open access atlas of otolaryngology, head & neck operative surgery
open access atlas of otolaryngology, head & neck operative surgery
open access atlas of otolaryngology, head & neck operative surgery
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
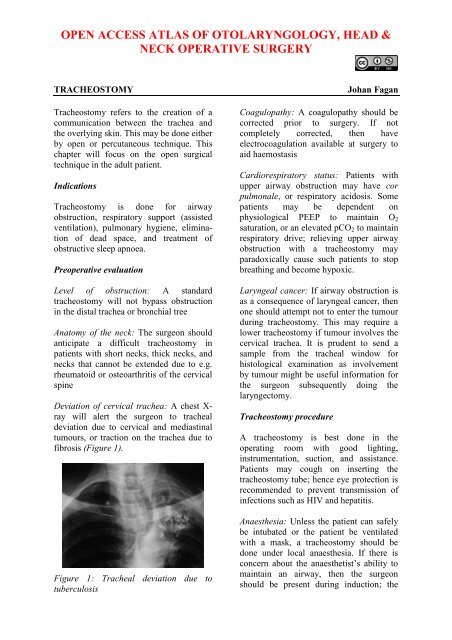
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD &NECK OPERATIVE SURGERYTRACHEOSTOMYTracheostomy refers to the creation <strong>of</strong> acommunication between the trachea andthe overlying skin. This may be done eitherby <strong>open</strong> or percutaneous technique. Thischapter will focus on the <strong>open</strong> surgicaltechnique in the adult patient.IndicationsTracheostomy is done for airwayobstruction, respiratory support (assistedventilation), pulmonary hygiene, elimination<strong>of</strong> dead space, and treatment <strong>of</strong>obstructive sleep apnoea.Pre<strong>operative</strong> evaluationLevel <strong>of</strong> obstruction: A standardtracheostomy will not bypass obstructionin the distal trachea or bronchial treeAnatomy <strong>of</strong> the <strong>neck</strong>: The surgeon shouldanticipate a difficult tracheostomy inpatients with short <strong>neck</strong>s, thick <strong>neck</strong>s, and<strong>neck</strong>s that cannot be extended due to e.g.rheumatoid or osteoarthritis <strong>of</strong> the cervicalspineDeviation <strong>of</strong> cervical trachea: A chest X-ray will alert the surgeon to trachealdeviation due to cervical and mediastinaltumours, or traction on the trachea due t<strong>of</strong>ibrosis (Figure 1).Figure 1: Tracheal deviation due totuberculosisJohan FaganCoagulopathy: A coagulopathy should becorrected prior to <strong>surgery</strong>. If notcompletely corrected, then haveelectrocoagulation available at <strong>surgery</strong> toaid haemostasisCardiorespiratory status: Patients withupper airway obstruction may have corpulmonale, or respiratory acidosis. Somepatients may be dependent onphysiological PEEP to maintain O 2saturation, or an elevated pCO 2 to maintainrespiratory drive; relieving upper airwayobstruction with a tracheostomy mayparadoxically cause such patients to stopbreathing and become hypoxic.Laryngeal cancer: If airway obstruction isas a consequence <strong>of</strong> laryngeal cancer, thenone should attempt not to enter the tumourduring tracheostomy. This may require alower tracheostomy if tumour involves thecervical trachea. It is prudent to send asample from the tracheal window forhistological examination as involvementby tumour might be useful information forthe surgeon subsequently doing thelaryngectomy.Tracheostomy procedureA tracheostomy is best done in theoperating room with good lighting,instrumentation, suction, and assistance.Patients may cough on inserting thetracheostomy tube; hence eye protection isrecommended to prevent transmission <strong>of</strong>infections such as HIV and hepatitis.Anaesthesia: Unless the patient can safelybe intubated or the patient be ventilatedwith a mask, a tracheostomy should bedone under local anaesthesia. If there isconcern about the anaesthetist’s ability tomaintain an airway, then the surgeonshould be present during induction; the
skin, s<strong>of</strong>t tissue and trachea (into thelumen) should be infiltrated with localanaesthesia with adrenaline beforeinduction; and a set <strong>of</strong> tracheostomyinstruments should be set out beforeinduction <strong>of</strong> anaesthesia so that anemergency tracheostomy can be done ifrequired.Positioning and draping: The patient isplaced in a supine position with <strong>neck</strong>extended by a pillow or sandbag placedunder the shoulders in order to deliver thetrachea out <strong>of</strong> the thorax and to give thesurgeon adequate <strong>access</strong> to the cervicaltrachea. Such extension may not bepossible in patients with <strong>neck</strong> injuries, orrheumatoid and osteoarthritis <strong>of</strong> thecervical spine. Some patients withimpending airway obstruction may nottolerate a recumbent position; thetracheotomy may then be done with thepatient in a sitting