Download The Pharos Winter 2012 Edition - Alpha Omega Alpha
Download The Pharos Winter 2012 Edition - Alpha Omega Alpha
Download The Pharos Winter 2012 Edition - Alpha Omega Alpha
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Editorial Board Officers and Directors at LargeMedical Organization DirectorCouncilor DirectorsCoordinator, Residency InitiativesStudent DirectorsAdministrative Office525 Middlefield Road, Suite 130
Find joy in your mentee’simprovement and successesHave a clear understanding of theexpectations and goals of yourmenteeEncourage your mentee’s ideasand workProvide constructive and usefulcritique of your mentee’s workChallenge your mentee toexpand and improve his abilitiesRespect the uniqueness andcontributions of your menteeTable 2: Working with Your MenteeAcknowledge contributions ofyour menteeHelp your mentee develophumilityHelp your mentee develop selfesteemBe aware of biases and don’t letassumptions interfereEncourage your mentee to takeon leadership rolesObserve your mentee at herprofessional workIn contrast, coaching holds that no matter how well preparedpeople are after their education and training, few canachieve and maintain their best performance on their own.Most people continue to practice what they are already goodat, but need an outside perspective to learn how to continueto improve.Good coaches or mentors can observe a performance andbreak it down into crucial individual components, then makesuggestions about how to improve. A good coach makes youaware of where you are falling short. <strong>The</strong>n, with the coach’sfeedback and suggestions and your own self-effacement andpersonal practice, you can move forward.<strong>The</strong>re are currently no recognized coaches in medicine.<strong>The</strong> practice of medicine is largely unwitnessed by anyone.After a number of years of “practice,” a doctor is considered anexpert forever. But this is clearly not true. Gawande writes: “AsI went along, I compared my results against national data, andI began beating the averages. My rates of complications movedsteadily lower and lower. And then, a couple of years ago, theydidn’t. It started to seem that the only direction things couldgo from here was the wrong one.” Recalling an afternoon spentwith a tennis coach improving his serve, Gawande decidedwhat he needed was a surgical coach. He enlisted a formermentor who observed him in practice and made many helpfulsuggestions for improvement in his operations. With thatcoaching, he was successful in improving performance, andhopefully patient outcomes.Gawande concludes, “Coaching done well may be the mosteffective intervention designed for human performance.” Hewrites, “In the past year, I’ve thought nothing of asking myhospital to spend some hundred thousand dollars to upgradethe surgical equipment I use, in the vague hope of giving mefiner precision and reducing complications. . . But the three orfour hours I’ve spent with [my coach] each month have almostcertainly added more to my capabilities than any of this.”While many of us empirically know the value and importanceof teaching, mentoring, and coaching in professionalSelf-AssessmentHave a clear understanding ofyour motivation to be mentoredSelect a mentor based on yourshort-term goals and careerinterestsHave a clear understandingof your expectations of yourmentorBe proactive to find mentorsBe realistic about timecommitmentsEnsure a noncompetitiverelationshipDetermine your areas of needDetermine the help needed toreach your potential and goalsDecide what you hope to gainfrom mentoringCommunicate your expectationsBe reliableBe honestFollow throughTable 3: Tips for Menteesdevelopment and in medicine, the effects of mentoring aredifficult to measure and the literature is limited. Among theperceived benefits of mentoring include greater satisfactionin the profession, help with and a widening of career choices,improved coping skills, increased social support, improvedprofessional development, improved bedside and learningskills, better ability to monitor personal development, improvedprofessional behavior, broader educational experience,and increased networking.Our profession requires us to be continual students andlearners and show continual improvement as physicians. Allof us can use good teachers, mentors, and coaches.Physicians have always been teachers. We often think aboutteaching medicine in the traditional sense of lectures, casepresentations, ward rounds, surgery, and other learning experiences.I believe we should view mentoring as a professionalobligation and seek opportunities to mentor others.I hope you will read and reflect on mentors, mentoring,and coaching and pursue opportunities to give back to otherswhat you have learned and experienced preparing for andpracticing in medicine.Richard L. Byyny, MD, FACPExecutive Director, <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong>Editor, <strong>The</strong> <strong>Pharos</strong>LearnActively listen and contribute tothe conversationsDo your homeworkUse other resources to look upuseful informationDemonstrate the ability to setagendasAsk what knowledge, skills, andexpertise you need to developfurtherDiscuss what you believe to be thestrengths you already haveBe aware when the relationshiphas run its courseSay “thank you”Celebrate accomplishmentsGive back to the profession bymentoring othersSet the PrinciplesAccept criticismContinually reassess performanceBe respectfulAct on your own initiative<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 3
DEPARTMENTSARTICLES1 EditorialMentoring and coaching inmedicineRichard L. Byyny, MD, editor“My life, my soul, my body I owe to youand God”Harvey Cushing and the patient-physicianrelationship seen through correspondence2011 Robert J. Glaser42 Distinguished TeacherCourtney PendletonAwardsReviews and reflections44Choosing a medical specialtyExploring Happiness: FromAristotle to Brain ScienceEpiphany, where are you?Reviewed by Stephen G. Post,PhDJenna L. Thomason, BSMatch Day: One Day and OneDramatic Year in the Lives ofThree New DoctorsReviewed by R. MacDonell-Yilmaz, MPHWe’re NOT Leaving: 9/11Daniel LiebowitzResponders Tell <strong>The</strong>ir Storiesof Courage, Sacrifice, andRenewalReviewed by Richard Bronson,MD50 LettersCarlos Finlay, Walter Reed, and the politicsof imperialism in early tropical medicinePhoto by Walter Willard Boyd, MD, Yale University, HarveyCushing/John Hay Whitney Medical Library.
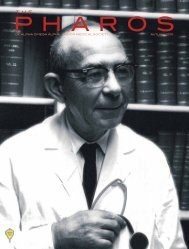
On the coverDr. Harvey Cushing closing2000th verified brain tumor, April15, 1931.Photo by Walter Willard Boyd, MD. YaleUniversity, Harvey Cushing/John Hay WhitneyMedical Library.See page 6<strong>The</strong> AMA and health care reformAllison Hinko, MDCompetencies as the basis for reformedpremedical education<strong>The</strong> case for an unrestricted liberal artscollegiate educationNathan Kase, MD, and David Muller, MD424823POETRYBreaking Bad NewsSarah Leeper31 A ReminderAllison Jiang4152INSIDEBACK39 COVERAΩA NEWS2011 Robert J. GlaserDistinguished TeacherAwardsN a t i o n a l and Chapter news2011 meeting of the AΩA boardof directorsInstructions for authorsLeaders in American MedicineMechanical ManHenry Langhorne, MDGraduatin, We PackSarah Buckley, MDAdagio Ma Non TroppoRichard Bronson, MD
MCourtney Pendleton
<strong>The</strong> author is a member of the Class of <strong>2012</strong> at the JohnsHopkins University School of Medicine. This essay wonfirst prize in the 2011 Helen H. Glaser Student EssayCompetition.<strong>The</strong> need for written documentation in the medicalprofession has grown over the past century, in responseto the increasing complexity of medico-legalregulations. Yet, for all the written notes charting phone calls,lab reports, clinic visits, and follow-up, the contemporaryclinician meets the classic definition of a cynic, “A man whoknows the price of everything, and the value of nothing.” 1p116In the era of e-mail, social networking, and electronic patientrecords, written correspondence has arguably become less anecessity and more a quaint pastime, and the immense valueof the letter as a tool for patient-physician communication hasbeen forgotten.Through IRB approval and courtesy of the medical recordsoffice and the Alan Mason Chesney Archives of the JohnsHopkins Medical Institutions, the surgical files from the JohnsHopkins Hospital from 1896 to 1912 were accessed. <strong>The</strong> casesattended by Harvey Cushing, an inveterate letter writer, 2 wereLeft, Harvey Cushing at the bedside of a child. Photo by T. W. Dixon.Yale University, Harvey Cushing/John Hay Whitney Medical Library.Above, Harvey Cushing in a straw hat, 1903.Yale University, Harvey Cushing/John Hay Whitney Medical Library.reviewed and analyzed. Unless otherwise noted, all quotationsare taken from the unpublished surgical records. 3<strong>The</strong>se files contain the tremendous volume of written correspondencebetween Cushing and his patients and colleaguesacross the globe. <strong>The</strong> many facets of the patient-physicianrelationship are illuminated through the lens of the writtencorrespondence between Cushing and his patients.Post-operative follow-upAt the turn of the twentieth century, Cushing had establisheda nationwide referral base, operating on patients fromas far west as California and as far north as Canada. 3,4 Withtravel still a time-consuming endeavor of long locomotivejourneys, it was often impossible for patients to return to theHopkins clinic for post-operative observation and care. Manypatients were lost to follow-up, presumably obtaining furthercare closer to home from specialists or primary care physicians.Cushing regularly wrote to these former patients, askingfor information regarding their health and post-operativecourse. Most of them offered straightforward descriptions oftheir health conditions, as in the letter written by a thirty-sixyear-oldsailor whom Cushing treated for epilepsy:I am very glad to let you now of my condition as it is overninety days since I had a convulsion and I am very hopefulof getting well again. My physical condition is fairly goodbut I still retain those periods of quiet not caring to conversewith anyone.<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 7
“My life, my soul, my body I owe to you and God”A handwritten letter from the first patient Cushingoperated on through the omega incision for a sellarlesion. He wrote: “I hope there is something that youcan send that will lessen the pain. <strong>The</strong> least amountof urine in twenty four hrs was a bout three pts—& themost—about four pts—it varies as some days I drinkmore water than others. Thanking you for past favors Iremain as ever”Courtesy of the Medical Records Office and the Alan Mason Chesney MedicalArchives of Johns Hopkins Institutions.Cushing’s intraoperative illustration of a surgical interventionfor epilepsy in a seventeen-year-old femalepatient. Stimulation of the cortex was done to mapthe motor area, and Cushing labeled the areas “hand,”“face,” [illegible], “tongue” from top to bottom. <strong>The</strong>patient’s mother later wrote that there had been noimprovement in her daughter’s condition.Courtesy of the Medical Records Office and the Alan Mason Chesney MedicalArchives of Johns Hopkins Institutions.Not all follow-up reports were positive, however. <strong>The</strong>mother of a seventeen-year-old girl who had also undergoneoperative intervention for epilepsy wrote to Cushing almostthree years post-operatively:In regards to your letter about my daughter I don’t seethat she is any better now she has that bad feeling in hurhead like she had when she went there and the attacks arthe same her helth is very good only once a month she hashur bad attacks drawing in hur lages and arms and pain inhur back and head. She had a bad spell after she came homefrom the hospital she was taken the 1 of june with a sleepyfeeling in hur hands and feat and lost the use of hur self andstade so till the next springAlthough the operation was not successful in treating thepatient’s epilepsy, the mother’s letter contains no trace of bitterness,and she closed with a request to Cushing to “let usheair from you a gain.”Patients often faced a difficult conundrum: they werenot well enough to travel to Baltimore, but were unable toobtain specialized medical care or pharmaceuticals close tohome. Many patients wrote to Cushing asking that he sendmedications and supplies, including large batteries for theelectrical stimulation he prescribed for patients who hadundergone peripheral nerve operations. One such patientwas the first patient Cushing operated upon for a presumedsellar lesion using the so-called omega incision. This patientdiligently catalogued his symptoms in letters to Cushing, presumablyin response to instructions from the neurosurgeon:I can’t see that there is an increase in the amount ofurine within the last year but will try t measure it . . . mykidneys act from two to four + sometimes five times duringthe night.Clearly the patient tried to follow Cushing’s instructions to theletter, going so far as to redact his words to show that he wouldnot merely attempt to perform a task, he would complete it.Probably unbeknownst to him, he was using these epistlesto describe the presence or absence of symptoms of diabetesinspidus, a syndrome Cushing knew occurred after sellar operations.4 Later, the patient wrote to Cushing:I do not feel able to go to Baltimore. Why can you notdoctor me here by sending the treatment here so I can remainat home.8 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
