comprehensive pain assessment form — cognitively intact
comprehensive pain assessment form — cognitively intact
comprehensive pain assessment form — cognitively intact
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
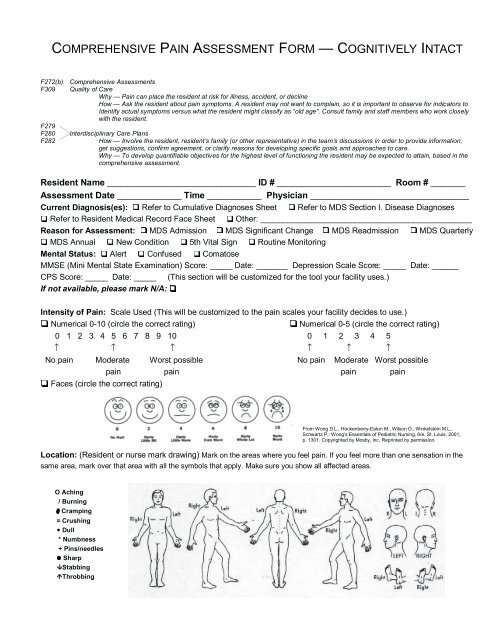
COMPREHENSIVE PAIN ASSESSMENT FORM <strong>—</strong> COGNITIVELY INTACTF272(b)F309F279F280F282Comprehensive AssessmentsQuality of CareWhy <strong>—</strong> Pain can place the resident at risk for illness, accident, or declineHow <strong>—</strong> Ask the resident about <strong>pain</strong> symptoms. A resident may not want to complain, so it is important to observe for indicators toIdentify actual symptoms versus what the resident might classify as “old age”. Consult family and staff members who work closelywith the resident.Interdisciplinary Care PlansHow <strong>—</strong> Involve the resident, resident’s family (or other representative) in the team’s discussions in order to provide in<strong>form</strong>ation,get suggestions, confirm agreement, or clarify reasons for developing specific goals and approaches to care.Why <strong>—</strong> To develop quantifiable objectives for the highest level of functioning the resident may be expected to attain, based in the<strong>comprehensive</strong> <strong>assessment</strong>.Resident Name ______________________________ ID # _______________________ Room # _______Assessment Date _____________ Time ___________ Physician ________________________________Current Diagnosis(es): Refer to Cumulative Diagnoses Sheet Refer to MDS Section I. Disease DiagnosesRefer to Resident Medical Record Face Sheet Other: _______________________________________________Reason for Assessment: MDS Admission MDS Significant Change MDS Readmission MDS QuarterlyMDS Annual New Condition 5th Vital Sign Routine MonitoringMental Status: Alert Confused ComatoseMMSE (Mini Mental State Examination) Score: _____ Date: _______ Depression Scale Score: _____ Date: ______CPS Score: _____ Date: _____ (This section will be customized for the tool your facility uses.)If not available, please mark N/A:Intensity of Pain: Scale Used (This will be customized to the <strong>pain</strong> scales your facility decides to use.)Numerical 0-10 (circle the correct rating)Numerical 0-5 (circle the correct rating)0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 ↑ ↑ ↑ ↑ ↑ ↑No <strong>pain</strong> Moderate Worst possible No <strong>pain</strong> Moderate Worst possible<strong>pain</strong> <strong>pain</strong> <strong>pain</strong> <strong>pain</strong>Faces (circle the correct rating)From Wong D.L., Hockenberry-Eaton M., Wilson D., Winkelstein M.L.,Schwartz P.: Wong’s Essentials of Pediatric Nursing, 6/e, St. Louis, 2001,p. 1301. Copyrighted by Mosby, Inc. Reprinted by permission.Location: (Resident or nurse mark drawing) Mark on the areas where you feel <strong>pain</strong>. If you feel more than one sensation in thesame area, mark over that area with all the symbols that apply. Make sure you show all affected areas.O Aching/ Burning# Cramping= CrushingDull* Numbness+ Pins/needlesSharpStabbingThrobbing
History of PainOnset of Pain: New (within the last 7 days) Recent (within the last 3 mos.) More distant (> 3 mos.)Type/Frequency of Pain: Constant Intermittent Other, describe: _________________________________Description of Pain: Aching Burning Cramping Crushing Dull Numbness Pins & NeedlesSharp Shooting Throbbing Other, describe: _________________________________________________Change in Pattern of Pain: Has the discomfort changed in description or intensity the last 7 days? Yes NoIf yes, describe the change: ______________________________________________________________________Causes/Increases in Pain: Movement Coughing Cold Heat Fatigue Anxiety Other, describe: _______________________________________________________________________________________________What Relieves the Pain: Cold Eating Exercise Heat Medication Massage Relaxation RestRepositioning Other, describe: _______________________________________________________________Manner of expressing <strong>pain</strong>: (per resident