position with <strong>neck</strong>extended. The skin <strong>of</strong> the anterior <strong>neck</strong> andchest is sterilised and the <strong>neck</strong> draped. Ifthe tracheostomy is being done under localanaesthesia, the face should not becovered.Surface landmarks: The tracheostomy iscreated below the 1 st tracheal ring, so as toavoid subglottic stenosis as a result <strong>of</strong>scarring. Therefore palpating to determinethe location <strong>of</strong> the cricoid cartilage isimportant. When you run your fingers upthe midline <strong>of</strong> the <strong>neck</strong> starting inferiorlyat the sternal notch, you 1 st encounterprominence <strong>of</strong> the thyroid isthmus,followed by the cricoid.Figure 2: Minimum set <strong>of</strong> instrumentsSkin incision: A horizontal incision ismade one fingerbreadth below the cricoidprominence. This is cosmeticallypreferable to a vertical midline incision.The incision is carried through the skin andthe subcutaneous tissue. Note that theplatysma is generally absent in the midline.Take care not to transect the anteriorjugular veins, which are just superficial tothe strap muscles within the investingcervical fascia, and can be preserved andretracted laterally (Figure 3). Theremainder <strong>of</strong> the dissection should remainstrictly in the midline in a vertical planeto avoid injury to the inferior thyroid veins.Minimum instruments: A minimum set <strong>of</strong>instruments is demonstrated in Figure 2.Figure 3: Exposure <strong>of</strong> anterior jugularveins and cervical fascia2
Infrahyoid strap muscles: Figure 4illustrates the infrahyoid strap muscles.Thyroid cartilageCricoid cartilageThyroid glandSternohyoid muscleSternothyroid muscleFigure 4: Infrahyoid strap musclesIdentify the midline cervical fascial planebetween the sternohyoid muscles. Dividethis intermuscular plane by spreading witha pair <strong>of</strong> scissors. Repeat this manoeuvre toseparate the sternothyroid muscles, andretract the muscles laterally (Figure 5).The trachea and cricoid can now bepalpated.Figure 5: Retracting sternohyoid andsternothyroid muscles to expose thethyroid glandThyroid isthmus: The thyroid isthmusoverlies the 2 nd /3 rd tracheal rings. Theisthmus should be retracted superiorly toexpose the trachea (Figure 6). Only veryrarely does the thyroid isthmus need to bedoubly clamped, divided, and (suture)ligated.Figure 6: Thyroid retracted superiorly andan inferiorly based flap cut (along redlines) in anterior tracheal wallExpose trachea: The infrathyroid tracheais exposed anteriorly by carefully partingoverlying s<strong>of</strong>t tissues with a pair <strong>of</strong>scissors, taking care not to tear the inferiorthyroid veins. Ensure that the surgical fieldis dry before proceeding, as it is difficult toachieve haemostasis once the tracheostomytube has been inserted. Should there bedoubt about the location <strong>of</strong> the trachea, orthere be concern it being confused with thecarotid artery, aspirating air with a needleattached to a syringe will confirm itslocation.Create tracheostoma: In the wake patient,lignocaine may again be injected intotracheal lumen prior to incising the tracheaand inserting the tube in order to reducecoughing. Upward traction may be appliedto a tracheal hook inserted under a trachealring to stabilise the trachea and deliver itfrom the chest. The safest means to createa tracheostomy in adults is by creating aninferiorly based flap raised from theanterior wall <strong>of</strong> the 3 rd and 4 th trachealrings. A silk traction suture is passedthrough this anterior tracheal flap andloosely secured to the skin (Figure 7).Traction on the suture facilitatesreinsertion <strong>of</strong> the tracheostomy tube incase <strong>of</strong> accidental decannulation.3