Cushing must have responded in the affirmative, because thenext letter, dated nearly four months later, says:Dear Dr.I have finished taking the tablets but am feeling a boutthe same as I did before taking them.Death notificationContemporary physicians customarily use Internet searchesand national databases such as the Social Security Death Indexto find information about patient deaths. In Cushing’s era, informationtraveled more slowly, with no central repository toaccess for this information. <strong>The</strong> majority of Cushing’s patientstreated at the Johns Hopkins Hospital lived and died withouthaving a Social Security number (the program was institutedin 1935), making their fates difficult to ascertain even with allthe resources of modern technology.Families often sent letters to simultaneously informCushing of the death of a former patient and to express gratitudefor his operative services and continued interest.<strong>The</strong> mother of a five-year-old child who was operated onfor a brain tumor wrote a little less than three weeks followingthe end of their hospital stay:Dr. Cushing,Dear Friend,Just a few lines to let you know that my dear little girldied last week July 20. She died without a struggle just asthough she were asleep.I only wish she would have been where you could havetapped that place as it was very full . . .Thanking you for all your many kindnesses shown us.Cushing was clearly viewed as a healer in the truest sense bythis family. That the mother offered her thanks to the surgeonwho failed to save her daughter’s life is a testament toCushing’s skill at the bedside as well as within the operatingtheater.Patients’ families used these notifications of death to searchfor answers as much as to give information. <strong>The</strong> family of atwenty-four-year-old woman on whom Cushing performedsurgery for a brain tumor wrote to him upon her death:Writing to you today is with a different feeling than theone over a month ago, I would not dare think our darlingwould not recover, however without pain and in so terriblecondition we try to be reconciled though now as I study andwonder it would be so comforting to know, where did youlocate the pressure . . . and what was the immediate causeof her going?GratitudePatients most frequently wrote to Cushing to express theirgratitude for his interventions, almost regardless of his success.Some of the most effusive letters were written by patientswho underwent surgical treatment for trigeminal neuralgia, aparoxysmal pain syndrome dubbed the “suicide disease” becauseof the intractable pain it causes those suffering from it.This point is certainly emphasized by the chief complaint of“misery in the head” documented for a patient diagnosed withthe disease. One fifty-seven-year-old patient, treated in 1908,wrote that he experienced:never a twinge from the nerve! A world of thanks and praiseto you, my dear sir. May your hand never lose its wonderfulcunning!A young man whose epilepsy made him incapable of workingwas able to return to light work in the family business afterCushing operated. <strong>The</strong> patient wrote:I am surely thankful I became aquainted with Dr HarveyCushing for I feel sure my Lord hath blessed me in this wayand through you has enabled me to reash my highest aspirationsand also fulfilled an anxious mothers hope<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 9
“My life, my soul, my body I owe to you and God”Cushing’s original intraoperative drawing ofcortical softening in a thirty-eight-year-oldman treated for thrombosis of the middlecerebral artery.Courtesy of the Medical Records Office and the Alan MasonChesney Medical Archives of Johns Hopkins Institutions.<strong>The</strong> closing of the final letter to Cushing fromthe above patient. He wrote to Cushing onmany occasions, expressing his gratitude.Courtesy of the Medical Records Office and the Alan MasonChesney Medical Archives of Johns Hopkins Institutions.Despite Cushing’s best efforts, the patient had continued tohave seizures during his post-operative stay in the hospital,but his letter reflects no frustration or disappointment.This profuse gratitude in the face of less than ideal resultsis not unique—multiple letters echo these sentiments. At theturn of the twentieth century, neurosurgery was still consideredby many to be a fool’s errand at worst, and a desperatelast resort at best. <strong>The</strong>se patients may have recognized thatCushing had shepherded them through the no-man’s-land ofan intracranial operation and brought them out unscathed,possibly even improved. One thirty-eight-year-old patientwith symptoms consistent with a left-sided lesion underwentsurgery. Cushing expected a brain tumor, but a second operationrevealed a thrombosed middle cerebral artery andsoftening of the surrounding brain parenchyma. <strong>The</strong> patientwas discharged in “improved” condition, but his right-sidedweakness and aphasia remained. He wrote nearly three yearslater, stating:First of all, My life, my soul, my body I owe to you andGod. I am gaining nicely and it is the first time for prettynear three years that I thought I would write to you to-day.He wrote again in December 1911:Again I want to thank you with all my heart that you havesaved me, of course nature is trying to heal in the brains butnever-the-less it was you who saved me. <strong>The</strong>re is no doubtabout it.Five years later, the patient’s last letter to Cushing reads:So in a way, I am happy because for the last three years itis a beautiful world. . . . even now I cannot express myselfthe way I want to but I go where I please now. I was in LosAngeles and San Diego last spring myself and that is proofthat I go where I please by myself and for a good many yearsI could not do it. It was certainly a wonderful operation inBaltimore.Overall, the letters of thanks from Cushing’s patients appearto value increased independence over complete cure oftheir ailments.10 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
Other requests<strong>The</strong> written correspondence filed in the surgical records isby no means confined to clinical outcomes and medical questions;many of the letters reflect the complexities and conundrumsof the patient-physician relationship that Cushing musthave struggled with throughout his career.appears that Cushing himself attempted to avoid respondingin either way.Dr. Cushing,Why don’t you write. You did not answer my last letter.. . . I would like to see you and tell you all and I want you tosee K . . . ever time she gets sick she says she wants to seeDr. Cushing.<strong>The</strong>re is no record that K and her mother ever returnedto Hopkins, or that Cushing proffered a response.<strong>The</strong> last letter from the family was datedMarch 1906:I know you will be surprised to hear from me.Guess you remember me and little K who you operatedon for spasms, I am glad to say she is so muchbetter and doing fine you certainly did help her sometimes she goes for months and don’t have one. And Ithink she will get entirely over them. I wish you couldsee her she looks fine. And thinking of getting marriedthis summer what do you think about it let me haveyour opinion. I told her I was going to ask you aboutit first. She sends her love to you and said tell you shewould love to see you.A handwritten from the mother of a girl Cushing had operated onfor idiopathic epilepsy when the patient was sixteen years old.<strong>The</strong> mother wrote multiple letters attempting to set up a meetingbetween her daughter and Cushing, with unknown intentions.Courtesy of the Medical Records Office and the Alan Mason Chesney Medical Archives ofJohns Hopkins Institutions.In the spring of 1903, Cushing operated on a sixteen-yearoldgirl for the treatment of “idiopathic epilepsy.” She had anuneventful recovery, and was sent home in improved condition.Her mother began a correspondence with Cushing thatspanned the next three years; the letters begin innocuouslyenough, with the mother writing:Enclosed is record of K’s attacks during month of September,her condition generally is about the same . . . Please let me hearfrom you soon, what do you think of her now?<strong>The</strong> postscript to that letter begins to develop shades ofstrangeness:PS.I would like for you to see K I can bring her to see you ifyou want to see her. Let me know. I want you to see her andthen I can explain all to you. She looks so well.Within the hundreds of letters contained in the surgical records,most contain patients’ regrets at being unable to travelto Baltimore to see Cushing; this mother’s letters are the onlywritten correspondence that so steadily pursues an appointmentwith Cushing. From the next letter, dated early 1904, itOne of the delights of the written letter is the potentialof inferring what the author might have implied. Inthis case, it may be that the mother merely sought Cushing’s inpersonevaluation of her daughter, but the persistence of theseefforts, coupled with the request that Cushing weigh in on herdaughter’s impending marriage, offer a titillating alternate possibility—shemay have attempted to play matchmaker for herdaughter and the young, albeit newly married, neurosurgeon.While such a scenario may seem unlikely, Cushing had afair share of ardent admirers among his female patients. InApril 1911 Cushing operated upon a twenty-three-year-oldwoman for a “cerebellar pontine tumor.” <strong>The</strong> operation metwith success and she was discharged in “improved” condition.In November 1911, two months after leaving the hospital, thepatient wrote a very flattering letter to Cushing:Dear Dr. Cushing,I suppose you wonder who in the world this is, so I’ll tellyou it is none other than M who so often thinks and talks ofyou, her favorite Dr. . . .. . . If you were near enough I’d give you some of the nicethings I get to eat.Dr. Cushing, would it be asking too much to ask you tosend me your picture? I’m sure if you knew how much I wantit you would grant my request.I declare, Dr., I want it worse than any thing I know of.Please write, in your own hand, your name and date underthe picture. . . .If you practice your profession forty thousand years youwill never have a patient who loves you likeM<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 11
“My life, my soul, my body I owe to you and God”Dr. Harvey Cushing, the 2000th verified brain tumor operation, April 15, 1931.Photo by Walter Willard Boyd, MD. Yale University, Harvey Cushing/John Hay Whitney Medical Library.Though Cushing regularly corresponded with his patients,and may have written to M and her family, he appears to haveavoided responding to this particular request, much as he didwith K’s mother. M was not to be dissuaded, however, and inMarch 1912 she wrote Cushing again:Dear Dr. Cushing,I’m writing this note to find out if the extremely coldwinter has frozen your memory— Do you know that you saidyou would sometime send me a picture of yourself— ? Haveyou not yet been the victim of a photographer?”Cushing continued this correspondence, although his lettersare not preserved in the surgical files. <strong>The</strong> last handwrittennote is dated March 1915, and describes M’s continued interestin seeing Cushing again:we are hoping that business or pleasure may sometime bringyou to this part of the U.S. and that we may have the verygreat pleasure of entertaining you here. Don’t you think thatmight be a possibility.This letter includes a glimpse at the general fondness she hadfor all her attendings at the hospital:Was I to infer from your last letter that Dr.Goetsch is now a Bostonian . . . I certainly wouldlike to see him if he wouldn’t shave my head again.<strong>The</strong> chart contains a final letter, dated July1921, which was excerpted and typed into thesurgical record. <strong>The</strong> excerpts contain entirelyclinically relevant descriptions of the patient’scondition at that time, without a hint of the morepersonal communication she had held in earlierletters.<strong>The</strong> handwritten letter from a former patient, who wasoperated on for a suspected brain tumor in 1911.Courtesy of the Medical Records Office and the Alan Mason Chesney MedicalArchives of Johns Hopkins Institutions.12 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
ReferralsAs an up-and-coming young neurosurgeon, Cushingcertainly strove to develop his practice beyond the confinesof Baltimore. By the early 1900s, he had expanded his practiceto include patients traveling great distances to visit theJohns Hopkins Hospital. Many of his former patients wrotedescribing cases of friends and loved ones that they hopedwould fall within the purview of Cushing’s practice.In addition to advocating for personal care for her daughter,K’s mother sought a consult from Cushing for a family friend:Now Dr. Cushing, I have a friend here, and he has a brotherthat is insane caused from kick in the head over 9 years go.<strong>The</strong> poor man has large family and not much money for hehas been sick so long. What would you operate on him for?How cheap could you do it. Please let me know by returnmail. He is not wild very quiet and his brother will bring himto you. Please let me know at once.No patient chart matching this description can be found in thesurgical records. It is uncertain if Cushing declined to see thepatient, or if the patient came to the Johns Hopkins Hospitalunder the care of another attending.Another rich source of referrals was Cushing’s growinggroup of satisfied former patients. While the surgical recordsdo not indicate whether patients were referred by friends oracquaintances who had been treated by Cushing, many lettersindicate that patients translated gratitude into referrals. Inparticular, Cushing’s success at treating trigeminal neuralgiaearned him much admiration among his patients. One sixtythree-year-oldman who underwent avulsion of the sensoryroot of the trigeminal nerve wrote expressing his gratitude:Now my dear doctor, how to express my gratitude to youfor what you have done for me, I am at a loss to know. I shallever regard you as my greatest benefactor in this world, andpray the good Lord to shower upon you His heavenly blessings,and make you instrumental in giving relief to manymore such afflicted mortals as I was.He was not content to leave matters entirely in the hands of“the good Lord,” and later wrote:Several parties afflicted as I was have either written to me orcalled on me personally and I have recommended you as aspecialist, who can certainly give them relief.Conclusions<strong>The</strong> surgical records reveal the truly diverse patient populationtreated by Cushing during his time at the Johns HopkinsAbout Courtney PendletonI studied studio art and Englishliterature at New York University,graduating in 2004, and am currentlya fourth-year student at the JohnsHopkins School of Medicine. I planto pursue a career in neurosurgery, and I thank Dr.Alfredo Quiñones-Hinojosa for supporting this work.Hospital, from African-Americans born in the South before theCivil War to urban socialites with charts full of documentationfrom European specialists. <strong>The</strong> letters written by these patientsare equally varied, including well-written genteel epistles andharried notes full of misspellings. Unlike the documentationthat fills contemporary medical records, which often provideonly abstracted clinical data, these letters offer insights intothe lives of the patients who painstakingly wrote them, as wellas the surgeon bound to receive them. <strong>The</strong> handwriting oftenchronicles the decline of patients suffering from incurablebrain tumors; the laboriously written, misspelled letters showus the perseverance of patients with limited education whodesired nothing more than to communicate their gratitude;and the detailed descriptions of symptoms and signs over timedemonstrate patients’ efforts to provide a trusted physicianwith adequate information to treat them from afar. Througheach letter we see Cushing not as the curmudgeonly taskmasteroften portrayed in biographies, 2,5 but as a young neurosurgeonwith enough humanity to inspire this volume of earnest letterwriting.References1. Wilde O. Lady Windermere’s Fan. London: A.R. Keller; 1907.2. Bliss M. Harvey Cushing: a Life in Surgery. New York: OxfordUniversity Press; 2005.3. <strong>The</strong> Johns Hopkins Hospital Surgical Records 1896 to 1912.Courtesy of the Alan Mason Chesney Archives of the Johns HopkinsMedical Institutions.4. Cushing H. <strong>The</strong> Pituitary Body and Its Disorders: ClinicalStates Produced by Disorders of the Hypophysis Cerebri. Philadelphia:J.B. Lippincott; 1979.5. Fulton JF. Harvey Cushing: a Biography. Springfield (IL):Charles C. Thomas; 1946.<strong>The</strong> author’s e-mail address is: courtney.pendleton@gmail.com.<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 13
