Strategic Indicators Report: Results - Ontario Hospital Association
Strategic Indicators Report: Results - Ontario Hospital Association
Strategic Indicators Report: Results - Ontario Hospital Association
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Data AvailabilityQuarterlyBaseline25% in the 2009/2010 fiscal year (57% good/very good and 18% poor/fair)TargetsYear 1 (March 31, 2011) – 25% of patients rating overall quality in ER as excellentYear 2 (March 31, 2012) – 30% of patients rating overall quality in ER as excellentYear 3 (March 31, 2013) – 35% of patients rating overall quality in ER as excellentSupporting Strategies and ActivitiesAn ER Patient Satisfaction Performance Improvement Advisory Committee has been convened to advise andassist the OHA and the MOHLTC with an ER patient satisfaction performance improvement strategy. TheMinistry funded strategy and partnership to improve patient satisfaction in the ER has been extended untilMarch 31, 2012 and includes a worldwide review of leading practices, educational sessions and a toolkit.The strategy is also now more closely aligned with Health Quality <strong>Ontario</strong> as they work to support hospitalswith their QIPs.<strong>Results</strong><strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 4 of 24
Indicator 2: Patient SafetyOverviewIndicator: <strong>Hospital</strong> Standardized Mortality Ratio (HSMR), All CasesRationale: Rigorously validated by the Canadian Institute for Health Information (CIHI) and publicly reported,HSMR can help support efforts to improve patient safety and quality of care by providing a starting point toassess mortality rate and identify areas for improvement, which may help to reduce deaths from adverseevents.Baseline: 73% of reportable hospitals with a one-year rate decrease from 2007-08 to 2008-093-Year Target: 90% of reportable hospitals with a rate decrease since 2008-09Indicator Definition and CalculationRatio of actual (observed) deaths to expected deaths, adjusted for several factors that affect in-hospitalmortality, including age, sex, length of stay, admission category, diagnosis group, comorbidity and transferfrom another acute care institution. An HSMR equal to 100 suggests that there is no difference between alocal mortality rate and the average national experience, given the types of patients cared for. An HSMRgreater or less than 100 suggests that a local mortality rate is higher or lower than the national experience,respectively.Numerator: Observed deaths, or actual number of in-hospital deaths that occurred in a hospital or region.Denominator: Expected deaths, or number of deaths that would have occurred in a hospital or region had themortality of these patients been the same as the mortality of similar patients across the country, based on thereference year (2004-2005).OHA Calculation of Baseline and <strong>Results</strong>Calculation for Percent of <strong>Report</strong>able <strong>Hospital</strong>s with a Rate Decrease:Numerator = Total Number of <strong>Hospital</strong>s with a Negative Change in HSMR from 2008-09 to Current YearDenominator = Total Number of <strong>Report</strong>able <strong>Hospital</strong>sNotes:Calculations are for HSMR (All Cases)Most Recent HSMR refers to most recent HSMR score available since 2008-09Oldest HSMR refers to the oldest HSMR score available since 2008-09Change in HSMR for a <strong>Hospital</strong> = Most Recent HSMR – Oldest HSMR<strong>Report</strong>able <strong>Hospital</strong>s refers to hospitals with at least two HSMR scores reported between 2008-09 and 2010-11<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 5 of 24
Data SourceCIHI, <strong>Hospital</strong> Standard Mortality Ratio, 2009, 2010, 2011 and 2012The 2009 HSMR public release is the third release of HSMRs for eligible hospitals and regions across Canada byCIHI. It includes HSMR All Cases results for 2004-2005, 2005-2006, 2006-2007, 2007-2008 and 2008-2009. Since the HSMR measure was first developed and disseminated by CIHI, many hospitals and healthproviders across Canada began using it as part of their ongoing efforts to improve care.Data AvailabilityAnnualBaseline73% of reportable hospitals with a rate decrease since 2008-09TargetsYear 1 (2009-10) – 73% of reportable hospitals with a rate decrease since 2008-09Year 2 (2010-11) – 85% of reportable hospitals with a rate decrease since 2008-09Year 3 (2011-12) – 90% of reportable hospitals with a rate decrease since 2008-09Supporting Strategies and ActivitiesThe OHA is currently reviewing existing supports provided or previously provided to help hospitals with HSMRwith the intent of identifying the various initiatives most likely to impact HSMR. This includes consideringthe adapting of an American <strong>Hospital</strong> <strong>Association</strong> resource on this issue.<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 6 of 24