or by observation) Facial expressions Guarding MoaningReadily describes <strong>pain</strong> Restlessness Rubbing area Other, describe: _____________________________Effects of Pain: (Note decreased function) Using the following scale, rate how the <strong>pain</strong> has had an effect in eacharea in the past 24 hours: 0 (no effect) 2 (mild effect) 5 (moderate effect) 10 (severe effect)Accompanying Symptoms (e.g., nausea) _____ Sleep Disturbance _____ Appetite Change _____Physical Activity Change _____ Mood/Behavior ______ Concentration _____Relationship with Others ______Other (describe): _________________________________Worst Pain in the Last 24 hours: 0 1 2 3 4 5 6 7 8 9 10↑ ↑ ↑No <strong>pain</strong> Moderate Worst possible<strong>pain</strong><strong>pain</strong>In the past 24 hours, how much have the medications or treatments eased your <strong>pain</strong>?0 No relief 2 Mild relief 5 Moderate relief 8 Relief 10 Complete reliefIn<strong>form</strong>ation provided by: (Check all that apply) resident family significant others staffPlan for Addressing Pain: Initiate <strong>pain</strong> management flow sheet Call physician/NP/PA-C Refer to <strong>pain</strong>teamRehab referral (PT, OT, ST) Non-med intervention Medications prescribed Spiritual counselingStaff education/communicationComments: __________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________Resident’s Pain Control GoalResident’s Pain Intensity GoalSleep comfortablyComfort at restComfort with movementTotal <strong>pain</strong> controlStay alertPer<strong>form</strong> activitiesOther: ____________________________________________________1 2 3 4 5 6 7 8 9 10(Circle the correct rating)(Will customize to Numerical 0-5 or 0-10)Signature/Title of person completing <strong>assessment</strong>: _____________________________________ Date: __________Resident _____________________ ID#____________________Room # ____________ PhysicianAugust 2001
Pain Management Flow SheetDate TimeLocation of Pain(refer to <strong>pain</strong> <strong>assessment</strong>,if applicable)CurrentIntensityScale usedPrecipitating/Aggravating Factor(s)Non-MedInterventionMedication/Dose(See MAR for details,e.g.,route,frequency)DateFollow-up Monitoring ofEffective InterventionI ntensity of Painl3 0 min. 2 hour sArousaScaleInitialsPain Scale CodesN = Numer caF = Faces(Willcustomizefor<strong>pain</strong>sca esused)A.Rehab services1 = Safety <strong>assessment</strong>2 = Immobilization of joi nts3 = Strength & endurance4 = Other <strong>pain</strong> management techn iquessuch as ultrasound & transcutaneouselectrical nerve st mulat on (TENS)B.NON-MED INTERVENTION CODESPhysical modalities1 = Heat2 = Ice3 = MassageC.Relaxationtechniques1 = Individual2 =3 =Group1:1 activities& distractionD.Psychological & social1 = Fam il y v isits2 = Spiritual counse ling3 = OthersupportSUGGESTED AROUSAL SCALE1 = Wide2 = Drowsy3 =4 =5 =awakeDozing intermittentlyOnly awakens whenAsleep at the time ofaroused<strong>assessment</strong>Comments:____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________I nitials S ignature/ T itleI nitial s S ignature/ T itleI nitial sS g nature/ T itl eI nitial sSignature/ T itl eI nitials S ignature/ T itleI nitial s S ignature/ T itleI nitial sS g nature/ T itl eI nitial sSignature/ T itl eResident_____________________ ID# ___________________Room # ____________ Phys(ora facilitylabecanbep acedhere)ician ________________________August2001/illlliiii
Pain Management Interdisciplinary Team SummaryPhysician and IDT should discuss physician’s findings and develop interventionsP roblem related to: D efining Characteristic sG oal sIntervention s( check those that apply)check those that apply )( check those that apply )Responsible( ( check those that apply )Disciplin eC hronic physicalResident self report o f Resident will:5 th vital sign monitoring Collaborate with physician /Verbalize or acknowledge <strong>pain</strong> C omplete <strong>pain</strong> <strong>assessment</strong> PA-C/NP if <strong>pain</strong> contro ld isability<strong>pain</strong>, discomfort, fatigu ewhen questioned