14 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
Choosing a medical specialtyEpiphany, where are you?Jenna L. Thomason, BS<strong>The</strong> author is an MD/MPH candidatein the Class of <strong>2012</strong> at EmoryUniversity School of Medicine andthe Rollins School of Public Health atEmory University.epiph·a·ny noun \i-΄pi-fә-nē\: (1) :a usually sudden manifestation orperception of the essential nature ormeaning of something (2) : an intuitivegrasp of reality through something(as an event) usually simpleand striking (3) : an illuminatingdiscovery, realization, or disclosure.—Merriam-Webster OnlineOh Epiphany, where are you?I attended a year and a halfof lectures and absorbed asmuch information as possible aboutevery molecular, biochemical, andcellular mechanism imperative tomaintaining the body’s homeostasis.I spent countless hours in the basementof the medical school learninganatomy from my cadaver (whom wefondly named “Arnold”). I have studiedevery organ system—integumentary,musculoskeletal, respiratory, lymphatic,cardiovascular, endocrine, genitourinary,gastrointestinal, nervous, reproductive—aswell as the hundreds ofdisease processes that cause these systemsto go awry.I wielded a blade like a surgeon.I walked the halls of Grady like aninternist. I delivered a baby like anobstetrician. I held the hand of a dyingpatient as a palliative care provider. Idistinguished macules from papulesand patches from plaques on my dermatologyrotation. I treated everyonefrom tiny babies to pregnant ladiesto the elderly as the understudy of afamily physician. I tested each reflexand every nerve during my neurologyclerkship. At the side of a radiologist, Ilearned anatomy that Arnold couldn’tteach me. I cared for many minds onpsychiatry and many tiny bodies onpediatrics. I have witnessed the fullrange of disease etiologies, includinggenetic, developmental, toxic, infectious,traumatic, metabolic, chemical,neoplastic, and degenerative. I havestudied the vast spectrum of treatmentoptions, including behavioral, pharmacologic,and surgical, and I understandthe rationale and application of eachto the above disease etiologies. All thishas led me to the most difficult professionalcrossroads of my life: Where do Igo from here?<strong>The</strong> decision to pursue medicalschool was the easiest decision thatI have ever made. I’ve never knowna stronger desire than the one that Ifelt (and still feel) to become a doctor.I wanted to make the commitmentto caring for people and possess theknowledge to do so. I hardly knew whatI was getting myself into, but I couldn’twait to get started.So how did the simplest decisionturn into the hardest one? And whendid life become a multiple choice test?All of sudden I have to chose between:(a) kids; (b) adult males and females;(c) females only; or (d) both (a) and(c). I have to decide whether I want tointeract with patients or examine theirpictures or inspect their pieces (in theform of pathological specimens). DoI want to know a little about a lot or alot about a little bit? I have to factor inlifestyle, inpatient versus outpatient,academics versus private practice,seeing mostly healthy patients versusseeing mostly sick patients, skin versusbones versus eyes . . . and it’s morecomplicated than those aforementionedmolecular, biochemical, and cellularmechanisms ever were.So, dear Epiphany, why are you solate? You were supposed to make thisan easy decision. Is this punishmentfor all of those days during first year ofmedical school when I snuck into 8 AMlecture when the minute hand was a fewdegrees past 12? I thought for sure thatyou would be here by now. I was countingon you. I’m starting to think you’renot coming. Maybe you never were.Contrary to my idealistic expectations,many medical students—if notmost—end up marking you down as a“no show” in our appointment books.<strong>The</strong> truth is, there may not be onesingle specialty that’s right for any ofus. If we are having trouble decidingbetween two or three, any one is likelyto fit roughly equally as well as the others.After spending many months agonizingover this decision, I have finallyfound that Jenna the pediatrician is notso different from Jenna the dermatologistor Jenna the geriatrician—becauseI will not be defined by the type of patientI see, but how I see them.Stress over what divides us is temporary,but preserving what unitesus—commitment to lifelong learning,medical ethics, and our patients—isunceasing, and is what earns all of usthe extra letters that follow our lastnames.Epiphany, we meet at last.<strong>The</strong> author’s address is:2210 Westchester Ridge NEAtlanta, Georgia 30329E-mail: jennalthomason@gmail.com<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 15
Breaking Bad NewsWe practice all afternoon, telling each other,“I have some bad news. Your mother has died.” Sometimesit’s a sister, a son. We say, “We did everything,everything we could” and “I’m so sorry” and“Do you want to see her now?”Our teacher is an emergency physician. She does this all the time.We ask, “What if the family gets angry?” She says, “That’s whyyou always stand near the door.”We ask, “What if we start to cry?” She says, “If you can help it,don’t cry. But it probably won’t make things worse.”We ask, “Do you always say the word dead?” She says,“I try to say it twice. Usually, even then, they’ll ask—‘So you mean he’s dead?’ ‘Yes,’ I say, ‘He’s dead.’ “We ask, “What if they want to know if he was in pain?” She says, “Say no.”She pauses. “Although,” she says, “I believethe feat of dying is not un-painful. <strong>The</strong> brain mustpanic, even if the body doesn’t. But,” she continues, “Say no.Always just say no.”Sarah LeeperMs. Leeper is a member of the Class of <strong>2012</strong> at the Warren Alpert Medical School of BrownUniversity. This poem won first prize in the 2011 <strong>Pharos</strong> Poetry Competition.Ms. Leeper’s e-mail address: sarah_leeper@brown.edu.Illustration by Jim M’Guinness.
A ReminderAn intellectual is someone whose mind watches itself.I entered into this profession, this art—It is easy to slip into a selfish thirst to prove myself,Amidst all the memorization of complex body parts.I entered into this profession, this art.But I sometimes forget the patients whom I am working for,amidst all the memorization of complex body parts.(Biochemical pathways, reactions, and science galore.)I sometimes forget the patients whom I am working for,We were all so idealistic—bright-eyed and bushy-tailed at the inception.In spite of biochemical pathways, reactions, and science galore,It is crucial to keep clear and undimmed our perception.We were all so idealistic—bright-eyed and bushy-tailed at the inception;More difficult is now to stay the course and remain consistent.It is crucial to keep clear and undimmed our perception:Integrity, honesty, communication—to these we must be persistent.More difficult is now to stay the course and remaining consistent—It is easy to slip into a selfish thirst to prove myself.Integrity, honesty, communication—to these we must be persistent.Recall—an intellectual is someone whose mind watches itself.Angela JiangMs. Jiang is a member of the Class of 2014 at the Ohio State University Collegeof Medicine. This poem won third prize in the 2011 <strong>Pharos</strong> Poetry Competition. Ms.Jiang’s address is: 1062 Pennsylvania Avenue, Columbus, Ohio 43201. E-mail: angela.jiang@osumc.edu.Illustration by Erica Aitken<strong>The</strong> <strong>Pharos</strong>/Autumn 2011 31
Illustration by Erica Aitken.
<strong>The</strong> case for an unrestricted liberal arts collegiate educationNathan Kase, MD, and David Muller, MDDr. Kase (AΩA, Yale University, 1968) is Dean Emeritus,professor of Obstetrics/Gynecology and ReproductiveScience, and professor of Medicine in the Division ofEndocrinology, Diabetes, and Bone Disease at theMount Sinai School of Medicine. Dr. Muller (AΩA, MountSinai School of Medicine, 1965) is the Dean for MedicalEducation at Mount Sinai.ne hundred years ago Abraham Flexner changed theparadigm by which physicians are trained in thiscountry. 1,2 Among his many contributions was theprinciple that successful performance in universal, standardized,and demanding premedical basic science courses berequired of undergraduates applying for admission to U.S.medical schools. By 1930 these requirements were fully entrenched,requiring two semesters each of chemistry, biology,and physics, and one semester of organic chemistry. Eightyyears later, despite continued and mounting opposition, thesepremed requirements continue to be enforced.Calls for change of this status quo have persisted and, inrecent years, intensified. 3–8 While the displeasure is uniform,the ways in which baccalaureate preparation for medicalschool and medical school admissions policies might beamended reflect differing and sometimes even opposing perspectives.Most representative of this polarity are two majoradvocacy statements: on the one hand the 2009 report of theAAMC-HHMI Committee, “Scientific Foundations for FuturePhysicians,” 9 and on the other the now decades old but stillpertinent “Physicians for the Twenty-First Century” report ofthe AAMC Project Panel on General Professional Educationof the Physician and College Preparation for Medicine (GPEP)which appeared in the early 1980s. 10 Both the AAMC-HHMIand GPEP expert panels were commissioned to examine,among other elements of medical education, the aims andcontent of the premedical curriculum. <strong>The</strong>ir vastly differentconclusions are emblematic of the major themes that characterizediverging objectives of premedical education reforms.<strong>The</strong> case for SCIENCE competencies:<strong>The</strong> HHMI-AAMC Report<strong>The</strong> AAMC and HHMI convened a diverse group of scientists,physicians, and science educators drawn from smallcolleges, large universities, and medical schools to address thefollowing paradox: while the scientific knowledge essentialfor acquiring and successfully applying the skills necessary forthe expert practice of clinical medicine has changed “dramatically,”the medical prerequisites and admission requirementshave remained “essentially unchanged.” <strong>The</strong> group was askedto address the inherent tension between “teaching scientificfacts” and “preparing physicians to actually use scientificknowledge.” It set out to identify “the most important scientificcompetencies in the natural sciences required of studentsgraduating from college prior to matriculating into medicalschool.” 9ExecSumIn keeping with the National Academies’ BIO 2010 conclusionsthat premedical course requirements and the MCATcontent constrain undergraduate science education, 11 theHHMI/AAMC group defined eleven knowledge principlesand eight scientific competencies that reflect acquisition andeffective application of those principles. Proficiency in eachdetermines readiness for medical school admission.In the view of the committee, the shift from testing facts toachieving competencies will allow greater flexibility for collegiatefaculty and curriculum planners to exploit the talentsand resources of their institutions when revising course content.Ultimately, such changes will help to engage and personalizethe curricula of their science/premedicine students andtheir science faculties.<strong>The</strong> report acknowledged that these recommendationswere a “first step” in a continuing “conversation” about theappropriate skills, knowledge, values, and attitudes futurephysicians should possess. In this regard the AAMC has alsoconvened a separate panel to examine the behavioral andsocial science (our emphasis) competencies for future physicians,which will be released at a later date.<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 33
Competencies as the basis for reformed premedical education1. Apply quantitative reasoning and appropriate mathematics todescribe and explain phenomena in the natural world.• Interpret data sets andcommunicate thoseinterpretations using visual andother tools• Demonstrate quantitativenumeracy and facility with thelanguage of mathematics• Make statistical inferences fromdata setsTable 1HHMI: Scientific Foundations for Future PhysiciansEight Expectations of Entering Medical Students• Apply algorithmic approachesand principles of logic (includingthe distinction between cause/effect and association) toproblem solving• Extract relevant informationfrom large data sets2. Demonstrate understanding of the process of scientific inquiry, andexplain how scientific knowledge is discovered and validated.• Develop observational andinterpretive skills throughhands-on laboratory or fieldexperiences• Demonstrate the ability tomeasure with precision,accuracy, and safety• Operate basic laboratoryinstrumentation for scientificmeasurement• Articulate (in guided inquiryor in project-based research)scientific questions andhypotheses, design experiments,acquire data, perform dataanalysis, and present results• Demonstrate the ability tosearch effectively, to evaluatecritically, and to communicateand analyze the scientificliterature3. Demonstrate knowledge of basic physical principles and theirapplication to the understanding of living systems.• Mechanics as applied to humanand diagnostic systems• Electricity and magnetism (e.g.,charge, current flow, resistance,capacitance, electrical potential,and magnetic fields)• Wave generation andpropagation to the productionand transmission of radiation• <strong>The</strong>rmodynamics and fluidmotion• Quantum mechanics, such asatomic and molecular energylevels, spin, and ionizingradiation• Systems behavior, includinginput-output relationships andpositive and negative feedback4. Demonstrate knowledge of basic principles of chemistry and someof their applications to the understanding of living systems.• Atomic structure• Molecular structure• Molecular interaction• <strong>The</strong>rmodynamic criteriafor spontaneity of physicalprocesses and chemicalactions and the relationship ofthermodynamics to chemicalequilibriumSource: Reference 9.• Principles of chemical reactivityto explain chemical kineticsand derive possible reactionmechanicms• Chemistry of carbon containingcompounds relevant to theirbehavior in an aqueousenvironment5. Demonstrate knowledge of how biomolecules contribute to thestructure and function of cells.• Structure, biosynthesis, anddegradation of biologicalmacromolecules• Principles of chemicalthermodynamics and kineticsthat drive biological processesin the context of space (i.e.,compartmentation) and time:enzyme-catalyzed reactions andmetabolic pathways, regulation,integration, and the chemicallogic of sequential reaction steps• Biochemical processes thatcarry out transfer of biologicalinformation from DNA, andhow these processes areregulated• Principles of genetics andepigenetics to explain heritabletraits in a variety of organisms6. Apply understanding of the principles of how molecular and cellassemblies, organs, and organisms develop structure and carry outfunction.• General components ofprokaryotic and eukaryotic cells,such as molecular, microscopic,macroscopic, and threedimensionalstructure, to explainhow different componentscontribute to cellular andorganismal function• How cell-cell junctions and theextracellular matrix interact toform tissues with specializedfunctions• Mechanisms governing celldivision and development ofthe embryos• Principles of biomechanicsand explain structural andfunctional properties of tissuesand organisms7. How organisms sense and control their internal environment andhow they respond to external change. Explain:• Maintenance of homeostasisin living organisms by usingprinciples of mass transport, heattransfer, energy balance, andfeedback and control systems• Physical and chemicalmechanisms used fortransduction and informationprocessing in the sensing andintegration of internal andenvironmental signals• How living organisms useinternal and external defenseand avoidance mechanismsto protect themselves fromthreats, spanning the spectrumfrom behavioral to structuraland immunologic responses8. Demonstrate an understanding of how the organizing principle ofevolution by natural selection explains the diversity of life on earth.How:• Genomic variability and mutationcontribute to the success ofpopulations• Evolutionary mechanismscontribute to change in genefrequencies in populations andto reproductive isolation34 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