Alternately one may remove an anteriorcartilage segment <strong>of</strong> the 2 nd , 3 rd or 4 thtracheal rings.<strong>neck</strong>, and tied, with the <strong>neck</strong> flexed. If theties are placed with the <strong>neck</strong> extended,they are too loose when the patient flexesthe <strong>neck</strong>.EpiglottisGlottisBack wall <strong>of</strong> tracheaInferiorly based trachealflapTraction sutureanchoring flapThyroid cartilageCricoidThyroid glandInnominate arterySternumFigure 8: Position <strong>of</strong> tracheostomy tubeFigure 7: Flap reflected inferiorly withtraction suture attached to flapInsertion <strong>of</strong> tracheostomy tube: Thesurgeon assesses the size <strong>of</strong> the trachea,and selects the largest sized cuffedtracheostomy tube that will comfortably fitthe tracheal lumen. Inject air into thetracheostomy inflatable cuff to test theintegrity <strong>of</strong> the cuff. Insert the introducerinto the tracheostomy tube. If the patienthas been intubated, the anaesthetist isasked to slowly withdraw the endotrachealtube, so that the tracheostomy tube can beinserted under direct vision. Advance thetube into the trachea while applyingtraction to the silk traction suture attachedto the tracheal flap. Ensure that the tubehas been inserted into the tracheal lumen,and not a false passage in the paratracheals<strong>of</strong>t tissues. Inflate the cuff, attach theanaesthetic tubing, and hand-ventilate untilone has confirmed correct placement <strong>of</strong> thetube within the trachea (Figure 8). Do notsuture the skin tightly around thetracheostomy tube, as this can promotesurgical emphysema.Securing the tracheostomy tube: Tapes arethreaded through the holes in the flanges <strong>of</strong>the tracheostomy tube, passed around theThe ties should be tight enough to admit nomore than a single finger under the tape(Figure 9).Figure 9: Tracheostomy tube secured withVelcro tapeIt is prudent to suture the tracheotomy tubeto the skin for the first few days to allowmaturation <strong>of</strong> the tracheocutaneous tract.The sutures can then be removed andtraditional tracheotomy tapes can then beused. Following free microvasculartransfer flap reconstruction, tracheostomytapes should be avoided; the tracheostomyshould preferably be sutured to thesuprastomal skin, as tracheal tapes maycause jugular vein compression,thrombosis, and venous outflowobstruction and flap failure.4
PitfallsHigh tracheostomy: It is important not toplace the tracheotomy above the 2 ndtracheal ring, as inflammation may causesubglottic oedema, chondritis <strong>of</strong> the cricoidcartilage, and subglottic stenosis.Low tracheostomy: A tracheotomy shouldnot be placed below the 4 th tracheal ringas:The distance between the skin and thetrachea increases inferiorly, whichmakes tracheal intubation moredifficultA low tracheostomy may compress anderode the innominate artery whichpasses between the manubrium sterniand the trachea (Figure 8). This maycause innominate artery erosion andfatal haemorrhage. This may bepreceded by a so-called “sentinelbleed”Paratracheal false tract: Inadvertentextratracheal placement <strong>of</strong> thetracheostomy tube can be fatal. It isrecognised by the absence <strong>of</strong> breath soundson auscultation <strong>of</strong> the lungs, highventilatory pressures, failure to ventilatethe lungs, hypoxia, absence <strong>of</strong> expiredCO 2 , surgical emphysema, and an inabilityto pass a suction catheter down thebronchial tree, and on chest X-ray.Surgical emphysema, pneumomediastinum,and pneumothorax: Injury to the pleuraldomes is more likely to occur in children,struggling patients and patients on positivepressure ventilation. It can be complicatedby a tension pneumothorax. Henceauscultation <strong>of</strong> the chest and a CXR shouldbe performed after tracheostomy,especially in ventilated patients. Surgicalemphysema may also be promoted bysuturing the tracheostomy wound aroundthe tracheostomy tube.Airway fire: Do not enter the trachea withdiathermy, as this may cause an airway firein a patient being ventilated with a highconcentration <strong>of</strong> oxygen.Choice <strong>of</strong> Tracheostomy TubeA variety <strong>of</strong> tube designs and materials areavailable. The choice <strong>of</strong> tube shouldconform to the indication for which it is tobe used. All tubes should have an innercannula; this