strong>diabetes</strong> that preceded the hospitalization.Hemoglob<strong>in</strong> A 1ctest<strong>in</strong>g can also beuseful <strong>to</strong> assess glycemic control before admission<strong>and</strong> <strong>in</strong> design<strong>in</strong>g an optional regimen atthe time of discharge. In <strong>patients</strong> with newlyrecognized hyperglycemia, a hemoglob<strong>in</strong> A 1cmeasurement can help differentiate <strong>patients</strong>with previously undiagnosed <strong>diabetes</strong> fromthose with stress-<strong>in</strong>duced hyperglycemia.Cl<strong>in</strong>icians should keep <strong>in</strong> m<strong>in</strong>d that a hemoglob<strong>in</strong>A 1ccu<strong>to</strong>ff of 6.5% identifies fewercases of undiagnosed <strong>diabetes</strong> than does a highfast<strong>in</strong>g glucose concentration, <strong>and</strong> that a levelless than 6.5% does not rule out the diagnosisof <strong>diabetes</strong>. Several epidemiologic studies 6have reported a low sensitivity (44% <strong>to</strong> 66%)but a high specificity (76% <strong>to</strong> 99%) for hemoglob<strong>in</strong>A 1cvalues higher than 6.5% <strong>in</strong> anoutpatient population. The high specificitytherefore supports the use of hemoglob<strong>in</strong> A 1c<strong>to</strong> confirm the diagnosis of <strong>diabetes</strong> <strong>in</strong> <strong>patients</strong>with hyperglycemia, but the low sensitivity<strong>in</strong>dicates that this test should not be used foruniversal screen<strong>in</strong>g <strong>in</strong> the hospital.Many fac<strong>to</strong>rs can <strong>in</strong>fluence the hemoglob<strong>in</strong>A 1clevel, such as anemia, iron deficiency,blood transfusions, hemolytic anemia, <strong>and</strong> renalfailure.Until now, if <strong>patients</strong> had hyperglycemiabut no prior diagnosis of <strong>diabetes</strong>, the recommendationwas for an oral 2-hour glucose <strong>to</strong>lerancetest shortly after discharge <strong>to</strong> confirmthe diagnosis of <strong>diabetes</strong>. Norhammar et al 7performed oral glucose <strong>to</strong>lerance tests <strong>in</strong> <strong>patients</strong>admitted with acute myocardial <strong>in</strong>farction,<strong>and</strong> Matz et al 8 performed glucose <strong>to</strong>lerancetests <strong>in</strong> <strong>patients</strong> with acute stroke. Theyfound that impaired glucose <strong>to</strong>lerance <strong>and</strong>undiagnosed <strong>type</strong> 2 <strong>diabetes</strong> were very common<strong>in</strong> these two groups. <strong>How</strong>ever, physiciansrarely order oral glucose <strong>to</strong>lerance tests. Webelieve that hemoglob<strong>in</strong> A 1cwill be a better<strong>to</strong>ol than an oral glucose <strong>to</strong>lerance test <strong>to</strong> confirm<strong>diabetes</strong> <strong>in</strong> hyperglycemic <strong>patients</strong> <strong>in</strong> thehospital sett<strong>in</strong>g.In its January 2010 recommendations, 9 theADA lists criteria for the categories of normal,pre<strong>diabetes</strong>, <strong>and</strong> <strong>diabetes</strong>, based on fast<strong>in</strong>g <strong>and</strong>2-hour postpr<strong>and</strong>ial plasma glucose levels <strong>and</strong>hemoglob<strong>in</strong> A 1c (TABLE 1).380 CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 78 • NUMBER 6 JUNE 2011