<strong>Results</strong>Change in HSMR 2007-2008 2008-2009 2009-2010Rate Decrease 22 29 28No Change 1 3 3Rate Increase 14 8 10Total <strong>Report</strong>able<strong>Hospital</strong>s37 40 41Change in HSMR 2007-2008 2008-2009 2009-2010Rate Decrease 59% 73% 68%No Change 3% 8% 7%Rate Increase 38% 20% 24%<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 7 of 24
Indicator 3: Wait Times in Emergency RoomOverviewIndicator: 90th percentile time spent in ER for complex conditions – Admitted PatientsRationale: Due to the lack of available inpatient beds, patients are housed in the ER while waiting for a bed tobecome available. Significant progress on this issue is required to make significant improvement on overallER wait times and improved patient flow.Baseline: 31.4 hours as of March 20103-Year Target: 20.0 hours as of March 2013Indicator Definition and Calculation90th percentile time spent in ER for complex conditions requiring more time for diagnosis, treatment or hospitalbed admission – Admitted PatientsThe amount of time a patient spends in the Emergency Room is referred to as “Total Time Spent in the ER” andis measured from the time patients register or initially see a triage nurse, until the time they leave the ER.The time patients leave the ER may be when they are sent home after being treated or when they areadmitted to a hospital bed, if medically necessary.Time Spent in ER is measured by subtracting the triage time or registration time from "time patient left ER" andis the maximum amount of time in which 9 out of 10 patients have completed their ER visit. The data isbased on ER visits completed for the most current time period at the 126 hospital sites across <strong>Ontario</strong>, thatare submitting ER data to the National Ambulatory Care <strong>Report</strong>ing System (NACRS).OHA Calculation of Baseline and <strong>Results</strong>None requiredData SourceMinistry of Health and Long-Term Care Website, <strong>Ontario</strong> Wait Times, Health Care Professionals, ProvincialSummary of Time Spent in ERData AvailabilityMonthly<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 8 of 24
Baseline31.4 hours as of March 2010TargetsYear 1 (March 2011) – 27.6 hoursYear 2 (March 2012) – 23.8 hoursYear 3 (March 2013) – 20.0 hoursTargets based on decrease of 3.8 hours each year and one-third reduction by Year 3Supporting Strategies and ActivitiesCommittees• QUARTERLY: Member of the MOHLTC ER-ALC Expert Panel• CEO is a member of the MOHLTC Emergency Room Task ForceEducational EventsProjects• ONGOING: Educational Services support for MOHLTC ER Performance Improvement Programworkshops• AUG 12-10: Physician Time to Assessment & Improving Admit Flow - Webcast• OCT 13-10: Reducing ED Wait Times: Building on Momentum and Operationlizing Best Practices -Conference.• NOV 2010: ER-ALC Session at HealthAchieveCOMPLETED: Living Lab Survey – MOHLTC Inventory of Leading Practices/Readmissions• OHA explored the development of business case opportunities pertaining to the North York General<strong>Hospital</strong> Emergency Department Diversion Project• ONGOING: OHA staff participating in the MOHLTC’s Emergency Services Definition & StandardsWork GroupDevelopment of Evidence-Based Information• Monthly: OHA ALC/ER Survey and <strong>Results</strong> shared with stakeholders and LHINs• Monthly: CEO is a member of the Data Certification Council<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 9 of 24
Status and Communications• Monthly: OHA Bulletins/Tom Talks (To members/stakeholders)• Developed a site on oha.com where:ooMonthly posting: ALC <strong>Results</strong> (including ER) are posted monthlyQuarterly posting: OHA ALC <strong>Results</strong> and MOHLTC/CCO ER Wait Times by LHIN<strong>Results</strong><strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 10 of 24
