Luminal & intestinal flagellates
Luminal & intestinal flagellates Luminal & intestinal flagellates
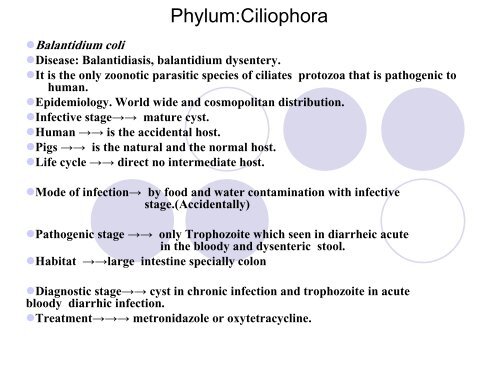
Phylum:Ciliophora•Balantidium coli•Disease: Balantidiasis, balantidium dysentery.•It is the only zoonotic parasitic species of ciliates protozoa that is pathogenic tohuman.•Epidemiology. World wide and cosmopolitan distribution.•Infective stage→→ mature cyst.•Human →→ is the accidental host.•Pigs →→ is the natural and the normal host.•Life cycle →→ direct no intermediate host.•Mode of infection → by food and water contamination with infectivestage.)Accidentally)•Pathogenic stage →→ only Trophozoite which seen in diarrheic acutein the bloody and dysenteric stool.•Habitat →→large intestine specially colon•Diagnostic stage→→ cyst in chronic infection and trophozoite in acutebloody diarrhic infection.•Treatment→→→ metronidazole or oxytetracycline.
- Page 2 and 3: Life cycle of Balantidium coli.
- Page 4 and 5: Life cycle of Giardia lambelia
- Page 6 and 7: GIARDIA Treatment•Treatment:• K
- Page 8 and 9: Trichomonas vaginalis• Etiology:
- Page 10 and 11: Hemoflagellate(Blood and Tissue)•
- Page 12 and 13: Life cycle in general of leishmania
- Page 14: Cutaneous leishmaniasis
Phylum:Ciliophora•Balantidium coli•Disease: Balantidiasis, balantidium dysentery.•It is the only zoonotic parasitic species of ciliates protozoa that is pathogenic tohuman.•Epidemiology. World wide and cosmopolitan distribution.•Infective stage→→ mature cyst.•Human →→ is the accidental host.•Pigs →→ is the natural and the normal host.•Life cycle →→ direct no intermediate host.•Mode of infection → by food and water contamination with infectivestage.)Accidentally)•Pathogenic stage →→ only Trophozoite which seen in diarrheic acutein the bloody and dysenteric stool.•Habitat →→large intestine specially colon•Diagnostic stage→→ cyst in chronic infection and trophozoite in acutebloody diarrhic infection.•Treatment→→→ metronidazole or oxytetracycline.
Life cycle of Balantidium coli.
Sub-phylum: Mastigophora(<strong>Luminal</strong> & <strong>intestinal</strong> <strong>flagellates</strong>)• Giardia lamblia (flagellate).• Disease : Giardiasis (lambliasis)• Epidemiology →→ World wide and cosmopolitan distribution.• Infective stage→→ Quadrinucleate oval mature cyst.• Life cycle →→ Direct no intermediate host.• Mode of infection→ by food and water contamination withinfective stage.• Pathogenic stage →→ only Trophozoite which seen indiarrheic acute steatorrhae stool.• Habitat →→small intestine specially duodenum• Diagnostic stage→→ cyst in chronic infection and trophozoitein acute fatty diarrhic infection.
Life cycle of Giardia lambelia
Symptoms & Pathology:•Symptoms:•The abdominal distension, fattydiarrhea (steatorrhea) The stoolcontains excessive lipids but veryrarely any blood.•The more chronic stage is associatedwith vitamin B12 malabsorption•disaccharides deficiency.
GIARDIA Treatment•Treatment:• Keep the child hydrated.If it isdehydrated.• using drugs• 1-Metronidazole(Flagyle).2-Tindazole a new Giardia drugsunder 3 years children.
Genus:TrichomonasThere are three species of genus Trichomonas• Trichomonas tenax :It is non pathogenic parasiticflagellate of the mouth, saliva, teeth pockets.• Trichomonas hominis: It is non pathogenic parasiticflagellate of the intestine.• Trichomonas vaginalis: It is pathogenic parasiticflagellate of the male and female urogenital system• All these species have only trophozoite, no cyst stage.• Trophozoite is the pathogenic, infective, and diagnosticstage
Trichomonas vaginalis• Etiology: Trichomonas vaginalis , it is urogenital (flagellate)• Epidemiology: It has a world-wide distribution; as low as 5% in normal females.• Disease →→Trichomonad vaginitis, trichomonad prostatis• Only has trophozoite during its life cycle. NO CYST STAGE. and divides by binaryfission• Infective stage→→ Trophozoite.• Human →→ male and female both are infected• Life cycle →→ direct no intermediate host.• Mode of infection → sexually or by direct contamination from contaminatedbathroom.• Pathogenic stage →→ only Trophozoites.• Habitat →→female and male urogenital system• Diagnostic stage→→ only Trophozoite which seen in urine or vaginal swab.• Treatment → Metronidazole (Flagyle) tablets for men and vaginalsuppository for females.
Life cycle of Trichomonas vaginalis
Hemoflagellate(Blood and Tissue)•Protozoan <strong>flagellates</strong> that are parasitic inthe blood and tissue of many species ofanimals and of humans; they include the2 genera which are medically important:•A-Genus→ Leishmania.•B-Genus→ Trypanosoma.•several species of which are importantpathogens.
A-Genus: Leishmania• Leishmania is a genus of protozoa.• is the parasite responsible for the disease leishmaniasis.• Most Leishmania vector are females sandflies of the genus Phlebotomus• Their primary hosts are vertebrates and Human.• All species habitat is obligatory intracelluar(Mostly macrophages, in less neutrophile.• reservoir hosts →→fox, jackal, rodents and wolves .• All human Leishmania are zoonotic pathogenic protozoa.• All human species have indirect life cycle.• Mode of infection → by vector sand fly bit of skin.• Route of infection→ exposed skin places.• All human Leishmania species are seriously and medically pathogenic.• Treatment –• 1-Amphoteracin B• 2-pentostam( Sodium stibogluconate) is a medicine used to treat leishmaniasis and is only availablefor administration by injection• Prevention. Protection from sand fly bite is essential• All human species of leishmania have two stages in its life cycle:1-Amastigote: is a stage that does not have a visible external flagella. The term. itisthe form the parasite lives in the human macrophages skin.2-Promastigote. is a stage that does have a visible external flagella. it is the formtheparasite lives in the vector sand fly gut.
Life cycle in general of leishmania
Leishmania speciesLeishmania tropica and major.• Disease →cutanious leishmaniasis, oriental sore, Baghdad boil, Delhi ulcer.• Habitat →obligatory intracellular specially macrophages of skin.• Symptoms• The disease begins as a small, red, painless papule.• usually 2 to 4 weeks after the sand fly bite.• The papule enlarges to approximately 2 cm over the next weeks The papulesbecomes crusted over, and if the crust is removed, a shallow indurate maydeveloped to expanding satellite shape ulcer.• After the lesion has been present for 2 months, it ceases expanding and after 3to 6 months begins to heal, leaving a depressed scar.• The number of lesions can range from 1 to 100 or more.• Diagnosis depends upon finding the amasitgote stage in the skin(Macrophages).
Cutaneous leishmaniasis