<strong>The</strong> case for ATTITUDES AND VALUES competencies:<strong>The</strong> GPEP ReportAssembled three decades ago, the GPEP committee includedcollege presidents, medical school deans, chairmen,professors, practitioners, and nonmedical members. Its chargewas an ambitious, all-encompassing review of the entirelandscape of American medical education: collegiate, medicalschool, graduate medical education, and faculty development.In particular, the panel was commissioned to assess the adequacyof medical education and admissions policies and thenature of premedical undergraduate preparation to “meet thechallenges of medical care in the twenty-first century.” 10pxiii<strong>The</strong> report’s recommendations reflected the panel’s perceptionof a widening disconnect between (1) increasingmedical specialization fueled by the accelerating expansionof medical science, technology, and information services, and(2) the individual patient’s—indeed the general public’s—concernsabout quality and access to health care.With respect to premedical education, their major recommendationswere as follows:• Broaden the baccalaureate preparation in the social sciencesand the humanities.• Modify medical school admissions requirements toaccommodate broader and more diverse baccalaureatepreparation.• Require an undergraduate scholarly endeavor.• Final admissions decisions should incorporate an applicant’sability “to learn independently, acquire critical analyticalskills, [and] develop the values and attitudes essential formembers of a caring profession.” 10p9Table 2General Professional Education of the Physician and CollegePreparation for Medicine in the Twenty-First CenturyRecommendations: Baccalaureate Education1. Broadenpreparationof everystudent2. Modifyadmissions3. Requiringscholarlyendeavor4. MakingselectiondecisionsSource: Reference 10.“….to achieve an education that encompassesbroad study in the natural and social sciences andin the humanities.” First to publicly define and decryexistence of “a Premed Syndrome.”“Medical school admissions committees’ practiceof recommending additional courses beyondthose required for admission should cease. Someinstitutions may wish to experiment by notrecommending any specific course requirements.”“College faculties should make the pursuit ofscholarly endeavor and the development ofeffective writing skills” a requirement.“Medical school admissions committees shouldmake final decisions using criteria that appraisestudents’ abilities to learn independently, toacquire critical analytic skills, to develop attitudesessential for members of a caring profession and tocontribute to the society of which they are a part.”In the panel’s view, the tendency of college students toshape their education prematurely towards the narrow objectiveof admission to medical school generates an unbalancedcollege experience resulting in exclusion of a broad liberal artseducation. <strong>The</strong> panel predicted a further reinforcement ofthese adverse tendencies if medical school admissions policiescontinued to emphasize high MCAT scores and exceptionalscience grade point averages. <strong>The</strong> fundamental position underlyingthe panel’s conclusion was the conviction that allphysicians, regardless of specialty, should not only acquireand sustain clinical expertise, skills, and knowledge, but alsoretain, hone, and apply humanistic values and attitudes nurturedand expanded in college and inherent to a professiondedicated to caring and healing. 10pp18–19 In support of thisconclusion, the panel recommended that evidence of strongrhetorical skills be included in medical school admissionscriteria and given greater weight in their selection processes.<strong>The</strong>se skills were defined as cogent, effective writing demonstratingoriginality, thorough research, sound analysis, andpersuasive argument that was developed and sharpened in avariety of liberal arts disciplines.GPEP also suggested that “medical school admissions committees’practice of recommending additional courses beyondthose required for admission should cease” and that “someinstitutions may wish to experiment by not recommendingany specific course requirements.” 10p20In conclusion, both HHMI and GPEP, albeit with verydifferent approaches and reasoning, seek to distinguish andnurture the self-initiating, self-directed, independent studentfrom the equally intelligent, well prepared, but passive recipientof current knowledge.<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 35
Competencies as the basis for reformed premedical educationEfforts to meld these principles are ongoing. For example,the Accreditation Council for Graduate Medical Education(ACGME) introduced the “General Competencies” for graduatemedical education in 1999. 12 This broad set of general skillsand attitudes (including competence in patient care, medicalknowledge, and interpersonal and communication skills,among others) was meant to serve as a framework for residenttraining and development. To sustain ACGME accreditation,each training program, regardless of specialty, is now responsiblefor documenting its trainees’ performance and progresswithin each competency element.In 1998 the AAMC, with broad input from national leadersin medical education, published the “Learning Objectivesfor Medical Student Education” as part of its Medical SchoolObjectives Project (MSOP). 13 This aimed to define the essentialattributes physicians need to fulfill their “duty to society”(including requiring physicians to be altruistic, knowledgeable,skillful, and dutiful). 13Two elements of the proposals by GPEP, ACGME, and theAAMC (MSOP) are strikingly similar: the inextricable connectionbetween competency in communication skills and effectivepatient care, and the fact that altruism and accountability(performing in a “dutiful” manner) are essential elementsinherent to the behavioral attributes we call “professionalism.”How will medical schools respond?While both the HHMI and GPEP positions are appealing,it seems that meaningful reform can only be achieved by acombination of (1) individual colleges developing competencybased curricula, (2) the AAMC altering the MCAT to assessthe acquisition of competencies, and (3) medical schools modifyingthe philosophies governing their admissions criteria.That degree of change is daunting on many levels, not the leastof which is medical schools’ apparent collective reluctance tofix something they believe isn’t broken.What is missing is formal, persuasive evidence defininghow well students perform if admitted to medical school withradically different post-Flexnerian baccalaureate backgrounds,foregoing the MCAT and allowing them to undertake a diverseand flexible array of undergraduate coursework.<strong>The</strong> Humanities and Medicine Program at MountSinai School of MedicineIn partial answer to this challenge, a recent detailed reportof the Mount Sinai School of Medicine Humanities inMedicine (HuMed) Program is worthy of consideration. 14 <strong>The</strong>HuMed Program, founded in the late 1980s, sought to embodythe essence of the GPEP principles. A portion of the medicalschool entering class applicants who were exclusively liberalarts majors were exempted from all the standard premed curriculumcourses and omitted the MCAT examination. In thisday of evidence-based decision making, it must be noted thatthis major decision was based on expert opinion alone.Applicants to the HuMed program are college sophomores(and rarely juniors). <strong>The</strong>refore admission decisions are basedon high school and initial college freshman and partial sophomoregrades and SAT scores. As important, however, aretwo personal essays, three letters of recommendation, and alisting of extracurricular (school and community) activities.Approximately fifteen percent of the applicant pool is invitedfor personal interviews at Mount Sinai.<strong>The</strong> assessment process therefore involves two majorelements.1. In addition to excellent GPA performance, high SATscores are admittedly crucial. Although the stipulated minimumscore for each element is 650, in recent years the poolof applicants chosen for interview generally exceed 750 onaverage and those chosen for final admission to the programscore over 750.2. In the personal essays, interviews, and extracurricularevidence of personal interests and involvement, we seek evidenceof rhetorical “skills defined by cogent, effective writingdisplaying originality, thorough research, sound analysis, andpersuasive argument developed and sharpened” in a varietyof activities. In the interviews we seek cogent, lucid, thoughtfulresponses—evidence of “competency in communication”to challenging questions. 10 Finally personal activities shoulddemonstrate depth of involvement and conclusive impact onsome aspect of human welfare.Accordingly, the HuMed selection process seeks to distinguishthe self-initiating, self-directed, and independent36 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
student from the equally intelligent, well prepared, but passiverecipient of current knowledge.Once accepted, students must maintain a college GPA of3.5. Although they forego the full traditional requirements andMCAT, they are required to take and achieve a minimum gradeof B in biology and general chemistry (two semesters each).After completing their junior year in college, studentsare required to spend an eight-week summer term at MountSinai. This experience includes clinical service rotations inall specialties, seminars in medical topics (e.g., bioethics,health policy, palliative care), and an abbreviated course inthe Principles of Organic Chemistry and Physics Related toMedicine (six credit hours for organic chemistry; two credithours for physics). Students complete weekly examinationsthat are graded pass/fail.During the summer prior to matriculation, HuMed studentsmay attend an optional Summer Enrichment Program(SEP) that serves to acclimate incoming HuMed students to themedical school curriculum and environment. Approximatelyseventy-five percent of the matriculating HuMed cohortparticipates each year. <strong>The</strong> SEP curriculum includes overviewsof biochemistry, anatomy, embryology, cell biology, andhistology. Examinations are the self-assessment type and arereviewed in class. Students do not receive grades.<strong>The</strong> first-year medical school curriculum is not altered toaccommodate the HuMed students.Aims of the HuMed programThis new program sought to encourage a group of applicantswith an interest in the humanistic elements of medicineto consider pursuing a career in the profession. At a minimum,the program would result in a more diverse and enriched poolof potential applicants. Mount Sinai believed that these policieswould eliminate the initial reluctance of these applicantsto pursue medicine, typically based on an uncertain interest inscience, concern over their ability to meet the high scholasticexpectations of medical school admissions committees, and/or their unwillingness to divert the time and effort required tomeet standard medical school requirements.<strong>The</strong> keen awareness premed students have of the competitivenature of the admissions process and the need foroutstanding performance in science GPA and MCAT scoresmight induce them to cram for grades without appreciationof the science being studied. As a result, their retention of theinformation might only be transitory. Educators have turned“what should be a comprehensive meritocracy into a narrowminded and mean spirited ‘testocracy.’ ” 15This narrow focus fosters other negative results:• Cultivation of true scientific curiosity is diminished asthe satisfactions of scientific discovery are lost.• <strong>The</strong> process of assessing student performance by “objective”validating memorized current knowledge ignores the factthat science is not static.• Science is not presented as the portal of entry throughwhich the wonders of biomedicine can be engaged. Rather itis distorted into a set of obstacles to be surmounted and functionssolely as a filter through which medical school admissioncommittees select applicants. 6,7But more important than simply enriching the applicantpool, HuMed was founded on the principle that a broad liberalarts education might supply the values, skills, and attitudesGPEP espoused. As such, a liberal arts education might enhancestudent appreciation and understanding of the range ofcharacteristics describing the human condition, the contextin which dysfunction, disability, and disease intrudes and distorts.It was felt that this benefit might be accrued from threeelements of a challenging liberal arts background: amplification,self-discovery, and the development of professionalism.• Amplification—Fiction at its best can depict in severalhours of reading and reflection more about the nature of thehuman condition (that brew of joy, sadness, fright, relief, bewilderment,confusion, and pain) than the untutored, intuitiveobservations derived through the single, often imperfect lensof a maturing adolescent. Reading the best fiction as part ofa colloquium led by an experienced preceptor/facilitator in asmall group of able, interactive classmates identifies and amplifieselements that may be ephemeral in life, often unseen orunremarked. Focused insight through reading, discussion, andinterpretation replaces and completes the surmised and theunexperienced. It gives meaning to a life-altering event andthe needs of the individual(s) involved.• Self-discovery—Not only does a liberal arts educationprepare the student for what to look for in others, it alsoinforms the sensitized and guided student of his or her owndiverse reactions and sensitivities. It induces and expandspersonal scrutiny of one’s own preferences, prejudices, miscalculations,and ignorance. Under the best circumstances it expandsthe individual’s sense of self: what talents and resourcesone possesses and which need development, strengthening,and correction, all in preparation for a career dedicated tohealing others.• Professionalism—A liberal arts collegiate education, sooften undertaken in a small-group faculty-facilitated format,reinforces awareness of the importance and benefits of productiveinteraction with others. <strong>The</strong>se benefits are twofold.<strong>The</strong> best students will endeavor to hone the skills that maximizeeffective written and oral communication: conciseness,cogency, lucidity, and fluency. <strong>The</strong>y discover and emulatethose virtues in their most effective classmates, and they developa personal style of interactive conduct of their own thatleads to more successful subsequent interactions. Moreoverthe benefit of interdependence induces positive socializingbehavior, personal control, ethical interactions, civility, andcourtesy.<strong>The</strong>se are the essential elements of all human interactions,be they with patients or peers. Over time, students successful<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 37