UMPIERREZ■■WHAT IS THE ASSOCIATION BETWEENHYPERGLYCEMIA AND OUTCOMES?In 2,471 <strong>patients</strong> admitted <strong>to</strong> the hospital withcommunity-acquired pneumonia, McAlisteret al 10 found that the rates of hospital complications<strong>and</strong> of death rose with blood glucoselevels.Falguera et al 11 found that, <strong>in</strong> 660 episodesof community-acquired pneumonia, the ratesof hospitalization, death, pleural effusion, <strong>and</strong>concomitant illnesses were all significantlyhigher <strong>in</strong> diabetic <strong>patients</strong> than <strong>in</strong> nondiabetic<strong>patients</strong>.Noordzij et al 12 performed a case-controlstudy of 108,593 <strong>patients</strong> who underwentnoncardiac surgery. The odds ratio for perioperativedeath was 1.19 (95% confidence <strong>in</strong>terval[CI] 1.1–1.3) for every 1-mmol/L <strong>in</strong>crease<strong>in</strong> the glucose level.Frisch et al, 13 <strong>in</strong> <strong>patients</strong> undergo<strong>in</strong>g noncardiacsurgery, found that the 30-day rates ofdeath <strong>and</strong> of <strong>in</strong>-hospital complications wereall higher <strong>in</strong> <strong>patients</strong> with <strong>diabetes</strong> than without<strong>diabetes</strong>.Our group 3 identified hyperglycemia as an<strong>in</strong>dependent marker of <strong>in</strong>-hospital death <strong>in</strong><strong>patients</strong> with undiagnosed <strong>diabetes</strong>. The ratesof death were 1.7% <strong>in</strong> those with normoglycemia,3.0% <strong>in</strong> those with known <strong>diabetes</strong>, <strong>and</strong>16.0% (P < .01) <strong>in</strong> those with new hyperglycemia.The ACE/ADA consensus panel 14 set thefollow<strong>in</strong>g glucose targets for <strong>patients</strong> <strong>in</strong> thenon-ICU sett<strong>in</strong>g:• Pre-meal blood glucose < 140 mg/dL• R<strong>and</strong>om blood glucose < 180 mg/dL.On the other h<strong>and</strong>, hypoglycemia is alsoassociated with adverse outcomes. Therefore,<strong>to</strong> avoid hypoglycemia, the <strong>in</strong>sul<strong>in</strong> regimenshould be reassessed if blood glucose levels fallbelow 100 mg/dL. New guidel<strong>in</strong>es will suggestkeep<strong>in</strong>g the blood glucose between 100 <strong>and</strong>140 mg/dL.■■HOW SHOULD WE MANAGE HYPERGLYCEMIAIN THE NON-ICU SETTING?The ACE/ADA guidel<strong>in</strong>es recommend subcutaneous<strong>in</strong>sul<strong>in</strong> therapy for most <strong>medical</strong><strong>surgical</strong><strong>patients</strong> with <strong>diabetes</strong>, reserv<strong>in</strong>g <strong>in</strong>travenous<strong>in</strong>sul<strong>in</strong> therapy for hyperglycemiccrises <strong>and</strong> uncontrolled hyperglycemia. 14Oral antidiabetic agents are not generallyrecommended, as we have no data <strong>to</strong> supporttheir use <strong>in</strong> the hospital. Another argumentaga<strong>in</strong>st us<strong>in</strong>g non<strong>in</strong>sul<strong>in</strong> therapies <strong>in</strong> the hospitalis that sulfonylureas, especially glyburide(Diabeta, Micronase) are a major cause of hypoglycemia.Metform<strong>in</strong> (Glucophage) is contra<strong>in</strong>dicated<strong>in</strong> decreased renal function, <strong>in</strong>hemodynamic <strong>in</strong>stability, <strong>in</strong> <strong>surgical</strong> <strong>patients</strong>,<strong>and</strong> with the use of iod<strong>in</strong>ated contrast dye.Thiazolid<strong>in</strong>ediones are associated with edema<strong>and</strong> congestive heart failure, <strong>and</strong> they take up<strong>to</strong> 12 weeks <strong>to</strong> lower blood glucose levels. Alpha-glucosidase<strong>in</strong>hibi<strong>to</strong>rs are weak glucoselower<strong>in</strong>gagents. Also, therapies directed atglucagon-like-prote<strong>in</strong> 1 can cause nausea <strong>and</strong>have a greater effect on postpr<strong>and</strong>ial glucose. 