Advancing an Integrated Health SystemIndicator 4: Number of Alternate Level of Care (ALC) PatientsOverviewIndicator: Total (acute + non-acute) ALC patients in hospitalRationale: The major operational factor causing long emergency room wait times is the high number of ALCpatients occupying acute care hospital beds, making it difficult to admit patients from the ER. Reduced ALCdays will result in a cost-effective shift of services to the community and better expected clinical outcomesfor patients as they move into more appropriate environments.Baseline: 4,926 ALC patients3-Year Target: 2,781 ALC patientsIndicator Definition and CalculationNumber of ALC cases on waitlist - All LHINsOHA Calculation of Baseline and <strong>Results</strong>None requiredData SourceALC Data:Cancer Care <strong>Ontario</strong>, Access-to-Care Informatics• Number of ALC Cases on Waitlist• Provincial Monthly Alternate Level of Care Highlights <strong>Report</strong>Bed Data to Set 3-Year Target:Ministry of Health and Long-Term Care WERS and Daily Census bed dataData AvailabilityMonthly<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 11 of 24
Baseline4,689 patients as of March 2010TargetsYear 1 (March 2011) – 4,053 ALC patientsYear 2 (March 2012) – 3,417 ALC patientsYear 3 (March 2013) – 2,781 ALC patientsTarget reduction based on government acute care target of 9.6%Supporting Strategies and ActivitiesCommittees• QUARTERLY: Member of the MOHLTC ER-ALC Expert Panel• COMPLETED: ER-ALC Rehab-CCC Expert Panel (Subcommittee of the ER-ALC Expert Panel)• QUARTERLY: CCO WTIP ALC Advisory Committee• BI-MONTHLY: ALC Business Intelligence Advisory CommitteeEducational EventsProjects• NOV 2010: ER-ALC Session at HealthAchieve• DEC 9-10: Patient Safety Transitions in Care Summit: Improving the Patient Journey and ReducingReadmissions - Conference• DEC 14-10 - Managing Transitions: LTCHA Requirements – Webcast (Joint with OHA andOACCAC)• APRIL 28-10: ALC and Specialty Populations Roundtable (Facilitated by OHA and hosted byMOHLTC)• JUNE 16/17-11: A Call to Action on ER/ALC: Promoting Effective Care Across the HealthContinuum – Conference• JUNE 28-11: ALC Learning Collaborative – Roundtable (Facilitated by OHA and hosted byMOHLTC)• COMPLETED: Living Lab Survey – MOHLTC Inventory of Leading Practices/Readmissions• OHA and OACCAC explored a business case study for increased community resources to reduceER/ALC Waits in conjunction with Hamilton Health Sciences Centre and HNHB CCAC<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 12 of 24
Development of Evidence-Based Information• Monthly: OHA ALC Survey and <strong>Results</strong> shared with stakeholders and LHINs• Monthly: CEO is a member of the Data Certification CouncilStatus and Communications• Monthly: OHA Bulletins/Tom Talks (To members/stakeholders)• Developed a site on oha.com where:ooMonthly posting: ALC <strong>Results</strong> (including ER) are posted monthlyQuarterly posting: OHA ALC <strong>Results</strong> and MOHLTC/CCO ER Wait Times by LHIN<strong>Results</strong><strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 13 of 24
Indicator 5: Health Information Technology AdoptionOverviewIndicator: HIMSS Analytics Electronic Medical Record Adoption ModelSM (EMRAM) Score for <strong>Ontario</strong>Acute <strong>Hospital</strong> CorporationsRationale: Advancements in the adoption of e-Health technology is a necessary precursor to making significantgains in the areas of integration, better outcomes and efficiency.Baseline: 19 acute hospitals advance at least one EMRAM stage from Q4 2009 to Q3 20103-Year Target: 50% of acute hospitals (61) advance at least one EMRAM stage since Q4 2009Indicator Definition and CalculationElectronic Medical Record Adoption ModelSM (EMRAM) score tracks hospitals progress along the 8-stagecontinuum toward creating a paperless patient record environment.Self-reported data on the status of implementation across numerous clinical technologies and applications areapplied to a methodology that generates a hospital index score between 0 and 7. The methodology assignspoints for achievement of “live and operational” status on individual technologies on an eight-stage linearpath to having a fully-electronic medical record. The EMRAM methodology is proprietary to HIMSSAnalytics. <strong>Hospital</strong> results are audited before the highest two stages (6 and 7) are awarded.• All application capabilities within each stage must be operational before that stage can be achieved.• All lower stages must have been achieved before a higher level will be considered as achieved.