Competencies as the basis for reformed premedical educationin these encounters appreciate language and the methodologiesand the targets of precise communication. <strong>The</strong>y becomeas aware of the needs of others as they are of their own. Insum, the defining philosophy of HuMed posits that the resultof such an education will be a receptive, interactive, communicative,and sensitive prospective medical professional.Outcomes<strong>The</strong> HuMed Program has been in place for over twentyyears. A recent report in Academic Medicine reviewed outcomedata for six graduating classes. 14 <strong>The</strong> report comparesmedical school performance outcomes of undergraduatehumanities and social science majors who specifically omittedall standard premed requirements and the MCAT withclassmates who pursued the traditional premed science-basedpreparation. Using a Medical Student Performance Evaluation(MSPE) grid, the report compares academic data reflecting basicscience knowledge, clinical performance, leadership, communityservice, humanism and professionalism, and research/scholarship of the two groups of students. No statisticallysignificant differences were identified between HuMed andnon-HuMed students for the following academic outcomes:• USMLE Step 1 failures• Exceptional performance on the end of third-yearComprehensive Clinical Assessment• Honors grades in clerkship (except Psychiatry, wheresignificantly more HuMed students received honors grades)• School leadership• Gold Humanism Honor Society awards• Rank in the top twenty-five percent of the class• Nomination to AΩAHuMed students were significantly more likely (thirty-twopercent versus twelve percent) to do a scholarly year dedicatedto research and be awarded Doris Duke Clinical ResearchFellowships (twelve percent versus three percent) <strong>The</strong>re wasa nonsignificant trend among the HuMed students (elevenpercent versus seven percent) to graduate with Distinction inResearch (first-author peer-reviewed publication). Notably,HuMed students were also more likely to require nonscholarlyleaves of absence, typically for academic or personaldifficulties.Finally, although difficult to quantify, a trend was identifiedamong HuMed students versus non-HuMed students towardsresidency choices in Primary Care (fifty percent versusforty-two percent) and Psychiatry (thirteen percent versus sixpercent), and away from surgical subspecialties (five percentversus twelve percent) and Anesthesiology (seven percentversus eleven percent).<strong>The</strong> results provide evidence that for these HuMed studentsa significant reduction of standard premed requirementsdid not result in a limited ability to assimilate the basic scienceknowledge necessary for promotion to the clinical clerkshipyears, nor did it limit success in the clinical years either inclerkships, electives, clinical skills exams, research endeavors,or residency selection.Discussion<strong>The</strong> HuMed Program at Mount Sinai School of Medicinewas designed to encourage application from students whowere interested in the altruistic and humanistic elements ofa medical career but were deterred by the rigid academicrequirements.Directly or indirectly, intentionally or not, the traditionalrequirements appear to be very effective barriers that limitthe diversity of applicant premed preparation. Humanities andsocial science majors matriculating in U.S. medical schools in2010 comprised less than eighteen percent of the total. 16We believe however, these prerequisites need not be a barrierto dual-major collegiate education, provided the medicalschool has known policies that welcome, not exclude, suchapplicants. This has certainly been the case at Mount Sinai,where from the first entering classes in 1968 and thereafter theschool has welcomed dual majors. 17 In 2009, the proportionof these dual majors among the entering class was twentyfivepercent, excluding the HuMed students, and almosthalf (forty-three percent) when HuMed was included. <strong>The</strong>senontraditional students had pursued a wide range of liberal38 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
arts majors—music, history, theology, economics, and finearts, among others. <strong>The</strong> number one student in the class of2010 was a Religious Studies major, one of the top graduatesin 2009 (AΩA and currently a PGY2 in Medicine at MountSinai) a Dramatic Arts major, and the number one graduatein the class of 2008 a Music major. Finally, a member of theclass of 2014 spent his entire collegiate career in the extremelycompetitive combined Columbia-Juilliard Performing Artsprogram studying and performing as a cellist.This story does not always apply. Many students acceptedto Mount Sinai via the HuMed program decide to pursueother, nonmedical careers. Case in point: one acceptedHuMed student continued his interest in creative writing andis now a New York Times best-selling novelist!As an experiment in educational philosophy defining theingredients necessary for a career in medicine, the HuMed programclarifies the extent to which traditional courses in organicchemistry, physics, and mathematics are necessary for successfulcompletion of a medical school curriculum. For example,we compared the USMLE Step 1 scores, Step 1 failure rates, andserious academic difficulty (defined as three course failures ortwo course failures and two marginal grades in the first or secondyear of medical school) for the HuMed and non-HuMedcohorts. <strong>The</strong>se outcomes were respectively, Step 1 scores 221versus 227, Step 1 failure four percent versus two percent, andserious academic difficulty 2.4 percent versus 2.3 percent. Onlythe Step 1 score difference was statistically significant.More troubling is the higher rate for HuMed students ofnonscholarly leave of absence (eleven percent versus threepercent, P=.001). 14 This may indicate that a very small numberof students are troubled as they struggle academicallywith unfamiliar material (but do not fail) and require a pausebefore returning to school. Still others find they are unsureof their career choice. Mount Sinai addresses these concernsin a variety of ways: admission standards attempt to identifystudents with very high academic potential and intellectual“flexibility,” students who attend SEP learn studying and testtakingskills for the sciences, prospective students are stronglyencouraged to take at least one year off before matriculating.We believe this does allow ample time for most to reflect ontheir career choice. Happily, HuMed students in this categoryreturn to school and graduate at a rate no different from theirnon-HuMed classmates.HuMed outcomes suggest that no essential preparatoryingredient was missing by having had an extensive liberal artscollege education at the expense of the traditional requirementsand outstanding performance on MCATs. It is clearthat a significant reduction of the traditional requirements didnot result in either significant failure or significant inability toassimilate and apply the predoctoral basic science material inyears 1 and 2, nor did it limit success in the clinical years eitherin clerkships or clinical skills exams. <strong>The</strong> HuMed students didnot significantly fail the challenges of the basic sciences. Inaddition, they have performed as well, and in some instancesbetter, than their premed classmates in the clinical years.<strong>The</strong> success of HuMed over the years has had an unanticipatedbut gratifying impact on our medical school community.It has broadened the spectrum of criteria for admission forthe entire pool of applicants. In addition, it has encouragedinitiation and expansion of required and elective humanismin medicine courses within the medical school curriculum.Finally and yet to be determined is whether the expandedliberal arts background obtained in a variety of experiencessuch as electives, community service, additional degrees, andpersonal avocations will lead these HuMed students to pursuesuccessful, fruitful lifetime careers in the profession. Canfollow-up ever accurately measure fulfillment and satisfaction?Will burn-out frequencies or incidents of unprofessional behaviorbe reduced?Alas, incidents of immoral behavior occur in all elementsof society. Those of us in medicine—as practitioners, educators,or investigators—are painfully aware of the egregiousexamples of criminality, addiction, mendacity, abuse, plagiarism,and bribery that have tarnished our profession. We haveassumed, and continue to rely on, our ability to identify andweed out those with such tendencies as they emerge, howeversubtly, during the challenging and stressful years of medicalschool and residency training. Clearly, this process is an imperfectand deficient filter.We invite the <strong>Pharos</strong> readership to suggest applicable measureswe might employ to judge the long-term impact, if any,of the HuMed program on these students.What can be said with certainty, however, is that such a<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 39
change in requirements does not adversely influence successfulperformance in a demanding and highly competitive medicalschool environment.SummaryAs the HHMI-AAMC declared, their report should betaken as a “first step in a continuing conversation about theappropriate skills and knowledge,” and, echoing the ACGMEand GPEP, “values and attitudes that future physicians shouldpossess.” 9pExecSum As a new formulation evolves, the premedicalcurriculum must foster “scholastic vigor, analyticthinking, quantitative assessment and analysis of complexsystems.” 9pExecSum Based on the Mount Sinai experience, thesequalities are not engendered solely nor confined to engagementin natural sciences. Students involved in a variety ofbaccalaureate liberal arts endeavors appear to acquire similarintellectual competencies. Furthermore, when performed successfullyin challenging collegiate environments, a thoroughliberal arts education may yield precisely the same values,attitudes, and behavioral characteristics all agree are essentialto the medical profession and preparing physicians for thetwenty-first century.References1. Beck AH. <strong>The</strong> Flexner Report and the standardization ofAmerican medical education. JAMA 2004; 291: 2139–40.2. Flexner A. Medical education in the United States andCanada: A Report to the Carnegie Foundation for the Advancementof Teaching. Bulletin Number Four. New York: Carnegie Foundationfor the Advancement of Teaching; 1910. Available online at books.google.com.3. Dalen JE, Alpert JS. Premed requirements: <strong>The</strong> time forchange is long overdue! Am J Med 2009; 122: 104–06.4. Dienstag JL. Relevance and rigor in premedical education. NEngl J Med 2008; 359: 221–24.5. Emmanuel EJ. Changing premed requirements and themedical curriculum. JAMA 2006; 296: 1128–31.6. Kanter SL. Toward a sound philosophy of premedical education.Acad Med 2008; 83: 423–24.7. Gross JP, Mommaerts CD, Earl D, DeVries RG. After a centuryof criticizing premedical education, are we missing the point?Acad Med 2008; 83: 516–20.8. Thomas L. How to fix the premedical curriculum. N Engl JMed 1978; 298: 1180–81.9. AAMC-HHMI Committee. Scientific Foundations for FuturePhysicians. Washington (DC): Association of American MedicalColleges; 2009.10. Project Panel on the General Professional Education of thePhysician and College Preparation for Medicine. Physicians for theTwenty-First Century. Washington (DC): Association of AmericanMedical Colleges; 1984.11. Committee on Undergraduate Biology Education to PrepareResearch Scientists for the 21st Century, Board on Life Sciences,Division on Earth and Life Studies, National Research Council of theNational Academies. Bio 2010: Transforming Undergraduate Educationfor Future Research Biologists. Washington (DC): <strong>The</strong> NationalAcademies Press; 2003.12. ACGME Outcome Project. General Competencies. http://www.acgme.org/outcome/comp/compmin.asp. Accessed October2011.13. Medical School Objectives Project—Initiatives—AAMC.Medical School Objectives Project (MSOP). https: www.aamc.org/initiatives/msop. Accessed October 2011.14. Muller D, Kase N. Challenging traditional premedical requirementsas predictors of success in medical school: <strong>The</strong> MountSinai School of Medicine Humanities and Medicine Program. AcadMed 2010; 85: 1378–83.15. Gunderman RB, Kanter SL. “How to fix the premedical curriculum”revisited. Acad Med 2008; 83: 1158–61.16. Association of American Medical Colleges. Table 18: MCATand GPAs for Applicants and Matriculants to U.S. Medical Schoolsby Primary Undergraduate Major, 2010. https://www.aamc.org/download/161692/data/. Accessed October 2011.17. Rifkin MR, Smith KD, Stimmel BD, Stagnaro-Green A, KaseNG. <strong>The</strong> Mount Sinai Humanities and Medicine Program: An alternativepathway to medical school. Acad Med 2000; 75: S124–26.Address correspondence to:Nathan Kase, MDMount Sinai School of MedicineOne Gustave L. Levy Place, Box 1025New York, New York 10029E-mail: nathan.kase@mssm.edu40 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