14The two ma<strong>in</strong> options for manag<strong>in</strong>g hyperglycemia<strong>and</strong> <strong>diabetes</strong> <strong>in</strong> the non-ICU sett<strong>in</strong>gare short-act<strong>in</strong>g <strong>in</strong>sul<strong>in</strong> on a slid<strong>in</strong>g scale<strong>and</strong> basal-bolus therapy, the latter with eitherNPH plus regular <strong>in</strong>sul<strong>in</strong> or long-act<strong>in</strong>g plusrapid-act<strong>in</strong>g <strong>in</strong>sul<strong>in</strong> analogues.Basal-bolus vs slid<strong>in</strong>g scale <strong>in</strong>sul<strong>in</strong>:The RABBIT-2 trialIn the RABBIT 2 trial (R<strong>and</strong>omized BasalBolus Versus Slid<strong>in</strong>g Scale Regular Insul<strong>in</strong><strong>in</strong> Patients With Type 2 Diabetes Mellitus), 15our group compared the efficacy <strong>and</strong> safety ofa basal-bolus regimen <strong>and</strong> a slid<strong>in</strong>g-scale regimen<strong>in</strong> 130 hospitalized <strong>patients</strong> with <strong>type</strong> 2<strong>diabetes</strong> treated with diet, with oral hypoglycemicagents, or with both. Oral antidiabeticdrugs were discont<strong>in</strong>ued on admission, <strong>and</strong><strong>patients</strong> were r<strong>and</strong>omized <strong>to</strong> one of the treatmentgroups.In the basal-bolus group, the start<strong>in</strong>g <strong>to</strong>taldaily dose was 0.4 U/kg/day if the bloodglucose level on admission was between 140<strong>and</strong> 200 mg/dL, or 0.5 U/kg/day if the glucoselevel was between 201 <strong>and</strong> 400 mg/dL. Halfof the <strong>to</strong>tal daily dose was given as <strong>in</strong>sul<strong>in</strong>glarg<strong>in</strong>e (Lantus) once daily, <strong>and</strong> the otherhalf was given as <strong>in</strong>sul<strong>in</strong> glulis<strong>in</strong>e (Apidra)before meals. These doses were adjusted if thepatient’s fast<strong>in</strong>g or pre-meal blood glucose levelsrose above 140 mg/dL or fell below 70 mg/dL.The slid<strong>in</strong>g-scale group received regular<strong>in</strong>sul<strong>in</strong> four times daily (before meals <strong>and</strong> atReassess the<strong>in</strong>sul<strong>in</strong> regimenif blood glucoselevels fallbelow 100 mg/dLCLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 78 • NUMBER 6 JUNE 2011 381
TYPE 2 DIABETES IN THE HOSPITALOralantidiabeticagents are notgenerallyrecommended<strong>in</strong> the hospitalbedtime) for glucose levels higher than 140mg/dL; the higher the level, the more they got.The basal-bolus regimen was better thanslid<strong>in</strong>g-scale regular <strong>in</strong>sul<strong>in</strong>. At admission,the mean glucose values <strong>and</strong> hemoglob<strong>in</strong>A 1cvalues were similar <strong>in</strong> both groups, butthe mean glucose level on therapy was significantlylower <strong>in</strong> the basal-bolus group than<strong>in</strong> the slid<strong>in</strong>g-scale group, 166 ± 32 mg/dL vs193 ± 54 mg/dL, P < .001). About two-thirdsof the basal-bolus group achieved a blood glucosetarget of less than 140 mg/dL, comparedwith only about one-third of the slid<strong>in</strong>g-scalegroup. The basal-bolus group received more<strong>in</strong>sul<strong>in</strong>, a mean of 42 units per day vs 12.5units per day <strong>in</strong> the slid<strong>in</strong>g-scale group. Yetthe <strong>in</strong>cidence of hypoglycemia was 3% <strong>in</strong>both groups.NPH plus regular vs detemir plus aspart:The DEAN trialSeveral long-act<strong>in</strong>g <strong>in</strong>sul<strong>in</strong> analogues areavailable <strong>and</strong> have a longer duration of actionthan NPH. Similarly, several newer rapidact<strong>in</strong>ganalogues act more rapidly than regular<strong>in</strong>sul<strong>in</strong>. Do these pharmacok<strong>in</strong>etic advantagesmatter? And do they justify the higher costs ofthe newer agents?In the r<strong>and</strong>omized Insul<strong>in</strong> Detemir VersusNPH Insul<strong>in</strong> <strong>in</strong> Hospitalized Patients WithDiabetes (DEAN) trial, 16 we compared tworegimens: detemir plus aspart <strong>in</strong> a