• A hospital can achieve Stages 3-6 if it has met all of the application requirements for a single patientcare service (e.g. single nursing floor, cardiology service).Using the rules above, additional points are given for the implementation of applications in stages higher than theone fully achieved by the healthcare organization. In this fashion, other implementation paths than thoseprescribed by the stages can be taken into consideration for correlation with quality and financial research.OHA Calculation of Baseline and <strong>Results</strong>A count of the number of Acute <strong>Hospital</strong> Corporations up one or more stage(s)Data SourceOHA eHealth Technologies and Applications Inventory, Q4 2009, 2010, 2011, 2012OHA eHealth Technologies and Applications Inventory provides individual acute hospital scores on adoptionranging from Stages 0 to 7. <strong>Ontario</strong> hospital EMRAMSM score data is collected by the OHA. December2009 (Q4) scores currently exist for hospitals representing over 90% of <strong>Ontario</strong>’s hospital beds. OHA has arobust approach to ongoing data collection and reporting. Data was used in 2010 <strong>Ontario</strong> Health QualityCouncil (OHQC) <strong>Report</strong> and can be compared to results from the rest of Canada and in the US.<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 14 of 24
Data AvailabilityEMRAMSM scores are generated and provided to <strong>Ontario</strong> hospitals on a quarterly basis throughout the calendaryear. Q4 scores will be available in February each year.BaselineQ4, 2009HIMSSAnalyticsEMRAMStageAcute<strong>Hospital</strong>s (Q42009)Acute<strong>Hospital</strong>s(Q32010)ChangeStage 0 25.4% 18.9% -6.6%Stage 1 8.2% 4.1% -4.1%Stage 2 24.6% 27.0% 2.5%Stage 3 38.5% 40.2% 1.6%Stage 4 3.3% 9.8% 6.6%Stage 5 0.0% 0.0% 0.0%Stage 6 0.0% 0.0% 0.0%Stage 7 0.0% 0.0% 0.0%# of Acute <strong>Hospital</strong> Corporationsup one or more stage(s)19(15.6%)# of Acute <strong>Hospital</strong> Corporations 122TargetsYear 1 (Q4 2010) – 20 hospitals advanced at least one stage since Q4 2009Year 2 (Q4 2011) – 40 hospitals advanced at least one stage since Q4 2009Year 3 (Q4 2012) – 61 hospitals advanced at least one stage since Q4 2009Targets based on 1/3 of 50% of hospital corporations (approximately 20) advanced at least one stage each yearSupporting Strategies and ActivitiesProvide quarterly benchmarking and peer comparisons and improve measurement, strategic planning and goalsetting through the following online tools:• eHealth Technologies & Applications Inventory (online data entry interface)• eHealth Applications Viewer (online data portal)• <strong>Hospital</strong>-specific status reports made available each quarter• Quarterly communications/marketing and one-on-one efforts<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 15 of 24
Work with Small, Rural and Northern (SRN) Provincial Leadership Council and SRN hospitals to identifybarriers and solutions to advance adoption among typically the lowest performers.Election advocacy planning: Encourage government to act as a strategic investor of provider-level eHealthAdvocate for removal of hospital accounting (HAPS and cost per weighted case) disincentives to eHealthinvestment.<strong>Results</strong><strong>Ontario</strong> Acute <strong>Hospital</strong>s Comparison (Q4, 2011)<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 16 of 24
Indicator 6: Expenditures in Community SettingsOverviewIndicator: Annual percentage change in Community Care Access Centre (CCAC) and Community MentalHealth and Addictions (CMH&A) provincial government expenditures per capita.Rationale: Enhancing community expenditures in specific targeted areas will facilitate a cost effective shift ofservices resulting in a positive impact expected in terms of hospital utilization (hospital beds, ALC days,length of stay, cost) and better care for patients.Baseline: $ 201.18 Per Capita Community Expenditures at 2009/10 Year End3-Year Target: $239.81 Community Expenditures at 2012/13 Year EndIndicator Definition and CalculationAnnual percentage change in Community Care Access Centre (CCAC) and Community Mental Health AndAddictions (CMH&A) provincial government expenditures per capitaPer Capita CCAC Expenditures = (CCAC Total Revenue – CCAC Non-MOHLTC Global Revenue) / <strong>Ontario</strong>PopulationPer Capita CMH&A Expenditures = (CMH&A Total Revenue – CMH&A