Mechanical ManSpread-eagled in full restraints,Donald Bates glares at me,a plastic tube in his throatconnecting with a Bennett respiratorwhose dials dictate his breathing.<strong>The</strong> lump under the skin of his chest,a Medtronic pacemakersince his November heart attack,clicks its seventy beats a minute.Each night they debate their total controlas he struggles to sleep—the respirator, heaving and sighingin a whish thump voicechallenging him to live without it,the electronic genius inside his chestboasting its controlof pump and flow to every organneeded to survive.This morning he scribbleson a clipboard like a third-grade child,“Why are you doing this to me?”Outside the CCU his family waitsfor my morning report.I avoid the clichés—they see in my eyesthe news they expect to hear.I go home to fix a doorknob in the kitchen.Henry Langhorne, MDDr. Langhorne (AΩA, Tulane MedicalSchool, 1957) is in private practice incardiology at Cardiology Consultants inPensacola, Florida. His address is: 1910Seville Drive, Pensacola, Florida 32503.E-mail: bardwhl@aol.com.Illustration by Jim M’Guinness.<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 41
2011 Robert J. Glaser DistinguishedTeacher Awards<strong>The</strong> 2011 AΩA Robert J. Glaser Distinguished Teachers. Left to right: Dr. Thomas Lawley, immediatepast-chair of the AAMC, Dr. Richard L. Byyny, Executive Director of <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong>, Dr. Mark T.O'Connell, Dr. LuAnn Wilkerson, Dr. Dennis H. Novack, Dr. Gerald D. Abrams, and Dr. Darrell Kirch,President of the AAMC.Each year since 1988, <strong>Alpha</strong> (Jack) Nolte, PhD; Jeanette Norden, Gerald D. Abrams, MD<strong>Omega</strong> <strong>Alpha</strong>, in cooperation PhD; James L. Sebastian, MD; Professor Emeritus of Pathology,with the Association of AmericanMedical Colleges, presents fourAΩA Distinguished TeacherAwards to faculty members inAmerican medical schools. Twoawards are for accomplishmentsin teaching the basic sciences andtwo are for inspired teaching inthe clinical sciences. In 1997, AΩAnamed the award to honor its retiringexecutive secretary Robert J.Glaser, MD. Nominations for theKelley M. Skeff, MD; Jeffrey G.Wiese, MD.Winners of the award receive$10,000, their schools receive$2,500, and active AΩA chaptersat those schools receive $1,000.Schools nominating candidates forthe award receive a plaque with thename of the nominee.Brief summaries of the accomplishmentsin medical educationof the 2011 award recipients follow.University of Michigan MedicalSchoolIn his more than five-decade career,Dr. Abrams (AΩA, University ofMichigan, 1953) has educated nearly10,000 students on the intricacies ofpathology, and has been consistentlyrated the highest performing basic sciencefaculty teacher at the University ofMichigan Medical School. For much ofhis career, Dr. Abrams has contributedto the oversight, design, and modificationof the medical school curriculum.award are submitted to the AAMCRichard L. Byyny, MDeach spring by the deans of medicalIn the 1970s, he developed a series ofExecutive Directorschools.lectures in general pathology that inNominations were reviewed bya committee chosen by AΩA andthe AAMC. This year’s committeemembers were: Helen C. Davies,PhD; Joel M. Felner, MD; WilliamH. Frishman, MD; Aviad Haramati,PhD; Robert M. Klein, MD; Johnthe 1990s was made an independent,permanent part of the first-year curriculum.Over the years, Dr. Abramshas adapted his teaching methods toincorporate advances in informationtechnology. He developed an interactiveCD-ROM to accompany a histopathologycourse he developed and later digitizedthe slides from the course to createa “virtual microscope” format to be used42in teaching labs and on the Internet.<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
Dennis H. Novack, MDProfessor of Medicine, AssociateDean for Medical Education, DrexelUniversity College of MedicineDr. Novack (AΩA, Drexel University,2001) has made significant contributionsto the way in which academicmedicine teaches and assessesphysician-patient communications.He was integral to the development ofan Internet-based clinical skills curriculumand more recently developeda complementary Internet-based assessmenttool. In partnership with theAmerican Academy on Communicationin Healthcare and Drexel University,Dr. Novack led the creation of doc.com. Using text and video, doc.comdemonstrates basic and advanced interviewingskills through more thanforty modules tailored to various learnerdevelopmental stages. Dr. Novack alsohelped develop WebOSCE, which enablesstudents to interview standardizedpatient-actors through videoconferenceand provides both immediate feedbackfrom the patient-actor and a video of theinteraction for further review, as wellas links to doc.com and other sites thathelp learners enhance their skills. AtDrexel, Dr. Novack created and directsthe Physician and Patient course, whichprovides fundamental skills to first-yearstudents, and also directs and teachesthe doctoring curriculum for internalmedicine residents.Mark T. O’Connell, MDSenior Associate Dean forEducational Development, SeniorAdvisor to the Dean, Bernard J.Fogel, M.D., Endowed Chair inMedical Education, and AssociateProfessor of Medicine, University ofMiami Leonard M. Miller School ofMedicineFor more than a quarter-century, Dr.O’Connell (AΩA, University of Miami,1995) has made numerous contributionsin the areas of information technology,curriculum design, program development,and student initiatives. Heestablished the Office of BiomedicalComputing, one of the first microcomputerlabs at a medical school, whichallowed Miller School students to beamong the first trained on MEDLINE.He pioneered the use of a controlledvocabulary to index the Miller School’scurriculum and then worked withthe AAMC to develop the curriculardatabase that was the forerunner ofCurrMIT. Described as a consummateprogram builder, Dr. O’Connell wasinstrumental in creating a two-yearsatellite program at Florida AtlanticUniversity. When the program expandedto four years, he helped develop the curriculumand oversaw all aspects of theaccreditation process. His influence isfelt throughout the Miller School, havingbeen responsible for establishing theDepartment of Community Service, astudent-run nonprofit that consistentlyachieves nearly one hundred percentparticipation, the Office of ProfessionalDevelopment and Career Guidance tomentor students, and the Physicianshipand Professionalism Advocacy Program.LuAnn Wilkerson, EdDProfessor of Medicine, SeniorAssociate Dean for MedicalEducation, University of California,Los Angeles David Geffen School ofMedicineDr. Wilkerson’s vision for medicaleducation is one in which engagedlearners and passionate teachers implementa coordinated and ever-evolvingcurriculum. For more than three decades,she has pursued this goal throughthe design of medical school curriculaand enhanced faculty development. Toensure that UCLA’s students possess thecompetencies needed for modern medicalpractice, Dr. Wilkerson helped pioneerthe Doctoring program. She alsooversaw the creation of fourth-year “colleges”—learningcommunities that pairstudents and faculty to enhance careermentoring. Dr. Wilkerson directs theCenter for Educational Developmentand Research, which helps faculty improvecurriculum and fosters teachingskills and the use of technology. Sheis dedicated to faculty development,particularly as it relates to ambulatoryteaching and problem-based learning.Dr. Wilkerson has been described as “ateacher of teachers,” whose “accomplishmentsand contributions to the fieldof medical education are colossal andprofound.”<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 43
Reviews and reflectionsDavid A. Bennhaum, MD, and Jack Coulehan, MD, Book Review EditorsExploring Happiness: FromAristotle to Brain ScienceSissela BokYale University Press, New Haven, CT,2010Reviewed by Stephen G. Post, PhDIn 1978 while I was at the Universityof Chicago, Martin E. Marty placed ahardback copy of Sissela Bok’s then newbook, Lying, in my hand and said, “Readit!” Fortunately, his intention was nonremedial.In reading Lying, I discoveredwhat it means to write masterful philosophicalhistory for a wide audiencewhile articulating a clear normativeposition that is balanced, notoverbearing, and of value forthe wider culture. Manyremarkable books fromSissela Bok have followed,all of themmaking real conceptual progress oncarefully selected topics that beg to beaddressed across many sectors of society.But this newest book, ExploringHappiness, is Bok’s best ever. Why?Methodologically, Bok has now positionedherself at the new interface betweenmoral thought and the sciences,both social and biological. Here sheglides with astonishing clarity throughthe works of philosophical, and evensome theological, luminaries, pickingand choosing her key figures with innovativediligence. But she is equallyadept in her familiarity with key scientificfindings on happiness as sheengages with national and internationalhappiness surveys, the genetics of “setpoint” happiness, evolutionary psychology,economic investigations of moneyin relation to happiness, game theory,neuroscience, pro-social behavior, socialcapital theory, positive psychology,and so forth. Those of us who believethat meaningful progress can best bemade on big topics such as happinessonly at such a dialogical interface withthe sciences are of course delighted tosee an eminent philosopher like Bokturning in this direction.<strong>The</strong> astonishing thing aboutExploring Happiness is that the clearand probing exegesis of the great philosophersis matched in quality by thepenetrating analysis of major scientificinvestigations. Bok weaves these twostrands together with precision andan ability to make the connections betweendomains of knowledge that wouldotherwise remain apart in separate academicsilos, making real progress unlikely.She provides what is, in my view,the best example of integrative scholarshipon happiness to date. This is thereforea book that any neo- Aristotelian,utilitarian, or Kantian philosopher willhave to grapple with, and that any scientistinterested in a deeper conceptualunderstanding of the “happiness”that they are investigating will have toread before focusing on methodologicaltechnocracies. Both the philosophy andthe science are presented in a way thatmost lay readers will easily handle, andin her skillful, almost pastoral, style,Bok is able to make all this relevant tothe reader on an existential level. It ispossible to read this book and be transformedto some degree.Bok is always an innovative thinkerby virtue of her ability to pick importantand timely topics, often ones that havenot been handled before with muchclarity. What do we mean by happiness?How much of it can be had inthis life? How can it be measured? Isour happiness something for which weare responsible as individuals at somelevel, despite genetically shaped predispositionsand personality types? Howcan we nurture it? Can happiness everbe lasting, or is it always fleeting andunstable? Do we always fear its loss?Is there any one view of happiness that44 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
trumps others, or should we be verycautious about such assertions? Howdoes my “pursuit” of happiness pertainmorally to your pursuit? Whose happinessare we ultimately responsible for, orcan we be responsible for?Exploring Happiness is great expositionalwriting. Bok warns that thetopic is extremely complex, and thatwe should not seek premature closure.She is clear in her conclusion that thepursuit of happiness needs to be morallycircumscribed. After all, there arethose who, like the al-Qaeda pilots whoflew into the World Trade Towers, dogreat damage while pursuing their ownvisions of a promised eternal bliss. Inother words, at some level, we do needto relate our individual pursuits of happinessto the notion of a shared or acommon humanity rather than to somesmall fragment thereof, and we must becareful of arrogance.In humility, Bok does not wish toprescribe any one vision of happiness,or to set out a method for achieving it.As she writes,I have argued for the greatest possiblefreedom and leeway in the pursuitof happiness, subject to morallimits. <strong>The</strong>re is no one view of happinessthat should exclude all others,much less be imposed on therecalcitrant. But the pursuit cannotmerely involve “choosing happiness”as many advice manuals propose.Pursuits of happiness that abide byfundamental moral values differ cruciallyfrom those that call for deceit,violence, betrayal. p176One wonders, though, if this retreatfrom much objectivity in the pursuit ofhappiness really suffices. It is of courseimportant that our pursuits of happinessbe limited by some foundational andminimalist moral restraints. But are wenot rightly tempted to encourage a viewof happiness comprised by some setof goods pursued over the course of alifetime, such as contributing to the livesof others, moral integrity, and nobilityof purpose? <strong>The</strong> neo-Aristotelians andeudaemonists will no doubt engage insome critique of Exploring Happinessbecause it clearly constitutes the finestliberal (minimally prescriptive) analysisof happiness to date, and as suchdeserves very high praise indeed. It isnormative not in asserting what happinessis, but in articulating proceduraland minimalist contractarian moral restraintson its pursuit. Perhaps this isenough, for as they say, “hard lessonsare learned hard,” and perhaps we canonly teach ourselves how to pursue happinesswell in all our idiosyncratic error.This book is highly recommended asthe best liberal contractarian statementto date. But the neo-Aristotelians whoare coming into dominance in manyAmerican universities will wish for atreatment of happiness that is in facta little more prescriptive than whatBok offers. Perhaps they have met theirmatch.Dr. Post is the director of the Center forMedical Humanities, Compassionate Careand Bioethics at Stony Brook UniversityMedical School. His address is:Center for Medical Humanities,Compassionate Care, and BioethicsHealth Sciences CenterStony Brook UniversityStony Brook, New York 11794-8335E-mail: steven.post@stonybrook.eduMatch Day: One Day and OneDramatic Year in the Lives ofThree New DoctorsBrian EuleSt. Martin’s Griffin, New York, 2010, 272pagesReviewed by R. MacDonell-Yilmaz,MPHWhen I approached Brian Eule’sMatch Day, I imagined it mightmake an apt birthday gift for a goodfriend, a fellow third-year medical student.Given its focus on “a ritual thathad grown more intense and anticipatedthan graduation itself,” as experiencedby three young women—Eule’sgirlfriend Stephanie, and friends Rakhiand Michele—I anticipated that itmight offer a glimpse into our own fastapproachingfutures.<strong>The</strong> prologue depicts the tensionof Match Day morning, leading up tothe moment when envelopes across thecountry will be opened. It then leaves ushanging, stepping back to orient readersto the Match, complete with its originsand modifications. This history is trulyenlightening; I had no idea that theMatch computer resides in Washington,DC, and runs its annual algorithm tocompletion in less than ten minutes.Subsequent chapters examine the applicationprocess and the nuances of applyingto specific residencies, especiallythose offering more flexible lifestyleswithout a sacrifice in pay: the “R.O.A.D.(radiology, ophthalmology, anesthesiology,dermatology) to Happiness.” It alsoprovides an honest look at what influencesapplicants’ decisions about whereto apply and how to rank programs. Oneparticularly compelling scene depictsRakhi’s struggle to finalize her rank listhours before the deadline. She mustweigh the program she has dreamed offor years against one at another universitywhere her husband—who movedacross the country, worked unfulfillingjobs, and weathered rejections from<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 45