basal-bolusregimen, <strong>and</strong> NPH plus regular <strong>in</strong>sul<strong>in</strong> <strong>in</strong> twodivided doses, two-thirds of the <strong>to</strong>tal dailydose <strong>in</strong> the morn<strong>in</strong>g before breakfast <strong>and</strong> onethirdbefore d<strong>in</strong>ner, both doses <strong>in</strong> a ratio oftwo-thirds NPH <strong>and</strong> one-third regular, mixed<strong>in</strong> the same syr<strong>in</strong>ge. We recruited 130 <strong>patients</strong>with <strong>type</strong> 2 <strong>diabetes</strong> mellitus who were on oralhypoglycemic agents or <strong>in</strong>sul<strong>in</strong> therapy.NPH plus regular was just as good as detemirplus aspart <strong>in</strong> improv<strong>in</strong>g glycemic control.Blood glucose levels fell dur<strong>in</strong>g the firstday of therapy <strong>and</strong> were similar <strong>in</strong> both groupsthroughout the trial, as measured beforebreakfast, lunch, <strong>and</strong> d<strong>in</strong>ner <strong>and</strong> at bedtime.The mean <strong>to</strong>tal daily <strong>in</strong>sul<strong>in</strong> dose was not significantlydifferent between treatment groups:56 ± 45 units <strong>in</strong> the basal-bolus detemir-aspartgroup <strong>and</strong> 45 ± 32 units <strong>in</strong> the NPH-regulargroup. <strong>How</strong>ever, the basal-bolus group receivedsignificantly more short-act<strong>in</strong>g <strong>in</strong>sul<strong>in</strong>:27 ± 20 units a day of aspart vs 18 ± 14 unitsof regular.Somewhat fewer <strong>patients</strong> <strong>in</strong> the NPHregulargroup had episodes of hypoglycemia,although the difference between groups wasnot statistically significant.In a univariate analysis of the RABBIT-2<strong>and</strong> DEAN trials, 17 fac<strong>to</strong>rs that predicted ablood glucose level less than 60 mg/dL wereolder age, lower body weight, higher serumcreat<strong>in</strong><strong>in</strong>e level, <strong>and</strong> previous <strong>in</strong>sul<strong>in</strong> therapy.Fac<strong>to</strong>rs that were not predictive were the hemoglob<strong>in</strong>A 1clevel <strong>and</strong> the enrollment bloodglucose level. Based on these data, we believethat <strong>to</strong> reduce the rate of hypoglycemia, lower<strong>in</strong>sul<strong>in</strong> doses are needed <strong>in</strong> elderly <strong>patients</strong><strong>and</strong> <strong>patients</strong> with renal impairment, <strong>and</strong> thatif <strong>patients</strong> have been tak<strong>in</strong>g <strong>in</strong>sul<strong>in</strong> beforethey come <strong>to</strong> the hospital, the dose should becut back by about 25% while they are hospitalized.Basal-bolus vs slid<strong>in</strong>g-scale <strong>in</strong>sul<strong>in</strong> for<strong>surgical</strong> <strong>patients</strong>: The RABBIT 2 Surgery trialDoes better glucose control <strong>in</strong> <strong>surgical</strong> <strong>patients</strong>affect outcomes <strong>in</strong> <strong>patients</strong> undergo<strong>in</strong>ggeneral surgery? To f<strong>in</strong>d out, we performed aprospective, multicenter, r<strong>and</strong>omized, openlabeltrial <strong>in</strong> general surgery <strong>patients</strong> not <strong>in</strong>the ICU. 18 We recruited <strong>and</strong> r<strong>and</strong>omized 211<strong>patients</strong> with <strong>type</strong> 2 <strong>diabetes</strong> who were on diettherapy or oral hypoglycemic agents or <strong>in</strong>sul<strong>in</strong><strong>in</strong> low doses (< 0.4 U/kg/day).Oral drugs were discont<strong>in</strong>ued on admission,<strong>and</strong> <strong>patients</strong> were r<strong>and</strong>omized <strong>to</strong> receiveeither a basal-bolus regimen of glarg<strong>in</strong>e plusglulis<strong>in</strong>e or regular <strong>in</strong>sul<strong>in</strong> on a slid<strong>in</strong>g scale.The basal-bolus group got 0.5 U/kg/day, halfof it as glarg<strong>in</strong>e once daily <strong>and</strong> half as glulis<strong>in</strong>ebefore meals. The <strong>to</strong>tal daily dose was reduced<strong>to</strong> 0.3 U/kg/day <strong>in</strong> <strong>patients</strong> age 70 <strong>and</strong> older orwho had a serum creat<strong>in</strong><strong>in</strong>e level of 2.0 mg/dLor higher.The goal was <strong>to</strong> ma<strong>in</strong>ta<strong>in</strong> fast<strong>in</strong>g <strong>and</strong> premealglucose concentrations between 100 <strong>and</strong>140 mg/dL. The <strong>to</strong>tal daily dose was raised by10% (mostly <strong>in</strong> the glarg<strong>in</strong>e dose) if the bloodglucose level was <strong>in</strong> the range of 141 <strong>to</strong> 180mg/dL, <strong>and</strong> by 20% if the glucose level washigher than 181 mg/dL. The dose was decreasedby 10% for glucose levels between 70<strong>and</strong> 99 mg/dL, was decreased by 20% if the382 CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 78 • NUMBER 6 JUNE 2011
UMPIERREZglucose level was between 40 <strong>and</strong> 69, <strong>and</strong> washeld if the glucose level was lower than 40 mg/dL. If a patient was not able <strong>to</strong> eat, <strong>in</strong>sul<strong>in</strong> glulis<strong>in</strong>ewas held until meals were resumed.The slid<strong>in</strong>g-scale group received regular<strong>in</strong>sul<strong>in</strong> four times a day for blood glucose levelshigher than 140 mg/dL.The primary outcomes measured werethe difference between groups <strong>in</strong> mean dailyblood glucose concentration <strong>and</strong> a compositeof hospital complications <strong>in</strong>clud<strong>in</strong>g pos<strong>to</strong>perativewound <strong>in</strong>fection, pneumonia, respira<strong>to</strong>ryfailure, acute renal failure, <strong>and</strong> bacteremia.Secondary outcomes were differences betweengroups <strong>in</strong> mean fast<strong>in</strong>g <strong>and</strong> pre-meal blood glucose,number of hypoglycemic episodes (bloodglucose < 70 mg/dL), hyperglycemic episodes(blood glucose > 200 mg/dL), length of hospitalstay, need for <strong>in</strong>tensive care, <strong>and</strong> rateof complications <strong>in</strong>clud<strong>in</strong>g wound <strong>in</strong>fection,pneumonia, acute renal failure, <strong>and</strong> death.Blood glucose levels were significantly lower<strong>in</strong> the basal-bolus group through the first 7days after r<strong>and</strong>omization, as measured beforebreakfast, lunch, <strong>and</strong> d<strong>in</strong>ner, <strong>and</strong> at bedtime,<strong>and</strong> then they converged.More <strong>patients</strong> <strong>in</strong> the slid<strong>in</strong>g-scale grouphad hospital complications, 26 vs 9, P = .003.On the other h<strong>and</strong>, more <strong>patients</strong> <strong>in</strong> the basalbolusgroup had episodes of hypoglycemia: 24(23%) vs 5 (4.7%) had episodes of less than 70mg/dL (P < .001), 12 (12%) vs 2 (1.9%) hadepisodes of less than 60 mg/dL (P = .005), <strong>and</strong>4 (3.8%) vs 0 had episodes of less than 40 mg/dL (P = .057). The mean <strong>to</strong>tal daily dose of<strong>in</strong>sul<strong>in</strong> was 33.4 units <strong>in</strong> the basal-bolus group<strong>and</strong> 12.3 units <strong>in</strong> the slid<strong>in</strong>g-scale group.