can safely be removed andcleaned without a need to remove the outercannula and hence endanger the airway.The following factors may influence thechoice <strong>of</strong> tube:Tube diameter: Because airway resistanceis related to the 4 th power <strong>of</strong> the radiuswith laminar flow, and the 5 th power <strong>of</strong> theradius with turbulent flow, it is importantto select a tube that that fits the tracheasnugly. A range <strong>of</strong> sizes should beavailable. It also underscores theimportance <strong>of</strong> keeping the tube clean, asaccumulation <strong>of</strong> mucus increases airwayresistance not only by reducing thediameter, but also by causing turbulent airflow.Tracheal seal: A cuffed, plastictracheostomy tube is used to create a sealwith the trachea in patients on positivepressure ventilation, and with freshtracheostomy wounds (Figure 10) toprevent saliva or blood entering the lowerairways. The cuffed tube may be replacedwith an uncuffed tube, either plastic ormetal (Figure 11) in patients who do notrequire positive pressure ventilation oncethe tract between the skin and the tracheahas become well defined by granulationtissue at 48hrs, and tracheostomal bleedinghas settled.5
curvature to conform to the stoma and thetrachea.Figure 10: Plastic low pressure cuffedtracheostomy tube with outer cannula,inner cannula and introducer (L to R)Figure 12: Tracheostomy tube withadjustable flangeNeck Flange: The <strong>neck</strong> flange shouldconform to the shape <strong>of</strong> the <strong>neck</strong> and fitsnugly against the skin to avoid excessivetube movement, accidental decannulation,and s<strong>of</strong>t tissue trauma.Tube material: Metal tubes are thinnerwalled, and hence have a better ratio <strong>of</strong>outer to inner wall diameter, therebyoptimising airway resistance.Figure 11: Metal tracheostomy tube withouter cannula, inner cannula andintroducer (L to R)Tube length: Patients with very thick <strong>neck</strong>scan be fitted with a tracheostomy tube witha flange that can be adjusted up or downthe shaft <strong>of</strong> the tube (Figure 12). Tubelength may also need to be adjusted whenthe carina is close to the tracheostoma orwith tracheal stenosis or tracheamalaciadistal to the tracheostoma that needs tostented by the tube. Chest and <strong>neck</strong> X-raysare <strong>of</strong> value to determine the requiredlength.Tube shape: Laryngectomy patientsrequire shorter tubes with a gentlerPhonation: Patients with uncuffed tubes orfenestrated tubes (Figure 13) can phonateby occluding the end <strong>of</strong> the tracheostomytube with a finger which permits air tobypass the tube and to pass through thelarynx.Figure 13: Fenestrated tracheostomy tube6
Speaking valves fitted to the ends <strong>of</strong>tracheostomy tubes are one-way valvesthat <strong>open</strong> on inspiration, but close onexpiration, thereby directing expired airthrough the larynx and permit hands-freespeech (Figure14).Figure 14: Speaking valve that fits onto theend <strong>of</strong> a tracheostomy tube and permitshands-free speechFenestrated tubes with speaking valves areparticularly well suited to patients withobstructive sleep apnoea, as they can havenormal speech by day with the valve inplace, but uncap the tracheostomy tube atnight to ensure unobstructed breathing.Post<strong>operative</strong> carePulmonary oedema: This may occurfollowing sudden relief <strong>of</strong> airwayobstruction and reduction in highintraluminal airway pressures. It may becorrected by CPAP or positive pressureventilation.Respiratory arrest: This may occurimmediately following insertion <strong>of</strong> thetracheostomy tube, and is attributed to therapid reduction in arterial pCO 2 followingrestoration <strong>of</strong> normal ventilation, andhence loss <strong>of</strong> respiratory drive.Humidification: Tracheostomy bypassesthe nose and upper aerodigestive tractwhich normally warms, filters, andhumidifies inspired air. To avoid trachealdesiccation and damage to the respiratorycilia and epithelium, and obstruction due tomucous