Non-MOHLTC Global Revenue) /<strong>Ontario</strong> PopulationOHA Calculation of Baseline and <strong>Results</strong>Calculation of BaselineBaseline = $201.18 for 2009/10 Fiscal YearCalculation of Annual Percentage ChangeNumerator: Per Capita Community Expenditures in Current Year – Per Capita Community Expenditures inPrevious YearDenominator: Per Capita Community Expenditures in Previous YearNotes:Per Capita Community Expenditures = Per Capita (CCAC Expenditures + CMH&A Expenditures)CCAC Expenditures = CCAC Total Revenue – CCAC Non-MOHLTC Global RevenueCMH&A Expenditures = CMH&A Total Revenue – CMH&A Non-MOHLTC Global Revenue<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 17 of 24
Data SourceExpenditures DataMinistry of Health and Long-Term Care (MOHLTC), Health Data Branch, Information Management Unit,Healthcare Indicator Tool (HIT Tool)Community Care Access Centres (CCAC New) - Global <strong>Indicators</strong>, ProvinceIndicator ID 1 - Total RevenueIndicator ID 6 - % Non-MOHLTC Global RevenueCommunity Mental Health And Addictions (CMH&A) - Global <strong>Indicators</strong>Indicator ID 1 - Total RevenueIndicator ID 6 - % Non-MOHLTC Global RevenueThe HIT Tool was created to assist <strong>Ontario</strong> Healthcare Service Providers. The information contained is accurateas presented in the databases. Data is used as submitted. Therefore any existing Data Quality issues haveneither been adjusted nor corrected by the MOHLTC.Consumer Price Index Data (used in calculation of targets)Statistics Canada, Consumer Price Index, Table 9-6, The Consumer Price Index, major components, selectedsub-groups and special aggregates, provinces, Whitehorse and Yellowknife, not seasonally adjusted —<strong>Ontario</strong>Percentage Change from March to March, each yearPopulation DataMinistry of Finance as reported in the 2011 <strong>Ontario</strong> Budget.Data AvailabilityAnnualBaseline$141.49 Per Capita CCAC Expenditures+ 59.69 Per Capita CMH&A Expenditures$ 201.18 Per Capita Community Expenditures at 2009/10 Year EndTargetsYear 1 (2010/11) – $215.46 (Baseline plus actual 3.6% CPI + 3.5%, total of 7.1% increase)Year 2 (2011/12) – $227.31 (Year 1 plus estimated 5.5% increase)Year 3 (2012/13) – $239.81 (Year 2 plus estimated 5.5% increase)Calculation of Targets:Targets based on 3.5% annual increase plus estimated 2% inflation (Bank of Canada target). Actual Target willbe calculated using 3.5% plus actual inflation rate. Actual Inflation Rate = Percentage Change in CPI fromMarch to March each year.<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 18 of 24
Supporting Strategies and ActivitiesProjects• Increase in community investment included in election platform jointly produced with the OACCAC• <strong>Strategic</strong> advocacy efforts include consistent and frequent messaging of needed community investmentsin pre-budget submissions and ongoing liaison with government staff and officials• COMPLETED: Living Lab Survey – MOHLTC Inventory of Leading Practices/Readmissions• Development of a Business Case: HHS and HNHB CCAC• OHA explored the development of business case opportunities pertaining to the North York General<strong>Hospital</strong> Emergency Department Diversion ProjectDevelopment of Evidence-Based Information• Monthly: OHA ALC/ER Survey and <strong>Results</strong> shared with stakeholders and LHINs• Monthly: CEO is a member of the Data Certification CouncilStatus and Communications• Monthly: OHA Bulletins/Tom Talks (To members/stakeholders)Educational Events -Nov/Dec 2010 - 2011• Dec 2010: Transitions in Care Summit• Dec 14-10 - Webcast OHA and OACCAC - Managing Transitions: LTCHA Regulations• February 2011 - Conference with OHA and OACCAC on Managing Transitions<strong>Results</strong>Community Expenditures$240$230$227.31$239.81Per Capita$220$210$215.46$201.18 $207.14$200Baseline(2009/10)Year 1 (2010/11) Year 2 (2011/12) Year 3 (2012/13)Target $215.46 $227.31 $239.81Actual $201.18 $207.14<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 19 of 24