■■WHAT HAVE WE LEARNED?Don’t use a slid<strong>in</strong>g-scale regimen as a s<strong>in</strong>gleagent <strong>in</strong> <strong>patients</strong> with <strong>diabetes</strong>. Glycemiccontrol is better with a basal-bolus regimenthan with a slid<strong>in</strong>g-scale regimen, <strong>and</strong> a basalbolus<strong>in</strong>sul<strong>in</strong> regimen is preferred for most <strong>patients</strong>with hyperglycemia.The old human <strong>in</strong>sul<strong>in</strong>s (ie, regular <strong>and</strong>NPH) are still good <strong>and</strong> improve glycemiccontrol as well as the new basal <strong>in</strong>sul<strong>in</strong> analogues(detemir <strong>and</strong> aspart) do.Improved control may reduce the rate ofhospital complications, accord<strong>in</strong>g <strong>to</strong> prelim<strong>in</strong>aryevidence. More studies are under way.One size does not fit all. Those who areelderly or who have impaired renal functionshould receive lower doses of <strong>in</strong>sul<strong>in</strong>, eg, 0.3U/kg/day <strong>in</strong>stead of 0.5 U/kg/day. Those whoare on <strong>in</strong>sul<strong>in</strong> should have their dose decreasedwhen they are admitted <strong>to</strong> the hospital.Perhaps lean <strong>patients</strong> with <strong>type</strong> 2 <strong>diabetes</strong>should also have a lower dose.Most hospitalized <strong>patients</strong> with <strong>diabetes</strong><strong>and</strong> elevated blood glucose values (or hyperglycemia)should receive subcutaneous <strong>in</strong>sul<strong>in</strong>treatment with a basal-bolus regimen or amultidose comb<strong>in</strong>ation of NPH plus regular<strong>in</strong>sul<strong>in</strong>. Selected <strong>patients</strong> with severe <strong>in</strong>sul<strong>in</strong>resistance <strong>and</strong> persistent hyperglycemia despitesubcutaneous <strong>in</strong>sul<strong>in</strong> may benefit fromcont<strong>in</strong>uous <strong>in</strong>travenous <strong>in</strong>sul<strong>in</strong> <strong>in</strong>fusion.Patients treated with <strong>in</strong>sul<strong>in</strong> at homeshould cont<strong>in</strong>ue <strong>to</strong> receive <strong>in</strong>sul<strong>in</strong> therapy<strong>in</strong> the hospital. <strong>How</strong>ever, the <strong>in</strong>sul<strong>in</strong> dosageshould be reduced by about 25% <strong>to</strong> allow forlower food <strong>in</strong>take.■■QUESTIONS FOR FURTHER STUDYShould we modify the st<strong>and</strong>ard basal-bolusregimen?In a typical basal-bolus regimen, <strong>patients</strong> get50% of their <strong>to</strong>tal daily <strong>in</strong>sul<strong>in</strong> dose <strong>in</strong> theform of a basal <strong>in</strong>jection <strong>and</strong> 50% <strong>in</strong> the formof rapid-act<strong>in</strong>g boluses before meals. <strong>How</strong>ever,for a variety of reasons, hospitalized <strong>patients</strong>do not eat very much. Thus, a 50-50 basal-bolusregimen may not be ideal for <strong>patients</strong> withpoor oral <strong>in</strong>take.In the Basal-PLUS trial, currently underway, we are compar<strong>in</strong>g the safety <strong>and</strong> efficacyof a daily dose of basal <strong>in</strong>sul<strong>in</strong> (glarg<strong>in</strong>e)plus correction doses of a rapid-act<strong>in</strong>g <strong>in</strong>sul<strong>in</strong>analogue (glulis<strong>in</strong>e) on a slid<strong>in</strong>g scale <strong>and</strong> ast<strong>and</strong>ard basal-bolus regimen <strong>in</strong> <strong>medical</strong> <strong>and</strong><strong>surgical</strong> <strong>patients</strong>.Does one glycemic target fit all <strong>patients</strong>?Falciglia et al 19 found an association betweenhyperglycemia <strong>and</strong> death <strong>in</strong> <strong>patients</strong> with unstableang<strong>in</strong>a, arrhythmias, stroke, pneumonia,gastro<strong>in</strong>test<strong>in</strong>al bleed<strong>in</strong>g, respira<strong>to</strong>ry failure,sepsis, acute renal failure, <strong>and</strong> congestiveheart failure. <strong>How</strong>ever, they found no suchassociation <strong>in</strong> <strong>patients</strong> with chronic obstruc-NPH plusregular<strong>in</strong>sul<strong>in</strong> wasjust as good asdetemir plusaspart <strong>in</strong>improv<strong>in</strong>gglycemiccontrolCLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 78 • NUMBER 6 JUNE 2011 383