crusting, the tracheostomy patientneeds to breathe humidified warm air bymeans <strong>of</strong> a humidifier, heat and moistureexchange filter, or a tracheostomy bib.Pulmonary Toilette: The presence <strong>of</strong> atracheostomy tube and inspiration <strong>of</strong> dryair irritates the mucosa and increasessecretions. Tracheostomy also promotesaspiration <strong>of</strong> saliva and food as tethering <strong>of</strong>the airway prevents elevation <strong>of</strong> the larynxduring swallowing. Patients are unable toclear secretions as effectively astracheostomy prevents generation <strong>of</strong>subglottic pressure, hence makingcoughing and clearing secretionsineffective; it also disturbs ciliary function.Therefore secretions need to be suctionedin an aseptic and atraumatic manner.Cleaning the tube: Airway resistance isrelated to the 4 th power <strong>of</strong> the radius withlaminar flow, and the 5 th power <strong>of</strong> theradius with turbulent flow. Therefore evena small reduction <strong>of</strong> airway diameterand/or conversion to turbulent airflow as aresult <strong>of</strong> secretions in the tube cansignificantly affect airway resistance.Therefore regular cleaning <strong>of</strong> the innercannula is required using a pipe cleaner orbrush.Securing the tube: Accidental decannulationand failure to quickly reinsert the tubemay be fatal. This is especiallyproblematic during the 1 st 48hrs when thetracheocutaneous tract has not matured andattempted reinsertion <strong>of</strong> the tube may becomplicated by the tube entering a falsetract. Therefore the tightness <strong>of</strong> thetracheostomy tapes should be regularlychecked. Traction sutures on the trachealflap facilitate reinsertion <strong>of</strong> thetracheotomy tube.Cuff pressures: When tracheostomy tubecuff pressures against the tracheal wallmucosa exceed 30cm H 2 0, mucosalcapillary perfusion ceases, ischaemicdamage ensues and tracheal stenosis mayresult. Mucosal injury has been shown to7
occur within 15 minutes. Therefore cuffinflation pressures <strong>of</strong> >25cm H 2 0 should beavoided. A number <strong>of</strong> studies havedemonstrated the inadequacy <strong>of</strong> manualpalpation <strong>of</strong> the pilot balloon as a means toestimate appropriate cuff pressures.Measures to prevent cuff related injuryinclude:Only to inflate the cuff if required(ventilated, aspiration)Minimal Occluding Volume Technique:Deflate the cuff, and then slowlyreinflate until one can no longer hearair going past the cuff with astethoscope applied to the side <strong>of</strong> the<strong>neck</strong> near the tracheostomy tube(ventilated patient)Minimal Leak Technique: The sameprocedure as above, except that oncethe airway is sealed, slowly towithdraw approximately 1ml <strong>of</strong> air sothat a slight leak is heard at the end <strong>of</strong>inspirationPressure gauge: Regular or continuousmonitoring <strong>of</strong> cuff pressuresAuthor & EditorJohan Fagan MBChB, FCORL, MMedPr<strong>of</strong>essor and ChairmanDivision <strong>of</strong> OtolaryngologyUniversity <strong>of</strong> Cape TownCape TownSouth Africajohannes.fagan@uct.ac.zaThe Open Access Atlas <strong>of</strong> Otolaryngology, Head &Neck Operative Surgery by Johan Fagan (Editor)johannes.fagan@uct.ac.za is licensed under a CreativeCommons Attribution - Non-Commercial 3.0 UnportedLicenseDecannulationThe tracheostomy tube can be removedonce the cause <strong>of</strong> the airway obstructionhas been resolved. If any doubt existsabout the adequacy <strong>of</strong> the airway, e.g.following pharyngeal or laryngeal <strong>surgery</strong>,then the tracheostomy tube is firstdownsized and plugged, so that the patientcan breathe freely past the tube. The tubeis then plugged. The patient should beunder close observation during this time,and may be monitored with pulseoximetry. If the patient can tolerate thetracheostomy tube being pluggedovernight, it can then be removed. Thetracheostomy wound is covered with anocclusive dressing, and generally healsover a matter a week.8