Reviews and reflectionsgraduate schools while she studied medicine—hasjust gained admission. Thisglimpse of a couple sorting throughcomplex if-this-then-that scenarios, attemptingto reconcile disparate personalgoals with an entwined future,poignantly illustrates how this profession’straining taxes many lives beyondthat of the trainee.We arrive back at Match Day to learnthe contents of the women’s envelopesand then set out with the newly-mintedphysicians as they navigate the challengesof internship. Along the way, Euleexplains the controversies surroundinglegal work-hour restrictions.He also explores the difficulties of“finding time for a life,” especially forStephanie, a surgical intern. In a raremoment of expressing his own feelings,Eule confesses how the strain of interns’lives extends to their loved ones:<strong>The</strong> problem with Stephanie’sschedule, in addition to the longhours, was the lack of predictability.. . . I could never tell what time shewould get home from the hospital.And she never knew the four individualdays she would get off in amonth until that month’s rotationbegan. . . .It was impossible to make plansto see friends or family. . . . My resentmentgrew. pp135–36Happily, we learn, she does find at leasta smidgeon of free time—enough fortheir wedding at year’s end.Throughout the book, Eule’s tone variesbetween journalistic and narrative.Using the former, he explains the Matchand its permutations, including theCouple’s Match and the transitional year.His account of the infamous Zion caseand the resulting Bell Commission areexcellent as well; his words flow smoothlyand authoritatively, easily capturing andmaintaining the reader’s attention.Much of the actual storytelling, however,is not handled as deftly. His narrationof the women’s experiences lacksthe spark of his journalism. It feels asif Eule is trying to convince us that hissubjects are likeable and their storiesmoving, but the details are often forcedand generic rather than unique anddefining. He notes, for example, thatMichele’s “keen awareness of fashionoften led her to opt for a trendy hat,knit scarf, or big sunglasses” p32 and thatan end-of-year party is “sure to includedrinking and celebrations.” p234This tendency is especially frustratingin his depictions of the women’smedical experiences. For a practitioner,the incidents he highlights and his descriptionsof them are neither earthshatteringnor revelatory—a medicalstudent nervous about practicing blooddraws with classmates, a surgeon snappingat an intern, a cancer patient refusingfurther treatment. I wanted to pullhim aside and whisper, You think this isbad? You don’t know the half of it.Admittedly, my irritation at hiswordiness might simply stem from myown impatience, a trait Stephanie alsopossesses: “After hours of moving fast,of talking quickly and efficiently, shesometimes expected the same at home.If I answered a question in a roundaboutway, I could see aggravation inher eyes.” p210 Slower sections of writinginspired similar aggravation as I wadedalong, eager to reach the next exampleof his journalistic prowess.Overall, Match Day offers a fascinatinghistory and fresh perspectiveon medical training from an authorwho, though neither practitioner norpatient, finds his life deeply affectedby the process. Just as House of Godserves as an unofficial handbook formedical students and residents, MatchDay is an excellent guide for family andfriends. Ultimately, I bought my friend abouquet of flowers and passed the bookalong to my mother.Ms. MacDonell-Yilmaz is a member of theClass of <strong>2012</strong> at the School of Medicine atStony Brook University Medical Center.Her e-mail address is: beckymacd28@gmail.com.We’re NOT Leaving: 9/11Responders Tell <strong>The</strong>ir Storiesof Courage, Sacrifice, andRenewalBenjamin J. Luft, MDGreenport Press, New York, 2011Reviewed by Richard Bronson, MD(AΩA, New York University, 1965)Williamsburg Bridge, sun hits thetrainAs it rises over the city again.Nobody speaks, everyone staresRemembering all that used to bethere.“Brooklyn Train,” Lucy KaplanskyMy waiting room had a televisionattached to the wall. In the middleof morning hours, a nurse cried, “Come,look at this.” Against a blue, cloudlesssky, I saw the tail of an airplane stickingout of the upper stories of one of theTwin Towers, surrounded by flames!<strong>The</strong>n the second jet, the realization thatthis was not an accident, the unexpectedcollapse of both towers, the horror andfear as the day went on and the magnitudeof the attack became clear. It was atime of candlelight vigils, firemen andpolicemen marching to bagpipes at funerals,and photos of missing husbands,wives, sons, and daughters stapled totelegraph poles. Twin searchlights rose46 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
into the night for months, a reminderof what had been there. But the invasionof Baghdad, two lengthy wars, theeconomic crisis, and a major recessionintervened. We largely lost trackof the responders who were imprintedwith the trauma of those days and havecontinued to lead their lives, altered bythat experience. We’re NOT Leavingrestores our emotional connection withthat event, and the people who played aheroic role in the initial response to theattack and the subsequent clean up andreclamation. This is their oral history.Created by Dr. Benjamin Luft, theEdward D. Pellegrino Professor ofMedicine at Stony Brook UniversityMedical Center and Director of theLong Island Medical Monitoringand Treatment Program, We’re NOTLeaving contains a selection of firstpersonnarratives from more than 125videotaped interviews. Many of thesemen and women are still recoveringfrom the disaster. As Dr. Luft notes,“<strong>The</strong>y suffer from post-traumatic stressdisorder, nightmares, sleep apnea, anxiety,asthma, persistent cough, and inmany cases, anger and disillusionmentabout how they were treated by a societythat dragged its feet in respondingto their needs when they became illas a result of responding to the disaster.”p14 He has recognized the necessityof remembering.<strong>The</strong> book consists of thirty-two chapters(each an individual’s personal narrative),divided into five sections, and anepilogue. <strong>The</strong>se sections, titled “Caughtin the Collapse,” “Looking for Survivors,”“Recover, Recovery, Recovery,” “<strong>The</strong>Responders Need Help,” and “Renewal,”take us from the initial moments of theattack, before and following the collapseof the Towers, the experiences of earlyresponders, the realization that therewere few survivors, the search for bodiesor portions of bodies, the work ofdismantling the wreckage, and, finally,efforts to support those who worked on“<strong>The</strong> Pile” and minister to their needs.Dr. Luft best describes these testimonies.“<strong>The</strong> stories are powerful . . . <strong>The</strong>irlanguage is simple, frank, and descriptive. . . Although they speak of sorrowand pain, to me they are a source ofcelebration of the human spirit’s abilityto transcend unimaginable hardships,and still maintain its humanity.” p8 <strong>The</strong>reis no better way of conveying what hemeans than to quote a few representativestories:I was actually inside the building,near the escalators, when the Towercollapsed. . . . And I was able to holdonto the doorway with my left arm.People blew by me and under meand through me. Only with one arm,did I hold on. . . . there was utterterror. . . .. . . As we crawled out we sawpeople and we tried to help themand they were dead. . . .. . . Our radios didn’t work. . . .I couldn’t call my command. pp24–27In the beginning, the first fewdays, it was very hard to get around.<strong>The</strong>re were makeshift morguesaround the place, and you could seepeople picking up body parts andputting them in bags and peoplecrying. It was very sad and scary, Iactually felt like I was in a war zone.. . . We were working twentyfourhours a day, seven days a week.We were sleeping on the floor at 60Hudson Street. We just take a nap,get up, and . . . It was taking its toll.A couple days without showering,everyone smelling, stinking. pp39–41I’m a psychiatrist . . . volunteerresponder. . . .. . . We’re learning about all thesephysiological interactions betweenstress, depression, PTSD and heartdisease and the immune system andother things that shorten lives . . . .. . . I think the press and the publiclook at it as though it was oneevent . . . .. . . But it was hundreds of eventsto any one person who responded.. . .. . . <strong>The</strong>re were fires, there wereexplosions, there were tons of steeland debris falling. <strong>The</strong>re were jumpers,there were bodies falling. . . .It’s etched in their brains, in theirminds, in their memory and theirspirit. pp317–21I am very proud that in time ofcrisis, 9/11, that our church showedup and we stood there . . . We werethere every day, 24/7, for eight and ahalf months. We served over half amillion meals . . . .. . . and many days I would doblessings and last rites on body bags,and it meant the world to the workersto have the clergy in the site withthem . . .. . . <strong>The</strong>y wore respirators insteadof neckties and Kevlar suits insteadof Brooks Brothers suits. So this wasa community that was brought togetherout of love, through love andcompassion and service. I like to describeit as a season of love. pp380–82When I started to read We’re NOTLeaving, I was concerned that muchmight be lost in transcription. This wasnot the case. <strong>The</strong>re were times when Icould not continue reading. It was tooemotionally difficult, and I had to putthe book down. <strong>The</strong>re is a deep truth inthese voices of people who placed theirduty above their own personal healthand gave everything they could give ata time when our country was attacked.Dr. Bronson is Professor of Obstetrics &Gynecology and Pathology at Stony BrookUniversity Medical Center and a memberof the editorial board of <strong>The</strong> <strong>Pharos</strong>. Hisaddress is:Stony Brook University Medical Center,T9-080Stony Brook, New York 11794-8091E-mail: richard.bronson@sbumed.org<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 47
2011 meeting of the AΩA board of directors<strong>The</strong> annual meeting of the board of directors of <strong>Alpha</strong><strong>Omega</strong> <strong>Alpha</strong> was held in Chicago, Illinois, on September24, 2011. Present were:Officers: President Rae-Ellen W. Kavey, MD, MPH;Vice President Donald E. Wilson, MD, MACP; Secretary-Treasurer C. Bruce Alexander, MD.Members at large: Robert G. Atnip, MD; N. JosephEspat, MD; Ruth-Marie Fincher, MD, MACP; Eve J.Higginbotham, MD; Douglas S. Paauw, MD; Don W.Powell, MD; Joseph W. Stubbs, MD, FACP.Councilor directors: Richard B. Gunderman, MD, PhD,Indiana University School of Medicine; Sheryl Pfeil, MD,the Ohio State University College of Medicine; Alan G.Wasserman, MD, George Washington University School ofMedicine and Health Sciences.Student directors: Alicia Alcamo, MD, the Ohio StateUniversity College of Medicine; William E. Bynum IV,MD, University of South Carolina School of Medicine;Tonya Cramer, MSIV, Chicago Medical School at RosalindFranklin University of Medicine and Science; Cason Pierce,MD, University of Texas Southwestern Medical School.Medical Organization Director: John Tooker, MD,MBA, American College of Physicians.Coordinator, Residency Initiatives: Suzann Pershing,MD.National office staff: Executive Director Richard L. Byyny,MD; Assistant Treasurer William F. Nichols; ManagingEditor Debbie Lancaster; Programs Administrator JudyYee; Membership Administrator Lena Beavers; ControllerBarbara Prince.Absent were: Anne Mancino, MD, councilor director forthe University of Arkansas School of Medicine, and CarolA. Aschenbrener, MD, of the Association of AmericanMedical Colleges.New to the board are: Eve J. Higginbotham, MD,elected to a three-year term as member at large; Alan G.Wasserman, MD, elected to a three-year term as councilordirector; Tonya Cramer, MSIV, elected to a three-yearterm as student director; and Carol A. Aschenbrener,MD, elected to a three-year term as Medical OrganizationDirector.Retiring from the board are: Cason Pierce, MD; AnneMancino, MD; Donald E. Wilson, MD.Renewed for three-year terms are: C. Bruce Alexander,MD; Robert Atnip, MD; Joseph Stubbs, MD.Constitutional changes<strong>The</strong> board voted to approve the following constitutionalchanges:1. Eliminate the office of Vice President2. Add the office of President-Elect3. Add the office of Immediate Past President<strong>The</strong> relevant changes to the constitution may be seen onAΩA’s web site: www.alphaomegaalpha.org/constitution.html, Article V. Organization and Central Administration.Dr. Tooker will chair a committee to explore furtherconstitutional changes.Elections<strong>The</strong> following members of the board were elected asofficers:1. Ruth-Marie Fincher, MD, MACP, President2. Rae-Ellen W. Kavey, MD, MPH, Immediate PastPresident3. C. Bruce Alexander, MD, President-Elect4. Joseph W. Stubbs, MD, FACP, Secretary-TreasurerTwo honorary members were proposed this year. Bothwere elected to honorary membership for their distinguishedcontributions to medicine. Profiles of these honorarymembers will appear in a future issue of <strong>The</strong> <strong>Pharos</strong>:1. Thomas R. Cech, PhD2. Martin George Tauber, MDReportsDr. Kavey and Dr. Byyny presented their reports forthe year, summarizing the year for AΩA programs, newmedical school chapters, chapter visits, fundraising, themembership directory and database, communications andpublic relations, and staffing.<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 48