TYPE 2 DIABETES IN THE HOSPITALMore <strong>patients</strong><strong>in</strong> the slid<strong>in</strong>gscalegroupthan <strong>in</strong> thebasal-bolusgroup hadhospitalcomplicationstive pulmonary disease, liver failure, diabeticke<strong>to</strong>acidosis, gastro<strong>in</strong>test<strong>in</strong>al neoplasm, musculoskeletaldisease, peripheral vascular diseasewith bypass, hip fracture, amputation due<strong>to</strong> peripheral vascular disease, or prostate surgery.Should <strong>patients</strong> <strong>in</strong> this second group betreated with a less-<strong>in</strong>tensive <strong>in</strong>sul<strong>in</strong> regimen?What is the best regimen after hospitaldischarge?We are conduct<strong>in</strong>g a prospective cl<strong>in</strong>ical trial<strong>to</strong> assess the impact of <strong>in</strong>sul<strong>in</strong> after hospitaldischarge. Our current practice when a patientis discharged from the hospital is as follows:■■REFERENCES1. Cook CB, Kongable GL, Potter DJ, Abad VJ, Leija DE,Anderson M. Inpatient glucose control: a glycemic surveyof 126 U.S. hospitals. J Hosp Med 2009; 4:E7–E14.2. Kosiborod M, Inzucchi S, Clark B, et al. National patternsof glucose control among <strong>patients</strong> hospitalized withacute myocardial <strong>in</strong>farction [abstract]. J Am Coll Cardiol2007; 49:283A–284A.3. Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM,Kitabchi AE. Hyperglycemia: an <strong>in</strong>dependent markerof <strong>in</strong>-hospital mortality <strong>in</strong> <strong>patients</strong> with undiagnosed<strong>diabetes</strong>. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 2002; 87:978–982.4. Robb<strong>in</strong>s JM, Webb DA. Diagnos<strong>in</strong>g <strong>diabetes</strong> <strong>and</strong> prevent<strong>in</strong>grehospitalizations: the urban <strong>diabetes</strong> study.Med Care 2006; 44:292–296.5. Moghissi ES, Korytkowski MT, DiNardo M, et al.American Association of Cl<strong>in</strong>ical Endocr<strong>in</strong>ologists <strong>and</strong>American Diabetes Association consensus statemen<strong>to</strong>n <strong>in</strong>patient glycemic control. Diabetes Care 2009;32:1119–1131.6. Saudek D, Herman WH, Sacks DB, Bergenstal RM,Edelman D, Davidson MB. A new look at screen<strong>in</strong>g <strong>and</strong>diagnos<strong>in</strong>g <strong>diabetes</strong> mellitus. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab2008; 93:2447–2453.7. Norhammar A, Tenerz A, Nilsson G, et al. Glucose metabolism<strong>in</strong> <strong>patients</strong> with acute myocardial <strong>in</strong>farction <strong>and</strong>no previous diagnosis of <strong>diabetes</strong> mellitus: a prospectivestudy. Lancet 2002; 359:2140–2144.8. Matz K, Keresztes K, Tatschl C, et al. Disorders of glucosemetabolism <strong>in</strong> acute stroke <strong>patients</strong>: an underrecognizedproblem. Diabetes Care 2006; 29:792–797.9. American Diabetes Association. Diagnosis <strong>and</strong> classificationof <strong>diabetes</strong> mellitus. Diabetes Care 2010; 33(suppl1):S62–S69.10. McAlister FA, Majumdar SR, Blitz S, Rowe BH, RomneyJ, Marrie TJ. The relation between hyperglycemia <strong>and</strong>outcomes <strong>in</strong> 2,471 <strong>patients</strong> admitted <strong>to</strong> the hospital withcommunity-acquired pneumonia. Diabetes Care 2005;28:810–815.11. Falguera M, Pifarre R, Mart<strong>in</strong> A, Sheikh A, Moreno A. Etiology<strong>and</strong> outcome of community-acquired pneumonia <strong>in</strong>• If the admission hemoglob<strong>in</strong> A 1clevel isless than 7%, we restart the previous outpatienttreatment regimen of oral antidiabeticagents, or <strong>in</strong>sul<strong>in</strong>, or both.