Optimising Health Human ResourcesIndicator 7: Staff EngagementOverviewIndicator: Overall Staff Engagement ScoreRationale: Recognized indicator of a healthy workplaceBaseline and Target: To be established within 3 years. As no provincial-wide standardized assessment currentlyexists, no baseline exists and its use as a strategic plan evaluation indicator is limited. However, given therecognized importance of staff engagement and its relationships to quality of care and patient experience,OHA is committing to the implementation of a standardized staff engagement assessment tool and willestablish the baseline and future target within the 2010–2013 <strong>Strategic</strong> Plan timeframe.Indicator Definition and CalculationA single score measure of employee engagement. Employee engagement integrates the constructs of jobsatisfaction and organizational commitment. Two job satisfaction items, when combined with the 3commitment items plus an item rating the organization as a place to work will provide a robust overallmeasure of engagement in a multi-item scale. First wave data will allow validation of multi-scaleengagement measure.OHA Calculation of Baseline and <strong>Results</strong>To Be DeterminedData SourceOHA-NRC Picker Employee Experience Survey indicatorsKey survey questions that will contribute to the score:1. I am proud to tell others I am part of this organization.2. I find that my values and the organization’s values are similar.3. This organization really inspires the very best in me in the way of job performance.4. Overall, how satisfied are you with your current job?5. How frequently do you look forward to going to work?6. Overall, how would you rate ____ as a place to work?The scale will first be validated and statistics techniques will involve confirmatory factor analysis and reliabilityscaling.<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 20 of 24
Data AvailabilityAnnuallyBaselineTBD through assessment of first wave data in 2011TargetsYear 1 (2011) – Baseline prediction established from first wave participantsYear 2 (2012) – Assess engagement results from minimum of 50% of member organizations (note: organizationstypically survey every two years, so comparative information will be in Year 4)Year 3 (2013) – Assess ongoing engagement resultsSupporting Strategies and ActivitiesCurrent State• Work with Ministry of Health and Long-Term Care to establish that the survey or subsets of itsindicators fulfill Excellent Care for All Act (ECFAA) requirements. OHA facilitating meeting with theMinistry of Health and Health Quality <strong>Ontario</strong> to establish common strategic path for thestandardization of employee and physician surveying and advice to hospitals on short term QIPapproaches.• Competitive pricing: lowest common price point available to sector; group benefits plan membersoffered further discount.• Promote quality and performance improvement capacities of the comprehensive assessment.• OHA Quality Healthcare Workplace Framework including model and progressive awards program• Discussions to ensure a subset of common indicators meet Accreditation Canada requirements as theyupgrade their mandatory Worklife Pulse tool.<strong>Results</strong>The goal is to define the calculation of the indicator and have the baseline in about 18 months.<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 21 of 24
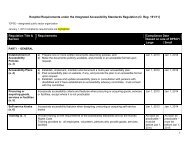
Leading Governance ExcellenceIndicator 8: Adoption of Governance Leading Practices for QualityOverviewIndicator: Time spent by hospital Board on discussing quality issues (full Board meetings)Rationale: This measure is to support the accepted correlation between time spent discussing quality at theboard level, and a board’s focus on quality improvement. It also reflects the recognized need to enhanceboard performance in patient safety and quality.Baseline: 20% of a full board meeting spent on discussing quality issues3-Year Target: 25% of a full board meeting spent on discussing quality issuesIndicator Definition and CalculationThe provincial average of the average percent of a board meeting spent of quality andpatient safety by each hospital.OHA Calculation of Baseline and <strong>Results</strong>Provincial Average Calculation:Numerator = Σ (Average Percent of a Board Meeting Spent on the Quality and Patient Safety Issue forResponse Category * Number of <strong>Hospital</strong>s in Response Category)Denominator = NNotes:Response Categories for Average Percent of a Board Meeting Spent on the Quality and Patient Safety Issue: 0%,5%, 10%, 15%, 20%, 25%, 30%, 35%, 40%, 45%, 50%, More Than 50%, Don’t Know (Note: “More than50%” is counted as “50%” in calculation)N = Total Number of <strong>Hospital</strong> Responses – Total Number of “Don’t Know” ResponsesData SourceOHA/GCE Governance Survey, Question 7.2: On average, approximately what percentage of a board meetingis spent on the quality and patient safety issue?The OHA, along with its Governance Centre of Excellence (GCE) released the 2010 OHA/GCE GovernanceSurvey in May 2010. The 2010 survey builds on baseline information on governance policies and practicesof hospital boards collected in the 2007 survey. The survey also helps measure the progress hospital boardshave made in the uptake of leading practices in a broad range of areas, and provide members the opportunityto share and detail their governance issues and challenges.<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 22 of 24