National and chapter news<strong>The</strong> financial review was presented by Mr. Nichols andDr. Alexander. A presentation on AΩA’s investment programwas given by Jennifer Ellison and Diana Liebermanof Bingham Osborne & Scarborough.A report on <strong>The</strong> <strong>Pharos</strong> was presented by DebbieLancaster.Dr. Gunderman and former councilor director Dr.Gabriel Virella reported on the 2011 AΩA CouncilorsMeeting, held on September 22 and 23, just before theboard of directors meeting. Drs. Gunderman and Virellachaired the meeting. A report on the meeting will appearin a future issue of <strong>The</strong> <strong>Pharos</strong>.Dr. Pershing presented a report on the ResidentsInitiative project, which has resulted in the AΩAPostgraduate Award (see our web site for more details:www.alphaomegaalpha.org/postgrad_award.html).New businessDr. Byyny discussed the possibility of AΩA support fora leadership development program. A committee chairedby Dr. Tooker will investigate the proposal and possibleways for AΩA to contribute to leadership in medicine.Dr. Byyny led discussion on communication strategiesand public relations outreach to members and the public.A Communications committee was formed, chaired by Dr.Atnip. A PR Committee chaired by Dr. Higginbotham wasestablished.Miscellaneous<strong>The</strong> minutes of the 2010 board meeting were approved.A final budget was also approved. <strong>The</strong> <strong>2012</strong> board meetingwill be held in San Francisco in October <strong>2012</strong>.Instructions for <strong>Pharos</strong> authorsWe welcome material that addresses scholarly andnontechnical topics in medicine and public health such ashistory, biography, health services research, ethics, education,and social issues, as well as philosophy, literature,the arts, professionalism, leadership, and humor. Poetryis welcome, as well as photograph/poetry combinations.Photography and art may also be submitted. Scholarly fictionis accepted. All submissions are subject to editorialboard review. Contributors need not be members of <strong>Alpha</strong><strong>Omega</strong> <strong>Alpha</strong>. Papers by medical students and residentsare particularly welcome.Submissions must meet the following criteria:1. Submissions may not have been published elsewhereor be under review by another journal.2. Essays should have a maximum of 15 pages (approximately5000 words), and be submitted in 12-pointtype, double-spaced, with one-inch margins. <strong>The</strong>y shouldbe accompanied by a covering letter and a title page withthe word count (or page count), return address, and e-mail address. References should not exceed 20 uniqueitems (see below).3. Poems or photograph/poetry combinations shouldbe in 12-point type, with one-inch margins, with the author’sname, address, and e-mail address on the first page.4. Electronic submissions are preferred. Send them toinfo@alphaomegaalpha.org. Or send by mail to Richard L.Byyny, MD, Editor of <strong>The</strong> <strong>Pharos</strong>, 525 Middlefield Road,Suite 130, Menlo Park, California 94025.5. After peer review, comments on the manuscriptwill be sent to the author along with an editorial decision.Every attempt is made to complete preliminary reviewswithin six weeks.6. <strong>The</strong> editors of <strong>The</strong> <strong>Pharos</strong> will edit all manuscriptsthat are accepted for publication for style, usage, relevance,and grace of expression, and may provide appropriateillustrative material. Authors should not purchaseillustrative material because the editors cannot guaranteethat it will be used.7. In accordance with revised copyright laws, eachcontributor will need to sign an Author’s Agreement,which will be sent with the edited galleys. Informationon copyright ownership and re- publication of articles isdetailed in the Author’s Agreement.Reference informationAuthors are responsible for the accuracy of citationsand quotations in their papers. Once a manuscript hasbeen accepted for publication, therefore, the authorwill be required to provide photocopies of all directquotations from the primary source material, indicatingpage numbers. (Please mark the quoted material on thephotocopies with highlighter.) In addition, the editorswill require photocopies of all references: the title pageand copyright pages of all books cited, the first and lastpages of book chapters cited, and the first and last pagesof journal articles cited, as well as the Table of Contentsof the particular issue of the journal in which the citedarticle appeared. PubMed or MedLine citations are alsoacceptable. <strong>The</strong> foregoing items will be used to verify theaccuracy of the quotations in the text and the referencescited, and to correct any errors or omissions. <strong>The</strong> photocopieswill not be returned.49 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
National and chapter newsReferences should be double-spaced, numbered consecutivelyin the text, and cited at the end in the followingstandard form:Journal: Zilm DH, Sellers EM, MacLeod SM, Degani N.Propranolol effect on tremor in alcoholic withdrawal. AnnIntern Med 1975; 83: 234–36.Book: Harris ED Jr. Rheumatoid Arthritis. Philadelphia:WB Saunders; 1997.Book chapter: Pelligrini CA. PostoperativeComplications. In: Way LW, editor. Current SurgicalDiagnosis and Treatment, Ninth <strong>Edition</strong>. Norwalk (CT):Appleton & Lange; 1991: pp 25–41.Each reference should be listed in the bibliography onlyonce, with multiple uses of a single reference citing thesame bibliography reference number. Examples are availableat our web site: www.alphaomegaalpha.org.Citation of web sites as references is discouraged unlessa site is the single source of the information in questionor has official or academic credentials. Examples of suchsites are official government web pages such as that ofthe National Institutes of Health. Encyclopedia sites suchas britannica.com are not primary references. Do not useWikipedia as a reference.Leaders in American MedicineIn 1967, as a result of a generous gift from Drs. DavidE. and Beatrice C. Seegal, <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong> initiated aprogram of one-hour videotapes featuring interviews withdistinguished American physicians and medical scientists.<strong>The</strong> collection has been donated to the National Libraryof Medicine, which will maintain it for permanent use byscholars visiting the library. <strong>The</strong> collection has been digitizedand excerpts will be featured on AΩA’s web site in thefuture. A listing of videos available for loan as DVD or VHStape can be found on our web site: www. alphaomegaalpha.org, or by contacting Debbie Lancaster at d.lancaster@alphaomegaalpha.org or (650) 329-0291. Those wishing topurchase copies may do so by contacting Ms. Nancy Dosch,manager, Historical Audiovisuals, History of Medicine,Building 38, Room 1E-21, 8600 Rockville Pike, Bethesda,Maryland 20891. Telephone (301) 402-8818, e-mail nancy_dosch@nlm.nih.gov.Letters to the editorRe “AΩA and Professionalism inMedicine”Your editorial in the Summer issueof <strong>The</strong> <strong>Pharos</strong> is very well done(Summer 2011, pp. 1–3).Here is a brief passage from myfile—to me it is a like expression ofsome of the points of your essay:teachers by “osmosis.” My sources wereWilliam L. Bradford, MD, and WilliamS. McCann, MD.Russell M. Lane, MD(AΩA, University of Rochester, 1955)Sunderland, Massachusettsa voice that medicine can ill affordto lose—one of clearheadedness, unsentimentalidealism, and the greatwisdom of affectionate optimism.—Hans Zinsser commenting onFrancis Weld Peabody,circa 1928I am 83, a retired G.P.—in my medicalschool days, we talked about learning“professionalism” from our reveredRe “<strong>The</strong> Light Switch,” Summer2011, pp. 30–32Thank you for sharing yourunfortunate experience on theobstetric anesthesia servicein <strong>The</strong> <strong>Pharos</strong>. That samething happened to meon my last call nightin anesthesiologyresidency sixteenyearsago. I was<strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong> 50
on overnight with one of the cardiacanesthesia attendings. Lucky, becauseit quickly turned into a cardiac case.Mother and one of the twins did notmake it, the other twin survived. Afterthree hours of resuscitation and opencardiac massage, we rolled the patientdown the hall to the ICU on fem-fembypass. <strong>The</strong> look of the husband’s sobbing,anguished face is still seared intomy memory. <strong>The</strong>n when Dr. SheilaCohn, Chief of Obstetric Anesthesia atStanford, came in at 6 AM and lookeddown at me with her wise, sympatheticeyes while I was writing my note, I justlost it. <strong>The</strong> diagnosis at the time wasfairly obvious looking at the bloated,quivering right ventricle and studieslater confirmed it: amniotic fluid embolism.But that didn’t make it any easier. . . my first intra-operative death,and my career had not even begun.And then the feelings of doubt andguilt. Of thinking over and over, wasthere something I did to cause this orcould have done to prevent it? Maybethere was something more I could havedone to save her? It had a huge impacton me as I purposefully chose a jobthat did not have obstetric anesthesiaservice despite really enjoying OB anesthesiaduring my residency.Reading the beautifully written accountof your experience on that fatefulnight eight years ago helped meremember and reprocess my event.Thanks. I, too, still think about thatlonesome father and his daughter, nowage sixteen, and grieve.Jeffrey Clayton, MD(AΩA, Medical College of Wisconsin,1990)Department of AnesthesiologySutter Medical CenterSacramento, CaliforniaE-mail: jclaytonmd@surewest.netMy wife and I really enjoyed readingyour article, “<strong>The</strong> Light Switch.” It wasan extremely well-written account ofan incident that every physician fearsand dreads facing in their professionalcareer. One can only imagine yourthoughts and reactions at the time, butyour telling of your experience servesas an example of the compassion thatall physicians should have towards theirpatients and families, as well as part ofthe process of catharsis that must comesooner or later if one is to continue tobe an effective physician. Thank you somuch for sharing what must have beena most difficult process for you and allothers involved, including the family ofyour patient.Roger A. Meyer, MD, DDS, FACS(AΩA, Creighton University, 1975)Greensboro, GeorgiaE-mail: rameyer@aol.comThank you for your article. I am apracticing anesthesiologist in suburbanChicago. We graduated medical schoolthe same year and I can tell our careershave much in common.I recently cut back to part timepractice, but OB anesthesia remainsmy most treasured work environment.You clearly captured the joy and potentialagony of OB anesthesia and Iempathize with you and your patient’sfamily.A bad outcome in anesthesia is verypainful for experienced practitionerslike ourselves to accept, but is somethingwe all must learn to live with.Your caring and open response to thefamily and situation provides a modelfor our profession.I plan to share your most thoughtfularticle with my colleagues.Thank you again for your contributionand best regards.Ed Matthew, MD(AΩA, University of Illinois, 1982)E-mail: putuout@yahoo.comRe “<strong>The</strong> History of Tracheotomy”I enjoyed reading the article ofDrs. Choby and Goldenberg on “<strong>The</strong>History of Tracheotomy” (Summer2011, pp. 34–38). <strong>The</strong>ir exposé ofthe evolution of the procedure fromprehistoric times until today is comprehensiveand very interesting. I dotake issue with their assertion concerningthe death of George Washingtonwhich perpetuates the misconceptionthat “the first President of the UnitedStates died of an acute upper airwayobstruction secondary to a peritonsillarabscess.” p36 A review of the historicalaccounts of George Washington’s demiseand the chronology of his symptomssuggests that his final illness wasmost likely adult acute epiglottitis. <strong>The</strong>clinical picture of a rapidly escalatingsore throat, hoarseness, and respiratoryobstruction is most consistent with thisdiagnosis. Even though a peritonsillarabscess causes sore throat and fever,it rarely results in significant airwaycompromise, especially in an adult, andis even more rarely a cause of death.A peritonsillar abscess in its naturalhistory will usually rupture and selfdrainprior to causing upper airwayobstruction. As an otolaryngologist, Ihave seen many patients return to theEmergency Room in extremis a fewhours after being diagnosed with acutepharyngitis and sent home on oral antibiotics,to undergo emergency treatmentfor acute epiglottitis.I thank Drs. Choby and Goldenbergfor their interesting presentation.Elias Hilal, MD(AΩA, American University of Beirut,1970)Chief, Division of Otolaryngology—Head &Neck SurgeryUPMC MercyPittsburgh, PennsylvaniaE-mail: eliashilal@msn.com51 <strong>The</strong> <strong>Pharos</strong>/<strong>Winter</strong> <strong>2012</strong>
We sold all the furniture (of course lamps went first)And are left sifting through dim rooms of inventory• Old Halloween costumes (and all of my clothes and all of his clothes)• Harrison’s, Bates’, Sapira, Nuland, non-medical books• Piles of dirty scrubs, piles of clean scrubs, all other piles• Business cards for various restaurants we have loved in the cityEvening: we sort by the light of laptop screens.Our apartment collapses into discrete shippable units.Our French press, bread maker, fruit parer become Kitchen BoxOur two-person tent, camping stove, hiking boots become Activities BoxOur African masks, Brooklyn Bridge print, Quechua tapestry become Art BoxA photograph of our life is filtered, pointillized,<strong>The</strong> finer points brushed into smudges, mere suggestions of our world<strong>The</strong>se last four years.Sarah Buckley, MDDr. Buckley is an Internal Medicine resident at the University of Washington Medical Center. Her e-mail address is: sarahbbb@gmail.com.Illustration by Laura Aitken
“the last master of resounding song, thegracious mouth by which music spoke hasceased to be.”—Vienna, March 26, 1827physician to the Maestro in his last illness?into the depths of the man.Had he only followed them!<strong>The</strong>n, the apologies. I knew it all.Beethoven knew too well these tappingsonly palliative.“You are dying. Whom should I call for?”Next day, he was gone.notes fading into darkness.Richard Bronson, MDDr. Bronson (AΩA, New York University, 1966) is Professor of Obstetrics & Gynecology and Pathology at Stony Brook UniversityMedical Center and a member of the editorial board of <strong>The</strong> <strong>Pharos</strong>. His address is: Stony Brook University Medical Center, T9-080, StonyBrook, New York 11794-8091. E-mail: richard.bronson@sbumed.org.
Presenting the AΩA scarfPresenting the AΩA scarfAΩA's new scarf highlights the society's insignia, based on the shapeof the manubrium sterni. <strong>The</strong> center medallion features the <strong>Pharos</strong>lighthouse of Alexandria, one of the seven wonders of the ancientworld, for which AΩA's journal is named. <strong>The</strong> borders are stylizedDNA strands.Scarves are 35 x 35 inches, of 12 m/m silk twill with handrolled hems. Fourcolorways are available as shown: red/black, turquoise/purple, peach/mint,and navy/lavender. Scarf design by J&J Designs of San Francisco.$65To order, send a check for $65 to: <strong>Alpha</strong> <strong>Omega</strong> <strong>Alpha</strong>, 525 Middlefield Road, Suite 130, Menlo Park, CA 94025Or order online at www.alphaomegaalpha.org/store.html (Price includes shipping and handling)