• If the admission hemoglob<strong>in</strong> A 1cis between7% <strong>and</strong> 9%, we restart the outpatient oralagents <strong>and</strong> cont<strong>in</strong>ue glarg<strong>in</strong>e once daily at50% <strong>to</strong> 80% of the hospital dose.• If the hemoglob<strong>in</strong> A 1clevel is higher than9%, we discharge the patient on a basalbolusregimen at the same dosage as <strong>in</strong> thehospital. As an alternative, we could restartthe oral agents <strong>and</strong> add glarg<strong>in</strong>e once dailyat 80% of the hospital dose.■<strong>patients</strong> with <strong>diabetes</strong> mellitus. Chest 2005; 128:3233–3239.12. Noordzij PG, Boersma E, Schre<strong>in</strong>er F, et al. Increasedpreoperative glucose levels are associated with perioperativemortality <strong>in</strong> <strong>patients</strong> undergo<strong>in</strong>g noncardiac,nonvascular surgery. Eur J Endocr<strong>in</strong>ol 2007; 156:137–142.13. Frisch A, Ch<strong>and</strong>ra P, Smiley D, et al. Prevalence <strong>and</strong>cl<strong>in</strong>ical outcome of hyperglycemia <strong>in</strong> the perioperativeperiod <strong>in</strong> noncardiac surgery. Diabetes Care 2010;33:1783–1788.14. Moghissi ES, Korythowski MT, DiNardo M, et al.American Association of Cl<strong>in</strong>ical Endocr<strong>in</strong>ologists <strong>and</strong>American Diabetes Association consensus statemen<strong>to</strong>n <strong>in</strong>patient glycemic control. Endocr<strong>in</strong>e Pract 2009;15:1–17.15. Umpierrrez GE, Smiley D, Zisman A, et al. R<strong>and</strong>omizedstudy of basal-bolus <strong>in</strong>sul<strong>in</strong> therapy <strong>in</strong> the <strong>in</strong>patient<strong>manage</strong>ment of <strong>patients</strong> with <strong>type</strong> 2 <strong>diabetes</strong> (RABBIT 2trial). Diabetes Care 2007; 30:2181–2186.16. Umpierrez GE, Hor T, Smiley D, et al. Comparison of <strong>in</strong>patient<strong>in</strong>sul<strong>in</strong> regimens with detemir plus aspart versusneutral protam<strong>in</strong>e Hagedorn plus regular <strong>in</strong> <strong>medical</strong><strong>patients</strong> with <strong>type</strong> 2 <strong>diabetes</strong>. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab2009; 94:564–569.17. Umpierrez GE, Smiley D, Umpierrez D, Ceron M, TemponiA. Hypoglycemic events dur<strong>in</strong>g subcutaneous <strong>in</strong>sul<strong>in</strong>therapy <strong>in</strong> <strong>type</strong> 2 <strong>diabetes</strong> (abstract). Presented atAmerican Diabetes Association 69th Scientific Sessions,New Orleans, LA, June 5–9, 2009.18. Umpierrez GE, Smiley D, Jacobs S, et al. R<strong>and</strong>omizedstudy of basal-bolus <strong>in</strong>sul<strong>in</strong> therapy <strong>in</strong> the <strong>in</strong>patient<strong>manage</strong>ment of <strong>patients</strong> with <strong>type</strong> 2 <strong>diabetes</strong> undergo<strong>in</strong>ggeneral surgery (RABBIT 2 surgery). Diabetes Care2011; 34:256–261.19. Falciglia M, Freyberg RW, Almenoff PL, D’Alessio DA,Render ML. Hyperglycemia-related mortality <strong>in</strong> criticallyill <strong>patients</strong> varies with admission diagnosis. Crit CareMed 2009; 37:3001–3009.ADDRESS: Guillermo Umpierrez, MD, Emory University Schoolof Medic<strong>in</strong>e, Department of Medic<strong>in</strong>e, Division of Endocr<strong>in</strong>ology<strong>and</strong> Metabolism, 49 Jesse Hill Jr. Drive, Atlanta, GA30303; geumpie@emory.edu.CME ANSWERSAnswers <strong>to</strong> the credit tests on page 415 of this issueDiabetes 1D 2D Progressive weakness 1D 2C Stat<strong>in</strong> myopathy 1E 2A ST depression, T-wave <strong>in</strong>version 1E 2D384 CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 78 • NUMBER 6 JUNE 2011