by staffM onitor elements of <strong>pain</strong>: measures currently ordere dC hronic psychological O bserved non-verba lIndicate location of <strong>pain</strong> whenF requenc yare ineffectiv ed isabilityb ehavior cues of pai n questioned by staffI ntensit yTeach, coach, and monito rM usculoskeletalP hysical and socialEstablish a <strong>pain</strong> goal of tolerabl eL ocatio nadjuvant therapy (distractio nS tandardized <strong>pain</strong> scale imagery, relaxation )impairmentw ithdrawa llimits on a standardized pai nu sedDocument <strong>pain</strong> ratin gC irculatory impairment A ltered ability to continu e scaleA ssess resident 20-3 0before/after intervention sS kin or tissue impair-previous activitie sA lert staff of need for PRNm inutes after medicatio n Monitor sleep pattern, adjus ta nalgesic to maintain comfortm entAnorexi aa dministration fo rmedications and non -E xpress relief or decreasede ffectivenes smedication interventions t oN eurological impairment W eight change sd iscomfort 20-30 minutes afte r R ecord response t oallow 3-4 hour sA dvanced diseaseC hanges in slee pa nalgesic us em edications and adjus t uninterrupted slee pp rocesspatternsAlert staff of need for non-m edication as necessar y Assess GI status an dA geFacial mask of pai nmedication interventions toOffer support and reassur-tolerance to medications;improve/maintain comforta nce that <strong>pain</strong> relief will be implement bowel program t oD iagnosis/medicalG uarded movemen tReport or exhibit increased ROM p rovided quickly and to th e prevent constipatio nh istory of: ( circle th e L imited range of motio n20-30 minutes after analgesic use m aximum extent possibl e Assess changes in <strong>pain</strong> tha tc orrect Dx/Hx)L imited ability to perfor mE ducate resident/significant may indicate new proble mDemonstrate muscle relaxatio nD iabetesA DL so thers about <strong>pain</strong>/<strong>pain</strong> re-1:1 visits to provid ewhen experiencing increase dliefmeasurestherapeutic interventio nA SHD ( Arteriosclerotic Hear t L imited ability to transfe r discomfortU tilize <strong>pain</strong> managemen t 1:1 visits to encourag eD isease)a nd ambulateVerbalize frustrations & feeling s f low shee tspiritual resource sP VD ( Peripheral Vascular Disease )Gait disturbancer egarding disease proces sT each and per<strong>form</strong> non - Volunteer visit sArthritisE xpress loss of intimacy andm edication intervention s 1:1 visits to identify foo dFallsHip Fracturec ompanionshipa nd evaluate effect (circl e preferences and comfor tD econditioningP articipate in activity programs o r t hose that apply )food sOsteoporosisS low rehabilitationleisure activitiesP ositionin gInvolve family in initial pai nP athological Bone FxCognitive dysfunction Have 3-4 hours of uninterrupted M assag eassessmen tO ther Fracturessleep at nightC old/hea tDocument historica l(impaired memory)M ultiple SclerosisWill have decreased or resolve d R elaxationbehavior to express pai nI ncontinenceindicators of discomfort (crying,D iversio nAround the clock (ATC )DepressionC onstipationExerciseacting out, restlessness,dosing of medication sO ther: _____________D eep breathin ginsomnia, etc.)Medicate before planne dT ENSactivities/exercise sMusicElevation of extremitiesImmobilizationD ate I nitial s S ignature/Titl eI nitial s Signature/Titl eR NS = Nursing Service sESPONSIBLE DISCIPLINESC H = ChaplainPT = Physical Therap yD ate I nitials S ignature/Titl eI nitial s Signature/Titl eDT = Dietar yST = Speech TherapyPR = Physician/Mid-Level Practitioner RT = Recreational Therapy/Activities= Occupational TherapySS = Social ServicesResident_____________________ ID# ___________________Room # ____________ Physician ________________________(ora facilitylabelcanbeplacedhere)Provided by the Oklahoma Foundation forMedical Quality, the Medicare QualityImprovement Organization for Oklahoma,under contract with the Centers forMedicare & Medicaid Services, US Dept.of Health and Human Services. Thecontents do not necessarily reflect CMSspolicy. 1A-032-CPACIM-OK-040306.OTFAM = FamilyAugust2001