Data AvailabilityOHA/GCE Governance Survey, June 2010 and June 2012Possible annual mini survey on governance and qualityBaseline20% of a full board meeting spent on discussing quality issues in 2010TargetsThe 25% target is accepted international leading practice (Institute for Healthcare Improvement’s 5 MillionLives Campaign; OHA’s Quality and Patient Safety: Understanding the Role of the Board (2008))Year 1 (2011) – Data possibly available from mini surveyYear 2 (2012) – 25% (based on 2012 OHA/GCE Governance survey)Year 3 (2013) – 25%Supporting Strategies and ActivitiesOHA/OHQC Patient Safety and Quality Governance Toolkit:The OHA and <strong>Ontario</strong> Health Quality Council (OHQC) have partnered to create an online patient safety andquality governance toolkit which will be hosted on the GCE’s website. This effort is supported by theworking group of OHA members (Board Chairs, CEOs, Directors of Patient Safety) and was launched inJune, 2011.Effective Governance for Quality and Patient Safety – Regional Series:To help hospitals meet the legislative requirements of the Excellent Care For All Act (ECFAA), the CanadianPatient Safety Institute (CPSI), Canadian Health Services Research Foundation (CHSRF) and the OHApartnered with the <strong>Ontario</strong> Ministry of Health and Long-Term Care to help equip hospital leaders with theskills and tools required to drive the principles of quality and patient safety throughout <strong>Ontario</strong>’s hospitals.The Effective Governance for Quality and Patient Safety program offered hospital boards the opportunity toexplore evidence-informed approaches to governance and leadership, and to share innovative healthgovernance practices, resources and tools.These education sessions, funded by the Government of <strong>Ontario</strong>, offered a unique and comprehensive curriculumthat supports <strong>Ontario</strong> hospital boards in their ongoing efforts to improve governance in the area of qualityand patient safety. Sessions were held at six locations throughout the province in spring of 2011.Updates to OHA/GCE Governance Publications:Certain OHA/GCE governance publications are scheduled to be updated in 2011 to reflect new legislatedrequirements for quality and patient safety. This includes, but is not limited to, the new Guide to GoodGovernance, OHA Prototype By-Laws and Compliance Framework. Starting in 2011, GCE educationalprogramming and the GCE website will also be updated to reflect the increased oversight responsibilitiesboards now have of quality and patient safety issues.”Into the future, the OHA GCE will be redesigning its business plan to further strengthen efforts to elevate healthsystem governance. Quality improvement will be a key element of this undertaking.<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 23 of 24
<strong>Results</strong><strong>Results</strong> also to be reported by hospital type, OHA Region, and LHINOriginal Survey <strong>Results</strong>CalculationsA B C D EAverage Percent of aBoard Meeting Spent onthe Quality and PatientSafety IssueNumberof<strong>Hospital</strong>sAverage Percent of aBoard Meeting Spent onthe Quality and PatientSafety IssueNumberof<strong>Hospital</strong>sProvincial Average of theAverage Percent of a BoardMeeting Spent on Quality andPatient Safety IssueE = (C * D)/1260% 0 0% 0 05% 13 5% 13 6510% 24 10% 24 24015% 19 15% 19 28520% 21 20% 21 42025% 18 25% 18 45030% 13 30% 13 39035% 6 35% 6 21040% 4 40% 4 16045% 1 45% 1 4550% 2 50% 3 150*More than 50% 1**Don't Know 2n 124**N =122 2415mode (62) 20% 19.8047/12425% or higher (37.9%)* One response of “More than 50%” is counted as “50%”** N = 126 (three “Don’t Know” responses were excluded from calculations)<strong>Strategic</strong> <strong>Indicators</strong>: June 2011 -- Page 24 of 24