Plan Year 7/1/11 - 6/30/12 Plan Facts Cost
Plan Year 7/1/11 - 6/30/12 Plan Facts Cost
Plan Year 7/1/11 - 6/30/12 Plan Facts Cost
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
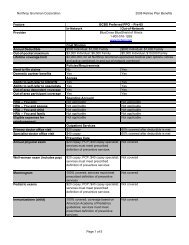
Annual Rx out-of-pocket maximumRetail genericRetail formulary brandRetail nonformulary brandMail order genericMail order formulary brandMail order nonformulary brandOral contraceptivesFertility drugsNot applicableIn NetworkNot applicableOut of NetworkNot applicableIn Network$7 copay; <strong>30</strong> day supply; participating pharmaciesonlyOut of Network80% covered; after $7 copay; <strong>30</strong> day supplyIn Network$<strong>30</strong> copay; <strong>30</strong> day supply; participating pharmaciesonlyOut of Network80% covered; after $<strong>30</strong> copay; <strong>30</strong> day supplyIn Network$<strong>30</strong> copay; plus $35 cost-sharing charge for nonformularydrug; participating pharmacies only; <strong>30</strong> daysupplyOut of Network80% covered; after $<strong>30</strong> copay and $35 cost-sharingcharge for non-formulary drug$<strong>11</strong> copay; 90 day supply$65 copay; 90 day supply$170 copay; 90 day supplyIn NetworkRetail and mail order available; applicable prescriptiondrug formulary and copays apply; check with <strong>Plan</strong> fordetailsOut of NetworkRetail available only; applicable prescription drugformulary and copays apply; check with <strong>Plan</strong> fordetailsIn NetworkCheck with <strong>Plan</strong> for detailsOut of NetworkCheck with <strong>Plan</strong> for detailsCoverageHMSA PPOAnnual physical examWell-woman exam (includes pap)In NetworkNot covered; health assessment available only throughthe HealthPass program; HealthPass screenings 100%covered; check with <strong>Plan</strong> for detailsOut of NetworkNot coveredIn Network100% coveredOut of Network
MammogramColonoscopyCancer screeningsCardiovascular screeningsAllergy tests and treatments70% coveredIn Network100% coveredOut of Network70% covered; deductible does not applyIn Network90% coveredOut of Network70% coveredIn NetworkCheck with <strong>Plan</strong> for detailsOut of NetworkCheck with <strong>Plan</strong> for detailsIn NetworkCheck with <strong>Plan</strong> for detailsOut of NetworkCheck with <strong>Plan</strong> for detailsIn Network80% coveredOut of Network70% coveredFertility servicesIn vitro fertilizationArtificial inseminationFemale tubal ligationMale vasectomyIn Network90% covered; limited to one IVF procedure perlifetime; preauthorization required; diagnosis andtreatment of infertility not coveredOut of Network70% covered; limited to one IVF procedure perlifetime; preauthorization required; diagnosis andtreatment of infertility not coveredIn Network90% covered; limited to one procedure per lifetime;eligibility criteria and limitations apply; check with <strong>Plan</strong>for detailsOut of Network70% covered; limited to one procedure per lifetime;eligibility criteria and limitations apply; check with <strong>Plan</strong>for detailsIn NetworkNot coveredOut of NetworkNot coveredIn Network90% coveredOut of Network70% coveredIn Network90% coveredOut of Network
70% coveredOffice visit: Pre/postnatalIn-hospital delivery servicesNewborn nursery servicesIn Network$<strong>12</strong> copay; initial visit onlyOut of Network70% coveredIn Network90% coveredOut of Network70% coveredIn Network90% coveredOut of Network70% coveredPediatric examsImmunizations (child)Mental Health: Combined with substance abuseMental Health: Outpatient coverageMental Health: Inpatient coverageBehavioral health member servicesBehavioral health vendorBehavioral health Web siteIn Network100% covered; through age 5Out of Network70% covered; through age 5; deductible does notapplyIn Network100% covered; through age 5Out of Network100% covered; through age 5; deductible does notapplyIn NetworkNoOut of NetworkNoIn Network$<strong>12</strong> copayOut of Network70% coveredIn Network90% covered; facility; $<strong>12</strong> copay for physicianOut of Network70% coveredSame as medical planSame as medical planSame as medical planDetox: Outpatient coverageDetox: Inpatient coverageIn Network$<strong>12</strong> copayOut of Network70% coveredIn Network
Rehab: Outpatient coverageRehab: Inpatient coverage90% covered; facility; $<strong>12</strong> copay for physicianOut of Network70% coveredIn Network$<strong>12</strong> copayOut of Network70% coveredIn Network90% covered; facility; $<strong>12</strong> copay for physicianOut of Network70% coveredDental implantsAccidental injury to teethSurgical removal of tumors, cysts, and impacted teethIn NetworkNot coveredOut of NetworkNot coveredIn Network90% covered; check with <strong>Plan</strong> about details forlimitations to oral surgeryOut of Network70% covered; check with <strong>Plan</strong> about details forlimitations to oral surgeryIn Network90% covered; removal of impacted teeth not coveredOut of Network70% covered; removal of impacted teeth not coveredRoutine vision examsRegular lenses and framesContact lensesIn NetworkNot coveredOut of NetworkNot coveredIn NetworkNot coveredOut of NetworkNot coveredIn NetworkNot coveredOut of NetworkNot coveredHearing evaluationsHearing aidsIn Network90% coveredOut of Network70% coveredIn Network
80% covered; limited to one hearing aid per ear everyfive years; digital aids limited to no more than theamount <strong>Plan</strong> would pay for analog aidsOut of Network70% covered; limited to one hearing aid per ear everyfive years; digital aids limited to no more than theamount <strong>Plan</strong> would pay for analog aidsAcupunctureChiropracticOutpatient physical therapyIn NetworkNot coveredOut of NetworkNot coveredIn NetworkNot coveredOut of NetworkNot coveredIn Network80% covered; must be medically necessary; checkwith <strong>Plan</strong> for details about benefit maximumsOut of Network70% covered; must be medically necessary; checkwith <strong>Plan</strong> for details about benefit maximumsOutpatient speech therapyOutpatient occupational therapyIn Network80% covered; must be medically necessary; limited toshort-term only; check with <strong>Plan</strong> for details aboutbenefit maximumsOut of Network70% covered; must be medically necessary; limited toshort-term only; check with <strong>Plan</strong> for details aboutbenefit maximumsIn Network80% covered; must be medically necessary; checkwith <strong>Plan</strong> for details about benefit maximumsOut of Network70% covered; must be medically necessary; checkwith <strong>Plan</strong> for details about benefit maximumsNoncustodial home health careIn Network100% covered; limited to 150 visits per calendar yearOut of Network70% covered; limited to 150 visits per calendar yearPrescribed care in noncustodial skilled nursing facilityIn Network90% covered; limited to <strong>12</strong>0 days per calendar yearOut of Network70% covered; limited to <strong>12</strong>0 days per calendar year
Hospice careIn Network100% coveredOut of NetworkNot coveredAmbulance servicesProsthetic devices80% covered; in-network; 70% covered out-ofnetworkIn Network90% coveredOut of Network70% coveredAccessOut-of-area dependent coverageOut-of-area participant coverageDomestic partner benefitsHMSA PPOYesYesYesEase of UseAbility to self-refer to OB/GYNAbility to self-refer to specialistsHMSA PPOYesYesMember SatisfactionHMSA PPOHealth plan averageNational average 88%Not availableHealth plan averageNational average 94%Not availableHealth plan averageNational average 90%Not availableHealth plan averageNational average 89%Not availableCare Management: Education and AssistanceHMSA PPOAsthma care managementCancer care managementDiabetes care managementHeart disease care managementHypertension care managementSmoking cessation programYesNoYesYesNoYes
Weight control programPrenatal care managementYesYesThe comparison charts are compiled using information that applies to a large number of health plan users andis commonly reported by the health plans. Depending on the chart type, such as charts for dental and visionplans, certain information and/or sections won't appear because the necessary data isn't available. If you havequestions about a topic that isn't covered in the charts, refer to the plan's SPD or contact the health provider'smember services department for additional information. Also, keep in mind that the information on access andquality of care is provided by the health plans. Neither Northrop Grumman nor Hewitt Associates is responsiblefor the accuracy of this information. If there is a discrepancy between the information displayed on thesecharts and the official plan documents, the official plan documents will control. Northrop Grumman reservesthe right to amend, suspend, or terminate the plan(s) or program(s) at any time.